ORAL CANCER IN GERMANY
VerifiedAdded on 2021/06/14
|70
|18968
|322
AI Summary
Oral cancer refers to the presence of tumor cells which can be noticed as early as the presence of lymph nodes or the presence of cancerous tissues in the throat (Blomberg et al. It may also lead to the presence of tumor cells which can be noticed as early as the presence of lymph nodes or the presence of cancerous tissues in the throat (Blomberg et al. DEFINITION AND CAUSES OF ORAL CANCER 57 Diagnosis 57 Stages of Mouth Cancer 57 Treatment 58 Radiation therapy
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
ORAL CANCER IN GERMANY
[Author Name(s), First M. Last, Omit Titles and Degrees]
[Institutional Affiliation(s)]
[Author Name(s), First M. Last, Omit Titles and Degrees]
[Institutional Affiliation(s)]
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Contents
ABSTRACT....................................................................................................................................................5
DEFINITION AND CAUSES............................................................................................................................5
TYPES OF ORAL CANCER..............................................................................................................................7
DENTAL BACKGROUND................................................................................................................................8
The Mouth...............................................................................................................................................8
Structure of the Mouth........................................................................................................................9
The function of the Mouth................................................................................................................10
Cancerous tumors of the Mouth...........................................................................................................11
Rare Mouth tumors...............................................................................................................................11
Precancerous Mouth Conditions...........................................................................................................11
Leukoplakia........................................................................................................................................11
Erythroplakia.....................................................................................................................................13
Non-cancerous tumors and mouth conditions..................................................................................14
MAIN DRIVERS CAUSING ORAL CANCER....................................................................................................16
Known Risk Factors................................................................................................................................17
Tobacco.............................................................................................................................................18
Betel quid and areca nut....................................................................................................................18
Human papillomavirus.......................................................................................................................20
Inherited conditions..........................................................................................................................20
Graft versus host disease...................................................................................................................21
Lichen planus.....................................................................................................................................21
Weakened immune system...............................................................................................................21
Family history regarding squamous cell carcinoma...........................................................................21
Exposure to sun.................................................................................................................................21
Previous cancer.................................................................................................................................22
Poor oral health.................................................................................................................................22
Unbalanced diet (low in fruits and vegetables).................................................................................22
LINK OF ORAL CANCER WITH ALCOHOL AND SMOKING............................................................................22
SIGNS AND SYMPTOMS OF ORAL CANCER................................................................................................25
ABSTRACT....................................................................................................................................................5
DEFINITION AND CAUSES............................................................................................................................5
TYPES OF ORAL CANCER..............................................................................................................................7
DENTAL BACKGROUND................................................................................................................................8
The Mouth...............................................................................................................................................8
Structure of the Mouth........................................................................................................................9
The function of the Mouth................................................................................................................10
Cancerous tumors of the Mouth...........................................................................................................11
Rare Mouth tumors...............................................................................................................................11
Precancerous Mouth Conditions...........................................................................................................11
Leukoplakia........................................................................................................................................11
Erythroplakia.....................................................................................................................................13
Non-cancerous tumors and mouth conditions..................................................................................14
MAIN DRIVERS CAUSING ORAL CANCER....................................................................................................16
Known Risk Factors................................................................................................................................17
Tobacco.............................................................................................................................................18
Betel quid and areca nut....................................................................................................................18
Human papillomavirus.......................................................................................................................20
Inherited conditions..........................................................................................................................20
Graft versus host disease...................................................................................................................21
Lichen planus.....................................................................................................................................21
Weakened immune system...............................................................................................................21
Family history regarding squamous cell carcinoma...........................................................................21
Exposure to sun.................................................................................................................................21
Previous cancer.................................................................................................................................22
Poor oral health.................................................................................................................................22
Unbalanced diet (low in fruits and vegetables).................................................................................22
LINK OF ORAL CANCER WITH ALCOHOL AND SMOKING............................................................................22
SIGNS AND SYMPTOMS OF ORAL CANCER................................................................................................25
Stages of Oral Cancer.............................................................................................................................27
Grading of Oral Cancer..........................................................................................................................29
Low-grade oral cancer...........................................................................................................................29
High-grade oral cancers.........................................................................................................................29
SCREENING METHODS FOR ORAL CANCER................................................................................................30
Visual oral cancer examination..............................................................................................................31
Oral cytology.........................................................................................................................................31
Direct visualization................................................................................................................................32
Aspiration..............................................................................................................................................32
Excisional Biopsy....................................................................................................................................32
Incisional Biopsy....................................................................................................................................33
EPIDEMIOLOGY..........................................................................................................................................33
Epidemiology of Oral Cancer in Germany..............................................................................................36
EPIDEMIOLOGY OF DRINKING AND SMOKING IN GERMANY.....................................................................41
EPIDEMIOLOGY OF SMOKING IN GERMANY..............................................................................................44
ECONOMIC BURDEN OF ORAL CANCER.....................................................................................................47
Estimates of the Cost of Illness..............................................................................................................47
LIMITATIONS.............................................................................................................................................51
TREATMENT OPTIONS FOR ORAL CAVITY AND OROPHARYNGEAL CANCER BY STAGE..............................52
Stage 0...................................................................................................................................................52
Stages I and II.........................................................................................................................................53
Stages III, IV, IVA....................................................................................................................................54
Stages IV B and IV C...............................................................................................................................55
DIAGNOSIS AND TREATMENT OF ORAL CANCER.......................................................................................57
Diagnosis...............................................................................................................................................57
Stages of Mouth Cancer........................................................................................................................57
Treatment..............................................................................................................................................58
Radiation therapy..............................................................................................................................58
Surgery..................................................................................................................................................58
Surgery for reconstructing the mouth...............................................................................................59
Surgery to eliminate tumor...............................................................................................................59
Surgery for the removal of cancer that has spread to the neck.........................................................59
Grading of Oral Cancer..........................................................................................................................29
Low-grade oral cancer...........................................................................................................................29
High-grade oral cancers.........................................................................................................................29
SCREENING METHODS FOR ORAL CANCER................................................................................................30
Visual oral cancer examination..............................................................................................................31
Oral cytology.........................................................................................................................................31
Direct visualization................................................................................................................................32
Aspiration..............................................................................................................................................32
Excisional Biopsy....................................................................................................................................32
Incisional Biopsy....................................................................................................................................33
EPIDEMIOLOGY..........................................................................................................................................33
Epidemiology of Oral Cancer in Germany..............................................................................................36
EPIDEMIOLOGY OF DRINKING AND SMOKING IN GERMANY.....................................................................41
EPIDEMIOLOGY OF SMOKING IN GERMANY..............................................................................................44
ECONOMIC BURDEN OF ORAL CANCER.....................................................................................................47
Estimates of the Cost of Illness..............................................................................................................47
LIMITATIONS.............................................................................................................................................51
TREATMENT OPTIONS FOR ORAL CAVITY AND OROPHARYNGEAL CANCER BY STAGE..............................52
Stage 0...................................................................................................................................................52
Stages I and II.........................................................................................................................................53
Stages III, IV, IVA....................................................................................................................................54
Stages IV B and IV C...............................................................................................................................55
DIAGNOSIS AND TREATMENT OF ORAL CANCER.......................................................................................57
Diagnosis...............................................................................................................................................57
Stages of Mouth Cancer........................................................................................................................57
Treatment..............................................................................................................................................58
Radiation therapy..............................................................................................................................58
Surgery..................................................................................................................................................58
Surgery for reconstructing the mouth...............................................................................................59
Surgery to eliminate tumor...............................................................................................................59
Surgery for the removal of cancer that has spread to the neck.........................................................59
Targeted drug therapy...........................................................................................................................60
Chemotherapy.......................................................................................................................................60
PREVENTION OF ORAL CANCER.................................................................................................................60
Quit tobacco smoking............................................................................................................................60
Quit consumption of alcohol.................................................................................................................61
Alternative medicine.............................................................................................................................61
CONCLUSION.............................................................................................................................................62
REFERENCES..............................................................................................................................................62
Chemotherapy.......................................................................................................................................60
PREVENTION OF ORAL CANCER.................................................................................................................60
Quit tobacco smoking............................................................................................................................60
Quit consumption of alcohol.................................................................................................................61
Alternative medicine.............................................................................................................................61
CONCLUSION.............................................................................................................................................62
REFERENCES..............................................................................................................................................62
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
ABSTRACT
The main causes of oral cancer are among them use of tobacco, heavy consumption of
alcohol and chewing areca nut all of which can be avoided and thus preventing the disease.
Preceded by precancerous conditions and lesions, early-stage oral cancers present themselves as
tiny painless growths or ulcers which can be noticed through careful and elaborate examination
and further effective treatment administered. Prevention, early detection alongside treatment is
among the most effective interventions that can be used in the reduction of the burden of oral
cancer in Germany and the world at large.
DEFINITION AND CAUSES
Cancer can generally be defined as the presence of uncontrollable growth which attacks
and results in damage or wearing out of the neighboring cells and tissues. Oral cancer (mouth
cancer) comes out as a sore or growth inside the mouth but that does not disappear (Alkureishi et
al. 2010). There are various types of oral cancer among them cancer of lips, sinuses, throat or
pharynx, tongue, cheeks, and cancer of the floor of the mouth may turn out to be one of the
devastating occurrences in the human life in case treatment and diagnosis is not done early
enough. Oral cancer is a head and neck type of cancer having the growth of its cancerous tissue
being located in the oral cavity.
It may be as a primary lesion that is coming from any of the tissues found in the mouth
through metastasis, that is, from a different site of origin. Cancer may also be through an
extension from an anatomic structure that is from the neighboring cells, for example, the nasal
cavity (Audeh et al. 2010). Still, oral cancers may be from any of the numerous issues that are
found in the mouth and could be of different histologic types among them teratoma and
The main causes of oral cancer are among them use of tobacco, heavy consumption of
alcohol and chewing areca nut all of which can be avoided and thus preventing the disease.
Preceded by precancerous conditions and lesions, early-stage oral cancers present themselves as
tiny painless growths or ulcers which can be noticed through careful and elaborate examination
and further effective treatment administered. Prevention, early detection alongside treatment is
among the most effective interventions that can be used in the reduction of the burden of oral
cancer in Germany and the world at large.
DEFINITION AND CAUSES
Cancer can generally be defined as the presence of uncontrollable growth which attacks
and results in damage or wearing out of the neighboring cells and tissues. Oral cancer (mouth
cancer) comes out as a sore or growth inside the mouth but that does not disappear (Alkureishi et
al. 2010). There are various types of oral cancer among them cancer of lips, sinuses, throat or
pharynx, tongue, cheeks, and cancer of the floor of the mouth may turn out to be one of the
devastating occurrences in the human life in case treatment and diagnosis is not done early
enough. Oral cancer is a head and neck type of cancer having the growth of its cancerous tissue
being located in the oral cavity.
It may be as a primary lesion that is coming from any of the tissues found in the mouth
through metastasis, that is, from a different site of origin. Cancer may also be through an
extension from an anatomic structure that is from the neighboring cells, for example, the nasal
cavity (Audeh et al. 2010). Still, oral cancers may be from any of the numerous issues that are
found in the mouth and could be of different histologic types among them teratoma and
adenocarcinoma which originate from a major or minor salivary gland. It may also be from
melanoma which is from the cells which produce pigment the oral mucosa or even from the
lymphoma which is from the tonsillar or the other tissues of the lymphoid system.
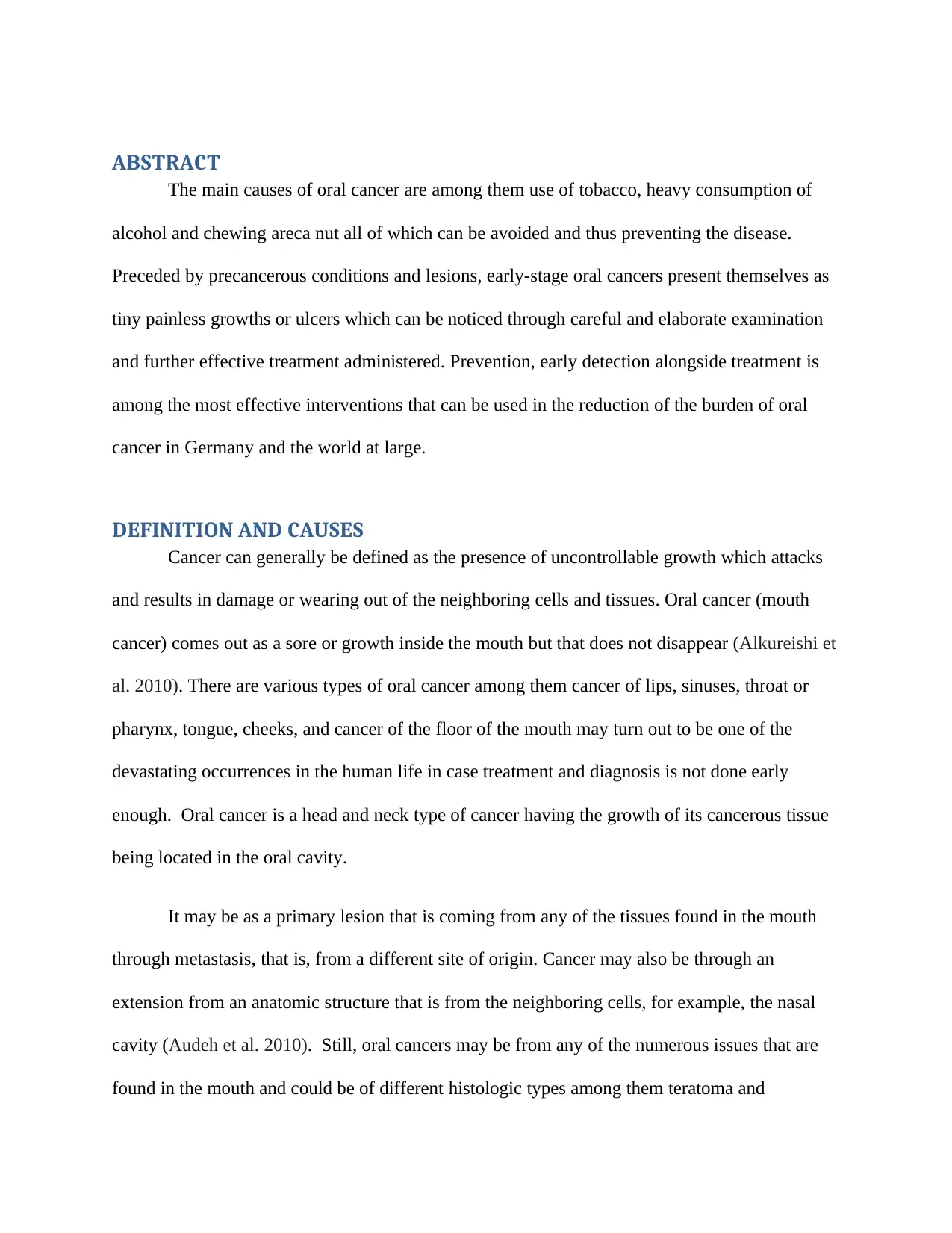
Figure 1: Oral Cancer can appear as a tumor or lesion anywhere in the mouth extracted from
medicalnewstoday.com
Oral cancer starts in the cells of the mouth. A malignant or cancerous tumor refers to a
collection of cancer cells that have the capability to grow into the surrounding tissues and lead to
their destruction. A tumor may also spread or metastasize to the other various body parts. In most
cases, oral cancer spread to the lymph nodes that are found in the neck (Blomberg et al. 2011).
The mouth cells at times change and do not undergo normal growth or behavior. Such changes
result in non-cancerous tumors among them fibromas and warts. Such changes in the cells of the
mouth may also lead to precancerous conditions which basically refer to abnormal cells that are
not yet declared as cancer even though they have chances of becoming cancer should treatment
and diagnosis not be carried out (Brailo et al. 2012). Erythroplakia and leukoplakia are the most
common precancerous conditions of the mouth that may with time turn to be cancerous.
melanoma which is from the cells which produce pigment the oral mucosa or even from the
lymphoma which is from the tonsillar or the other tissues of the lymphoid system.
Figure 1: Oral Cancer can appear as a tumor or lesion anywhere in the mouth extracted from
medicalnewstoday.com
Oral cancer starts in the cells of the mouth. A malignant or cancerous tumor refers to a
collection of cancer cells that have the capability to grow into the surrounding tissues and lead to
their destruction. A tumor may also spread or metastasize to the other various body parts. In most
cases, oral cancer spread to the lymph nodes that are found in the neck (Blomberg et al. 2011).
The mouth cells at times change and do not undergo normal growth or behavior. Such changes
result in non-cancerous tumors among them fibromas and warts. Such changes in the cells of the
mouth may also lead to precancerous conditions which basically refer to abnormal cells that are
not yet declared as cancer even though they have chances of becoming cancer should treatment
and diagnosis not be carried out (Brailo et al. 2012). Erythroplakia and leukoplakia are the most
common precancerous conditions of the mouth that may with time turn to be cancerous.
In other cases, the variations on the cells of the mouth may also result in oral cancer. A
lining called oral mucosa or the mucous membrane is a lining that covers the mouth. Oral
mucosa is composed of squamous cells known as squamous epithelium. In most cases, it is at
these flat and thin squamous cells that oral cancer begins. Such cancer types are called squamous
cell carcinomas of the mouth (Chaturvedi et al. 2011).
TYPES OF ORAL CANCER
There are numerous types of oral cancers of which 90% of them are squamous cell
carcinomas which come from the tissues that are lining the lips and the mouth. In most cases,
oral or mouth cancer involve the tongue even though it may also take place in the floor of the
mouth, the lining of the cheek, lips, gingiva or gums or in the palate (roof of the mouth). The
various oral cancer types are mostly similar in their appearance under the microscopes and are
known as squamous cell carcinomas however other types of cancer that are less common can
also occur among them Kaposi’s sarcoma (Cheema et al. 2012).
Oral cancer results when the cells on the human lips or inside one’s mouth undergo
changes or mutations into their DNA. Such mutations enable the cancer cells to continue
growing and undergo differentiation and division upon the death of mouth cells. The
accumulation of the unusual cells of mouth cancer may result in a tumor. As time goes, these
cells may spread across the mouth as well onto either different areas of the neck and head or the
other parts of the human body (Coelho 2012). Most of the mouth cancers often start in the flat
and thin cells also called the squamous cells which are lining the inside of the human mouth and
hence most of the oral cancers are squamous cell carcinomas.
lining called oral mucosa or the mucous membrane is a lining that covers the mouth. Oral
mucosa is composed of squamous cells known as squamous epithelium. In most cases, it is at
these flat and thin squamous cells that oral cancer begins. Such cancer types are called squamous
cell carcinomas of the mouth (Chaturvedi et al. 2011).
TYPES OF ORAL CANCER
There are numerous types of oral cancers of which 90% of them are squamous cell
carcinomas which come from the tissues that are lining the lips and the mouth. In most cases,
oral or mouth cancer involve the tongue even though it may also take place in the floor of the
mouth, the lining of the cheek, lips, gingiva or gums or in the palate (roof of the mouth). The
various oral cancer types are mostly similar in their appearance under the microscopes and are
known as squamous cell carcinomas however other types of cancer that are less common can
also occur among them Kaposi’s sarcoma (Cheema et al. 2012).
Oral cancer results when the cells on the human lips or inside one’s mouth undergo
changes or mutations into their DNA. Such mutations enable the cancer cells to continue
growing and undergo differentiation and division upon the death of mouth cells. The
accumulation of the unusual cells of mouth cancer may result in a tumor. As time goes, these
cells may spread across the mouth as well onto either different areas of the neck and head or the
other parts of the human body (Coelho 2012). Most of the mouth cancers often start in the flat
and thin cells also called the squamous cells which are lining the inside of the human mouth and
hence most of the oral cancers are squamous cell carcinomas.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
There has not been established a clarity on the cause of the mutation in the squamous
cells which then results in the cancer of the mouth even though doctors and other medical
practitioners have been able to establish the factors that are at stake of causing oral cancer. As of
2013, there were reported deaths to the tune of 135,000 resulting from cancer which is a
tremendous increase from 84,000 deaths that were reported in 1990.
DENTAL BACKGROUND
The Mouth
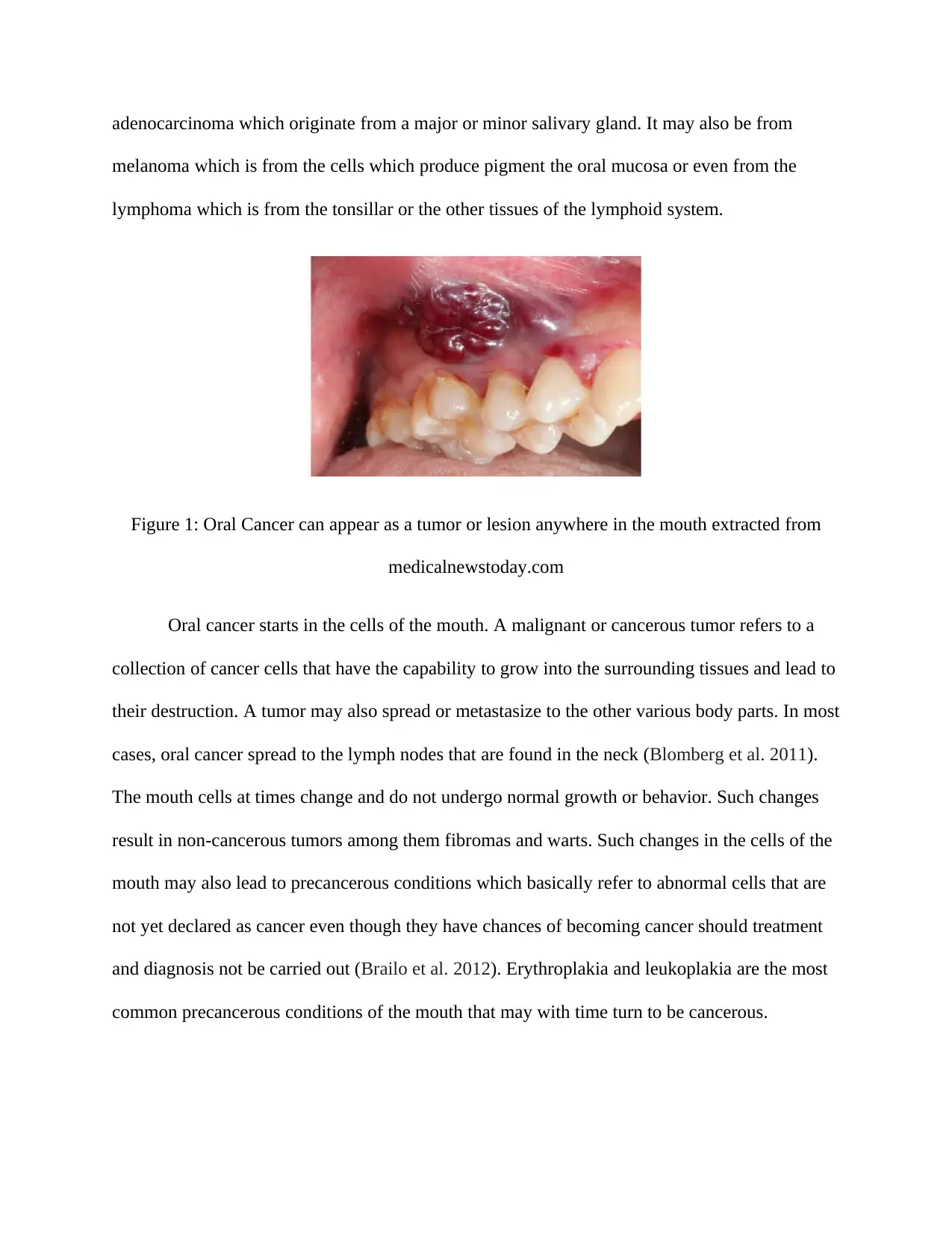
The mouth or the oral cavity is one of the most important parts of the digestive system
and is inclusive of the lips, cheeks, the floor of the mouth, the palate which is the roof of the
mouth, as well as part of the tongue, is found in the mouth also known as the oral tongue. The
structures found in the mouth are used in speaking, tasting and chewing.
Figure 2 (a): Head and Neck (Cheema et al. 2012)
cells which then results in the cancer of the mouth even though doctors and other medical
practitioners have been able to establish the factors that are at stake of causing oral cancer. As of
2013, there were reported deaths to the tune of 135,000 resulting from cancer which is a
tremendous increase from 84,000 deaths that were reported in 1990.
DENTAL BACKGROUND
The Mouth
The mouth or the oral cavity is one of the most important parts of the digestive system
and is inclusive of the lips, cheeks, the floor of the mouth, the palate which is the roof of the
mouth, as well as part of the tongue, is found in the mouth also known as the oral tongue. The
structures found in the mouth are used in speaking, tasting and chewing.
Figure 2 (a): Head and Neck (Cheema et al. 2012)
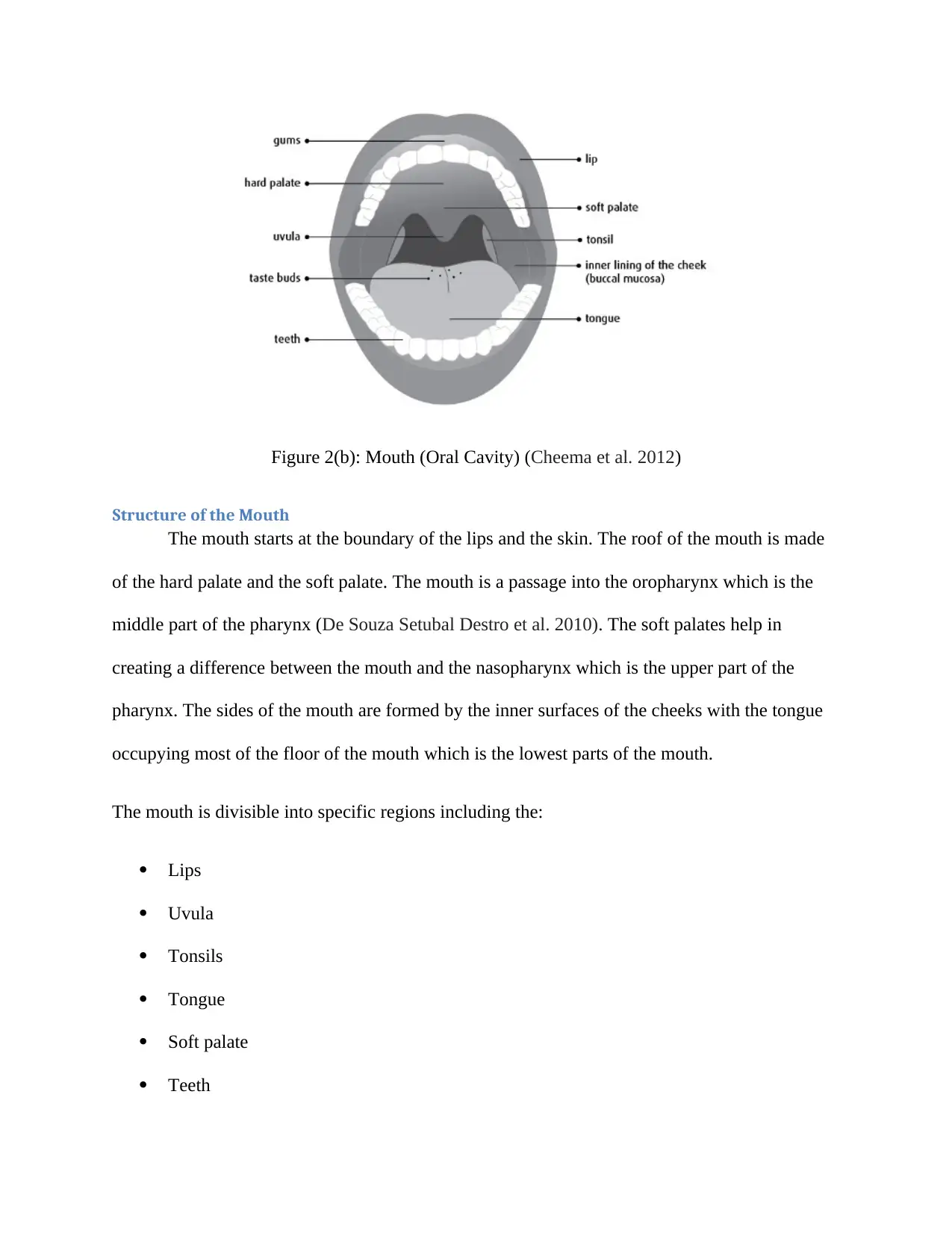
Figure 2(b): Mouth (Oral Cavity) (Cheema et al. 2012)
Structure of the Mouth
The mouth starts at the boundary of the lips and the skin. The roof of the mouth is made
of the hard palate and the soft palate. The mouth is a passage into the oropharynx which is the
middle part of the pharynx (De Souza Setubal Destro et al. 2010). The soft palates help in
creating a difference between the mouth and the nasopharynx which is the upper part of the
pharynx. The sides of the mouth are formed by the inner surfaces of the cheeks with the tongue
occupying most of the floor of the mouth which is the lowest parts of the mouth.
The mouth is divisible into specific regions including the:
Lips
Uvula
Tonsils
Tongue
Soft palate
Teeth
Structure of the Mouth
The mouth starts at the boundary of the lips and the skin. The roof of the mouth is made
of the hard palate and the soft palate. The mouth is a passage into the oropharynx which is the
middle part of the pharynx (De Souza Setubal Destro et al. 2010). The soft palates help in
creating a difference between the mouth and the nasopharynx which is the upper part of the
pharynx. The sides of the mouth are formed by the inner surfaces of the cheeks with the tongue
occupying most of the floor of the mouth which is the lowest parts of the mouth.
