Patient Assessment and Nursing Care
VerifiedAdded on 2021/04/24
|21
|4840
|44
AI Summary
This assignment involves assessing a palliative care patient, Mrs. X, who presents with impaired mobility, decreased appetite, and severe pain. The nurse must document her physiological changes, including tachypnoea, and collaborate with healthcare professionals to develop an effective plan of care. Key nursing actions include monitoring vital signs, administering oxygen, and providing reassurance through communication. The assignment emphasizes the importance of proper documentation, patient mobility assistance, and pain medication administration.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: NURSING ASSIGNMENT
Questions and Answers for Case Studies
Name of the Student
Name of the University
Author Note
Questions and Answers for Case Studies
Name of the Student
Name of the University
Author Note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1NURSING ASSIGNMENT
Module 1
Q.1 Order of tasks on the basis of priority:
The noble profession of nursing plays different roles in the lives of all nurses. Nurses are
entrusted with a variety of tasks, such as, acting as a care provider, advocating for patient rights,
liaisoning, providing education, and many other responsibilities. Furthermore, nurses also play a
crucial role by acting as leaders in interdisciplinary medical teams. The health outcomes and
satisfaction of patients are greatly dependent on the role and clinical expertise of a nurse. In
addition, nurses display excellent clinical judgment skills that are governed by their
communication capabilities and delegation skills (Huber, 2014). In the given context, the
primary objective should be to prioritise addressing needs of the elderly patient, who has been
found unconscious. This situation should be considered a medical emergency, which if not
treated immediately, might result in potentially harmful and fatal health consequences. Owing to
the fact that there are a plethora of issues in this context, I would focus on delegating the nursing
staff according to their expertise and scope of clinical practice. The NMBA standards of practice
(standard 6) illustrates the importance of delivering high quality, and responsive healthcare
services to all patients, which in turn is facilitated by effective delegation of enrolled nurses and
other staff according to their scope of practice and clinical roles (NMBA, 2018). In a similar
way, I would request the concerned NUM, also a registered nurse to collaborate with us, in this
emergency situation.
I would also seek help from the surgical consultant until appropriate services are made
available by the emergency team. A patient’s health outcomes are directly influenced by
medication administration. During our nursing course, we were taught the importance of
Module 1
Q.1 Order of tasks on the basis of priority:
The noble profession of nursing plays different roles in the lives of all nurses. Nurses are
entrusted with a variety of tasks, such as, acting as a care provider, advocating for patient rights,
liaisoning, providing education, and many other responsibilities. Furthermore, nurses also play a
crucial role by acting as leaders in interdisciplinary medical teams. The health outcomes and
satisfaction of patients are greatly dependent on the role and clinical expertise of a nurse. In
addition, nurses display excellent clinical judgment skills that are governed by their
communication capabilities and delegation skills (Huber, 2014). In the given context, the
primary objective should be to prioritise addressing needs of the elderly patient, who has been
found unconscious. This situation should be considered a medical emergency, which if not
treated immediately, might result in potentially harmful and fatal health consequences. Owing to
the fact that there are a plethora of issues in this context, I would focus on delegating the nursing
staff according to their expertise and scope of clinical practice. The NMBA standards of practice
(standard 6) illustrates the importance of delivering high quality, and responsive healthcare
services to all patients, which in turn is facilitated by effective delegation of enrolled nurses and
other staff according to their scope of practice and clinical roles (NMBA, 2018). In a similar
way, I would request the concerned NUM, also a registered nurse to collaborate with us, in this
emergency situation.
I would also seek help from the surgical consultant until appropriate services are made
available by the emergency team. A patient’s health outcomes are directly influenced by
medication administration. During our nursing course, we were taught the importance of
2NURSING ASSIGNMENT
checking and confirming the 7 rights related to medication administration by nurses, before
giving any medicine to a patient. We were taught that ‘right time’ of administering a medicine is
imperative to improved health outcomes of a patient, and that a registered nurse is bound to
adhere to these guidelines. Thus, I would attend the patient Mrs. Chew, and would reposition the
cannula placement. I would also administer her necessary fluids upon arrival of the emergency
team, following which the NUM would be requested to stay. Although, it is an essential duty of
all nurses to document and record the exact time of antibiotic and other therapeutic
administration, I would try administering the intravenous (IV) antibiotic to the patient, even if
there is a delay in its administration by 30-60 minutes.
Recording accurate time of medication administration helps in preventing adverse health
effects due to overdose due to the fact that there should be considerable time between
administration of the first and second antibiotic (Roughead, Semple & Rosenfeld, 2013). I would
also request the concerned enrolled nurse to provide proper medications to the patient Mr.
Esposito, before sending him off for the medical procedure. She would also be requested to
attend the visitor who has come to see Mr. Smith. Furthermore, I would also place a request in
front of the AIN (Assistant in Nursing) for attending the visitor. This would be followed by
measuring the vital signs of the patient and subsequently reporting the readings to the EN or the
physician, upon encountering abnormalities in the ranges. Enrolled nurses also have the expertise
of measuring vital signs of a patient (NSW Health, 2010). In addition, the ward clerk would also
be requested to assist in solving the problem of blocked toilet for the staff. The clerk would also
be asked to reassure the patient Mr. Smith, and his family members, regarding his recovery. This
would be followed by a discussion of the error that occurred due to a delay in administering the
antibiotic, with the surgeon because it does not show any adverse effects on the patient’s health
checking and confirming the 7 rights related to medication administration by nurses, before
giving any medicine to a patient. We were taught that ‘right time’ of administering a medicine is
imperative to improved health outcomes of a patient, and that a registered nurse is bound to
adhere to these guidelines. Thus, I would attend the patient Mrs. Chew, and would reposition the
cannula placement. I would also administer her necessary fluids upon arrival of the emergency
team, following which the NUM would be requested to stay. Although, it is an essential duty of
all nurses to document and record the exact time of antibiotic and other therapeutic
administration, I would try administering the intravenous (IV) antibiotic to the patient, even if
there is a delay in its administration by 30-60 minutes.
Recording accurate time of medication administration helps in preventing adverse health
effects due to overdose due to the fact that there should be considerable time between
administration of the first and second antibiotic (Roughead, Semple & Rosenfeld, 2013). I would
also request the concerned enrolled nurse to provide proper medications to the patient Mr.
