Evidence Based Nursing Research
VerifiedAdded on 2023/01/09
|11
|2697
|40
AI Summary
This document discusses evidence based nursing research and its importance in healthcare. It covers topics such as medication administration, nursing interventions, and patient education. The case study focuses on the use of Ipratropium Bromide for a patient with COPD.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: NURSING
Evidence Based Nursing Research
Name of the Student
Name of the University
Author note
Evidence Based Nursing Research
Name of the Student
Name of the University
Author note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1NURSING
Table of Contents
Answer 1....................................................................................................................................2
Answer 2....................................................................................................................................2
Answer 3....................................................................................................................................3
Answer 4....................................................................................................................................4
Answer 5....................................................................................................................................5
Answer 6....................................................................................................................................6
References..................................................................................................................................8
Table of Contents
Answer 1....................................................................................................................................2
Answer 2....................................................................................................................................2
Answer 3....................................................................................................................................3
Answer 4....................................................................................................................................4
Answer 5....................................................................................................................................5
Answer 6....................................................................................................................................6
References..................................................................................................................................8
2NURSING
Answer 1
Ipratropium Bromide
250 micrograms
Thrice daily
Answer 2
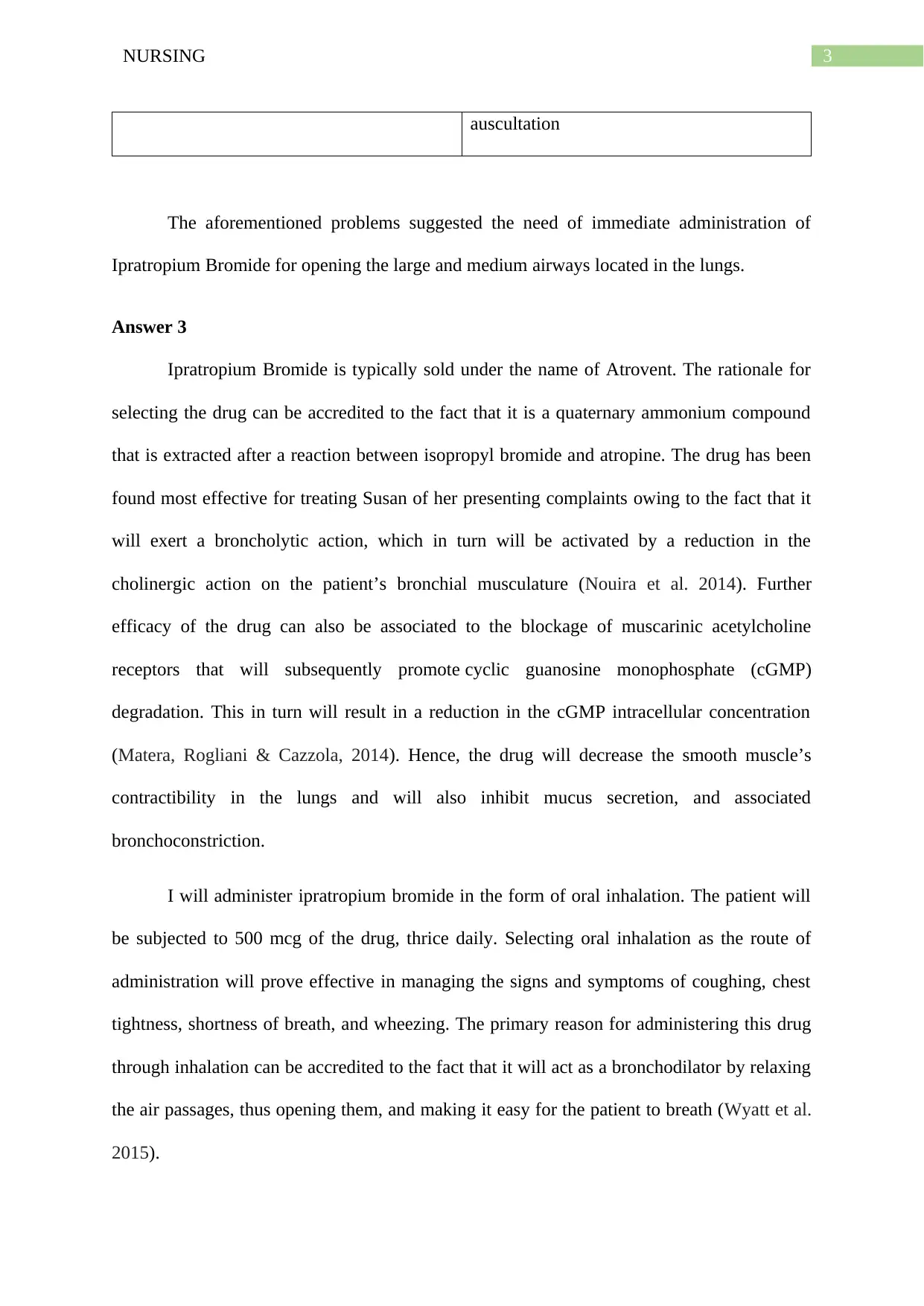
Name of the patient- Susan Sly, age 58 years
Presenting condition- She has been admitted to the medical ward following an
episode of chronic cough, wheezing sounds during breathing, and shortness of breath, with a
bluish tinge in her fingernails. During admission, her son also stated that she has been
reporting signs and symptoms of swelling in her ankles over the past three weeks.
