Critical Investigation of Evidence-Based Practice for Gastrointestinal Tube Placement in Nursing
VerifiedAdded on 2023/04/25
|17
|5140
|340
Assignment
AI Summary
In this assignment we will discuss about nursing assignment and below are the summaries point:-
Evidence-Based Practice: The paper critically investigates evidence-based practice in determining correct gastrointestinal tube placement.
Potential Barriers: The study identifies barriers to implementing evidence-based practice in healthcare settings.
Recommendations: The paper proposes recommendations to overcome barriers and promote positive patient outcomes in tube placement.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: NURSING ASSIGNMENT
NURSING ASSIGNMENT
Name of the Student:
Name of the University:
Author Note:
NURSING ASSIGNMENT
Name of the Student:
Name of the University:
Author Note:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1NURSING ASSIGNMENT
According to Stevens (2013), Evidence Based Practice can be defined as the process
of making use of the explicit and recent evidence base that is available in order to make
decisions in the best interest of the patient. The nursing profession widely relies upon making
use of the evidence based practice in order to undertake effective clinical decisions and
promote effective patient care (Nursing and Midwifery Council 2015). In this regard, it
should be mentioned that this paper intends to critically investigate the evidence base in order
to identify the best practice for determining the correct placement of the gastrointestinal
tube. In addition to this, the paper would also identify the potential barriers that hinder the
implementation of the best evidence based practice within a healthcare setting. It should also
be noted that the paper would propose a set of recommendations that could be applied in
order to overcome the potential barriers within the healthcare setting and effectively make
use of the best evidence based practice so as to promote positive patient outcomes.
A gastrointestinal tube which is also known as the enema tube or the feeding tube is
used in a condition where the patient is experiencing difficulty in feeding and normal bowel
movement (Baker et al. 2015). The procedure for the placement of the NG tube requires
Nurses to gather the equipment and use non-sterile gloves. The next step includes providing
health literacy to the patient about the procedure. The patient is then made to sit upright to
obtain neck, stomach alignment. The next step requires the nurses to measure tubing from the
nose to earlobe and then at a halfway distance between the end of sternum and navel. The
distance is then marked and recorded. The next step involves lubrication of the tube up to 2 to
4 inches with 2% Xylocaine (Nursing and Midwifery Council, 2015). This process causes
inconvenience to the patients and therefore nurses should apply Xylocaine jelly within the
nostril and spray Xylocaine at the back side of the throat. The tube should then be passed
posteriorly through the nare, past the parynx, into the oesophagus to the stomach. The patient
must be offered chips or water as it facilitates entry of the tube into the oesophagus. Care
According to Stevens (2013), Evidence Based Practice can be defined as the process
of making use of the explicit and recent evidence base that is available in order to make
decisions in the best interest of the patient. The nursing profession widely relies upon making
use of the evidence based practice in order to undertake effective clinical decisions and
promote effective patient care (Nursing and Midwifery Council 2015). In this regard, it
should be mentioned that this paper intends to critically investigate the evidence base in order
to identify the best practice for determining the correct placement of the gastrointestinal
tube. In addition to this, the paper would also identify the potential barriers that hinder the
implementation of the best evidence based practice within a healthcare setting. It should also
be noted that the paper would propose a set of recommendations that could be applied in
order to overcome the potential barriers within the healthcare setting and effectively make
use of the best evidence based practice so as to promote positive patient outcomes.
A gastrointestinal tube which is also known as the enema tube or the feeding tube is
used in a condition where the patient is experiencing difficulty in feeding and normal bowel
movement (Baker et al. 2015). The procedure for the placement of the NG tube requires
Nurses to gather the equipment and use non-sterile gloves. The next step includes providing
health literacy to the patient about the procedure. The patient is then made to sit upright to
obtain neck, stomach alignment. The next step requires the nurses to measure tubing from the
nose to earlobe and then at a halfway distance between the end of sternum and navel. The
distance is then marked and recorded. The next step involves lubrication of the tube up to 2 to
4 inches with 2% Xylocaine (Nursing and Midwifery Council, 2015). This process causes
inconvenience to the patients and therefore nurses should apply Xylocaine jelly within the
nostril and spray Xylocaine at the back side of the throat. The tube should then be passed
posteriorly through the nare, past the parynx, into the oesophagus to the stomach. The patient
must be offered chips or water as it facilitates entry of the tube into the oesophagus. Care
2NURSING ASSIGNMENT
must be taken to ensure that the tube does not enter the respiratory tract or cause facial
trauma (Patient Safety Alert 2016). The placement of the tube must be checked by injecting
aspirate into rthe gastric content through the free end of the tube. The pH should be below 6
and an X-ray should be obtained to confirm the placement (Covarrubias et al. 2013). The tube
should then be secured with a tube holder and in case of suction the tube must be connection
to the suction machine with optimal pressure. Finally, details about the reason for tube
insertion, type and size of tube, nature and amount of aspirate, suction type, pressure for
suction, type and amount of discharge and effectiveness of the treatment should be
documented by the nurses The incorrect positioning of the tubes could invite risks such as a
blockage within the oesophagus or the bronchus of the patient (Goldin et al. 2016; Hucl and
Spicak 2016). It should further be noted that not noticing the faulty placement could even
lead to death. Almost 15% of the in-patient deaths every year are reported because of a fatal
medical error caused due to the incorrect placement of the G-tubes (Lohsiriwat 2013). On
critically analysing the problem, it can be said that the lack of correct knowledge about the
tube-placement procedure within the care professionals and excessive work load can be
attributed to be the major reasons that account for the estimated death rate.
Therefore, this research aims to investigate the electronic databases and retrieve
relevant literatures in order to identify the correct placement of the gastrointestinal tubes in
order to avoid medical error.
Therefore, on the basis of the background information and the problem statement, the
systematic review would critically revolve around investigating the best practice for
determining the correct placement of the gastrointestinal tube in adult patients. It would also
evaluate the risks that are involved with the incorrect placement of the gastrointestinal tube.
In addition to this, the systematic review would also identify the potential barriers that hinder
the application of the best practice within the healthcare setting.
must be taken to ensure that the tube does not enter the respiratory tract or cause facial
trauma (Patient Safety Alert 2016). The placement of the tube must be checked by injecting
aspirate into rthe gastric content through the free end of the tube. The pH should be below 6
and an X-ray should be obtained to confirm the placement (Covarrubias et al. 2013). The tube
should then be secured with a tube holder and in case of suction the tube must be connection
to the suction machine with optimal pressure. Finally, details about the reason for tube
insertion, type and size of tube, nature and amount of aspirate, suction type, pressure for
suction, type and amount of discharge and effectiveness of the treatment should be
documented by the nurses The incorrect positioning of the tubes could invite risks such as a
blockage within the oesophagus or the bronchus of the patient (Goldin et al. 2016; Hucl and
Spicak 2016). It should further be noted that not noticing the faulty placement could even
lead to death. Almost 15% of the in-patient deaths every year are reported because of a fatal
medical error caused due to the incorrect placement of the G-tubes (Lohsiriwat 2013). On
critically analysing the problem, it can be said that the lack of correct knowledge about the
tube-placement procedure within the care professionals and excessive work load can be
attributed to be the major reasons that account for the estimated death rate.