Esposito, before sending him off for the medical procedure. She would also be requested to
attend the visitor who has come to see Mr. Smith. Furthermore, I would also place a request in
front of the AIN (Assistant in Nursing) for attending the visitor. This would be followed by
measuring the vital signs of the patient and subsequently reporting the readings to the EN or the
physician, upon encountering abnormalities in the ranges. Enrolled nurses also have the expertise
of measuring vital signs of a patient (NSW Health, 2010). In addition, the ward clerk would also
be requested to assist in solving the problem of blocked toilet for the staff. The clerk would also
be asked to reassure the patient Mr. Smith, and his family members, regarding his recovery. This
would be followed by a discussion of the error that occurred due to a delay in administering the
antibiotic, with the surgeon because it does not show any adverse effects on the patient’s health

3NURSING ASSIGNMENT
at present. Situations as such are often encountered in the nursing profession due to the fact that
health of an individual is a dynamic state of the wellbeing and often makes it difficult to
anticipate beforehand. Thus, it is essential for all nurses to have an idea that such emergency
situations might arise in a healthcare setting. Therefore, it is imperative for all nurses to have a
sound understanding of the rights related to workforce delegation, task prioritization, scope of
practice, critical thinking, effective communication, and clinical judgement, with the aim of
improving the overall health, wellbeing and satisfaction of all patients.
at present. Situations as such are often encountered in the nursing profession due to the fact that
health of an individual is a dynamic state of the wellbeing and often makes it difficult to
anticipate beforehand. Thus, it is essential for all nurses to have an idea that such emergency
situations might arise in a healthcare setting. Therefore, it is imperative for all nurses to have a
sound understanding of the rights related to workforce delegation, task prioritization, scope of
practice, critical thinking, effective communication, and clinical judgement, with the aim of
improving the overall health, wellbeing and satisfaction of all patients.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4NURSING ASSIGNMENT
References
Huber, D. (2014). Leadership & nursing care management (5th ed.). St. Louis:
Elsevier/Saunders. Retrieved from
http://unilincalmanew.hosted.exlibrisgroup.com/ACU:ACU_ALL:alma71482433800023
51
NSW Health. (2010). Assistants in Nursing working in the acute care environment. Retrieved
from http://www.health.nsw.gov.au/workforce/Publications/ain-acute-care.pdf
Nursingmidwiferyboard.gov.au. (2018). Nursing and Midwifery Board of Australia - Registered
nurse standards for practice. Retrieved 3 March 2018, from
http://www.nursingmidwiferyboard.gov.au/Codes-Guidelines-Statements/Professional-
standards/registered-nurse-standards-for-practice.aspx
Roughead. L., Semple. S., & Rosenfeld, E. (2013). Literature Review: Medication Safety in
Australia. Retrieved from
https://safetyandquality.gov.au/wp-content/uploads/2014/02/Literature-Review-
Medication-Safety-in-Australia-2013.pdf
References
Huber, D. (2014). Leadership & nursing care management (5th ed.). St. Louis:
Elsevier/Saunders. Retrieved from
http://unilincalmanew.hosted.exlibrisgroup.com/ACU:ACU_ALL:alma71482433800023
51
NSW Health. (2010). Assistants in Nursing working in the acute care environment. Retrieved
from http://www.health.nsw.gov.au/workforce/Publications/ain-acute-care.pdf
Nursingmidwiferyboard.gov.au. (2018). Nursing and Midwifery Board of Australia - Registered
nurse standards for practice. Retrieved 3 March 2018, from
http://www.nursingmidwiferyboard.gov.au/Codes-Guidelines-Statements/Professional-
standards/registered-nurse-standards-for-practice.aspx
Roughead. L., Semple. S., & Rosenfeld, E. (2013). Literature Review: Medication Safety in
Australia. Retrieved from
https://safetyandquality.gov.au/wp-content/uploads/2014/02/Literature-Review-
Medication-Safety-in-Australia-2013.pdf
5NURSING ASSIGNMENT
Module2
Identify factors that determine which healthcare professionals are required to be involved
in a health care team?
Major factors are associated with disease severity. Motor Neuron Diseases (MND) are
most commonly found to affect the ability of a person to talk, walk, breath or swallow food.
Therefore, it is essential to seek help from a respiratory specialist for addressing the respiratory
distress, the patient is suffering from. An occupational therapist and physiotherapist will be
called for assisting the patient in improving the motor skills, thereby facilitating mobility. Social
workers and case managers will also play a crucial role in managing the financial and social
issues faced by the patient. Furthermore, a speech pathologist will prove effective in treating the
impairment associated with language comprehension and swallowing food. The neurological
abnormalities will be treated by a neurologist and an MND nurse specialist.
Who should lead the health care team?
The MND nurse specialist shall be held responsible for leading the healthcare team due to
the fact that she would be responsible for forming a liaison with other members who are a part of
the multidisciplinary team, thereby facilitating solving of the medical issues that have been
identified in this context.
Who is the most important member of the health care team?
All members of a healthcare team are equally important, as they are responsible for
maintaining safety and optimal health outcomes for their clients. However, a patient is the most
essential member of the team because the experiences, preferences and demands of a patient
assist the healthcare professionals to deliver appropriate healthcare services. Moreover, it is the
Module2
Identify factors that determine which healthcare professionals are required to be involved
in a health care team?
Major factors are associated with disease severity. Motor Neuron Diseases (MND) are
most commonly found to affect the ability of a person to talk, walk, breath or swallow food.
Therefore, it is essential to seek help from a respiratory specialist for addressing the respiratory
distress, the patient is suffering from. An occupational therapist and physiotherapist will be
called for assisting the patient in improving the motor skills, thereby facilitating mobility. Social
workers and case managers will also play a crucial role in managing the financial and social
issues faced by the patient. Furthermore, a speech pathologist will prove effective in treating the
impairment associated with language comprehension and swallowing food. The neurological
abnormalities will be treated by a neurologist and an MND nurse specialist.
Who should lead the health care team?
The MND nurse specialist shall be held responsible for leading the healthcare team due to
the fact that she would be responsible for forming a liaison with other members who are a part of
the multidisciplinary team, thereby facilitating solving of the medical issues that have been
identified in this context.
Who is the most important member of the health care team?
All members of a healthcare team are equally important, as they are responsible for
maintaining safety and optimal health outcomes for their clients. However, a patient is the most
essential member of the team because the experiences, preferences and demands of a patient
assist the healthcare professionals to deliver appropriate healthcare services. Moreover, it is the
6NURSING ASSIGNMENT
primary right of all patients to remain involved in their treatment. This concept of respecting the
autonomy of a patient is therefore responsible for challenging the paternalistic duties of a
physician (Carman et al., 2013).
ACTIVITY 2: CASE STUDY 3
Robert Hughes is a 52 year old male who was injured in a bicycle accident two months
ago where he suffered fractures to his (R) tibia/fibula and (R) radius. Robert is intellectually
impaired and was living with his elderly mother until the accident. Robert has been known to
engage in verbally aggressive outbursts towards staff and other patients. His mother who is now
75 years of age feels she can no longer look after Robert. You are the NUM of the rehabilitation
unit that is admitting Robert for his ongoing rehabilitation. You are required to gather together a
health care team to determine immediate and long term care options for Robert.
What are the key issues in this situation?
One major issue in this context refers to the incapability of the patient Robert’s mother,
the primary carer, aged 75 years, to care for her son. Old age of his mother does not permit her to
provide appropriate healthcare services to her son, thereby resulting in her impairment to
improve Robert’s optimal health outcome. Another issue is associated with Robert’s intellectual
flaws that restrict him from taking self-care. This makes him dependent on his mother. Socio-
economic factors might also have an influence in this context. This can be attributed to the fact
that although Robert is 52 years old, he does not earn a living. This makes him being looked
down upon by members of his community and society. Moreover, his mother also demonstrates a
failure to control his unruly behaviour, as evident by his bicycle accident and verbally aggressive
primary right of all patients to remain involved in their treatment. This concept of respecting the
autonomy of a patient is therefore responsible for challenging the paternalistic duties of a
physician (Carman et al., 2013).