Medical history- An assessment of her medical history suggests that she had a
flattened diaphragm, systemic hypertension diagnosis in 2005, broken right leg as a child, and
appendectomy at the age of 15. In addition, she has been an active smoker and smoked at
least 30 cigarettes every day, till the age of 55. Bone density test had been done two years ago
that demonstrated poor score (-3), thus providing an indication for possible osteoporosis.
Nursing assessment findings-
Subjective Objective
“..this morning I suddenly felt that I could
not breath”
Physical examination: BP 140/90; P 72, RR
30; Ht 5ft 2 in; Wt 101 lbs; T 101.7 °F
“Often I feel a sensation of tightness in my
chest that makes me very scared”
Audible wheezing sounds on auscultation
Stains on nails and diffuse wheezing to
Answer 1
Ipratropium Bromide
250 micrograms
Thrice daily
Answer 2
Name of the patient- Susan Sly, age 58 years
Presenting condition- She has been admitted to the medical ward following an
episode of chronic cough, wheezing sounds during breathing, and shortness of breath, with a
bluish tinge in her fingernails. During admission, her son also stated that she has been
reporting signs and symptoms of swelling in her ankles over the past three weeks.
Medical history- An assessment of her medical history suggests that she had a
flattened diaphragm, systemic hypertension diagnosis in 2005, broken right leg as a child, and
appendectomy at the age of 15. In addition, she has been an active smoker and smoked at
least 30 cigarettes every day, till the age of 55. Bone density test had been done two years ago
that demonstrated poor score (-3), thus providing an indication for possible osteoporosis.
Nursing assessment findings-
Subjective Objective
“..this morning I suddenly felt that I could
not breath”
Physical examination: BP 140/90; P 72, RR
30; Ht 5ft 2 in; Wt 101 lbs; T 101.7 °F
“Often I feel a sensation of tightness in my
chest that makes me very scared”
Audible wheezing sounds on auscultation
Stains on nails and diffuse wheezing to
3NURSING
auscultation
The aforementioned problems suggested the need of immediate administration of
Ipratropium Bromide for opening the large and medium airways located in the lungs.
Answer 3
Ipratropium Bromide is typically sold under the name of Atrovent. The rationale for
selecting the drug can be accredited to the fact that it is a quaternary ammonium compound
that is extracted after a reaction between isopropyl bromide and atropine. The drug has been
found most effective for treating Susan of her presenting complaints owing to the fact that it
will exert a broncholytic action, which in turn will be activated by a reduction in the
cholinergic action on the patient’s bronchial musculature (Nouira et al. 2014). Further
efficacy of the drug can also be associated to the blockage of muscarinic acetylcholine
receptors that will subsequently promote cyclic guanosine monophosphate (cGMP)
degradation. This in turn will result in a reduction in the cGMP intracellular concentration
(Matera, Rogliani & Cazzola, 2014). Hence, the drug will decrease the smooth muscle’s
contractibility in the lungs and will also inhibit mucus secretion, and associated
bronchoconstriction.