Therefore, this research aims to investigate the electronic databases and retrieve
relevant literatures in order to identify the correct placement of the gastrointestinal tubes in
order to avoid medical error.
Therefore, on the basis of the background information and the problem statement, the
systematic review would critically revolve around investigating the best practice for
determining the correct placement of the gastrointestinal tube in adult patients. It would also
evaluate the risks that are involved with the incorrect placement of the gastrointestinal tube.
In addition to this, the systematic review would also identify the potential barriers that hinder
the application of the best practice within the healthcare setting.
3NURSING ASSIGNMENT
The research objectives thus formulated from the above research questions can be enlisted as
follows:
To investigate the best practice for the determination of the correct placement of the
gastrointestinal tube
To evaluate the risks involved with the incorrect placement of the gastrointestinal tube
To identify the potential barriers that hinder the application of the identified best practice
within the healthcare setting
The rationale for conducting the research can be mentioned as the need for training
care professionals to use the correct method of placing the gastrointestinal tubes in order to
avoid the occurrence of fatal medical errors. In addition to this, it would also help in
identifying the risk factors involved with the incorrect placement of the G-tubes and
accordingly create awareness among the care professionals to make use of the appropriate
procedure for the placement of the G-tubes in order to avoid fatal outcomes in patient.
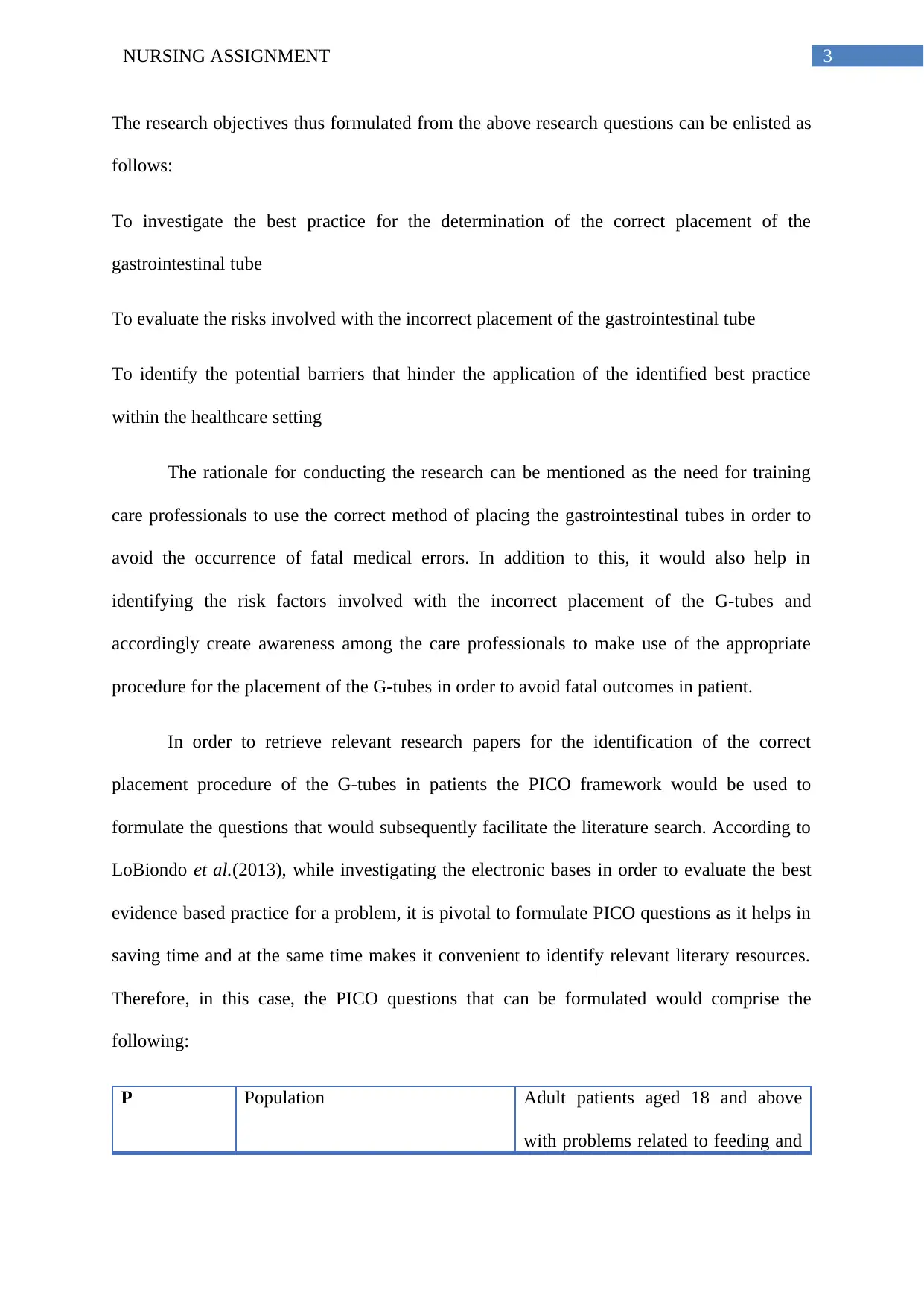
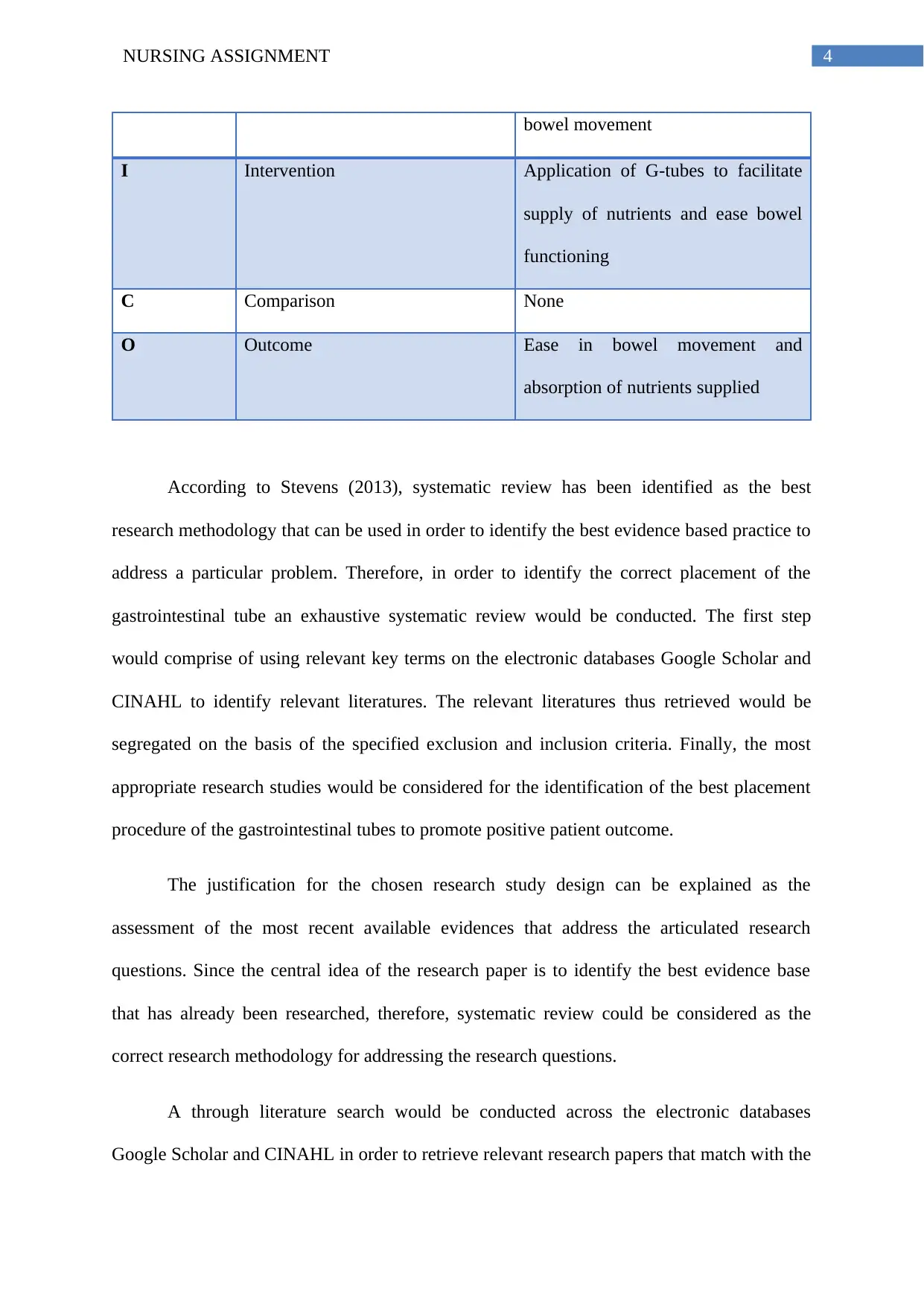
In order to retrieve relevant research papers for the identification of the correct
placement procedure of the G-tubes in patients the PICO framework would be used to
formulate the questions that would subsequently facilitate the literature search. According to
LoBiondo et al.(2013), while investigating the electronic bases in order to evaluate the best
evidence based practice for a problem, it is pivotal to formulate PICO questions as it helps in
saving time and at the same time makes it convenient to identify relevant literary resources.
