Palliative Care Practice for Lung Cancer Patient - Medication Management Review
VerifiedAdded on 2023/06/12
|15
|3825
|250
AI Summary
This article discusses the medication management review for a lung cancer patient in palliative care. It covers the patient's initial diagnosis, expected medications, and recommendations for transitioning to end-of-life care. The article also includes a GP letter and a table of recommendations.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: Palliative care practice
Palliative care practice
Name of the student:
Name of the University:
Author’s note
Palliative care practice
Name of the student:
Name of the University:
Author’s note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1PALLIATIVE CARE PRACTICE
Initial diagnosis and brief explanation of the Patient condition
The pathogenesis of lung cancer along with other forms is commenced after the induction from
various habits like smoking which the patient was exposed to for a long time. The diseases
progression promoted the development of the multiple metastases in the patient (1). The patient
Tom was a chain smoker since sixteen years of age and that has rendered the development of
other associated pathogenesis like breathing troubles and susceptibility to pulmonary infection.
The patient complained breathing troubles along with chest pain. Lung cancer is known to be
facilitated by smoking cigarettes, which leads to severe disease manifestation. The diseases
manifestation occurs when the mutations in p53 gene which is a known tumor suppressor.
Smoking induces the pathogenesis by a phenomenon called “field effect” which affects the
epithelial tissues in the lungs and initiates cellular transformation (2). The continuation of
smoking induces the mutation process, which further alter the tissue structure and metastasis
generation in the surrounding tissues. This form of diseases progression takes about 20-25 years
to develop and since the onset of mutation. The risk of cancer exposure is initiated by the
smoking habits, which is enhanced by the effect of environment factors like pollutants. In case of
Tom, who is a construction worker received risk of exposure of environmental factors. The
condition of the patient was of centrally located tumor type. The patient showed signs of tumor
growth, which induced coughing, chest pain, atelectasis, post obstructive pneumonia. Tom also
showed sign wheezing breath and pericardial effusion. Diagnosis showed that the type of cancer
in Tom was of small cell lung carcinoma (SCLC) which is common for rigorous smokers (3). It
is centrally located where the tumor blocks the bifurcation of the airways. The origin of the
cancer was seen in the neuro-endocrine cells which produce neurotransmitters, growth factors
and vasoactive compounds which regulate the functionality of the lungs. Tom is detected to
Initial diagnosis and brief explanation of the Patient condition
The pathogenesis of lung cancer along with other forms is commenced after the induction from
various habits like smoking which the patient was exposed to for a long time. The diseases
progression promoted the development of the multiple metastases in the patient (1). The patient
Tom was a chain smoker since sixteen years of age and that has rendered the development of
other associated pathogenesis like breathing troubles and susceptibility to pulmonary infection.
The patient complained breathing troubles along with chest pain. Lung cancer is known to be
facilitated by smoking cigarettes, which leads to severe disease manifestation. The diseases
manifestation occurs when the mutations in p53 gene which is a known tumor suppressor.
Smoking induces the pathogenesis by a phenomenon called “field effect” which affects the
epithelial tissues in the lungs and initiates cellular transformation (2). The continuation of
smoking induces the mutation process, which further alter the tissue structure and metastasis
generation in the surrounding tissues. This form of diseases progression takes about 20-25 years
to develop and since the onset of mutation. The risk of cancer exposure is initiated by the
smoking habits, which is enhanced by the effect of environment factors like pollutants. In case of
Tom, who is a construction worker received risk of exposure of environmental factors. The
condition of the patient was of centrally located tumor type. The patient showed signs of tumor
growth, which induced coughing, chest pain, atelectasis, post obstructive pneumonia. Tom also
showed sign wheezing breath and pericardial effusion. Diagnosis showed that the type of cancer
in Tom was of small cell lung carcinoma (SCLC) which is common for rigorous smokers (3). It
is centrally located where the tumor blocks the bifurcation of the airways. The origin of the
cancer was seen in the neuro-endocrine cells which produce neurotransmitters, growth factors
and vasoactive compounds which regulate the functionality of the lungs. Tom is detected to
2PALLIATIVE CARE PRACTICE
secrete ADH or ACTH. The growth of the tumor is very quick and the condition has spread to
various parts of his body. The CT scan report revealed that pathogenesis of his report. Low dose
x-ray scan showed abnormal mass index of the lung tissues in Tom. Lesions and other
abnormalities were detected which showed signs of carcinogenesis. Tom was diagnosed also on
the basis of sputum generation which showed abnormality. The main biopsy report showed that
Tom had stage II carcinoma (5). Tom also displayed symptoms of chest pain, asthma and
diabetes. The blood test revealed that Tom had 180mg/dl blood glucose level, which needed to
be controlled. Tom complained breathing trouble from time to time, which was diagnosed to be
asthma. The associated co morbidities made it more complicated to care for Tom.
