Strategies to Improve Healthcare for Indigenous Australians: Report
VerifiedAdded on 2023/01/07
|12
|3146
|84
Report
AI Summary
This report provides a comprehensive analysis of the healthcare challenges faced by Aboriginal and Torres Strait Islander people in Australia, with a specific focus on respiratory diseases. It begins with an introduction that highlights the health disparities, including higher infant mortality rates and lower life expectancy, experienced by these populations. The main body of the report delves into the health issues, particularly respiratory diseases like asthma, pneumonia, and COPD, and the contemporary healthcare strategies to address these issues, such as immunisation programs, health promotion, and early detection and treatment. The report also examines the impact of demographic and socio-cultural factors, including low literacy rates, poverty, overcrowded housing, and smoking, on respiratory health. Furthermore, it outlines effective program models, emphasizing accessible health services, community participation, continuous quality improvement, a culturally appropriate workforce, and flexible approaches to care. The report concludes by summarizing the key findings and emphasizing the need for tailored healthcare interventions to improve the health outcomes of Aboriginal and Torres Strait Islander people.
IMPROVING
HEALTHCARE SERVICES
FOR ABORIGINAL AND
TORRES STRAIT
ISLANDER PEOPLE
HEALTHCARE SERVICES
FOR ABORIGINAL AND
TORRES STRAIT
ISLANDER PEOPLE
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
TABLE OF CONTENTS
INTRODUCTION...........................................................................................................................3
MAIN BODY..................................................................................................................................3
Health issue experienced by Aboriginal and Torres Strait Islander people................................3
Contemporary healthcare strategy to improve respiratory health of Aboriginal and Torres
Strait Islander people................................................................................................................5
Impact of demographic and socio-cultural factors on respiratory health issues.........................7
Effective program model of practices from healthcare perspective acceptable to Aboriginal
and Torres Strait Islander people.............................................................................................9
CONCLUSION..............................................................................................................................11
REFERENCES..............................................................................................................................12
INTRODUCTION...........................................................................................................................3
MAIN BODY..................................................................................................................................3
Health issue experienced by Aboriginal and Torres Strait Islander people................................3
Contemporary healthcare strategy to improve respiratory health of Aboriginal and Torres
Strait Islander people................................................................................................................5
Impact of demographic and socio-cultural factors on respiratory health issues.........................7
Effective program model of practices from healthcare perspective acceptable to Aboriginal
and Torres Strait Islander people.............................................................................................9
CONCLUSION..............................................................................................................................11
REFERENCES..............................................................................................................................12
INTRODUCTION
According to Master and et.al., (2018) aboriginal and Torres Strait Island peoples are
Australian people who have achieved nationality of Australia. These are two type people such as
aboriginal people who are known as indigenous people while Torres Strait Islander people who
lives in North Australia. But both type peoples have poor living condition as compared other
Australian people. These type people have high infant mortality rate and poor life expectancy
instead of other Australian population. Authors have highlighted in their published books that
aboriginal and Torres Strait Islanders have minimum literacy ratio while drug and alcohol
consumption are too high which is the major reason less life expectancy rate. Due to weak
educational level, such people unable to get good job that brings poverty which often bring
domestic violence as compared non-indigenous. Aboriginal and Torres Strait Islanders lives in
rural areas of Australia associated with poor nutrition, malnutrition, type of diabetes, tooth decay
and various type of cancers. Due to wide distance between rural and urban area of Australia it
has very limited transportation of suppliers and high cost as well. Such difference leads wide cost
difference around 150 to 180% of items that is not possible for the aboriginal to pay. Such people
consume high level of Tobacco that is another leading risk factor for illness. So around 50 to
60% aboriginal and Torres Strait Islander people are hospitalized as compared non-aboriginal
people.
In this essay will discuss over health issue experiences of aboriginal and Torres Strait
Islander people. Then it will further be evaluated contemporary healthcare strategy to increase
health issue experience of Aboriginal and Torres Strait Islander. Demographical and socio-
cultural factors impact over health issue of aboriginal and Torres Strait Islander will discuss in
this report.
MAIN BODY
Health issue experienced by Aboriginal and Torres Strait Islander people
A major health issue prevalent in the community of Aboriginal and Torres Strait Islander
people in Australia is respiratory disease. The respiratory system consists of those parts of the
human body which are involved in breathing, such as throat, nose, trachea, larynx and lungs.
Respiratory disease happens when any of these body parts get damaged and impact breathing
process. Common diseases include pneumonia, asthma and COPD (chronic obstructive
3
According to Master and et.al., (2018) aboriginal and Torres Strait Island peoples are
Australian people who have achieved nationality of Australia. These are two type people such as
aboriginal people who are known as indigenous people while Torres Strait Islander people who
lives in North Australia. But both type peoples have poor living condition as compared other
Australian people. These type people have high infant mortality rate and poor life expectancy
instead of other Australian population. Authors have highlighted in their published books that
aboriginal and Torres Strait Islanders have minimum literacy ratio while drug and alcohol
consumption are too high which is the major reason less life expectancy rate. Due to weak
educational level, such people unable to get good job that brings poverty which often bring
domestic violence as compared non-indigenous. Aboriginal and Torres Strait Islanders lives in
rural areas of Australia associated with poor nutrition, malnutrition, type of diabetes, tooth decay
and various type of cancers. Due to wide distance between rural and urban area of Australia it
has very limited transportation of suppliers and high cost as well. Such difference leads wide cost
difference around 150 to 180% of items that is not possible for the aboriginal to pay. Such people
consume high level of Tobacco that is another leading risk factor for illness. So around 50 to
60% aboriginal and Torres Strait Islander people are hospitalized as compared non-aboriginal
people.
In this essay will discuss over health issue experiences of aboriginal and Torres Strait
Islander people. Then it will further be evaluated contemporary healthcare strategy to increase
health issue experience of Aboriginal and Torres Strait Islander. Demographical and socio-
cultural factors impact over health issue of aboriginal and Torres Strait Islander will discuss in
this report.
