Logic Diagram for a Program Based on Prioritized Need
VerifiedAdded on 2023/06/09
|17
|2401
|97
AI Summary
This presentation provides a logic diagram for a program based on prioritized need for managing overweight and obesity in adults. It includes strategies, objectives, and evaluation plan for the program. The program aims to provide weight loss health benefits for overweight and obese adults in reducing cardiovascular risk elements as well as events, morbidity or mortality.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
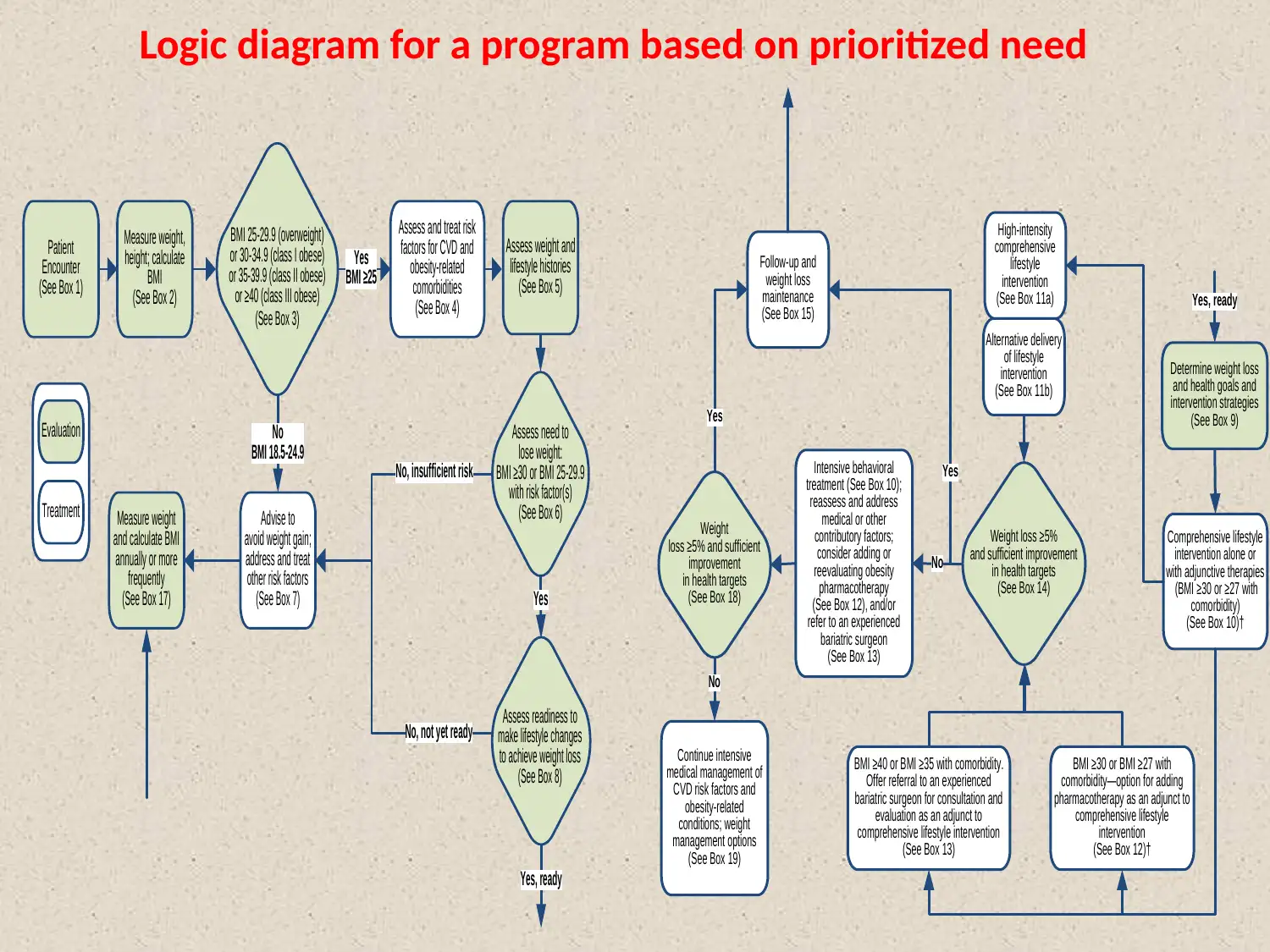
Logic diagram for a program based on prioritized need
Patient
Encounter
(See Box 1)
Measure weight,
height; calculate
BMI
(See Box 2)
Yes
BMI ≥25
Assess and treat risk
factors for CVD and
obesity-related
comorbidities
(See Box 4)
Assess weight and
lifestyle histories
(See Box 5)
Advise to
avoid weight gain;
address and treat
other risk factors
(See Box 7)
No, insufficient risk
No, not yet ready
No
BMI 18.5-24.9
Measure weight
and calculate BMI
annually or more
frequently
(See Box 17) Yes
Evaluation
Treatment
BMI 25-29.9 (overweight)
or 30-34.9 (class I obese)
or 35-39.9 (class II obese)
or ≥40 (class III obese)
(See Box 3)
Assess need to
lose weight:
BMI ≥30 or BMI 25-29.9
with risk factor(s)
(See Box 6)
Assess readiness to
make lifestyle changes
to achieve weight loss
(See Box 8)
Yes, ready
Follow-up and
weight loss
maintenance
(See Box 15)
Determine weight loss
and health goals and
intervention strategies
(See Box 9)
Comprehensive lifestyle
intervention alone or
with adjunctive therapies
(BMI ≥30 or ≥27 with
comorbidity)
(See Box 10)†
High-intensity
comprehensive
lifestyle
intervention
(See Box 11a)
Alternative delivery
of lifestyle
intervention
(See Box 11b)
BMI ≥30 or BMI ≥27 with
comorbidity—option for adding
pharmacotherapy as an adjunct to
comprehensive lifestyle
intervention
(See Box 12)†
BMI ≥40 or BMI ≥35 with comorbidity.
Offer referral to an experienced
bariatric surgeon for consultation and
evaluation as an adjunct to
comprehensive lifestyle intervention
(See Box 13)
Yes
Yes
Continue intensive
medical management of
CVD risk factors and
obesity-related
conditions; weight
management options
(See Box 19)
Intensive behavioral
treatment (See Box 10);
reassess and address
medical or other
contributory factors;
consider adding or
reevaluating obesity
pharmacotherapy
(See Box 12), and/or
refer to an experienced
bariatric surgeon
(See Box 13)
No
No
Yes, ready
Weight loss ≥5%
and sufficient improvement
in health targets
(See Box 14)
Weight
loss ≥5% and sufficient
improvement
in health targets
(See Box 18)
Patient
Encounter
(See Box 1)
Measure weight,
height; calculate
BMI
(See Box 2)
Yes
BMI ≥25
Assess and treat risk
factors for CVD and
obesity-related
comorbidities
(See Box 4)
Assess weight and
lifestyle histories
(See Box 5)
Advise to
avoid weight gain;
address and treat
other risk factors
(See Box 7)
No, insufficient risk
No, not yet ready
No
BMI 18.5-24.9
Measure weight
and calculate BMI
annually or more
frequently
(See Box 17) Yes
Evaluation
Treatment
BMI 25-29.9 (overweight)
or 30-34.9 (class I obese)
or 35-39.9 (class II obese)
or ≥40 (class III obese)
(See Box 3)
Assess need to
lose weight:
BMI ≥30 or BMI 25-29.9
with risk factor(s)
(See Box 6)
Assess readiness to
make lifestyle changes
to achieve weight loss
(See Box 8)
Yes, ready
Follow-up and
weight loss
maintenance
(See Box 15)
Determine weight loss
and health goals and
intervention strategies
(See Box 9)
Comprehensive lifestyle
intervention alone or
with adjunctive therapies
(BMI ≥30 or ≥27 with
comorbidity)
(See Box 10)†
High-intensity
comprehensive
lifestyle
intervention
(See Box 11a)
Alternative delivery
of lifestyle
intervention
(See Box 11b)
BMI ≥30 or BMI ≥27 with
comorbidity—option for adding
pharmacotherapy as an adjunct to
comprehensive lifestyle
intervention
(See Box 12)†
BMI ≥40 or BMI ≥35 with comorbidity.