ACTIVITY 2: CASE STUDY 3
Robert Hughes is a 52 year old male who was injured in a bicycle accident two months
ago where he suffered fractures to his (R) tibia/fibula and (R) radius. Robert is intellectually
impaired and was living with his elderly mother until the accident. Robert has been known to
engage in verbally aggressive outbursts towards staff and other patients. His mother who is now
75 years of age feels she can no longer look after Robert. You are the NUM of the rehabilitation
unit that is admitting Robert for his ongoing rehabilitation. You are required to gather together a
health care team to determine immediate and long term care options for Robert.
What are the key issues in this situation?
One major issue in this context refers to the incapability of the patient Robert’s mother,
the primary carer, aged 75 years, to care for her son. Old age of his mother does not permit her to
provide appropriate healthcare services to her son, thereby resulting in her impairment to
improve Robert’s optimal health outcome. Another issue is associated with Robert’s intellectual
flaws that restrict him from taking self-care. This makes him dependent on his mother. Socio-
economic factors might also have an influence in this context. This can be attributed to the fact
that although Robert is 52 years old, he does not earn a living. This makes him being looked
down upon by members of his community and society. Moreover, his mother also demonstrates a
failure to control his unruly behaviour, as evident by his bicycle accident and verbally aggressive
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7NURSING ASSIGNMENT
behavior towards the nursing staff and co-patients. Another issue could be poor literacy about
role of the community support system in providing help, as demonstrated by his mother.
Who would be included in the health care team and what role would they play?
A clinical psychologist or a neurologist will be included in the multidisciplinary team for
managing the neurological abnormalities that result in intellectual impairment in the patient. An
orthopaedic surgeon will also play an essential role in addressing the physical problems that are
presented by Robert, following his accident. This surgeon will be able to collaborate with the
pain management team, in treating the fracture and associated pain. Moreover, a physiotherapist
will also play a crucial role in making him show compliance to exercises that would improve his
mobility, muscle and bone strength. An occupational therapist might also be included in the team
with the aim of providing necessary equipments that would assist Robert to perform daily
activities, all by himself. Similarly, a nurse specialist having expertise in treating intellectual
disabilities can also be asked to adorn the role of an educator, and advocate, in addition to
liaising between all members of the interdisciplinary team. The nurse will also be imperative in
conducting a holistic assessment of the patient that will include a thorough measurement of his
bio-psychosocial aspects.
A case manager and social worker will be able to provide assistance to Robert, with
regards to better living amenities, and an appropriate physical, psychological and medical
environment. This in turn will relive his mother of her responsibilities, and of the fact that Robert
might get hurt in a new environment. Furthermore, a vocational trainer or recreational therapist
can also be contacted for arranging music or art classes that would engage Robert in an activity
of his interest (Clare et al., 2017). Depending on his symptoms, assistance can also be taken from
an optometrist or a speech pathologist (Carmeli & Imam, 2014).
behavior towards the nursing staff and co-patients. Another issue could be poor literacy about
role of the community support system in providing help, as demonstrated by his mother.
Who would be included in the health care team and what role would they play?
A clinical psychologist or a neurologist will be included in the multidisciplinary team for
managing the neurological abnormalities that result in intellectual impairment in the patient. An
orthopaedic surgeon will also play an essential role in addressing the physical problems that are
presented by Robert, following his accident. This surgeon will be able to collaborate with the
pain management team, in treating the fracture and associated pain. Moreover, a physiotherapist
will also play a crucial role in making him show compliance to exercises that would improve his
mobility, muscle and bone strength. An occupational therapist might also be included in the team
with the aim of providing necessary equipments that would assist Robert to perform daily
activities, all by himself. Similarly, a nurse specialist having expertise in treating intellectual
disabilities can also be asked to adorn the role of an educator, and advocate, in addition to
liaising between all members of the interdisciplinary team. The nurse will also be imperative in
conducting a holistic assessment of the patient that will include a thorough measurement of his
bio-psychosocial aspects.
A case manager and social worker will be able to provide assistance to Robert, with
regards to better living amenities, and an appropriate physical, psychological and medical
environment. This in turn will relive his mother of her responsibilities, and of the fact that Robert
might get hurt in a new environment. Furthermore, a vocational trainer or recreational therapist
can also be contacted for arranging music or art classes that would engage Robert in an activity
of his interest (Clare et al., 2017). Depending on his symptoms, assistance can also be taken from
an optometrist or a speech pathologist (Carmeli & Imam, 2014).
8NURSING ASSIGNMENT
References
Carman, K. L., Dardess, P., Maurer, M., Sofaer, S., Adams, K., Bechtel, C., & Sweeney, J.
(2013). Patient and family engagement: a framework for understanding the elements and
developing interventions and policies. Health Affairs, 32(2), 223-231.
https://doi.org/10.1377/hlthaff.2012.1133
Carmeli, E., & Imam, B. (2014). Health promotion and disease prevention strategies in older
adults with intellectual and developmental disabilities. Frontiers in public health, 2, 31.
https://doi.org/10.3389/fpubh.2014.00031
Clare, I. C. H., Madden, E. M., Holland, A. J., Farrington, C. J. T., Whitson, S., Broughton, S., ...
& Wagner, A. P. (2017). ‘What vision?’: experiences of Team members in a community
service for adults with intellectual disabilities. Journal of Intellectual Disability
Research, 61(3), 197-209. DOI: 10.1111/jir.12312
References
Carman, K. L., Dardess, P., Maurer, M., Sofaer, S., Adams, K., Bechtel, C., & Sweeney, J.
(2013). Patient and family engagement: a framework for understanding the elements and
developing interventions and policies. Health Affairs, 32(2), 223-231.
https://doi.org/10.1377/hlthaff.2012.1133
Carmeli, E., & Imam, B. (2014). Health promotion and disease prevention strategies in older
adults with intellectual and developmental disabilities. Frontiers in public health, 2, 31.
https://doi.org/10.3389/fpubh.2014.00031
Clare, I. C. H., Madden, E. M., Holland, A. J., Farrington, C. J. T., Whitson, S., Broughton, S., ...
& Wagner, A. P. (2017). ‘What vision?’: experiences of Team members in a community
service for adults with intellectual disabilities. Journal of Intellectual Disability
Research, 61(3), 197-209. DOI: 10.1111/jir.12312
9NURSING ASSIGNMENT
MODULE 3:
You are working on the morning shift on the ward, and receive a patient from ED. The
ED nurse provides you with the following handover, using the ISOBAR format. Further
information about the ISOBAR format can be found on page 7 of this module. Please click on
the handover link in LEO within Module 3 section, titled: ‘Module 3 Activity 2 Verbal
Handover’. Listen to this recording, and then please answer the following:
What further questions will you need to ask the nurse?
The handover in this context covers all essential aspects of the ISOBAR framework.
Hence, it can be considered satisfactory. However, there are few details missing in the handover.
I would like to ask few questions related to measurements of the patient’s vital signs for
determining presence of any potentially threatening infections in the body. An analysis of the
responses to the questions will help me evaluate presence of tachycardia, hyperthermia,
tachypnoea, hypertension, and low oxygen saturation. Presence of pneumonia is confirmed by
the current handover. Moreover, I would also question on the medications that are currently
being administered to the patient and would try to find out previous history of allergies or
surgeries. Furthermore, positive diagnosis for pneumonia would also require maintaining
adequate droplet precaution. I would also question the nurse on symptoms of weight loss and
abdominal pain.