MAIN BODY
Health issue experienced by Aboriginal and Torres Strait Islander people
A major health issue prevalent in the community of Aboriginal and Torres Strait Islander
people in Australia is respiratory disease. The respiratory system consists of those parts of the
human body which are involved in breathing, such as throat, nose, trachea, larynx and lungs.
Respiratory disease happens when any of these body parts get damaged and impact breathing
process. Common diseases include pneumonia, asthma and COPD (chronic obstructive
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
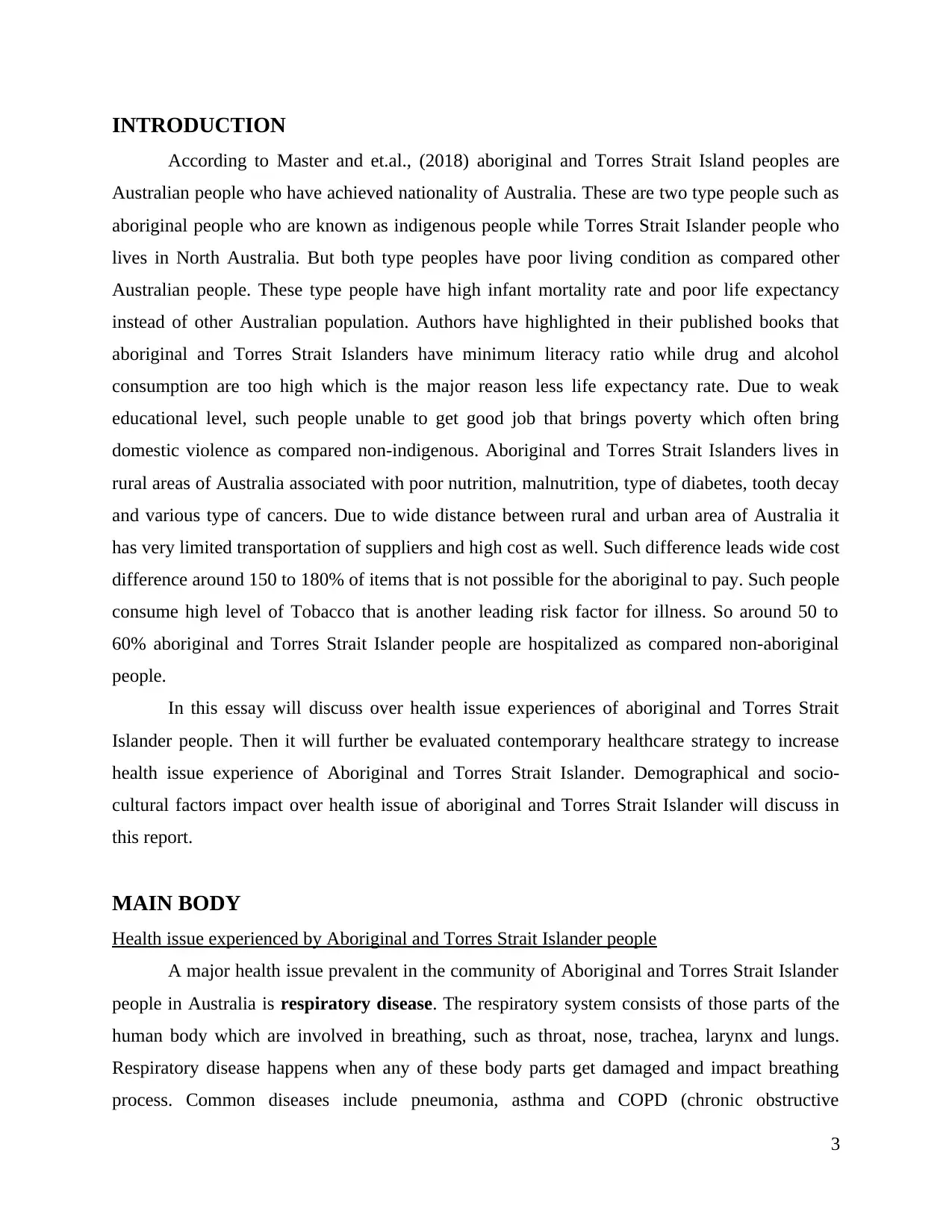
pulmonary disease). About one-third of Aboriginal and Torres Strait Islander people face one or
more respiratory conditions, most common of which is Asthma. The diseases are twice as likely
to impact the indigenous community than non-indigenous people of Australia (O'Grady and et.al
2018).
Figure 1: Cause of death due to respiratory diseases
Source: AIHW, 2017
Higher rates of pneumonia are linked to factors like smoking and alcohol, poor living
conditions, untreated respiratory diseases, malnutrition etc. Indigenous children in the Northern
Territory have the highest rates of radiologically confirmed pneumonia in the world. Asthma can
impact on bodily functions and attendance at work or school. It generally coexists with various
chronic conditions and lower socio-economic status. The risk of death from asthma tends to
increase with age. COPD, a serious lung disease primarily affects aged people and is linked to
4
more respiratory conditions, most common of which is Asthma. The diseases are twice as likely
to impact the indigenous community than non-indigenous people of Australia (O'Grady and et.al
2018).
Figure 1: Cause of death due to respiratory diseases
Source: AIHW, 2017
Higher rates of pneumonia are linked to factors like smoking and alcohol, poor living
conditions, untreated respiratory diseases, malnutrition etc. Indigenous children in the Northern
Territory have the highest rates of radiologically confirmed pneumonia in the world. Asthma can
impact on bodily functions and attendance at work or school. It generally coexists with various
chronic conditions and lower socio-economic status. The risk of death from asthma tends to
increase with age. COPD, a serious lung disease primarily affects aged people and is linked to
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
environmental pollutants, smoking, diseases incurred in childhood etc. Presently, 42% of
Indigenous Australians above the age of 15 tend to do excessive smoking, 2.7 times more the
non-Indigenous people (AIHW, 2017). COPD is attributed by chronic obstruction of airflow to
lungs which interferes with breathing (HealthInfoNet and et.al., 2020).
