Reflective Practice: RN Standards & Workplace Learning at CSU
VerifiedAdded on 2023/06/07
|9
|2336
|284
Report
AI Summary
This report reflects on workplace learning experiences during a Bachelor of Nursing course, using Gibbs' Reflective Cycle to analyze three case studies. These case studies address critical thinking in nursing practice, therapeutic relationships, and maintaining practice capability, referencing the Registered Nurse Standards for Practice in Australia. The first case involves a patient with leg ulcers whose mental health hindered recovery, highlighting the importance of comprehensive assessment and therapeutic communication. The second case describes a chaotic situation where effective communication and collaboration were crucial. The third case discusses an ethical dilemma regarding disclosing a terminal illness diagnosis to a patient, emphasizing the importance of ethical conduct and patient-centered care. The report concludes that reflective practice enhances understanding and improves future nursing practice, with a professional development plan included to guide ongoing growth as a Registered Nurse. Desklib provides access to similar solved assignments and resources for students.

Nursing Reflective Practice
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Introduction:
This report has been written in accordance with the reflection of learning of the workplace
and the experience that I’ve collected while completing my Bachelor of Nursing course at
CSU. Three experiences of mine from the workplace will be stated in this report and will also
be addressed with the help of Gibbs reflective Cycle to know the knowledge that I’ve
gathered from the workplace experiences. Gibbs reflective Cycle is used for the purpose of
reflective leaning and to share the experiences gained while performing a task and the
framework was provided by Graham Gibbs in the year 1988 (Davies, 2012). There are
altogether seven Registered Nurse Standards for Practice in Australia and three of them,
which include thinking critically and analyzing Nursing Practices, engaging in therapeutic
and professional relationship as well as maintaining capability of practices will be described
respectively with the help of case studies along with personal experience from Gibbs
reflective Cycle.
Case study 1- Ms X
Description
Ms X was admitted to the elderly ward when she was diagnosed with advanced mixed
bilateral leg ulcers. I along with my superior professionals started delivering care to her
according to the guidelines. She was very quiet and unwilling to talk with me during my
sessions with her. We gave her evidence-based safe and quality practice for wound
management as per the first NMBA standard, but her ulcers did not heal. In order to
understand her case study and as per the fourth NMBA standards RNs must accurately
conduct comprehensive and systematic assessments, I redid all the assessments with her
(Nursing and Midwifery Board of Australia, 2016). I cultivated an interpersonal association
with her and found out that her mental condition is disturbed as she was self-conscious and
This report has been written in accordance with the reflection of learning of the workplace
and the experience that I’ve collected while completing my Bachelor of Nursing course at
CSU. Three experiences of mine from the workplace will be stated in this report and will also
be addressed with the help of Gibbs reflective Cycle to know the knowledge that I’ve
gathered from the workplace experiences. Gibbs reflective Cycle is used for the purpose of
reflective leaning and to share the experiences gained while performing a task and the
framework was provided by Graham Gibbs in the year 1988 (Davies, 2012). There are
altogether seven Registered Nurse Standards for Practice in Australia and three of them,
which include thinking critically and analyzing Nursing Practices, engaging in therapeutic
and professional relationship as well as maintaining capability of practices will be described
respectively with the help of case studies along with personal experience from Gibbs
reflective Cycle.
Case study 1- Ms X
Description
Ms X was admitted to the elderly ward when she was diagnosed with advanced mixed
bilateral leg ulcers. I along with my superior professionals started delivering care to her
according to the guidelines. She was very quiet and unwilling to talk with me during my
sessions with her. We gave her evidence-based safe and quality practice for wound
management as per the first NMBA standard, but her ulcers did not heal. In order to
understand her case study and as per the fourth NMBA standards RNs must accurately
conduct comprehensive and systematic assessments, I redid all the assessments with her
(Nursing and Midwifery Board of Australia, 2016). I cultivated an interpersonal association
with her and found out that her mental condition is disturbed as she was self-conscious and
stressed due to her obesity. She underwent psychoanalysis and then psychotherapy. Her
behaviour as well as her wounds improved.
Feelings
I was astonished to find out that Ms X’s mental issues were hindering her physical care so
much that her wounds did not heal. I also felt disappointed with myself that we could not
identify the state of her mental condition as I did not follow the second standard of NMBA,
which suggests engaging in therapeutic and professional relationship through effective
communication.
