MRSA Infection: Impact and Control
VerifiedAdded on 2020/04/21
|12
|2993
|69
AI Summary
This assignment delves into the serious issue of Methicillin-Resistant Staphylococcus Aureus (MRSA) infection. It examines the bacteria's resistance mechanisms, particularly focusing on how MRSA hinders antibiotic penetration. The impact of MRSA is highlighted through examples like hospital outbreaks and its effect on cancer patients. The text also touches upon global antibiotic resistance patterns, emphasizing the need for effective control strategies.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: MRSA
MRSA
Name of the Student
Name of the University
Author note
MRSA
Name of the Student
Name of the University
Author note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1MRSA
Table of Contents
Introduction....................................................................................................................................2
Implications of MRSA outbreak..................................................................................................2
Results (MRSA treatment).............................................................................................................4
Discussion.....................................................................................................................................5
Consequences...........................................................................................................................5
Conclusion.....................................................................................................................................6
References....................................................................................................................................7
Appendix........................................................................................................................................9
Table of Contents
Introduction....................................................................................................................................2
Implications of MRSA outbreak..................................................................................................2
Results (MRSA treatment).............................................................................................................4
Discussion.....................................................................................................................................5
Consequences...........................................................................................................................5
Conclusion.....................................................................................................................................6
References....................................................................................................................................7
Appendix........................................................................................................................................9
2MRSA
Introduction
Methicillin-resistant Staphylococcus aureus (MRSA) is an infection caused by Staph
or type of Staphylococcus aureus bacteria that is resistant to antibiotics naturally residing on
the skin and nose. This bacterium is highly contagious and spread from an infected person
through direct contact. This infection occurs in groups who have prolonged hospital stays
impacting their health and at the same time result in dissemination of the organism to people
and environment. MRSA infection is divided into two forms: (hospital-acquired) HA-MRSA and
(community acquired) CA-MRSA. HA-MRSA is associated with infections occurring in medical
facilities like nursing homes or hospitals occurs through direct contact with contaminated hands
or infected wounds (1). CA-MRSA infections are transmitted through close contact with an
infected person and develop due to poor hygiene such as improper or infrequent hand washing.
HA-MRSA causes serious complications like pneumonia, sepsis or urinary tract infections
causing notable symptoms like rash, headaches, chills, fevers, cough, and fatigue, shortness of
breath or chest pain. CA-MRSA causes skin infections in the form of painful and woollen bump
on the skin called cellulitis. MRSA outbreak in hospitals has serious implications as it mainly
occur in individuals who have prolonged hospital stays. MRSA infection is resistant to antibiotics
and has severe side effects; however, it is treated with limited antibiotics higher than usual
antibiotics (2). These consequences have serious implications on the public health and
therefore, the following report deals with the implications of MRSA outbreak, treatment
procedures and consequences.
Of the 116 articles retrieved, only 26 were reviewed. A total number of 10 articles were included
in the present review as they met the inclusion criteria. Of these, 3 articles were selected for
studying the implications of MRSA outbreak; 2 articles were selected for highlighting the
methods for MRSA treatment; 5 articles were selected for assessing the consequences of
MRSA infection.
Implications of MRSA outbreak
MRSA has serious implications on public health in acute and long-term health settings
worldwide. The spread of infection in the hospitals are dangerous as it defy treatment and can
cause life-threatening illness. It can spread by direct contact or patients having open wounds
are mostly at risk for skin infections. According to Centres for Disease Control and Prevention
(CDC), one in three (33%) individuals is the carriers of this staph bacterium with absent of
Introduction
Methicillin-resistant Staphylococcus aureus (MRSA) is an infection caused by Staph
or type of Staphylococcus aureus bacteria that is resistant to antibiotics naturally residing on
the skin and nose. This bacterium is highly contagious and spread from an infected person
through direct contact. This infection occurs in groups who have prolonged hospital stays
impacting their health and at the same time result in dissemination of the organism to people
and environment. MRSA infection is divided into two forms: (hospital-acquired) HA-MRSA and
(community acquired) CA-MRSA. HA-MRSA is associated with infections occurring in medical
facilities like nursing homes or hospitals occurs through direct contact with contaminated hands
or infected wounds (1). CA-MRSA infections are transmitted through close contact with an
infected person and develop due to poor hygiene such as improper or infrequent hand washing.
HA-MRSA causes serious complications like pneumonia, sepsis or urinary tract infections
causing notable symptoms like rash, headaches, chills, fevers, cough, and fatigue, shortness of
breath or chest pain. CA-MRSA causes skin infections in the form of painful and woollen bump
on the skin called cellulitis. MRSA outbreak in hospitals has serious implications as it mainly
occur in individuals who have prolonged hospital stays. MRSA infection is resistant to antibiotics
and has severe side effects; however, it is treated with limited antibiotics higher than usual
antibiotics (2). These consequences have serious implications on the public health and
therefore, the following report deals with the implications of MRSA outbreak, treatment
procedures and consequences.
Of the 116 articles retrieved, only 26 were reviewed. A total number of 10 articles were included
in the present review as they met the inclusion criteria. Of these, 3 articles were selected for
studying the implications of MRSA outbreak; 2 articles were selected for highlighting the
methods for MRSA treatment; 5 articles were selected for assessing the consequences of
MRSA infection.
Implications of MRSA outbreak
MRSA has serious implications on public health in acute and long-term health settings
worldwide. The spread of infection in the hospitals are dangerous as it defy treatment and can
cause life-threatening illness. It can spread by direct contact or patients having open wounds
are mostly at risk for skin infections. According to Centres for Disease Control and Prevention
(CDC), one in three (33%) individuals is the carriers of this staph bacterium with absent of
3MRSA
illness and 2 in 100 are the MRSA carriers (3). MRSA is a drug resistant bacterium having
limited treatment options is affecting the lives of patients through massive spread of the infection
in the hospitals and communities. It is becoming impossible to eliminate the risk for infection as
it sustains antibiotics and is highly contagious.
In a study of MRSA outbreak in Orange County, California, it was found that hospitals
are the main regions where MRSA outbreak occurs that is affecting the hospital as a whole (4).
The extensive data collected from the hospital wards in terms of hospital stays, intraward
transmission coefficients (beta), time of readmission and loss rate. The result findings showed
that it not only affected single hospital, but also all the hospitals in the network depending upon
the demographic and outbreak size. The average transmission rate was high from single
hospital to other hospitals from 5% to 15%. This result suggests that MRSA infection is not
confined to one hospital. It spread to all the hospitals in that particular region. The strength of
the paper is that the result findings highlighted the need for prevention and infection control
strategies and policies accounting for interconnectedness in the healthcare facilities. The
obtained data can be applied to other regions, as it may be not unique. However, the paper has
certain limitations. The study was limited to the adult population and excluded the neonates in
long-term facilities or nursing homes. There might be fair chances of hospital outbreak when a
patient is being transferred in a nursing home patient.