I will administer ipratropium bromide in the form of oral inhalation. The patient will
be subjected to 500 mcg of the drug, thrice daily. Selecting oral inhalation as the route of
administration will prove effective in managing the signs and symptoms of coughing, chest
tightness, shortness of breath, and wheezing. The primary reason for administering this drug
through inhalation can be accredited to the fact that it will act as a bronchodilator by relaxing
the air passages, thus opening them, and making it easy for the patient to breath (Wyatt et al.
2015).
auscultation
The aforementioned problems suggested the need of immediate administration of
Ipratropium Bromide for opening the large and medium airways located in the lungs.
Answer 3
Ipratropium Bromide is typically sold under the name of Atrovent. The rationale for
selecting the drug can be accredited to the fact that it is a quaternary ammonium compound
that is extracted after a reaction between isopropyl bromide and atropine. The drug has been
found most effective for treating Susan of her presenting complaints owing to the fact that it
will exert a broncholytic action, which in turn will be activated by a reduction in the
cholinergic action on the patient’s bronchial musculature (Nouira et al. 2014). Further
efficacy of the drug can also be associated to the blockage of muscarinic acetylcholine
receptors that will subsequently promote cyclic guanosine monophosphate (cGMP)
degradation. This in turn will result in a reduction in the cGMP intracellular concentration
(Matera, Rogliani & Cazzola, 2014). Hence, the drug will decrease the smooth muscle’s
contractibility in the lungs and will also inhibit mucus secretion, and associated
bronchoconstriction.
I will administer ipratropium bromide in the form of oral inhalation. The patient will
be subjected to 500 mcg of the drug, thrice daily. Selecting oral inhalation as the route of
administration will prove effective in managing the signs and symptoms of coughing, chest
tightness, shortness of breath, and wheezing. The primary reason for administering this drug
through inhalation can be accredited to the fact that it will act as a bronchodilator by relaxing
the air passages, thus opening them, and making it easy for the patient to breath (Wyatt et al.
2015).
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4NURSING
The clinical practice also requires me to administer the drug accurately, based on the
prescribed indications. Two puffs need to be inhaled by Susan, thrice a day, after a minimum
interval of four hours. While initially, it might be necessary to administer four puffs each day
for exerting maximum impact on the COPD signs and symptoms. According to the Global
Initiative for Chronic Obstructive Lung Disease (GOLD) COPD guidelines, ipratropium has
been recommended as the first line therapy for Group A and might also be administered for
additional symptom control in Group B, C, and D (Rieger-Reyes et al. 2014). In addition, I
might have to use the drug in conjunction with some short-acting beta-2 agonist, if the patient
does not show response to the treatment.
Susan will be educated on the precautionary steps that she must follow, after
discharge from the hospital. She will be advised to stay away from any kind of smoke, refrain
from smoking, and will also be trained to perform pursed-lip breathing, under circumstances
when she feels shortness of breath (Cabral et al. 2015). Further education will also encompass
teaching her the dosage and timing of the medications. I will also encourage her to regularly
exercise and eat healthy food that will help her gain weight.
However, ipratropium inhalation aerosols have been found to contain several
flammable ingredients that are under pressure. Hence, with the aim of avoiding any form of
injury, efforts must be taken to keep the aerosol away from flames or extreme heat. I will also
take care to prevent puncture of the container. In addition, potential side effects of the drug
encompass closed-angle glaucoma, acute bronchospasm, paradoxical bronchospasm, cardiac
arrhythmia, and urinary retention.
