Comprehensive Nursing Plan for Exogenous Cushing’s Syndrome
VerifiedAdded on 2023/04/12
|11
|2028
|374
Report
AI Summary
This report provides a detailed analysis of Exogenous Cushing’s Syndrome, focusing on its causes, incidence, and risk factors, particularly in the context of Ms. Maureen Smith's case. It explores the impact of the disease on patients and their families, highlighting common signs and symptoms such as a round face, abdominal fat accumulation, and high LDL cholesterol, explaining their underlying pathophysiology. The report also discusses the pharmacodynamics and pharmacokinetics of Mitotane, a common drug used in treatment. Furthermore, it presents a comprehensive nursing care plan for the first 8 hours post-admission, outlining goals, interventions, and rationales for managing respiratory and cardiac status, electrolyte balance, vital signs, and specific symptoms like hypertension and hyperglycemia. This thorough examination provides valuable insights for healthcare professionals in managing Exogenous Cushing’s Syndrome.

Running head: NURSING ASSIGNMENT
NURSING ASSIGNMENT
Name of the Student:
Name of the University:
Author Note:
NURSING ASSIGNMENT
Name of the Student:
Name of the University:
Author Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

1NURSING ASSIGNMENT
Outline the disease, causes, incidence and risk factors. Discuss the impact of the selected
disease on the patient and their family.
On analyzing the case presentment of Ms. Maureen Smith, the disease impression can be
stated as Exogenous Cushing’s Syndrome. As mentioned by Liew et al. (2013), Exogenous
Cushing’s Syndrome is extremely common in people who take glucocorticoid medications or
other corticosteroid hormones. The syndrome typically manifests itself when the body has a
higher than normal level of the cortisol hormone. The cortisol hormone is synthesized in the
body by the adrenal gland. In this context, it should be mentioned that the term ‘exogenous’
refers to an agent outside the body. This means that Exogenous Cushing Syndrome is caused
upon taking synthetic glucocorticoid medication which might be prescribed to treat another
disorder. Glucocorticoid medications are prescribed for a number of disease conditions such as
lung diseases, joint related diseases, inflammatory bowel disease, cancer, skin diseases or brain
tumor (Lacroix et al., 2015). The medications can either be taken in the form of pills or are
administered intravenously, injected to the affected joint area, administered through enema, used
as skin creams, inhaled from inhalers or used as eye drops (Raff & Carroll, 2015).
Research studies suggest that the prevalence rate of the syndrome is 40 in every million.
The incidence rate has been studied to be 1 or 2 cases per million of the total population
(Betterhealth.vic.gov.au, 2019). Studied suggest that 60% of the syndrome is caused due to the
condition of hypercortisolism (Betterhealth.vic.gov.au, 2019). Also, the syndrome is more
common in women than in men and manifests itself in the ratio 8:1 (Raff & Carroll, 2015). Also,
Exogenous Cushing Syndrome affects women belonging to the age group between 20-40 years
(Raff & Carroll, 2015).
Outline the disease, causes, incidence and risk factors. Discuss the impact of the selected
disease on the patient and their family.
On analyzing the case presentment of Ms. Maureen Smith, the disease impression can be
stated as Exogenous Cushing’s Syndrome. As mentioned by Liew et al. (2013), Exogenous
Cushing’s Syndrome is extremely common in people who take glucocorticoid medications or
other corticosteroid hormones. The syndrome typically manifests itself when the body has a
higher than normal level of the cortisol hormone. The cortisol hormone is synthesized in the
body by the adrenal gland. In this context, it should be mentioned that the term ‘exogenous’
refers to an agent outside the body. This means that Exogenous Cushing Syndrome is caused
upon taking synthetic glucocorticoid medication which might be prescribed to treat another
disorder. Glucocorticoid medications are prescribed for a number of disease conditions such as
lung diseases, joint related diseases, inflammatory bowel disease, cancer, skin diseases or brain
tumor (Lacroix et al., 2015). The medications can either be taken in the form of pills or are
administered intravenously, injected to the affected joint area, administered through enema, used
as skin creams, inhaled from inhalers or used as eye drops (Raff & Carroll, 2015).
Research studies suggest that the prevalence rate of the syndrome is 40 in every million.