In another study using Regional Healthcare Ecosystem Analyst (RHEA), authors
augmented that existing outbreaks in hospitals of California are added with nursing homes and
MRSA simulated outbreaks too other healthcare facilities (5). The results suggested that
although nursing homes are not directly connected with patient transfer also plays a vital role in
the spreading of hospital infection. Nursing homes and hospitals are connected to each other
both directly and indirectly in patients sharing contributing to the outbreak of MRSA having
serious implications for the patents, hospital staffs and community as a whole. The strength of
the study is that main findings provided understandable information for the spread and control of
infectious pathogen is important for all inpatient facilities like hospitals and nursing homes. The
main limitation of the paper is that it considered only in hospitals and underestimated the MRSA
in nursing homes and no data on emergency departments and again considered adult
population and not paediatrics as witnessed in the above study.
MRSA outbreak also has serious implications remaining above provincial benchmarks.
Due to MRSA-hospital, acquired infection (HAI), the daily work life and health of healthcare
illness and 2 in 100 are the MRSA carriers (3). MRSA is a drug resistant bacterium having
limited treatment options is affecting the lives of patients through massive spread of the infection
in the hospitals and communities. It is becoming impossible to eliminate the risk for infection as
it sustains antibiotics and is highly contagious.
In a study of MRSA outbreak in Orange County, California, it was found that hospitals
are the main regions where MRSA outbreak occurs that is affecting the hospital as a whole (4).
The extensive data collected from the hospital wards in terms of hospital stays, intraward
transmission coefficients (beta), time of readmission and loss rate. The result findings showed
that it not only affected single hospital, but also all the hospitals in the network depending upon
the demographic and outbreak size. The average transmission rate was high from single
hospital to other hospitals from 5% to 15%. This result suggests that MRSA infection is not
confined to one hospital. It spread to all the hospitals in that particular region. The strength of
the paper is that the result findings highlighted the need for prevention and infection control
strategies and policies accounting for interconnectedness in the healthcare facilities. The
obtained data can be applied to other regions, as it may be not unique. However, the paper has
certain limitations. The study was limited to the adult population and excluded the neonates in
long-term facilities or nursing homes. There might be fair chances of hospital outbreak when a
patient is being transferred in a nursing home patient.
In another study using Regional Healthcare Ecosystem Analyst (RHEA), authors
augmented that existing outbreaks in hospitals of California are added with nursing homes and
MRSA simulated outbreaks too other healthcare facilities (5). The results suggested that
although nursing homes are not directly connected with patient transfer also plays a vital role in
the spreading of hospital infection. Nursing homes and hospitals are connected to each other
both directly and indirectly in patients sharing contributing to the outbreak of MRSA having
serious implications for the patents, hospital staffs and community as a whole. The strength of
the study is that main findings provided understandable information for the spread and control of
infectious pathogen is important for all inpatient facilities like hospitals and nursing homes. The
main limitation of the paper is that it considered only in hospitals and underestimated the MRSA
in nursing homes and no data on emergency departments and again considered adult
population and not paediatrics as witnessed in the above study.
MRSA outbreak also has serious implications remaining above provincial benchmarks.
Due to MRSA-hospital, acquired infection (HAI), the daily work life and health of healthcare
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4MRSA
professionals is affected. Nurses experience challenges in workload, time pressures and
increase in documentation. The responsibilities of infection control measures are expanded
increasing the burden of financial costs in the healthcare organizations. In addition, there is also
intense cleaning and hygiene procedures required to control and prevent the transmission of
infection to other locations or individuals. Concisely, there is disruption of patient care and
hospital cost due to nosocomial outbreak demanding aggressive efforts for the prevention of
transmission to other healthcare settings.
Results (MRSA treatment)
MRSA infection spread and emergence need to be controlled, as there are limited
treatment options available due to its resistance to antibiotics. However, there are fewer
treatment options like prudent use of antibiotics towards antibiotic resistant bacteria (MRSA)
along with good hygiene and infection control practices like compliance to hand hygiene in both
hospital and community healthcare settings. MRSA is resistant to antibiotics like amoxicillin,
methicillin, oxacillin and penicillin that makes MRSA treatment challenging.
A research was conducted to study the effectiveness of treatment of MRSA by
antibiotics. Firstly, MRSA infection is incised and area is drained. IV antibiotics is effective for
the treatment of MRSA infections where first-line therapy, Vancomycin at an appropriate dose of
30 mg/kg is given in any 24 hours and gradually slowed down to 90 minutes for the prevention
of hypersensitivity called “red man syndrome”. Second-line therapy, Cubicin or Daptomycin at a
dosage of 4 to 6 mg/kg is administered every 24 hours. This drug is safe, although there are
implications like increase in creatine kinase levels. Linezolid is a third-line therapy given at a
dosage of 600mg every 12 hours and being a monoamine oxidase inhibitor, it offers
bioavailability of 100%.
Vancomycin has been the gold-standard treatment option for MRSA infections in
hospitalized patients, however, due to antibiotic resistance, clinical failure and dosing, poor
activity and slow cidality. A study conducted to show the treatment and resistance of MRSA
illustrated that vancomycin-intermediate S. aureus (VISA) contribute to the treatment failure due
to vancomycin and increased in MRSA related death rates. Heteroresistance results iin
reduction of MRSA response rates without affecting the mortality rates (6). Linezolid is effective
over vancomycin in soft tissues with 87% and 49% efficiency. Daptomycin is also effective
against MRSA infection belonging to newer group of oxazolidinones. The study is useful as it
provided ample amount of information regarding MRSA antibiotics for its treatment highlighting
professionals is affected. Nurses experience challenges in workload, time pressures and
increase in documentation. The responsibilities of infection control measures are expanded
increasing the burden of financial costs in the healthcare organizations. In addition, there is also
intense cleaning and hygiene procedures required to control and prevent the transmission of
infection to other locations or individuals. Concisely, there is disruption of patient care and
hospital cost due to nosocomial outbreak demanding aggressive efforts for the prevention of
transmission to other healthcare settings.
Results (MRSA treatment)
MRSA infection spread and emergence need to be controlled, as there are limited
treatment options available due to its resistance to antibiotics. However, there are fewer
treatment options like prudent use of antibiotics towards antibiotic resistant bacteria (MRSA)
along with good hygiene and infection control practices like compliance to hand hygiene in both
hospital and community healthcare settings. MRSA is resistant to antibiotics like amoxicillin,
methicillin, oxacillin and penicillin that makes MRSA treatment challenging.
