Nursing Home Resident Risks: Falls, Weight Loss, Pressure Ulcers
VerifiedAdded on 2022/11/16
|11
|9558
|341
Report
AI Summary
This research article, published in the Journal of Clinical Nursing, investigates the factors associated with falls, weight loss, and pressure ulcers among nursing home residents. The study utilizes the Downton Fall Risk Index, the short form of Mini Nutritional Assessment, and the Modified Norton Scale to assess risks. Findings indicate that a significant portion of residents face multiple risks. While physical activity increased falls, it decreased pressure ulcers. Cognitive decline and general health status were most important for weight loss. The study emphasizes the need for a comprehensive approach to prevention, highlighting mobility as a critical factor. The research aims to provide insights into the interplay of different scale items and their relation to severe outcomes, contributing to improved care processes for frail older adults in nursing homes. The study highlights the complexity of risk group categorization and the importance of considering multiple factors in risk assessment, suggesting that total scores alone are insufficient for effective preventive work. The research underscores the challenge of balancing physical activity to prevent falls and pressure ulcers.

ORIGINAL ARTICLE
Factors related to falls, weight-loss and pressure ulcers – more insi
in risk assessment among nursing home residents
Christina Lannering, Marie Ernsth Bravell, Patrik Midl€ov, Carl-Johan€Ostgren and Sigvard M€olstad
Aims and objectives.To describe how the included items in three different scales,
Downton Fall Risk Index, the short form of Mini Nutritional Assessment and the
Modified Norton Scale are associated to severe outcomes as falls, weight loss and
pressure ulcers.
Background.Falls, malnutrition and pressure ulcers are common adverse events
among nursing home residents and risk scoring are common preventive activities,
mainly focusing on single risks.In Sweden the three scalesare routinely used
together with the purpose to improve the quality of prevention.
Design.Longitudinal quantitative study.
Methods.Descriptive analyses and Cox regression analyses.
Results.Only 4% scored no risk for any of these serious events. Longitudinal risk
scoring showed significantimpaired mean scores indicating increased risks.This
confirms the complexity of this population’s status of general condition. There were
no statisticalsignificantdifferences between residents categorised atrisk or not
regarding events. Physical activity increased falls, but decreased pressure ulcers. For
weight loss, cognitive decline and the status of general health were most important.
Conclusions.Risk tendencies for falls,malnutrition and pressure ulcers are high in
nursing homes, and when measure them at the same time the majority will have several
of these risks. Items assessing mobility or items affecting mobility were of most impor-
tance. Care processes can always be improved and this study can add to the topic.
Relevance to clinical practice.A more comprehensive view is needed and prevention
can not only be based on total scores. Mobility is an important factor for falls and
pressure ulcers, both as a risk factor and a protective factor. This involves a challenge
for care – to keep the inmates physical active and at the same time prevent falls.
Key words:falls, frail older, malnutrition,nursing homes,pressure ulcers,risk
assessment
What does this paper contribute
to the wider global clinical
community?
The complexity to risk group cat-
egorise frailolder persons.Risk
tendencies for falls,malnutrition
and pressureulcers are high
among older people living in
nursing homes and the majority
will have severalrisks.The total
scores, which constitute basis for
risk grouping,are not always
sufficient information for the
preventive work as a more com-
prehensive view is needed.
Care processescan always be
improved.The resultsfrom this
study can contribute to the knowl-
edge on how to assess older frail
persons.Maybe thereare other
ways than using severalassessing
scales. Mobility remains an impor-
tantfactor,both as a risk factor
and a protective factor and that is
challenge for care to manage.
Accepted for publication: 5 November 2015
Authors: Christina Lannering, RN, PhD Student, Unit of Research and
Developmentin Primary Care,Futurum,J€onk€oping;Marie Ernsth
Bravell, PhD, RN, Associate professor, Institute of Gerontology, School
of Health Sciences,J €onk€oping University,J€onk€oping;Patrik Midl€ov,
MD, Associate Professor,Department of ClinicalSciences in Malm€o,
GeneralPractice/Family Medicine,Lund University,Malm€o; Carl-
Johan €Ostgren,MD, Professor,Departmentof Medicaland Health
Sciences,GeneralPractice,Link€oping University,Link€oping;Sigvard
M€olstad,MD, Professor,Department of ClinicalSciences in Malm€o,
General Practice/Family Medicine, Lund University, Malm€o, Sweden
Correspondence:Christina Lannering, PhD Student, Unit of
Research and Developmentin Primary Care,Futurum,SE-551 85
J €onk€oping, Sweden. Telephone: +4636325205.
E-mail: christina.lannering@rjl.se
A study aimed to provide more insight in how different scale items
interact with each other and how they are associated to severe out-
comes.It is not a prediction study or a study ofdiagnostic accu-
racy,but a study that can contribute to the field of knowledge of
assessments in older persons.
© 2016 John Wiley & Sons Ltd
940 Journal of Clinical Nursing, 25, 940–950, doi: 10.1111/jocn.13154
Factors related to falls, weight-loss and pressure ulcers – more insi
in risk assessment among nursing home residents
Christina Lannering, Marie Ernsth Bravell, Patrik Midl€ov, Carl-Johan€Ostgren and Sigvard M€olstad
Aims and objectives.To describe how the included items in three different scales,
Downton Fall Risk Index, the short form of Mini Nutritional Assessment and the
Modified Norton Scale are associated to severe outcomes as falls, weight loss and
pressure ulcers.
Background.Falls, malnutrition and pressure ulcers are common adverse events
among nursing home residents and risk scoring are common preventive activities,
mainly focusing on single risks.In Sweden the three scalesare routinely used
together with the purpose to improve the quality of prevention.
Design.Longitudinal quantitative study.
Methods.Descriptive analyses and Cox regression analyses.
Results.Only 4% scored no risk for any of these serious events. Longitudinal risk
scoring showed significantimpaired mean scores indicating increased risks.This
confirms the complexity of this population’s status of general condition. There were
no statisticalsignificantdifferences between residents categorised atrisk or not
regarding events. Physical activity increased falls, but decreased pressure ulcers. For
weight loss, cognitive decline and the status of general health were most important.
Conclusions.Risk tendencies for falls,malnutrition and pressure ulcers are high in
nursing homes, and when measure them at the same time the majority will have several
of these risks. Items assessing mobility or items affecting mobility were of most impor-
tance. Care processes can always be improved and this study can add to the topic.
Relevance to clinical practice.A more comprehensive view is needed and prevention
can not only be based on total scores. Mobility is an important factor for falls and
pressure ulcers, both as a risk factor and a protective factor. This involves a challenge
for care – to keep the inmates physical active and at the same time prevent falls.
Key words:falls, frail older, malnutrition,nursing homes,pressure ulcers,risk
assessment
What does this paper contribute
to the wider global clinical
community?
The complexity to risk group cat-
egorise frailolder persons.Risk
tendencies for falls,malnutrition
and pressureulcers are high
among older people living in
nursing homes and the majority
will have severalrisks.The total
scores, which constitute basis for
risk grouping,are not always
sufficient information for the
preventive work as a more com-
prehensive view is needed.
Care processescan always be
improved.The resultsfrom this
study can contribute to the knowl-
edge on how to assess older frail
persons.Maybe thereare other
ways than using severalassessing
scales. Mobility remains an impor-
tantfactor,both as a risk factor
and a protective factor and that is
challenge for care to manage.
Accepted for publication: 5 November 2015
Authors: Christina Lannering, RN, PhD Student, Unit of Research and
Developmentin Primary Care,Futurum,J€onk€oping;Marie Ernsth
Bravell, PhD, RN, Associate professor, Institute of Gerontology, School
of Health Sciences,J €onk€oping University,J€onk€oping;Patrik Midl€ov,
MD, Associate Professor,Department of ClinicalSciences in Malm€o,
GeneralPractice/Family Medicine,Lund University,Malm€o; Carl-
Johan €Ostgren,MD, Professor,Departmentof Medicaland Health
Sciences,GeneralPractice,Link€oping University,Link€oping;Sigvard
M€olstad,MD, Professor,Department of ClinicalSciences in Malm€o,
General Practice/Family Medicine, Lund University, Malm€o, Sweden
Correspondence:Christina Lannering, PhD Student, Unit of
Research and Developmentin Primary Care,Futurum,SE-551 85
J €onk€oping, Sweden. Telephone: +4636325205.
E-mail: christina.lannering@rjl.se
A study aimed to provide more insight in how different scale items
interact with each other and how they are associated to severe out-
comes.It is not a prediction study or a study ofdiagnostic accu-
racy,but a study that can contribute to the field of knowledge of
assessments in older persons.
© 2016 John Wiley & Sons Ltd
940 Journal of Clinical Nursing, 25, 940–950, doi: 10.1111/jocn.13154
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Introduction
In Sweden, like in the rest of Western societies the numbers
of older people are increasing, and also the number of older
people needing care and services (WHO 2012). The munici-
pality has the responsibility to offer care in nursing home
facilities when the older person can no longermanage at
home. According to national statistics Sweden had approxi-
mately 87,600 persons at the age 65 and over permanently
staying in nursing home facilities.From these,80% were
aged above80 yearsand 69% were women (Board of
National Health and Welfare 2012). Old age care in Sweden
requires a need assessmentperformed by a specialtrained
social worker.The need assessment is based on the amount
of functionalproblemsperforming activitiesin daily life
(ADL). As a ‘stay-in-place’ policy is applied, home care ser-
vice is offered as long as possible. Moreover, the number of
beds in nursing homes has decreased by 20% during the last
10 years in Sweden (Board of National Health and Welfare
2012).These circumstances indicates that individuals mov-
ing in to nursing homes today are frailer and in more
extended need of care than previously.
To provide optimalcare and foremost preventive actions
it is essentialto know risk status, and helpful tools to
establish action policiescan be assessing scales.Accord-
ingly, scoring risk for falls, malnutrition and pressure ulcers
are common preventive activities in the care of older people
and numerous scales and assessments are used for this pur-
pose.In Sweden the most common tools are Downton Fall
Risk Index (DFRI)to assess fallrisk (Downton 1993),the
short form of Mini Nutritional Assessment(MNA-SF)
(Rubenstein et al.2001) to assess risk for malnutrition and
the Modified Norton Scale (MNS) (Ek 1987) to assess risk
for developing pressure ulcers.
Background
Falls by older people in nursing home facilities are common
events. The prevalence of falls in institutionalised older peo-
ple is reported at 53–62% of the inmates (Rosendahlet al.
2003,Meyer et al.2009).Risk factors have been described
as gait and balanceinstability,cognitiveand functional
impairment, sedating and psychoactive medications (Ruben-
stein et al.1994) and numberof diseases(Damian et al.
2013). Some falls may be caused by a single factor,but the
majority of falls are caused by a combination offactors
(Cameron et al. 2010).
Older persons are also considered to be athigh risk of
malnutrition.Severalstudies in nursing homes populations
have shown both high risk and high prevalence of malnutri-
tion; a recent review showed that approximately 14% were
classified as malnourished and more than half were at risk
of malnutrition (Kaiser et al.2011).A follow-up study in
Swedish nursing homes showed thatnutritionalstatus was
improved,but still63% were assessed at risk,and 30% of
those were malnourished (Torma et al. 2013).
A third major and serious eventthat is common among
older persons in nursing homes is pressure ulcers.A recent
systematic review of pressure ulcers risk factor studies iden-
tified three primary risk domains;mobility/activity,perfu-
sion and generalskin status.However,no single factor can
predictpressure ulcer risk,which is caused by a complex
interplay of factors (Coleman et al.2013). A Swedish nurs-
ing home study showed a prevalence ofpressure ulcers at
14% and according to risk assessment,a risk between 26–
30% (Gunningberg et al.2013)which is similarto other
European studies (Meesterberends et al. 2013).
One must also consider ageing as a risk factor for these
outcomes,knowing that biological ageing increases the vul-
nerability and decreasesthe reserve capacity (Fried et al.
2001, Rockwood & Mitnitski 2007).
In Sweden,DFRI, MNS and MNA-SF are routinely used
togetherto assessrisks in older personsliving in nursing
homes. The scales are included in the quality registry Senior
Alert which is a nationalinvestmentaimed to increase the
quality of the preventive work.The widely used MNA was
developed and validated for the assessmentof older, frail
persons.MNA has a long history (Secher et al.2007) and
seems to be wellsuited for nursing home residents (Diek-
mann et al.2013).Further validation has shown thatthe
short-form can be used as a stand-alone unit(Bauer et al.
2008,Salviet al. 2008,Dent et al. 2012).DFRI was vali-
dated in a Swedish study(Rosendahlet al. 2003) and
appeared to bea useful tool for predicting fallsamong
older people in residentialcare facilities.However,a com-
parison with DFRI and nurses judgement alone showed no
clinical benefitfor DFRI (Meyer et al. 2009). MNS is
tested, recommended and well known in Sweden (Gunning-
berg et al.2013)and it is validated to itsactualcontent
(Ek & Bjurulf 1987).
It is reasonable to believe thatfrail older persons have
severalrisks and that generaldecline increasesserious
events,but using severaldifferentinstruments can be time
consuming and increase the workload asresultsmust be
documentedand interventionsshould be planned and
followed.Therefore,it is importantto put knowledge to
this topic so that nursescan reflectupon the usefulness.
One problem when using the three scales together is that
severalfunctionsare assessed repeatedly asthey existin
more than one scale. Mobility and cognition are,for exam-
© 2016 John Wiley & Sons Ltd
Journal of Clinical Nursing, 25, 940–950 941
Original article Risk assessment among nursing home residents
In Sweden, like in the rest of Western societies the numbers
of older people are increasing, and also the number of older
people needing care and services (WHO 2012). The munici-
pality has the responsibility to offer care in nursing home
facilities when the older person can no longermanage at
home. According to national statistics Sweden had approxi-
mately 87,600 persons at the age 65 and over permanently
staying in nursing home facilities.From these,80% were
aged above80 yearsand 69% were women (Board of
National Health and Welfare 2012). Old age care in Sweden
requires a need assessmentperformed by a specialtrained
social worker.The need assessment is based on the amount
of functionalproblemsperforming activitiesin daily life
(ADL). As a ‘stay-in-place’ policy is applied, home care ser-
vice is offered as long as possible. Moreover, the number of
beds in nursing homes has decreased by 20% during the last
10 years in Sweden (Board of National Health and Welfare
2012).These circumstances indicates that individuals mov-
ing in to nursing homes today are frailer and in more
extended need of care than previously.
To provide optimalcare and foremost preventive actions
it is essentialto know risk status, and helpful tools to
establish action policiescan be assessing scales.Accord-
ingly, scoring risk for falls, malnutrition and pressure ulcers
are common preventive activities in the care of older people
and numerous scales and assessments are used for this pur-
pose.In Sweden the most common tools are Downton Fall
Risk Index (DFRI)to assess fallrisk (Downton 1993),the
short form of Mini Nutritional Assessment(MNA-SF)
(Rubenstein et al.2001) to assess risk for malnutrition and
the Modified Norton Scale (MNS) (Ek 1987) to assess risk
for developing pressure ulcers.
Background
Falls by older people in nursing home facilities are common
events. The prevalence of falls in institutionalised older peo-
ple is reported at 53–62% of the inmates (Rosendahlet al.
