TB in India: Incidence, Needs, Intervention, and Actions
VerifiedAdded on 2022/08/14
|16
|1893
|21
Report
AI Summary
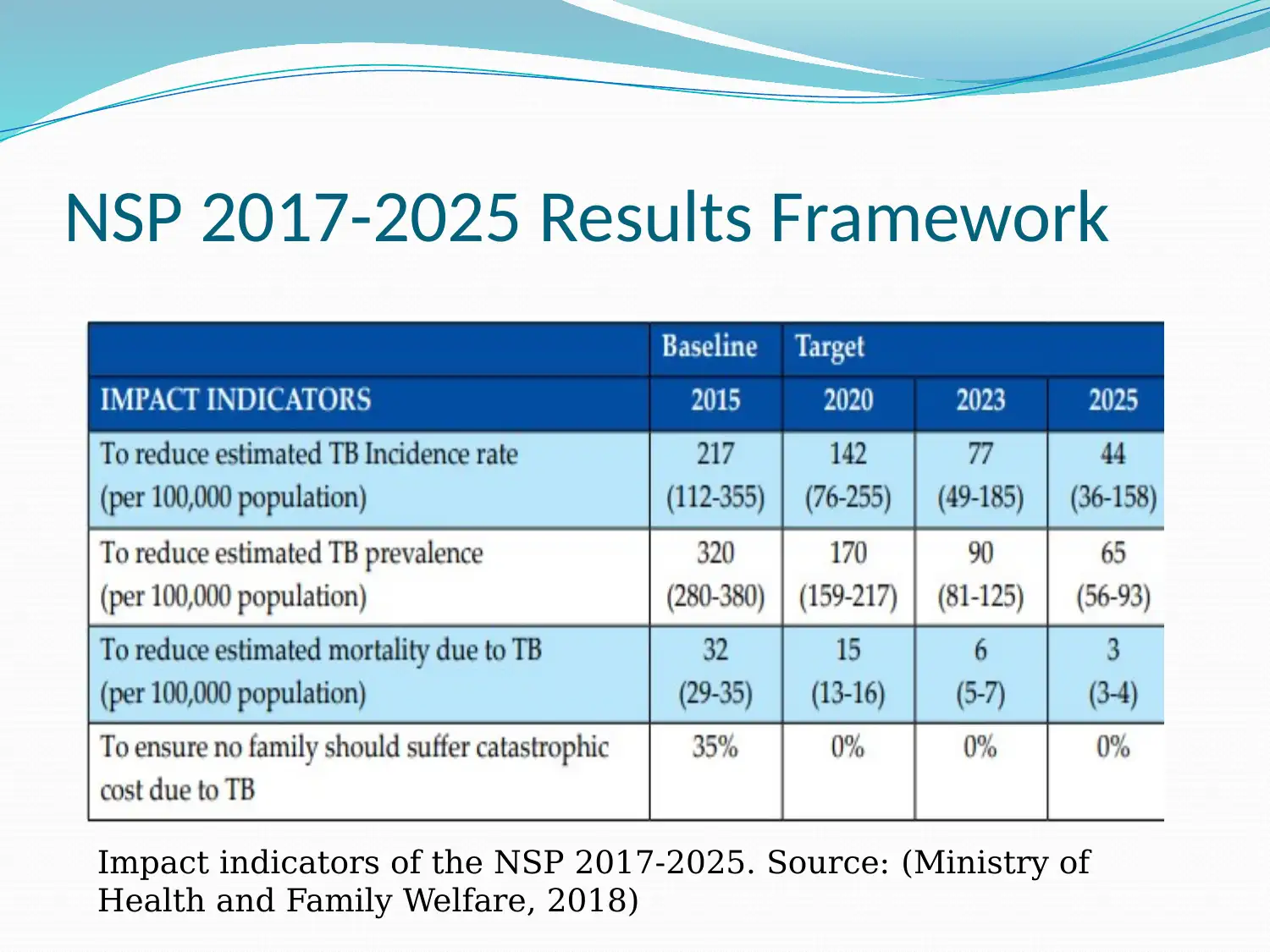
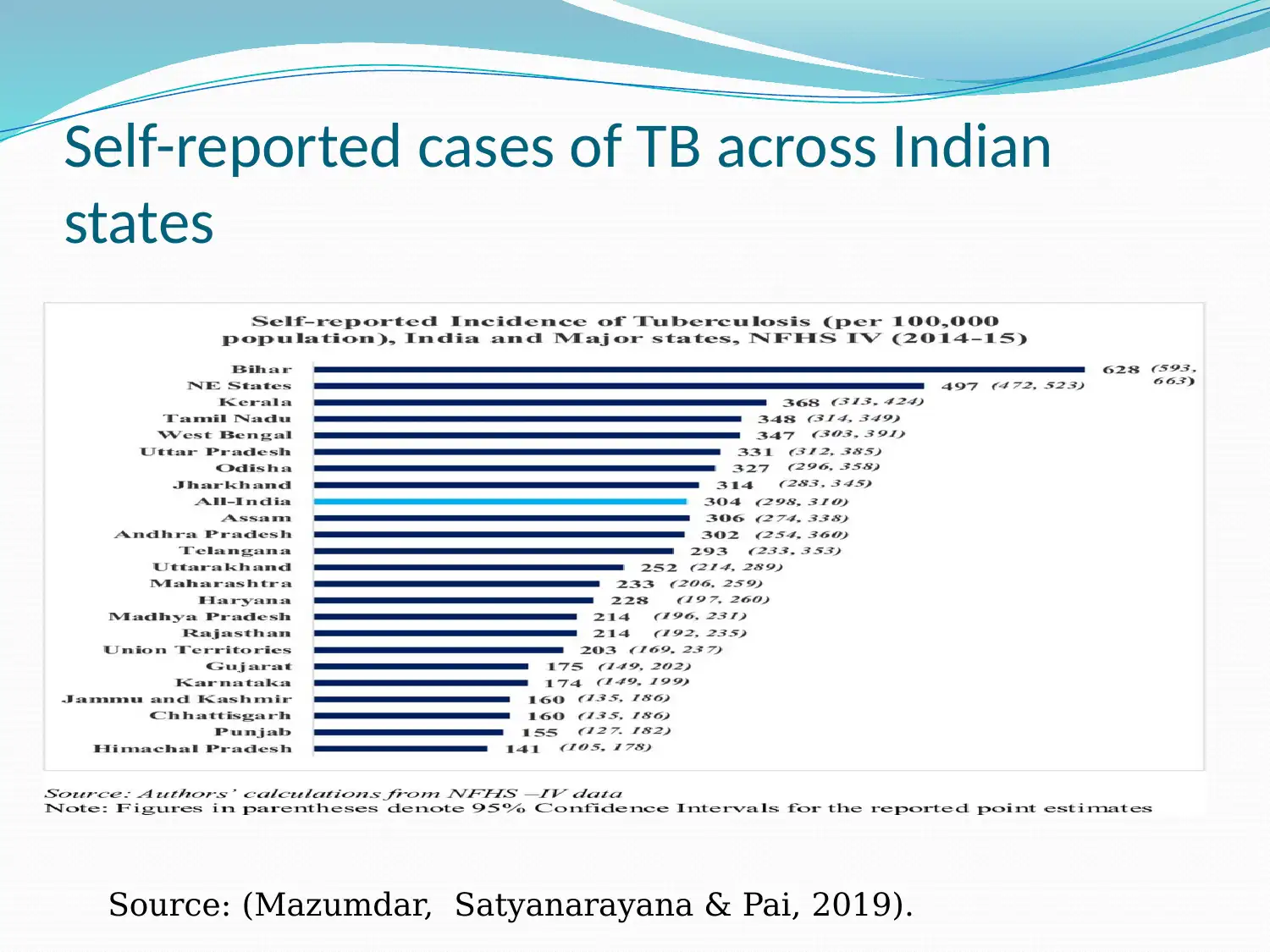
This report provides a comprehensive overview of Tuberculosis (TB) in India. It begins by defining TB, its clinical manifestations, and associated risk factors, including low body weight, HIV infection, and overcrowded areas. The report then delves into the epidemiology of TB in India, highlighting its status as a high-burden country, with a significant number of cases and deaths annually. It references data from the WHO and the Indian government, including the NSP 2017-2025 framework. The report identifies key concerns, such as the rise of multi-drug resistant TB (MDR TB) and challenges in TB care, including fragmented healthcare delivery and the high cost of treatment. It also addresses barriers to TB notification, such as operational complexities and geographical limitations. To reduce the burden of TB, the report suggests implementing fixed-dose regimens, improving disease surveillance, and strengthening patient tracking. It outlines the actions needed for effective implementation, including increased budgetary provisions, intersectoral coordination, and stakeholder engagement. The report emphasizes the importance of public and private care providers, policymakers, and health informatics groups in achieving the goals of the RNTCP.
1 out of 16







![[object Object]](/_next/static/media/star-bottom.7253800d.svg)