Nursing Assignment: DETECT Framework for Patient Deterioration
VerifiedAdded on 2023/06/15
|13
|3077
|171
AI Summary
This nursing assignment discusses the DETECT framework for detecting patient deterioration and prioritizing nursing actions. It includes a case study of a patient post-operation of Right Total Knee Replacement (RTKR) and provides recommendations for pain management, neurovascular status, and infection risk assessment.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: NURSING ASSIGNMENT
Nursing assignment
Name of the Student
Name of the University
Author note
Nursing assignment
Name of the Student
Name of the University
Author note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1
NURSING ASSIGNMENT
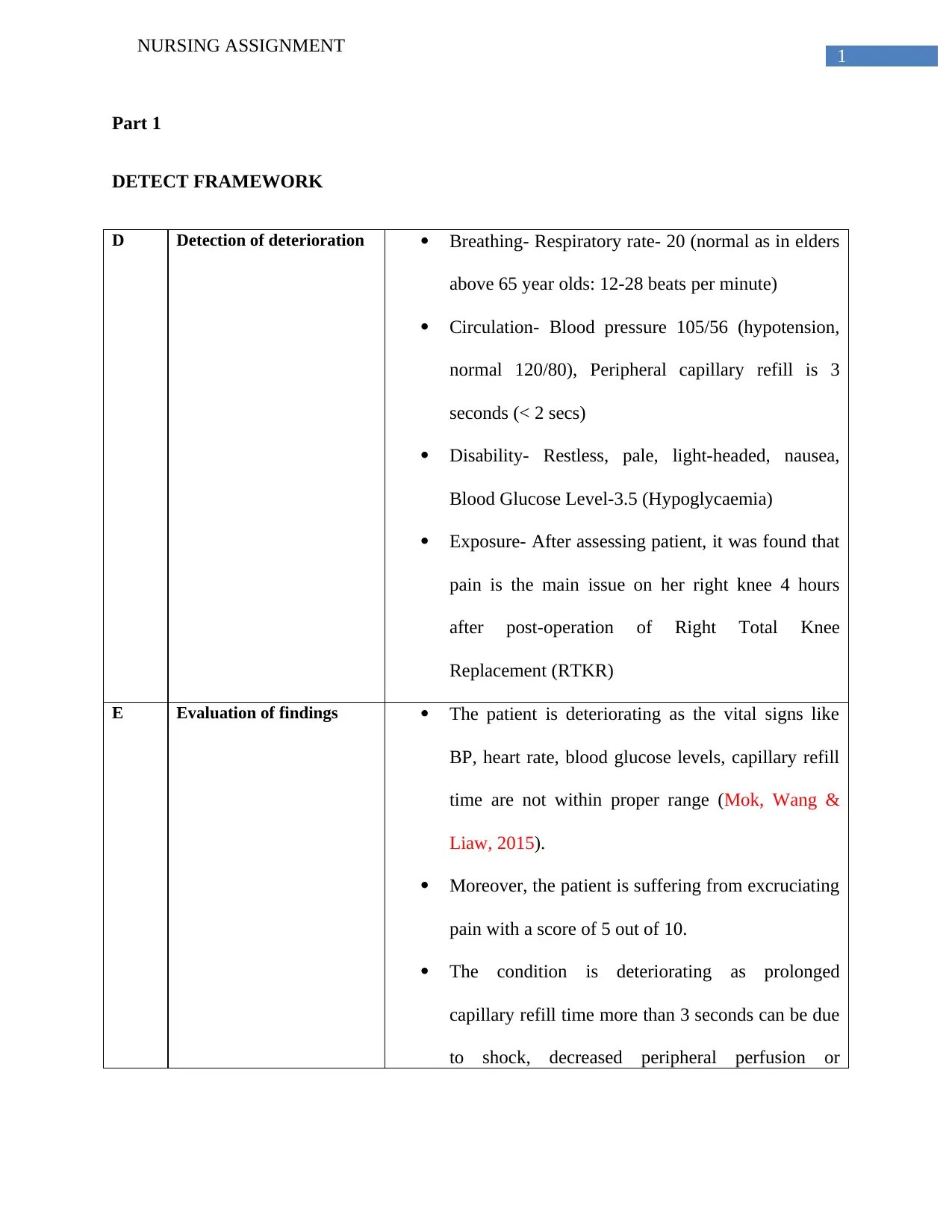
Part 1
DETECT FRAMEWORK
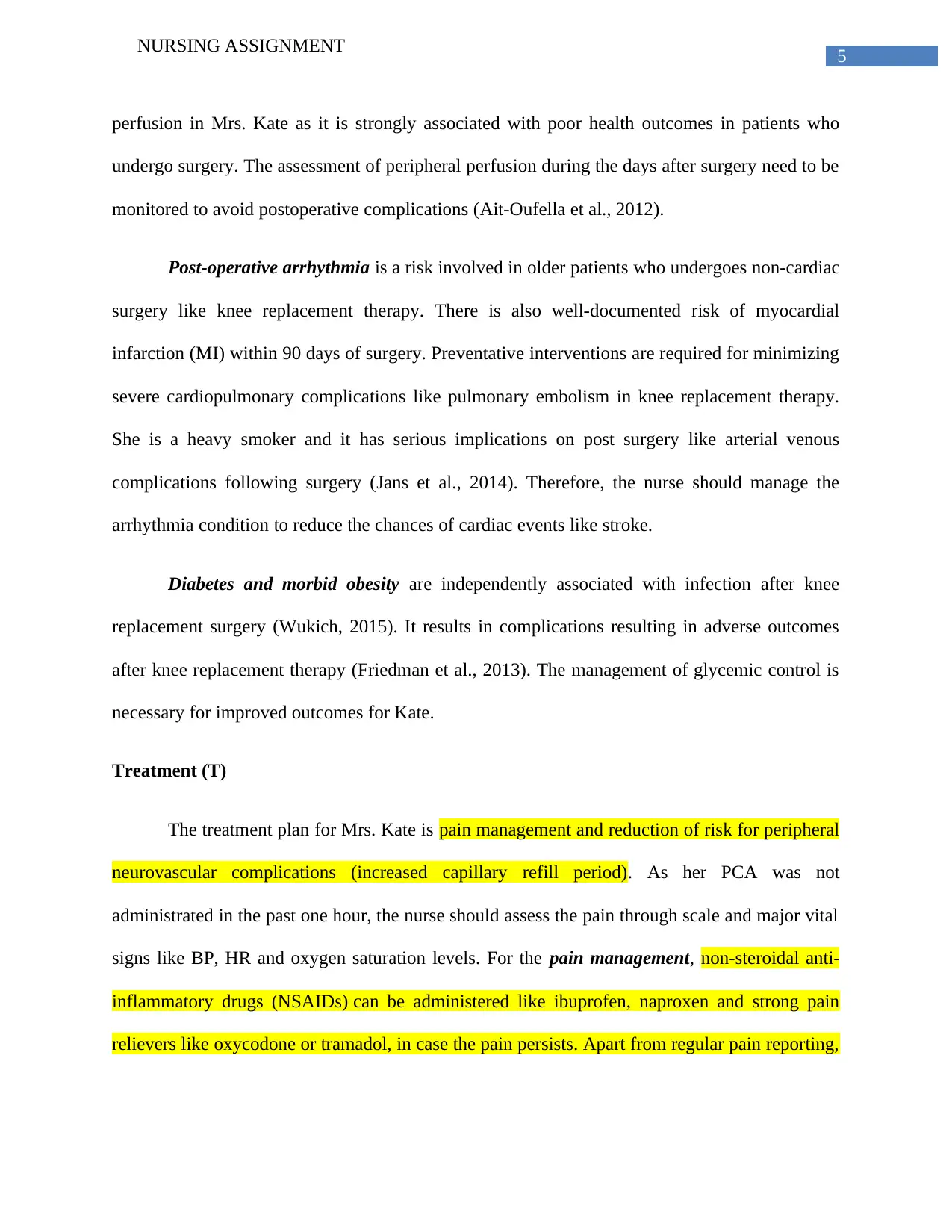
D Detection of deterioration Breathing- Respiratory rate- 20 (normal as in elders
above 65 year olds: 12-28 beats per minute)
Circulation- Blood pressure 105/56 (hypotension,
normal 120/80), Peripheral capillary refill is 3
seconds (< 2 secs)
Disability- Restless, pale, light-headed, nausea,
Blood Glucose Level-3.5 (Hypoglycaemia)
Exposure- After assessing patient, it was found that
pain is the main issue on her right knee 4 hours
after post-operation of Right Total Knee
Replacement (RTKR)
E Evaluation of findings The patient is deteriorating as the vital signs like
BP, heart rate, blood glucose levels, capillary refill
time are not within proper range (Mok, Wang &
Liaw, 2015).