The mouth is divisible into specific regions including the:
Lips
Uvula
Tonsils
Tongue
Soft palate
Teeth
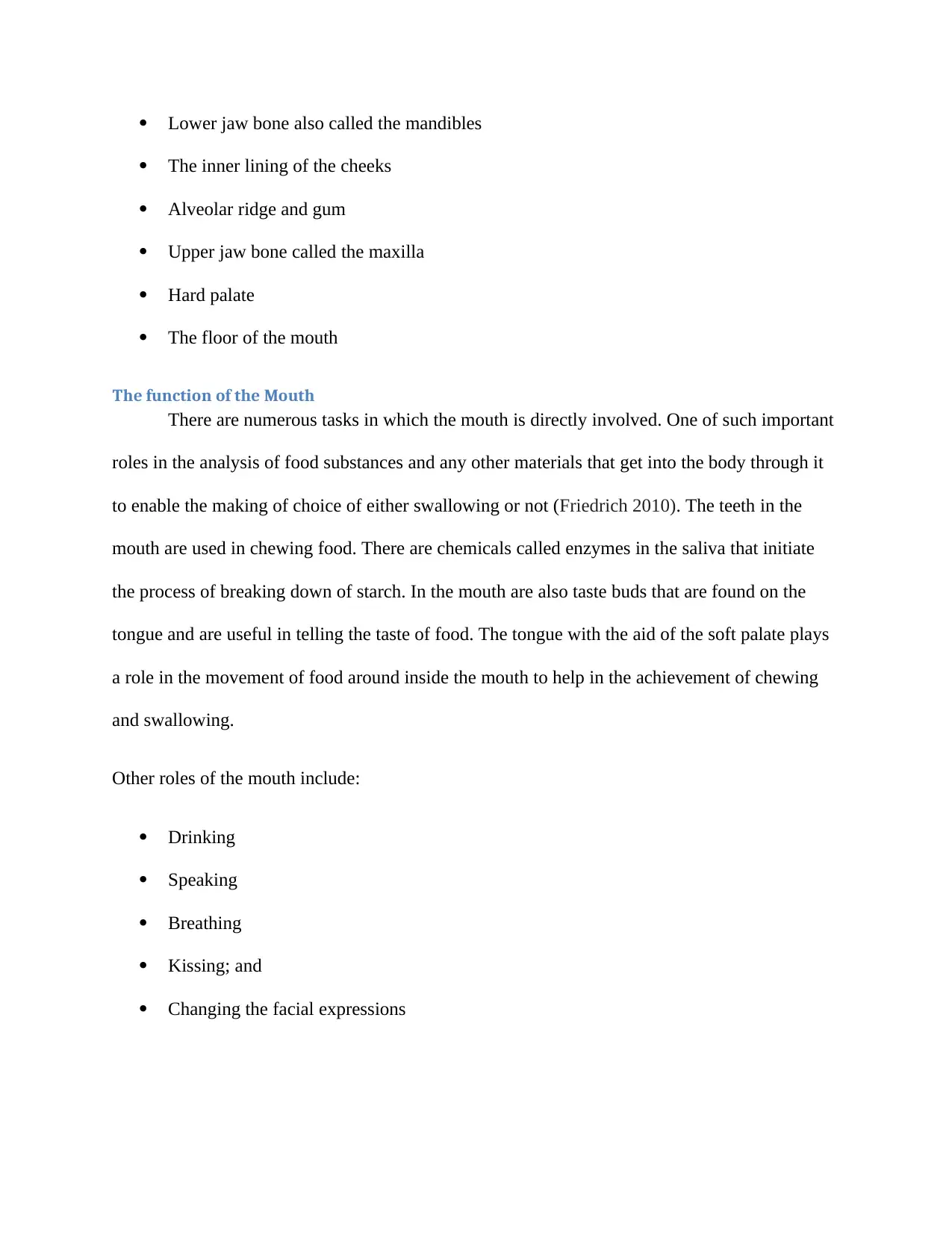
Lower jaw bone also called the mandibles
The inner lining of the cheeks
Alveolar ridge and gum
Upper jaw bone called the maxilla
Hard palate
The floor of the mouth
The function of the Mouth
There are numerous tasks in which the mouth is directly involved. One of such important
roles in the analysis of food substances and any other materials that get into the body through it
to enable the making of choice of either swallowing or not (Friedrich 2010). The teeth in the
mouth are used in chewing food. There are chemicals called enzymes in the saliva that initiate
the process of breaking down of starch. In the mouth are also taste buds that are found on the
tongue and are useful in telling the taste of food. The tongue with the aid of the soft palate plays
a role in the movement of food around inside the mouth to help in the achievement of chewing
and swallowing.
Other roles of the mouth include:
Drinking
Speaking
Breathing
Kissing; and
Changing the facial expressions
The inner lining of the cheeks
Alveolar ridge and gum
Upper jaw bone called the maxilla
Hard palate
The floor of the mouth
The function of the Mouth
There are numerous tasks in which the mouth is directly involved. One of such important
roles in the analysis of food substances and any other materials that get into the body through it
to enable the making of choice of either swallowing or not (Friedrich 2010). The teeth in the
mouth are used in chewing food. There are chemicals called enzymes in the saliva that initiate
the process of breaking down of starch. In the mouth are also taste buds that are found on the
tongue and are useful in telling the taste of food. The tongue with the aid of the soft palate plays
a role in the movement of food around inside the mouth to help in the achievement of chewing
and swallowing.
Other roles of the mouth include:
Drinking
Speaking
Breathing
Kissing; and
Changing the facial expressions
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

Cancerous tumors of the Mouth
A cancerous tumor of the mouth has the capability to grow and lead to the destruction of
the surrounding tissues. It also has the capability to spread to the other body part. The cancerous
tumors are also known as malignant tumors (Garavello et al. 2010).
Squamous cell carcinoma
This is the most common oral cancer type and it has been established to begin from the
flat and thin cells that are also called squamous cells which are an integral aspect of the oral
mucosa
Rare Mouth tumors
Some of the cancerous tumors of the mouth that seldom include:
Lymphoma
Melanoma
Cancer of the salivary glands
Bone and soft tissue sarcoma
Precancerous Mouth Conditions
Precancerous conditions of the mouth define the alterations that occur to the cells of the
mouth which make the cells more susceptible to the development of cancer. Such conditions are
not yet cancer, however, if they are left untreated, there is a potential that such abnormal
alterations may culminate into oral cancer (Gomes et al. 2012). Leukoplakia and erythroplakia
are the main and most common precancerous mouth conditions.
Leukoplakia
This refers to an unusual white or grey region which forms on the tongue, the floor of the
mouth, the gums or even inside of the cheek. Leukoplakia presence in the body is not a direct
A cancerous tumor of the mouth has the capability to grow and lead to the destruction of
the surrounding tissues. It also has the capability to spread to the other body part. The cancerous
tumors are also known as malignant tumors (Garavello et al. 2010).
Squamous cell carcinoma
This is the most common oral cancer type and it has been established to begin from the
flat and thin cells that are also called squamous cells which are an integral aspect of the oral
mucosa
Rare Mouth tumors
Some of the cancerous tumors of the mouth that seldom include:
Lymphoma
Melanoma
Cancer of the salivary glands
Bone and soft tissue sarcoma
Precancerous Mouth Conditions
Precancerous conditions of the mouth define the alterations that occur to the cells of the
mouth which make the cells more susceptible to the development of cancer. Such conditions are
not yet cancer, however, if they are left untreated, there is a potential that such abnormal
alterations may culminate into oral cancer (Gomes et al. 2012). Leukoplakia and erythroplakia
are the main and most common precancerous mouth conditions.
Leukoplakia
This refers to an unusual white or grey region which forms on the tongue, the floor of the
mouth, the gums or even inside of the cheek. Leukoplakia presence in the body is not a direct
indication of cancer. The risk of the development of oral cancer is influenced by the various
shapes, appearances, and sizes of the unusual cells in comparison to the normal cells of the
mouth. Such an abnormality is defined as dysplasia. A close look at people that have leukoplakia
or related symptoms is done by a team of healthcare professionals to establish the presence of
any signs of cancer (Guntinas-Lichius et al. 2010).
Risk factors for Leukoplakia
Among the factors that increase the chances of development of leukoplakia include:
Chewing tobacco
Heavy smoking
Excessive consumption of alcohol
Signs and Symptoms of leukoplakia
The signs and symptoms of leukoplakia are inclusive of a whitish region or spots that are
found inside the mouth which cannot easily be scrapped off (Hensel et al. 2011).
Diagnosis
The diagnosis of leukoplakia would involve the doctor interrogating the patient of any
symptoms experienced and perform a dental or oral examination. Still, a sample of the cells may
be taken from the abnormal region for a testing to be conducted in the laboratory.
Treatment
Research has not established any standard treatments for leukoplakia. The condition is
managed through active surveillance. In active surveillance, the team of healthcare professionals
closely monitors the condition of the patient (Hertrampf et al. 2012). Regular tests and
examinations are done on the patient to establish any changes that are indicative of cancer in the
early stages. Since leukoplakia has the potential of developing into cancer, it is of importance
shapes, appearances, and sizes of the unusual cells in comparison to the normal cells of the
mouth. Such an abnormality is defined as dysplasia. A close look at people that have leukoplakia
or related symptoms is done by a team of healthcare professionals to establish the presence of
any signs of cancer (Guntinas-Lichius et al. 2010).
Risk factors for Leukoplakia
Among the factors that increase the chances of development of leukoplakia include:
Chewing tobacco
Heavy smoking
Excessive consumption of alcohol
Signs and Symptoms of leukoplakia
The signs and symptoms of leukoplakia are inclusive of a whitish region or spots that are
found inside the mouth which cannot easily be scrapped off (Hensel et al. 2011).
Diagnosis
The diagnosis of leukoplakia would involve the doctor interrogating the patient of any
symptoms experienced and perform a dental or oral examination. Still, a sample of the cells may
be taken from the abnormal region for a testing to be conducted in the laboratory.
Treatment
Research has not established any standard treatments for leukoplakia. The condition is
managed through active surveillance. In active surveillance, the team of healthcare professionals
closely monitors the condition of the patient (Hertrampf et al. 2012). Regular tests and
examinations are done on the patient to establish any changes that are indicative of cancer in the
early stages. Since leukoplakia has the potential of developing into cancer, it is of importance
and medical practice that people suffering from such a condition keep off the famous risk factors
among the drinking of alcohol and tobacco smoking.
Erythroplakia
Erythroplakia refers to an unusual red region or a collection of red spots which develop
on the lining of the mucous membrane of the mouth and have no defined cause. Just like
leukoplakia, the presence of erythroplakia in the body is not a necessary indication of cancer in
as much it is a precancerous condition that has high risks and chances of developing into cancer.
Approximately half of these lesions change to squamous cell carcinoma (Hoffmann et al. 2010).
Risk factors for Erythroplakia
Among the factors that increase the chances of development of leukoplakia include:
Chewing tobacco
Heavy smoking
Excessive consumption of alcohol
Signs and Symptoms
The signs and symptoms of erythroplakia are inclusive of the raised region or a smooth
red region which in most cases bleeds upon scrapping.
Diagnosis
Research has not established any standard treatments for leukoplakia. The condition is
managed through active surveillance. In active surveillance, the team of healthcare professionals
closely monitors the condition of the patient. Regular tests and examinations are done on the
patient to establish any changes that are indicative of cancer in the early stages (Jalouli et al.
2011).
Treatment
Among the available treatment options for erythroplakia include:
among the drinking of alcohol and tobacco smoking.
Erythroplakia
Erythroplakia refers to an unusual red region or a collection of red spots which develop
on the lining of the mucous membrane of the mouth and have no defined cause. Just like
leukoplakia, the presence of erythroplakia in the body is not a necessary indication of cancer in
as much it is a precancerous condition that has high risks and chances of developing into cancer.
Approximately half of these lesions change to squamous cell carcinoma (Hoffmann et al. 2010).
Risk factors for Erythroplakia
Among the factors that increase the chances of development of leukoplakia include:
Chewing tobacco
Heavy smoking
Excessive consumption of alcohol
Signs and Symptoms
The signs and symptoms of erythroplakia are inclusive of the raised region or a smooth
red region which in most cases bleeds upon scrapping.
Diagnosis
Research has not established any standard treatments for leukoplakia. The condition is
managed through active surveillance. In active surveillance, the team of healthcare professionals
closely monitors the condition of the patient. Regular tests and examinations are done on the
patient to establish any changes that are indicative of cancer in the early stages (Jalouli et al.
2011).
Treatment
Among the available treatment options for erythroplakia include:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Laser surgery
Surgery
Careful watching which involves active surveillance accompanied by frequent follow-ups
Cryosurgery
Since erythroplakia has the potential of developing into cancer, it is of importance and
medical practice that people suffering from such a condition keep off the famous risk factors
among the drinking of alcohol and tobacco smoking (Jemal et al. 2011).
Non-cancerous tumors and mouth conditions
A non-cancerous tumor is defined as a tumor of the mouth has does not have the
capability to spread to the other various parts of the body. It is an alteration in the cells of the
mouth but not cancer. In most cases, non-cancerous tumors do not pose a threat to life. There are
various and numerous kinds of non-cancerous tumors and conditions that affect the mouth
among them:
Warts: This is a small oval or round growth and may occur either in the lips or in the
mouth. They are normally caused by various types of human papillomavirus. It also has the
capability of spreading to the mouth from the hands. Genital warts can be spread through oral
sex to the mouth. Warts may disappear on their own or may be treated with the use of some
special medicine which is administered by direct application to the surgery or wart (Jung et al.
2011).
Cold sores: It is also called herpes labialis and defines an oral infection that is caused by
the herpes simplex virus. It results in a swelling in the shape of a bubble or a cyst and sores
which mainly form on the mucous membrane as well as on the skin that is surrounding the
Surgery
Careful watching which involves active surveillance accompanied by frequent follow-ups
Cryosurgery
Since erythroplakia has the potential of developing into cancer, it is of importance and
medical practice that people suffering from such a condition keep off the famous risk factors
among the drinking of alcohol and tobacco smoking (Jemal et al. 2011).
Non-cancerous tumors and mouth conditions
A non-cancerous tumor is defined as a tumor of the mouth has does not have the
capability to spread to the other various parts of the body. It is an alteration in the cells of the
mouth but not cancer. In most cases, non-cancerous tumors do not pose a threat to life. There are
various and numerous kinds of non-cancerous tumors and conditions that affect the mouth
among them:
Warts: This is a small oval or round growth and may occur either in the lips or in the
mouth. They are normally caused by various types of human papillomavirus. It also has the
capability of spreading to the mouth from the hands. Genital warts can be spread through oral
sex to the mouth. Warts may disappear on their own or may be treated with the use of some
special medicine which is administered by direct application to the surgery or wart (Jung et al.
2011).
Cold sores: It is also called herpes labialis and defines an oral infection that is caused by
the herpes simplex virus. It results in a swelling in the shape of a bubble or a cyst and sores
which mainly form on the mucous membrane as well as on the skin that is surrounding the
mouth. Cold sores in most cases take up to one week to heal even though they may recur. The
infection may be treated with the aid of antiviral medications.
Canker sores: A cancer sore refers to a sore that is covered with a membrane that is
yellowish white in color having a red ring around it (Kadam et al. 2011). The cause of the
condition is undefined. The condition in most cases recurs even though it quickly heals which
usually takes about 1 to 2 weeks. Creams or corticosteroids are used in the treatment of canker
scores through direct application.
Thrush: An overgrowth of the candida type of fungus may result into an infection
referred to as thrush. Candida is a fungus type often found in the mouth. The condition is formed
mostly in people with weak immune systems and is for a long time on antibiotics or steroids. The
use of antifungal drugs is used in the treatment of the condition.
Frictional hyperkeratosis: This refers to a thickening of the lining of the inner mouth,
whitish in color, and maybe as a result of continuous rubbing. It is usually observed on the
surface of the inside of the cheek, gums, lips or tongue (Kim et al. 2012). Elimination of the
cause of the friction is used as a cure for the condition for example denture or by ensuring that
are rough teeth are smoothened.
Mucocele: These are tender swellings that resemble bubbles or cysts and often form in
the gums or in the roof of the mouth, beneath the tongue or even inside the lower lip. They, in
most cases, result from accidental biting of the lower lip those results into the damage of the
salivary glands hence bringing about a build-up in the saliva (Kiyohara & Ohno 2010). They in
most cases disappear without any treatment being administered even though they may as well be
eliminated through surgery.
infection may be treated with the aid of antiviral medications.
Canker sores: A cancer sore refers to a sore that is covered with a membrane that is
yellowish white in color having a red ring around it (Kadam et al. 2011). The cause of the
condition is undefined. The condition in most cases recurs even though it quickly heals which
usually takes about 1 to 2 weeks. Creams or corticosteroids are used in the treatment of canker
scores through direct application.
Thrush: An overgrowth of the candida type of fungus may result into an infection
referred to as thrush. Candida is a fungus type often found in the mouth. The condition is formed
mostly in people with weak immune systems and is for a long time on antibiotics or steroids. The
use of antifungal drugs is used in the treatment of the condition.
Frictional hyperkeratosis: This refers to a thickening of the lining of the inner mouth,
whitish in color, and maybe as a result of continuous rubbing. It is usually observed on the
surface of the inside of the cheek, gums, lips or tongue (Kim et al. 2012). Elimination of the
cause of the friction is used as a cure for the condition for example denture or by ensuring that
are rough teeth are smoothened.
Mucocele: These are tender swellings that resemble bubbles or cysts and often form in
the gums or in the roof of the mouth, beneath the tongue or even inside the lower lip. They, in
most cases, result from accidental biting of the lower lip those results into the damage of the
salivary glands hence bringing about a build-up in the saliva (Kiyohara & Ohno 2010). They in
most cases disappear without any treatment being administered even though they may as well be
eliminated through surgery.
Lichen planus: This is an inflammatory condition which can have impacts on the mouth,
skin, gums, and tongue. A few numbers of oral cancers have an association with oral lichen
planus. Treatment of oral lichen planus is achieved through enhanced hygiene and local steroids.
Fibroma: This is around, tender and firm lump that forms inside the mouth. They are
mostly found in the inner linings of the cheeks and the lips and are eliminated through surgical
procedures (Klosa et al. 2011).
Torus: This refers to a growth, bony in nature, which is able to develop in the roof of the
mouth or even in the lower jaw by the side of the tongue. In most cases, they do not require any
specialized treatment but may also be an issue in circumstances where they interfere with eating
or in the wearing of dentures.
MAIN DRIVERS CAUSING ORAL CANCER
A risk factor defines a condition or substance that enhances the chances or risks of
development of cancer. Most of the cancers result from numerous risks in which tobacco and
alcohol tend to be the leading and most important risk factors when it comes to oral cancer.
While oral cancer is rare in both children and adults, the risk of its development has been
established to increase with an increase in the age and has been found to be highest after one
attains 45 years of age. The prevalence of oral cancer is higher in women than in men and most
prevalent in men of African origin (Koh et al. 2011).
The precancerous conditions of the mouth are among the erythroplakia and leukoplakia.
These conditions are not normally cancer but have the potential to change to oral cancer should
they not be treated. Some of the risk factors for oral cancer may also have an influence on the
development of the precancerous conditions. Below is a list of the risk factors from the most
skin, gums, and tongue. A few numbers of oral cancers have an association with oral lichen
planus. Treatment of oral lichen planus is achieved through enhanced hygiene and local steroids.
Fibroma: This is around, tender and firm lump that forms inside the mouth. They are
mostly found in the inner linings of the cheeks and the lips and are eliminated through surgical
procedures (Klosa et al. 2011).
Torus: This refers to a growth, bony in nature, which is able to develop in the roof of the
mouth or even in the lower jaw by the side of the tongue. In most cases, they do not require any
specialized treatment but may also be an issue in circumstances where they interfere with eating
or in the wearing of dentures.
MAIN DRIVERS CAUSING ORAL CANCER
A risk factor defines a condition or substance that enhances the chances or risks of
development of cancer. Most of the cancers result from numerous risks in which tobacco and
alcohol tend to be the leading and most important risk factors when it comes to oral cancer.
While oral cancer is rare in both children and adults, the risk of its development has been
established to increase with an increase in the age and has been found to be highest after one
attains 45 years of age. The prevalence of oral cancer is higher in women than in men and most
prevalent in men of African origin (Koh et al. 2011).
The precancerous conditions of the mouth are among the erythroplakia and leukoplakia.
These conditions are not normally cancer but have the potential to change to oral cancer should
they not be treated. Some of the risk factors for oral cancer may also have an influence on the
development of the precancerous conditions. Below is a list of the risk factors from the most
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
important to the least important even though in real practice, arranging the factors in such an
order of rank is quite impossible as there is no such certainty.
Known Risk Factors
Tobacco
Alcohol
Betel quid and areca nut
Human papillomavirus
Previous attacks
Family history with regard to squamous cell carcinoma
Exposure to sun
Unbalanced diet (low in fruits and vegetables)
The weakened immune system of the body
Grat versus just disease
Lichen planus
Poor oral health and hygiene
Inherited conditions
There are also possible risk factors whose impact have not been fully exploited but are
believed to have an influence or other a potential to cause oral cancer (Lee et al. 2010). Such
include:
Consumption of very hot beverages
Poor fitting dentures
Known risk factors
order of rank is quite impossible as there is no such certainty.
Known Risk Factors
Tobacco
Alcohol
Betel quid and areca nut
Human papillomavirus
Previous attacks
Family history with regard to squamous cell carcinoma
Exposure to sun
Unbalanced diet (low in fruits and vegetables)
The weakened immune system of the body
Grat versus just disease
Lichen planus
Poor oral health and hygiene
Inherited conditions
There are also possible risk factors whose impact have not been fully exploited but are
believed to have an influence or other a potential to cause oral cancer (Lee et al. 2010). Such
include:
Consumption of very hot beverages
Poor fitting dentures
Known risk factors
Research and study have developed convinced and elaborate evidence and information
that the factors discussed below have the potential to increase the risk of oral cancer:
Tobacco: A great percentage of the oral cancers have been linked to the use of tobacco.
Tobacco exits in various forms and types among the smokeless tobacco, pipes, cigarettes, cigars
and even bidis. All of the forms inclusive of the chewing tobacco and snuff have been found to
increase the risk of mouth cancer. The longer an individual uses tobacco, the more quantity is
absorbed into the body and thus the greater the risks of the disease (Linsen, Martini & Stark
2012). This risk is even increased further in cases where smoking is combined with smokeless
tobacco, drinking alcohol or even both. There are chances of development of a second oral
cancer after treatment of the first one in cases where an individual decides to continue smoking.
Smoking of pipes, cigars, and cigarettes also have a role in increasing the risk of oral
cancer. Such substances have been established to have a correlation with the cancer of the lips
when they sit on the lips. On the other hand, the use of smokeless tobacco has an association
with the cancer of the gums as well as that of the inner lining of the cheeks and lips. This alludes
to the fact that the smokeless tobacco quite often touches such areas. Studies have also
established that second-hand smoke has the potential of increase sing the risk of development of
oral cancer (Liu et al. 2012).
Betel quid and areca nut: The chewing of betel quid or areca nut is very common in
South Asia besides among some immigrants of South Asia who live in Canada. Bet quid, also
known as paan is areca nut which is a seed derived from the oriental palm fruit and limes that has
been wrapped in a betel leaf. While some people opt to chew the areca nut by itself, other take
that the factors discussed below have the potential to increase the risk of oral cancer:
Tobacco: A great percentage of the oral cancers have been linked to the use of tobacco.
Tobacco exits in various forms and types among the smokeless tobacco, pipes, cigarettes, cigars
and even bidis. All of the forms inclusive of the chewing tobacco and snuff have been found to
increase the risk of mouth cancer. The longer an individual uses tobacco, the more quantity is
absorbed into the body and thus the greater the risks of the disease (Linsen, Martini & Stark
2012). This risk is even increased further in cases where smoking is combined with smokeless
tobacco, drinking alcohol or even both. There are chances of development of a second oral
cancer after treatment of the first one in cases where an individual decides to continue smoking.
Smoking of pipes, cigars, and cigarettes also have a role in increasing the risk of oral
cancer. Such substances have been established to have a correlation with the cancer of the lips
when they sit on the lips. On the other hand, the use of smokeless tobacco has an association
with the cancer of the gums as well as that of the inner lining of the cheeks and lips. This alludes
to the fact that the smokeless tobacco quite often touches such areas. Studies have also
established that second-hand smoke has the potential of increase sing the risk of development of
oral cancer (Liu et al. 2012).
Betel quid and areca nut: The chewing of betel quid or areca nut is very common in
South Asia besides among some immigrants of South Asia who live in Canada. Bet quid, also
known as paan is areca nut which is a seed derived from the oriental palm fruit and limes that has
been wrapped in a betel leaf. While some people opt to chew the areca nut by itself, other take
betel quid alongside tobacco or in other cases the betel quid may be having tobacco as part of its
constituents.
Figure 3(a): Betel plant Figure 3(b): Paan
Figure 3(c): Areca Plant and Nut
The two substances, betel quid, and areca nut contain substances that cause cancer and
hence the reason for the higher risks of development of oral cancer among people who chew
areca nut or betel quid. This is even higher in the inner linings of the lips and cheeks (Malhotra et
al. 2010).
constituents.
Figure 3(a): Betel plant Figure 3(b): Paan
Figure 3(c): Areca Plant and Nut
The two substances, betel quid, and areca nut contain substances that cause cancer and
hence the reason for the higher risks of development of oral cancer among people who chew
areca nut or betel quid. This is even higher in the inner linings of the lips and cheeks (Malhotra et
al. 2010).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Alcohol: Alcohol tends to be one of the leading risk factors for cancer. A higher
consumption of alcohol increases such risks which are even inflated further when alcohol is used
alongside tobacco.
Human papillomavirus: Human papillomavirus refers to a collection of more than 100
various types of related viruses. Most of these groups of viruses are spread through sexual
contact which includes oral sex. There may infect the sexual organs i.e. the vagina, vulva, and
cervix in the females and the penis in men (Marsh et al. 2011). They may also infect the anus and
the rectum. Human papillomavirus also has the potential of infecting the mouth and the throat.
The various types of human papillomavirus are normally assigned a number that is used
in their identification. Human papillomavirus, the HPV-16 infection has been associated with the
risk of oral cancer while an infection by HPV-18 also has chances of increased risks. Human
papillomavirus may cause cancer that is not linked with the use of alcohol or tobacco.
Inherited conditions: A genetic or inherited condition is transferred from the parent to
the children through the genes. People having the inherited conditions discussed below have
higher chances of developing precancerous alterations in the mouth and oral cancer. These
conditions may develop at much earlier ages that oral cancer that results from the other risk
factors (Rana et al. 2012).
Dyskeratosis congenital which is a genetic syndrome that has the potential to cause
abnormalities of the red blood cells, toenails, skin rashes and even abnormal fingernails
(Trellakis et al. 2011)
Fanconi anemia is quite a rare genetic condition and mainly affects the bone marrow in
such a way that in inhibits making of enough red blood cells, platelets, and white blood cells.
consumption of alcohol increases such risks which are even inflated further when alcohol is used
alongside tobacco.
Human papillomavirus: Human papillomavirus refers to a collection of more than 100
various types of related viruses. Most of these groups of viruses are spread through sexual
contact which includes oral sex. There may infect the sexual organs i.e. the vagina, vulva, and
cervix in the females and the penis in men (Marsh et al. 2011). They may also infect the anus and
the rectum. Human papillomavirus also has the potential of infecting the mouth and the throat.
The various types of human papillomavirus are normally assigned a number that is used
in their identification. Human papillomavirus, the HPV-16 infection has been associated with the
risk of oral cancer while an infection by HPV-18 also has chances of increased risks. Human
papillomavirus may cause cancer that is not linked with the use of alcohol or tobacco.
Inherited conditions: A genetic or inherited condition is transferred from the parent to
the children through the genes. People having the inherited conditions discussed below have
higher chances of developing precancerous alterations in the mouth and oral cancer. These
conditions may develop at much earlier ages that oral cancer that results from the other risk
factors (Rana et al. 2012).
Dyskeratosis congenital which is a genetic syndrome that has the potential to cause
abnormalities of the red blood cells, toenails, skin rashes and even abnormal fingernails
(Trellakis et al. 2011)
Fanconi anemia is quite a rare genetic condition and mainly affects the bone marrow in
such a way that in inhibits making of enough red blood cells, platelets, and white blood cells.
Graft versus host disease: The chances of development of Graft versus host disease
increase among individuals who have had a stem cell transplant. Graft versus host disease refers
to a condition in which the transplanted stem cells perceived the body as a foreign organism and
hence begin to destroy the cells of the body among them the cells that are found in the mouth.
The damage to such cells of the mouth by Graft versus host disease enhances the chances of
developments of oral cancer (Sobral et al. 2014).
Lichen planus: This refers to a chronic condition that generates sores or rashes on the
skin as well as to the inside of the mouth in most cases on the gums, tongue, and linings of the
cheek. At times, such sores may develop into ulcers. The chances of oral cancer are increased by
having ulcers and lichen planus in the mouth for a long time.
Weakened immune system: The immune system may be weakened after a treatment of
a disease of the immune system or after an organ transplant. The risk and chances of developing
oral cancer are higher among people with a weakened immune system, especially lip cancer.
Such a high risk may be attributed to the use of drugs in suppressing the immune system. Still,
people suffering from the weakened immune system also have higher chances of being infected
by the human papillomavirus that in turn increases the risk of oral cancer.
Family history regarding squamous cell carcinoma: Squamous cell carcinoma is one of
the most common types of oral cancer and has a higher risk of development in the neck and head
region inclusive of the mouth in cases where a first degree member of a family i.e. sibling, child
or parent has been diagnosed with the condition of the neck and head (Sugimoto et al. 2010).
Exposure to sun: An exposure to the sun increases the risk of development of lip cancer.
This is mostly applicable to people who work for very long periods of time in the sun including
increase among individuals who have had a stem cell transplant. Graft versus host disease refers
to a condition in which the transplanted stem cells perceived the body as a foreign organism and
hence begin to destroy the cells of the body among them the cells that are found in the mouth.
The damage to such cells of the mouth by Graft versus host disease enhances the chances of
developments of oral cancer (Sobral et al. 2014).
Lichen planus: This refers to a chronic condition that generates sores or rashes on the
skin as well as to the inside of the mouth in most cases on the gums, tongue, and linings of the
cheek. At times, such sores may develop into ulcers. The chances of oral cancer are increased by
having ulcers and lichen planus in the mouth for a long time.
Weakened immune system: The immune system may be weakened after a treatment of
a disease of the immune system or after an organ transplant. The risk and chances of developing
oral cancer are higher among people with a weakened immune system, especially lip cancer.
Such a high risk may be attributed to the use of drugs in suppressing the immune system. Still,
people suffering from the weakened immune system also have higher chances of being infected
by the human papillomavirus that in turn increases the risk of oral cancer.