A research was conducted to study the effectiveness of treatment of MRSA by
antibiotics. Firstly, MRSA infection is incised and area is drained. IV antibiotics is effective for
the treatment of MRSA infections where first-line therapy, Vancomycin at an appropriate dose of
30 mg/kg is given in any 24 hours and gradually slowed down to 90 minutes for the prevention
of hypersensitivity called “red man syndrome”. Second-line therapy, Cubicin or Daptomycin at a
dosage of 4 to 6 mg/kg is administered every 24 hours. This drug is safe, although there are
implications like increase in creatine kinase levels. Linezolid is a third-line therapy given at a
dosage of 600mg every 12 hours and being a monoamine oxidase inhibitor, it offers
bioavailability of 100%.
Vancomycin has been the gold-standard treatment option for MRSA infections in
hospitalized patients, however, due to antibiotic resistance, clinical failure and dosing, poor
activity and slow cidality. A study conducted to show the treatment and resistance of MRSA
illustrated that vancomycin-intermediate S. aureus (VISA) contribute to the treatment failure due
to vancomycin and increased in MRSA related death rates. Heteroresistance results iin
reduction of MRSA response rates without affecting the mortality rates (6). Linezolid is effective
over vancomycin in soft tissues with 87% and 49% efficiency. Daptomycin is also effective
against MRSA infection belonging to newer group of oxazolidinones. The study is useful as it
provided ample amount of information regarding MRSA antibiotics for its treatment highlighting
5MRSA
the significant developments that has taken place in the recent years to enhance the
understanding o treatment and resistance that occur in MRSA infections. However, the paper
did not address the novel molecular mechanisms for the development of new antibiotics in
MRSA infections treatment.
Fourth-line therapy can also be considered like Tygacil at a dosage of 100 mg IV once
followed by 50 mg IV every 12 hours having effective broad-spectrum antimicrobial activity.
Fifth-line therapy like dalfopristin (Synercid) or quinupristin can be used for MRSA treatment.
Oral antibiotics (first-line therapy) can also be used for MRSA treatment like
trimethoprim-sulfamethoxazole having 95% efficiency. clindamycin (Cleocin) is the second line
therapy, although the organism may develop resistance to the drug if the individual has
erythromycin resistance. Novel targets need to be identified for the treatment of MRSA
infections. A study explained that fifth generation antibiotics like carbapenems,
monobactams, cephalosporins, glycopeptides, and tetracyclines are effective in nature for
curbing the antimicrobial resistance in MRSA infection. However, the study did not address the
use of new antibiotics that is required for managing the antimicrobial resistance (7)
Discussion
Consequences
MRSA infection affects the quality of life of inpatients as it affects individuals suffering
from various life-threatening diseases in different clinical settings like ICUs, emergency
debarments, palliative care and among paediatric population. It poses serious burden on the
quality of life leading to patient isolation and burden of disease in the community and hospitals
(8). For example, the first study on MRSA infection among cancer patients explored the impact
of the infection on the patient and their family members (9). The main findings showed that it
has significant impact on the patients giving rise to distress and ineffective coping mechanisms
with MRSA infection in cancer patients. It has a negative impact on the patients as they
experience stigmatization and feelings of anger and frustration when being diagnosed with
MRSA infection. It also has negative impact on their relationships and overall care as they
experience isolation where patients are not at fault. However, the paper has certain limitations,
as the sample size was small that prevented generalizations to wider cancer population. The
comparison of perceived impact of cancer to MRSA infection was a major limitation of the study
the significant developments that has taken place in the recent years to enhance the
understanding o treatment and resistance that occur in MRSA infections. However, the paper
did not address the novel molecular mechanisms for the development of new antibiotics in
MRSA infections treatment.
Fourth-line therapy can also be considered like Tygacil at a dosage of 100 mg IV once
followed by 50 mg IV every 12 hours having effective broad-spectrum antimicrobial activity.
Fifth-line therapy like dalfopristin (Synercid) or quinupristin can be used for MRSA treatment.
Oral antibiotics (first-line therapy) can also be used for MRSA treatment like
trimethoprim-sulfamethoxazole having 95% efficiency. clindamycin (Cleocin) is the second line
therapy, although the organism may develop resistance to the drug if the individual has
erythromycin resistance. Novel targets need to be identified for the treatment of MRSA
infections. A study explained that fifth generation antibiotics like carbapenems,
monobactams, cephalosporins, glycopeptides, and tetracyclines are effective in nature for
curbing the antimicrobial resistance in MRSA infection. However, the study did not address the
use of new antibiotics that is required for managing the antimicrobial resistance (7)
Discussion
Consequences
MRSA infection affects the quality of life of inpatients as it affects individuals suffering
from various life-threatening diseases in different clinical settings like ICUs, emergency
debarments, palliative care and among paediatric population. It poses serious burden on the
quality of life leading to patient isolation and burden of disease in the community and hospitals
(8). For example, the first study on MRSA infection among cancer patients explored the impact
of the infection on the patient and their family members (9). The main findings showed that it
has significant impact on the patients giving rise to distress and ineffective coping mechanisms
with MRSA infection in cancer patients. It has a negative impact on the patients as they
experience stigmatization and feelings of anger and frustration when being diagnosed with
MRSA infection. It also has negative impact on their relationships and overall care as they
experience isolation where patients are not at fault. However, the paper has certain limitations,
as the sample size was small that prevented generalizations to wider cancer population. The
comparison of perceived impact of cancer to MRSA infection was a major limitation of the study
6MRSA
and pose implications for future studies for the evaluation of psychiatric impact of MRSA
infection on patients with advanced cancer.
Staph bacterium antibiotic resistance is another consequence that is contributing to
the increase in infections spread and transmission rates. Due to the widespread infection rates,
MRSA has clinical and economic impact on the patient, healthcare settings and community (10).
This poses a substantial burden of infections that are resistant on the hospital for the analysis of
cost parameters associated with the infection episode. There is also increase in total costs
contributing to the antimicrobial therapy that includes delivery costs and drug acquisition. Apart
from economic outcomes, there is increase in length of hospital stays being another
consequence of S.aureus. The increase in hospital stays promotes late hospital discharge
increasing the financial costs and inefficiency of hospital (11).
MRSA infection has serious consequences on patient health and quality of life. It causes
guilt, humiliation and anger among the patients who encounter with ignorant staffs while seeking
care. MRSA infection also makes the patients feel isolated, being traumatic and encounter a
feeling of being imprisoned with improper rehabilitation. Patients feel stigmatized as they
experience fear and unprofessional behaviour from the medical staffs. There are increased
ineffective infection measures taken by hospital staffs that also pose serious consequences on
patient suffering. Concisely, MRSA infection outbreak in a particular hospital or community pose
clinical and economic burden to the overall care, quality of life of inpatients and healthcare
systems as a whole (12).
