NURS 9123 - Obesity and Heart Failure: Epidemiology, Clinical Study
VerifiedAdded on 2023/06/11
|12
|12738
|352
Essay
AI Summary
This essay provides a comprehensive overview of the relationship between obesity and heart failure, drawing upon epidemiological studies and clinical research. It begins by defining obesity based on BMI and discussing the global prevalence of heart failure. The essay then explores the pathophysiology of obesity-related heart failure, including hemodynamic alterations and neurohormonal abnormalities. It examines the 'obesity paradox,' where overweight and moderately obese individuals with heart failure exhibit lower mortality rates compared to normal weight or underweight individuals. The role of weight loss in reversing cardiac abnormalities and improving outcomes is also discussed. The essay highlights the importance of understanding the complex interplay between obesity and heart failure for effective clinical management. The assignment also includes a section on determinants of health and an understanding of epidemiological and statistical terms used in the chosen articles.
REVIEW ARTICLE
Obesity and heart failure: epidemiology,
pathophysiology, clinicalmanifestations,
and managementQ1
Q17 MARTIN A. ALPERT, CARL J. LAVIE, HARSH AGRAWAL, KUL B. AGGARWAL, and
SENTHIL A. KUMAR
COLUMBIA, MISSOURI; AND NEW ORLEANS, LOUISIANA
Obesity is a risk factor for heart failure (HF) in both men and women. The mortality risk
of overweight and class I and II obese adults with HF is lower than that ofnormal
weight or underweight adults with HF of comparable severity, a phenomenon
referred to as the obesity paradox. Severe obesity produces hemodynamic alter-
ations that predispose to changes in cardiac morphology and ventricular function,
which may lead to the development of HF. The presence of systemic hypertension,
sleep apnea, and hypoventilation, comorbidities that occur commonly with severe
obesity, may contribute to HF in such patients. The resultant syndrome is known as
obesity cardiomyopathy. Substantial weight loss in severely obese persons is
capable of reversing mostobesity-related abnormalities ofcardiac performance
and morphology and improving the clinical manifestations of obesity cardiomyopa-
thy. (Translational Research 2014;-:1–12)
Abbreviations: --- ¼ ---Q2
INTRODUCTIONQ3
O besity is both a risk factor for and a direct
cause of heart failure (HF) and is associated
with a varietyof adversehemodynamic
changesthatpredispose to cardiac remodeling and
ventricular dysfunction.1-3 These alterations are most
pronouncedin severelyobese personsand may
predispose to the developmentof HF, even in the
absenceof comorbiditiessuch as coronaryartery
disease(CAD), valvularheartdisease,pericardial
disease,and congenitalheartdisease.1,2 Recently,a
variety of neurohormonal and metabolic abnormalities
associatedwith obesityhave been identifiedthat
may contributeto cardiacremodeling,ventricular
dysfunction,and subsequentHF.1,3 In this review,we
describe the epidemiology, pathophysiology, and clinical
manifestations of HF as they relate to obesity in adults.
We also discuss the managementof HF attributable to
severe obesity with specialemphasison the role of
purposeful weight loss.
DEFINITIONS
The World Health Organization (WHO) classifies obesity
in termsof body massindex(BMI).4 The WHO
From the Division of CardiovascularMedicine,Universityof
Missouri,Columbia,Missouri;Departmentof Cardiology,John
Ochsner Heart and Vascular Institute, New Orleans, Louisiana.
Conflict of interests: None.
Editorial support: None.
Submitted for publication January 30, 2014; revision submitted April
10, 2014; accepted for publication April 12, 2014.
Reprintrequests:Martin A.Alpert,University of Missouri,Health
Sciences Center,Room CE-338,5 HospitalDrive,Columbia,MO
65212; e-mail: malpert815@yahoo.com.
1931-5244/$ - see front matter
Ó 2014 Mosby, Inc. All rights reserved.
http://dx.doi.org/10.1016/j.trsl.2014.04.010
1
REV 5.2.0 DTD TRSL776_proof 6 May 2014 3:36 pm ce
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
55
56
57
58
59
60
61
62
63
64
65
66
67
68
69
70
71
72
73
74
75
76
77
78
79
80
81
82
83
84
85
86
87
88
89
90
91
92
93
94
95
96
97
98
99
100
101
102
103
104
105
106
107
108
109
110
111
112
113
114
115
116
117
118
119
120
121
122
123
124
125
126
127
128
Obesity and heart failure: epidemiology,
pathophysiology, clinicalmanifestations,
and managementQ1
Q17 MARTIN A. ALPERT, CARL J. LAVIE, HARSH AGRAWAL, KUL B. AGGARWAL, and
SENTHIL A. KUMAR
COLUMBIA, MISSOURI; AND NEW ORLEANS, LOUISIANA
Obesity is a risk factor for heart failure (HF) in both men and women. The mortality risk
of overweight and class I and II obese adults with HF is lower than that ofnormal
weight or underweight adults with HF of comparable severity, a phenomenon
referred to as the obesity paradox. Severe obesity produces hemodynamic alter-
ations that predispose to changes in cardiac morphology and ventricular function,
which may lead to the development of HF. The presence of systemic hypertension,
sleep apnea, and hypoventilation, comorbidities that occur commonly with severe
obesity, may contribute to HF in such patients. The resultant syndrome is known as
obesity cardiomyopathy. Substantial weight loss in severely obese persons is
capable of reversing mostobesity-related abnormalities ofcardiac performance
and morphology and improving the clinical manifestations of obesity cardiomyopa-
thy. (Translational Research 2014;-:1–12)
Abbreviations: --- ¼ ---Q2
INTRODUCTIONQ3
O besity is both a risk factor for and a direct
cause of heart failure (HF) and is associated
with a varietyof adversehemodynamic
changesthatpredispose to cardiac remodeling and
ventricular dysfunction.1-3 These alterations are most
pronouncedin severelyobese personsand may
predispose to the developmentof HF, even in the
absenceof comorbiditiessuch as coronaryartery
disease(CAD), valvularheartdisease,pericardial
disease,and congenitalheartdisease.1,2 Recently,a
variety of neurohormonal and metabolic abnormalities
associatedwith obesityhave been identifiedthat
may contributeto cardiacremodeling,ventricular
dysfunction,and subsequentHF.1,3 In this review,we
describe the epidemiology, pathophysiology, and clinical
manifestations of HF as they relate to obesity in adults.
We also discuss the managementof HF attributable to
severe obesity with specialemphasison the role of
purposeful weight loss.
DEFINITIONS
The World Health Organization (WHO) classifies obesity
in termsof body massindex(BMI).4 The WHO
From the Division of CardiovascularMedicine,Universityof
Missouri,Columbia,Missouri;Departmentof Cardiology,John
Ochsner Heart and Vascular Institute, New Orleans, Louisiana.
Conflict of interests: None.
Editorial support: None.
Submitted for publication January 30, 2014; revision submitted April
10, 2014; accepted for publication April 12, 2014.
Reprintrequests:Martin A.Alpert,University of Missouri,Health
Sciences Center,Room CE-338,5 HospitalDrive,Columbia,MO
65212; e-mail: malpert815@yahoo.com.
1931-5244/$ - see front matter
Ó 2014 Mosby, Inc. All rights reserved.
http://dx.doi.org/10.1016/j.trsl.2014.04.010
1
REV 5.2.0 DTD TRSL776_proof 6 May 2014 3:36 pm ce
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
55
56
57
58
59
60
61
62
63
64
65
66
67
68
69
70
71
72
73
74
75
76
77
78
79
80
81
82
83
84
85
86
87
88
89
90
91
92
93
94
95
96
97
98
99
100
101
102
103
104
105
106
107
108
109
110
111
112
113
114
115
116
117
118
119
120
121
122
123
124
125
126
127
128
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
classification is as follows: underweight (BMI , 18.5 kg/
m2), normal weight (BMI: 18.5–24.9 kg/m2), overweight
(BMI: 25.0–29.9 kg/m2), classI obesity (BMI:30.0–
34.9 kg/m2), class II obesity (BMI: 35.0–39.9 kg/m2), and
class III obesity (BMI $ 40 kg/m2).4 In recent years the
term ‘‘superobesity’’ has been used to characterize those
whose BMIis $50 kg/m2.5,6 For the purpose ofthis
review,the term ‘‘severe obesity’’ willapply to persons
with class III obesity including those with superobesity.
Centralobesity has mostcommonly been defined as a
waist circumference .102 cm in males and .88 cm in
females.7 Peripheral obesity is traditionally defined as waist
circumferencesat or below thesethresholds.7 Central
obesity hasalso been defined asa waist-to-hip ratio
of .0.9 in males and .0.85 in females.7
The American College of Cardiology and American
Heart Association define HF as ‘‘a complex clinical syn-
drome that can result from any structural or functional
cardiac disorder that impairs the ability of the heart to
fill with or eject blood.’’8 However, most of the studies
concerning HF and obesity predate this definition. Many
of these studies used the Framingham criteria described
by Mckee et al9 to define HF.
EPIDEMIOLOGY
HF afflicts 23 million persons worldwide and 5.8
million persons in the United States.8,10,11
Reportedly,
40%–71%Q4 (mean:56%) of those with HF havea
normal or near normal (left ventricular [LV]) ejection
fraction(LVEF).9,10 In a study of 6076 patients
hospitalized and discharged with a diagnosis ofHF
reported by Owan et al,12 the incidence of obesity was
41.4% in subjects with a preserved LVEF and 35.5%
in those with a reduced LVEF.It has been estimated
thatobesity is presentin up to 86% ofall patients
with HF and a preserved LVEF, many of them elderly.13
It is well established thatclassIII obesity isa
risk factor for HF, even in the absence of comorbidities
including systemic hypertension (HTN) and CAD.14-17
In a study of 74 normotensive class III obese subjects,
nearly one-third had clinicalevidence ofHF.14 The
probability of HF increased markedly when the duration
of obesity exceeded 10 yearswith prevalence rates
of 70% at 20 years and 90% at 30 years. Obesity also
appears to be a risk factor for HF in overweight patients
and those with class I and II obesity. In a study of 5881
participants in the Framingham Heart Study (mean age:
55 years; 54% women), 496 (8.4%) developed HF over a
mean follow-up period of 14 years.15 After adjustment
for traditional risk factors there was an increased risk
of HF of 5% in men and 7% in women for every unit
increase in BMI. The risk of HF was significantly greater
in overweight than in normal weight subjects and signif-
icantly greater in obese than in overweight patients in
both men and woman. Baena-Diez et al16found obesity
to be and independent risk factor for HF in a low risk
Mediterraneanpopulation.These studiesdid not
consider the distribution of fat, but limited evidence sug-
geststhatabdominalobesity may be independently
associated with a high risk for the development of HF,
particularly in the elderly.17
Epidemiologic studies have demonstrated unequivo-
cally that in the general population, HF confers dispropor
tionately high mortality risk overtime.8-11 However,
analysis ofmortality risk in HF populations strongly
suggests thatthe risk of death is lower in overweight
and class I and II obese patients than in normal weight
or underweightsubjectsbasedon BMI classifica-
tion.1,2,18-22
In 2008,Oreopoulos etal18 reported the
results of a meta-analysis involving 28,209 patients with
HF. They compared all-cause and cardiovascular (CV)
mortality in patients with a normal BMI with those who
were overweight and with subjects who were obese base
on WHO criteria. Compared with patients with a normal
BMI all-cause mortality decreased by 16% and 33%,
respectively, in overweight and obese subjects. CV mor-
tality decreased by 19% and 40%,respectively,in the
overweightand obese subgroupscompared with the
normal BMI subgroups. This ‘‘obesity paradox’’ appears
to be consistentin diverse HF populations including
both genders,those with peripheral and central obesity,
personswith chronicand acutedecompensated HF,
patients with preserved and reduced LVEFs,and in the
elderly.1,2,19-22
It has become increasingly clearthat
underweight patients with HF (BMI , 18.5 kg/m2) have
the worst prognosis followed by normal weight subjects
(BMI: 18.5–24.9 kg/m2).1,2,19-22
Overweight and class I
obese patients have the bestprognosis1,2,19-22
Class II
obese patients have a better prognosis than underweigh
and normal weight persons, but exhibit a trend toward a
worse prognosis compared with overweight and class I
obese patients.1,2,19-22
When included,class III obese
patients have a worse prognosis than overweight, class I
and II obesepatients,and a similarprognosisas
underweight subjects.1,2Lavie et al1,2have provided the
following explanations as potential mechanisms for the
obesity paradox in patients with HF: (1) nonpurposeful
weightloss because of catabolic diseases;(2) younger
age atpresentation;(3) lowerprevalence ofcigarette
smoking; (4) greater metabolic reserves; (5) less frailty
and cachexia;(6) lower natriureticpeptidelevels;
(7) higherprevalence ofdyspnea resulting in earlier
evaluation,diagnosis,and therapy;(8) higherblood
pressure facilitating the use ofCV medications;(9)
attenuated response to the renin angiotensin-aldosteron
system (RAAS);(10) differing etiologiesassociated
with a better prognosis; (11) increased muscle mass and
strength; and (12) better cardiorespiratory fitness in som
REV 5.2.0 DTD TRSL776_proof 6 May 2014 3:36 pm ce
TranslationalResearch
2 Alpert et al - 2014
129
130
131
132
133
134
135
136
137
138
139
140
141
142
143
144
145
146
147
148
149
150
151
152
153
154
155
156
157
158
159
160
161
162
163
164
165
166
167
168
169
170
171
172
173
174
175
176
177
178
179
180
181
182
183
184
185
186
187
188
189
190
191
192
193
194
195
196
197
198
199
200
201
202
203
204
205
206
207
208
209
210
211
212
213
214
215
216
217
218
219
220
221
222
223
224
225
226
227
228
229
230
231
232
233
234
235
236
237
238
239
240
241
242
243
244
245
246
247
248
249
250
251
252
253
254
255
256
m2), normal weight (BMI: 18.5–24.9 kg/m2), overweight
(BMI: 25.0–29.9 kg/m2), classI obesity (BMI:30.0–
34.9 kg/m2), class II obesity (BMI: 35.0–39.9 kg/m2), and
class III obesity (BMI $ 40 kg/m2).4 In recent years the
term ‘‘superobesity’’ has been used to characterize those
whose BMIis $50 kg/m2.5,6 For the purpose ofthis
review,the term ‘‘severe obesity’’ willapply to persons
with class III obesity including those with superobesity.
Centralobesity has mostcommonly been defined as a
waist circumference .102 cm in males and .88 cm in
females.7 Peripheral obesity is traditionally defined as waist
circumferencesat or below thesethresholds.7 Central
obesity hasalso been defined asa waist-to-hip ratio
of .0.9 in males and .0.85 in females.7
The American College of Cardiology and American
Heart Association define HF as ‘‘a complex clinical syn-
drome that can result from any structural or functional
cardiac disorder that impairs the ability of the heart to
fill with or eject blood.’’8 However, most of the studies
concerning HF and obesity predate this definition. Many
of these studies used the Framingham criteria described
by Mckee et al9 to define HF.
EPIDEMIOLOGY
HF afflicts 23 million persons worldwide and 5.8
million persons in the United States.8,10,11
Reportedly,
40%–71%Q4 (mean:56%) of those with HF havea
normal or near normal (left ventricular [LV]) ejection
fraction(LVEF).9,10 In a study of 6076 patients
hospitalized and discharged with a diagnosis ofHF
reported by Owan et al,12 the incidence of obesity was
41.4% in subjects with a preserved LVEF and 35.5%
in those with a reduced LVEF.It has been estimated
thatobesity is presentin up to 86% ofall patients
with HF and a preserved LVEF, many of them elderly.13
It is well established thatclassIII obesity isa
risk factor for HF, even in the absence of comorbidities
including systemic hypertension (HTN) and CAD.14-17
In a study of 74 normotensive class III obese subjects,
nearly one-third had clinicalevidence ofHF.14 The
probability of HF increased markedly when the duration
of obesity exceeded 10 yearswith prevalence rates
of 70% at 20 years and 90% at 30 years. Obesity also
appears to be a risk factor for HF in overweight patients
and those with class I and II obesity. In a study of 5881
participants in the Framingham Heart Study (mean age:
55 years; 54% women), 496 (8.4%) developed HF over a
mean follow-up period of 14 years.15 After adjustment
for traditional risk factors there was an increased risk
of HF of 5% in men and 7% in women for every unit
increase in BMI. The risk of HF was significantly greater
in overweight than in normal weight subjects and signif-
icantly greater in obese than in overweight patients in
both men and woman. Baena-Diez et al16found obesity
to be and independent risk factor for HF in a low risk
Mediterraneanpopulation.These studiesdid not
consider the distribution of fat, but limited evidence sug-
geststhatabdominalobesity may be independently
associated with a high risk for the development of HF,
particularly in the elderly.17
Epidemiologic studies have demonstrated unequivo-
cally that in the general population, HF confers dispropor
tionately high mortality risk overtime.8-11 However,
analysis ofmortality risk in HF populations strongly
suggests thatthe risk of death is lower in overweight
and class I and II obese patients than in normal weight
or underweightsubjectsbasedon BMI classifica-
tion.1,2,18-22
In 2008,Oreopoulos etal18 reported the
results of a meta-analysis involving 28,209 patients with
HF. They compared all-cause and cardiovascular (CV)
mortality in patients with a normal BMI with those who
were overweight and with subjects who were obese base
on WHO criteria. Compared with patients with a normal
BMI all-cause mortality decreased by 16% and 33%,
respectively, in overweight and obese subjects. CV mor-
tality decreased by 19% and 40%,respectively,in the
overweightand obese subgroupscompared with the
normal BMI subgroups. This ‘‘obesity paradox’’ appears
to be consistentin diverse HF populations including
both genders,those with peripheral and central obesity,
personswith chronicand acutedecompensated HF,
patients with preserved and reduced LVEFs,and in the
elderly.1,2,19-22
It has become increasingly clearthat
underweight patients with HF (BMI , 18.5 kg/m2) have
the worst prognosis followed by normal weight subjects
(BMI: 18.5–24.9 kg/m2).1,2,19-22
Overweight and class I
obese patients have the bestprognosis1,2,19-22
Class II
obese patients have a better prognosis than underweigh
and normal weight persons, but exhibit a trend toward a
worse prognosis compared with overweight and class I
obese patients.1,2,19-22
When included,class III obese
patients have a worse prognosis than overweight, class I
and II obesepatients,and a similarprognosisas
underweight subjects.1,2Lavie et al1,2have provided the
following explanations as potential mechanisms for the
obesity paradox in patients with HF: (1) nonpurposeful
weightloss because of catabolic diseases;(2) younger
age atpresentation;(3) lowerprevalence ofcigarette
smoking; (4) greater metabolic reserves; (5) less frailty
and cachexia;(6) lower natriureticpeptidelevels;
(7) higherprevalence ofdyspnea resulting in earlier
evaluation,diagnosis,and therapy;(8) higherblood
pressure facilitating the use ofCV medications;(9)
attenuated response to the renin angiotensin-aldosteron
system (RAAS);(10) differing etiologiesassociated
with a better prognosis; (11) increased muscle mass and
strength; and (12) better cardiorespiratory fitness in som
REV 5.2.0 DTD TRSL776_proof 6 May 2014 3:36 pm ce
TranslationalResearch
2 Alpert et al - 2014
129
130
131
132
133
134
135
136
137
138
139
140
141
142
143
144
145
146
147
148
149
150
151
152
153
154
155
156
157
158
159
160
161
162
163
164
165
166
167
168
169
170
171
172
173
174
175
176
177
178
179
180
181
182
183
184
185
186
187
188
189
190
191
192
193
194
195
196
197
198
199
200
201
202
203
204
205
206
207
208
209
210
211
212
213
214
215
216
217
218
219
220
221
222
223
224
225
226
227
228
229
230
231
232
233
234
235
236
237
238
239
240
241
242
243
244
245
246
247
248
249
250
251
252
253
254
255
256
PATHOPHYSIOLOGY
Hemodynamic alterations with obesity.An early hemo-
dynamic study by Alexander et al23 showed a positive
correlation between the amountoverweightand both
total blood volumeand cardiacoutput(CO). In
subsequentstudyof 50 extremelyobesepatients,
Alexander24 confirmed that CO increasedin
proportion to the excess in body weight.In this study,
heartrate did notdiffer from thatpredicted for ideal
body weight. Stroke volume (SV) increasedin
proportion to the excess in body weight.