The incidence rate has been studied to be 1 or 2 cases per million of the total population
(Betterhealth.vic.gov.au, 2019). Studied suggest that 60% of the syndrome is caused due to the
condition of hypercortisolism (Betterhealth.vic.gov.au, 2019). Also, the syndrome is more
common in women than in men and manifests itself in the ratio 8:1 (Raff & Carroll, 2015). Also,
Exogenous Cushing Syndrome affects women belonging to the age group between 20-40 years
(Raff & Carroll, 2015).

2NURSING ASSIGNMENT
The common risk factors for the syndrome include medical history of Type II Diabetes,
obesity, hypertension and high blood glucose level (Duan et al., 2015). It is important to note
here that, these factors are not directly responsible for causing the syndrome but have been
studied to indirectly affect the prevalence of the syndrome. In addition to this, higher cortisol due
to the intake of glucocorticoid medications, adrenal adenomas, ectopic ACTH and Pituitary
diseases are also considered as high risk factors (Duan et al., 2015).
The diagnosis of Exogenous Cushing Syndrome would negatively affect the quality of
life of the patient as well as her husband. As a result of the syndrome, the patient might feel
fatigued, emotionally unstable because of changes in her physical appearance, experience
cognitive problems, sleeping difficulties or experience depression (Starkman, 2013). The
emotional turmoil experienced by the patient would also affect her husband and deteriorate their
quality of life.
Discuss three (3) common signs and symptoms of the selected disease and explain the
underlying pathophysiology of each.
Thee three common symptoms and their underlying pathophysiology as observed in the
patient has been described in the table below:
Signs and symptoms observed in Ms. Smith Pathophysiology
Presence of round and full face as observed by her
husband
Presence of a round face or moon face is a
characteristic symptom of the Cushing syndrome.
The symptom is also referred to as a Cushingoid
appearance. The face becomes round and fluffy and
fat accumulated on the sides of the face which
makes the face looks round in the shape of a moon
The common risk factors for the syndrome include medical history of Type II Diabetes,
obesity, hypertension and high blood glucose level (Duan et al., 2015). It is important to note
here that, these factors are not directly responsible for causing the syndrome but have been
studied to indirectly affect the prevalence of the syndrome. In addition to this, higher cortisol due
to the intake of glucocorticoid medications, adrenal adenomas, ectopic ACTH and Pituitary
diseases are also considered as high risk factors (Duan et al., 2015).
The diagnosis of Exogenous Cushing Syndrome would negatively affect the quality of
life of the patient as well as her husband. As a result of the syndrome, the patient might feel
fatigued, emotionally unstable because of changes in her physical appearance, experience
cognitive problems, sleeping difficulties or experience depression (Starkman, 2013). The
emotional turmoil experienced by the patient would also affect her husband and deteriorate their
quality of life.
Discuss three (3) common signs and symptoms of the selected disease and explain the
underlying pathophysiology of each.
Thee three common symptoms and their underlying pathophysiology as observed in the
patient has been described in the table below:
Signs and symptoms observed in Ms. Smith Pathophysiology
Presence of round and full face as observed by her
husband
Presence of a round face or moon face is a
characteristic symptom of the Cushing syndrome.
The symptom is also referred to as a Cushingoid
appearance. The face becomes round and fluffy and
fat accumulated on the sides of the face which
makes the face looks round in the shape of a moon
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

3NURSING ASSIGNMENT
(Kargi & Iacobellis, 2014). The symptom is
characterized by the excessive release of the
cortisol hormone by the adrenal glands that are
located on the upper region of the kidneys (Kargi
& Iacobellis, 2014).
Presence of fat mainly around her abdominal area
and as a hump between her shoulders
Exogenous Cushing Syndrome is caused due to the
excessive secretion of the Cortisol hormone (Colao
et al., 2014). The process of accumulation and
distribution of fat is significantly influenced by a
number of genes and hormones. Studies suggest
that the adipocytes or the fat cells that are present
in the central region of the body are more receptive
to the effect of the insulin compared to the fat cells
that are present in the periphery (Tchernof &
Despres, 2013). The high level of cortisol in the
body affects the process of insulin secretion and
sensitivity and the process of fat metabolism. As a
result of which the adipocytes present in the central
region accumulate fat and appear as a buffalo hump
(Kargi & Iacobellis, 2014).