Offer referral to an experienced
bariatric surgeon for consultation and
evaluation as an adjunct to
comprehensive lifestyle intervention
(See Box 13)
Yes
Yes
Continue intensive
medical management of
CVD risk factors and
obesity-related
conditions; weight
management options
(See Box 19)
Intensive behavioral
treatment (See Box 10);
reassess and address
medical or other
contributory factors;
consider adding or
reevaluating obesity
pharmacotherapy
(See Box 12), and/or
refer to an experienced
bariatric surgeon
(See Box 13)
No
No
Yes, ready
Weight loss ≥5%
and sufficient improvement
in health targets
(See Box 14)
Weight
loss ≥5% and sufficient
improvement
in health targets
(See Box 18)
Management of overweight and obesity in
adults.
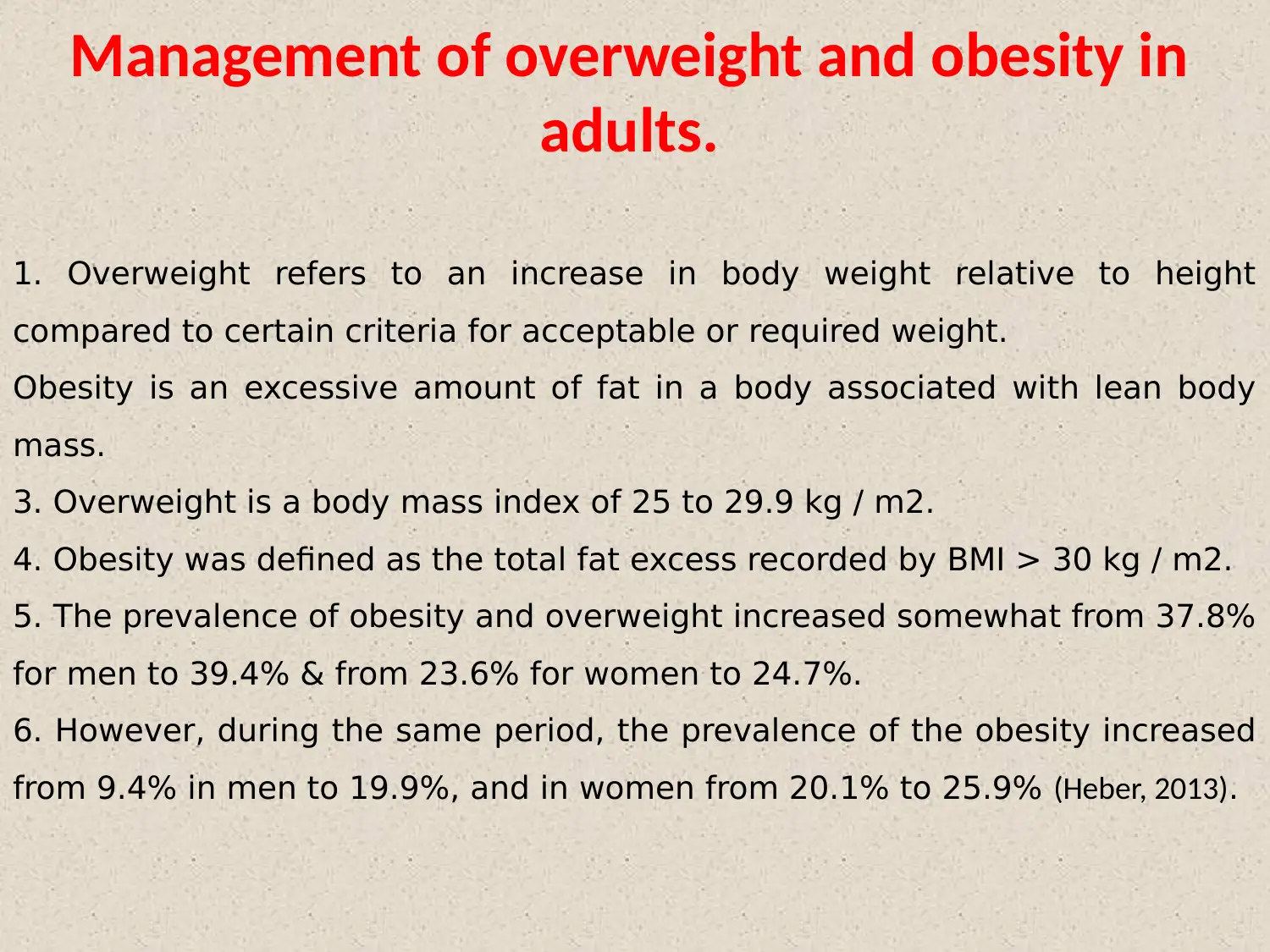
1. Overweight refers to an increase in body weight relative to height
compared to certain criteria for acceptable or required weight.
Obesity is an excessive amount of fat in a body associated with lean body
mass.
3. Overweight is a body mass index of 25 to 29.9 kg / m2.
4. Obesity was defined as the total fat excess recorded by BMI > 30 kg / m2.
5. The prevalence of obesity and overweight increased somewhat from 37.8%
for men to 39.4% & from 23.6% for women to 24.7%.
6. However, during the same period, the prevalence of the obesity increased
from 9.4% in men to 19.9%, and in women from 20.1% to 25.9% (Heber, 2013).
adults.
1. Overweight refers to an increase in body weight relative to height
compared to certain criteria for acceptable or required weight.
Obesity is an excessive amount of fat in a body associated with lean body
mass.
3. Overweight is a body mass index of 25 to 29.9 kg / m2.
4. Obesity was defined as the total fat excess recorded by BMI > 30 kg / m2.
5. The prevalence of obesity and overweight increased somewhat from 37.8%
for men to 39.4% & from 23.6% for women to 24.7%.
6. However, during the same period, the prevalence of the obesity increased
from 9.4% in men to 19.9%, and in women from 20.1% to 25.9% (Heber, 2013).
