NUR251 S1 2018 Assessment 1: Chronic Kidney Disease Nursing Case Study
VerifiedAdded on 2023/06/15
|17
|4191
|169
Case Study
AI Summary
This case study provides a comprehensive nursing assessment and care plan for a patient, John Doe, with Chronic Kidney Disease (CKD). The assessment includes a physical examination focused on CKD risks, a renal examination to understand renal system functionality, and a nutritional status asse...
CASE STUDY NURSING
1
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
1
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Task 1
Nursing Assessment 1 – Physical examination for Chronic Kidney Disease
This physical examination is a level up from general physical examination process;
this examination is done for patients having a risk of chronic kidney failure (Urden, Stacy &
Lough, 2014). This involves assessing patient general condition, appetite, and weight
changes, past history, risk factors and nutritional status in each visit. Further, assessing pulse
and blood pressure in supine and upright position to check orthostatic changes and effect of
high blood pressure detected as vital sign of the patient. The patient skin should be evaluated
for determining signs of severe CKD (Harris, Nagy & Vardaxis, 2014).
The study patient, John is at high risk of kidney damage as per his vital signs,
therefore, this physical assessment would help to identify any minute sign of risk to the
kidney as well as determining best possible interventions for the care plan. Along with CKD,
this assessment will also help the nurse to determine any further risk of bacterial infection
and effect of high blood pressure in case of John. Planning nursing care without assessing
these physical factors can lead to the risk of developing severity in chronic condition as well
as the requirement of emergency (Gulanick & Myers, 2013).
Nursing Assessment 2 – Renal examination
Nurse need to perform a renal examination for understanding the renal system functionality.
This involves a subjective and objective data assessment by the registered nurse. The
subjective data assessment involves determining renal and urinary function by asking
questions to the patient and studying the provided patient report. This will help to determine
pain, urgency, burning, retention and incontinence of disease. Further, objective data
assessment involves determining overall appearance, abdominal inspection (kidney
enlargement or bladder detention), and determining abdominal bruit using a stethoscope and
regular observation of urinary outcome (Willis, Reynolds, & Keleher, 2016).
This assessment is required to determine the proper functionality of the renal system in case
of John having the high-risk symptoms of kidney damage like protein, blood in urine, high
BP etc. The renal examination is important to determine the risk to the renal system before
developing nursing interventions (Banks, 2013).
2
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
Nursing Assessment 1 – Physical examination for Chronic Kidney Disease
This physical examination is a level up from general physical examination process;
this examination is done for patients having a risk of chronic kidney failure (Urden, Stacy &
Lough, 2014). This involves assessing patient general condition, appetite, and weight
changes, past history, risk factors and nutritional status in each visit. Further, assessing pulse
and blood pressure in supine and upright position to check orthostatic changes and effect of
high blood pressure detected as vital sign of the patient. The patient skin should be evaluated
for determining signs of severe CKD (Harris, Nagy & Vardaxis, 2014).
The study patient, John is at high risk of kidney damage as per his vital signs,
therefore, this physical assessment would help to identify any minute sign of risk to the
kidney as well as determining best possible interventions for the care plan. Along with CKD,
this assessment will also help the nurse to determine any further risk of bacterial infection
and effect of high blood pressure in case of John. Planning nursing care without assessing
these physical factors can lead to the risk of developing severity in chronic condition as well
as the requirement of emergency (Gulanick & Myers, 2013).
Nursing Assessment 2 – Renal examination
Nurse need to perform a renal examination for understanding the renal system functionality.
This involves a subjective and objective data assessment by the registered nurse. The
subjective data assessment involves determining renal and urinary function by asking
questions to the patient and studying the provided patient report. This will help to determine
pain, urgency, burning, retention and incontinence of disease. Further, objective data
assessment involves determining overall appearance, abdominal inspection (kidney
enlargement or bladder detention), and determining abdominal bruit using a stethoscope and
regular observation of urinary outcome (Willis, Reynolds, & Keleher, 2016).
This assessment is required to determine the proper functionality of the renal system in case
of John having the high-risk symptoms of kidney damage like protein, blood in urine, high
BP etc. The renal examination is important to determine the risk to the renal system before
developing nursing interventions (Banks, 2013).
2
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
Nursing Assessment 3 – Assessing and monitoring nutritional status, BMI and
weight/height history
Assessment and monitoring of nutritional status will help to determine the food and fluid
balance for case study patient. As the provided information contains no information about the
nutritional status of the patient further followed by a medical order of food elevation (Banks,
2013). Therefore, the registered nurse needs to perform this assessment to gather information
on the nutritional status that will help to develop an effective nursing care plan. Further,
information on food and fluid balance will help to gain proper kidney functionality.
3
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
weight/height history
Assessment and monitoring of nutritional status will help to determine the food and fluid
balance for case study patient. As the provided information contains no information about the
nutritional status of the patient further followed by a medical order of food elevation (Banks,
2013). Therefore, the registered nurse needs to perform this assessment to gather information
on the nutritional status that will help to develop an effective nursing care plan. Further,
information on food and fluid balance will help to gain proper kidney functionality.
3
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
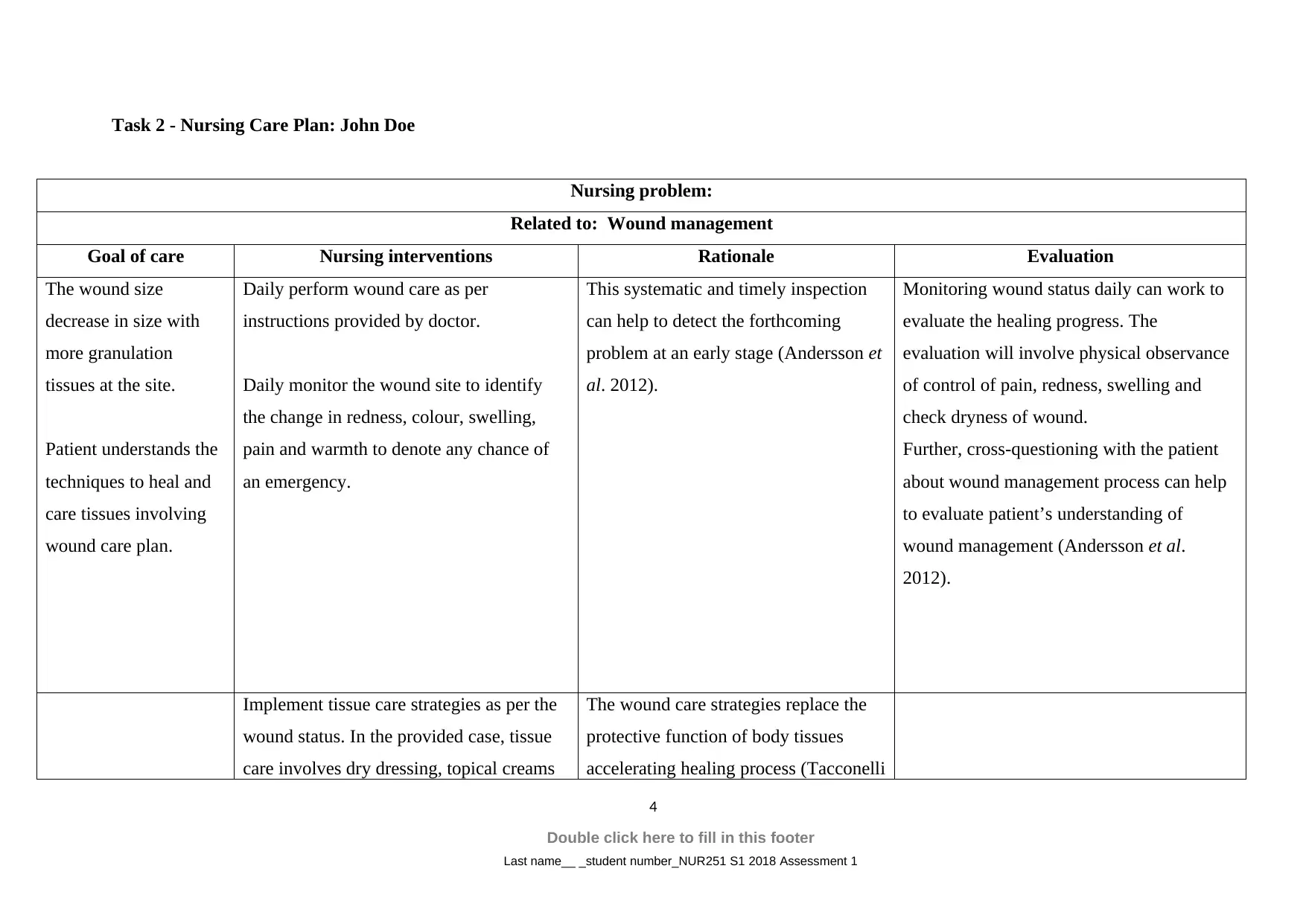
Task 2 - Nursing Care Plan: John Doe
Nursing problem:
Related to: Wound management
Goal of care Nursing interventions Rationale Evaluation
The wound size
decrease in size with
more granulation
tissues at the site.
Patient understands the
techniques to heal and
care tissues involving
wound care plan.