Therefore, in this case, the PICO questions that can be formulated would comprise the
following:
P Population Adult patients aged 18 and above
with problems related to feeding and
The research objectives thus formulated from the above research questions can be enlisted as
follows:
To investigate the best practice for the determination of the correct placement of the
gastrointestinal tube
To evaluate the risks involved with the incorrect placement of the gastrointestinal tube
To identify the potential barriers that hinder the application of the identified best practice
within the healthcare setting
The rationale for conducting the research can be mentioned as the need for training
care professionals to use the correct method of placing the gastrointestinal tubes in order to
avoid the occurrence of fatal medical errors. In addition to this, it would also help in
identifying the risk factors involved with the incorrect placement of the G-tubes and
accordingly create awareness among the care professionals to make use of the appropriate
procedure for the placement of the G-tubes in order to avoid fatal outcomes in patient.
In order to retrieve relevant research papers for the identification of the correct
placement procedure of the G-tubes in patients the PICO framework would be used to
formulate the questions that would subsequently facilitate the literature search. According to
LoBiondo et al.(2013), while investigating the electronic bases in order to evaluate the best
evidence based practice for a problem, it is pivotal to formulate PICO questions as it helps in
saving time and at the same time makes it convenient to identify relevant literary resources.
Therefore, in this case, the PICO questions that can be formulated would comprise the
following:
P Population Adult patients aged 18 and above
with problems related to feeding and
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4NURSING ASSIGNMENT
bowel movement
I Intervention Application of G-tubes to facilitate
supply of nutrients and ease bowel
functioning
C Comparison None
O Outcome Ease in bowel movement and
absorption of nutrients supplied
According to Stevens (2013), systematic review has been identified as the best
research methodology that can be used in order to identify the best evidence based practice to
address a particular problem. Therefore, in order to identify the correct placement of the
gastrointestinal tube an exhaustive systematic review would be conducted. The first step
would comprise of using relevant key terms on the electronic databases Google Scholar and
CINAHL to identify relevant literatures. The relevant literatures thus retrieved would be
segregated on the basis of the specified exclusion and inclusion criteria. Finally, the most
appropriate research studies would be considered for the identification of the best placement
procedure of the gastrointestinal tubes to promote positive patient outcome.
The justification for the chosen research study design can be explained as the
assessment of the most recent available evidences that address the articulated research
questions. Since the central idea of the research paper is to identify the best evidence base
that has already been researched, therefore, systematic review could be considered as the
correct research methodology for addressing the research questions.
A through literature search would be conducted across the electronic databases
Google Scholar and CINAHL in order to retrieve relevant research papers that match with the
bowel movement
I Intervention Application of G-tubes to facilitate
supply of nutrients and ease bowel
functioning
C Comparison None
O Outcome Ease in bowel movement and
absorption of nutrients supplied
According to Stevens (2013), systematic review has been identified as the best
research methodology that can be used in order to identify the best evidence based practice to
address a particular problem. Therefore, in order to identify the correct placement of the
gastrointestinal tube an exhaustive systematic review would be conducted. The first step
would comprise of using relevant key terms on the electronic databases Google Scholar and
CINAHL to identify relevant literatures. The relevant literatures thus retrieved would be
segregated on the basis of the specified exclusion and inclusion criteria. Finally, the most
appropriate research studies would be considered for the identification of the best placement
procedure of the gastrointestinal tubes to promote positive patient outcome.
The justification for the chosen research study design can be explained as the
assessment of the most recent available evidences that address the articulated research
questions. Since the central idea of the research paper is to identify the best evidence base
that has already been researched, therefore, systematic review could be considered as the
correct research methodology for addressing the research questions.
A through literature search would be conducted across the electronic databases
Google Scholar and CINAHL in order to retrieve relevant research papers that match with the
5NURSING ASSIGNMENT
mentioned key words. The papers thus retrieved would be scanned on the basis of the
specified inclusion and exclusion criteria.
The key words used to conduct the search on the electronic databases comprised of
the following:
Correct placement, G-tubes, Gastrointestinal tubes, correct procedure, risks, medical error,
critical care, adults, fatal outcomes
It should be noted here that the BOOLEAN operators AND/OR were used in order to
in combination with the key terms in order to conduct a search on the electronic databases.
The exclusion criteria comprises of the characteristics that are used in order to
exclude relevant research studies so as to narrow down the retrieved literatures and consider
the most relevant research studies (LoBiondo et al. 2013). The exclusion criteria used for this
research study comprised the following:
Papers that were published before the year 2013
Papers that included animal trials
Papers that were published in foreign languages other than English
Papers that considered the target population as infants and children
The inclusion criteria, on the other hand comprises of the characteristics that are used
to include the retrieved research papers in the research study (Stevens et al. 2013). The
inclusion criteria in this case comprised the following characteristics:
Papers that were published in between the year 2013-2017
Papers that were published in English Language
Papers that included the target audience as adults and senior adults
mentioned key words. The papers thus retrieved would be scanned on the basis of the
specified inclusion and exclusion criteria.
The key words used to conduct the search on the electronic databases comprised of
the following:
Correct placement, G-tubes, Gastrointestinal tubes, correct procedure, risks, medical error,
critical care, adults, fatal outcomes
It should be noted here that the BOOLEAN operators AND/OR were used in order to
in combination with the key terms in order to conduct a search on the electronic databases.
