Nursing Care Plan for Patient with Hyperglycemia: NURSING 5
VerifiedAdded on 2021/04/19
|7
|860
|129
Case Study
AI Summary
This nursing care plan addresses a patient with hyperglycemia, detailing assessment findings, diagnoses (including uncontrolled diabetes, dehydration, and hypertension), and interventions. The plan outlines both subjective and objective data, such as the patient's reported symptoms, blood glucose levels, urine output, and vital signs. Interventions include insulin administration, intravenous fluids, medication for hypertension, and monitoring of vital signs and blood glucose levels. The rationale behind each intervention is provided, referencing relevant medical literature. The plan aims to bring blood glucose levels within a normal range, correct dehydration, and manage hypertension, with specific evaluation criteria to assess the effectiveness of the interventions over a 24-48 hour period. The document concludes with a list of cited references.

Running head- NURSING
Care plan for patient with hyperglycemia
Name of the Student
Name of the University
Author Note
Care plan for patient with hyperglycemia
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1NURSING
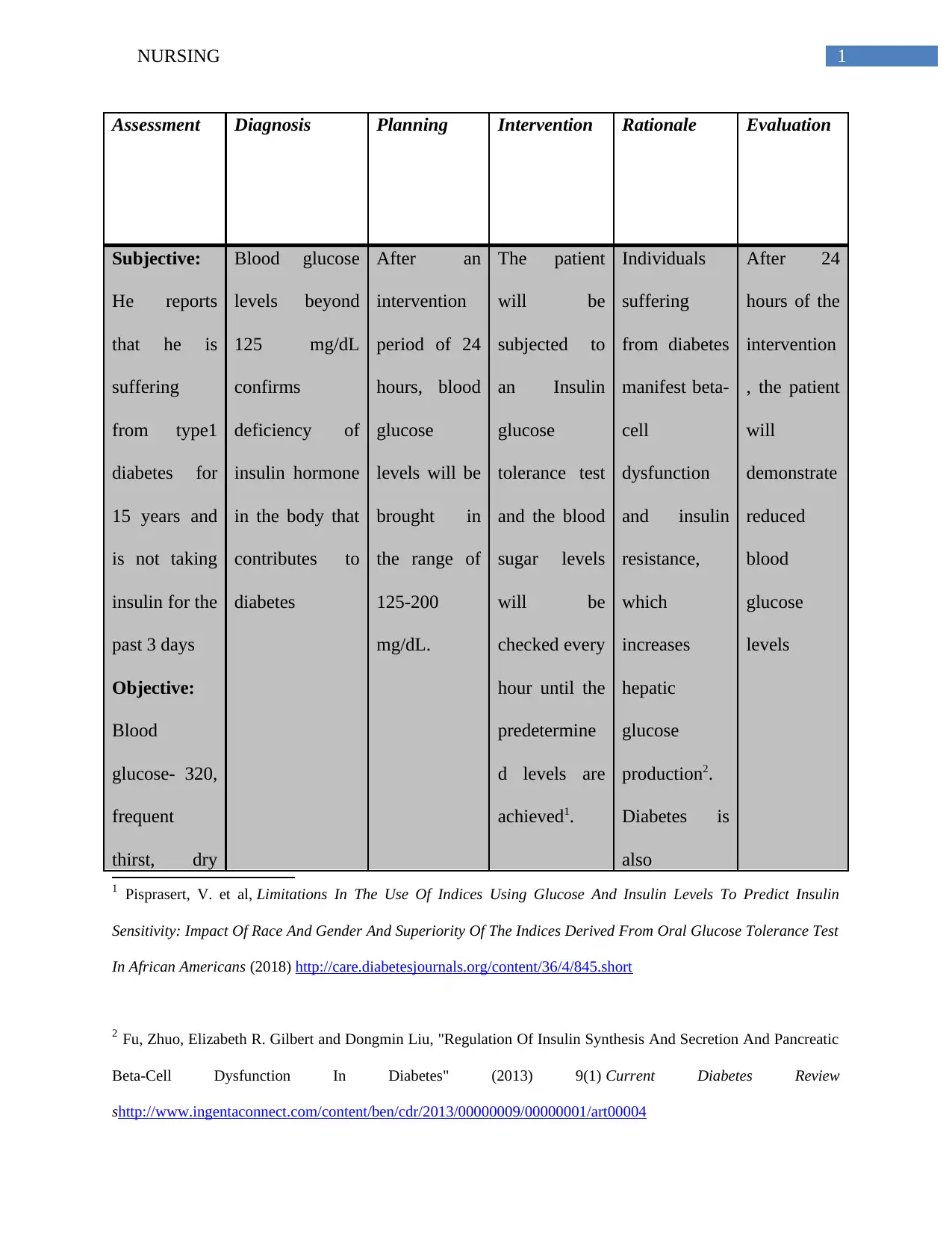
Assessment Diagnosis Planning Intervention Rationale Evaluation
Subjective:
He reports
that he is
suffering
from type1
diabetes for
15 years and
is not taking
insulin for the
past 3 days
Objective:
Blood
glucose- 320,
frequent
thirst, dry
Blood glucose
levels beyond
125 mg/dL
confirms
deficiency of
insulin hormone
in the body that
contributes to
diabetes
After an
intervention
period of 24
hours, blood
glucose
levels will be
brought in
the range of
125-200
mg/dL.
The patient
will be