Moreover, the patient is suffering from excruciating
pain with a score of 5 out of 10.
The condition is deteriorating as prolonged
capillary refill time more than 3 seconds can be due
to shock, decreased peripheral perfusion or
NURSING ASSIGNMENT
Part 1
DETECT FRAMEWORK
D Detection of deterioration Breathing- Respiratory rate- 20 (normal as in elders
above 65 year olds: 12-28 beats per minute)
Circulation- Blood pressure 105/56 (hypotension,
normal 120/80), Peripheral capillary refill is 3
seconds (< 2 secs)
Disability- Restless, pale, light-headed, nausea,
Blood Glucose Level-3.5 (Hypoglycaemia)
Exposure- After assessing patient, it was found that
pain is the main issue on her right knee 4 hours
after post-operation of Right Total Knee
Replacement (RTKR)
E Evaluation of findings The patient is deteriorating as the vital signs like
BP, heart rate, blood glucose levels, capillary refill
time are not within proper range (Mok, Wang &
Liaw, 2015).
Moreover, the patient is suffering from excruciating
pain with a score of 5 out of 10.
The condition is deteriorating as prolonged
capillary refill time more than 3 seconds can be due
to shock, decreased peripheral perfusion or
2
NURSING ASSIGNMENT
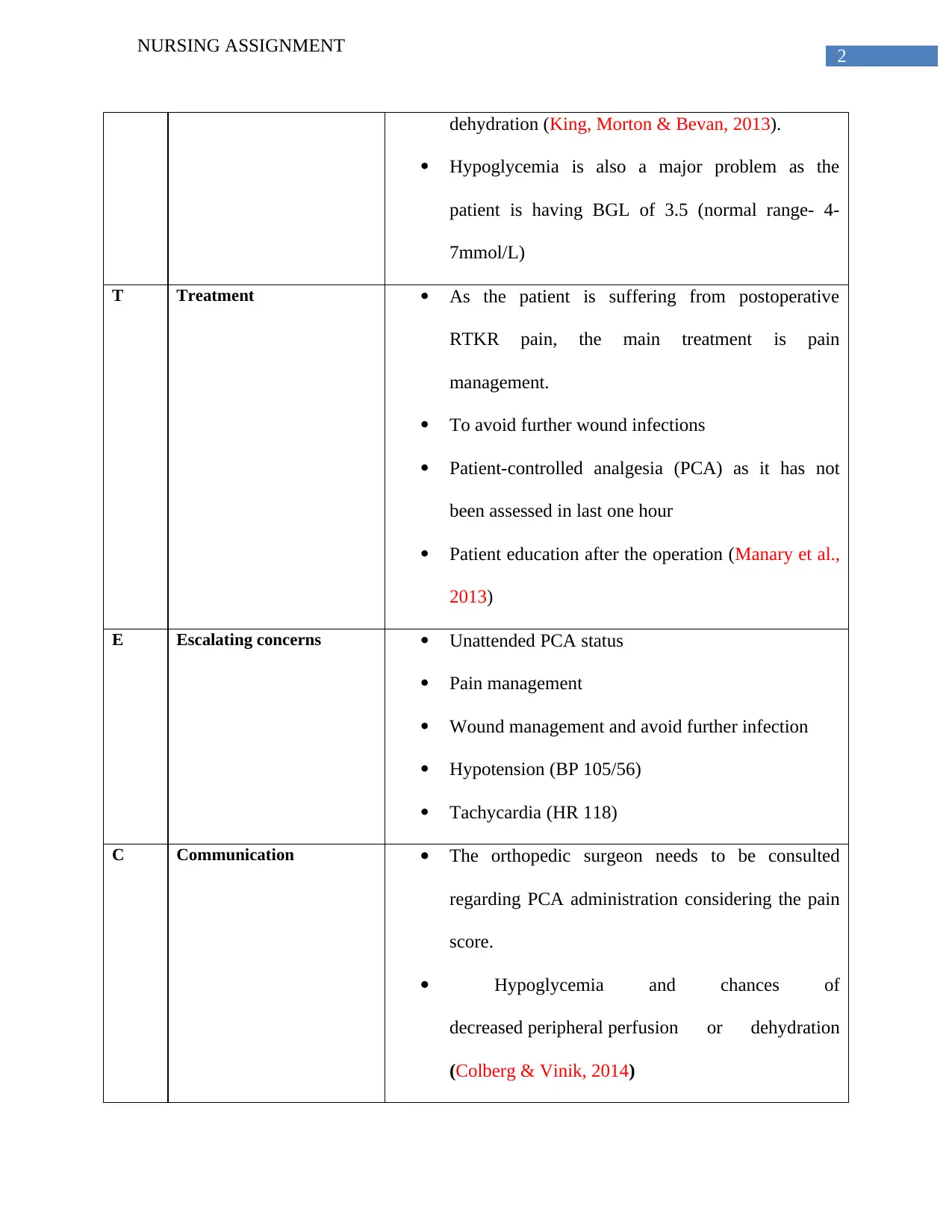
dehydration (King, Morton & Bevan, 2013).