2003,Meyer et al.2009).Risk factors have been described
as gait and balanceinstability,cognitiveand functional
impairment, sedating and psychoactive medications (Ruben-
stein et al.1994) and numberof diseases(Damian et al.
2013). Some falls may be caused by a single factor,but the
majority of falls are caused by a combination offactors
(Cameron et al. 2010).
Older persons are also considered to be athigh risk of
malnutrition.Severalstudies in nursing homes populations
have shown both high risk and high prevalence of malnutri-
tion; a recent review showed that approximately 14% were
classified as malnourished and more than half were at risk
of malnutrition (Kaiser et al.2011).A follow-up study in
Swedish nursing homes showed thatnutritionalstatus was
improved,but still63% were assessed at risk,and 30% of
those were malnourished (Torma et al. 2013).
A third major and serious eventthat is common among
older persons in nursing homes is pressure ulcers.A recent
systematic review of pressure ulcers risk factor studies iden-
tified three primary risk domains;mobility/activity,perfu-
sion and generalskin status.However,no single factor can
predictpressure ulcer risk,which is caused by a complex
interplay of factors (Coleman et al.2013). A Swedish nurs-
ing home study showed a prevalence ofpressure ulcers at
14% and according to risk assessment,a risk between 26–
30% (Gunningberg et al.2013)which is similarto other
European studies (Meesterberends et al. 2013).
One must also consider ageing as a risk factor for these
outcomes,knowing that biological ageing increases the vul-
nerability and decreasesthe reserve capacity (Fried et al.
2001, Rockwood & Mitnitski 2007).
In Sweden,DFRI, MNS and MNA-SF are routinely used
togetherto assessrisks in older personsliving in nursing
homes. The scales are included in the quality registry Senior
Alert which is a nationalinvestmentaimed to increase the
quality of the preventive work.The widely used MNA was
developed and validated for the assessmentof older, frail
persons.MNA has a long history (Secher et al.2007) and
seems to be wellsuited for nursing home residents (Diek-
mann et al.2013).Further validation has shown thatthe
short-form can be used as a stand-alone unit(Bauer et al.
2008,Salviet al. 2008,Dent et al. 2012).DFRI was vali-
dated in a Swedish study(Rosendahlet al. 2003) and
appeared to bea useful tool for predicting fallsamong
older people in residentialcare facilities.However,a com-
parison with DFRI and nurses judgement alone showed no
clinical benefitfor DFRI (Meyer et al. 2009). MNS is
tested, recommended and well known in Sweden (Gunning-
berg et al.2013)and it is validated to itsactualcontent
(Ek & Bjurulf 1987).
It is reasonable to believe thatfrail older persons have
severalrisks and that generaldecline increasesserious
events,but using severaldifferentinstruments can be time
consuming and increase the workload asresultsmust be
documentedand interventionsshould be planned and
followed.Therefore,it is importantto put knowledge to
this topic so that nursescan reflectupon the usefulness.
One problem when using the three scales together is that
severalfunctionsare assessed repeatedly asthey existin
more than one scale. Mobility and cognition are,for exam-
© 2016 John Wiley & Sons Ltd
Journal of Clinical Nursing, 25, 940–950 941
Original article Risk assessment among nursing home residents
ple, assessed in allthree scalesbut in differentways and
with different grading. The ambition with the present study
is to gain knowledge aboutthe relationsamong the out-
comes and the included scale items.
Aim
This study aims to find patterns of associations among scale
risk items in MNA-SF,DFRI and MNS, with the outcomes
falls, pressure ulcers and weight-loss.
Method
Study population
Data from this study were collected from a longitudinal
cohort study of older people living in nursing homesin
Sweden;The Study on Health and Drugs in Elderly
(SHADES). The SHADES study was launched in 2008
and completed in 2011 and the overall aims were to
describeand analyse morbidity, health-conditionsand
drug-useamong olderpeoplein nursing homefacilities.
A convenience sample of12 nursing homes including 443
beds was included in the SHADES study. The nursing
homes were located in three differentregions in southern
Sweden and were allin the public sector.As participants
were included during the whole study period,the partici-
pants had differentdurationswhich consequently led to
varying number offollow-up assessments.When the study
nurse returned for a follow-up visit,all new inmates were
asked to participate,not just those who moved in where
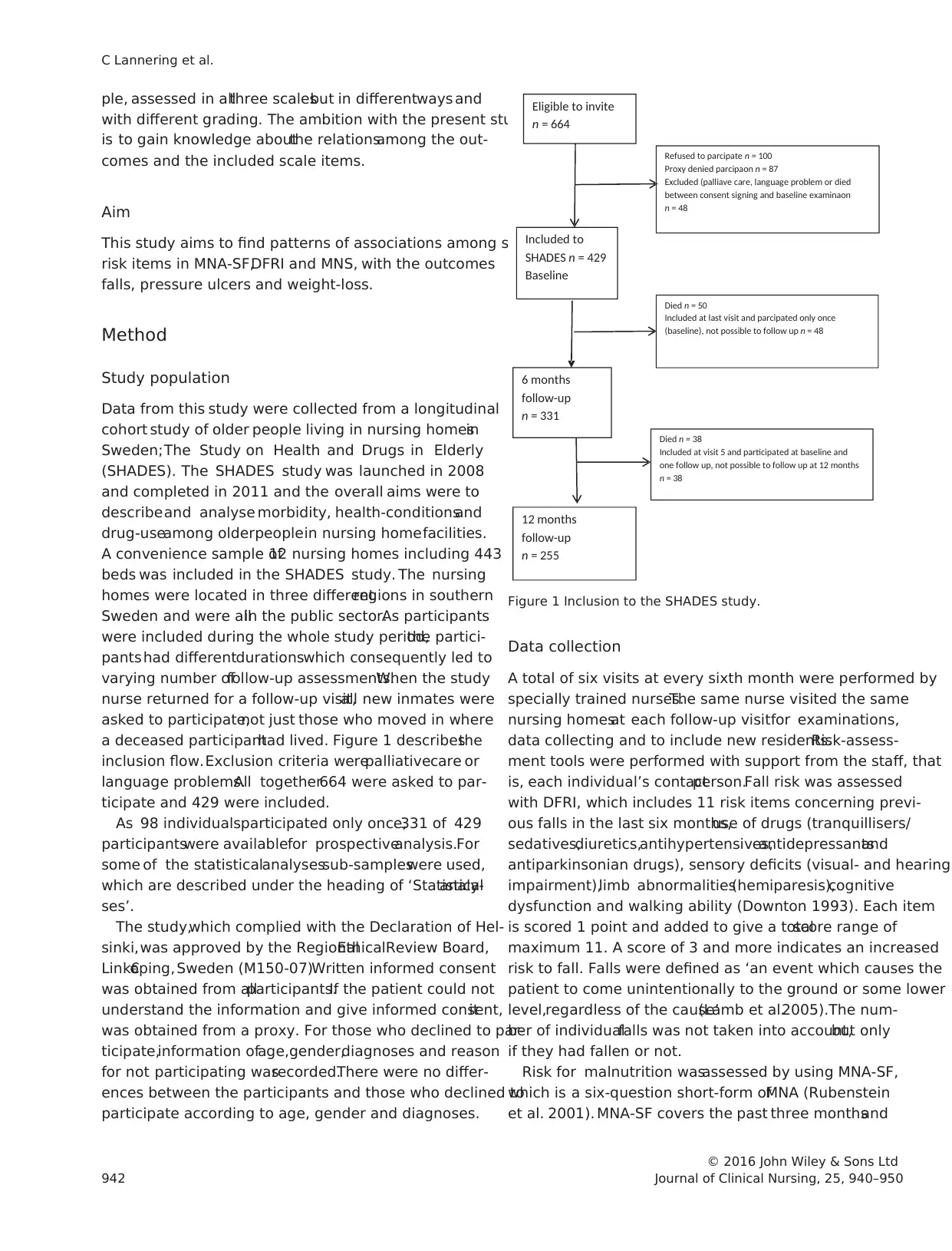
a deceased participanthad lived. Figure 1 describesthe
inclusion flow.Exclusion criteria werepalliativecare or
language problems.All together664 were asked to par-
ticipate and 429 were included.
As 98 individualsparticipated only once,331 of 429
participantswere availablefor prospectiveanalysis.For
some of the statisticalanalysessub-sampleswere used,
which are described under the heading of ‘Statisticalanaly-
ses’.
The study,which complied with the Declaration of Hel-
sinki,was approved by the RegionalEthicalReview Board,
Link€oping, Sweden (M150-07).Written informed consent
was obtained from allparticipants.If the patient could not
understand the information and give informed consent,it
was obtained from a proxy. For those who declined to par-
ticipate,information ofage,gender,diagnoses and reason
for not participating wasrecorded.There were no differ-
ences between the participants and those who declined to
participate according to age, gender and diagnoses.
Data collection
A total of six visits at every sixth month were performed by
specially trained nurses.The same nurse visited the same
nursing homesat each follow-up visitfor examinations,
data collecting and to include new residents.Risk-assess-
ment tools were performed with support from the staff, that
is, each individual’s contactperson.Fall risk was assessed
with DFRI, which includes 11 risk items concerning previ-
ous falls in the last six months,use of drugs (tranquillisers/
sedatives,diuretics,antihypertensives,antidepressantsand
antiparkinsonian drugs), sensory deficits (visual- and hearing
impairment),limb abnormalities(hemiparesis),cognitive
dysfunction and walking ability (Downton 1993). Each item
is scored 1 point and added to give a totalscore range of
maximum 11. A score of 3 and more indicates an increased
risk to fall. Falls were defined as ‘an event which causes the
patient to come unintentionally to the ground or some lower
level,regardless of the cause’(Lamb et al.2005).The num-
ber of individualfalls was not taken into account,but only
if they had fallen or not.
Risk for malnutrition wasassessed by using MNA-SF,
which is a six-question short-form ofMNA (Rubenstein
et al. 2001). MNA-SF covers the past three monthsand
Eligible to invite
n = 664
Refused to parcipate n = 100
Proxy denied parcipaon n = 87
Excluded (palliave care, language problem or died
between consent signing and baseline examinaon
n = 48
Included to
SHADES n = 429
Baseline
6 months
follow-up
n = 331
Died n = 50
Included at last visit and parcipated only once
(baseline), not possible to follow up n = 48
Died n = 38
Included at visit 5 and participated at baseline and
one follow up, not possible to follow up at 12 months
n = 38
12 months
follow-up
n = 255
Figure 1 Inclusion to the SHADES study.
© 2016 John Wiley & Sons Ltd
942 Journal of Clinical Nursing, 25, 940–950
C Lannering et al.
with different grading. The ambition with the present study
is to gain knowledge aboutthe relationsamong the out-
comes and the included scale items.
Aim
This study aims to find patterns of associations among scale
risk items in MNA-SF,DFRI and MNS, with the outcomes
falls, pressure ulcers and weight-loss.
Method
Study population
Data from this study were collected from a longitudinal
cohort study of older people living in nursing homesin
Sweden;The Study on Health and Drugs in Elderly
(SHADES). The SHADES study was launched in 2008
and completed in 2011 and the overall aims were to
describeand analyse morbidity, health-conditionsand
drug-useamong olderpeoplein nursing homefacilities.
A convenience sample of12 nursing homes including 443
beds was included in the SHADES study. The nursing
homes were located in three differentregions in southern
Sweden and were allin the public sector.As participants
were included during the whole study period,the partici-
pants had differentdurationswhich consequently led to
varying number offollow-up assessments.When the study
nurse returned for a follow-up visit,all new inmates were
asked to participate,not just those who moved in where
a deceased participanthad lived. Figure 1 describesthe
inclusion flow.Exclusion criteria werepalliativecare or
language problems.All together664 were asked to par-
ticipate and 429 were included.
As 98 individualsparticipated only once,331 of 429
participantswere availablefor prospectiveanalysis.For
some of the statisticalanalysessub-sampleswere used,
which are described under the heading of ‘Statisticalanaly-
ses’.
The study,which complied with the Declaration of Hel-
sinki,was approved by the RegionalEthicalReview Board,
Link€oping, Sweden (M150-07).Written informed consent
was obtained from allparticipants.If the patient could not
understand the information and give informed consent,it
was obtained from a proxy. For those who declined to par-
ticipate,information ofage,gender,diagnoses and reason
for not participating wasrecorded.There were no differ-
ences between the participants and those who declined to
participate according to age, gender and diagnoses.
Data collection
A total of six visits at every sixth month were performed by
specially trained nurses.The same nurse visited the same
nursing homesat each follow-up visitfor examinations,
data collecting and to include new residents.Risk-assess-
ment tools were performed with support from the staff, that
is, each individual’s contactperson.Fall risk was assessed
with DFRI, which includes 11 risk items concerning previ-
ous falls in the last six months,use of drugs (tranquillisers/
sedatives,diuretics,antihypertensives,antidepressantsand
antiparkinsonian drugs), sensory deficits (visual- and hearing
impairment),limb abnormalities(hemiparesis),cognitive
dysfunction and walking ability (Downton 1993). Each item
is scored 1 point and added to give a totalscore range of
maximum 11. A score of 3 and more indicates an increased
risk to fall. Falls were defined as ‘an event which causes the
patient to come unintentionally to the ground or some lower
level,regardless of the cause’(Lamb et al.2005).The num-
ber of individualfalls was not taken into account,but only
if they had fallen or not.
Risk for malnutrition wasassessed by using MNA-SF,
which is a six-question short-form ofMNA (Rubenstein
et al. 2001). MNA-SF covers the past three monthsand
Eligible to invite
n = 664
Refused to parcipate n = 100
Proxy denied parcipaon n = 87
Excluded (palliave care, language problem or died
between consent signing and baseline examinaon
n = 48
Included to
SHADES n = 429
Baseline
6 months
follow-up
n = 331
Died n = 50
Included at last visit and parcipated only once
(baseline), not possible to follow up n = 48
Died n = 38
Included at visit 5 and participated at baseline and
one follow up, not possible to follow up at 12 months
n = 38
12 months
follow-up
n = 255
Figure 1 Inclusion to the SHADES study.
© 2016 John Wiley & Sons Ltd
942 Journal of Clinical Nursing, 25, 940–950
C Lannering et al.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
addressesdecreased food intake(0–2 points), estimated
weight loss (0–3 points), mobility (0–2 points), acute diseases
or psychologicalstress (0 or 2 points),neuropsychological
impairment (0–2 points) and BMI (0–3 points).The higher
the value the lower the risk. The maximum MNA-SF score is
14 points. A score of 7 points or less indicates malnutrition,
8–11 indicates risk of malnutrition and 12–14 points indi-
cates no risk for malnutrition.
Risk for pressure ulcers was assessed with MNS. In addi-
tion to the more internationally known Norton Scale, MNS
also includestwo items assessing nutrition status.MNS
consists of seven items; mental condition, activity, mobility,
food intake,fluid intake,incontinence and generalphysical
condition.Each item is assessed with a range from 1 (lack
of function) to 4 (normalfunction).The maximum score is
28 and a score at20 or lower indicates an increased risk
for pressure ulcers (Ek 1987).
The scales internal consistency in this study, measured by
Cronbach’salpha showed 05 for DFRI, 066 for MNS
and 045 for MNA-SF.