Expected medications
The medication for Tom was provided by the practitioner to minimize his chest pain. Morphine
was selected the best choice for his condition which Tom was reluctant to take due to his lack of
knowledge and literacy. Tom was prescribed mitiglinide to treat his diabetes and for controlling
asthma, Formoterol was administered. Mitiglinide is the most preferred drug for treating type 2
diabetes as in case of Tom, it stimulates the by the blocking the channels and influx of calcium in
the cells (4). The excitation of the cell due to influx of calcium triggers the exocytosis of insulin
compounds. Formoterol is the beta 2 agonist, which causes dilation of bronchial cells and
provides passage off blood in the pulmonary compartments and induces the relaxation of smooth
myocytes such that the air is forced inside the lungs and the breathlessness is inhibited (6). The
severity of Tom’s cancer progression needed immediate chemotherapy to min size the growth of
the tumor. The biopsy report showed that Tom has stage IIa, meaning his tumor was 5cm in
diameter. The practitioner also prescribed targeted drug therapy for Tom, which included
administration of specialized drugs which bind to specialized receptors of the tumors and
secrete ADH or ACTH. The growth of the tumor is very quick and the condition has spread to
various parts of his body. The CT scan report revealed that pathogenesis of his report. Low dose
x-ray scan showed abnormal mass index of the lung tissues in Tom. Lesions and other
abnormalities were detected which showed signs of carcinogenesis. Tom was diagnosed also on
the basis of sputum generation which showed abnormality. The main biopsy report showed that
Tom had stage II carcinoma (5). Tom also displayed symptoms of chest pain, asthma and
diabetes. The blood test revealed that Tom had 180mg/dl blood glucose level, which needed to
be controlled. Tom complained breathing trouble from time to time, which was diagnosed to be
asthma. The associated co morbidities made it more complicated to care for Tom.
Expected medications
The medication for Tom was provided by the practitioner to minimize his chest pain. Morphine
was selected the best choice for his condition which Tom was reluctant to take due to his lack of
knowledge and literacy. Tom was prescribed mitiglinide to treat his diabetes and for controlling
asthma, Formoterol was administered. Mitiglinide is the most preferred drug for treating type 2
diabetes as in case of Tom, it stimulates the by the blocking the channels and influx of calcium in
the cells (4). The excitation of the cell due to influx of calcium triggers the exocytosis of insulin
compounds. Formoterol is the beta 2 agonist, which causes dilation of bronchial cells and
provides passage off blood in the pulmonary compartments and induces the relaxation of smooth
myocytes such that the air is forced inside the lungs and the breathlessness is inhibited (6). The
severity of Tom’s cancer progression needed immediate chemotherapy to min size the growth of
the tumor. The biopsy report showed that Tom has stage IIa, meaning his tumor was 5cm in
diameter. The practitioner also prescribed targeted drug therapy for Tom, which included
administration of specialized drugs which bind to specialized receptors of the tumors and
3PALLIATIVE CARE PRACTICE
identify the tumor proteins and destroy their functionality. The therapy was associated with
chemotherapy, radiation therapy and interventional pulmonology from time to time. The
practitioner selected Crizotinib and Erlotinib, which is a known inhibitors of the kinase enzymes
in the cancer cells and help checking the cancer cell growth (7).
Summary of assumptions:
Medications usage during transition to palliative care and medications needed during progress
to end stage of disease:
At the end stage of lung cancer, the main issue for Mr. Tom is that he is having extensive
breathing problem and chronic pain. When palliative care is initiated, it is expected that patients
current medication regimen needs to be changed. Pain is a symptom that is seen in lung cancer
patient due to local effect of tumor or distant spread of tumor. Since Mr. Tom has been shifted to
end of life care because deteriorating symptom of pain, it is expected that palliative pain
management in initiated for Mr. Tom. Morphine is the first medication for pain management in
patients. However, this medication is associated with increase in symptom alleviation at end of
life (8). Hence, to provide high quality palliative care, it is expected that low dose of Opioid is
given to Mr. Tom. The use of opioids is considered effective for the management of advanced
lung cancer patient as it has no impact on their quality of life. The evidence also suggested that
opioid administration has no impact on survival rate of patient in acute care setting. The study
done regarding survival rate on opioid users in acute care setting suggested that there is no
significant difference in survival time of patient after mean daily dose of opioid (8). Hence,
opioid use is efficacious for Mr. Tom, only thing that needs to be considered by palliative care
identify the tumor proteins and destroy their functionality. The therapy was associated with
chemotherapy, radiation therapy and interventional pulmonology from time to time. The
practitioner selected Crizotinib and Erlotinib, which is a known inhibitors of the kinase enzymes
in the cancer cells and help checking the cancer cell growth (7).
