Nursing Decision Making: Analyzing Patient Care Through Case Studies
VerifiedAdded on 2023/06/18
|9
|2234
|189
Case Study
AI Summary
This assignment presents a series of case studies focusing on nursing decision-making in various patient scenarios. The cases include a 28-year-old female with chest pain and palpitation, a 63-year-old male with cyanosis, a 46-year-old male with hypoglycemia, and a 72-year-old male with suspected autonomic dysfunction. Each case provides a diagnosis, plan of care, assessment using the ABCDE approach, and discharge planning considerations. The analysis covers symptoms, causes, and pathophysiology of each condition, emphasizing the importance of accurate assessment, appropriate interventions, and patient education for effective management. The document highlights the critical role of nurses in making informed decisions to optimize patient outcomes and safety. Desklib offers additional solved assignments and resources for students.
THE SCIENCE OF
NURSING DECISION
MAKING
NURSING DECISION
MAKING
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
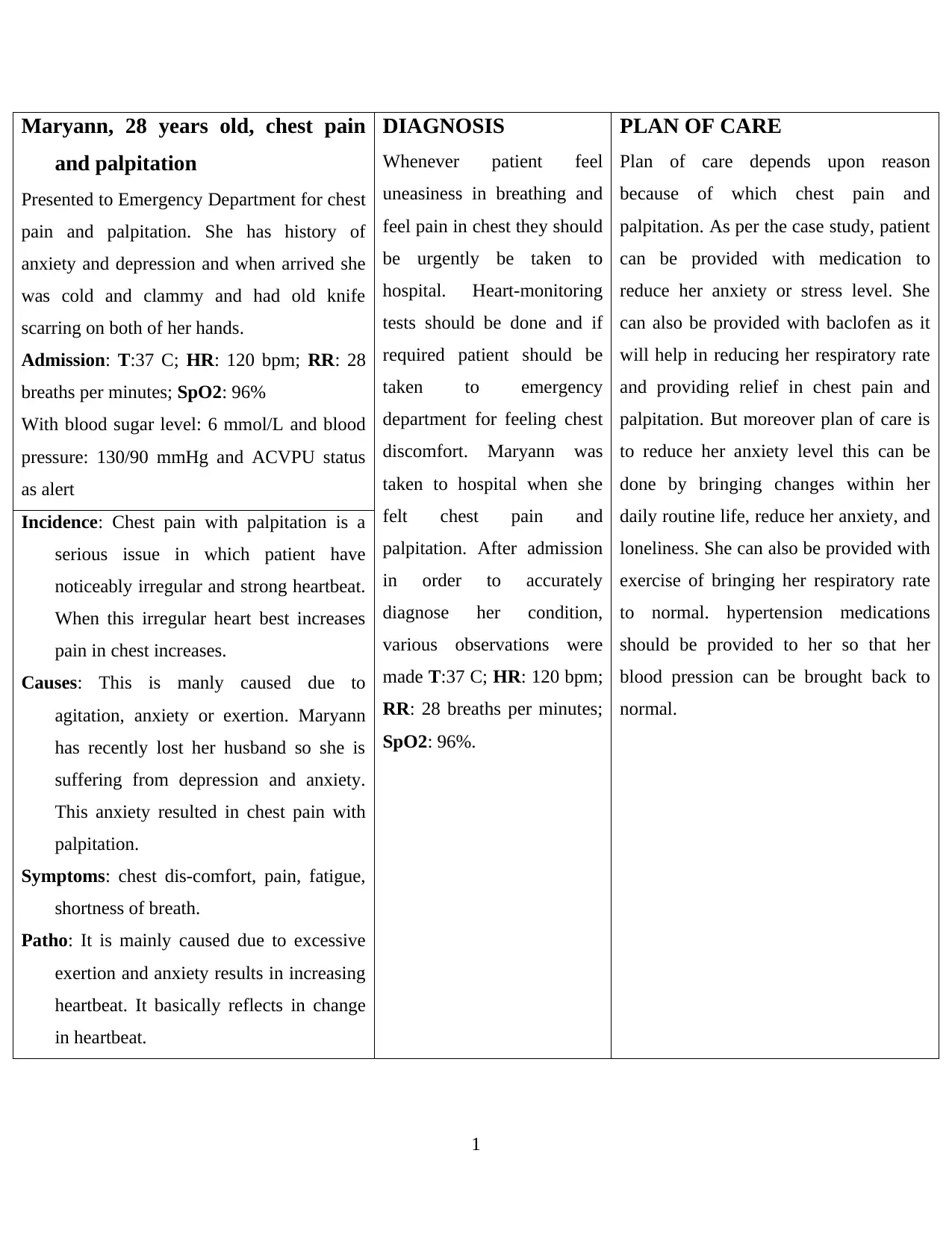
Maryann, 28 years old, chest pain
and palpitation
Presented to Emergency Department for chest
pain and palpitation. She has history of
anxiety and depression and when arrived she
was cold and clammy and had old knife
scarring on both of her hands.
Admission: T:37 C; HR: 120 bpm; RR: 28
breaths per minutes; SpO2: 96%
With blood sugar level: 6 mmol/L and blood
pressure: 130/90 mmHg and ACVPU status
as alert
DIAGNOSIS
Whenever patient feel
uneasiness in breathing and
feel pain in chest they should
be urgently be taken to
hospital. Heart-monitoring
tests should be done and if
required patient should be
taken to emergency
department for feeling chest
discomfort. Maryann was
taken to hospital when she
felt chest pain and
palpitation. After admission
in order to accurately
diagnose her condition,
various observations were
made T:37 C; HR: 120 bpm;
RR: 28 breaths per minutes;
SpO2: 96%.