Arteriovenous oxygen difference was normalat rest,
but correlatedpositivelywith increasingweight.
Cardiac work exceeded thatpredicted for idealbody
weightbecause ofincreased stroke work.DeDivitiis
et al25 reported the results of hemodynamic study of
10 class II and III obese patients.Myocardial oxygen
consumption,CO, and SV values exceededthose
predicted fornormalweightas did rightventricular
(RV) end-diastolic pressure,mean pulmonary artery
pressure,mean pulmonary capillary wedge pressure,
pulmonary vascular resistance,mean arterial pressure,
and systemic vascular resistance (SVR). LV dP/dt was
normal and Vmaxwas lower than predicted for normal
weight.Other hemodynamic studies in obese patients
have reported similar findings and increased baseline
LV end-diastolic pressure (LVEDP).26-31SVR in obese
patientsis variableand dependslargely on the
presence or absence of HTN.In normotensive obese
subjects,SVR is typically lower than that of
normotensive lean patients.26 One recentstudy found
that CO was lower and SVR higher in centrally obese
patients than in peripherally obese subjects.29 In an
exercise study reported by Kaltman and Goldring,30
centralblood volume (CBV) increased from 2485 to
2990 mL,LVEDP increased from 21 to 31 mm Hg,
and LV dP/dt increasedfrom 1612 to 2531.At
workloads2–3 timesthe resting levelthe increase
in CO and its relation to oxygen consumption are
appropriate. At higher workloads CO decreases to low
normallevelsand arteriovenousoxygen difference
widens.Increasesin CO in severely obese patients
are associatedwith increasedLVEDP and right
heartpressures.26 Backman etal31 noted thatLVEDP
increased disproportionately to LV stroke work with
exerciseindicating thepresenceof poor LV com-
pliance.In hypertensive obese patients total and CBV
are elevated,but less than in normotensiveobese
subjects with comparable degrees ofexcess adipose
tissue.26,32,33
LV SV and CO are equal to or greater in
hypertensive obese subjects than those ofnormoten-
sive obesepatients.26,32,33SVR is often elevated
in hypertensiveobesesubjects,but lower than in
normotensive obese patients with comparable severity
of obesity.26,32,33
Peripheral hemodynamics have not been extensively
studied in obese subjects.In classII and III obese
patients,central blood flow and renal blood flow have
been reported to be low normalor mildly reduced,
whereassplanchnic blood flow wasreported to be
increased.26Blood flow in adipose tissue is on average
2–3 mL/min/100 g of adipose tissue,less than that of
other parenchymalorgans.Blood flow attributable to
adipose tissue and parenchymal organs cannot fully ac-
count for the aforementioned increase in CO.26For this
reason, increases in CBVand CO in class I and II obesity
are attributable as much or more to fat-free (predomi-
nantly muscle) mass than to fatmass.26 Whether this
relationship is also true for class III obesity is unknown.
Thus, excessive adipose accumulation in combination
with increased fat-free mass augments CBV and CO, a
phenomenon thatis facilitated by a decrease in SVR.
Because heart rate changes little if at all with obesity,
the increase in CO is attributable primarily to an increase
in SV.Augmentation of CBV contributes to increased
rightheartpressures and eventually to increased LV
filling pressure.These hemodynamic changes predis-
pose to alterations in cardiac morphology and ventricu-
lar function, and subsequently to the development of HF
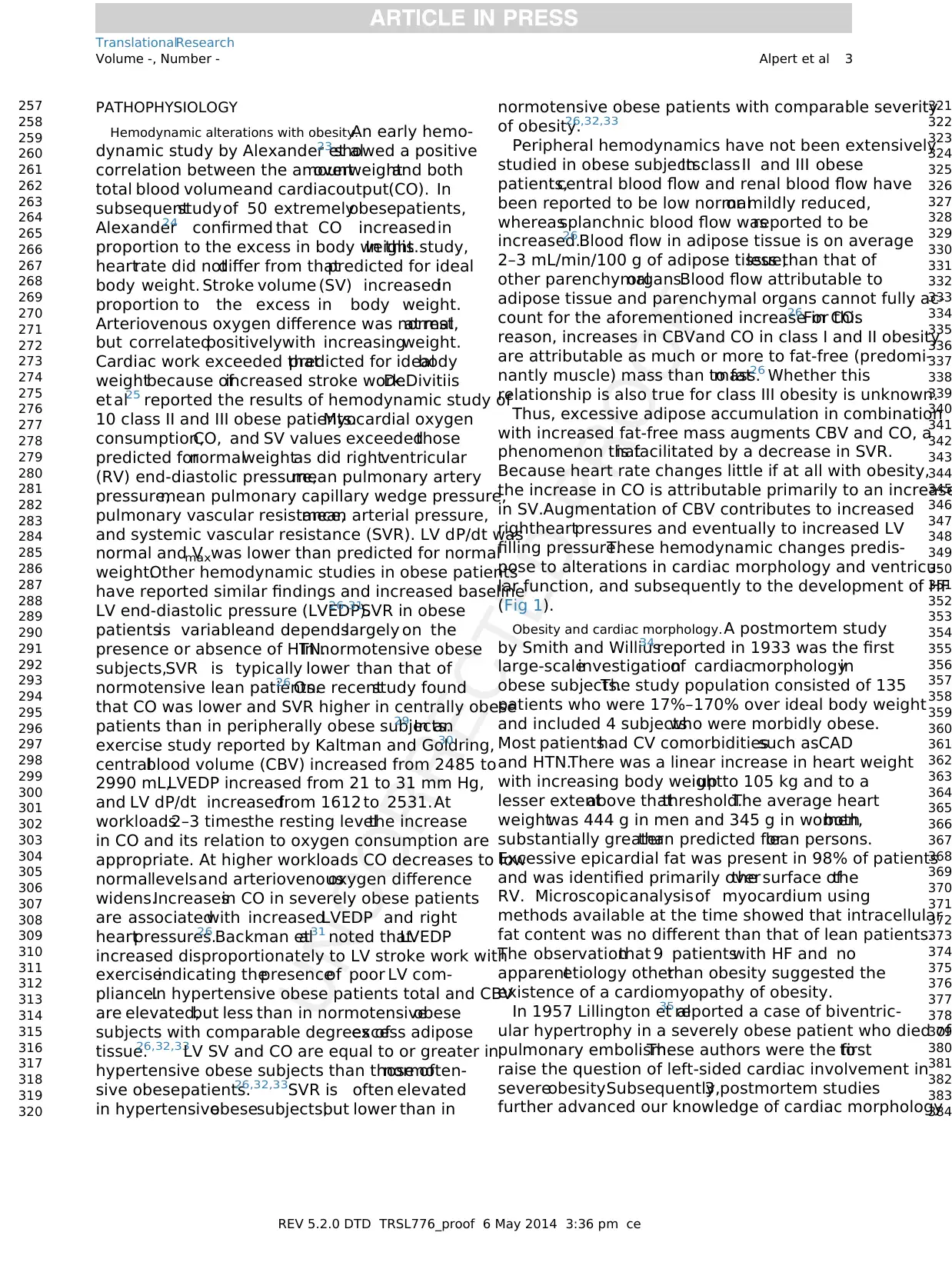
(Fig 1).
Obesity and cardiac morphology. A postmortem study
by Smith and Willius34 reported in 1933 was the first
large-scaleinvestigationof cardiacmorphologyin
obese subjects.The study population consisted of 135
patients who were 17%–170% over ideal body weight
and included 4 subjectswho were morbidly obese.
Most patientshad CV comorbiditiessuch asCAD
and HTN.There was a linear increase in heart weight
with increasing body weightup to 105 kg and to a
lesser extentabove thatthreshold.The average heart
weightwas 444 g in men and 345 g in women,both
substantially greaterthan predicted forlean persons.
Excessive epicardial fat was present in 98% of patients
and was identified primarily overthe surface ofthe
RV. Microscopicanalysisof myocardium using
methods available at the time showed that intracellular
fat content was no different than that of lean patients.
The observationthat 9 patientswith HF and no
apparentetiology otherthan obesity suggested the
existence of a cardiomyopathy of obesity.
In 1957 Lillington et al35reported a case of biventric-
ular hypertrophy in a severely obese patient who died of
pulmonary embolism.These authors were the firstto
raise the question of left-sided cardiac involvement in
severeobesity.Subsequently,3 postmortem studies
further advanced our knowledge of cardiac morphology
REV 5.2.0 DTD TRSL776_proof 6 May 2014 3:36 pm ce
TranslationalResearch
Volume -, Number - Alpert et al 3
257
258
259
260
261
262
263
264
265
266
267
268
269
270
271
272
273
274
275
276
277
278
279
280
281
282
283
284
285
286
287
288
289
290
291
292
293
294
295
296
297
298
299
300
301
302
303
304
305
306
307
308
309
310
311
312
313
314
315
316
317
318
319
320
321
322
323
324
325
326
327
328
329
330
331
332
333
334
335
336
337
338
339
340
341
342
343
344
345
346
347
348
349
350
351
352
353
354
355
356
357
358
359
360
361
362
363
364
365
366
367
368
369
370
371
372
373
374
375
376
377
378
379
380
381
382
383
384
Hemodynamic alterations with obesity.An early hemo-
dynamic study by Alexander et al23 showed a positive
correlation between the amountoverweightand both
total blood volumeand cardiacoutput(CO). In
subsequentstudyof 50 extremelyobesepatients,
Alexander24 confirmed that CO increasedin
proportion to the excess in body weight.In this study,
heartrate did notdiffer from thatpredicted for ideal
body weight. Stroke volume (SV) increasedin
proportion to the excess in body weight.
Arteriovenous oxygen difference was normalat rest,
but correlatedpositivelywith increasingweight.
Cardiac work exceeded thatpredicted for idealbody
weightbecause ofincreased stroke work.DeDivitiis
et al25 reported the results of hemodynamic study of
10 class II and III obese patients.Myocardial oxygen
consumption,CO, and SV values exceededthose
predicted fornormalweightas did rightventricular
(RV) end-diastolic pressure,mean pulmonary artery
pressure,mean pulmonary capillary wedge pressure,
pulmonary vascular resistance,mean arterial pressure,
and systemic vascular resistance (SVR). LV dP/dt was
normal and Vmaxwas lower than predicted for normal
weight.Other hemodynamic studies in obese patients
have reported similar findings and increased baseline
LV end-diastolic pressure (LVEDP).26-31SVR in obese
patientsis variableand dependslargely on the
presence or absence of HTN.In normotensive obese
subjects,SVR is typically lower than that of
normotensive lean patients.26 One recentstudy found
that CO was lower and SVR higher in centrally obese
patients than in peripherally obese subjects.29 In an
exercise study reported by Kaltman and Goldring,30
centralblood volume (CBV) increased from 2485 to
2990 mL,LVEDP increased from 21 to 31 mm Hg,
and LV dP/dt increasedfrom 1612 to 2531.At
workloads2–3 timesthe resting levelthe increase
in CO and its relation to oxygen consumption are
appropriate. At higher workloads CO decreases to low
normallevelsand arteriovenousoxygen difference
widens.Increasesin CO in severely obese patients
are associatedwith increasedLVEDP and right
heartpressures.26 Backman etal31 noted thatLVEDP
increased disproportionately to LV stroke work with
exerciseindicating thepresenceof poor LV com-
pliance.In hypertensive obese patients total and CBV
are elevated,but less than in normotensiveobese
subjects with comparable degrees ofexcess adipose
tissue.26,32,33
LV SV and CO are equal to or greater in
hypertensive obese subjects than those ofnormoten-
sive obesepatients.26,32,33SVR is often elevated
in hypertensiveobesesubjects,but lower than in
normotensive obese patients with comparable severity
of obesity.26,32,33
Peripheral hemodynamics have not been extensively
studied in obese subjects.In classII and III obese
patients,central blood flow and renal blood flow have
been reported to be low normalor mildly reduced,
whereassplanchnic blood flow wasreported to be
increased.26Blood flow in adipose tissue is on average
2–3 mL/min/100 g of adipose tissue,less than that of
other parenchymalorgans.Blood flow attributable to
adipose tissue and parenchymal organs cannot fully ac-
count for the aforementioned increase in CO.26For this
reason, increases in CBVand CO in class I and II obesity
are attributable as much or more to fat-free (predomi-
nantly muscle) mass than to fatmass.26 Whether this
relationship is also true for class III obesity is unknown.
Thus, excessive adipose accumulation in combination
with increased fat-free mass augments CBV and CO, a
phenomenon thatis facilitated by a decrease in SVR.
Because heart rate changes little if at all with obesity,
the increase in CO is attributable primarily to an increase
in SV.Augmentation of CBV contributes to increased
rightheartpressures and eventually to increased LV
filling pressure.These hemodynamic changes predis-
pose to alterations in cardiac morphology and ventricu-
lar function, and subsequently to the development of HF
(Fig 1).
Obesity and cardiac morphology. A postmortem study
by Smith and Willius34 reported in 1933 was the first
large-scaleinvestigationof cardiacmorphologyin
obese subjects.The study population consisted of 135
patients who were 17%–170% over ideal body weight
and included 4 subjectswho were morbidly obese.
Most patientshad CV comorbiditiessuch asCAD
and HTN.There was a linear increase in heart weight
with increasing body weightup to 105 kg and to a
lesser extentabove thatthreshold.The average heart
weightwas 444 g in men and 345 g in women,both
substantially greaterthan predicted forlean persons.
Excessive epicardial fat was present in 98% of patients
and was identified primarily overthe surface ofthe
RV. Microscopicanalysisof myocardium using
methods available at the time showed that intracellular
fat content was no different than that of lean patients.
The observationthat 9 patientswith HF and no
apparentetiology otherthan obesity suggested the
existence of a cardiomyopathy of obesity.
In 1957 Lillington et al35reported a case of biventric-
ular hypertrophy in a severely obese patient who died of
pulmonary embolism.These authors were the firstto
raise the question of left-sided cardiac involvement in
severeobesity.Subsequently,3 postmortem studies
further advanced our knowledge of cardiac morphology
REV 5.2.0 DTD TRSL776_proof 6 May 2014 3:36 pm ce
TranslationalResearch
Volume -, Number - Alpert et al 3
257
258
259
260
261
262
263
264
265
266
267
268
269
270
271
272
273
274
275
276
277
278
279
280
281
282
283
284
285
286
287
288
289
290
291
292
293
294
295
296
297
298
299
300
301
302
303
304
305
306
307
308
309
310
311
312
313
314
315
316
317
318
319
320
321
322
323
324
325
326
327
328
329
330
331
332
333
334
335
336
337
338
339
340
341
342
343
344
345
346
347
348
349
350
351
352
353
354
355
356
357
358
359
360
361
362
363
364
365
366
367
368
369
370
371
372
373
374
375
376
377
378
379
380
381
382
383
384
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
in severely obese patients.36-38
Of the 33 patients in these
3 studies,all demonstrated increased heart weight and
microscopic LV hypertrophy (LVH) and all but one had
increased LV wallthickness.36-38Increased RV wall
thickness was present in only 6 patients and excessive
epicardialfat was presentin 21 subjects.36-38None
of these studies excluded patients with comorbid CV
disease such asHTN or CAD. Thus,it is unclear
whether the pathology identified was caused solely by
obesity. A postmortem study by Kasper et al28reported
in 1992 helped to resolve this issue. The study consisted
of 43 obese and 409 lean patients with HF. Among those
undergoing myocardialbiopsy,a specific underlying
cause for HF was identified in 64.5% of lean patients,
butin only 23.3% ofobese subjects,mostof whom
demonstrated LVH.28 This study provided further evi-
dence for the existence of a cardiomyopathy of obesity,
one that is characterized primarily by LVH.
Little information exists concerning the incidence of
cardiac chamber enlargement and LVH in obesity based
on noninvasive (primarily echocardiographic) evalua-
tion.39-45 Increased LV masshas been reported to
occurin 6%–87% of obese subjects.Increased LV
wall thickness has been reported to occur in 6%–56%
Fig 1. Pathophysiology of obesity cardiomyopathy.This diagram shows central hemodynamic alterations that
result from excessive adipose accumulation in severely obese patients and their subsequent effects on cardiac
morphology and ventricular function. LVH in severe obesity may be eccentric or concentric. Factors influencing
LV remodeling and geometry include severity and duration of obesity, duration and severity of adverse LV loading
conditions(particularly hypertension),and possibly,neurohormonaland metabolic abnormalitiessuch as
increased sympathetic nervous system tone, activation of the RAAS, insulin resistance with hyperinsulinemia, lep-
tin resistance with hyperleptinemia, adiponectin deficiency, lipotoxicity, and lipoapoptosis. These alterations may
contribute to the development of LV failure. LV failure, facilitated by pulmonary arterial hypertension from sleep
apnea/obesity hypoventilation,may subsequently lead to RV failure.Adapted from Ref.1 LV, left ventricular;
LVH, left ventricular hypertrophy; RAAS, renin angiotensin-aldosterone system; RV, right ventricular.
REV 5.2.0 DTD TRSL776_proof 6 May 2014 3:36 pm ce
TranslationalResearch
4 Alpert et al - 2014
385
386
387
388
389
390
391
392
393
394
395
396
397
398
399
400
401
402
403
404
405
406
407
408
409
410
411
412
413
414
415
416
417
418
419
420
421
422
423
424
425
426
427
428
429
430
431
432
433
434
435
436
437
438
439
440
441
442
443
444
445
446
447
448
449
450
451
452
453
454
455
456
457
458
459
460
461
462
463
464
465
466
467
468
469
470
471
472
473
474
475
476
477
478
479
480
481
482
483
484
485
486
487
488
489
490
491
492
493
494
495
496
497
498
499
500
501
502
503
504
505
506
507
508
509
510
511
512
Of the 33 patients in these
3 studies,all demonstrated increased heart weight and
microscopic LV hypertrophy (LVH) and all but one had
increased LV wallthickness.36-38Increased RV wall
thickness was present in only 6 patients and excessive
epicardialfat was presentin 21 subjects.36-38None
of these studies excluded patients with comorbid CV
disease such asHTN or CAD. Thus,it is unclear
whether the pathology identified was caused solely by
obesity. A postmortem study by Kasper et al28reported
in 1992 helped to resolve this issue. The study consisted
of 43 obese and 409 lean patients with HF. Among those
undergoing myocardialbiopsy,a specific underlying
cause for HF was identified in 64.5% of lean patients,
butin only 23.3% ofobese subjects,mostof whom
demonstrated LVH.28 This study provided further evi-
dence for the existence of a cardiomyopathy of obesity,
one that is characterized primarily by LVH.
