University Nursing Assignment: Hand Hygiene and Infection Reduction
VerifiedAdded on 2023/04/20
|16
|3918
|161
Report
AI Summary
This nursing assignment explores the impact of hand hygiene on reducing infection rates in hospitals. The research employs a qualitative study design, interviewing five nursing professionals to analyze the effectiveness of hand hygiene practices. The study investigates the correlation between hand hygiene compliance and infection rates, highlighting the obstacles nurses face in adhering to hand hygiene protocols. Key themes emerging from the research include the prioritization of patient care, which can sometimes compromise hand hygiene routines, and the positive impact of incorporating training programs to improve compliance. The literature review supports the significance of hand hygiene, referencing studies on the reduction of hospital-acquired infections. The report also outlines a four-step project framework, including identifying research gaps, formulating research questions, selecting study designs, and data analysis. The findings emphasize the need for effective training and stringent infection control policies to enhance hand hygiene practices among healthcare professionals. The assignment underscores the vital role of hand hygiene in preventing the transmission of infections within healthcare settings, supporting patient safety, and improving overall healthcare outcomes.

Running head: NURSING ASSIGNMENT
NURSING ASSIGNMENT
Name of the Student:
Name of the University:
Author Note:
NURSING ASSIGNMENT
Name of the Student:
Name of the University:
Author Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

1NURSING ASSIGNMENT
Abstract:
This research project deals with the evaluation of the impact of hand hygiene on the reduction
of infection rate across hospital settings. A number of studies have revealed the positive
impact of effective hand hygiene on reduced rate of infection but the compliance rate with the
hand hygiene routine is significantly low among the nursing professionals. To analyze the
underlying reason for lower rate of compliance a qualitative research study design was
adapted. Five nursing professionals were interviewed by the researcher, who were asked a
total of 5 semi-structured questions. The findings revealed two important themes, patient
priority leads to compromise with HH routine and incorporation of training helps in effective
compliance with HH among professionals. Hence, to conclude it can be said that with
effective training and stringent infection control policies professionals can be trained to
comply with hand hygiene practices.
Abstract:
This research project deals with the evaluation of the impact of hand hygiene on the reduction
of infection rate across hospital settings. A number of studies have revealed the positive
impact of effective hand hygiene on reduced rate of infection but the compliance rate with the
hand hygiene routine is significantly low among the nursing professionals. To analyze the
underlying reason for lower rate of compliance a qualitative research study design was
adapted. Five nursing professionals were interviewed by the researcher, who were asked a
total of 5 semi-structured questions. The findings revealed two important themes, patient
priority leads to compromise with HH routine and incorporation of training helps in effective
compliance with HH among professionals. Hence, to conclude it can be said that with
effective training and stringent infection control policies professionals can be trained to
comply with hand hygiene practices.
2NURSING ASSIGNMENT
Table of Contents
Research Question:.....................................................................................................................3
Literature Review:......................................................................................................................3
Relevance to nursing knowledge:..............................................................................................4
Research Gap:............................................................................................................................5
Project Framework:....................................................................................................................5
Method of data-collection:.........................................................................................................6
Method of data-analysis:............................................................................................................6
Findings of research:..................................................................................................................7
Conclusion:................................................................................................................................7
References:.................................................................................................................................8
Table of Contents
Research Question:.....................................................................................................................3
Literature Review:......................................................................................................................3
Relevance to nursing knowledge:..............................................................................................4
Research Gap:............................................................................................................................5
Project Framework:....................................................................................................................5
Method of data-collection:.........................................................................................................6
Method of data-analysis:............................................................................................................6
Findings of research:..................................................................................................................7
Conclusion:................................................................................................................................7
References:.................................................................................................................................8
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3NURSING ASSIGNMENT
Research Question:
Whether hand-hygiene can effectively help in the reduction of communicable
infections within hospital setting (I: Intervention)among nursing professionals (P:
Population)in order to effectively acquire positive patient outcome and reduce the possibility
of in-hospital infections.