Family history regarding squamous cell carcinoma: Squamous cell carcinoma is one of
the most common types of oral cancer and has a higher risk of development in the neck and head
region inclusive of the mouth in cases where a first degree member of a family i.e. sibling, child
or parent has been diagnosed with the condition of the neck and head (Sugimoto et al. 2010).
Exposure to sun: An exposure to the sun increases the risk of development of lip cancer.
This is mostly applicable to people who work for very long periods of time in the sun including
farmers. People with fair skins also have a greater risk of developing cancer of the lip (Trellakis
et al. 2011). More often, the lip cancer takes place on the bottom of the lip due to the fact that is
more subjected to the sun.
Previous cancer: People who have had, in the past, oral cancer have greater risks of
developing yet another oral cancer which is even enhanced in cases where such people are
continually used alcohol or tobacco. Suffering from cancer of the esophagus, lung, larynx or
cervix enhances the risk of oral cancer.
Poor oral health: Poor oral health in an individual may lead to the missing of several
teeth, chronic infections and even bleeding gums all of which result from viruses bacteria and
viruses among them human papillomavirus (Supic et al. 2012).
Unbalanced diet (low in fruits and vegetables): Research and several studies have
established that failure to incorporate enough vitamins i.e. fruits and vegetables in diet enhances
the risk of development of oral cancer. Such studies and findings in return further recommend
the use of substances like carotenoids that are mostly found in vegetables and fruits in lowering
the risk of infection by oral cancer.
LINK OF ORAL CANCER WITH ALCOHOL AND SMOKING
The use of tobacco has been proven beyond doubts to have an increase in the risk of oral
cancer. It has further been established that those who consume alcohol and at the same time
smoke tobacco stand at an even higher risk of contracting oral cancer (Trellakis et al. 2011).
Scientist and scholars have a strong belief that there is a synergetic interaction between these two
substances with each of the increasing the harmful effects of the other. Abuse of alcohol which
et al. 2011). More often, the lip cancer takes place on the bottom of the lip due to the fact that is
more subjected to the sun.
Previous cancer: People who have had, in the past, oral cancer have greater risks of
developing yet another oral cancer which is even enhanced in cases where such people are
continually used alcohol or tobacco. Suffering from cancer of the esophagus, lung, larynx or
cervix enhances the risk of oral cancer.
Poor oral health: Poor oral health in an individual may lead to the missing of several
teeth, chronic infections and even bleeding gums all of which result from viruses bacteria and
viruses among them human papillomavirus (Supic et al. 2012).
Unbalanced diet (low in fruits and vegetables): Research and several studies have
established that failure to incorporate enough vitamins i.e. fruits and vegetables in diet enhances
the risk of development of oral cancer. Such studies and findings in return further recommend
the use of substances like carotenoids that are mostly found in vegetables and fruits in lowering
the risk of infection by oral cancer.
LINK OF ORAL CANCER WITH ALCOHOL AND SMOKING
The use of tobacco has been proven beyond doubts to have an increase in the risk of oral
cancer. It has further been established that those who consume alcohol and at the same time
smoke tobacco stand at an even higher risk of contracting oral cancer (Trellakis et al. 2011).
Scientist and scholars have a strong belief that there is a synergetic interaction between these two
substances with each of the increasing the harmful effects of the other. Abuse of alcohol which
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
is loosely defined as the consumption of more than 21 standard units in a week has been
classified as the second greatest risk factor in the development of oral cancer.
A study that was conducted more than three decades ago in Utah that majored in the
heavy consumption of alcohol as a key factor in the development of cancer established than a
state that has its population at about two thirds Mormon, there were relatively less chances of
oral cancer as compared to the other western states (Trellakis et al. 2011). The study established
that the rate was much less than the nation as a whole. This would attribute partly to the religious
beliefs of Mormon which expected and demanded that they abstain from both alcohol and
tobacco completely.
The effects of alcohol on the mouth may be treated to the main understanding of how the
substances work alongside tobacco in enhancing the risk of the development of oral cancer.
Alcohol dehydrates the cell walls which in turn increases the ability of carcinogens of tobacco to
permeate the tissues of the mouth. In addition, the nutrition deficiencies that are related with a
heavy intake of alcohol have the capability to reduce the natural ability of the human n body to
make use of antioxidants in the prevention of the formation of cancer (Tutt et al. 2010).
There has been established statistical evidence that is in support of such claims. Other
studies have even further hinted that cirrhosis of the liver which results from heavy intake of
alcohol could have a close association with increased risks of oral cancer. Liver cirrhosis patients
in most cases develop an appearance which is smooth and glossy to the oral mucosae which are
the tissue of the mouth and throat. This may be caused by cellular changes that are caused by the
liver including an increase in the content of cytoplasmic acetaldehyde. The real mechanism that
classified as the second greatest risk factor in the development of oral cancer.
A study that was conducted more than three decades ago in Utah that majored in the
heavy consumption of alcohol as a key factor in the development of cancer established than a
state that has its population at about two thirds Mormon, there were relatively less chances of
oral cancer as compared to the other western states (Trellakis et al. 2011). The study established
that the rate was much less than the nation as a whole. This would attribute partly to the religious
beliefs of Mormon which expected and demanded that they abstain from both alcohol and
tobacco completely.
The effects of alcohol on the mouth may be treated to the main understanding of how the
substances work alongside tobacco in enhancing the risk of the development of oral cancer.
Alcohol dehydrates the cell walls which in turn increases the ability of carcinogens of tobacco to
permeate the tissues of the mouth. In addition, the nutrition deficiencies that are related with a
heavy intake of alcohol have the capability to reduce the natural ability of the human n body to
make use of antioxidants in the prevention of the formation of cancer (Tutt et al. 2010).
There has been established statistical evidence that is in support of such claims. Other
studies have even further hinted that cirrhosis of the liver which results from heavy intake of
alcohol could have a close association with increased risks of oral cancer. Liver cirrhosis patients
in most cases develop an appearance which is smooth and glossy to the oral mucosae which are
the tissue of the mouth and throat. This may be caused by cellular changes that are caused by the
liver including an increase in the content of cytoplasmic acetaldehyde. The real mechanism that
leads to this occurrence and the correlation with the development of oral cancer is not yet
thoroughly exhausted and calls for the need for further examination (Tutt et al. 2010).
It is quite of a challenge in studying tobacco and alcohol as risk factors for oral cancer
patients as the victims are found to have used both products. Despite such challenges, it is widely
accepted that the removal of oral tobacco and minimization or other complete elimination of the
intake of alcohol would have an immediate impact in the reduction of the risk of development of
oral cancer. Regular drinking of alcohol makes the mouth and the throat to keep a close contact
with alcohol which turns out to be a risk factor for all the various types of oral cancer (Zhang et
al. 2011). A study conducted in 2010 established that when an individual stops drinking, there is
up to 2% reduction every year in alcohol-related risks of contracting oral cancer. For this reason,
one of the reasons for the consumption of alcohol within the provided low-risk drinking
guidelines is to reduce the risk of contracting oral cancer. The guideline provides that an
individual should not consume more than 14 standard units of the substance.
With reference to smoking and the risk of oral cancer, some of the chemicals that are
found in tobacco smoke are able to cause, ignite or even promote the development of oral cancer.
These chemicals work in such a way that they initiate genetic changes in the cells that are found
in the mouth cavity which in turn lead to the development of oral cancer (Worthington et al.
2010). The use of tobacco as well enhances the risk of oral cancer by subjecting the mouth to
such carcinogenic chemicals either by inhalation during smoking or even via direct contact when
one is chewing the products of tobacco.
Among the chemical contained in tobacco include chemical which causes cancer,
benzene as well as fine particles. Tobacco smoke is composed of more than 4000 chemicals
thoroughly exhausted and calls for the need for further examination (Tutt et al. 2010).
It is quite of a challenge in studying tobacco and alcohol as risk factors for oral cancer
patients as the victims are found to have used both products. Despite such challenges, it is widely
accepted that the removal of oral tobacco and minimization or other complete elimination of the
intake of alcohol would have an immediate impact in the reduction of the risk of development of
oral cancer. Regular drinking of alcohol makes the mouth and the throat to keep a close contact
with alcohol which turns out to be a risk factor for all the various types of oral cancer (Zhang et
al. 2011). A study conducted in 2010 established that when an individual stops drinking, there is
up to 2% reduction every year in alcohol-related risks of contracting oral cancer. For this reason,
one of the reasons for the consumption of alcohol within the provided low-risk drinking
guidelines is to reduce the risk of contracting oral cancer. The guideline provides that an
individual should not consume more than 14 standard units of the substance.
With reference to smoking and the risk of oral cancer, some of the chemicals that are
found in tobacco smoke are able to cause, ignite or even promote the development of oral cancer.
These chemicals work in such a way that they initiate genetic changes in the cells that are found
in the mouth cavity which in turn lead to the development of oral cancer (Worthington et al.
2010). The use of tobacco as well enhances the risk of oral cancer by subjecting the mouth to
such carcinogenic chemicals either by inhalation during smoking or even via direct contact when
one is chewing the products of tobacco.
Among the chemical contained in tobacco include chemical which causes cancer,
benzene as well as fine particles. Tobacco smoke is composed of more than 4000 chemicals
among which are about 70 known carcinogens (Zhang et al. 2011). Carcinogens are chemicals
which have the ability to cause, initiate or even enhance cancer. Most of these chemicals are
found in second-hand smoke and a recurrent expose to such carcinogens have the potential to
increase the chances of developing cancer.
Benzene, on the other hand, is one of the most abundant chemicals that are found in
tobacco smoke. Benzene has been classified as a carcinogenic substance that is harmful to
humans. Tobacco smoke forms a major source of pollution of the indoor air in the place of
residence of the smoker. The smoke is composed of a mixture of chemicals that are in the form
of particles and gases (Zhang et al. 2011). The particles are very tiny and are able to find their
ways into the lungs. Such particles may be composed of carcinogenic materials among them
tobacco-specific nitrosamines and polycyclic hydrocarbon besides on heavy metals.
Upon being inhaled, such particles can find their way into the deepest ends of the
respiratory system and hence resulting into severe health implications among them worsening of
the symptoms of asthma, a decrease in the functions of the lungs, increase in the mortality risk
from lung cancer and inflammation and infection of the lungs. Hydrogen cyanide is yet another
chemical that is found in tobacco smoke. Hydrogen cyanide works by interfering with how the
body used oxygen and may cause such complications as nausea, headaches, vomiting and even
dizziness.
SIGNS AND SYMPTOMS OF ORAL CANCER
Oral cancer can go unnoticed in its early stages in which it may be painless and with very
slight physical variations. At this stage, the doctors are able to notice the changes in the precursor
tissues. The symptoms in the early stages include
which have the ability to cause, initiate or even enhance cancer. Most of these chemicals are
found in second-hand smoke and a recurrent expose to such carcinogens have the potential to
increase the chances of developing cancer.
Benzene, on the other hand, is one of the most abundant chemicals that are found in
tobacco smoke. Benzene has been classified as a carcinogenic substance that is harmful to
humans. Tobacco smoke forms a major source of pollution of the indoor air in the place of
residence of the smoker. The smoke is composed of a mixture of chemicals that are in the form
of particles and gases (Zhang et al. 2011). The particles are very tiny and are able to find their
ways into the lungs. Such particles may be composed of carcinogenic materials among them
tobacco-specific nitrosamines and polycyclic hydrocarbon besides on heavy metals.
Upon being inhaled, such particles can find their way into the deepest ends of the
respiratory system and hence resulting into severe health implications among them worsening of
the symptoms of asthma, a decrease in the functions of the lungs, increase in the mortality risk
from lung cancer and inflammation and infection of the lungs. Hydrogen cyanide is yet another
chemical that is found in tobacco smoke. Hydrogen cyanide works by interfering with how the
body used oxygen and may cause such complications as nausea, headaches, vomiting and even
dizziness.
SIGNS AND SYMPTOMS OF ORAL CANCER
Oral cancer can go unnoticed in its early stages in which it may be painless and with very
slight physical variations. At this stage, the doctors are able to notice the changes in the precursor
tissues. The symptoms in the early stages include
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Persistent white or red patches
An ulcer that is never healing
A progressive enlargement or swelling (Trellakis et al. 2011)
Abnormal changes in the surfaces
Abnormal epistaxis or oral bleeding
The sudden mobility of the tooth without an apparent cause
Prolonged hoarseness
The late symptoms, on the other hand, are inclusive of:
An indurated area
Obstruction of the airway (Zini et al. 2010)
Nostalgia
Trismus
Paraesthesia or other times dysesthesias of the lips or the tongue
Prolonged pain or referred pain
Altered vision
Dysphagia
Cervical lymphadenopathy
A dramatic loss of weight
Ear pain
Challenges with chewing or swallowing, moving the jaw or the tongue or speaking
A change in the fitting of the teeth of dentures
A bleeding in the mouth with no apparent cause
An ulcer that is never healing
A progressive enlargement or swelling (Trellakis et al. 2011)
Abnormal changes in the surfaces
Abnormal epistaxis or oral bleeding
The sudden mobility of the tooth without an apparent cause
Prolonged hoarseness
The late symptoms, on the other hand, are inclusive of:
An indurated area
Obstruction of the airway (Zini et al. 2010)
Nostalgia
Trismus
Paraesthesia or other times dysesthesias of the lips or the tongue
Prolonged pain or referred pain
Altered vision
Dysphagia
Cervical lymphadenopathy
A dramatic loss of weight
Ear pain
Challenges with chewing or swallowing, moving the jaw or the tongue or speaking
A change in the fitting of the teeth of dentures
A bleeding in the mouth with no apparent cause
Stages of Oral Cancer
Staging of a disease defines or groups cancer depending on the quantity that is available
in the human body and at the time of its first diagnosis. This is in most cases referred to as the
extent of cancer. The size of the tumor is determined using the information from the tests that
have been carried out, the parts of the organs that are bearing cancer, whether or not cancer has
spread from the initial part of observation and the points to which it has spread. The TNM
system is the most commonly used staging system for oral cancer (Torre et al. 2015). There are
five distinct stages of oral cancer which runs from the stage of all the way to stage 4 through
stages 1, 2 and 3. Stages 1 to 4 is usually written in Roman numerals as I, II, III, and IV.
The stages illustrate the extent of cancer in the body such that the higher the stage the
greater the spread of cancer. In the description of the stages, in most cases, the medical
practitioner adopts the use of regional, distant or local words. Local words in this context mean
that cancer only found in the mouth and has not yet spread to the other body parts. Regional on
the other hand refers to cancer spreading to the lymph nodes that are found in the neck (cervical
lymph nodes) (Trellakis et al. 2011). Distant in the context of oral cancer description refers to a
part of the body that is far from the mouth.
Stage 0 (carcinoma in situ): In this stage, the cancer is only found in the lining of the mouth or
the lips.
Stage I: A tumor is about 2 cm in length or even less
Stage II: The length of a tumor is ranging from more than 2 cm to less at most 4 cm
Staging of a disease defines or groups cancer depending on the quantity that is available
in the human body and at the time of its first diagnosis. This is in most cases referred to as the
extent of cancer. The size of the tumor is determined using the information from the tests that
have been carried out, the parts of the organs that are bearing cancer, whether or not cancer has
spread from the initial part of observation and the points to which it has spread. The TNM
system is the most commonly used staging system for oral cancer (Torre et al. 2015). There are
five distinct stages of oral cancer which runs from the stage of all the way to stage 4 through
stages 1, 2 and 3. Stages 1 to 4 is usually written in Roman numerals as I, II, III, and IV.
The stages illustrate the extent of cancer in the body such that the higher the stage the
greater the spread of cancer. In the description of the stages, in most cases, the medical
practitioner adopts the use of regional, distant or local words. Local words in this context mean
that cancer only found in the mouth and has not yet spread to the other body parts. Regional on
the other hand refers to cancer spreading to the lymph nodes that are found in the neck (cervical
lymph nodes) (Trellakis et al. 2011). Distant in the context of oral cancer description refers to a
part of the body that is far from the mouth.
Stage 0 (carcinoma in situ): In this stage, the cancer is only found in the lining of the mouth or
the lips.
Stage I: A tumor is about 2 cm in length or even less
Stage II: The length of a tumor is ranging from more than 2 cm to less at most 4 cm
Stage III: In this stage, the tumor is greater than 4 cm or in other cancer has spread one of the
lymph nodes that are found in the neck which lie on the same side as the tumor and the lymph
node is about 3 cm or even less (Rahib et al. 2014).
Stage IVA: A tumor is of any size and might have grown into either of the following:
skin of the face
a bone found in the lower palate or lower jaw
a floor of the mouth
a nerve found on the lower jaw also known as the inferior alveolar nerve
At this stage, cancer might also have spread to one or more of the lymph nodes that are
found in the neck and during this stage, they are about 6 cm long or smaller.
Stage IV B: At this stage, the cancerous cells or a tumor has developed into the tender
tissues of the cheek including the nerves, blood vessels and the muscles or maybe into the base
of the skull. In other cases, the tumor is found to be wrapped about the internal carotid artery of
the neck. Still, at this stage, cancer has effectively spread to the lymph nodes that are found in
the neck in which one of the tumors is greater than 6 cm or otherwise cancer in the lymph nodes
has developed into the neighboring tissue.
Stage IV C: At this stage, the tumor has spread to the various other parts of the human
body and is referred to as distant metastasis. Among the regions of spread include bone, liver and
the lungs. This is also defined as metastatic cancer (Torre et al. 2015).
Recurrent Oral Cancer: Recurrent oral cancer refers to cancer that has repeated itself after
being treated before. In cases where such cancer gets to the initial place where it first began, it is
lymph nodes that are found in the neck which lie on the same side as the tumor and the lymph
node is about 3 cm or even less (Rahib et al. 2014).
Stage IVA: A tumor is of any size and might have grown into either of the following:
skin of the face
a bone found in the lower palate or lower jaw
a floor of the mouth
a nerve found on the lower jaw also known as the inferior alveolar nerve
At this stage, cancer might also have spread to one or more of the lymph nodes that are
found in the neck and during this stage, they are about 6 cm long or smaller.
Stage IV B: At this stage, the cancerous cells or a tumor has developed into the tender
tissues of the cheek including the nerves, blood vessels and the muscles or maybe into the base
of the skull. In other cases, the tumor is found to be wrapped about the internal carotid artery of
the neck. Still, at this stage, cancer has effectively spread to the lymph nodes that are found in
the neck in which one of the tumors is greater than 6 cm or otherwise cancer in the lymph nodes
has developed into the neighboring tissue.
Stage IV C: At this stage, the tumor has spread to the various other parts of the human
body and is referred to as distant metastasis. Among the regions of spread include bone, liver and
the lungs. This is also defined as metastatic cancer (Torre et al. 2015).
Recurrent Oral Cancer: Recurrent oral cancer refers to cancer that has repeated itself after
being treated before. In cases where such cancer gets to the initial place where it first began, it is
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
called local recurrence when should it come back to the lymph nodes or the tissues that are
proximate to the place of initial attack; it is defined as regional recurrence. It is also possible that
cancer may recur in other various body parts, defined as distant metastasis or in other words
distant recurrence (Tutt et al. 2010).
Grading of Oral Cancer
Grading of Oral Cancer defines the appearance of the cancer cells in comparison with the
normal and healthy cells. The knowledge on the grade offers information on the idea son the
nature of the quick growth of cancer and the manner in which it is likely to spread. Establishing
the grade of a cancer cell of oral cancer is done through looking a sample of a tissue derived
from the mouth under a microscope (Fitzmaurice et al. 2015). The difference in the look of the
cells from the normal cells also defined as differentiation is of significance in the study among
other features of the cancer cells among them their sizes and shapes and the arrangement of such
cells. Such properties are used in telling how fast the cancer is growing especially when looking
at the number of cells that are undergoing differentiation. Oral cancer is graded from grade 1 to
grade 4 in which grade 1 represents the lowest level while grade 4 illustrates the highest level.
Low-grade oral cancer bears cancer cells that are properly differentiated. Even
though these cells are abnormal, the closely resemble the normal cells and are organized more
like the normal cells. Lower grade cancer in most case grow at a relatively slow rate and thus
less likely to spread.
High-grade oral cancers show poor differentiation or even in other cases completely
undifferentiated. These do not have any resemblance with the normal cells and their arrangement
is quite different (Finch et al. 2014). The rate of growth in higher grade cancers tend to be very
quick and the chances of spread are higher in comparison with the low-grade oral cancers.
proximate to the place of initial attack; it is defined as regional recurrence. It is also possible that
cancer may recur in other various body parts, defined as distant metastasis or in other words
distant recurrence (Tutt et al. 2010).
Grading of Oral Cancer
Grading of Oral Cancer defines the appearance of the cancer cells in comparison with the
normal and healthy cells. The knowledge on the grade offers information on the idea son the
nature of the quick growth of cancer and the manner in which it is likely to spread. Establishing
the grade of a cancer cell of oral cancer is done through looking a sample of a tissue derived
from the mouth under a microscope (Fitzmaurice et al. 2015). The difference in the look of the
cells from the normal cells also defined as differentiation is of significance in the study among
other features of the cancer cells among them their sizes and shapes and the arrangement of such
cells. Such properties are used in telling how fast the cancer is growing especially when looking
at the number of cells that are undergoing differentiation. Oral cancer is graded from grade 1 to
grade 4 in which grade 1 represents the lowest level while grade 4 illustrates the highest level.
Low-grade oral cancer bears cancer cells that are properly differentiated. Even
though these cells are abnormal, the closely resemble the normal cells and are organized more
like the normal cells. Lower grade cancer in most case grow at a relatively slow rate and thus
less likely to spread.
High-grade oral cancers show poor differentiation or even in other cases completely
undifferentiated. These do not have any resemblance with the normal cells and their arrangement
is quite different (Finch et al. 2014). The rate of growth in higher grade cancers tend to be very
quick and the chances of spread are higher in comparison with the low-grade oral cancers.
SCREENING METHODS FOR ORAL CANCER
Oral cancer screening is an evaluation that is conducted by a qualified healthcare
professional to establish the signs of cancer or otherwise precancerous conditions that may be
found in the mouth. Oral cancer screening aims at identifying mouth cancer as early as possible
where the chances of treatment are still high (Tutt et al. 2010). In cases where the symptoms
have already manifested, it could be an indication that cancer might have already begun
spreading. A distinction is made by the World Health Organization that the early detection of
oral cancer through the use of visual inspection of the mouth should be treated as a different
entity and different from an organized program for screening.
Owing to the fact that oral cancer mostly occurs in a region that is typically accessible to
a physical examination by the patient and the healthcare practitioner the most commonly used
technique for screening is a visual examination in the detection of the visible lesions (Mallath et
al. 2014). There are however other adjuvant testing techniques among the biomarkers, brush
biopsy, salivary proteomics, DNA analysis, spectroscopy, autofluorescence, toluidine blue
staining which has been for a while advocated for use in clinical detection of oral lesions.
The public awareness about oral cancer might have been enhanced through the direct to
patient market of some of this testing method. However, there is no information in the available
literature that is in support of the fact that these technologies and techniques offer any
improvements in the detection of oral cancers besides precancerous lesions more than it can be
done using an elaborate conventional oral examination mostly in populations with low risk
(Ussher, Taylor & Faulkner 2017). A good screening system should bear the following
characteristics:
Simple, acceptable and safe to the general public
Oral cancer screening is an evaluation that is conducted by a qualified healthcare
professional to establish the signs of cancer or otherwise precancerous conditions that may be
found in the mouth. Oral cancer screening aims at identifying mouth cancer as early as possible
where the chances of treatment are still high (Tutt et al. 2010). In cases where the symptoms
have already manifested, it could be an indication that cancer might have already begun
spreading. A distinction is made by the World Health Organization that the early detection of
oral cancer through the use of visual inspection of the mouth should be treated as a different
entity and different from an organized program for screening.
Owing to the fact that oral cancer mostly occurs in a region that is typically accessible to
a physical examination by the patient and the healthcare practitioner the most commonly used
technique for screening is a visual examination in the detection of the visible lesions (Mallath et
al. 2014). There are however other adjuvant testing techniques among the biomarkers, brush
biopsy, salivary proteomics, DNA analysis, spectroscopy, autofluorescence, toluidine blue
staining which has been for a while advocated for use in clinical detection of oral lesions.
The public awareness about oral cancer might have been enhanced through the direct to
patient market of some of this testing method. However, there is no information in the available
literature that is in support of the fact that these technologies and techniques offer any
improvements in the detection of oral cancers besides precancerous lesions more than it can be
done using an elaborate conventional oral examination mostly in populations with low risk
(Ussher, Taylor & Faulkner 2017). A good screening system should bear the following
characteristics:
Simple, acceptable and safe to the general public
Detect lesion that can be treated or in cases where intervention would stop the
progression
Possess a high positive predictive value and low false negative values
Detect an illness in the earliest stages of its natural history
Preferentially identify the lesions which exhibit chances of progressing
The methods used in the screening of oral cancer are as discussed below:
Visual oral cancer examination: In this method, a medical clinical examination is
conducted in the oral cavity and the neighboring structures of the neck and the head. A dental
mirror alongside a good lighting system is used intraoral to enhance a comprehensive
examination. The floor of the mouth and the tongue which are the most common locations of
oral cancer alongside other intraoral structures are also remained (Finch et al. 2014).
On the extraoral aspect, properly gloved hands and an excellent lighting is used in the
examination of the palpate muscles and the skin, the lymph nodes, and the TMJ. This method
should be conducted during every dental visit and offers a good indication for monitoring of
every patient. An advantage of this method is that it is a very simple and invasive way that can
be used to the screen the changes in tissues.
Oral cytology: This is also called oral brush cytology and involves rotating a bush
between 5 to 10 times under strong pressure. It is ideal for monitoring patients that have a history
of mucosal changes. It offers a quick chairside tool that can be used in the screen of suspicious
lesions. Advantages include: being precise with minimal discomfort to the patents (Oh et al.
2016). It is thus advisable that patients with positive or atypical results be taken through scalpel
biopsy.
progression
Possess a high positive predictive value and low false negative values
Detect an illness in the earliest stages of its natural history
Preferentially identify the lesions which exhibit chances of progressing
The methods used in the screening of oral cancer are as discussed below:
Visual oral cancer examination: In this method, a medical clinical examination is
conducted in the oral cavity and the neighboring structures of the neck and the head. A dental
mirror alongside a good lighting system is used intraoral to enhance a comprehensive
examination. The floor of the mouth and the tongue which are the most common locations of
oral cancer alongside other intraoral structures are also remained (Finch et al. 2014).
On the extraoral aspect, properly gloved hands and an excellent lighting is used in the
examination of the palpate muscles and the skin, the lymph nodes, and the TMJ. This method
should be conducted during every dental visit and offers a good indication for monitoring of
every patient. An advantage of this method is that it is a very simple and invasive way that can
be used to the screen the changes in tissues.
Oral cytology: This is also called oral brush cytology and involves rotating a bush
between 5 to 10 times under strong pressure. It is ideal for monitoring patients that have a history
of mucosal changes. It offers a quick chairside tool that can be used in the screen of suspicious
lesions. Advantages include: being precise with minimal discomfort to the patents (Oh et al.
2016). It is thus advisable that patients with positive or atypical results be taken through scalpel
biopsy.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Direct visualization: This is done using tissue fluorescence and involves the use of a
blue light to illuminate the tissues of the oral cavity. A decrease in the tissue fluoresce INS
indicative of changes in the tissues. The benefits are that it can be applied as a screening tool as
well as a helpful aid in the determination of the margins when there is need to conduct the
surgical removal of a lesion (Finch et al. 2014).
Aspiration: In this method, an 18-gauge needle with a syringe that is about 5 to 10 mL
in dipped to a depth of mass. In this method, it is assumed that any lesion could be containing a
fluid. The intraosseous lesion is done before surgical operations to eliminate chances of vascular
lesion. An air aspirate could be a traumatic bone cavity in this method. There may be pus which
could be an indication of the inflammatory lesion or infection lesion (Denis et al. 2017). It often
yields a cystic lesion which is straw colored.
Excisional Biopsy: In this method, the whole lesion is removed during a surgical
diagnostic procedure. The method makes use of a blade and scalpel to generate two incisions
which then forms an ellipse at the surface being examined and a Vat its base. About 2 to 3 mm of
the normal tissues should be added in the periphery should the lesion appear benign. In cases
where the lesion appears malignant, then about 5 mm of the normal tissue is added to the
periphery. The indications include:
Lesions that is greater than 1 cm in diameter
Vascular lesions that are pigmented and small
Lesions that look benign
Lesions in regions which facilitate removal
blue light to illuminate the tissues of the oral cavity. A decrease in the tissue fluoresce INS
indicative of changes in the tissues. The benefits are that it can be applied as a screening tool as
well as a helpful aid in the determination of the margins when there is need to conduct the
surgical removal of a lesion (Finch et al. 2014).
Aspiration: In this method, an 18-gauge needle with a syringe that is about 5 to 10 mL
in dipped to a depth of mass. In this method, it is assumed that any lesion could be containing a
fluid. The intraosseous lesion is done before surgical operations to eliminate chances of vascular
lesion. An air aspirate could be a traumatic bone cavity in this method. There may be pus which
could be an indication of the inflammatory lesion or infection lesion (Denis et al. 2017). It often
yields a cystic lesion which is straw colored.
Excisional Biopsy: In this method, the whole lesion is removed during a surgical
diagnostic procedure. The method makes use of a blade and scalpel to generate two incisions
which then forms an ellipse at the surface being examined and a Vat its base. About 2 to 3 mm of
the normal tissues should be added in the periphery should the lesion appear benign. In cases
where the lesion appears malignant, then about 5 mm of the normal tissue is added to the
periphery. The indications include:
Lesions that is greater than 1 cm in diameter
Vascular lesions that are pigmented and small
Lesions that look benign
Lesions in regions which facilitate removal
Incisional Biopsy: In this method, a sample of a fraction of the lesion is taken. Two
incisions are made using a scalpel and a blade to form an ellipse on the surface and a V at the
base that would be inclusive of normal tissue (Edwards et al. 2014). The indications include:
Lesions that are more than 1 cm in diameter
Lesions that is located in a region that makes it challenging to remove them
When there is suspicion of malignancy or an aggressive benign lesion
While performing this method, the incision should be done at the edge of the lesion in order
to ensure that both the abnormal and the normal tissue are included. Still, necrotic tissue should
not be included in the specimen when conducting this method. There may need to use more than
a single biopsy in cases where the lesion various from one region to another (Edwards et al.