Little information exists concerning the incidence of
cardiac chamber enlargement and LVH in obesity based
on noninvasive (primarily echocardiographic) evalua-
tion.39-45 Increased LV masshas been reported to
occurin 6%–87% of obese subjects.Increased LV
wall thickness has been reported to occur in 6%–56%
Fig 1. Pathophysiology of obesity cardiomyopathy.This diagram shows central hemodynamic alterations that
result from excessive adipose accumulation in severely obese patients and their subsequent effects on cardiac
morphology and ventricular function. LVH in severe obesity may be eccentric or concentric. Factors influencing
LV remodeling and geometry include severity and duration of obesity, duration and severity of adverse LV loading
conditions(particularly hypertension),and possibly,neurohormonaland metabolic abnormalitiessuch as
increased sympathetic nervous system tone, activation of the RAAS, insulin resistance with hyperinsulinemia, lep-
tin resistance with hyperleptinemia, adiponectin deficiency, lipotoxicity, and lipoapoptosis. These alterations may
contribute to the development of LV failure. LV failure, facilitated by pulmonary arterial hypertension from sleep
apnea/obesity hypoventilation,may subsequently lead to RV failure.Adapted from Ref.1 LV, left ventricular;
LVH, left ventricular hypertrophy; RAAS, renin angiotensin-aldosterone system; RV, right ventricular.
REV 5.2.0 DTD TRSL776_proof 6 May 2014 3:36 pm ce
TranslationalResearch
4 Alpert et al - 2014
385
386
387
388
389
390
391
392
393
394
395
396
397
398
399
400
401
402
403
404
405
406
407
408
409
410
411
412
413
414
415
416
417
418
419
420
421
422
423
424
425
426
427
428
429
430
431
432
433
434
435
436
437
438
439
440
441
442
443
444
445
446
447
448
449
450
451
452
453
454
455
456
457
458
459
460
461
462
463
464
465
466
467
468
469
470
471
472
473
474
475
476
477
478
479
480
481
482
483
484
485
486
487
488
489
490
491
492
493
494
495
496
497
498
499
500
501
502
503
504
505
506
507
508
509
510
511
512
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
of obese patients.LV dilatation has been reported in
8%–40%,and leftatrialenlargementhas been noted
in 10%–50% of obese subjects.RV enlargementwas
described in 32% of severely obese patients. The wide
variation in incidence values is probably attributable
to variation in the severity and duration of obesity and
to the presence orabsence ofcomorbid conditions
affecting the heart.
Numerous echocardiographic studies have compared
LV morphology in lean and obese subjects.38,39In all
classesof obesity indicesof LV mass,LV internal
diastolic chambersize,and LV wall thickness were
consistently significantly greater in obese than in lean
subjects.39-41 Multiple studieshave assessedthe
relation of various body weightindices and LV mor-
phology.39-51Various indices ofLV mass have been
used in studiesof obesepatients.LV mass/height
and morerecently LV mass/height2.7 areQ5 generally
preferred to LV mass because they adjustin partfor
the differential effects of fat mass and lean body mass.
LV mass index may be a better predictor of mortality
in obesity than other indices of LV mass.Strong cor-
relations exist between these indices of LV mass3,39,49
and such body weight indices as BMI, relative weight,
% overweight, and fat mass. Positive correlations have
also been reported between body weightindices and
LV wall thicknessand relative wallthickness.35-38
Most, but not all studieshave reportedpositive
correlationsbetween body weightand LV diastolic
chamber dimension or volume.39-43In severely obese
patientswith HF, indicesof LV mass, LV internal
dimension in diastole,and LV wallthickness are all
significantly greaterthan in severely obese patients
without HF.14
A variety of factors may affect the relation
between body weightand LV mass in obeseper-
sons.3,39-42,46-52
Chief among them is blood pressure.
Hypertensive obesepatientshave consistently been
shown to have greaterLV mass than normotensive
obesesubjects.3,33,39Systolic blood pressure (SBP)
and LV end-systolic wallstress (indices of afterload)
correlated positively and strongly with LV mass/height
index.LV internaldimension in diastole (a possible
surrogate forpreload) also correlated positively with
LV mass/height index. Two studies have shown a rela-
tion between duration ofmoderate to severe obesity
and various indices of LV mass as well as LV internal
dimensionin diastole.47,48 This relationis most
pronounced in thosewhoseduration ofobesity is
$15 years.47In a study of normotensive class III obese
patients, there was a sharp rise in the incidence of HF in
those whose duration of obesity was $10 years.48 In
one study,abdominal adiposity was a better predictor
of LVH than peripheraladiposity.52 For many years
increased fat mass was considered the trigger for these
alterations in LV morphology.However,studies using
multivariate analysis have identified fat-free mass as
a more importantpredictor of LV mass and chamber
size than fatmass.53 In one study,epicardialadipose
tissue mass correlated positively with LV mass.40
On the basisof the aforementioned findings,it
was postulated that the hemodynamic alterations associ-
ated with obesity discussed previously predispose to
eccentric or concentric LVH depending on LV loading
conditions,particularlyin severely obesesubjects.
However,hemodynamicsmay be only partof the
story.In recentyears,studies in animals and humans
suggest that certain metabolic and neurohormonal vari-
ables may also play a role in altering LV morphology in
obesity.3,40,41Theseincludehyperinsulinemiaasso-
ciated with insulin resistance,hyperleptinemia asso-
ciated with leptin resistance,and activation ofthe
RAAS and sympatheticnervoussystem.All these
mechanisms occur with obesity and may contribute to
alterationsin LV mass, LV wall thickness,and LV
chamber size.
On the basis of the proven hemodynamic alterations
associated with obesity, it was hypothesized that in un-
complicated obesity, increased CBVand high CO would
produce LV dilatation and ultimately lead to eccentric
LVH. Early studies seemed to support this hypothesis
by demonstrating high LV radius to thickness ratios.39
In recent years,however,multiple studies have shown
thatconcentric LV remodeling or hypertrophy occurs
as commonly ormore commonly in obese subjects
than eccentric LVH.54-62 One recentstudy reported
thatcentralobesity wasmore commonly associated
with concentricLV remodelingor LVH, whereas
peripheralobesity wasmorecommonly associated
with eccentric LVH.29 A key variable in this debate,
however, is HTN. Obesity HTN may promote a hybrid
form ofLVH previously termed eccentric-concentric
LVH, but now classified asa form of concentric
LVH.46None of the studies showing a high prevalence
of concentric LV remodeling or hypertrophy excluded
patientswith HTN and only one attemptedto
adjustfor its presence.55 In studies of uncomplicated
(normotensive) obesity,eccentric LVH has tended to
predominate among patients with abnormal LV geome-
try.39,61,62
Thus,the issue of LV geometry in obesity
remainsunsettled.Nevertheless,scrutinyof older
studiesindicatesthatconcentricLV remodeling or
hypertrophy waspresentto a variableextenteven
when eccentric LVH predominated.Potentialreasons
for the developmentof concentric LV geometry in
obese subjects include failure to fully accountfor the
relative duration and severity ofHTN and obesity,
underdiagnosis of HTN,reclassification of eccentric-
REV 5.2.0 DTD TRSL776_proof 6 May 2014 3:36 pm ce
TranslationalResearch
Volume -, Number - Alpert et al 5
513
514
515
516
517
518
519
520
521
522
523
524
525
526
527
528
529
530
531
532
533
534
535
536
537
538
539
540
541
542
543
544
545
546
547
548
549
550
551
552
553
554
555
556
557
558
559
560
561
562
563
564
565
566
567
568
569
570
571
572
573
574
575
576
577
578
579
580
581
582
583
584
585
586
587
588
589
590
591
592
593
594
595
596
597
598
599
600
601
602
603
604
605
606
607
608
609
610
611
612
613
614
615
616
617
618
619
620
621
622
623
624
625
626
627
628
629
630
631
632
633
634
635
636
637
638
639
640
8%–40%,and leftatrialenlargementhas been noted
in 10%–50% of obese subjects.RV enlargementwas
described in 32% of severely obese patients. The wide
variation in incidence values is probably attributable
to variation in the severity and duration of obesity and
to the presence orabsence ofcomorbid conditions
affecting the heart.
Numerous echocardiographic studies have compared
LV morphology in lean and obese subjects.38,39In all
classesof obesity indicesof LV mass,LV internal
diastolic chambersize,and LV wall thickness were
consistently significantly greater in obese than in lean
subjects.39-41 Multiple studieshave assessedthe
relation of various body weightindices and LV mor-
phology.39-51Various indices ofLV mass have been
used in studiesof obesepatients.LV mass/height
and morerecently LV mass/height2.7 areQ5 generally
preferred to LV mass because they adjustin partfor
the differential effects of fat mass and lean body mass.
LV mass index may be a better predictor of mortality
in obesity than other indices of LV mass.Strong cor-
relations exist between these indices of LV mass3,39,49
and such body weight indices as BMI, relative weight,
% overweight, and fat mass. Positive correlations have
also been reported between body weightindices and
LV wall thicknessand relative wallthickness.35-38
Most, but not all studieshave reportedpositive
correlationsbetween body weightand LV diastolic
chamber dimension or volume.39-43In severely obese
patientswith HF, indicesof LV mass, LV internal
dimension in diastole,and LV wallthickness are all
significantly greaterthan in severely obese patients
without HF.14
A variety of factors may affect the relation
between body weightand LV mass in obeseper-
sons.3,39-42,46-52
Chief among them is blood pressure.
Hypertensive obesepatientshave consistently been
shown to have greaterLV mass than normotensive
obesesubjects.3,33,39Systolic blood pressure (SBP)
and LV end-systolic wallstress (indices of afterload)
correlated positively and strongly with LV mass/height
index.LV internaldimension in diastole (a possible
surrogate forpreload) also correlated positively with
LV mass/height index. Two studies have shown a rela-
tion between duration ofmoderate to severe obesity
and various indices of LV mass as well as LV internal
dimensionin diastole.47,48 This relationis most
pronounced in thosewhoseduration ofobesity is
$15 years.47In a study of normotensive class III obese
patients, there was a sharp rise in the incidence of HF in
those whose duration of obesity was $10 years.48 In
one study,abdominal adiposity was a better predictor
of LVH than peripheraladiposity.52 For many years
increased fat mass was considered the trigger for these
alterations in LV morphology.However,studies using
multivariate analysis have identified fat-free mass as
a more importantpredictor of LV mass and chamber
size than fatmass.53 In one study,epicardialadipose
tissue mass correlated positively with LV mass.40
On the basisof the aforementioned findings,it
was postulated that the hemodynamic alterations associ-
ated with obesity discussed previously predispose to
eccentric or concentric LVH depending on LV loading
conditions,particularlyin severely obesesubjects.
However,hemodynamicsmay be only partof the
story.In recentyears,studies in animals and humans
suggest that certain metabolic and neurohormonal vari-
ables may also play a role in altering LV morphology in
obesity.3,40,41Theseincludehyperinsulinemiaasso-
ciated with insulin resistance,hyperleptinemia asso-
ciated with leptin resistance,and activation ofthe
RAAS and sympatheticnervoussystem.All these
mechanisms occur with obesity and may contribute to
alterationsin LV mass, LV wall thickness,and LV
chamber size.
On the basis of the proven hemodynamic alterations
associated with obesity, it was hypothesized that in un-
complicated obesity, increased CBVand high CO would
produce LV dilatation and ultimately lead to eccentric
LVH. Early studies seemed to support this hypothesis
by demonstrating high LV radius to thickness ratios.39
In recent years,however,multiple studies have shown
thatconcentric LV remodeling or hypertrophy occurs
as commonly ormore commonly in obese subjects
than eccentric LVH.54-62 One recentstudy reported
thatcentralobesity wasmore commonly associated
with concentricLV remodelingor LVH, whereas
peripheralobesity wasmorecommonly associated
with eccentric LVH.29 A key variable in this debate,
however, is HTN. Obesity HTN may promote a hybrid
form ofLVH previously termed eccentric-concentric
LVH, but now classified asa form of concentric
LVH.46None of the studies showing a high prevalence
of concentric LV remodeling or hypertrophy excluded
patientswith HTN and only one attemptedto
adjustfor its presence.55 In studies of uncomplicated
(normotensive) obesity,eccentric LVH has tended to
predominate among patients with abnormal LV geome-
try.39,61,62
Thus,the issue of LV geometry in obesity
remainsunsettled.Nevertheless,scrutinyof older
studiesindicatesthatconcentricLV remodeling or
hypertrophy waspresentto a variableextenteven
when eccentric LVH predominated.Potentialreasons
for the developmentof concentric LV geometry in
obese subjects include failure to fully accountfor the
relative duration and severity ofHTN and obesity,
underdiagnosis of HTN,reclassification of eccentric-
REV 5.2.0 DTD TRSL776_proof 6 May 2014 3:36 pm ce
TranslationalResearch
Volume -, Number - Alpert et al 5
513
514
515
516
517
518
519
520
521
522
523
524
525
526
527
528
529
530
531
532
533
534
535
536
537
538
539
540
541
542
543
544
545
546
547
548
549
550
551
552
553
554
555
556
557
558
559
560
561
562
563
564
565
566
567
568
569
570
571
572
573
574
575
576
577
578
579
580
581
582
583
584
585
586
587
588
589
590
591
592
593
594
595
596
597
598
599
600
601
602
603
604
605
606
607
608
609
610
611
612
613
614
615
616
617
618
619
620
621
622
623
624
625
626
627
628
629
630
631
632
633
634
635
636
637
638
639
640
concentric LVH as concentric LVH, activation of RAAS
and sympathetic nervous system,and the effectsof
various growth factors (eg,insulin-related growth fac-
tor).
Left atrialenlargementhas been reported to occur
commonly in severe obesity, but may relate more to LV
mass than to BMI.39,44,45,63
Noninvasivestudies
relatingto RV morphologyin obesityare sparse
primarily because of the limitations of
echocardiography.43,64Magnetic resonance imaging is
able to provide accurate assessment of RV morphology
and holds promisefor future answersto this
understudied question.
Obesity and LV diastolic function. Hemodynamic
studies have shown that LVEDP is frequently elevated
at rest in severely obese people and may rise substan-
tially with exercise.24-31A wide variety of noninvasive
techniqueshavebeenusedto assessLV diastolic
functionin obesesubjectsincludingradionuclide
angiography, 2-dimensional echocardiography, Doppler
echocardiography, and tissue Doppler imaging.65-72
Regardlessof the noninvasivecardiactechnique
used,studieshave consistentlyshownimpairment
of LV diastolic function in obese (all classes) relative
to lean subjects.65-72 Moreover,indices of body
weighthave consistently and significantly correlated
with progressively greater impairment of LV diastolic
function.65,69,70
A variety of factors may contribute to LV diastolic
dysfunctionin obesity.65-72 Chief amongthem is
the presence of LVH.65,70In one study,impaired LV
diastolicfilling occurred exclusively in thosewith
LVH.70 However,more recentevidence indicates that
LV diastolic dysfunction may occur in obese subjects
in the absence of LVH.40 LV diastolic filling becomes
progressively moreabnormalwith increasing SBP,
LV end-systolic wall stress, and LV internal dimension
diastole.65-70Duration ofobesity also appears to be
important,possibly related to timeof exposureto
adverse LV loading conditions and to the development
of LVH.48 Otherfactorsthatmay contribute to LV
diastolicdysfunction in obesity includeolder age,
diabetes mellitus with insulin resistance, and transform-
ing growth factor b1.3,65Severity of obesity is also an
importantdeterminantof LV diastolic function.
Pascualet al69 reported abnormalLV diastolic filling
in 12% of class I,35% of class II,and 45% of class
III obese patients using Doppler echocardiography.
Most of the noninvasive cardiac techniquesused
to assessLV diastolic filling are influenced by LV
loadingconditions(afterloadand preload).Tissue
Dopplerimaging is thoughtto be load-independent.
The results ofstudies using tissue Dopplerimaging
in obesity have mirrored those of studies using load-
dependenttechniques.73,74 TissueDopplerimaging
is more sensitive than these other techniques and may
identify subclinicalLV diastolic dysfunction in obese
persons.73,74 Studiesusing tissueDopplerimaging
in class I and II obesesubjectsindicatethat LV
diastolic dysfunction atrest,when present,is usually
mild.73,74
Obesity and LV systolic function.Most studies assess-
ing LV systolic function in obesity have used echocardi-
ography orradionuclide angiography to measure LV
ejection phase indices such as LVEF or LV fractional
shortening.1,3,40,41,75-78
Most studieshave reported
normalor supranormalLV systolic function in all
classesof obesity.1,3,36,37,63,71,72
In some studies,
primarilyin class III obesepatients,LV ejection
phase indices were significantly lower in obese than in
lean patients.75,76In others there was no significant
difference between the 2 groups.75,76Variablesthat
have been shown to influence LV systolic function in
severe obesity include adverse LV loading conditions,
duration ofobesity,and severity ofobesity.47,48,75,76
However,even when LV systolic function is impaired
in obese persons, it is typically only mildly so. Severe
LV systolic dysfunction is extremely rare in all classes
of obesity and should elicit a search for comorbid CV
conditions.
Tissue Dopplerand speckletrack imaging,by
measuring mitralannularvelocities in systole and LV
deformation (stress,strain,and strain rate),has demon-
strated impairmentof regionaland globalLV systolic
function in obesity77,79
, even when load-dependent indices
of LV systolic function are normal.This suggests that
obesity is associated with subclinical LV systolic dysfunc
tion even when LV ejection phase indices are normal.
Left atrial and RV function in obesity. Little infor-
mation exists concerning leftatrialand RV function
in obesity.78,80
Abnormalleft atrial strain hasbeen
reportedin hypertensiveobesesubjectswith left
atrial enlargement.80 Recently,studiesusing tissue
Doppler imaging of the lateral tricuspid annulus have
demonstrated decreased RV systolicvelocitiesand
abnormalRV strain in obese subjects.79 The clinical
significance of these findings is unknown.
Metabolic alterations that may affect cardiac structure
and function. Most investigative activities assessing the
relation ofobesity to cardiac structure and function
have focused on the role ofhemodynamics and CV
comorbidities.In recent years,certain metabolic alter-
ations, observed mainly in animal models, have received
increasingattention.3,36,37,78,79,81
Among the most
prominentof these is lipotoxicity.3,40,41,82
Myocardial
lipotoxicity is a process by which excess fatty acids
and triglyceridesaccumulatein cardiacmyocytes,
producing cellulardysfunction and death,eventually
REV 5.2.0 DTD TRSL776_proof 6 May 2014 3:36 pm ce
TranslationalResearch
6 Alpert et al - 2014
641
642
643
644
645
646
647
648
649
650
651
652
653
654
655
656
657
658
659
660
661
662
663
664
665
666
667
668
669
670
671
672
673
674
675
676
677
678
679
680
681
682
683
684
685
686
687
688
689
690
691
692
693
694
695
696
697
698
699
700
701
702
703
704
705
706
707
708
709
710
711
712
713
714
715
716
717
718
719
720
721
722
723
724
725
726
727
728
729
730
731
732
733
734
735
736
737
738
739
740
741
742
743
744
745
746
747
748
749
750
751
752
753
754
755
756
757
758
759
760
761
762
763
764
765
766
767
768
and sympathetic nervous system,and the effectsof
various growth factors (eg,insulin-related growth fac-
tor).
Left atrialenlargementhas been reported to occur
commonly in severe obesity, but may relate more to LV
mass than to BMI.39,44,45,63
Noninvasivestudies
relatingto RV morphologyin obesityare sparse
primarily because of the limitations of
echocardiography.43,64Magnetic resonance imaging is
able to provide accurate assessment of RV morphology
and holds promisefor future answersto this
understudied question.
