Nursing Case Study: Wound Management and Diabetic Foot Ulcer Treatment
VerifiedAdded on 2020/05/04
|20
|4935
|259
Case Study
AI Summary
This case study presents a 62-year-old male patient, Mr. Mclean, who developed a diabetic foot ulcer following coronary artery bypass surgery. The report details the patient's medical history, including type 2 diabetes, hypertension, atherosclerosis, and peripheral neuropathy, highlighting the factors contributing to the ulcer's development and progression. It examines the anatomy and pathophysiology of the wound, explaining the involvement of different foot compartments and the impact of vascular insufficiency and neuropathy. The study then outlines the stages of wound healing—inflammation, proliferation, and maturation—and emphasizes the importance of integrated wound assessment. It discusses the wound management principles and nursing interventions, including the need for surgical removal or amputation to prevent further infection spread, focusing on the current non-healing ulcer on the right foot. The case underscores the challenges of diabetic foot ulcers, their impact on patient quality of life, and the importance of proactive wound management strategies to prevent lower extremity amputation.

Running head: NURSING ASSIGNMENT
Case Study on Wound Management
Name of the Student
Name of the University
Author Note
Case Study on Wound Management
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

1NURSING ASSIGNMENT
Executive summary
Incidence of diabetes has almost quadrupled among the entire adult population of the world in
the past three decades. Within this adult population, diabetic foot ulcers (DFUs) are reported to
be prevalent. 1 in 4 persons develop a risk of ulceration in their life time. High financial costs are
associated with the complications of the disease. A significant proportion of the high costs,
account for the treatment of lower limb extremities. Escalating costs and increased incidence
create a devastating impact on health services. They put pressure on resources. This report aims
to explain a case study of a patient suffering from diabetic foot ulcer. It will describe the wound
management principles and nursing interventions that will be followed to treat him.
Executive summary
Incidence of diabetes has almost quadrupled among the entire adult population of the world in
the past three decades. Within this adult population, diabetic foot ulcers (DFUs) are reported to
be prevalent. 1 in 4 persons develop a risk of ulceration in their life time. High financial costs are
associated with the complications of the disease. A significant proportion of the high costs,
account for the treatment of lower limb extremities. Escalating costs and increased incidence
create a devastating impact on health services. They put pressure on resources. This report aims
to explain a case study of a patient suffering from diabetic foot ulcer. It will describe the wound
management principles and nursing interventions that will be followed to treat him.
2NURSING ASSIGNMENT
Table of Contents
Introduction..........................................................................................................................3
Patient summary..................................................................................................................3
Anatomy and pathophysiology of the wound......................................................................5
Stages of wound healing......................................................................................................7
Inflammation....................................................................................................................8
Proliferation.....................................................................................................................8
Maturation........................................................................................................................9
Integrated wound assessment..............................................................................................9
Wound management..........................................................................................................10
Nursing interventions.........................................................................................................13
Conclusion.........................................................................................................................14
References..........................................................................................................................15
Table of Contents
Introduction..........................................................................................................................3
Patient summary..................................................................................................................3
Anatomy and pathophysiology of the wound......................................................................5
Stages of wound healing......................................................................................................7
Inflammation....................................................................................................................8
Proliferation.....................................................................................................................8
Maturation........................................................................................................................9
Integrated wound assessment..............................................................................................9
Wound management..........................................................................................................10
Nursing interventions.........................................................................................................13
Conclusion.........................................................................................................................14
References..........................................................................................................................15
You're viewing a preview
Unlock full access by subscribing today!
3NURSING ASSIGNMENT
Introduction
Diabetic foot ulcers (DFUs) are serious complications associated with adverse health
consequences and high treatment costs. They create a significant impact on the quality of life of
the patients. Diabetes is responsible for causing damage to the vascular supply and nerves
present in the legs and feet. Patients who experience diabetic neuropathy, often report reduced or
absence of sensation in their arms. Therefore, these patients become unaware of any trauma or
injury to their feet that has been caused by presence of unwanted objects such as stone, pins or
glass in their shoes or due to ill-fitting footwear (Yazdanpanah, Nasiri & Adarvishi 2015, p. 37).
Continuing walking on such an injured foot damages it further and creates serious consequences
from the minor lesions. DFUs co-exist with vascular insufficiency.
They account for the major cause of amputation and gangrene among people with
diabetes. Management of such diabetic foot ulcers therefore requires wound offloading with the
usage of appropriate therapeutic footwear, administration of daily saline or dressings that provide
a moist environment to the wound environment. This report will focus on a case study of a
patient with diabetic foot ulcer and will illustrate the wound management techniques that are
needed to be practiced.
Patient summary
Mr. Mclean (name changed) is a 62-year old male who was admitted to the post-
operative ward following a coronary artery bypass surgery. He suffered from coronary artery
disease that occurred due to plaque deposition in the inner walls of the coronary arteries. The
surgery was performed to improve blood flow to his heart. His previous history of hypertension
Introduction
Diabetic foot ulcers (DFUs) are serious complications associated with adverse health
consequences and high treatment costs. They create a significant impact on the quality of life of
the patients. Diabetes is responsible for causing damage to the vascular supply and nerves
present in the legs and feet. Patients who experience diabetic neuropathy, often report reduced or
absence of sensation in their arms. Therefore, these patients become unaware of any trauma or
injury to their feet that has been caused by presence of unwanted objects such as stone, pins or
glass in their shoes or due to ill-fitting footwear (Yazdanpanah, Nasiri & Adarvishi 2015, p. 37).
Continuing walking on such an injured foot damages it further and creates serious consequences
from the minor lesions. DFUs co-exist with vascular insufficiency.
They account for the major cause of amputation and gangrene among people with
diabetes. Management of such diabetic foot ulcers therefore requires wound offloading with the
usage of appropriate therapeutic footwear, administration of daily saline or dressings that provide
a moist environment to the wound environment. This report will focus on a case study of a
patient with diabetic foot ulcer and will illustrate the wound management techniques that are
needed to be practiced.
Patient summary
Mr. Mclean (name changed) is a 62-year old male who was admitted to the post-
operative ward following a coronary artery bypass surgery. He suffered from coronary artery
disease that occurred due to plaque deposition in the inner walls of the coronary arteries. The
surgery was performed to improve blood flow to his heart. His previous history of hypertension
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4NURSING ASSIGNMENT
and type 2 diabetes mellitus acted as major contributing factors in the occurrence of the
cardiovascular disorder. On observing his medical charts it was known that he had a previous
history of atherosclerosis and hypercholesterolemia. The former occurred due to thickening of
the arterial walls due to invasion and accumulation of WBCs. On the other hand, the
hypercholesterolemia indicated high cholesterol levels in his blood. This principally occurred
due to obesity and diet patterns. Upon admission it was observed that he presented symptoms of
depression, anxiety and peripheral neuropathy. Mr. Mclean reported signs of ulcer between his
first and second toe prior to the surgery. He had been prescribed oral antibiotics for the ulcer. He
followed the prescriptions accordingly and the ulcer seemed to heal well before the surgical
intervention.
However, on the third day post the CABG surgery, he presented with a left foot swelling.
The swelling began to deteriorate on the fourth day and presented symptoms of oedema and
erythema. There was pain, swelling and redness in the ulcer region on his foot. The surface of the
skin around the wound became red due to an increase in blood flow in the capillaries. On the
tenth day, extensive ulceration was observed between his first and second toe. There was deep
space abscess due to pus accumulation in the ulcer site. The first toe on the left foot got severely
affected and the bone became tender due to lump formation and got exposed. He reported severe
pain in the bone along with a high body temperature. This led to the development of
osteomyelitis. The bone was amputated to prevent further spread of the infection to other parts of
the legs. The amputated site got healed rapidly. However, the current site of ulcer formation is
the fourth toe on his right foot. The ulcer is non-healing and will supposedly cause severe
damage to the surrounding bones and tissues. Therefore, a surgical removal procedure or
amputation needs to be followed to prevent the spread of this infection. The present study will
and type 2 diabetes mellitus acted as major contributing factors in the occurrence of the
cardiovascular disorder. On observing his medical charts it was known that he had a previous
history of atherosclerosis and hypercholesterolemia. The former occurred due to thickening of
the arterial walls due to invasion and accumulation of WBCs. On the other hand, the
hypercholesterolemia indicated high cholesterol levels in his blood. This principally occurred
due to obesity and diet patterns. Upon admission it was observed that he presented symptoms of
depression, anxiety and peripheral neuropathy. Mr. Mclean reported signs of ulcer between his
first and second toe prior to the surgery. He had been prescribed oral antibiotics for the ulcer. He
followed the prescriptions accordingly and the ulcer seemed to heal well before the surgical
intervention.
However, on the third day post the CABG surgery, he presented with a left foot swelling.
The swelling began to deteriorate on the fourth day and presented symptoms of oedema and
erythema. There was pain, swelling and redness in the ulcer region on his foot. The surface of the
skin around the wound became red due to an increase in blood flow in the capillaries. On the
tenth day, extensive ulceration was observed between his first and second toe. There was deep
space abscess due to pus accumulation in the ulcer site. The first toe on the left foot got severely
affected and the bone became tender due to lump formation and got exposed. He reported severe
pain in the bone along with a high body temperature. This led to the development of
osteomyelitis. The bone was amputated to prevent further spread of the infection to other parts of
the legs. The amputated site got healed rapidly. However, the current site of ulcer formation is
the fourth toe on his right foot. The ulcer is non-healing and will supposedly cause severe
damage to the surrounding bones and tissues. Therefore, a surgical removal procedure or
amputation needs to be followed to prevent the spread of this infection. The present study will
5NURSING ASSIGNMENT
focus on the wound management techniques that need to be adopted to prevent lower extremity
amputation in the patient.