Answer 4
It can be deduced from the assessment findings that continuous exposure to tobacco
smoke was the major contributing factor to the onset and development of COPD in the
The clinical practice also requires me to administer the drug accurately, based on the
prescribed indications. Two puffs need to be inhaled by Susan, thrice a day, after a minimum
interval of four hours. While initially, it might be necessary to administer four puffs each day
for exerting maximum impact on the COPD signs and symptoms. According to the Global
Initiative for Chronic Obstructive Lung Disease (GOLD) COPD guidelines, ipratropium has
been recommended as the first line therapy for Group A and might also be administered for
additional symptom control in Group B, C, and D (Rieger-Reyes et al. 2014). In addition, I
might have to use the drug in conjunction with some short-acting beta-2 agonist, if the patient
does not show response to the treatment.
Susan will be educated on the precautionary steps that she must follow, after
discharge from the hospital. She will be advised to stay away from any kind of smoke, refrain
from smoking, and will also be trained to perform pursed-lip breathing, under circumstances
when she feels shortness of breath (Cabral et al. 2015). Further education will also encompass
teaching her the dosage and timing of the medications. I will also encourage her to regularly
exercise and eat healthy food that will help her gain weight.
However, ipratropium inhalation aerosols have been found to contain several
flammable ingredients that are under pressure. Hence, with the aim of avoiding any form of
injury, efforts must be taken to keep the aerosol away from flames or extreme heat. I will also
take care to prevent puncture of the container. In addition, potential side effects of the drug
encompass closed-angle glaucoma, acute bronchospasm, paradoxical bronchospasm, cardiac
arrhythmia, and urinary retention.
Answer 4
It can be deduced from the assessment findings that continuous exposure to tobacco
smoke was the major contributing factor to the onset and development of COPD in the
5NURSING
patient (Camp et al. 2014). Three major nursing interventions for the medication under
consideration are as follows:
Providing protection to the ipratropium solution for inhalation from a strong light
source. The vials containing the solution that are unused will be stored inside foil
pouch. Exposure to any source of strong light will act as a major concern due to the
possibility of some chemical and/or photo-degradation reactions (Skidmore-Roth
2018). These reactions will bring about an alteration in the stability of the drug.
Efforts will be taken to ensure that the patient Susan is adequately hydrated, in
addition to controlling the environmental temperature, with the aim of preventing
hyperpyrexia. This can be associated with the fact that toxic dosage of the drug has
often been allied with CNS stimulation and hyperpyrexia that increases the body
temperature drastically (Kamimura et al. 2016).
Patient void will also be collected, prior to administration of the medication, for
avoiding signs of urinary retention because the drug might interfere with the ability
of the urinary bladder to partially or completely empty itself (Alotaibi & Wali 2014).
Answer 5
Medications are one of the most common form of intervention that are implemented
in healthcare facilities and when administered appropriately and safely, they are found to
contribute to noteworthy improvements in wellbeing and health of the patients (Adhikari et
al. 2014). The National Safety and Quality Health Service Standards place an emphasis on
the strategies and systems that must be in place for allowing clinicians to conduct safe
prescribing, dispensing, and administering of medicines (ACSQH 2011). The standard 4
elaborates on the fact that a patient’s past medication history must be accurately recorded by
the clinical workforce, which in turn must be made available to registered nurses during the
episode of care delivery.
patient (Camp et al. 2014). Three major nursing interventions for the medication under
consideration are as follows:
Providing protection to the ipratropium solution for inhalation from a strong light
source. The vials containing the solution that are unused will be stored inside foil
pouch. Exposure to any source of strong light will act as a major concern due to the
possibility of some chemical and/or photo-degradation reactions (Skidmore-Roth
2018). These reactions will bring about an alteration in the stability of the drug.
Efforts will be taken to ensure that the patient Susan is adequately hydrated, in
addition to controlling the environmental temperature, with the aim of preventing
hyperpyrexia. This can be associated with the fact that toxic dosage of the drug has
often been allied with CNS stimulation and hyperpyrexia that increases the body
temperature drastically (Kamimura et al. 2016).
Patient void will also be collected, prior to administration of the medication, for
avoiding signs of urinary retention because the drug might interfere with the ability
of the urinary bladder to partially or completely empty itself (Alotaibi & Wali 2014).
