Nursing Leadership: Policy Issue of Nurse Staffing Ratio in San Jose Hospital
VerifiedAdded on 2023/06/07
|11
|2684
|410
AI Summary
The effect of nurses staffing ratio is widely a problem in many hospitals and healthcare facilities. The San Jose hospital is not an exception. There is a shortage of nurses in the hospital. Like its known nurse's low staffing leads to the quality of health care of a hospital. Adverse effects and outcomes are seen in the patients. The patients stay longer in the hospitals than expected, other related complications and worse enough mortality. Low staffing does not only affect patients but also affects the few nurses who are in the hospital. Nurses suffer from job dissatisfaction, fatigue and staff burn-out.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: NURSING LEADERSHIP 1
Nursing leadership
Name
Institution
Nursing leadership
Name
Institution
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
NURSING LEADERSHIP 2
NURSING LEADERSHIP
Issue related to the organizational priorities
Policy issue; nurses staffing ratio
The effect of nurses staffing ratio is widely a problem in many hospitals and healthcare
facilities. The San Jose hospital is not an exception. There is a shortage of nurses in the hospital.
Like its known nurse's low staffing leads to the quality of health care of a hospital. Adverse
effects and outcomes are seen in the patients. The patients stay longer in the hospitals than
expected, other related complications and worse enough mortality. Low staffing does not only
affect patients but also affects the few nurses who are in the hospital. Nurses suffer from job
dissatisfaction, fatigue and staff burn-out. The WHO organization standard for nurse ratio is
supposed to be calculated regarding the patient they handle and the standard working time. In a
hospital like San Jose, there has to be the correct staffing ratio for nurses for the hospital to
deliver quality healthcare services (Cho, Sloane, Kim, Choi, Yoo & Aiken, 2015).
Patient to nurse ratio is supposed to be 2-bed patients to one nurse. However, the rule
accepts a team of 5 rotational group nurses to work on 15 patients. That is the acceptable
standard. Concerning working hours, the staffing ratio has a WHO designated formula. This
method is referred to as productive hours method. The productive hours are minus vacation,
illness or continuing education duration (Aiken, Sloane, Bruyneel, Heede, Griffiths, Busse &
McHugh,2014).
NURSING LEADERSHIP
Issue related to the organizational priorities
Policy issue; nurses staffing ratio
The effect of nurses staffing ratio is widely a problem in many hospitals and healthcare
facilities. The San Jose hospital is not an exception. There is a shortage of nurses in the hospital.
Like its known nurse's low staffing leads to the quality of health care of a hospital. Adverse
effects and outcomes are seen in the patients. The patients stay longer in the hospitals than
expected, other related complications and worse enough mortality. Low staffing does not only
affect patients but also affects the few nurses who are in the hospital. Nurses suffer from job
dissatisfaction, fatigue and staff burn-out. The WHO organization standard for nurse ratio is
supposed to be calculated regarding the patient they handle and the standard working time. In a
hospital like San Jose, there has to be the correct staffing ratio for nurses for the hospital to
deliver quality healthcare services (Cho, Sloane, Kim, Choi, Yoo & Aiken, 2015).