Hypoglycemia is also a major problem as the
patient is having BGL of 3.5 (normal range- 4-
7mmol/L)
T Treatment As the patient is suffering from postoperative
RTKR pain, the main treatment is pain
management.
To avoid further wound infections
Patient-controlled analgesia (PCA) as it has not
been assessed in last one hour
Patient education after the operation (Manary et al.,
2013)
E Escalating concerns Unattended PCA status
Pain management
Wound management and avoid further infection
Hypotension (BP 105/56)
Tachycardia (HR 118)
C Communication The orthopedic surgeon needs to be consulted
regarding PCA administration considering the pain
score.
Hypoglycemia and chances of
decreased peripheral perfusion or dehydration
(Colberg & Vinik, 2014)
NURSING ASSIGNMENT
dehydration (King, Morton & Bevan, 2013).
Hypoglycemia is also a major problem as the
patient is having BGL of 3.5 (normal range- 4-
7mmol/L)
T Treatment As the patient is suffering from postoperative
RTKR pain, the main treatment is pain
management.
To avoid further wound infections
Patient-controlled analgesia (PCA) as it has not
been assessed in last one hour
Patient education after the operation (Manary et al.,
2013)
E Escalating concerns Unattended PCA status
Pain management
Wound management and avoid further infection
Hypotension (BP 105/56)
Tachycardia (HR 118)
C Communication The orthopedic surgeon needs to be consulted
regarding PCA administration considering the pain
score.
Hypoglycemia and chances of
decreased peripheral perfusion or dehydration
(Colberg & Vinik, 2014)
3
NURSING ASSIGNMENT
Multi-disciplinary team assessment and
interventions
T Teams PCA administration and pain management
Abnormality in vital signs that need consideration
like heart rate, BP and wound care like a tissue
trauma team (Mok et al., 2015)
Part 2
The ability to detect the nursing priorities and harms is a major challenge for the nurses.
DETECT table acts as a theoretical framework for nurses to detect the immediate nursing actions
and interpret the risk signals of patients in context to patient safety and better health outcomes. In
the given case scenario, the DETECT table is used for Mrs. Kate to recognize the immediate
nursing actions and interventions to stabilize her condition.
Deteriorating pain (D)
RTKR is a mainstream surgery and from the case study, it is evident that Kate is
suffering from post-operative pain (4 hours after surgery) (Carr et al., 2012). The pain score is
5/10 that is alarming enough indicating serious complications. In this situation, pain assessment,
wound location and chances of infection is important. The nurse should assess the pain and avoid
complications of post-operative pain in RTKR like injuries to veins, arteries from anesthesia
NURSING ASSIGNMENT
Multi-disciplinary team assessment and
interventions
T Teams PCA administration and pain management
Abnormality in vital signs that need consideration
like heart rate, BP and wound care like a tissue
trauma team (Mok et al., 2015)
Part 2
The ability to detect the nursing priorities and harms is a major challenge for the nurses.
DETECT table acts as a theoretical framework for nurses to detect the immediate nursing actions
and interpret the risk signals of patients in context to patient safety and better health outcomes. In
the given case scenario, the DETECT table is used for Mrs. Kate to recognize the immediate
nursing actions and interventions to stabilize her condition.
Deteriorating pain (D)
RTKR is a mainstream surgery and from the case study, it is evident that Kate is
suffering from post-operative pain (4 hours after surgery) (Carr et al., 2012). The pain score is
5/10 that is alarming enough indicating serious complications. In this situation, pain assessment,
wound location and chances of infection is important. The nurse should assess the pain and avoid
complications of post-operative pain in RTKR like injuries to veins, arteries from anesthesia
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4
NURSING ASSIGNMENT
administration. Moreover, there was no monitoring of PCA in the past one hour. This is
important to avoid any kind of postoperative pain or complications (Lamplot, Wagner &
Manning, 2014). The vital signs of the patient was also concerning. The HR was 118 indicating
tachycardia, BP-105/56 (hypotension) and BGL 3.5 (hypoglycemic) condition. Hypoglycemic
condition need to be stopped from falling as it can make the patient unwell like creating
disorientation, confusion and loss of consciousness (Han & Kang, 2013). As Kate is a NIDDM
patient, it is evident that sepsis or anesthesia complications can lead to hypoglycemic condition
(Jørgensen et al., 2015). Another nursing priority is increase in peripheral capillary refill, >3
seconds (normal <2 seconds) and this prolonged capillary refill time can be a sign of shock,
decreased peripheral perfusion and dehydration (Ait-Oufella et al., 2014).
Apart from pain assessment, neurovascular complications are also associated with
RKRT (Parvizi & Diaz-Ledezma, 2013). Although, the incidence is low, it is underestimated and
can be devastating. The monitoring of the neurovascular deterioration is also a nursing priority as
delay in recognition can cause severe complications like permanent deficits that occurs after
surgery (Solimeno et al., 2012). These abnormalities in vital signs and complications are
witnessed in Mrs. Kate indicating deterioration.
Evaluation of findings (E)
Considering Mrs. Kate deteriorating condition, tachycardia and increase in capillary
refill period are the major concerns. Hypoglycemia also need immediate intervention as it may
cause complications in RKRT post operation. These are early signs of nonvascular deterioration
in the patient. The increase in capillary refill time with pale cool digits is the major
complications after knee replacement therapy. The nurse need to evaluate the alternate peripheral
NURSING ASSIGNMENT
administration. Moreover, there was no monitoring of PCA in the past one hour. This is
important to avoid any kind of postoperative pain or complications (Lamplot, Wagner &
Manning, 2014). The vital signs of the patient was also concerning. The HR was 118 indicating
tachycardia, BP-105/56 (hypotension) and BGL 3.5 (hypoglycemic) condition. Hypoglycemic
condition need to be stopped from falling as it can make the patient unwell like creating
disorientation, confusion and loss of consciousness (Han & Kang, 2013). As Kate is a NIDDM
patient, it is evident that sepsis or anesthesia complications can lead to hypoglycemic condition
(Jørgensen et al., 2015). Another nursing priority is increase in peripheral capillary refill, >3
seconds (normal <2 seconds) and this prolonged capillary refill time can be a sign of shock,
decreased peripheral perfusion and dehydration (Ait-Oufella et al., 2014).
Apart from pain assessment, neurovascular complications are also associated with
RKRT (Parvizi & Diaz-Ledezma, 2013). Although, the incidence is low, it is underestimated and
can be devastating. The monitoring of the neurovascular deterioration is also a nursing priority as
delay in recognition can cause severe complications like permanent deficits that occurs after
surgery (Solimeno et al., 2012). These abnormalities in vital signs and complications are
witnessed in Mrs. Kate indicating deterioration.