Answer 5
Medications are one of the most common form of intervention that are implemented
in healthcare facilities and when administered appropriately and safely, they are found to
contribute to noteworthy improvements in wellbeing and health of the patients (Adhikari et
al. 2014). The National Safety and Quality Health Service Standards place an emphasis on
the strategies and systems that must be in place for allowing clinicians to conduct safe
prescribing, dispensing, and administering of medicines (ACSQH 2011). The standard 4
elaborates on the fact that a patient’s past medication history must be accurately recorded by
the clinical workforce, which in turn must be made available to registered nurses during the
episode of care delivery.
6NURSING
Taking into consideration the fact that wrong administration of medicines are related
with greater incidence of medication errors and opposing events, the standard makes it
mandatory for a registered nurse to conduct comprehensive and regular assessment of the
medication, in order to identify potential risks to patient health (4.2). Furthermore, current
clinical information and medication history must be documented accurately (4.6.1). Presence
of any known medical hypersensitivities and prior instances of adverse drug reactions also
need to be recorded, with the aim of facilitating transfer of care (4.7.1) (ACSQH 2011).
The National Practice Standards also make it imperative for all registered nurses to
function both collaboratively and autonomously in the clinical role. Thorough and
comprehensive assessments must be conducted by the nurse, by implementing advanced
nursing knowledge, in relation to prescribing and administering medications (standard 7)
(ANMF 2014). Furthermore, registered nurses also have the duty of effectively implementing
preventive care and health promotion practices, in the form of evidence-based
pharmacological or non-pharmacological interventions that will enhance the overall health
and wellbeing of the patients. Effective delivery of evidence-based medical information for
promoting patient self-management and improving health literacy is also expected of the
nurses (standard 11). In addition, conducting an evaluation and assessment of the
effectiveness and quality of medication is an important aspect of nursing care (standard 12).
Answer 6
It can be analysed from the case study that continuous smoking for several years led
to the onset of COPD in the patient, which in turn brought about an obstruction of the airways
located in the lungs. Excess production of sputum resulted in poor airflow that subsequently
caused wheezing sounds and shortness of breath. An analysis of her physical state suggested
that airflow limitation was responsible for decreasing the ability of her lungs in breathing out
completely, thus casing air trapping (Eckerblad et al. 2014). On assessing her physical signs,
Taking into consideration the fact that wrong administration of medicines are related
with greater incidence of medication errors and opposing events, the standard makes it
mandatory for a registered nurse to conduct comprehensive and regular assessment of the
medication, in order to identify potential risks to patient health (4.2). Furthermore, current
clinical information and medication history must be documented accurately (4.6.1). Presence
of any known medical hypersensitivities and prior instances of adverse drug reactions also
need to be recorded, with the aim of facilitating transfer of care (4.7.1) (ACSQH 2011).
The National Practice Standards also make it imperative for all registered nurses to
function both collaboratively and autonomously in the clinical role. Thorough and
comprehensive assessments must be conducted by the nurse, by implementing advanced
nursing knowledge, in relation to prescribing and administering medications (standard 7)
(ANMF 2014). Furthermore, registered nurses also have the duty of effectively implementing
preventive care and health promotion practices, in the form of evidence-based
pharmacological or non-pharmacological interventions that will enhance the overall health
and wellbeing of the patients. Effective delivery of evidence-based medical information for
promoting patient self-management and improving health literacy is also expected of the
nurses (standard 11). In addition, conducting an evaluation and assessment of the
effectiveness and quality of medication is an important aspect of nursing care (standard 12).
Answer 6
It can be analysed from the case study that continuous smoking for several years led
to the onset of COPD in the patient, which in turn brought about an obstruction of the airways
located in the lungs. Excess production of sputum resulted in poor airflow that subsequently
caused wheezing sounds and shortness of breath. An analysis of her physical state suggested
that airflow limitation was responsible for decreasing the ability of her lungs in breathing out
completely, thus casing air trapping (Eckerblad et al. 2014). On assessing her physical signs,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7NURSING
it was also note that she manifested symptoms of a flare-up that called for the need of
immediate medication administration (Pennington & Louis 2016). It was further deduced
from the case scenario that although inhalation of ipratropium bromide helps in reducing
severe exacerbations, there lies the possibility of renal impairment and/or hepatic impairment.