2014).
EPIDEMIOLOGY
There were up to about 135, 000 death that was recorded resulting from oral cancer
globally in 2013, compared to 84,000 that was reported in 1990. Oral cancer is common among
people that are on the lower end of the socioeconomic scale. Below is an overview of the
countries that are mostly affected by oral cancer in the world.
United Kingdom: Research in Britain established that there were 2386 death resulting
from oral cancer in the year 2014 while other studies in the same country established that the
dead were more prone in the category of the elderly population with just about 6% of the deaths
being people under 45 years (Kasznicki, Sliwinska & Drzewoski 2014). The statistics
demonstrate that the United Kingdom comes 16th lowest in the males category and 11th highest
for the female category in terms of the incidence of oral cancer among Europe. Oral cancer
incisions are made using a scalpel and a blade to form an ellipse on the surface and a V at the
base that would be inclusive of normal tissue (Edwards et al. 2014). The indications include:
Lesions that are more than 1 cm in diameter
Lesions that is located in a region that makes it challenging to remove them
When there is suspicion of malignancy or an aggressive benign lesion
While performing this method, the incision should be done at the edge of the lesion in order
to ensure that both the abnormal and the normal tissue are included. Still, necrotic tissue should
not be included in the specimen when conducting this method. There may need to use more than
a single biopsy in cases where the lesion various from one region to another (Edwards et al.
2014).
EPIDEMIOLOGY
There were up to about 135, 000 death that was recorded resulting from oral cancer
globally in 2013, compared to 84,000 that was reported in 1990. Oral cancer is common among
people that are on the lower end of the socioeconomic scale. Below is an overview of the
countries that are mostly affected by oral cancer in the world.
United Kingdom: Research in Britain established that there were 2386 death resulting
from oral cancer in the year 2014 while other studies in the same country established that the
dead were more prone in the category of the elderly population with just about 6% of the deaths
being people under 45 years (Kasznicki, Sliwinska & Drzewoski 2014). The statistics
demonstrate that the United Kingdom comes 16th lowest in the males category and 11th highest
for the female category in terms of the incidence of oral cancer among Europe. Oral cancer
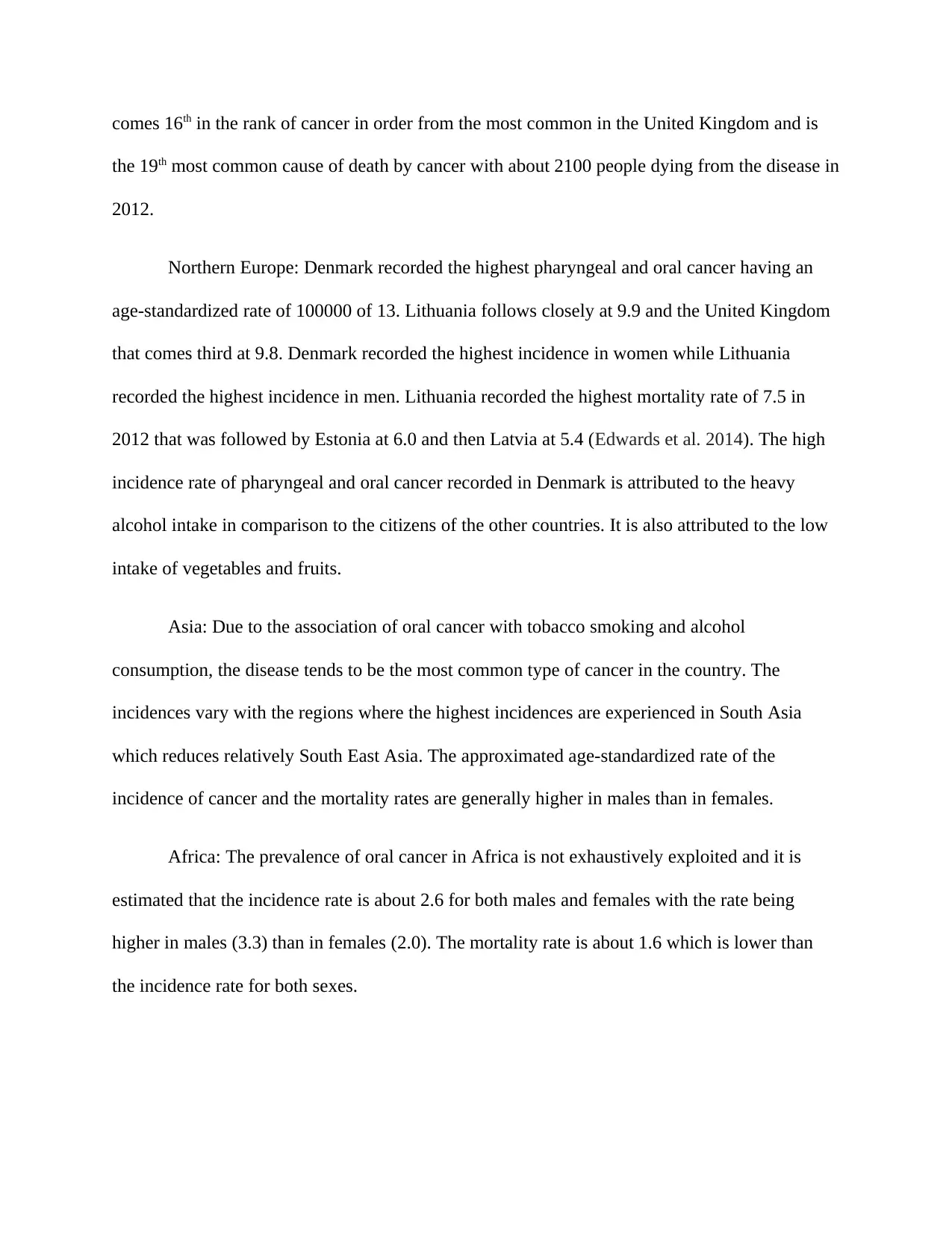
comes 16th in the rank of cancer in order from the most common in the United Kingdom and is
the 19th most common cause of death by cancer with about 2100 people dying from the disease in
2012.
Northern Europe: Denmark recorded the highest pharyngeal and oral cancer having an
age-standardized rate of 100000 of 13. Lithuania follows closely at 9.9 and the United Kingdom
that comes third at 9.8. Denmark recorded the highest incidence in women while Lithuania
recorded the highest incidence in men. Lithuania recorded the highest mortality rate of 7.5 in
2012 that was followed by Estonia at 6.0 and then Latvia at 5.4 (Edwards et al. 2014). The high
incidence rate of pharyngeal and oral cancer recorded in Denmark is attributed to the heavy
alcohol intake in comparison to the citizens of the other countries. It is also attributed to the low
intake of vegetables and fruits.
Asia: Due to the association of oral cancer with tobacco smoking and alcohol
consumption, the disease tends to be the most common type of cancer in the country. The
incidences vary with the regions where the highest incidences are experienced in South Asia
which reduces relatively South East Asia. The approximated age-standardized rate of the
incidence of cancer and the mortality rates are generally higher in males than in females.
Africa: The prevalence of oral cancer in Africa is not exhaustively exploited and it is
estimated that the incidence rate is about 2.6 for both males and females with the rate being
higher in males (3.3) than in females (2.0). The mortality rate is about 1.6 which is lower than
the incidence rate for both sexes.
the 19th most common cause of death by cancer with about 2100 people dying from the disease in
2012.
Northern Europe: Denmark recorded the highest pharyngeal and oral cancer having an
age-standardized rate of 100000 of 13. Lithuania follows closely at 9.9 and the United Kingdom
that comes third at 9.8. Denmark recorded the highest incidence in women while Lithuania
recorded the highest incidence in men. Lithuania recorded the highest mortality rate of 7.5 in
2012 that was followed by Estonia at 6.0 and then Latvia at 5.4 (Edwards et al. 2014). The high
incidence rate of pharyngeal and oral cancer recorded in Denmark is attributed to the heavy
alcohol intake in comparison to the citizens of the other countries. It is also attributed to the low
intake of vegetables and fruits.
Asia: Due to the association of oral cancer with tobacco smoking and alcohol
consumption, the disease tends to be the most common type of cancer in the country. The
incidences vary with the regions where the highest incidences are experienced in South Asia
which reduces relatively South East Asia. The approximated age-standardized rate of the
incidence of cancer and the mortality rates are generally higher in males than in females.
Africa: The prevalence of oral cancer in Africa is not exhaustively exploited and it is
estimated that the incidence rate is about 2.6 for both males and females with the rate being
higher in males (3.3) than in females (2.0). The mortality rate is about 1.6 which is lower than
the incidence rate for both sexes.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
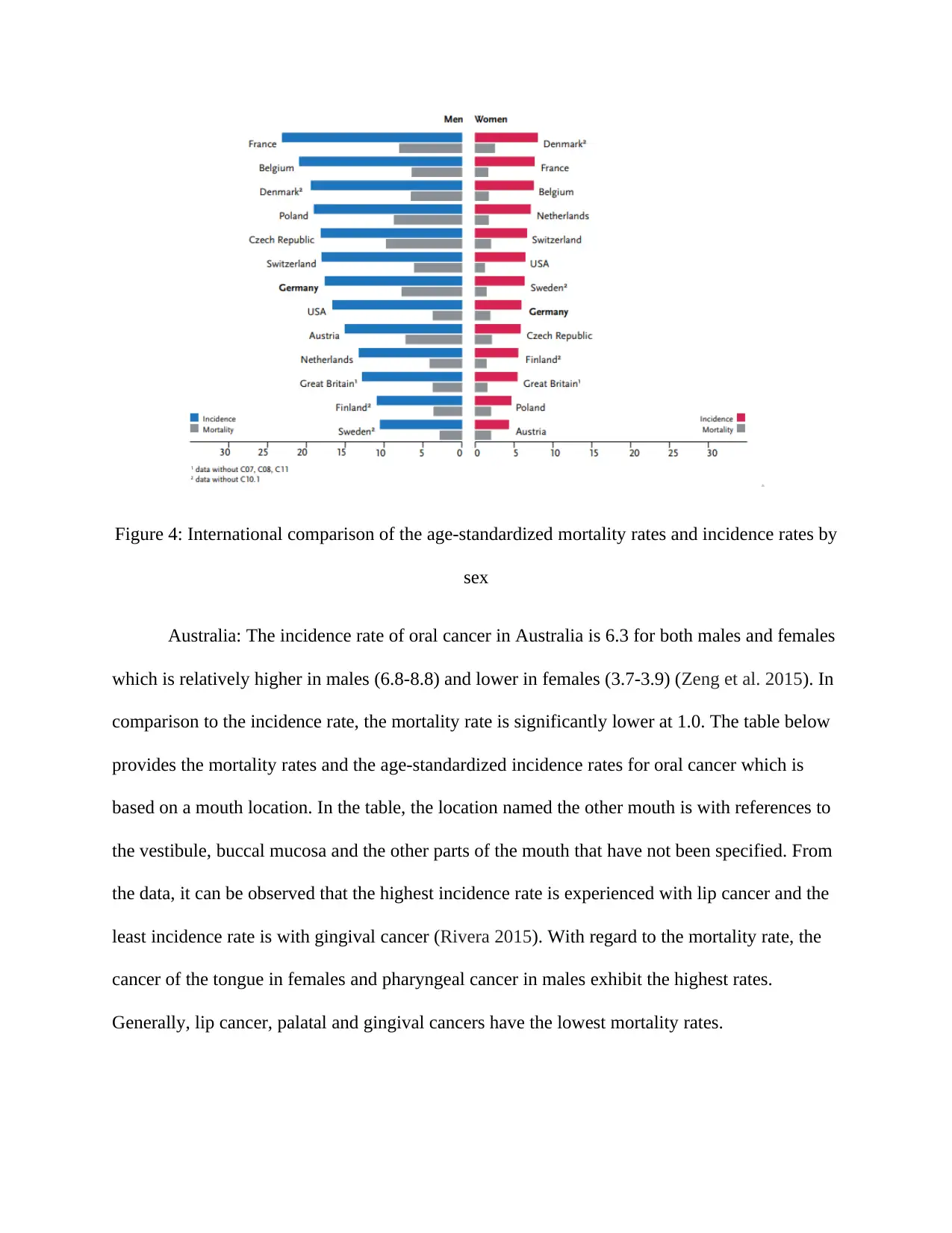
Figure 4: International comparison of the age-standardized mortality rates and incidence rates by
sex
Australia: The incidence rate of oral cancer in Australia is 6.3 for both males and females
which is relatively higher in males (6.8-8.8) and lower in females (3.7-3.9) (Zeng et al. 2015). In
comparison to the incidence rate, the mortality rate is significantly lower at 1.0. The table below
provides the mortality rates and the age-standardized incidence rates for oral cancer which is
based on a mouth location. In the table, the location named the other mouth is with references to
the vestibule, buccal mucosa and the other parts of the mouth that have not been specified. From
the data, it can be observed that the highest incidence rate is experienced with lip cancer and the
least incidence rate is with gingival cancer (Rivera 2015). With regard to the mortality rate, the
cancer of the tongue in females and pharyngeal cancer in males exhibit the highest rates.
Generally, lip cancer, palatal and gingival cancers have the lowest mortality rates.
sex
Australia: The incidence rate of oral cancer in Australia is 6.3 for both males and females
which is relatively higher in males (6.8-8.8) and lower in females (3.7-3.9) (Zeng et al. 2015). In
comparison to the incidence rate, the mortality rate is significantly lower at 1.0. The table below
provides the mortality rates and the age-standardized incidence rates for oral cancer which is
based on a mouth location. In the table, the location named the other mouth is with references to
the vestibule, buccal mucosa and the other parts of the mouth that have not been specified. From
the data, it can be observed that the highest incidence rate is experienced with lip cancer and the
least incidence rate is with gingival cancer (Rivera 2015). With regard to the mortality rate, the
cancer of the tongue in females and pharyngeal cancer in males exhibit the highest rates.
Generally, lip cancer, palatal and gingival cancers have the lowest mortality rates.
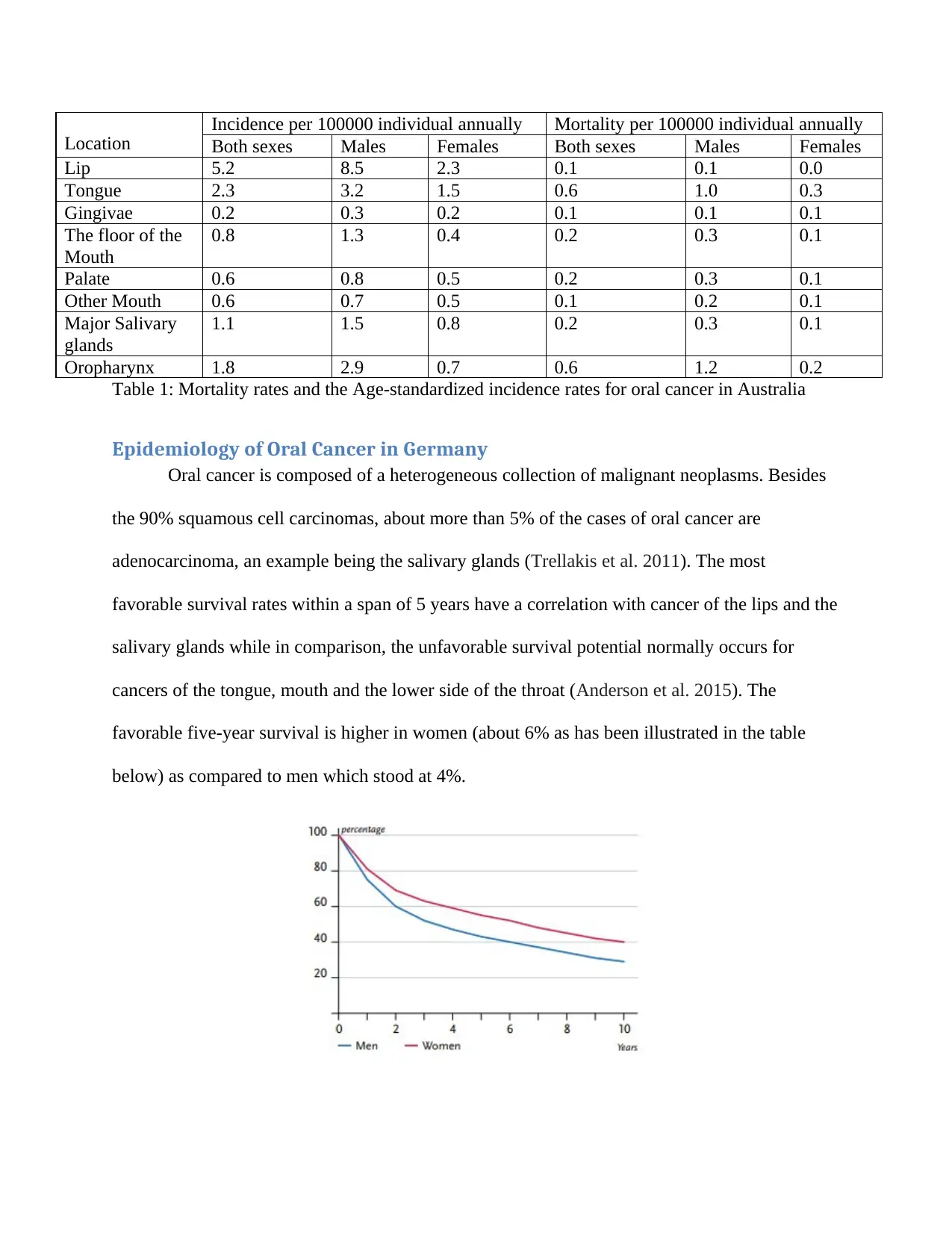
Location
Incidence per 100000 individual annually Mortality per 100000 individual annually
Both sexes Males Females Both sexes Males Females
Lip 5.2 8.5 2.3 0.1 0.1 0.0
Tongue 2.3 3.2 1.5 0.6 1.0 0.3
Gingivae 0.2 0.3 0.2 0.1 0.1 0.1
The floor of the
Mouth
0.8 1.3 0.4 0.2 0.3 0.1
Palate 0.6 0.8 0.5 0.2 0.3 0.1
Other Mouth 0.6 0.7 0.5 0.1 0.2 0.1
Major Salivary
glands
1.1 1.5 0.8 0.2 0.3 0.1
Oropharynx 1.8 2.9 0.7 0.6 1.2 0.2
Table 1: Mortality rates and the Age-standardized incidence rates for oral cancer in Australia
Epidemiology of Oral Cancer in Germany
Oral cancer is composed of a heterogeneous collection of malignant neoplasms. Besides
the 90% squamous cell carcinomas, about more than 5% of the cases of oral cancer are
adenocarcinoma, an example being the salivary glands (Trellakis et al. 2011). The most
favorable survival rates within a span of 5 years have a correlation with cancer of the lips and the
salivary glands while in comparison, the unfavorable survival potential normally occurs for
cancers of the tongue, mouth and the lower side of the throat (Anderson et al. 2015). The
favorable five-year survival is higher in women (about 6% as has been illustrated in the table
below) as compared to men which stood at 4%.
Incidence per 100000 individual annually Mortality per 100000 individual annually
Both sexes Males Females Both sexes Males Females
Lip 5.2 8.5 2.3 0.1 0.1 0.0
Tongue 2.3 3.2 1.5 0.6 1.0 0.3
Gingivae 0.2 0.3 0.2 0.1 0.1 0.1
The floor of the
Mouth
0.8 1.3 0.4 0.2 0.3 0.1
Palate 0.6 0.8 0.5 0.2 0.3 0.1
Other Mouth 0.6 0.7 0.5 0.1 0.2 0.1
Major Salivary
glands
1.1 1.5 0.8 0.2 0.3 0.1
Oropharynx 1.8 2.9 0.7 0.6 1.2 0.2
Table 1: Mortality rates and the Age-standardized incidence rates for oral cancer in Australia
Epidemiology of Oral Cancer in Germany
Oral cancer is composed of a heterogeneous collection of malignant neoplasms. Besides
the 90% squamous cell carcinomas, about more than 5% of the cases of oral cancer are
adenocarcinoma, an example being the salivary glands (Trellakis et al. 2011). The most
favorable survival rates within a span of 5 years have a correlation with cancer of the lips and the
salivary glands while in comparison, the unfavorable survival potential normally occurs for
cancers of the tongue, mouth and the lower side of the throat (Anderson et al. 2015). The
favorable five-year survival is higher in women (about 6% as has been illustrated in the table
below) as compared to men which stood at 4%.
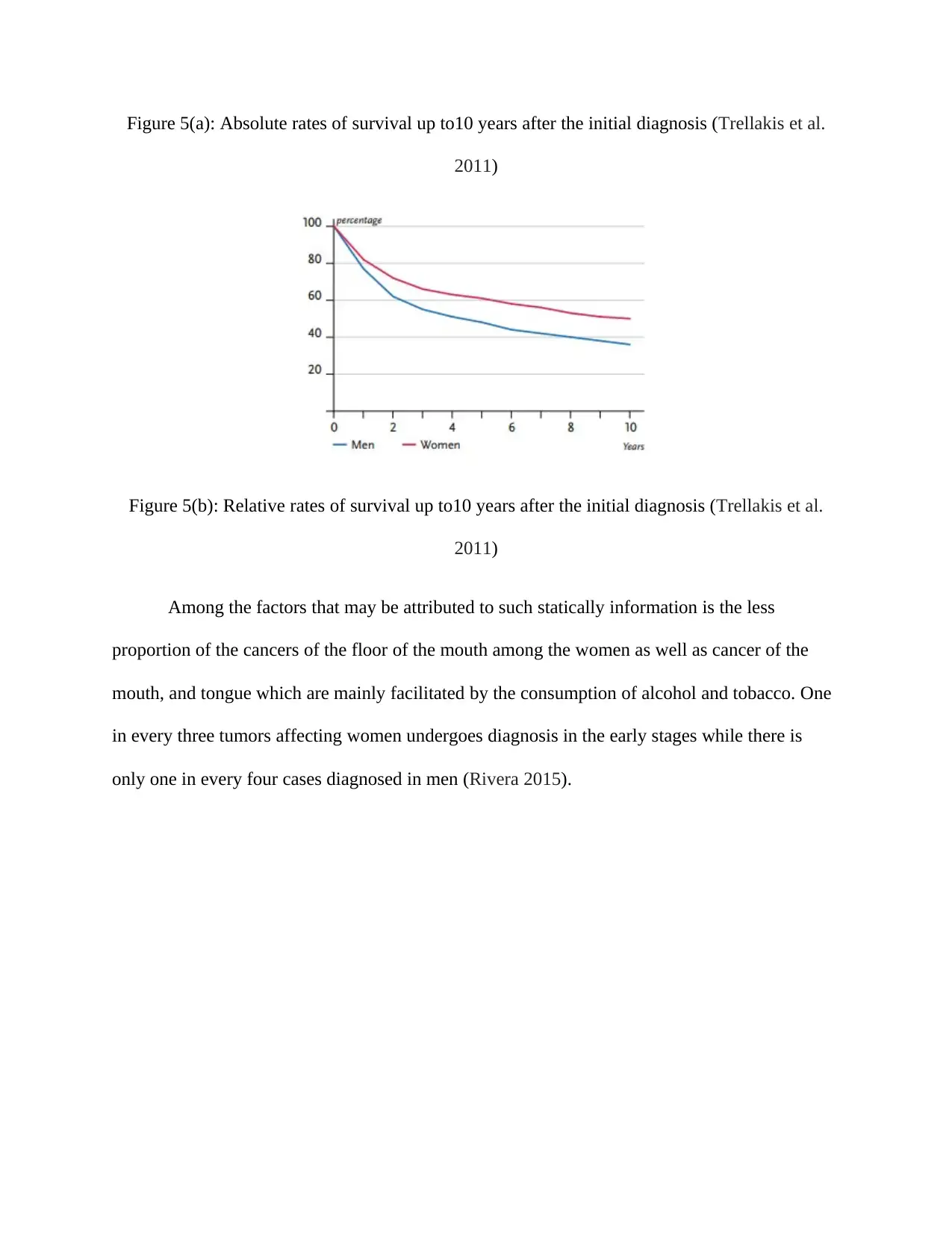
Figure 5(a): Absolute rates of survival up to10 years after the initial diagnosis (Trellakis et al.
2011)
Figure 5(b): Relative rates of survival up to10 years after the initial diagnosis (Trellakis et al.
2011)
Among the factors that may be attributed to such statically information is the less
proportion of the cancers of the floor of the mouth among the women as well as cancer of the
mouth, and tongue which are mainly facilitated by the consumption of alcohol and tobacco. One
in every three tumors affecting women undergoes diagnosis in the early stages while there is
only one in every four cases diagnosed in men (Rivera 2015).
2011)
Figure 5(b): Relative rates of survival up to10 years after the initial diagnosis (Trellakis et al.
2011)
Among the factors that may be attributed to such statically information is the less
proportion of the cancers of the floor of the mouth among the women as well as cancer of the
mouth, and tongue which are mainly facilitated by the consumption of alcohol and tobacco. One
in every three tumors affecting women undergoes diagnosis in the early stages while there is
only one in every four cases diagnosed in men (Rivera 2015).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
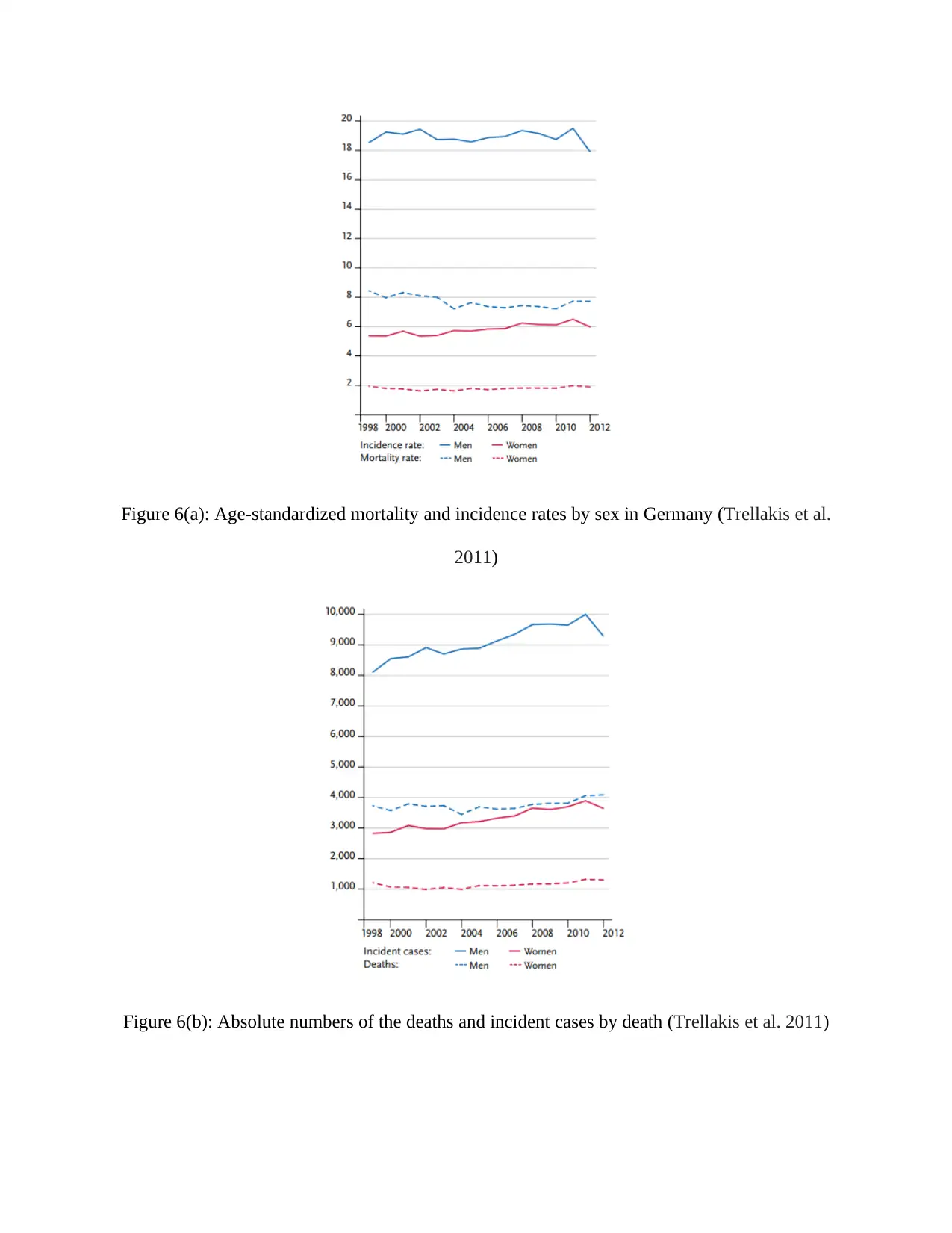
Figure 6(a): Age-standardized mortality and incidence rates by sex in Germany (Trellakis et al.