Evaluation of findings (E)
Considering Mrs. Kate deteriorating condition, tachycardia and increase in capillary
refill period are the major concerns. Hypoglycemia also need immediate intervention as it may
cause complications in RKRT post operation. These are early signs of nonvascular deterioration
in the patient. The increase in capillary refill time with pale cool digits is the major
complications after knee replacement therapy. The nurse need to evaluate the alternate peripheral
5
NURSING ASSIGNMENT
perfusion in Mrs. Kate as it is strongly associated with poor health outcomes in patients who
undergo surgery. The assessment of peripheral perfusion during the days after surgery need to be
monitored to avoid postoperative complications (Ait-Oufella et al., 2012).
Post-operative arrhythmia is a risk involved in older patients who undergoes non-cardiac
surgery like knee replacement therapy. There is also well-documented risk of myocardial
infarction (MI) within 90 days of surgery. Preventative interventions are required for minimizing
severe cardiopulmonary complications like pulmonary embolism in knee replacement therapy.
She is a heavy smoker and it has serious implications on post surgery like arterial venous
complications following surgery (Jans et al., 2014). Therefore, the nurse should manage the
arrhythmia condition to reduce the chances of cardiac events like stroke.
Diabetes and morbid obesity are independently associated with infection after knee
replacement surgery (Wukich, 2015). It results in complications resulting in adverse outcomes
after knee replacement therapy (Friedman et al., 2013). The management of glycemic control is
necessary for improved outcomes for Kate.
Treatment (T)
The treatment plan for Mrs. Kate is pain management and reduction of risk for peripheral
neurovascular complications (increased capillary refill period). As her PCA was not
administrated in the past one hour, the nurse should assess the pain through scale and major vital
signs like BP, HR and oxygen saturation levels. For the pain management, non-steroidal anti-
inflammatory drugs (NSAIDs) can be administered like ibuprofen, naproxen and strong pain
relievers like oxycodone or tramadol, in case the pain persists. Apart from regular pain reporting,
NURSING ASSIGNMENT
perfusion in Mrs. Kate as it is strongly associated with poor health outcomes in patients who
undergo surgery. The assessment of peripheral perfusion during the days after surgery need to be
monitored to avoid postoperative complications (Ait-Oufella et al., 2012).
Post-operative arrhythmia is a risk involved in older patients who undergoes non-cardiac
surgery like knee replacement therapy. There is also well-documented risk of myocardial
infarction (MI) within 90 days of surgery. Preventative interventions are required for minimizing
severe cardiopulmonary complications like pulmonary embolism in knee replacement therapy.
She is a heavy smoker and it has serious implications on post surgery like arterial venous
complications following surgery (Jans et al., 2014). Therefore, the nurse should manage the
arrhythmia condition to reduce the chances of cardiac events like stroke.
Diabetes and morbid obesity are independently associated with infection after knee
replacement surgery (Wukich, 2015). It results in complications resulting in adverse outcomes
after knee replacement therapy (Friedman et al., 2013). The management of glycemic control is
necessary for improved outcomes for Kate.
Treatment (T)
The treatment plan for Mrs. Kate is pain management and reduction of risk for peripheral
neurovascular complications (increased capillary refill period). As her PCA was not
administrated in the past one hour, the nurse should assess the pain through scale and major vital
signs like BP, HR and oxygen saturation levels. For the pain management, non-steroidal anti-
inflammatory drugs (NSAIDs) can be administered like ibuprofen, naproxen and strong pain
relievers like oxycodone or tramadol, in case the pain persists. Apart from regular pain reporting,
6
NURSING ASSIGNMENT
it is important to maintain proper position as it helps to reduce undue tension and muscle spasms
on prosthesis and surrounding area (Chang & Cho, 2012).
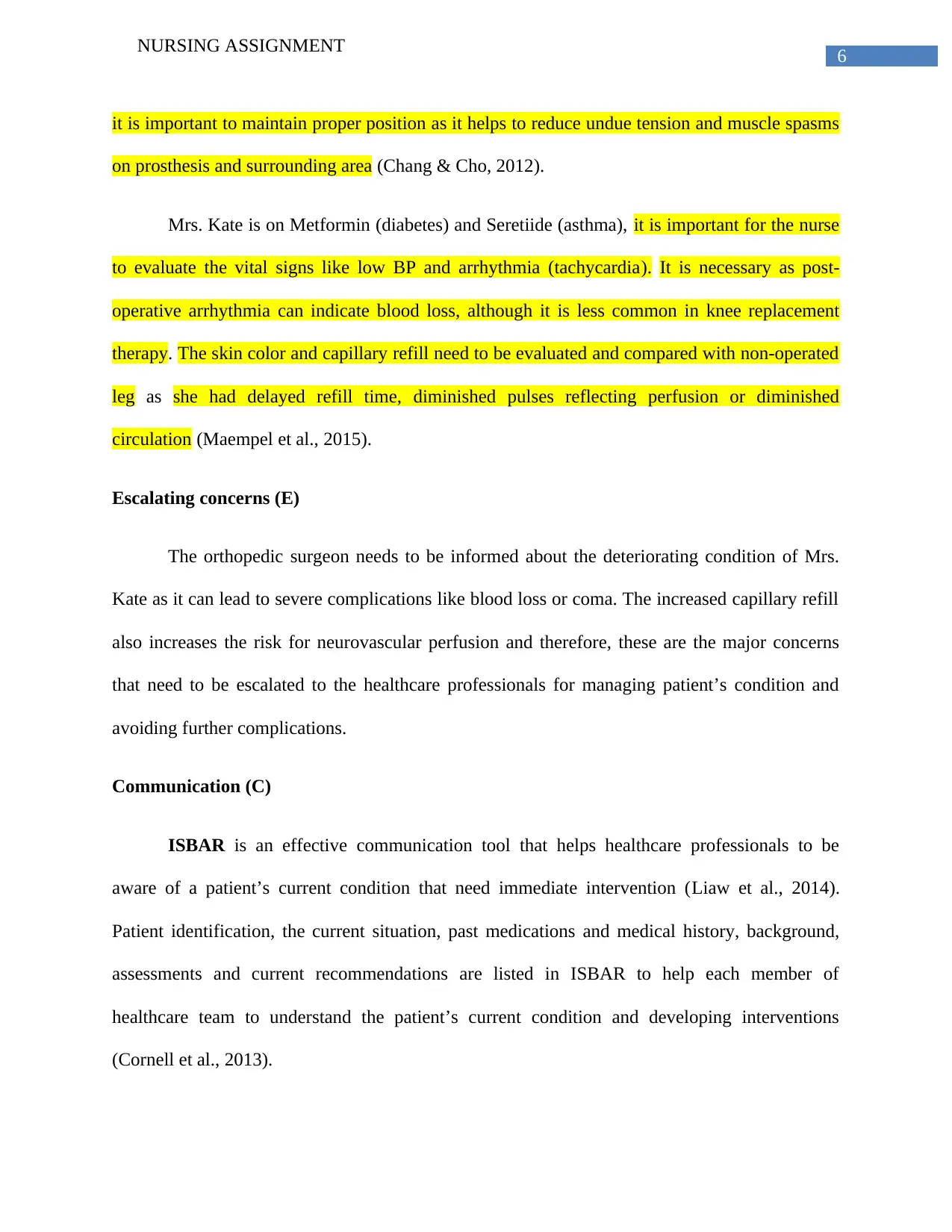
Mrs. Kate is on Metformin (diabetes) and Seretiide (asthma), it is important for the nurse
to evaluate the vital signs like low BP and arrhythmia (tachycardia). It is necessary as post-
operative arrhythmia can indicate blood loss, although it is less common in knee replacement
therapy. The skin color and capillary refill need to be evaluated and compared with non-operated
leg as she had delayed refill time, diminished pulses reflecting perfusion or diminished
circulation (Maempel et al., 2015).
