NRSG366 Individual Case Study: Chronic Care & Clinical Reasoning
VerifiedAdded on 2023/04/11
|7
|2219
|207
Case Study
AI Summary
This case study analyzes the care priorities for Peter Mitchell, a 52-year-old male with type 2 diabetes, obesity ventilation syndrome, and sleep apnea, using the Levett-Jones Clinical Reasoning Cycle. The analysis identifies Peter's poorly managed diabetes, obesity, smoking habits, and depression as key factors influencing his health. The two main priorities of care are identified as effective management of diabetes mellitus while improving the quality of life and increase in the level of social participation. The action plan involves community health nurse-led education, self-monitoring of blood glucose levels, smoking cessation assistance, and interventions to reduce depression through increased self-acceptance and social participation. The evaluation of outcomes focuses on reduced blood sugar levels, weight, and smoking, along with improved mental health and social engagement. The analysis highlights the interconnectedness of physical and mental health and the importance of health education and disease awareness in promoting effective self-management.

Running head: NURSING
Nursing
Name of the Student
Name of the University
Author Notes
Nursing
Name of the Student
Name of the University
Author Notes
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
NURSING
Numerous factors influence the development of the nursing care plans for the
patients who are suffering from chronic healthcare conditions. For a primary healthcare
nurse, the clinical priority must be designed based on the exact needs of the patients (Cruz,
Carvalho & Sousa, 2014) stated that prioritization can be defined as a n integral part of the
nursing profession and prioritization of care helps to increase the effectiveness of the overall
outcome of care. Prioritization is mainly achieved through collaboration and integration of the
diverse aspects of the patient’s requirement. The following essay aims to analyse the two
different priorities care on the basis of the critical evaluation of the case study of Peter
Mitchell, a 52-year old male suffering from type 2 diabetes. The generation of the two care
priority will be based on the framework of the Levett Jones Clinical reasoning cycle.
Clinical reasoning cycle is a framework through which the nursing professionals
make use of their critical thinking and cognitive skills in order to frame the care plan for the
patients by highlighting the main priority of care(Alfaro-LeFevre, 2015). Levett Jones clinical
reasoning cycle helps the nursing professionals to deduced the care priority based on the
structured framework that is starting from collection of cues, processing of the relevant
information, establishment of goals, taking appropriate actions and simultaneous evaluation
of the outcomes of care (Levett-Jones, 2017).
In “considering of the patient’s information”, the main factors that must be taken
under consideration is Peter Mitchell is suffering from obesity ventilation syndrome, poorly
managed type 2 diabetes mellitus (T2DM) and sleep apnoea. Other associated symptoms
include increased rate of hunger, visible symptoms of shakiness while admitted to medical
ward, difficulty breathing whilst sleeping and high level of blood glucose. According to
Abdelaal, le Roux & Docherty, 2017), morbid obesity has fatal health consequences in
comparison to moderate obesity. Severely over-weight individuals, weighing around 100 to
200 pounds and are over 50-year of age have more complex health issues in comparison to
individuals who weigh moderately. The conditions become even more serious when the
person is predisposed with T2DM. Peter Mitchell is 145 kgs and thus his escalating body
mass index (BMI) is an important point of consideration while framing the priority of care.
This high blood glucose level (BGL) and increases rate of hunger indicates his poorly
controlled state of the T2DM. Lavie, McAuley, Church, Milani and Blair (2014) stated that
people who are overweight and is suffering from T2DM, are vulnerable towards developing
cardiovascular complication, hepatic malfunction and renal failure. Peter’s smoking habits
(20 cigarettes per day) is another point that must be taken into urgent consideration. Pan,
Wang, Talaei, Hu & Wu(2015) stated that smoking of cigarettes increases the vulnerability
and severity of T2DM.