subjected to
an Insulin
glucose
tolerance test
and the blood
sugar levels
will be
checked every
hour until the
predetermine
d levels are
achieved1.
Individuals
suffering
from diabetes
manifest beta-
cell
dysfunction
and insulin
resistance,
which
increases
hepatic
glucose
production2.
Diabetes is
also
After 24
hours of the
intervention
, the patient
will
demonstrate
reduced
blood
glucose
levels
1 Pisprasert, V. et al, Limitations In The Use Of Indices Using Glucose And Insulin Levels To Predict Insulin
Sensitivity: Impact Of Race And Gender And Superiority Of The Indices Derived From Oral Glucose Tolerance Test
In African Americans (2018) http://care.diabetesjournals.org/content/36/4/845.short
2 Fu, Zhuo, Elizabeth R. Gilbert and Dongmin Liu, "Regulation Of Insulin Synthesis And Secretion And Pancreatic
Beta-Cell Dysfunction In Diabetes" (2013) 9(1) Current Diabetes Review
shttp://www.ingentaconnect.com/content/ben/cdr/2013/00000009/00000001/art00004
Assessment Diagnosis Planning Intervention Rationale Evaluation
Subjective:
He reports
that he is
suffering
from type1
diabetes for
15 years and
is not taking
insulin for the
past 3 days
Objective:
Blood
glucose- 320,
frequent
thirst, dry
Blood glucose
levels beyond
125 mg/dL
confirms
deficiency of
insulin hormone
in the body that
contributes to
diabetes
After an
intervention
period of 24
hours, blood
glucose
levels will be
brought in
the range of
125-200
mg/dL.
The patient
will be
subjected to
an Insulin
glucose
tolerance test
and the blood
sugar levels
will be
checked every
hour until the
predetermine
d levels are
achieved1.
Individuals
suffering
from diabetes
manifest beta-
cell
dysfunction
and insulin
resistance,
which
increases
hepatic
glucose
production2.