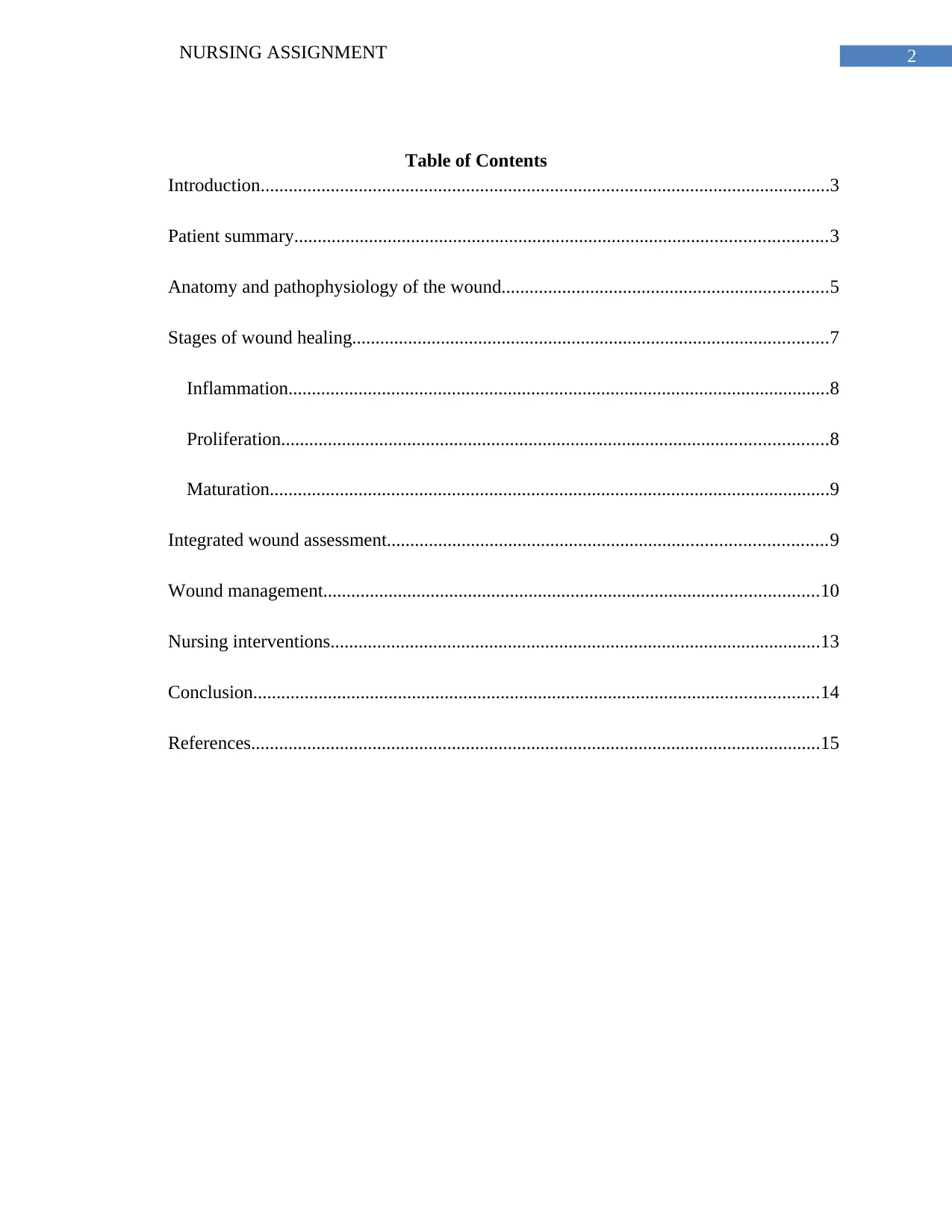
Anatomy and pathophysiology of the wound
The foot infection is a limb threatening condition for the patient. There are several
compartments in the foot, which inter-communicate with each other and lead to the spread of the
infection. The foot is divided into 3 plantar compartments: lateral, central and medial. A rigid
plantar aponeurosis forms the compartments floor. It is attached to a calcaneus and distally
extends to the toes. The outermost fascia forms the plantar aponeurosis and represents the layer
located beneath the subcutaneous tissue (Telfer et al. 2014, p. e109994). The medial
intermuscular septum separates the central and medial foot compartments and extends to the first
head of the metatarsal from the medial calcaneal tuberosity. A lateral intermuscular septum
separates the lateral and central compartments. It extends to the fifth head of the metatarsal from
the calcaneus.
Figure 1- Diabetic Foot Ulcer
(Source- Thenurseszone.com 2017)
focus on the wound management techniques that need to be adopted to prevent lower extremity
amputation in the patient.
Anatomy and pathophysiology of the wound
The foot infection is a limb threatening condition for the patient. There are several
compartments in the foot, which inter-communicate with each other and lead to the spread of the
infection. The foot is divided into 3 plantar compartments: lateral, central and medial. A rigid
plantar aponeurosis forms the compartments floor. It is attached to a calcaneus and distally
extends to the toes. The outermost fascia forms the plantar aponeurosis and represents the layer
located beneath the subcutaneous tissue (Telfer et al. 2014, p. e109994). The medial
intermuscular septum separates the central and medial foot compartments and extends to the first
head of the metatarsal from the medial calcaneal tuberosity. A lateral intermuscular septum
separates the lateral and central compartments. It extends to the fifth head of the metatarsal from
the calcaneus.
Figure 1- Diabetic Foot Ulcer
(Source- Thenurseszone.com 2017)
You're viewing a preview
Unlock full access by subscribing today!
6NURSING ASSIGNMENT
During ulcer formation, the tendons and thin layer of subcutaneous tissue present in the
dorsal compartment got exposed. There was poor vascularisation in the tendons located in the
compartments. This lead to infection spread throughout the foot structure. The tendons that get
infected become oedematous, thickened, broad and purulent (Alavi et al. 2014, p. 3 ). Moreover,
these infections spread from a region of higher pressure to that of lower pressure. Therefore, it is
essential to physically examine an infected diabetic foot. That helps in identification of the point
of bacterial entry.
A prior foot ulcer is almost considered as a prerequisite for such infections. Results from
several studies indicate that these foot ulcers have a multifactorial nature. Insulin deficiency
forms the basis of various biochemical abnormalities that lead to the occurrence of diabetic
complications such as peripheral neuropathy. Evidence suggests that persistent glycemic control,
with either the administration of oral medications or insulin are effective in preventing or
regressing these complications. A complex interaction of 2 risk factors, peripheral vascular
disease and diabetic neuropathy governs the occurrence of foot ulcers (Noor, Zubair and Ahmad
2015, p. 195). Bilateral and symmetric neuropathy plays an essential role and lead to varying
degrees of sensory, autonomic and motor functions. Peripheral vascular disease that results from
atherosclerosis plays a secondary role. More than 60% of diabetic foot ulcers are classified as
neuropathic. This makes the ulcers go unnoticed as the patients are fail to detect injuries or
trauma in their lower extremities (Alavi et al. 2014, p. 22).
More than a quarter of all diabetic hospital admissions, are accounted for by foot ulcers
or infections. Owing to their high recurrence rates, the cost of treatment increases tremendously
(Rice et al. 2014, p. 655). Diabetic patients have a greater incidence of atherosclerosis, arteriolar
hyalinosis, thickening of capillary basement membrane, and endothelial proliferation. Various
During ulcer formation, the tendons and thin layer of subcutaneous tissue present in the
dorsal compartment got exposed. There was poor vascularisation in the tendons located in the
compartments. This lead to infection spread throughout the foot structure. The tendons that get
infected become oedematous, thickened, broad and purulent (Alavi et al. 2014, p. 3 ). Moreover,
these infections spread from a region of higher pressure to that of lower pressure. Therefore, it is
essential to physically examine an infected diabetic foot. That helps in identification of the point
of bacterial entry.
A prior foot ulcer is almost considered as a prerequisite for such infections. Results from
several studies indicate that these foot ulcers have a multifactorial nature. Insulin deficiency
forms the basis of various biochemical abnormalities that lead to the occurrence of diabetic
complications such as peripheral neuropathy. Evidence suggests that persistent glycemic control,
with either the administration of oral medications or insulin are effective in preventing or
regressing these complications. A complex interaction of 2 risk factors, peripheral vascular
disease and diabetic neuropathy governs the occurrence of foot ulcers (Noor, Zubair and Ahmad
2015, p. 195). Bilateral and symmetric neuropathy plays an essential role and lead to varying
degrees of sensory, autonomic and motor functions. Peripheral vascular disease that results from
atherosclerosis plays a secondary role. More than 60% of diabetic foot ulcers are classified as
neuropathic. This makes the ulcers go unnoticed as the patients are fail to detect injuries or
trauma in their lower extremities (Alavi et al. 2014, p. 22).