Escalating concerns (E)
The orthopedic surgeon needs to be informed about the deteriorating condition of Mrs.
Kate as it can lead to severe complications like blood loss or coma. The increased capillary refill
also increases the risk for neurovascular perfusion and therefore, these are the major concerns
that need to be escalated to the healthcare professionals for managing patient’s condition and
avoiding further complications.
Communication (C)
ISBAR is an effective communication tool that helps healthcare professionals to be
aware of a patient’s current condition that need immediate intervention (Liaw et al., 2014).
Patient identification, the current situation, past medications and medical history, background,
assessments and current recommendations are listed in ISBAR to help each member of
healthcare team to understand the patient’s current condition and developing interventions
(Cornell et al., 2013).
NURSING ASSIGNMENT
it is important to maintain proper position as it helps to reduce undue tension and muscle spasms
on prosthesis and surrounding area (Chang & Cho, 2012).
Mrs. Kate is on Metformin (diabetes) and Seretiide (asthma), it is important for the nurse
to evaluate the vital signs like low BP and arrhythmia (tachycardia). It is necessary as post-
operative arrhythmia can indicate blood loss, although it is less common in knee replacement
therapy. The skin color and capillary refill need to be evaluated and compared with non-operated
leg as she had delayed refill time, diminished pulses reflecting perfusion or diminished
circulation (Maempel et al., 2015).
Escalating concerns (E)
The orthopedic surgeon needs to be informed about the deteriorating condition of Mrs.
Kate as it can lead to severe complications like blood loss or coma. The increased capillary refill
also increases the risk for neurovascular perfusion and therefore, these are the major concerns
that need to be escalated to the healthcare professionals for managing patient’s condition and
avoiding further complications.
Communication (C)
ISBAR is an effective communication tool that helps healthcare professionals to be
aware of a patient’s current condition that need immediate intervention (Liaw et al., 2014).
Patient identification, the current situation, past medications and medical history, background,
assessments and current recommendations are listed in ISBAR to help each member of
healthcare team to understand the patient’s current condition and developing interventions
(Cornell et al., 2013).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
NURSING ASSIGNMENT
Teams (T)
Collaboration between the members of the multi-disciplinary team is necessary as it helps
to manage Kate’s condition in a coordinated and timely manner (Tomek et al., 2012). The nurse-
in-charge can help to supervise the interventions, promote clear communication between the
members so that there are no medical errors, and stabilize Kate’s condition (Pape et al., 2013).
The orthopedic surgeon along with the physiotherapist can be helpful in restoring her mobility
and avoid further complications.
From the above discussion, it can be concluded that tachycardia, hypoglycemia and
increase in capillary refill are the main nursing priorities that are guided by DETECT framework.
The recognition of clinical deterioration in Kate is recognized through this framework. It
comprises of detection of deterioration, evaluation of patient, treatment, escalation to the
concerned authorities, communication and collaborative teamwork to stabilize her condition.
Part 3
ISBAR
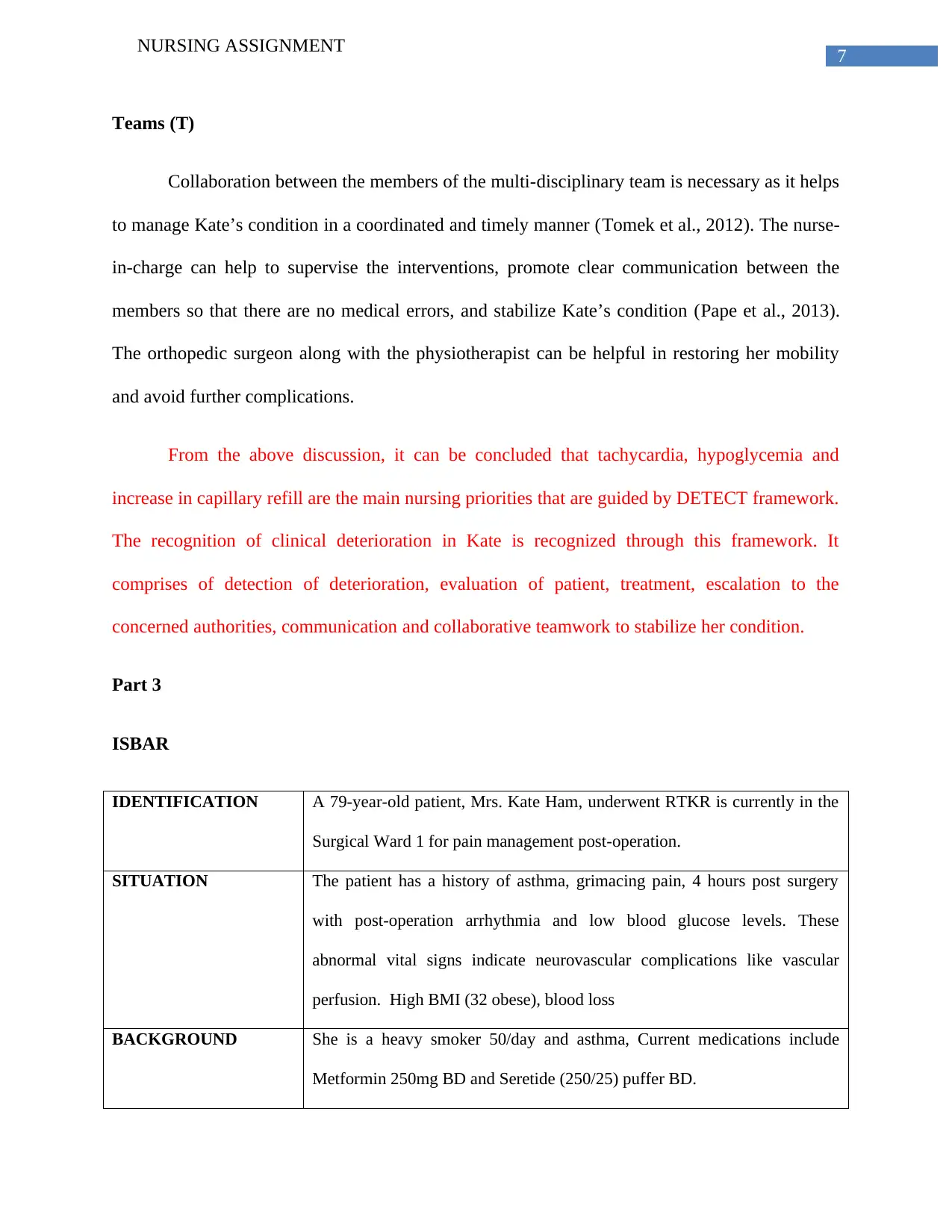
IDENTIFICATION A 79-year-old patient, Mrs. Kate Ham, underwent RTKR is currently in the
Surgical Ward 1 for pain management post-operation.