Diabetes is
also
After 24
hours of the
intervention
, the patient
will
demonstrate
reduced
blood
glucose
levels
1 Pisprasert, V. et al, Limitations In The Use Of Indices Using Glucose And Insulin Levels To Predict Insulin
Sensitivity: Impact Of Race And Gender And Superiority Of The Indices Derived From Oral Glucose Tolerance Test
In African Americans (2018) http://care.diabetesjournals.org/content/36/4/845.short
2 Fu, Zhuo, Elizabeth R. Gilbert and Dongmin Liu, "Regulation Of Insulin Synthesis And Secretion And Pancreatic
Beta-Cell Dysfunction In Diabetes" (2013) 9(1) Current Diabetes Review
shttp://www.ingentaconnect.com/content/ben/cdr/2013/00000009/00000001/art00004
2NURSING
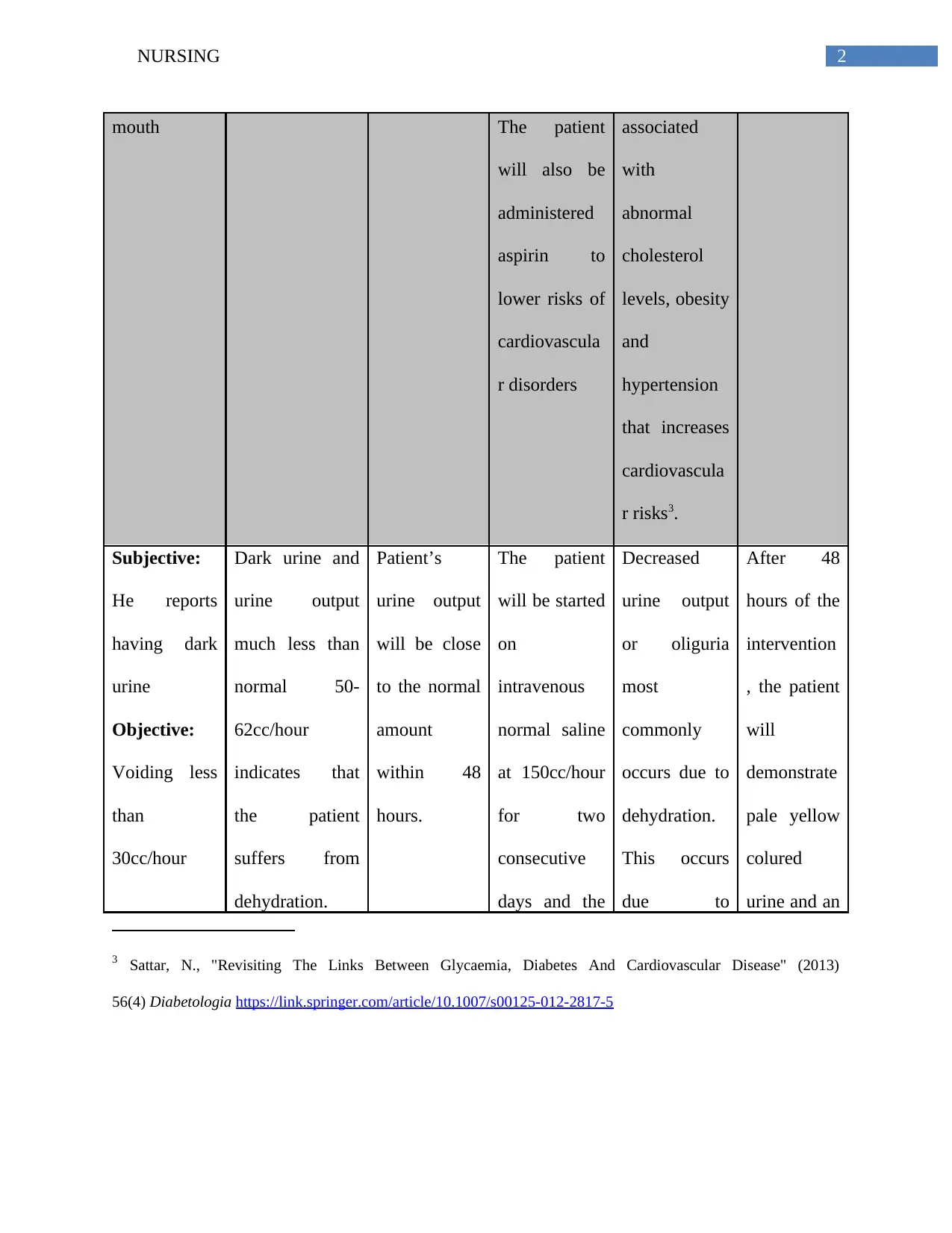
mouth The patient
will also be
administered
aspirin to
lower risks of
cardiovascula
r disorders
associated
with
abnormal
cholesterol
levels, obesity
and
hypertension
that increases
cardiovascula
r risks3.