PLAN OF CARE
Plan of care depends upon reason
because of which chest pain and
palpitation. As per the case study, patient
can be provided with medication to
reduce her anxiety or stress level. She
can also be provided with baclofen as it
will help in reducing her respiratory rate
and providing relief in chest pain and
palpitation. But moreover plan of care is
to reduce her anxiety level this can be
done by bringing changes within her
daily routine life, reduce her anxiety, and
loneliness. She can also be provided with
exercise of bringing her respiratory rate
to normal. hypertension medications
should be provided to her so that her
blood pression can be brought back to
normal.
Incidence: Chest pain with palpitation is a
serious issue in which patient have
noticeably irregular and strong heartbeat.
When this irregular heart best increases
pain in chest increases.
Causes: This is manly caused due to
agitation, anxiety or exertion. Maryann
has recently lost her husband so she is
suffering from depression and anxiety.
This anxiety resulted in chest pain with
palpitation.
Symptoms: chest dis-comfort, pain, fatigue,
shortness of breath.
Patho: It is mainly caused due to excessive
exertion and anxiety results in increasing
heartbeat. It basically reflects in change
in heartbeat.
1
and palpitation
Presented to Emergency Department for chest
pain and palpitation. She has history of
anxiety and depression and when arrived she
was cold and clammy and had old knife
scarring on both of her hands.
Admission: T:37 C; HR: 120 bpm; RR: 28
breaths per minutes; SpO2: 96%
With blood sugar level: 6 mmol/L and blood
pressure: 130/90 mmHg and ACVPU status
as alert
DIAGNOSIS
Whenever patient feel
uneasiness in breathing and
feel pain in chest they should
be urgently be taken to
hospital. Heart-monitoring
tests should be done and if
required patient should be
taken to emergency
department for feeling chest
discomfort. Maryann was
taken to hospital when she
felt chest pain and
palpitation. After admission
in order to accurately
diagnose her condition,
various observations were
made T:37 C; HR: 120 bpm;
RR: 28 breaths per minutes;
SpO2: 96%.
PLAN OF CARE
Plan of care depends upon reason
because of which chest pain and
palpitation. As per the case study, patient
can be provided with medication to
reduce her anxiety or stress level. She
can also be provided with baclofen as it
will help in reducing her respiratory rate
and providing relief in chest pain and
palpitation. But moreover plan of care is
to reduce her anxiety level this can be
done by bringing changes within her
daily routine life, reduce her anxiety, and
loneliness. She can also be provided with
exercise of bringing her respiratory rate
to normal. hypertension medications
should be provided to her so that her
blood pression can be brought back to
normal.
Incidence: Chest pain with palpitation is a
serious issue in which patient have
noticeably irregular and strong heartbeat.
When this irregular heart best increases
pain in chest increases.
Causes: This is manly caused due to
agitation, anxiety or exertion. Maryann
has recently lost her husband so she is
suffering from depression and anxiety.
This anxiety resulted in chest pain with
palpitation.
Symptoms: chest dis-comfort, pain, fatigue,
shortness of breath.
Patho: It is mainly caused due to excessive
exertion and anxiety results in increasing
heartbeat. It basically reflects in change
in heartbeat.
1

ASSESSMENT
ABCDE approach for assessment of current
condition of patient
A: Airway of patient was normal and there
was no obstruction
B: respiratory rate was high i.e., 28 breaths
per minutes but SpO2 level was normal i.e.,
96%
C: she was a bit cold but her heart rate was
normal i.e., 120 bpm
D: her ACVPU was at alert, has history of
depression and anxiety
E: full body examination was done and her
temperature was also normal 37 C
DISCHARGE PLANNING
Requirement of change in lifestyle,
meditation, reducing anxiety and
depression should be provided to patient
and her family members. Education
about psychological exercises important
to be carried should be given to patient
as well. Education about medications
that are required to be continued should
also be provided
2
ABCDE approach for assessment of current
condition of patient
A: Airway of patient was normal and there
was no obstruction
B: respiratory rate was high i.e., 28 breaths
per minutes but SpO2 level was normal i.e.,
96%
C: she was a bit cold but her heart rate was
normal i.e., 120 bpm
D: her ACVPU was at alert, has history of
depression and anxiety
E: full body examination was done and her
temperature was also normal 37 C
DISCHARGE PLANNING
Requirement of change in lifestyle,
meditation, reducing anxiety and
depression should be provided to patient
and her family members. Education
about psychological exercises important
to be carried should be given to patient
as well. Education about medications
that are required to be continued should
also be provided
2
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

Thomas, 63 years old, Cyanosis.
Mr Thomas Murphy was seen by
intermediate care team at his home due to
worsening breathing difficulties in past few
days. He was sitting on his arm chain with his
home oxygen turned on.
Admission: Wt: 76 kg; T: 37.5; HR: 105
bpm; RR: 36 breaths per minutes; SpO2:
86%
He was wheezing, using pursed lip breathing,
using accessory muscles when breathing and
also showed signs of cyanosis.
DIAGNOSIS
When diagnosis of Cyanosis
is done a combination of
physical test should be done
including X-ray and blood
test. When oxygen level is
below normal level then in
such case immediately
medication attention should
be provided. When bluish
discoloration of skin, lips,
fingers and toes and mucous
membranes is visible then in
such case health professional
should be consulted. When
this condition is diagnosed
then it should be identified
that what kind of Cyanosis is
patient suffer from. In
peripheral cyanosis there is
usually problem with
circulation of the blood in
the fingers and toe and then
it turns blue it can occur due
to exposure to cold and
becomes normal
immediately. But central
cyanosis is serious and can
damage heart and lungs.