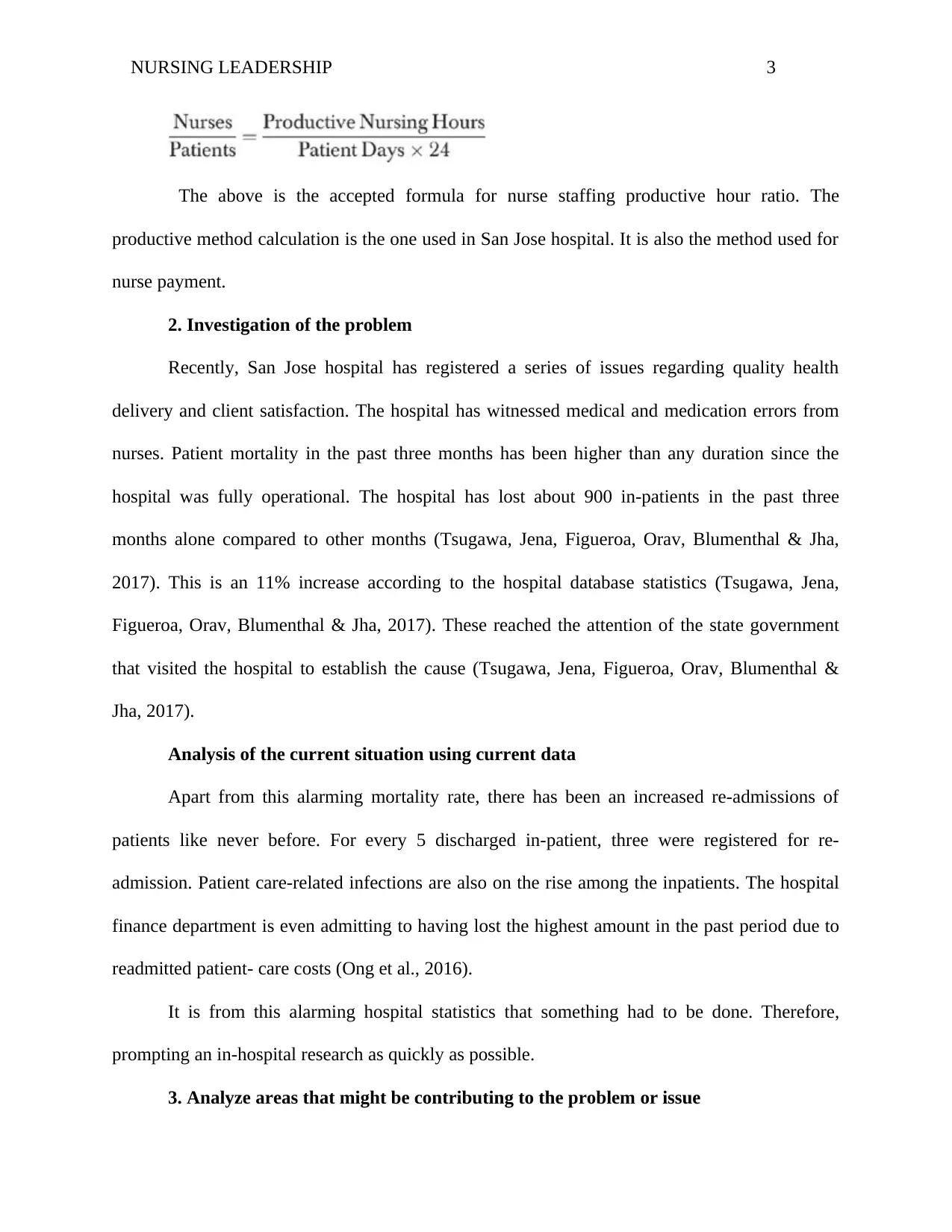
Patient to nurse ratio is supposed to be 2-bed patients to one nurse. However, the rule
accepts a team of 5 rotational group nurses to work on 15 patients. That is the acceptable
standard. Concerning working hours, the staffing ratio has a WHO designated formula. This
method is referred to as productive hours method. The productive hours are minus vacation,
illness or continuing education duration (Aiken, Sloane, Bruyneel, Heede, Griffiths, Busse &
McHugh,2014).
NURSING LEADERSHIP 3
The above is the accepted formula for nurse staffing productive hour ratio. The
productive method calculation is the one used in San Jose hospital. It is also the method used for
nurse payment.
2. Investigation of the problem
Recently, San Jose hospital has registered a series of issues regarding quality health
delivery and client satisfaction. The hospital has witnessed medical and medication errors from
nurses. Patient mortality in the past three months has been higher than any duration since the
hospital was fully operational. The hospital has lost about 900 in-patients in the past three
months alone compared to other months (Tsugawa, Jena, Figueroa, Orav, Blumenthal & Jha,
2017). This is an 11% increase according to the hospital database statistics (Tsugawa, Jena,
Figueroa, Orav, Blumenthal & Jha, 2017). These reached the attention of the state government
that visited the hospital to establish the cause (Tsugawa, Jena, Figueroa, Orav, Blumenthal &
Jha, 2017).