List specifically what further assessments you would complete when the patient arrives
onto the ward 3.
On arrival of the patient to the ward, I would perform a comprehensive assessment of the
physiological condition. My assessment would be based on a systematic examination from head
MODULE 3:
You are working on the morning shift on the ward, and receive a patient from ED. The
ED nurse provides you with the following handover, using the ISOBAR format. Further
information about the ISOBAR format can be found on page 7 of this module. Please click on
the handover link in LEO within Module 3 section, titled: ‘Module 3 Activity 2 Verbal
Handover’. Listen to this recording, and then please answer the following:
What further questions will you need to ask the nurse?
The handover in this context covers all essential aspects of the ISOBAR framework.
Hence, it can be considered satisfactory. However, there are few details missing in the handover.
I would like to ask few questions related to measurements of the patient’s vital signs for
determining presence of any potentially threatening infections in the body. An analysis of the
responses to the questions will help me evaluate presence of tachycardia, hyperthermia,
tachypnoea, hypertension, and low oxygen saturation. Presence of pneumonia is confirmed by
the current handover. Moreover, I would also question on the medications that are currently
being administered to the patient and would try to find out previous history of allergies or
surgeries. Furthermore, positive diagnosis for pneumonia would also require maintaining
adequate droplet precaution. I would also question the nurse on symptoms of weight loss and
abdominal pain.
List specifically what further assessments you would complete when the patient arrives
onto the ward 3.
On arrival of the patient to the ward, I would perform a comprehensive assessment of the
physiological condition. My assessment would be based on a systematic examination from head
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10NURSING ASSIGNMENT
to toe, such as, pain assessment, temperature sensation, CVS assessment which includes
measurement of vital sign, perfusion, and capillary refill. I would also determine whether the
patient demonstrates and accurate orientation to place time and person. This will be followed by
conduction of a detailed GI and respiratory assessment, with procedures, such as auscultation,
inspection, percussion and palpation. I would also assess his skin condition and evaluate
presence of pressure injuries, or sores. This will be followed by determining placement of the IV
cannula.
I would also evaluate conditions that require ambulation. Baseline measurements of the
patient would include checking his weight and BGL. I would also record the patient’s subjective
data that will provide information on presence of pneumonia like condition. This data would be
based on measurements related to swallowing difficulty, and persistent cough. This can be
attributed to the fact that since the patient is aged (92 years old), it can possibly result in
aspiration pneumonia. His recent hospitalization can also contribute to hospital acquired
pneumonia (Suarez & Ortega, 2011). Furthermore, I will record information related to his social
history such as the primary caregiver, his living conditions, current medications and previous
history of hypersensitivity. During a clinical placement, it is essential to select a patient who
presents symptoms that are off interest. Selecting a patient what difficulties faced while linking
clinical theory to nursing practice would be helpful. The clinical reasoning cycle worksheet,
present on the LEO page will be filled up for providing assistance in understanding the current
physiological conditions of the patient.
to toe, such as, pain assessment, temperature sensation, CVS assessment which includes
measurement of vital sign, perfusion, and capillary refill. I would also determine whether the
patient demonstrates and accurate orientation to place time and person. This will be followed by
conduction of a detailed GI and respiratory assessment, with procedures, such as auscultation,
inspection, percussion and palpation. I would also assess his skin condition and evaluate
presence of pressure injuries, or sores. This will be followed by determining placement of the IV
cannula.
I would also evaluate conditions that require ambulation. Baseline measurements of the
patient would include checking his weight and BGL. I would also record the patient’s subjective
data that will provide information on presence of pneumonia like condition. This data would be
based on measurements related to swallowing difficulty, and persistent cough. This can be
attributed to the fact that since the patient is aged (92 years old), it can possibly result in
aspiration pneumonia. His recent hospitalization can also contribute to hospital acquired
pneumonia (Suarez & Ortega, 2011). Furthermore, I will record information related to his social
history such as the primary caregiver, his living conditions, current medications and previous
history of hypersensitivity. During a clinical placement, it is essential to select a patient who
presents symptoms that are off interest. Selecting a patient what difficulties faced while linking
clinical theory to nursing practice would be helpful. The clinical reasoning cycle worksheet,
present on the LEO page will be filled up for providing assistance in understanding the current
physiological conditions of the patient.
11NURSING ASSIGNMENT
References
Suarez, M. & Ortega, S. (2011). Pneumonia. New York: Nova Science Publishers. Retrieved
from http://site.ebrary.com/lib/australiancathu/reader.action?docID=10686285
References
Suarez, M. & Ortega, S. (2011). Pneumonia. New York: Nova Science Publishers. Retrieved
from http://site.ebrary.com/lib/australiancathu/reader.action?docID=10686285
12NURSING ASSIGNMENT
MODULE 4:
You are a Registered Nurse on the afternoon shift on a short-stay (24 hours) surgical
ward. One other RN, an EN and three AINs are also on duty. The NUM is off sick and the other
RN is acting as NUM as well as taking a patient load. The ward is full: there are 22 patients, 14
of whom went to surgery in the morning, and 8 are going on your shift. Half of these a patients
have intravenous access and antibiotics at some time during your shift.
Using your knowledge and experience of various patient allocation models (e.g. total
patient care, team nursing and task allocation), outline how you would allocate the staff to
the patients. Include in your discussion your rationale for the model of allocation chosen
and the scope of practice of the various staff.
A plethora of models exist related to patient care and allocation such as, team nursing,
indivisible patient allocation, primary nursing, total patient care, and functional nursing.
However, there is lack of evidence regarding the model that is most effective in enhancing
patient health outcomes, through delivery of optimal health care services. Most research studies
have been found to establish the effectiveness of team nursing as the commonly preferred patient
allocation model (Fairbrother, Jones & Rivas, 2010; Dubois et al., 2013). Several factors, such
as, complexity of the current clinical situation, structure, and organizational policies, availability
of adequate funding, nursing scope of practice, skill mix, and an increase in demand of
experience of healthcare professionals play a major role in determining the allocation and care
model that should be applied while treating a patient (King, Long & Lisy, 2014). In the current
case scenario, I would implement team nursing model for treating the patient. This model will be
selected due to the fact that it focuses on management of the entire multidisciplinary team by a
MODULE 4:
You are a Registered Nurse on the afternoon shift on a short-stay (24 hours) surgical
ward. One other RN, an EN and three AINs are also on duty. The NUM is off sick and the other
RN is acting as NUM as well as taking a patient load. The ward is full: there are 22 patients, 14
of whom went to surgery in the morning, and 8 are going on your shift. Half of these a patients
have intravenous access and antibiotics at some time during your shift.
Using your knowledge and experience of various patient allocation models (e.g. total
patient care, team nursing and task allocation), outline how you would allocate the staff to
the patients. Include in your discussion your rationale for the model of allocation chosen
and the scope of practice of the various staff.
A plethora of models exist related to patient care and allocation such as, team nursing,
indivisible patient allocation, primary nursing, total patient care, and functional nursing.