In the SHADES study the nursesexamined the partici-
pants in many ways regarding differentassessmentscales,
blood testing,use of drugs,different measurements etc.For
this presentstudy we used data from DFRI, MNA-SF,
MNS, data of weight and data of eventual presence of pres-
sure ulcers.Pressure ulcerswere graded as:(1) persistent
discoloration,with intactskin surface;(2) epithelialdam-
age;(3) damage to the fullthickness of the skin without a
deep cavity and (4) damage to the full thickness of the skin
with deep cavity.In this study,all kinds of pressure ulcers
were taken into account,but not gradated,only counted as
existing ornot. Description ofthe study population con-
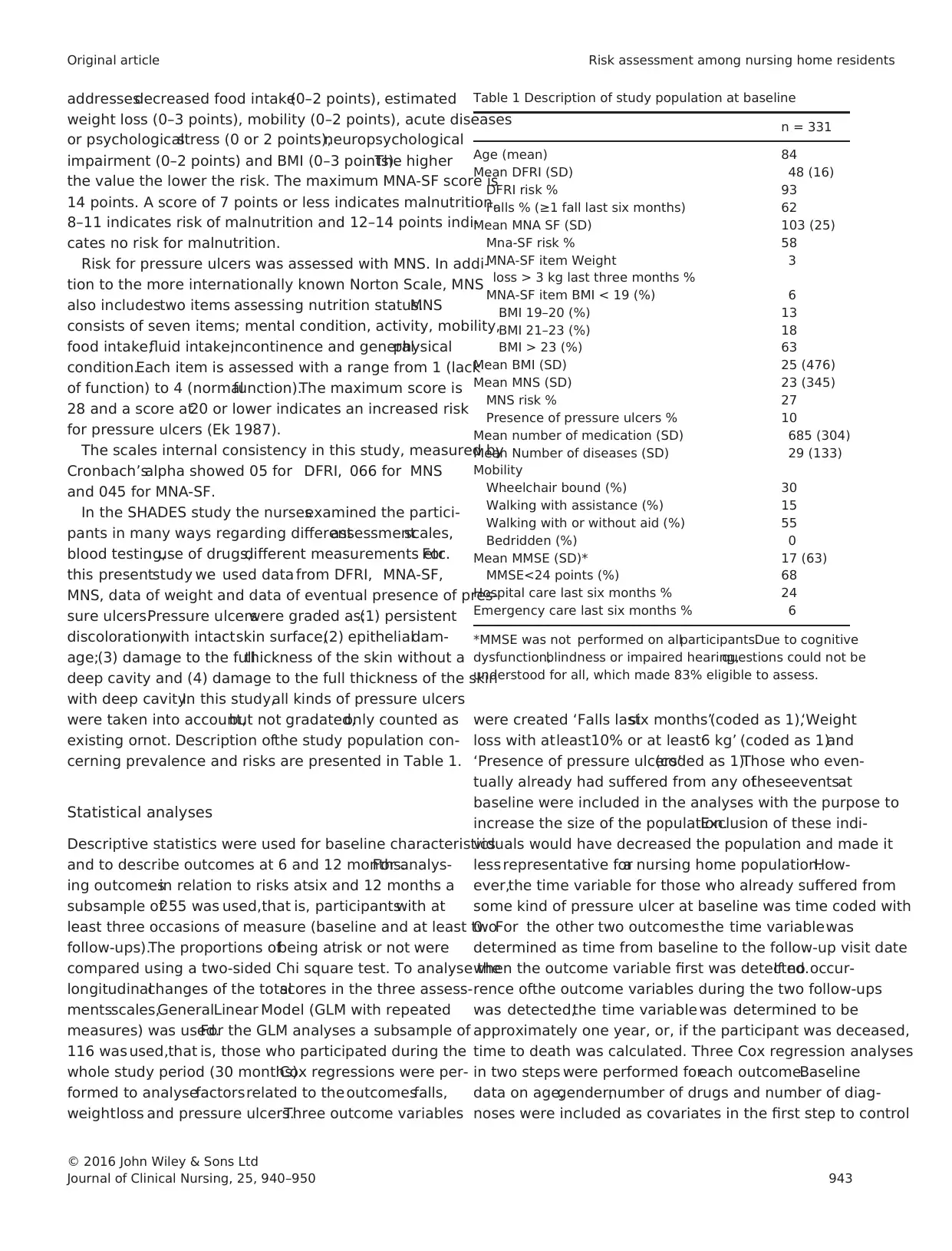
cerning prevalence and risks are presented in Table 1.
Statistical analyses
Descriptive statistics were used for baseline characteristics
and to describe outcomes at 6 and 12 months.For analys-
ing outcomesin relation to risks atsix and 12 months a
subsample of255 was used,that is, participantswith at
least three occasions of measure (baseline and at least two
follow-ups).The proportions ofbeing atrisk or not were
compared using a two-sided Chi square test. To analyse the
longitudinalchanges of the totalscores in the three assess-
mentsscales,GeneralLinear Model (GLM with repeated
measures) was used.For the GLM analyses a subsample of
116 was used,that is, those who participated during the
whole study period (30 months).Cox regressions were per-
formed to analysefactorsrelated to the outcomesfalls,
weightloss and pressure ulcers.Three outcome variables
were created ‘Falls lastsix months’(coded as 1),‘Weight
loss with atleast10% or at least6 kg’ (coded as 1)and
‘Presence of pressure ulcers’(coded as 1).Those who even-
tually already had suffered from any oftheseeventsat
baseline were included in the analyses with the purpose to
increase the size of the population.Exclusion of these indi-
viduals would have decreased the population and made it
less representative fora nursing home population.How-
ever,the time variable for those who already suffered from
some kind of pressure ulcer at baseline was time coded with
0. For the other two outcomesthe time variablewas
determined as time from baseline to the follow-up visit date
when the outcome variable first was detected.If no occur-
rence ofthe outcome variables during the two follow-ups
was detected,the time variable was determined to be
approximately one year, or, if the participant was deceased,
time to death was calculated. Three Cox regression analyses
in two steps were performed foreach outcome.Baseline
data on age,gender,number of drugs and number of diag-
noses were included as covariates in the first step to control
Table 1 Description of study population at baseline
n = 331
Age (mean) 84
Mean DFRI (SD) 48 (16)
DFRI risk % 93
Falls % (≥1 fall last six months) 62
Mean MNA SF (SD) 103 (25)
Mna-SF risk % 58
MNA-SF item Weight
loss > 3 kg last three months %
3
MNA-SF item BMI < 19 (%) 6
BMI 19–20 (%) 13
BMI 21–23 (%) 18
BMI > 23 (%) 63
Mean BMI (SD) 25 (476)
Mean MNS (SD) 23 (345)
MNS risk % 27
Presence of pressure ulcers % 10
Mean number of medication (SD) 685 (304)
Mean Number of diseases (SD) 29 (133)
Mobility
Wheelchair bound (%) 30
Walking with assistance (%) 15
Walking with or without aid (%) 55
Bedridden (%) 0
Mean MMSE (SD)* 17 (63)
MMSE<24 points (%) 68
Hospital care last six months % 24
Emergency care last six months % 6
*MMSE was not performed on allparticipants.Due to cognitive
dysfunction,blindness or impaired hearing,questions could not be
understood for all, which made 83% eligible to assess.
© 2016 John Wiley & Sons Ltd
Journal of Clinical Nursing, 25, 940–950 943
Original article Risk assessment among nursing home residents
weight loss (0–3 points), mobility (0–2 points), acute diseases
or psychologicalstress (0 or 2 points),neuropsychological
impairment (0–2 points) and BMI (0–3 points).The higher
the value the lower the risk. The maximum MNA-SF score is
14 points. A score of 7 points or less indicates malnutrition,
8–11 indicates risk of malnutrition and 12–14 points indi-
cates no risk for malnutrition.
Risk for pressure ulcers was assessed with MNS. In addi-
tion to the more internationally known Norton Scale, MNS
also includestwo items assessing nutrition status.MNS
consists of seven items; mental condition, activity, mobility,
food intake,fluid intake,incontinence and generalphysical
condition.Each item is assessed with a range from 1 (lack
of function) to 4 (normalfunction).The maximum score is
28 and a score at20 or lower indicates an increased risk
for pressure ulcers (Ek 1987).
The scales internal consistency in this study, measured by
Cronbach’salpha showed 05 for DFRI, 066 for MNS
and 045 for MNA-SF.
In the SHADES study the nursesexamined the partici-
pants in many ways regarding differentassessmentscales,
blood testing,use of drugs,different measurements etc.For
this presentstudy we used data from DFRI, MNA-SF,
MNS, data of weight and data of eventual presence of pres-
sure ulcers.Pressure ulcerswere graded as:(1) persistent
discoloration,with intactskin surface;(2) epithelialdam-
age;(3) damage to the fullthickness of the skin without a
deep cavity and (4) damage to the full thickness of the skin
with deep cavity.In this study,all kinds of pressure ulcers
were taken into account,but not gradated,only counted as
existing ornot. Description ofthe study population con-
cerning prevalence and risks are presented in Table 1.
Statistical analyses
Descriptive statistics were used for baseline characteristics
and to describe outcomes at 6 and 12 months.For analys-
ing outcomesin relation to risks atsix and 12 months a
subsample of255 was used,that is, participantswith at
least three occasions of measure (baseline and at least two
follow-ups).The proportions ofbeing atrisk or not were
compared using a two-sided Chi square test. To analyse the
longitudinalchanges of the totalscores in the three assess-
mentsscales,GeneralLinear Model (GLM with repeated
measures) was used.For the GLM analyses a subsample of
116 was used,that is, those who participated during the
whole study period (30 months).Cox regressions were per-
formed to analysefactorsrelated to the outcomesfalls,
weightloss and pressure ulcers.Three outcome variables
were created ‘Falls lastsix months’(coded as 1),‘Weight
loss with atleast10% or at least6 kg’ (coded as 1)and
‘Presence of pressure ulcers’(coded as 1).Those who even-
tually already had suffered from any oftheseeventsat
baseline were included in the analyses with the purpose to
increase the size of the population.Exclusion of these indi-
viduals would have decreased the population and made it
less representative fora nursing home population.How-
ever,the time variable for those who already suffered from
some kind of pressure ulcer at baseline was time coded with
0. For the other two outcomesthe time variablewas
determined as time from baseline to the follow-up visit date
when the outcome variable first was detected.If no occur-
rence ofthe outcome variables during the two follow-ups
was detected,the time variable was determined to be
approximately one year, or, if the participant was deceased,
time to death was calculated. Three Cox regression analyses
in two steps were performed foreach outcome.Baseline
data on age,gender,number of drugs and number of diag-
noses were included as covariates in the first step to control
Table 1 Description of study population at baseline
n = 331
Age (mean) 84
Mean DFRI (SD) 48 (16)
DFRI risk % 93
Falls % (≥1 fall last six months) 62
Mean MNA SF (SD) 103 (25)
Mna-SF risk % 58
MNA-SF item Weight
loss > 3 kg last three months %
3
MNA-SF item BMI < 19 (%) 6
BMI 19–20 (%) 13
BMI 21–23 (%) 18
BMI > 23 (%) 63
Mean BMI (SD) 25 (476)
Mean MNS (SD) 23 (345)
MNS risk % 27
Presence of pressure ulcers % 10
Mean number of medication (SD) 685 (304)
Mean Number of diseases (SD) 29 (133)
Mobility
Wheelchair bound (%) 30
Walking with assistance (%) 15
Walking with or without aid (%) 55
Bedridden (%) 0
Mean MMSE (SD)* 17 (63)
MMSE<24 points (%) 68
Hospital care last six months % 24
Emergency care last six months % 6
*MMSE was not performed on allparticipants.Due to cognitive
dysfunction,blindness or impaired hearing,questions could not be
understood for all, which made 83% eligible to assess.
© 2016 John Wiley & Sons Ltd
Journal of Clinical Nursing, 25, 940–950 943
Original article Risk assessment among nursing home residents
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
for sociodemographics and health.In the second step,the
scale items for one scale were included as covariates.This
procedure wasthen repeated foreach scale,respectively,
which made a total of nine regression models. Finally, three
two-step Cox regression analyses were performed with the
sociodemographics described above as covariates in the first
step and the totalscores of each scale as covariates in the
next step.
Analyseswere performed using theSPSS statisticalsoft-
ware (IBM SPSS version 20, IBM Corp, Armonk, NY).
p-values ≤005 were considered statistically significant.
Results
Description of study population
A sample oftotal 331 residents had consecutive and com-
plete data from baseline to at least one follow-up. Of those,
mean age was 84 years (SD 7) and 71% were female.The
subjects had been staying at the nursing homes for in med-
ian 10 months.At baseline (Table 1),the study population
demonstrated a considerable risk forfall n = 307 (93%),
malnutrition n = 192 (58%)and pressureulcers n = 89
(27%). Combination of risks were more common than sin-
gle risk as 25% had risk for both fall, malnutrition and
pressure ulcers and 32% had risk for two ofthese condi-
tions.Single risk was demonstrated at39%, but only 4%
of the sample scored no risk atany of the three assessing
scales at baseline.
To see how the totalscore values for DFRI,MNS and
MNA-SF varied over time, repeated measureswere anal-
ysed in several GLMs. The result showed statistically signif-
icant impaired mean scores;MNS decreased from 2309 to
2094 (p < 0001),MNA-SF decreased from 1076 to 934
(p < 0001) and DRFI increasedfrom 458 to 488
(p < 005).