NURSING
Numerous factors influence the development of the nursing care plans for the
patients who are suffering from chronic healthcare conditions. For a primary healthcare
nurse, the clinical priority must be designed based on the exact needs of the patients (Cruz,
Carvalho & Sousa, 2014) stated that prioritization can be defined as a n integral part of the
nursing profession and prioritization of care helps to increase the effectiveness of the overall
outcome of care. Prioritization is mainly achieved through collaboration and integration of the
diverse aspects of the patient’s requirement. The following essay aims to analyse the two
different priorities care on the basis of the critical evaluation of the case study of Peter
Mitchell, a 52-year old male suffering from type 2 diabetes. The generation of the two care
priority will be based on the framework of the Levett Jones Clinical reasoning cycle.
Clinical reasoning cycle is a framework through which the nursing professionals
make use of their critical thinking and cognitive skills in order to frame the care plan for the
patients by highlighting the main priority of care(Alfaro-LeFevre, 2015). Levett Jones clinical
reasoning cycle helps the nursing professionals to deduced the care priority based on the
structured framework that is starting from collection of cues, processing of the relevant
information, establishment of goals, taking appropriate actions and simultaneous evaluation
of the outcomes of care (Levett-Jones, 2017).
In “considering of the patient’s information”, the main factors that must be taken
under consideration is Peter Mitchell is suffering from obesity ventilation syndrome, poorly
managed type 2 diabetes mellitus (T2DM) and sleep apnoea. Other associated symptoms
include increased rate of hunger, visible symptoms of shakiness while admitted to medical
ward, difficulty breathing whilst sleeping and high level of blood glucose. According to
Abdelaal, le Roux & Docherty, 2017), morbid obesity has fatal health consequences in
comparison to moderate obesity. Severely over-weight individuals, weighing around 100 to
200 pounds and are over 50-year of age have more complex health issues in comparison to
individuals who weigh moderately. The conditions become even more serious when the
person is predisposed with T2DM. Peter Mitchell is 145 kgs and thus his escalating body
mass index (BMI) is an important point of consideration while framing the priority of care.
This high blood glucose level (BGL) and increases rate of hunger indicates his poorly
controlled state of the T2DM. Lavie, McAuley, Church, Milani and Blair (2014) stated that
people who are overweight and is suffering from T2DM, are vulnerable towards developing
cardiovascular complication, hepatic malfunction and renal failure. Peter’s smoking habits
(20 cigarettes per day) is another point that must be taken into urgent consideration. Pan,
Wang, Talaei, Hu & Wu(2015) stated that smoking of cigarettes increases the vulnerability
and severity of T2DM.
2
NURSING
“Collection cues or information” is the second step of the clinical reasoning cycle.
Peter Mitchell was initially 105 kgs in weight however after he left his job ( 3 years ago) and
went to insulin medication for management of diabetes and this is followed by the drastic
increase in weight (145 kgs at present). Peter Mitchell was diagnosed with T2DM 9 years
ago and is also suffering depression (since past 3 months) along with hypertension.
American Diabetes Association (2014) stated that uncontrolled diabetes is associated with
increase rate of hunger. Individuals who are unable to control their hunger or follow the
proper diet plan, develops high BGL. The depression of Peter Mitchell might be due to his
sudden loss of job and also because of his poor social image as embarrassed about his
size. Matthewset al. (2016) stated that social isolation due to poor body image or lack of self-
esteem leads to the development of depression. However, Tabák, Akbaraly, Batty and
Kivimäki (2014)stated that development of T2DM for a prolong period of time lead to the
development of persistent depression. The study conducted by De Boer et al. (2017)
revealed that diabetes and hypertension and inter-related. There is a substantial overlap
between the T2DM and development of high blood pressure in the disease mechanisms and
etiology. The increase in the blood pressure level leads to increase in the severity of T2DM.
Lifestyle of Peter Mitchell is also unhealthy as he is unable to follow an anti-diabetic diet plan
and at the same time smokes 20 cigarettes per day. His lack of observance of low-energy
high protein diet is associated with lack of proper support at home (Peter Mitchell stays
alone) leading to further gain in weight.