However, there is lack of evidence regarding the model that is most effective in enhancing
patient health outcomes, through delivery of optimal health care services. Most research studies
have been found to establish the effectiveness of team nursing as the commonly preferred patient
allocation model (Fairbrother, Jones & Rivas, 2010; Dubois et al., 2013). Several factors, such
as, complexity of the current clinical situation, structure, and organizational policies, availability
of adequate funding, nursing scope of practice, skill mix, and an increase in demand of
experience of healthcare professionals play a major role in determining the allocation and care
model that should be applied while treating a patient (King, Long & Lisy, 2014). In the current
case scenario, I would implement team nursing model for treating the patient. This model will be
selected due to the fact that it focuses on management of the entire multidisciplinary team by a
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13NURSING ASSIGNMENT
registered nurse, who functions as a team leader. In such cases, there is enormous workload on
the nursing staff. Moreover, all healthcare professionals demonstrate differences in their clinical
competencies and level of nursing education, thereby collaborating together, with the primary
objective of improving health outcome of the patient. Furthermore, this model will also assist
nursing stuff in realizing their maximum potential, while delivering optimal health care services
to the patient (Tran, Johnson, Fernandez & Jones, 2010). Further benefits of the team nursing
model are associated with its potential in advancing and promoting role of RNs as effective care
coordinators and team leaders. However, it is crucial for the team leaders to display appropriate
delegation skills and interpersonal communication skills, in addition to adequate knowledge on
the scope of practice of their colleagues (Tran, Johnson, Fernandez & Jones, 2010).
According to Polis, Higgs, Manning, Netto and Fernandez (2017) the team nursing model
have been proved successful in improving optimal patient outcomes, enhancing patient safety,
and reducing adverse events such as death. Moreover, the model has also been effective in staff
retention and enhancing job satisfaction among healthcare professionals. It has also proved
beneficial in supervising staff with less experience and providing them adequate support. Thus,
this team nursing model is most commonly used in instances where there is an amalgamation of
wide variety of nursing skills. This can be elucidated by the fact that enrolled nurses display
different levels of nursing expertise, upon comparison with registered nurse, and AINs.
However, all of them are required to work in collaboration in healthcare settings while caring for
a patient (Ferguson & Cioffi, 2011). Therefore, I would follow this model and allocate AINs to
experience EN and RNs. The patient load will be divided accordingly, such as, 8 to myself and
the AIN with whom I form a partnership, 8 to another AIN in partnership with an EN, and 6 to
the partnership of an RN (working as NUM) and an AIN.
registered nurse, who functions as a team leader. In such cases, there is enormous workload on
the nursing staff. Moreover, all healthcare professionals demonstrate differences in their clinical
competencies and level of nursing education, thereby collaborating together, with the primary
objective of improving health outcome of the patient. Furthermore, this model will also assist
nursing stuff in realizing their maximum potential, while delivering optimal health care services
to the patient (Tran, Johnson, Fernandez & Jones, 2010). Further benefits of the team nursing
model are associated with its potential in advancing and promoting role of RNs as effective care
coordinators and team leaders. However, it is crucial for the team leaders to display appropriate
delegation skills and interpersonal communication skills, in addition to adequate knowledge on
the scope of practice of their colleagues (Tran, Johnson, Fernandez & Jones, 2010).
According to Polis, Higgs, Manning, Netto and Fernandez (2017) the team nursing model
have been proved successful in improving optimal patient outcomes, enhancing patient safety,
and reducing adverse events such as death. Moreover, the model has also been effective in staff
retention and enhancing job satisfaction among healthcare professionals. It has also proved
beneficial in supervising staff with less experience and providing them adequate support. Thus,
this team nursing model is most commonly used in instances where there is an amalgamation of
wide variety of nursing skills. This can be elucidated by the fact that enrolled nurses display
different levels of nursing expertise, upon comparison with registered nurse, and AINs.
However, all of them are required to work in collaboration in healthcare settings while caring for
a patient (Ferguson & Cioffi, 2011). Therefore, I would follow this model and allocate AINs to
experience EN and RNs. The patient load will be divided accordingly, such as, 8 to myself and
the AIN with whom I form a partnership, 8 to another AIN in partnership with an EN, and 6 to
the partnership of an RN (working as NUM) and an AIN.
14NURSING ASSIGNMENT
The registered nurse will work as NUM because she will be responsible for managing the
entire word as well. The NSW health standard state that AINs are entrusted with the
responsibility of performing simple clinical tasks related to measuring vital signs of patients
admitted in acute health care ward (NSW Health, 2010). Hence, I would request all the AINs to
measure vital signs of their corresponding patients. I would also presume that the EN has
relevant knowledge in medication and is competent with administration of intravenous drugs.
Thus, I would expect them to appropriately administer medication two patients present in the
surgical ward. I would also delegate the EN for administering intravenous drugs when required,
and would ask her to seek assistance if needed. According to the NMBA (2018), enrolled nurses
should be capable of administering drugs intravenously, provided they have completed their
education on IV medication administration. Moreover, I would also focus on using other
intravenous antibiotics for the concerned patient, and would provide assistance to other
registered nurses, because the core idea of team nursing model is focused on supervising and
helping each member of the team.
The registered nurse will work as NUM because she will be responsible for managing the
entire word as well. The NSW health standard state that AINs are entrusted with the
responsibility of performing simple clinical tasks related to measuring vital signs of patients
admitted in acute health care ward (NSW Health, 2010). Hence, I would request all the AINs to
measure vital signs of their corresponding patients. I would also presume that the EN has
relevant knowledge in medication and is competent with administration of intravenous drugs.
Thus, I would expect them to appropriately administer medication two patients present in the
surgical ward. I would also delegate the EN for administering intravenous drugs when required,
and would ask her to seek assistance if needed. According to the NMBA (2018), enrolled nurses
should be capable of administering drugs intravenously, provided they have completed their
education on IV medication administration. Moreover, I would also focus on using other
intravenous antibiotics for the concerned patient, and would provide assistance to other
registered nurses, because the core idea of team nursing model is focused on supervising and
helping each member of the team.
15NURSING ASSIGNMENT
References
Dubois, C. A., D'amour, D., Tchouaket, E., Clarke, S., Rivard, M., & Blais, R. (2013).
Associations of patient safety outcomes with models of nursing care organization at unit
level in hospitals. International Journal for Quality in Health Care, 25(2), 110-117.
https://doi.org/10.1093/intqhc/mzt019
Fairbrother, G., Jones, A., & Rivas, K. (2010). Changing model of nursing care from individual
patient allocation to team nursing in the acute inpatient environment. Contemporary
Nurse, 35(2), 202-220. https://doi.org/10.5172/conu.2010.35.2.202
Ferguson, L., & Cioffi, J. (2011). Team nursing: experiences of nurse managers in acute care
settings. Australian Journal of Advanced Nursing, 28(4), 5-11. Retrieved from-
http://www.ajan.com.au/Vol28/28-4.pdf#page=6
King, A., Long, L., & Lisy, K. (2014). Effectiveness of team nursing compared with total patient
care on staff wellbeing when organizing nursing work in acute care ward settings: a
systematic review protocol. JBI Database of Systematic Reviews and implementation
reports, 12(1), 59-73. doi: 10.11124/jbisrir-2014-1533
NSW Health. (2010). Assistants in Nursing working in the acute care environment. Retrieved
from http://www.health.nsw.gov.au/workforce/Publications/ain-acute-care.pdf
Nursingmidwiferyboard.gov.au. (2018). Nursing and Midwifery Board of Australia - Fact sheet:
Enrolled nurses and medicine administration. Retrieved 3 March 2018, from
http://www.nursingmidwiferyboard.gov.au/Codes-Guidelines-Statements/FAQ/Enrolled-
nurses-and-medicine-administration.aspx
References
Dubois, C. A., D'amour, D., Tchouaket, E., Clarke, S., Rivard, M., & Blais, R. (2013).