Literature Review:
According to Castle et al. (2014), it has been mentioned that 1 out of 10 patients
experience nosocomial infection during the tenure of their hospital stay. It has further been
estimated that, approximately 1.4 million people suffer from Health-care associated
infections (HAI) every year on account of poor hygiene practices at hospitals (Castle et al.,
2014). It should be critically noted in this context that, hospital acquired infection contribute
to a cumulative of 1.7 million infections and almost 99,000 death every year (Ariyaratne et
al., 2015). As mentioned by Allegranzi et al.(2013), healthcare associated infections can be
defined as infections that patients invariably acquire while receiving treatment for their
medical condition. The infections are preventable and are mainly transmitted to the patients
during surgical procedures and through medical equipment that include catheters, syringes,
surgical instruments and ventilators. As stated by Chun et al. (2015), HAIs account for a
major proportion of morbidity and mortality cases across the United States of America.
Further, it has been stated that at any point of time, 1 out of 25 hospitalized patients are
affected by an infection worldwide (Cruz & Bashtawi, 2016) . In general, health-associated
infections occur across a multitude of hospital settings that include, Acute care hospitals,
Ambulatory surgical centres, Dialysis facilities, Outpatient care unit and Long-term care
facilities (Gould et al., 2017). In order to address the emerging health concern, the U.S
department of Health and Human Services, has laid down healthcare-associated infection
Research Question:
Whether hand-hygiene can effectively help in the reduction of communicable
infections within hospital setting (I: Intervention)among nursing professionals (P:
Population)in order to effectively acquire positive patient outcome and reduce the possibility
of in-hospital infections.
Literature Review:
According to Castle et al. (2014), it has been mentioned that 1 out of 10 patients
experience nosocomial infection during the tenure of their hospital stay. It has further been
estimated that, approximately 1.4 million people suffer from Health-care associated
infections (HAI) every year on account of poor hygiene practices at hospitals (Castle et al.,
2014). It should be critically noted in this context that, hospital acquired infection contribute
to a cumulative of 1.7 million infections and almost 99,000 death every year (Ariyaratne et
al., 2015). As mentioned by Allegranzi et al.(2013), healthcare associated infections can be
defined as infections that patients invariably acquire while receiving treatment for their
medical condition. The infections are preventable and are mainly transmitted to the patients
during surgical procedures and through medical equipment that include catheters, syringes,
surgical instruments and ventilators. As stated by Chun et al. (2015), HAIs account for a
major proportion of morbidity and mortality cases across the United States of America.
Further, it has been stated that at any point of time, 1 out of 25 hospitalized patients are
affected by an infection worldwide (Cruz & Bashtawi, 2016) . In general, health-associated
infections occur across a multitude of hospital settings that include, Acute care hospitals,
Ambulatory surgical centres, Dialysis facilities, Outpatient care unit and Long-term care
facilities (Gould et al., 2017). In order to address the emerging health concern, the U.S
department of Health and Human Services, has laid down healthcare-associated infection
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4NURSING ASSIGNMENT
objectives for the promotion of health and well-being (Gould et al., 2017). The high-priority
objectives intend to prevent infections caused by methicillin-resistant Staphylococcus aureus
and central line associated bloodstream infections (Higgins & Hannan, 2013). In this regard,
it should be mentioned that the most common type of health associated infections include,
catheter-associated urinary tract infections, surgical site infections, bloodstream infections,
Pneumonia and Clostridium difficile (Chun et al., 2015). HAIs pose an increased risk of
developing complications within the care facility and at the same time also possesses the
potential to transmit from one unit to another (Huis et al., 2014). However, it is interesting to
note in this context, that studies have suggested that proper implementation of preventive
practices can help in reducing the rate of infection to almost 70% (Liu et al., 204). The Work
Health and Safety Act 2011, aims at the prevention of harm caused to the health, safety and
welfare of the care providers (Huis et al., 2013). In context to the healthcare sector, the act
considers the implementation of infection control measures. Implementation of effective
infection control such as hand hygiene is essential to maintain a reduced incidence of
infection. It should be mentioned in this regard that, between 1977 and 2011, a total of 20
studies have been conducted at hospital based setting that clearly indicated a direct co-
relation between the impact of hand hygiene and infection rate (Luangasanatip et al., 2015).