SITUATION The patient has a history of asthma, grimacing pain, 4 hours post surgery
with post-operation arrhythmia and low blood glucose levels. These
abnormal vital signs indicate neurovascular complications like vascular
perfusion. High BMI (32 obese), blood loss
BACKGROUND She is a heavy smoker 50/day and asthma, Current medications include
Metformin 250mg BD and Seretide (250/25) puffer BD.
NURSING ASSIGNMENT
Teams (T)
Collaboration between the members of the multi-disciplinary team is necessary as it helps
to manage Kate’s condition in a coordinated and timely manner (Tomek et al., 2012). The nurse-
in-charge can help to supervise the interventions, promote clear communication between the
members so that there are no medical errors, and stabilize Kate’s condition (Pape et al., 2013).
The orthopedic surgeon along with the physiotherapist can be helpful in restoring her mobility
and avoid further complications.
From the above discussion, it can be concluded that tachycardia, hypoglycemia and
increase in capillary refill are the main nursing priorities that are guided by DETECT framework.
The recognition of clinical deterioration in Kate is recognized through this framework. It
comprises of detection of deterioration, evaluation of patient, treatment, escalation to the
concerned authorities, communication and collaborative teamwork to stabilize her condition.
Part 3
ISBAR
IDENTIFICATION A 79-year-old patient, Mrs. Kate Ham, underwent RTKR is currently in the
Surgical Ward 1 for pain management post-operation.
SITUATION The patient has a history of asthma, grimacing pain, 4 hours post surgery
with post-operation arrhythmia and low blood glucose levels. These
abnormal vital signs indicate neurovascular complications like vascular
perfusion. High BMI (32 obese), blood loss
BACKGROUND She is a heavy smoker 50/day and asthma, Current medications include
Metformin 250mg BD and Seretide (250/25) puffer BD.
8
NURSING ASSIGNMENT
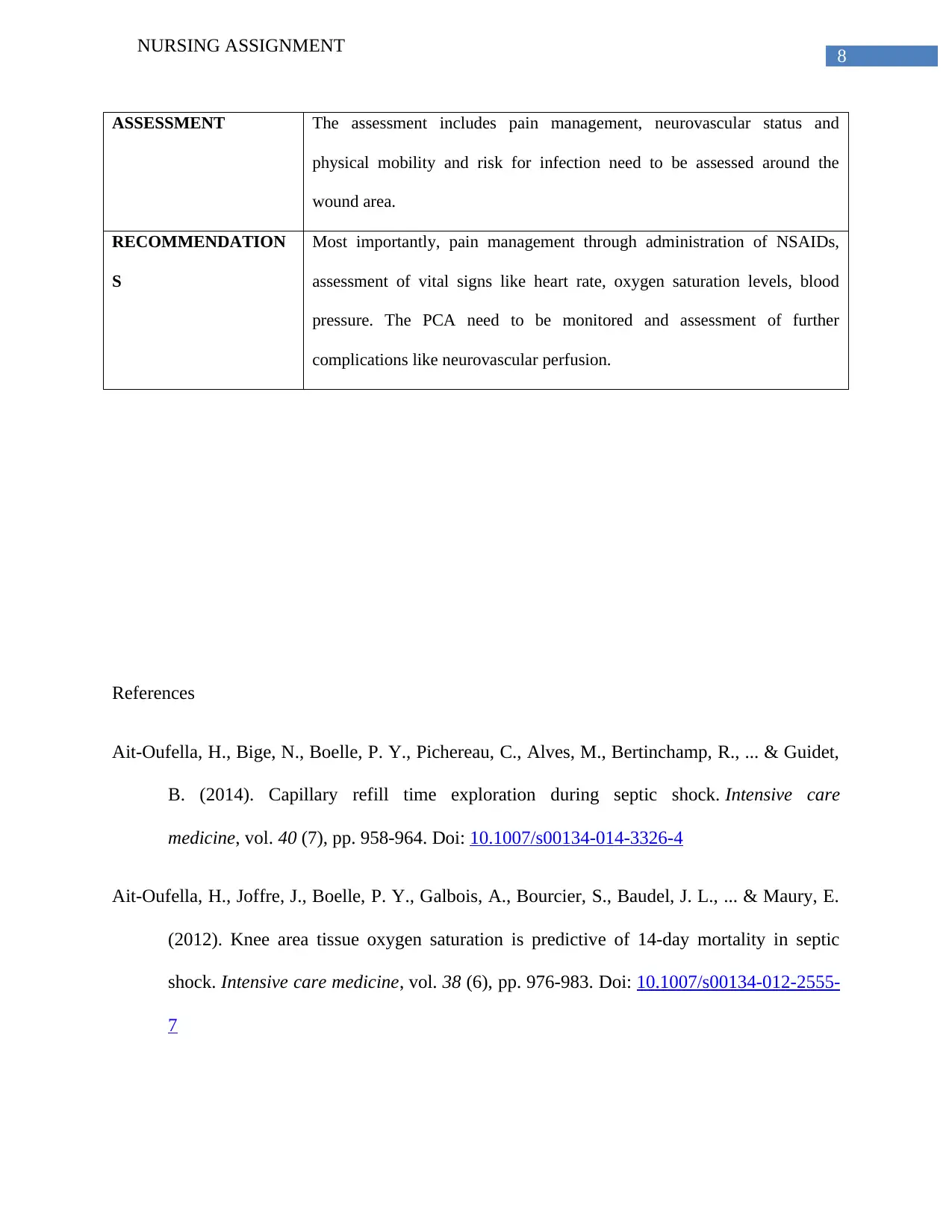
ASSESSMENT The assessment includes pain management, neurovascular status and
physical mobility and risk for infection need to be assessed around the
wound area.
RECOMMENDATION
S
Most importantly, pain management through administration of NSAIDs,
assessment of vital signs like heart rate, oxygen saturation levels, blood
pressure. The PCA need to be monitored and assessment of further
complications like neurovascular perfusion.
References
Ait-Oufella, H., Bige, N., Boelle, P. Y., Pichereau, C., Alves, M., Bertinchamp, R., ... & Guidet,
B. (2014). Capillary refill time exploration during septic shock. Intensive care
medicine, vol. 40 (7), pp. 958-964. Doi: 10.1007/s00134-014-3326-4
Ait-Oufella, H., Joffre, J., Boelle, P. Y., Galbois, A., Bourcier, S., Baudel, J. L., ... & Maury, E.