Associations of patient safety outcomes with models of nursing care organization at unit
level in hospitals. International Journal for Quality in Health Care, 25(2), 110-117.
https://doi.org/10.1093/intqhc/mzt019
Fairbrother, G., Jones, A., & Rivas, K. (2010). Changing model of nursing care from individual
patient allocation to team nursing in the acute inpatient environment. Contemporary
Nurse, 35(2), 202-220. https://doi.org/10.5172/conu.2010.35.2.202
Ferguson, L., & Cioffi, J. (2011). Team nursing: experiences of nurse managers in acute care
settings. Australian Journal of Advanced Nursing, 28(4), 5-11. Retrieved from-
http://www.ajan.com.au/Vol28/28-4.pdf#page=6
King, A., Long, L., & Lisy, K. (2014). Effectiveness of team nursing compared with total patient
care on staff wellbeing when organizing nursing work in acute care ward settings: a
systematic review protocol. JBI Database of Systematic Reviews and implementation
reports, 12(1), 59-73. doi: 10.11124/jbisrir-2014-1533
NSW Health. (2010). Assistants in Nursing working in the acute care environment. Retrieved
from http://www.health.nsw.gov.au/workforce/Publications/ain-acute-care.pdf
Nursingmidwiferyboard.gov.au. (2018). Nursing and Midwifery Board of Australia - Fact sheet:
Enrolled nurses and medicine administration. Retrieved 3 March 2018, from
http://www.nursingmidwiferyboard.gov.au/Codes-Guidelines-Statements/FAQ/Enrolled-
nurses-and-medicine-administration.aspx
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
16NURSING ASSIGNMENT
Polis, S., Higgs, M., Manning, V., Netto, G., & Fernandez, R. (2017). Factors contributing to
nursing team work in an acute care tertiary hospital. Collegian, 24(1), 19-25.
https://doi.org/10.1016/j.colegn.2015.09.002
Tran, D. T., Johnson, M., Fernandez, R., & Jones, S. (2010). A shared care model vs. a patient
allocation model of nursing care delivery: Comparing nursing staff satisfaction and stress
outcomes. International Journal of Nursing Practice, 16(2), 148-158.
DOI: 10.1111/j.1440-172X.2010.01823.x
Polis, S., Higgs, M., Manning, V., Netto, G., & Fernandez, R. (2017). Factors contributing to
nursing team work in an acute care tertiary hospital. Collegian, 24(1), 19-25.
https://doi.org/10.1016/j.colegn.2015.09.002
Tran, D. T., Johnson, M., Fernandez, R., & Jones, S. (2010). A shared care model vs. a patient
allocation model of nursing care delivery: Comparing nursing staff satisfaction and stress
outcomes. International Journal of Nursing Practice, 16(2), 148-158.
DOI: 10.1111/j.1440-172X.2010.01823.x
17NURSING ASSIGNMENT
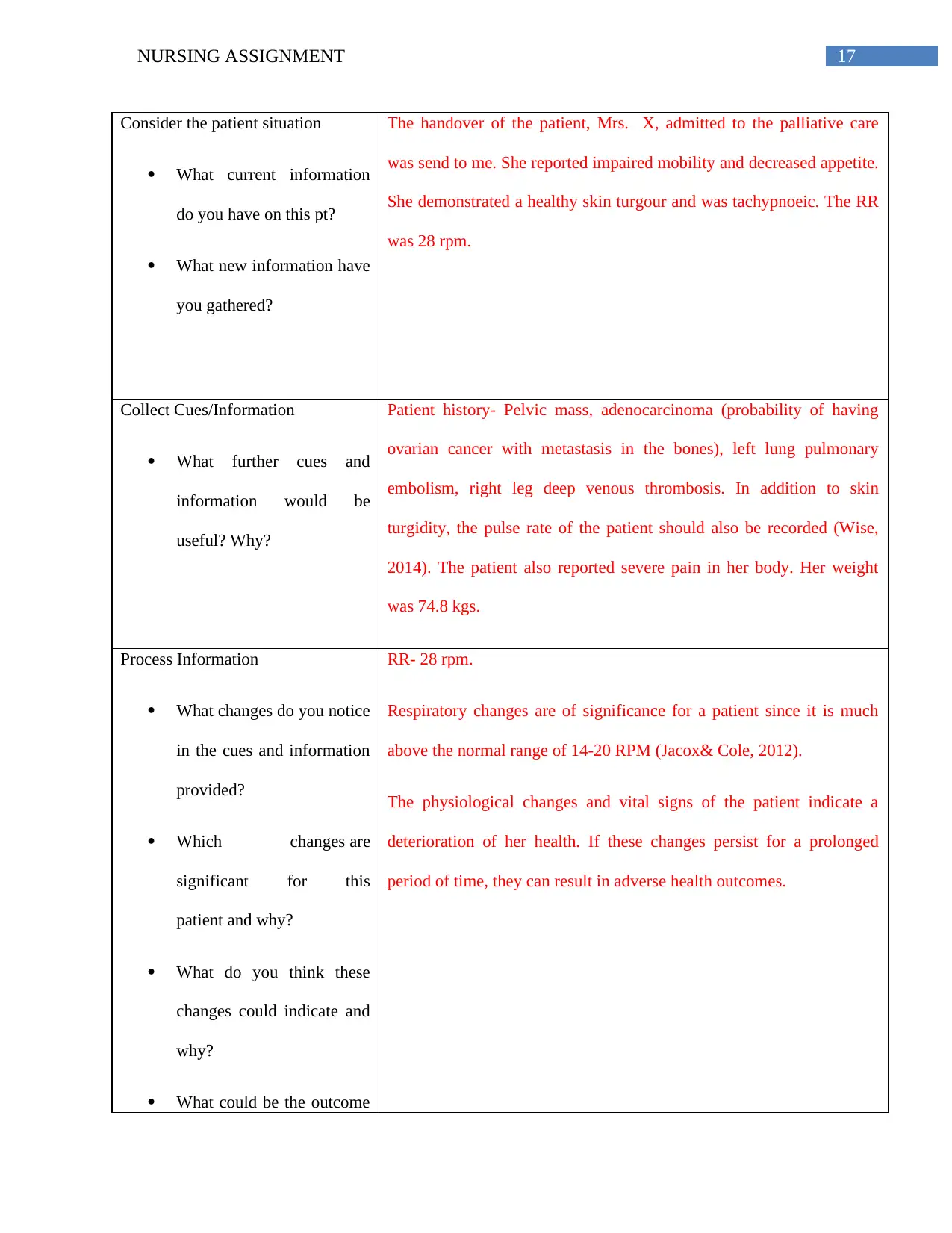
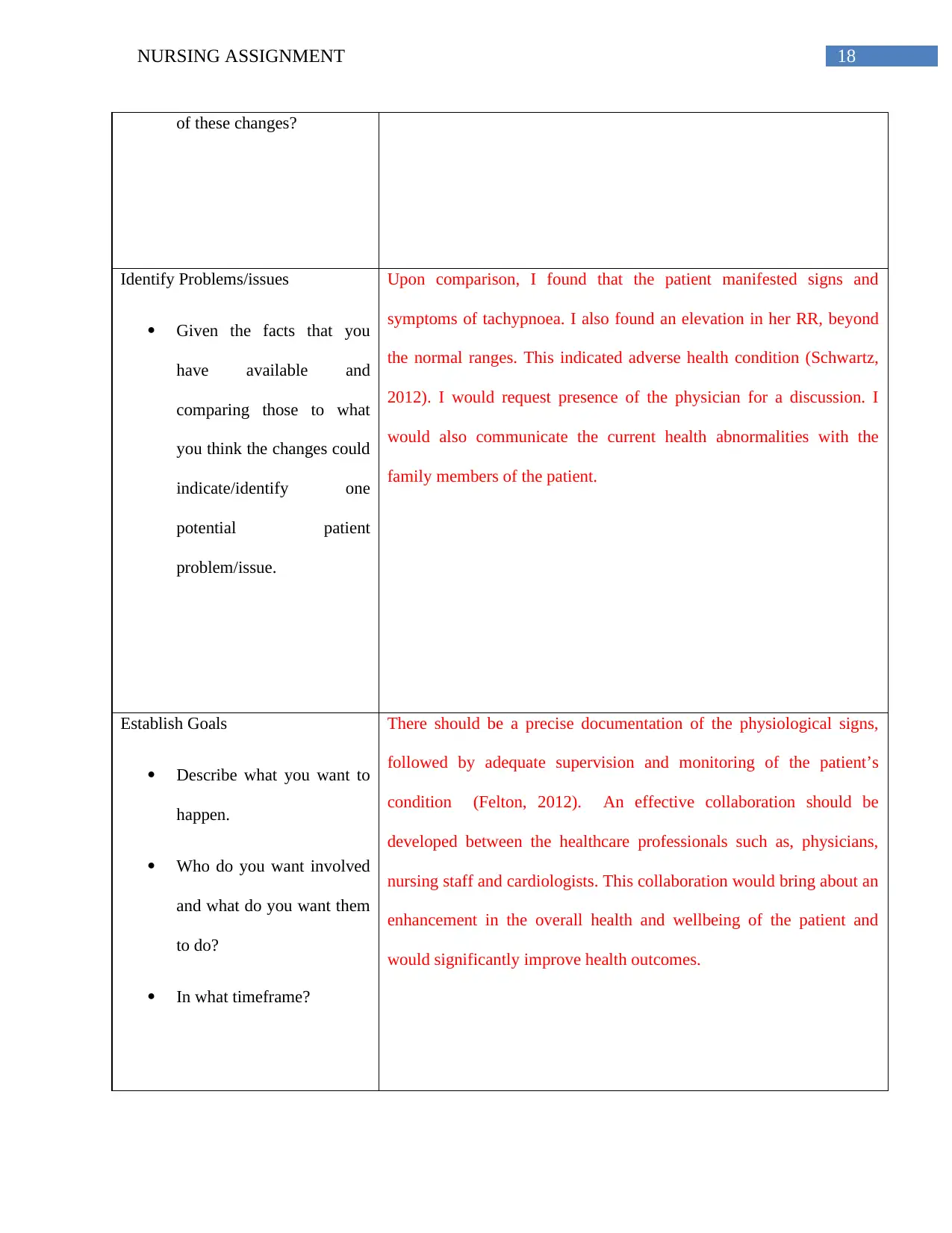
Consider the patient situation
What current information
do you have on this pt?
What new information have
you gathered?
The handover of the patient, Mrs. X, admitted to the palliative care
was send to me. She reported impaired mobility and decreased appetite.
She demonstrated a healthy skin turgour and was tachypnoeic. The RR
was 28 rpm.
Collect Cues/Information
What further cues and
information would be
useful? Why?
Patient history- Pelvic mass, adenocarcinoma (probability of having
ovarian cancer with metastasis in the bones), left lung pulmonary
embolism, right leg deep venous thrombosis. In addition to skin
turgidity, the pulse rate of the patient should also be recorded (Wise,