Further, some of the studies mentioned that improved hand hygiene led to reduced rate of
infection and transmission of the infection. Studies have further revealed that, use of alcohol
based hand rub can reduce the infection rate but is less effective in comparison to increased
hand washing compliance. A number of research studies have revealed that improved hand
hygiene can prevent the rate of infection caused by microorganisms. The most common
microorganisms that cause infection include, bacteria, fungus and viruses. While 90% of the
infections are caused by bacteria, the remaining 10% are caused by viruses and fungi
(Maheshwari, 2014, Huis et al., 2013). Staphylococcus aureus, Escherichia coli, Enterococci
objectives for the promotion of health and well-being (Gould et al., 2017). The high-priority
objectives intend to prevent infections caused by methicillin-resistant Staphylococcus aureus
and central line associated bloodstream infections (Higgins & Hannan, 2013). In this regard,
it should be mentioned that the most common type of health associated infections include,
catheter-associated urinary tract infections, surgical site infections, bloodstream infections,
Pneumonia and Clostridium difficile (Chun et al., 2015). HAIs pose an increased risk of
developing complications within the care facility and at the same time also possesses the
potential to transmit from one unit to another (Huis et al., 2014). However, it is interesting to
note in this context, that studies have suggested that proper implementation of preventive
practices can help in reducing the rate of infection to almost 70% (Liu et al., 204). The Work
Health and Safety Act 2011, aims at the prevention of harm caused to the health, safety and
welfare of the care providers (Huis et al., 2013). In context to the healthcare sector, the act
considers the implementation of infection control measures. Implementation of effective
infection control such as hand hygiene is essential to maintain a reduced incidence of
infection. It should be mentioned in this regard that, between 1977 and 2011, a total of 20
studies have been conducted at hospital based setting that clearly indicated a direct co-
relation between the impact of hand hygiene and infection rate (Luangasanatip et al., 2015).
Further, some of the studies mentioned that improved hand hygiene led to reduced rate of
infection and transmission of the infection. Studies have further revealed that, use of alcohol
based hand rub can reduce the infection rate but is less effective in comparison to increased
hand washing compliance. A number of research studies have revealed that improved hand
hygiene can prevent the rate of infection caused by microorganisms. The most common
microorganisms that cause infection include, bacteria, fungus and viruses. While 90% of the
infections are caused by bacteria, the remaining 10% are caused by viruses and fungi
(Maheshwari, 2014, Huis et al., 2013). Staphylococcus aureus, Escherichia coli, Enterococci
5NURSING ASSIGNMENT
and Pseudomonas aeruginosa are the most common types of bacteria that cause medical
infections (Gould et al., 2017). Infections caused by microorganisms have the potential to
spread from one individual to another through contact. Contact here refers to unclean hands
and handling contaminated surgical instruments and hospital equipment. Contact does not
necessarily refer to touching an infected person but also includes touching an infected door or
handle that could spread the infection to a normal patient. Cross contamination is also another
method through which infection can spread. The process of cross-contamination is a
multistep process and includes a number of steps that comprises of the following (Nair et al.,
2014):
Presence of organisms wither on the skin or inanimate objects
The transfer of infectious agent to the hands of the healthcare worker
The organisms have the tendency to survive on the skin for several minutes
Inadequate and ineffective hand hygiene, that causes the organism to remain on the
skin
Direct contact with a normal patient and transmission of the infection
The possibility of transmission of infection does not remain restricted to hospitals but also
includes aged care facilities and community nursing homes. Microorganisms such as bacteria
are typically found on the hands of the care providers who engage themselves in dressing of
wound and handle patient secretions (Shinde & Mohite, 2014). In fact presence of bacteria
has also been detected after the completion of clean procedures such as checking blood
pressure or checking pulse of the patient. Studies reveal that the correct procedure of hand
washing and maintenance of hand hygiene must include five moments. The moments include;
observing hand hygiene before touching a patient, prior to a procedure, after a procedure is
performed or exposure of body fluid, after touching a patient and after touching the