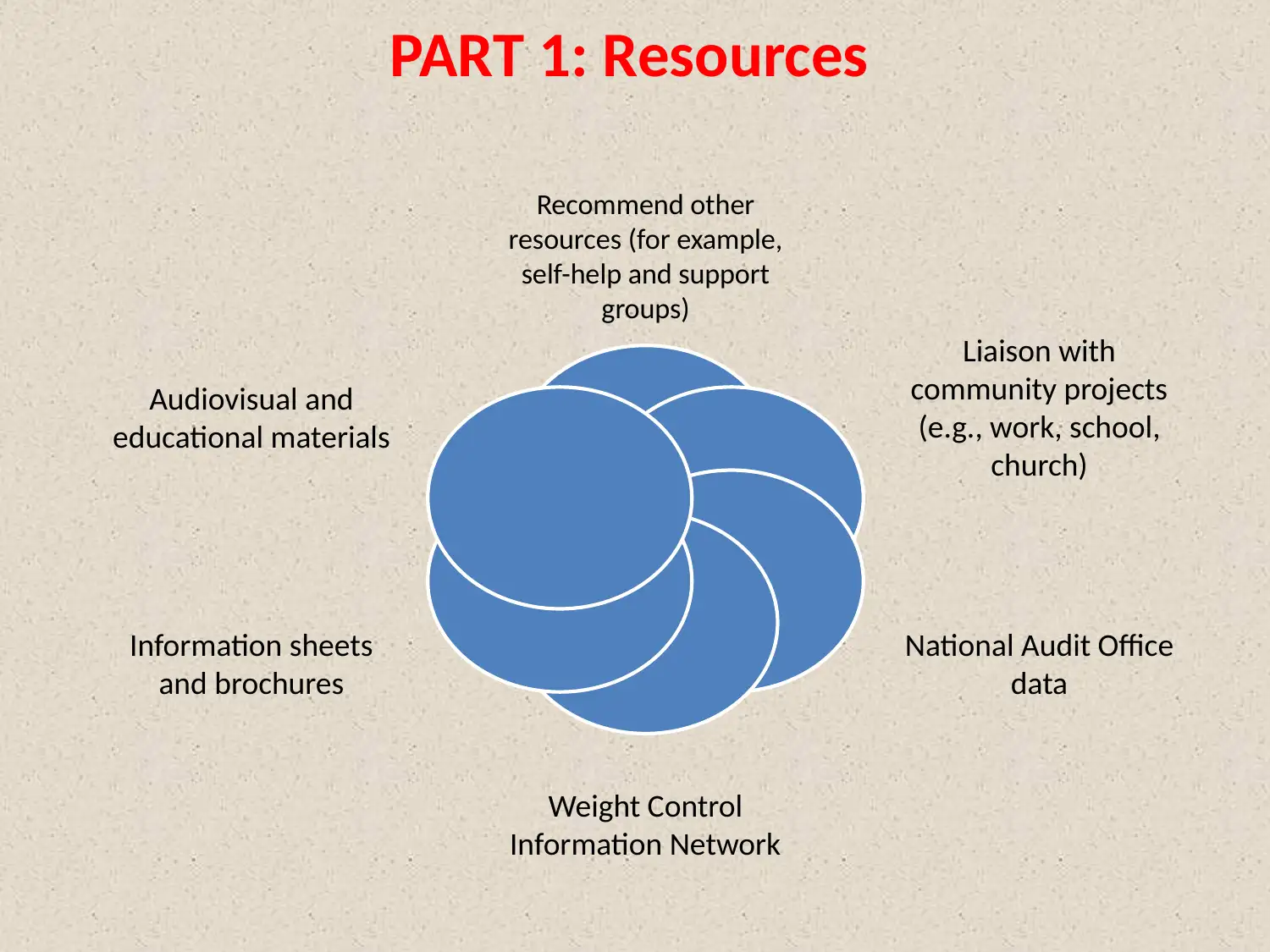
PART 1: Resources
Recommend other
resources (for example,
self-help and support
groups)
Liaison with
community projects
(e.g., work, school,
church)
National Audit Office
data
Weight Control
Information Network
Information sheets
and brochures
Audiovisual and
educational materials
Recommend other
resources (for example,
self-help and support
groups)
Liaison with
community projects
(e.g., work, school,
church)
National Audit Office
data
Weight Control
Information Network
Information sheets
and brochures
Audiovisual and
educational materials
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Activities
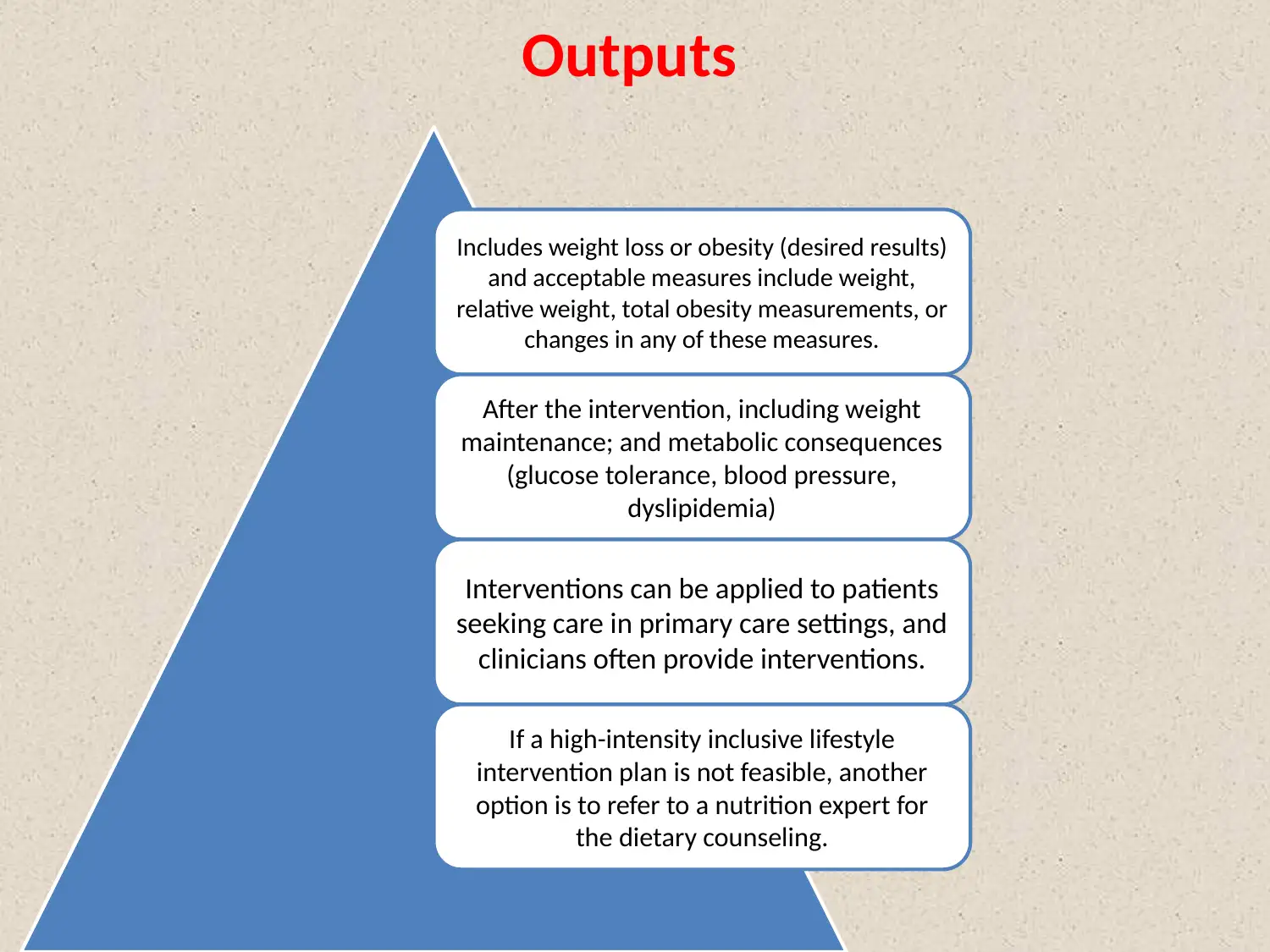
Outputs
Includes weight loss or obesity (desired results)
and acceptable measures include weight,
relative weight, total obesity measurements, or
changes in any of these measures.