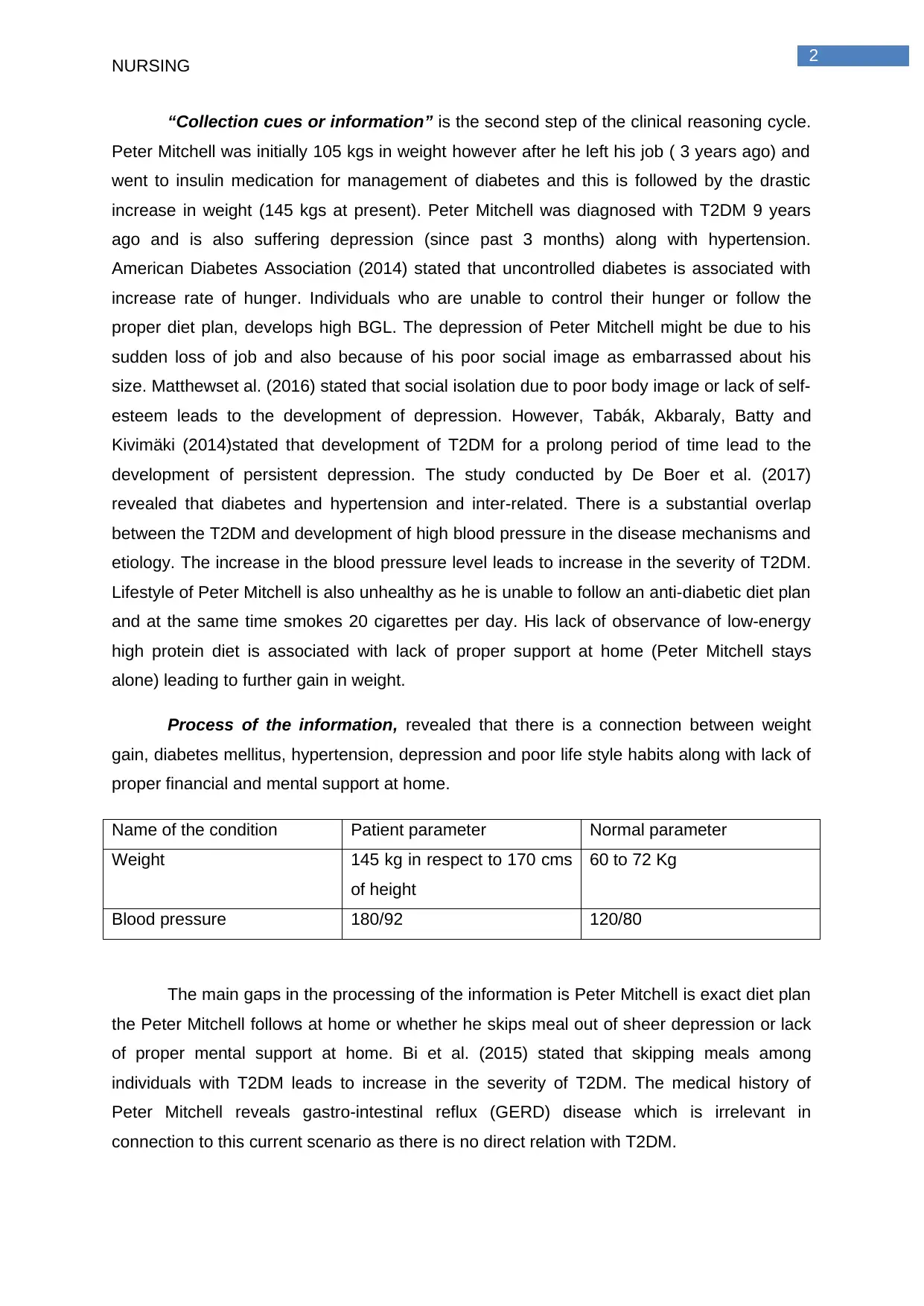
Process of the information, revealed that there is a connection between weight
gain, diabetes mellitus, hypertension, depression and poor life style habits along with lack of
proper financial and mental support at home.