Summary of assumptions:
Medications usage during transition to palliative care and medications needed during progress
to end stage of disease:
At the end stage of lung cancer, the main issue for Mr. Tom is that he is having extensive
breathing problem and chronic pain. When palliative care is initiated, it is expected that patients
current medication regimen needs to be changed. Pain is a symptom that is seen in lung cancer
patient due to local effect of tumor or distant spread of tumor. Since Mr. Tom has been shifted to
end of life care because deteriorating symptom of pain, it is expected that palliative pain
management in initiated for Mr. Tom. Morphine is the first medication for pain management in
patients. However, this medication is associated with increase in symptom alleviation at end of
life (8). Hence, to provide high quality palliative care, it is expected that low dose of Opioid is
given to Mr. Tom. The use of opioids is considered effective for the management of advanced
lung cancer patient as it has no impact on their quality of life. The evidence also suggested that
opioid administration has no impact on survival rate of patient in acute care setting. The study
done regarding survival rate on opioid users in acute care setting suggested that there is no
significant difference in survival time of patient after mean daily dose of opioid (8). Hence,
opioid use is efficacious for Mr. Tom, only thing that needs to be considered by palliative care
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4PALLIATIVE CARE PRACTICE
staff is to provide optimal dose of Morphine. It any side-effects like drowsiness persist, then
other opioids can also be provided.
During the transition of patient to end stage of disease, it is likely that pain related
symptom of Mr. Tom will exacebarate. At this time, strong opioid like Oxycodone should be
started for patient. Other advanced analgesics like NDM receptor antagonist may also be initiated
for patient as it acts on the central nervous system to treat underlying chronic pain.
Corticosteroid is also a useful treatment option for cancer related pain (9). It is also necessary to
consider patient and families cultural factosr while providing palliative care. Clinician or
palliative care should be vigilatnt to review adverse impact of any medication and change theme
instantly. The focus should to support patient at end-of-life and not aggravate presenting
symptom of patient (10).
Another major problem for patient is chronic pain. Hence, when palliative care is
provided, it is necessary to review appropriate medication to manage breathing problem.
Shortness of breath and cough are disturbing symptoms of end-of-life care patient and the
challenges for patient increase particularly for advanced lung cancer. In case of Mr. Tom, the
main challenge is that his symptom of pain has aggravated because of history of asthma and
smoking. This has increased risk of complication in patient. As this medication management
review is focused on reviewing medication management regimen of Mr. Tom, reviewing
pharmacological options for management of lung cancer patient is necessary. Opiods can be used
to treat dyspnea in patient. Many stuies have shown the effectiveness of oral opioids on shortness
of breath in cancer patient. Another special consideration during end-stage of life is that low dose
of opioid should be given to treat breathing problem. The initial does should be 2.4 mg morphine
every four hours in Mr Tom. This can relief symptom of patient. As Mr. Tom is reluctant to take
staff is to provide optimal dose of Morphine. It any side-effects like drowsiness persist, then
other opioids can also be provided.
During the transition of patient to end stage of disease, it is likely that pain related
symptom of Mr. Tom will exacebarate. At this time, strong opioid like Oxycodone should be
started for patient. Other advanced analgesics like NDM receptor antagonist may also be initiated
for patient as it acts on the central nervous system to treat underlying chronic pain.
Corticosteroid is also a useful treatment option for cancer related pain (9). It is also necessary to
consider patient and families cultural factosr while providing palliative care. Clinician or
palliative care should be vigilatnt to review adverse impact of any medication and change theme
instantly. The focus should to support patient at end-of-life and not aggravate presenting
symptom of patient (10).
Another major problem for patient is chronic pain. Hence, when palliative care is
provided, it is necessary to review appropriate medication to manage breathing problem.
Shortness of breath and cough are disturbing symptoms of end-of-life care patient and the
challenges for patient increase particularly for advanced lung cancer. In case of Mr. Tom, the
main challenge is that his symptom of pain has aggravated because of history of asthma and
smoking. This has increased risk of complication in patient. As this medication management
review is focused on reviewing medication management regimen of Mr. Tom, reviewing
pharmacological options for management of lung cancer patient is necessary. Opiods can be used
to treat dyspnea in patient. Many stuies have shown the effectiveness of oral opioids on shortness
of breath in cancer patient. Another special consideration during end-stage of life is that low dose
of opioid should be given to treat breathing problem. The initial does should be 2.4 mg morphine
every four hours in Mr Tom. This can relief symptom of patient. As Mr. Tom is reluctant to take
5PALLIATIVE CARE PRACTICE
morphine because of fear of sedation, it is necessary to clearly advice to Mr. Tom that low does
of Morphine will not cause any effect on patient.
During the end-stage of life, oxygen can also be administered for pain relief. However,
for end-of-life patient, stringent criteria exist for treatment with supplementation oxygen because
of adverse effects like poor mobility and dryness of respiratory mucosa. Opioids are effective
antitussants that has low toxicity and maximum health benefits for lung cancer patient. They
suppress cough and helps patient to recover from deteriorating sign and symptoms of breathing
problem (11).