surroundings of a patient (Shinde & Mohite, 2014). This clearly is against the common notion
and Pseudomonas aeruginosa are the most common types of bacteria that cause medical
infections (Gould et al., 2017). Infections caused by microorganisms have the potential to
spread from one individual to another through contact. Contact here refers to unclean hands
and handling contaminated surgical instruments and hospital equipment. Contact does not
necessarily refer to touching an infected person but also includes touching an infected door or
handle that could spread the infection to a normal patient. Cross contamination is also another
method through which infection can spread. The process of cross-contamination is a
multistep process and includes a number of steps that comprises of the following (Nair et al.,
2014):
Presence of organisms wither on the skin or inanimate objects
The transfer of infectious agent to the hands of the healthcare worker
The organisms have the tendency to survive on the skin for several minutes
Inadequate and ineffective hand hygiene, that causes the organism to remain on the
skin
Direct contact with a normal patient and transmission of the infection
The possibility of transmission of infection does not remain restricted to hospitals but also
includes aged care facilities and community nursing homes. Microorganisms such as bacteria
are typically found on the hands of the care providers who engage themselves in dressing of
wound and handle patient secretions (Shinde & Mohite, 2014). In fact presence of bacteria
has also been detected after the completion of clean procedures such as checking blood
pressure or checking pulse of the patient. Studies reveal that the correct procedure of hand
washing and maintenance of hand hygiene must include five moments. The moments include;
observing hand hygiene before touching a patient, prior to a procedure, after a procedure is
performed or exposure of body fluid, after touching a patient and after touching the
surroundings of a patient (Shinde & Mohite, 2014). This clearly is against the common notion
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6NURSING ASSIGNMENT
that states observing hand hygiene is only important after direct contact with the patients.
Observing hand hygiene is important on many other occasions and according to the WHO
guidelines is an integral procedure that healthcare professionals must comply with. It is
critical to note in this context, that despite the underlying importance of observing hand
hygiene, healthcare professionals encounter a large number of obstacles that prevent the
professionals from complying with the standard routine of hand hygiene (Salamati et al.,
2013). The prevalent perception about patient priority over hand hygiene, and gloves being
an effective barrier that prevent the transmission of infection serve as obstacles that prevent
care providers to comply with hand hygiene technique.
Relevance to nursing knowledge:
Hand hygiene can be defined as the single most important tool that effectively helps
in the transmission of the infections between the patients and professionals (Nair et al., 2014).
As stated by WHO, a few definitive data on patient studies have identified a number of
patient-care activities that can possibly lead to the transmission of the infection (Salamti et
al., 2013). Majorly, presence of bacteria have been detected in the hands of the hands of the
healthcare workers after activities like wound care dressing, intravascular catheter care,
respiratory tract care and handling body fluid or secretions. In addition to this, presence of
bacteria have also detected on the hands of the care providers after clean contact that
comprises of activities such as recording patient temperature, pulse or blood pressure.
According to Shinde and Mohite (2014), hand washing technique is the most effective
method of reducing the incidence of infections as it works effectively on a broad range of
microorganisms. Studies have reported that effective compliance with hand hygiene
technique can help in the reduction of infection rate by an impressive 60% (Luangasanatip et
al., 2015). Therefore, it can be said that the importance of hand hygiene has been proven to
that states observing hand hygiene is only important after direct contact with the patients.
Observing hand hygiene is important on many other occasions and according to the WHO
guidelines is an integral procedure that healthcare professionals must comply with. It is
critical to note in this context, that despite the underlying importance of observing hand
hygiene, healthcare professionals encounter a large number of obstacles that prevent the
professionals from complying with the standard routine of hand hygiene (Salamati et al.,
2013). The prevalent perception about patient priority over hand hygiene, and gloves being
an effective barrier that prevent the transmission of infection serve as obstacles that prevent
care providers to comply with hand hygiene technique.