While caring for other patients, the selection of face mask versus mouth piece shall be
made based on the understanding and skills of individual patients. In addition, patients who
have hypersensitivity to ipratropium bromide will not be administered the medicine. In
contrast, formoterol, salmeterol, or titropium will be given to those patients (Singh et al.
2014). The aerosol spray will also be test sprayed at least thrice, prior to the use of a new
canister, in order to prevent instances of paradoxical bronchospasm. Extra care will also be
taken for patients who have closed-angle glaucoma, to prevent worsening of their health
condition (Ah-kee et al. 2015). Under circumstances when patients report blurred vision or
dizziness, they must be cautioned to refrain from participation in activities that require
operation of machinery or driving. Elderly patients also manifest an increased likelihood of
suffering from complications occurring from anticholinergic side effects. In addition, it will
be administered to COPD patients during pregnancy only if the potential value of the drug to
the mother overshadows the possible hazards to the foetus.
it was also note that she manifested symptoms of a flare-up that called for the need of
immediate medication administration (Pennington & Louis 2016). It was further deduced
from the case scenario that although inhalation of ipratropium bromide helps in reducing
severe exacerbations, there lies the possibility of renal impairment and/or hepatic impairment.
While caring for other patients, the selection of face mask versus mouth piece shall be
made based on the understanding and skills of individual patients. In addition, patients who
have hypersensitivity to ipratropium bromide will not be administered the medicine. In
contrast, formoterol, salmeterol, or titropium will be given to those patients (Singh et al.
2014). The aerosol spray will also be test sprayed at least thrice, prior to the use of a new
canister, in order to prevent instances of paradoxical bronchospasm. Extra care will also be
taken for patients who have closed-angle glaucoma, to prevent worsening of their health
condition (Ah-kee et al. 2015). Under circumstances when patients report blurred vision or
dizziness, they must be cautioned to refrain from participation in activities that require
operation of machinery or driving. Elderly patients also manifest an increased likelihood of
suffering from complications occurring from anticholinergic side effects. In addition, it will
be administered to COPD patients during pregnancy only if the potential value of the drug to
the mother overshadows the possible hazards to the foetus.
8NURSING
References
Adhikari, R., Tocher, J., Smith, P., Corcoran, J. & MacArthur, J., 2014, ‘A multi-disciplinary
approach to medication safety and the implication for nursing education and practice’,
Nurse education today, vol.34, no.2, pp.185-190.
Ah-kee, E.Y., Egong, E., Shafi, A., Lim, L.T. & Yim, J.L., 2015, ‘A review of drug-induced
acute angle closure glaucoma for non-ophthalmologists’, Qatar medical journal, p.6.
Alotaibi, M.A. & Wali, S.O., 2014, ‘Anisocoria with high dose ipratropium bromide inhaler’,
Saudi medical journal, vol.35, no.5, pp.508-509.
Australian Commission on Safety and Quality in Healthcare., 2011, National Safety and
Quality Health Service Standards, viewed 29 March 2019,
https://www.safetyandquality.gov.au/wp-content/uploads/2011/01/NSQHS-
Standards-Sept2011.pdf
Australian Nursing & Midwifery Federation., 2014, NATIONAL PRACTICE STANDARDS
for NURSES IN GENERAL PRACTICE, viewed 29 March 2019,
https://www.anmf.org.au/documents/National_Practice_Standards_for_Nurses_in_Ge
neral_Practice.pdf
Cabral, L.F., D'Elia, T.C., Marins, D.S., Zin, W.A. & Guimaraes, F.S., 2015, ‘Pursed lip
breathing improves exercise tolerance in COPD: a randomized crossover study’, Eur
J Phys Rehabil Med, vol.51, no.1, pp.79-88.