Subjective:
He reports
having dark
urine
Objective:
Voiding less
than
30cc/hour
Dark urine and
urine output
much less than
normal 50-
62cc/hour
indicates that
the patient
suffers from
dehydration.
Patient’s
urine output
will be close
to the normal
amount
within 48
hours.
The patient
will be started
on
intravenous
normal saline
at 150cc/hour
for two
consecutive
days and the
Decreased
urine output
or oliguria
most
commonly
occurs due to
dehydration.
This occurs
due to
After 48
hours of the
intervention
, the patient
will
demonstrate
pale yellow
colured
urine and an
3 Sattar, N., "Revisiting The Links Between Glycaemia, Diabetes And Cardiovascular Disease" (2013)
56(4) Diabetologia https://link.springer.com/article/10.1007/s00125-012-2817-5
mouth The patient
will also be
administered
aspirin to
lower risks of
cardiovascula
r disorders
associated
with
abnormal
cholesterol
levels, obesity
and
hypertension
that increases
cardiovascula
r risks3.
Subjective:
He reports
having dark
urine
Objective:
Voiding less
than
30cc/hour
Dark urine and
urine output
much less than
normal 50-
62cc/hour
indicates that
the patient
suffers from
dehydration.
Patient’s
urine output
will be close
to the normal
amount
within 48
hours.
The patient
will be started
on
intravenous
normal saline
at 150cc/hour
for two
consecutive
days and the
Decreased
urine output
or oliguria
most
commonly
occurs due to
dehydration.
This occurs
due to
After 48