More than a quarter of all diabetic hospital admissions, are accounted for by foot ulcers
or infections. Owing to their high recurrence rates, the cost of treatment increases tremendously
(Rice et al. 2014, p. 655). Diabetic patients have a greater incidence of atherosclerosis, arteriolar
hyalinosis, thickening of capillary basement membrane, and endothelial proliferation. Various
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7NURSING ASSIGNMENT
medium and large-sized arteries like, femoropopliteal vessels and aortoiliac vessels show
symptoms of atherosclerosis. In combination with digital artery disease and in absence of
adequate blood flow, these ulcers quickly develop and progress to form gangrene (type of
necrosis) (Pickwell et al. 2015, p. 855). The patient’s previous history of atherosclerosis and
peripheral neuropathy contributed to the occurrence of the ulcer. Furthermore, he reported a
history of depression and smoking habit. Both of these factors trigger the formation of ulcers
among diabetic patients and may directly interfere with the healing of the wound located at the
fourth toe of his right foot.
Stages of wound healing
Diabetic foot ulcers are thought to be the leading cause of amputations and affect more
than 15% diabetic patients. Wound healing is defined as a natural response to restore injured
tissues. It is a result of interaction between a cascade of cellular events that work to reconstruct
and restore the injured skin tissues. Wound healing is generally divided into three phases as
stated below:
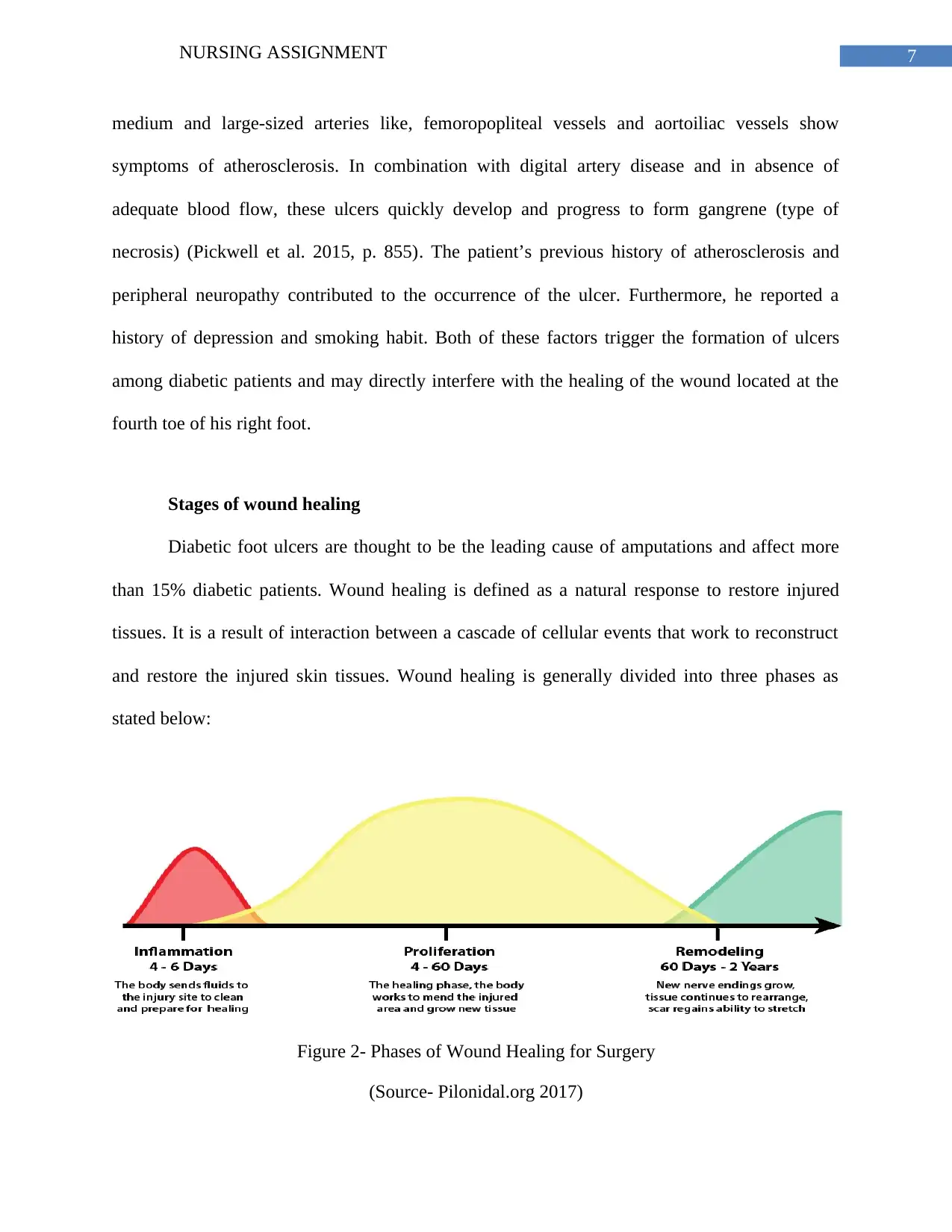
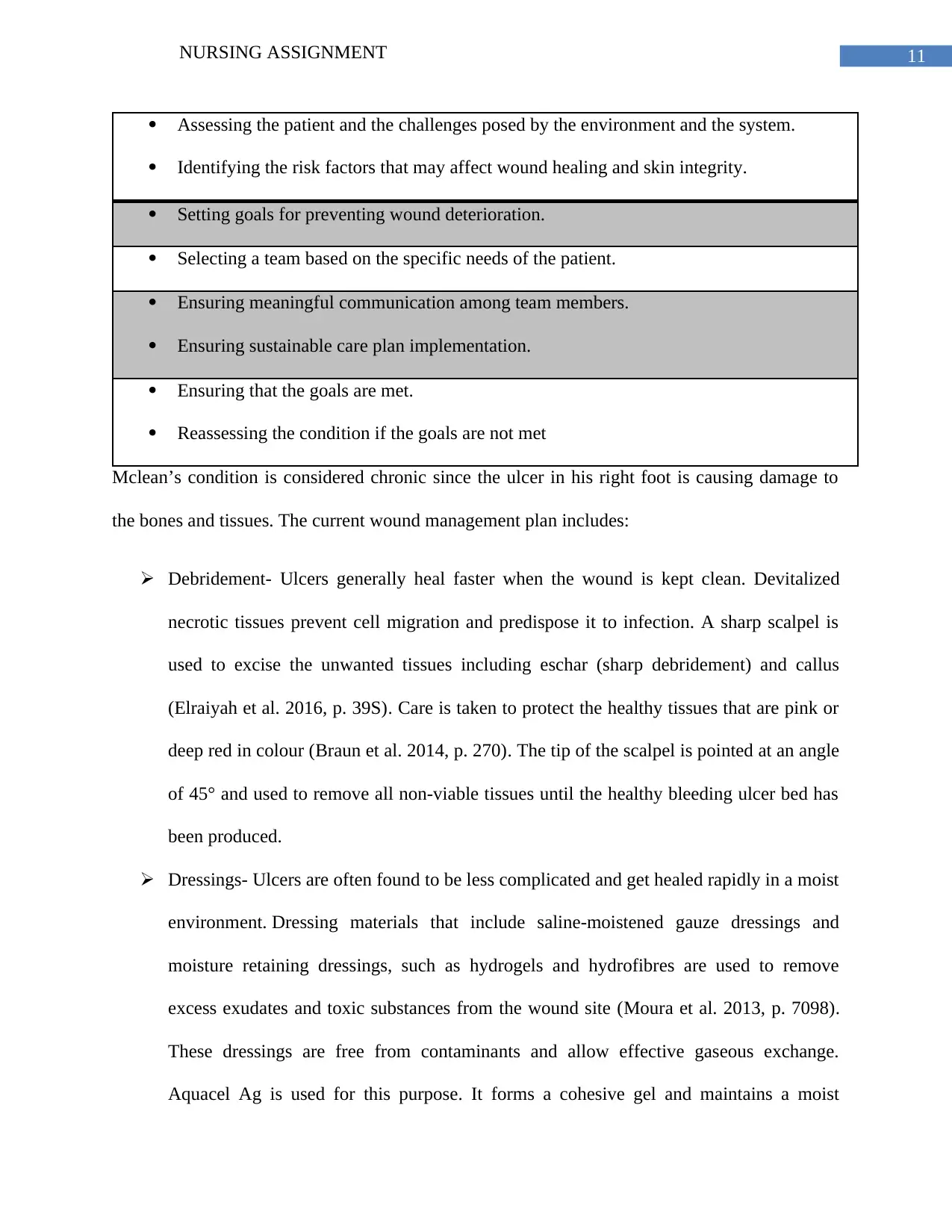
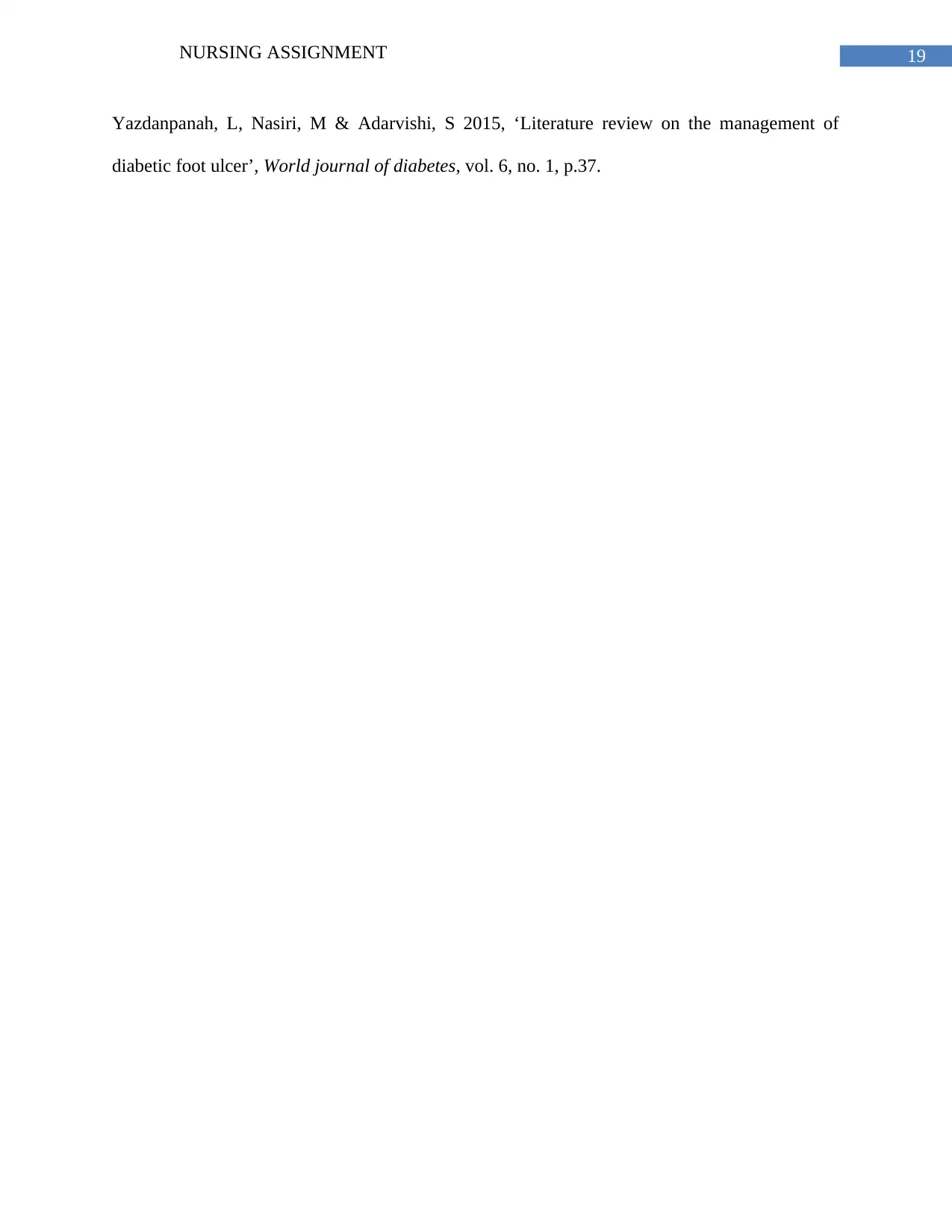
Figure 2- Phases of Wound Healing for Surgery
(Source- Pilonidal.org 2017)
medium and large-sized arteries like, femoropopliteal vessels and aortoiliac vessels show
symptoms of atherosclerosis. In combination with digital artery disease and in absence of
adequate blood flow, these ulcers quickly develop and progress to form gangrene (type of
necrosis) (Pickwell et al. 2015, p. 855). The patient’s previous history of atherosclerosis and
peripheral neuropathy contributed to the occurrence of the ulcer. Furthermore, he reported a
history of depression and smoking habit. Both of these factors trigger the formation of ulcers
among diabetic patients and may directly interfere with the healing of the wound located at the
fourth toe of his right foot.
Stages of wound healing
Diabetic foot ulcers are thought to be the leading cause of amputations and affect more
than 15% diabetic patients. Wound healing is defined as a natural response to restore injured
tissues. It is a result of interaction between a cascade of cellular events that work to reconstruct
and restore the injured skin tissues. Wound healing is generally divided into three phases as
stated below:
Figure 2- Phases of Wound Healing for Surgery
(Source- Pilonidal.org 2017)
8NURSING ASSIGNMENT
Inflammation
It is the first phase and is described as the natural response of the body to trauma. Once
the wound has been inflicted on the tissues, the blood vessels begin to constrict and seal
themselves. This occurs simultaneously with the formation of clot by the platelets. The clot
prevents further bleeding (Douaiher et al. 2014, p. 211). Thus, homeostasis is achieved. On
reaching a steady state, there is dilation of the blood vessels which allows antibodies, WBCs,
enzymes and other useful elements to reach the wounded area and promote wound healing. Thus,
infection gets prevented.
Proliferation
The second stage involves rebuilding of new granulation tissue. It is essential for the
blood vessels to receive adequate supply of oxygen and nutrient to facilitate the formation of
granulation tissue. A mixture of collagen and extracellular matrix leads helps in generation for
the new tissue. This provides opportunities for development of a network of blood vessels that
replace the damaged vessels, by a process known as angiogenesis (Greaves et al. 2013, p. 210).
The colour of the granulation tissue indicates the severity of the injury. A pink or red colour
generally indicates a healthy wound. However, a dark coloured tissue often indicates serious
infection or insufficient blood delivery to the site of wound formation.
In addition to the development of granulation tissues, the damaged mesenchymal cells of
the body get transformed into fibroblasts (Maxson et al. 2012, p. 147). These fibroblasts act as
bridges and facilitate the movement of cells around the affected area. In presence of a healthy