According to Aboriginal and Torres Strait Islander health performance framework 2017,
the morbidity and mortality rate of Indigenous Australians is higher in case of respiratory
illnesses like asthma, emphysema, bronchitis, invasive pneumococcal disease and pneumonia
than other Australians. As per a more recent study, respiratory diseases accounted for 8% out of
the total burden of disease, i.e. impact of the disease on Aboriginal and Torres Strait Islander
people (AIHW, 2017).
Diseases like Asthma, bronchiectasis, COPD, emphysema and bronchitis, which are termed as
chronic lower respiratory diseases were the third leading cause of death in Aboriginal and Torres
Strait Islander people.
Contemporary healthcare strategy to improve respiratory health of Aboriginal and Torres Strait
Islander people
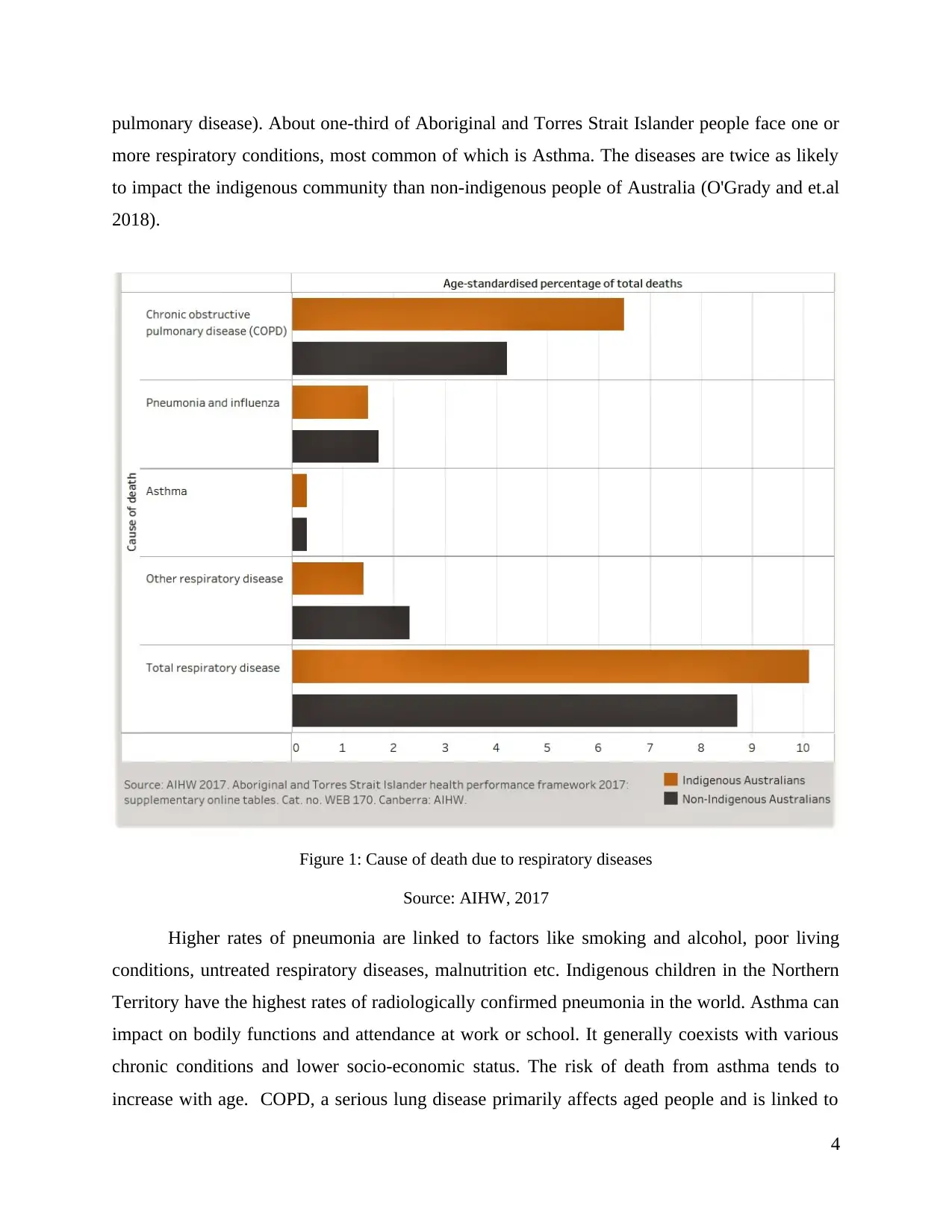
A contemporary health strategy and initiatives that address the problems of
immunisation, active and passive smoking, living conditions, chronic diseases, overcrowding,
hospitalisation and access to health care contribute towards the developments in tackling the
respiratory diseases. Studies show that an integrated COPD community service of
multidisciplinary nature help in reducing the respiratory hospitalisations in the long-term.