(2012). Knee area tissue oxygen saturation is predictive of 14-day mortality in septic
shock. Intensive care medicine, vol. 38 (6), pp. 976-983. Doi: 10.1007/s00134-012-2555-
7
NURSING ASSIGNMENT
ASSESSMENT The assessment includes pain management, neurovascular status and
physical mobility and risk for infection need to be assessed around the
wound area.
RECOMMENDATION
S
Most importantly, pain management through administration of NSAIDs,
assessment of vital signs like heart rate, oxygen saturation levels, blood
pressure. The PCA need to be monitored and assessment of further
complications like neurovascular perfusion.
References
Ait-Oufella, H., Bige, N., Boelle, P. Y., Pichereau, C., Alves, M., Bertinchamp, R., ... & Guidet,
B. (2014). Capillary refill time exploration during septic shock. Intensive care
medicine, vol. 40 (7), pp. 958-964. Doi: 10.1007/s00134-014-3326-4
Ait-Oufella, H., Joffre, J., Boelle, P. Y., Galbois, A., Bourcier, S., Baudel, J. L., ... & Maury, E.
(2012). Knee area tissue oxygen saturation is predictive of 14-day mortality in septic
shock. Intensive care medicine, vol. 38 (6), pp. 976-983. Doi: 10.1007/s00134-012-2555-
7
9
NURSING ASSIGNMENT
Carr, A. J., Robertsson, O., Graves, S., Price, A. J., Arden, N. K., Judge, A., & Beard, D. J.
(2012). Knee replacement. The Lancet, vol. 379 (9823), pp. 1331-1340. Doi:
https://doi.org/10.1016/S0140-6736(11)60752-6
Chang, C. B., & Cho, W. S. (2012). Pain management protocols, peri-operative pain and patient
satisfaction after total knee replacement: a multicentre study. J Bone Joint Surg Br, vol.
94 (11), pp. 1511-1516. Doi: https://doi.org/10.1302/0301-620X.94B11.29165
Colberg, S. R., & Vinik, A. I. (2014). Exercising with peripheral or autonomic neuropathy: what
health care providers and diabetic patients need to know. The Physician and
sportsmedicine, 42(1), 15-23. Doi: https://doi.org/10.3810/psm.2014.02.2043
Cornell, P., Gervis, M. T., Yates, L., & Vardaman, J. M. (2013). Improving shift report focus and
consistency with the situation, background, assessment, recommendation
protocol. Journal of Nursing Administration, vol. 43 (7/8), pp. 422-428. Doi:
10.1097/NNA.0b013e31829d6303
Friedman, R. J., Hess, S., Berkowitz, S. D., & Homering, M. (2013). Complication rates after hip
or knee arthroplasty in morbidly obese patients. Clinical Orthopaedics and Related
Research®, vol. 471 (10), pp. 3358-3366. Doi: https://doi.org/10.1007/s11999-013-3049-
9
Han, H. S., & Kang, S. B. (2013). Relations between long-term glycemic control and
postoperative wound and infectious complications after total knee arthroplasty in type 2
diabetics. Clinics in orthopedic surgery, vol. 5 (2), pp. 118-123. Doi:
https://doi.org/10.4055/cios.2013.5.2.118
NURSING ASSIGNMENT
Carr, A. J., Robertsson, O., Graves, S., Price, A. J., Arden, N. K., Judge, A., & Beard, D. J.
(2012). Knee replacement. The Lancet, vol. 379 (9823), pp. 1331-1340. Doi:
https://doi.org/10.1016/S0140-6736(11)60752-6
Chang, C. B., & Cho, W. S. (2012). Pain management protocols, peri-operative pain and patient
satisfaction after total knee replacement: a multicentre study. J Bone Joint Surg Br, vol.
94 (11), pp. 1511-1516. Doi: https://doi.org/10.1302/0301-620X.94B11.29165
Colberg, S. R., & Vinik, A. I. (2014). Exercising with peripheral or autonomic neuropathy: what
health care providers and diabetic patients need to know. The Physician and
sportsmedicine, 42(1), 15-23. Doi: https://doi.org/10.3810/psm.2014.02.2043
Cornell, P., Gervis, M. T., Yates, L., & Vardaman, J. M. (2013). Improving shift report focus and
consistency with the situation, background, assessment, recommendation
protocol. Journal of Nursing Administration, vol. 43 (7/8), pp. 422-428. Doi:
10.1097/NNA.0b013e31829d6303
Friedman, R. J., Hess, S., Berkowitz, S. D., & Homering, M. (2013). Complication rates after hip
or knee arthroplasty in morbidly obese patients. Clinical Orthopaedics and Related
Research®, vol. 471 (10), pp. 3358-3366. Doi: https://doi.org/10.1007/s11999-013-3049-
9
Han, H. S., & Kang, S. B. (2013). Relations between long-term glycemic control and
postoperative wound and infectious complications after total knee arthroplasty in type 2
diabetics. Clinics in orthopedic surgery, vol. 5 (2), pp. 118-123. Doi:
https://doi.org/10.4055/cios.2013.5.2.118
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10
NURSING ASSIGNMENT
Jans, Ø., Jørgensen, C., Kehlet, H., & Johansson, P. I. (2014). Role of preoperative anemia for
risk of transfusion and postoperative morbidity in fast‐track hip and knee
arthroplasty. Transfusion, vol. 54 (3), pp.717-726. Doi: 10.1111/trf.12332
Jørgensen, C. C., Madsbad, S., Kehlet, H., & Lundbeck Foundation Centre for Fast-track Hip
and Knee Replacement Collaborative Group. (2015). Postoperative morbidity and
mortality in type-2 diabetics after fast-track primary total hip and knee
arthroplasty. Anesthesia & Analgesia, vol. 120 (1), pp. 230-238. Doi:
10.1213/ANE.0000000000000451
King, D., Morton, R., & Bevan, C. (2013). How to use capillary refill time. Archives of Disease
in Childhood-Education and Practice, edpract-2013. Doi:
http://dx.doi.org/10.1136/archdischild-2013-305198
Lamplot, J. D., Wagner, E. R., & Manning, D. W. (2014). Multimodal pain management in total
knee arthroplasty: a prospective randomized controlled trial. The Journal of
arthroplasty, vol.29 (2), pp. 329-334. Doi: https://doi.org/10.1016/j.arth.2013.06.005
Liaw, S. Y., Zhou, W. T., Lau, T. C., Siau, C., & Chan, S. W. C. (2014). An interprofessional
communication training using simulation to enhance safe care for a deteriorating
patient. Nurse Education Today, vol. 34 (2), pp. 259-264.