Daily perform wound care as per
instructions provided by doctor.
Daily monitor the wound site to identify
the change in redness, colour, swelling,
pain and warmth to denote any chance of
an emergency.
This systematic and timely inspection
can help to detect the forthcoming
problem at an early stage (Andersson et
al. 2012).
Monitoring wound status daily can work to
evaluate the healing progress. The
evaluation will involve physical observance
of control of pain, redness, swelling and
check dryness of wound.
Further, cross-questioning with the patient
about wound management process can help
to evaluate patient’s understanding of
wound management (Andersson et al.
2012).
Implement tissue care strategies as per the
wound status. In the provided case, tissue
care involves dry dressing, topical creams
The wound care strategies replace the
protective function of body tissues
accelerating healing process (Tacconelli
4
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
Nursing problem:
Related to: Wound management
Goal of care Nursing interventions Rationale Evaluation
The wound size
decrease in size with
more granulation
tissues at the site.
Patient understands the
techniques to heal and
care tissues involving
wound care plan.
Daily perform wound care as per
instructions provided by doctor.
Daily monitor the wound site to identify
the change in redness, colour, swelling,
pain and warmth to denote any chance of
an emergency.
This systematic and timely inspection
can help to detect the forthcoming
problem at an early stage (Andersson et
al. 2012).
Monitoring wound status daily can work to
evaluate the healing progress. The
evaluation will involve physical observance
of control of pain, redness, swelling and
check dryness of wound.
Further, cross-questioning with the patient
about wound management process can help
to evaluate patient’s understanding of
wound management (Andersson et al.
2012).
Implement tissue care strategies as per the
wound status. In the provided case, tissue
care involves dry dressing, topical creams
The wound care strategies replace the
protective function of body tissues
accelerating healing process (Tacconelli
4
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
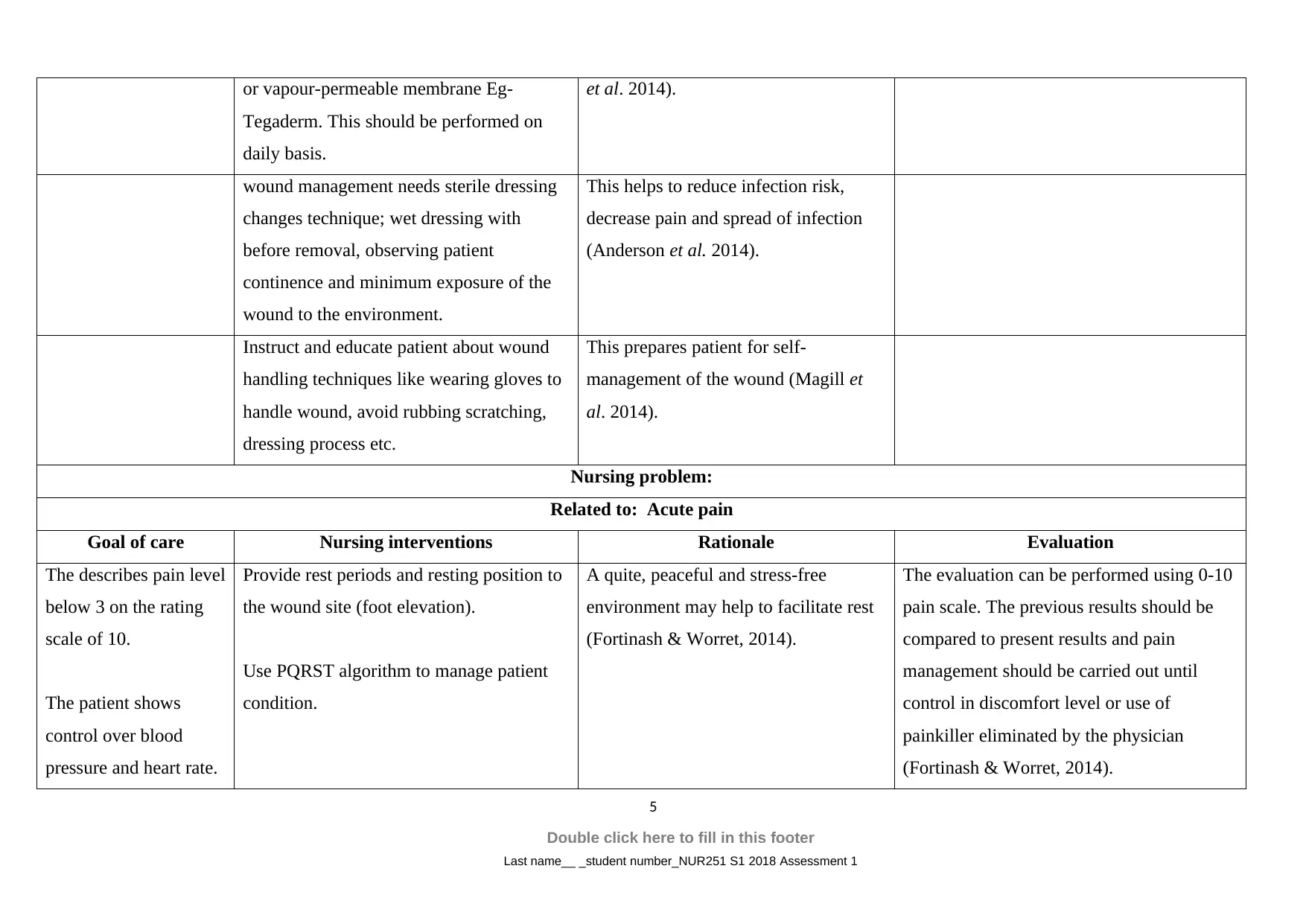
or vapour-permeable membrane Eg-
Tegaderm. This should be performed on
daily basis.
et al. 2014).
wound management needs sterile dressing
changes technique; wet dressing with
before removal, observing patient
continence and minimum exposure of the
wound to the environment.
This helps to reduce infection risk,
decrease pain and spread of infection
(Anderson et al. 2014).
Instruct and educate patient about wound
handling techniques like wearing gloves to
handle wound, avoid rubbing scratching,
dressing process etc.
This prepares patient for self-
management of the wound (Magill et
al. 2014).
Nursing problem:
Related to: Acute pain
Goal of care Nursing interventions Rationale Evaluation
The describes pain level
below 3 on the rating
scale of 10.
The patient shows
control over blood
pressure and heart rate.
Provide rest periods and resting position to
the wound site (foot elevation).
Use PQRST algorithm to manage patient
condition.
A quite, peaceful and stress-free
environment may help to facilitate rest
(Fortinash & Worret, 2014).
The evaluation can be performed using 0-10
pain scale. The previous results should be
compared to present results and pain
management should be carried out until
control in discomfort level or use of
painkiller eliminated by the physician
(Fortinash & Worret, 2014).
5
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
Tegaderm. This should be performed on
daily basis.
et al. 2014).
wound management needs sterile dressing
changes technique; wet dressing with
before removal, observing patient
continence and minimum exposure of the
wound to the environment.
This helps to reduce infection risk,
decrease pain and spread of infection
(Anderson et al. 2014).
Instruct and educate patient about wound
handling techniques like wearing gloves to
handle wound, avoid rubbing scratching,
dressing process etc.
This prepares patient for self-
management of the wound (Magill et
al. 2014).
Nursing problem:
Related to: Acute pain
Goal of care Nursing interventions Rationale Evaluation
The describes pain level
below 3 on the rating
scale of 10.
The patient shows
control over blood
pressure and heart rate.
Provide rest periods and resting position to
the wound site (foot elevation).
Use PQRST algorithm to manage patient
condition.
A quite, peaceful and stress-free
environment may help to facilitate rest
(Fortinash & Worret, 2014).
The evaluation can be performed using 0-10
pain scale. The previous results should be
compared to present results and pain
management should be carried out until
control in discomfort level or use of
painkiller eliminated by the physician
(Fortinash & Worret, 2014).
5
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
Patient eliminates the
use of painkiller
(Nuromol).
Use cognitive-behavioral techniques like
relaxation exercises, music therapy,
breathing exercises and distraction.
These techniques can help to distract
patient’s attention from pain
experiences (Davison et al. 2015).