Events related to risk
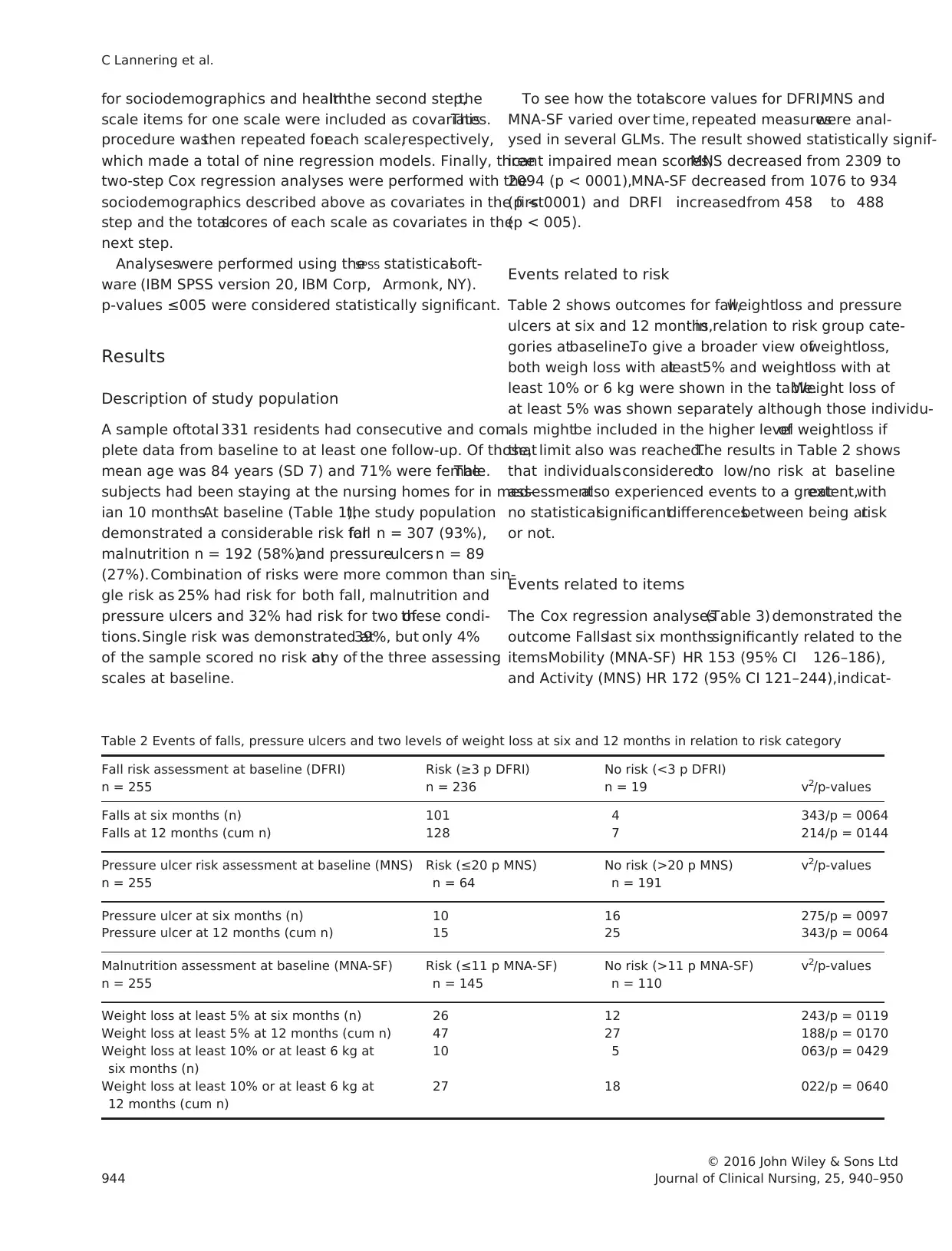
Table 2 shows outcomes for fall,weightloss and pressure
ulcers at six and 12 months,in relation to risk group cate-
gories atbaseline.To give a broader view ofweightloss,
both weigh loss with atleast5% and weightloss with at
least 10% or 6 kg were shown in the table.Weight loss of
at least 5% was shown separately although those individu-
als mightbe included in the higher levelof weightloss if
that limit also was reached.The results in Table 2 shows
that individualsconsideredto low/no risk at baseline
assessmentalso experienced events to a greatextent,with
no statisticalsignificantdifferencesbetween being atrisk
or not.
Events related to items
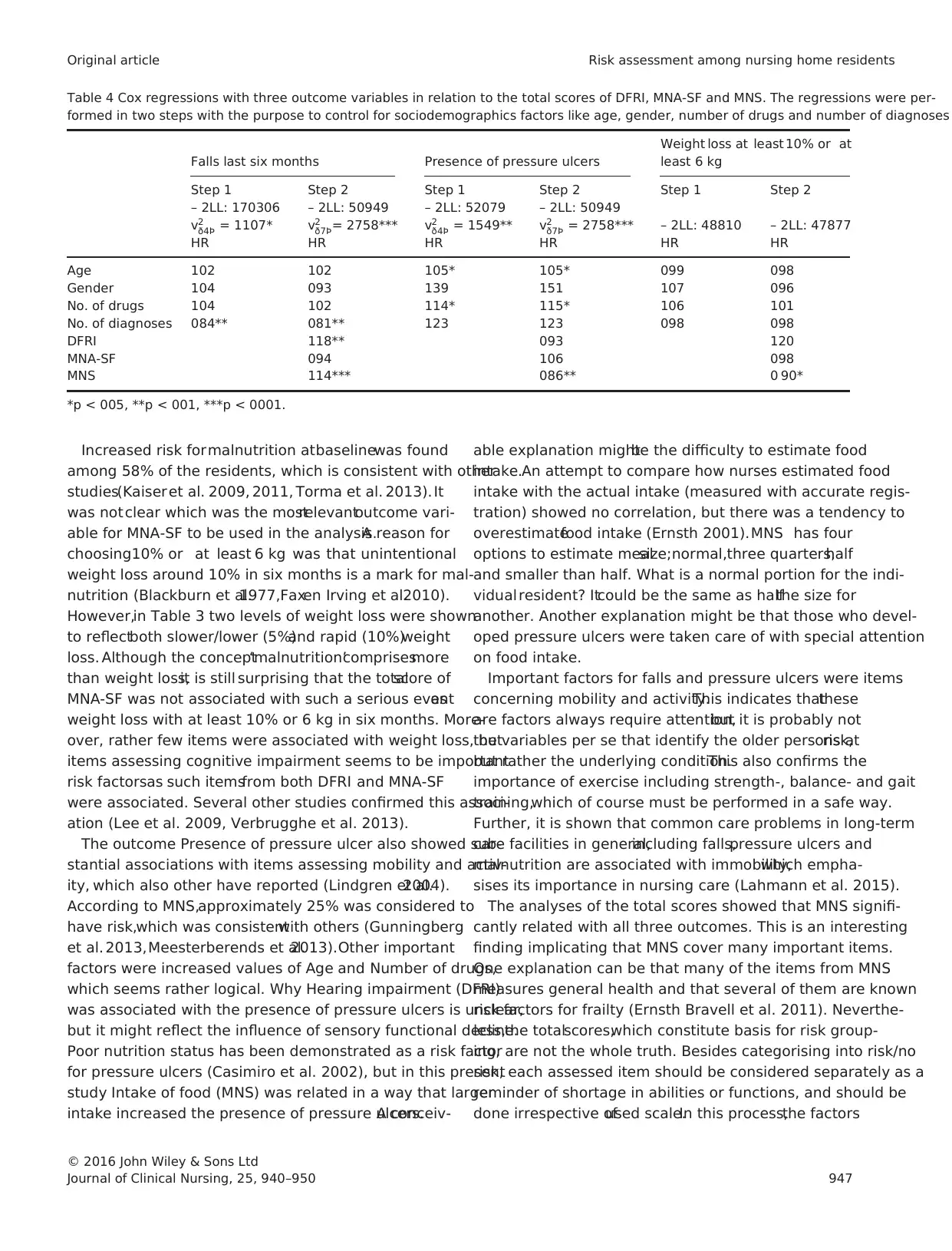
The Cox regression analyses(Table 3) demonstrated the
outcome Fallslast six monthssignificantly related to the
itemsMobility (MNA-SF) HR 153 (95% CI 126–186),
and Activity (MNS) HR 172 (95% CI 121–244),indicat-
Table 2 Events of falls, pressure ulcers and two levels of weight loss at six and 12 months in relation to risk category
Fall risk assessment at baseline (DFRI)
n = 255
Risk (≥3 p DFRI)
n = 236
No risk (<3 p DFRI)
n = 19 v2/p-values
Falls at six months (n) 101 4 343/p = 0064
Falls at 12 months (cum n) 128 7 214/p = 0144
Pressure ulcer risk assessment at baseline (MNS)
n = 255
Risk (≤20 p MNS)
n = 64
No risk (>20 p MNS)
n = 191
v2/p-values
Pressure ulcer at six months (n) 10 16 275/p = 0097
Pressure ulcer at 12 months (cum n) 15 25 343/p = 0064
Malnutrition assessment at baseline (MNA-SF)
n = 255
Risk (≤11 p MNA-SF)
n = 145
No risk (>11 p MNA-SF)
n = 110
v2/p-values
Weight loss at least 5% at six months (n) 26 12 243/p = 0119
Weight loss at least 5% at 12 months (cum n) 47 27 188/p = 0170
Weight loss at least 10% or at least 6 kg at
six months (n)
10 5 063/p = 0429
Weight loss at least 10% or at least 6 kg at
12 months (cum n)
27 18 022/p = 0640
© 2016 John Wiley & Sons Ltd
944 Journal of Clinical Nursing, 25, 940–950
C Lannering et al.
scale items for one scale were included as covariates.This
procedure wasthen repeated foreach scale,respectively,
which made a total of nine regression models. Finally, three
two-step Cox regression analyses were performed with the
sociodemographics described above as covariates in the first
step and the totalscores of each scale as covariates in the
next step.
Analyseswere performed using theSPSS statisticalsoft-
ware (IBM SPSS version 20, IBM Corp, Armonk, NY).
p-values ≤005 were considered statistically significant.
Results
Description of study population
A sample oftotal 331 residents had consecutive and com-
plete data from baseline to at least one follow-up. Of those,
mean age was 84 years (SD 7) and 71% were female.The
subjects had been staying at the nursing homes for in med-
ian 10 months.At baseline (Table 1),the study population
demonstrated a considerable risk forfall n = 307 (93%),
malnutrition n = 192 (58%)and pressureulcers n = 89
(27%). Combination of risks were more common than sin-
gle risk as 25% had risk for both fall, malnutrition and
pressure ulcers and 32% had risk for two ofthese condi-
tions.Single risk was demonstrated at39%, but only 4%
of the sample scored no risk atany of the three assessing
scales at baseline.
To see how the totalscore values for DFRI,MNS and
MNA-SF varied over time, repeated measureswere anal-
ysed in several GLMs. The result showed statistically signif-
icant impaired mean scores;MNS decreased from 2309 to
2094 (p < 0001),MNA-SF decreased from 1076 to 934
(p < 0001) and DRFI increasedfrom 458 to 488
(p < 005).
Events related to risk
Table 2 shows outcomes for fall,weightloss and pressure
ulcers at six and 12 months,in relation to risk group cate-
gories atbaseline.To give a broader view ofweightloss,
both weigh loss with atleast5% and weightloss with at
least 10% or 6 kg were shown in the table.Weight loss of
at least 5% was shown separately although those individu-
als mightbe included in the higher levelof weightloss if
that limit also was reached.The results in Table 2 shows
that individualsconsideredto low/no risk at baseline
assessmentalso experienced events to a greatextent,with
no statisticalsignificantdifferencesbetween being atrisk
or not.
Events related to items
The Cox regression analyses(Table 3) demonstrated the
outcome Fallslast six monthssignificantly related to the
itemsMobility (MNA-SF) HR 153 (95% CI 126–186),
and Activity (MNS) HR 172 (95% CI 121–244),indicat-
Table 2 Events of falls, pressure ulcers and two levels of weight loss at six and 12 months in relation to risk category
Fall risk assessment at baseline (DFRI)
n = 255
Risk (≥3 p DFRI)
n = 236
No risk (<3 p DFRI)
n = 19 v2/p-values
Falls at six months (n) 101 4 343/p = 0064
Falls at 12 months (cum n) 128 7 214/p = 0144
Pressure ulcer risk assessment at baseline (MNS)
n = 255
Risk (≤20 p MNS)
n = 64
No risk (>20 p MNS)
n = 191
v2/p-values
Pressure ulcer at six months (n) 10 16 275/p = 0097
Pressure ulcer at 12 months (cum n) 15 25 343/p = 0064
Malnutrition assessment at baseline (MNA-SF)
n = 255
Risk (≤11 p MNA-SF)
n = 145
No risk (>11 p MNA-SF)
n = 110
v2/p-values
Weight loss at least 5% at six months (n) 26 12 243/p = 0119
Weight loss at least 5% at 12 months (cum n) 47 27 188/p = 0170
Weight loss at least 10% or at least 6 kg at
six months (n)
10 5 063/p = 0429
Weight loss at least 10% or at least 6 kg at
12 months (cum n)
27 18 022/p = 0640
© 2016 John Wiley & Sons Ltd
944 Journal of Clinical Nursing, 25, 940–950
C Lannering et al.
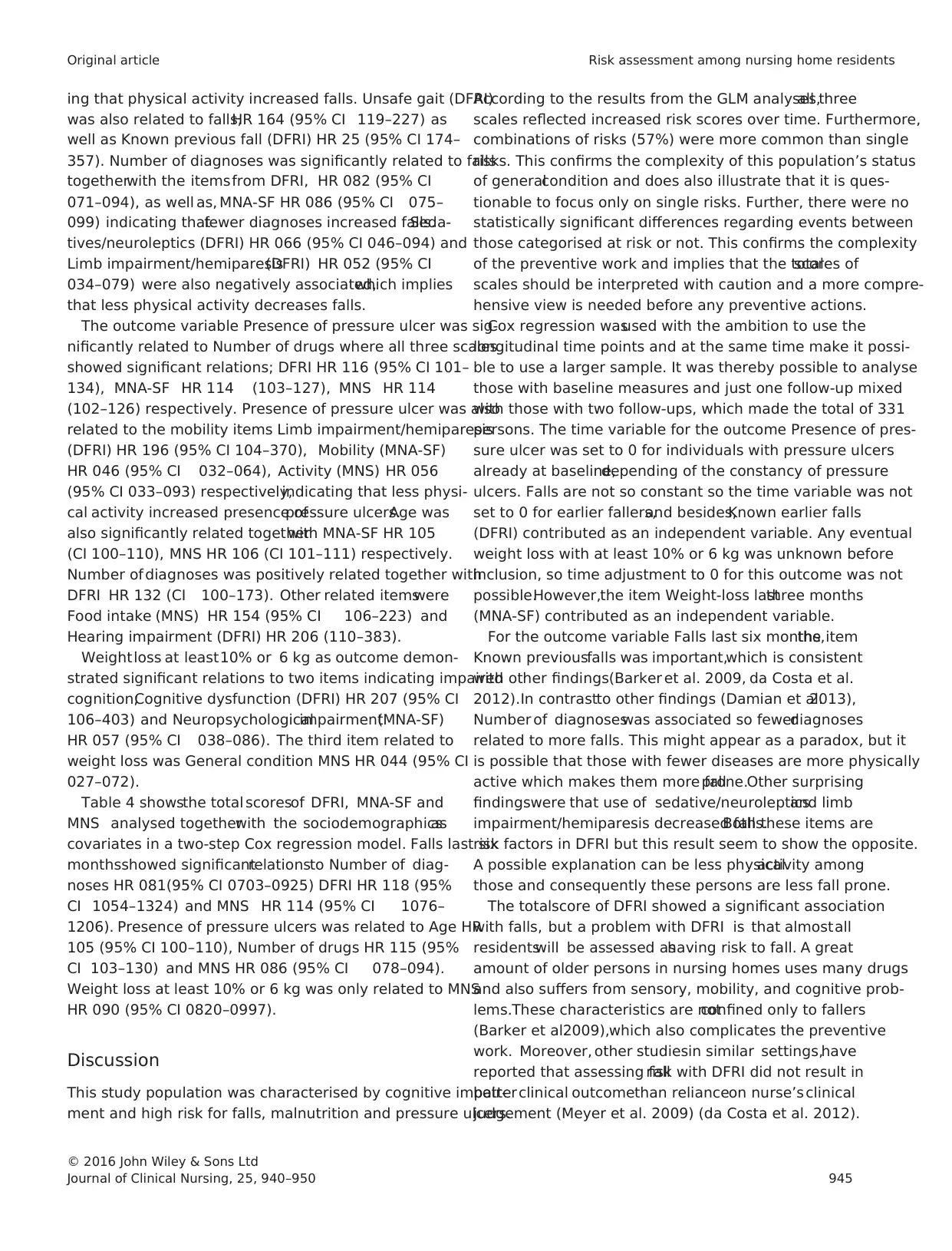
ing that physical activity increased falls. Unsafe gait (DFRI)
was also related to falls,HR 164 (95% CI 119–227) as
well as Known previous fall (DFRI) HR 25 (95% CI 174–
357). Number of diagnoses was significantly related to falls
togetherwith the itemsfrom DFRI, HR 082 (95% CI
071–094), as well as, MNA-SF HR 086 (95% CI 075–
099) indicating thatfewer diagnoses increased falls.Seda-
tives/neuroleptics (DFRI) HR 066 (95% CI 046–094) and
Limb impairment/hemiparesis(DFRI) HR 052 (95% CI
034–079) were also negatively associated,which implies
that less physical activity decreases falls.