Name of the condition Patient parameter Normal parameter
Weight 145 kg in respect to 170 cms
of height
60 to 72 Kg
Blood pressure 180/92 120/80
The main gaps in the processing of the information is Peter Mitchell is exact diet plan
the Peter Mitchell follows at home or whether he skips meal out of sheer depression or lack
of proper mental support at home. Bi et al. (2015) stated that skipping meals among
individuals with T2DM leads to increase in the severity of T2DM. The medical history of
Peter Mitchell reveals gastro-intestinal reflux (GERD) disease which is irrelevant in
connection to this current scenario as there is no direct relation with T2DM.
NURSING
“Collection cues or information” is the second step of the clinical reasoning cycle.
Peter Mitchell was initially 105 kgs in weight however after he left his job ( 3 years ago) and
went to insulin medication for management of diabetes and this is followed by the drastic
increase in weight (145 kgs at present). Peter Mitchell was diagnosed with T2DM 9 years
ago and is also suffering depression (since past 3 months) along with hypertension.
American Diabetes Association (2014) stated that uncontrolled diabetes is associated with
increase rate of hunger. Individuals who are unable to control their hunger or follow the
proper diet plan, develops high BGL. The depression of Peter Mitchell might be due to his
sudden loss of job and also because of his poor social image as embarrassed about his
size. Matthewset al. (2016) stated that social isolation due to poor body image or lack of self-
esteem leads to the development of depression. However, Tabák, Akbaraly, Batty and
Kivimäki (2014)stated that development of T2DM for a prolong period of time lead to the
development of persistent depression. The study conducted by De Boer et al. (2017)
revealed that diabetes and hypertension and inter-related. There is a substantial overlap
between the T2DM and development of high blood pressure in the disease mechanisms and
etiology. The increase in the blood pressure level leads to increase in the severity of T2DM.
Lifestyle of Peter Mitchell is also unhealthy as he is unable to follow an anti-diabetic diet plan
and at the same time smokes 20 cigarettes per day. His lack of observance of low-energy
high protein diet is associated with lack of proper support at home (Peter Mitchell stays
alone) leading to further gain in weight.
Process of the information, revealed that there is a connection between weight
gain, diabetes mellitus, hypertension, depression and poor life style habits along with lack of
proper financial and mental support at home.
Name of the condition Patient parameter Normal parameter
Weight 145 kg in respect to 170 cms
of height
60 to 72 Kg
Blood pressure 180/92 120/80
The main gaps in the processing of the information is Peter Mitchell is exact diet plan
the Peter Mitchell follows at home or whether he skips meal out of sheer depression or lack
of proper mental support at home. Bi et al. (2015) stated that skipping meals among
individuals with T2DM leads to increase in the severity of T2DM. The medical history of
Peter Mitchell reveals gastro-intestinal reflux (GERD) disease which is irrelevant in
connection to this current scenario as there is no direct relation with T2DM.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
NURSING
The identified problems are poor quality of life leading to poor diabetes
management, lack of proper self-awareness and depression arising out of social isolation.
In the section of the establishment of goals, fifth step of the clinical reasoning cycle.
The two main priorities of care will be effective management of diabetes Mellitus while
improving the quality of life and increase in the level of social participation.
It can be said that Peter is aware of his weight issues however is not willing to take
active initiative to fight against his weight issues through exercise and diet. However, he was
advised to follow light exercise taught by the physiotherapist. Thus Priorities of care will be
effective management of diabetes mellitus by improving the lifestyle through health
awareness This can be achieved through proper health education about the prognosis of
T2DM. Chrvala, Sherr and Lipman (2016) stated that disease education helps in effective
diabetes self-management. The action plan includes education must be given by a
community health nurse under the community healthcare setting. Education given under
settings of community health settings, under presence of similar peers, suffering from
identical healthcare complications, is found to promote significant level of disease
awareness (Chrvala, Sherr & Lipman, 2016). The disease education will also help Peter to
follow high protein low calorie diet. Peter Mitchell must be taught about the periodic
monitoring of the BGL based on the use of glucometer. This self-monitoring helps o track the
disease progression and simultaneous change in the dosage of insulin. For improving the
quality of life while managing diabetes, education and assistance must be given for smoking
cessation. Nicotine Replacement Therapy (NRT) can be prove to be effective to assisting
individuals to fight against withdrawal symptoms of smoking and thereby helping to quit
tobacco smoking (Baker et al., 2016). Decreasing in smoking, proper monitoring of BGL
along with inclination to self-management T2DM will help to reduce the severity of T2DM
along with improving the overall quality of life.