The exclusion criteria comprises of the characteristics that are used in order to
exclude relevant research studies so as to narrow down the retrieved literatures and consider
the most relevant research studies (LoBiondo et al. 2013). The exclusion criteria used for this
research study comprised the following:
Papers that were published before the year 2013
Papers that included animal trials
Papers that were published in foreign languages other than English
Papers that considered the target population as infants and children
The inclusion criteria, on the other hand comprises of the characteristics that are used
to include the retrieved research papers in the research study (Stevens et al. 2013). The
inclusion criteria in this case comprised the following characteristics:
Papers that were published in between the year 2013-2017
Papers that were published in English Language
Papers that included the target audience as adults and senior adults
6NURSING ASSIGNMENT
Therefore, on the basis of the exclusion and inclusion criteria a number of research
papers were identified. The findings of the research papers would be critically discussed in
this section. According to Hannah and John (2013), patients that lack a functioning
gastrointestinal tract require an alternative intervention in order to derive nutrition. In
accordance to the recommended Patient safety guideline, the use of feeding tube (G-tube)
could help in providing nutrition to the patients who encounter problems with the oral
administration of bolus (Patient Safety Alert 2016). The laparoscopic as well as the PEG
method are the most prevalent methods that are used to treat patients (Tiancha et al. 2015;
Rahnemai et al.2014). As stated by Lohrisiriwat (2013), the laparoscopic method requires
general anaesthesia followed by the insertion of a 10mm port below the umbilicus under
direct vision. The next step involves the creation of a pneumoperitoneum with a CO2 pressure
of 5-10mmHg. The table is then tilted to 20 degrees in the head-upright position and a 10mm
port is then introduced to the gastric wall under direct vision. The gastric wall is subsequently
grasped with a toothed grasper and deflating the abdomen is brought through the port site.
The gastric wall is then held with two babcocks and two (2-0) vicryl purse strings are then
inserted to form a gastronomy within the centre using the blade numbered 11 (Merli et al.
2016; Cole 2015). The orifice is then widened using the artery clip and the feeding tube is
inserted. The balloon of the feeding tube is then positioned at the back of the purse string and
the stomach is secured with the suture to the abdominal wall. The correct positioning of the
tube and bleeding is checked with the recreation of the Pneumoperitoneum (Merli et al. 2016;
Hermanowicz et al. 2013; Wiegand 2013).
As stated by Hannah and John (2013) the laparoscopic method of insertion has been
identified as a safer method with lower mortality rates and better visibility of the placement
site while performing the procedure. As argued by Milsom et al. (2015), the best procedure
for the placement of G-tube in patients was to first conduct an ultrasound followed by
Therefore, on the basis of the exclusion and inclusion criteria a number of research
papers were identified. The findings of the research papers would be critically discussed in
this section. According to Hannah and John (2013), patients that lack a functioning
gastrointestinal tract require an alternative intervention in order to derive nutrition. In
accordance to the recommended Patient safety guideline, the use of feeding tube (G-tube)
could help in providing nutrition to the patients who encounter problems with the oral
administration of bolus (Patient Safety Alert 2016). The laparoscopic as well as the PEG
method are the most prevalent methods that are used to treat patients (Tiancha et al. 2015;
Rahnemai et al.2014). As stated by Lohrisiriwat (2013), the laparoscopic method requires
general anaesthesia followed by the insertion of a 10mm port below the umbilicus under
direct vision. The next step involves the creation of a pneumoperitoneum with a CO2 pressure
of 5-10mmHg. The table is then tilted to 20 degrees in the head-upright position and a 10mm
port is then introduced to the gastric wall under direct vision. The gastric wall is subsequently
grasped with a toothed grasper and deflating the abdomen is brought through the port site.
The gastric wall is then held with two babcocks and two (2-0) vicryl purse strings are then
inserted to form a gastronomy within the centre using the blade numbered 11 (Merli et al.
2016; Cole 2015). The orifice is then widened using the artery clip and the feeding tube is
inserted. The balloon of the feeding tube is then positioned at the back of the purse string and
the stomach is secured with the suture to the abdominal wall. The correct positioning of the
tube and bleeding is checked with the recreation of the Pneumoperitoneum (Merli et al. 2016;
Hermanowicz et al. 2013; Wiegand 2013).
As stated by Hannah and John (2013) the laparoscopic method of insertion has been
identified as a safer method with lower mortality rates and better visibility of the placement
site while performing the procedure. As argued by Milsom et al. (2015), the best procedure
for the placement of G-tube in patients was to first conduct an ultrasound followed by
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7NURSING ASSIGNMENT
external magnetic guidance to be subsequently followed by capnometry. As mentioned by
Bear et al. (2016), the three important characteristics that make the technique ideal for the
correct placement of the tube include, effective cost, huge success rate and global
applicability. The researchers typically conducted an exhaustive systematic review in order to
identify the best procedure for the placement of G-tubes. The findings indicated that the
electromagnetic placement of the tube yielded positive outcome. Another study conducted by
Powers et al. (2013), mentioned that the use of electromagnetically guided placement device
could positively help in the correct placement of the G-tube in patients. This technique has
been mentioned to reduce radiographic exposure (Velázquez‐Aviña et al. 2015; Metheny and
Meert 2014). The findings of the research study suggested that the duodenum or the jejunum
placement was achieved by the care professionals with the use of the electromagnetically
guided placement device with 97.2% accuracy (Powers et al. 2013). Further, studies also
indicated that the use of the device significantly lowered the prevalence of any incorrect
placement or adverse events (Metheny and Meert 2014; Bourgault et al. 2017). Studies also
indicated that the measurement of the gastric pH and auscultation technique could help in
determining the correct placement of the gastrointestinal tube (Baker et al. 2015; Boeykens et
al. 2014; Schimidt et al. 2014; Frerk et al., 2015). As mentioned by Covarrubias et al.(2013)
and Amorosa et al. (2013), the radiologic method has been identified as the least invasive
method with lower morbidity and mortality rate and with cost effectiveness that could be
used to place the G-tubes. However, the method has been reported to be unfavourable for
patients with abnormal stomach anatomy (Baker et al. 2015; Triantafyllou et al. 2014).
The research study conducted by Wang et al. (2013), clearly focused on conducting a
research to investigate the best procedure for the placement of G-tubes in patients. The
researchers had considered the case of critically ill patients who present severely impaired
gastric functioning. The researchers essentially made use of the electromagnetically guided
external magnetic guidance to be subsequently followed by capnometry. As mentioned by
Bear et al. (2016), the three important characteristics that make the technique ideal for the
correct placement of the tube include, effective cost, huge success rate and global
applicability. The researchers typically conducted an exhaustive systematic review in order to
identify the best procedure for the placement of G-tubes. The findings indicated that the
electromagnetic placement of the tube yielded positive outcome. Another study conducted by
Powers et al. (2013), mentioned that the use of electromagnetically guided placement device
could positively help in the correct placement of the G-tube in patients. This technique has
been mentioned to reduce radiographic exposure (Velázquez‐Aviña et al. 2015; Metheny and
Meert 2014). The findings of the research study suggested that the duodenum or the jejunum
placement was achieved by the care professionals with the use of the electromagnetically
guided placement device with 97.2% accuracy (Powers et al. 2013). Further, studies also
indicated that the use of the device significantly lowered the prevalence of any incorrect
placement or adverse events (Metheny and Meert 2014; Bourgault et al. 2017). Studies also
indicated that the measurement of the gastric pH and auscultation technique could help in
determining the correct placement of the gastrointestinal tube (Baker et al. 2015; Boeykens et
al. 2014; Schimidt et al. 2014; Frerk et al., 2015). As mentioned by Covarrubias et al.(2013)
and Amorosa et al. (2013), the radiologic method has been identified as the least invasive
method with lower morbidity and mortality rate and with cost effectiveness that could be
used to place the G-tubes. However, the method has been reported to be unfavourable for
patients with abnormal stomach anatomy (Baker et al. 2015; Triantafyllou et al. 2014).