Obesity and LV diastolic function. Hemodynamic
studies have shown that LVEDP is frequently elevated
at rest in severely obese people and may rise substan-
tially with exercise.24-31A wide variety of noninvasive
techniqueshavebeenusedto assessLV diastolic
functionin obesesubjectsincludingradionuclide
angiography, 2-dimensional echocardiography, Doppler
echocardiography, and tissue Doppler imaging.65-72
Regardlessof the noninvasivecardiactechnique
used,studieshave consistentlyshownimpairment
of LV diastolic function in obese (all classes) relative
to lean subjects.65-72 Moreover,indices of body
weighthave consistently and significantly correlated
with progressively greater impairment of LV diastolic
function.65,69,70
A variety of factors may contribute to LV diastolic
dysfunctionin obesity.65-72 Chief amongthem is
the presence of LVH.65,70In one study,impaired LV
diastolicfilling occurred exclusively in thosewith
LVH.70 However,more recentevidence indicates that
LV diastolic dysfunction may occur in obese subjects
in the absence of LVH.40 LV diastolic filling becomes
progressively moreabnormalwith increasing SBP,
LV end-systolic wall stress, and LV internal dimension
diastole.65-70Duration ofobesity also appears to be
important,possibly related to timeof exposureto
adverse LV loading conditions and to the development
of LVH.48 Otherfactorsthatmay contribute to LV
diastolicdysfunction in obesity includeolder age,
diabetes mellitus with insulin resistance, and transform-
ing growth factor b1.3,65Severity of obesity is also an
importantdeterminantof LV diastolic function.
Pascualet al69 reported abnormalLV diastolic filling
in 12% of class I,35% of class II,and 45% of class
III obese patients using Doppler echocardiography.
Most of the noninvasive cardiac techniquesused
to assessLV diastolic filling are influenced by LV
loadingconditions(afterloadand preload).Tissue
Dopplerimaging is thoughtto be load-independent.
The results ofstudies using tissue Dopplerimaging
in obesity have mirrored those of studies using load-
dependenttechniques.73,74 TissueDopplerimaging
is more sensitive than these other techniques and may
identify subclinicalLV diastolic dysfunction in obese
persons.73,74 Studiesusing tissueDopplerimaging
in class I and II obesesubjectsindicatethat LV
diastolic dysfunction atrest,when present,is usually
mild.73,74
Obesity and LV systolic function.Most studies assess-
ing LV systolic function in obesity have used echocardi-
ography orradionuclide angiography to measure LV
ejection phase indices such as LVEF or LV fractional
shortening.1,3,40,41,75-78
Most studieshave reported
normalor supranormalLV systolic function in all
classesof obesity.1,3,36,37,63,71,72
In some studies,
primarilyin class III obesepatients,LV ejection
phase indices were significantly lower in obese than in
lean patients.75,76In others there was no significant
difference between the 2 groups.75,76Variablesthat
have been shown to influence LV systolic function in
severe obesity include adverse LV loading conditions,
duration ofobesity,and severity ofobesity.47,48,75,76
However,even when LV systolic function is impaired
in obese persons, it is typically only mildly so. Severe
LV systolic dysfunction is extremely rare in all classes
of obesity and should elicit a search for comorbid CV
conditions.
Tissue Dopplerand speckletrack imaging,by
measuring mitralannularvelocities in systole and LV
deformation (stress,strain,and strain rate),has demon-
strated impairmentof regionaland globalLV systolic
function in obesity77,79
, even when load-dependent indices
of LV systolic function are normal.This suggests that
obesity is associated with subclinical LV systolic dysfunc
tion even when LV ejection phase indices are normal.
Left atrial and RV function in obesity. Little infor-
mation exists concerning leftatrialand RV function
in obesity.78,80
Abnormalleft atrial strain hasbeen
reportedin hypertensiveobesesubjectswith left
atrial enlargement.80 Recently,studiesusing tissue
Doppler imaging of the lateral tricuspid annulus have
demonstrated decreased RV systolicvelocitiesand
abnormalRV strain in obese subjects.79 The clinical
significance of these findings is unknown.
Metabolic alterations that may affect cardiac structure
and function. Most investigative activities assessing the
relation ofobesity to cardiac structure and function
have focused on the role ofhemodynamics and CV
comorbidities.In recent years,certain metabolic alter-
ations, observed mainly in animal models, have received
increasingattention.3,36,37,78,79,81
Among the most
prominentof these is lipotoxicity.3,40,41,82
Myocardial
lipotoxicity is a process by which excess fatty acids
and triglyceridesaccumulatein cardiacmyocytes,
producing cellulardysfunction and death,eventually
REV 5.2.0 DTD TRSL776_proof 6 May 2014 3:36 pm ce
TranslationalResearch
6 Alpert et al - 2014
641
642
643
644
645
646
647
648
649
650
651
652
653
654
655
656
657
658
659
660
661
662
663
664
665
666
667
668
669
670
671
672
673
674
675
676
677
678
679
680
681
682
683
684
685
686
687
688
689
690
691
692
693
694
695
696
697
698
699
700
701
702
703
704
705
706
707
708
709
710
711
712
713
714
715
716
717
718
719
720
721
722
723
724
725
726
727
728
729
730
731
732
733
734
735
736
737
738
739
740
741
742
743
744
745
746
747
748
749
750
751
752
753
754
755
756
757
758
759
760
761
762
763
764
765
766
767
768
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
leading to myocardialdysfunction.82 Accumulation of
free fatty acidsand triglyceridesin cardiomyocytes
results from an imbalance between uptake and use of
these substances.82 Increased myocardialtriglyceride
accumulationhas been linked to LVH and LV
dysfunction in genetically obese rats.BMI correlates
positively with myocardialtriglyceridecontentand
LV mass in humans.41,42,82Adipocytesare known
to stimulate orinhibitvarious enzymes and proteins
thataffectlipid uptake orturnover.3,42,82
Transgenic
murine models of lipotoxicity and lipoapoptosis have
been developed to determine theireffects on cardiac
structure and function. Cardiomyocte overexpression of
acyl Co-A synthetase causes lipotoxic cardiomyopathy
and lipoapoptosis,which is characterizedby LV
systolic dysfunction. This process is reversed by leptin
and alpha lipoic acid.Cardiomyocyte overexpression
of peroxisome proliferator–activated receptor (PPAR)-
alphaQ6 produces lipotoxic cardiomyopathy and increased
fatty acid oxidation,a process reversed with knockout
of CD-36.Cardiomyocyte overexpression of fatty acid
transportprotein causesmyocardiallipotoxicity and
increased fatty acid oxidation leading to LV diastolic
dysfunction.Cardiomyocyte expression ofmembrane
anchoredlipid-proteinlipase produceslipotoxic
cardiomyopathy associated with triglyceride-containing
lipoproteins. This process is reversed by PPAR gamma
agonists such as troglitazoneQ7 . Cardiomyocyte restricted
knockoutof PPAR gamma causeslipotoxic cardio-
myopathy,a decrease in myocardialfatty acid oxi-
dation and HF. Inhibition of adipose tissue triglyceride
lipase resultsin massive cardiac lipid accumulation
becauseof inability to break down triglyceride.
Overexpressionof diacylglycerolacyl transferase
promotes triglyceride accumulation in cardiomyocytes
resulting in LV systolic and diastolic dysfunction and
increased cardiac fibrosis.Regardlessof the mecha-
nism, all these abnormalities promote cardiac steatosis,
which in turn leads to cardiac remodeling,myocardial
damage,and eventually to myocardialdysfunction.
These effects are thought to be mediated by long chain
fatty acids and their metabolicproductssuch as
diglyceroland ceramides.The extentto which these
transgenicmurinemodelsrelateto humanpatho-
physiology in obesity isuncertain.However,recent
studiesin type 2 diabeticpatientshave reported
myocardialsteatosisassociatedwith LV diastolic
dysfunction.83,84
Other metabolic factors that have contributed to car-
diac remodeling and dysfunction in animalmodels
and in limited human studies include hyperleptinemia
because of leptin resistance, insulin resistance with hy-
perinsulinemia, and adiponectin deficiency.3,41,42,85,86
CLINICAL MANIFESTATIONS OF OBESITY
CARDIOMYOPATHY
Obesity serves as a risk factor for HF. In such patients,
clinical manifestations of HF are similar to those of HF
from other causes. Severe obesity, however, is capable
of causing HF in the absence of other forms of organic
heart disease.87When this occurs, the clinical syndrome
that resultsis termed ‘‘obesity cardiomyopathy.’’87
Most peoplewho develop obesity cardiomyopathy
have a body weight$135 kg, a relative weightof
175%–200%, or a BMI $40 kg/m2.87 Most have been
severelyobesefor at least 10 years.87 There is
frequently a history ofrecentweightgain preceding
the development of symptoms of HF.87 Acute pulmo-
nary edema is relatively uncommon, unlike other forms
of HF with a preserved LVEF.80Episodes of atrial fibril-
lation and atrial flutter may occur.87The natural history
of this condition is characterized by repeated bouts of
pulmonary and systemiccongestion,often tracking
with recent weight gain.87In severe obesity, sleep apnea
may occur in up to 50% of patients. Severe hypoventi-
lation occurs in approximately 10% of individuals.87
Hypoxemia related to sleep apnea/obesity hypoventila-
tion Q8may contribute to pulmonary arterial HTN and RV
failure.80However, LV failure is the predominant cause
of RV failure in those with obesity cardiomyopathy.87
Isolated cor pulmonale does notoccur with this syn-
drome.87The pathophysiology of obesity cardiomyopa-
thy is summarized in Figure 1.
Obesity cardiomyopathy sharessome clinicalfea-
tures with other causes of HF, but possesses some that
are unique to this syndrome.87Symptoms of obesity car-
diomyopathy include dyspnea on exertion,orthopnea,
and paroxysmalnocturnaldyspnea,recentweight
gain,recentincrease in lowerextremity edema and
abdominalgirth,mentalconfusion and disorientation,
and somnolence and in some cases coma and death
(often sudden).87Physical signs of obesity cardiomyop-
athy include jugular venous distension and hepatojugu-
lar reflux, pulmonary crackles, a fourth heart sound or
a summation gallop,hepatomegaly,brawny edema,
cyanosis(often accompaniedby polycythemia),a
Cheyne-Stokes breathing pattern,conjunctivalsuffu-
sion, retinalvenouscongestion,and papilledema.87
Heartmurmurs occur relatively infrequently.87 These
symptoms and signs resultfrom the combination of
LV and RV failure and thesequelaeof the sleep
apnea/obesity hypoventilation syndrome.87
Electrocardiographic abnormalities associated with
severe obesity include low QRS voltage and rightward
shift in the QRS Q9axis.88 Electrocardiographic evidence
of LVH occurs with a lower frequency than echocardio-
graphic LVH.88 Multiple studieshave demonstrated
REV 5.2.0 DTD TRSL776_proof 6 May 2014 3:36 pm ce
TranslationalResearch
Volume -, Number - Alpert et al 7
769
770
771
772
773
774
775
776
777
778
779
780
781
782
783
784
785
786
787
788
789
790
791
792
793
794
795
796
797
798
799
800
801
802
803
804
805
806
807
808
809
810
811
812
813
814
815
816
817
818
819
820
821
822
823
824
825
826
827
828
829
830
831
832
833
834
835
836
837
838
839
840
841
842
843
844
845
846
847
848
849
850
851
852
853
854
855
856
857
858
859
860
861
862
863
864
865
866
867
868
869
870
871
872
873
874
875
876
877
878
879
880
881
882
883
884
885
886
887
888
889
890
891
892
893
894
895
896
free fatty acidsand triglyceridesin cardiomyocytes
results from an imbalance between uptake and use of
these substances.82 Increased myocardialtriglyceride
accumulationhas been linked to LVH and LV
dysfunction in genetically obese rats.BMI correlates
positively with myocardialtriglyceridecontentand
LV mass in humans.41,42,82Adipocytesare known
to stimulate orinhibitvarious enzymes and proteins
thataffectlipid uptake orturnover.3,42,82
Transgenic
murine models of lipotoxicity and lipoapoptosis have
been developed to determine theireffects on cardiac
structure and function. Cardiomyocte overexpression of
acyl Co-A synthetase causes lipotoxic cardiomyopathy
and lipoapoptosis,which is characterizedby LV
systolic dysfunction. This process is reversed by leptin
and alpha lipoic acid.Cardiomyocyte overexpression
of peroxisome proliferator–activated receptor (PPAR)-
alphaQ6 produces lipotoxic cardiomyopathy and increased
fatty acid oxidation,a process reversed with knockout
of CD-36.Cardiomyocyte overexpression of fatty acid
transportprotein causesmyocardiallipotoxicity and
increased fatty acid oxidation leading to LV diastolic
dysfunction.Cardiomyocyte expression ofmembrane
anchoredlipid-proteinlipase produceslipotoxic
cardiomyopathy associated with triglyceride-containing
lipoproteins. This process is reversed by PPAR gamma
agonists such as troglitazoneQ7 . Cardiomyocyte restricted
knockoutof PPAR gamma causeslipotoxic cardio-
myopathy,a decrease in myocardialfatty acid oxi-
dation and HF. Inhibition of adipose tissue triglyceride
lipase resultsin massive cardiac lipid accumulation
becauseof inability to break down triglyceride.
Overexpressionof diacylglycerolacyl transferase
promotes triglyceride accumulation in cardiomyocytes
resulting in LV systolic and diastolic dysfunction and
increased cardiac fibrosis.Regardlessof the mecha-
nism, all these abnormalities promote cardiac steatosis,
which in turn leads to cardiac remodeling,myocardial
damage,and eventually to myocardialdysfunction.
These effects are thought to be mediated by long chain
fatty acids and their metabolicproductssuch as
diglyceroland ceramides.The extentto which these
transgenicmurinemodelsrelateto humanpatho-
physiology in obesity isuncertain.However,recent
studiesin type 2 diabeticpatientshave reported
myocardialsteatosisassociatedwith LV diastolic
dysfunction.83,84
Other metabolic factors that have contributed to car-
diac remodeling and dysfunction in animalmodels
and in limited human studies include hyperleptinemia
because of leptin resistance, insulin resistance with hy-
perinsulinemia, and adiponectin deficiency.3,41,42,85,86
CLINICAL MANIFESTATIONS OF OBESITY
CARDIOMYOPATHY
Obesity serves as a risk factor for HF. In such patients,
clinical manifestations of HF are similar to those of HF
from other causes. Severe obesity, however, is capable
of causing HF in the absence of other forms of organic
heart disease.87When this occurs, the clinical syndrome
that resultsis termed ‘‘obesity cardiomyopathy.’’87
Most peoplewho develop obesity cardiomyopathy
have a body weight$135 kg, a relative weightof
175%–200%, or a BMI $40 kg/m2.87 Most have been
severelyobesefor at least 10 years.87 There is
frequently a history ofrecentweightgain preceding
the development of symptoms of HF.87 Acute pulmo-
nary edema is relatively uncommon, unlike other forms
of HF with a preserved LVEF.80Episodes of atrial fibril-
lation and atrial flutter may occur.87The natural history
of this condition is characterized by repeated bouts of
pulmonary and systemiccongestion,often tracking
with recent weight gain.87In severe obesity, sleep apnea
may occur in up to 50% of patients. Severe hypoventi-
lation occurs in approximately 10% of individuals.87
Hypoxemia related to sleep apnea/obesity hypoventila-
tion Q8may contribute to pulmonary arterial HTN and RV
failure.80However, LV failure is the predominant cause
of RV failure in those with obesity cardiomyopathy.87
Isolated cor pulmonale does notoccur with this syn-
drome.87The pathophysiology of obesity cardiomyopa-
thy is summarized in Figure 1.
Obesity cardiomyopathy sharessome clinicalfea-
tures with other causes of HF, but possesses some that
are unique to this syndrome.87Symptoms of obesity car-
diomyopathy include dyspnea on exertion,orthopnea,
and paroxysmalnocturnaldyspnea,recentweight
gain,recentincrease in lowerextremity edema and
abdominalgirth,mentalconfusion and disorientation,
and somnolence and in some cases coma and death
(often sudden).87Physical signs of obesity cardiomyop-
athy include jugular venous distension and hepatojugu-
lar reflux, pulmonary crackles, a fourth heart sound or
a summation gallop,hepatomegaly,brawny edema,
cyanosis(often accompaniedby polycythemia),a
Cheyne-Stokes breathing pattern,conjunctivalsuffu-
sion, retinalvenouscongestion,and papilledema.87
Heartmurmurs occur relatively infrequently.87 These
symptoms and signs resultfrom the combination of
LV and RV failure and thesequelaeof the sleep
apnea/obesity hypoventilation syndrome.87
Electrocardiographic abnormalities associated with
severe obesity include low QRS voltage and rightward
shift in the QRS Q9axis.88 Electrocardiographic evidence
of LVH occurs with a lower frequency than echocardio-
graphic LVH.88 Multiple studieshave demonstrated
REV 5.2.0 DTD TRSL776_proof 6 May 2014 3:36 pm ce
TranslationalResearch
Volume -, Number - Alpert et al 7
769
770
771
772
773
774
775
776
777
778
779
780
781
782
783
784
785
786
787
788
789
790
791
792
793
794
795
796
797
798
799
800
801
802
803
804
805
806
807
808
809
810
811
812
813
814
815
816
817
818
819
820
821
822
823
824
825
826
827
828
829
830
831
832
833
834
835
836
837
838
839
840
841
842
843
844
845
846
847
848
849
850
851
852
853
854
855
856
857
858
859
860
861
862
863
864
865
866
867
868
869
870
871
872
873
874
875
876
877
878
879
880
881
882
883
884
885
886
887
888
889
890
891
892
893
894
895
896
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
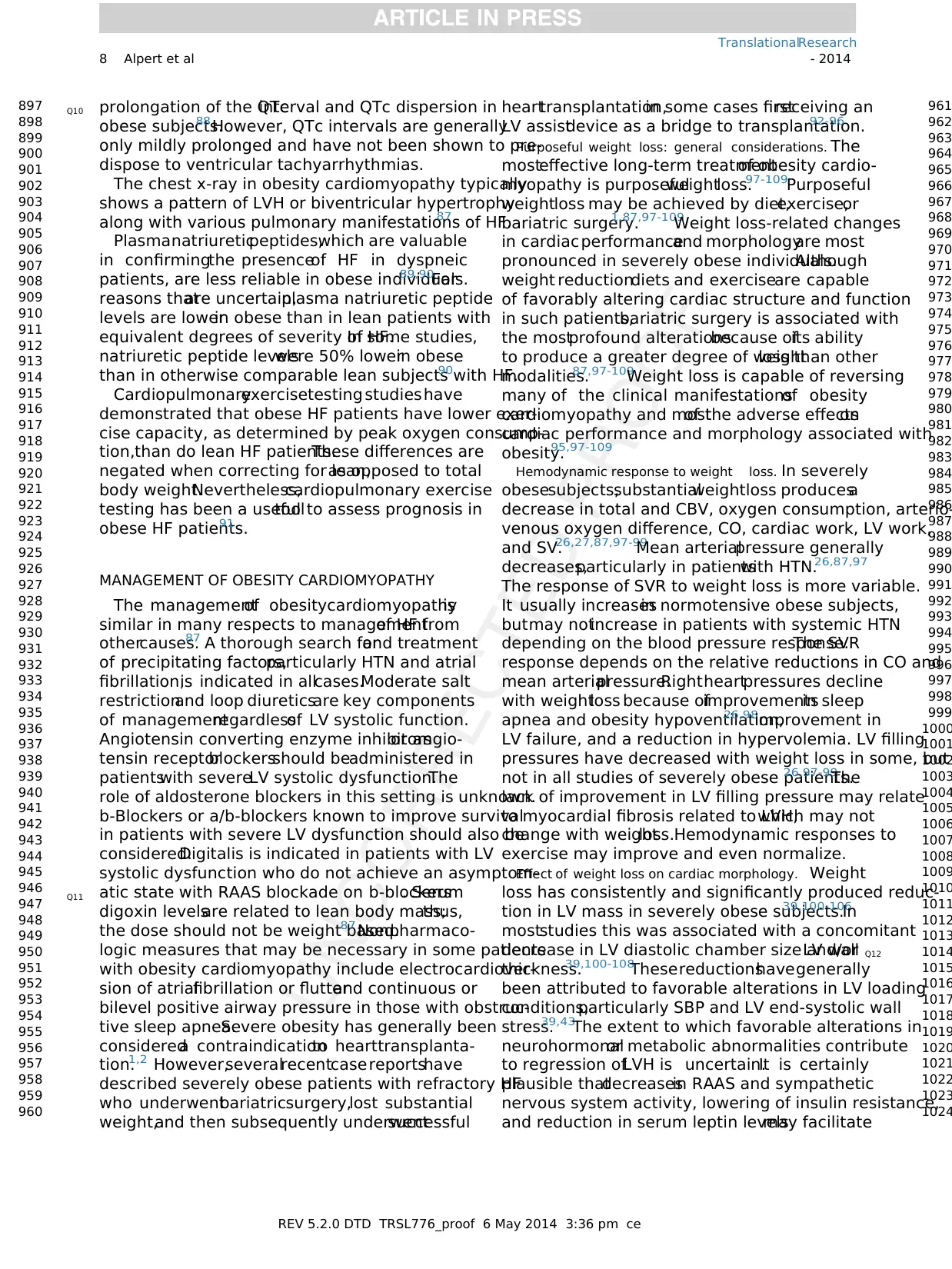
prolongation of the QTcQ10 interval and QTc dispersion in
obese subjects.88 However, QTc intervals are generally
only mildly prolonged and have not been shown to pre-
dispose to ventricular tachyarrhythmias.