wound, the fibroblasts appear within three days of infection and start secreting collagen and
other liquids. These secretions play an active role in strengthening the wound site. During
Inflammation
It is the first phase and is described as the natural response of the body to trauma. Once
the wound has been inflicted on the tissues, the blood vessels begin to constrict and seal
themselves. This occurs simultaneously with the formation of clot by the platelets. The clot
prevents further bleeding (Douaiher et al. 2014, p. 211). Thus, homeostasis is achieved. On
reaching a steady state, there is dilation of the blood vessels which allows antibodies, WBCs,
enzymes and other useful elements to reach the wounded area and promote wound healing. Thus,
infection gets prevented.
Proliferation
The second stage involves rebuilding of new granulation tissue. It is essential for the
blood vessels to receive adequate supply of oxygen and nutrient to facilitate the formation of
granulation tissue. A mixture of collagen and extracellular matrix leads helps in generation for
the new tissue. This provides opportunities for development of a network of blood vessels that
replace the damaged vessels, by a process known as angiogenesis (Greaves et al. 2013, p. 210).
The colour of the granulation tissue indicates the severity of the injury. A pink or red colour
generally indicates a healthy wound. However, a dark coloured tissue often indicates serious
infection or insufficient blood delivery to the site of wound formation.
In addition to the development of granulation tissues, the damaged mesenchymal cells of
the body get transformed into fibroblasts (Maxson et al. 2012, p. 147). These fibroblasts act as
bridges and facilitate the movement of cells around the affected area. In presence of a healthy
wound, the fibroblasts appear within three days of infection and start secreting collagen and
other liquids. These secretions play an active role in strengthening the wound site. During
You're viewing a preview
Unlock full access by subscribing today!
9NURSING ASSIGNMENT
proliferation, the wound continuously grows stronger along with reorganisation of the
fibroblasts. This assists in new tissue development and accelerates the wound healing process.
Maturation
Maturation or remodelling is the last phase of wound healing. It occurs after closure of
the wound and may take more than 2 years. The dermal tissues are overhauled in this stage. This
enhances their tensile strength. Furthermore, there is replacement of the non-functional
fibroblasts by functional ones (Darby et al. 2014, p. 301). A decline in cellular activity is
observed with time, followed by a decrease in the number of blood vessels present at the site of
injury. Failure to abide by the treatment plan may lead to breaking down of the wound.
Integrated wound assessment
There are several intrinsic and extrinsic factors that can inhibit wound healing in Mclean.
Before a wound management plan is undertaken, it is essential to investigate the underlying
cause for the occurrence of the wound.
Diabetes- Diabetic foot ulcers are accelerated by several microvascular and
macrovascular changes that precede diabetic retinopathy. Cardiovascular diseases also play a key
role in the formatioin of such ulcers. Moreover, wound healing gets impaired by elevated blood
sugar levels. Leukocyte function gets impaired, angiogenesis is reduced and the risk of infection
increases (Deribe, Woldemichael & Nemera 2014, p. 5). Mclean has a long history of type 2
diabetes. The elevated blood glucose levels will make him more prone to infection, slow wound
healing and create more ulcers.
Peripheral neuropathy- Gycemic control and duration of diabetes are associated with the
incidence of neuropathy (Dubský et al. 2013, p. 558). Mcclean’s medical records suggest that he
proliferation, the wound continuously grows stronger along with reorganisation of the
fibroblasts. This assists in new tissue development and accelerates the wound healing process.
Maturation
Maturation or remodelling is the last phase of wound healing. It occurs after closure of
the wound and may take more than 2 years. The dermal tissues are overhauled in this stage. This
enhances their tensile strength. Furthermore, there is replacement of the non-functional
fibroblasts by functional ones (Darby et al. 2014, p. 301). A decline in cellular activity is
observed with time, followed by a decrease in the number of blood vessels present at the site of
injury. Failure to abide by the treatment plan may lead to breaking down of the wound.