2011)
Figure 6(b): Absolute numbers of the deaths and incident cases by death (Trellakis et al. 2011)
2011)
Figure 6(b): Absolute numbers of the deaths and incident cases by death (Trellakis et al. 2011)
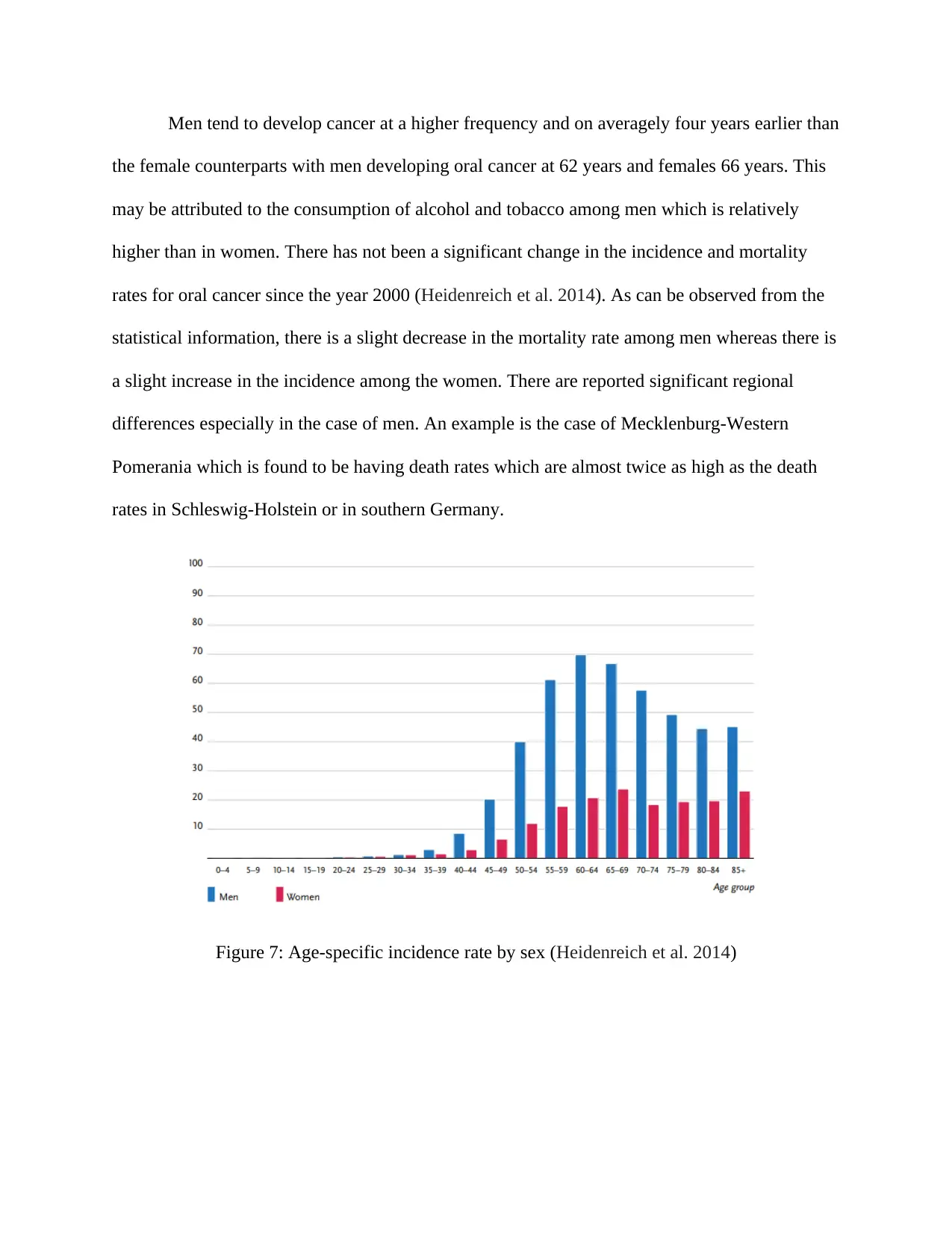
Men tend to develop cancer at a higher frequency and on averagely four years earlier than
the female counterparts with men developing oral cancer at 62 years and females 66 years. This
may be attributed to the consumption of alcohol and tobacco among men which is relatively
higher than in women. There has not been a significant change in the incidence and mortality
rates for oral cancer since the year 2000 (Heidenreich et al. 2014). As can be observed from the
statistical information, there is a slight decrease in the mortality rate among men whereas there is
a slight increase in the incidence among the women. There are reported significant regional
differences especially in the case of men. An example is the case of Mecklenburg-Western
Pomerania which is found to be having death rates which are almost twice as high as the death
rates in Schleswig-Holstein or in southern Germany.
Figure 7: Age-specific incidence rate by sex (Heidenreich et al. 2014)
the female counterparts with men developing oral cancer at 62 years and females 66 years. This
may be attributed to the consumption of alcohol and tobacco among men which is relatively
higher than in women. There has not been a significant change in the incidence and mortality
rates for oral cancer since the year 2000 (Heidenreich et al. 2014). As can be observed from the
statistical information, there is a slight decrease in the mortality rate among men whereas there is
a slight increase in the incidence among the women. There are reported significant regional
differences especially in the case of men. An example is the case of Mecklenburg-Western
Pomerania which is found to be having death rates which are almost twice as high as the death
rates in Schleswig-Holstein or in southern Germany.
Figure 7: Age-specific incidence rate by sex (Heidenreich et al. 2014)
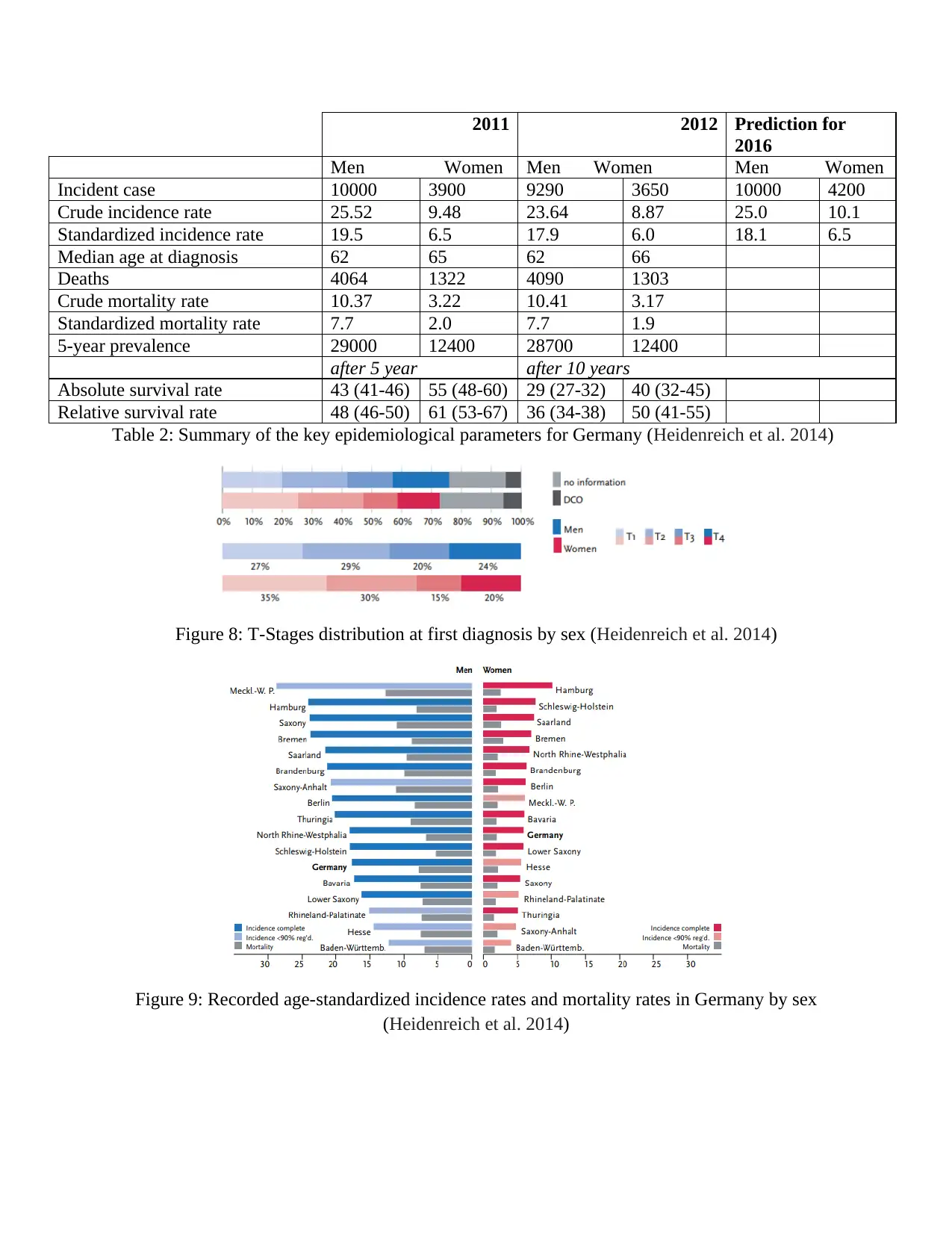
2011 2012 Prediction for
2016
Men Women Men Women Men Women
Incident case 10000 3900 9290 3650 10000 4200
Crude incidence rate 25.52 9.48 23.64 8.87 25.0 10.1
Standardized incidence rate 19.5 6.5 17.9 6.0 18.1 6.5
Median age at diagnosis 62 65 62 66
Deaths 4064 1322 4090 1303
Crude mortality rate 10.37 3.22 10.41 3.17
Standardized mortality rate 7.7 2.0 7.7 1.9
5-year prevalence 29000 12400 28700 12400
after 5 year after 10 years
Absolute survival rate 43 (41-46) 55 (48-60) 29 (27-32) 40 (32-45)
Relative survival rate 48 (46-50) 61 (53-67) 36 (34-38) 50 (41-55)
Table 2: Summary of the key epidemiological parameters for Germany (Heidenreich et al. 2014)
Figure 8: T-Stages distribution at first diagnosis by sex (Heidenreich et al. 2014)
Figure 9: Recorded age-standardized incidence rates and mortality rates in Germany by sex
(Heidenreich et al. 2014)
2016
Men Women Men Women Men Women
Incident case 10000 3900 9290 3650 10000 4200
Crude incidence rate 25.52 9.48 23.64 8.87 25.0 10.1
Standardized incidence rate 19.5 6.5 17.9 6.0 18.1 6.5
Median age at diagnosis 62 65 62 66
Deaths 4064 1322 4090 1303
Crude mortality rate 10.37 3.22 10.41 3.17
Standardized mortality rate 7.7 2.0 7.7 1.9
5-year prevalence 29000 12400 28700 12400
after 5 year after 10 years
Absolute survival rate 43 (41-46) 55 (48-60) 29 (27-32) 40 (32-45)
Relative survival rate 48 (46-50) 61 (53-67) 36 (34-38) 50 (41-55)
Table 2: Summary of the key epidemiological parameters for Germany (Heidenreich et al. 2014)
Figure 8: T-Stages distribution at first diagnosis by sex (Heidenreich et al. 2014)
Figure 9: Recorded age-standardized incidence rates and mortality rates in Germany by sex
(Heidenreich et al. 2014)
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
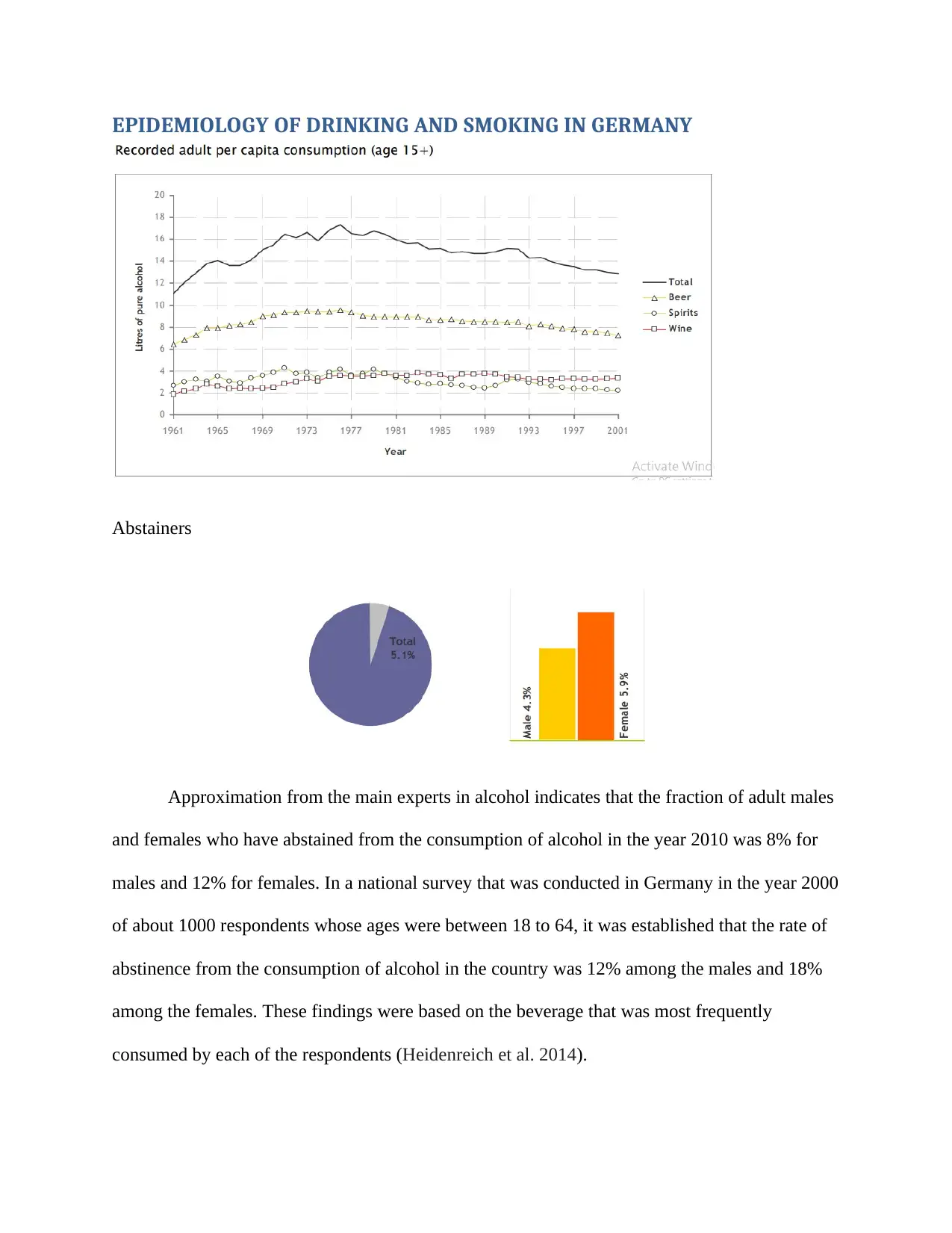
EPIDEMIOLOGY OF DRINKING AND SMOKING IN GERMANY
Abstainers
Approximation from the main experts in alcohol indicates that the fraction of adult males
and females who have abstained from the consumption of alcohol in the year 2010 was 8% for
males and 12% for females. In a national survey that was conducted in Germany in the year 2000
of about 1000 respondents whose ages were between 18 to 64, it was established that the rate of
abstinence from the consumption of alcohol in the country was 12% among the males and 18%
among the females. These findings were based on the beverage that was most frequently
consumed by each of the respondents (Heidenreich et al. 2014).
Abstainers
Approximation from the main experts in alcohol indicates that the fraction of adult males
and females who have abstained from the consumption of alcohol in the year 2010 was 8% for
males and 12% for females. In a national survey that was conducted in Germany in the year 2000
of about 1000 respondents whose ages were between 18 to 64, it was established that the rate of
abstinence from the consumption of alcohol in the country was 12% among the males and 18%
among the females. These findings were based on the beverage that was most frequently
consumed by each of the respondents (Heidenreich et al. 2014).
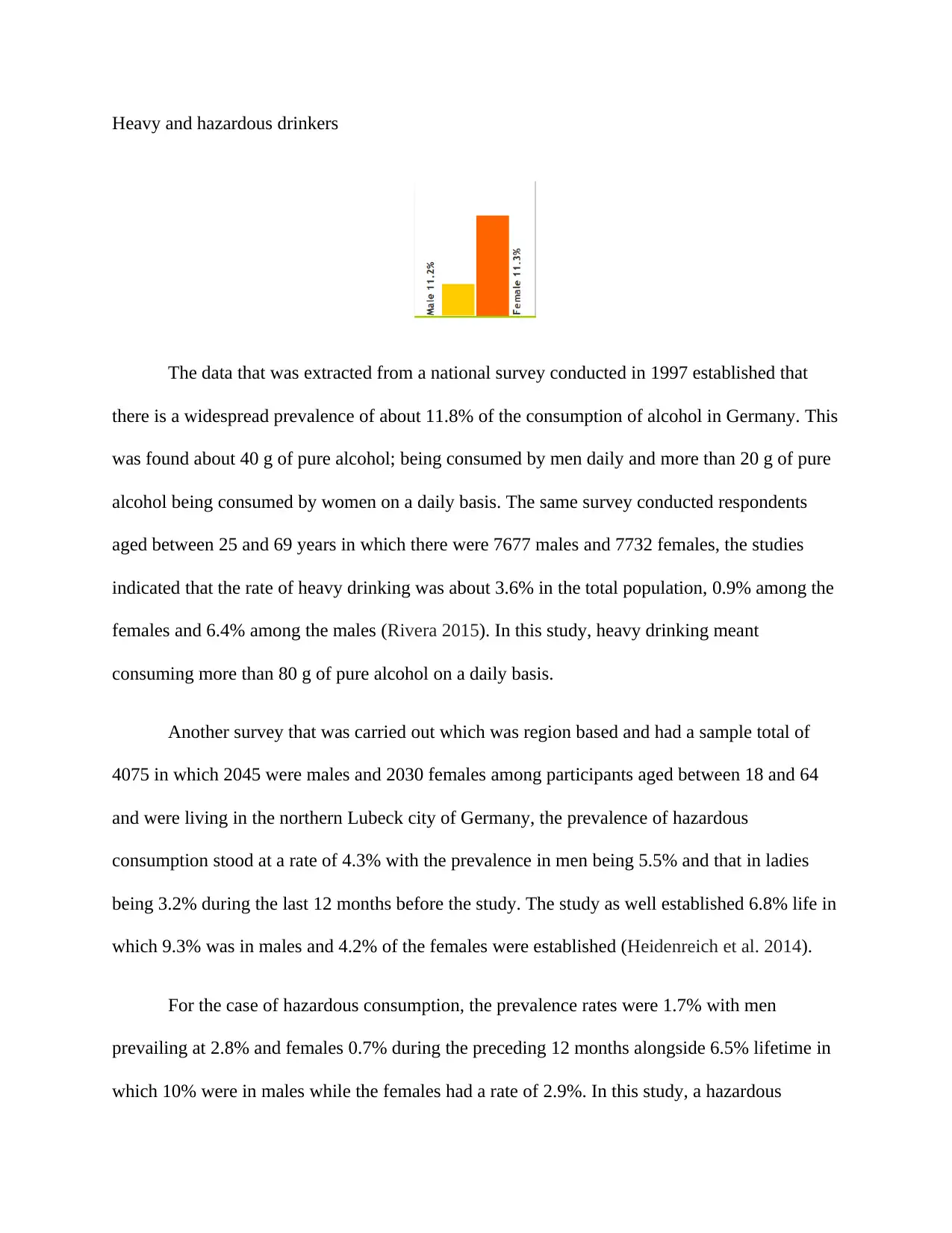
Heavy and hazardous drinkers
The data that was extracted from a national survey conducted in 1997 established that
there is a widespread prevalence of about 11.8% of the consumption of alcohol in Germany. This
was found about 40 g of pure alcohol; being consumed by men daily and more than 20 g of pure
alcohol being consumed by women on a daily basis. The same survey conducted respondents
aged between 25 and 69 years in which there were 7677 males and 7732 females, the studies
indicated that the rate of heavy drinking was about 3.6% in the total population, 0.9% among the
females and 6.4% among the males (Rivera 2015). In this study, heavy drinking meant
consuming more than 80 g of pure alcohol on a daily basis.
Another survey that was carried out which was region based and had a sample total of
4075 in which 2045 were males and 2030 females among participants aged between 18 and 64
and were living in the northern Lubeck city of Germany, the prevalence of hazardous
consumption stood at a rate of 4.3% with the prevalence in men being 5.5% and that in ladies
being 3.2% during the last 12 months before the study. The study as well established 6.8% life in
which 9.3% was in males and 4.2% of the females were established (Heidenreich et al. 2014).
For the case of hazardous consumption, the prevalence rates were 1.7% with men
prevailing at 2.8% and females 0.7% during the preceding 12 months alongside 6.5% lifetime in
which 10% were in males while the females had a rate of 2.9%. In this study, a hazardous
The data that was extracted from a national survey conducted in 1997 established that
there is a widespread prevalence of about 11.8% of the consumption of alcohol in Germany. This
was found about 40 g of pure alcohol; being consumed by men daily and more than 20 g of pure
alcohol being consumed by women on a daily basis. The same survey conducted respondents
aged between 25 and 69 years in which there were 7677 males and 7732 females, the studies
indicated that the rate of heavy drinking was about 3.6% in the total population, 0.9% among the
females and 6.4% among the males (Rivera 2015). In this study, heavy drinking meant
consuming more than 80 g of pure alcohol on a daily basis.
Another survey that was carried out which was region based and had a sample total of
4075 in which 2045 were males and 2030 females among participants aged between 18 and 64
and were living in the northern Lubeck city of Germany, the prevalence of hazardous
consumption stood at a rate of 4.3% with the prevalence in men being 5.5% and that in ladies
being 3.2% during the last 12 months before the study. The study as well established 6.8% life in
which 9.3% was in males and 4.2% of the females were established (Heidenreich et al. 2014).
For the case of hazardous consumption, the prevalence rates were 1.7% with men
prevailing at 2.8% and females 0.7% during the preceding 12 months alongside 6.5% lifetime in
which 10% were in males while the females had a rate of 2.9%. In this study, a hazardous
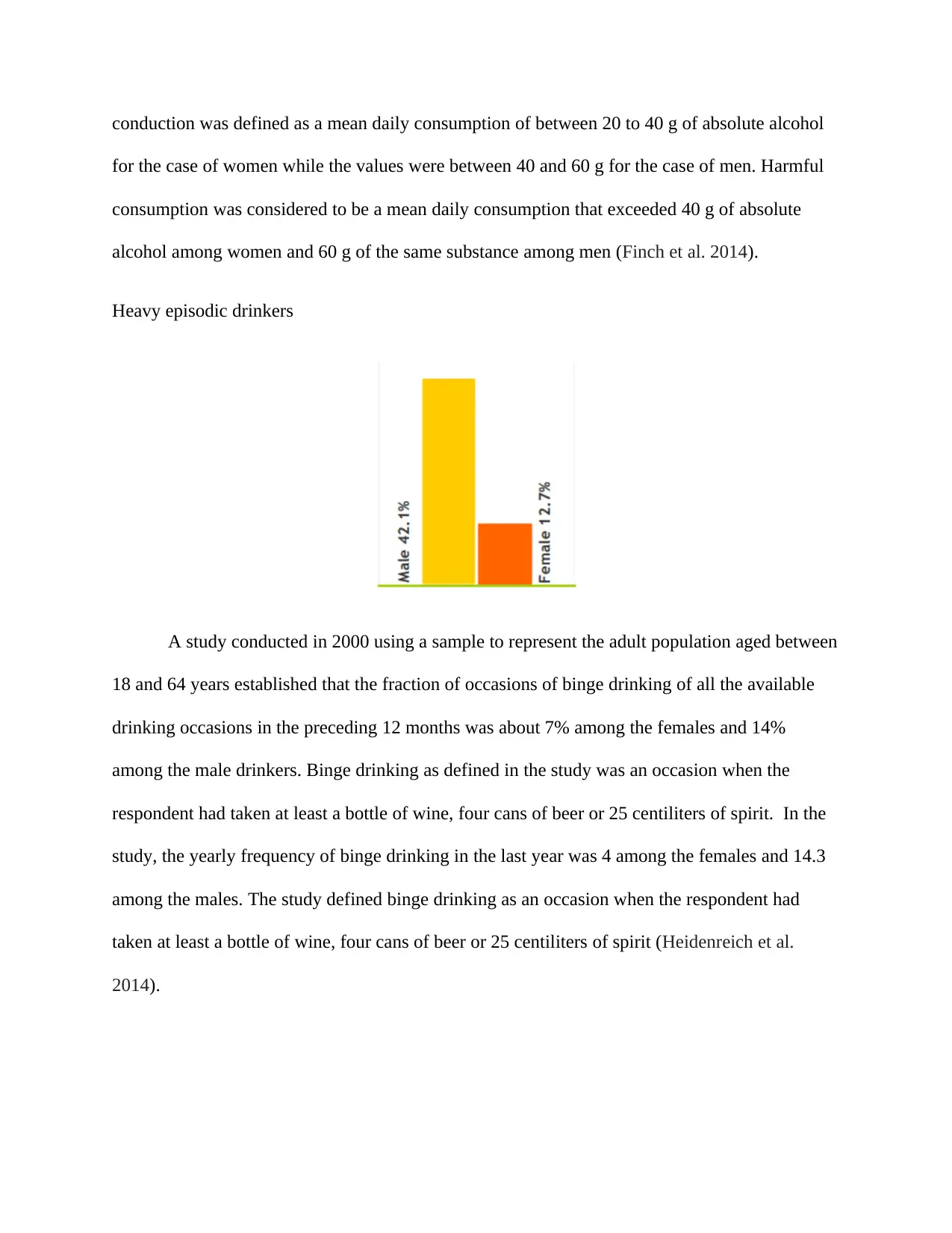
conduction was defined as a mean daily consumption of between 20 to 40 g of absolute alcohol
for the case of women while the values were between 40 and 60 g for the case of men. Harmful
consumption was considered to be a mean daily consumption that exceeded 40 g of absolute
alcohol among women and 60 g of the same substance among men (Finch et al. 2014).
Heavy episodic drinkers
A study conducted in 2000 using a sample to represent the adult population aged between
18 and 64 years established that the fraction of occasions of binge drinking of all the available
drinking occasions in the preceding 12 months was about 7% among the females and 14%
among the male drinkers. Binge drinking as defined in the study was an occasion when the
respondent had taken at least a bottle of wine, four cans of beer or 25 centiliters of spirit. In the
study, the yearly frequency of binge drinking in the last year was 4 among the females and 14.3
among the males. The study defined binge drinking as an occasion when the respondent had
taken at least a bottle of wine, four cans of beer or 25 centiliters of spirit (Heidenreich et al.
2014).
for the case of women while the values were between 40 and 60 g for the case of men. Harmful
consumption was considered to be a mean daily consumption that exceeded 40 g of absolute
alcohol among women and 60 g of the same substance among men (Finch et al. 2014).
Heavy episodic drinkers
A study conducted in 2000 using a sample to represent the adult population aged between
18 and 64 years established that the fraction of occasions of binge drinking of all the available
drinking occasions in the preceding 12 months was about 7% among the females and 14%
among the male drinkers. Binge drinking as defined in the study was an occasion when the
respondent had taken at least a bottle of wine, four cans of beer or 25 centiliters of spirit. In the
study, the yearly frequency of binge drinking in the last year was 4 among the females and 14.3
among the males. The study defined binge drinking as an occasion when the respondent had
taken at least a bottle of wine, four cans of beer or 25 centiliters of spirit (Heidenreich et al.
2014).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
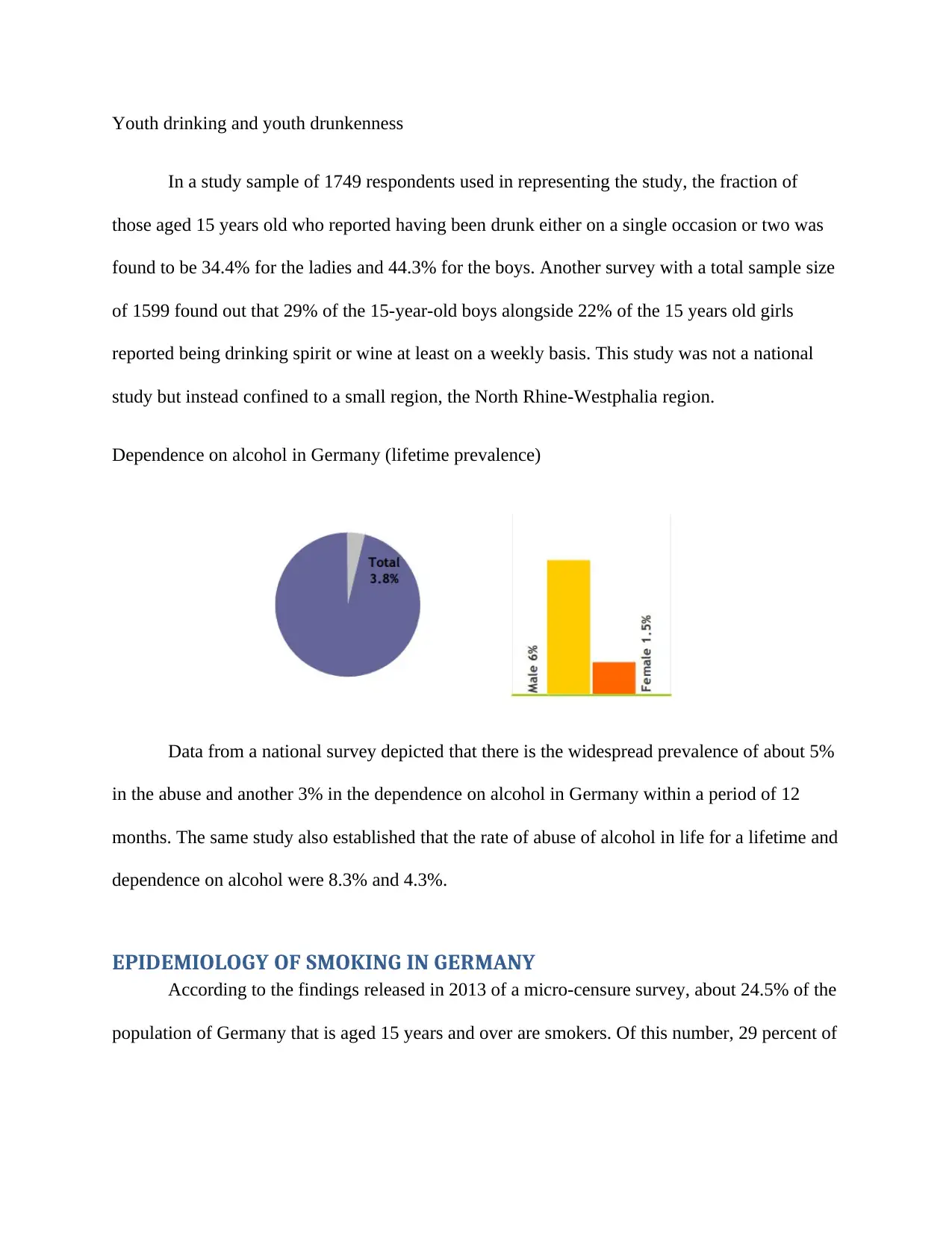
Youth drinking and youth drunkenness
In a study sample of 1749 respondents used in representing the study, the fraction of
those aged 15 years old who reported having been drunk either on a single occasion or two was
found to be 34.4% for the ladies and 44.3% for the boys. Another survey with a total sample size
of 1599 found out that 29% of the 15-year-old boys alongside 22% of the 15 years old girls
reported being drinking spirit or wine at least on a weekly basis. This study was not a national
study but instead confined to a small region, the North Rhine-Westphalia region.