The chest x-ray in obesity cardiomyopathy typically
shows a pattern of LVH or biventricular hypertrophy
along with various pulmonary manifestations of HF.87
Plasmanatriureticpeptides,which are valuable
in confirmingthe presenceof HF in dyspneic
patients, are less reliable in obese individuals.89,90
For
reasons thatare uncertain,plasma natriuretic peptide
levels are lowerin obese than in lean patients with
equivalent degrees of severity of HF.In some studies,
natriuretic peptide levelswere 50% lowerin obese
than in otherwise comparable lean subjects with HF.90
Cardiopulmonaryexercisetesting studieshave
demonstrated that obese HF patients have lower exer-
cise capacity, as determined by peak oxygen consump-
tion,than do lean HF patients.These differences are
negated when correcting for lean,as opposed to total
body weight.Nevertheless,cardiopulmonary exercise
testing has been a usefultool to assess prognosis in
obese HF patients.91
MANAGEMENT OF OBESITY CARDIOMYOPATHY
The managementof obesitycardiomyopathyis
similar in many respects to managementof HF from
othercauses.87 A thorough search forand treatment
of precipitating factors,particularly HTN and atrial
fibrillation,is indicated in allcases.Moderate salt
restrictionand loop diureticsare key components
of managementregardlessof LV systolic function.
Angiotensin converting enzyme inhibitorsor angio-
tensin receptorblockersshould beadministered in
patientswith severeLV systolic dysfunction.The
role of aldosterone blockers in this setting is unknown.
b-Blockers or a/b-blockers known to improve survival
in patients with severe LV dysfunction should also be
considered.Digitalis is indicated in patients with LV
systolic dysfunction who do not achieve an asymptom-
atic state with RAAS blockade on b-blockersQ11 . Serum
digoxin levelsare related to lean body mass;thus,
the dose should not be weight based.87 Nonpharmaco-
logic measures that may be necessary in some patients
with obesity cardiomyopathy include electrocardiover-
sion of atrialfibrillation or flutterand continuous or
bilevel positive airway pressure in those with obstruc-
tive sleep apnea.Severe obesity has generally been
considereda contraindicationto hearttransplanta-
tion.1,2 However,severalrecentcasereportshave
described severely obese patients with refractory HF
who underwentbariatricsurgery,lost substantial
weight,and then subsequently underwentsuccessful
hearttransplantation,in some cases firstreceiving an
LV assistdevice as a bridge to transplantation.92-96
Purposeful weight loss: general considerations. The
mosteffective long-term treatmentof obesity cardio-
myopathy is purposefulweightloss.97-109Purposeful
weightloss may be achieved by diet,exercise,or
bariatric surgery.1,87,97-109
Weight loss-related changes
in cardiac performanceand morphologyare most
pronounced in severely obese individuals.Although
weight reductiondiets and exerciseare capable
of favorably altering cardiac structure and function
in such patients,bariatric surgery is associated with
the mostprofound alterationsbecause ofits ability
to produce a greater degree of weightloss than other
modalities.87,97-109
Weight loss is capable of reversing
many of the clinical manifestationsof obesity
cardiomyopathy and mostof the adverse effectson
cardiac performance and morphology associated with
obesity.95,97-109
Hemodynamic response to weight loss. In severely
obesesubjects,substantialweightloss producesa
decrease in total and CBV, oxygen consumption, arterio-
venous oxygen difference, CO, cardiac work, LV work,
and SV.26,27,87,97-99
Mean arterialpressure generally
decreases,particularly in patientswith HTN.26,87,97
The response of SVR to weight loss is more variable.
It usually increasesin normotensive obese subjects,
butmay notincrease in patients with systemic HTN
depending on the blood pressure response.The SVR
response depends on the relative reductions in CO and
mean arterialpressure.Rightheartpressures decline
with weightloss because ofimprovementsin sleep
apnea and obesity hypoventilation,26,98
improvement in
LV failure, and a reduction in hypervolemia. LV filling
pressures have decreased with weight loss in some, but
not in all studies of severely obese patients.26,97-99
The
lack of improvement in LV filling pressure may relate
to myocardial fibrosis related to LVH,which may not
change with weightloss.Hemodynamic responses to
exercise may improve and even normalize.
Effect of weight loss on cardiac morphology. Weight
loss has consistently and significantly produced reduc-
tion in LV mass in severely obese subjects.39,100-106
In
moststudies this was associated with a concomitant
decrease in LV diastolic chamber size and/or Q12LV wall
thickness.39,100-108
Thesereductionshavegenerally
been attributed to favorable alterations in LV loading
conditions,particularly SBP and LV end-systolic wall
stress.39,43
The extent to which favorable alterations in
neurohormonalor metabolic abnormalities contribute
to regression ofLVH is uncertain.It is certainly
plausible thatdecreasesin RAAS and sympathetic
nervous system activity, lowering of insulin resistance,
and reduction in serum leptin levelsmay facilitate
REV 5.2.0 DTD TRSL776_proof 6 May 2014 3:36 pm ce
TranslationalResearch
8 Alpert et al - 2014
897
898
899
900
901
902
903
904
905
906
907
908
909
910
911
912
913
914
915
916
917
918
919
920
921
922
923
924
925
926
927
928
929
930
931
932
933
934
935
936
937
938
939
940
941
942
943
944
945
946
947
948
949
950
951
952
953
954
955
956
957
958
959
960
961
962
963
964
965
966
967
968
969
970
971
972
973
974
975
976
977
978
979
980
981
982
983
984
985
986
987
988
989
990
991
992
993
994
995
996
997
998
999
1000
1001
1002
1003
1004
1005
1006
1007
1008
1009
1010
1011
1012
1013
1014
1015
1016
1017
1018
1019
1020
1021
1022
1023
1024
obese subjects.88 However, QTc intervals are generally
only mildly prolonged and have not been shown to pre-
dispose to ventricular tachyarrhythmias.
The chest x-ray in obesity cardiomyopathy typically
shows a pattern of LVH or biventricular hypertrophy
along with various pulmonary manifestations of HF.87
Plasmanatriureticpeptides,which are valuable
in confirmingthe presenceof HF in dyspneic
patients, are less reliable in obese individuals.89,90
For
reasons thatare uncertain,plasma natriuretic peptide
levels are lowerin obese than in lean patients with
equivalent degrees of severity of HF.In some studies,
natriuretic peptide levelswere 50% lowerin obese
than in otherwise comparable lean subjects with HF.90
Cardiopulmonaryexercisetesting studieshave
demonstrated that obese HF patients have lower exer-
cise capacity, as determined by peak oxygen consump-
tion,than do lean HF patients.These differences are
negated when correcting for lean,as opposed to total
body weight.Nevertheless,cardiopulmonary exercise
testing has been a usefultool to assess prognosis in
obese HF patients.91
MANAGEMENT OF OBESITY CARDIOMYOPATHY
The managementof obesitycardiomyopathyis
similar in many respects to managementof HF from
othercauses.87 A thorough search forand treatment
of precipitating factors,particularly HTN and atrial
fibrillation,is indicated in allcases.Moderate salt
restrictionand loop diureticsare key components
of managementregardlessof LV systolic function.
Angiotensin converting enzyme inhibitorsor angio-
tensin receptorblockersshould beadministered in
patientswith severeLV systolic dysfunction.The
role of aldosterone blockers in this setting is unknown.
b-Blockers or a/b-blockers known to improve survival
in patients with severe LV dysfunction should also be
considered.Digitalis is indicated in patients with LV
systolic dysfunction who do not achieve an asymptom-
atic state with RAAS blockade on b-blockersQ11 . Serum
digoxin levelsare related to lean body mass;thus,
the dose should not be weight based.87 Nonpharmaco-
logic measures that may be necessary in some patients
with obesity cardiomyopathy include electrocardiover-
sion of atrialfibrillation or flutterand continuous or
bilevel positive airway pressure in those with obstruc-
tive sleep apnea.Severe obesity has generally been
considereda contraindicationto hearttransplanta-
tion.1,2 However,severalrecentcasereportshave
described severely obese patients with refractory HF
who underwentbariatricsurgery,lost substantial
weight,and then subsequently underwentsuccessful
hearttransplantation,in some cases firstreceiving an
LV assistdevice as a bridge to transplantation.92-96
Purposeful weight loss: general considerations. The
mosteffective long-term treatmentof obesity cardio-
myopathy is purposefulweightloss.97-109Purposeful
weightloss may be achieved by diet,exercise,or
bariatric surgery.1,87,97-109
Weight loss-related changes
in cardiac performanceand morphologyare most
pronounced in severely obese individuals.Although
weight reductiondiets and exerciseare capable
of favorably altering cardiac structure and function
in such patients,bariatric surgery is associated with
the mostprofound alterationsbecause ofits ability
to produce a greater degree of weightloss than other
modalities.87,97-109
Weight loss is capable of reversing
many of the clinical manifestationsof obesity
cardiomyopathy and mostof the adverse effectson
cardiac performance and morphology associated with
obesity.95,97-109
Hemodynamic response to weight loss. In severely
obesesubjects,substantialweightloss producesa
decrease in total and CBV, oxygen consumption, arterio-
venous oxygen difference, CO, cardiac work, LV work,
and SV.26,27,87,97-99
Mean arterialpressure generally
decreases,particularly in patientswith HTN.26,87,97
The response of SVR to weight loss is more variable.
It usually increasesin normotensive obese subjects,
butmay notincrease in patients with systemic HTN
depending on the blood pressure response.The SVR
response depends on the relative reductions in CO and
mean arterialpressure.Rightheartpressures decline
with weightloss because ofimprovementsin sleep
apnea and obesity hypoventilation,26,98
improvement in
LV failure, and a reduction in hypervolemia. LV filling
pressures have decreased with weight loss in some, but
not in all studies of severely obese patients.26,97-99
The
lack of improvement in LV filling pressure may relate
to myocardial fibrosis related to LVH,which may not
change with weightloss.Hemodynamic responses to
exercise may improve and even normalize.
Effect of weight loss on cardiac morphology. Weight
loss has consistently and significantly produced reduc-
tion in LV mass in severely obese subjects.39,100-106
In
moststudies this was associated with a concomitant
decrease in LV diastolic chamber size and/or Q12LV wall
thickness.39,100-108
Thesereductionshavegenerally
been attributed to favorable alterations in LV loading
conditions,particularly SBP and LV end-systolic wall
stress.39,43
The extent to which favorable alterations in
neurohormonalor metabolic abnormalities contribute
to regression ofLVH is uncertain.It is certainly
plausible thatdecreasesin RAAS and sympathetic
nervous system activity, lowering of insulin resistance,
and reduction in serum leptin levelsmay facilitate
REV 5.2.0 DTD TRSL776_proof 6 May 2014 3:36 pm ce
TranslationalResearch
8 Alpert et al - 2014
897
898
899
900
901
902
903
904
905
906
907
908
909
910
911
912
913
914
915
916
917
918
919
920
921
922
923
924
925
926
927
928
929
930
931
932
933
934
935
936
937
938
939
940
941
942
943
944
945
946
947
948
949
950
951
952
953
954
955
956
957
958
959
960
961
962
963
964
965
966
967
968
969
970
971
972
973
974
975
976
977
978
979
980
981
982
983
984
985
986
987
988
989
990
991
992
993
994
995
996
997
998
999
1000
1001
1002
1003
1004
1005
1006
1007
1008
1009
1010
1011
1012
1013
1014
1015
1016
1017
1018
1019
1020
1021
1022
1023
1024
reverse remodeling of the LV. In several studies the LV
radius-to-thicknessratio or relativewall thickness
decreased with substantial weight loss.39,100-106
In one
recentstudy,the incidence of abnormalLV geometry
(concentric LV remodeling or hypertrophy and eccen-
tric LVH) decreasedfrom 70.7% to 42.5% with
substantial weight loss in severely obese subjects.102
Although the mostdramatic reductions in LV mass
have occurred in severely obese patients, usually after bar-
iatric surgery, studies of class I and II obese patients have
consistently shown significantdecreases in LV mass,
usually associated with diet and exercise.39,102,104
When
studied,left atrialdimension/volumeQ13 has reportedly
decreased with weightloss in patientswith severe
obesity.39Limited information suggests that weight loss
is also capable of reducing RV chamber size.100
Effect of weight loss on LV diastolic function.As noted
previously,hemodynamicstudiesassessing LVEDP
or pulmonary capillary wedge pressure have shown
variable responses to weightloss.Some studies have
shown a decrease,whereasothershaveshown no
change.In contrast,studies using noninvasive cardiac
techniques to assess LV diastolic filling have consis-
tently shown improvement with weight reduction,not
only in severely obese patients,but also in class I and
II obese patients.65,100,102-107
One study demonstrated
improvementin LV filling in severely obese subjects
only in thosewith LVH.70 Most studiesassessing
LV diastolic function noninvasively have used load-
sensitivetechniques.65,70,100,102-107
Not surprisingly,
improved LV loading conditionsafterweightloss
havecorrelated strongly with improvementin LV
diastolicfilling. More recentstudiesusing tissue
Doppler imaging to assess LV diastolic function have
shown improvementin mitral annularvelocitiesin
diastole in all classes of obesity.3,41,74
Why there is a
lack of concordancebetweenweight loss-related
changes in LVEDP and weight loss-related changes in
LV diastolic filling assessed noninvasively is unknown.
Effect of weight loss on LV systolic function.In severely
obese patients,LV systolic function assessed using LV
ejection phase indices is usually normal or supranormal.
Thus, it is not surprising that most studies assessing LV
systolicfunction beforeand afterweightloss have
reported no significantdifference.75,76,106,107
In one
study,LV systolic function in severely obese patients
improved afterweightloss predominantly in those
with LV systolic dysfunction beforeweightloss.76
In contrast,recentstudiesusing tissue Dopplerand
speckle track imaging to evaluate LV systolic function
before and after weight loss have reported improvement
in mitral annular velocities in systole and reduction of
myocardialdeformation in allclasses of obesity,even
when LV ejection phase indices were normal.3,41,74,100
ThesefindingssuggestthatsubclinicalLV systolic
dysfunction occurs commonly in obesity and may be
reversible with weight loss.
Effect of weight loss on clinical manifestations of obesity
cardiomyopathy. Surprisingly little information exists
concerning the effectof weightloss on the clinical
manifestations of obesity cardiomyopathy. Estes et al108
reported reversal of such manifestations as somnolence,
periodic breathing,and polycythemia as wellas less
dyspnea in 5 of 6 severely obese subjects studied after
weight loss ranging from 38 to143 pounds.In a study
of 14 severely obese patients with HF,a substantial
weight loss was achieved with bariatric surgery Alpert
et al14 reported improvements in New York functional
class from II to I in 5,from III to I in 3,and from III
to II in 4 subjects.Two class III patients experienced
no improvement. Class IV patients were not included in
the study.Miranda et al109studied the effect of weight
loss in 13 severely obese patients (bariatric surgery in
7 and diet in 6 patients).Significantimprovement
in quality oflife, dyspnea,and leg edema occurred
exclusively in patients undergoing bariatric surgery.109
These results suggest that substantial weight loss (parti-
cularly from bariatric surgery) produces improvement
in symptoms and signs of HF in severely obese patients
with obesity cardiomyopathy and should beconsi-
dered for this reason.There are no large-scale studies
assessingthe effectof purposefulweightloss on
mortality in severely obese patients.
Whether purposefulweightloss improves mortality
risk in class I and II obese patients with HF is unknown.
Obesity is less likely to be the driving factor for HF in
such patients.The obesity paradox,discussed previ-
ously, suggests that the presence of overweightedness,
class I obesity, and possibly class II obesity is associated
with lower mortality rates than those of underweight
or normal weight persons.Some studies have actually
reported a worse prognosis with weightreduction in
such individuals; however, these studies did not exclude
patients with nonpurposeful weight loss.1,2
CONCLUSIONS Q14
Obesity is both a risk factor for and a direct cause of
HF. Severe obesity in particular is capable of producing
hemodynamic alterations that may cause cardiac remod-
eling and changes in ventricular function that may lead
to LV and RV failure (Fig 1).Certain neurohormonal
and metabolic abnormalities associated with obesity
may contribute to this process.Purposeful weight loss
is the mosteffective long-term measure for reversing
abnormalities of cardiac performance and morphology
associated with obesity and for improving the clinical
manifestations of HF in patients with obesity cardiomy-
opathy.
REV 5.2.0 DTD TRSL776_proof 6 May 2014 3:36 pm ce
TranslationalResearch
Volume -, Number - Alpert et al 9
1025
1026
1027
1028
1029
1030
1031
1032
1033
1034
1035
1036
1037
1038
1039
1040
1041
1042
1043
1044
1045
1046
1047
1048
1049
1050
1051
1052
1053
1054
1055
1056
1057
1058
1059
1060
1061
1062
1063
1064
1065
1066
1067
1068
1069
1070
1071
1072
1073
1074
1075
1076
1077
1078
1079
1080
1081
1082
1083
1084
1085
1086
1087
1088
1089
1090
1091
1092
1093
1094
1095
1096
1097
1098
1099
1100
1101
1102
1103
1104
1105
1106
1107
1108
1109
1110
1111
1112
1113
1114
1115
1116
1117
1118
1119
1120
1121
1122
1123
1124
1125
1126
1127
1128
1129
1130
1131
1132
1133
1134
1135
1136
1137
1138
1139
1140
1141
1142
1143
1144
1145
1146
1147
1148
1149
1150
1151
1152
radius-to-thicknessratio or relativewall thickness
decreased with substantial weight loss.39,100-106
In one
recentstudy,the incidence of abnormalLV geometry
(concentric LV remodeling or hypertrophy and eccen-
tric LVH) decreasedfrom 70.7% to 42.5% with
substantial weight loss in severely obese subjects.102
Although the mostdramatic reductions in LV mass
have occurred in severely obese patients, usually after bar-
iatric surgery, studies of class I and II obese patients have
consistently shown significantdecreases in LV mass,
usually associated with diet and exercise.39,102,104
When
studied,left atrialdimension/volumeQ13 has reportedly
decreased with weightloss in patientswith severe
obesity.39Limited information suggests that weight loss
is also capable of reducing RV chamber size.100
Effect of weight loss on LV diastolic function.As noted
previously,hemodynamicstudiesassessing LVEDP
or pulmonary capillary wedge pressure have shown
variable responses to weightloss.Some studies have
shown a decrease,whereasothershaveshown no
change.In contrast,studies using noninvasive cardiac
techniques to assess LV diastolic filling have consis-
tently shown improvement with weight reduction,not
only in severely obese patients,but also in class I and
II obese patients.65,100,102-107
One study demonstrated
improvementin LV filling in severely obese subjects
only in thosewith LVH.70 Most studiesassessing
LV diastolic function noninvasively have used load-
sensitivetechniques.65,70,100,102-107
Not surprisingly,
improved LV loading conditionsafterweightloss
havecorrelated strongly with improvementin LV
diastolicfilling. More recentstudiesusing tissue
Doppler imaging to assess LV diastolic function have
shown improvementin mitral annularvelocitiesin
diastole in all classes of obesity.3,41,74
Why there is a
lack of concordancebetweenweight loss-related
changes in LVEDP and weight loss-related changes in
LV diastolic filling assessed noninvasively is unknown.