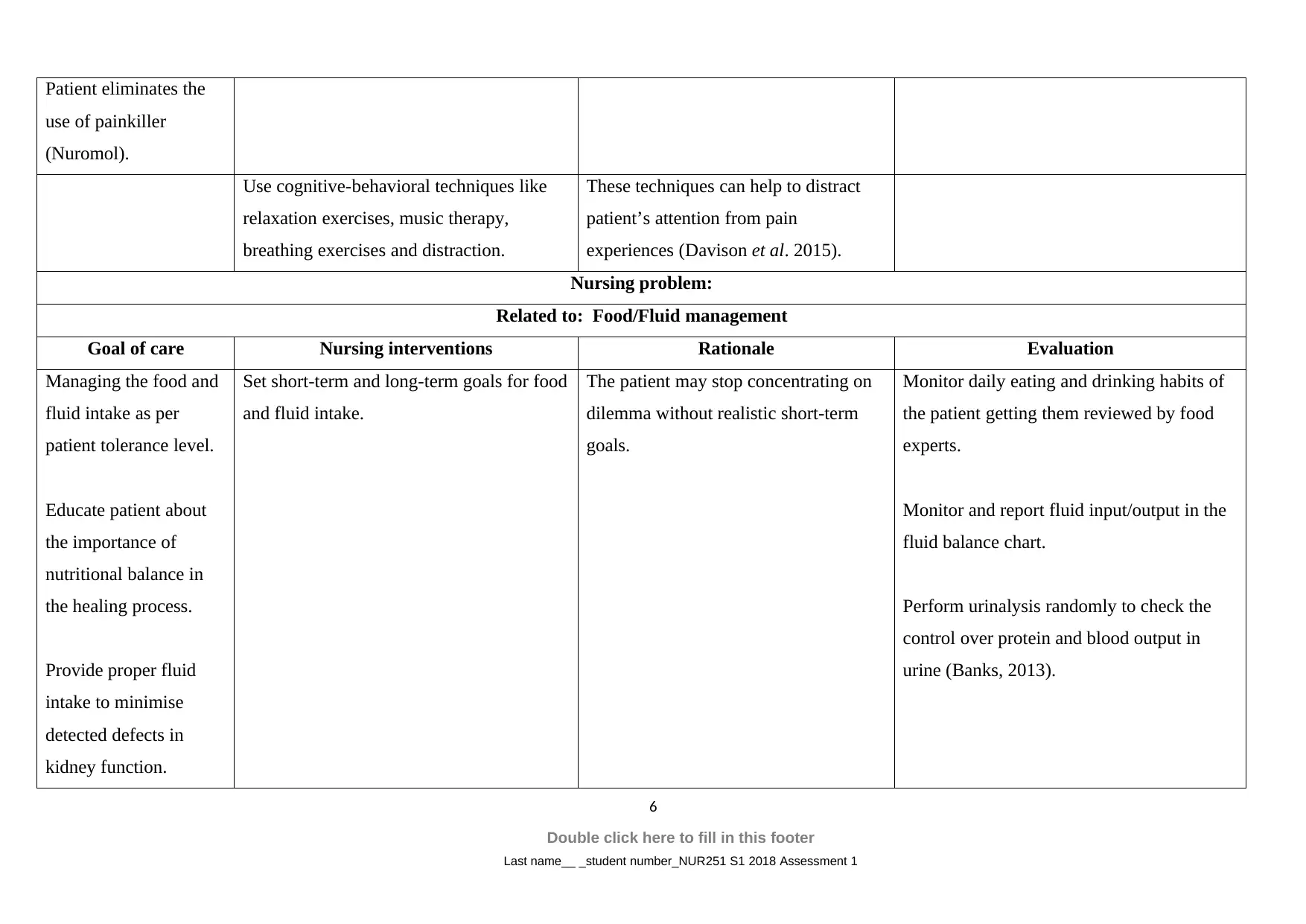
Nursing problem:
Related to: Food/Fluid management
Goal of care Nursing interventions Rationale Evaluation
Managing the food and
fluid intake as per
patient tolerance level.
Educate patient about
the importance of
nutritional balance in
the healing process.
Provide proper fluid
intake to minimise
detected defects in
kidney function.
Set short-term and long-term goals for food
and fluid intake.
The patient may stop concentrating on
dilemma without realistic short-term
goals.
Monitor daily eating and drinking habits of
the patient getting them reviewed by food
experts.
Monitor and report fluid input/output in the
fluid balance chart.
Perform urinalysis randomly to check the
control over protein and blood output in
urine (Banks, 2013).
6
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
use of painkiller
(Nuromol).
Use cognitive-behavioral techniques like
relaxation exercises, music therapy,
breathing exercises and distraction.
These techniques can help to distract
patient’s attention from pain
experiences (Davison et al. 2015).
Nursing problem:
Related to: Food/Fluid management
Goal of care Nursing interventions Rationale Evaluation
Managing the food and
fluid intake as per
patient tolerance level.
Educate patient about
the importance of
nutritional balance in
the healing process.
Provide proper fluid
intake to minimise
detected defects in
kidney function.
Set short-term and long-term goals for food
and fluid intake.
The patient may stop concentrating on
dilemma without realistic short-term
goals.
Monitor daily eating and drinking habits of
the patient getting them reviewed by food
experts.
Monitor and report fluid input/output in the
fluid balance chart.
Perform urinalysis randomly to check the
control over protein and blood output in
urine (Banks, 2013).
6
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
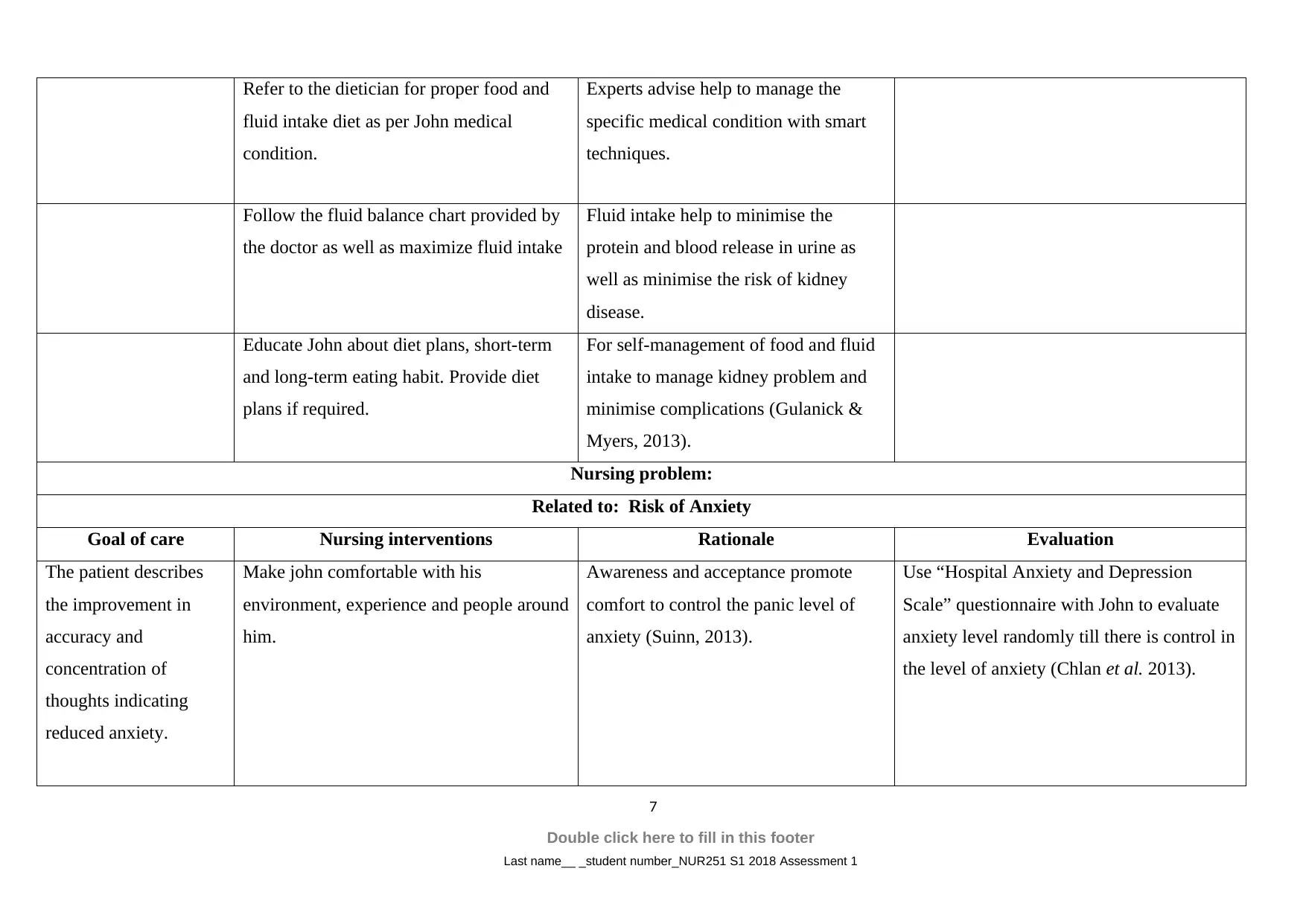
Refer to the dietician for proper food and
fluid intake diet as per John medical
condition.
Experts advise help to manage the
specific medical condition with smart
techniques.
Follow the fluid balance chart provided by
the doctor as well as maximize fluid intake
Fluid intake help to minimise the
protein and blood release in urine as
well as minimise the risk of kidney
disease.
Educate John about diet plans, short-term
and long-term eating habit. Provide diet
plans if required.
For self-management of food and fluid
intake to manage kidney problem and
minimise complications (Gulanick &
Myers, 2013).
Nursing problem:
Related to: Risk of Anxiety
Goal of care Nursing interventions Rationale Evaluation
The patient describes
the improvement in
accuracy and
concentration of
thoughts indicating
reduced anxiety.
Make john comfortable with his
environment, experience and people around
him.
Awareness and acceptance promote
comfort to control the panic level of
anxiety (Suinn, 2013).
Use “Hospital Anxiety and Depression
Scale” questionnaire with John to evaluate
anxiety level randomly till there is control in
the level of anxiety (Chlan et al. 2013).