Dependence on alcohol in Germany (lifetime prevalence)
Data from a national survey depicted that there is the widespread prevalence of about 5%
in the abuse and another 3% in the dependence on alcohol in Germany within a period of 12
months. The same study also established that the rate of abuse of alcohol in life for a lifetime and
dependence on alcohol were 8.3% and 4.3%.
EPIDEMIOLOGY OF SMOKING IN GERMANY
According to the findings released in 2013 of a micro-censure survey, about 24.5% of the
population of Germany that is aged 15 years and over are smokers. Of this number, 29 percent of
In a study sample of 1749 respondents used in representing the study, the fraction of
those aged 15 years old who reported having been drunk either on a single occasion or two was
found to be 34.4% for the ladies and 44.3% for the boys. Another survey with a total sample size
of 1599 found out that 29% of the 15-year-old boys alongside 22% of the 15 years old girls
reported being drinking spirit or wine at least on a weekly basis. This study was not a national
study but instead confined to a small region, the North Rhine-Westphalia region.
Dependence on alcohol in Germany (lifetime prevalence)
Data from a national survey depicted that there is the widespread prevalence of about 5%
in the abuse and another 3% in the dependence on alcohol in Germany within a period of 12
months. The same study also established that the rate of abuse of alcohol in life for a lifetime and
dependence on alcohol were 8.3% and 4.3%.
EPIDEMIOLOGY OF SMOKING IN GERMANY
According to the findings released in 2013 of a micro-censure survey, about 24.5% of the
population of Germany that is aged 15 years and over are smokers. Of this number, 29 percent of
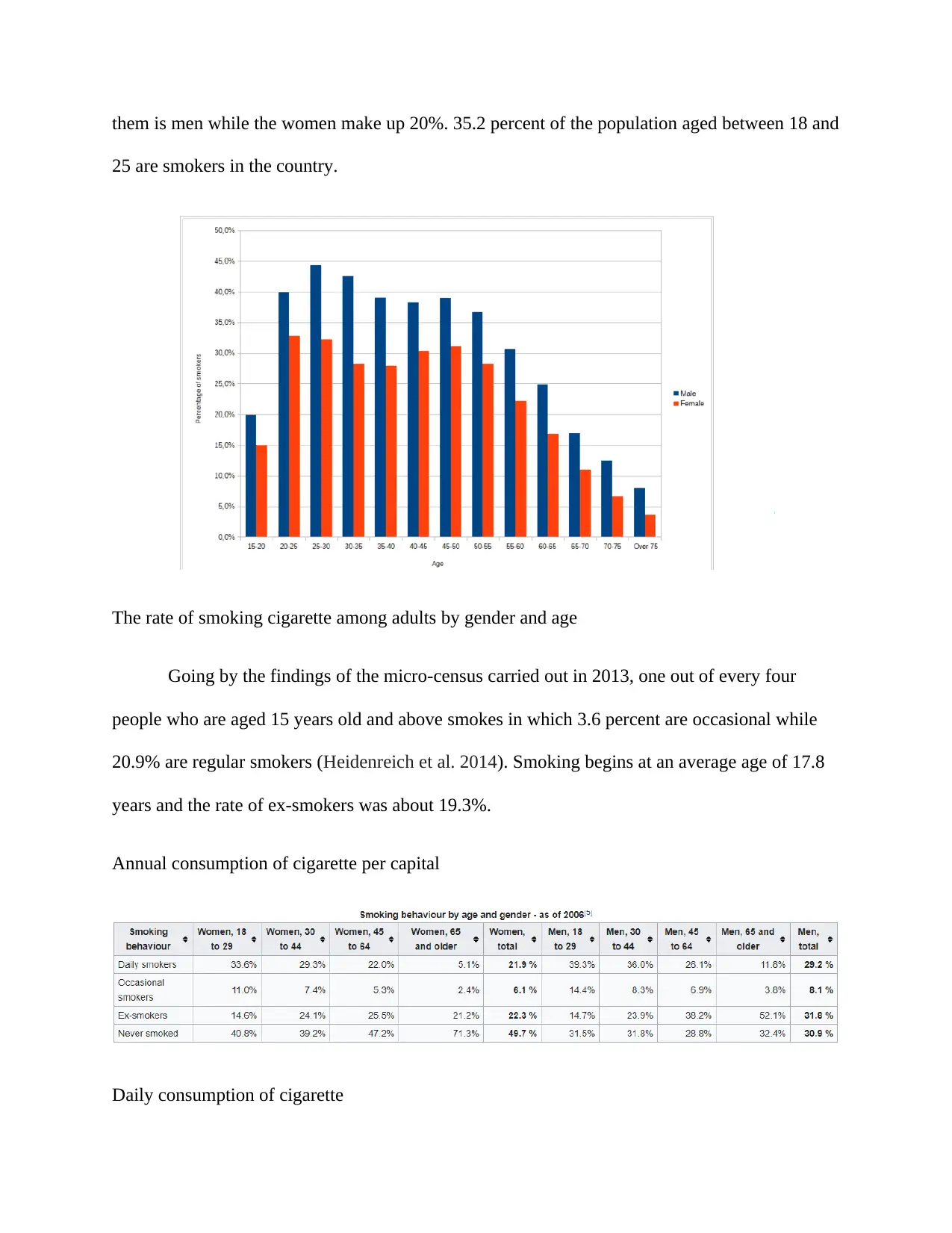
them is men while the women make up 20%. 35.2 percent of the population aged between 18 and
25 are smokers in the country.
The rate of smoking cigarette among adults by gender and age
Going by the findings of the micro-census carried out in 2013, one out of every four
people who are aged 15 years old and above smokes in which 3.6 percent are occasional while
20.9% are regular smokers (Heidenreich et al. 2014). Smoking begins at an average age of 17.8
years and the rate of ex-smokers was about 19.3%.
Annual consumption of cigarette per capital
Daily consumption of cigarette
25 are smokers in the country.
The rate of smoking cigarette among adults by gender and age
Going by the findings of the micro-census carried out in 2013, one out of every four
people who are aged 15 years old and above smokes in which 3.6 percent are occasional while
20.9% are regular smokers (Heidenreich et al. 2014). Smoking begins at an average age of 17.8
years and the rate of ex-smokers was about 19.3%.
Annual consumption of cigarette per capital
Daily consumption of cigarette
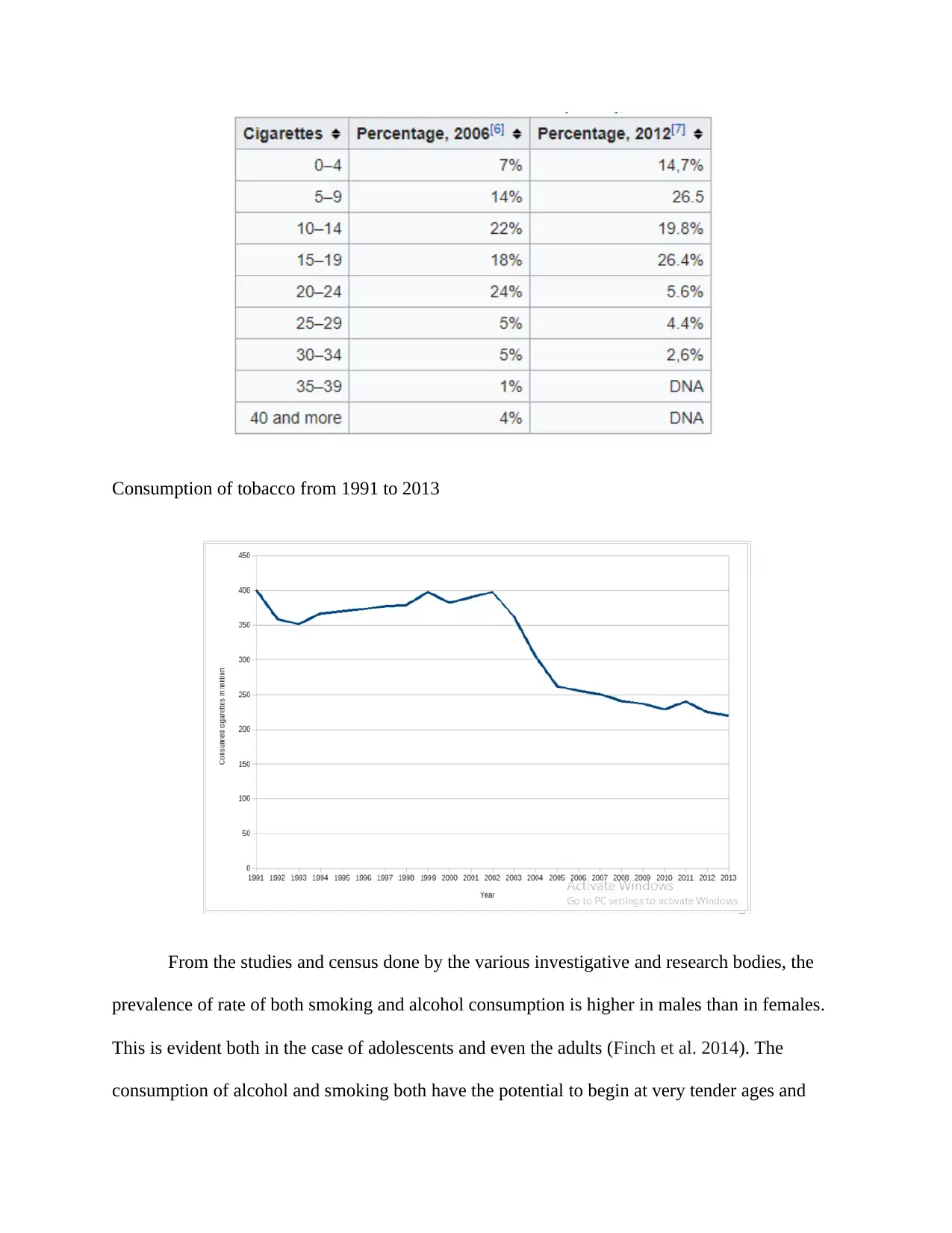
Consumption of tobacco from 1991 to 2013
From the studies and census done by the various investigative and research bodies, the
prevalence of rate of both smoking and alcohol consumption is higher in males than in females.
This is evident both in the case of adolescents and even the adults (Finch et al. 2014). The
consumption of alcohol and smoking both have the potential to begin at very tender ages and
From the studies and census done by the various investigative and research bodies, the
prevalence of rate of both smoking and alcohol consumption is higher in males than in females.
This is evident both in the case of adolescents and even the adults (Finch et al. 2014). The
consumption of alcohol and smoking both have the potential to begin at very tender ages and
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
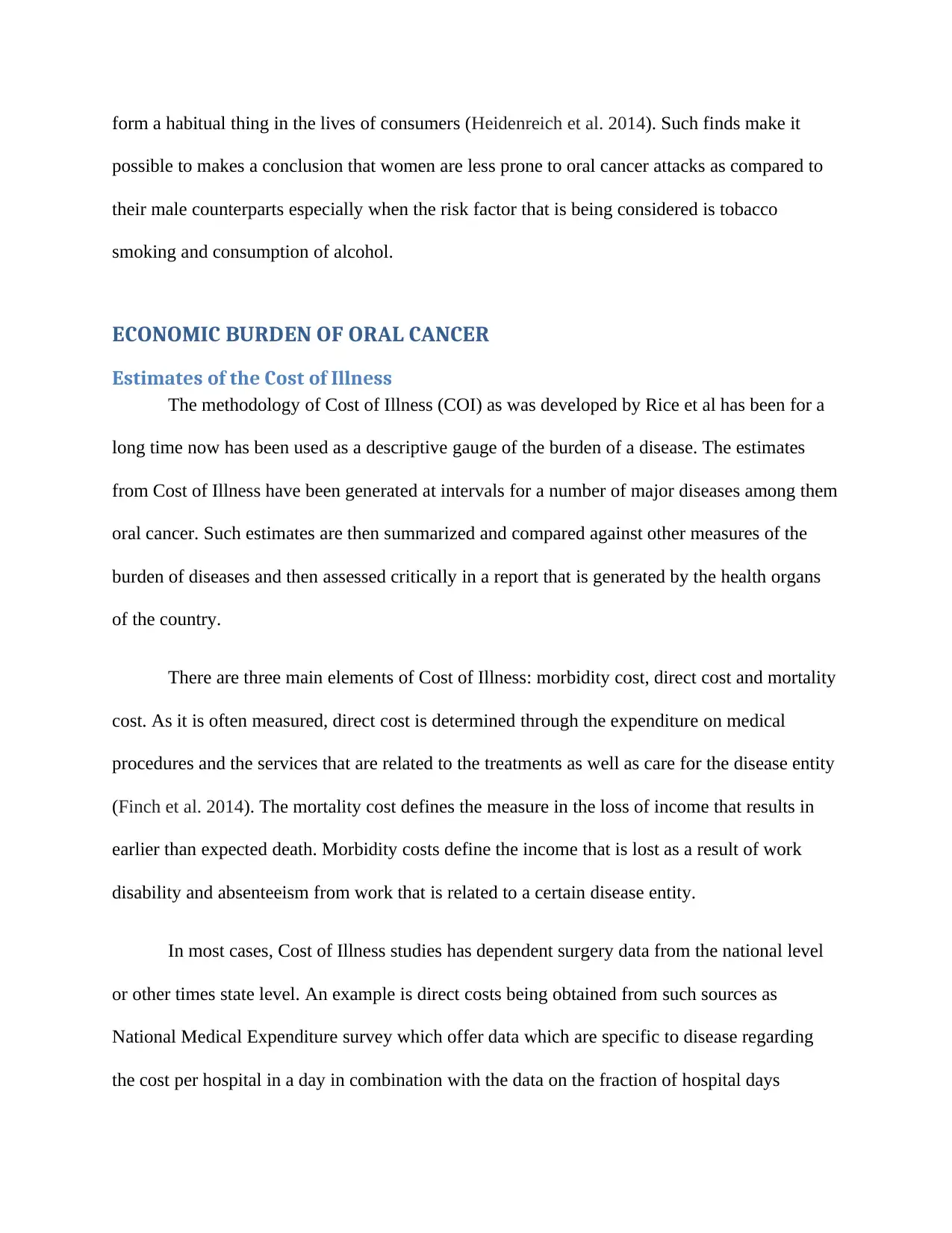
form a habitual thing in the lives of consumers (Heidenreich et al. 2014). Such finds make it
possible to makes a conclusion that women are less prone to oral cancer attacks as compared to
their male counterparts especially when the risk factor that is being considered is tobacco
smoking and consumption of alcohol.
ECONOMIC BURDEN OF ORAL CANCER
Estimates of the Cost of Illness
The methodology of Cost of Illness (COI) as was developed by Rice et al has been for a
long time now has been used as a descriptive gauge of the burden of a disease. The estimates
from Cost of Illness have been generated at intervals for a number of major diseases among them
oral cancer. Such estimates are then summarized and compared against other measures of the
burden of diseases and then assessed critically in a report that is generated by the health organs
of the country.
There are three main elements of Cost of Illness: morbidity cost, direct cost and mortality
cost. As it is often measured, direct cost is determined through the expenditure on medical
procedures and the services that are related to the treatments as well as care for the disease entity
(Finch et al. 2014). The mortality cost defines the measure in the loss of income that results in
earlier than expected death. Morbidity costs define the income that is lost as a result of work
disability and absenteeism from work that is related to a certain disease entity.
In most cases, Cost of Illness studies has dependent surgery data from the national level
or other times state level. An example is direct costs being obtained from such sources as
National Medical Expenditure survey which offer data which are specific to disease regarding
the cost per hospital in a day in combination with the data on the fraction of hospital days
possible to makes a conclusion that women are less prone to oral cancer attacks as compared to
their male counterparts especially when the risk factor that is being considered is tobacco
smoking and consumption of alcohol.
ECONOMIC BURDEN OF ORAL CANCER
Estimates of the Cost of Illness
The methodology of Cost of Illness (COI) as was developed by Rice et al has been for a
long time now has been used as a descriptive gauge of the burden of a disease. The estimates
from Cost of Illness have been generated at intervals for a number of major diseases among them
oral cancer. Such estimates are then summarized and compared against other measures of the
burden of diseases and then assessed critically in a report that is generated by the health organs
of the country.
There are three main elements of Cost of Illness: morbidity cost, direct cost and mortality
cost. As it is often measured, direct cost is determined through the expenditure on medical
procedures and the services that are related to the treatments as well as care for the disease entity
(Finch et al. 2014). The mortality cost defines the measure in the loss of income that results in
earlier than expected death. Morbidity costs define the income that is lost as a result of work
disability and absenteeism from work that is related to a certain disease entity.
In most cases, Cost of Illness studies has dependent surgery data from the national level
or other times state level. An example is direct costs being obtained from such sources as
National Medical Expenditure survey which offer data which are specific to disease regarding
the cost per hospital in a day in combination with the data on the fraction of hospital days
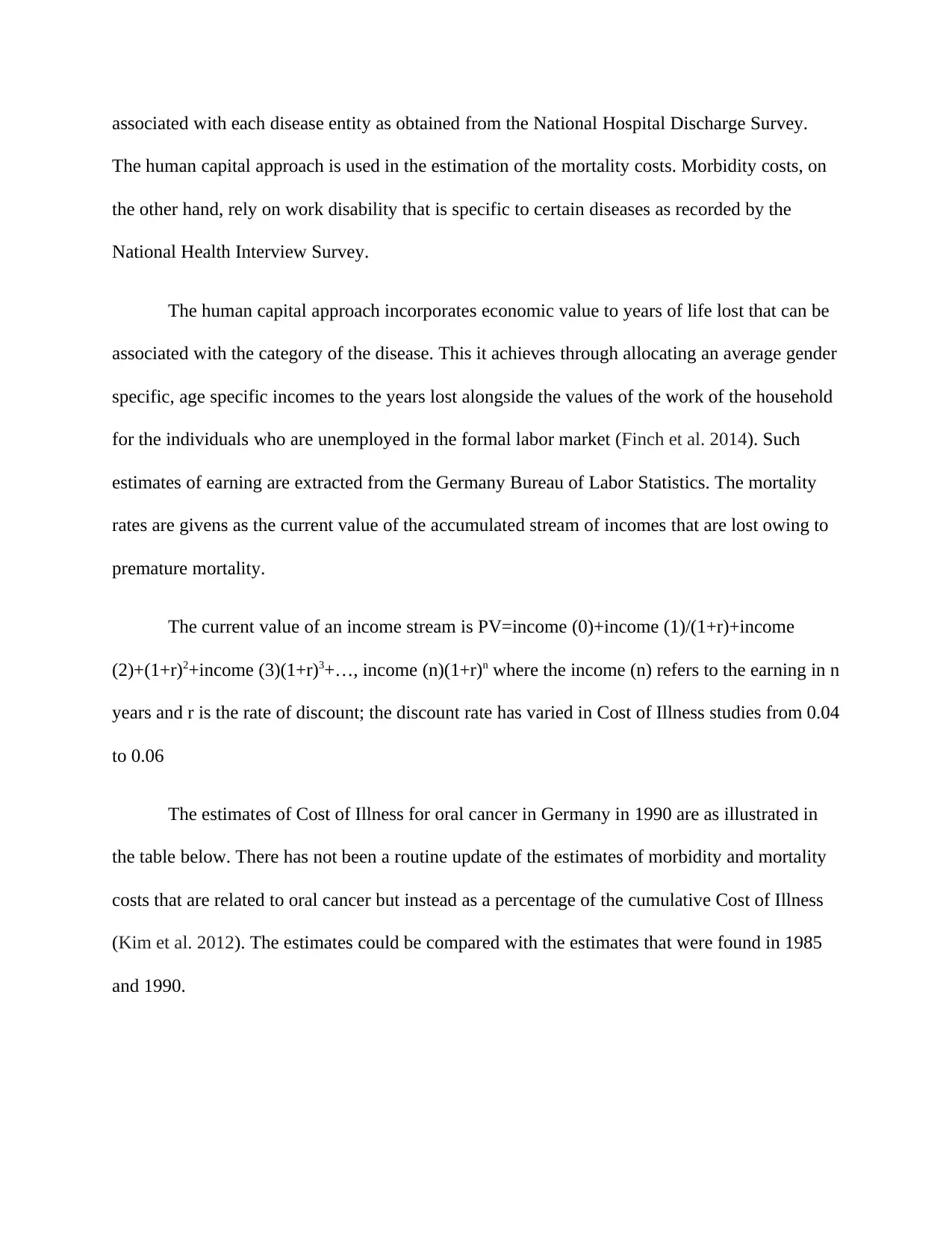
associated with each disease entity as obtained from the National Hospital Discharge Survey.
The human capital approach is used in the estimation of the mortality costs. Morbidity costs, on
the other hand, rely on work disability that is specific to certain diseases as recorded by the
National Health Interview Survey.
The human capital approach incorporates economic value to years of life lost that can be
associated with the category of the disease. This it achieves through allocating an average gender
specific, age specific incomes to the years lost alongside the values of the work of the household
for the individuals who are unemployed in the formal labor market (Finch et al. 2014). Such
estimates of earning are extracted from the Germany Bureau of Labor Statistics. The mortality
rates are givens as the current value of the accumulated stream of incomes that are lost owing to
premature mortality.
The current value of an income stream is PV=income (0)+income (1)/(1+r)+income
(2)+(1+r)2+income (3)(1+r)3+…, income (n)(1+r)n where the income (n) refers to the earning in n
years and r is the rate of discount; the discount rate has varied in Cost of Illness studies from 0.04
to 0.06
The estimates of Cost of Illness for oral cancer in Germany in 1990 are as illustrated in
the table below. There has not been a routine update of the estimates of morbidity and mortality
costs that are related to oral cancer but instead as a percentage of the cumulative Cost of Illness
(Kim et al. 2012). The estimates could be compared with the estimates that were found in 1985
and 1990.
The human capital approach is used in the estimation of the mortality costs. Morbidity costs, on
the other hand, rely on work disability that is specific to certain diseases as recorded by the
National Health Interview Survey.
The human capital approach incorporates economic value to years of life lost that can be
associated with the category of the disease. This it achieves through allocating an average gender
specific, age specific incomes to the years lost alongside the values of the work of the household
for the individuals who are unemployed in the formal labor market (Finch et al. 2014). Such
estimates of earning are extracted from the Germany Bureau of Labor Statistics. The mortality
rates are givens as the current value of the accumulated stream of incomes that are lost owing to
premature mortality.
The current value of an income stream is PV=income (0)+income (1)/(1+r)+income
(2)+(1+r)2+income (3)(1+r)3+…, income (n)(1+r)n where the income (n) refers to the earning in n
years and r is the rate of discount; the discount rate has varied in Cost of Illness studies from 0.04
to 0.06
The estimates of Cost of Illness for oral cancer in Germany in 1990 are as illustrated in
the table below. There has not been a routine update of the estimates of morbidity and mortality
costs that are related to oral cancer but instead as a percentage of the cumulative Cost of Illness
(Kim et al. 2012). The estimates could be compared with the estimates that were found in 1985
and 1990.
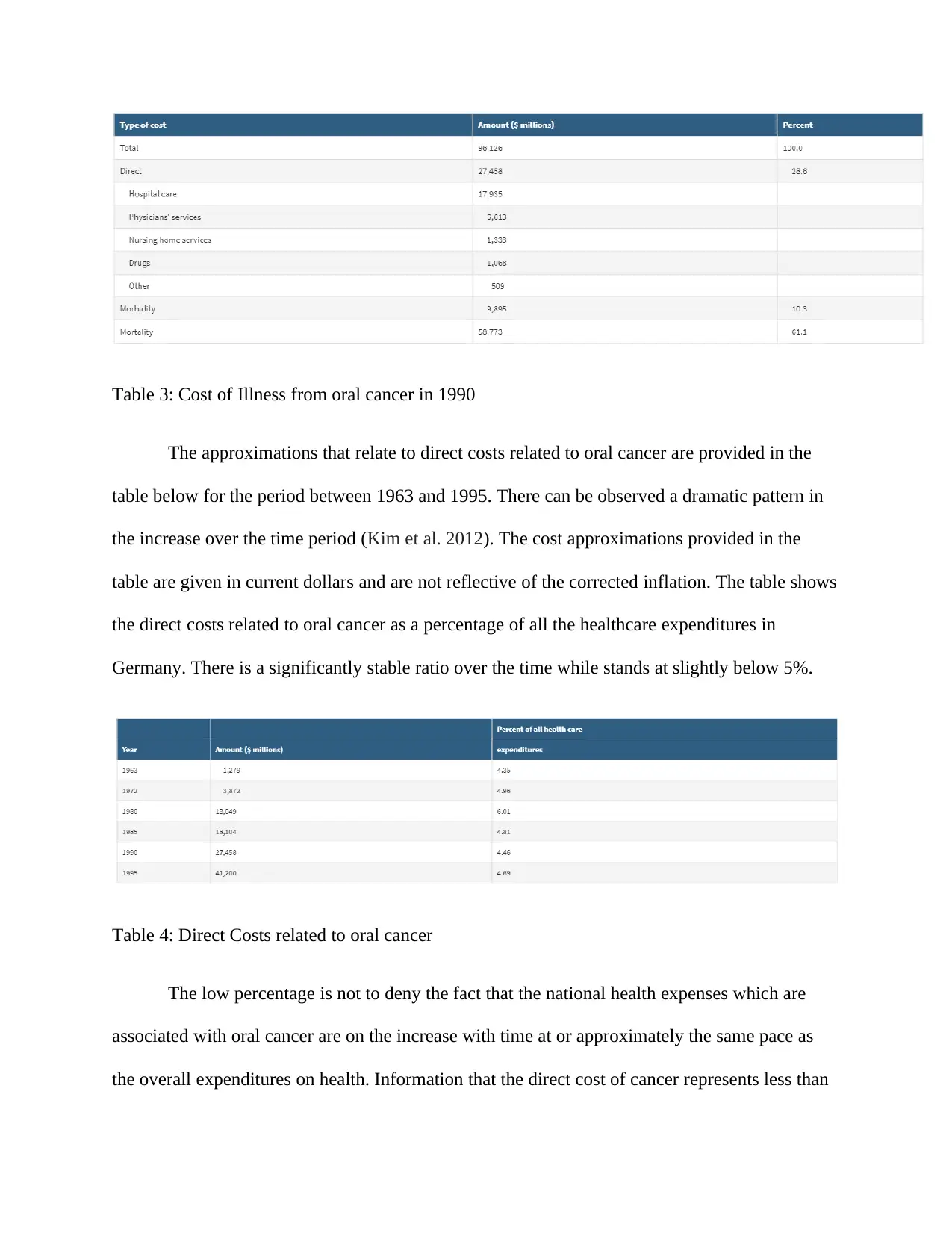
Table 3: Cost of Illness from oral cancer in 1990
The approximations that relate to direct costs related to oral cancer are provided in the
table below for the period between 1963 and 1995. There can be observed a dramatic pattern in
the increase over the time period (Kim et al. 2012). The cost approximations provided in the
table are given in current dollars and are not reflective of the corrected inflation. The table shows
the direct costs related to oral cancer as a percentage of all the healthcare expenditures in
Germany. There is a significantly stable ratio over the time while stands at slightly below 5%.
Table 4: Direct Costs related to oral cancer
The low percentage is not to deny the fact that the national health expenses which are
associated with oral cancer are on the increase with time at or approximately the same pace as
the overall expenditures on health. Information that the direct cost of cancer represents less than
The approximations that relate to direct costs related to oral cancer are provided in the
table below for the period between 1963 and 1995. There can be observed a dramatic pattern in
the increase over the time period (Kim et al. 2012). The cost approximations provided in the
table are given in current dollars and are not reflective of the corrected inflation. The table shows
the direct costs related to oral cancer as a percentage of all the healthcare expenditures in
Germany. There is a significantly stable ratio over the time while stands at slightly below 5%.
Table 4: Direct Costs related to oral cancer
The low percentage is not to deny the fact that the national health expenses which are
associated with oral cancer are on the increase with time at or approximately the same pace as
the overall expenditures on health. Information that the direct cost of cancer represents less than
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5% of the cumulative health expenditures could sound quite unrealistic since cancer, in general,
accounted for to the tune of 23% of deaths in the country, which was an increase of 6% from the
recorded values in 1973 (Heidenreich et al. 2014). Cancer, more specifically oral cancer is a
disease that mainly takes place in the late ages of a life cycle. In as much on the basis of a
person-year, the cost of medical care for oral cancer is relatively expensive in comparison with
numerous other diseases, the other conditions and diseases which do not result into death may
call for expenditure over a phase that is much more extended of the life cycle. For oral cancer
types that have high survivability, the cost related to cancer may be representative of a modest
fraction of the cost of health even for patients with a diagnosis for cancer (Kim et al. 2012).
There is also a bit of a surprise in the stability of the direct cost of oral cancer as a
fraction of all the expenditures of healthcare. Over the study period, there has been an upward
trend in the incidence of cancer and more expensive and intensive therapy techniques are being
introduced for the purposes of treatment of cancer. Nevertheless, there were as well
countervailing trends among them an enhancement in the detection of the stage cancers as a
result of the screening programs and minimized lengths of the stay in the hospital for oral cancer
treatment which could call for treatments that are less expensive (Kim et al. 2012). There is no
clarity on the actual balance of the factors that have led to the stability of the direct cost of oral
cancer as a fraction of the cumulative expenditures on health care. It would be thus of
fundamental and great interest to conduct studies touching on the long-term trends in the nature
of direct cost of oral cancer and its constituents.
accounted for to the tune of 23% of deaths in the country, which was an increase of 6% from the
recorded values in 1973 (Heidenreich et al. 2014). Cancer, more specifically oral cancer is a
disease that mainly takes place in the late ages of a life cycle. In as much on the basis of a
person-year, the cost of medical care for oral cancer is relatively expensive in comparison with
numerous other diseases, the other conditions and diseases which do not result into death may
call for expenditure over a phase that is much more extended of the life cycle. For oral cancer
types that have high survivability, the cost related to cancer may be representative of a modest
fraction of the cost of health even for patients with a diagnosis for cancer (Kim et al. 2012).