Integrated wound assessment
There are several intrinsic and extrinsic factors that can inhibit wound healing in Mclean.
Before a wound management plan is undertaken, it is essential to investigate the underlying
cause for the occurrence of the wound.
Diabetes- Diabetic foot ulcers are accelerated by several microvascular and
macrovascular changes that precede diabetic retinopathy. Cardiovascular diseases also play a key
role in the formatioin of such ulcers. Moreover, wound healing gets impaired by elevated blood
sugar levels. Leukocyte function gets impaired, angiogenesis is reduced and the risk of infection
increases (Deribe, Woldemichael & Nemera 2014, p. 5). Mclean has a long history of type 2
diabetes. The elevated blood glucose levels will make him more prone to infection, slow wound
healing and create more ulcers.
Peripheral neuropathy- Gycemic control and duration of diabetes are associated with the
incidence of neuropathy (Dubský et al. 2013, p. 558). Mcclean’s medical records suggest that he
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10NURSING ASSIGNMENT
has a history of peripheral neuropathy. This led to lack of sensation in both feet. It also put him
at risk of developing ulcers (Waaijman et al. 2014, p. 1703). Loss of sensation prevented him
from detecting any trauma or injury to the legs.
Depression- Depression directly influences the immune and endocrine system. In
addition, it also leads to the formation of unhealthy habits, poor sleep patterns, sedentary
lifestyle, inadequate nutrition and substance abuse (Iversen et al. 2015, p. 22). The prevalence of
depressive symptoms adversely affected his health and wound healing.
Smoking- It creates detrimental effects on wound healing process. Smoking has been
associated with insulin resistance, which in turn increases blood sugar levels. This increased the
likelihood of getting affected with diabetic ulcer and may inhibit the healing process.
The management plan would include:
Removal of non-viable tissues (debridement).
Awareness on exposed capsule or tendon.
Management of exudates (appropriate dressing).
Management of bacterial burden (antimicrobial agents) (Lavery et al. 2016, p. 115).
Protection of granulation or epithelial tissue (non-adherent dressings).
Rehydration of wound bed (hydrogels).
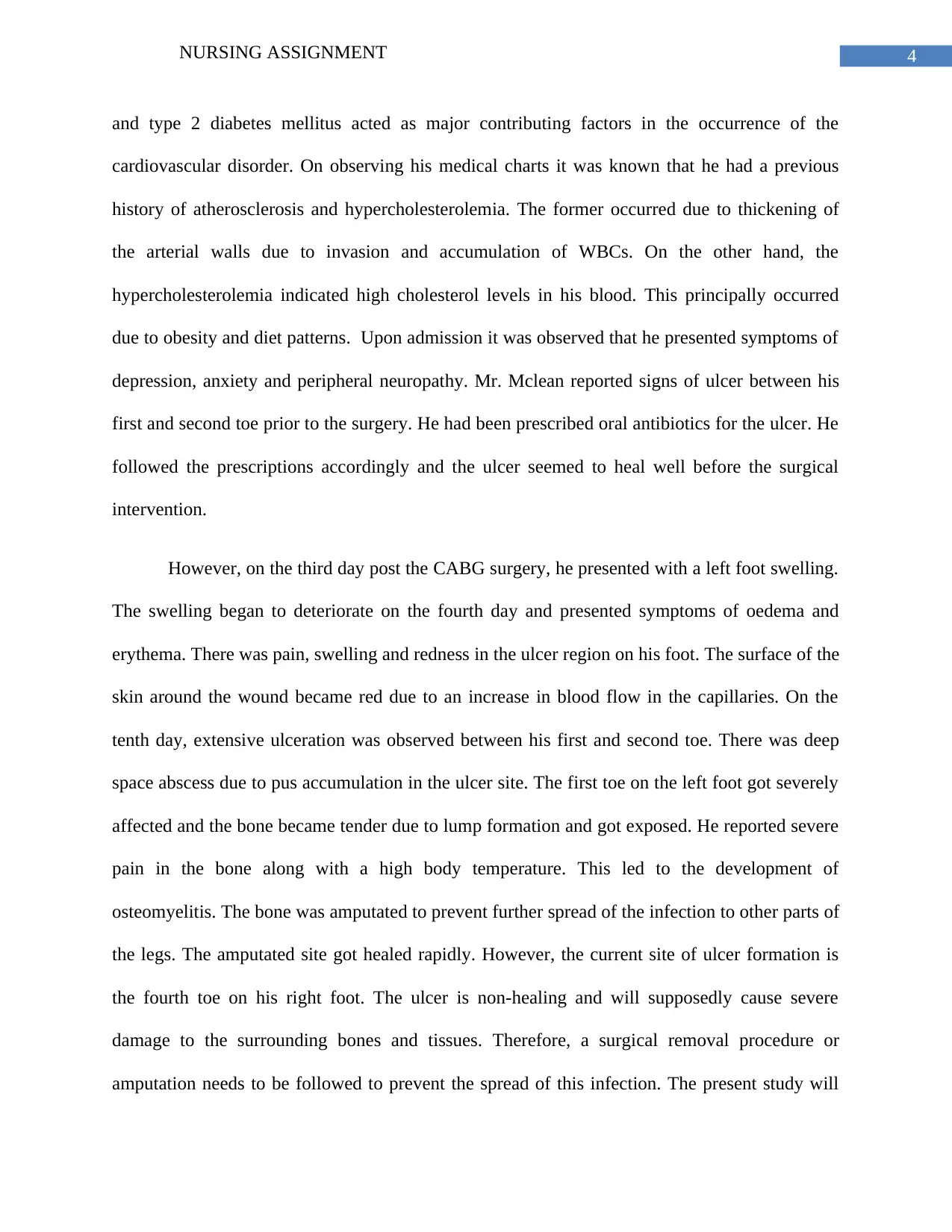
Wound management
The management of diabetic foot ulcer involves development of a systematic plan that
helps in preventing the spread of the wound. The various aspects of the wound management plan
are:
has a history of peripheral neuropathy. This led to lack of sensation in both feet. It also put him
at risk of developing ulcers (Waaijman et al. 2014, p. 1703). Loss of sensation prevented him
from detecting any trauma or injury to the legs.
Depression- Depression directly influences the immune and endocrine system. In
addition, it also leads to the formation of unhealthy habits, poor sleep patterns, sedentary
lifestyle, inadequate nutrition and substance abuse (Iversen et al. 2015, p. 22). The prevalence of
depressive symptoms adversely affected his health and wound healing.
Smoking- It creates detrimental effects on wound healing process. Smoking has been
associated with insulin resistance, which in turn increases blood sugar levels. This increased the
likelihood of getting affected with diabetic ulcer and may inhibit the healing process.
The management plan would include:
Removal of non-viable tissues (debridement).
Awareness on exposed capsule or tendon.
Management of exudates (appropriate dressing).
Management of bacterial burden (antimicrobial agents) (Lavery et al. 2016, p. 115).
Protection of granulation or epithelial tissue (non-adherent dressings).
Rehydration of wound bed (hydrogels).
Wound management
The management of diabetic foot ulcer involves development of a systematic plan that
helps in preventing the spread of the wound. The various aspects of the wound management plan
are:
11NURSING ASSIGNMENT
Assessing the patient and the challenges posed by the environment and the system.
Identifying the risk factors that may affect wound healing and skin integrity.
Setting goals for preventing wound deterioration.
Selecting a team based on the specific needs of the patient.
Ensuring meaningful communication among team members.
Ensuring sustainable care plan implementation.
Ensuring that the goals are met.