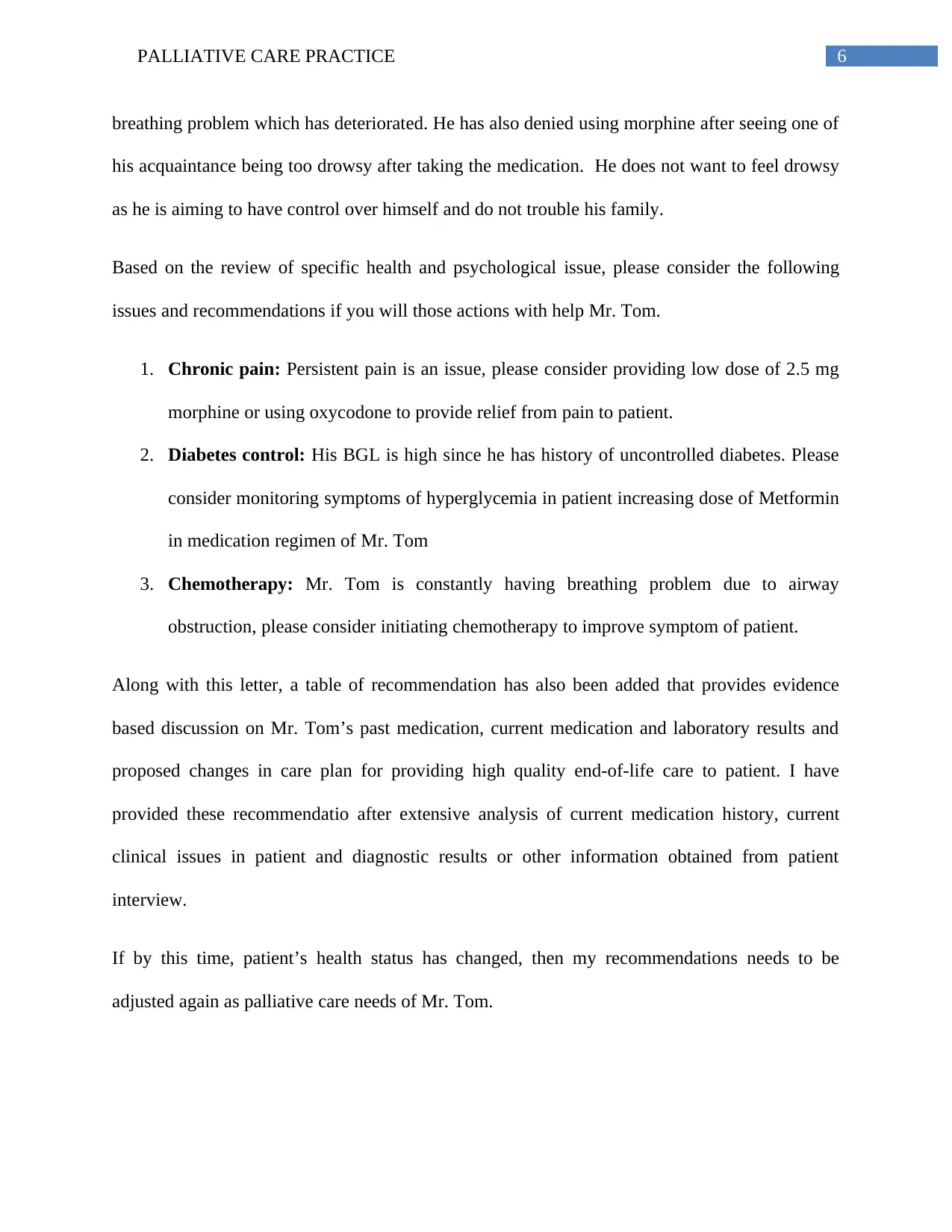
GP letter:
Dr. Philips (Hyopothetical)
Oncologist
Date: 28th April 2018
Re: Mr. Tom’s Medication Management Review Referral Report
Dear Dr. Philips,
I would like to thank you for referring Mr. Tom, a 55 year old patient, residence of Grove, NSW
for a MMR. Based on review of case history of client, it has been found that Mr. Tom is worried
about the medication that is going to be used for his treatment in the palliative care. His mental
compliance is ok and he has no psychosocial issues. However, he has reported acute pain and
morphine because of fear of sedation, it is necessary to clearly advice to Mr. Tom that low does
of Morphine will not cause any effect on patient.
During the end-stage of life, oxygen can also be administered for pain relief. However,
for end-of-life patient, stringent criteria exist for treatment with supplementation oxygen because
of adverse effects like poor mobility and dryness of respiratory mucosa. Opioids are effective
antitussants that has low toxicity and maximum health benefits for lung cancer patient. They
suppress cough and helps patient to recover from deteriorating sign and symptoms of breathing
problem (11).