Relevance to nursing knowledge:
Hand hygiene can be defined as the single most important tool that effectively helps
in the transmission of the infections between the patients and professionals (Nair et al., 2014).
As stated by WHO, a few definitive data on patient studies have identified a number of
patient-care activities that can possibly lead to the transmission of the infection (Salamti et
al., 2013). Majorly, presence of bacteria have been detected in the hands of the hands of the
healthcare workers after activities like wound care dressing, intravascular catheter care,
respiratory tract care and handling body fluid or secretions. In addition to this, presence of
bacteria have also detected on the hands of the care providers after clean contact that
comprises of activities such as recording patient temperature, pulse or blood pressure.
According to Shinde and Mohite (2014), hand washing technique is the most effective
method of reducing the incidence of infections as it works effectively on a broad range of
microorganisms. Studies have reported that effective compliance with hand hygiene
technique can help in the reduction of infection rate by an impressive 60% (Luangasanatip et
al., 2015). Therefore, it can be said that the importance of hand hygiene has been proven to
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7NURSING ASSIGNMENT
be effective by different researchers, but at the same time on account of lower compliance,
the infection rate is yet to be controlled to an appropriate percentage.
Research Gap:
Therefore, on the basis of the exhaustive literature review, it can be said thata
significant number of papers have talked about the efficacy of maintenance of hand hygiene
and its positive implication on the reduction of the infection. It was typically revealed that
ineffective and improper hand washing technique has resulted in an increase in the hospital
based infection rate among the patients. The literature review vividly described the five
important instances that have been identified as the moments that can lead to the transmission
of the infection. The review also highlighted the important WHO guidelines that list the hand
washing routine that must be followed by the care professionals (Salamati et al., 2013).
However, it should be noted that despite the effectiveness of the hand hygiene technique on
the reduction of infection, the technique is yet to be assimilated within the healthcare sector
(Ariyaratne et al., 2015). A major gap has been identified in terms of attitude and perception
of care professionals towards compliance with hand hygiene. None of the papers in the