The research study conducted by Wang et al. (2013), clearly focused on conducting a
research to investigate the best procedure for the placement of G-tubes in patients. The
researchers had considered the case of critically ill patients who present severely impaired
gastric functioning. The researchers essentially made use of the electromagnetically guided
8NURSING ASSIGNMENT
placement of the G-tube within the patients. Further, the important parameters were
considered and the target population comprised of 142 critically ill patients. The research
outcomes were clearly addressed and the study significantly pointed out the risks, benefits
and complications related to the placement of the tube in critically ill patients. It can thus be
mentioned, that the precise results of the study stated that care professionals could
successfully place 135 tubes in the first attempt within a time period of 20.12 minute. The
placement of the tip was confirmed with an X-ray. The sample size considered by the
researchers was significant and therefore the results can be generalised. Also the important
findings can be correlated to the clinical nutrition guidelines in elderly patients (McClave et
al. 2016). It can be said that the correct knowledge about the electromagnetically guided
placement procedure of enteral tubes in health care professionals can help in avoiding risks
and complications in infants. Another study conducted by Boeykens et al. (2014) focused on
researching about the correct confirmatory test that would help in getting an accurate idea
about the placement of the gastric tube in patients. The researchers conducted a large
prospective observational study and compared the auscultatory method with the pH
measurement method followed by comparing the results withthe gold standard (conducting a
X-ray) to detect the positioning of the Gastric tube. The sample size considered in this
research comprised of testing the positioning of 331 tubes in adult patients. All important
parameters and confounding factors were taken into consideration. The outcome was
appropriately addressed. The overall result of the research study indicated that a pH of <5.5
from tube aspirate could help in checking the positioning of tube in the stomach. Precisely,
the results indicated that the auscultatory method to check the positioning was incorrect.
Thus, it can be said that the results can be generalised and the outcomes were appropriately
covered. The findings are reliable and can be implied to nursing practice. The pH
measurement after placement could help in determining the correct positioning of the G-tube.
placement of the G-tube within the patients. Further, the important parameters were
considered and the target population comprised of 142 critically ill patients. The research
outcomes were clearly addressed and the study significantly pointed out the risks, benefits
and complications related to the placement of the tube in critically ill patients. It can thus be
mentioned, that the precise results of the study stated that care professionals could
successfully place 135 tubes in the first attempt within a time period of 20.12 minute. The
placement of the tip was confirmed with an X-ray. The sample size considered by the
researchers was significant and therefore the results can be generalised. Also the important
findings can be correlated to the clinical nutrition guidelines in elderly patients (McClave et
al. 2016). It can be said that the correct knowledge about the electromagnetically guided
placement procedure of enteral tubes in health care professionals can help in avoiding risks
and complications in infants. Another study conducted by Boeykens et al. (2014) focused on
researching about the correct confirmatory test that would help in getting an accurate idea
about the placement of the gastric tube in patients. The researchers conducted a large
prospective observational study and compared the auscultatory method with the pH
measurement method followed by comparing the results withthe gold standard (conducting a
X-ray) to detect the positioning of the Gastric tube. The sample size considered in this
research comprised of testing the positioning of 331 tubes in adult patients. All important
parameters and confounding factors were taken into consideration. The outcome was
appropriately addressed. The overall result of the research study indicated that a pH of <5.5
from tube aspirate could help in checking the positioning of tube in the stomach. Precisely,
the results indicated that the auscultatory method to check the positioning was incorrect.
Thus, it can be said that the results can be generalised and the outcomes were appropriately
covered. The findings are reliable and can be implied to nursing practice. The pH
measurement after placement could help in determining the correct positioning of the G-tube.
9NURSING ASSIGNMENT
Another study conducted by Milsom et al. (2015) focused on conducting an exhaustive
systematic review in order to access the best method for the positioning of the gastrointestinal
tube in adult patients. The researchers performed a systematic review and included 76
articles. Hence, it can be said that the results and findings can be generalised. Also, it can be
said that all important and confounding factors were not taken into consideration by the
researchers. The overall results can be summarized as the use of ultrasound, external
electromagnetic guidance followed by capnography can help in the effective placement of the
gastrointestinal tube in patients. It can also be mentioned that the best method accessed by the
group of researchers essentially met the primary criteria of cost effectiveness, global
application and huge success rate. The limitation of the study can be mentioned as the
primary focus of the study on the selection of the best method from a wide category of
methods. The study does not discuss any possible risks or complications that could occur due
to the failure of the technique.
The research study conducted by Powers et al. (2013) focused on the use of an
electromagnetic guided device in order to ensure the correct placement of the gastrointestinal
tube. The research study considered a sample size of 632 patients. All important and
confounding factors were taken into consideration by the patients and the overall results
stated that electromagnetically guided placement devise helped in accurate placement of
gastrointestinal tubes. Also, the findings predicted that electromagnetically guided placement
device could ensure 97.2% efficacy in the placement of the G-tube without radiographic
confirmation. The results can therefore be generalized on account of the success rate and the
large sample size. Also the findings of the study are relevant and can be implied to future
nursing practice. The use of EMPD technology could minimise the use of confirmatory
radiography.
Another study conducted by Milsom et al. (2015) focused on conducting an exhaustive
systematic review in order to access the best method for the positioning of the gastrointestinal
tube in adult patients. The researchers performed a systematic review and included 76
articles. Hence, it can be said that the results and findings can be generalised. Also, it can be
said that all important and confounding factors were not taken into consideration by the
researchers. The overall results can be summarized as the use of ultrasound, external
electromagnetic guidance followed by capnography can help in the effective placement of the
gastrointestinal tube in patients. It can also be mentioned that the best method accessed by the
group of researchers essentially met the primary criteria of cost effectiveness, global
application and huge success rate. The limitation of the study can be mentioned as the
primary focus of the study on the selection of the best method from a wide category of
methods. The study does not discuss any possible risks or complications that could occur due
to the failure of the technique.