The outcome variable Presence of pressure ulcer was sig-
nificantly related to Number of drugs where all three scales
showed significant relations; DFRI HR 116 (95% CI 101–
134), MNA-SF HR 114 (103–127), MNS HR 114
(102–126) respectively. Presence of pressure ulcer was also
related to the mobility items Limb impairment/hemiparesis
(DFRI) HR 196 (95% CI 104–370), Mobility (MNA-SF)
HR 046 (95% CI 032–064), Activity (MNS) HR 056
(95% CI 033–093) respectively,indicating that less physi-
cal activity increased presence ofpressure ulcers.Age was
also significantly related togetherwith MNA-SF HR 105
(CI 100–110), MNS HR 106 (CI 101–111) respectively.
Number of diagnoses was positively related together with
DFRI HR 132 (CI 100–173). Other related itemswere
Food intake (MNS) HR 154 (95% CI 106–223) and
Hearing impairment (DFRI) HR 206 (110–383).
Weightloss at least10% or 6 kg as outcome demon-
strated significant relations to two items indicating impaired
cognition;Cognitive dysfunction (DFRI) HR 207 (95% CI
106–403) and Neuropsychologicalimpairment(MNA-SF)
HR 057 (95% CI 038–086). The third item related to
weight loss was General condition MNS HR 044 (95% CI
027–072).
Table 4 showsthe total scoresof DFRI, MNA-SF and
MNS analysed togetherwith the sociodemographicsas
covariates in a two-step Cox regression model. Falls last six
monthsshowed significantrelationsto Number of diag-
noses HR 081(95% CI 0703–0925) DFRI HR 118 (95%
CI 1054–1324) and MNS HR 114 (95% CI 1076–
1206). Presence of pressure ulcers was related to Age HR
105 (95% CI 100–110), Number of drugs HR 115 (95%
CI 103–130) and MNS HR 086 (95% CI 078–094).
Weight loss at least 10% or 6 kg was only related to MNS
HR 090 (95% CI 0820–0997).
Discussion
This study population was characterised by cognitive impair-
ment and high risk for falls, malnutrition and pressure ulcers.
According to the results from the GLM analyses,all three
scales reflected increased risk scores over time. Furthermore,
combinations of risks (57%) were more common than single
risks. This confirms the complexity of this population’s status
of generalcondition and does also illustrate that it is ques-
tionable to focus only on single risks. Further, there were no
statistically significant differences regarding events between
those categorised at risk or not. This confirms the complexity
of the preventive work and implies that the totalscores of
scales should be interpreted with caution and a more compre-
hensive view is needed before any preventive actions.
Cox regression wasused with the ambition to use the
longitudinal time points and at the same time make it possi-
ble to use a larger sample. It was thereby possible to analyse
those with baseline measures and just one follow-up mixed
with those with two follow-ups, which made the total of 331
persons. The time variable for the outcome Presence of pres-
sure ulcer was set to 0 for individuals with pressure ulcers
already at baseline,depending of the constancy of pressure
ulcers. Falls are not so constant so the time variable was not
set to 0 for earlier fallers,and besides,Known earlier falls
(DFRI) contributed as an independent variable. Any eventual
weight loss with at least 10% or 6 kg was unknown before
inclusion, so time adjustment to 0 for this outcome was not
possible.However,the item Weight-loss lastthree months
(MNA-SF) contributed as an independent variable.
For the outcome variable Falls last six months,the item
Known previousfalls was important,which is consistent
with other findings(Barker et al. 2009, da Costa et al.
2012).In contrastto other findings (Damian et al.2013),
Number of diagnoseswas associated so fewerdiagnoses
related to more falls. This might appear as a paradox, but it
is possible that those with fewer diseases are more physically
active which makes them more fallprone.Other surprising
findingswere that use of sedative/neurolepticsand limb
impairment/hemiparesis decreased falls.Both these items are
risk factors in DFRI but this result seem to show the opposite.
A possible explanation can be less physicalactivity among
those and consequently these persons are less fall prone.
The totalscore of DFRI showed a significant association
with falls, but a problem with DFRI is that almostall
residentswill be assessed ashaving risk to fall. A great
amount of older persons in nursing homes uses many drugs
and also suffers from sensory, mobility, and cognitive prob-
lems.These characteristics are notconfined only to fallers
(Barker et al.2009),which also complicates the preventive
work. Moreover, other studiesin similar settings,have
reported that assessing fallrisk with DFRI did not result in
betterclinical outcomethan relianceon nurse’s clinical
judgement (Meyer et al. 2009) (da Costa et al. 2012).
© 2016 John Wiley & Sons Ltd
Journal of Clinical Nursing, 25, 940–950 945
Original article Risk assessment among nursing home residents
was also related to falls,HR 164 (95% CI 119–227) as
well as Known previous fall (DFRI) HR 25 (95% CI 174–
357). Number of diagnoses was significantly related to falls
togetherwith the itemsfrom DFRI, HR 082 (95% CI
071–094), as well as, MNA-SF HR 086 (95% CI 075–
099) indicating thatfewer diagnoses increased falls.Seda-
tives/neuroleptics (DFRI) HR 066 (95% CI 046–094) and
Limb impairment/hemiparesis(DFRI) HR 052 (95% CI
034–079) were also negatively associated,which implies
that less physical activity decreases falls.
The outcome variable Presence of pressure ulcer was sig-
nificantly related to Number of drugs where all three scales
showed significant relations; DFRI HR 116 (95% CI 101–
134), MNA-SF HR 114 (103–127), MNS HR 114
(102–126) respectively. Presence of pressure ulcer was also
related to the mobility items Limb impairment/hemiparesis
(DFRI) HR 196 (95% CI 104–370), Mobility (MNA-SF)
HR 046 (95% CI 032–064), Activity (MNS) HR 056
(95% CI 033–093) respectively,indicating that less physi-
cal activity increased presence ofpressure ulcers.Age was
also significantly related togetherwith MNA-SF HR 105
(CI 100–110), MNS HR 106 (CI 101–111) respectively.
Number of diagnoses was positively related together with
DFRI HR 132 (CI 100–173). Other related itemswere
Food intake (MNS) HR 154 (95% CI 106–223) and
Hearing impairment (DFRI) HR 206 (110–383).
Weightloss at least10% or 6 kg as outcome demon-
strated significant relations to two items indicating impaired
cognition;Cognitive dysfunction (DFRI) HR 207 (95% CI
106–403) and Neuropsychologicalimpairment(MNA-SF)
HR 057 (95% CI 038–086). The third item related to
weight loss was General condition MNS HR 044 (95% CI
027–072).
Table 4 showsthe total scoresof DFRI, MNA-SF and
MNS analysed togetherwith the sociodemographicsas
covariates in a two-step Cox regression model. Falls last six
monthsshowed significantrelationsto Number of diag-
noses HR 081(95% CI 0703–0925) DFRI HR 118 (95%
CI 1054–1324) and MNS HR 114 (95% CI 1076–
1206). Presence of pressure ulcers was related to Age HR
105 (95% CI 100–110), Number of drugs HR 115 (95%
CI 103–130) and MNS HR 086 (95% CI 078–094).
Weight loss at least 10% or 6 kg was only related to MNS
HR 090 (95% CI 0820–0997).
Discussion
This study population was characterised by cognitive impair-
ment and high risk for falls, malnutrition and pressure ulcers.
According to the results from the GLM analyses,all three
scales reflected increased risk scores over time. Furthermore,
combinations of risks (57%) were more common than single
risks. This confirms the complexity of this population’s status
of generalcondition and does also illustrate that it is ques-
tionable to focus only on single risks. Further, there were no
statistically significant differences regarding events between
those categorised at risk or not. This confirms the complexity
of the preventive work and implies that the totalscores of
scales should be interpreted with caution and a more compre-
hensive view is needed before any preventive actions.
Cox regression wasused with the ambition to use the
longitudinal time points and at the same time make it possi-
ble to use a larger sample. It was thereby possible to analyse
those with baseline measures and just one follow-up mixed
with those with two follow-ups, which made the total of 331
persons. The time variable for the outcome Presence of pres-
sure ulcer was set to 0 for individuals with pressure ulcers
already at baseline,depending of the constancy of pressure
ulcers. Falls are not so constant so the time variable was not
set to 0 for earlier fallers,and besides,Known earlier falls
(DFRI) contributed as an independent variable. Any eventual
weight loss with at least 10% or 6 kg was unknown before
inclusion, so time adjustment to 0 for this outcome was not
possible.However,the item Weight-loss lastthree months
(MNA-SF) contributed as an independent variable.
For the outcome variable Falls last six months,the item
Known previousfalls was important,which is consistent
with other findings(Barker et al. 2009, da Costa et al.
2012).In contrastto other findings (Damian et al.2013),
Number of diagnoseswas associated so fewerdiagnoses
related to more falls. This might appear as a paradox, but it
is possible that those with fewer diseases are more physically
active which makes them more fallprone.Other surprising
findingswere that use of sedative/neurolepticsand limb
impairment/hemiparesis decreased falls.Both these items are
risk factors in DFRI but this result seem to show the opposite.
A possible explanation can be less physicalactivity among
those and consequently these persons are less fall prone.
The totalscore of DFRI showed a significant association
with falls, but a problem with DFRI is that almostall
residentswill be assessed ashaving risk to fall. A great
amount of older persons in nursing homes uses many drugs
and also suffers from sensory, mobility, and cognitive prob-
lems.These characteristics are notconfined only to fallers
(Barker et al.2009),which also complicates the preventive
work. Moreover, other studiesin similar settings,have
reported that assessing fallrisk with DFRI did not result in
betterclinical outcomethan relianceon nurse’s clinical
judgement (Meyer et al. 2009) (da Costa et al. 2012).
© 2016 John Wiley & Sons Ltd
Journal of Clinical Nursing, 25, 940–950 945
Original article Risk assessment among nursing home residents
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
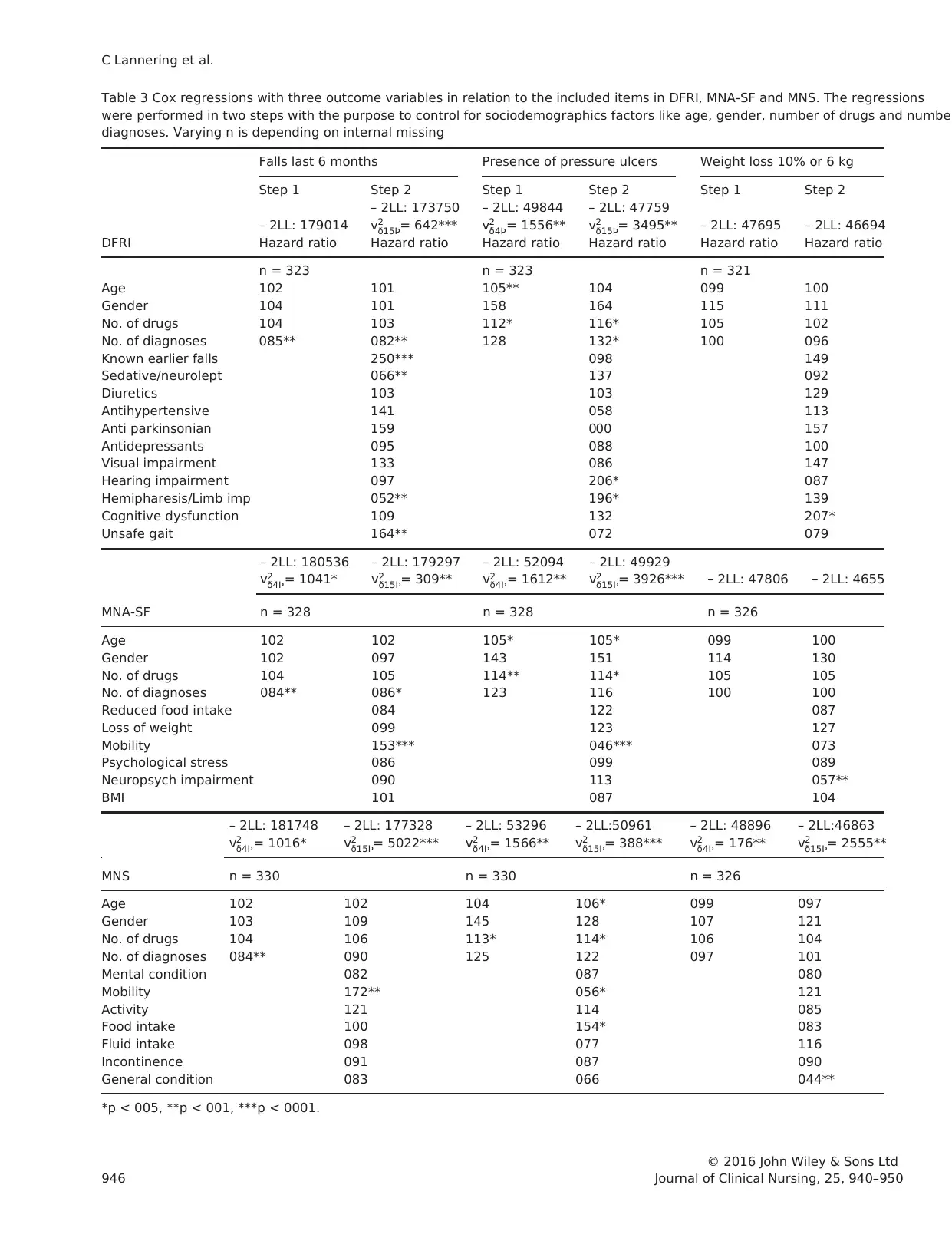
Table 3 Cox regressions with three outcome variables in relation to the included items in DFRI, MNA-SF and MNS. The regressions
were performed in two steps with the purpose to control for sociodemographics factors like age, gender, number of drugs and number
diagnoses. Varying n is depending on internal missing
DFRI
Falls last 6 months Presence of pressure ulcers Weight loss 10% or 6 kg
Step 1 Step 2 Step 1 Step 2 Step 1 Step 2
– 2LL: 179014
– 2LL: 173750
v2
ð15Þ= 642***
– 2LL: 49844
v2
ð4Þ= 1556**
– 2LL: 47759
v2
ð15Þ= 3495** – 2LL: 47695 – 2LL: 46694
Hazard ratio Hazard ratio Hazard ratio Hazard ratio Hazard ratio Hazard ratio
n = 323 n = 323 n = 321
Age 102 101 105** 104 099 100
Gender 104 101 158 164 115 111
No. of drugs 104 103 112* 116* 105 102
No. of diagnoses 085** 082** 128 132* 100 096
Known earlier falls 250*** 098 149
Sedative/neurolept 066** 137 092
Diuretics 103 103 129
Antihypertensive 141 058 113
Anti parkinsonian 159 000 157
Antidepressants 095 088 100
Visual impairment 133 086 147
Hearing impairment 097 206* 087
Hemipharesis/Limb imp 052** 196* 139
Cognitive dysfunction 109 132 207*
Unsafe gait 164** 072 079
– 2LL: 180536
v2
ð4Þ= 1041*
– 2LL: 179297
v2
ð15Þ= 309**
– 2LL: 52094
v2
ð4Þ= 1612**
– 2LL: 49929
v2
ð15Þ= 3926*** – 2LL: 47806 – 2LL: 4655
MNA-SF n = 328 n = 328 n = 326
Age 102 102 105* 105* 099 100
Gender 102 097 143 151 114 130
No. of drugs 104 105 114** 114* 105 105
No. of diagnoses 084** 086* 123 116 100 100
Reduced food intake 084 122 087
Loss of weight 099 123 127
Mobility 153*** 046*** 073
Psychological stress 086 099 089
Neuropsych impairment 090 113 057**
BMI 101 087 104
– 2LL: 181748
v2
ð4Þ= 1016*
– 2LL: 177328
v2
ð15Þ= 5022***
– 2LL: 53296
v2
ð4Þ= 1566**
– 2LL:50961
v2
ð15Þ= 388***
– 2LL: 48896
v2
ð4Þ= 176**
– 2LL:46863
v2
ð15Þ= 2555**
MNS n = 330 n = 330 n = 326
Age 102 102 104 106* 099 097
Gender 103 109 145 128 107 121
No. of drugs 104 106 113* 114* 106 104
No. of diagnoses 084** 090 125 122 097 101
Mental condition 082 087 080
Mobility 172** 056* 121
Activity 121 114 085
Food intake 100 154* 083
Fluid intake 098 077 116
Incontinence 091 087 090
General condition 083 066 044**
*p < 005, **p < 001, ***p < 0001.