Conclusion
From the above discussion, it can be concluded that MRSA infection and its outbreak is
an epidemic that not only infects a particular hospital or community, but also infect the whole
region posing serious implications. It has serious clinical and economic impact on the patients,
their families and hospital staffs, especially nurses. As MRSA gives rise to antibiotic resistance,
it has limited treatment options. Some of the antibiotics especially, second-line therapyis
effective like Linezolid and Daptomycin through IV. Oral antibiotics are also given in some
special cases having 95% efficiency. Although, there are treatments options available for the
MRSA infection treatment, there are serious consequences of MRSA infection spread. It
hampers the quality of life of the patients due to isolation and stigmatization. As a result, they
feel distressed, scared, and guilty and agitated however, the patients are not at fault. It also
and pose implications for future studies for the evaluation of psychiatric impact of MRSA
infection on patients with advanced cancer.
Staph bacterium antibiotic resistance is another consequence that is contributing to
the increase in infections spread and transmission rates. Due to the widespread infection rates,
MRSA has clinical and economic impact on the patient, healthcare settings and community (10).
This poses a substantial burden of infections that are resistant on the hospital for the analysis of
cost parameters associated with the infection episode. There is also increase in total costs
contributing to the antimicrobial therapy that includes delivery costs and drug acquisition. Apart
from economic outcomes, there is increase in length of hospital stays being another
consequence of S.aureus. The increase in hospital stays promotes late hospital discharge
increasing the financial costs and inefficiency of hospital (11).
MRSA infection has serious consequences on patient health and quality of life. It causes
guilt, humiliation and anger among the patients who encounter with ignorant staffs while seeking
care. MRSA infection also makes the patients feel isolated, being traumatic and encounter a
feeling of being imprisoned with improper rehabilitation. Patients feel stigmatized as they
experience fear and unprofessional behaviour from the medical staffs. There are increased
ineffective infection measures taken by hospital staffs that also pose serious consequences on
patient suffering. Concisely, MRSA infection outbreak in a particular hospital or community pose
clinical and economic burden to the overall care, quality of life of inpatients and healthcare
systems as a whole (12).
Conclusion
From the above discussion, it can be concluded that MRSA infection and its outbreak is
an epidemic that not only infects a particular hospital or community, but also infect the whole
region posing serious implications. It has serious clinical and economic impact on the patients,
their families and hospital staffs, especially nurses. As MRSA gives rise to antibiotic resistance,
it has limited treatment options. Some of the antibiotics especially, second-line therapyis
effective like Linezolid and Daptomycin through IV. Oral antibiotics are also given in some
special cases having 95% efficiency. Although, there are treatments options available for the
MRSA infection treatment, there are serious consequences of MRSA infection spread. It
hampers the quality of life of the patients due to isolation and stigmatization. As a result, they
feel distressed, scared, and guilty and agitated however, the patients are not at fault. It also
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7MRSA
pose burden of financial costs and affect the work life of healthcare professionals. Nurses and
other healthcare professionals have to look for effective infection control measures to reduce
the transmission of the disease. In addition, MRSA is getting resistant towards antibiotics with
novel genetic mechanisms. Therefore, there is requirement of effective infection control
measure and antibiotics that target the novel genetic mechanism that causes resistance to anti-
MRSA antibiotics with enhanced research efforts.
References
1. Tong SY, Davis JS, Eichenberger E, Holland TL, Fowler VG. Staphylococcus aureus
infections: epidemiology, pathophysiology, clinical manifestations, and management.
Clinical microbiology reviews. 2015 Jul 1;28(3):603-61.
2. Ray P, Gautam V, Singh R. Methicillin-resistant Staphylococcus aureus (MRSA) in
developing and developed countries: implications and solutions. InRegional Health
Forum 2011 (Vol. 15, No. 1, pp. 74-82).
3. Dantes R, Mu Y, Belflower R, Aragon D, Dumyati G, Harrison LH, Lessa FC, Lynfield R,
Nadle J, Petit S, Ray SM. National burden of invasive methicillin-resistant
Staphylococcus aureus infections, United States, 2011. JAMA internal medicine. 2013
Nov 25;173(21):1970-8.
4. Lee BY, McGlone SM, Wong KF, Yilmaz SL, Avery TR, Song Y, Christie R, Eubank S,
Brown ST, Epstein JM, Parker JI. Modeling the spread of methicillin-resistant
Staphylococcus aureus (MRSA) outbreaks throughout the hospitals in Orange County,
California. Infection Control & Hospital Epidemiology. 2011 Jun;32(6):562-72.
5. Lee BY, Bartsch SM, Wong KF, Singh A, Avery TR, Kim DS, Brown ST, Murphy CR,
Yilmaz SL, Potter MA, Huang SS. The importance of nursing homes in the spread of
methicillin-resistant Staphylococcus aureus (MRSA) among hospitals. Medical care.
2013 Mar;51(3):205.
6. Gould IM, David MZ, Esposito S, Garau J, Lina G, Mazzei T, Peters G. New insights into
meticillin-resistant Staphylococcus aureus (MRSA) pathogenesis, treatment and
resistance. International journal of antimicrobial agents. 2012 Feb 29;39(2):96-104.
7. Bassetti M, Merelli M, Temperoni C, Astilean A. New antibiotics for bad bugs: where are
we?. Annals of clinical microbiology and antimicrobials. 2013 Aug 28;12(1):22.
8. Bükki J, Klein J, But L, Montag T, Wenchel HM, Voltz R, Ostgathe C. Methicillin-resistant
Staphylococcus aureus (MRSA) management in palliative care units and hospices in
pose burden of financial costs and affect the work life of healthcare professionals. Nurses and
other healthcare professionals have to look for effective infection control measures to reduce
the transmission of the disease. In addition, MRSA is getting resistant towards antibiotics with
novel genetic mechanisms. Therefore, there is requirement of effective infection control
measure and antibiotics that target the novel genetic mechanism that causes resistance to anti-
MRSA antibiotics with enhanced research efforts.
References
1. Tong SY, Davis JS, Eichenberger E, Holland TL, Fowler VG. Staphylococcus aureus
infections: epidemiology, pathophysiology, clinical manifestations, and management.
Clinical microbiology reviews. 2015 Jul 1;28(3):603-61.
2. Ray P, Gautam V, Singh R. Methicillin-resistant Staphylococcus aureus (MRSA) in
developing and developed countries: implications and solutions. InRegional Health
Forum 2011 (Vol. 15, No. 1, pp. 74-82).
3. Dantes R, Mu Y, Belflower R, Aragon D, Dumyati G, Harrison LH, Lessa FC, Lynfield R,
Nadle J, Petit S, Ray SM. National burden of invasive methicillin-resistant
Staphylococcus aureus infections, United States, 2011. JAMA internal medicine. 2013
Nov 25;173(21):1970-8.