Second priority is social isolation due to poor body image. Peter also lives along after
his divorce and his wards rarely visit him. Social isolation along with lack of proper support of
the family members generate a sense of loneliness and depression contributing to significant
morbidity among the patients with T2DM. The main action plan will be centred on nursing
interventions to reduce level of Peter’s depression through increasing acceptance along with
awareness about self. Awareness of self can be achieved by giving a detailed insight who
we can effectively manage his weight along and thereby helping to increase self-confidence
(Chrvala, Sherr & Lipman, 2016). Peter can be advised to perform light physical exercise
reviewed by the physiotherapist for at-least 115 to 20 minutes per day. Such physical activity
can be done in groups of similar individuals like those who are suffering from diabetes along
NURSING
The identified problems are poor quality of life leading to poor diabetes
management, lack of proper self-awareness and depression arising out of social isolation.
In the section of the establishment of goals, fifth step of the clinical reasoning cycle.
The two main priorities of care will be effective management of diabetes Mellitus while
improving the quality of life and increase in the level of social participation.
It can be said that Peter is aware of his weight issues however is not willing to take
active initiative to fight against his weight issues through exercise and diet. However, he was
advised to follow light exercise taught by the physiotherapist. Thus Priorities of care will be
effective management of diabetes mellitus by improving the lifestyle through health
awareness This can be achieved through proper health education about the prognosis of
T2DM. Chrvala, Sherr and Lipman (2016) stated that disease education helps in effective
diabetes self-management. The action plan includes education must be given by a
community health nurse under the community healthcare setting. Education given under
settings of community health settings, under presence of similar peers, suffering from
identical healthcare complications, is found to promote significant level of disease
awareness (Chrvala, Sherr & Lipman, 2016). The disease education will also help Peter to
follow high protein low calorie diet. Peter Mitchell must be taught about the periodic
monitoring of the BGL based on the use of glucometer. This self-monitoring helps o track the
disease progression and simultaneous change in the dosage of insulin. For improving the
quality of life while managing diabetes, education and assistance must be given for smoking
cessation. Nicotine Replacement Therapy (NRT) can be prove to be effective to assisting
individuals to fight against withdrawal symptoms of smoking and thereby helping to quit
tobacco smoking (Baker et al., 2016). Decreasing in smoking, proper monitoring of BGL
along with inclination to self-management T2DM will help to reduce the severity of T2DM
along with improving the overall quality of life.
Second priority is social isolation due to poor body image. Peter also lives along after
his divorce and his wards rarely visit him. Social isolation along with lack of proper support of
the family members generate a sense of loneliness and depression contributing to significant
morbidity among the patients with T2DM. The main action plan will be centred on nursing
interventions to reduce level of Peter’s depression through increasing acceptance along with
awareness about self. Awareness of self can be achieved by giving a detailed insight who
we can effectively manage his weight along and thereby helping to increase self-confidence
(Chrvala, Sherr & Lipman, 2016). Peter can be advised to perform light physical exercise
reviewed by the physiotherapist for at-least 115 to 20 minutes per day. Such physical activity
can be done in groups of similar individuals like those who are suffering from diabetes along
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
NURSING
with weight issues. This will help to bring inner motivation. During physical exercise class,.