The research study conducted by Powers et al. (2013) focused on the use of an
electromagnetic guided device in order to ensure the correct placement of the gastrointestinal
tube. The research study considered a sample size of 632 patients. All important and
confounding factors were taken into consideration by the patients and the overall results
stated that electromagnetically guided placement devise helped in accurate placement of
gastrointestinal tubes. Also, the findings predicted that electromagnetically guided placement
device could ensure 97.2% efficacy in the placement of the G-tube without radiographic
confirmation. The results can therefore be generalized on account of the success rate and the
large sample size. Also the findings of the study are relevant and can be implied to future
nursing practice. The use of EMPD technology could minimise the use of confirmatory
radiography.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10NURSING ASSIGNMENT
The study by Rahnemai et al. (2014) focused on evaluating the outcome of the patients
who had undergone a PEG placement. The researchers conducted a review that included case
histories of patients who had undergone PEG placement to evaluate the long-term
complication or adverse effect. All important parameters were considered and outcomes were
appropriately addressed. The overall results stated that PEG placement was directly
associated with three important categories that included endoscopic technical difficulties,
PEG procedure related complications and PEG tube use and wound. Precisely it can be
mentioned that patients who underwent PEG placement were exposed to long term high risk
of morbidity related to tube placement. The results can thus be generalized and all important
outcomes were considered in the research. The findings are reliable and can be implied into
future practice. PEG related complication might manifest after many years of placement and
research studies accessing risk factors associated with PEG associated complications could
help promote positive outcome.
Therefore, on the basis of the findings it can be said that the most appropriate method
for the correct placement of the Gastrointestinal tube would be to make use of the
electromagnetically guided placement device (Metheny and Meert 2014; Powers et al. 2013).
Also the laparoscopic insertion method was identified to be safe and effective (Hermanowicz
et al. 2013). However, the implementation of the techniques to practice is laden with a
number of problems such as involvement of higher cost, lack of appropriate training or skills
to perform the procedure and negative attitude of professionals to readily accept a change. In
addition to this, the lack of monitoring tools to determine the effectiveness of the care
professionals in performing the procedure can also be counted as one of the major reasons
that serve as an obstacle in the implementation process. Also, lack of quality assessment and
monitoring tool to check safe equipment supply can be considered as one of the causes that
serve as a barrier in the implementation process (Nursing and Midwifery Council 2015).
The study by Rahnemai et al. (2014) focused on evaluating the outcome of the patients
who had undergone a PEG placement. The researchers conducted a review that included case
histories of patients who had undergone PEG placement to evaluate the long-term
complication or adverse effect. All important parameters were considered and outcomes were
appropriately addressed. The overall results stated that PEG placement was directly
associated with three important categories that included endoscopic technical difficulties,
PEG procedure related complications and PEG tube use and wound. Precisely it can be
mentioned that patients who underwent PEG placement were exposed to long term high risk
of morbidity related to tube placement. The results can thus be generalized and all important
outcomes were considered in the research. The findings are reliable and can be implied into
future practice. PEG related complication might manifest after many years of placement and
research studies accessing risk factors associated with PEG associated complications could
help promote positive outcome.
Therefore, on the basis of the findings it can be said that the most appropriate method
for the correct placement of the Gastrointestinal tube would be to make use of the
electromagnetically guided placement device (Metheny and Meert 2014; Powers et al. 2013).
Also the laparoscopic insertion method was identified to be safe and effective (Hermanowicz
et al. 2013). However, the implementation of the techniques to practice is laden with a
number of problems such as involvement of higher cost, lack of appropriate training or skills
to perform the procedure and negative attitude of professionals to readily accept a change. In
addition to this, the lack of monitoring tools to determine the effectiveness of the care
professionals in performing the procedure can also be counted as one of the major reasons
that serve as an obstacle in the implementation process. Also, lack of quality assessment and
monitoring tool to check safe equipment supply can be considered as one of the causes that
serve as a barrier in the implementation process (Nursing and Midwifery Council 2015).
11NURSING ASSIGNMENT
Therefore, hand on workshops can be organized within the healthcare organization to educate
professionals about the use of the correct placement procedure.
Therefore to conclude, it can be mentioned that the use of electromagnetic guided
placement device could help in accurate positioning of the G-tubes in patient. Also, the PEG
method of placement was identified to lead to complications in a study that considered a
review of the cases that reported complications after PEG placement. Also, the laparoscopic
method of placement was identified to be a safe technique and the confirmatory test for the
detection of correct placement was identified to be the pH test of the aspirate. The
radiography confirmation test was also found to be effective. Therefore, the implementation
of the best evidence based practice along with quality innovation and continuous monitoring
by the administrative department can help in reinforcing positive implementation to acquire
positive patient outcome.
Therefore, hand on workshops can be organized within the healthcare organization to educate
professionals about the use of the correct placement procedure.
Therefore to conclude, it can be mentioned that the use of electromagnetic guided
placement device could help in accurate positioning of the G-tubes in patient. Also, the PEG
method of placement was identified to lead to complications in a study that considered a
review of the cases that reported complications after PEG placement. Also, the laparoscopic
method of placement was identified to be a safe technique and the confirmatory test for the
detection of correct placement was identified to be the pH test of the aspirate. The
radiography confirmation test was also found to be effective. Therefore, the implementation
of the best evidence based practice along with quality innovation and continuous monitoring
by the administrative department can help in reinforcing positive implementation to acquire
positive patient outcome.
12NURSING ASSIGNMENT
References:
Amorosa, J.K., Bramwit, M.P., Mohammed, T.L.H., Reddy, G.P., Brown, K., Dyer, D.S.,
Ginsburg, M.E., Heitkamp, D.E., Jeudy, J., Kirsch, J. and MacMahon, H., 2013. ACR
appropriateness criteria routine chest radiographs in intensive care unit patients. Journal of
the American College of Radiology, 10(3), pp.170-174.
Baker, L., Beres, A.L. and Baird, R., 2015. A systematic review and meta-analysis of
gastrostomy insertion techniques in children. Journal of pediatric surgery, 50(5), pp.718-725.
Bear, D.E., Champion, A., Lei, K., Smith, J., Beale, R., Camporota, L. and Barrett, N.A.,
2016. Use of an electromagnetic device compared with chest X-ray to confirm nasogastric
feeding tube position in critical care. Journal of Parenteral and Enteral Nutrition, 40(4),
pp.581-586.
Boeykens, K., Steeman, E. and Duysburgh, I., 2014. Reliability of pH measurement and the
auscultatory method to confirm the position of a nasogastric tube. International journal of
nursing studies, 51(11), pp.1427-1433.
Bourgault, A.M., Aguirre, L. and Ibrahim, J., 2017. Cortrak-assisted feeding tube insertion: a
comprehensive review of adverse events in the MAUDE database. American Journal of
Critical Care, 26(2), pp.149-156.
Cole, E., 2015. Improving the documentation of nasogastric tube insertion and adherence to
local enteral nutrition guidelines. BMJ Open Quality, 4(1), pp.u203207-w1513.
Covarrubias, D.A., O'Connor, O.J., McDermott, S. and Arellano, R.S., 2013. Radiologic
percutaneous gastrostomy: review of potential complications and approach to managing the
unexpected outcome. American Journal of Roentgenology, 200(4), pp.921-931.
References:
Amorosa, J.K., Bramwit, M.P., Mohammed, T.L.H., Reddy, G.P., Brown, K., Dyer, D.S.,
Ginsburg, M.E., Heitkamp, D.E., Jeudy, J., Kirsch, J. and MacMahon, H., 2013. ACR
appropriateness criteria routine chest radiographs in intensive care unit patients. Journal of
the American College of Radiology, 10(3), pp.170-174.
Baker, L., Beres, A.L. and Baird, R., 2015. A systematic review and meta-analysis of
gastrostomy insertion techniques in children. Journal of pediatric surgery, 50(5), pp.718-725.