7
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
fluid intake diet as per John medical
condition.
Experts advise help to manage the
specific medical condition with smart
techniques.
Follow the fluid balance chart provided by
the doctor as well as maximize fluid intake
Fluid intake help to minimise the
protein and blood release in urine as
well as minimise the risk of kidney
disease.
Educate John about diet plans, short-term
and long-term eating habit. Provide diet
plans if required.
For self-management of food and fluid
intake to manage kidney problem and
minimise complications (Gulanick &
Myers, 2013).
Nursing problem:
Related to: Risk of Anxiety
Goal of care Nursing interventions Rationale Evaluation
The patient describes
the improvement in
accuracy and
concentration of
thoughts indicating
reduced anxiety.
Make john comfortable with his
environment, experience and people around
him.
Awareness and acceptance promote
comfort to control the panic level of
anxiety (Suinn, 2013).
Use “Hospital Anxiety and Depression
Scale” questionnaire with John to evaluate
anxiety level randomly till there is control in
the level of anxiety (Chlan et al. 2013).
7
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
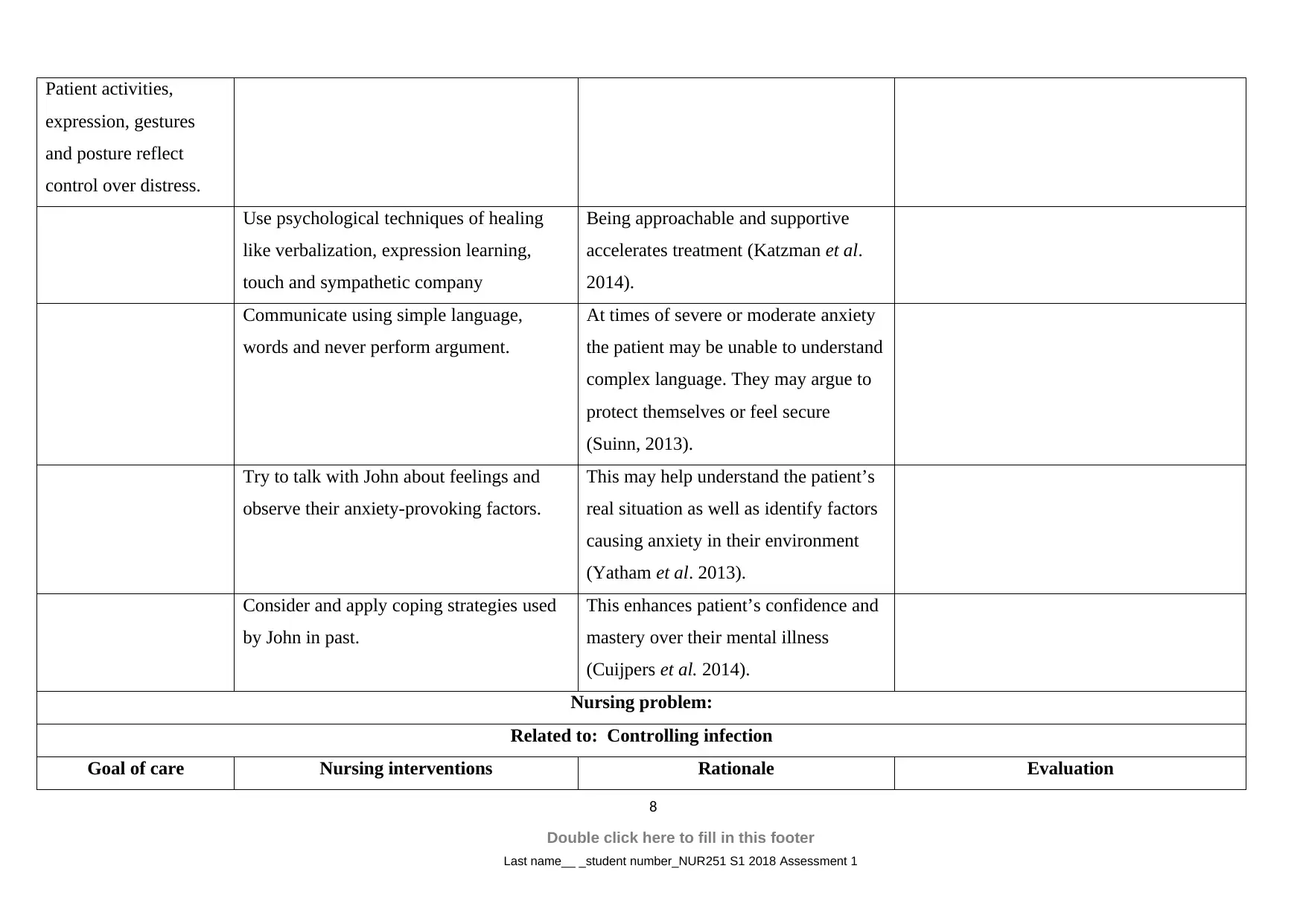
Patient activities,
expression, gestures
and posture reflect
control over distress.
Use psychological techniques of healing
like verbalization, expression learning,
touch and sympathetic company
Being approachable and supportive
accelerates treatment (Katzman et al.
2014).
Communicate using simple language,
words and never perform argument.
At times of severe or moderate anxiety
the patient may be unable to understand
complex language. They may argue to
protect themselves or feel secure
(Suinn, 2013).
Try to talk with John about feelings and
observe their anxiety-provoking factors.
This may help understand the patient’s
real situation as well as identify factors
causing anxiety in their environment
(Yatham et al. 2013).
Consider and apply coping strategies used
by John in past.
This enhances patient’s confidence and
mastery over their mental illness
(Cuijpers et al. 2014).
Nursing problem:
Related to: Controlling infection
Goal of care Nursing interventions Rationale Evaluation
8
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
expression, gestures
and posture reflect
control over distress.
Use psychological techniques of healing
like verbalization, expression learning,
touch and sympathetic company
Being approachable and supportive
accelerates treatment (Katzman et al.
2014).
Communicate using simple language,
words and never perform argument.
At times of severe or moderate anxiety
the patient may be unable to understand
complex language. They may argue to
protect themselves or feel secure
(Suinn, 2013).
Try to talk with John about feelings and
observe their anxiety-provoking factors.
This may help understand the patient’s
real situation as well as identify factors
causing anxiety in their environment
(Yatham et al. 2013).
Consider and apply coping strategies used
by John in past.
This enhances patient’s confidence and
mastery over their mental illness
(Cuijpers et al. 2014).
Nursing problem:
Related to: Controlling infection
Goal of care Nursing interventions Rationale Evaluation
8
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
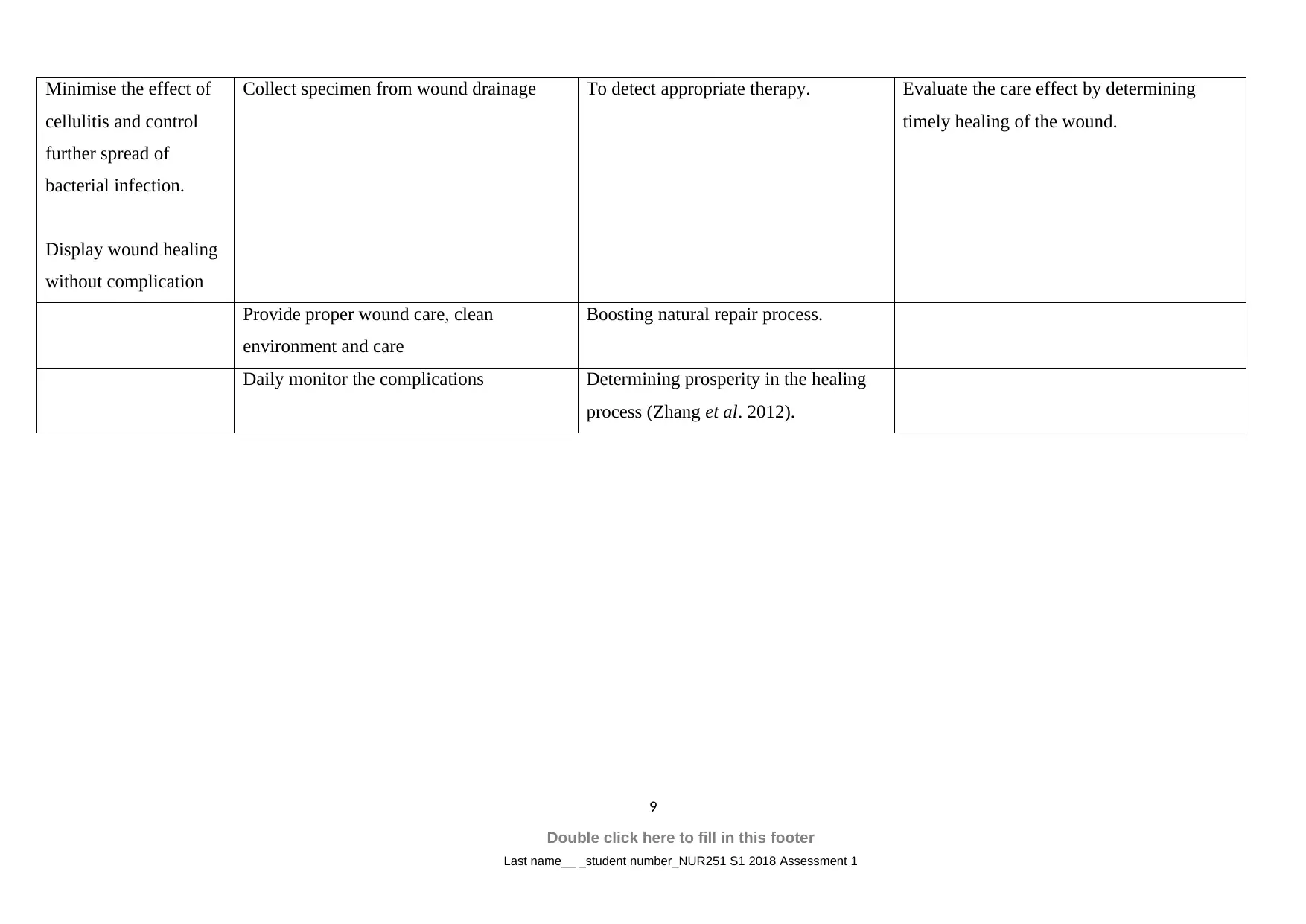
Minimise the effect of
cellulitis and control
further spread of
bacterial infection.