The mental (psychological) and physical health condition will be reviewed by mental health
professionals and primary care providers simultaneously. This type of care is known as
collaborative care. Staying within the same group of people who are also suffering from the
similar healthcare condition will help to increase the social participation while fight against
depression occurred due to diseased condition (Greenhalgh, Jackson, Shaw and Janamian
2016). Daily practice of mild to moderate physical exercise will help to reduce the
postprandial glucose secretion and thus reducing BGL (Wiklund, 2016).
Evaluation of the outcomes and reflection on the process of new learning is the
last two stage of the clinical reasoning cycle. The evaluation of the outcome will be based in
reduction in the blood sugar levels (BGL) of Peter Mitchell along with reduction in the body
weight and reduction in the tendency of smoking. Peter will be asked to fix appointments
with the local healthcare clinic once a week in order to monitor the vital signs to evaluate the
outcome of the care. The evaluation of the depression of Peter Mitchell will be done my
mental health nursing professionals. Mental health counselling and face-to-face interaction
will help to ascertain the degree of depression through which the Peter Mitchell is passing
through. The level of depression of Peter Mitchell can also be measured by monitoring the
degree of social participation. Increase in participation of the community activities can also
act as the marker to identify Peter Mitchell’s increased level of social participation and
recovery from depression due to poor body image (Matthews et al., 2016).
The analysis of the case study helped me to identify that physical health is directly
associated with the mental health of the patients. Disequilibrium in physical health leads to
negative mental health consequences. The case study analysis also helped me to
understand that health education along with disease awareness can be used to promote
effective self-management of the disease.
NURSING
with weight issues. This will help to bring inner motivation. During physical exercise class,.
The mental (psychological) and physical health condition will be reviewed by mental health
professionals and primary care providers simultaneously. This type of care is known as
collaborative care. Staying within the same group of people who are also suffering from the
similar healthcare condition will help to increase the social participation while fight against
depression occurred due to diseased condition (Greenhalgh, Jackson, Shaw and Janamian
2016). Daily practice of mild to moderate physical exercise will help to reduce the
postprandial glucose secretion and thus reducing BGL (Wiklund, 2016).
Evaluation of the outcomes and reflection on the process of new learning is the
last two stage of the clinical reasoning cycle. The evaluation of the outcome will be based in
reduction in the blood sugar levels (BGL) of Peter Mitchell along with reduction in the body
weight and reduction in the tendency of smoking. Peter will be asked to fix appointments
with the local healthcare clinic once a week in order to monitor the vital signs to evaluate the
outcome of the care. The evaluation of the depression of Peter Mitchell will be done my
mental health nursing professionals. Mental health counselling and face-to-face interaction
will help to ascertain the degree of depression through which the Peter Mitchell is passing
through. The level of depression of Peter Mitchell can also be measured by monitoring the
degree of social participation. Increase in participation of the community activities can also
act as the marker to identify Peter Mitchell’s increased level of social participation and
recovery from depression due to poor body image (Matthews et al., 2016).
The analysis of the case study helped me to identify that physical health is directly
associated with the mental health of the patients. Disequilibrium in physical health leads to
negative mental health consequences. The case study analysis also helped me to
understand that health education along with disease awareness can be used to promote
effective self-management of the disease.
5
NURSING
References
Abdelaal, M., le Roux, C. W., & Docherty, N. G. (2017). Morbidity and mortality associated
with obesity. Annals of translational medicine, 5(7). doi: 10.21037/atm.2017.03.107
Alfaro-LeFevre, R. (2015). Critical thinking, clinical reasoning, and clinical judgment: A
practical approach. Elsevier Health Sciences.
American Diabetes Association. (2014). Diagnosis and classification of diabetes
mellitus. Diabetes care, 37(Supplement 1), S81-S90.https://doi.org/10.2337/dc14-S081
Baker, T. B., Piper, M. E., Stein, J. H., Smith, S. S., Bolt, D. M., Fraser, D. L., & Fiore, M. C.