Evaluation
Ms X’s case was difficult for me as I could not identify the domain of practice which was
lacking in my care delivery. My practice included pain settlement, wound management,
educative sessions, etc. according to the standards of NMBA. In spite of giving appropriate
service, no positive outcome was observed. Ms X’s mental state obstructing her physical
symptoms improvement came as a surprise to me. I could not believe an elderly woman could
be so self-conscious about her weight.
Analysis
It can be analysed that Ms X’s mental condition should have been assessed at the start of her
care planning as the fifth standard of NMBA suggests development of safe and
comprehensive nursing plans based on the assessments. Various researches have proved the
significance of motivation, social assistance, spouse relationship in care delivery, etc. as a
contributor in wound healing. However, I only paid attention on medicinal therapy. I
practiced a disease-centred care instead of a person-centred framework which is should have
as per second NMBA standard. I should have understood that good therapeutic
behaviour as well as her wounds improved.
Feelings
I was astonished to find out that Ms X’s mental issues were hindering her physical care so
much that her wounds did not heal. I also felt disappointed with myself that we could not
identify the state of her mental condition as I did not follow the second standard of NMBA,
which suggests engaging in therapeutic and professional relationship through effective
communication.
Evaluation
Ms X’s case was difficult for me as I could not identify the domain of practice which was
lacking in my care delivery. My practice included pain settlement, wound management,
educative sessions, etc. according to the standards of NMBA. In spite of giving appropriate
service, no positive outcome was observed. Ms X’s mental state obstructing her physical
symptoms improvement came as a surprise to me. I could not believe an elderly woman could
be so self-conscious about her weight.
Analysis
It can be analysed that Ms X’s mental condition should have been assessed at the start of her
care planning as the fifth standard of NMBA suggests development of safe and
comprehensive nursing plans based on the assessments. Various researches have proved the
significance of motivation, social assistance, spouse relationship in care delivery, etc. as a
contributor in wound healing. However, I only paid attention on medicinal therapy. I
practiced a disease-centred care instead of a person-centred framework which is should have
as per second NMBA standard. I should have understood that good therapeutic
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
communication could have helped in fulfilling Ms X’s physical, emotional and spiritual
needs (Mills, 2017)
Conclusion
When I look back at this case, I feel disappointed that because of my lack of understanding
on handling this case Ms X had to experience the pain and ulcers for prolonged time. If I had
paid attention to her mental issues at the initiation of her care, her stress would have been
diagnosed earlier. I also regret discriminating her based on her age thinking that a person of
her age could not be conscious of her weight.
Action Plan
In future, I will make an effort to form a personal relationship with all my patients from the
beginning irrespective of their disease (Berman & Chutka, 2016). I will try to manage the
person as a whole and not just their illness (Morrissey & Callaghan, 2011). I will learn the
skills of therapeutic communication and assessments. I will abstain from discrimination.
Case study 2- Mr Y
Description
I and my peer Jon (pseudonym) had to observe a senior professional. While doing ward
rounds, the senio checked up on Mr Y’s current condition who was recently operated for
cholecystectomy and shifter to the ward. His mother was present as the attendant. After the
senior doctor went, Mr Y seemed restless and complained of severe pain. Seeing this, Mr.
Y’s mother got anxious and started crying. While all this was happening Jon got panicked
and froze at his place. I was unnerved initially but then established communication with Mr Y
and assured him that the Doctor is on his way. Then I asked Jon to call the senior doctor.
After my continuous motivation, Jon calmed down and was back with the doctor and he
managed Mr Y. I took Mr Y’s mother outside the ward and comforted her.
needs (Mills, 2017)
Conclusion
When I look back at this case, I feel disappointed that because of my lack of understanding
on handling this case Ms X had to experience the pain and ulcers for prolonged time. If I had
paid attention to her mental issues at the initiation of her care, her stress would have been
diagnosed earlier. I also regret discriminating her based on her age thinking that a person of
her age could not be conscious of her weight.
Action Plan
In future, I will make an effort to form a personal relationship with all my patients from the
beginning irrespective of their disease (Berman & Chutka, 2016). I will try to manage the
person as a whole and not just their illness (Morrissey & Callaghan, 2011). I will learn the
skills of therapeutic communication and assessments. I will abstain from discrimination.