Analysis of the current situation using current data
Apart from this alarming mortality rate, there has been an increased re-admissions of
patients like never before. For every 5 discharged in-patient, three were registered for re-
admission. Patient care-related infections are also on the rise among the inpatients. The hospital
finance department is even admitting to having lost the highest amount in the past period due to
readmitted patient- care costs (Ong et al., 2016).
It is from this alarming hospital statistics that something had to be done. Therefore,
prompting an in-hospital research as quickly as possible.
3. Analyze areas that might be contributing to the problem or issue
The above is the accepted formula for nurse staffing productive hour ratio. The
productive method calculation is the one used in San Jose hospital. It is also the method used for
nurse payment.
2. Investigation of the problem
Recently, San Jose hospital has registered a series of issues regarding quality health
delivery and client satisfaction. The hospital has witnessed medical and medication errors from
nurses. Patient mortality in the past three months has been higher than any duration since the
hospital was fully operational. The hospital has lost about 900 in-patients in the past three
months alone compared to other months (Tsugawa, Jena, Figueroa, Orav, Blumenthal & Jha,
2017). This is an 11% increase according to the hospital database statistics (Tsugawa, Jena,
Figueroa, Orav, Blumenthal & Jha, 2017). These reached the attention of the state government
that visited the hospital to establish the cause (Tsugawa, Jena, Figueroa, Orav, Blumenthal &
Jha, 2017).
Analysis of the current situation using current data
Apart from this alarming mortality rate, there has been an increased re-admissions of
patients like never before. For every 5 discharged in-patient, three were registered for re-
admission. Patient care-related infections are also on the rise among the inpatients. The hospital
finance department is even admitting to having lost the highest amount in the past period due to
readmitted patient- care costs (Ong et al., 2016).
It is from this alarming hospital statistics that something had to be done. Therefore,
prompting an in-hospital research as quickly as possible.
3. Analyze areas that might be contributing to the problem or issue
NURSING LEADERSHIP 4
From the statistics of the hospital, an investigation had to be done to get the cause of the
problem. Considering that the hospital had experienced and dedicated doctors, who had been
serving for more than ten years, the problem did not point to their direction. From the recorded
mortality rate, out of 10 dead patients, five were diagnosed to die due to a medication error, a
role played by a nurse (Makary & Daniel, 2016). Most re-admissions were done because of
inadequate assessment of the nurse on the patient. Other errors that were recorded in the wards
were not accounted for, but they were increasingly on the rise. The inpatient infections could
only be through hygiene or nurse medication error. But since the hospital was not suffering from
a hygiene break-out, the only possible explanation was a problem in the nursing department.
When followed-up through research and detective means, the result was never pleasant.
Nurses who might have lost a patient through medication error ethically should be sent on
compulsory leave while seeing the hospital therapist until the therapist clears them for patient
attendance once more (Van Cott, 2018). However, this was not the case in San Jose. Due to the
nursing staff ratio, it was impossible to send any nurse on compulsory leave. The nurses were
working long hours both night and day shifts. The nursing personnel that comprised of registered
nurses, licensed practical and vocational nurses, unlicensed assistive staff and nursing aides were
only totaling to 183 compared to the number of patient in the inpatient sections when all beds are
occupied which is about 12000. Without admitting the number of out-patients, the nurses were
getting overwhelmed due to staffing ratio, and something had to be done.
4. Proposed solution or innovation for the problem or issue
The perfect solution is to make a nurse-driven workforce quickly and constitute a
committee. The committee top-most goal would be creating staffing plans that will help achieve
patients’ needs while balancing patient population to that of skills and experience of nursing
From the statistics of the hospital, an investigation had to be done to get the cause of the
problem. Considering that the hospital had experienced and dedicated doctors, who had been
serving for more than ten years, the problem did not point to their direction. From the recorded
mortality rate, out of 10 dead patients, five were diagnosed to die due to a medication error, a
role played by a nurse (Makary & Daniel, 2016). Most re-admissions were done because of
inadequate assessment of the nurse on the patient. Other errors that were recorded in the wards
were not accounted for, but they were increasingly on the rise. The inpatient infections could
only be through hygiene or nurse medication error. But since the hospital was not suffering from
a hygiene break-out, the only possible explanation was a problem in the nursing department.