Working along with the indigenous staff and communities have helped in the development of the
reach of healthcare services by delivering accessible and culturally appropriate respiratory
services. IAPH or the Indigenous Australians' Health Program concentrates on early detection,
prevention and proper management of chronic respiratory diseases by expanding the access and
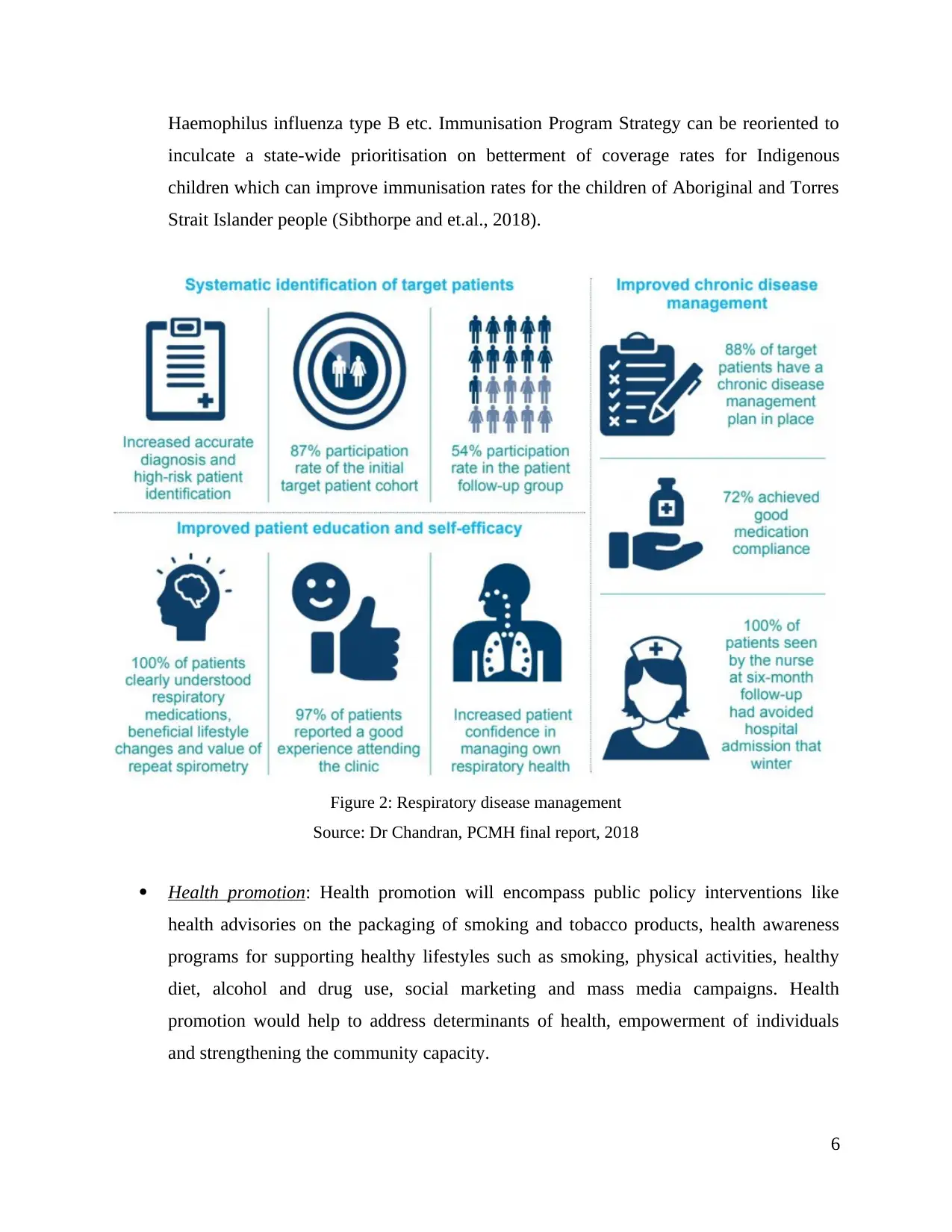
cooperation of a comprehensive primary health care. A systematic respiratory disease
management can be conducted as illustrated in the given diagram (PCMH final report, 2018).
Other safety procedures that need to be taken are as follows:
Immunisation: Immunisation is very effective in reducing mortality rates caused by
vaccine preventable diseases like seasonal influenza, invasive pneumococcal disease,
5
Indigenous Australians above the age of 15 tend to do excessive smoking, 2.7 times more the
non-Indigenous people (AIHW, 2017). COPD is attributed by chronic obstruction of airflow to
lungs which interferes with breathing (HealthInfoNet and et.al., 2020).
According to Aboriginal and Torres Strait Islander health performance framework 2017,
the morbidity and mortality rate of Indigenous Australians is higher in case of respiratory
illnesses like asthma, emphysema, bronchitis, invasive pneumococcal disease and pneumonia
than other Australians. As per a more recent study, respiratory diseases accounted for 8% out of
the total burden of disease, i.e. impact of the disease on Aboriginal and Torres Strait Islander
people (AIHW, 2017).
Diseases like Asthma, bronchiectasis, COPD, emphysema and bronchitis, which are termed as
chronic lower respiratory diseases were the third leading cause of death in Aboriginal and Torres
Strait Islander people.
Contemporary healthcare strategy to improve respiratory health of Aboriginal and Torres Strait
Islander people
A contemporary health strategy and initiatives that address the problems of
immunisation, active and passive smoking, living conditions, chronic diseases, overcrowding,
hospitalisation and access to health care contribute towards the developments in tackling the
respiratory diseases. Studies show that an integrated COPD community service of
multidisciplinary nature help in reducing the respiratory hospitalisations in the long-term.
Working along with the indigenous staff and communities have helped in the development of the
reach of healthcare services by delivering accessible and culturally appropriate respiratory
services. IAPH or the Indigenous Australians' Health Program concentrates on early detection,
prevention and proper management of chronic respiratory diseases by expanding the access and
cooperation of a comprehensive primary health care. A systematic respiratory disease
management can be conducted as illustrated in the given diagram (PCMH final report, 2018).
Other safety procedures that need to be taken are as follows:
Immunisation: Immunisation is very effective in reducing mortality rates caused by
vaccine preventable diseases like seasonal influenza, invasive pneumococcal disease,
5
Haemophilus influenza type B etc. Immunisation Program Strategy can be reoriented to
inculcate a state-wide prioritisation on betterment of coverage rates for Indigenous
children which can improve immunisation rates for the children of Aboriginal and Torres
Strait Islander people (Sibthorpe and et.al., 2018).
Figure 2: Respiratory disease management
Source: Dr Chandran, PCMH final report, 2018
Health promotion: Health promotion will encompass public policy interventions like
health advisories on the packaging of smoking and tobacco products, health awareness
programs for supporting healthy lifestyles such as smoking, physical activities, healthy
diet, alcohol and drug use, social marketing and mass media campaigns. Health
promotion would help to address determinants of health, empowerment of individuals
and strengthening the community capacity.
6
inculcate a state-wide prioritisation on betterment of coverage rates for Indigenous
children which can improve immunisation rates for the children of Aboriginal and Torres
Strait Islander people (Sibthorpe and et.al., 2018).