After the intervention, including weight
maintenance; and metabolic consequences
(glucose tolerance, blood pressure,
dyslipidemia)
Interventions can be applied to patients
seeking care in primary care settings, and
clinicians often provide interventions.
If a high-intensity inclusive lifestyle
intervention plan is not feasible, another
option is to refer to a nutrition expert for
the dietary counseling.
Includes weight loss or obesity (desired results)
and acceptable measures include weight,
relative weight, total obesity measurements, or
changes in any of these measures.
After the intervention, including weight
maintenance; and metabolic consequences
(glucose tolerance, blood pressure,
dyslipidemia)
Interventions can be applied to patients
seeking care in primary care settings, and
clinicians often provide interventions.
If a high-intensity inclusive lifestyle
intervention plan is not feasible, another
option is to refer to a nutrition expert for
the dietary counseling.
Short term impacts
A. Losing weight can reduce many of health risks connected
with obesity, also including insulin resistance, diabetes,
sleep apnea, high blood pressure, dyslipidemia,
hypoxemia, and hypercapnia, moreover osteoarthritis.
B. The Potential adverse effect of the weight loss includes
the greater threat of gallstone formation furthermore
cholecystitis, the excessive losses of lean body mass,
electrolyte problems or water, mild liver dysfunction, as
well as elevated uric acid level.
C. Minor consequences can also occur, for example diarrhea,
hair loss, constipation or cold intolerance.
D. Short-range adverse reactions are not sufficient to
prohibit weight loss and will not exceed their short-term
benefits.
A. Losing weight can reduce many of health risks connected
with obesity, also including insulin resistance, diabetes,
sleep apnea, high blood pressure, dyslipidemia,
hypoxemia, and hypercapnia, moreover osteoarthritis.
B. The Potential adverse effect of the weight loss includes
the greater threat of gallstone formation furthermore
cholecystitis, the excessive losses of lean body mass,
electrolyte problems or water, mild liver dysfunction, as
well as elevated uric acid level.
C. Minor consequences can also occur, for example diarrhea,
hair loss, constipation or cold intolerance.
D. Short-range adverse reactions are not sufficient to
prohibit weight loss and will not exceed their short-term
benefits.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Intermediate impacts
Long term impacts
Overarching goal of the program
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
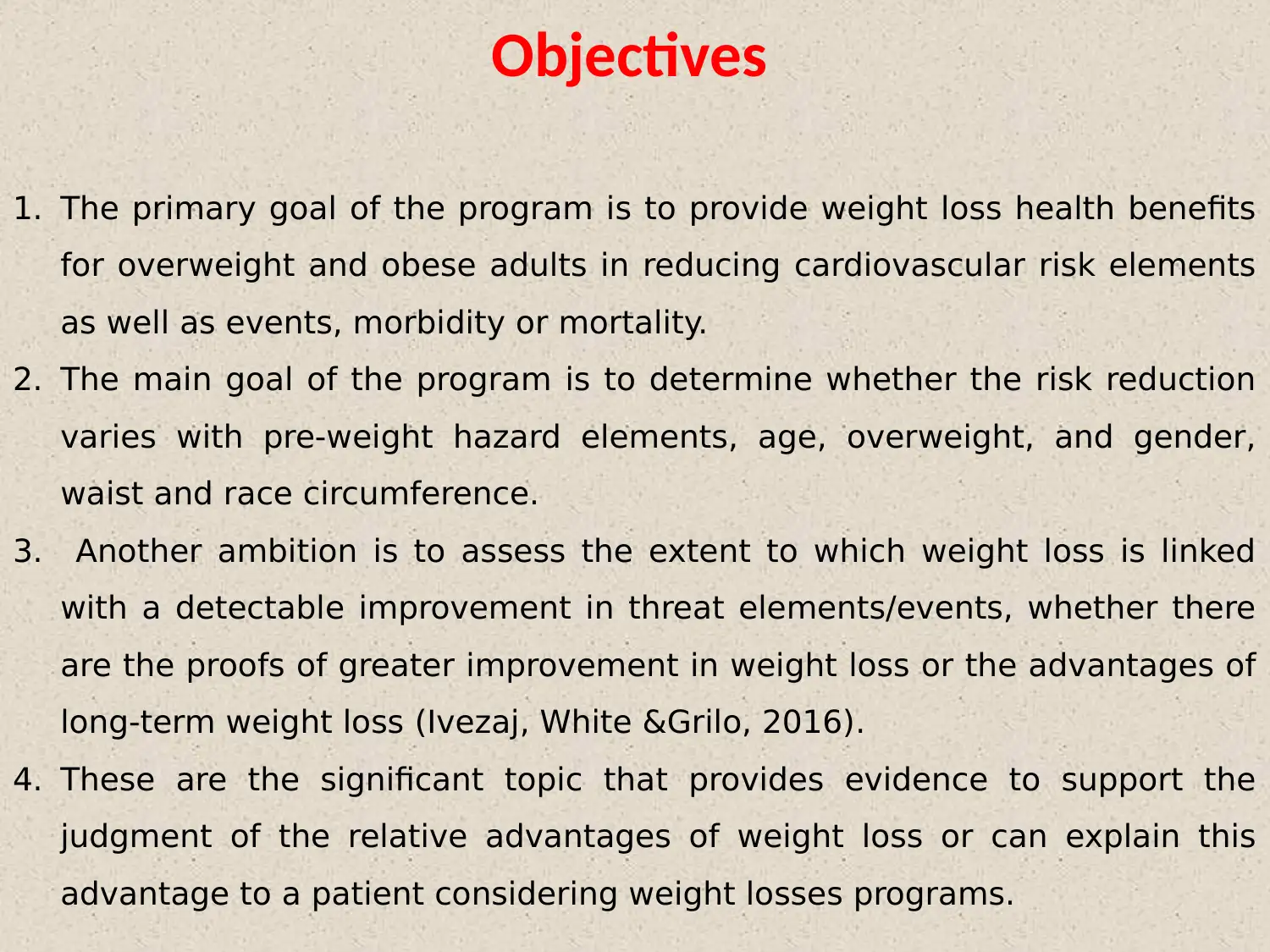
Objectives
1. The primary goal of the program is to provide weight loss health benefits
for overweight and obese adults in reducing cardiovascular risk elements
as well as events, morbidity or mortality.