GP letter:
Dr. Philips (Hyopothetical)
Oncologist
Date: 28th April 2018
Re: Mr. Tom’s Medication Management Review Referral Report
Dear Dr. Philips,
I would like to thank you for referring Mr. Tom, a 55 year old patient, residence of Grove, NSW
for a MMR. Based on review of case history of client, it has been found that Mr. Tom is worried
about the medication that is going to be used for his treatment in the palliative care. His mental
compliance is ok and he has no psychosocial issues. However, he has reported acute pain and
6PALLIATIVE CARE PRACTICE
breathing problem which has deteriorated. He has also denied using morphine after seeing one of
his acquaintance being too drowsy after taking the medication. He does not want to feel drowsy
as he is aiming to have control over himself and do not trouble his family.
Based on the review of specific health and psychological issue, please consider the following
issues and recommendations if you will those actions with help Mr. Tom.
1. Chronic pain: Persistent pain is an issue, please consider providing low dose of 2.5 mg
morphine or using oxycodone to provide relief from pain to patient.
2. Diabetes control: His BGL is high since he has history of uncontrolled diabetes. Please
consider monitoring symptoms of hyperglycemia in patient increasing dose of Metformin
in medication regimen of Mr. Tom
3. Chemotherapy: Mr. Tom is constantly having breathing problem due to airway
obstruction, please consider initiating chemotherapy to improve symptom of patient.
Along with this letter, a table of recommendation has also been added that provides evidence
based discussion on Mr. Tom’s past medication, current medication and laboratory results and
proposed changes in care plan for providing high quality end-of-life care to patient. I have
provided these recommendatio after extensive analysis of current medication history, current
clinical issues in patient and diagnostic results or other information obtained from patient
interview.
If by this time, patient’s health status has changed, then my recommendations needs to be
adjusted again as palliative care needs of Mr. Tom.
breathing problem which has deteriorated. He has also denied using morphine after seeing one of
his acquaintance being too drowsy after taking the medication. He does not want to feel drowsy
as he is aiming to have control over himself and do not trouble his family.
Based on the review of specific health and psychological issue, please consider the following
issues and recommendations if you will those actions with help Mr. Tom.
1. Chronic pain: Persistent pain is an issue, please consider providing low dose of 2.5 mg
morphine or using oxycodone to provide relief from pain to patient.
2. Diabetes control: His BGL is high since he has history of uncontrolled diabetes. Please
consider monitoring symptoms of hyperglycemia in patient increasing dose of Metformin
in medication regimen of Mr. Tom
3. Chemotherapy: Mr. Tom is constantly having breathing problem due to airway
obstruction, please consider initiating chemotherapy to improve symptom of patient.
Along with this letter, a table of recommendation has also been added that provides evidence
based discussion on Mr. Tom’s past medication, current medication and laboratory results and
proposed changes in care plan for providing high quality end-of-life care to patient. I have
provided these recommendatio after extensive analysis of current medication history, current
clinical issues in patient and diagnostic results or other information obtained from patient
interview.
If by this time, patient’s health status has changed, then my recommendations needs to be
adjusted again as palliative care needs of Mr. Tom.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7PALLIATIVE CARE PRACTICE
I am looking forward to hear from you soon regarding my proposed palliative care plan for Mr.
Tom. If you need to get any extra information related patient’s health status, please feel free to
contact me or discuss the same with Mrs Cec, Mr. Tom’s wife.