Clinical evaluation suggesting high level of low
density lipoprotein cholesterol
Studies suggest that excessive secretion of the
Cortisol hormone leads to an increase in the
cholesterol and triglyceride level in the blood
(Nieman et al., 2015; Starkman, 2013). This results
in elevating the cholesterol build up within the
(Kargi & Iacobellis, 2014). The symptom is
characterized by the excessive release of the
cortisol hormone by the adrenal glands that are
located on the upper region of the kidneys (Kargi
& Iacobellis, 2014).
Presence of fat mainly around her abdominal area
and as a hump between her shoulders
Exogenous Cushing Syndrome is caused due to the
excessive secretion of the Cortisol hormone (Colao
et al., 2014). The process of accumulation and
distribution of fat is significantly influenced by a
number of genes and hormones. Studies suggest
that the adipocytes or the fat cells that are present
in the central region of the body are more receptive
to the effect of the insulin compared to the fat cells
that are present in the periphery (Tchernof &
Despres, 2013). The high level of cortisol in the
body affects the process of insulin secretion and
sensitivity and the process of fat metabolism. As a
result of which the adipocytes present in the central
region accumulate fat and appear as a buffalo hump
(Kargi & Iacobellis, 2014).
Clinical evaluation suggesting high level of low
density lipoprotein cholesterol
Studies suggest that excessive secretion of the
Cortisol hormone leads to an increase in the
cholesterol and triglyceride level in the blood
(Nieman et al., 2015; Starkman, 2013). This results
in elevating the cholesterol build up within the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4NURSING ASSIGNMENT
arteries which hinders the process of smooth blood
supply to the heart (Colao et al., 2014).
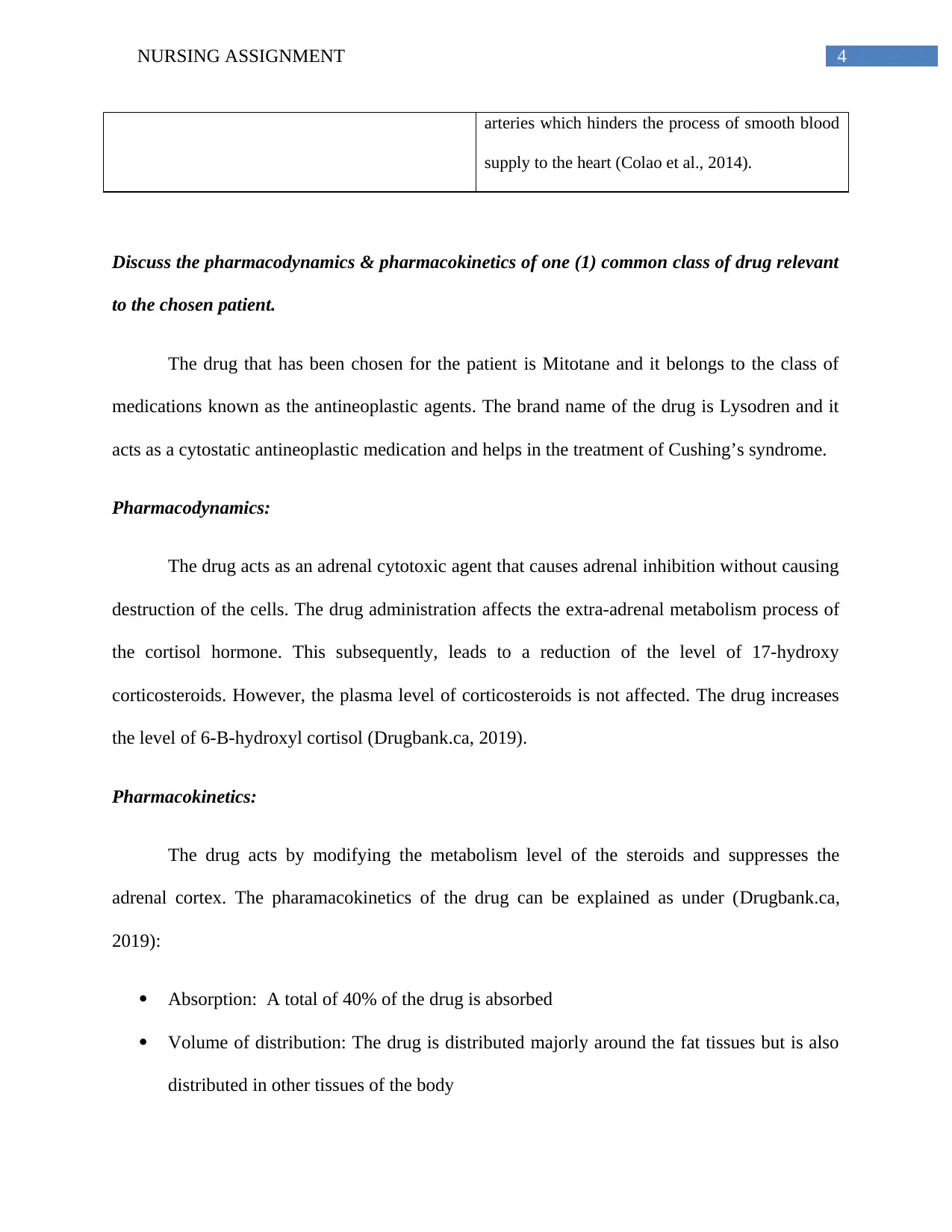
Discuss the pharmacodynamics & pharmacokinetics of one (1) common class of drug relevant
to the chosen patient.
The drug that has been chosen for the patient is Mitotane and it belongs to the class of
medications known as the antineoplastic agents. The brand name of the drug is Lysodren and it
acts as a cytostatic antineoplastic medication and helps in the treatment of Cushing’s syndrome.
Pharmacodynamics:
The drug acts as an adrenal cytotoxic agent that causes adrenal inhibition without causing
destruction of the cells. The drug administration affects the extra-adrenal metabolism process of