There is also a bit of a surprise in the stability of the direct cost of oral cancer as a
fraction of all the expenditures of healthcare. Over the study period, there has been an upward
trend in the incidence of cancer and more expensive and intensive therapy techniques are being
introduced for the purposes of treatment of cancer. Nevertheless, there were as well
countervailing trends among them an enhancement in the detection of the stage cancers as a
result of the screening programs and minimized lengths of the stay in the hospital for oral cancer
treatment which could call for treatments that are less expensive (Kim et al. 2012). There is no
clarity on the actual balance of the factors that have led to the stability of the direct cost of oral
cancer as a fraction of the cumulative expenditures on health care. It would be thus of
fundamental and great interest to conduct studies touching on the long-term trends in the nature
of direct cost of oral cancer and its constituents.
LIMITATIONS
The Cost of Illness method has been criticized based on numerous methodological and
conceptual grounds. A limitation of the Cost of Illness approach is its nature of mixing morbidity
cost and direct cost with a measure that is based on incidence i.e. a cost that results from an
incidence cases form diagnosis to death, mortality costs. It is possible to estimate direct costs and
morbidity cost in terms of incidence even though the data sources that were used made it
challenging to use Cost of Illness (Kim et al. 2012). There has also been criticism on the
mortality cost aspect of Cost of Illness based on various methodological and conceptual grounds.
Mortality costs are an accurate reflection of the economic costs to s society and this is
only under seriously restrictive assumptions on the costs of replacements, patterns of
employment and the trends of the labor market as projected over numerous decades into the
coming future. Mortality cost is more expansive as a tool in measuring the outcome of a disease
known as loss of life years that is often expressed in monetary terms. In as much as this entity is
very useful when it times to the economic framework of the cost-benefit analysis, it has minimal
compatibility with the cost-effective framework which has been over the past been increasingly
used for cost-benefit analysis especially in health-related issues (Kim et al. 2012).
There has been a recent development that has seen a review taxonomy of categories of
costs which has higher compatibility with the framework of cost-effectiveness and can hence be
used in the construction of economic measures of the burden of oral cancer. Such a taxonomy
incorporates direct costs just like is the case with Cost of Illness as well as acknowledging the
time costs, the care associated with the disease entity and the economic value of the time that is
spent by patients when undergoing medical treatments. Also considered as economic costs are
the production costs that are linked with loss or reduced ability to engage or work in some of the
The Cost of Illness method has been criticized based on numerous methodological and
conceptual grounds. A limitation of the Cost of Illness approach is its nature of mixing morbidity
cost and direct cost with a measure that is based on incidence i.e. a cost that results from an
incidence cases form diagnosis to death, mortality costs. It is possible to estimate direct costs and
morbidity cost in terms of incidence even though the data sources that were used made it
challenging to use Cost of Illness (Kim et al. 2012). There has also been criticism on the
mortality cost aspect of Cost of Illness based on various methodological and conceptual grounds.
Mortality costs are an accurate reflection of the economic costs to s society and this is
only under seriously restrictive assumptions on the costs of replacements, patterns of
employment and the trends of the labor market as projected over numerous decades into the
coming future. Mortality cost is more expansive as a tool in measuring the outcome of a disease
known as loss of life years that is often expressed in monetary terms. In as much as this entity is
very useful when it times to the economic framework of the cost-benefit analysis, it has minimal
compatibility with the cost-effective framework which has been over the past been increasingly
used for cost-benefit analysis especially in health-related issues (Kim et al. 2012).
There has been a recent development that has seen a review taxonomy of categories of
costs which has higher compatibility with the framework of cost-effectiveness and can hence be
used in the construction of economic measures of the burden of oral cancer. Such a taxonomy
incorporates direct costs just like is the case with Cost of Illness as well as acknowledging the
time costs, the care associated with the disease entity and the economic value of the time that is
spent by patients when undergoing medical treatments. Also considered as economic costs are
the production costs that are linked with loss or reduced ability to engage or work in some of the
most valued leisure activities in as much as over the time they have been included into the
primary analysis formally of most of the cost-effectiveness studies (Kim et al. 2012). Mortality
costs are also incorporated as part of the costs in this developed framework even though they are
trapped on the side of the outcome of the equation in the form of quality-adjusted life years.
Frictional costs are also taken into consideration in the cost side of the equation which is defined
as those related to permanent or temporary replacements of a worker who has been eliminated
from the workforce owing to mortality or morbidity. Frictional cost may be inclusive of training
costs, lowered productivity and search costs.
TREATMENT OPTIONS FOR ORAL CAVITY AND OROPHARYNGEAL
CANCER BY STAGE
The type of treatment that a medical practitioner would recommend depends on the
location of the tumor and the structure of the spread of cancer. Below are discussed a few of the
commonly used ways in the treatment of the various stages of the oral cavity and oropharyngeal
cancer. It should be noted however that each of the situations is unique and there could be
reasons offered by the medical practitioner for the adoption of a treatment option for a specific
stage (Kim et al. 2012).
Stage 0: In as much as cancer at this stage is often on the surface layer and thus has not
begun growing into the deeper layers of tissues, it has the potential to do so if it is not treated.
The treatment option that is commonly used here is surgery, in most cases Mohs surgery, thin
resection or even surgical stripping which is done to remove the layers of tissue at the topmost
alongside a small margin that contains normal tissues. There is a need to perform a close follow
up to a bid to check on any signs that could be indicative of the reoccurrence of cancer.
primary analysis formally of most of the cost-effectiveness studies (Kim et al. 2012). Mortality
costs are also incorporated as part of the costs in this developed framework even though they are
trapped on the side of the outcome of the equation in the form of quality-adjusted life years.
Frictional costs are also taken into consideration in the cost side of the equation which is defined
as those related to permanent or temporary replacements of a worker who has been eliminated
from the workforce owing to mortality or morbidity. Frictional cost may be inclusive of training
costs, lowered productivity and search costs.
TREATMENT OPTIONS FOR ORAL CAVITY AND OROPHARYNGEAL
CANCER BY STAGE
The type of treatment that a medical practitioner would recommend depends on the
location of the tumor and the structure of the spread of cancer. Below are discussed a few of the
commonly used ways in the treatment of the various stages of the oral cavity and oropharyngeal
cancer. It should be noted however that each of the situations is unique and there could be
reasons offered by the medical practitioner for the adoption of a treatment option for a specific
stage (Kim et al. 2012).
Stage 0: In as much as cancer at this stage is often on the surface layer and thus has not
begun growing into the deeper layers of tissues, it has the potential to do so if it is not treated.
The treatment option that is commonly used here is surgery, in most cases Mohs surgery, thin
resection or even surgical stripping which is done to remove the layers of tissue at the topmost
alongside a small margin that contains normal tissues. There is a need to perform a close follow
up to a bid to check on any signs that could be indicative of the reoccurrence of cancer.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
There may also be a need to treat carcinoma which keeping recurring after the surgery
and this can be achieved through radiation therapy. Almost everyone with stage 0 oral cancer
have a long time of survival without necessarily having to go through elaborate and more intense
treatment. It is of importance to retaliate that continued smoking enhances the risk of the
development of new cancer.
Stages I and II: Most of the victims of this stage of cancer have been noticed to do well
when subject to treated with oral therapy and/or surgery- Another option that may also be
considered is chemotherapy that is offered alongside radiation which may be used alone even
though in most cases it is done after a surgical procedure and aimed at the treatment of any
cancer cells that might have by chance been left behind. Both radiation and surgery are ideal
procedures in the treatment of these two stages of oral cancer and the choice of an option would
be influenced by the preferences of a patient as well as the anticipated side effects such as the
effects of the treatment ion the look of the patient and how he would speak and swallow (Kim et
al. 2012).
Lip: In the lips, the surgical procedure is usually preferred in the elimination of small
cancers which can be eliminated. Radiation on its own may be adopted as the first treatments
which may call for surgery at later stages should radiation fail to eliminate the tumor completely.
Larger or deeper concern, on the other hand, calls for the need of surgery. Under circumstances
of demand, reconstructive surgery may be used in the correction of the defects in the lips.
A thick tumor enhances the risk of the spread of the tumor to the lymph nodes that are
found on the neck and hence the need of their removal by the surgeon through a process called
lymph node dissection to enable checking for the spread of cancer.
and this can be achieved through radiation therapy. Almost everyone with stage 0 oral cancer
have a long time of survival without necessarily having to go through elaborate and more intense
treatment. It is of importance to retaliate that continued smoking enhances the risk of the
development of new cancer.
Stages I and II: Most of the victims of this stage of cancer have been noticed to do well
when subject to treated with oral therapy and/or surgery- Another option that may also be
considered is chemotherapy that is offered alongside radiation which may be used alone even
though in most cases it is done after a surgical procedure and aimed at the treatment of any
cancer cells that might have by chance been left behind. Both radiation and surgery are ideal
procedures in the treatment of these two stages of oral cancer and the choice of an option would
be influenced by the preferences of a patient as well as the anticipated side effects such as the
effects of the treatment ion the look of the patient and how he would speak and swallow (Kim et
al. 2012).
Lip: In the lips, the surgical procedure is usually preferred in the elimination of small
cancers which can be eliminated. Radiation on its own may be adopted as the first treatments
which may call for surgery at later stages should radiation fail to eliminate the tumor completely.
Larger or deeper concern, on the other hand, calls for the need of surgery. Under circumstances
of demand, reconstructive surgery may be used in the correction of the defects in the lips.
A thick tumor enhances the risk of the spread of the tumor to the lymph nodes that are
found on the neck and hence the need of their removal by the surgeon through a process called
lymph node dissection to enable checking for the spread of cancer.
Oral cavity: Surgery tends to be the main treatment option for that cancer of the front of
the tongue, gums, hard palate, floor of the mouth, inside of the cheeks. In this case, the lymph
nodes found on the neck may also be removed through lymph node dissection so as to enable a
check for the spread of cancer. Should it appear like the process of removal of the cancer cells
has not been done to completion or there are high risks of recurrence of the cancer cells
following a check of the nature of cancer as observed under a microscope, then radiation that I
mostly combined with chemo may be introduced (Cheema et al. 2012). Nevertheless, radiation
may also be adopted in place of surgery as the main treatment option in some patients, especially
among those who are unable to undergo surgery following other medical complications or
challenges.
Oropharynx: Radiation therapy geared toward cancer and the lymph nodes of the neck is
the main treatment option for cancer of the soft palate, back of the tongue and tonsils. Surgery
may also be adopted as the main treatment option instead of radiation and would be inclusive of
the removal of the lymph nodes in the neck. Any remains of cancer are eliminated through
chemoradiation.
Stages III, IV, IVA
Oropharyngeal cancers: These include cancers found in the soft palate, back of the tongue
and the tonsils which are in these stage larger cancers and have grown into the surrounding
tissues besides having spread to the nearby lymph nodes found in the neck. Such cancers are
mostly treated with, however, radiation and cetuximab are also applicable in certain cases
(Cheema et al. 2012). There are also going on studies on the impact of a combination of radiation
and both cetuximab and chemo. A surgical procedure is used for the removal of any cancer that
the tongue, gums, hard palate, floor of the mouth, inside of the cheeks. In this case, the lymph
nodes found on the neck may also be removed through lymph node dissection so as to enable a
check for the spread of cancer. Should it appear like the process of removal of the cancer cells
has not been done to completion or there are high risks of recurrence of the cancer cells
following a check of the nature of cancer as observed under a microscope, then radiation that I
mostly combined with chemo may be introduced (Cheema et al. 2012). Nevertheless, radiation
may also be adopted in place of surgery as the main treatment option in some patients, especially
among those who are unable to undergo surgery following other medical complications or
challenges.
Oropharynx: Radiation therapy geared toward cancer and the lymph nodes of the neck is
the main treatment option for cancer of the soft palate, back of the tongue and tonsils. Surgery
may also be adopted as the main treatment option instead of radiation and would be inclusive of
the removal of the lymph nodes in the neck. Any remains of cancer are eliminated through
chemoradiation.
Stages III, IV, IVA
Oropharyngeal cancers: These include cancers found in the soft palate, back of the tongue
and the tonsils which are in these stage larger cancers and have grown into the surrounding
tissues besides having spread to the nearby lymph nodes found in the neck. Such cancers are
mostly treated with, however, radiation and cetuximab are also applicable in certain cases
(Cheema et al. 2012). There are also going on studies on the impact of a combination of radiation
and both cetuximab and chemo. A surgical procedure is used for the removal of any cancer that
might have remained after chemoradiation. In cases where cancer has spread to the lymph nodes,
lymph node dissection is done to remove them just after conducting chemoradiation.
Another option that may be adopted for this case is first treating using surgery that would
remove the lymph nodes in the neck and cancer. This is then closely followed by chemoradiation
or radiation that is meant to lower the chancer of recurrence of cancer (Cheema et al. 2012).
Again, in this stage, the treatment choice is a factor of the location of cancer, the extent of its
spread at the time of treatment, the preferences of the patient, the anticipated side effects and
even the current health status of the patient. Some doctors may opt to provide chemo as the
initial treatment and then follow it using chemoradiation and thereafter surgery should there need
be. This is not to the agreement of all the doctors though.
Stages IV B and IV C: These stages involve the treatment of HPV-negative cancers,
which at the time of treatment have successfully spread into the surrounding tissues, lymph
nodes, and structures. Stage IV C cancers have even spread to the other various parts of the body
including the lungs. The treatment option that may be used in handling these cancers includes
chemo, cetuximab or even both (Cheema et al. 2012). Radiation among other treatment options
are also applicable and may be used in helping to relive the symptoms resulting from cancer or
even aid in the prevention of new problems.
Research and studies are on-going to establish the various ways through which a
combination of radiation and chemo may be carried out in the presence or absence of cetuximab
or any other new agents aimed at the improvement in the quality of life and chances of survival
as well as minimizing the need for a deforming radical surgical procedure in the treatment of
such advanced cancers in the throat and the mouth.
lymph node dissection is done to remove them just after conducting chemoradiation.
Another option that may be adopted for this case is first treating using surgery that would
remove the lymph nodes in the neck and cancer. This is then closely followed by chemoradiation
or radiation that is meant to lower the chancer of recurrence of cancer (Cheema et al. 2012).
Again, in this stage, the treatment choice is a factor of the location of cancer, the extent of its
spread at the time of treatment, the preferences of the patient, the anticipated side effects and
even the current health status of the patient. Some doctors may opt to provide chemo as the
initial treatment and then follow it using chemoradiation and thereafter surgery should there need
be. This is not to the agreement of all the doctors though.
Stages IV B and IV C: These stages involve the treatment of HPV-negative cancers,
which at the time of treatment have successfully spread into the surrounding tissues, lymph
nodes, and structures. Stage IV C cancers have even spread to the other various parts of the body
including the lungs. The treatment option that may be used in handling these cancers includes
chemo, cetuximab or even both (Cheema et al. 2012). Radiation among other treatment options
are also applicable and may be used in helping to relive the symptoms resulting from cancer or
even aid in the prevention of new problems.
Research and studies are on-going to establish the various ways through which a
combination of radiation and chemo may be carried out in the presence or absence of cetuximab
or any other new agents aimed at the improvement in the quality of life and chances of survival
as well as minimizing the need for a deforming radical surgical procedure in the treatment of
such advanced cancers in the throat and the mouth.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Recurrent mouth cancer: Recurrent cancer refers to cancer that comes back after
treatment. Recurrence may be local, regional or even distant. Local recurrence is where cancer
comes back on or close to the same place it first started while regional recurrence defines cancer
that comes back in the surrounding lymph nodes (Cheema et al. 2012). Distant recurrence, on the
other hand, defines that cancer that spreads to other organs of the body including bones or lungs.
The size of cancer, the general health of the patient, location of cancer and the previously
adopted treatments are the main determinants of the treatment options for use in recurrent
cancers.
Should cancer recur on the same area and the first treatment that was adopted being
radiation therapy, then surgery would be adopted as the next treatment option should there be a
possibility to completely remove cancer and the health of the patient permits surgical procedures.
In most cases, it is not possible to have a repeat of external beam radiation therapy on the same
site except for special cases. It is, however, possible to perform internal radiation in the control
of cancer should it recur on the very place of beginning (Cheema et al. 2012). More surgery,
cetuximab, radiotherapy or their combination may be adopted in cases where surgery was the
first treatment option.
If cancer recurs in the lymph nodes found in the neck, they would be eliminated through
lymph node dissection which would then be followed by radiation. In cases where the recurrence
is distant, cetuximab and/or chemo are preferred as they have the potential to shrink or lower the
rate of growth of some of the cancers for some time and aid in the removal of symptoms even
though such cancers are very hard to be treated. In cases where chemo is working no more, an
immunotherapy drug may be used as a new treatment option (Cheema et al. 2012). Examples of
treatment. Recurrence may be local, regional or even distant. Local recurrence is where cancer
comes back on or close to the same place it first started while regional recurrence defines cancer
that comes back in the surrounding lymph nodes (Cheema et al. 2012). Distant recurrence, on the
other hand, defines that cancer that spreads to other organs of the body including bones or lungs.
The size of cancer, the general health of the patient, location of cancer and the previously
adopted treatments are the main determinants of the treatment options for use in recurrent
cancers.
Should cancer recur on the same area and the first treatment that was adopted being
radiation therapy, then surgery would be adopted as the next treatment option should there be a
possibility to completely remove cancer and the health of the patient permits surgical procedures.
In most cases, it is not possible to have a repeat of external beam radiation therapy on the same
site except for special cases. It is, however, possible to perform internal radiation in the control
of cancer should it recur on the very place of beginning (Cheema et al. 2012). More surgery,
cetuximab, radiotherapy or their combination may be adopted in cases where surgery was the
first treatment option.
If cancer recurs in the lymph nodes found in the neck, they would be eliminated through
lymph node dissection which would then be followed by radiation. In cases where the recurrence
is distant, cetuximab and/or chemo are preferred as they have the potential to shrink or lower the
rate of growth of some of the cancers for some time and aid in the removal of symptoms even
though such cancers are very hard to be treated. In cases where chemo is working no more, an
immunotherapy drug may be used as a new treatment option (Cheema et al. 2012). Examples of
such drugs include nivolumab or pembrolizumab which help in building the immunity system of
the body against attacks from cancer.
DIAGNOSIS AND TREATMENT OF ORAL CANCER
Diagnosis
Various tests and procedures are used in the diagnosis of mouth cancer:
Tissue removal and testing: A sample of cells may be removed from a suspected area for
laboratory testing by a procedure called biopsy. Various techniques can be adopted in the
removal of unusual cells but are in most cases cut away with the aid of a scalpel, scissors or any
other relevant tool. During testing, and analysis is done on the cells for any precancerous
changes would be indicative of the risk of future cancer or cancer itself.
Stages of Mouth Cancer
As soon as the mouth is diagnosed, an analysis is done to establish the degree or the stage
of the mouth cancer. The tests for cancer staging include:
Imaging tests: Numerous imaging tests may be used in establishing if cancer has spread
to other regions beyond the mouth (Heidenreich et al. 2014). Among the imaging tests may be
inclusive of magnetic resonance, computerized tomography scans, X-rays and positron emission
tomography.
A small camera for inspection of the throat: During an endoscopy procedure, a small
flexible camera that has light may be passed through the nose to evaluate the voice box and the
throat. In so doing, any signs of cancer that have spread beyond the mouth are established.
the body against attacks from cancer.
DIAGNOSIS AND TREATMENT OF ORAL CANCER
Diagnosis
Various tests and procedures are used in the diagnosis of mouth cancer:
Tissue removal and testing: A sample of cells may be removed from a suspected area for
laboratory testing by a procedure called biopsy. Various techniques can be adopted in the
removal of unusual cells but are in most cases cut away with the aid of a scalpel, scissors or any
other relevant tool. During testing, and analysis is done on the cells for any precancerous
changes would be indicative of the risk of future cancer or cancer itself.
Stages of Mouth Cancer
As soon as the mouth is diagnosed, an analysis is done to establish the degree or the stage
of the mouth cancer. The tests for cancer staging include:
Imaging tests: Numerous imaging tests may be used in establishing if cancer has spread
to other regions beyond the mouth (Heidenreich et al. 2014). Among the imaging tests may be
inclusive of magnetic resonance, computerized tomography scans, X-rays and positron emission
tomography.
A small camera for inspection of the throat: During an endoscopy procedure, a small
flexible camera that has light may be passed through the nose to evaluate the voice box and the
throat. In so doing, any signs of cancer that have spread beyond the mouth are established.

Treatment
Radiation therapy
Radiation therapy makes use of beams of very high energy including X-rays and protons
in the killing of the cells that cause oral cancer. This treatment method is in most cases derived
from a machine that is placed outside the human body (external beam radiation). The beams may
also be derived from wires and radiative seeds that are put near cancer (Cheema et al. 2012).
Radiation therapy could be the only treatment receivable when an individual has oral
cancer that is still in its early stages. It may also be deployed after surgery. In some special cases,
radiation therapy is done in conjunction with chemotherapy. Such a conjunction leads to
increased effectiveness of the radiation therapy despite as well increasing the anticipated side
effects (Heidenreich et al. 2014). Radiation therapy has been found to be capable of relieving the
signs and symptoms that are caused by oral cancer among them a pain in the cases of advanced
mouth cancer.
Among the side effects of radiation therapy to the mouth include
Sores in the mouth
Bleeding of the gums
Tooth decay
Dry mouth
Damages to the bones of the jaw
The stiffness of the jaws
Burn like skin reactions that are fatigue and red
Surgery
Mouth cancer surgery may be inclusive of:
Radiation therapy
Radiation therapy makes use of beams of very high energy including X-rays and protons
in the killing of the cells that cause oral cancer. This treatment method is in most cases derived
from a machine that is placed outside the human body (external beam radiation). The beams may
also be derived from wires and radiative seeds that are put near cancer (Cheema et al. 2012).
Radiation therapy could be the only treatment receivable when an individual has oral
cancer that is still in its early stages. It may also be deployed after surgery. In some special cases,
radiation therapy is done in conjunction with chemotherapy. Such a conjunction leads to
increased effectiveness of the radiation therapy despite as well increasing the anticipated side
effects (Heidenreich et al. 2014). Radiation therapy has been found to be capable of relieving the
signs and symptoms that are caused by oral cancer among them a pain in the cases of advanced
mouth cancer.
Among the side effects of radiation therapy to the mouth include
Sores in the mouth
Bleeding of the gums
Tooth decay
Dry mouth
Damages to the bones of the jaw
The stiffness of the jaws
Burn like skin reactions that are fatigue and red
Surgery
Mouth cancer surgery may be inclusive of:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Surgery for reconstructing the mouth: This is a surgery performed after an operation
done to remove cancer and is aimed at rebuilding the mouth to restore it back to its ability to eat
and talk. It may include transplant of grafts of skin, bone or muscles from another part of the
body. Natural teeth may be replaced with dental implants. The implants may be introduced at the
time of treatment of cancer or upon healing.
Surgery to eliminate tumor: This involves cutting away cancer and a small section of
the healthy tissue that surrounds cancer to ascertain that all the cancer cells have been eliminated.
Minor surgery may be removed in the removal of smaller cancers whole larger cancers may call
upon the need for more extensive sophisticated procedures (Cheema et al. 2012).
Surgery for the removal of cancer that has spread to the neck: A procedure may be
recommended for the removal of the cancerous lymph nodes should the cancer cells spread to the
lymph nodes found in the neck or in cases where such chances are deemed to be high. This
procedure is called neck dissection and helps in the removal of any cancer-causing cells that
might have found their way to the lymph nodes (Cheema et al. 2012). A scar is left on the neck
after neck dissection even though it has no effect on the body with regarding fighting infections.
Among the risks associated with surgical procedures are infection and bleeding. Still,
surgeries for oral cancer usually interfere with the appearance besides the ability of an individual
to swallow, eat and speak. This may lead to the need for a tube in helping the individual to eat,
take drugs and drink. Such tubes may be inserted through the nose and get into the stomach for
short-term use. In the case of long-term uses, the tube may be driven into the body through the
skin into the stomach (Heidenreich et al. 2014). A procedure may also be needed in the insertion
of a breathing tube through the neck which is often temporary.
done to remove cancer and is aimed at rebuilding the mouth to restore it back to its ability to eat
and talk. It may include transplant of grafts of skin, bone or muscles from another part of the
body. Natural teeth may be replaced with dental implants. The implants may be introduced at the
time of treatment of cancer or upon healing.
Surgery to eliminate tumor: This involves cutting away cancer and a small section of
the healthy tissue that surrounds cancer to ascertain that all the cancer cells have been eliminated.
Minor surgery may be removed in the removal of smaller cancers whole larger cancers may call
upon the need for more extensive sophisticated procedures (Cheema et al. 2012).
Surgery for the removal of cancer that has spread to the neck: A procedure may be
recommended for the removal of the cancerous lymph nodes should the cancer cells spread to the
lymph nodes found in the neck or in cases where such chances are deemed to be high. This
procedure is called neck dissection and helps in the removal of any cancer-causing cells that
might have found their way to the lymph nodes (Cheema et al. 2012). A scar is left on the neck
after neck dissection even though it has no effect on the body with regarding fighting infections.
Among the risks associated with surgical procedures are infection and bleeding. Still,
surgeries for oral cancer usually interfere with the appearance besides the ability of an individual
to swallow, eat and speak. This may lead to the need for a tube in helping the individual to eat,
take drugs and drink. Such tubes may be inserted through the nose and get into the stomach for
short-term use. In the case of long-term uses, the tube may be driven into the body through the
skin into the stomach (Heidenreich et al. 2014). A procedure may also be needed in the insertion
of a breathing tube through the neck which is often temporary.
Targeted drug therapy
Targeted drugs work by changing the specific aspects of the cancer cells which facilitate
their growth hence treating oral cancer. Cetuximab is one such targeted therapy that has been
approved for use in the treatment of neck and head cancers in some situations (Cheema et al.
2012). Cetuximab works by halting the action of a protein that is found in numerous types of
healthy cells but is more common in some types of cancer cells. Targeted drugs may be used
when combined with radiation therapy or chemotherapy. Studies and research are still on-going
to establish more targeted drugs through clinical trials among them those drugs whose target is
the immune system.
Chemotherapy
This is a treatment option that makes use of chemicals in the kills of cancer cells.
Chemotherapy drugs may be administered alone, in combination with other treatments of cancer
and or even with other drugs for chemotherapy. Due to an increase in the effectiveness of
radiation therapy, the two treatment methods are often combined (Heidenreich et al. 2014). The
type of drugs received during chemotherapy determines the side effects. Among the common
side effects include vomiting, loss of hair and nausea.
PREVENTION OF ORAL CANCER
Quit tobacco smoking: There is a very close link between oral cancer and tobacco
smoking of any forms including cigars, pipes, snuff, cigarettes and chewing tobacco. Tobacco
has the following impacts:
Targeted drugs work by changing the specific aspects of the cancer cells which facilitate
their growth hence treating oral cancer. Cetuximab is one such targeted therapy that has been
approved for use in the treatment of neck and head cancers in some situations (Cheema et al.
2012). Cetuximab works by halting the action of a protein that is found in numerous types of
healthy cells but is more common in some types of cancer cells. Targeted drugs may be used
when combined with radiation therapy or chemotherapy. Studies and research are still on-going
to establish more targeted drugs through clinical trials among them those drugs whose target is
the immune system.
Chemotherapy
This is a treatment option that makes use of chemicals in the kills of cancer cells.
Chemotherapy drugs may be administered alone, in combination with other treatments of cancer
and or even with other drugs for chemotherapy. Due to an increase in the effectiveness of
radiation therapy, the two treatment methods are often combined (Heidenreich et al. 2014). The
type of drugs received during chemotherapy determines the side effects. Among the common
side effects include vomiting, loss of hair and nausea.
PREVENTION OF ORAL CANCER
Quit tobacco smoking: There is a very close link between oral cancer and tobacco
smoking of any forms including cigars, pipes, snuff, cigarettes and chewing tobacco. Tobacco
has the following impacts:
Reducing the efficiency of treatment of oral cancer
Making it difficult for the body to heal after a surgical procedure
Enhances the risk of recurrence of cancer and contracting another cancer in the future
Despite it being a challenge to quit smoking, it is even more stressful and harder to cope with
complicated medical conditions like oral cancer, diagnosis, and treatment (Heidenreich et al.
2014).
Quit consumption of alcohol: A combination of alcohol and the use of tobacco
especially offer the highly enhanced risk of oral cancer. Quitting drinking alcohol has the ability
to lower the risk of second cancer. Still, quitting drinking may as well facilitate better tolerance
with the treatment of mouth cancer.
Alternative medicine
There have not been established any alternative or complementary treatments for the cure of
mouth cancer. Complementary and alternative medicine treatments instead aid in coming up with
the mouth cancer and the accompanying side effects of the treatment of cancer for example
fatigue. Most of the patients undergoing radiation theory for the treatment of cancer are likely to
experience fatigue. This could be accompanied by a feeling of been worn out completely that is
persistent even though there are treatments on-going (Heidenreich et al. 2014). The use of
complementary therapies may play a role in helping to cope up with the fatigue.
Coping and support techniques
Share with other survivors of oral cancer
Have time for yourself
Learn exhaustively on mouth cancer to enable decision making on the treatment option
Making it difficult for the body to heal after a surgical procedure
Enhances the risk of recurrence of cancer and contracting another cancer in the future
Despite it being a challenge to quit smoking, it is even more stressful and harder to cope with
complicated medical conditions like oral cancer, diagnosis, and treatment (Heidenreich et al.
2014).
Quit consumption of alcohol: A combination of alcohol and the use of tobacco
especially offer the highly enhanced risk of oral cancer. Quitting drinking alcohol has the ability
to lower the risk of second cancer. Still, quitting drinking may as well facilitate better tolerance
with the treatment of mouth cancer.
Alternative medicine
There have not been established any alternative or complementary treatments for the cure of
mouth cancer. Complementary and alternative medicine treatments instead aid in coming up with
the mouth cancer and the accompanying side effects of the treatment of cancer for example
fatigue. Most of the patients undergoing radiation theory for the treatment of cancer are likely to
experience fatigue. This could be accompanied by a feeling of been worn out completely that is
persistent even though there are treatments on-going (Heidenreich et al. 2014). The use of
complementary therapies may play a role in helping to cope up with the fatigue.
Coping and support techniques
Share with other survivors of oral cancer
Have time for yourself
Learn exhaustively on mouth cancer to enable decision making on the treatment option
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Maintain closeness with the family and friends
CONCLUSION
A multifaceted approach that incorporates control of alcohol and tobacco, early
treatments, health education and detection are among the strategies that are most vital in the
reduction of the burden of this evidently preventable type of cancer. The modalities of
accomplishing such are known and have surprisingly been applied in some of the countries in
which it has been successful even though not at all in the countries that tend to be of the highest
burden.