Display wound healing
without complication
Collect specimen from wound drainage To detect appropriate therapy. Evaluate the care effect by determining
timely healing of the wound.
Provide proper wound care, clean
environment and care
Boosting natural repair process.
Daily monitor the complications Determining prosperity in the healing
process (Zhang et al. 2012).
9
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
cellulitis and control
further spread of
bacterial infection.
Display wound healing
without complication
Collect specimen from wound drainage To detect appropriate therapy. Evaluate the care effect by determining
timely healing of the wound.
Provide proper wound care, clean
environment and care
Boosting natural repair process.
Daily monitor the complications Determining prosperity in the healing
process (Zhang et al. 2012).
9
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
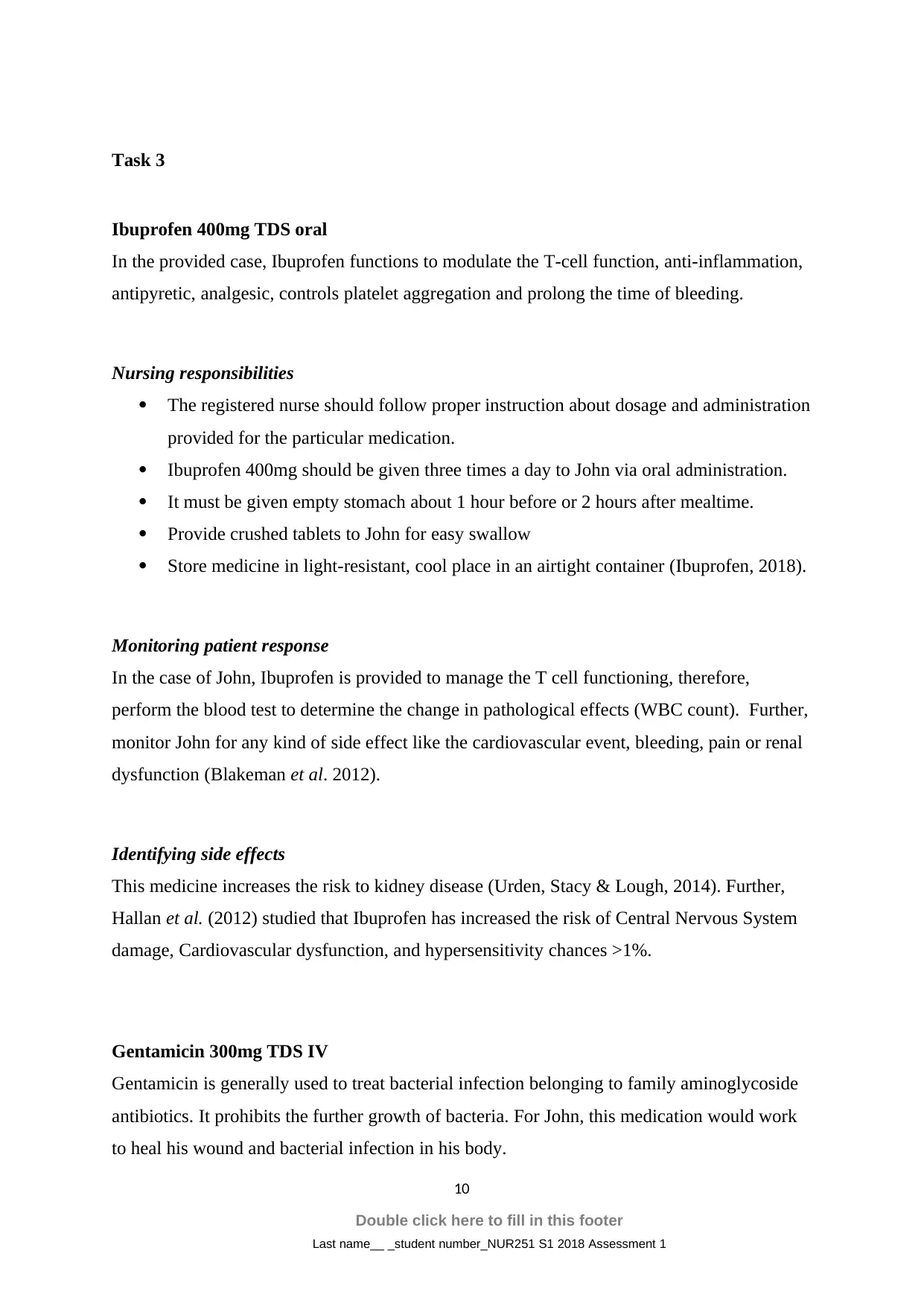
Task 3
Ibuprofen 400mg TDS oral
In the provided case, Ibuprofen functions to modulate the T-cell function, anti-inflammation,
antipyretic, analgesic, controls platelet aggregation and prolong the time of bleeding.
Nursing responsibilities
The registered nurse should follow proper instruction about dosage and administration
provided for the particular medication.
Ibuprofen 400mg should be given three times a day to John via oral administration.
It must be given empty stomach about 1 hour before or 2 hours after mealtime.
Provide crushed tablets to John for easy swallow
Store medicine in light-resistant, cool place in an airtight container (Ibuprofen, 2018).
Monitoring patient response
In the case of John, Ibuprofen is provided to manage the T cell functioning, therefore,
perform the blood test to determine the change in pathological effects (WBC count). Further,
monitor John for any kind of side effect like the cardiovascular event, bleeding, pain or renal
dysfunction (Blakeman et al. 2012).
Identifying side effects
This medicine increases the risk to kidney disease (Urden, Stacy & Lough, 2014). Further,
Hallan et al. (2012) studied that Ibuprofen has increased the risk of Central Nervous System
damage, Cardiovascular dysfunction, and hypersensitivity chances >1%.
Gentamicin 300mg TDS IV
Gentamicin is generally used to treat bacterial infection belonging to family aminoglycoside
antibiotics. It prohibits the further growth of bacteria. For John, this medication would work
to heal his wound and bacterial infection in his body.
10
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
Ibuprofen 400mg TDS oral
In the provided case, Ibuprofen functions to modulate the T-cell function, anti-inflammation,
antipyretic, analgesic, controls platelet aggregation and prolong the time of bleeding.
Nursing responsibilities
The registered nurse should follow proper instruction about dosage and administration
provided for the particular medication.
Ibuprofen 400mg should be given three times a day to John via oral administration.
It must be given empty stomach about 1 hour before or 2 hours after mealtime.
Provide crushed tablets to John for easy swallow
Store medicine in light-resistant, cool place in an airtight container (Ibuprofen, 2018).
Monitoring patient response
In the case of John, Ibuprofen is provided to manage the T cell functioning, therefore,
perform the blood test to determine the change in pathological effects (WBC count). Further,
monitor John for any kind of side effect like the cardiovascular event, bleeding, pain or renal
dysfunction (Blakeman et al. 2012).
Identifying side effects
This medicine increases the risk to kidney disease (Urden, Stacy & Lough, 2014). Further,
Hallan et al. (2012) studied that Ibuprofen has increased the risk of Central Nervous System
damage, Cardiovascular dysfunction, and hypersensitivity chances >1%.
Gentamicin 300mg TDS IV
Gentamicin is generally used to treat bacterial infection belonging to family aminoglycoside
antibiotics. It prohibits the further growth of bacteria. For John, this medication would work
to heal his wound and bacterial infection in his body.