2. The main goal of the program is to determine whether the risk reduction
varies with pre-weight hazard elements, age, overweight, and gender,
waist and race circumference.
3. Another ambition is to assess the extent to which weight loss is linked
with a detectable improvement in threat elements/events, whether there
are the proofs of greater improvement in weight loss or the advantages of
long-term weight loss (Ivezaj, White &Grilo, 2016).
4. These are the significant topic that provides evidence to support the
judgment of the relative advantages of weight loss or can explain this
advantage to a patient considering weight losses programs.
1. The primary goal of the program is to provide weight loss health benefits
for overweight and obese adults in reducing cardiovascular risk elements
as well as events, morbidity or mortality.
2. The main goal of the program is to determine whether the risk reduction
varies with pre-weight hazard elements, age, overweight, and gender,
waist and race circumference.
3. Another ambition is to assess the extent to which weight loss is linked
with a detectable improvement in threat elements/events, whether there
are the proofs of greater improvement in weight loss or the advantages of
long-term weight loss (Ivezaj, White &Grilo, 2016).
4. These are the significant topic that provides evidence to support the
judgment of the relative advantages of weight loss or can explain this
advantage to a patient considering weight losses programs.
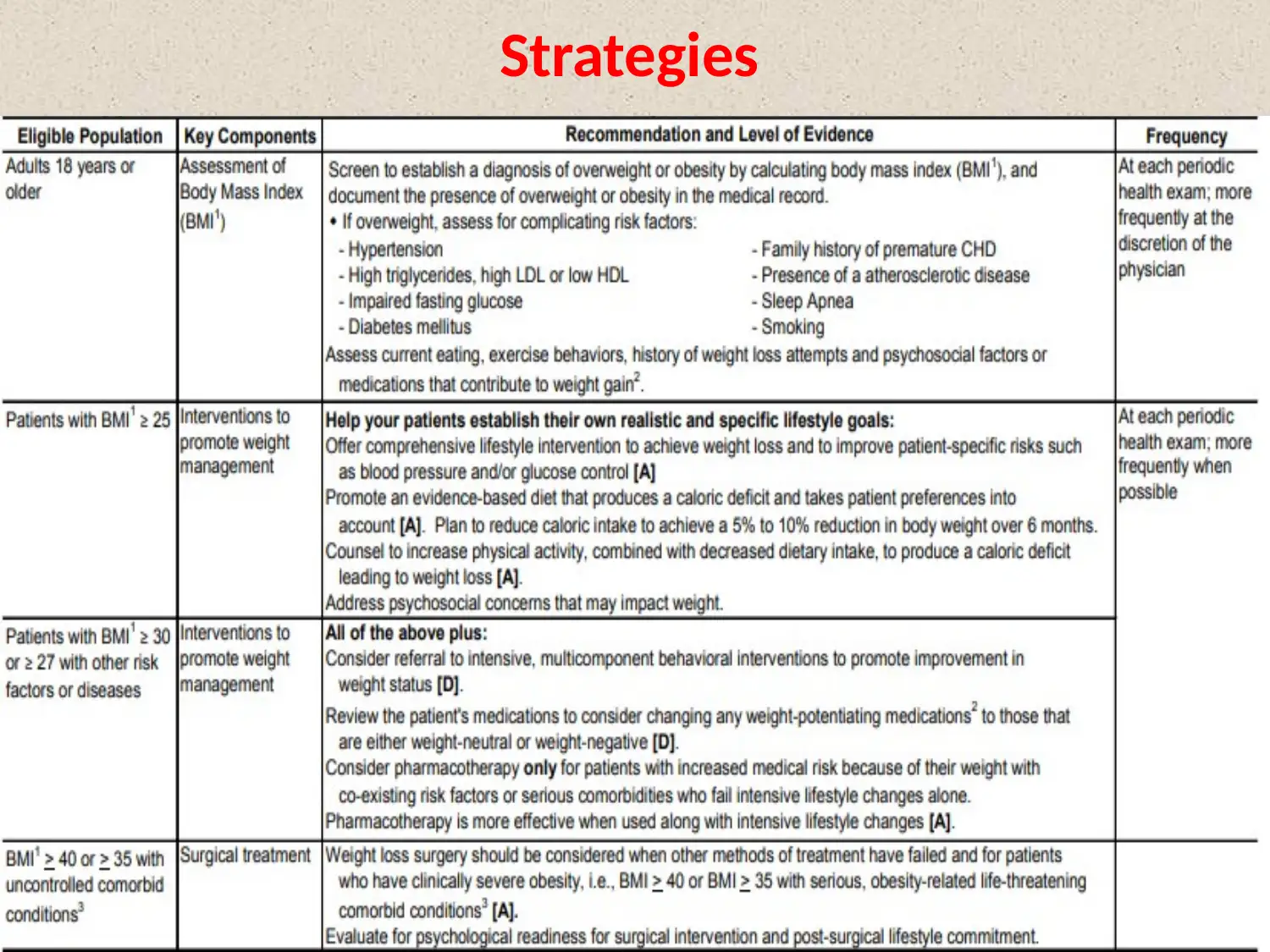
Strategies
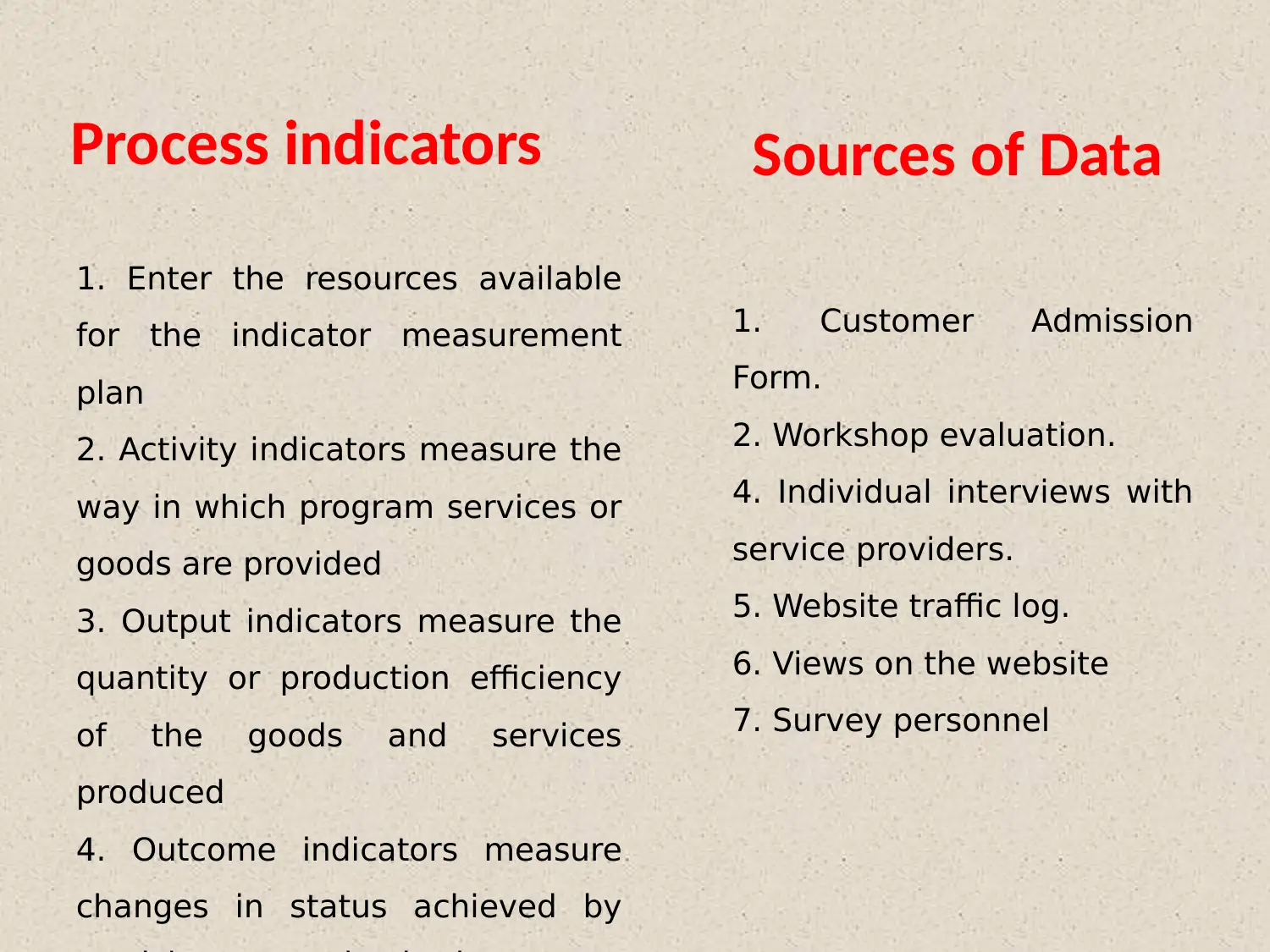
Process indicators Sources of Data
1. Enter the resources available
for the indicator measurement
plan
2. Activity indicators measure the