Yours faithfully,
(Name and date)
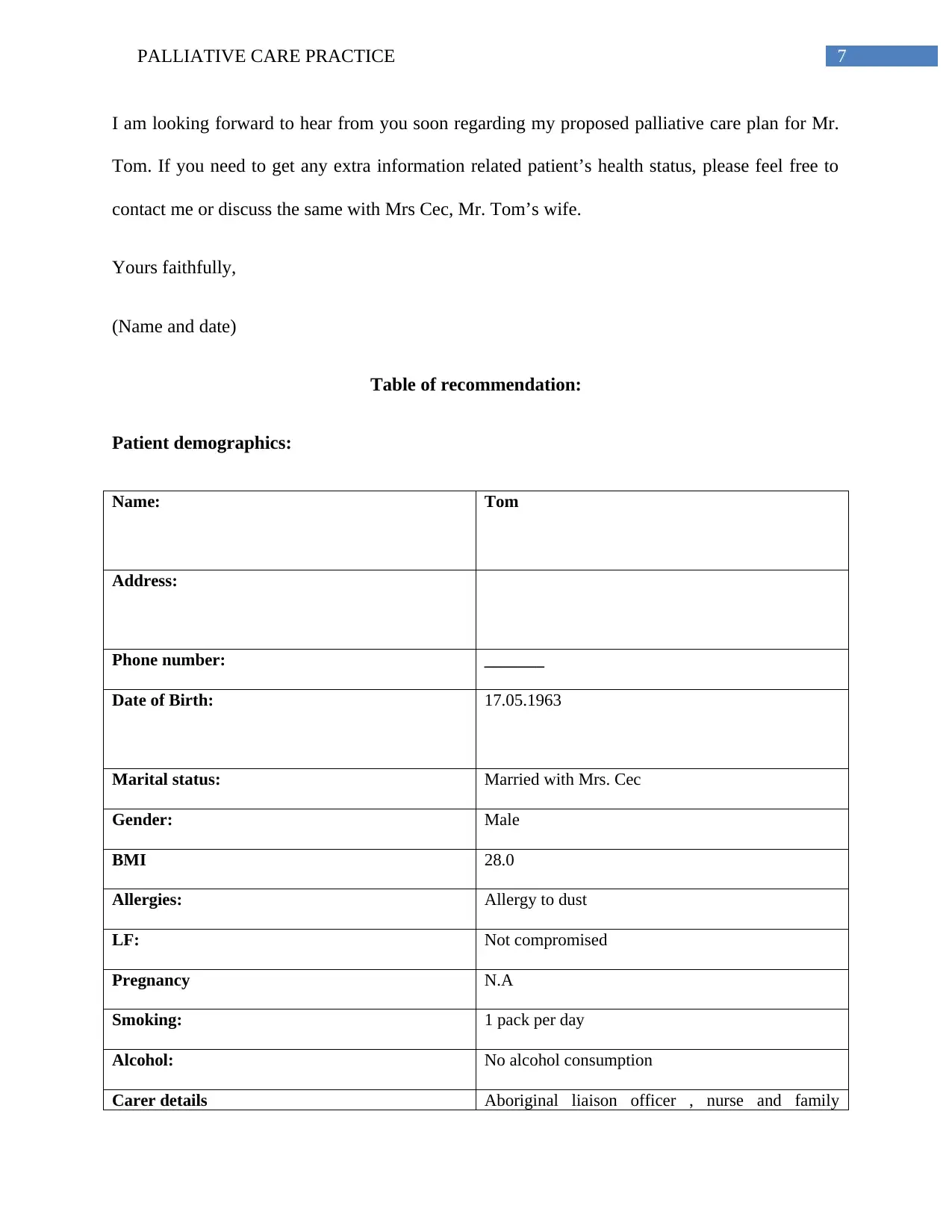
Table of recommendation:
Patient demographics:
Name: Tom
Address:
Phone number: _______
Date of Birth: 17.05.1963
Marital status: Married with Mrs. Cec
Gender: Male
BMI 28.0
Allergies: Allergy to dust
LF: Not compromised
Pregnancy N.A
Smoking: 1 pack per day
Alcohol: No alcohol consumption
Carer details Aboriginal liaison officer , nurse and family
I am looking forward to hear from you soon regarding my proposed palliative care plan for Mr.
Tom. If you need to get any extra information related patient’s health status, please feel free to
contact me or discuss the same with Mrs Cec, Mr. Tom’s wife.
Yours faithfully,
(Name and date)
Table of recommendation:
Patient demographics:
Name: Tom
Address:
Phone number: _______
Date of Birth: 17.05.1963
Marital status: Married with Mrs. Cec
Gender: Male
BMI 28.0
Allergies: Allergy to dust
LF: Not compromised
Pregnancy N.A
Smoking: 1 pack per day
Alcohol: No alcohol consumption
Carer details Aboriginal liaison officer , nurse and family
8PALLIATIVE CARE PRACTICE
members
Treating Dr. details Oncologist
Medical conditions: Advanced lung cancer
Medical history:
History of uncontrolled diabetes, heavy smoker and history of respiratory problem due to asthma
Medication history of Mr. Tom indicates the risk factor of lung cancer in patient. One researcher
states that smoking is one of the major risk factor of lung cancer (12). Mr. Tom’s past history of
chronic asthma also explains the pathway that led to lung cancer development in patient. Another
author gives the evidence that chronic inflammation during asthma plays an important role in
cancer development (13). Through meta-analysis of evidence, it was proved that asthma
increases risk of lung cancer I patient.
Current complaints:
Persistent pain and breathing problem is the main complaints of patient.
Evidence by (3) suggest that breathing problem is one major issue that challenges advanced lung
cancer patients and their family caregivers from coping with the disease. Many lung cancer
patients have reported that they have hard time catching their breath. The rate of anxiety and
depressive symptom in higher in lung cancer patient compared to other patient.