the cortisol hormone. This subsequently, leads to a reduction of the level of 17-hydroxy
corticosteroids. However, the plasma level of corticosteroids is not affected. The drug increases
the level of 6-B-hydroxyl cortisol (Drugbank.ca, 2019).
Pharmacokinetics:
The drug acts by modifying the metabolism level of the steroids and suppresses the
adrenal cortex. The pharamacokinetics of the drug can be explained as under (Drugbank.ca,
2019):
Absorption: A total of 40% of the drug is absorbed
Volume of distribution: The drug is distributed majorly around the fat tissues but is also
distributed in other tissues of the body
arteries which hinders the process of smooth blood
supply to the heart (Colao et al., 2014).
Discuss the pharmacodynamics & pharmacokinetics of one (1) common class of drug relevant
to the chosen patient.
The drug that has been chosen for the patient is Mitotane and it belongs to the class of
medications known as the antineoplastic agents. The brand name of the drug is Lysodren and it
acts as a cytostatic antineoplastic medication and helps in the treatment of Cushing’s syndrome.
Pharmacodynamics:
The drug acts as an adrenal cytotoxic agent that causes adrenal inhibition without causing
destruction of the cells. The drug administration affects the extra-adrenal metabolism process of
the cortisol hormone. This subsequently, leads to a reduction of the level of 17-hydroxy
corticosteroids. However, the plasma level of corticosteroids is not affected. The drug increases
the level of 6-B-hydroxyl cortisol (Drugbank.ca, 2019).
Pharmacokinetics:
The drug acts by modifying the metabolism level of the steroids and suppresses the
adrenal cortex. The pharamacokinetics of the drug can be explained as under (Drugbank.ca,
2019):
Absorption: A total of 40% of the drug is absorbed
Volume of distribution: The drug is distributed majorly around the fat tissues but is also
distributed in other tissues of the body

5NURSING ASSIGNMENT
Protein Binding: 6%
Metabolism: The drug is mainly metabolized in the hepatic and renal site
Route of elimination: Approximately 1% to 7% of the drug is excreted through bile and
the remaining proportion is stored in other tissues of the body
Half-life: The half life of the drug is in between 18-159 days
In order of priority, develop a nursing care plan for your chosen patient who has just arrived
on the ward from ED. Nursing care plan goals, interventions and rationales must relate to the
first 8 hours post ward admission.