Figure 2: Respiratory disease management
Source: Dr Chandran, PCMH final report, 2018
Health promotion: Health promotion will encompass public policy interventions like
health advisories on the packaging of smoking and tobacco products, health awareness
programs for supporting healthy lifestyles such as smoking, physical activities, healthy
diet, alcohol and drug use, social marketing and mass media campaigns. Health
promotion would help to address determinants of health, empowerment of individuals
and strengthening the community capacity.
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Early detection and treatment: Health check-ups, provision of Pharmaceutical Benefits
Scheme (PBS), additional MBS. Improvements in the follow-up of abnormal clinical
diagnosis and easy availability of referral services for achieving benefits of screening
programmes and health assessments. National Aboriginal and Torres Strait Islander
Health Plan and the Indigenous Australians’ Health Programme should emphasise more
upon respiratory diseases and the rate of health assessments for various age groups in
years has to be monitored (Hall, 2017).
Chronic disease management: Proper management of chronic diseases may delay the
progression of respiratory diseases, decrease high cost interventions which in turn
improve net savings, improvement in quality of life, increase in life expectancy and
accessibility to hospital procedures. PHC can conduct functions like transparent systems
in context on written diseases management, manuals and guidelines for regulation, proper
staffing and training policy, dedicated staff, intensive follow up procedures, recall and
reminder practices, patient centred approaches etc.
Impact of demographic and socio-cultural factors on respiratory health issues
Demographic and socio-cultural factors that have an effect on the health issue of
respiratory diseases among Aboriginal and Torres Strait Islander people are:
Low literacy rate and poor education are associated to poor health status, impacting the
capacity of people to use health information;
Low levels of income decrease the accessibility of medicines, diagnostic tests and health
care services.
Overcrowded and cramped up housing is linked to poverty and contributes in spreading
communicable respiratory diseases like Tuberculosis;
Bad infant diet and malnutrition leads to chronic diseases in later stages of life; and
Smoking and high-risk behaviour which is prevalent in indigenous community is linked
to diseases like lung cancer and chronic obstructive pulmonary diseases (Carson and
et.al., 2020).
7
Scheme (PBS), additional MBS. Improvements in the follow-up of abnormal clinical
diagnosis and easy availability of referral services for achieving benefits of screening
programmes and health assessments. National Aboriginal and Torres Strait Islander
Health Plan and the Indigenous Australians’ Health Programme should emphasise more
upon respiratory diseases and the rate of health assessments for various age groups in
years has to be monitored (Hall, 2017).
Chronic disease management: Proper management of chronic diseases may delay the
progression of respiratory diseases, decrease high cost interventions which in turn
improve net savings, improvement in quality of life, increase in life expectancy and
accessibility to hospital procedures. PHC can conduct functions like transparent systems
in context on written diseases management, manuals and guidelines for regulation, proper
staffing and training policy, dedicated staff, intensive follow up procedures, recall and
reminder practices, patient centred approaches etc.
Impact of demographic and socio-cultural factors on respiratory health issues
Demographic and socio-cultural factors that have an effect on the health issue of
respiratory diseases among Aboriginal and Torres Strait Islander people are:
Low literacy rate and poor education are associated to poor health status, impacting the
capacity of people to use health information;
Low levels of income decrease the accessibility of medicines, diagnostic tests and health
care services.
Overcrowded and cramped up housing is linked to poverty and contributes in spreading
communicable respiratory diseases like Tuberculosis;
Bad infant diet and malnutrition leads to chronic diseases in later stages of life; and
Smoking and high-risk behaviour which is prevalent in indigenous community is linked
to diseases like lung cancer and chronic obstructive pulmonary diseases (Carson and
et.al., 2020).
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

The factors which influence the health behaviour Indigenous Australians are driven by
control of the individual, perceived behavioural control and attitudes towards the behaviour. In
certain circumstances, the social disruption can be associated with historical or past which
promote health risk factors and behaviours. Specifically, tobacco smoking, active as well as
passive smoking and alcohol abuse can be associated with social disruptions, and the stress in the
daily lives of the indigenous people may accelerate health risk behavioural practices like tobacco
smoking. Along with that, it has been determined that social networks and racism can promote
health risk behaviours like smoking (Oakley, 2020).
At the time of Australia’s colonisation, racism was pervasive. Indigenous people were
coerced into living on reserves and in missions where freedom to socialise with friends and
relatives, hunting, practicing traditional rituals, and even marriage was restricted. Policies to
segregate and assimilate had been introduced as well as geographical restrictions and
institutionalisation. In few instances, Aboriginal and Torres Strait Islander people were restricted
to practice their culture, speak their traditional language and conveying history and traditions to
their children.
Such restrictions and conflicts which are linked to colonisation eventually led to loss of
lives and liberties and changed indigenous people’s social and cultural behaviour.
Economic and social circumstances such as unemployment and economic hardships reduced the
financial or monetary resources for Aboriginal and Torres Strait Islander people to avail funds
for health and medical needs. These economic challenges led to distress and also impacted the
psychological behaviour of overall health of the people. The results of these instances prevented
health being a priority for these people (Calma, Dudgeon and Bray, 2017). Inadequate, cramped
up accommodations were determined as general hindrances to positive health behaviour. Living
in overcrowded houses led to compromising of many aspects of health like nutrition. It can be
concluded that engagement of health risk attitudes which were considered coping mechanisms,
brought a detrimental effect on the health of the Aboriginal and Torres Strait Islander people.
8
control of the individual, perceived behavioural control and attitudes towards the behaviour. In
certain circumstances, the social disruption can be associated with historical or past which
promote health risk factors and behaviours. Specifically, tobacco smoking, active as well as
passive smoking and alcohol abuse can be associated with social disruptions, and the stress in the
daily lives of the indigenous people may accelerate health risk behavioural practices like tobacco
smoking. Along with that, it has been determined that social networks and racism can promote
health risk behaviours like smoking (Oakley, 2020).