Effect of weight loss on LV systolic function.In severely
obese patients,LV systolic function assessed using LV
ejection phase indices is usually normal or supranormal.
Thus, it is not surprising that most studies assessing LV
systolicfunction beforeand afterweightloss have
reported no significantdifference.75,76,106,107
In one
study,LV systolic function in severely obese patients
improved afterweightloss predominantly in those
with LV systolic dysfunction beforeweightloss.76
In contrast,recentstudiesusing tissue Dopplerand
speckle track imaging to evaluate LV systolic function
before and after weight loss have reported improvement
in mitral annular velocities in systole and reduction of
myocardialdeformation in allclasses of obesity,even
when LV ejection phase indices were normal.3,41,74,100
ThesefindingssuggestthatsubclinicalLV systolic
dysfunction occurs commonly in obesity and may be
reversible with weight loss.
Effect of weight loss on clinical manifestations of obesity
cardiomyopathy. Surprisingly little information exists
concerning the effectof weightloss on the clinical
manifestations of obesity cardiomyopathy. Estes et al108
reported reversal of such manifestations as somnolence,
periodic breathing,and polycythemia as wellas less
dyspnea in 5 of 6 severely obese subjects studied after
weight loss ranging from 38 to143 pounds.In a study
of 14 severely obese patients with HF,a substantial
weight loss was achieved with bariatric surgery Alpert
et al14 reported improvements in New York functional
class from II to I in 5,from III to I in 3,and from III
to II in 4 subjects.Two class III patients experienced
no improvement. Class IV patients were not included in
the study.Miranda et al109studied the effect of weight
loss in 13 severely obese patients (bariatric surgery in
7 and diet in 6 patients).Significantimprovement
in quality oflife, dyspnea,and leg edema occurred
exclusively in patients undergoing bariatric surgery.109
These results suggest that substantial weight loss (parti-
cularly from bariatric surgery) produces improvement
in symptoms and signs of HF in severely obese patients
with obesity cardiomyopathy and should beconsi-
dered for this reason.There are no large-scale studies
assessingthe effectof purposefulweightloss on
mortality in severely obese patients.
Whether purposefulweightloss improves mortality
risk in class I and II obese patients with HF is unknown.
Obesity is less likely to be the driving factor for HF in
such patients.The obesity paradox,discussed previ-
ously, suggests that the presence of overweightedness,
class I obesity, and possibly class II obesity is associated
with lower mortality rates than those of underweight
or normal weight persons.Some studies have actually
reported a worse prognosis with weightreduction in
such individuals; however, these studies did not exclude
patients with nonpurposeful weight loss.1,2
CONCLUSIONS Q14
Obesity is both a risk factor for and a direct cause of
HF. Severe obesity in particular is capable of producing
hemodynamic alterations that may cause cardiac remod-
eling and changes in ventricular function that may lead
to LV and RV failure (Fig 1).Certain neurohormonal
and metabolic abnormalities associated with obesity
may contribute to this process.Purposeful weight loss
is the mosteffective long-term measure for reversing
abnormalities of cardiac performance and morphology
associated with obesity and for improving the clinical
manifestations of HF in patients with obesity cardiomy-
opathy.
REV 5.2.0 DTD TRSL776_proof 6 May 2014 3:36 pm ce
TranslationalResearch
Volume -, Number - Alpert et al 9
1025
1026
1027
1028
1029
1030
1031
1032
1033
1034
1035
1036
1037
1038
1039
1040
1041
1042
1043
1044
1045
1046
1047
1048
1049
1050
1051
1052
1053
1054
1055
1056
1057
1058
1059
1060
1061
1062
1063
1064
1065
1066
1067
1068
1069
1070
1071
1072
1073
1074
1075
1076
1077
1078
1079
1080
1081
1082
1083
1084
1085
1086
1087
1088
1089
1090
1091
1092
1093
1094
1095
1096
1097
1098
1099
1100
1101
1102
1103
1104
1105
1106
1107
1108
1109
1110
1111
1112
1113
1114
1115
1116
1117
1118
1119
1120
1121
1122
1123
1124
1125
1126
1127
1128
1129
1130
1131
1132
1133
1134
1135
1136
1137
1138
1139
1140
1141
1142
1143
1144
1145
1146
1147
1148
1149
1150
1151
1152
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
The manuscripthas been reviewed and approved by allnamed
authors.
REFERENCES
1. Lavie CJ, Alpert MA, Arena R, Mehra MR, Milani RV,
Ventura HO. Impact of obesity and the obesity paradox on prev-
alence and prognosis in heart failure. J Am Coll Cardiol Heart
Failure 2013;1:93–102.
2. Lavie CJ,Milani RV,Ventura HO.Obesity and cardiovascular
disease: risk factors,paradox and impact of weight loss.J Am
Coll Cardiol 2009;53:1925–32.
3. Alpert MA, Omran J, Mehra A, Ardhanari S. Impact of obesity
and weightloss on cardiac performance and morphology in
adults. Prog Cardiovasc Dis 2014;56:391–400.
4. World Health Organization Technical Report 894. Obesity: pre-
venting and managing the globalepidemic.Geneva:World
Health Organization, 2000.
5. Poirier P, Cornier MA, Mazzone T, et al., for the American Heart
Association Obesity Committee ofthe Councilon Nutrition,
Physical Activity and Metabolism. Bariatric surgery and cardio-
vascular risk factors: a scientific statement from the American
Heart Association. Circulation 2011;19:1683–701.
6. Poirier P, Alpert MA, Fleisher LA, et al., for the American Heart
Association Obesity Committee ofthe Councilof Nutrition,
Physical Activity and Metabolism and the Council on Cardiopul-
monary Peri-operative and Critical Care. Cardiovascular evalua-
tion and managementof severely-obese patients undergoing
surgery: a science advisory from the American Heart Associa-
tion. Circulation 2009;120:86–95.
7. Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifi-
able risk factors associated with myocardialinfarction in 52
countries. The INTERHEART study: case-control study. Lancet
2004;364:937–52.
8. HuntSA, Abraham WT,Chin MH,et al. 2009 Update incor-
porated into the ACC/AHA 2005 guidelines for the diagnosis
and managementof heartfailure in adults.Circulation 2009;
119:e391.
9. Mckee PA, Castelli WP, McNamara PM, Kannel WR. The natu-
ral history of congestive heartfailure:the Framingham study.
N Engl J Med 1971;285:1441–6.
10. Anh LV, Horwich TB, Fonarow GC. Epidemiology and risk pro-
file in heart failure. Nat Rev Cardiol 2011;8:30–41.
11. Roger VL.Epidemiology of heart failure.Circ Res 2013;113:
646–59.
12. Owan TE, Hodge DO, Herges RM, et al. Trends in prevalence
and outcome of heartfailure with preserved ejection fraction.
N Engl J Med 2006;355:251–9.
13. Garg N, SenthilkumarA, NusairMB, Goyal N, Garg RK,
Alpert MA. Heart failure with a normal left ventricular ejection
fraction: epidemiology, pathophysiology, diagnosis and manage-
ment. Am J Med Sci 2013;346:129–36.
14. Alpert MA,Terry BE,Mulekar M,et al.Cardiac morphology
and leftventricular function in morbidly obese patients with
and withoutcongestive heartfailure.Am J Cardiol 1997;80:
736–40.
15. Kenchaiah S,Evans JC,Levy D,et al.Obesity and the risk of
heart failure. N Engl J Med 2002;347:305–13.
16. Baena-Diez JM, Bynam AO, Grau M, et al. Obesity as an inde-
pendent risk factor for heart failure: Zona Franco Cohort Study.
Clin Cardiol 2010;33:760–4.
17. Nicklas BJ, Lesari M, Penninx BW, et al. Abdominal obesity is
an independent risk factor for heart failure in older people. J Am
Geriatr Soc 2006;54:413–20.
18. OreopoulosA, PadwalR, Kalantar-Zadeh K,Fonarow GC,
Norris GM, McAlister FA. Body mass index in heart failure: a
meta-analysis. Am Heart J 2008;156:13–22.
19. PadwalR, McAlisterFA, McMurray JJ, et al. The obesity
paradox in patients with preserved versus reduced ejection frac-
tion: a meta-analysis of individual patient data. Int J Obes 2013.
http://dx.doi.org/10.1038/ijo.2013.203. Q15
20. Clark AL, Chya J,Horwich TB.The obesity paradox in men
versus women with systolic heart failure.Am J Cardiol 2012;
110:77–82.
21. Fonarow GC,Srikanthan P,Costanzo R,et al. The obesity
paradox in acute heart failure: analysis of body mass index and
in-hospital mortality for 108,927 patients in the Acute Decom-
pensated HeartFailure NationalRegistry.Am HeartJ 2007;
153:74–81.
22. Clark AL, Fonarow GC,Horwich TB.Waistcircumference,
body mass index and survival in systolic heart failure: the obesity
paradox. J Card Fail 2011;17:374–80.
23. Alexander JK, Dennis EW, Smith WG, et al. Blood volume, car-
diac output and distribution of systemic blood flow in extreme
obesity. Cardiovasc Res Cent Bull 1962;1:39–44.
24. Alexander JK. Obesity and cardiac performance. Am J Cardiol
1964;14:860–5.
25. DeDivitiis O, Fazio S, Petitto M, et al. Obesity and cardiac func-
tion. Circulation 1981;64:477–82.
26. AlexanderJK, Alpert MA. Hemodynamicalterationswith
obesity in man.In: Alpert MA,Alexander JK,eds.The heart
and lung in obesity. Armonk, NY: Futura Publishing Co, 1998:
45–56.
27. Alaud-din A, Meteressian S, Lisbona R, et al. Assessment of car-
diac function in patients who were morbidly obese.Surgery
1982;92:226–35.
28. Kasper EK,Hruban RH,Baughman KL.Cardiomyopathy of
obesity: a clinical pathological evaluation of 43 obese patients
with heart failure. Am J Cardiol 1992;70:921–4.
29. Neeland IJ, Gupta S, Ayers CR, et al. Relation of regional fat dis-
tribution to left ventricular structure and function. Circ Cardio-
vasc Imaging 2013;6:800–7.
30. Kaltman AJ,Goldring RM.Role of circulatory congestion in
the cardiorespiratory failure ofobesity.Am J Med 1976;60:
645–53.
31. Backman C,Freyschuss U,Hallberg D,et al. Cardiovascular
function in extreme obesity. Acta Med Scand 1973;193:437–46.
32. Fazio S, Ferraro S, De Simone G, et al. Hemodynamic adaptation
in severe obesity with or without arterial hypertension. Cardiolo-
gia 1989;34:967–72.
33. Thakur V, Richards R, Reisin E. Obesity, hypertension and the
heart. Am J Med Sci 2001;321:242–8.
34. Smith HL, Willius FA. Adiposity of the heart. Arch Intern Med
1933;52:911–31.
35. Lillington GA, Anderson MW, Branden-Gurg RO. The cardiore-
spiratory syndrome of obesity. Dis Chest 1957;32:1–20.
36. Amad RH, Brennan JC, Alexander JK. The cardiac pathology of
obesity. Circulation 1965;32:740–5.
37. Alexander JK, Pettigrove JK. Obesity and congestive heart fail-
ure. Geriatrics 1967;22:101–8.
38. Warnes CA, Roberts WC. The heart in massive (more than 300
pounds or 136 kilograms) obesity. Analysis of 12 patients studies
at necropsy. Am J Cardiol 1989;54:1087–91.
39. Alpert MA, Alexander JK. Cardiac morphology and obesity in
man. In: Alpert MA, Alexander JK, eds. The heart and lung in
obesity. Armonk, NY: Futura Publishing Co, 1998:25–49.
40. Abel ED, Litwin SE, Sweeney G. Cardiac remodeling in obesity.
Physiol Rev 2008;88:389–419.
REV 5.2.0 DTD TRSL776_proof 6 May 2014 3:36 pm ce
TranslationalResearch
10 Alpert et al - 2014
1153
1154
1155
1156
1157
1158
1159
1160
1161
1162
1163
1164
1165
1166
1167
1168
1169
1170
1171
1172
1173
1174
1175
1176
1177
1178
1179
1180
1181
1182
1183
1184
1185
1186
1187
1188
1189
1190
1191
1192
1193
1194
1195
1196
1197
1198
1199
1200
1201
1202
1203
1204
1205
1206
1207
1208
1209
1210
1211
1212
1213
1214
1215
1216
1217
1218
1219
1220
1221
1222
1223
1224
1225
1226
1227
1228
1229
1230
1231
1232
1233
1234
1235
1236
1237
1238
1239
1240
1241
1242
1243
1244
1245
1246
1247
1248
1249
1250
1251
1252
1253
1254
1255
1256
1257
1258
1259
1260
1261
1262
1263
1264
1265
1266
1267
1268
1269
1270
1271
1272
1273
1274
1275
1276
1277
1278
1279
1280
authors.
REFERENCES
1. Lavie CJ, Alpert MA, Arena R, Mehra MR, Milani RV,
Ventura HO. Impact of obesity and the obesity paradox on prev-
alence and prognosis in heart failure. J Am Coll Cardiol Heart
Failure 2013;1:93–102.
2. Lavie CJ,Milani RV,Ventura HO.Obesity and cardiovascular
disease: risk factors,paradox and impact of weight loss.J Am
Coll Cardiol 2009;53:1925–32.
3. Alpert MA, Omran J, Mehra A, Ardhanari S. Impact of obesity
and weightloss on cardiac performance and morphology in
adults. Prog Cardiovasc Dis 2014;56:391–400.
4. World Health Organization Technical Report 894. Obesity: pre-
venting and managing the globalepidemic.Geneva:World
Health Organization, 2000.
5. Poirier P, Cornier MA, Mazzone T, et al., for the American Heart
Association Obesity Committee ofthe Councilon Nutrition,
Physical Activity and Metabolism. Bariatric surgery and cardio-
vascular risk factors: a scientific statement from the American
Heart Association. Circulation 2011;19:1683–701.
6. Poirier P, Alpert MA, Fleisher LA, et al., for the American Heart
Association Obesity Committee ofthe Councilof Nutrition,
Physical Activity and Metabolism and the Council on Cardiopul-
monary Peri-operative and Critical Care. Cardiovascular evalua-
tion and managementof severely-obese patients undergoing
surgery: a science advisory from the American Heart Associa-
tion. Circulation 2009;120:86–95.
7. Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifi-
able risk factors associated with myocardialinfarction in 52
countries. The INTERHEART study: case-control study. Lancet
2004;364:937–52.
8. HuntSA, Abraham WT,Chin MH,et al. 2009 Update incor-
porated into the ACC/AHA 2005 guidelines for the diagnosis
and managementof heartfailure in adults.Circulation 2009;
119:e391.
9. Mckee PA, Castelli WP, McNamara PM, Kannel WR. The natu-
ral history of congestive heartfailure:the Framingham study.
N Engl J Med 1971;285:1441–6.
10. Anh LV, Horwich TB, Fonarow GC. Epidemiology and risk pro-
file in heart failure. Nat Rev Cardiol 2011;8:30–41.
11. Roger VL.Epidemiology of heart failure.Circ Res 2013;113:
646–59.
12. Owan TE, Hodge DO, Herges RM, et al. Trends in prevalence
and outcome of heartfailure with preserved ejection fraction.
N Engl J Med 2006;355:251–9.
13. Garg N, SenthilkumarA, NusairMB, Goyal N, Garg RK,
Alpert MA. Heart failure with a normal left ventricular ejection
fraction: epidemiology, pathophysiology, diagnosis and manage-
ment. Am J Med Sci 2013;346:129–36.
14. Alpert MA,Terry BE,Mulekar M,et al.Cardiac morphology
and leftventricular function in morbidly obese patients with
and withoutcongestive heartfailure.Am J Cardiol 1997;80:
736–40.
15. Kenchaiah S,Evans JC,Levy D,et al.Obesity and the risk of
heart failure. N Engl J Med 2002;347:305–13.
16. Baena-Diez JM, Bynam AO, Grau M, et al. Obesity as an inde-
pendent risk factor for heart failure: Zona Franco Cohort Study.
Clin Cardiol 2010;33:760–4.
17. Nicklas BJ, Lesari M, Penninx BW, et al. Abdominal obesity is
an independent risk factor for heart failure in older people. J Am
Geriatr Soc 2006;54:413–20.
18. OreopoulosA, PadwalR, Kalantar-Zadeh K,Fonarow GC,
Norris GM, McAlister FA. Body mass index in heart failure: a
meta-analysis. Am Heart J 2008;156:13–22.
19. PadwalR, McAlisterFA, McMurray JJ, et al. The obesity
paradox in patients with preserved versus reduced ejection frac-
tion: a meta-analysis of individual patient data. Int J Obes 2013.
http://dx.doi.org/10.1038/ijo.2013.203. Q15
20. Clark AL, Chya J,Horwich TB.The obesity paradox in men
versus women with systolic heart failure.Am J Cardiol 2012;
110:77–82.
21. Fonarow GC,Srikanthan P,Costanzo R,et al. The obesity
paradox in acute heart failure: analysis of body mass index and
in-hospital mortality for 108,927 patients in the Acute Decom-
pensated HeartFailure NationalRegistry.Am HeartJ 2007;
153:74–81.
22. Clark AL, Fonarow GC,Horwich TB.Waistcircumference,
body mass index and survival in systolic heart failure: the obesity
paradox. J Card Fail 2011;17:374–80.
23. Alexander JK, Dennis EW, Smith WG, et al. Blood volume, car-
diac output and distribution of systemic blood flow in extreme
obesity. Cardiovasc Res Cent Bull 1962;1:39–44.
24. Alexander JK. Obesity and cardiac performance. Am J Cardiol
1964;14:860–5.
25. DeDivitiis O, Fazio S, Petitto M, et al. Obesity and cardiac func-
tion. Circulation 1981;64:477–82.
26. AlexanderJK, Alpert MA. Hemodynamicalterationswith
obesity in man.In: Alpert MA,Alexander JK,eds.The heart
and lung in obesity. Armonk, NY: Futura Publishing Co, 1998:
45–56.
27. Alaud-din A, Meteressian S, Lisbona R, et al. Assessment of car-
diac function in patients who were morbidly obese.Surgery
1982;92:226–35.