Reassessing the condition if the goals are not met
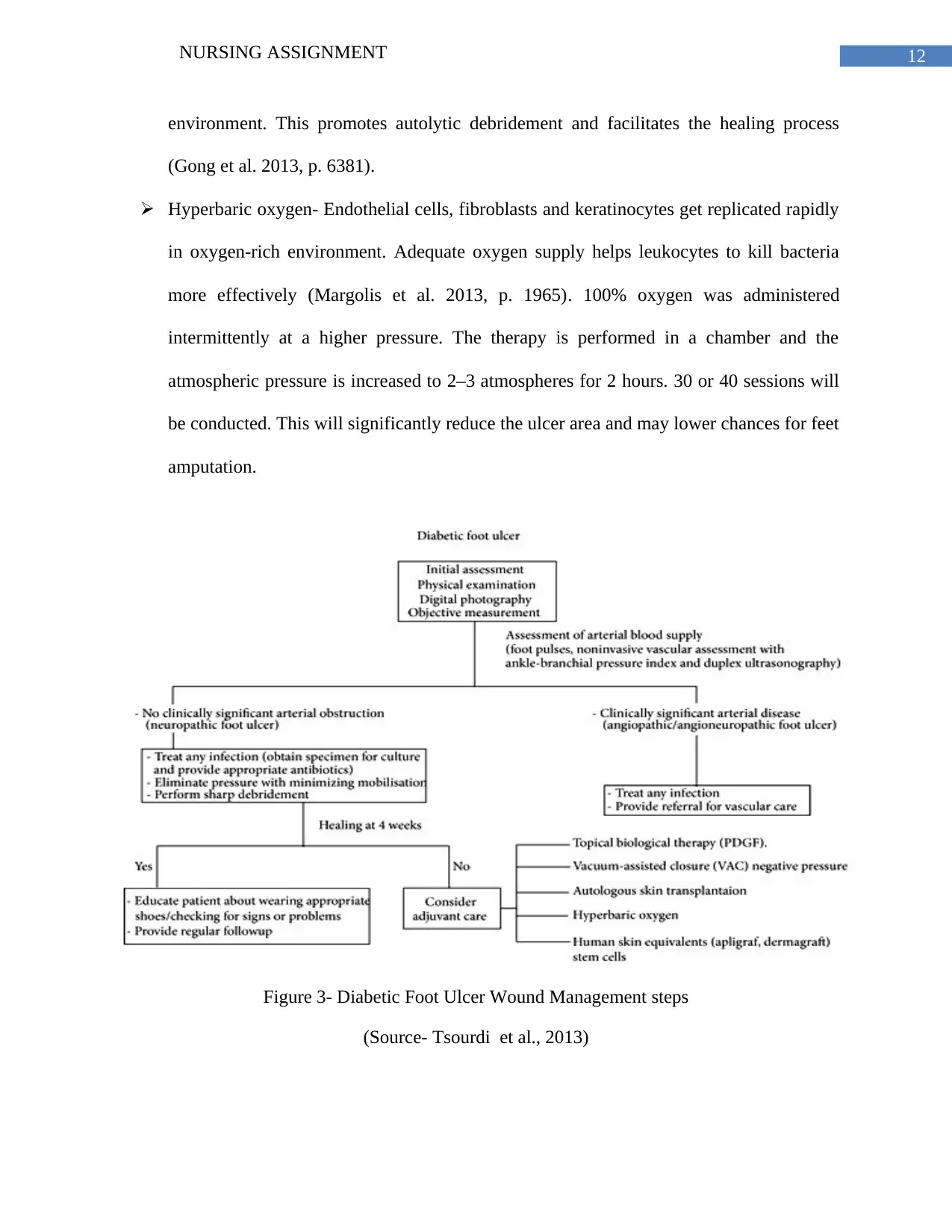
Mclean’s condition is considered chronic since the ulcer in his right foot is causing damage to
the bones and tissues. The current wound management plan includes:
Debridement- Ulcers generally heal faster when the wound is kept clean. Devitalized
necrotic tissues prevent cell migration and predispose it to infection. A sharp scalpel is
used to excise the unwanted tissues including eschar (sharp debridement) and callus
(Elraiyah et al. 2016, p. 39S). Care is taken to protect the healthy tissues that are pink or
deep red in colour (Braun et al. 2014, p. 270). The tip of the scalpel is pointed at an angle
of 45° and used to remove all non-viable tissues until the healthy bleeding ulcer bed has
been produced.
Dressings- Ulcers are often found to be less complicated and get healed rapidly in a moist
environment. Dressing materials that include saline-moistened gauze dressings and
moisture retaining dressings, such as hydrogels and hydrofibres are used to remove
excess exudates and toxic substances from the wound site (Moura et al. 2013, p. 7098).
These dressings are free from contaminants and allow effective gaseous exchange.
Aquacel Ag is used for this purpose. It forms a cohesive gel and maintains a moist
Assessing the patient and the challenges posed by the environment and the system.
Identifying the risk factors that may affect wound healing and skin integrity.
Setting goals for preventing wound deterioration.
Selecting a team based on the specific needs of the patient.
Ensuring meaningful communication among team members.
Ensuring sustainable care plan implementation.
Ensuring that the goals are met.
Reassessing the condition if the goals are not met
Mclean’s condition is considered chronic since the ulcer in his right foot is causing damage to
the bones and tissues. The current wound management plan includes:
Debridement- Ulcers generally heal faster when the wound is kept clean. Devitalized
necrotic tissues prevent cell migration and predispose it to infection. A sharp scalpel is
used to excise the unwanted tissues including eschar (sharp debridement) and callus
(Elraiyah et al. 2016, p. 39S). Care is taken to protect the healthy tissues that are pink or
deep red in colour (Braun et al. 2014, p. 270). The tip of the scalpel is pointed at an angle
of 45° and used to remove all non-viable tissues until the healthy bleeding ulcer bed has
been produced.
Dressings- Ulcers are often found to be less complicated and get healed rapidly in a moist
environment. Dressing materials that include saline-moistened gauze dressings and
moisture retaining dressings, such as hydrogels and hydrofibres are used to remove
excess exudates and toxic substances from the wound site (Moura et al. 2013, p. 7098).
These dressings are free from contaminants and allow effective gaseous exchange.
Aquacel Ag is used for this purpose. It forms a cohesive gel and maintains a moist
You're viewing a preview
Unlock full access by subscribing today!
12NURSING ASSIGNMENT
environment. This promotes autolytic debridement and facilitates the healing process
(Gong et al. 2013, p. 6381).
Hyperbaric oxygen- Endothelial cells, fibroblasts and keratinocytes get replicated rapidly
in oxygen-rich environment. Adequate oxygen supply helps leukocytes to kill bacteria
more effectively (Margolis et al. 2013, p. 1965). 100% oxygen was administered
intermittently at a higher pressure. The therapy is performed in a chamber and the
atmospheric pressure is increased to 2–3 atmospheres for 2 hours. 30 or 40 sessions will
be conducted. This will significantly reduce the ulcer area and may lower chances for feet
amputation.
Figure 3- Diabetic Foot Ulcer Wound Management steps
(Source- Tsourdi et al., 2013)
environment. This promotes autolytic debridement and facilitates the healing process
(Gong et al. 2013, p. 6381).
Hyperbaric oxygen- Endothelial cells, fibroblasts and keratinocytes get replicated rapidly
in oxygen-rich environment. Adequate oxygen supply helps leukocytes to kill bacteria
more effectively (Margolis et al. 2013, p. 1965). 100% oxygen was administered
intermittently at a higher pressure. The therapy is performed in a chamber and the
atmospheric pressure is increased to 2–3 atmospheres for 2 hours. 30 or 40 sessions will
be conducted. This will significantly reduce the ulcer area and may lower chances for feet
amputation.
Figure 3- Diabetic Foot Ulcer Wound Management steps
(Source- Tsourdi et al., 2013)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13NURSING ASSIGNMENT
Nursing interventions
Skin assessment- A complete skin assessment with special attention to the feet, legs and
toenails will help to identify any fissures or cracks that can lead to formation of ulcer in
the patient (Markova and Mostow 2012, p. 109). The colour, texture and odour will be
checked for early diagnosis of ulcer in other toes.
Footwear assessment- Orthotic and footwear assessments form key components of patient
assessment. Ill-fitting footwear leads to ulcers and amputations. It will be ensured that
Mclean’s footwear matches his activity and functional level. Steps will be taken to ensure
that his footwear is large enough to prevent toe pressure, has proper cushioning to absorb
shocks, limits overpronation (Bus & Netten 2016, p. 197). The shoes should be checked
for presence of foreign objects inside them.
Smoking- Every possible effort will be taken to encourage Mclean to stop smoking.
Smoking increases wound risks by compromising blood flow and delaying wound
healing. Appropriate referrals will be considered to help him get enrolled to smoking
cessation programs.
Education on nutrition and glycemic level- It has been established by evidences that
hyperglycemia leads to delay in wound healing process and compromises phagocytosis
and chemotaxis (Armstrong et al. 2014, p. 1072). Glycemic control and nutritional status
will be assessed to evaluate their impact on the feet. The patient will be made to undergo
a HbA1c test that will show the glucose levels for the past 3 months. His food patterns
will be closely monitored to control the amount to excess sugar, fats and carbohydrate in
the diet. He will be counselled by a registered dietician. An HbA1c level of <7% should
be maintained.
Nursing interventions
Skin assessment- A complete skin assessment with special attention to the feet, legs and
toenails will help to identify any fissures or cracks that can lead to formation of ulcer in
the patient (Markova and Mostow 2012, p. 109). The colour, texture and odour will be
checked for early diagnosis of ulcer in other toes.
Footwear assessment- Orthotic and footwear assessments form key components of patient
assessment. Ill-fitting footwear leads to ulcers and amputations. It will be ensured that
Mclean’s footwear matches his activity and functional level. Steps will be taken to ensure
that his footwear is large enough to prevent toe pressure, has proper cushioning to absorb
shocks, limits overpronation (Bus & Netten 2016, p. 197). The shoes should be checked
for presence of foreign objects inside them.
Smoking- Every possible effort will be taken to encourage Mclean to stop smoking.
Smoking increases wound risks by compromising blood flow and delaying wound
healing. Appropriate referrals will be considered to help him get enrolled to smoking
cessation programs.
Education on nutrition and glycemic level- It has been established by evidences that
hyperglycemia leads to delay in wound healing process and compromises phagocytosis
and chemotaxis (Armstrong et al. 2014, p. 1072). Glycemic control and nutritional status
will be assessed to evaluate their impact on the feet. The patient will be made to undergo
a HbA1c test that will show the glucose levels for the past 3 months. His food patterns
will be closely monitored to control the amount to excess sugar, fats and carbohydrate in
the diet. He will be counselled by a registered dietician. An HbA1c level of <7% should
be maintained.