2014). The patient also reported severe pain in her body. Her weight
was 74.8 kgs.
Process Information
What changes do you notice
in the cues and information
provided?
Which changes are
significant for this
patient and why?
What do you think these
changes could indicate and
why?
What could be the outcome
RR- 28 rpm.
Respiratory changes are of significance for a patient since it is much
above the normal range of 14-20 RPM (Jacox& Cole, 2012).
The physiological changes and vital signs of the patient indicate a
deterioration of her health. If these changes persist for a prolonged
period of time, they can result in adverse health outcomes.
Consider the patient situation
What current information
do you have on this pt?
What new information have
you gathered?
The handover of the patient, Mrs. X, admitted to the palliative care
was send to me. She reported impaired mobility and decreased appetite.
She demonstrated a healthy skin turgour and was tachypnoeic. The RR
was 28 rpm.
Collect Cues/Information
What further cues and
information would be
useful? Why?
Patient history- Pelvic mass, adenocarcinoma (probability of having
ovarian cancer with metastasis in the bones), left lung pulmonary
embolism, right leg deep venous thrombosis. In addition to skin
turgidity, the pulse rate of the patient should also be recorded (Wise,
2014). The patient also reported severe pain in her body. Her weight
was 74.8 kgs.
Process Information
What changes do you notice
in the cues and information
provided?
Which changes are
significant for this
patient and why?
What do you think these
changes could indicate and
why?
What could be the outcome
RR- 28 rpm.
Respiratory changes are of significance for a patient since it is much
above the normal range of 14-20 RPM (Jacox& Cole, 2012).
The physiological changes and vital signs of the patient indicate a
deterioration of her health. If these changes persist for a prolonged
period of time, they can result in adverse health outcomes.
18NURSING ASSIGNMENT
of these changes?
Identify Problems/issues
Given the facts that you
have available and
comparing those to what
you think the changes could
indicate/identify one
potential patient
problem/issue.
Upon comparison, I found that the patient manifested signs and
symptoms of tachypnoea. I also found an elevation in her RR, beyond
the normal ranges. This indicated adverse health condition (Schwartz,
2012). I would request presence of the physician for a discussion. I
would also communicate the current health abnormalities with the
family members of the patient.
Establish Goals
Describe what you want to
happen.
Who do you want involved
and what do you want them
to do?
In what timeframe?
There should be a precise documentation of the physiological signs,
followed by adequate supervision and monitoring of the patient’s
condition (Felton, 2012). An effective collaboration should be
developed between the healthcare professionals such as, physicians,
nursing staff and cardiologists. This collaboration would bring about an
enhancement in the overall health and wellbeing of the patient and
would significantly improve health outcomes.
of these changes?
Identify Problems/issues
Given the facts that you
have available and
comparing those to what
you think the changes could
indicate/identify one
potential patient
problem/issue.