28. Kasper EK,Hruban RH,Baughman KL.Cardiomyopathy of
obesity: a clinical pathological evaluation of 43 obese patients
with heart failure. Am J Cardiol 1992;70:921–4.
29. Neeland IJ, Gupta S, Ayers CR, et al. Relation of regional fat dis-
tribution to left ventricular structure and function. Circ Cardio-
vasc Imaging 2013;6:800–7.
30. Kaltman AJ,Goldring RM.Role of circulatory congestion in
the cardiorespiratory failure ofobesity.Am J Med 1976;60:
645–53.
31. Backman C,Freyschuss U,Hallberg D,et al. Cardiovascular
function in extreme obesity. Acta Med Scand 1973;193:437–46.
32. Fazio S, Ferraro S, De Simone G, et al. Hemodynamic adaptation
in severe obesity with or without arterial hypertension. Cardiolo-
gia 1989;34:967–72.
33. Thakur V, Richards R, Reisin E. Obesity, hypertension and the
heart. Am J Med Sci 2001;321:242–8.
34. Smith HL, Willius FA. Adiposity of the heart. Arch Intern Med
1933;52:911–31.
35. Lillington GA, Anderson MW, Branden-Gurg RO. The cardiore-
spiratory syndrome of obesity. Dis Chest 1957;32:1–20.
36. Amad RH, Brennan JC, Alexander JK. The cardiac pathology of
obesity. Circulation 1965;32:740–5.
37. Alexander JK, Pettigrove JK. Obesity and congestive heart fail-
ure. Geriatrics 1967;22:101–8.
38. Warnes CA, Roberts WC. The heart in massive (more than 300
pounds or 136 kilograms) obesity. Analysis of 12 patients studies
at necropsy. Am J Cardiol 1989;54:1087–91.
39. Alpert MA, Alexander JK. Cardiac morphology and obesity in
man. In: Alpert MA, Alexander JK, eds. The heart and lung in
obesity. Armonk, NY: Futura Publishing Co, 1998:25–49.
40. Abel ED, Litwin SE, Sweeney G. Cardiac remodeling in obesity.
Physiol Rev 2008;88:389–419.
REV 5.2.0 DTD TRSL776_proof 6 May 2014 3:36 pm ce
TranslationalResearch
10 Alpert et al - 2014
1153
1154
1155
1156
1157
1158
1159
1160
1161
1162
1163
1164
1165
1166
1167
1168
1169
1170
1171
1172
1173
1174
1175
1176
1177
1178
1179
1180
1181
1182
1183
1184
1185
1186
1187
1188
1189
1190
1191
1192
1193
1194
1195
1196
1197
1198
1199
1200
1201
1202
1203
1204
1205
1206
1207
1208
1209
1210
1211
1212
1213
1214
1215
1216
1217
1218
1219
1220
1221
1222
1223
1224
1225
1226
1227
1228
1229
1230
1231
1232
1233
1234
1235
1236
1237
1238
1239
1240
1241
1242
1243
1244
1245
1246
1247
1248
1249
1250
1251
1252
1253
1254
1255
1256
1257
1258
1259
1260
1261
1262
1263
1264
1265
1266
1267
1268
1269
1270
1271
1272
1273
1274
1275
1276
1277
1278
1279
1280
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
41. Wong C,Marwick TH.Obesity cardiomyopathy: pathogenesis
and pathophysiology. Nature Clin Pract Cardiovasc Med 2007;
4:436–43.
42. Alpert MA. Obesity cardiomyopathy. Pathophysiology and evo-
lution of the clinical syndrome. Am J Med Sci 2001;321:225–36.
43. Alpert MA, Terry BE, Kelly DL. Effect of weight loss on cardiac
chambersize,wall thickness and leftventricularfunction in
morbid obesity. Am J Cardiol 1985;55:783–6.
44. Zema MJ, Caccavano M. Feasibility of detailed M-mode echo-
cardiographic examination in markedly obese adults.Prospec-
tive study of 50 patients. J Clin Ultrasound 1982;10:31–4.
45. Garcia LC, Laredo C, Arriaga J, et al. Echocardiographic find-
ings in obesity. Rev Invest Clin 1982;34:235–42.
46. Messerli FH,Sundgaard-Riise K,Reisin ED,et al.Dimorphic
cardiac adaptation to obesity and arterialhypertension.Ann
Intern Med 1983;94:757–61.Q16
47. Nakajima T, Fujioka S, Tokunaga K, et al. Non-invasive study of
left ventricular performance in obese patients: influence of dura-
tion of obesity. Circulation 1985;71:481–5.
48. Alpert MA, Lambert CR, Panayiotou H, et al. Relation of dura-
tion of morbid obesity to left ventricular mass, systolic function
and diastolic filling,and effectof weightloss.Am J Cardiol
1996;76:1194–7.
49. Alpert MA, Lambert CR, Terry BE, et al. Effect of weight loss
on leftventricular mass in non-hypertensive morbidity obese
patients. Am J Cardiol 1994;73:918–21.
50. Danias RG,Tritos NA,Stuber M,et al.Cardiac structure and
function in the obese:a cardiac magnetic resonance imaging
study. J Cardiac Res 2003;5:431–8.
51. Iacobellis G, Ribaudo MC, Leto G, et al. Influence of excess fat
on cardiac morphology and function and function in uncompli-
cated obesity. Obes Res 2002;10:767–73.
52. Tian ZQ, Zhong J, Zhao ZG, et al. Relationship between abdom-
inal obesity and left ventricular weight/function. Zhonghua Xin
Xue Guan Bing Za Zhi 2007;35:155–8.
53. Bella JN, Devereux RB, Roman MJ, et al. Relations of left ven-
tricular mass to fat-free and adipose body mass: the Strong Heart
Study. Circulation 1998;98:2538–44.
54. Aurigemma GP, de Simone G, Fitzgibbons TP. Cardiac remodel-
ing in obesity. Circ Cardiovasc Imaging 2013;6:442–52.
55. Woodwiss AJ,Libhaber CD,Majane OHI,etal. Obesity pro-
motes left ventricular concentric rather than eccentric geometric
remodeling and hypertrophy independent of blood pressure. Am
J Hypertens 2008;21:1149–53.
56. Lauer MS, Anderson KM, Kannel WB, Levy D. The impact of
obesity on leftventricularmass and geometry.JAMA 1991;
266:231–6.
57. Lavie CJ, Milani RV, Patel D, et al. Disparate effects of hyperten-
sion and obesity on left ventricular geometry and mortality in
8088 elderly patients with preserved systolic function. Postgrad
Med 2009;121:119–25.
58. Smalcelj A, Pulievic D, Buljievic B, Brida V. Left ventricular hy-
pertrophy in obese hypertensives: is it really eccentric? An Echo-
cardiographic Study. Coll Antropol 2000;24:167–83.
59. Peterson LR, Waggoner AD, Schectman KB, et al. Alterations in
left ventricular structure and function in young healthy obese
women. J Am Coll Cardiol 2004;43:1388–404.
60. Turkbey EB, McClelland RL, Kronmal RA, et al. The impact of
obesity on the left ventricle; the multi-ethnic study of atheroscle-
rosis (MESA). JACC Cardiovasc Imaging 2010;3:266–74.
61. IacobellisG, Ribaudo MC,Zappaterreno A,et al. Adapted
changesin left ventricularstructure and function in severe
uncomplicated obesity. Obes Res 2004;12:1616–21.
62. Okpura IC, Adediran OS,Odia OJ,et al.Left ventricular geo-
metric patterns in obese Nigerian adults: an Echocardiographic
Study. Internet J Intern Med 2010;9:1–7.
63. Sasson Z, Rasooly Y, Gupta R, Rasooly I. Left atrial enlargement
in healthy obese: prevalence and relation to ventricular mass and
diastolic function. Am J Cardiol 1996;12:257–63.
64. Chahai H, McCelland RL, Tandai H, et al. Obesity and right ven-
tricularstructure and function:the MESA-RightVentricular
Study. Chest 2012;141:388–95.
65. Chakko S, Alpert MA. Obesity and ventricular function in man:
diastolic function. In: Alpert MA, Alexander JK, eds. The heart
and lung in obesity. Armonk, NY: Futura Publishing Co, 1998:
57–76.
66. Ferraro S, Pessone-Filardo P, Desiderio A, et al. Left ventricular
systolic and diastolic function in severe obesity: a radionuclide
study. Cardiology 1996;82:347–53.
67. Stoddard MF,Tseuda K,Thomas M,et al. The influence of
obesity on left ventricular filling and systolic function. Am Heart
J 1992;124:894–9.
68. Chakko S, Mayor M, Allison MD, et al. Abnormal left ventric-
ular diastolic filling in eccentric left ventricular hypertrophy of
obesity. Am J Cardiol 1991;68:95–8.
69. Pascual M, Pascual DA, Soria F, et al. Effects of isolated obesity
on systolic and diastolic left ventricular function. Heart 2003;89:
1152–6.
70. Alpert MA, Lambert CR, Terry BE, et al. Effect of weight loss on
left ventricular diastolic filling in morbid obesity. Am J Cardiol
1997;80:736–40.
71. Herszkowicz N,Barbato A,Salvi W, et al. Contribution of
Doppler echocardiography to the evaluation of systolic and dia-
stolic function of obese women versus a control group. Arq Bras
Cardiol 2001;76:189–96.
72. Ku CS, Lin S, Wang DJ, et al. Left ventricular filling in young
normotensive obese adults. Am J Cardiol 1994;73:613–5.
73. Talano AC, Bitigen A, Cevik C, et al. The role of tissue Doppler
study in the assessment of left ventricular dysfunction in obesity.
Acta Cardiol 2008;63:541–6.
74. Kossaify A, NicolaisN. Impactof overweightand obesity
on left ventriculardiastolicfunctionand value of tissue
Dopplerechocardiography.Clin Med Insights Cardiol2013;
7:43–50.
75. Alpert MA, Alexander JK.Obesity and ventricular function in
man: systolic function. In: Alpert MA, Alexander JK, eds. The
heart and lung in obesity.Armouk, NY: Futura Publishing Co,
1998:77–94.
76. Alpert MA, Terry BE, Lambert CR, et al. Factors influencing left
ventricular systolic function in non-hypertensive morbidly obese
patients and effect of weight loss induced by gastroplasty. Am J
Cardiol 1993;75:773–7.
77. Tumuklu MM, Etikan I, Kucasik B, et al. Effect of obesity on left
ventricular structure and myocardialsystolic function:assess-
ment by tissue Doppler imaging and strain/strain rate imaging.
Echocardiography 2007;24:802–9.
78. Barbosa MM, Beleigoli AM, de Fatima Diniz M, et al. Strain im-
aging and morbid obesity:insightinto subclinicalventricular
dysfunction. Clin Cardiol 2011;34:288–93.
79. Orhan AL, Uslu N, Davi SU, et al. Effects of isolated obesity on
left and right ventricular function: a tissue Doppler and strain
rate imaging study. Echocardiography 2010;22:236–43.
80. Gulel O, Yuksel S, Soylu K, et al. Evaluation of left atrial func-
tions by color tissue Doppler imaging in adults with body mass
indexes $ 30 kg/m2 or those with , 30 kg/m2. J Cardiovasc Im-
aging 2009;25:272–7.
REV 5.2.0 DTD TRSL776_proof 6 May 2014 3:36 pm ce
TranslationalResearch
Volume -, Number - Alpert et al 11
1281
1282
1283
1284
1285
1286
1287
1288
1289
1290
1291
1292
1293
1294
1295
1296
1297
1298
1299
1300
1301
1302
1303
1304
1305
1306
1307
1308
1309
1310
1311
1312
1313
1314
1315
1316
1317
1318
1319
1320
1321
1322
1323
1324
1325
1326
1327
1328
1329
1330
1331
1332
1333
1334
1335
1336
1337
1338
1339
1340
1341
1342
1343
1344
1345
1346
1347
1348
1349
1350
1351
1352
1353
1354
1355
1356
1357
1358
1359
1360
1361
1362
1363
1364
1365
1366
1367
1368
1369
1370
1371
1372
1373
1374
1375
1376
1377
1378
1379
1380
1381
1382
1383
1384
1385
1386
1387
1388
1389
1390
1391
1392
1393
1394
1395
1396
1397
1398
1399
1400
1401
1402
1403
1404
1405
1406
1407
1408
and pathophysiology. Nature Clin Pract Cardiovasc Med 2007;
4:436–43.
42. Alpert MA. Obesity cardiomyopathy. Pathophysiology and evo-
lution of the clinical syndrome. Am J Med Sci 2001;321:225–36.
43. Alpert MA, Terry BE, Kelly DL. Effect of weight loss on cardiac
chambersize,wall thickness and leftventricularfunction in
morbid obesity. Am J Cardiol 1985;55:783–6.
44. Zema MJ, Caccavano M. Feasibility of detailed M-mode echo-
cardiographic examination in markedly obese adults.Prospec-
tive study of 50 patients. J Clin Ultrasound 1982;10:31–4.
45. Garcia LC, Laredo C, Arriaga J, et al. Echocardiographic find-
ings in obesity. Rev Invest Clin 1982;34:235–42.
46. Messerli FH,Sundgaard-Riise K,Reisin ED,et al.Dimorphic
cardiac adaptation to obesity and arterialhypertension.Ann
Intern Med 1983;94:757–61.Q16
47. Nakajima T, Fujioka S, Tokunaga K, et al. Non-invasive study of
left ventricular performance in obese patients: influence of dura-
tion of obesity. Circulation 1985;71:481–5.
48. Alpert MA, Lambert CR, Panayiotou H, et al. Relation of dura-
tion of morbid obesity to left ventricular mass, systolic function
and diastolic filling,and effectof weightloss.Am J Cardiol
1996;76:1194–7.
49. Alpert MA, Lambert CR, Terry BE, et al. Effect of weight loss
on leftventricular mass in non-hypertensive morbidity obese
patients. Am J Cardiol 1994;73:918–21.
50. Danias RG,Tritos NA,Stuber M,et al.Cardiac structure and
function in the obese:a cardiac magnetic resonance imaging
study. J Cardiac Res 2003;5:431–8.
51. Iacobellis G, Ribaudo MC, Leto G, et al. Influence of excess fat
on cardiac morphology and function and function in uncompli-
cated obesity. Obes Res 2002;10:767–73.
52. Tian ZQ, Zhong J, Zhao ZG, et al. Relationship between abdom-
inal obesity and left ventricular weight/function. Zhonghua Xin
Xue Guan Bing Za Zhi 2007;35:155–8.
53. Bella JN, Devereux RB, Roman MJ, et al. Relations of left ven-
tricular mass to fat-free and adipose body mass: the Strong Heart
Study. Circulation 1998;98:2538–44.
54. Aurigemma GP, de Simone G, Fitzgibbons TP. Cardiac remodel-
ing in obesity. Circ Cardiovasc Imaging 2013;6:442–52.
55. Woodwiss AJ,Libhaber CD,Majane OHI,etal. Obesity pro-
motes left ventricular concentric rather than eccentric geometric
remodeling and hypertrophy independent of blood pressure. Am
J Hypertens 2008;21:1149–53.
56. Lauer MS, Anderson KM, Kannel WB, Levy D. The impact of
obesity on leftventricularmass and geometry.JAMA 1991;
266:231–6.
57. Lavie CJ, Milani RV, Patel D, et al. Disparate effects of hyperten-
sion and obesity on left ventricular geometry and mortality in
8088 elderly patients with preserved systolic function. Postgrad
Med 2009;121:119–25.
58. Smalcelj A, Pulievic D, Buljievic B, Brida V. Left ventricular hy-
pertrophy in obese hypertensives: is it really eccentric? An Echo-
cardiographic Study. Coll Antropol 2000;24:167–83.
59. Peterson LR, Waggoner AD, Schectman KB, et al. Alterations in
left ventricular structure and function in young healthy obese
women. J Am Coll Cardiol 2004;43:1388–404.
60. Turkbey EB, McClelland RL, Kronmal RA, et al. The impact of
obesity on the left ventricle; the multi-ethnic study of atheroscle-
rosis (MESA). JACC Cardiovasc Imaging 2010;3:266–74.
61. IacobellisG, Ribaudo MC,Zappaterreno A,et al. Adapted
changesin left ventricularstructure and function in severe
uncomplicated obesity. Obes Res 2004;12:1616–21.
62. Okpura IC, Adediran OS,Odia OJ,et al.Left ventricular geo-
metric patterns in obese Nigerian adults: an Echocardiographic
Study. Internet J Intern Med 2010;9:1–7.
63. Sasson Z, Rasooly Y, Gupta R, Rasooly I. Left atrial enlargement
in healthy obese: prevalence and relation to ventricular mass and
diastolic function. Am J Cardiol 1996;12:257–63.
64. Chahai H, McCelland RL, Tandai H, et al. Obesity and right ven-
tricularstructure and function:the MESA-RightVentricular
Study. Chest 2012;141:388–95.
65. Chakko S, Alpert MA. Obesity and ventricular function in man:
diastolic function. In: Alpert MA, Alexander JK, eds. The heart
and lung in obesity. Armonk, NY: Futura Publishing Co, 1998:
57–76.
66. Ferraro S, Pessone-Filardo P, Desiderio A, et al. Left ventricular
systolic and diastolic function in severe obesity: a radionuclide
study. Cardiology 1996;82:347–53.
67. Stoddard MF,Tseuda K,Thomas M,et al. The influence of
obesity on left ventricular filling and systolic function. Am Heart
J 1992;124:894–9.
68. Chakko S, Mayor M, Allison MD, et al. Abnormal left ventric-
ular diastolic filling in eccentric left ventricular hypertrophy of
obesity. Am J Cardiol 1991;68:95–8.
69. Pascual M, Pascual DA, Soria F, et al. Effects of isolated obesity
on systolic and diastolic left ventricular function. Heart 2003;89:
1152–6.
70. Alpert MA, Lambert CR, Terry BE, et al. Effect of weight loss on
left ventricular diastolic filling in morbid obesity. Am J Cardiol
1997;80:736–40.
71. Herszkowicz N,Barbato A,Salvi W, et al. Contribution of
Doppler echocardiography to the evaluation of systolic and dia-
stolic function of obese women versus a control group. Arq Bras
Cardiol 2001;76:189–96.
72. Ku CS, Lin S, Wang DJ, et al. Left ventricular filling in young
normotensive obese adults. Am J Cardiol 1994;73:613–5.
73. Talano AC, Bitigen A, Cevik C, et al. The role of tissue Doppler
study in the assessment of left ventricular dysfunction in obesity.
Acta Cardiol 2008;63:541–6.
74. Kossaify A, NicolaisN. Impactof overweightand obesity
on left ventriculardiastolicfunctionand value of tissue
Dopplerechocardiography.Clin Med Insights Cardiol2013;
7:43–50.
75. Alpert MA, Alexander JK.Obesity and ventricular function in
man: systolic function. In: Alpert MA, Alexander JK, eds. The
heart and lung in obesity.Armouk, NY: Futura Publishing Co,
1998:77–94.
76. Alpert MA, Terry BE, Lambert CR, et al. Factors influencing left
ventricular systolic function in non-hypertensive morbidly obese
patients and effect of weight loss induced by gastroplasty. Am J
Cardiol 1993;75:773–7.
77. Tumuklu MM, Etikan I, Kucasik B, et al. Effect of obesity on left
ventricular structure and myocardialsystolic function:assess-
ment by tissue Doppler imaging and strain/strain rate imaging.
Echocardiography 2007;24:802–9.
78. Barbosa MM, Beleigoli AM, de Fatima Diniz M, et al. Strain im-
aging and morbid obesity:insightinto subclinicalventricular
dysfunction. Clin Cardiol 2011;34:288–93.