way in which program services or
goods are provided
3. Output indicators measure the
quantity or production efficiency
of the goods and services
produced
4. Outcome indicators measure
changes in status achieved by
1. Customer Admission
Form.
2. Workshop evaluation.
4. Individual interviews with
service providers.
5. Website traffic log.
6. Views on the website
7. Survey personnel
1. Enter the resources available
for the indicator measurement
plan
2. Activity indicators measure the
way in which program services or
goods are provided
3. Output indicators measure the
quantity or production efficiency
of the goods and services
produced
4. Outcome indicators measure
changes in status achieved by
1. Customer Admission
Form.
2. Workshop evaluation.
4. Individual interviews with
service providers.
5. Website traffic log.
6. Views on the website
7. Survey personnel
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
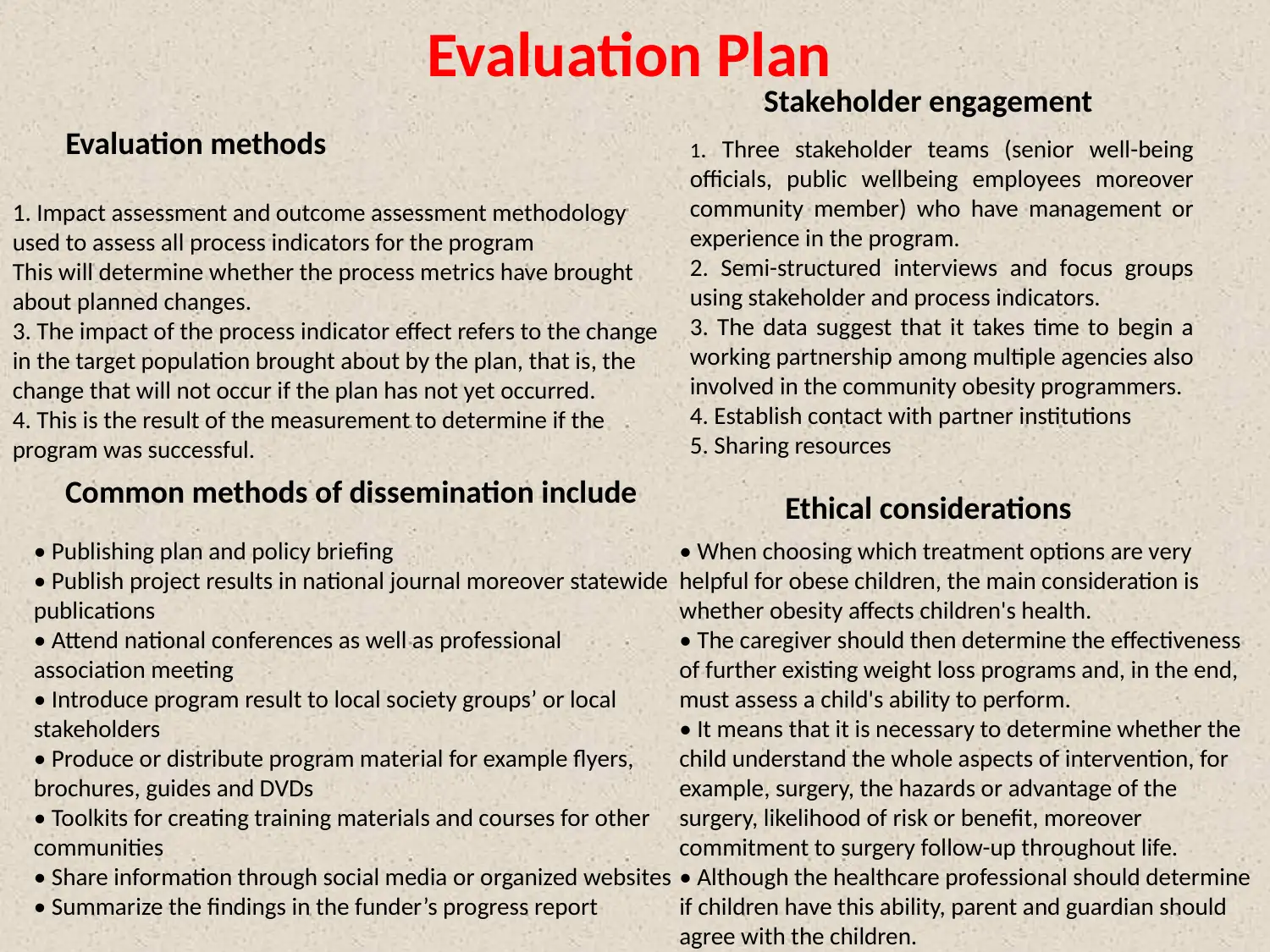
Evaluation Plan
Evaluation methods
Stakeholder engagement
Common methods of dissemination include Ethical considerations
1. Impact assessment and outcome assessment methodology
used to assess all process indicators for the program
This will determine whether the process metrics have brought
about planned changes.
3. The impact of the process indicator effect refers to the change
in the target population brought about by the plan, that is, the
change that will not occur if the plan has not yet occurred.
4. This is the result of the measurement to determine if the
program was successful.
1. Three stakeholder teams (senior well-being
officials, public wellbeing employees moreover
community member) who have management or
experience in the program.