PLAN OF CARE
Oxygenation for initial
stabilization with the help of breathing
machine and if serious case ventilators
might be required. Drug treatment to
patient is also given where Antibiotics
are prescribed to prevent infections and
for preventing patient from developing
further infection and as Mr Murphy is
already suffering from upper respiratory
infection so provision of drug therapy
will prevent him from worsening of
infection.Incidence: Mr Murphy was having breathing
issues and when by intermediate care
team approached, he had put on home
oxygen cylinder, and showed symptoms
of Cyanosis.
Causes: When saturated oxygen level
reduced to extremely low then in such
case many times bluish or purplish tinge
on skin starts forming which is known as
Cyanosis
Symptoms: Shortness of breath, gasping for
breath, skin discolouration and turned to
blue.
Patho: Bluish discoloration of the skin
occurs. When oxygen do not reach
haemoglobin in sufficient amount then in
such case as a result it starts affecting the
respiratory system.
3
Mr Thomas Murphy was seen by
intermediate care team at his home due to
worsening breathing difficulties in past few
days. He was sitting on his arm chain with his
home oxygen turned on.
Admission: Wt: 76 kg; T: 37.5; HR: 105
bpm; RR: 36 breaths per minutes; SpO2:
86%
He was wheezing, using pursed lip breathing,
using accessory muscles when breathing and
also showed signs of cyanosis.
DIAGNOSIS
When diagnosis of Cyanosis
is done a combination of
physical test should be done
including X-ray and blood
test. When oxygen level is
below normal level then in
such case immediately
medication attention should
be provided. When bluish
discoloration of skin, lips,
fingers and toes and mucous
membranes is visible then in
such case health professional
should be consulted. When
this condition is diagnosed
then it should be identified
that what kind of Cyanosis is
patient suffer from. In
peripheral cyanosis there is
usually problem with
circulation of the blood in
the fingers and toe and then
it turns blue it can occur due
to exposure to cold and
becomes normal
immediately. But central
cyanosis is serious and can
damage heart and lungs.
PLAN OF CARE
Oxygenation for initial
stabilization with the help of breathing
machine and if serious case ventilators
might be required. Drug treatment to
patient is also given where Antibiotics
are prescribed to prevent infections and
for preventing patient from developing
further infection and as Mr Murphy is
already suffering from upper respiratory
infection so provision of drug therapy
will prevent him from worsening of
infection.Incidence: Mr Murphy was having breathing
issues and when by intermediate care
team approached, he had put on home
oxygen cylinder, and showed symptoms
of Cyanosis.
Causes: When saturated oxygen level
reduced to extremely low then in such
case many times bluish or purplish tinge
on skin starts forming which is known as
Cyanosis
Symptoms: Shortness of breath, gasping for
breath, skin discolouration and turned to
blue.
Patho: Bluish discoloration of the skin
occurs. When oxygen do not reach
haemoglobin in sufficient amount then in
such case as a result it starts affecting the
respiratory system.
3
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
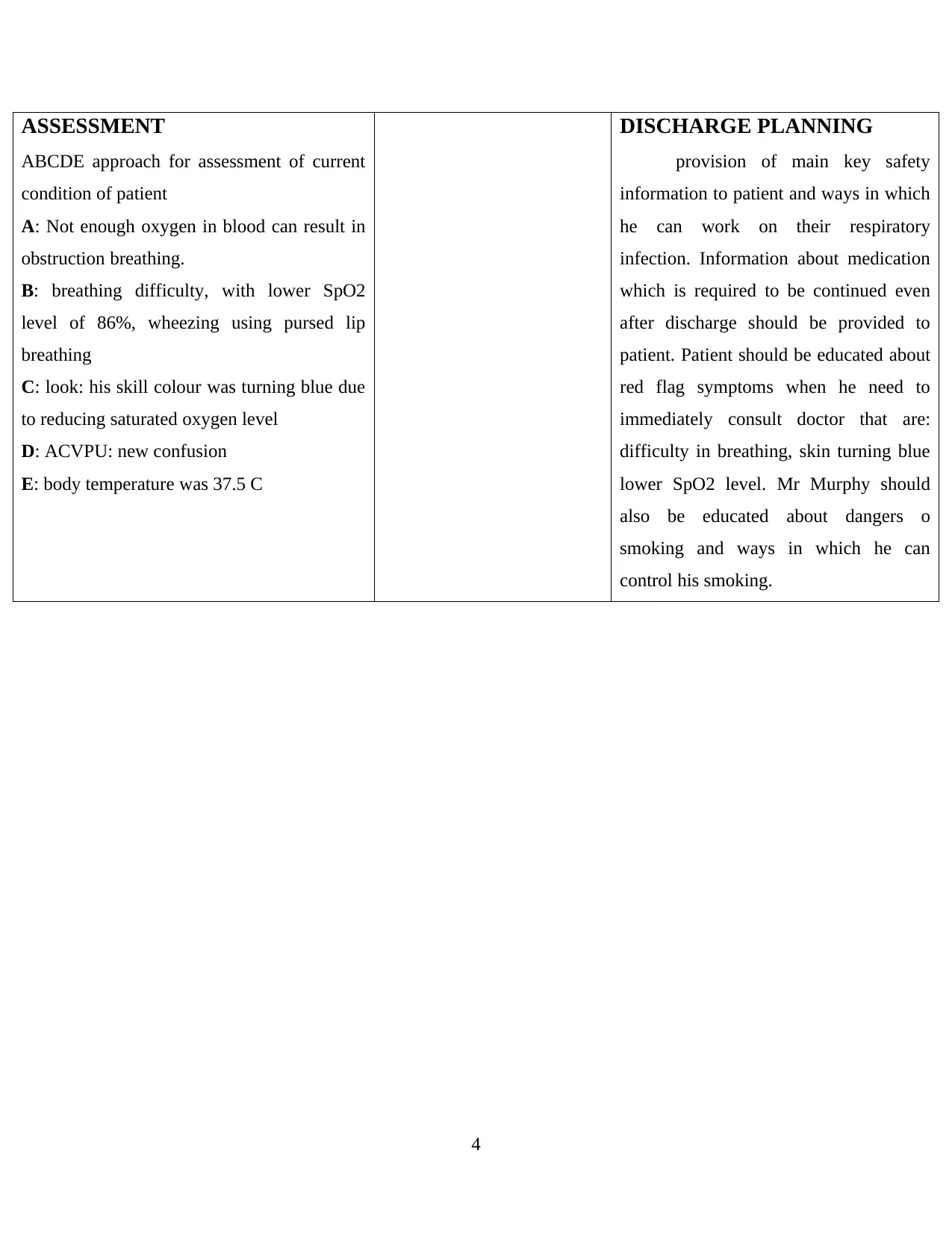
ASSESSMENT
ABCDE approach for assessment of current
condition of patient
A: Not enough oxygen in blood can result in
obstruction breathing.