literature review talked about the obstacles that professionals encounter while dealing with
patients that restricts them from complying with the hand hygiene procedure. Also, none of
the papers focused on the imparting training and knowledge about the efficacy of hand
hygiene to the health care professionals.
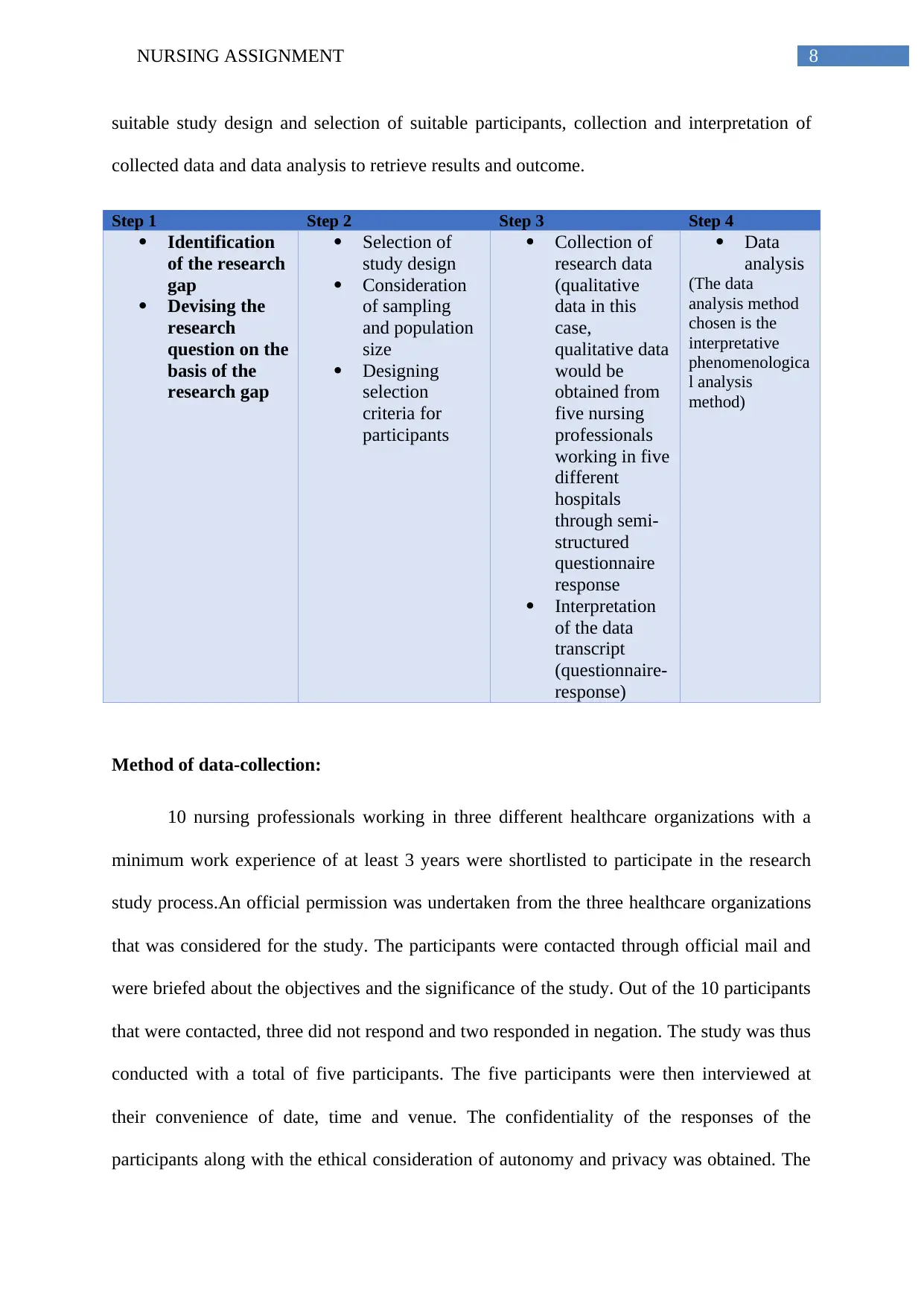
Project Framework:
The project framework that would be followed in order to address the research
question appropriately would include four major steps. The four steps would broadly
comprise of identification of the research gap and framing a research question, adapting a
be effective by different researchers, but at the same time on account of lower compliance,
the infection rate is yet to be controlled to an appropriate percentage.
Research Gap:
Therefore, on the basis of the exhaustive literature review, it can be said thata
significant number of papers have talked about the efficacy of maintenance of hand hygiene
and its positive implication on the reduction of the infection. It was typically revealed that
ineffective and improper hand washing technique has resulted in an increase in the hospital
based infection rate among the patients. The literature review vividly described the five
important instances that have been identified as the moments that can lead to the transmission
of the infection. The review also highlighted the important WHO guidelines that list the hand
washing routine that must be followed by the care professionals (Salamati et al., 2013).
However, it should be noted that despite the effectiveness of the hand hygiene technique on
the reduction of infection, the technique is yet to be assimilated within the healthcare sector
(Ariyaratne et al., 2015). A major gap has been identified in terms of attitude and perception
of care professionals towards compliance with hand hygiene. None of the papers in the
literature review talked about the obstacles that professionals encounter while dealing with
patients that restricts them from complying with the hand hygiene procedure. Also, none of
the papers focused on the imparting training and knowledge about the efficacy of hand
hygiene to the health care professionals.
Project Framework:
The project framework that would be followed in order to address the research
question appropriately would include four major steps. The four steps would broadly
comprise of identification of the research gap and framing a research question, adapting a
8NURSING ASSIGNMENT
suitable study design and selection of suitable participants, collection and interpretation of
collected data and data analysis to retrieve results and outcome.