At the time of Australia’s colonisation, racism was pervasive. Indigenous people were
coerced into living on reserves and in missions where freedom to socialise with friends and
relatives, hunting, practicing traditional rituals, and even marriage was restricted. Policies to
segregate and assimilate had been introduced as well as geographical restrictions and
institutionalisation. In few instances, Aboriginal and Torres Strait Islander people were restricted
to practice their culture, speak their traditional language and conveying history and traditions to
their children.
Such restrictions and conflicts which are linked to colonisation eventually led to loss of
lives and liberties and changed indigenous people’s social and cultural behaviour.
Economic and social circumstances such as unemployment and economic hardships reduced the
financial or monetary resources for Aboriginal and Torres Strait Islander people to avail funds
for health and medical needs. These economic challenges led to distress and also impacted the
psychological behaviour of overall health of the people. The results of these instances prevented
health being a priority for these people (Calma, Dudgeon and Bray, 2017). Inadequate, cramped
up accommodations were determined as general hindrances to positive health behaviour. Living
in overcrowded houses led to compromising of many aspects of health like nutrition. It can be
concluded that engagement of health risk attitudes which were considered coping mechanisms,
brought a detrimental effect on the health of the Aboriginal and Torres Strait Islander people.
8
Effective program model of practices from healthcare perspective acceptable to Aboriginal and
Torres Strait Islander people
Practices for helping patients experiencing respiratory diseases can include:
Dealing with indigenous smoking practices and deploying outreach workforce from
AMSs and primary healthcare services.
Proper General Practice (GP) health assessments which are funded by MBS for the
indigenous Australians should include a follow-on care.
Funding can be allotted to incentive payments in order to improve chronic respiratory
disease management and ensuring more availability of cheaper generic medicines through
Pharmaceuticals Benefits scheme.
National Health Asthma Strategy for indigenous Australians being the priority has to be
developed (Davy and et.al., 2016).
Features of Indigenous primary health care service delivery models:
1. Accessible Health Services: Provision of affordable health care services at low cost,
ensuring that a wide range of services are available in multiple locations along with
higher walk-in appointment facilities, open hours and transport. Awareness in indigenous
communities regarding mobile services and outreach, screening days and participation in
community events.
2. Community participation: To ensure indigenous ownership in health services which lets people
manage services on their own to ensure accountability within the community. Establishment of
indigenous governance to encourage involvement of local community, providing community
consultation, collaboration and engagement, involving role of elders in overall governance.
3. Continuous quality improvement: Collection and utilisation of data for evaluating program for
needs for indigenous people apart from improving health results, reporting and evaluation of
performance, participation in initiates for development, identification of patients requiring special
service, client-tacking and follow-up, assessment of economic outcomes, disease plans,
monitoring healthcare plans etc.
4. Culturally appropriate and skilled workforce: Employment of skilled workforce as well as
indigenous staff as social workers, health workers, doctors, nurses, traditional healers and
managers. Training and development programs for the staff like capacity building practices and
aiming at building an indigenous workforce for future.
9
Torres Strait Islander people
Practices for helping patients experiencing respiratory diseases can include:
Dealing with indigenous smoking practices and deploying outreach workforce from
AMSs and primary healthcare services.
Proper General Practice (GP) health assessments which are funded by MBS for the
indigenous Australians should include a follow-on care.
Funding can be allotted to incentive payments in order to improve chronic respiratory
disease management and ensuring more availability of cheaper generic medicines through
Pharmaceuticals Benefits scheme.
National Health Asthma Strategy for indigenous Australians being the priority has to be
developed (Davy and et.al., 2016).
Features of Indigenous primary health care service delivery models:
1. Accessible Health Services: Provision of affordable health care services at low cost,
ensuring that a wide range of services are available in multiple locations along with
higher walk-in appointment facilities, open hours and transport. Awareness in indigenous
communities regarding mobile services and outreach, screening days and participation in
community events.
2. Community participation: To ensure indigenous ownership in health services which lets people
manage services on their own to ensure accountability within the community. Establishment of
indigenous governance to encourage involvement of local community, providing community
consultation, collaboration and engagement, involving role of elders in overall governance.
3. Continuous quality improvement: Collection and utilisation of data for evaluating program for
needs for indigenous people apart from improving health results, reporting and evaluation of
performance, participation in initiates for development, identification of patients requiring special
service, client-tacking and follow-up, assessment of economic outcomes, disease plans,
monitoring healthcare plans etc.
4. Culturally appropriate and skilled workforce: Employment of skilled workforce as well as
indigenous staff as social workers, health workers, doctors, nurses, traditional healers and
managers. Training and development programs for the staff like capacity building practices and
aiming at building an indigenous workforce for future.