10
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
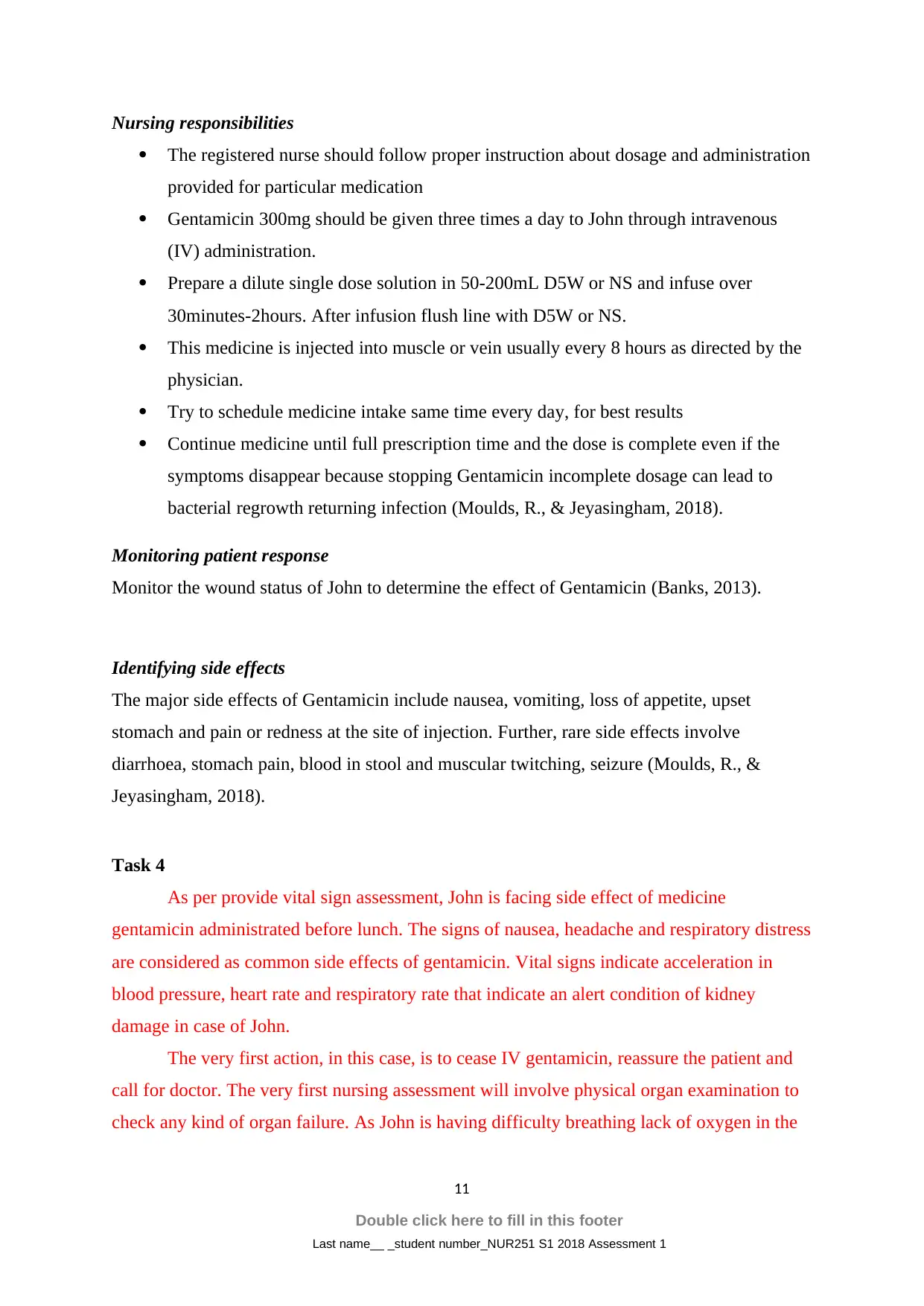
Nursing responsibilities
The registered nurse should follow proper instruction about dosage and administration
provided for particular medication
Gentamicin 300mg should be given three times a day to John through intravenous
(IV) administration.
Prepare a dilute single dose solution in 50-200mL D5W or NS and infuse over
30minutes-2hours. After infusion flush line with D5W or NS.
This medicine is injected into muscle or vein usually every 8 hours as directed by the
physician.
Try to schedule medicine intake same time every day, for best results
Continue medicine until full prescription time and the dose is complete even if the
symptoms disappear because stopping Gentamicin incomplete dosage can lead to
bacterial regrowth returning infection (Moulds, R., & Jeyasingham, 2018).
Monitoring patient response
Monitor the wound status of John to determine the effect of Gentamicin (Banks, 2013).
Identifying side effects
The major side effects of Gentamicin include nausea, vomiting, loss of appetite, upset
stomach and pain or redness at the site of injection. Further, rare side effects involve
diarrhoea, stomach pain, blood in stool and muscular twitching, seizure (Moulds, R., &
Jeyasingham, 2018).
Task 4
As per provide vital sign assessment, John is facing side effect of medicine
gentamicin administrated before lunch. The signs of nausea, headache and respiratory distress
are considered as common side effects of gentamicin. Vital signs indicate acceleration in
blood pressure, heart rate and respiratory rate that indicate an alert condition of kidney
damage in case of John.
The very first action, in this case, is to cease IV gentamicin, reassure the patient and
call for doctor. The very first nursing assessment will involve physical organ examination to
check any kind of organ failure. As John is having difficulty breathing lack of oxygen in the
11
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
The registered nurse should follow proper instruction about dosage and administration
provided for particular medication
Gentamicin 300mg should be given three times a day to John through intravenous
(IV) administration.
Prepare a dilute single dose solution in 50-200mL D5W or NS and infuse over
30minutes-2hours. After infusion flush line with D5W or NS.
This medicine is injected into muscle or vein usually every 8 hours as directed by the
physician.
Try to schedule medicine intake same time every day, for best results
Continue medicine until full prescription time and the dose is complete even if the
symptoms disappear because stopping Gentamicin incomplete dosage can lead to
bacterial regrowth returning infection (Moulds, R., & Jeyasingham, 2018).
Monitoring patient response
Monitor the wound status of John to determine the effect of Gentamicin (Banks, 2013).
Identifying side effects
The major side effects of Gentamicin include nausea, vomiting, loss of appetite, upset
stomach and pain or redness at the site of injection. Further, rare side effects involve
diarrhoea, stomach pain, blood in stool and muscular twitching, seizure (Moulds, R., &
Jeyasingham, 2018).
Task 4
As per provide vital sign assessment, John is facing side effect of medicine
gentamicin administrated before lunch. The signs of nausea, headache and respiratory distress
are considered as common side effects of gentamicin. Vital signs indicate acceleration in
blood pressure, heart rate and respiratory rate that indicate an alert condition of kidney
damage in case of John.
The very first action, in this case, is to cease IV gentamicin, reassure the patient and
call for doctor. The very first nursing assessment will involve physical organ examination to
check any kind of organ failure. As John is having difficulty breathing lack of oxygen in the
11
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
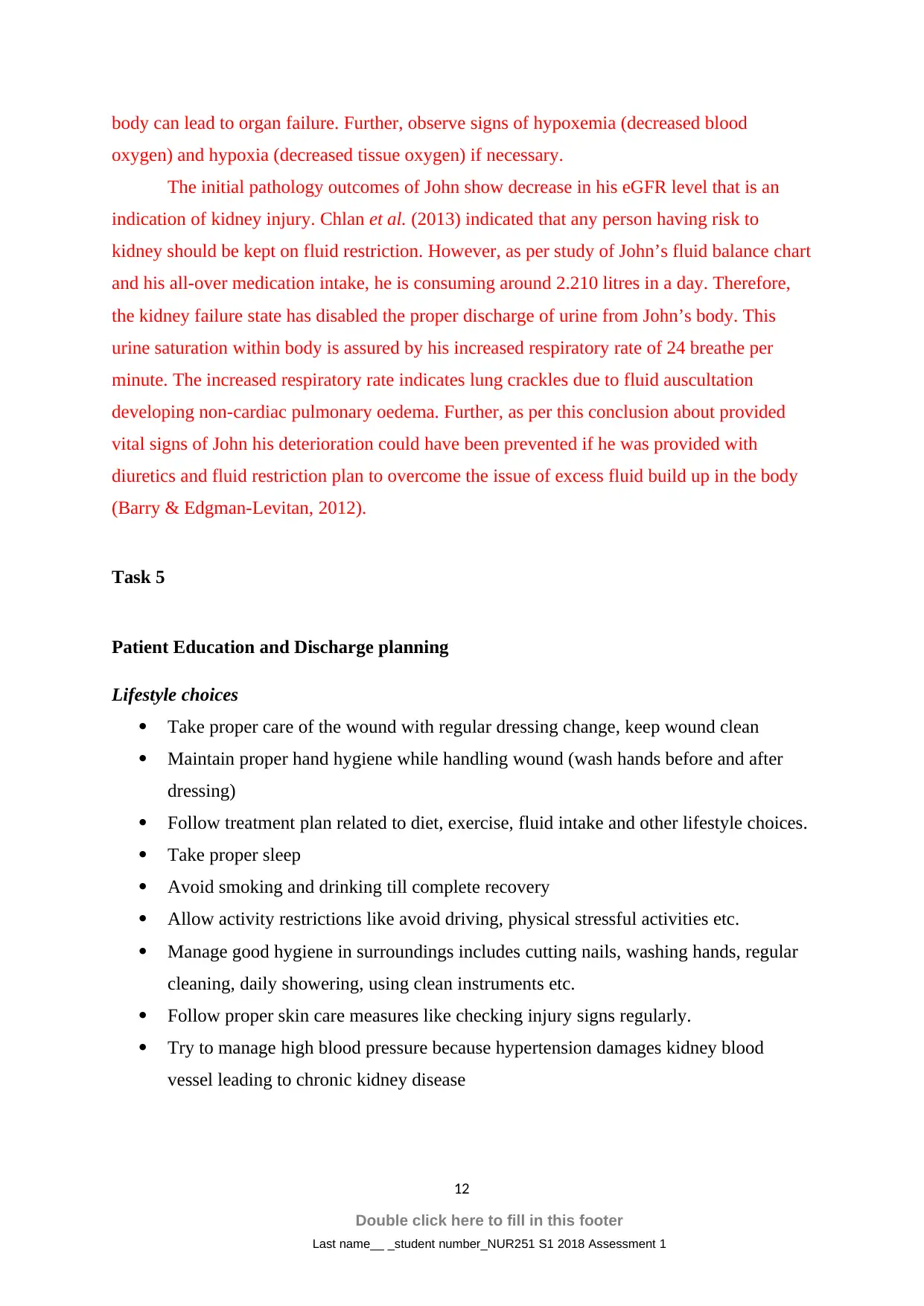
body can lead to organ failure. Further, observe signs of hypoxemia (decreased blood
oxygen) and hypoxia (decreased tissue oxygen) if necessary.