Case study 2- Mr Y
Description
I and my peer Jon (pseudonym) had to observe a senior professional. While doing ward
rounds, the senio checked up on Mr Y’s current condition who was recently operated for
cholecystectomy and shifter to the ward. His mother was present as the attendant. After the
senior doctor went, Mr Y seemed restless and complained of severe pain. Seeing this, Mr.
Y’s mother got anxious and started crying. While all this was happening Jon got panicked
and froze at his place. I was unnerved initially but then established communication with Mr Y
and assured him that the Doctor is on his way. Then I asked Jon to call the senior doctor.
After my continuous motivation, Jon calmed down and was back with the doctor and he
managed Mr Y. I took Mr Y’s mother outside the ward and comforted her.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Feelings
I felt helpless as I wanted Jon to take care of at least one of them (Mr Y or his mother) so that
the senior doctor could be called but it seemed that Jon himself needed to be calmed. At that
point, of time I really needed Robert to work alongside me but he couldn’t. My job became
difficult as Jon didn’t support me, as collaborative practice is one of the aspects of second
standard of NMBA.
Evaluation
The incident required quick thinking, action and communication. The accountability of
clinical decision-making was especially daunting for me as as per the second NMBA
standard, I had to lead the collaborative practice in this case.
Analysis
It should be understood that effective communication in health care is challenging to get as
the nature of the work environment is demanding. I used different verbal and non-verbal
communication techniques with Mr. Y (W.Y.Kee et al., 2017). I also focused on listening and
showing empathy towards Mr Y’s mother to build the emotional dynamics in the
communication.
Conclusion
When I look back at this incident, I realise the senior doctor must have called sooner as the
delay of even few seconds could have led to grave complications for Mr Y. I realise that I
need to be empathetic with colleagues by understanding the pressures they may be under, but
it needs to be made sure that their incompetence does not put patients at risk.
I felt helpless as I wanted Jon to take care of at least one of them (Mr Y or his mother) so that
the senior doctor could be called but it seemed that Jon himself needed to be calmed. At that
point, of time I really needed Robert to work alongside me but he couldn’t. My job became
difficult as Jon didn’t support me, as collaborative practice is one of the aspects of second
standard of NMBA.
Evaluation
The incident required quick thinking, action and communication. The accountability of
clinical decision-making was especially daunting for me as as per the second NMBA
standard, I had to lead the collaborative practice in this case.
Analysis
It should be understood that effective communication in health care is challenging to get as
the nature of the work environment is demanding. I used different verbal and non-verbal
communication techniques with Mr. Y (W.Y.Kee et al., 2017). I also focused on listening and
showing empathy towards Mr Y’s mother to build the emotional dynamics in the
communication.
Conclusion
When I look back at this incident, I realise the senior doctor must have called sooner as the
delay of even few seconds could have led to grave complications for Mr Y. I realise that I
need to be empathetic with colleagues by understanding the pressures they may be under, but
it needs to be made sure that their incompetence does not put patients at risk.
Action Plan
In future, in emergency situation, I will attempt to develop my communication skills with my
colleagues to ensure effective collaborative practice as it is essential in delivering best
possible care (Nijagal, Kupperman, Nakagawa, & Cheng, 2015) .
Case study 3- Mr Z
Description
This is the first stage of the Gibb’s reflective Cycle and this stage is concerned with the
experience that an individual had while working (Bassot, 2016). Mr Zwho is a patient of 57
years of age was diagnosed with terminal illness and the patient was not aware of his
condition. After the diagnosis I let the family members know the condition of the patient and
the family members told me to keep the illness of the patient a secret and not to disclose
anything to Mr. Z which is against the healthcare ethics.
Feelings
This is the second stage of the Gibbs reflective Cycle and this stage is related to the feelings
that were there during the happenings and what I’ve felt during these experiences (Howatson-
Jones, 2016). I felt that Mr. Z should know about his disease before the treatment is
conducted. As before the treatment of terminal illness, disclosing the patient’s disorder to the
patient can improve the motivation power, so I felt that the patient should be disclosed with
his illness and for that reason.
Evaluation
There are some positive as well as negatives about a situations that are created and these
things are necessary to make it understand to the other person (Smith, 2016). It was essential
to make the family of Mr. Z understand that terminal illness is a disease where disclosing the
disease to the patient make the situation better and also make the outcomes better. As the
family requested not to disclose anything to Mr. Z, this was a negative situation, while the
positive situation is related to disclosing his illness to Mr. Z which can help in the outcome of
the disease a better one.