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

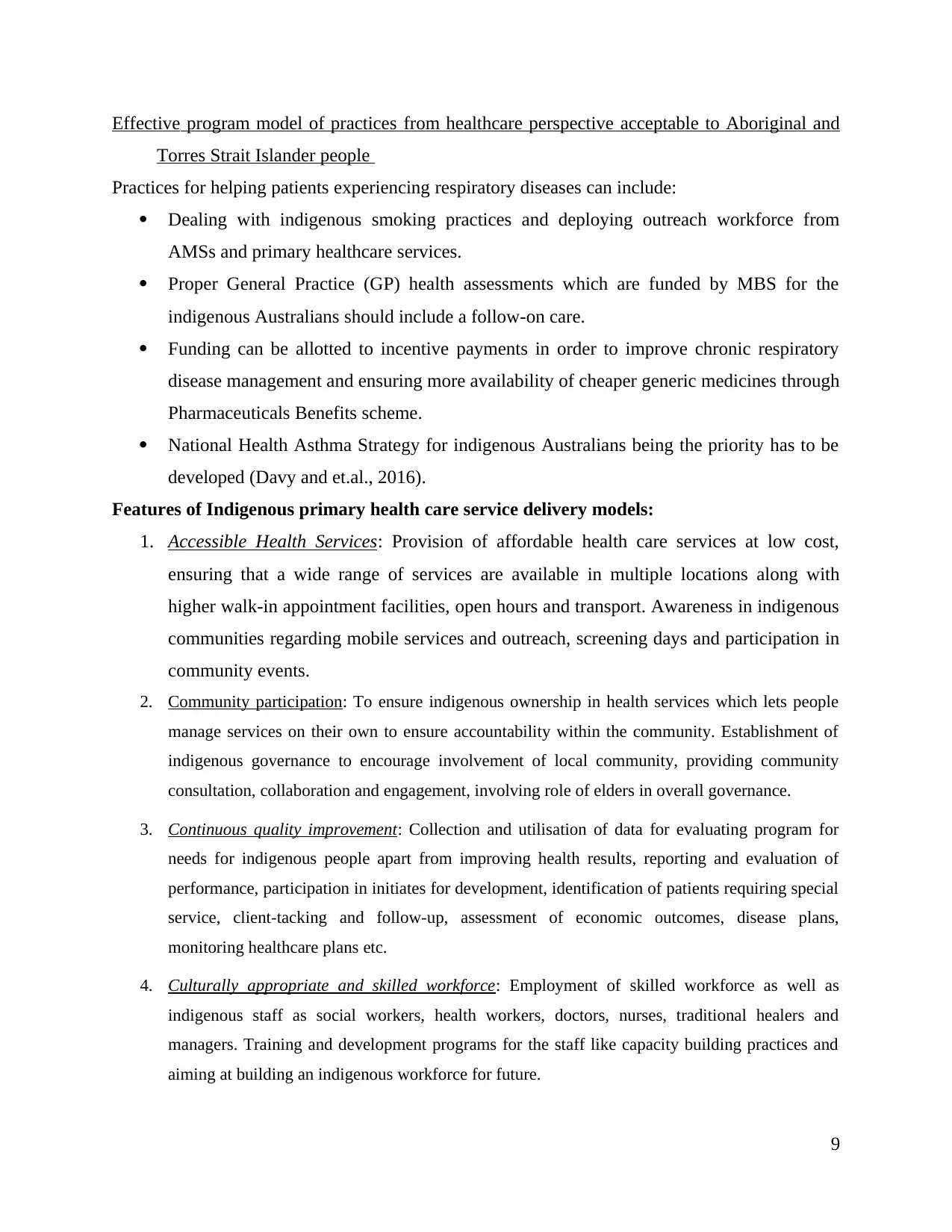
Figure 3: Characteristics of Indigenous Primary Health Care Service Delivery Model
Source: Harfield et al. Globalization and Health (2018)
5. Flexible approaches to care: Devising approaches to determine and meet the requirements of the
local community by delivering a wide range of healthcare services. Integration of health care with
multidisciplinary group approach, case management, care and other support services.
6. Holistic health care: Comprehensive and holistic primary healthcare services for individual as
well as family well-being including emotional, mental, physical health and spiritual needs.
Prevention programmes like healthy diet and lifestyle, injury prevention, smoking cessation
programs etc. along with improving health literacy among people and public health initiatives.
7. Self-determination and empowerment: Facilitation of indigenous healthcare services, employment
and training, leadership opportunities and promotion of social connectedness and community
development through camps, cultural days, reconciliation events etc (Harfield and et.al., 2018).
10
Source: Harfield et al. Globalization and Health (2018)
5. Flexible approaches to care: Devising approaches to determine and meet the requirements of the
local community by delivering a wide range of healthcare services. Integration of health care with
multidisciplinary group approach, case management, care and other support services.
6. Holistic health care: Comprehensive and holistic primary healthcare services for individual as
well as family well-being including emotional, mental, physical health and spiritual needs.
Prevention programmes like healthy diet and lifestyle, injury prevention, smoking cessation
programs etc. along with improving health literacy among people and public health initiatives.
7. Self-determination and empowerment: Facilitation of indigenous healthcare services, employment
and training, leadership opportunities and promotion of social connectedness and community
development through camps, cultural days, reconciliation events etc (Harfield and et.al., 2018).
10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

CONCLUSION
This essay fully dependent on aboriginal and Torres Strait Islander people’s health issues
and used different strategies to decrease health issues in them. HealthInfoNet and et.al., (2020)
have discussed about health issue experience that achieves by aboriginal and Torres Strait
Islander people through their published research papers. Aboriginal and Torres Strait Islander
people are highly suffered from respiratory disease because they consume high quantity alcohol
and smokes. Awareness in people about aboriginal and Torres Strait Islander people and their
disease will support to redeem their life. Prentice, Blair and O’Mullan, (2017) have mentioned in
his published article that there are various risk leading factors like Tobacco, Alcohol, drugs and
domestic violence which have reduced life expectancy in such people. It is important for the
Australian government and non-aboriginal people to give them effective education services and
health care services that have concluded in this essay. As per the view of HealthInfoNet, (2020)
different healthcare strategy decreases health issues like respiratory illness in aboriginal and
Torres Strait Islander as well as decreases death ratio. This information has provided above
which will support to take effective actions for the indigenous people. However, other Macniven
and et.al., (2017) have highlighted about effective program models of practices accordingly
healthcare aspect of aboriginal and Torres Strait Islander in their published articles. This
information will support Australian government and other non-aboriginal people to take effective
actions in their practices.
11
This essay fully dependent on aboriginal and Torres Strait Islander people’s health issues
and used different strategies to decrease health issues in them. HealthInfoNet and et.al., (2020)
have discussed about health issue experience that achieves by aboriginal and Torres Strait
Islander people through their published research papers. Aboriginal and Torres Strait Islander
people are highly suffered from respiratory disease because they consume high quantity alcohol
and smokes. Awareness in people about aboriginal and Torres Strait Islander people and their
disease will support to redeem their life. Prentice, Blair and O’Mullan, (2017) have mentioned in
his published article that there are various risk leading factors like Tobacco, Alcohol, drugs and
domestic violence which have reduced life expectancy in such people. It is important for the
Australian government and non-aboriginal people to give them effective education services and
health care services that have concluded in this essay. As per the view of HealthInfoNet, (2020)
different healthcare strategy decreases health issues like respiratory illness in aboriginal and
Torres Strait Islander as well as decreases death ratio. This information has provided above
which will support to take effective actions for the indigenous people. However, other Macniven
and et.al., (2017) have highlighted about effective program models of practices accordingly
healthcare aspect of aboriginal and Torres Strait Islander in their published articles. This
information will support Australian government and other non-aboriginal people to take effective
actions in their practices.