A nursing plan is used to treat a patient once the patient is transferred to the ward from
the emergency department. Typically a nursing plan comprises of important aspects such as
nursing care plan goals, interventions as well as supporting rationales collecting through
evidence base studies that help in the recovery process of the patient. With respect to the case
study, the following nursing plan would be adapted for the patient.
Nursing Care Plan Goals Intervention Supporting Rationale
Closely monitor and
evaluate respiratory
rate and cardiac
status
Promote comfort and
rest and maintain a
hygienic clinical
environment
Conduct 12-lead EKG
to eliminate the
possibility of cardiac
involvement
Ensure that the patient
is comfortable and is
able to rest and
observe infection
control routine
Studies suggest that a
shift in the fluid
balance or electrolytes
might lead to
difficulties in breathing
or arrhythmias
(Nieman et al., 2015)
Studies suggest that
prolong secretion of
high level of Cortisol
hormone weakens the
body and renders the
immune system weak.
It is important to
promote rest and also
monitor the patient for
Protein Binding: 6%
Metabolism: The drug is mainly metabolized in the hepatic and renal site
Route of elimination: Approximately 1% to 7% of the drug is excreted through bile and
the remaining proportion is stored in other tissues of the body
Half-life: The half life of the drug is in between 18-159 days
In order of priority, develop a nursing care plan for your chosen patient who has just arrived
on the ward from ED. Nursing care plan goals, interventions and rationales must relate to the
first 8 hours post ward admission.
A nursing plan is used to treat a patient once the patient is transferred to the ward from
the emergency department. Typically a nursing plan comprises of important aspects such as
nursing care plan goals, interventions as well as supporting rationales collecting through
evidence base studies that help in the recovery process of the patient. With respect to the case
study, the following nursing plan would be adapted for the patient.
Nursing Care Plan Goals Intervention Supporting Rationale
Closely monitor and
evaluate respiratory
rate and cardiac
status
Promote comfort and
rest and maintain a
hygienic clinical
environment
Conduct 12-lead EKG
to eliminate the
possibility of cardiac
involvement
Ensure that the patient
is comfortable and is
able to rest and
observe infection
control routine
Studies suggest that a
shift in the fluid
balance or electrolytes
might lead to
difficulties in breathing
or arrhythmias
(Nieman et al., 2015)
Studies suggest that
prolong secretion of
high level of Cortisol
hormone weakens the
body and renders the
immune system weak.
It is important to
promote rest and also
monitor the patient for
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

6NURSING ASSIGNMENT
possibly acquiring an
infection (Colao et al.,
2014)
Closely monitor
electrolyte and fluid
balance
Closely monitor the
vital signs to detect
higher blood pressure
or other
abnormalities
The intervention to
manage electrolyte and
fluid balance would
include regulating fluid
restrictions (I & O) as
and when necessary
Conduct vital
assessment and
document patient
assessment
Studies reveal that on
account of the high
level production of
Cortisol in the body,
the body develops the
tendency to retain
Sodium and Water
which can
subsequently lead to
cardiac stress or even
hypokalemia (Kargi &
Iacobellis, 2014)
Research studies
suggests that elevated
level of Cortisol
hormone in the body
leads to hypertension
which can potentially
increase the risk of a
cardiac stroke (Duan et
al., 2015)
Mange the symptoms
of the patient and
administer
appropriate
medication.
Consider the
symptoms of high
blood pressure and
high blood glucose
level.
Intervention for
managing hypertension
or high blood pressure
would include,
administration of
antihypertensives and
diuretics
On the other hand,
intervention for
managing high blood
glucose level would
include consulting the
physician and using
juice to treat
hypoglycemia
The excess level of the
stress hormone
Cortisol in the blood
leads to an elevation of
the blood pressure
level. Studies suggest
that administration of
antihypertensives can
help in changing the
cortisol level and help
in down regulating the
blood pressure within
the normal range. On
the other hand,
administration of
Diuretics has been
studied to promote
fluid retention and
prevent causing
excessive strain to the
heart (Liew et al.,
2013).
possibly acquiring an
infection (Colao et al.,
2014)
Closely monitor
electrolyte and fluid
balance
Closely monitor the
vital signs to detect
higher blood pressure
or other
abnormalities
The intervention to
manage electrolyte and
fluid balance would
include regulating fluid
restrictions (I & O) as
and when necessary
Conduct vital
assessment and
document patient
assessment
Studies reveal that on
account of the high
level production of
Cortisol in the body,
the body develops the
tendency to retain
Sodium and Water
which can
subsequently lead to
cardiac stress or even
hypokalemia (Kargi &
Iacobellis, 2014)
Research studies
suggests that elevated
level of Cortisol
hormone in the body
leads to hypertension
which can potentially
increase the risk of a
cardiac stroke (Duan et
al., 2015)
Mange the symptoms
of the patient and
administer
appropriate
medication.