Analysis
It can be analysed that as per the second standard of NMBA I should provide support and
direct Mr Z and his family to resources to take the most appropriate health-related decisions.
In future, in emergency situation, I will attempt to develop my communication skills with my
colleagues to ensure effective collaborative practice as it is essential in delivering best
possible care (Nijagal, Kupperman, Nakagawa, & Cheng, 2015) .
Case study 3- Mr Z
Description
This is the first stage of the Gibb’s reflective Cycle and this stage is concerned with the
experience that an individual had while working (Bassot, 2016). Mr Zwho is a patient of 57
years of age was diagnosed with terminal illness and the patient was not aware of his
condition. After the diagnosis I let the family members know the condition of the patient and
the family members told me to keep the illness of the patient a secret and not to disclose
anything to Mr. Z which is against the healthcare ethics.
Feelings
This is the second stage of the Gibbs reflective Cycle and this stage is related to the feelings
that were there during the happenings and what I’ve felt during these experiences (Howatson-
Jones, 2016). I felt that Mr. Z should know about his disease before the treatment is
conducted. As before the treatment of terminal illness, disclosing the patient’s disorder to the
patient can improve the motivation power, so I felt that the patient should be disclosed with
his illness and for that reason.
Evaluation
There are some positive as well as negatives about a situations that are created and these
things are necessary to make it understand to the other person (Smith, 2016). It was essential
to make the family of Mr. Z understand that terminal illness is a disease where disclosing the
disease to the patient make the situation better and also make the outcomes better. As the
family requested not to disclose anything to Mr. Z, this was a negative situation, while the
positive situation is related to disclosing his illness to Mr. Z which can help in the outcome of
the disease a better one.
Analysis
It can be analysed that as per the second standard of NMBA I should provide support and
direct Mr Z and his family to resources to take the most appropriate health-related decisions.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

Conclusion
The conclusion is the stage, when it is evaluated that which situation could have been handled
in a better way and if those situations arise again how those situations can be handled (Brock,
2014). As Mr. Z was suffering from diabetes, there were a few precautions that were required
to be taken but if he is not aware of his situation, he will not take any dietary control which
can result to higher diabetes or sugar in his blood level. Thus, this situation could have been
handled with communicating in a better way with the members of the family and this could
have helped in the process of avoidance of more serious life threat for the patient.
Action Plan
In future, I will make myself more aware with the ethical code of conduct and principles as
per the NMBA standards and ensure that my practice falls within the ethics.
Conclusion
Thus, from the above study, it can be concluded that Gibbs reflective Cycle plays an
important role in providing assistance to the knowledge and increases the experience of an
individual (Bulman et al., 2013). Similarly, in my case, Gibbs reflective Cycle has helped me
in the process of gaining understanding of the situations while working in healthcare during
my Bachelor of Nursing course at CSU and this will also assist me during the future course of
action preparation as well as will overall help me to increase my working ability.
References
Bassot, B., 2016. The reflective journal. Macmillan International Higher Education.
The conclusion is the stage, when it is evaluated that which situation could have been handled
in a better way and if those situations arise again how those situations can be handled (Brock,
2014). As Mr. Z was suffering from diabetes, there were a few precautions that were required
to be taken but if he is not aware of his situation, he will not take any dietary control which
can result to higher diabetes or sugar in his blood level. Thus, this situation could have been
handled with communicating in a better way with the members of the family and this could
have helped in the process of avoidance of more serious life threat for the patient.
Action Plan
In future, I will make myself more aware with the ethical code of conduct and principles as
per the NMBA standards and ensure that my practice falls within the ethics.
Conclusion
Thus, from the above study, it can be concluded that Gibbs reflective Cycle plays an
important role in providing assistance to the knowledge and increases the experience of an
individual (Bulman et al., 2013). Similarly, in my case, Gibbs reflective Cycle has helped me
in the process of gaining understanding of the situations while working in healthcare during
my Bachelor of Nursing course at CSU and this will also assist me during the future course of
action preparation as well as will overall help me to increase my working ability.