Step 1 Step 2 Step 3 Step 4
Identification
of the research
gap
Devising the
research
question on the
basis of the
research gap
Selection of
study design
Consideration
of sampling
and population
size
Designing
selection
criteria for
participants
Collection of
research data
(qualitative
data in this
case,
qualitative data
would be
obtained from
five nursing
professionals
working in five
different
hospitals
through semi-
structured
questionnaire
response
Interpretation
of the data
transcript
(questionnaire-
response)
Data
analysis
(The data
analysis method
chosen is the
interpretative
phenomenologica
l analysis
method)
Method of data-collection:
10 nursing professionals working in three different healthcare organizations with a
minimum work experience of at least 3 years were shortlisted to participate in the research
study process.An official permission was undertaken from the three healthcare organizations
that was considered for the study. The participants were contacted through official mail and
were briefed about the objectives and the significance of the study. Out of the 10 participants
that were contacted, three did not respond and two responded in negation. The study was thus
conducted with a total of five participants. The five participants were then interviewed at
their convenience of date, time and venue. The confidentiality of the responses of the
participants along with the ethical consideration of autonomy and privacy was obtained. The
suitable study design and selection of suitable participants, collection and interpretation of
collected data and data analysis to retrieve results and outcome.
Step 1 Step 2 Step 3 Step 4
Identification
of the research
gap
Devising the
research
question on the
basis of the
research gap
Selection of
study design
Consideration
of sampling
and population
size
Designing
selection
criteria for
participants
Collection of
research data
(qualitative
data in this
case,
qualitative data
would be
obtained from
five nursing
professionals
working in five
different
hospitals
through semi-
structured
questionnaire
response
Interpretation
of the data
transcript
(questionnaire-
response)
Data
analysis
(The data
analysis method
chosen is the
interpretative
phenomenologica
l analysis
method)
Method of data-collection:
10 nursing professionals working in three different healthcare organizations with a
minimum work experience of at least 3 years were shortlisted to participate in the research
study process.An official permission was undertaken from the three healthcare organizations
that was considered for the study. The participants were contacted through official mail and
were briefed about the objectives and the significance of the study. Out of the 10 participants
that were contacted, three did not respond and two responded in negation. The study was thus
conducted with a total of five participants. The five participants were then interviewed at
their convenience of date, time and venue. The confidentiality of the responses of the
participants along with the ethical consideration of autonomy and privacy was obtained. The
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9NURSING ASSIGNMENT
interview comprised of five questions and lasted for a period of ten minutes and the interview
was recorded using an audio recorder which was later transcribed into a hard copy format for
data interpretation.
Method of data-analysis:
The method used for analysing the data was qualitative data analysis. The interview
transcript was read and re-read a number of times in order to highlight important excerpts and
connect them to meaningful themes that were aligned to the aim of the research. This method
is known as the interpretive phenomenological analysis and is best suited for analyzing semi-
structured interviews (Smiddy et al., 2015). It helps in building new theories on existing one.
Theme 1: Patient priority leads to compromise with effective hand hygiene practices
Nurse 1: “Prioritizing patient becomes primary and many a times the routine is missed”
Nurse 2: “I think HH is not that important if I am using alcohol swabs”
Nurse 3: “HH is extremely important and it should be followed irrespective of using gloves”
Nurse 4: “If I am using gloves already, HH is secondary”
Nurse 5: “I think it is a waste of time and cuts down on the time given to the patient.”
Theme 2: Training helps in effective compliance with hand hygiene
Nurse 1: “HH training is important and helps in reducing the transmission of infection”
Nurse 2: “Training helps us in identifying events that require HH”
Nurse 3: “I am not aware of any such training”
Nurse 4: “Training is important and should be mandatory for professionals to follow”
Nurse 5: “I do not think you need training for that”
interview comprised of five questions and lasted for a period of ten minutes and the interview
was recorded using an audio recorder which was later transcribed into a hard copy format for
data interpretation.