4. Lee BY, McGlone SM, Wong KF, Yilmaz SL, Avery TR, Song Y, Christie R, Eubank S,
Brown ST, Epstein JM, Parker JI. Modeling the spread of methicillin-resistant
Staphylococcus aureus (MRSA) outbreaks throughout the hospitals in Orange County,
California. Infection Control & Hospital Epidemiology. 2011 Jun;32(6):562-72.
5. Lee BY, Bartsch SM, Wong KF, Singh A, Avery TR, Kim DS, Brown ST, Murphy CR,
Yilmaz SL, Potter MA, Huang SS. The importance of nursing homes in the spread of
methicillin-resistant Staphylococcus aureus (MRSA) among hospitals. Medical care.
2013 Mar;51(3):205.
6. Gould IM, David MZ, Esposito S, Garau J, Lina G, Mazzei T, Peters G. New insights into
meticillin-resistant Staphylococcus aureus (MRSA) pathogenesis, treatment and
resistance. International journal of antimicrobial agents. 2012 Feb 29;39(2):96-104.
7. Bassetti M, Merelli M, Temperoni C, Astilean A. New antibiotics for bad bugs: where are
we?. Annals of clinical microbiology and antimicrobials. 2013 Aug 28;12(1):22.
8. Bükki J, Klein J, But L, Montag T, Wenchel HM, Voltz R, Ostgathe C. Methicillin-resistant
Staphylococcus aureus (MRSA) management in palliative care units and hospices in
8MRSA
Germany: a nationwide survey on patient isolation policies and quality of life. Palliative
medicine. 2013 Jan;27(1):84-90.
9. Gleeson A, Larkin P, O’Sullivan N. The impact of meticillin-resistant Staphylococcus
aureus on patients with advanced cancer and their family members: A qualitative study.
Palliative medicine. 2016 Apr;30(4):382-91.
10. Shittu AO, Okon K, Adesida S, Oyedara O, Witte W, Strommenger B, Layer F, Nübel U.
Antibiotic resistance and molecular epidemiology of Staphylococcus aureus in Nigeria.
BMC microbiology. 2011 May 5;11(1):92.
11. de Kraker ME, Wolkewitz M, Davey PG, Grundmann H, BURDEN Study Group. The
clinical impact of antimicrobial resistance in European hospitals: excess mortality and
length of hospital stay related to methicillin resistant Staphylococcus aureus bloodstream
infections. Antimicrobial agents and chemotherapy. 2011 Jan 10.