Bear, D.E., Champion, A., Lei, K., Smith, J., Beale, R., Camporota, L. and Barrett, N.A.,
2016. Use of an electromagnetic device compared with chest X-ray to confirm nasogastric
feeding tube position in critical care. Journal of Parenteral and Enteral Nutrition, 40(4),
pp.581-586.
Boeykens, K., Steeman, E. and Duysburgh, I., 2014. Reliability of pH measurement and the
auscultatory method to confirm the position of a nasogastric tube. International journal of
nursing studies, 51(11), pp.1427-1433.
Bourgault, A.M., Aguirre, L. and Ibrahim, J., 2017. Cortrak-assisted feeding tube insertion: a
comprehensive review of adverse events in the MAUDE database. American Journal of
Critical Care, 26(2), pp.149-156.
Cole, E., 2015. Improving the documentation of nasogastric tube insertion and adherence to
local enteral nutrition guidelines. BMJ Open Quality, 4(1), pp.u203207-w1513.
Covarrubias, D.A., O'Connor, O.J., McDermott, S. and Arellano, R.S., 2013. Radiologic
percutaneous gastrostomy: review of potential complications and approach to managing the
unexpected outcome. American Journal of Roentgenology, 200(4), pp.921-931.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13NURSING ASSIGNMENT
Frerk, C., Mitchell, V.S., McNarry, A.F., Mendonca, C., Bhagrath, R., Patel, A., O'sullivan,
E.P., Woodall, N.M. and Ahmad, I., 2015. Difficult Airway Society 2015 guidelines for
management of unanticipated difficult intubation in adults. BJA: British Journal of
Anaesthesia, 115(6), pp.827-848.
Goldin, A.B., Heiss, K.F., Hall, M., Rothstein, D.H., Minneci, P.C., Blakely, M.L., Browne,
M., Raval, M.V., Shah, S.S., Rangel, S.J. and Snyder, C.L., 2016. Emergency department
visits and readmissions among children after gastrostomy tube placement. The Journal of
pediatrics, 174, pp.139-145.
Hannah, E. and John, R.M., 2013. Everything the nurse practitioner should know about
pediatric feeding tubes. Journal of the American Association of Nurse Practitioners, 25(11),
pp.567-577.
Hermanowicz, A., Matuszczak, E., Komarowska, M., Jarocka-Cyrta, E., Wojnar, J., Debek,
W., Matysiak, K. and Klek, S., 2013. Laparoscopy-assisted percutaneous endoscopic
gastrostomy enables enteral nutrition even in patients with distorted anatomy. World Journal
of Gastroenterology:WJG, 19(43), p.7696.
https://improvement.nhs.uk/documents/194/Patient_Safety_Alert_Stage_2_-
_NG_tube_resource_set.pdf [Accessed 12 February 2019].
Hucl, T. and Spicak, J., 2016. Complications of percutaneous endoscopic gastrostomy. Best
Practice & Research Clinical Gastroenterology, 30(5), pp.769-781.
LoBiondo-Wood, G., Haber, J., Berry, C. and Yost, J., 2013. Study Guide for Nursing
Research-E-Book: Methods and Critical Appraisal for Evidence-Based Practice. Elsevier
Health Sciences.
Frerk, C., Mitchell, V.S., McNarry, A.F., Mendonca, C., Bhagrath, R., Patel, A., O'sullivan,
E.P., Woodall, N.M. and Ahmad, I., 2015. Difficult Airway Society 2015 guidelines for
management of unanticipated difficult intubation in adults. BJA: British Journal of
Anaesthesia, 115(6), pp.827-848.
Goldin, A.B., Heiss, K.F., Hall, M., Rothstein, D.H., Minneci, P.C., Blakely, M.L., Browne,
M., Raval, M.V., Shah, S.S., Rangel, S.J. and Snyder, C.L., 2016. Emergency department
visits and readmissions among children after gastrostomy tube placement. The Journal of
pediatrics, 174, pp.139-145.
Hannah, E. and John, R.M., 2013. Everything the nurse practitioner should know about
pediatric feeding tubes. Journal of the American Association of Nurse Practitioners, 25(11),
pp.567-577.
Hermanowicz, A., Matuszczak, E., Komarowska, M., Jarocka-Cyrta, E., Wojnar, J., Debek,
W., Matysiak, K. and Klek, S., 2013. Laparoscopy-assisted percutaneous endoscopic
gastrostomy enables enteral nutrition even in patients with distorted anatomy. World Journal
of Gastroenterology:WJG, 19(43), p.7696.
https://improvement.nhs.uk/documents/194/Patient_Safety_Alert_Stage_2_-
_NG_tube_resource_set.pdf [Accessed 12 February 2019].
Hucl, T. and Spicak, J., 2016. Complications of percutaneous endoscopic gastrostomy. Best
Practice & Research Clinical Gastroenterology, 30(5), pp.769-781.
LoBiondo-Wood, G., Haber, J., Berry, C. and Yost, J., 2013. Study Guide for Nursing
Research-E-Book: Methods and Critical Appraisal for Evidence-Based Practice. Elsevier
Health Sciences.
14NURSING ASSIGNMENT
Lohsiriwat, V., 2013. Percutaneous endoscopic gastrostomy tube replacement: A simple
procedure?. World journal of gastrointestinal endoscopy, 5(1), p.14.
Lohsiriwat, V., 2013. Percutaneous endoscopic gastrostomy tube replacement: A simple
procedure?. World journal of gastrointestinal endoscopy, 5(1), p.14.
McClave, S.A., DiBaise, J.K., Mullin, G.E. and Martindale, R.G., 2016. ACG clinical
guideline: nutrition therapy in the adult hospitalized patient. The American journal of
gastroenterology, 111(3), p.315.
McSweeney, M.E., Jiang, H., Deutsch, A.J., Atmadja, M. and Lightdale, J.R., 2013. Long-
term outcomes of infants and children undergoing percutaneous endoscopy gastrostomy tube
placement. Journal of pediatric gastroenterology and nutrition, 57(5), pp.663-667.
Merli, L., De Marco, E.A., Fedele, C., Mason, E.J., Taddei, A., Paradiso, F.V., Catania, V.D.
and Nanni, L., 2016. Gastrostomy placement in children: percutaneous endoscopic
gastrostomy or laparoscopic gastrostomy?. Surgical laparoscopy, endoscopy & percutaneous
techniques, 26(5), p.381.
Metheny, N.A. and Meert, K.L., 2014. Effectiveness of an electromagnetic feeding tube
placement device in detecting inadvertent respiratory placement. American Journal of
Critical Care, 23(3), pp.240-248.
Morrison, R.J., Hollister, S.J., Niedner, M.F., Mahani, M.G., Park, A.H., Mehta, D.K., Ohye,
R.G. and Green, G.E., 2015. Mitigation of tracheobronchomalacia with 3D-printed
personalized medical devices in pediatric patients. Science translational medicine, 7(285),
pp.285ra64-285ra64.
Nursing and Midwifery Council 2015. The Code-Standards of Conduct, Performance and
Ethics for Nurses and Midwives: London: NMC.
Lohsiriwat, V., 2013. Percutaneous endoscopic gastrostomy tube replacement: A simple
procedure?. World journal of gastrointestinal endoscopy, 5(1), p.14.