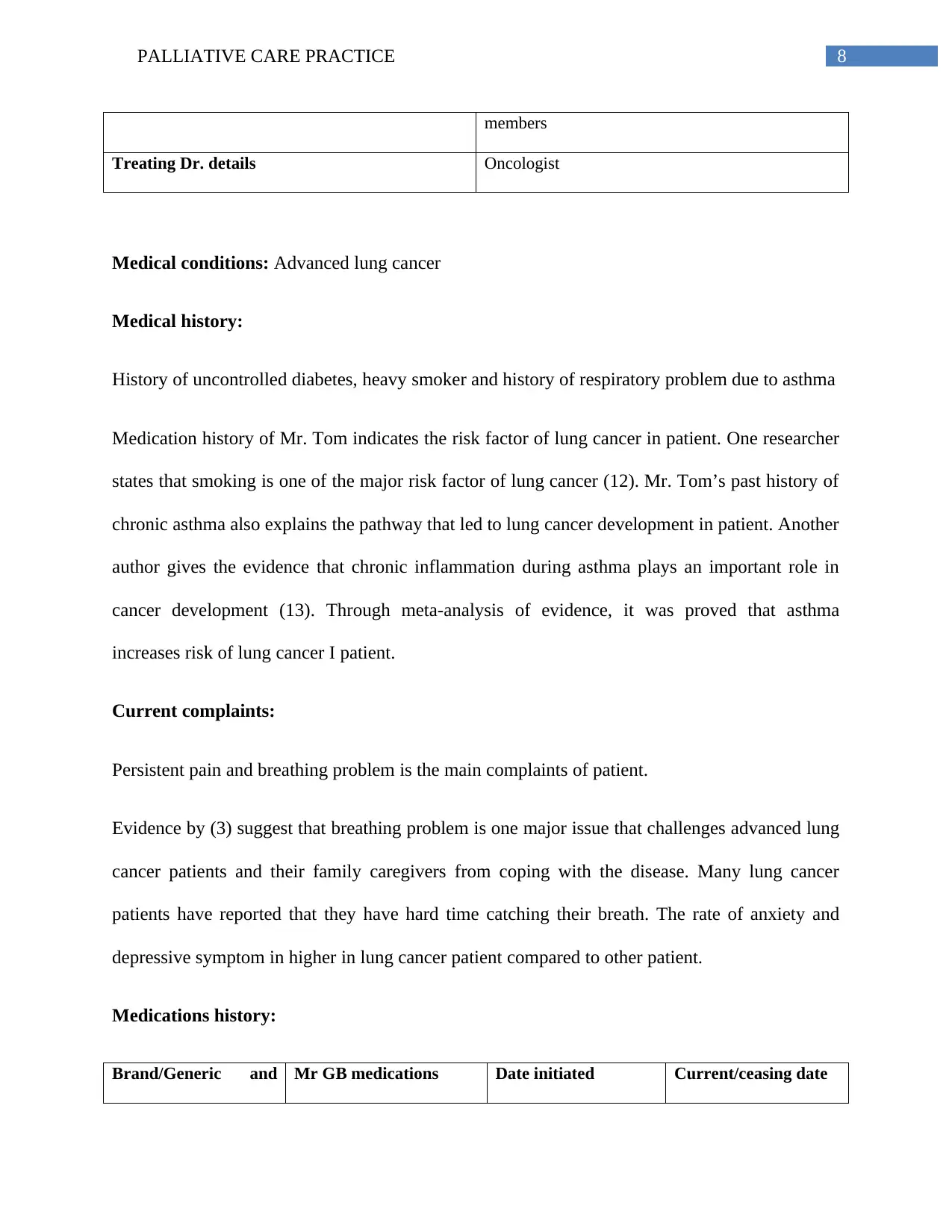
Medications history:
Brand/Generic and Mr GB medications Date initiated Current/ceasing date
members
Treating Dr. details Oncologist
Medical conditions: Advanced lung cancer
Medical history:
History of uncontrolled diabetes, heavy smoker and history of respiratory problem due to asthma
Medication history of Mr. Tom indicates the risk factor of lung cancer in patient. One researcher
states that smoking is one of the major risk factor of lung cancer (12). Mr. Tom’s past history of
chronic asthma also explains the pathway that led to lung cancer development in patient. Another
author gives the evidence that chronic inflammation during asthma plays an important role in
cancer development (13). Through meta-analysis of evidence, it was proved that asthma
increases risk of lung cancer I patient.
Current complaints:
Persistent pain and breathing problem is the main complaints of patient.
Evidence by (3) suggest that breathing problem is one major issue that challenges advanced lung
cancer patients and their family caregivers from coping with the disease. Many lung cancer
patients have reported that they have hard time catching their breath. The rate of anxiety and
depressive symptom in higher in lung cancer patient compared to other patient.