hours of the
intervention
, the patient
will
demonstrate
pale yellow
colured
urine and an
3 Sattar, N., "Revisiting The Links Between Glycaemia, Diabetes And Cardiovascular Disease" (2013)
56(4) Diabetologia https://link.springer.com/article/10.1007/s00125-012-2817-5
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3NURSING
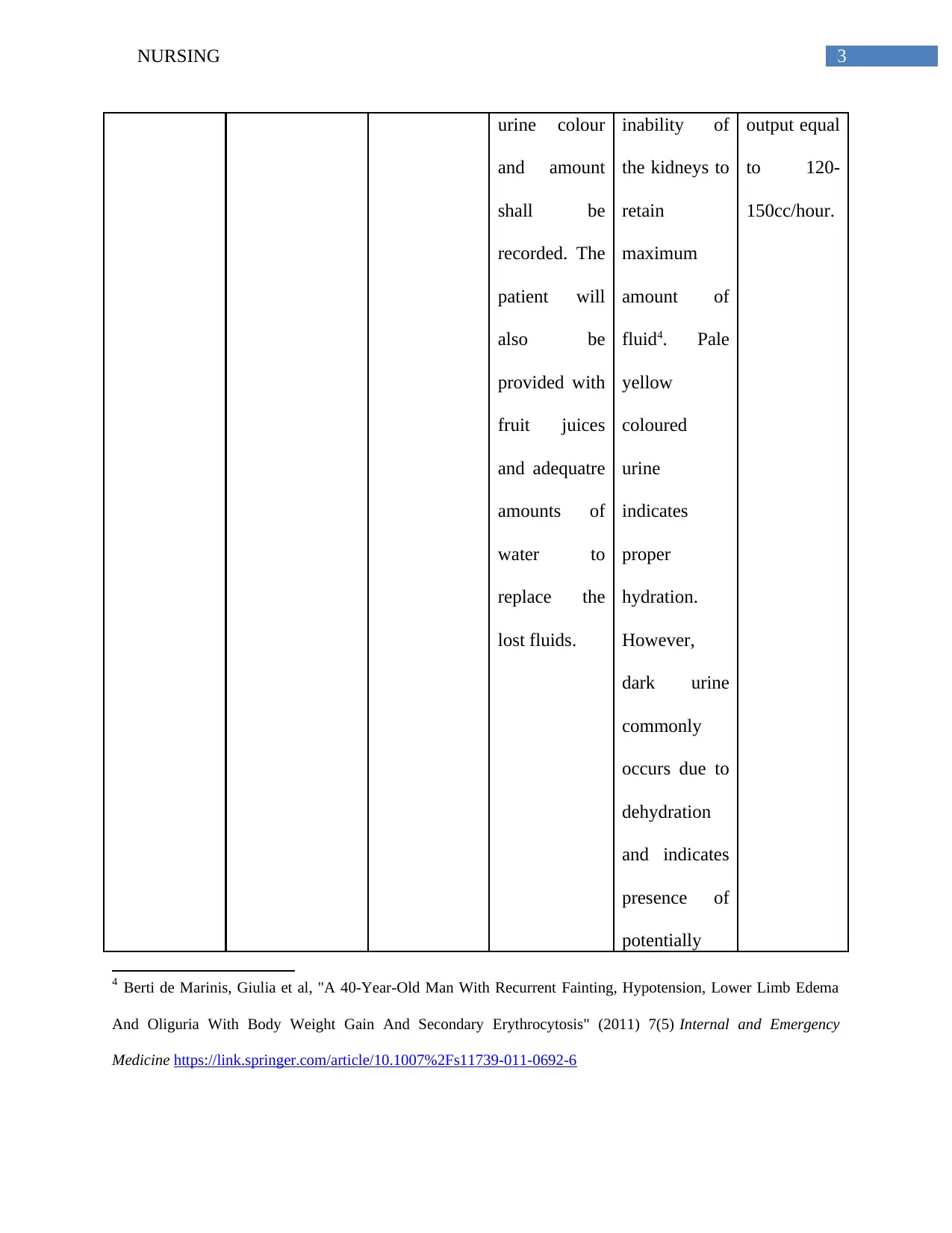
urine colour
and amount
shall be
recorded. The
patient will
also be
provided with
fruit juices
and adequatre
amounts of
water to
replace the
lost fluids.
inability of
the kidneys to
retain
maximum
amount of
fluid4. Pale
yellow
coloured
urine
indicates
proper
hydration.
However,
dark urine
commonly
occurs due to
dehydration
and indicates
presence of
potentially
output equal
to 120-
150cc/hour.
4 Berti de Marinis, Giulia et al, "A 40-Year-Old Man With Recurrent Fainting, Hypotension, Lower Limb Edema
And Oliguria With Body Weight Gain And Secondary Erythrocytosis" (2011) 7(5) Internal and Emergency
Medicine https://link.springer.com/article/10.1007%2Fs11739-011-0692-6
urine colour
and amount
shall be
recorded. The
patient will
also be
provided with
fruit juices
and adequatre
amounts of
water to
replace the
lost fluids.
inability of
the kidneys to
retain
maximum
amount of
fluid4. Pale
yellow
coloured
urine
indicates
proper
hydration.
However,
dark urine
commonly
occurs due to
dehydration
and indicates
presence of
potentially
output equal
to 120-
150cc/hour.