The critical most important oral control measures include improved awareness among the
public on the primary and public care practitioners, provision of suffice treatment to people
diagnosed with oral cancer and enhancing the investments on the healthcare services which offer
early-stage diagnosis and screening services. Most of the health care centers are not fully
equipped with term imaging, cancer surgery, radiotherapy infrastructure, histopathology, trained
personnel, optimum treatment as well as the availability of the agents of chemotherapy. These
have seen serious comprise and delays in the early detections as well as optimum treatment of
oral cancer.
REFERENCES
Alkureishi, L. W., Ross, G. L., Shoaib, T., Soutar, D. S., Robertson, A. G., Thompson, R., ... &
Alvarez, J. (2010). Sentinel node biopsy in head and neck squamous cell cancer: 5-year
follow-up of a European multicenter trial. Annals of surgical oncology, 17(9), 2459-2464
CONCLUSION
A multifaceted approach that incorporates control of alcohol and tobacco, early
treatments, health education and detection are among the strategies that are most vital in the
reduction of the burden of this evidently preventable type of cancer. The modalities of
accomplishing such are known and have surprisingly been applied in some of the countries in
which it has been successful even though not at all in the countries that tend to be of the highest
burden.
The critical most important oral control measures include improved awareness among the
public on the primary and public care practitioners, provision of suffice treatment to people
diagnosed with oral cancer and enhancing the investments on the healthcare services which offer
early-stage diagnosis and screening services. Most of the health care centers are not fully
equipped with term imaging, cancer surgery, radiotherapy infrastructure, histopathology, trained
personnel, optimum treatment as well as the availability of the agents of chemotherapy. These
have seen serious comprise and delays in the early detections as well as optimum treatment of
oral cancer.
REFERENCES
Alkureishi, L. W., Ross, G. L., Shoaib, T., Soutar, D. S., Robertson, A. G., Thompson, R., ... &
Alvarez, J. (2010). Sentinel node biopsy in head and neck squamous cell cancer: 5-year
follow-up of a European multicenter trial. Annals of surgical oncology, 17(9), 2459-2464
Anderson, K. N., Schwab, R. B., & Martinez, M. E. (2014). Reproductive risk factors and breast
cancer subtypes: a review of the literature. Breast cancer research and
treatment, 144(1), 1-10
Audeh, M. W., Carmichael, J., Penson, R. T., Friedlander, M., Powell, B., Bell-McGuinn, K. M.,
... & Lu, K. (2010). Oral poly (ADP-ribose) polymerase inhibitor olaparib in patients
with BRCA1 or BRCA2 mutations and recurrent ovarian cancer: a proof-of-concept
trial. The Lancet, 376(9737), 245-251
Blomberg, M., Nielsen, A., Munk, C., & Kjaer, S. K. (2011). Trends in head and neck cancer
incidence in Denmark, 1978–2007: focus on human papillomavirus-associated sites.
International Journal of Cancer, 129(3), 733-741
Brailo, V., Vucicevic-Boras, V., Lukac, J., Biocina-Lukenda, D., Zilic-Alajbeg, I., Milenovic,
A., & Balija, M. (2012). Salivary and serum interleukin 1 beta, interleukin 6 and tumor
necrosis factor alpha in patients with leukoplakia and oral cancer. Medicine oral,
patología oral y cirugía buccal, 17(1), e10
Chaturvedi, A. K., Engels, E. A., Pfeiffer, R. M., Hernandez, B. Y., Xiao, W., Kim, E., ... & Liu,
L. (2011). Human papillomavirus and rising oropharyngeal cancer incidence in the
United States. Journal of clinical oncology, 29(32), 4294
Cheema, P. K., Gavura, S., Migus, M., Godman, B., Yeung, L., & Trudeau, M. E. (2012).
International variability in the reimbursement of cancer drugs by publically funded drug
programs. Current oncology, 19(3), e165
Coelho, K. R. (2012). Challenges of the oral cancer burden in India. Journal of cancer
epidemiology, 2012
cancer subtypes: a review of the literature. Breast cancer research and
treatment, 144(1), 1-10
Audeh, M. W., Carmichael, J., Penson, R. T., Friedlander, M., Powell, B., Bell-McGuinn, K. M.,
... & Lu, K. (2010). Oral poly (ADP-ribose) polymerase inhibitor olaparib in patients
with BRCA1 or BRCA2 mutations and recurrent ovarian cancer: a proof-of-concept
trial. The Lancet, 376(9737), 245-251
Blomberg, M., Nielsen, A., Munk, C., & Kjaer, S. K. (2011). Trends in head and neck cancer
incidence in Denmark, 1978–2007: focus on human papillomavirus-associated sites.
International Journal of Cancer, 129(3), 733-741
Brailo, V., Vucicevic-Boras, V., Lukac, J., Biocina-Lukenda, D., Zilic-Alajbeg, I., Milenovic,
A., & Balija, M. (2012). Salivary and serum interleukin 1 beta, interleukin 6 and tumor
necrosis factor alpha in patients with leukoplakia and oral cancer. Medicine oral,
patología oral y cirugía buccal, 17(1), e10
Chaturvedi, A. K., Engels, E. A., Pfeiffer, R. M., Hernandez, B. Y., Xiao, W., Kim, E., ... & Liu,
L. (2011). Human papillomavirus and rising oropharyngeal cancer incidence in the
United States. Journal of clinical oncology, 29(32), 4294
Cheema, P. K., Gavura, S., Migus, M., Godman, B., Yeung, L., & Trudeau, M. E. (2012).
International variability in the reimbursement of cancer drugs by publically funded drug
programs. Current oncology, 19(3), e165
Coelho, K. R. (2012). Challenges of the oral cancer burden in India. Journal of cancer
epidemiology, 2012
De Souza Setubal Destro, M. F., Bitu, C. C., Zecchin, K. G., Graner, E., Lopes, M. A., Kowalski,
L. P., & Coletta, R. D. (2010). Overexpression of HOXB7 homeobox gene in oral cancer
induces cellular proliferation and is associated with poor prognosis. International
journal of oncology, 36(1), 141-149
Denis, C., Fatseas, M., Lavie, E., & Auriacombe, M. (2017). Pharmacological interventions for
benzodiazepine mono-dependence management in outpatient settings (withdrawn
review). Cancer
Edwards, B. K., Noone, A. M., Mariotto, A. B., Simard, E. P., Boscoe, F. P., Henley, S. J., ... &
Eheman, C. R. (2014). Annual Report to the Nation on the status of cancer, 1975‐2010,
featuring prevalence of comorbidity and impact on survival among persons with lung,
colorectal, breast, or prostate cancer. Cancer, 120(9), 1290-1314
Finch, A. P., Lubinski, J., Møller, P., Singer, C. F., Karlan, B., Senter, L., ... & Huzarski, T.
(2014). Impact of oophorectomy on cancer incidence and mortality in women with a
BRCA1 or BRCA2 mutation. Journal of Clinical Oncology, 32(15), 1547
Fitzmaurice, C., Allen, C., Barber, R. M., Barregard, L., Bhutta, Z. A., Brenner, H., ... &
Fleming, T. (2017). Global, regional, and national cancer incidence, mortality, years of
life lost, years lived with disability, and disability-adjusted life-years for 32 cancer
groups, 1990 to 2015: a systematic analysis for the global burden of disease study. JAMA
oncology, 3(4), 524-548
Friedrich, R. E. (2010). Delay in diagnosis and referral patterns of 646 patients with oral and
maxillofacial cancer: a report from a single institution in Hamburg,
Germany. Anticancer research, 30(5), 1833-1836
Garavello, W., Bertuccio, P., Levi, F., Lucchini, F., Bosetti, C., Malvezzi, M., ... & La Vecchia,
C. (2010). The oral cancer epidemic in central and eastern Europe. International journal
of cancer, 127(1), 160-171
L. P., & Coletta, R. D. (2010). Overexpression of HOXB7 homeobox gene in oral cancer
induces cellular proliferation and is associated with poor prognosis. International
journal of oncology, 36(1), 141-149
Denis, C., Fatseas, M., Lavie, E., & Auriacombe, M. (2017). Pharmacological interventions for
benzodiazepine mono-dependence management in outpatient settings (withdrawn
review). Cancer
Edwards, B. K., Noone, A. M., Mariotto, A. B., Simard, E. P., Boscoe, F. P., Henley, S. J., ... &
Eheman, C. R. (2014). Annual Report to the Nation on the status of cancer, 1975‐2010,
featuring prevalence of comorbidity and impact on survival among persons with lung,
colorectal, breast, or prostate cancer. Cancer, 120(9), 1290-1314
Finch, A. P., Lubinski, J., Møller, P., Singer, C. F., Karlan, B., Senter, L., ... & Huzarski, T.
(2014). Impact of oophorectomy on cancer incidence and mortality in women with a
BRCA1 or BRCA2 mutation. Journal of Clinical Oncology, 32(15), 1547
Fitzmaurice, C., Allen, C., Barber, R. M., Barregard, L., Bhutta, Z. A., Brenner, H., ... &
Fleming, T. (2017). Global, regional, and national cancer incidence, mortality, years of
life lost, years lived with disability, and disability-adjusted life-years for 32 cancer
groups, 1990 to 2015: a systematic analysis for the global burden of disease study. JAMA
oncology, 3(4), 524-548
Friedrich, R. E. (2010). Delay in diagnosis and referral patterns of 646 patients with oral and
maxillofacial cancer: a report from a single institution in Hamburg,
Germany. Anticancer research, 30(5), 1833-1836
Garavello, W., Bertuccio, P., Levi, F., Lucchini, F., Bosetti, C., Malvezzi, M., ... & La Vecchia,
C. (2010). The oral cancer epidemic in central and eastern Europe. International journal
of cancer, 127(1), 160-171
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Gomes, B., Higginson, I. J., Calanzani, N., Cohen, J., Deliens, L., Daveson, B. A., ... & Meñaca,
A. (2012). Preferences for place of death if faced with advanced cancer: a population
survey in England, Flanders, Germany, Italy, the Netherlands, Portugal, and Spain.
Annals of Oncology, 23(8), 2006-2015
Guntinas-Lichius, O., Wendt, T., Buentzel, J., Esser, D., Lochner, P., Mueller, A., ... &
Altendorf-Hofmann, A. (2010). Head and neck cancer in Germany: a site-specific
analysis of survival of the Thuringian cancer registration database. Journal of cancer
research and clinical oncology, 136(1), 55-63
Heidenreich, A., Bastian, P. J., Bellmunt, J., Bolla, M., Joniau, S., van der Kwast, T., ... &
Mottet, N. (2014). EAU guidelines on prostate cancer. Part 1: screening, diagnosis, and
local treatment with curative intent—update 2013. European Urology, 65(1), 124-137.
Hensel, M., Goetzenich, A., Lutz, T., Stoehr, A., Moll, A., Rockstroh, J., ... & Mosthaf, F.
(2011). HIV and cancer in Germany. Deutsches Ärzteblatt International, 108(8), 117
Hertrampf, K., Wenz, H. J., Koller, M., & Wiltfang, J. (2012). Public awareness about
prevention and early detection of oral cancer: a population-based study in Northern
Germany. Journal of Cranio-Maxillofacial Surgery, 40(3), e82-e86
Hoffmann, M., Ihloff, A. S., Görögh, T., Weise, J. B., Fazel, A., Krams, M., ... & Kahn, T.
(2010). p16INK4a overexpression predicts translational active human papillomavirus
infection in tonsillar cancer. International journal of cancer, 127(7), 1595-1602
Jalouli, J., Ibrahim, S. O., Mehrotra, R., Jalouli, M. M., Sapkota, D., Larsson, P. A., & Hirsch, J.
M. (2010). Prevalence of viral (HPV, EBV, HSV) infections in oral submucous fibrosis
and oral cancer from India. Acta to-laryngological, 130(11), 1306-1311
A. (2012). Preferences for place of death if faced with advanced cancer: a population
survey in England, Flanders, Germany, Italy, the Netherlands, Portugal, and Spain.
Annals of Oncology, 23(8), 2006-2015
Guntinas-Lichius, O., Wendt, T., Buentzel, J., Esser, D., Lochner, P., Mueller, A., ... &
Altendorf-Hofmann, A. (2010). Head and neck cancer in Germany: a site-specific
analysis of survival of the Thuringian cancer registration database. Journal of cancer
research and clinical oncology, 136(1), 55-63
Heidenreich, A., Bastian, P. J., Bellmunt, J., Bolla, M., Joniau, S., van der Kwast, T., ... &
Mottet, N. (2014). EAU guidelines on prostate cancer. Part 1: screening, diagnosis, and
local treatment with curative intent—update 2013. European Urology, 65(1), 124-137.
Hensel, M., Goetzenich, A., Lutz, T., Stoehr, A., Moll, A., Rockstroh, J., ... & Mosthaf, F.
(2011). HIV and cancer in Germany. Deutsches Ärzteblatt International, 108(8), 117
Hertrampf, K., Wenz, H. J., Koller, M., & Wiltfang, J. (2012). Public awareness about
prevention and early detection of oral cancer: a population-based study in Northern
Germany. Journal of Cranio-Maxillofacial Surgery, 40(3), e82-e86
Hoffmann, M., Ihloff, A. S., Görögh, T., Weise, J. B., Fazel, A., Krams, M., ... & Kahn, T.
(2010). p16INK4a overexpression predicts translational active human papillomavirus
infection in tonsillar cancer. International journal of cancer, 127(7), 1595-1602
Jalouli, J., Ibrahim, S. O., Mehrotra, R., Jalouli, M. M., Sapkota, D., Larsson, P. A., & Hirsch, J.
M. (2010). Prevalence of viral (HPV, EBV, HSV) infections in oral submucous fibrosis
and oral cancer from India. Acta to-laryngological, 130(11), 1306-1311
Jemal, A., Bray, F., Center, M. M., Ferlay, J., Ward, E., & Forman, D. (2011). Global cancer
statistics. CA: a cancer journal for clinicians, 61(2), 69-90
Jou, Y. J., Lin, C. D., Lai, C. H., Chen, C. H., Kao, J. Y., Chen, S. Y., ... & Lin, C. W. (2010).
Proteomic identification of salivary transferrin as a biomarker for early detection of oral
cancer. Analytica Chimica Acta, 681(1-2), 41-48
Jung, H. M., Phillips, B. L., Patel, R. S., Cohen, D. M., Jakymiw, A., Kong, W. W., ... & Chan,
E. K. (2012). Keratinization-associated miR-7 and miR-21 regulate tumor suppressor
reversion-inducing cysteine-rich protein with kazal motifs (RECK) in oral
cancer. Journal of Biological Chemistry, 287(35), 29261-29272
Kadam, C. Y., Katkam, R. V., Suryakar, A. N., Kumbar, K. M., & Kadam, D. P. (2011).
Biochemical markers in oral cancer. Biomedical research, 22(1)
Kasznicki, J., Sliwinska, A., & Drzewoski, J. (2014). Metformin in cancer prevention and
therapy. Annals of translational medicine, 2(6)
Kayamori, K., Sakamoto, K., Nakashima, T., Takayanagi, H., Morita, K. I., Omura, K., ... &
Akashi, T. (2010). Roles of interleukin-6 and parathyroid hormone-related peptide in
osteoclast formation associated with oral cancers: significance of interleukin-6
synthesized by stromal cells in response to cancer cells. The American journal of
pathology, 176(2), 968-980
Kim, J. Y., Cho, T. J., Woo, B. H., Choi, K. U., Lee, C. H., Ryu, M. H., & Park, H. R. (2012).
Curcumin-induced autophagy contributes to the decreased survival of oral cancer
cells. Archives of oral biology, 57(8), 1018-1025
statistics. CA: a cancer journal for clinicians, 61(2), 69-90
Jou, Y. J., Lin, C. D., Lai, C. H., Chen, C. H., Kao, J. Y., Chen, S. Y., ... & Lin, C. W. (2010).
Proteomic identification of salivary transferrin as a biomarker for early detection of oral
cancer. Analytica Chimica Acta, 681(1-2), 41-48
Jung, H. M., Phillips, B. L., Patel, R. S., Cohen, D. M., Jakymiw, A., Kong, W. W., ... & Chan,
E. K. (2012). Keratinization-associated miR-7 and miR-21 regulate tumor suppressor
reversion-inducing cysteine-rich protein with kazal motifs (RECK) in oral
cancer. Journal of Biological Chemistry, 287(35), 29261-29272
Kadam, C. Y., Katkam, R. V., Suryakar, A. N., Kumbar, K. M., & Kadam, D. P. (2011).
Biochemical markers in oral cancer. Biomedical research, 22(1)
Kasznicki, J., Sliwinska, A., & Drzewoski, J. (2014). Metformin in cancer prevention and
therapy. Annals of translational medicine, 2(6)
Kayamori, K., Sakamoto, K., Nakashima, T., Takayanagi, H., Morita, K. I., Omura, K., ... &
Akashi, T. (2010). Roles of interleukin-6 and parathyroid hormone-related peptide in
osteoclast formation associated with oral cancers: significance of interleukin-6
synthesized by stromal cells in response to cancer cells. The American journal of
pathology, 176(2), 968-980
Kim, J. Y., Cho, T. J., Woo, B. H., Choi, K. U., Lee, C. H., Ryu, M. H., & Park, H. R. (2012).
Curcumin-induced autophagy contributes to the decreased survival of oral cancer
cells. Archives of oral biology, 57(8), 1018-1025
Kiyohara, C., & Ohno, Y. (2010). Sex differences in lung cancer susceptibility: a review. Gender
medicine, 7(5), 381-401
Klosa, K., Wiltfang, J., Wenz, H. J., Koller, M., & Hertrampf, K. (2011). Dentists' opinions and
practices in oral cancer prevention and early detection in Northern Germany. European
Journal of Cancer Prevention, 20(4), 313-319
Koh, Y. W., Choi, E. C., Kang, S. U., Hwang, H. S., Lee, M. H., Pyun, J., ... & Kim, C. H.
(2011). Green tea (−)-epigallocatechin-3-gallate inhibits HGF-induced progression in
oral cavity cancer through suppression of HGF/c-Met. The Journal of nutritional
biochemistry, 22(11), 1074-1083
Lee, C. H., Hung, H. W., Hung, P. H., & Shieh, Y. S. (2010). Epidermal growth factor receptor
regulates the β-catenin location, stability, and transcriptional activity in oral cancer.
Molecular cancer, 9(1), 64
Linsen, S. S., Martini, M., & Stark, H. (2012). Long‐term results of endosteal implants following
radical oral cancer surgery with and without adjuvant radiation therapy. Clinical implant
dentistry and related research, 14(2), 250-258
Liu, W., Shi, L. J., Wu, L., Feng, J. Q., Yang, X., Li, J., ... & Zhang, C. P. (2012). Oral cancer
development in patients with leukoplakia–clinicopathological factors affecting the
outcome. PLoS One, 7(4), e34773
Malhotra, R., Patel, V., Vaqué, J. P., Gutkind, J. S., & Rusling, J. F. (2010). Ultrasensitive
electrochemical immunosensor for oral cancer biomarker IL-6 using carbon nanotube
forest electrodes and multilabel amplification. Analytical Chemistry, 82(8), 3118-3123
medicine, 7(5), 381-401
Klosa, K., Wiltfang, J., Wenz, H. J., Koller, M., & Hertrampf, K. (2011). Dentists' opinions and
practices in oral cancer prevention and early detection in Northern Germany. European
Journal of Cancer Prevention, 20(4), 313-319
Koh, Y. W., Choi, E. C., Kang, S. U., Hwang, H. S., Lee, M. H., Pyun, J., ... & Kim, C. H.
(2011). Green tea (−)-epigallocatechin-3-gallate inhibits HGF-induced progression in
oral cavity cancer through suppression of HGF/c-Met. The Journal of nutritional
biochemistry, 22(11), 1074-1083
Lee, C. H., Hung, H. W., Hung, P. H., & Shieh, Y. S. (2010). Epidermal growth factor receptor
regulates the β-catenin location, stability, and transcriptional activity in oral cancer.
Molecular cancer, 9(1), 64
Linsen, S. S., Martini, M., & Stark, H. (2012). Long‐term results of endosteal implants following
radical oral cancer surgery with and without adjuvant radiation therapy. Clinical implant
dentistry and related research, 14(2), 250-258
Liu, W., Shi, L. J., Wu, L., Feng, J. Q., Yang, X., Li, J., ... & Zhang, C. P. (2012). Oral cancer
development in patients with leukoplakia–clinicopathological factors affecting the
outcome. PLoS One, 7(4), e34773
Malhotra, R., Patel, V., Vaqué, J. P., Gutkind, J. S., & Rusling, J. F. (2010). Ultrasensitive
electrochemical immunosensor for oral cancer biomarker IL-6 using carbon nanotube
forest electrodes and multilabel amplification. Analytical Chemistry, 82(8), 3118-3123
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Mallath, M. K., Taylor, D. G., Badwe, R. A., Rath, G. K., Shanta, V., Pramesh, C. S., ... &
Kapoor, S. (2014). The growing burden of cancer in India: epidemiology and social
context. The Lancet Oncology, 15(6), e205-e212
Marsh, D., Suchak, K., Moutasim, K. A., Vallath, S., Hopper, C., Jerjes, W., ... & Chester, K. A.
(2011). Stromal features are predictive of disease mortality in oral cancer patients. The
Journal of Pathology, 223(4), 470-481
Oh, C. M., Won, Y. J., Jung, K. W., Kong, H. J., Cho, H., Lee, J. K., ... & Lee, K. H. (2016).
Cancer statistics in Korea: incidence, mortality, survival, and prevalence in
2013. Cancer research and treatment: official journal of Korean Cancer
Association, 48(2), 436
Rahib, L., Smith, B. D., Aizenberg, R., Rosenzweig, A. B., Fleshman, J. M., & Matrisian, L. M.
(2014). Projecting cancer incidence and deaths to 2030: the unexpected burden of
thyroid, liver, and pancreas cancers in the United States. Cancer research
Rana, M., Zapf, A., Kuehle, M., Gellrich, N. C., & Eckardt, A. M. (2012). Clinical evaluation of
an autofluorescence diagnostic device for oral cancer detection: a prospective
randomized diagnostic study. European Journal of Cancer Prevention, 21(5), 460-466
Rivera, C. (2015). Essentials of oral cancer. International journal of clinical and experimental
pathology, 8(9), 11884
Sobral, L. M., Bufalino, A., Lopes, M. A., Graner, E., Salo, T., & Coletta, R. D. (2011).
Myofibroblasts in the stroma of oral cancer promote tumorigenesis via secretion of
activin A. Oral oncology, 47(9), 840-846
Sugimoto, M., Wong, D. T., Hirayama, A., Soga, T., & Tomita, M. (2010). Capillary
electrophoresis-mass spectrometry-based saliva metabolomics identified oral, breast and
pancreatic cancer-specific profiles. Metabolomics, 6(1), 78-95
Kapoor, S. (2014). The growing burden of cancer in India: epidemiology and social
context. The Lancet Oncology, 15(6), e205-e212
Marsh, D., Suchak, K., Moutasim, K. A., Vallath, S., Hopper, C., Jerjes, W., ... & Chester, K. A.
(2011). Stromal features are predictive of disease mortality in oral cancer patients. The
Journal of Pathology, 223(4), 470-481
Oh, C. M., Won, Y. J., Jung, K. W., Kong, H. J., Cho, H., Lee, J. K., ... & Lee, K. H. (2016).
Cancer statistics in Korea: incidence, mortality, survival, and prevalence in
2013. Cancer research and treatment: official journal of Korean Cancer
Association, 48(2), 436
Rahib, L., Smith, B. D., Aizenberg, R., Rosenzweig, A. B., Fleshman, J. M., & Matrisian, L. M.
(2014). Projecting cancer incidence and deaths to 2030: the unexpected burden of
thyroid, liver, and pancreas cancers in the United States. Cancer research
Rana, M., Zapf, A., Kuehle, M., Gellrich, N. C., & Eckardt, A. M. (2012). Clinical evaluation of
an autofluorescence diagnostic device for oral cancer detection: a prospective
randomized diagnostic study. European Journal of Cancer Prevention, 21(5), 460-466
Rivera, C. (2015). Essentials of oral cancer. International journal of clinical and experimental
pathology, 8(9), 11884
Sobral, L. M., Bufalino, A., Lopes, M. A., Graner, E., Salo, T., & Coletta, R. D. (2011).
Myofibroblasts in the stroma of oral cancer promote tumorigenesis via secretion of
activin A. Oral oncology, 47(9), 840-846
Sugimoto, M., Wong, D. T., Hirayama, A., Soga, T., & Tomita, M. (2010). Capillary
electrophoresis-mass spectrometry-based saliva metabolomics identified oral, breast and
pancreatic cancer-specific profiles. Metabolomics, 6(1), 78-95
Supic, G., Kozomara, R., Jovic, N., Zeljic, K., & Magic, Z. (2011). Prognostic significance of
tumor-related genes hypermethylation detected in cancer-free surgical margins of oral
squamous cell carcinomas. Oral Oncology, 47(8), 702-708
Torre, L. A., Bray, F., Siegel, R. L., Ferlay, J., Lortet‐Tieulent, J., & Jemal, A. (2015). Global
cancer statistics, 2012. CA: a cancer journal for clinicians, 65(2), 87-108
Torre, L. A., Siegel, R. L., Ward, E. M., & Jemal, A. (2015). Global cancer incidence and
mortality rates and trends—an update. Cancer Epidemiology and Prevention Biomarkers
Trellakis, S., Bruderek, K., Dumitru, C. A., Gholaman, H., Gu, X., Bankfalvi, A., ... &
Hoffmann, T. K. (2011). Polymorphonuclear granulocytes in human head and neck
cancer: enhanced inflammatory activity, modulation by cancer cells and expansion in
advanced disease. International journal of cancer, 129(9), 2183-2193
Tutt, A., Robson, M., Garber, J. E., Domchek, S. M., Audeh, M. W., Weitzel, J. N., ... &
Wardley, A. (2010). Oral poly (ADP-ribose) polymerase inhibitor olaparib in patients
with BRCA1 or BRCA2 mutations and advanced breast cancer: a proof-of-concept
trial. The Lancet, 376(9737), 235-244
Ussher, M. H., Taylor, A., & Faulkner, G. (2017). Exercise interventions for smoking
cessation. Cancer
Ward, E., DeSantis, C., Robbins, A., Kohler, B., & Jemal, A. (2014). Childhood and adolescent
cancer statistics, 2014. CA: a cancer journal for clinicians, 64(2), 83-103
Worthington, H. V., Clarkson, J. E., Bryan, G., Furness, S., Glenny, A. M., Littlewood, A., ... &
Khalid, T. (2010). Interventions for preventing oral mucositis for patients with cancer
receiving treatment. Cochrane Database Syst Rev, 12
tumor-related genes hypermethylation detected in cancer-free surgical margins of oral
squamous cell carcinomas. Oral Oncology, 47(8), 702-708
Torre, L. A., Bray, F., Siegel, R. L., Ferlay, J., Lortet‐Tieulent, J., & Jemal, A. (2015). Global
cancer statistics, 2012. CA: a cancer journal for clinicians, 65(2), 87-108
Torre, L. A., Siegel, R. L., Ward, E. M., & Jemal, A. (2015). Global cancer incidence and
mortality rates and trends—an update. Cancer Epidemiology and Prevention Biomarkers
Trellakis, S., Bruderek, K., Dumitru, C. A., Gholaman, H., Gu, X., Bankfalvi, A., ... &
Hoffmann, T. K. (2011). Polymorphonuclear granulocytes in human head and neck
cancer: enhanced inflammatory activity, modulation by cancer cells and expansion in
advanced disease. International journal of cancer, 129(9), 2183-2193
Tutt, A., Robson, M., Garber, J. E., Domchek, S. M., Audeh, M. W., Weitzel, J. N., ... &
Wardley, A. (2010). Oral poly (ADP-ribose) polymerase inhibitor olaparib in patients
with BRCA1 or BRCA2 mutations and advanced breast cancer: a proof-of-concept
trial. The Lancet, 376(9737), 235-244
Ussher, M. H., Taylor, A., & Faulkner, G. (2017). Exercise interventions for smoking
cessation. Cancer
Ward, E., DeSantis, C., Robbins, A., Kohler, B., & Jemal, A. (2014). Childhood and adolescent
cancer statistics, 2014. CA: a cancer journal for clinicians, 64(2), 83-103
Worthington, H. V., Clarkson, J. E., Bryan, G., Furness, S., Glenny, A. M., Littlewood, A., ... &
Khalid, T. (2010). Interventions for preventing oral mucositis for patients with cancer
receiving treatment. Cochrane Database Syst Rev, 12
Zeng, H., Zheng, R., Guo, Y., Zhang, S., Zou, X., Wang, N., ... & Huang, S. (2015). Cancer
survival in C hina, 2003–2005: A population‐based study. International journal of
cancer, 136(8), 1921-1930
Zhang, Z. J., Hao, K., Shi, R., Zhao, G., Jiang, G. X., Song, Y., ... & Ma, J. (2011). Glutathione
S-transferase M1 (GSTM1) and glutathione S-transferase T1 (GSTT1) null
polymorphisms, smoking, and their interaction in oral cancer: a HuGE review and meta-
analysis. American journal of epidemiology, 173(8), 847-857
Zini, A., Czerninski, R., & Sgan‐Cohen, H. D. (2010). Oral cancer over four decades:
epidemiology, trends, histology, and survival by anatomical sites. Journal of oral
pathology & medicine, 39(4), 299-305
survival in C hina, 2003–2005: A population‐based study. International journal of
cancer, 136(8), 1921-1930
Zhang, Z. J., Hao, K., Shi, R., Zhao, G., Jiang, G. X., Song, Y., ... & Ma, J. (2011). Glutathione
S-transferase M1 (GSTM1) and glutathione S-transferase T1 (GSTT1) null
polymorphisms, smoking, and their interaction in oral cancer: a HuGE review and meta-
analysis. American journal of epidemiology, 173(8), 847-857
Zini, A., Czerninski, R., & Sgan‐Cohen, H. D. (2010). Oral cancer over four decades:
epidemiology, trends, histology, and survival by anatomical sites. Journal of oral
pathology & medicine, 39(4), 299-305
1 out of 70
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.