Upon comparison, I found that the patient manifested signs and
symptoms of tachypnoea. I also found an elevation in her RR, beyond
the normal ranges. This indicated adverse health condition (Schwartz,
2012). I would request presence of the physician for a discussion. I
would also communicate the current health abnormalities with the
family members of the patient.
Establish Goals
Describe what you want to
happen.
Who do you want involved
and what do you want them
to do?
In what timeframe?
There should be a precise documentation of the physiological signs,
followed by adequate supervision and monitoring of the patient’s
condition (Felton, 2012). An effective collaboration should be
developed between the healthcare professionals such as, physicians,
nursing staff and cardiologists. This collaboration would bring about an
enhancement in the overall health and wellbeing of the patient and
would significantly improve health outcomes.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
19NURSING ASSIGNMENT
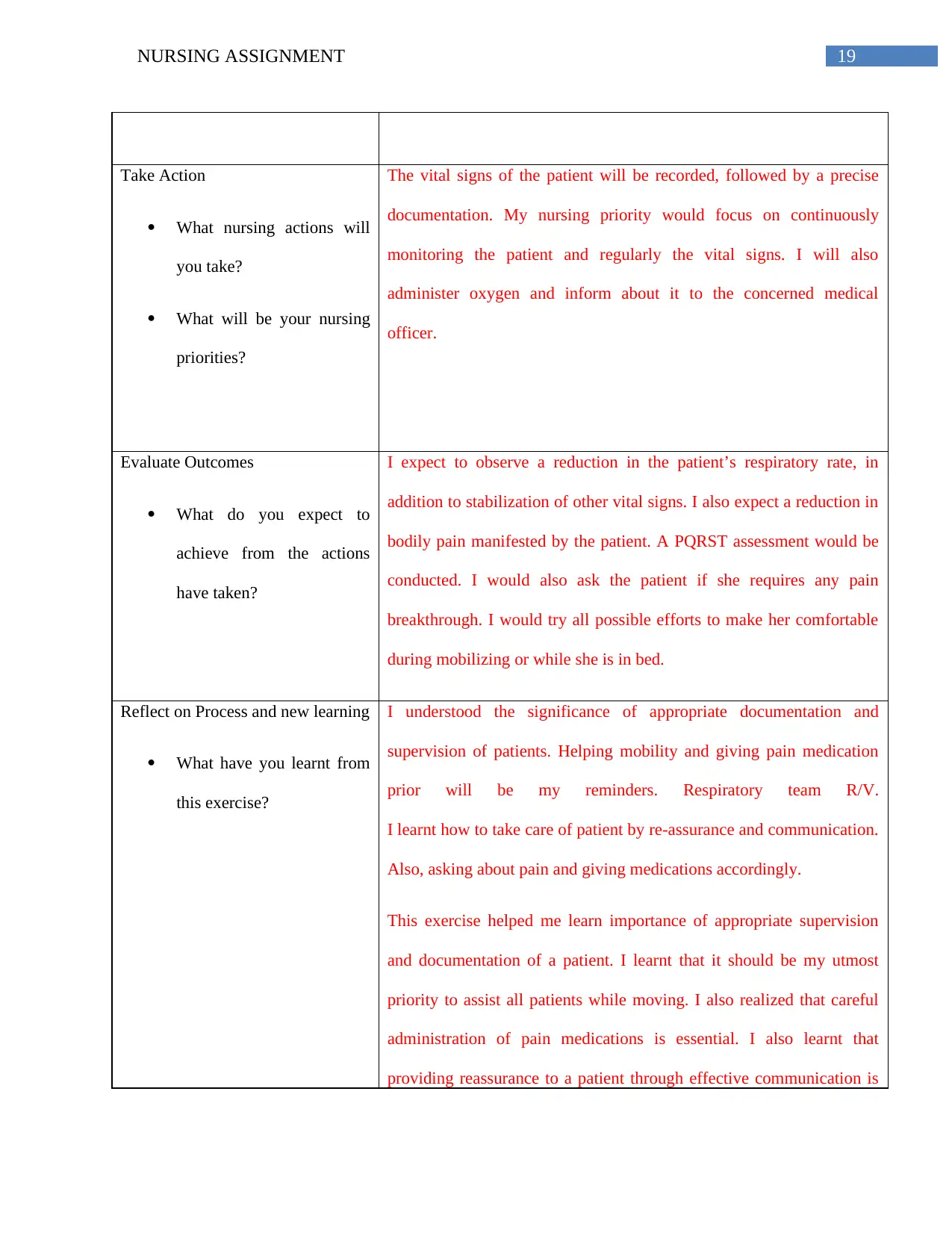
Take Action
What nursing actions will
you take?
What will be your nursing
priorities?
The vital signs of the patient will be recorded, followed by a precise
documentation. My nursing priority would focus on continuously
monitoring the patient and regularly the vital signs. I will also
administer oxygen and inform about it to the concerned medical
officer.
Evaluate Outcomes
What do you expect to
achieve from the actions
have taken?
I expect to observe a reduction in the patient’s respiratory rate, in
addition to stabilization of other vital signs. I also expect a reduction in
bodily pain manifested by the patient. A PQRST assessment would be
conducted. I would also ask the patient if she requires any pain
breakthrough. I would try all possible efforts to make her comfortable
during mobilizing or while she is in bed.
Reflect on Process and new learning
What have you learnt from
this exercise?
I understood the significance of appropriate documentation and
supervision of patients. Helping mobility and giving pain medication
prior will be my reminders. Respiratory team R/V.
I learnt how to take care of patient by re-assurance and communication.
Also, asking about pain and giving medications accordingly.
This exercise helped me learn importance of appropriate supervision
and documentation of a patient. I learnt that it should be my utmost
priority to assist all patients while moving. I also realized that careful
administration of pain medications is essential. I also learnt that
providing reassurance to a patient through effective communication is
Take Action
What nursing actions will
you take?
What will be your nursing
priorities?
The vital signs of the patient will be recorded, followed by a precise
documentation. My nursing priority would focus on continuously
monitoring the patient and regularly the vital signs. I will also
administer oxygen and inform about it to the concerned medical
officer.
Evaluate Outcomes
What do you expect to
achieve from the actions
have taken?
I expect to observe a reduction in the patient’s respiratory rate, in
addition to stabilization of other vital signs. I also expect a reduction in
bodily pain manifested by the patient. A PQRST assessment would be
conducted. I would also ask the patient if she requires any pain
breakthrough. I would try all possible efforts to make her comfortable
during mobilizing or while she is in bed.
Reflect on Process and new learning
What have you learnt from
this exercise?
I understood the significance of appropriate documentation and
supervision of patients. Helping mobility and giving pain medication
prior will be my reminders. Respiratory team R/V.
I learnt how to take care of patient by re-assurance and communication.
Also, asking about pain and giving medications accordingly.
This exercise helped me learn importance of appropriate supervision
and documentation of a patient. I learnt that it should be my utmost
priority to assist all patients while moving. I also realized that careful
administration of pain medications is essential. I also learnt that
providing reassurance to a patient through effective communication is

20NURSING ASSIGNMENT
imperative for nursing duty. Furthermore, a patient should also be
questioned for pain assessment and current medications.
imperative for nursing duty. Furthermore, a patient should also be
questioned for pain assessment and current medications.
1 out of 21
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