References
Bassot, B., 2016. The reflective journal. Macmillan International Higher Education.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Berman, A.C. & Chutka, D.S., 2016. Assessing effective physician-patient communication
skills: “Are you listening to me, doc?”. Korean journal of Medical education, 28(2), pp.243-
49.
Brock, A., 2014. What is reflection and reflective practice?. In The Early Years Reflective
Practice Handbook (pp. 25-39). Routledge
Bulman, C. and Schutz, S. eds., 2013. Reflective practice in nursing. John Wiley & Sons.
Davies, S., 2012. Embracing reflective practice. Education for Primary Care, 23(1), pp.9-12.
Howatson-Jones, L., 2016. Reflective practice in nursing. Learning Matters.
Mills, J., 2017. Therapeutic Communication In Mental Health Nursing: Aesthetic And
Metaphoric Processes In The Engagement With Challenging Patients. Issues in Mental
Health Nursing, 38(8),pp- 684.
Morrissey, Jean, Callaghan, & Patrick. (2011). Communication Skills For Mental Health
Nurses: An introduction. McGraw-Hill Education.
Nursing and Midwifery Board of Australia. (2016). Registered nurse standards for practice.
Melbourne: www.nursingmidwiferyboard.gov.au .
Smith, J. and Roberts, R., 2015. Reflective practice. Vital Signs for Nurses: An Introduction
to Clinical Observations, pp.222-230.
W.Y.Kee, J., gKhoo, H.S., Lim, I. & Y.H.Koh, M., 2017. Communication Skills in Patient-
Doctor Interactions: Learning from Patient Complaints. Health Professions Education.
Appendix
Professional Development Plan
Plan of Action Timeline Problems Actions taken
Communication 6 months In all the three case I will read books on
skills: “Are you listening to me, doc?”. Korean journal of Medical education, 28(2), pp.243-
49.
Brock, A., 2014. What is reflection and reflective practice?. In The Early Years Reflective
Practice Handbook (pp. 25-39). Routledge
Bulman, C. and Schutz, S. eds., 2013. Reflective practice in nursing. John Wiley & Sons.
Davies, S., 2012. Embracing reflective practice. Education for Primary Care, 23(1), pp.9-12.
Howatson-Jones, L., 2016. Reflective practice in nursing. Learning Matters.
Mills, J., 2017. Therapeutic Communication In Mental Health Nursing: Aesthetic And
Metaphoric Processes In The Engagement With Challenging Patients. Issues in Mental
Health Nursing, 38(8),pp- 684.
Morrissey, Jean, Callaghan, & Patrick. (2011). Communication Skills For Mental Health
Nurses: An introduction. McGraw-Hill Education.
Nursing and Midwifery Board of Australia. (2016). Registered nurse standards for practice.
Melbourne: www.nursingmidwiferyboard.gov.au .
Smith, J. and Roberts, R., 2015. Reflective practice. Vital Signs for Nurses: An Introduction
to Clinical Observations, pp.222-230.
W.Y.Kee, J., gKhoo, H.S., Lim, I. & Y.H.Koh, M., 2017. Communication Skills in Patient-
Doctor Interactions: Learning from Patient Complaints. Health Professions Education.