Camp, P.G., Ramirez-Venegas, A., Sansores, R.H., Alva, L.F., McDougall, J.E., Sin, D.D.,
Paré, P.D., Müller, N.L., Silva, C.I.S., Rojas, C.E. & Coxson, H.O., 2014, ‘COPD
phenotypes in biomass smoke-versus tobacco smoke-exposed Mexican women’,
European Respiratory Journal, vol.43, no.3, pp.725-734.
References
Adhikari, R., Tocher, J., Smith, P., Corcoran, J. & MacArthur, J., 2014, ‘A multi-disciplinary
approach to medication safety and the implication for nursing education and practice’,
Nurse education today, vol.34, no.2, pp.185-190.
Ah-kee, E.Y., Egong, E., Shafi, A., Lim, L.T. & Yim, J.L., 2015, ‘A review of drug-induced
acute angle closure glaucoma for non-ophthalmologists’, Qatar medical journal, p.6.
Alotaibi, M.A. & Wali, S.O., 2014, ‘Anisocoria with high dose ipratropium bromide inhaler’,
Saudi medical journal, vol.35, no.5, pp.508-509.
Australian Commission on Safety and Quality in Healthcare., 2011, National Safety and
Quality Health Service Standards, viewed 29 March 2019,
https://www.safetyandquality.gov.au/wp-content/uploads/2011/01/NSQHS-
Standards-Sept2011.pdf
Australian Nursing & Midwifery Federation., 2014, NATIONAL PRACTICE STANDARDS
for NURSES IN GENERAL PRACTICE, viewed 29 March 2019,
https://www.anmf.org.au/documents/National_Practice_Standards_for_Nurses_in_Ge
neral_Practice.pdf
Cabral, L.F., D'Elia, T.C., Marins, D.S., Zin, W.A. & Guimaraes, F.S., 2015, ‘Pursed lip
breathing improves exercise tolerance in COPD: a randomized crossover study’, Eur
J Phys Rehabil Med, vol.51, no.1, pp.79-88.
Camp, P.G., Ramirez-Venegas, A., Sansores, R.H., Alva, L.F., McDougall, J.E., Sin, D.D.,
Paré, P.D., Müller, N.L., Silva, C.I.S., Rojas, C.E. & Coxson, H.O., 2014, ‘COPD
phenotypes in biomass smoke-versus tobacco smoke-exposed Mexican women’,
European Respiratory Journal, vol.43, no.3, pp.725-734.
9NURSING
Eckerblad, J., Tödt, K., Jakobsson, P., Unosson, M., Skargren, E., Kentsson, M. & Theander,
K., 2014, ‘Symptom burden in stable COPD patients with moderate or severe airflow
limitation’, Heart & Lung: The Journal of Acute and Critical Care, vol.43, no.4,
pp.351-357.
Kamimura, M., Arimoto, Y., Homma, C., Takeoka, S., Fukusumi, M., Mouri, A. &
Hamamoto, Y., 2016, ‘The effects of daily bathing on symptoms of patients with
bronchial asthma’, Asia Pacific Allergy, vol.6, no.2, pp.112-119.
Matera, M.G., Rogliani, P. & Cazzola, M., 2014, ‘Muscarinic receptor antagonists for the
treatment of chronic obstructive pulmonary disease’, Expert opinion on
pharmacotherapy, vol.15, no.7, pp.961-977.
Nouira, S., Bouida, W., Grissa, M.H., Beltaief, K., Trimech, M.N., Boubaker, H., Marghli, S.,
Letaief, M. & Boukef, R., 2014, ‘Magnesium sulfate versus ipratropium bromide in
chronic obstructive pulmonary disease exacerbation: a randomized trial’, American
journal of therapeutics, vol.21, no.3, pp.152-158.
Pennington, K.M. & Louis, E.K.S., 2016, ‘“Don't Believe Your Eyes” Ipratropium Induced
Mydriasis: A Case Report and Review of the Literature’, General medicine (Los
Angeles, Calif.), vol.4, no.3.