The initial pathology outcomes of John show decrease in his eGFR level that is an
indication of kidney injury. Chlan et al. (2013) indicated that any person having risk to
kidney should be kept on fluid restriction. However, as per study of John’s fluid balance chart
and his all-over medication intake, he is consuming around 2.210 litres in a day. Therefore,
the kidney failure state has disabled the proper discharge of urine from John’s body. This
urine saturation within body is assured by his increased respiratory rate of 24 breathe per
minute. The increased respiratory rate indicates lung crackles due to fluid auscultation
developing non-cardiac pulmonary oedema. Further, as per this conclusion about provided
vital signs of John his deterioration could have been prevented if he was provided with
diuretics and fluid restriction plan to overcome the issue of excess fluid build up in the body
(Barry & Edgman-Levitan, 2012).
Task 5
Patient Education and Discharge planning
Lifestyle choices
Take proper care of the wound with regular dressing change, keep wound clean
Maintain proper hand hygiene while handling wound (wash hands before and after
dressing)
Follow treatment plan related to diet, exercise, fluid intake and other lifestyle choices.
Take proper sleep
Avoid smoking and drinking till complete recovery
Allow activity restrictions like avoid driving, physical stressful activities etc.
Manage good hygiene in surroundings includes cutting nails, washing hands, regular
cleaning, daily showering, using clean instruments etc.
Follow proper skin care measures like checking injury signs regularly.
Try to manage high blood pressure because hypertension damages kidney blood
vessel leading to chronic kidney disease
12
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
oxygen) and hypoxia (decreased tissue oxygen) if necessary.
The initial pathology outcomes of John show decrease in his eGFR level that is an
indication of kidney injury. Chlan et al. (2013) indicated that any person having risk to
kidney should be kept on fluid restriction. However, as per study of John’s fluid balance chart
and his all-over medication intake, he is consuming around 2.210 litres in a day. Therefore,
the kidney failure state has disabled the proper discharge of urine from John’s body. This
urine saturation within body is assured by his increased respiratory rate of 24 breathe per
minute. The increased respiratory rate indicates lung crackles due to fluid auscultation
developing non-cardiac pulmonary oedema. Further, as per this conclusion about provided
vital signs of John his deterioration could have been prevented if he was provided with
diuretics and fluid restriction plan to overcome the issue of excess fluid build up in the body
(Barry & Edgman-Levitan, 2012).
Task 5
Patient Education and Discharge planning
Lifestyle choices
Take proper care of the wound with regular dressing change, keep wound clean
Maintain proper hand hygiene while handling wound (wash hands before and after
dressing)
Follow treatment plan related to diet, exercise, fluid intake and other lifestyle choices.
Take proper sleep
Avoid smoking and drinking till complete recovery
Allow activity restrictions like avoid driving, physical stressful activities etc.
Manage good hygiene in surroundings includes cutting nails, washing hands, regular
cleaning, daily showering, using clean instruments etc.
Follow proper skin care measures like checking injury signs regularly.
Try to manage high blood pressure because hypertension damages kidney blood
vessel leading to chronic kidney disease
12
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Maximise intake of vegetables, fruit, fibres, nuts and healthy fats in the diet. Also
advice John to take potassium rich foods to control his risk situation of Kidney
damage.
Practice relaxations like massage, acupuncture and meditation.
Reduce intake of food having phosphorus, calcium, sodium and other minerals that
may harm kidney function. Food like beer, bread, processed meats, dairy, and
chocolate products (Gulanick & Myers, 2013).
Medication instructions
Study the use, administration and side effects of medication provided by the doctor
Take medication as per provided time and dosage
Carry medicine list or prescription in the wallet at all places
Always store medicines in cool and dry location.
Recommended resources
Follow the physician instructions about follow-up appointments and talk with the
physician for any further information, query or confusion related to treatment.
Try to practice rehabilitation program for wound care and recovery like physical
therapy (regain muscular strength), occupational therapy etc.
Refer to the dietician to manage diet properly as per health condition (Gulanick &
Myers, 2013).
13
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
advice John to take potassium rich foods to control his risk situation of Kidney
damage.
Practice relaxations like massage, acupuncture and meditation.
Reduce intake of food having phosphorus, calcium, sodium and other minerals that
may harm kidney function. Food like beer, bread, processed meats, dairy, and
chocolate products (Gulanick & Myers, 2013).
Medication instructions
Study the use, administration and side effects of medication provided by the doctor
Take medication as per provided time and dosage
Carry medicine list or prescription in the wallet at all places
Always store medicines in cool and dry location.
Recommended resources
Follow the physician instructions about follow-up appointments and talk with the
physician for any further information, query or confusion related to treatment.
Try to practice rehabilitation program for wound care and recovery like physical
therapy (regain muscular strength), occupational therapy etc.
Refer to the dietician to manage diet properly as per health condition (Gulanick &
Myers, 2013).
13
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
References
Books
Banks, A. (2013). Laboratory tests and diagnostic procedures with nursing diagnoses.
Pearson.
Fortinash, K. M., & Worret, P. A. H. (2014). Psychiatric Mental Health Nursing-E-Book.
Elsevier Health Sciences.
Gulanick, M., & Myers, J. L. (2013). Nursing Care Plans-E-Book: Nursing Diagnosis and
Intervention. Elsevier Health Sciences.
Harris, P., Nagy, S., & Vardaxis, N. (2014). Mosby's Dictionary of Medicine, Nursing and
Health Professions-Australian & New Zealand Edition-eBook. Elsevier Health Sciences.
Suinn, R. M. (2013). Anxiety management training: A behavior therapy. Springer Science &
Business Media.
Urden, L. D., Stacy, K. M., & Lough, M. E. (2014). Critical Care Nursing-E-Book:
Diagnosis and Management. Elsevier Health Sciences.
Willis, E., Reynolds, L., & Keleher, H. (Eds.). (2016). Understanding the Australian health
care system. Elsevier Health Sciences.
Journals
Books
Banks, A. (2013). Laboratory tests and diagnostic procedures with nursing diagnoses.
Pearson.
Fortinash, K. M., & Worret, P. A. H. (2014). Psychiatric Mental Health Nursing-E-Book.
Elsevier Health Sciences.
Gulanick, M., & Myers, J. L. (2013). Nursing Care Plans-E-Book: Nursing Diagnosis and
Intervention. Elsevier Health Sciences.
Suinn, R. M. (2013). Anxiety management training: A behavior therapy. Springer Science &
Business Media.
Urden, L. D., Stacy, K. M., & Lough, M. E. (2014). Critical Care Nursing-E-Book:
Diagnosis and Management. Elsevier Health Sciences.
14
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
Books
Banks, A. (2013). Laboratory tests and diagnostic procedures with nursing diagnoses.
Pearson.
Fortinash, K. M., & Worret, P. A. H. (2014). Psychiatric Mental Health Nursing-E-Book.
Elsevier Health Sciences.
Gulanick, M., & Myers, J. L. (2013). Nursing Care Plans-E-Book: Nursing Diagnosis and
Intervention. Elsevier Health Sciences.
Harris, P., Nagy, S., & Vardaxis, N. (2014). Mosby's Dictionary of Medicine, Nursing and
Health Professions-Australian & New Zealand Edition-eBook. Elsevier Health Sciences.
Suinn, R. M. (2013). Anxiety management training: A behavior therapy. Springer Science &
Business Media.
Urden, L. D., Stacy, K. M., & Lough, M. E. (2014). Critical Care Nursing-E-Book:
Diagnosis and Management. Elsevier Health Sciences.
Willis, E., Reynolds, L., & Keleher, H. (Eds.). (2016). Understanding the Australian health
care system. Elsevier Health Sciences.
Journals
Books
Banks, A. (2013). Laboratory tests and diagnostic procedures with nursing diagnoses.
Pearson.
Fortinash, K. M., & Worret, P. A. H. (2014). Psychiatric Mental Health Nursing-E-Book.