Consider the
symptoms of high
blood pressure and
high blood glucose
level.
Intervention for
managing hypertension
or high blood pressure
would include,
administration of
antihypertensives and
diuretics
On the other hand,
intervention for
managing high blood
glucose level would
include consulting the
physician and using
juice to treat
hypoglycemia
The excess level of the
stress hormone
Cortisol in the blood
leads to an elevation of
the blood pressure
level. Studies suggest
that administration of
antihypertensives can
help in changing the
cortisol level and help
in down regulating the
blood pressure within
the normal range. On
the other hand,
administration of
Diuretics has been
studied to promote
fluid retention and
prevent causing
excessive strain to the
heart (Liew et al.,
2013).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

7NURSING ASSIGNMENT
A high level of the
cortisol hormone has
been studied to cause
fluctuation in the blood
glucose level
(Giordano et al., 2014).
Continuous monitoring
of the blood glucose
level can help in
keeping a track of the
blood glucose reading
of the patient. Also, in
case the patient
experiences
hypoglycemia,
immediate intervention
in the form of a glass
of juice or a sweet
could help in
controlling the
situation. This is
important as it has
already been
mentioned in the case
study that the patient is
suffering from Type II
Diabetes. However,
studies also
recommend that the
patient must be
observed for rapid
spikes after an initial
episode of
hypoglycemia.
In addition to this, in
case the patient
experiences an episode
of hyperglycemia, the
immediate intervention
should include making
the patient drink water.
Also, the fluctuation in
the blood sugar level
must be documented
and immediately
conveyed to the
A high level of the
cortisol hormone has
been studied to cause
fluctuation in the blood
glucose level
(Giordano et al., 2014).
Continuous monitoring
of the blood glucose
level can help in
keeping a track of the
blood glucose reading
of the patient. Also, in
case the patient
experiences
hypoglycemia,
immediate intervention
in the form of a glass
of juice or a sweet
could help in
controlling the
situation. This is
important as it has
already been
mentioned in the case
study that the patient is
suffering from Type II
Diabetes. However,
studies also
recommend that the
patient must be
observed for rapid
spikes after an initial
episode of
hypoglycemia.
In addition to this, in
case the patient
experiences an episode
of hyperglycemia, the
immediate intervention
should include making
the patient drink water.
Also, the fluctuation in
the blood sugar level
must be documented
and immediately
conveyed to the

8NURSING ASSIGNMENT
physician for a
possible change in the
dose of the prescribed
medication routine or a
change in the
medication.
physician for a
possible change in the
dose of the prescribed
medication routine or a
change in the
medication.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

9NURSING ASSIGNMENT
References:
Betterhealth.vic.gov.au (2019). Cushing's syndrome. [online] Betterhealth.vic.gov.au. Available
at: https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/cushings-
syndrome [Accessed 26 Mar. 2019].
Colao, A., De Block, C., Gaztambide, M. S., Kumar, S., Seufert, J., & Casanueva, F. F. (2014).
Managing hyperglycemia in patients with Cushing’s disease treated with pasireotide:
medical expert recommendations. Pituitary, 17(2), 180-186.
Drugbank.ca (2019). Mitotane - DrugBank. [online] Drugbank.ca. Available at:
https://www.drugbank.ca/drugs/DB00648 [Accessed 26 Mar. 2019].
Duan, K., Hernandez, K. G., & Mete, O. (2015). Republished: Clinicopathological correlates of
adrenal Cushing's syndrome. Postgraduate medical journal, 91(1076), 331-342.
Giordano, C., Guarnotta, V., Pivonello, R., Amato, M. C., Simeoli, C., Ciresi, A., ... & Colao, A.