B: breathing difficulty, with lower SpO2
level of 86%, wheezing using pursed lip
breathing
C: look: his skill colour was turning blue due
to reducing saturated oxygen level
D: ACVPU: new confusion
E: body temperature was 37.5 C
DISCHARGE PLANNING
provision of main key safety
information to patient and ways in which
he can work on their respiratory
infection. Information about medication
which is required to be continued even
after discharge should be provided to
patient. Patient should be educated about
red flag symptoms when he need to
immediately consult doctor that are:
difficulty in breathing, skin turning blue
lower SpO2 level. Mr Murphy should
also be educated about dangers o
smoking and ways in which he can
control his smoking.
4
ABCDE approach for assessment of current
condition of patient
A: Not enough oxygen in blood can result in
obstruction breathing.
B: breathing difficulty, with lower SpO2
level of 86%, wheezing using pursed lip
breathing
C: look: his skill colour was turning blue due
to reducing saturated oxygen level
D: ACVPU: new confusion
E: body temperature was 37.5 C
DISCHARGE PLANNING
provision of main key safety
information to patient and ways in which
he can work on their respiratory
infection. Information about medication
which is required to be continued even
after discharge should be provided to
patient. Patient should be educated about
red flag symptoms when he need to
immediately consult doctor that are:
difficulty in breathing, skin turning blue
lower SpO2 level. Mr Murphy should
also be educated about dangers o
smoking and ways in which he can
control his smoking.
4
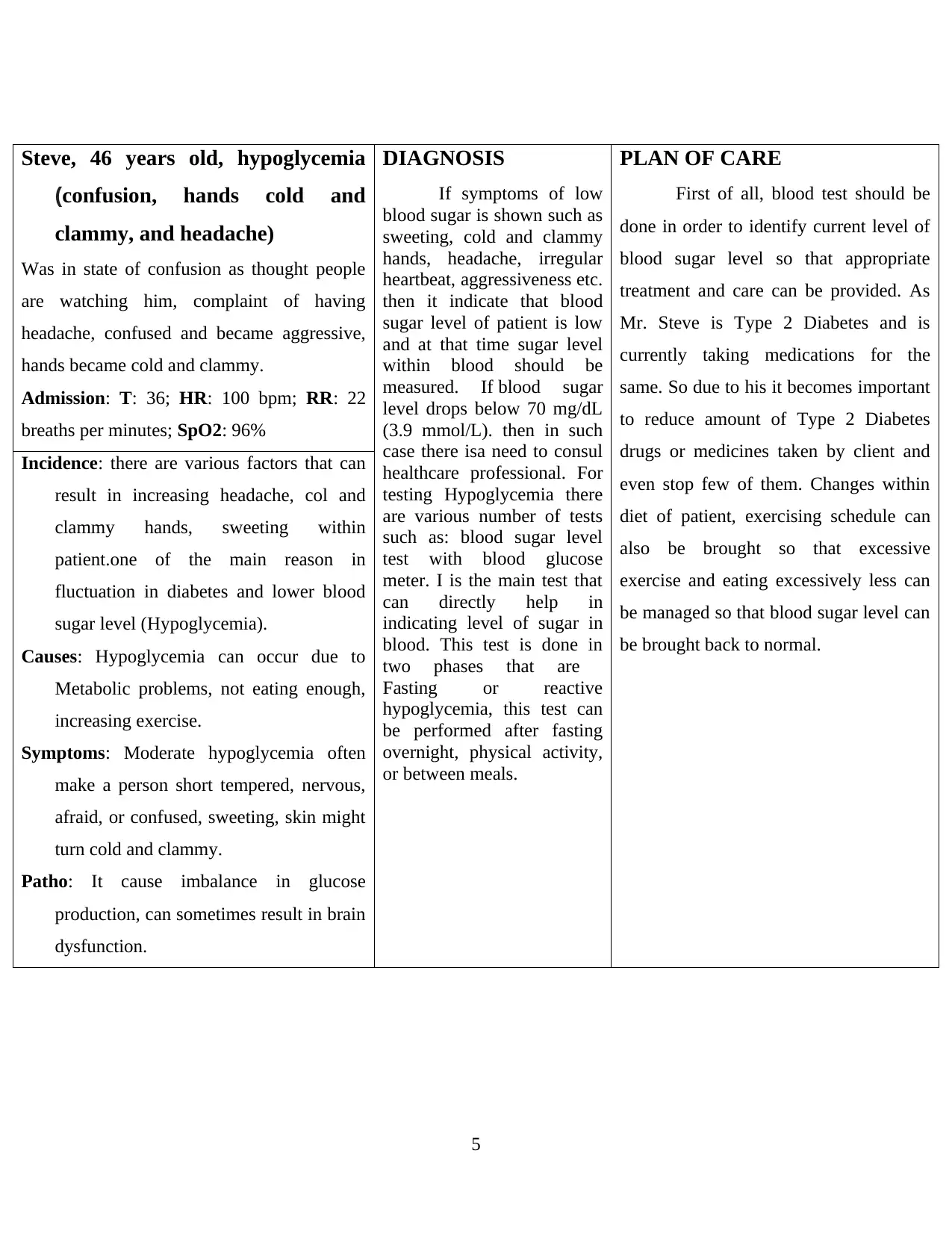
Steve, 46 years old, hypoglycemia
(confusion, hands cold and
clammy, and headache)
Was in state of confusion as thought people
are watching him, complaint of having
headache, confused and became aggressive,
hands became cold and clammy.