79. Orhan AL, Uslu N, Davi SU, et al. Effects of isolated obesity on
left and right ventricular function: a tissue Doppler and strain
rate imaging study. Echocardiography 2010;22:236–43.
80. Gulel O, Yuksel S, Soylu K, et al. Evaluation of left atrial func-
tions by color tissue Doppler imaging in adults with body mass
indexes $ 30 kg/m2 or those with , 30 kg/m2. J Cardiovasc Im-
aging 2009;25:272–7.
REV 5.2.0 DTD TRSL776_proof 6 May 2014 3:36 pm ce
TranslationalResearch
Volume -, Number - Alpert et al 11
1281
1282
1283
1284
1285
1286
1287
1288
1289
1290
1291
1292
1293
1294
1295
1296
1297
1298
1299
1300
1301
1302
1303
1304
1305
1306
1307
1308
1309
1310
1311
1312
1313
1314
1315
1316
1317
1318
1319
1320
1321
1322
1323
1324
1325
1326
1327
1328
1329
1330
1331
1332
1333
1334
1335
1336
1337
1338
1339
1340
1341
1342
1343
1344
1345
1346
1347
1348
1349
1350
1351
1352
1353
1354
1355
1356
1357
1358
1359
1360
1361
1362
1363
1364
1365
1366
1367
1368
1369
1370
1371
1372
1373
1374
1375
1376
1377
1378
1379
1380
1381
1382
1383
1384
1385
1386
1387
1388
1389
1390
1391
1392
1393
1394
1395
1396
1397
1398
1399
1400
1401
1402
1403
1404
1405
1406
1407
1408
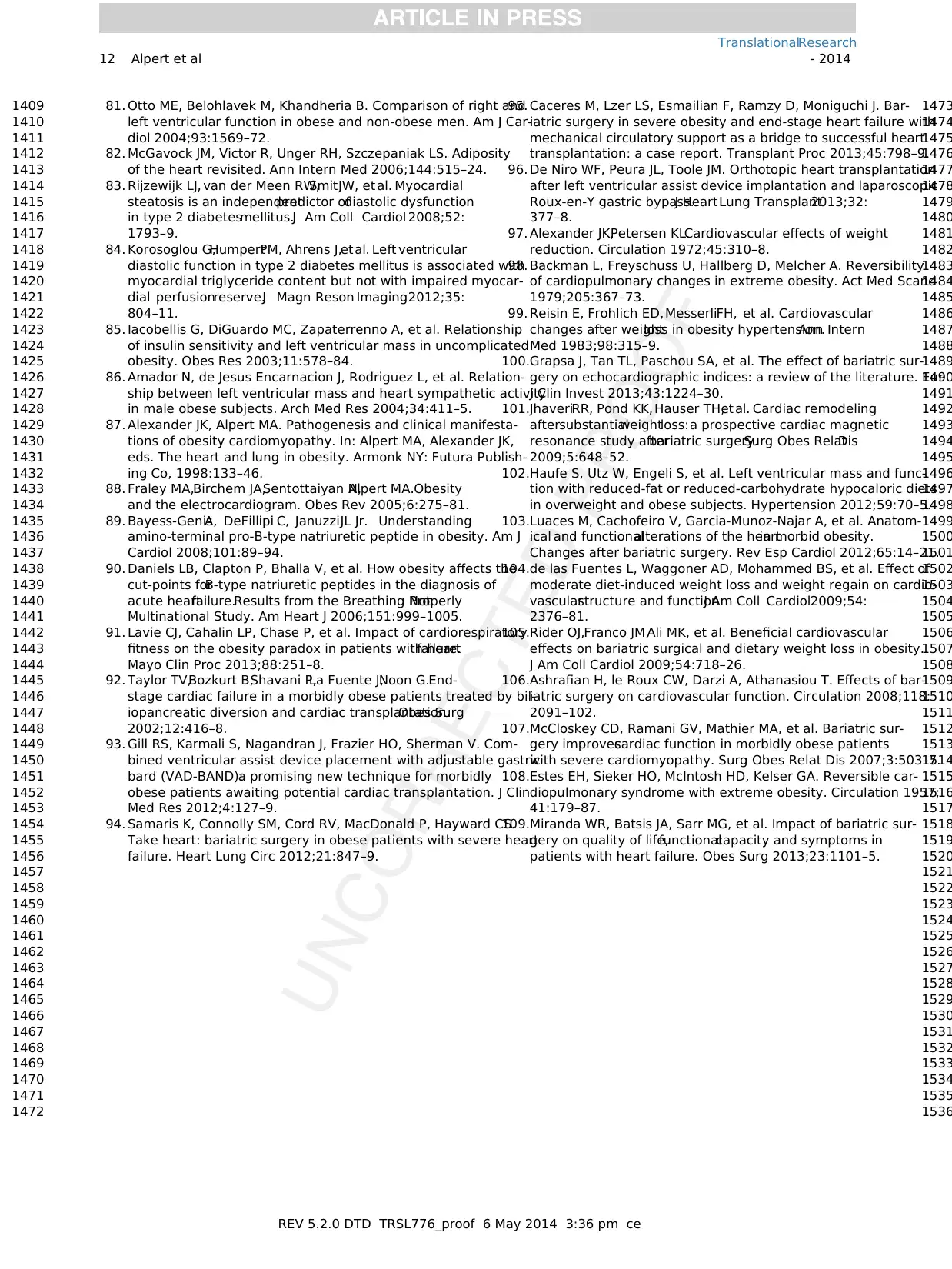
81. Otto ME, Belohlavek M, Khandheria B. Comparison of right and
left ventricular function in obese and non-obese men. Am J Car-
diol 2004;93:1569–72.
82. McGavock JM, Victor R, Unger RH, Szczepaniak LS. Adiposity
of the heart revisited. Ann Intern Med 2006;144:515–24.
83. Rijzewijk LJ, van der Meen RW,SmitJW, et al. Myocardial
steatosis is an independentpredictor ofdiastolic dysfunction
in type 2 diabetesmellitus.J Am Coll Cardiol 2008;52:
1793–9.
84. Korosoglou G,HumpertPM, Ahrens J,et al. Left ventricular
diastolic function in type 2 diabetes mellitus is associated with
myocardial triglyceride content but not with impaired myocar-
dial perfusionreserve.J Magn Reson Imaging2012;35:
804–11.
85. Iacobellis G, DiGuardo MC, Zapaterrenno A, et al. Relationship
of insulin sensitivity and left ventricular mass in uncomplicated
obesity. Obes Res 2003;11:578–84.
86. Amador N, de Jesus Encarnacion J, Rodriguez L, et al. Relation-
ship between left ventricular mass and heart sympathetic activity
in male obese subjects. Arch Med Res 2004;34:411–5.
87. Alexander JK, Alpert MA. Pathogenesis and clinical manifesta-
tions of obesity cardiomyopathy. In: Alpert MA, Alexander JK,
eds. The heart and lung in obesity. Armonk NY: Futura Publish-
ing Co, 1998:133–46.
88. Fraley MA,Birchem JA,Sentottaiyan N,Alpert MA.Obesity
and the electrocardiogram. Obes Rev 2005;6:275–81.
89. Bayess-GenisA, DeFillipi C, JanuzziJL Jr. Understanding
amino-terminal pro-B-type natriuretic peptide in obesity. Am J
Cardiol 2008;101:89–94.
90. Daniels LB, Clapton P, Bhalla V, et al. How obesity affects the
cut-points forB-type natriuretic peptides in the diagnosis of
acute heartfailure.Results from the Breathing NotProperly
Multinational Study. Am Heart J 2006;151:999–1005.
91. Lavie CJ, Cahalin LP, Chase P, et al. Impact of cardiorespiratory
fitness on the obesity paradox in patients with heartfailure.
Mayo Clin Proc 2013;88:251–8.
92. Taylor TV,Bozkurt B,Shavani P,La Fuente J,Noon G.End-
stage cardiac failure in a morbidly obese patients treated by bil-
iopancreatic diversion and cardiac transplantation.Obes Surg
2002;12:416–8.
93. Gill RS, Karmali S, Nagandran J, Frazier HO, Sherman V. Com-
bined ventricular assist device placement with adjustable gastric
bard (VAD-BAND):a promising new technique for morbidly
obese patients awaiting potential cardiac transplantation. J Clin
Med Res 2012;4:127–9.
94. Samaris K, Connolly SM, Cord RV, MacDonald P, Hayward CS.
Take heart: bariatric surgery in obese patients with severe heart
failure. Heart Lung Circ 2012;21:847–9.
95. Caceres M, Lzer LS, Esmailian F, Ramzy D, Moniguchi J. Bar-
iatric surgery in severe obesity and end-stage heart failure with
mechanical circulatory support as a bridge to successful heart
transplantation: a case report. Transplant Proc 2013;45:798–9.
96. De Niro WF, Peura JL, Toole JM. Orthotopic heart transplantation
after left ventricular assist device implantation and laparoscopic
Roux-en-Y gastric bypass.J HeartLung Transplant2013;32:
377–8.
97. Alexander JK,Petersen KL.Cardiovascular effects of weight
reduction. Circulation 1972;45:310–8.
98. Backman L, Freyschuss U, Hallberg D, Melcher A. Reversibility
of cardiopulmonary changes in extreme obesity. Act Med Scand
1979;205:367–73.
99. Reisin E, Frohlich ED, MesserliFH, et al. Cardiovascular
changes after weightloss in obesity hypertension.Ann Intern
Med 1983;98:315–9.
100.Grapsa J, Tan TL, Paschou SA, et al. The effect of bariatric sur-
gery on echocardiographic indices: a review of the literature. Eur
J Clin Invest 2013;43:1224–30.
101.JhaveriRR, Pond KK, Hauser TH,et al. Cardiac remodeling
aftersubstantialweightloss:a prospective cardiac magnetic
resonance study afterbariatric surgery.Surg Obes RelatDis
2009;5:648–52.
102.Haufe S, Utz W, Engeli S, et al. Left ventricular mass and func-
tion with reduced-fat or reduced-carbohydrate hypocaloric diets
in overweight and obese subjects. Hypertension 2012;59:70–5.
103.Luaces M, Cachofeiro V, Garcia-Munoz-Najar A, et al. Anatom-
ical and functionalalterations of the heartin morbid obesity.
Changes after bariatric surgery. Rev Esp Cardiol 2012;65:14–21.
104.de las Fuentes L, Waggoner AD, Mohammed BS, et al. Effect of
moderate diet-induced weight loss and weight regain on cardio-
vascularstructure and function.J Am Coll Cardiol2009;54:
2376–81.
105.Rider OJ,Franco JM,Ali MK, et al. Beneficial cardiovascular
effects on bariatric surgical and dietary weight loss in obesity.
J Am Coll Cardiol 2009;54:718–26.
106.Ashrafian H, le Roux CW, Darzi A, Athanasiou T. Effects of bar-
iatric surgery on cardiovascular function. Circulation 2008;118:
2091–102.
107.McCloskey CD, Ramani GV, Mathier MA, et al. Bariatric sur-
gery improvescardiac function in morbidly obese patients
with severe cardiomyopathy. Surg Obes Relat Dis 2007;3:503–7.
108.Estes EH, Sieker HO, McIntosh HD, Kelser GA. Reversible car-
diopulmonary syndrome with extreme obesity. Circulation 1957;
41:179–87.
109.Miranda WR, Batsis JA, Sarr MG, et al. Impact of bariatric sur-
gery on quality of life,functionalcapacity and symptoms in
patients with heart failure. Obes Surg 2013;23:1101–5.
REV 5.2.0 DTD TRSL776_proof 6 May 2014 3:36 pm ce
TranslationalResearch
12 Alpert et al - 2014
1409
1410
1411
1412
1413
1414
1415
1416
1417
1418
1419
1420
1421
1422
1423
1424
1425
1426
1427
1428
1429
1430
1431
1432
1433
1434
1435
1436
1437
1438
1439
1440
1441
1442
1443
1444
1445
1446
1447
1448
1449
1450
1451
1452
1453
1454
1455
1456
1457
1458
1459
1460
1461
1462
1463
1464
1465
1466
1467
1468
1469
1470
1471
1472
1473
1474
1475
1476
1477
1478
1479
1480
1481
1482
1483
1484
1485
1486
1487
1488
1489
1490
1491
1492
1493
1494
1495
1496
1497
1498
1499
1500
1501
1502
1503
1504
1505
1506
1507
1508
1509
1510
1511
1512
1513
1514
1515
1516
1517
1518
1519
1520
1521
1522
1523
1524
1525
1526
1527
1528
1529
1530
1531
1532
1533
1534
1535
1536
left ventricular function in obese and non-obese men. Am J Car-
diol 2004;93:1569–72.
82. McGavock JM, Victor R, Unger RH, Szczepaniak LS. Adiposity
of the heart revisited. Ann Intern Med 2006;144:515–24.
83. Rijzewijk LJ, van der Meen RW,SmitJW, et al. Myocardial
steatosis is an independentpredictor ofdiastolic dysfunction
in type 2 diabetesmellitus.J Am Coll Cardiol 2008;52:
1793–9.
84. Korosoglou G,HumpertPM, Ahrens J,et al. Left ventricular
diastolic function in type 2 diabetes mellitus is associated with
myocardial triglyceride content but not with impaired myocar-
dial perfusionreserve.J Magn Reson Imaging2012;35:
804–11.
85. Iacobellis G, DiGuardo MC, Zapaterrenno A, et al. Relationship
of insulin sensitivity and left ventricular mass in uncomplicated
obesity. Obes Res 2003;11:578–84.
86. Amador N, de Jesus Encarnacion J, Rodriguez L, et al. Relation-
ship between left ventricular mass and heart sympathetic activity
in male obese subjects. Arch Med Res 2004;34:411–5.
87. Alexander JK, Alpert MA. Pathogenesis and clinical manifesta-
tions of obesity cardiomyopathy. In: Alpert MA, Alexander JK,
eds. The heart and lung in obesity. Armonk NY: Futura Publish-
ing Co, 1998:133–46.
88. Fraley MA,Birchem JA,Sentottaiyan N,Alpert MA.Obesity
and the electrocardiogram. Obes Rev 2005;6:275–81.
89. Bayess-GenisA, DeFillipi C, JanuzziJL Jr. Understanding
amino-terminal pro-B-type natriuretic peptide in obesity. Am J
Cardiol 2008;101:89–94.
90. Daniels LB, Clapton P, Bhalla V, et al. How obesity affects the
cut-points forB-type natriuretic peptides in the diagnosis of
acute heartfailure.Results from the Breathing NotProperly
Multinational Study. Am Heart J 2006;151:999–1005.
91. Lavie CJ, Cahalin LP, Chase P, et al. Impact of cardiorespiratory
fitness on the obesity paradox in patients with heartfailure.
Mayo Clin Proc 2013;88:251–8.
92. Taylor TV,Bozkurt B,Shavani P,La Fuente J,Noon G.End-
stage cardiac failure in a morbidly obese patients treated by bil-
iopancreatic diversion and cardiac transplantation.Obes Surg
2002;12:416–8.
93. Gill RS, Karmali S, Nagandran J, Frazier HO, Sherman V. Com-
bined ventricular assist device placement with adjustable gastric
bard (VAD-BAND):a promising new technique for morbidly
obese patients awaiting potential cardiac transplantation. J Clin
Med Res 2012;4:127–9.
94. Samaris K, Connolly SM, Cord RV, MacDonald P, Hayward CS.
Take heart: bariatric surgery in obese patients with severe heart
failure. Heart Lung Circ 2012;21:847–9.
95. Caceres M, Lzer LS, Esmailian F, Ramzy D, Moniguchi J. Bar-
iatric surgery in severe obesity and end-stage heart failure with
mechanical circulatory support as a bridge to successful heart
transplantation: a case report. Transplant Proc 2013;45:798–9.
96. De Niro WF, Peura JL, Toole JM. Orthotopic heart transplantation
after left ventricular assist device implantation and laparoscopic
Roux-en-Y gastric bypass.J HeartLung Transplant2013;32:
377–8.
97. Alexander JK,Petersen KL.Cardiovascular effects of weight
reduction. Circulation 1972;45:310–8.
98. Backman L, Freyschuss U, Hallberg D, Melcher A. Reversibility
of cardiopulmonary changes in extreme obesity. Act Med Scand
1979;205:367–73.
99. Reisin E, Frohlich ED, MesserliFH, et al. Cardiovascular
changes after weightloss in obesity hypertension.Ann Intern
Med 1983;98:315–9.
100.Grapsa J, Tan TL, Paschou SA, et al. The effect of bariatric sur-
gery on echocardiographic indices: a review of the literature. Eur
J Clin Invest 2013;43:1224–30.
101.JhaveriRR, Pond KK, Hauser TH,et al. Cardiac remodeling
aftersubstantialweightloss:a prospective cardiac magnetic
resonance study afterbariatric surgery.Surg Obes RelatDis
2009;5:648–52.
102.Haufe S, Utz W, Engeli S, et al. Left ventricular mass and func-
tion with reduced-fat or reduced-carbohydrate hypocaloric diets
in overweight and obese subjects. Hypertension 2012;59:70–5.
103.Luaces M, Cachofeiro V, Garcia-Munoz-Najar A, et al. Anatom-
ical and functionalalterations of the heartin morbid obesity.
Changes after bariatric surgery. Rev Esp Cardiol 2012;65:14–21.
104.de las Fuentes L, Waggoner AD, Mohammed BS, et al. Effect of
moderate diet-induced weight loss and weight regain on cardio-
vascularstructure and function.J Am Coll Cardiol2009;54:
2376–81.
105.Rider OJ,Franco JM,Ali MK, et al. Beneficial cardiovascular
effects on bariatric surgical and dietary weight loss in obesity.
J Am Coll Cardiol 2009;54:718–26.
106.Ashrafian H, le Roux CW, Darzi A, Athanasiou T. Effects of bar-
iatric surgery on cardiovascular function. Circulation 2008;118:
2091–102.
107.McCloskey CD, Ramani GV, Mathier MA, et al. Bariatric sur-
gery improvescardiac function in morbidly obese patients
with severe cardiomyopathy. Surg Obes Relat Dis 2007;3:503–7.
108.Estes EH, Sieker HO, McIntosh HD, Kelser GA. Reversible car-
diopulmonary syndrome with extreme obesity. Circulation 1957;
41:179–87.
109.Miranda WR, Batsis JA, Sarr MG, et al. Impact of bariatric sur-
gery on quality of life,functionalcapacity and symptoms in
patients with heart failure. Obes Surg 2013;23:1101–5.
REV 5.2.0 DTD TRSL776_proof 6 May 2014 3:36 pm ce
TranslationalResearch
12 Alpert et al - 2014
1409
1410
1411
1412
1413
1414
1415
1416
1417
1418
1419
1420
1421
1422
1423
1424
1425
1426
1427
1428
1429
1430
1431
1432
1433
1434
1435
1436
1437
1438
1439
1440
1441
1442
1443
1444
1445
1446
1447
1448
1449
1450
1451
1452
1453
1454
1455
1456
1457
1458
1459
1460
1461
1462
1463
1464
1465
1466
1467
1468
1469
1470
1471
1472
1473
1474
1475
1476
1477
1478
1479
1480
1481
1482
1483
1484
1485
1486
1487
1488
1489
1490
1491
1492
1493
1494
1495
1496
1497
1498
1499
1500
1501
1502
1503
1504
1505
1506
1507
1508
1509
1510
1511
1512
1513
1514
1515
1516
1517
1518
1519
1520
1521
1522
1523
1524
1525
1526
1527
1528
1529
1530
1531
1532
1533
1534
1535
1536
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.