(2014). Is diabetes in Cushing's syndrome only a consequence of
hypercortisolism?. European journal of endocrinology, 170(2), 311-319.
Kargi, A. Y., & Iacobellis, G. (2014). Adipose tissue and adrenal glands: novel
pathophysiological mechanisms and clinical applications. International journal of
endocrinology, 2014.
Lacroix, A., Feelders, R. A., Stratakis, C. A., & Nieman, L. K. (2015). Cushing's syndrome. The
lancet, 386(9996), 913-927.
References:
Betterhealth.vic.gov.au (2019). Cushing's syndrome. [online] Betterhealth.vic.gov.au. Available
at: https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/cushings-
syndrome [Accessed 26 Mar. 2019].
Colao, A., De Block, C., Gaztambide, M. S., Kumar, S., Seufert, J., & Casanueva, F. F. (2014).
Managing hyperglycemia in patients with Cushing’s disease treated with pasireotide:
medical expert recommendations. Pituitary, 17(2), 180-186.
Drugbank.ca (2019). Mitotane - DrugBank. [online] Drugbank.ca. Available at:
https://www.drugbank.ca/drugs/DB00648 [Accessed 26 Mar. 2019].
Duan, K., Hernandez, K. G., & Mete, O. (2015). Republished: Clinicopathological correlates of
adrenal Cushing's syndrome. Postgraduate medical journal, 91(1076), 331-342.
Giordano, C., Guarnotta, V., Pivonello, R., Amato, M. C., Simeoli, C., Ciresi, A., ... & Colao, A.
(2014). Is diabetes in Cushing's syndrome only a consequence of
hypercortisolism?. European journal of endocrinology, 170(2), 311-319.
Kargi, A. Y., & Iacobellis, G. (2014). Adipose tissue and adrenal glands: novel
pathophysiological mechanisms and clinical applications. International journal of
endocrinology, 2014.
Lacroix, A., Feelders, R. A., Stratakis, C. A., & Nieman, L. K. (2015). Cushing's syndrome. The
lancet, 386(9996), 913-927.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

10NURSING ASSIGNMENT
Liew, G., Quin, G., Gillies, M., & Fraser‐Bell, S. (2013). Central serous chorioretinopathy: a
review of epidemiology and pathophysiology. Clinical & experimental
ophthalmology, 41(2), 201-214.
Nieman, L. K., Biller, B. M., Findling, J. W., Murad, M. H., Newell-Price, J., Savage, M. O., &
Tabarin, A. (2015). Treatment of Cushing's syndrome: an endocrine society clinical
practice guideline. The Journal of Clinical Endocrinology & Metabolism, 100(8), 2807-
2831.
Raff, H., & Carroll, T. (2015). Cushing's syndrome: from physiological principles to diagnosis
and clinical care. The Journal of physiology, 593(3), 493-506.
Starkman, M. N. (2013). Neuropsychiatric findings in Cushing syndrome and exogenous
glucocorticoid administration. Endocrinology and Metabolism Clinics, 42(3), 477-488.
Tchernof, A., & Després, J. P. (2013). Pathophysiology of human visceral obesity: an
update. Physiological reviews, 93(1), 359-404.
Liew, G., Quin, G., Gillies, M., & Fraser‐Bell, S. (2013). Central serous chorioretinopathy: a
review of epidemiology and pathophysiology. Clinical & experimental
ophthalmology, 41(2), 201-214.
Nieman, L. K., Biller, B. M., Findling, J. W., Murad, M. H., Newell-Price, J., Savage, M. O., &
Tabarin, A. (2015). Treatment of Cushing's syndrome: an endocrine society clinical
practice guideline. The Journal of Clinical Endocrinology & Metabolism, 100(8), 2807-
2831.
Raff, H., & Carroll, T. (2015). Cushing's syndrome: from physiological principles to diagnosis
and clinical care. The Journal of physiology, 593(3), 493-506.
Starkman, M. N. (2013). Neuropsychiatric findings in Cushing syndrome and exogenous
glucocorticoid administration. Endocrinology and Metabolism Clinics, 42(3), 477-488.
Tchernof, A., & Després, J. P. (2013). Pathophysiology of human visceral obesity: an
update. Physiological reviews, 93(1), 359-404.
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