Admission: T: 36; HR: 100 bpm; RR: 22
breaths per minutes; SpO2: 96%
DIAGNOSIS
If symptoms of low
blood sugar is shown such as
sweeting, cold and clammy
hands, headache, irregular
heartbeat, aggressiveness etc.
then it indicate that blood
sugar level of patient is low
and at that time sugar level
within blood should be
measured. If blood sugar
level drops below 70 mg/dL
(3.9 mmol/L). then in such
case there isa need to consul
healthcare professional. For
testing Hypoglycemia there
are various number of tests
such as: blood sugar level
test with blood glucose
meter. I is the main test that
can directly help in
indicating level of sugar in
blood. This test is done in
two phases that are
Fasting or reactive
hypoglycemia, this test can
be performed after fasting
overnight, physical activity,
or between meals.
PLAN OF CARE
First of all, blood test should be
done in order to identify current level of
blood sugar level so that appropriate
treatment and care can be provided. As
Mr. Steve is Type 2 Diabetes and is
currently taking medications for the
same. So due to his it becomes important
to reduce amount of Type 2 Diabetes
drugs or medicines taken by client and
even stop few of them. Changes within
diet of patient, exercising schedule can
also be brought so that excessive
exercise and eating excessively less can
be managed so that blood sugar level can
be brought back to normal.
Incidence: there are various factors that can
result in increasing headache, col and
clammy hands, sweeting within
patient.one of the main reason in
fluctuation in diabetes and lower blood
sugar level (Hypoglycemia).
Causes: Hypoglycemia can occur due to
Metabolic problems, not eating enough,
increasing exercise.
Symptoms: Moderate hypoglycemia often
make a person short tempered, nervous,
afraid, or confused, sweeting, skin might
turn cold and clammy.
Patho: It cause imbalance in glucose
production, can sometimes result in brain
dysfunction.
5
(confusion, hands cold and
clammy, and headache)
Was in state of confusion as thought people
are watching him, complaint of having
headache, confused and became aggressive,
hands became cold and clammy.
Admission: T: 36; HR: 100 bpm; RR: 22
breaths per minutes; SpO2: 96%
DIAGNOSIS
If symptoms of low
blood sugar is shown such as
sweeting, cold and clammy
hands, headache, irregular
heartbeat, aggressiveness etc.
then it indicate that blood
sugar level of patient is low
and at that time sugar level
within blood should be
measured. If blood sugar
level drops below 70 mg/dL
(3.9 mmol/L). then in such
case there isa need to consul
healthcare professional. For
testing Hypoglycemia there
are various number of tests
such as: blood sugar level
test with blood glucose
meter. I is the main test that
can directly help in
indicating level of sugar in
blood. This test is done in
two phases that are
Fasting or reactive
hypoglycemia, this test can
be performed after fasting
overnight, physical activity,
or between meals.
PLAN OF CARE
First of all, blood test should be
done in order to identify current level of
blood sugar level so that appropriate
treatment and care can be provided. As
Mr. Steve is Type 2 Diabetes and is
currently taking medications for the
same. So due to his it becomes important
to reduce amount of Type 2 Diabetes
drugs or medicines taken by client and
even stop few of them. Changes within
diet of patient, exercising schedule can
also be brought so that excessive
exercise and eating excessively less can
be managed so that blood sugar level can
be brought back to normal.
Incidence: there are various factors that can
result in increasing headache, col and
clammy hands, sweeting within
patient.one of the main reason in
fluctuation in diabetes and lower blood
sugar level (Hypoglycemia).
Causes: Hypoglycemia can occur due to
Metabolic problems, not eating enough,
increasing exercise.
Symptoms: Moderate hypoglycemia often
make a person short tempered, nervous,
afraid, or confused, sweeting, skin might
turn cold and clammy.
Patho: It cause imbalance in glucose
production, can sometimes result in brain
dysfunction.