When followed-up through research and detective means, the result was never pleasant.
Nurses who might have lost a patient through medication error ethically should be sent on
compulsory leave while seeing the hospital therapist until the therapist clears them for patient
attendance once more (Van Cott, 2018). However, this was not the case in San Jose. Due to the
nursing staff ratio, it was impossible to send any nurse on compulsory leave. The nurses were
working long hours both night and day shifts. The nursing personnel that comprised of registered
nurses, licensed practical and vocational nurses, unlicensed assistive staff and nursing aides were
only totaling to 183 compared to the number of patient in the inpatient sections when all beds are
occupied which is about 12000. Without admitting the number of out-patients, the nurses were
getting overwhelmed due to staffing ratio, and something had to be done.
4. Proposed solution or innovation for the problem or issue
The perfect solution is to make a nurse-driven workforce quickly and constitute a
committee. The committee top-most goal would be creating staffing plans that will help achieve
patients’ needs while balancing patient population to that of skills and experience of nursing
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
NURSING LEADERSHIP 5
personnel. Considering that staffing scheduling can be a source of nursing dissatisfaction, the
committee is to be comprised of all members of the nursing personnel and stakeholders (Pineau,
Stam, Spence, Regan & Wong, 2015). However, 65% should consist of nursing personnel
representatives and the rest of the hospital stakeholders. The roles of the committee would help
solve the nursing staffing problem completely. The committee will develop, review and
implement San Jose’s nurse staffing plans and rules. This will help in reducing nursing errors for
medication and medical arising from job dissatisfaction and fatigue (Paulsen, 2018).
Creating partnering team that jell correctly for unit based nursing staff teams will be
productive. The nursing staff teams will be consulting on patient care regulations, therefore,
reducing error. Error reduction will lead to a reduced number of discharged re-admission in-
patients and also minimize the mortality rate (Paulsen, 2018)
The committee will also organize education days for nurses and nurses’ benchmark days
to ensure all nurses are physically, mentally and emotionally fit to handle nursing responsibilities
and challenges.
5. Recommended resources to implement the proposed solution.
The most important resource required for the solution is the human resource. The
committee will consist of 65% direct-care nurses and 35% hospital leadership, support staff and
patient care assistants (Kalisch, Aebersold, McLaughlin, Tschannen & Lane, 2015).
The committee will require a meeting hall space which is the boardroom that is already in
existence. The committee will not operate on allowances until they succeed and will require a
meeting to pass the same. Therefore, they will be no financial cost for the committee set-up. The
finance department of the hospital will give files and necessary writing materials for planning. A
planning health software is already in existence in the hospital, in case an upgrade will be
personnel. Considering that staffing scheduling can be a source of nursing dissatisfaction, the
committee is to be comprised of all members of the nursing personnel and stakeholders (Pineau,
Stam, Spence, Regan & Wong, 2015). However, 65% should consist of nursing personnel
representatives and the rest of the hospital stakeholders. The roles of the committee would help
solve the nursing staffing problem completely. The committee will develop, review and
implement San Jose’s nurse staffing plans and rules. This will help in reducing nursing errors for
medication and medical arising from job dissatisfaction and fatigue (Paulsen, 2018).
Creating partnering team that jell correctly for unit based nursing staff teams will be
productive. The nursing staff teams will be consulting on patient care regulations, therefore,
reducing error. Error reduction will lead to a reduced number of discharged re-admission in-
patients and also minimize the mortality rate (Paulsen, 2018)
The committee will also organize education days for nurses and nurses’ benchmark days
to ensure all nurses are physically, mentally and emotionally fit to handle nursing responsibilities
and challenges.
5. Recommended resources to implement the proposed solution.
The most important resource required for the solution is the human resource. The
committee will consist of 65% direct-care nurses and 35% hospital leadership, support staff and
patient care assistants (Kalisch, Aebersold, McLaughlin, Tschannen & Lane, 2015).