4 Berti de Marinis, Giulia et al, "A 40-Year-Old Man With Recurrent Fainting, Hypotension, Lower Limb Edema
And Oliguria With Body Weight Gain And Secondary Erythrocytosis" (2011) 7(5) Internal and Emergency
Medicine https://link.springer.com/article/10.1007%2Fs11739-011-0692-6
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4NURSING
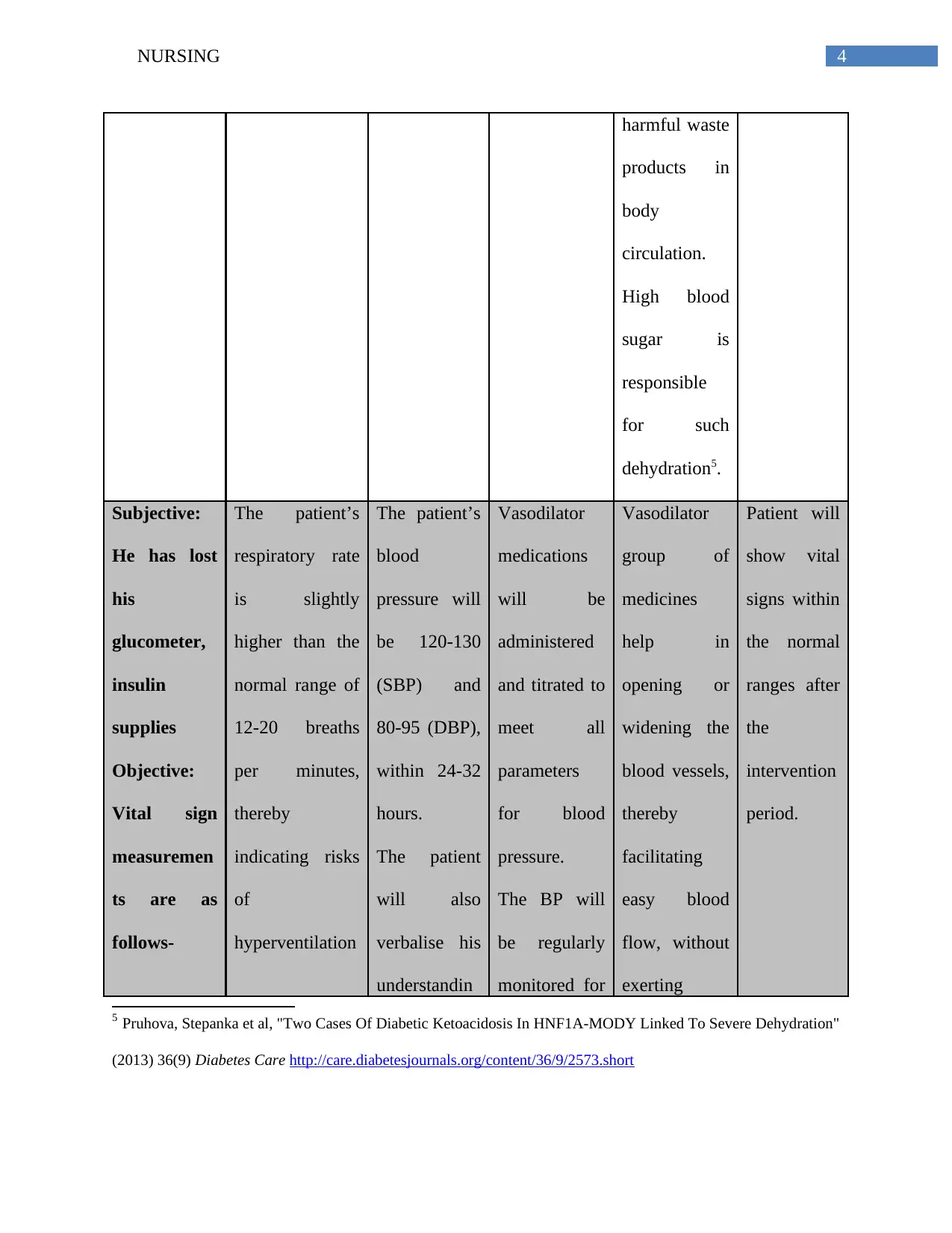
harmful waste
products in
body
circulation.
High blood
sugar is
responsible
for such
dehydration5.
Subjective:
He has lost
his
glucometer,
insulin
supplies
Objective:
Vital sign
measuremen
ts are as
follows-
The patient’s
respiratory rate
is slightly
higher than the
normal range of
12-20 breaths
per minutes,
thereby
indicating risks
of
hyperventilation
The patient’s
blood
pressure will
be 120-130
(SBP) and
80-95 (DBP),
within 24-32
hours.