Method of data-analysis:
The method used for analysing the data was qualitative data analysis. The interview
transcript was read and re-read a number of times in order to highlight important excerpts and
connect them to meaningful themes that were aligned to the aim of the research. This method
is known as the interpretive phenomenological analysis and is best suited for analyzing semi-
structured interviews (Smiddy et al., 2015). It helps in building new theories on existing one.
Theme 1: Patient priority leads to compromise with effective hand hygiene practices
Nurse 1: “Prioritizing patient becomes primary and many a times the routine is missed”
Nurse 2: “I think HH is not that important if I am using alcohol swabs”
Nurse 3: “HH is extremely important and it should be followed irrespective of using gloves”
Nurse 4: “If I am using gloves already, HH is secondary”
Nurse 5: “I think it is a waste of time and cuts down on the time given to the patient.”
Theme 2: Training helps in effective compliance with hand hygiene
Nurse 1: “HH training is important and helps in reducing the transmission of infection”
Nurse 2: “Training helps us in identifying events that require HH”
Nurse 3: “I am not aware of any such training”
Nurse 4: “Training is important and should be mandatory for professionals to follow”
Nurse 5: “I do not think you need training for that”
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10NURSING ASSIGNMENT
Findings of research:
Therefore, it can be stated that the findings of the research has significantly
highlighted two important themes that include: patient priority leads to compromise with HH
routine and incorporation of training helps in effective compliance with HH among
professionals. Hence, it can be said that with effective training and stringent infection control
policies professionals can be trained to comply with hand hygiene practices.
Conclusion:
Therefore, on the basis of the discussion it can be said that the research study could
properly address the research question. Further, the study helped in the identification of the
underlying reasons that serve as barriers for professionals to comply with HH practices. Also,
it can be said that implementation of effective training programs can help in significant
infection control.
Findings of research:
Therefore, it can be stated that the findings of the research has significantly
highlighted two important themes that include: patient priority leads to compromise with HH
routine and incorporation of training helps in effective compliance with HH among
professionals. Hence, it can be said that with effective training and stringent infection control
policies professionals can be trained to comply with hand hygiene practices.
Conclusion:
Therefore, on the basis of the discussion it can be said that the research study could
properly address the research question. Further, the study helped in the identification of the
underlying reasons that serve as barriers for professionals to comply with HH practices. Also,
it can be said that implementation of effective training programs can help in significant
infection control.
11NURSING ASSIGNMENT
References:
Allegranzi, B., Gayet-Ageron, A., Damani, N., Bengaly, L., McLaws, M. L., Moro, M. L., ...
& Donaldson, L. (2013). Global implementation of WHO's multimodal strategy for
improvement of hand hygiene: a quasi-experimental study. The Lancet infectious
diseases, 13(10), 843-851.
Ariyaratne, M. H. J. D., Gunasekara, T. D. C. P., Weerasekara, M. M., Kottahachchi, J.,
Kudavidanage, B. P., & Fernando, S. S. N. (2015). Knowledge, attitudes and practices
of hand hygiene among final year medical and nursing students at the University of
Sri Jayewardenepura.
Castle, N., Wagner, L., Ferguson, J., & Handler, S. (2014). Hand hygiene deficiency citations
in nursing homes. Journal of Applied Gerontology, 33(1), 24-50.
References:
Allegranzi, B., Gayet-Ageron, A., Damani, N., Bengaly, L., McLaws, M. L., Moro, M. L., ...
& Donaldson, L. (2013). Global implementation of WHO's multimodal strategy for
improvement of hand hygiene: a quasi-experimental study. The Lancet infectious
diseases, 13(10), 843-851.
Ariyaratne, M. H. J. D., Gunasekara, T. D. C. P., Weerasekara, M. M., Kottahachchi, J.,
Kudavidanage, B. P., & Fernando, S. S. N. (2015). Knowledge, attitudes and practices
of hand hygiene among final year medical and nursing students at the University of
Sri Jayewardenepura.
Castle, N., Wagner, L., Ferguson, J., & Handler, S. (2014). Hand hygiene deficiency citations
in nursing homes. Journal of Applied Gerontology, 33(1), 24-50.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 16
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