Lohsiriwat, V., 2013. Percutaneous endoscopic gastrostomy tube replacement: A simple
procedure?. World journal of gastrointestinal endoscopy, 5(1), p.14.
McClave, S.A., DiBaise, J.K., Mullin, G.E. and Martindale, R.G., 2016. ACG clinical
guideline: nutrition therapy in the adult hospitalized patient. The American journal of
gastroenterology, 111(3), p.315.
McSweeney, M.E., Jiang, H., Deutsch, A.J., Atmadja, M. and Lightdale, J.R., 2013. Long-
term outcomes of infants and children undergoing percutaneous endoscopy gastrostomy tube
placement. Journal of pediatric gastroenterology and nutrition, 57(5), pp.663-667.
Merli, L., De Marco, E.A., Fedele, C., Mason, E.J., Taddei, A., Paradiso, F.V., Catania, V.D.
and Nanni, L., 2016. Gastrostomy placement in children: percutaneous endoscopic
gastrostomy or laparoscopic gastrostomy?. Surgical laparoscopy, endoscopy & percutaneous
techniques, 26(5), p.381.
Metheny, N.A. and Meert, K.L., 2014. Effectiveness of an electromagnetic feeding tube
placement device in detecting inadvertent respiratory placement. American Journal of
Critical Care, 23(3), pp.240-248.
Morrison, R.J., Hollister, S.J., Niedner, M.F., Mahani, M.G., Park, A.H., Mehta, D.K., Ohye,
R.G. and Green, G.E., 2015. Mitigation of tracheobronchomalacia with 3D-printed
personalized medical devices in pediatric patients. Science translational medicine, 7(285),
pp.285ra64-285ra64.
Nursing and Midwifery Council 2015. The Code-Standards of Conduct, Performance and
Ethics for Nurses and Midwives: London: NMC.
15NURSING ASSIGNMENT
Patient Safety Alert 2016. PSA from NHS Improvement: Nasogastric tube misplacement,
continued risk of death and severe harm.[Online] Available from:
https://improvement.nhs.uk/documents/194/Patient_Safety_Alert_Stage_2_-
_NG_tube_resource_set.pdf [Accessed 12 February 2019]
Powers, J., Fischer, M.H., Ziemba-Davis, M., Brown, J. and Phillips, D.M., 2013.
Elimination of radiographic confirmation for small-bowel feeding tubes in critical
care. American Journal of Critical Care, 22(6), pp.521-527.
Rahnemai-Azar, A.A., Rahnemaiazar, A.A., Naghshizadian, R., Kurtz, A. and Farkas, D.T.,
2014. Percutaneous endoscopic gastrostomy: indications, technique, complications and
management. World Journal of Gastroenterology: WJG, 20(24), p.7739.
Schmidt, A.R., Buehler, P., Seglias, L., Stark, T., Brotschi, B., Renner, T., Sabandal, C.,
Klaghofer, R., Weiss, M. and Schmitz, A., 2014. Gastric pH and residual volume after 1 and
2 h fasting time for clear fluids in children. British Journal of Anaesthesia, 114(3), pp.477-
482.
Stevens, K., 2013. The impact of evidence-based practice in nursing and the next big
ideas. OJIN:The Online Journal of Issues in Nursing, 18(2), p.4.
Tiancha, H., Jiyong, J. and Min, Y., 2015. How to promote bedside placement of the
postpyloric feeding tube: a network meta-analysis of randomized controlled trials. Journal of
Parenteral and Enteral Nutrition, 39(5), pp.521-530.
Triantafyllou, K., Papanikolaou, I.S., Stasinos, I., Polymeros, D. and Dimitriadis, G.D., 2014.
Percutaneous endoscopic gastrostomy tube replacement unexpected serious events. Nutrition
in Clinical Practice, 29(1), pp.142-145.
Patient Safety Alert 2016. PSA from NHS Improvement: Nasogastric tube misplacement,
continued risk of death and severe harm.[Online] Available from:
https://improvement.nhs.uk/documents/194/Patient_Safety_Alert_Stage_2_-
_NG_tube_resource_set.pdf [Accessed 12 February 2019]
Powers, J., Fischer, M.H., Ziemba-Davis, M., Brown, J. and Phillips, D.M., 2013.
Elimination of radiographic confirmation for small-bowel feeding tubes in critical
care. American Journal of Critical Care, 22(6), pp.521-527.
Rahnemai-Azar, A.A., Rahnemaiazar, A.A., Naghshizadian, R., Kurtz, A. and Farkas, D.T.,
2014. Percutaneous endoscopic gastrostomy: indications, technique, complications and
management. World Journal of Gastroenterology: WJG, 20(24), p.7739.
Schmidt, A.R., Buehler, P., Seglias, L., Stark, T., Brotschi, B., Renner, T., Sabandal, C.,
Klaghofer, R., Weiss, M. and Schmitz, A., 2014. Gastric pH and residual volume after 1 and
2 h fasting time for clear fluids in children. British Journal of Anaesthesia, 114(3), pp.477-
482.
Stevens, K., 2013. The impact of evidence-based practice in nursing and the next big
ideas. OJIN:The Online Journal of Issues in Nursing, 18(2), p.4.
Tiancha, H., Jiyong, J. and Min, Y., 2015. How to promote bedside placement of the
postpyloric feeding tube: a network meta-analysis of randomized controlled trials. Journal of
Parenteral and Enteral Nutrition, 39(5), pp.521-530.
Triantafyllou, K., Papanikolaou, I.S., Stasinos, I., Polymeros, D. and Dimitriadis, G.D., 2014.
Percutaneous endoscopic gastrostomy tube replacement unexpected serious events. Nutrition
in Clinical Practice, 29(1), pp.142-145.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
16NURSING ASSIGNMENT
Velázquez‐Aviña, J., Beyer, R., Díaz‐Tobar, C.P., Peter, S., Kyanam Kabir Baig, K.R.,
Wilcox, C.M. and Mönkemüller, K., 2015. New method of direct percutaneous endoscopic
jejunostomy tube placement using balloon‐assisted enteroscopy with fluoroscopy. Digestive
Endoscopy, 27(3), pp.317-322.
Wang, X., Zhang, L., Wu, C., Li, N. and Li, J., 2014. The application of electromagnetically
guided post-pyloric feeding tube placement in critically ill patients. Journal of Investigative
Surgery, 27(1), pp.21-26.
Wiegand, D.L. ed., 2013. AACN Procedure Manual for Critical Care-E-Book. Elsevier
Health Sciences.
Velázquez‐Aviña, J., Beyer, R., Díaz‐Tobar, C.P., Peter, S., Kyanam Kabir Baig, K.R.,
Wilcox, C.M. and Mönkemüller, K., 2015. New method of direct percutaneous endoscopic
jejunostomy tube placement using balloon‐assisted enteroscopy with fluoroscopy. Digestive
Endoscopy, 27(3), pp.317-322.
Wang, X., Zhang, L., Wu, C., Li, N. and Li, J., 2014. The application of electromagnetically
guided post-pyloric feeding tube placement in critically ill patients. Journal of Investigative
Surgery, 27(1), pp.21-26.
Wiegand, D.L. ed., 2013. AACN Procedure Manual for Critical Care-E-Book. Elsevier
Health Sciences.
1 out of 17
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