The patient
will also
verbalise his
understandin
Vasodilator
medications
will be
administered
and titrated to
meet all
parameters
for blood
pressure.
The BP will
be regularly
monitored for
Vasodilator
group of
medicines
help in
opening or
widening the
blood vessels,
thereby
facilitating
easy blood
flow, without
exerting
Patient will
show vital
signs within
the normal
ranges after
the
intervention
period.
5 Pruhova, Stepanka et al, "Two Cases Of Diabetic Ketoacidosis In HNF1A-MODY Linked To Severe Dehydration"
(2013) 36(9) Diabetes Care http://care.diabetesjournals.org/content/36/9/2573.short
harmful waste
products in
body
circulation.
High blood
sugar is
responsible
for such
dehydration5.
Subjective:
He has lost
his
glucometer,
insulin
supplies
Objective:
Vital sign
measuremen
ts are as
follows-
The patient’s
respiratory rate
is slightly
higher than the
normal range of
12-20 breaths
per minutes,
thereby
indicating risks
of
hyperventilation
The patient’s
blood
pressure will
be 120-130
(SBP) and
80-95 (DBP),
within 24-32
hours.
The patient
will also
verbalise his
understandin
Vasodilator
medications
will be
administered
and titrated to
meet all
parameters
for blood
pressure.
The BP will
be regularly
monitored for
Vasodilator
group of
medicines
help in
opening or
widening the
blood vessels,
thereby
facilitating
easy blood
flow, without
exerting
Patient will
show vital
signs within
the normal
ranges after
the
intervention
period.
5 Pruhova, Stepanka et al, "Two Cases Of Diabetic Ketoacidosis In HNF1A-MODY Linked To Severe Dehydration"
(2013) 36(9) Diabetes Care http://care.diabetesjournals.org/content/36/9/2573.short
5NURSING
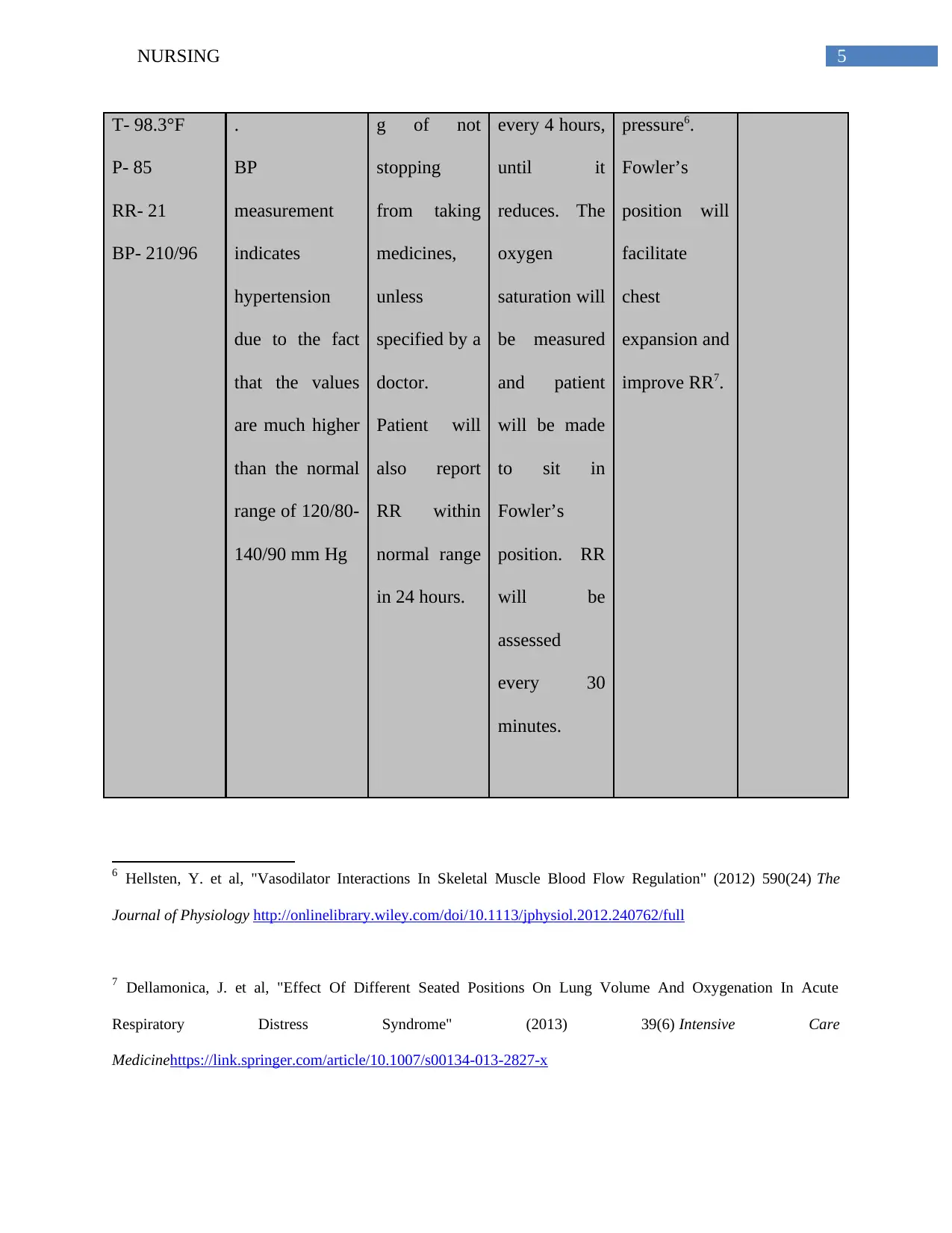
T- 98.3°F
P- 85
RR- 21
BP- 210/96
.
BP
measurement
indicates
hypertension
due to the fact
that the values
are much higher
than the normal
range of 120/80-
140/90 mm Hg
g of not
stopping