The committee will require a meeting hall space which is the boardroom that is already in
existence. The committee will not operate on allowances until they succeed and will require a
meeting to pass the same. Therefore, they will be no financial cost for the committee set-up. The
finance department of the hospital will give files and necessary writing materials for planning. A
planning health software is already in existence in the hospital, in case an upgrade will be
NURSING LEADERSHIP 6
needed, it will cost the hospital 250 dollars. That amount will only be possible after the
committee is set-up and has considered a new schedule set-up software.
6. Timeline for the proposed solution
The committee shall hold meetings every month. Each session is expected to take up to
one hour-thirty minutes. However, the first meeting will take longer since the committee will
plan on how to make up with a new operating schedule for the nurses. The first meeting will be
considered an emergency control meeting. Therefore, as an emergency control meeting, the
committee has to come up with new nurses scheduling plan. A well reflected discussion of the
past events and proposed solutions. It is within the first meeting of the proposed solution where a
timeline will be developed to analyze the benefits of the committee. However, the committee
suggested duration should not be less than three months and more than a year. Within the
proposed timeline, effectiveness of the committee will be established.
7. Discuss why each key stakeholder or partner is essential for the implementation
of the solution or innovation
Their chosen leaders should represent the nursing staff who are the majority members of
the committee. That is, leaders of registered nurses, another set of leaders from licensed assistant
nurses, another set of leaders from vocational nurses etc. Being the principal shareholder, the
nursing staff provides the insight into what is happening during the health care provision
duration. They responded well by accepting to join the committee.
All the stakeholders showed positivity towards the committee idea and agreed to send
different and capable representatives. The financial department agreed to sacrifice a few vote-
head that will cater for allowances of the committee members. This was a sign of a very positive
needed, it will cost the hospital 250 dollars. That amount will only be possible after the
committee is set-up and has considered a new schedule set-up software.
6. Timeline for the proposed solution
The committee shall hold meetings every month. Each session is expected to take up to
one hour-thirty minutes. However, the first meeting will take longer since the committee will
plan on how to make up with a new operating schedule for the nurses. The first meeting will be
considered an emergency control meeting. Therefore, as an emergency control meeting, the
committee has to come up with new nurses scheduling plan. A well reflected discussion of the
past events and proposed solutions. It is within the first meeting of the proposed solution where a
timeline will be developed to analyze the benefits of the committee. However, the committee
suggested duration should not be less than three months and more than a year. Within the
proposed timeline, effectiveness of the committee will be established.
7. Discuss why each key stakeholder or partner is essential for the implementation
of the solution or innovation
Their chosen leaders should represent the nursing staff who are the majority members of
the committee. That is, leaders of registered nurses, another set of leaders from licensed assistant
nurses, another set of leaders from vocational nurses etc. Being the principal shareholder, the
nursing staff provides the insight into what is happening during the health care provision
duration. They responded well by accepting to join the committee.
All the stakeholders showed positivity towards the committee idea and agreed to send
different and capable representatives. The financial department agreed to sacrifice a few vote-
head that will cater for allowances of the committee members. This was a sign of a very positive
NURSING LEADERSHIP 7
feedback. All the stakeholders provided two names that would represent each department in the
committee.
How to work with the key stakeholders to achieve success
The HR and finance representative helped provide the link to crucial topics like pay,
financial incentives and compensations. The representative from the hospital managing director
helps link the nurse’s grievances to the top-most management of the hospital, therefore, directly
contributing to policy and management of the hospital (Grubaugh & Flynn, 2018).
8. Discuss how your proposed solution or innovation could be implemented,
including how the Implementation could be evaluated for success
The committee implementation plan would begin immediately. An emergency meeting
would be held where the committee members will come up with a nursing staff roll-out schedule
and planning program. The committee will only come up with the plan after comparing the
number of expected patients to the number of operating nursing staff. The implementation of the
plan should begin the immediate week after the complete schedule by the committee is out.
Evaluation for the success of the committee implementation program will be reached
when there is reduced medical and medication errors by nurses. It will be determined by proper
and well planned out therapy for nurses. Incorporation of nurse’s turnover and vacancy data will
also indicate success (Duffield, Roche, Dimitrelis, Homer & Buchan, 2015).
Other side effects like patient re-admission and mortality due to nursing error should be
at less than a percentage. Finally, there should be a well-structured vacation and holiday period
for operating nurses after the schedule, and the nursing ratio is balanced evenly (Henkin et al.,
2016).
feedback. All the stakeholders provided two names that would represent each department in the
committee.