Appendix
Professional Development Plan
Plan of Action Timeline Problems Actions taken
Communication 6 months In all the three case I will read books on
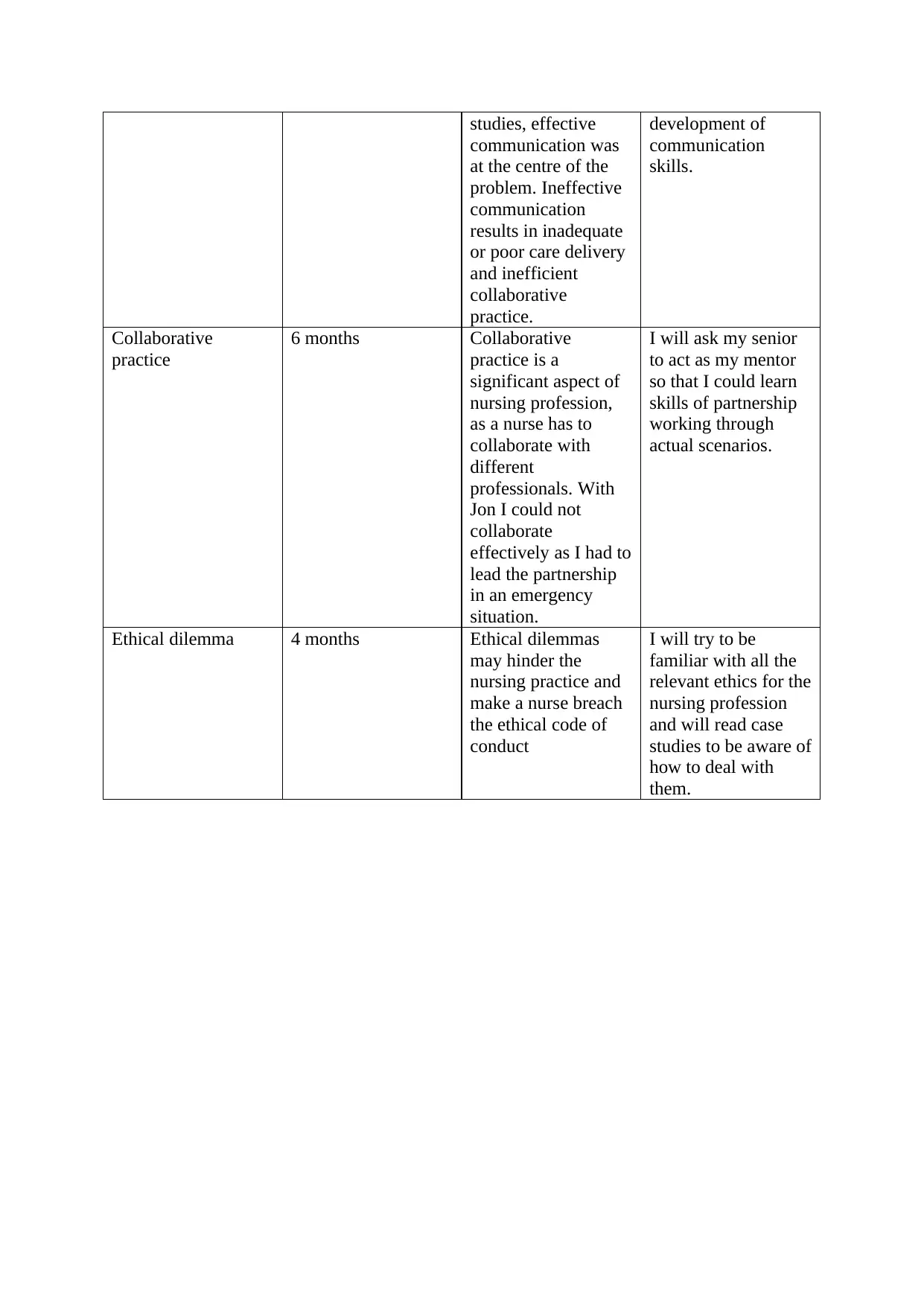
studies, effective
communication was
at the centre of the
problem. Ineffective
communication
results in inadequate
or poor care delivery
and inefficient
collaborative
practice.
development of
communication
skills.
Collaborative
practice
6 months Collaborative
practice is a
significant aspect of
nursing profession,
as a nurse has to
collaborate with
different
professionals. With
Jon I could not
collaborate
effectively as I had to
lead the partnership
in an emergency
situation.
I will ask my senior
to act as my mentor
so that I could learn
skills of partnership
working through
actual scenarios.
Ethical dilemma 4 months Ethical dilemmas
may hinder the
nursing practice and
make a nurse breach
the ethical code of
conduct
I will try to be
familiar with all the
relevant ethics for the
nursing profession
and will read case
studies to be aware of
how to deal with
them.
communication was
at the centre of the
problem. Ineffective
communication
results in inadequate
or poor care delivery
and inefficient
collaborative
practice.
development of
communication
skills.
Collaborative
practice
6 months Collaborative
practice is a
significant aspect of
nursing profession,
as a nurse has to
collaborate with
different
professionals. With
Jon I could not
collaborate
effectively as I had to
lead the partnership
in an emergency
situation.
I will ask my senior
to act as my mentor
so that I could learn
skills of partnership
working through
actual scenarios.
Ethical dilemma 4 months Ethical dilemmas
may hinder the
nursing practice and
make a nurse breach
the ethical code of
conduct
I will try to be
familiar with all the
relevant ethics for the
nursing profession
and will read case
studies to be aware of
how to deal with
them.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