2. Semi-structured interviews and focus groups
using stakeholder and process indicators.
3. The data suggest that it takes time to begin a
working partnership among multiple agencies also
involved in the community obesity programmers.
4. Establish contact with partner institutions
5. Sharing resources
• Publishing plan and policy briefing
• Publish project results in national journal moreover statewide
publications
• Attend national conferences as well as professional
association meeting
• Introduce program result to local society groups’ or local
stakeholders
• Produce or distribute program material for example flyers,
brochures, guides and DVDs
• Toolkits for creating training materials and courses for other
communities
• Share information through social media or organized websites
• Summarize the findings in the funder’s progress report
• When choosing which treatment options are very
helpful for obese children, the main consideration is
whether obesity affects children's health.
• The caregiver should then determine the effectiveness
of further existing weight loss programs and, in the end,
must assess a child's ability to perform.
• It means that it is necessary to determine whether the
child understand the whole aspects of intervention, for
example, surgery, the hazards or advantage of the
surgery, likelihood of risk or benefit, moreover
commitment to surgery follow-up throughout life.
• Although the healthcare professional should determine
if children have this ability, parent and guardian should
agree with the children.
Evaluation methods
Stakeholder engagement
Common methods of dissemination include Ethical considerations
1. Impact assessment and outcome assessment methodology
used to assess all process indicators for the program
This will determine whether the process metrics have brought
about planned changes.
3. The impact of the process indicator effect refers to the change
in the target population brought about by the plan, that is, the
change that will not occur if the plan has not yet occurred.
4. This is the result of the measurement to determine if the
program was successful.
1. Three stakeholder teams (senior well-being
officials, public wellbeing employees moreover
community member) who have management or
experience in the program.
2. Semi-structured interviews and focus groups
using stakeholder and process indicators.
3. The data suggest that it takes time to begin a
working partnership among multiple agencies also
involved in the community obesity programmers.
4. Establish contact with partner institutions
5. Sharing resources
• Publishing plan and policy briefing
• Publish project results in national journal moreover statewide
publications
• Attend national conferences as well as professional
association meeting
• Introduce program result to local society groups’ or local
stakeholders
• Produce or distribute program material for example flyers,
brochures, guides and DVDs
• Toolkits for creating training materials and courses for other
communities
• Share information through social media or organized websites
• Summarize the findings in the funder’s progress report
• When choosing which treatment options are very
helpful for obese children, the main consideration is
whether obesity affects children's health.
• The caregiver should then determine the effectiveness
of further existing weight loss programs and, in the end,
must assess a child's ability to perform.
• It means that it is necessary to determine whether the
child understand the whole aspects of intervention, for
example, surgery, the hazards or advantage of the
surgery, likelihood of risk or benefit, moreover
commitment to surgery follow-up throughout life.
• Although the healthcare professional should determine
if children have this ability, parent and guardian should
agree with the children.
Risks or
Challenges Management of
risks
1. The stigma of the obesity is general in the
society, as a well as an obese person often faces
negative attitude moreover discriminatory
behavior.
2. Healthcare professionals can exhibit lazy, and
fewer competent negative stereotypes for obese
people.
3. Obese often patients feel unwelcome in the
medical environment and can decide to avoid and
delay the attention to seek medical issues.
1. For people who are determined to be
obese, that person - not obesity - must be
the focus of the treatment.
2. Perceptive care for obese patients also
needed respect or compassion.
3. For clinicians, it is significant to first
establish a trust relationship by addressing
the patient's defined health care goals to
address weight loss issues.
Challenges Management of
risks
1. The stigma of the obesity is general in the
society, as a well as an obese person often faces
negative attitude moreover discriminatory
behavior.
2. Healthcare professionals can exhibit lazy, and
fewer competent negative stereotypes for obese
people.
3. Obese often patients feel unwelcome in the
medical environment and can decide to avoid and
delay the attention to seek medical issues.
1. For people who are determined to be
obese, that person - not obesity - must be
the focus of the treatment.
2. Perceptive care for obese patients also
needed respect or compassion.
3. For clinicians, it is significant to first
establish a trust relationship by addressing
the patient's defined health care goals to
address weight loss issues.
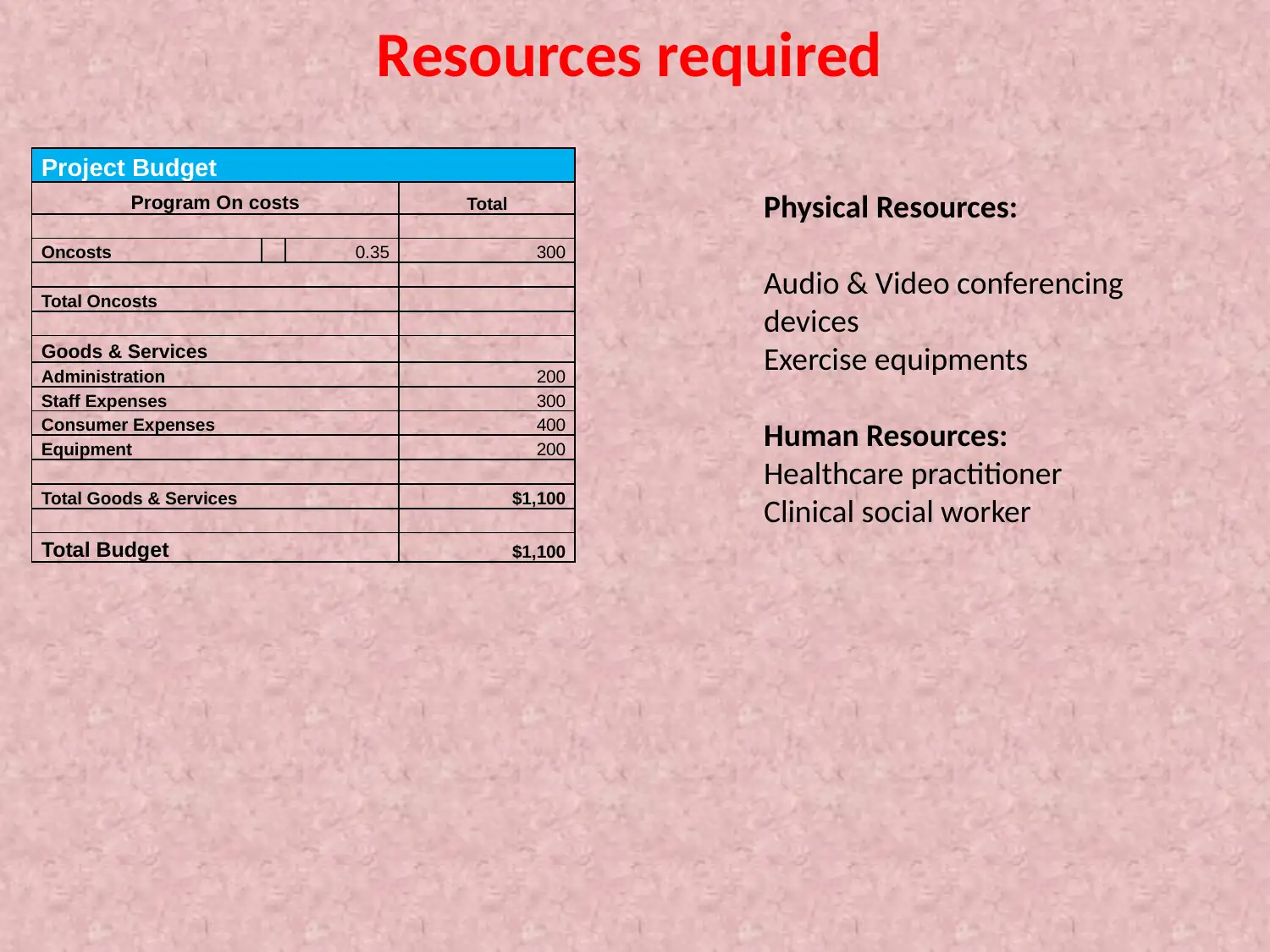
Resources required
Project Budget
Program On costs Total
Oncosts 0.35 300
Total Oncosts
Goods & Services
Administration 200
Staff Expenses 300
Consumer Expenses 400
Equipment 200
Total Goods & Services $1,100
Total Budget $1,100
Physical Resources:
Audio & Video conferencing
devices
Exercise equipments
Human Resources:
Healthcare practitioner
Clinical social worker
Project Budget
Program On costs Total
Oncosts 0.35 300
Total Oncosts
Goods & Services
Administration 200
Staff Expenses 300
Consumer Expenses 400
Equipment 200
Total Goods & Services $1,100
Total Budget $1,100
Physical Resources:
Audio & Video conferencing
devices
Exercise equipments
Human Resources:
Healthcare practitioner
Clinical social worker
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
References
Ayatollahi, S., &Ghoreshizadeh, Z. (2012). Prevalence of obesity and overweight among adults in Iran. Obesity
Reviews, 11(5), 335-337.