5
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
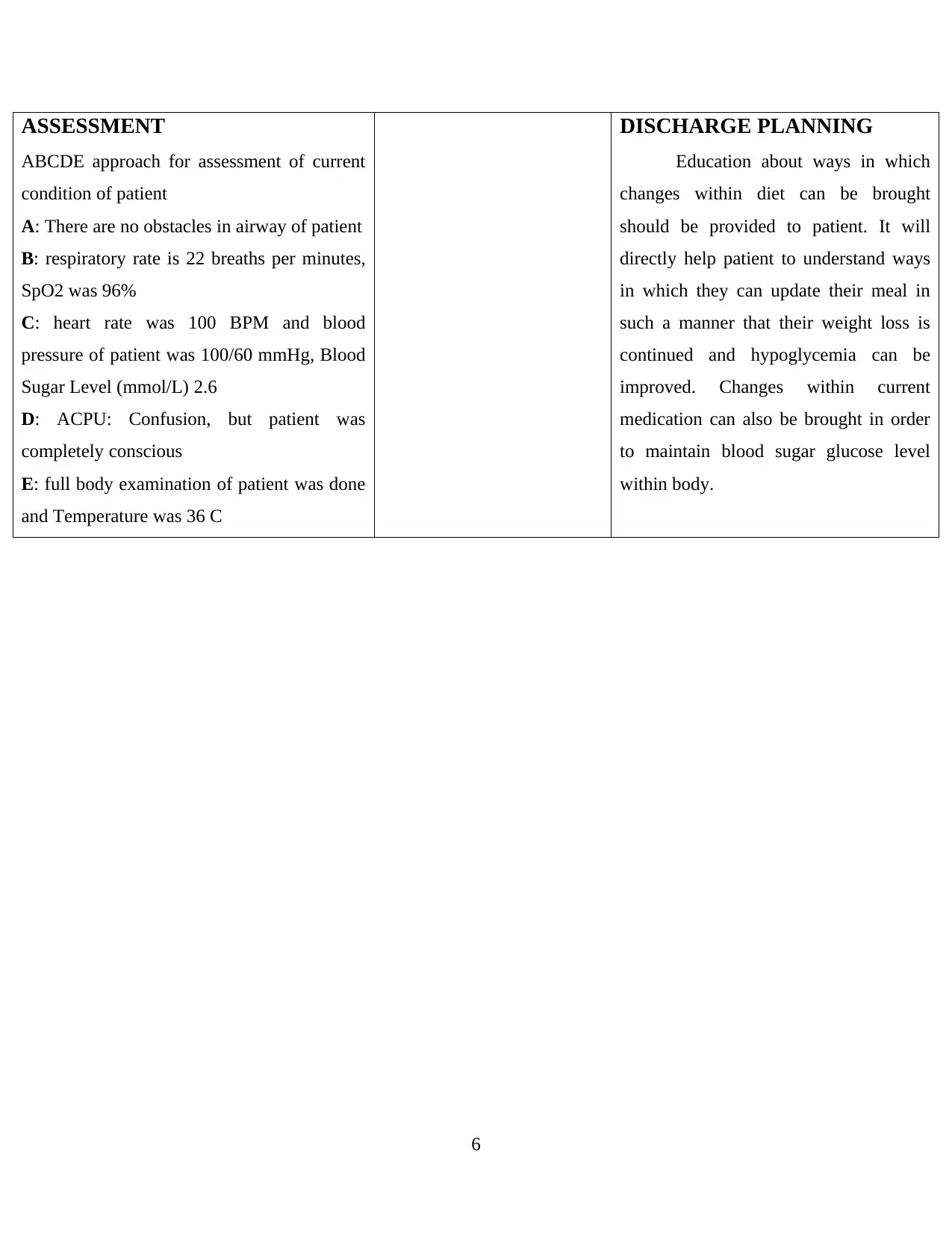
ASSESSMENT
ABCDE approach for assessment of current
condition of patient
A: There are no obstacles in airway of patient
B: respiratory rate is 22 breaths per minutes,
SpO2 was 96%
C: heart rate was 100 BPM and blood
pressure of patient was 100/60 mmHg, Blood
Sugar Level (mmol/L) 2.6
D: ACPU: Confusion, but patient was
completely conscious
E: full body examination of patient was done
and Temperature was 36 C
DISCHARGE PLANNING
Education about ways in which
changes within diet can be brought
should be provided to patient. It will
directly help patient to understand ways
in which they can update their meal in
such a manner that their weight loss is
continued and hypoglycemia can be
improved. Changes within current
medication can also be brought in order
to maintain blood sugar glucose level
within body.
6
ABCDE approach for assessment of current
condition of patient
A: There are no obstacles in airway of patient
B: respiratory rate is 22 breaths per minutes,
SpO2 was 96%
C: heart rate was 100 BPM and blood
pressure of patient was 100/60 mmHg, Blood
Sugar Level (mmol/L) 2.6
D: ACPU: Confusion, but patient was
completely conscious
E: full body examination of patient was done
and Temperature was 36 C
DISCHARGE PLANNING
Education about ways in which
changes within diet can be brought
should be provided to patient. It will
directly help patient to understand ways
in which they can update their meal in
such a manner that their weight loss is
continued and hypoglycemia can be
improved. Changes within current
medication can also be brought in order
to maintain blood sugar glucose level
within body.