Doi: https://doi.org/10.1016/j.nedt.2013.02.019
Maempel, J. F., Riddoch, F., Calleja, N., & Brenkel, I. J. (2015). Longer hospital stay, more
complications, and increased mortality but substantially improved function after knee
replacement in older patients: A study of 3,144 primary unilateral total knee
NURSING ASSIGNMENT
Jans, Ø., Jørgensen, C., Kehlet, H., & Johansson, P. I. (2014). Role of preoperative anemia for
risk of transfusion and postoperative morbidity in fast‐track hip and knee
arthroplasty. Transfusion, vol. 54 (3), pp.717-726. Doi: 10.1111/trf.12332
Jørgensen, C. C., Madsbad, S., Kehlet, H., & Lundbeck Foundation Centre for Fast-track Hip
and Knee Replacement Collaborative Group. (2015). Postoperative morbidity and
mortality in type-2 diabetics after fast-track primary total hip and knee
arthroplasty. Anesthesia & Analgesia, vol. 120 (1), pp. 230-238. Doi:
10.1213/ANE.0000000000000451
King, D., Morton, R., & Bevan, C. (2013). How to use capillary refill time. Archives of Disease
in Childhood-Education and Practice, edpract-2013. Doi:
http://dx.doi.org/10.1136/archdischild-2013-305198
Lamplot, J. D., Wagner, E. R., & Manning, D. W. (2014). Multimodal pain management in total
knee arthroplasty: a prospective randomized controlled trial. The Journal of
arthroplasty, vol.29 (2), pp. 329-334. Doi: https://doi.org/10.1016/j.arth.2013.06.005
Liaw, S. Y., Zhou, W. T., Lau, T. C., Siau, C., & Chan, S. W. C. (2014). An interprofessional
communication training using simulation to enhance safe care for a deteriorating
patient. Nurse Education Today, vol. 34 (2), pp. 259-264.
Doi: https://doi.org/10.1016/j.nedt.2013.02.019
Maempel, J. F., Riddoch, F., Calleja, N., & Brenkel, I. J. (2015). Longer hospital stay, more
complications, and increased mortality but substantially improved function after knee
replacement in older patients: A study of 3,144 primary unilateral total knee
11
NURSING ASSIGNMENT
replacements. Acta orthopaedica, vol. 86 (4), pp. 451-456. Doi:
https://doi.org/10.3109/17453674.2015.1040304
Manary, M. P., Boulding, W., Staelin, R., & Glickman, S. W. (2013). The patient experience and
health outcomes. New England Journal of Medicine, 368(3), 201-203.Doi:
10.1056/NEJMp1211775
Mok, W. Q., Wang, W., & Liaw, S. Y. (2015). Vital signs monitoring to detect patient
deterioration: An integrative literature review. International journal of nursing
practice, 21(S2), 91-98. Doi: 10.1111/ijn.12329
Mok, W., Wang, W., Cooper, S., Ang, E. N. K., & Liaw, S. Y. (2015). Attitudes towards vital
signs monitoring in the detection of clinical deterioration: scale development and survey
of ward nurses. International Journal for Quality in Health Care, 27(3), 207-213. Doi:
tps://doi.org/10.1093/intqhc/mzv019
Pape, B., Thiessen, P. S., Jakobsen, F., & Hansen, T. B. (2013). Interprofessional collaboration
may pay off: Introducing a collaborative approach in an orthopaedic ward. Journal of
interprofessional care, vol. 27 (6), pp. 496-500. Doi:
https://doi.org/10.3109/13561820.2013.808611
Parvizi, J., & Diaz-Ledezma, C. (2013). Total knee replacement with the use of a tourniquet:
more pros than cons. Bone Joint J, vol. 95(11 Supple A), pp.133-134. Doi:
https://doi.org/10.1302/0301-620X.95B11.32903
NURSING ASSIGNMENT
replacements. Acta orthopaedica, vol. 86 (4), pp. 451-456. Doi:
https://doi.org/10.3109/17453674.2015.1040304
Manary, M. P., Boulding, W., Staelin, R., & Glickman, S. W. (2013). The patient experience and
health outcomes. New England Journal of Medicine, 368(3), 201-203.Doi:
10.1056/NEJMp1211775
Mok, W. Q., Wang, W., & Liaw, S. Y. (2015). Vital signs monitoring to detect patient
deterioration: An integrative literature review. International journal of nursing
practice, 21(S2), 91-98. Doi: 10.1111/ijn.12329
Mok, W., Wang, W., Cooper, S., Ang, E. N. K., & Liaw, S. Y. (2015). Attitudes towards vital
signs monitoring in the detection of clinical deterioration: scale development and survey
of ward nurses. International Journal for Quality in Health Care, 27(3), 207-213. Doi:
tps://doi.org/10.1093/intqhc/mzv019
Pape, B., Thiessen, P. S., Jakobsen, F., & Hansen, T. B. (2013). Interprofessional collaboration
may pay off: Introducing a collaborative approach in an orthopaedic ward. Journal of
interprofessional care, vol. 27 (6), pp. 496-500. Doi:
https://doi.org/10.3109/13561820.2013.808611
Parvizi, J., & Diaz-Ledezma, C. (2013). Total knee replacement with the use of a tourniquet:
more pros than cons. Bone Joint J, vol. 95(11 Supple A), pp.133-134. Doi:
https://doi.org/10.1302/0301-620X.95B11.32903
12
NURSING ASSIGNMENT
Solimeno, L., Luck, J., Fondanesche, C., McLaughlin, P., Narayan, P., Sabbour, A., ... & Pasta,
G. (2012). Knee arthropathy: when things go wrong. Haemophilia, vol. 18 (s4), pp. 105-
111.Doi: 10.1111/j.1365-2516.2012.02834.x
Tomek, I. M., Sabel, A. L., Froimson, M. I., Muschler, G., Jevsevar, D. S., Koenig, K. M., ... &
Weeks, W. B. (2012). A collaborative of leading health systems finds wide variations in
total knee replacement delivery and takes steps to improve value. Health Affairs, vol. 31
(6), pp. 1329-1338. Doi: https://doi.org/10.1377/hlthaff.2011.0935
Wukich, D. K. (2015). Diabetes and its negative impact on outcomes in orthopaedic
surgery. World journal of orthopedics, vol. 6 (3), pp. 331. Doi: 10.5312/wjo.v6.i3.331
NURSING ASSIGNMENT
Solimeno, L., Luck, J., Fondanesche, C., McLaughlin, P., Narayan, P., Sabbour, A., ... & Pasta,
G. (2012). Knee arthropathy: when things go wrong. Haemophilia, vol. 18 (s4), pp. 105-
111.Doi: 10.1111/j.1365-2516.2012.02834.x
Tomek, I. M., Sabel, A. L., Froimson, M. I., Muschler, G., Jevsevar, D. S., Koenig, K. M., ... &
Weeks, W. B. (2012). A collaborative of leading health systems finds wide variations in
total knee replacement delivery and takes steps to improve value. Health Affairs, vol. 31
(6), pp. 1329-1338. Doi: https://doi.org/10.1377/hlthaff.2011.0935
Wukich, D. K. (2015). Diabetes and its negative impact on outcomes in orthopaedic
surgery. World journal of orthopedics, vol. 6 (3), pp. 331. Doi: 10.5312/wjo.v6.i3.331
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