© 2016 John Wiley & Sons Ltd
946 Journal of Clinical Nursing, 25, 940–950
C Lannering et al.
were performed in two steps with the purpose to control for sociodemographics factors like age, gender, number of drugs and number
diagnoses. Varying n is depending on internal missing
DFRI
Falls last 6 months Presence of pressure ulcers Weight loss 10% or 6 kg
Step 1 Step 2 Step 1 Step 2 Step 1 Step 2
– 2LL: 179014
– 2LL: 173750
v2
ð15Þ= 642***
– 2LL: 49844
v2
ð4Þ= 1556**
– 2LL: 47759
v2
ð15Þ= 3495** – 2LL: 47695 – 2LL: 46694
Hazard ratio Hazard ratio Hazard ratio Hazard ratio Hazard ratio Hazard ratio
n = 323 n = 323 n = 321
Age 102 101 105** 104 099 100
Gender 104 101 158 164 115 111
No. of drugs 104 103 112* 116* 105 102
No. of diagnoses 085** 082** 128 132* 100 096
Known earlier falls 250*** 098 149
Sedative/neurolept 066** 137 092
Diuretics 103 103 129
Antihypertensive 141 058 113
Anti parkinsonian 159 000 157
Antidepressants 095 088 100
Visual impairment 133 086 147
Hearing impairment 097 206* 087
Hemipharesis/Limb imp 052** 196* 139
Cognitive dysfunction 109 132 207*
Unsafe gait 164** 072 079
– 2LL: 180536
v2
ð4Þ= 1041*
– 2LL: 179297
v2
ð15Þ= 309**
– 2LL: 52094
v2
ð4Þ= 1612**
– 2LL: 49929
v2
ð15Þ= 3926*** – 2LL: 47806 – 2LL: 4655
MNA-SF n = 328 n = 328 n = 326
Age 102 102 105* 105* 099 100
Gender 102 097 143 151 114 130
No. of drugs 104 105 114** 114* 105 105
No. of diagnoses 084** 086* 123 116 100 100
Reduced food intake 084 122 087
Loss of weight 099 123 127
Mobility 153*** 046*** 073
Psychological stress 086 099 089
Neuropsych impairment 090 113 057**
BMI 101 087 104
– 2LL: 181748
v2
ð4Þ= 1016*
– 2LL: 177328
v2
ð15Þ= 5022***
– 2LL: 53296
v2
ð4Þ= 1566**
– 2LL:50961
v2
ð15Þ= 388***
– 2LL: 48896
v2
ð4Þ= 176**
– 2LL:46863
v2
ð15Þ= 2555**
MNS n = 330 n = 330 n = 326
Age 102 102 104 106* 099 097
Gender 103 109 145 128 107 121
No. of drugs 104 106 113* 114* 106 104
No. of diagnoses 084** 090 125 122 097 101
Mental condition 082 087 080
Mobility 172** 056* 121
Activity 121 114 085
Food intake 100 154* 083
Fluid intake 098 077 116
Incontinence 091 087 090
General condition 083 066 044**
*p < 005, **p < 001, ***p < 0001.
© 2016 John Wiley & Sons Ltd
946 Journal of Clinical Nursing, 25, 940–950
C Lannering et al.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Increased risk formalnutrition atbaselinewas found
among 58% of the residents, which is consistent with other
studies(Kaiser et al. 2009, 2011, Torma et al. 2013). It
was not clear which was the mostrelevantoutcome vari-
able for MNA-SF to be used in the analysis.A reason for
choosing10% or at least 6 kg was that unintentional
weight loss around 10% in six months is a mark for mal-
nutrition (Blackburn et al.1977,Faxen Irving et al.2010).
However,in Table 3 two levels of weight loss were shown
to reflectboth slower/lower (5%)and rapid (10%)weight
loss. Although the concept‘malnutrition’comprisesmore
than weight loss,it is still surprising that the totalscore of
MNA-SF was not associated with such a serious eventas
weight loss with at least 10% or 6 kg in six months. More-
over, rather few items were associated with weight loss, but
items assessing cognitive impairment seems to be important
risk factorsas such itemsfrom both DFRI and MNA-SF
were associated. Several other studies confirmed this associ-
ation (Lee et al. 2009, Verbrugghe et al. 2013).
The outcome Presence of pressure ulcer also showed sub-
stantial associations with items assessing mobility and activ-
ity, which also other have reported (Lindgren et al.2004).
According to MNS,approximately 25% was considered to
have risk,which was consistentwith others (Gunningberg
et al. 2013,Meesterberends et al.2013).Other important
factors were increased values of Age and Number of drugs,
which seems rather logical. Why Hearing impairment (DFRI)
was associated with the presence of pressure ulcers is unclear,
but it might reflect the influence of sensory functional decline.
Poor nutrition status has been demonstrated as a risk factor
for pressure ulcers (Casimiro et al. 2002), but in this present
study Intake of food (MNS) was related in a way that larger
intake increased the presence of pressure ulcers.A conceiv-
able explanation mightbe the difficulty to estimate food
intake.An attempt to compare how nurses estimated food
intake with the actual intake (measured with accurate regis-
tration) showed no correlation, but there was a tendency to
overestimatefood intake (Ernsth 2001).MNS has four
options to estimate mealsize;normal,three quarters,half
and smaller than half. What is a normal portion for the indi-
vidual resident? Itcould be the same as halfthe size for
another. Another explanation might be that those who devel-
oped pressure ulcers were taken care of with special attention
on food intake.
Important factors for falls and pressure ulcers were items
concerning mobility and activity.This indicates thatthese
are factors always require attention,but it is probably not
the variables per se that identify the older persons atrisk,
but rather the underlying condition.This also confirms the
importance of exercise including strength-, balance- and gait
training,which of course must be performed in a safe way.
Further, it is shown that common care problems in long-term
care facilities in general,including falls,pressure ulcers and
malnutrition are associated with immobility,which empha-
sises its importance in nursing care (Lahmann et al. 2015).
The analyses of the total scores showed that MNS signifi-
cantly related with all three outcomes. This is an interesting
finding implicating that MNS cover many important items.
One explanation can be that many of the items from MNS
measures general health and that several of them are known
risk factors for frailty (Ernsth Bravell et al. 2011). Neverthe-
less,the totalscores,which constitute basis for risk group-
ing, are not the whole truth. Besides categorising into risk/no
risk, each assessed item should be considered separately as a
reminder of shortage in abilities or functions, and should be
done irrespective ofused scale.In this process,the factors
Table 4 Cox regressions with three outcome variables in relation to the total scores of DFRI, MNA-SF and MNS. The regressions were per-
formed in two steps with the purpose to control for sociodemographics factors like age, gender, number of drugs and number of diagnoses
Falls last six months Presence of pressure ulcers
Weight loss at least 10% or at
least 6 kg
Step 1 Step 2 Step 1 Step 2 Step 1 Step 2
– 2LL: 170306
v2
ð4Þ = 1107*
– 2LL: 50949
v2
ð7Þ= 2758***
– 2LL: 52079
v2
ð4Þ = 1549**
– 2LL: 50949
v2
ð7Þ = 2758*** – 2LL: 48810 – 2LL: 47877
HR HR HR HR HR HR
Age 102 102 105* 105* 099 098
Gender 104 093 139 151 107 096
No. of drugs 104 102 114* 115* 106 101
No. of diagnoses 084** 081** 123 123 098 098
DFRI 118** 093 120
MNA-SF 094 106 098
MNS 114*** 086** 0 90*
*p < 005, **p < 001, ***p < 0001.
© 2016 John Wiley & Sons Ltd
Journal of Clinical Nursing, 25, 940–950 947
Original article Risk assessment among nursing home residents
among 58% of the residents, which is consistent with other
studies(Kaiser et al. 2009, 2011, Torma et al. 2013). It
was not clear which was the mostrelevantoutcome vari-
able for MNA-SF to be used in the analysis.A reason for
choosing10% or at least 6 kg was that unintentional
weight loss around 10% in six months is a mark for mal-
nutrition (Blackburn et al.1977,Faxen Irving et al.2010).
However,in Table 3 two levels of weight loss were shown
to reflectboth slower/lower (5%)and rapid (10%)weight
loss. Although the concept‘malnutrition’comprisesmore
than weight loss,it is still surprising that the totalscore of
MNA-SF was not associated with such a serious eventas
weight loss with at least 10% or 6 kg in six months. More-
over, rather few items were associated with weight loss, but
items assessing cognitive impairment seems to be important
risk factorsas such itemsfrom both DFRI and MNA-SF
were associated. Several other studies confirmed this associ-
ation (Lee et al. 2009, Verbrugghe et al. 2013).
The outcome Presence of pressure ulcer also showed sub-
stantial associations with items assessing mobility and activ-
ity, which also other have reported (Lindgren et al.2004).
According to MNS,approximately 25% was considered to
have risk,which was consistentwith others (Gunningberg
et al. 2013,Meesterberends et al.2013).Other important
factors were increased values of Age and Number of drugs,
which seems rather logical. Why Hearing impairment (DFRI)
was associated with the presence of pressure ulcers is unclear,
but it might reflect the influence of sensory functional decline.
Poor nutrition status has been demonstrated as a risk factor
for pressure ulcers (Casimiro et al. 2002), but in this present
study Intake of food (MNS) was related in a way that larger
intake increased the presence of pressure ulcers.A conceiv-
able explanation mightbe the difficulty to estimate food
intake.An attempt to compare how nurses estimated food
intake with the actual intake (measured with accurate regis-
tration) showed no correlation, but there was a tendency to
overestimatefood intake (Ernsth 2001).MNS has four
options to estimate mealsize;normal,three quarters,half
and smaller than half. What is a normal portion for the indi-
vidual resident? Itcould be the same as halfthe size for
another. Another explanation might be that those who devel-
oped pressure ulcers were taken care of with special attention
on food intake.
Important factors for falls and pressure ulcers were items
concerning mobility and activity.This indicates thatthese
are factors always require attention,but it is probably not
the variables per se that identify the older persons atrisk,
but rather the underlying condition.This also confirms the
importance of exercise including strength-, balance- and gait
training,which of course must be performed in a safe way.
Further, it is shown that common care problems in long-term
care facilities in general,including falls,pressure ulcers and
malnutrition are associated with immobility,which empha-
sises its importance in nursing care (Lahmann et al. 2015).
The analyses of the total scores showed that MNS signifi-
cantly related with all three outcomes. This is an interesting
finding implicating that MNS cover many important items.
One explanation can be that many of the items from MNS
measures general health and that several of them are known
risk factors for frailty (Ernsth Bravell et al. 2011). Neverthe-
less,the totalscores,which constitute basis for risk group-
ing, are not the whole truth. Besides categorising into risk/no
risk, each assessed item should be considered separately as a
reminder of shortage in abilities or functions, and should be
done irrespective ofused scale.In this process,the factors
Table 4 Cox regressions with three outcome variables in relation to the total scores of DFRI, MNA-SF and MNS. The regressions were per-
formed in two steps with the purpose to control for sociodemographics factors like age, gender, number of drugs and number of diagnoses
Falls last six months Presence of pressure ulcers
Weight loss at least 10% or at
least 6 kg
Step 1 Step 2 Step 1 Step 2 Step 1 Step 2
– 2LL: 170306
v2
ð4Þ = 1107*
– 2LL: 50949
v2
ð7Þ= 2758***
– 2LL: 52079
v2
ð4Þ = 1549**
– 2LL: 50949
v2
ð7Þ = 2758*** – 2LL: 48810 – 2LL: 47877
HR HR HR HR HR HR
Age 102 102 105* 105* 099 098
Gender 104 093 139 151 107 096
No. of drugs 104 102 114* 115* 106 101
No. of diagnoses 084** 081** 123 123 098 098
DFRI 118** 093 120
MNA-SF 094 106 098
MNS 114*** 086** 0 90*
*p < 005, **p < 001, ***p < 0001.