How to work with the key stakeholders to achieve success
The HR and finance representative helped provide the link to crucial topics like pay,
financial incentives and compensations. The representative from the hospital managing director
helps link the nurse’s grievances to the top-most management of the hospital, therefore, directly
contributing to policy and management of the hospital (Grubaugh & Flynn, 2018).
8. Discuss how your proposed solution or innovation could be implemented,
including how the Implementation could be evaluated for success
The committee implementation plan would begin immediately. An emergency meeting
would be held where the committee members will come up with a nursing staff roll-out schedule
and planning program. The committee will only come up with the plan after comparing the
number of expected patients to the number of operating nursing staff. The implementation of the
plan should begin the immediate week after the complete schedule by the committee is out.
Evaluation for the success of the committee implementation program will be reached
when there is reduced medical and medication errors by nurses. It will be determined by proper
and well planned out therapy for nurses. Incorporation of nurse’s turnover and vacancy data will
also indicate success (Duffield, Roche, Dimitrelis, Homer & Buchan, 2015).
Other side effects like patient re-admission and mortality due to nursing error should be
at less than a percentage. Finally, there should be a well-structured vacation and holiday period
for operating nurses after the schedule, and the nursing ratio is balanced evenly (Henkin et al.,
2016).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NURSING LEADERSHIP 8
Roles during the investigative process
Scientist
As a scientist, the ability to compare, analyze and evaluate data on patients and the
hospital is empirical. Coming up with percentages against duration is a scientific genius.
Detective
Help detect all reasons that could cause the hospital or the stated problems. Finding out
that the problem was the nursing staff ratio is a detective technique.
Manager of the healing environment
Bringing all the hospital departments together and helping to form a nursing helping
committee showed the prowess in management. Taking the supervisory role and chair of the
committee is further proof.
Roles during the investigative process
Scientist
As a scientist, the ability to compare, analyze and evaluate data on patients and the
hospital is empirical. Coming up with percentages against duration is a scientific genius.
Detective
Help detect all reasons that could cause the hospital or the stated problems. Finding out
that the problem was the nursing staff ratio is a detective technique.
Manager of the healing environment
Bringing all the hospital departments together and helping to form a nursing helping
committee showed the prowess in management. Taking the supervisory role and chair of the
committee is further proof.
NURSING LEADERSHIP 9
References
Aiken, L. H., Sloane, D. M., Bruyneel, L., Van den Heede, K., Griffiths, P., Busse, R., ... &
McHugh, M. D. (2014). Nurse staffing and education and hospital mortality in nine
European countries: a retrospective observational study. The Lancet, 383(9931), 1824-
1830.
Cho, E., Sloane, D. M., Kim, E. Y., Kim, S., Choi, M., Yoo, I. Y., ... & Aiken, L. H. (2015).
Effects of nurse staffing, work environments, and education on patient mortality: an
observational study. International journal of nursing studies, 52(2), 535-542.
Duffield, C. M., Roche, M. A., Dimitrelis, S., Homer, C., & Buchan, J. (2015). Instability in
patient and nurse characteristics, unit complexity and patient and system outcomes.
Journal of Advanced Nursing, 71(6), 1288-1298.
References
Aiken, L. H., Sloane, D. M., Bruyneel, L., Van den Heede, K., Griffiths, P., Busse, R., ... &
McHugh, M. D. (2014). Nurse staffing and education and hospital mortality in nine
European countries: a retrospective observational study. The Lancet, 383(9931), 1824-
1830.
Cho, E., Sloane, D. M., Kim, E. Y., Kim, S., Choi, M., Yoo, I. Y., ... & Aiken, L. H. (2015).
Effects of nurse staffing, work environments, and education on patient mortality: an
observational study. International journal of nursing studies, 52(2), 535-542.
Duffield, C. M., Roche, M. A., Dimitrelis, S., Homer, C., & Buchan, J. (2015). Instability in
patient and nurse characteristics, unit complexity and patient and system outcomes.
Journal of Advanced Nursing, 71(6), 1288-1298.