(2016). Effects of nicotine patch vs varenicline vs combination nicotine replacement
therapy on smoking cessation at 26 weeks: a randomized clinical trial. Jama, 315(4),
371-379. doi:10.1001/jama.2015.19284
Bi, H., Gan, Y., Yang, C., Chen, Y., Tong, X., & Lu, Z. (2015). Breakfast skipping and the risk
of type 2 diabetes: a meta-analysis of observational studies. Public health
nutrition, 18(16), 3013-3019.
Brunisholz, K. D., Briot, P., Hamilton, S., Joy, E. A., Lomax, M., Barton, N., ... & Cannon, W.
(2014). Diabetes self-management education improves quality of care and clinical
outcomes determined by a diabetes bundle measure. Journal of multidisciplinary
healthcare, 7, 533.https://doi.org/10.1016/j.pec.2015.11.003
Chrvala, C. A., Sherr, D., & Lipman, R. D. (2016). Diabetes self-management education for
adults with type 2 diabetes mellitus: a systematic review of the effect on glycemic
control. Patient education and counseling, 99(6), 926-943.
https://doi.org/10.1016/j.pec.2015.11.003
Cruz, S., Carvalho, A. L., & Sousa, P. (2014). Clinical supervision: priority strategy to a
better health. Procedia-Social and Behavioral Sciences, 112, 97-101.
https://doi.org/10.1016/j.sbspro.2014.01.1143
De Boer, I. H., Bangalore, S., Benetos, A., Davis, A. M., Michos, E. D., Muntner, P., ... &
Bakris, G. (2017). Diabetes and hypertension: a position statement by the American
Diabetes Association. Diabetes Care, 40(9), 1273-1284. https://doi.org/10.2337/dci17-
0026
NURSING
References
Abdelaal, M., le Roux, C. W., & Docherty, N. G. (2017). Morbidity and mortality associated
with obesity. Annals of translational medicine, 5(7). doi: 10.21037/atm.2017.03.107
Alfaro-LeFevre, R. (2015). Critical thinking, clinical reasoning, and clinical judgment: A
practical approach. Elsevier Health Sciences.
American Diabetes Association. (2014). Diagnosis and classification of diabetes
mellitus. Diabetes care, 37(Supplement 1), S81-S90.https://doi.org/10.2337/dc14-S081
Baker, T. B., Piper, M. E., Stein, J. H., Smith, S. S., Bolt, D. M., Fraser, D. L., & Fiore, M. C.
(2016). Effects of nicotine patch vs varenicline vs combination nicotine replacement
therapy on smoking cessation at 26 weeks: a randomized clinical trial. Jama, 315(4),
371-379. doi:10.1001/jama.2015.19284
Bi, H., Gan, Y., Yang, C., Chen, Y., Tong, X., & Lu, Z. (2015). Breakfast skipping and the risk
of type 2 diabetes: a meta-analysis of observational studies. Public health
nutrition, 18(16), 3013-3019.
Brunisholz, K. D., Briot, P., Hamilton, S., Joy, E. A., Lomax, M., Barton, N., ... & Cannon, W.
(2014). Diabetes self-management education improves quality of care and clinical
outcomes determined by a diabetes bundle measure. Journal of multidisciplinary
healthcare, 7, 533.https://doi.org/10.1016/j.pec.2015.11.003
Chrvala, C. A., Sherr, D., & Lipman, R. D. (2016). Diabetes self-management education for
adults with type 2 diabetes mellitus: a systematic review of the effect on glycemic
control. Patient education and counseling, 99(6), 926-943.
https://doi.org/10.1016/j.pec.2015.11.003
Cruz, S., Carvalho, A. L., & Sousa, P. (2014). Clinical supervision: priority strategy to a
better health. Procedia-Social and Behavioral Sciences, 112, 97-101.
https://doi.org/10.1016/j.sbspro.2014.01.1143
De Boer, I. H., Bangalore, S., Benetos, A., Davis, A. M., Michos, E. D., Muntner, P., ... &
Bakris, G. (2017). Diabetes and hypertension: a position statement by the American
Diabetes Association. Diabetes Care, 40(9), 1273-1284. https://doi.org/10.2337/dci17-
0026
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
NURSING
Greenhalgh, T., Jackson, C., Shaw, S., & Janamian, T. (2016). Achieving research impact
through co‐creation in community‐based health services: literature review and case
study. The Milbank Quarterly, 94(2), 392-429. https://doi.org/10.1111/1468-0009.12197
Lavie, C. J., McAuley, P. A., Church, T. S., Milani, R. V., & Blair, S. N. (2014). Obesity and
cardiovascular diseases: implications regarding fitness, fatness, and severity in the
obesity paradox. Journal of the American College of Cardiology, 63(14), 1345-1354.