© 2016 John Wiley & Sons Ltd
Journal of Clinical Nursing, 25, 940–950 947
Original article Risk assessment among nursing home residents
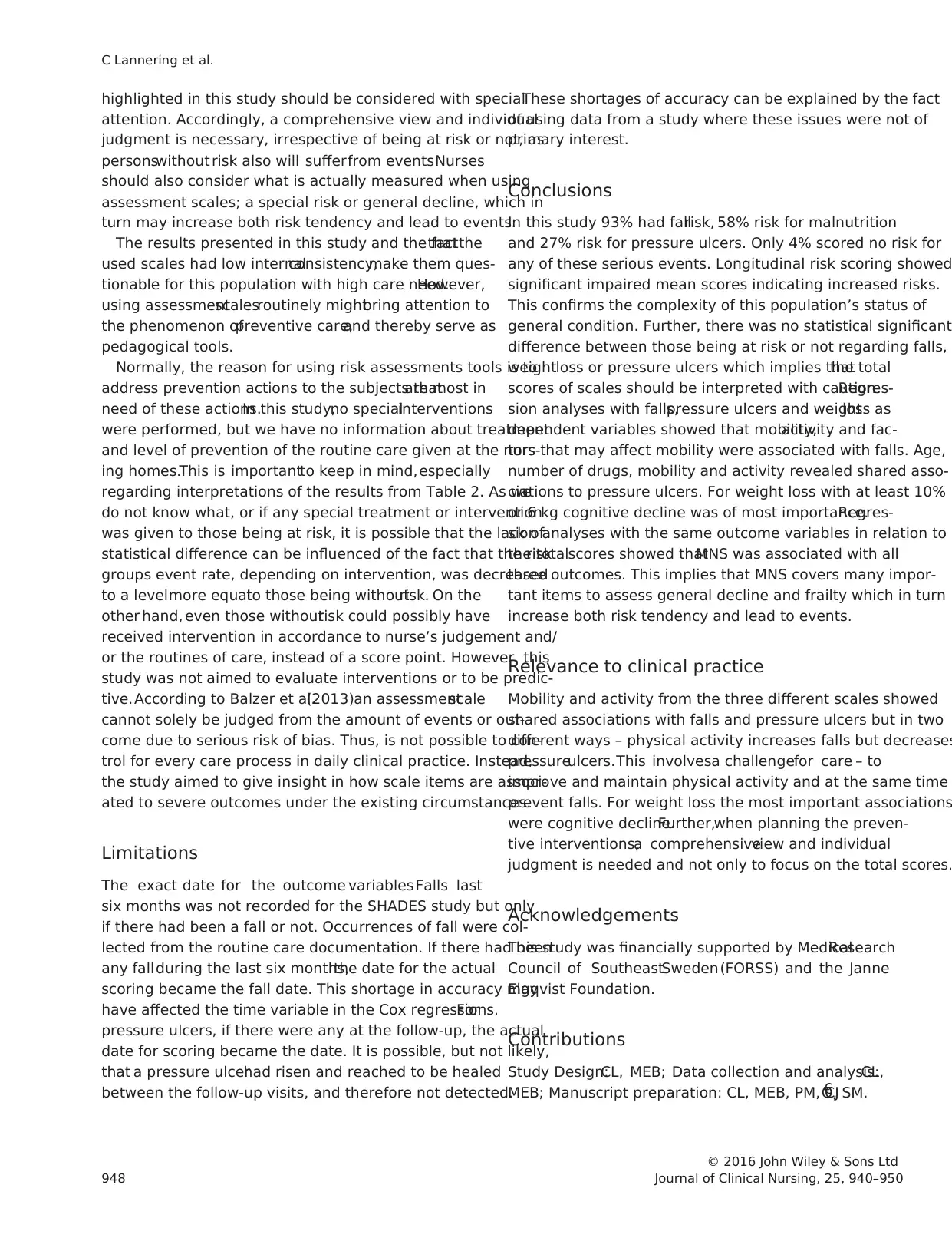
highlighted in this study should be considered with special
attention. Accordingly, a comprehensive view and individual
judgment is necessary, irrespective of being at risk or not, as
personswithout risk also will sufferfrom events.Nurses
should also consider what is actually measured when using
assessment scales; a special risk or general decline, which in
turn may increase both risk tendency and lead to events.
The results presented in this study and the factthat the
used scales had low internalconsistency,make them ques-
tionable for this population with high care need.However,
using assessmentscalesroutinely mightbring attention to
the phenomenon ofpreventive care,and thereby serve as
pedagogical tools.
Normally, the reason for using risk assessments tools is to
address prevention actions to the subjects thatare most in
need of these actions.In this study,no specialinterventions
were performed, but we have no information about treatment
and level of prevention of the routine care given at the nurs-
ing homes.This is importantto keep in mind,especially
regarding interpretations of the results from Table 2. As we
do not know what, or if any special treatment or intervention
was given to those being at risk, it is possible that the lack of
statistical difference can be influenced of the fact that the risk
groups event rate, depending on intervention, was decreased
to a levelmore equalto those being withoutrisk. On the
other hand, even those withoutrisk could possibly have
received intervention in accordance to nurse’s judgement and/
or the routines of care, instead of a score point. However, this
study was not aimed to evaluate interventions or to be predic-
tive. According to Balzer et al.(2013)an assessmentscale
cannot solely be judged from the amount of events or out-
come due to serious risk of bias. Thus, is not possible to con-
trol for every care process in daily clinical practice. Instead,
the study aimed to give insight in how scale items are associ-
ated to severe outcomes under the existing circumstances.
Limitations
The exact date for the outcome variables Falls last
six months was not recorded for the SHADES study but only
if there had been a fall or not. Occurrences of fall were col-
lected from the routine care documentation. If there had been
any fallduring the last six months,the date for the actual
scoring became the fall date. This shortage in accuracy may
have affected the time variable in the Cox regressions.For
pressure ulcers, if there were any at the follow-up, the actual
date for scoring became the date. It is possible, but not likely,
that a pressure ulcerhad risen and reached to be healed
between the follow-up visits, and therefore not detected.
These shortages of accuracy can be explained by the fact
of using data from a study where these issues were not of
primary interest.
Conclusions
In this study 93% had fallrisk, 58% risk for malnutrition
and 27% risk for pressure ulcers. Only 4% scored no risk for
any of these serious events. Longitudinal risk scoring showed
significant impaired mean scores indicating increased risks.
This confirms the complexity of this population’s status of
general condition. Further, there was no statistical significant
difference between those being at risk or not regarding falls,
weightloss or pressure ulcers which implies thatthe total
scores of scales should be interpreted with caution.Regres-
sion analyses with falls,pressure ulcers and weightloss as
dependent variables showed that mobility,activity and fac-
tors that may affect mobility were associated with falls. Age,
number of drugs, mobility and activity revealed shared asso-
ciations to pressure ulcers. For weight loss with at least 10%
or 6 kg cognitive decline was of most importance.Regres-
sion analyses with the same outcome variables in relation to
the totalscores showed thatMNS was associated with all
three outcomes. This implies that MNS covers many impor-
tant items to assess general decline and frailty which in turn
increase both risk tendency and lead to events.
Relevance to clinical practice
Mobility and activity from the three different scales showed
shared associations with falls and pressure ulcers but in two
different ways – physical activity increases falls but decreases
pressureulcers.This involvesa challengefor care – to
improve and maintain physical activity and at the same time
prevent falls. For weight loss the most important associations
were cognitive decline.Further,when planning the preven-
tive interventions,a comprehensiveview and individual
judgment is needed and not only to focus on the total scores.
Acknowledgements
This study was financially supported by MedicalResearch
Council of SoutheastSweden(FORSS) and the Janne
Elgqvist Foundation.
Contributions
Study Design:CL, MEB; Data collection and analysis:CL,
MEB; Manuscript preparation: CL, MEB, PM, CJ€O, SM.
© 2016 John Wiley & Sons Ltd
948 Journal of Clinical Nursing, 25, 940–950
C Lannering et al.
attention. Accordingly, a comprehensive view and individual
judgment is necessary, irrespective of being at risk or not, as
personswithout risk also will sufferfrom events.Nurses
should also consider what is actually measured when using
assessment scales; a special risk or general decline, which in
turn may increase both risk tendency and lead to events.
The results presented in this study and the factthat the
used scales had low internalconsistency,make them ques-
tionable for this population with high care need.However,
using assessmentscalesroutinely mightbring attention to
the phenomenon ofpreventive care,and thereby serve as
pedagogical tools.
Normally, the reason for using risk assessments tools is to
address prevention actions to the subjects thatare most in
need of these actions.In this study,no specialinterventions
were performed, but we have no information about treatment
and level of prevention of the routine care given at the nurs-
ing homes.This is importantto keep in mind,especially
regarding interpretations of the results from Table 2. As we
do not know what, or if any special treatment or intervention
was given to those being at risk, it is possible that the lack of
statistical difference can be influenced of the fact that the risk
groups event rate, depending on intervention, was decreased
to a levelmore equalto those being withoutrisk. On the
other hand, even those withoutrisk could possibly have
received intervention in accordance to nurse’s judgement and/
or the routines of care, instead of a score point. However, this
study was not aimed to evaluate interventions or to be predic-
tive. According to Balzer et al.(2013)an assessmentscale
cannot solely be judged from the amount of events or out-
come due to serious risk of bias. Thus, is not possible to con-
trol for every care process in daily clinical practice. Instead,
the study aimed to give insight in how scale items are associ-
ated to severe outcomes under the existing circumstances.
Limitations
The exact date for the outcome variables Falls last
six months was not recorded for the SHADES study but only
if there had been a fall or not. Occurrences of fall were col-
lected from the routine care documentation. If there had been
any fallduring the last six months,the date for the actual
scoring became the fall date. This shortage in accuracy may
have affected the time variable in the Cox regressions.For
pressure ulcers, if there were any at the follow-up, the actual
date for scoring became the date. It is possible, but not likely,
that a pressure ulcerhad risen and reached to be healed
between the follow-up visits, and therefore not detected.
These shortages of accuracy can be explained by the fact
of using data from a study where these issues were not of
primary interest.
Conclusions
In this study 93% had fallrisk, 58% risk for malnutrition
and 27% risk for pressure ulcers. Only 4% scored no risk for
any of these serious events. Longitudinal risk scoring showed
significant impaired mean scores indicating increased risks.
This confirms the complexity of this population’s status of
general condition. Further, there was no statistical significant
difference between those being at risk or not regarding falls,
weightloss or pressure ulcers which implies thatthe total
scores of scales should be interpreted with caution.Regres-
sion analyses with falls,pressure ulcers and weightloss as
dependent variables showed that mobility,activity and fac-
tors that may affect mobility were associated with falls. Age,
number of drugs, mobility and activity revealed shared asso-
ciations to pressure ulcers. For weight loss with at least 10%
or 6 kg cognitive decline was of most importance.Regres-
sion analyses with the same outcome variables in relation to
the totalscores showed thatMNS was associated with all
three outcomes. This implies that MNS covers many impor-
tant items to assess general decline and frailty which in turn
increase both risk tendency and lead to events.
Relevance to clinical practice
Mobility and activity from the three different scales showed
shared associations with falls and pressure ulcers but in two
different ways – physical activity increases falls but decreases
pressureulcers.This involvesa challengefor care – to
improve and maintain physical activity and at the same time
prevent falls. For weight loss the most important associations
were cognitive decline.Further,when planning the preven-
tive interventions,a comprehensiveview and individual
judgment is needed and not only to focus on the total scores.
Acknowledgements
This study was financially supported by MedicalResearch
Council of SoutheastSweden(FORSS) and the Janne
Elgqvist Foundation.
Contributions
Study Design:CL, MEB; Data collection and analysis:CL,
MEB; Manuscript preparation: CL, MEB, PM, CJ€O, SM.
© 2016 John Wiley & Sons Ltd
948 Journal of Clinical Nursing, 25, 940–950
C Lannering et al.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Conflict of interest
The authors have no conflicts of interest to declare.
References
Balzer K, Kopke S, Luhmann D,Haastert
B, Kottner J & Meyer G (2013)
Designing trials for pressure ulcer risk
assessmentresearch:methodological
challenges.International Journal of
Nursing Studies 50, 1136–1150.
Barker AL, Nitz JC, Low Choy NL &
Haines T (2009) Measuring fall risk
and predicting who willfall: clinimet-
ric properties offour fall risk assess-
ment tools for residentialaged care.
The Journals of Gerontology.Series
A, Biological Sciencesand Medical
Sciences 64A, 916–924.
Bauer JM, Kaiser MJ, Anthony P, Guigoz Y
& Sieber CC (2008)The Mini Nutri-
tional Assessment – its history,today’s
practice, and future perspectives. Nutri-
tion in Clinical Practice 23, 388–396.
Blackburn GL, Bistrian BR, Maini BS, Sch-
lamm HT & Smith MF (1977) Nutri-
tional and metabolic assessment of the
hospitalized patient.Journal of Par-
enteral and Enteral Nutrition 1, 11–22.
Board of National Health and Welfare
(2012)€Aldre – vard och omsorg den 1
oktober 2012 – Kommunala insatser
enligt socialtj€anstlagensamt h€also-
och sjukvardslagen.National Board of
Health and Welfare. Available at:
http://www.socialstyrelsen.se/Lists/
Artikelkatalog/Attachments/19051/
2013-4-15.pdf
Cameron ID, Murray GR, Gillespie LD,
Robertson MC, Hill KD, Cumming
RG & Kerse N (2010) Interventions
for preventing falls in older people in
nursing care facilities and hospitals.
Cochrane Database Systematic
Reviews, Issue 1, 1–78.
Casimiro C, Garcia-de-Lorenzo A & Usan
L (2002) Prevalence of decubitus ulcer
and associated risk factors in an insti-
tutionalizedSpanish elderly popula-
tion. Nutrition 18, 408–414.
Coleman S,Gorecki C, Nelson EA, Closs
SJ, Defloor T, Halfens R, Farrin A,
Brown J, Schoonhoven L & Nixon J
(2013) Patient risk factors for pressure
ulcer development:systematic review.
International Journalof Nursing Stud-
ies 50, 974–1003.
da Costa BR, Rutjes AW, Mendy A, Fre-
und-Heritage R & Vieira ER (2012)
Can falls risk prediction tools cor-
rectly identify fall-prone elderly reha-
bilitation inpatients? A systematic
review and meta-analysis.PLoS One
7, e41061.
Damian J, Pastor-Barriuso R,Valderrama-
Gama E & de Pedro-Cuesta J (2013)
Factors associated with falls among
older adults living in institutions.
BioMed Central Geriatrics 13, 6.
Dent E, Visvanathan R,PiantadosiC &
Chapman I (2012) Use of the Mini
Nutritional Assessment to detect
frailty in hospitalisedolder people.
The Journal of Nutrition, Health &
Aging 16, 764–767.
Diekmann R,Winning K, Uter W, Kaiser
MJ, SieberCC, Volkert D & Bauer
JM (2013) Screening for malnutrition
among nursing home residents– a
comparativeanalysis of the Mini
Nutritional Assessment,the Nutri-
tional Risk Screening,and the Malnu-
trition UniversalScreening Tool.The
Journal of Nutrition, Health & Aging
17, 326–331.
Downton JH (1993) Falls in the Elderly.
Edward Arnold, London.
Ek AC (1987) Prediction ofpressure sore
development.Scandinavian Journalof
Caring Sciences 1, 77–84.
Ek A-C & Bjurulf P (1987) Interrater vari-
ability in a modified Norton Scale.
Scandinavian Journal of Caring
Sciences 1, 99–102.
Ernsth M (2001) Att €ata i
tr€adgarden. . ..Ettf€ors€ok med berikn-
ing av vardtagarnas mat och dryck pa
Tr€adgardens€aldreboende,J €onk€opings
kommun. Rapport nr 87, Institutet f€or
gerontologi, J€onk€oping.
Ernsth BravellM, Westerlind B,Midlov P,
Ostgren CJ,Borgquist L,Lannering C
& Molstad S (2011) How to
assessfrailty and the need for care?
Reportfrom the Study ofHealth and
Drugs in the Elderly (SHADES) in com-
munity dwellings in Sweden.Archives
of Gerontology and Geriatrics 53,
40–45.
Faxen Irving G, Karlstr€om B & Rothen-
berg E (2010) Geriatrisk Nutrition.
Studentlitteratur, Lund.