Castro, M., Venutolo, C., Yau, P., &Convit, A. (2016). Fitness, insulin sensitivity, and frontal lobe integrity in adults with
overweight and obesity. Obesity, 24(6), 1283-1289.
Foulds, H., Bredin, S., & Warburton, D. (2011). The prevalence of overweight and obesity in British Columbian Aboriginal
adults. Obesity Reviews, 12(5), e4-e11.
Heber, D. (2013). Overweight and Obesity in Cancer Risk and Survival. Obesity Management, 3(3), 111-114.
Hill, J. (2014). Increasing Overweight to Address the Obesity Epidemic. Obesity Management, 5(2), 41-42.
Ivezaj, V., White, M., &Grilo, C. (2016). Examining binge-eating disorder and food addiction in adults with overweight and
obesity. Obesity, 24(10), 2064-2069.
JF, G., CR, C., & AW, T. (2016). Parental Midlife Body Shape Influences Offspring Self-Perception of Weight in a Cohort of
Australian Adults. Journal Of Obesity And Overweight.
Katulanda, P., Jayawardena, M., Sheriff, M., Constantine, G., & Matthews, D. (2013). Prevalence of overweight and obesity in
Sri Lankan adults. Obesity Reviews, 11(11), 751-756.
Khambalia, A., & Seen, L. (2014). Trends in overweight and obese adults in Malaysia (1996-2009): a systematic
review. Obesity Reviews, 11(6), 403-412.
Papadopoulos, S., & Brennan, L. (2015). Correlates of weight stigma in adults with overweight and obesity: A systematic
literature review. Obesity, 23(9), 1743-1760.
Parnell, J., Klancic, T., & Reimer, R. (2017). Oligofructose decreases serum lipopolysaccharide and plasminogen activator
inhibitor-1 in adults with overweight/obesity. Obesity, 25(3), 510-513.
Peres, A. (2015). Body Composition but not Cardiorespiratory Fitness Correlate with Adipokines in Overweight-Obese
Adults. Advances In Obesity, Weight Management & Control, 2(2).
Shin, M. (2014). Management of Overweight and Obesity: Review of the "2013 AHA/ACC/TOS Guideline for the
Management of Overweight and Obesity in Adults". Korean Journal Of Medicine, 87(2), 136.
Udo, T., &Grilo, C. (2016). Perceived weight discrimination, childhood maltreatment, and weight gain in U.S. adults with
overweight/obesity. Obesity, 24(6), 1366-1372.
Wunderlich, S. (2012). Overweight and Obesity among Older Adults: How should Obesity be Determined?. Journal Of
Obesity & Weight Loss Therapy, 02(08).
Ayatollahi, S., &Ghoreshizadeh, Z. (2012). Prevalence of obesity and overweight among adults in Iran. Obesity
Reviews, 11(5), 335-337.
Castro, M., Venutolo, C., Yau, P., &Convit, A. (2016). Fitness, insulin sensitivity, and frontal lobe integrity in adults with
overweight and obesity. Obesity, 24(6), 1283-1289.
Foulds, H., Bredin, S., & Warburton, D. (2011). The prevalence of overweight and obesity in British Columbian Aboriginal
adults. Obesity Reviews, 12(5), e4-e11.
Heber, D. (2013). Overweight and Obesity in Cancer Risk and Survival. Obesity Management, 3(3), 111-114.
Hill, J. (2014). Increasing Overweight to Address the Obesity Epidemic. Obesity Management, 5(2), 41-42.
Ivezaj, V., White, M., &Grilo, C. (2016). Examining binge-eating disorder and food addiction in adults with overweight and
obesity. Obesity, 24(10), 2064-2069.
JF, G., CR, C., & AW, T. (2016). Parental Midlife Body Shape Influences Offspring Self-Perception of Weight in a Cohort of
Australian Adults. Journal Of Obesity And Overweight.
Katulanda, P., Jayawardena, M., Sheriff, M., Constantine, G., & Matthews, D. (2013). Prevalence of overweight and obesity in
Sri Lankan adults. Obesity Reviews, 11(11), 751-756.
Khambalia, A., & Seen, L. (2014). Trends in overweight and obese adults in Malaysia (1996-2009): a systematic
review. Obesity Reviews, 11(6), 403-412.
Papadopoulos, S., & Brennan, L. (2015). Correlates of weight stigma in adults with overweight and obesity: A systematic
literature review. Obesity, 23(9), 1743-1760.
Parnell, J., Klancic, T., & Reimer, R. (2017). Oligofructose decreases serum lipopolysaccharide and plasminogen activator
inhibitor-1 in adults with overweight/obesity. Obesity, 25(3), 510-513.
Peres, A. (2015). Body Composition but not Cardiorespiratory Fitness Correlate with Adipokines in Overweight-Obese
Adults. Advances In Obesity, Weight Management & Control, 2(2).
Shin, M. (2014). Management of Overweight and Obesity: Review of the "2013 AHA/ACC/TOS Guideline for the
Management of Overweight and Obesity in Adults". Korean Journal Of Medicine, 87(2), 136.
Udo, T., &Grilo, C. (2016). Perceived weight discrimination, childhood maltreatment, and weight gain in U.S. adults with
overweight/obesity. Obesity, 24(6), 1366-1372.
Wunderlich, S. (2012). Overweight and Obesity among Older Adults: How should Obesity be Determined?. Journal Of
Obesity & Weight Loss Therapy, 02(08).
1 out of 17
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.