12. Giedraitienė A, Vitkauskienė A, Naginienė R, Pavilonis A. Antibiotic resistance
mechanisms of clinically important bacteria. Medicina. 2011;47(3):137-46.
Germany: a nationwide survey on patient isolation policies and quality of life. Palliative
medicine. 2013 Jan;27(1):84-90.
9. Gleeson A, Larkin P, O’Sullivan N. The impact of meticillin-resistant Staphylococcus
aureus on patients with advanced cancer and their family members: A qualitative study.
Palliative medicine. 2016 Apr;30(4):382-91.
10. Shittu AO, Okon K, Adesida S, Oyedara O, Witte W, Strommenger B, Layer F, Nübel U.
Antibiotic resistance and molecular epidemiology of Staphylococcus aureus in Nigeria.
BMC microbiology. 2011 May 5;11(1):92.
11. de Kraker ME, Wolkewitz M, Davey PG, Grundmann H, BURDEN Study Group. The
clinical impact of antimicrobial resistance in European hospitals: excess mortality and
length of hospital stay related to methicillin resistant Staphylococcus aureus bloodstream
infections. Antimicrobial agents and chemotherapy. 2011 Jan 10.
12. Giedraitienė A, Vitkauskienė A, Naginienė R, Pavilonis A. Antibiotic resistance
mechanisms of clinically important bacteria. Medicina. 2011;47(3):137-46.
9MRSA
Appendix
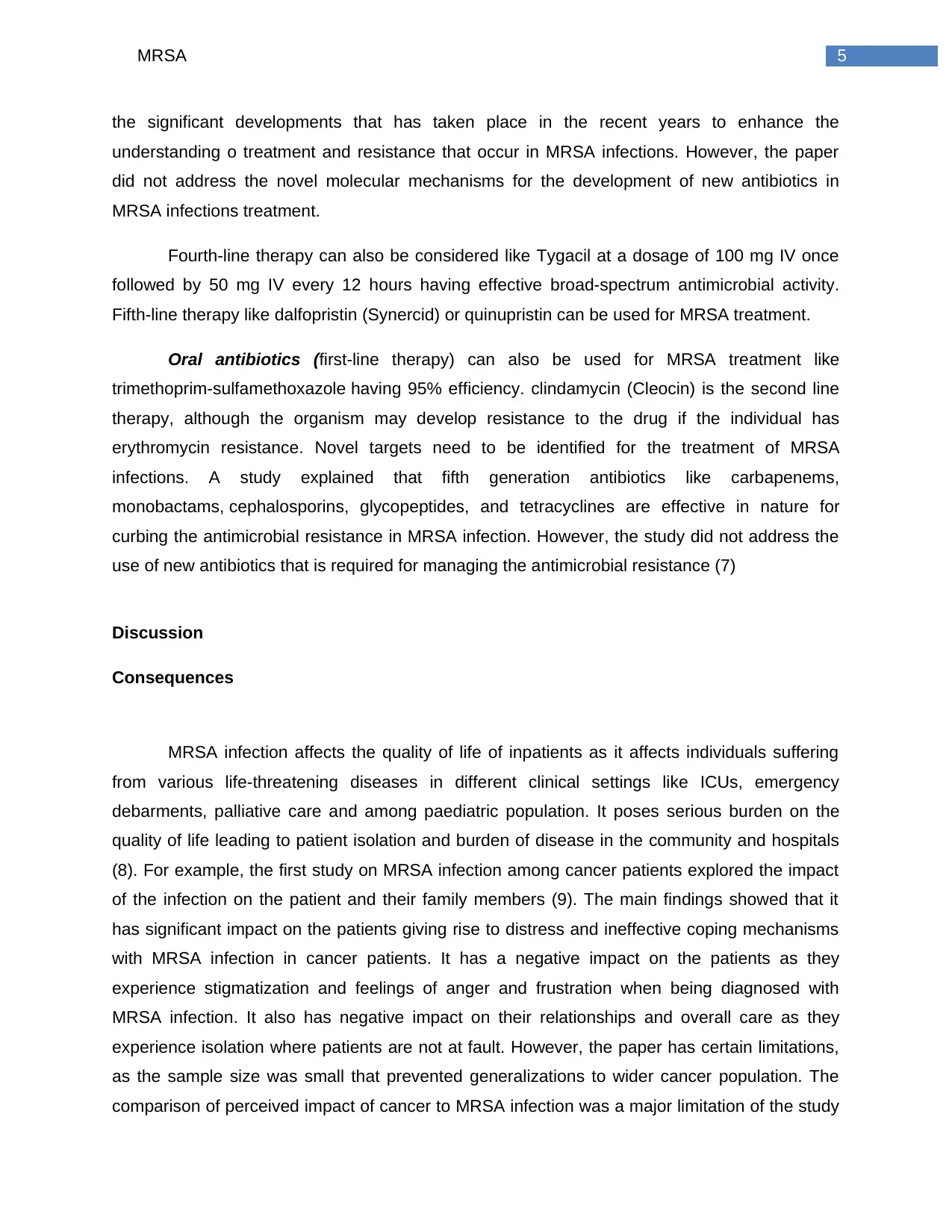
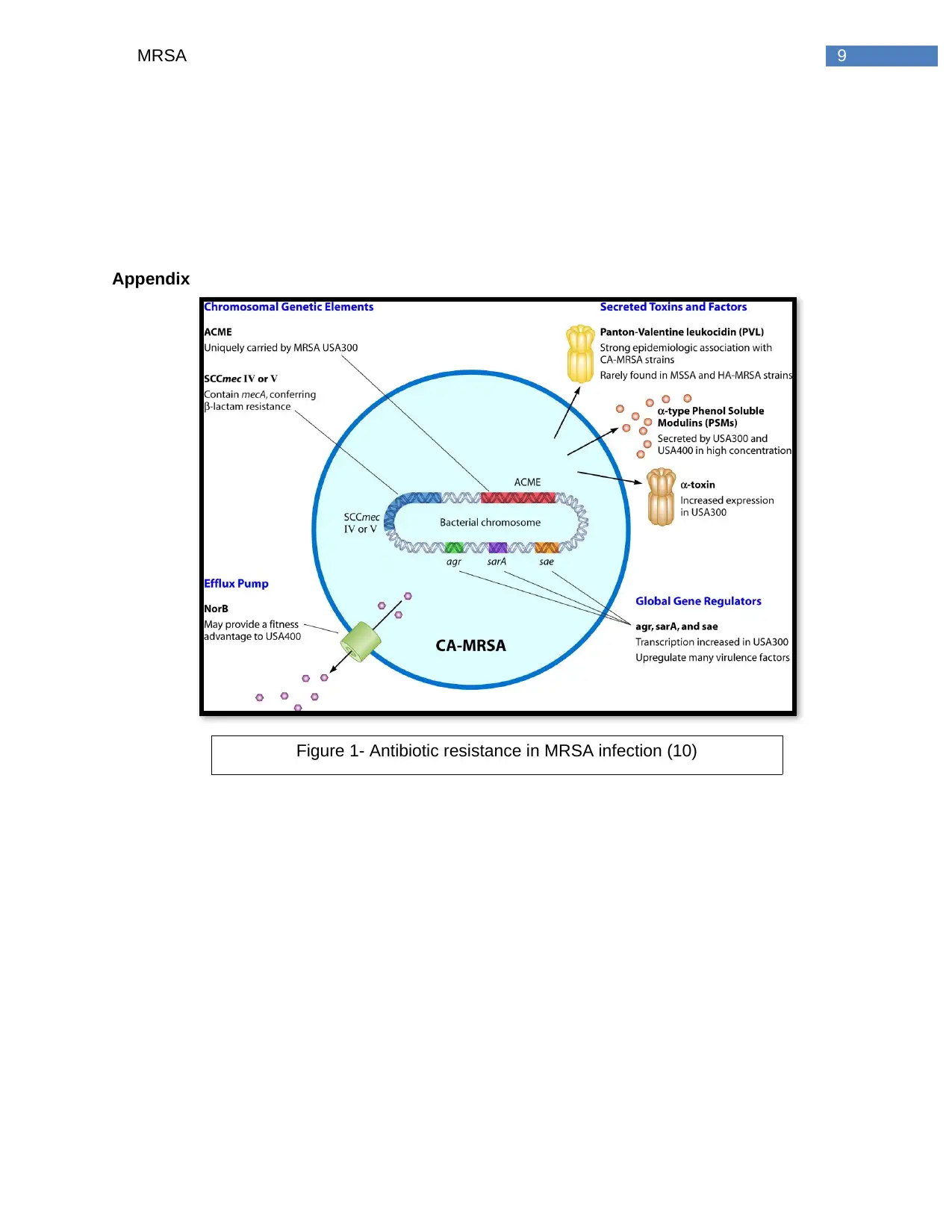
Figure 1- Antibiotic resistance in MRSA infection (10)
Appendix
Figure 1- Antibiotic resistance in MRSA infection (10)
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10MRSA
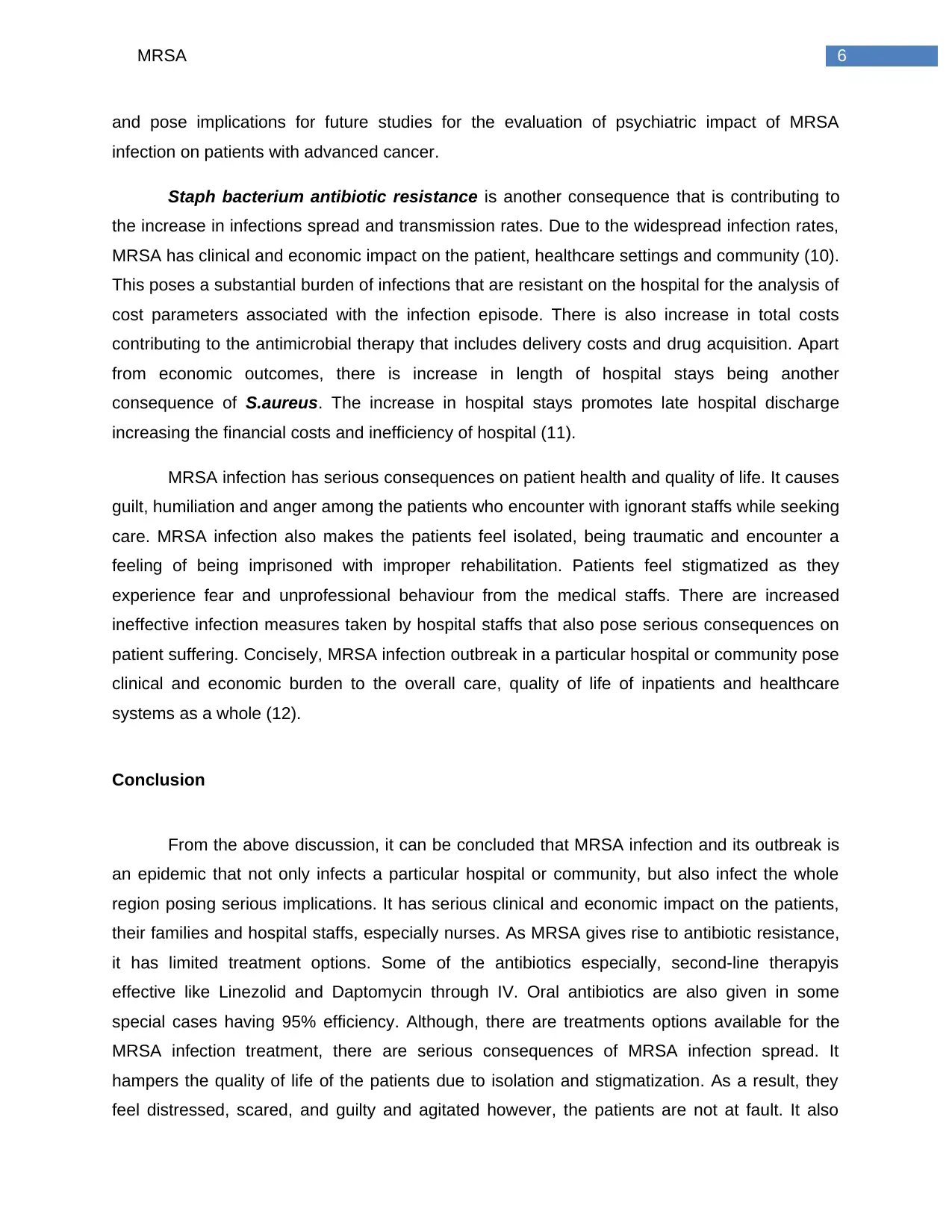
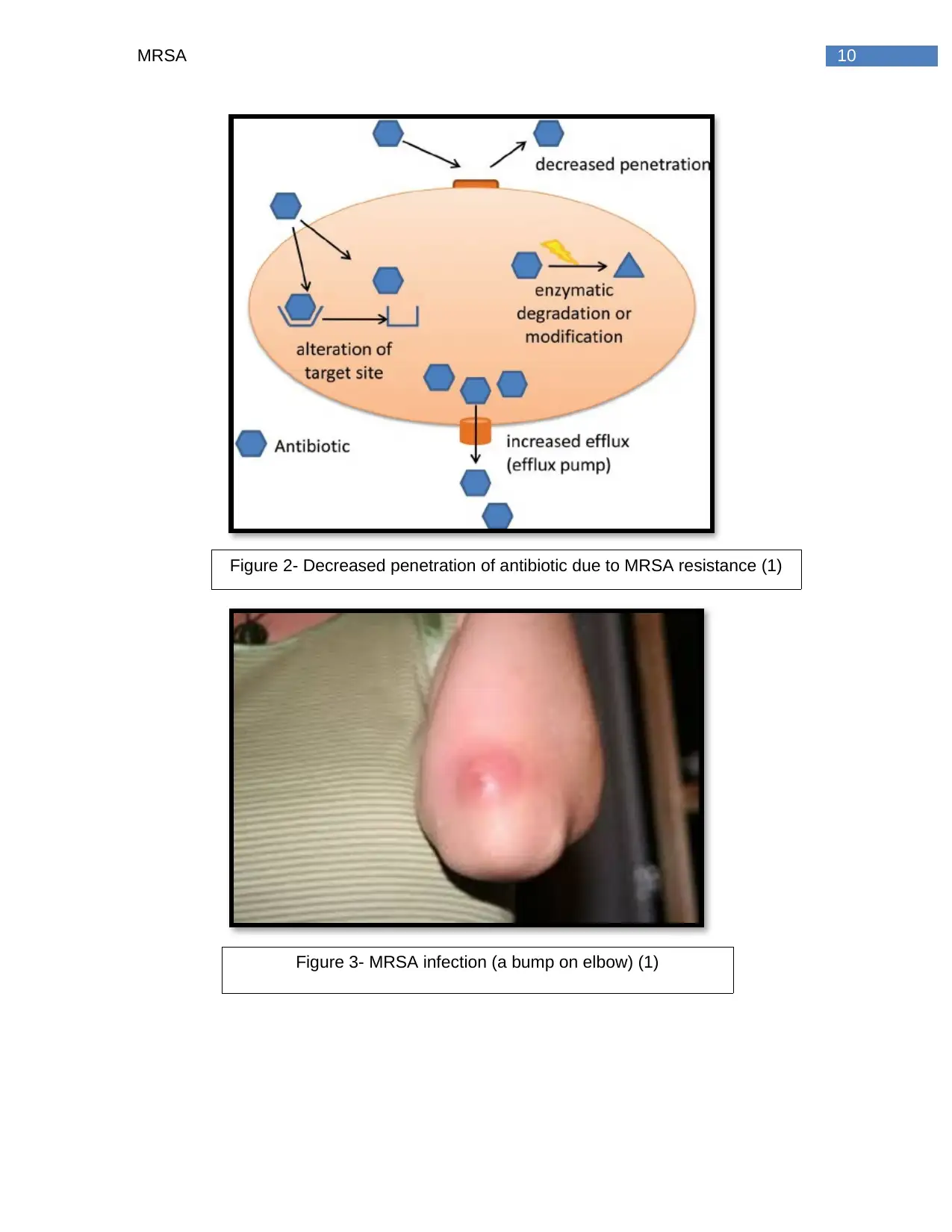
Figure 2- Decreased penetration of antibiotic due to MRSA resistance (1)
Figure 3- MRSA infection (a bump on elbow) (1)
Figure 2- Decreased penetration of antibiotic due to MRSA resistance (1)
Figure 3- MRSA infection (a bump on elbow) (1)
11MRSA
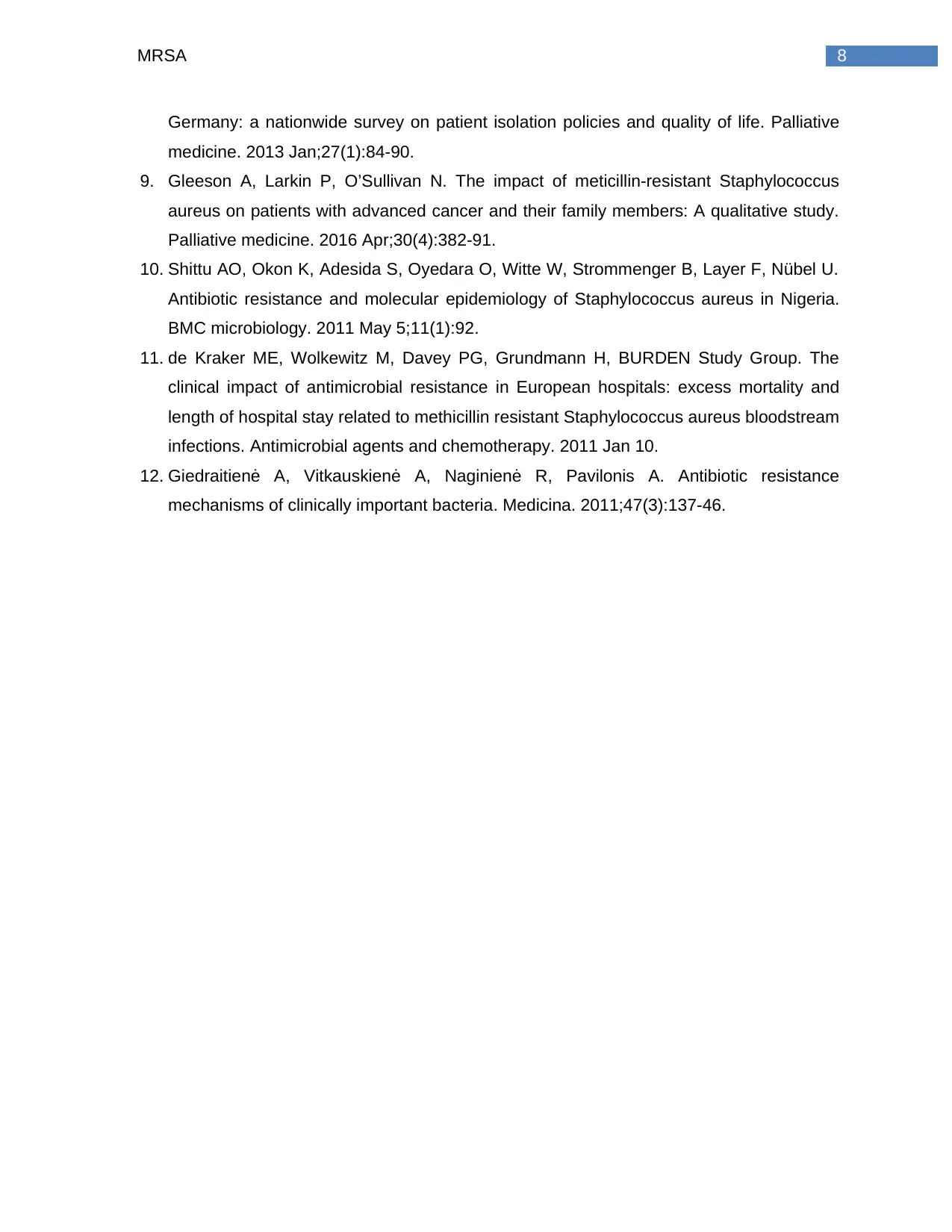
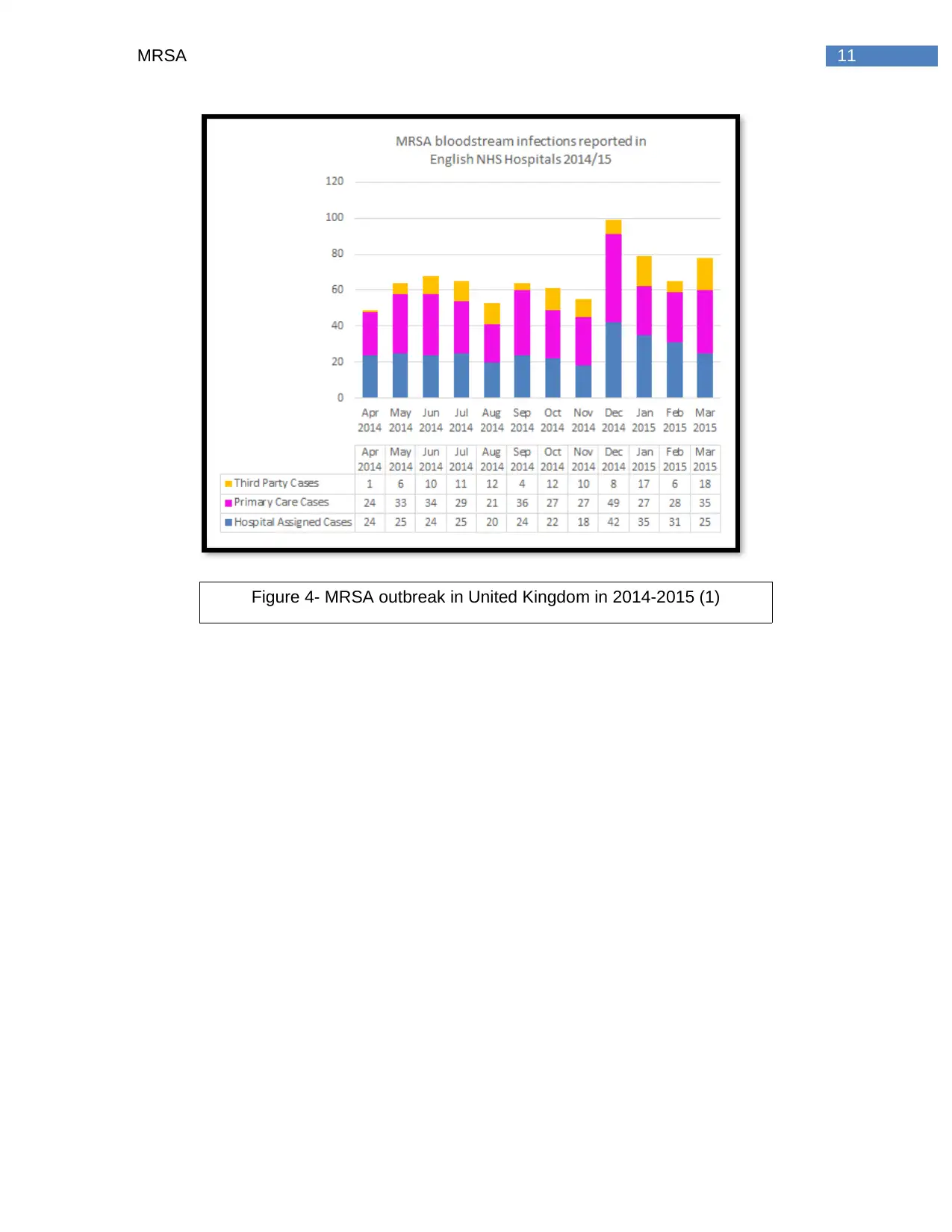
Figure 4- MRSA outbreak in United Kingdom in 2014-2015 (1)
Figure 4- MRSA outbreak in United Kingdom in 2014-2015 (1)
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