14NURSING ASSIGNMENT
Pain control- Anticonvulsants will be given to control the neuropathic pain.
Psychological factor- His depressive symptoms will be managed by administering
atypical antipsychotics such as clozapine and risperidone.
Liaising with health professionals- A close collaboration of several healthcare
practitioners and specialists are need to treat patients with diabetic foot ulcer (Bakker,
Apelqvist & Schaper 2012, p. 229). A multidisciplinary team is caring for Mclean. Future
interventions will include effective communication and transfer of information among the
concerned healthcare staff to closely monitor his health status and immediately report
events of deterioration in his condition.
Conclusion
Thus, it can be concluded that diabetic foot ulcer is a common complication of high blood
glucose levels. Nurses and other health care providers are actively involved in early detection
and prevention such complications. Effective nursing can improve his health by taking
appropriate foot care assessments to prevent injuries, cleaning the injured wound tissue and
providing a moist environment to facilitate easy wound healing.
He will be advised to make lifestyle and nutritional changes. The barriers that can delay
wound healing process will be evaluated. Although his wound has aggravated, input from several
healthcare practitioners will help in timely healing of the wound.
Pain control- Anticonvulsants will be given to control the neuropathic pain.
Psychological factor- His depressive symptoms will be managed by administering
atypical antipsychotics such as clozapine and risperidone.
Liaising with health professionals- A close collaboration of several healthcare
practitioners and specialists are need to treat patients with diabetic foot ulcer (Bakker,
Apelqvist & Schaper 2012, p. 229). A multidisciplinary team is caring for Mclean. Future
interventions will include effective communication and transfer of information among the
concerned healthcare staff to closely monitor his health status and immediately report
events of deterioration in his condition.
Conclusion
Thus, it can be concluded that diabetic foot ulcer is a common complication of high blood
glucose levels. Nurses and other health care providers are actively involved in early detection
and prevention such complications. Effective nursing can improve his health by taking
appropriate foot care assessments to prevent injuries, cleaning the injured wound tissue and
providing a moist environment to facilitate easy wound healing.
He will be advised to make lifestyle and nutritional changes. The barriers that can delay
wound healing process will be evaluated. Although his wound has aggravated, input from several
healthcare practitioners will help in timely healing of the wound.
You're viewing a preview
Unlock full access by subscribing today!
15NURSING ASSIGNMENT
References
Alavi, A, Sibbald, RG, Mayer, D, Goodman, L, Botros, M, Armstrong, DG, Woo, K, Boeni, T,
Ayello, EA & Kirsner, RS 2014, ‘Diabetic foot ulcers: Part I. Pathophysiology and
prevention’, Journal of the American Academy of Dermatology, vol.70, no. 1, pp.1-e1.
Alavi, A, Sibbald, RG, Mayer, D, Goodman, L, Botros, M, Armstrong, DG, Woo, K, Boeni, T,
Ayello, EA & Kirsner, RS 2014, ‘Diabetic foot ulcers: part II. Management’, Journal of the
American Academy of Dermatology, vol. 70, no. 1, pp.21-e1.
Armstrong, DG, Hanft, JR, Driver, VR, Smith, APS, Lazaro‐Martinez, JL, Reyzelman, AM,
Furst, GJ, Vayser, DJ, Cervantes, HL, Snyder, RJ & Moore, MF 2014, ‘Effect of oral nutritional
supplementation on wound healing in diabetic foot ulcers: a prospective randomized controlled
trial’, Diabetic Medicine, vol. 31, no. 9, pp.1069-1077.
Bakker, K, Apelqvist, J & Schaper, NC 2012, ‘Practical guidelines on the management and
prevention of the diabetic foot 2011’, Diabetes/metabolism research and reviews, vol. 28, no.
S1, pp.225-231.
Braun, LR, Fisk, WA, Lev-Tov, H, Kirsner, RS & Isseroff, RR 2014, ‘Diabetic foot ulcer: an
evidence-based treatment update’, American journal of clinical dermatology, vol. 15, no. 3,
pp.267-281.
Bus, SA & Netten, JJ 2016, ‘A shift in priority in diabetic foot care and research: 75% of foot
ulcers are preventable’, Diabetes/metabolism research and reviews, vol. 32, no. S1, pp.195-200.
References
Alavi, A, Sibbald, RG, Mayer, D, Goodman, L, Botros, M, Armstrong, DG, Woo, K, Boeni, T,
Ayello, EA & Kirsner, RS 2014, ‘Diabetic foot ulcers: Part I. Pathophysiology and
prevention’, Journal of the American Academy of Dermatology, vol.70, no. 1, pp.1-e1.
Alavi, A, Sibbald, RG, Mayer, D, Goodman, L, Botros, M, Armstrong, DG, Woo, K, Boeni, T,
Ayello, EA & Kirsner, RS 2014, ‘Diabetic foot ulcers: part II. Management’, Journal of the
American Academy of Dermatology, vol. 70, no. 1, pp.21-e1.
Armstrong, DG, Hanft, JR, Driver, VR, Smith, APS, Lazaro‐Martinez, JL, Reyzelman, AM,
Furst, GJ, Vayser, DJ, Cervantes, HL, Snyder, RJ & Moore, MF 2014, ‘Effect of oral nutritional
supplementation on wound healing in diabetic foot ulcers: a prospective randomized controlled
trial’, Diabetic Medicine, vol. 31, no. 9, pp.1069-1077.
Bakker, K, Apelqvist, J & Schaper, NC 2012, ‘Practical guidelines on the management and
prevention of the diabetic foot 2011’, Diabetes/metabolism research and reviews, vol. 28, no.
S1, pp.225-231.
Braun, LR, Fisk, WA, Lev-Tov, H, Kirsner, RS & Isseroff, RR 2014, ‘Diabetic foot ulcer: an
evidence-based treatment update’, American journal of clinical dermatology, vol. 15, no. 3,
pp.267-281.
Bus, SA & Netten, JJ 2016, ‘A shift in priority in diabetic foot care and research: 75% of foot
ulcers are preventable’, Diabetes/metabolism research and reviews, vol. 32, no. S1, pp.195-200.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
16NURSING ASSIGNMENT
Darby, IA, Laverdet, B, Bonté, F & Desmoulière, A 2014, ‘Fibroblasts and myofibroblasts in
wound healing’, Clinical, cosmetic and investigational dermatology, vol. 7, p.301.
Deribe, B, Woldemichael, K & Nemera, G 2014, ‘Prevalence and factors influencing diabetic
foot ulcer among diabetic patients attending Arbaminch Hospital, South Ethiopia’, J Diabetes
Metab, vol. 5, no. 1, pp.1-7.
Douaiher, J, Succar, J, Lancerotto, L, Gurish, MF, Orgill, DP, Hamilton, MJ, Krilis, SA &
Stevens, RL 2014, ‘Development of mast cells and importance of their tryptase and chymase
serine proteases in inflammation and wound healing’, Advances in immunology, vol. 122, p.211.
Dubský, M, Jirkovská, A, Bem, R, Fejfarová, V, Skibová, J, Schaper, NC & Lipsky, BA 2013,
‘Risk factors for recurrence of diabetic foot ulcers: prospective follow‐up analysis in the
Eurodiale subgroup’, International wound journal, vol. 10, no. 5, pp.555-561.
Elraiyah, T, Domecq, J.P, Prutsky, G, Tsapas, A, Nabhan, M, Frykberg, R.G, Hasan, R, Firwana,
B, Prokop, LJ & Murad, MH 2016, ‘A systematic review and meta-analysis of débridement
methods for chronic diabetic foot ulcers’, Journal of vascular surgery, vol. 63, no. 2, pp.37S-
45S.
Gong, C, Wu, Q, Wang, Y, Zhang, D, Luo, F, Zhao, X, Wei, Y & Qian, Z 2013, ‘A
biodegradable hydrogel system containing curcumin encapsulated in micelles for cutaneous
wound healing’, Biomaterials, vol. 34, no. 27, pp.6377-6387.
Greaves, NS, Ashcroft, KJ, Baguneid, M & Bayat, A 2013, ‘Current understanding of molecular
and cellular mechanisms in fibroplasia and angiogenesis during acute wound healing’, Journal
of dermatological science', vol. 72, no. 3, pp.206-217.
Darby, IA, Laverdet, B, Bonté, F & Desmoulière, A 2014, ‘Fibroblasts and myofibroblasts in
wound healing’, Clinical, cosmetic and investigational dermatology, vol. 7, p.301.
Deribe, B, Woldemichael, K & Nemera, G 2014, ‘Prevalence and factors influencing diabetic
foot ulcer among diabetic patients attending Arbaminch Hospital, South Ethiopia’, J Diabetes
Metab, vol. 5, no. 1, pp.1-7.
Douaiher, J, Succar, J, Lancerotto, L, Gurish, MF, Orgill, DP, Hamilton, MJ, Krilis, SA &
Stevens, RL 2014, ‘Development of mast cells and importance of their tryptase and chymase
serine proteases in inflammation and wound healing’, Advances in immunology, vol. 122, p.211.
Dubský, M, Jirkovská, A, Bem, R, Fejfarová, V, Skibová, J, Schaper, NC & Lipsky, BA 2013,
‘Risk factors for recurrence of diabetic foot ulcers: prospective follow‐up analysis in the
Eurodiale subgroup’, International wound journal, vol. 10, no. 5, pp.555-561.