DOI: 10.1016/j.jacc.2014.01.022
Levett-Jones, T. (Ed.). (2017). Clinical reasoning: Learning to think like a nurse. Pearson
Australia.
Matthews, T., Danese, A., Wertz, J., Odgers, C. L., Ambler, A., Moffitt, T. E., & Arseneault,
L. (2016). Social isolation, loneliness and depression in young adulthood: a
behavioural genetic analysis. Social psychiatry and psychiatric epidemiology, 51(3),
339-348. https://doi.org/10.1007/s00127-016-1178-7
Pan, A., Wang, Y., Talaei, M., Hu, F. B., & Wu, T. (2015). Relation of active, passive, and
quitting smoking with incident type 2 diabetes: a systematic review and meta-
analysis. The lancet Diabetes & endocrinology, 3(12), 958-967.
https://doi.org/10.1016/S2213-8587(15)00316-2
Tabák, A. G., Akbaraly, T. N., Batty, G. D., & Kivimäki, M. (2014). Depression and type 2
diabetes: a causal association?. The lancet Diabetes & endocrinology, 2(3), 236-245.
https://doi.org/10.1016/S2213-8587(13)70139-6
Wiklund, P. (2016). The role of physical activity and exercise in obesity and weight
management: Time for critical appraisal. Journal of Sport and Health Science, 5(2),
151-154. https://doi.org/10.1016/j.jshs.2016.04.001
NURSING
Greenhalgh, T., Jackson, C., Shaw, S., & Janamian, T. (2016). Achieving research impact
through co‐creation in community‐based health services: literature review and case
study. The Milbank Quarterly, 94(2), 392-429. https://doi.org/10.1111/1468-0009.12197
Lavie, C. J., McAuley, P. A., Church, T. S., Milani, R. V., & Blair, S. N. (2014). Obesity and
cardiovascular diseases: implications regarding fitness, fatness, and severity in the
obesity paradox. Journal of the American College of Cardiology, 63(14), 1345-1354.
DOI: 10.1016/j.jacc.2014.01.022
Levett-Jones, T. (Ed.). (2017). Clinical reasoning: Learning to think like a nurse. Pearson
Australia.
Matthews, T., Danese, A., Wertz, J., Odgers, C. L., Ambler, A., Moffitt, T. E., & Arseneault,
L. (2016). Social isolation, loneliness and depression in young adulthood: a
behavioural genetic analysis. Social psychiatry and psychiatric epidemiology, 51(3),
339-348. https://doi.org/10.1007/s00127-016-1178-7
Pan, A., Wang, Y., Talaei, M., Hu, F. B., & Wu, T. (2015). Relation of active, passive, and
quitting smoking with incident type 2 diabetes: a systematic review and meta-
analysis. The lancet Diabetes & endocrinology, 3(12), 958-967.
https://doi.org/10.1016/S2213-8587(15)00316-2
Tabák, A. G., Akbaraly, T. N., Batty, G. D., & Kivimäki, M. (2014). Depression and type 2
diabetes: a causal association?. The lancet Diabetes & endocrinology, 2(3), 236-245.
https://doi.org/10.1016/S2213-8587(13)70139-6
Wiklund, P. (2016). The role of physical activity and exercise in obesity and weight
management: Time for critical appraisal. Journal of Sport and Health Science, 5(2),
151-154. https://doi.org/10.1016/j.jshs.2016.04.001
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