6
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
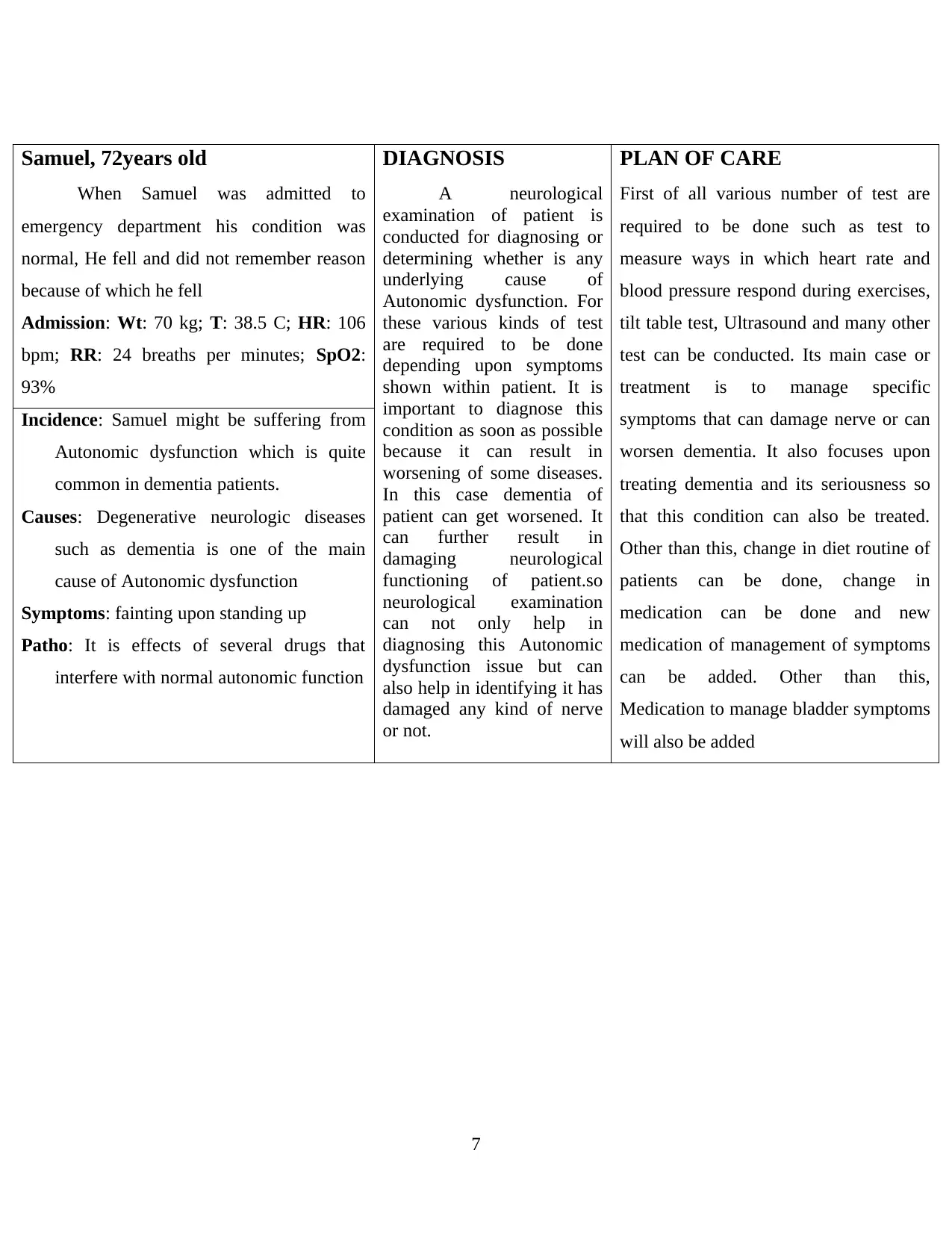
Samuel, 72years old
When Samuel was admitted to
emergency department his condition was
normal, He fell and did not remember reason
because of which he fell
Admission: Wt: 70 kg; T: 38.5 C; HR: 106
bpm; RR: 24 breaths per minutes; SpO2:
93%
DIAGNOSIS
A neurological
examination of patient is
conducted for diagnosing or
determining whether is any
underlying cause of
Autonomic dysfunction. For
these various kinds of test
are required to be done
depending upon symptoms
shown within patient. It is
important to diagnose this
condition as soon as possible
because it can result in
worsening of some diseases.
In this case dementia of
patient can get worsened. It
can further result in
damaging neurological
functioning of patient.so
neurological examination
can not only help in
diagnosing this Autonomic
dysfunction issue but can
also help in identifying it has
damaged any kind of nerve
or not.
PLAN OF CARE
First of all various number of test are
required to be done such as test to
measure ways in which heart rate and
blood pressure respond during exercises,
tilt table test, Ultrasound and many other
test can be conducted. Its main case or
treatment is to manage specific
symptoms that can damage nerve or can
worsen dementia. It also focuses upon
treating dementia and its seriousness so
that this condition can also be treated.
Other than this, change in diet routine of
patients can be done, change in
medication can be done and new
medication of management of symptoms
can be added. Other than this,
Medication to manage bladder symptoms
will also be added
Incidence: Samuel might be suffering from
Autonomic dysfunction which is quite
common in dementia patients.
Causes: Degenerative neurologic diseases
such as dementia is one of the main
cause of Autonomic dysfunction
Symptoms: fainting upon standing up
Patho: It is effects of several drugs that
interfere with normal autonomic function
7
When Samuel was admitted to
emergency department his condition was
normal, He fell and did not remember reason
because of which he fell
Admission: Wt: 70 kg; T: 38.5 C; HR: 106
bpm; RR: 24 breaths per minutes; SpO2:
93%
DIAGNOSIS
A neurological
examination of patient is
conducted for diagnosing or
determining whether is any
underlying cause of
Autonomic dysfunction. For
these various kinds of test
are required to be done
depending upon symptoms
shown within patient. It is
important to diagnose this
condition as soon as possible
because it can result in
worsening of some diseases.
In this case dementia of
patient can get worsened. It
can further result in
damaging neurological
functioning of patient.so
neurological examination
can not only help in
diagnosing this Autonomic
dysfunction issue but can
also help in identifying it has
damaged any kind of nerve
or not.
PLAN OF CARE
First of all various number of test are
required to be done such as test to
measure ways in which heart rate and
blood pressure respond during exercises,
tilt table test, Ultrasound and many other
test can be conducted. Its main case or
treatment is to manage specific
symptoms that can damage nerve or can
worsen dementia. It also focuses upon
treating dementia and its seriousness so
that this condition can also be treated.
Other than this, change in diet routine of
patients can be done, change in
medication can be done and new
medication of management of symptoms
can be added. Other than this,
Medication to manage bladder symptoms
will also be added
Incidence: Samuel might be suffering from
Autonomic dysfunction which is quite
common in dementia patients.