Elraiyah, T, Domecq, J.P, Prutsky, G, Tsapas, A, Nabhan, M, Frykberg, R.G, Hasan, R, Firwana,
B, Prokop, LJ & Murad, MH 2016, ‘A systematic review and meta-analysis of débridement
methods for chronic diabetic foot ulcers’, Journal of vascular surgery, vol. 63, no. 2, pp.37S-
45S.
Gong, C, Wu, Q, Wang, Y, Zhang, D, Luo, F, Zhao, X, Wei, Y & Qian, Z 2013, ‘A
biodegradable hydrogel system containing curcumin encapsulated in micelles for cutaneous
wound healing’, Biomaterials, vol. 34, no. 27, pp.6377-6387.
Greaves, NS, Ashcroft, KJ, Baguneid, M & Bayat, A 2013, ‘Current understanding of molecular
and cellular mechanisms in fibroplasia and angiogenesis during acute wound healing’, Journal
of dermatological science', vol. 72, no. 3, pp.206-217.
17NURSING ASSIGNMENT
Iversen, MM, Tell, GS, Espehaug, B, Midthjell, K, Graue, M, Rokne, B, Berge, LI & Østbye, T
2015, ‘Is depression a risk factor for diabetic foot ulcers? 11-years follow-up of the Nord-
Trøndelag Health Study (HUNT)’, Journal of diabetes and its complications, vol. 29, no. 1,
pp.20-25.
Lavery, L.A, Davis, KE, Berriman, SJ, Braun, L, Nichols, A, Kim, PJ, Margolis, D, Peters, EJ &
Attinger, C 2016, ‘WHS guidelines update: Diabetic foot ulcer treatment guidelines’, Wound
Repair and Regeneration, vol. 24, no. 1, pp.112-126.
Margolis, D.J, Gupta, J, Hoffstad, O, Papdopoulos, M, Glick, HA, Thom, SR & Mitra, N 2013,
‘Lack of effectiveness of hyperbaric oxygen therapy for the treatment of diabetic foot ulcer and
the prevention of amputation’, Diabetes care, vol. 36, no.7, pp.1961-1966.
Markova, A. and Mostow, E.N., 2012. US skin disease assessment: ulcer and wound
care. Dermatologic clinics, 30(1), pp.107-111.
Maxson, S, Lopez, EA, Yoo, D, Danilkovitch-Miagkova, A & LeRoux, MA 2012, ‘Concise
review: role of mesenchymal stem cells in wound repair’, Stem cells translational medicine, vol.
1, no. 2, pp.142-149.
Moura, LI, Dias, AM, Carvalho, E & de Sousa, HC 2013, ‘Recent advances on the development
of wound dressings for diabetic foot ulcer treatment—a review’, Acta biomaterialia, vol. 9, no.
7, pp.7093-7114.
Noor, S, Zubair, M & Ahmad, J 2015, ‘Diabetic foot ulcer—a review on pathophysiology,
classification and microbial etiology’, Diabetes & Metabolic Syndrome: Clinical Research &
Reviews, vol. 9, no. 3, pp.192-199.
Iversen, MM, Tell, GS, Espehaug, B, Midthjell, K, Graue, M, Rokne, B, Berge, LI & Østbye, T
2015, ‘Is depression a risk factor for diabetic foot ulcers? 11-years follow-up of the Nord-
Trøndelag Health Study (HUNT)’, Journal of diabetes and its complications, vol. 29, no. 1,
pp.20-25.
Lavery, L.A, Davis, KE, Berriman, SJ, Braun, L, Nichols, A, Kim, PJ, Margolis, D, Peters, EJ &
Attinger, C 2016, ‘WHS guidelines update: Diabetic foot ulcer treatment guidelines’, Wound
Repair and Regeneration, vol. 24, no. 1, pp.112-126.
Margolis, D.J, Gupta, J, Hoffstad, O, Papdopoulos, M, Glick, HA, Thom, SR & Mitra, N 2013,
‘Lack of effectiveness of hyperbaric oxygen therapy for the treatment of diabetic foot ulcer and
the prevention of amputation’, Diabetes care, vol. 36, no.7, pp.1961-1966.
Markova, A. and Mostow, E.N., 2012. US skin disease assessment: ulcer and wound
care. Dermatologic clinics, 30(1), pp.107-111.
Maxson, S, Lopez, EA, Yoo, D, Danilkovitch-Miagkova, A & LeRoux, MA 2012, ‘Concise
review: role of mesenchymal stem cells in wound repair’, Stem cells translational medicine, vol.
1, no. 2, pp.142-149.
Moura, LI, Dias, AM, Carvalho, E & de Sousa, HC 2013, ‘Recent advances on the development
of wound dressings for diabetic foot ulcer treatment—a review’, Acta biomaterialia, vol. 9, no.
7, pp.7093-7114.
Noor, S, Zubair, M & Ahmad, J 2015, ‘Diabetic foot ulcer—a review on pathophysiology,
classification and microbial etiology’, Diabetes & Metabolic Syndrome: Clinical Research &
Reviews, vol. 9, no. 3, pp.192-199.
You're viewing a preview
Unlock full access by subscribing today!
18NURSING ASSIGNMENT
Pickwell, K, Siersma, V, Kars, M, Apelqvist, J, Bakker, K, Edmonds, M, Holstein, P, Jirkovská,
A, Jude, E, Mauricio, D & Piaggesi, A 2015, ‘Predictors of lower-extremity amputation in
patients with an infected diabetic foot ulcer’, Diabetes Care, vol. 38, no. 5, pp.852-857.
Pilonidal.org (2017). [online] Pilonidal.org. Available at:
https://www.pilonidal.org/wp-content/uploads/2016/02/stages_of_wound_healing.png [Accessed
30 Oct. 2017].
Rice, JB, Desai, U, Cummings, AKG, Birnbaum, HG, Skornicki, M & Parsons, NB 2014,
‘Burden of diabetic foot ulcers for medicare and private insurers’, Diabetes care, vol. 37, no. 3,
pp.651-658.
Telfer, S, Erdemir, A, Woodburn, J & Cavanagh, PR 2014, ‘What has finite element analysis
taught us about diabetic foot disease and its management? A systematic review’, PloS one, vol.
9, no. 10, p.e109994.
Thenurseszone.com (2017). [online] Thenurseszone.com. Available at:
http://thenurseszone.com/wp-content/uploads/2016/05/diabetic-foot.jpg [Accessed 30 Oct.
2017].
Tsourdi, E., Barthel, A., Rietzsch, H., Reichel, A. and Bornstein, S.R., 2013. Current aspects in
the pathophysiology and treatment of chronic wounds in diabetes mellitus. BioMed research
international, 2013.
Waaijman, R, de Haart, M, Arts, ML, Wever, D, Verlouw, AJ, Nollet, F & Bus, SA 2014, ‘Risk
factors for plantar foot ulcer recurrence in neuropathic diabetic patients’, Diabetes care, vol. 37,
no. 6, pp.1697-1705.
Pickwell, K, Siersma, V, Kars, M, Apelqvist, J, Bakker, K, Edmonds, M, Holstein, P, Jirkovská,
A, Jude, E, Mauricio, D & Piaggesi, A 2015, ‘Predictors of lower-extremity amputation in
patients with an infected diabetic foot ulcer’, Diabetes Care, vol. 38, no. 5, pp.852-857.
Pilonidal.org (2017). [online] Pilonidal.org. Available at:
https://www.pilonidal.org/wp-content/uploads/2016/02/stages_of_wound_healing.png [Accessed
30 Oct. 2017].
Rice, JB, Desai, U, Cummings, AKG, Birnbaum, HG, Skornicki, M & Parsons, NB 2014,
‘Burden of diabetic foot ulcers for medicare and private insurers’, Diabetes care, vol. 37, no. 3,
pp.651-658.
Telfer, S, Erdemir, A, Woodburn, J & Cavanagh, PR 2014, ‘What has finite element analysis
taught us about diabetic foot disease and its management? A systematic review’, PloS one, vol.
9, no. 10, p.e109994.
Thenurseszone.com (2017). [online] Thenurseszone.com. Available at:
http://thenurseszone.com/wp-content/uploads/2016/05/diabetic-foot.jpg [Accessed 30 Oct.
2017].
Tsourdi, E., Barthel, A., Rietzsch, H., Reichel, A. and Bornstein, S.R., 2013. Current aspects in
the pathophysiology and treatment of chronic wounds in diabetes mellitus. BioMed research
international, 2013.
Waaijman, R, de Haart, M, Arts, ML, Wever, D, Verlouw, AJ, Nollet, F & Bus, SA 2014, ‘Risk
factors for plantar foot ulcer recurrence in neuropathic diabetic patients’, Diabetes care, vol. 37,
no. 6, pp.1697-1705.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
19NURSING ASSIGNMENT
Yazdanpanah, L, Nasiri, M & Adarvishi, S 2015, ‘Literature review on the management of
diabetic foot ulcer’, World journal of diabetes, vol. 6, no. 1, p.37.
Yazdanpanah, L, Nasiri, M & Adarvishi, S 2015, ‘Literature review on the management of
diabetic foot ulcer’, World journal of diabetes, vol. 6, no. 1, p.37.
1 out of 20
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.