from taking
medicines,
unless
specified by a
doctor.
Patient will
also report
RR within
normal range
in 24 hours.
every 4 hours,
until it
reduces. The
oxygen
saturation will
be measured
and patient
will be made
to sit in
Fowler’s
position. RR
will be
assessed
every 30
minutes.
pressure6.
Fowler’s
position will
facilitate
chest
expansion and
improve RR7.
6 Hellsten, Y. et al, "Vasodilator Interactions In Skeletal Muscle Blood Flow Regulation" (2012) 590(24) The
Journal of Physiology http://onlinelibrary.wiley.com/doi/10.1113/jphysiol.2012.240762/full
7 Dellamonica, J. et al, "Effect Of Different Seated Positions On Lung Volume And Oxygenation In Acute
Respiratory Distress Syndrome" (2013) 39(6) Intensive Care
Medicinehttps://link.springer.com/article/10.1007/s00134-013-2827-x
T- 98.3°F
P- 85
RR- 21
BP- 210/96
.
BP
measurement
indicates
hypertension
due to the fact
that the values
are much higher
than the normal
range of 120/80-
140/90 mm Hg
g of not
stopping
from taking
medicines,
unless
specified by a
doctor.
Patient will
also report
RR within
normal range
in 24 hours.
every 4 hours,
until it
reduces. The
oxygen
saturation will
be measured
and patient
will be made
to sit in
Fowler’s
position. RR
will be
assessed
every 30
minutes.
pressure6.
Fowler’s
position will
facilitate
chest
expansion and
improve RR7.
6 Hellsten, Y. et al, "Vasodilator Interactions In Skeletal Muscle Blood Flow Regulation" (2012) 590(24) The
Journal of Physiology http://onlinelibrary.wiley.com/doi/10.1113/jphysiol.2012.240762/full
7 Dellamonica, J. et al, "Effect Of Different Seated Positions On Lung Volume And Oxygenation In Acute
Respiratory Distress Syndrome" (2013) 39(6) Intensive Care
Medicinehttps://link.springer.com/article/10.1007/s00134-013-2827-x
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

6NURSING
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