Elsevier Health Sciences.
Gulanick, M., & Myers, J. L. (2013). Nursing Care Plans-E-Book: Nursing Diagnosis and
Intervention. Elsevier Health Sciences.
Suinn, R. M. (2013). Anxiety management training: A behavior therapy. Springer Science &
Business Media.
Urden, L. D., Stacy, K. M., & Lough, M. E. (2014). Critical Care Nursing-E-Book:
Diagnosis and Management. Elsevier Health Sciences.
14
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
Journals
Anderson, D. J., Podgorny, K., Berríos-Torres, S. I., Bratzler, D. W., Dellinger, E. P., Greene,
L., ... & Kaye, K. S. (2014). Strategies to prevent surgical site infections in acute care
hospitals: 2014 update. Infection Control & Hospital Epidemiology, 35(S2), S66-S88.
Andersson, H., Lindholm, C., Iversen, A., Giske, C. G., Örtqvist, Å., Kalin, M., & Fossum,
B. (2012). Prevalence of antibiotic-resistant bacteria in residents of nursing homes in a
Swedish municipality: healthcare staff knowledge of and adherence to principles of basic
infection prevention. Scandinavian journal of infectious diseases, 44(9), 641-649.
Barry, M. J., & Edgman-Levitan, S. (2012). Shared decision making—the pinnacle of
patient-centered care. New England Journal of Medicine, 366(9), 780-781.
Blakeman, T., Protheroe, J., Chew-Graham, C., Rogers, A., & Kennedy, A. (2012).
Understanding the management of early-stage chronic kidney disease in primary care: a
qualitative study. Br J Gen Pract, 62(597), e233-e242.
Chlan, L. L., Weinert, C. R., Heiderscheit, A., Tracy, M. F., Skaar, D. J., Guttormson, J. L.,
& Savik, K. (2013). Effects of patient-directed music intervention on anxiety and sedative
exposure in critically ill patients receiving mechanical ventilatory support: a randomized
clinical trial. Jama, 309(22), 2335-2344.
Cuijpers, P., Sijbrandij, M., Koole, S., Huibers, M., Berking, M., & Andersson, G. (2014).
Psychological treatment of generalized anxiety disorder: a meta-analysis. Clinical
psychology review, 34(2), 130-140.
Davison, S. N., Levin, A., Moss, A. H., Jha, V., Brown, E. A., Brennan, F., ... & Morton, R.
L. (2015). Executive summary of the KDIGO Controversies Conference on Supportive
Care in Chronic Kidney Disease: developing a roadmap to improving quality care. Kidney
international, 88(3), 447-459.
Hallan, S. I., Matsushita, K., Sang, Y., Mahmoodi, B. K., Black, C., Ishani, A., ... & Wetzels,
J. F. (2012). Age and association of kidney measures with mortality and end-stage renal
disease. Jama, 308(22), 2349-2360.
Katzman, M. A., Bleau, P., Blier, P., Chokka, P., Kjernisted, K., & Van Ameringen, M.
(2014). Canadian clinical practice guidelines for the management of anxiety, posttraumatic
stress and obsessive-compulsive disorders. BMC psychiatry, 14(1), S1.
Magill, S. S., Edwards, J. R., Bamberg, W., Beldavs, Z. G., Dumyati, G., Kainer, M. A., ... &
Ray, S. M. (2014). Multistate point-prevalence survey of health care–associated
infections. New England Journal of Medicine, 370(13), 1198-1208.
15
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
Anderson, D. J., Podgorny, K., Berríos-Torres, S. I., Bratzler, D. W., Dellinger, E. P., Greene,
L., ... & Kaye, K. S. (2014). Strategies to prevent surgical site infections in acute care
hospitals: 2014 update. Infection Control & Hospital Epidemiology, 35(S2), S66-S88.
Andersson, H., Lindholm, C., Iversen, A., Giske, C. G., Örtqvist, Å., Kalin, M., & Fossum,
B. (2012). Prevalence of antibiotic-resistant bacteria in residents of nursing homes in a
Swedish municipality: healthcare staff knowledge of and adherence to principles of basic
infection prevention. Scandinavian journal of infectious diseases, 44(9), 641-649.
Barry, M. J., & Edgman-Levitan, S. (2012). Shared decision making—the pinnacle of
patient-centered care. New England Journal of Medicine, 366(9), 780-781.
Blakeman, T., Protheroe, J., Chew-Graham, C., Rogers, A., & Kennedy, A. (2012).
Understanding the management of early-stage chronic kidney disease in primary care: a
qualitative study. Br J Gen Pract, 62(597), e233-e242.
Chlan, L. L., Weinert, C. R., Heiderscheit, A., Tracy, M. F., Skaar, D. J., Guttormson, J. L.,
& Savik, K. (2013). Effects of patient-directed music intervention on anxiety and sedative
exposure in critically ill patients receiving mechanical ventilatory support: a randomized
clinical trial. Jama, 309(22), 2335-2344.
Cuijpers, P., Sijbrandij, M., Koole, S., Huibers, M., Berking, M., & Andersson, G. (2014).
Psychological treatment of generalized anxiety disorder: a meta-analysis. Clinical
psychology review, 34(2), 130-140.
Davison, S. N., Levin, A., Moss, A. H., Jha, V., Brown, E. A., Brennan, F., ... & Morton, R.
L. (2015). Executive summary of the KDIGO Controversies Conference on Supportive
Care in Chronic Kidney Disease: developing a roadmap to improving quality care. Kidney
international, 88(3), 447-459.
Hallan, S. I., Matsushita, K., Sang, Y., Mahmoodi, B. K., Black, C., Ishani, A., ... & Wetzels,
J. F. (2012). Age and association of kidney measures with mortality and end-stage renal
disease. Jama, 308(22), 2349-2360.
Katzman, M. A., Bleau, P., Blier, P., Chokka, P., Kjernisted, K., & Van Ameringen, M.
(2014). Canadian clinical practice guidelines for the management of anxiety, posttraumatic
stress and obsessive-compulsive disorders. BMC psychiatry, 14(1), S1.
Magill, S. S., Edwards, J. R., Bamberg, W., Beldavs, Z. G., Dumyati, G., Kainer, M. A., ... &
Ray, S. M. (2014). Multistate point-prevalence survey of health care–associated
infections. New England Journal of Medicine, 370(13), 1198-1208.
15
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

Tacconelli, E., Cataldo, M. A., Dancer, S. J., Angelis, G., Falcone, M., Frank, U., ... & Singh,
N. (2014). ESCMID guidelines for the management of the infection control measures to
reduce transmission of multidrug‐resistant Gram‐negative bacteria in hospitalized
patients. Clinical Microbiology and Infection, 20(s1), 1-55.
Yatham, L. N., Kennedy, S. H., Parikh, S. V., Schaffer, A., Beaulieu, S., Alda, M., ... &
Ravindran, A. (2013). Canadian Network for Mood and Anxiety Treatments (CANMAT)
and International Society for Bipolar Disorders (ISBD) collaborative update of CANMAT
guidelines for the management of patients with bipolar disorder: update 2013. Bipolar
disorders, 15(1), 1-44.
Zhang, L., Wang, F., Wang, L., Wang, W., Liu, B., Liu, J., ... & Chen, N. (2012). Prevalence
of chronic kidney disease in China: a cross-sectional survey. The Lancet, 379(9818), 815-
822.
Websites
Ibuprofen. (2018). Healthdirect.gov.au. Retrieved 10 April 2018, from
https://www.healthdirect.gov.au/ibuprofen.
Moulds, R., & Jeyasingham, M. (2018). Gentamicin: a great way to start. NPS medicinewise.
Retrieved 10 April 2018, from
https://www.nps.org.au/australian-prescriber/articles/gentamicin-a-great-way-to-start.
16
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
N. (2014). ESCMID guidelines for the management of the infection control measures to
reduce transmission of multidrug‐resistant Gram‐negative bacteria in hospitalized
patients. Clinical Microbiology and Infection, 20(s1), 1-55.
Yatham, L. N., Kennedy, S. H., Parikh, S. V., Schaffer, A., Beaulieu, S., Alda, M., ... &
Ravindran, A. (2013). Canadian Network for Mood and Anxiety Treatments (CANMAT)
and International Society for Bipolar Disorders (ISBD) collaborative update of CANMAT
guidelines for the management of patients with bipolar disorder: update 2013. Bipolar
disorders, 15(1), 1-44.
Zhang, L., Wang, F., Wang, L., Wang, W., Liu, B., Liu, J., ... & Chen, N. (2012). Prevalence
of chronic kidney disease in China: a cross-sectional survey. The Lancet, 379(9818), 815-
822.
Websites
Ibuprofen. (2018). Healthdirect.gov.au. Retrieved 10 April 2018, from
https://www.healthdirect.gov.au/ibuprofen.
Moulds, R., & Jeyasingham, M. (2018). Gentamicin: a great way to start. NPS medicinewise.
Retrieved 10 April 2018, from
https://www.nps.org.au/australian-prescriber/articles/gentamicin-a-great-way-to-start.
16
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

17
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
Double click here to fill in this footer
Last name__ _student number_NUR251 S1 2018 Assessment 1
1 out of 17
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.