11
REFERENCES
Books and Journals
Calma, T., Dudgeon, P. and Bray, A., 2017. Aboriginal and Torres Strait Islander social and
emotional wellbeing and mental health. Australian Psychologist, 52(4). pp.255-260.
Carson, B., and et.al., 2020. Social determinants of Indigenous health. Routledge.
Davy, C., and et.al., 2016. Access to primary health care services for Indigenous peoples: A
framework synthesis. International journal for equity in health. 15(1). p.163.
Hall, K.K., 2017. Acute respiratory illness in urban Aboriginal and Torres Strait Islander
children (Doctoral dissertation, Queensland University of Technology).
Harfield, S.G., and et.al., 2018. Characteristics of Indigenous primary health care service
delivery models: a systematic scoping review. Globalization and health. 14(1). p.12.
HealthInfoNet, A.I and et.al., 2020. Overview of Aboriginal and Torres Strait Islander health
status 2019.
HealthInfoNet, A.I., 2020. Summary of nutrition among Aboriginal and Torres Strait Islander
people.
HealthInfoNet, A.I., and et.al., 2020. Overview of Aboriginal and Torres Strait Islander health
status 2019.
Macniven, R and et.al., 2017. A snapshot of physical activity programs targeting Aboriginal and
Torres Strait Islander people in Australia. Health Promotion Journal of Australia, 28(3),
pp.185-206.
Master, B.J and et.al., 2018. " I want to be heard": an analysis of needs of Aboriginal and Torres
Strait Islander illegal drug users in the ACT and region for treatment and other services.
Community Report. " I want to be heard": an analysis of needs of Aboriginal and Torres
Strait Islander illegal drug users in the ACT and region for treatment and other services.
Oakley, G., 2020. HLSC120 Assessment 1-What health disparities are faced by Aboriginal and
Torres Strait Islander people?. Essa. p.2021.
O'Grady, K.A.F., and et.al 2018. Review of respiratory disease among Aboriginal and Torres
Strait Islander children. Australian Indigenous HealthBulletin, 18(2).
Prentice, K., Blair, B. and O’Mullan, C., 2017. Sexual and family violence: Overcoming barriers
to service access for Aboriginal and Torres Strait Islander clients. Australian social
work.70(2). pp.241-252.
Sibthorpe, B., and et.al., 2018. Impacts of continuous quality improvement in Aboriginal and
Torres Strait islander primary health care in Australia. Journal of health organization and
management.
Online
Cause of death due to respiratory diseases, AIHW, 2017, Available through:
<https://www.aihw.gov.au/reports/indigenous-health-welfare/health-performance-
framework/contents/tier-1-health-status-and-outcomes/1-04-respiratory-disease>
Respiratory disease management, Dr Chandran , PCMH final report, 2018, Available through:
<https://www.coordinare.org.au/about-us/showcasing-our-success/respiratory-disease-
management-clinic/>
12
Books and Journals
Calma, T., Dudgeon, P. and Bray, A., 2017. Aboriginal and Torres Strait Islander social and
emotional wellbeing and mental health. Australian Psychologist, 52(4). pp.255-260.
Carson, B., and et.al., 2020. Social determinants of Indigenous health. Routledge.
Davy, C., and et.al., 2016. Access to primary health care services for Indigenous peoples: A
framework synthesis. International journal for equity in health. 15(1). p.163.
Hall, K.K., 2017. Acute respiratory illness in urban Aboriginal and Torres Strait Islander
children (Doctoral dissertation, Queensland University of Technology).
Harfield, S.G., and et.al., 2018. Characteristics of Indigenous primary health care service
delivery models: a systematic scoping review. Globalization and health. 14(1). p.12.
HealthInfoNet, A.I and et.al., 2020. Overview of Aboriginal and Torres Strait Islander health
status 2019.
HealthInfoNet, A.I., 2020. Summary of nutrition among Aboriginal and Torres Strait Islander
people.
HealthInfoNet, A.I., and et.al., 2020. Overview of Aboriginal and Torres Strait Islander health
status 2019.
Macniven, R and et.al., 2017. A snapshot of physical activity programs targeting Aboriginal and
Torres Strait Islander people in Australia. Health Promotion Journal of Australia, 28(3),
pp.185-206.
Master, B.J and et.al., 2018. " I want to be heard": an analysis of needs of Aboriginal and Torres
Strait Islander illegal drug users in the ACT and region for treatment and other services.
Community Report. " I want to be heard": an analysis of needs of Aboriginal and Torres
Strait Islander illegal drug users in the ACT and region for treatment and other services.
Oakley, G., 2020. HLSC120 Assessment 1-What health disparities are faced by Aboriginal and
Torres Strait Islander people?. Essa. p.2021.
O'Grady, K.A.F., and et.al 2018. Review of respiratory disease among Aboriginal and Torres
Strait Islander children. Australian Indigenous HealthBulletin, 18(2).
Prentice, K., Blair, B. and O’Mullan, C., 2017. Sexual and family violence: Overcoming barriers
to service access for Aboriginal and Torres Strait Islander clients. Australian social
work.70(2). pp.241-252.
Sibthorpe, B., and et.al., 2018. Impacts of continuous quality improvement in Aboriginal and
Torres Strait islander primary health care in Australia. Journal of health organization and
management.
Online
Cause of death due to respiratory diseases, AIHW, 2017, Available through:
<https://www.aihw.gov.au/reports/indigenous-health-welfare/health-performance-
framework/contents/tier-1-health-status-and-outcomes/1-04-respiratory-disease>
Respiratory disease management, Dr Chandran , PCMH final report, 2018, Available through:
<https://www.coordinare.org.au/about-us/showcasing-our-success/respiratory-disease-
management-clinic/>
12
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