Rieger-Reyes, C., García-Tirado, F.J., Rubio-Galán, F.J. & Marín-Trigo, J.M., 2014,
‘Classification of chronic obstructive pulmonary disease severity according to the new
Global Initiative for Chronic Obstructive Lung Disease 2011 guidelines: COPD
assessment test versus modified Medical Research Council scale’, Archivos de
Bronconeumología (English Edition), vol.50, no.4, pp.129-134.
Singh, D., Jones, P.W., Bateman, E.D., Korn, S., Serra, C., Molins, E., Caracta, C., Gil, E.G.
& Leselbaum, A., 2014, ‘Efficacy and safety of aclidinium bromide/formoterol
Eckerblad, J., Tödt, K., Jakobsson, P., Unosson, M., Skargren, E., Kentsson, M. & Theander,
K., 2014, ‘Symptom burden in stable COPD patients with moderate or severe airflow
limitation’, Heart & Lung: The Journal of Acute and Critical Care, vol.43, no.4,
pp.351-357.
Kamimura, M., Arimoto, Y., Homma, C., Takeoka, S., Fukusumi, M., Mouri, A. &
Hamamoto, Y., 2016, ‘The effects of daily bathing on symptoms of patients with
bronchial asthma’, Asia Pacific Allergy, vol.6, no.2, pp.112-119.
Matera, M.G., Rogliani, P. & Cazzola, M., 2014, ‘Muscarinic receptor antagonists for the
treatment of chronic obstructive pulmonary disease’, Expert opinion on
pharmacotherapy, vol.15, no.7, pp.961-977.
Nouira, S., Bouida, W., Grissa, M.H., Beltaief, K., Trimech, M.N., Boubaker, H., Marghli, S.,
Letaief, M. & Boukef, R., 2014, ‘Magnesium sulfate versus ipratropium bromide in
chronic obstructive pulmonary disease exacerbation: a randomized trial’, American
journal of therapeutics, vol.21, no.3, pp.152-158.
Pennington, K.M. & Louis, E.K.S., 2016, ‘“Don't Believe Your Eyes” Ipratropium Induced
Mydriasis: A Case Report and Review of the Literature’, General medicine (Los
Angeles, Calif.), vol.4, no.3.
Rieger-Reyes, C., García-Tirado, F.J., Rubio-Galán, F.J. & Marín-Trigo, J.M., 2014,
‘Classification of chronic obstructive pulmonary disease severity according to the new
Global Initiative for Chronic Obstructive Lung Disease 2011 guidelines: COPD
assessment test versus modified Medical Research Council scale’, Archivos de
Bronconeumología (English Edition), vol.50, no.4, pp.129-134.
Singh, D., Jones, P.W., Bateman, E.D., Korn, S., Serra, C., Molins, E., Caracta, C., Gil, E.G.
& Leselbaum, A., 2014, ‘Efficacy and safety of aclidinium bromide/formoterol
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10NURSING
fumarate fixed-dose combinations compared with individual components and placebo
in patients with COPD (ACLIFORM-COPD): a multicentre, randomised study’, BMC
pulmonary medicine, vol.14, no.1, p.178.
Skidmore-Roth, L., 2018, Mosby's 2019 Nursing Drug Reference E-Book, Elsevier Health
Sciences.
Wyatt, E.L., Borland, M.L., Doyle, S.K. & Geelhoed, G.C., 2015, ‘Metered‐dose inhaler
ipratropium bromide in moderate acute asthma in children: A single‐blinded
randomised controlled trial’, Journal of paediatrics and child health, vol.51, no.2,
pp.192-198.
fumarate fixed-dose combinations compared with individual components and placebo
in patients with COPD (ACLIFORM-COPD): a multicentre, randomised study’, BMC
pulmonary medicine, vol.14, no.1, p.178.
Skidmore-Roth, L., 2018, Mosby's 2019 Nursing Drug Reference E-Book, Elsevier Health
Sciences.
Wyatt, E.L., Borland, M.L., Doyle, S.K. & Geelhoed, G.C., 2015, ‘Metered‐dose inhaler
ipratropium bromide in moderate acute asthma in children: A single‐blinded
randomised controlled trial’, Journal of paediatrics and child health, vol.51, no.2,
pp.192-198.
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