Causes: Degenerative neurologic diseases
such as dementia is one of the main
cause of Autonomic dysfunction
Symptoms: fainting upon standing up
Patho: It is effects of several drugs that
interfere with normal autonomic function
7
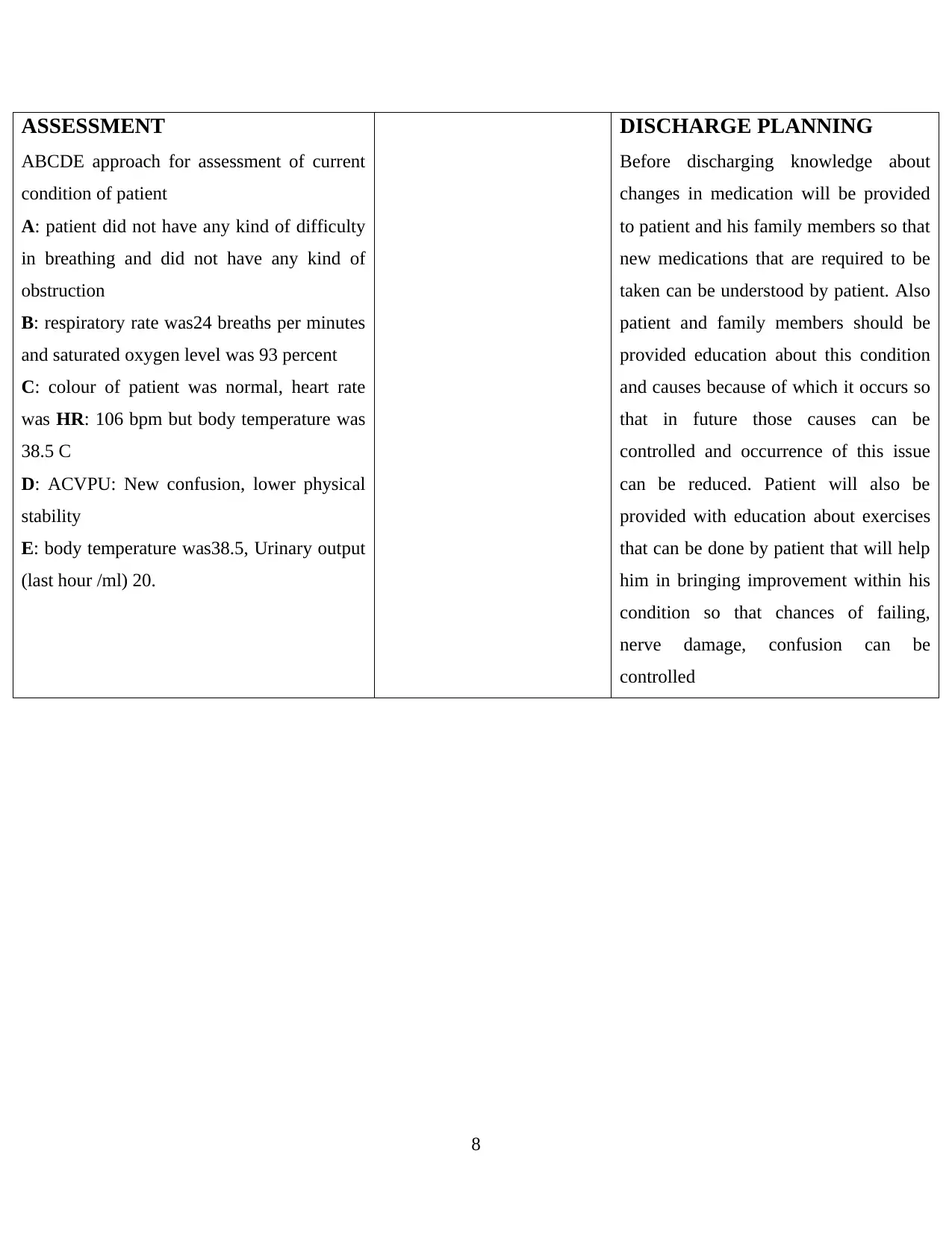
ASSESSMENT
ABCDE approach for assessment of current
condition of patient
A: patient did not have any kind of difficulty
in breathing and did not have any kind of
obstruction
B: respiratory rate was24 breaths per minutes
and saturated oxygen level was 93 percent
C: colour of patient was normal, heart rate
was HR: 106 bpm but body temperature was
38.5 C
D: ACVPU: New confusion, lower physical
stability
E: body temperature was38.5, Urinary output
(last hour /ml) 20.
DISCHARGE PLANNING
Before discharging knowledge about
changes in medication will be provided
to patient and his family members so that
new medications that are required to be
taken can be understood by patient. Also
patient and family members should be
provided education about this condition
and causes because of which it occurs so
that in future those causes can be
controlled and occurrence of this issue
can be reduced. Patient will also be
provided with education about exercises
that can be done by patient that will help
him in bringing improvement within his
condition so that chances of failing,
nerve damage, confusion can be
controlled
8
ABCDE approach for assessment of current
condition of patient
A: patient did not have any kind of difficulty
in breathing and did not have any kind of
obstruction
B: respiratory rate was24 breaths per minutes
and saturated oxygen level was 93 percent
C: colour of patient was normal, heart rate
was HR: 106 bpm but body temperature was
38.5 C
D: ACVPU: New confusion, lower physical
stability
E: body temperature was38.5, Urinary output
(last hour /ml) 20.
DISCHARGE PLANNING
Before discharging knowledge about
changes in medication will be provided
to patient and his family members so that
new medications that are required to be
taken can be understood by patient. Also
patient and family members should be
provided education about this condition
and causes because of which it occurs so
that in future those causes can be
controlled and occurrence of this issue
can be reduced. Patient will also be
provided with education about exercises
that can be done by patient that will help
him in bringing improvement within his
condition so that chances of failing,
nerve damage, confusion can be
controlled
8
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