Fried LP, Tangen CM, Walston J, New-
man AB, Hirsch C, Gottdiener J,See-
man T, Tracy R, Kop WJ, Burke G &
McBurnie MA (2001)Frailty in older
adults: evidence for a phenotype. Jour-
nals of Gerontology. Series A, Biologi-
cal Sciences and MedicalSciences 56,
M146–M156.
Gunningberg L,Hommel A, Baath C &
Idvall E (2013) The first national pres-
sure ulcer prevalence survey in county
council and municipality settingsin
Sweden. Journal of Evaluation in Clin-
ical Practice 19, 862–867.
Kaiser MJ, Bauer JM, Ramsch C,Uter W,
Guigoz Y, Cederholm T,Thomas DR,
Anthony P, Charlton KE, Maggio M,
Tsai AC, Grathwohl D, Vellas B &
SieberCC (2009) Validation of the
Mini Nutritional Assessmentshort-
form (MNA-SF): a practical tool for
identification of nutritional status. The
Journal of Nutrition, Health & Aging
13, 782–788.
Kaiser MJ, Bauer JM, Uter W, Donini LM,
StangeI, Volkert D, Diekmann R,
Drey M, Bollwein J, Tempera S,
Guerra A, RicciardiLM & Sieber CC
(2011) Prospectivevalidation of the
modified mini nutritional assessment
short-forms in the community, nursing
home,and rehabilitation setting.Jour-
nal of the American Geriatrics Society
59, 2124–2128.
Lahmann NA,Tannen A,Kuntz S,Raeder
K, Schmitz G,Dassen T & Kottner J
(2015) Mobility is the key! Trends
and associations of common care prob-
lems in German long-term care facili-
ties from 2008 to 2012.International
Journal of Nursing Studies52, 167–
174.
Lamb SE, Jorstad-Stein EC,Hauer K &
Becker C (2005) Developmentof a
common outcome data set for fall
injury prevention trials: the Prevention
of Falls Network Europe consensus.
Journal of the American Geriatrics
Society 53, 1618–1622.
© 2016 John Wiley & Sons Ltd
Journal of Clinical Nursing, 25, 940–950 949
Original article Risk assessment among nursing home residents
The authors have no conflicts of interest to declare.
References
Balzer K, Kopke S, Luhmann D,Haastert
B, Kottner J & Meyer G (2013)
Designing trials for pressure ulcer risk
assessmentresearch:methodological
challenges.International Journal of
Nursing Studies 50, 1136–1150.
Barker AL, Nitz JC, Low Choy NL &
Haines T (2009) Measuring fall risk
and predicting who willfall: clinimet-
ric properties offour fall risk assess-
ment tools for residentialaged care.
The Journals of Gerontology.Series
A, Biological Sciencesand Medical
Sciences 64A, 916–924.
Bauer JM, Kaiser MJ, Anthony P, Guigoz Y
& Sieber CC (2008)The Mini Nutri-
tional Assessment – its history,today’s
practice, and future perspectives. Nutri-
tion in Clinical Practice 23, 388–396.
Blackburn GL, Bistrian BR, Maini BS, Sch-
lamm HT & Smith MF (1977) Nutri-
tional and metabolic assessment of the
hospitalized patient.Journal of Par-
enteral and Enteral Nutrition 1, 11–22.
Board of National Health and Welfare
(2012)€Aldre – vard och omsorg den 1
oktober 2012 – Kommunala insatser
enligt socialtj€anstlagensamt h€also-
och sjukvardslagen.National Board of
Health and Welfare. Available at:
http://www.socialstyrelsen.se/Lists/
Artikelkatalog/Attachments/19051/
2013-4-15.pdf
Cameron ID, Murray GR, Gillespie LD,
Robertson MC, Hill KD, Cumming
RG & Kerse N (2010) Interventions
for preventing falls in older people in
nursing care facilities and hospitals.
Cochrane Database Systematic
Reviews, Issue 1, 1–78.
Casimiro C, Garcia-de-Lorenzo A & Usan
L (2002) Prevalence of decubitus ulcer
and associated risk factors in an insti-
tutionalizedSpanish elderly popula-
tion. Nutrition 18, 408–414.
Coleman S,Gorecki C, Nelson EA, Closs
SJ, Defloor T, Halfens R, Farrin A,
Brown J, Schoonhoven L & Nixon J
(2013) Patient risk factors for pressure
ulcer development:systematic review.
International Journalof Nursing Stud-
ies 50, 974–1003.
da Costa BR, Rutjes AW, Mendy A, Fre-
und-Heritage R & Vieira ER (2012)
Can falls risk prediction tools cor-
rectly identify fall-prone elderly reha-
bilitation inpatients? A systematic
review and meta-analysis.PLoS One
7, e41061.
Damian J, Pastor-Barriuso R,Valderrama-
Gama E & de Pedro-Cuesta J (2013)
Factors associated with falls among
older adults living in institutions.
BioMed Central Geriatrics 13, 6.
Dent E, Visvanathan R,PiantadosiC &
Chapman I (2012) Use of the Mini
Nutritional Assessment to detect
frailty in hospitalisedolder people.
The Journal of Nutrition, Health &
Aging 16, 764–767.
Diekmann R,Winning K, Uter W, Kaiser
MJ, SieberCC, Volkert D & Bauer
JM (2013) Screening for malnutrition
among nursing home residents– a
comparativeanalysis of the Mini
Nutritional Assessment,the Nutri-
tional Risk Screening,and the Malnu-
trition UniversalScreening Tool.The
Journal of Nutrition, Health & Aging
17, 326–331.
Downton JH (1993) Falls in the Elderly.
Edward Arnold, London.
Ek AC (1987) Prediction ofpressure sore
development.Scandinavian Journalof
Caring Sciences 1, 77–84.
Ek A-C & Bjurulf P (1987) Interrater vari-
ability in a modified Norton Scale.
Scandinavian Journal of Caring
Sciences 1, 99–102.
Ernsth M (2001) Att €ata i
tr€adgarden. . ..Ettf€ors€ok med berikn-
ing av vardtagarnas mat och dryck pa
Tr€adgardens€aldreboende,J €onk€opings
kommun. Rapport nr 87, Institutet f€or
gerontologi, J€onk€oping.
Ernsth BravellM, Westerlind B,Midlov P,
Ostgren CJ,Borgquist L,Lannering C
& Molstad S (2011) How to
assessfrailty and the need for care?
Reportfrom the Study ofHealth and
Drugs in the Elderly (SHADES) in com-
munity dwellings in Sweden.Archives
of Gerontology and Geriatrics 53,
40–45.
Faxen Irving G, Karlstr€om B & Rothen-
berg E (2010) Geriatrisk Nutrition.
Studentlitteratur, Lund.
Fried LP, Tangen CM, Walston J, New-
man AB, Hirsch C, Gottdiener J,See-
man T, Tracy R, Kop WJ, Burke G &
McBurnie MA (2001)Frailty in older
adults: evidence for a phenotype. Jour-
nals of Gerontology. Series A, Biologi-
cal Sciences and MedicalSciences 56,
M146–M156.
Gunningberg L,Hommel A, Baath C &
Idvall E (2013) The first national pres-
sure ulcer prevalence survey in county
council and municipality settingsin
Sweden. Journal of Evaluation in Clin-
ical Practice 19, 862–867.
Kaiser MJ, Bauer JM, Ramsch C,Uter W,
Guigoz Y, Cederholm T,Thomas DR,
Anthony P, Charlton KE, Maggio M,
Tsai AC, Grathwohl D, Vellas B &
SieberCC (2009) Validation of the
Mini Nutritional Assessmentshort-
form (MNA-SF): a practical tool for
identification of nutritional status. The
Journal of Nutrition, Health & Aging
13, 782–788.
Kaiser MJ, Bauer JM, Uter W, Donini LM,
StangeI, Volkert D, Diekmann R,
Drey M, Bollwein J, Tempera S,
Guerra A, RicciardiLM & Sieber CC
(2011) Prospectivevalidation of the
modified mini nutritional assessment
short-forms in the community, nursing
home,and rehabilitation setting.Jour-
nal of the American Geriatrics Society
59, 2124–2128.
Lahmann NA,Tannen A,Kuntz S,Raeder
K, Schmitz G,Dassen T & Kottner J
(2015) Mobility is the key! Trends
and associations of common care prob-
lems in German long-term care facili-
ties from 2008 to 2012.International
Journal of Nursing Studies52, 167–
174.
Lamb SE, Jorstad-Stein EC,Hauer K &
Becker C (2005) Developmentof a
common outcome data set for fall
injury prevention trials: the Prevention
of Falls Network Europe consensus.
Journal of the American Geriatrics
Society 53, 1618–1622.
© 2016 John Wiley & Sons Ltd
Journal of Clinical Nursing, 25, 940–950 949
Original article Risk assessment among nursing home residents
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Lee KS, Cheong HK, Kim EA, Kim KR,
Oh BH & Hong CH (2009) Nutri-
tional risk and cognitiveimpairment
in the elderly. Archivesof Gerontol-
ogy and Geriatrics 48, 95–99.
Lindgren M,Unosson M,Fredrikson M &
Ek AC (2004) Immobility – a major
risk factor for development of pressure
ulcers among adult hospitalized
patients:a prospective study.Scandi-
navian Journalof Caring Sciences 18,
57–64.
Meesterberends E,Halfens RJ, Spreeuwen-
berg MD, Ambergen TA, Lohrmann
C, Neyens JC & Schols JM (2013) Do
patients in Dutch nursing homes have
more pressure ulcersthan patientsin
German nursing homes? A prospective
multicentercohort study. Journal of
the American MedicalDirectors Asso-
ciation 14, 605–610.
Meyer G, Kopke S, HaastertB & Muhl-
hauser I(2009)Comparison ofa fall
risk assessmenttool with nurses’
judgement alone:a cluster-randomised
controlled trial.Age and Ageing 38,
417–423.
Rockwood K & Mitnitski A (2007) Frailty
in relation to the accumulation of defi-
cits. Journals of Gerontology.Series
A, Biological Sciencesand Medical
Sciences 62, 722–727.
RosendahlE, Lundin-Olsson L, Kallin K,
Jensen J, Gustafson Y & Nyberg L
(2003) Prediction of falls among older
people in residentialcare facilities by
the Downton index. Aging Clinical and
Experimental Research 15, 142–147.
Rubenstein LZ,Josephson KR & Robbins
AS (1994) Falls in the nursing home.
Annals of Internal Medicine 121,
442–451.
Rubenstein LZ,Harker JO, Salva A, Gui-
goz Y & Vellas B (2001) Screening for
undernutritionin geriatric practice:
developing the short-form mini-nutri-
tional assessment(MNA-SF). Journals
of Gerontology.SeriesA, Biological
Sciencesand Medical Sciences56,
M366–M372.
Salvi F, Giorgi R, Grilli A, Morichi V,
Espinosa E,Spazzafumo L,Marinozzi
ML & Dessi-Fulgheri P (2008) Mini
Nutritional Assessment(short form)
and functional decline in older
patients admitted to an acute medical
ward. Aging Clinical and Experimen-
tal Research 20, 322–328.
SecherM, Soto ME, Villars H, van Kan
GA & Vellas B (2007) The Mini
Nutritional Assessment(MNA) after
20 years of research and clinicalprac-
tice. Reviews in ClinicalGerontology
17, 293–310.
Torma J, Winblad U, Cederholm T &
SalettiA (2013) Does undernutrition
still prevailamong nursing home resi-
dents? Clinical Nutrition 32, 562–568.
Verbrugghe M, Beeckman D, Van Hecke A,
Vanderwee K,Van Herck K, Clays E,
Bocquaert I, Derycke H, Geurden B &
Verhaeghe S (2013)Malnutrition and
associated factors in nursing home resi-
dents: a cross-sectional,multi-centre
study. Clinical Nutrition 32, 438–443.
WHO (2012) Interesting Facts About Age-
ing. WHO. Available at: http://
www.who.int/ageing/about/facts/eng/.
© 2016 John Wiley & Sons Ltd
950 Journal of Clinical Nursing, 25, 940–950
C Lannering et al.
Oh BH & Hong CH (2009) Nutri-
tional risk and cognitiveimpairment
in the elderly. Archivesof Gerontol-
ogy and Geriatrics 48, 95–99.
Lindgren M,Unosson M,Fredrikson M &
Ek AC (2004) Immobility – a major
risk factor for development of pressure
ulcers among adult hospitalized
patients:a prospective study.Scandi-
navian Journalof Caring Sciences 18,
57–64.
Meesterberends E,Halfens RJ, Spreeuwen-
berg MD, Ambergen TA, Lohrmann
C, Neyens JC & Schols JM (2013) Do
patients in Dutch nursing homes have
more pressure ulcersthan patientsin
German nursing homes? A prospective
multicentercohort study. Journal of
the American MedicalDirectors Asso-
ciation 14, 605–610.
Meyer G, Kopke S, HaastertB & Muhl-
hauser I(2009)Comparison ofa fall
risk assessmenttool with nurses’
judgement alone:a cluster-randomised
controlled trial.Age and Ageing 38,
417–423.
Rockwood K & Mitnitski A (2007) Frailty
in relation to the accumulation of defi-
cits. Journals of Gerontology.Series
A, Biological Sciencesand Medical
Sciences 62, 722–727.
RosendahlE, Lundin-Olsson L, Kallin K,
Jensen J, Gustafson Y & Nyberg L
(2003) Prediction of falls among older
people in residentialcare facilities by
the Downton index. Aging Clinical and
Experimental Research 15, 142–147.
Rubenstein LZ,Josephson KR & Robbins
AS (1994) Falls in the nursing home.
Annals of Internal Medicine 121,
442–451.
Rubenstein LZ,Harker JO, Salva A, Gui-
goz Y & Vellas B (2001) Screening for
undernutritionin geriatric practice:
developing the short-form mini-nutri-
tional assessment(MNA-SF). Journals
of Gerontology.SeriesA, Biological
Sciencesand Medical Sciences56,
M366–M372.
Salvi F, Giorgi R, Grilli A, Morichi V,
Espinosa E,Spazzafumo L,Marinozzi
ML & Dessi-Fulgheri P (2008) Mini
Nutritional Assessment(short form)
and functional decline in older
patients admitted to an acute medical
ward. Aging Clinical and Experimen-
tal Research 20, 322–328.
SecherM, Soto ME, Villars H, van Kan
GA & Vellas B (2007) The Mini
Nutritional Assessment(MNA) after
20 years of research and clinicalprac-
tice. Reviews in ClinicalGerontology
17, 293–310.
Torma J, Winblad U, Cederholm T &
SalettiA (2013) Does undernutrition
still prevailamong nursing home resi-
dents? Clinical Nutrition 32, 562–568.
Verbrugghe M, Beeckman D, Van Hecke A,
Vanderwee K,Van Herck K, Clays E,
Bocquaert I, Derycke H, Geurden B &
Verhaeghe S (2013)Malnutrition and
associated factors in nursing home resi-
dents: a cross-sectional,multi-centre
study. Clinical Nutrition 32, 438–443.
WHO (2012) Interesting Facts About Age-
ing. WHO. Available at: http://
www.who.int/ageing/about/facts/eng/.
© 2016 John Wiley & Sons Ltd
950 Journal of Clinical Nursing, 25, 940–950
C Lannering et al.
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