NURSING LEADERSHIP 10
Grubaugh, M. L., & Flynn, L. (2018). Relationships Among Nurse Manager Leadership Skills,
Conflict Management, and Unit Teamwork. Journal of Nursing Administration, 48(7/8),
383-388.
Henkin, S., Chon, T. Y., Christopherson, M. L., Halvorsen, A. J., Worden, L. M., & Ratelle, J. T.
(2016). Improving nurse–physician teamwork through interprofessional bedside
rounding. Journal of multidisciplinary healthcare, 9, 201.
Kalisch, B. J., Aebersold, M., McLaughlin, M., Tschannen, D., & Lane, S. (2015). An
intervention to improve nursing teamwork using virtual simulation. Western journal of
nursing research, 37(2), 164-179.
Makary, M. A., & Daniel, M. (2016). Medical error—the third leading cause of death in the US.
Bmj, 353, i2139.
Ong, M. K., Romano, P. S., Edgington, S., Aronow, H. U., Auerbach, A. D., Black, J. T., ... &
Ganiats, T. G. (2016). Effectiveness of remote patient monitoring after discharge of
hospitalized patients with heart failure: the better effectiveness after transition–heart
failure (BEAT-HF) randomized clinical trial. JAMA internal medicine, 176(3), 310-318.
Paulsen, R. A. (2018). Taking nurse staffing research to the unit level. Nursing management,
49(7), 42.
Pineau Stam, L. M., Spence Laschinger, H. K., Regan, S., & Wong, C. A. (2015). The influence
of personal and workplace resources on new graduate nurses' job satisfaction. Journal of
nursing management, 23(2), 190-199.
Tsugawa, Y., Jena, A. B., Figueroa, J. F., Orav, E. J., Blumenthal, D. M., & Jha, A. K. (2017).
Comparison of hospital mortality and readmission rates for Medicare patients treated by
male vs female physicians. JAMA internal medicine, 177(2), 206-213.
Grubaugh, M. L., & Flynn, L. (2018). Relationships Among Nurse Manager Leadership Skills,
Conflict Management, and Unit Teamwork. Journal of Nursing Administration, 48(7/8),
383-388.
Henkin, S., Chon, T. Y., Christopherson, M. L., Halvorsen, A. J., Worden, L. M., & Ratelle, J. T.
(2016). Improving nurse–physician teamwork through interprofessional bedside
rounding. Journal of multidisciplinary healthcare, 9, 201.
Kalisch, B. J., Aebersold, M., McLaughlin, M., Tschannen, D., & Lane, S. (2015). An
intervention to improve nursing teamwork using virtual simulation. Western journal of
nursing research, 37(2), 164-179.
Makary, M. A., & Daniel, M. (2016). Medical error—the third leading cause of death in the US.
Bmj, 353, i2139.
Ong, M. K., Romano, P. S., Edgington, S., Aronow, H. U., Auerbach, A. D., Black, J. T., ... &
Ganiats, T. G. (2016). Effectiveness of remote patient monitoring after discharge of
hospitalized patients with heart failure: the better effectiveness after transition–heart
failure (BEAT-HF) randomized clinical trial. JAMA internal medicine, 176(3), 310-318.
Paulsen, R. A. (2018). Taking nurse staffing research to the unit level. Nursing management,
49(7), 42.
Pineau Stam, L. M., Spence Laschinger, H. K., Regan, S., & Wong, C. A. (2015). The influence
of personal and workplace resources on new graduate nurses' job satisfaction. Journal of
nursing management, 23(2), 190-199.
Tsugawa, Y., Jena, A. B., Figueroa, J. F., Orav, E. J., Blumenthal, D. M., & Jha, A. K. (2017).
Comparison of hospital mortality and readmission rates for Medicare patients treated by
male vs female physicians. JAMA internal medicine, 177(2), 206-213.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
NURSING LEADERSHIP 11
Van Cott, H. (2018). Human errors: Their causes and reduction. In Human error in medicine (pp.
53-65). CRC Press.
Van Cott, H. (2018). Human errors: Their causes and reduction. In Human error in medicine (pp.
53-65). CRC Press.
1 out of 11
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.