Medications history:
Brand/Generic and Mr GB medications Date initiated Current/ceasing date
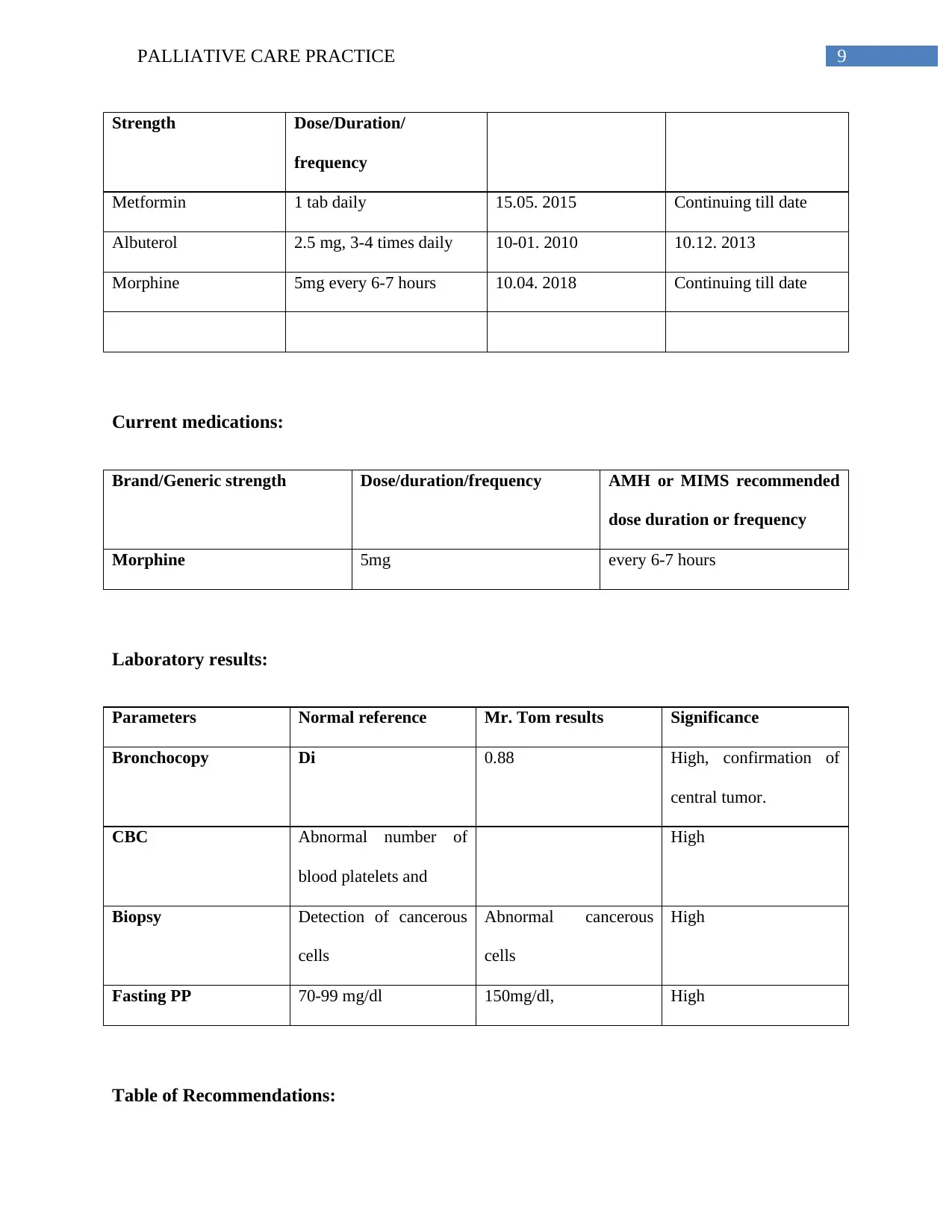
9PALLIATIVE CARE PRACTICE
Strength Dose/Duration/
frequency
Metformin 1 tab daily 15.05. 2015 Continuing till date
Albuterol 2.5 mg, 3-4 times daily 10-01. 2010 10.12. 2013
Morphine 5mg every 6-7 hours 10.04. 2018 Continuing till date
Current medications:
Brand/Generic strength Dose/duration/frequency AMH or MIMS recommended
dose duration or frequency
Morphine 5mg every 6-7 hours
Laboratory results:
Parameters Normal reference Mr. Tom results Significance
Bronchocopy Di 0.88 High, confirmation of
central tumor.
CBC Abnormal number of
blood platelets and
High
Biopsy Detection of cancerous
cells
Abnormal cancerous
cells
High
Fasting PP 70-99 mg/dl 150mg/dl, High
Table of Recommendations:
Strength Dose/Duration/
frequency
Metformin 1 tab daily 15.05. 2015 Continuing till date
Albuterol 2.5 mg, 3-4 times daily 10-01. 2010 10.12. 2013
Morphine 5mg every 6-7 hours 10.04. 2018 Continuing till date
Current medications:
Brand/Generic strength Dose/duration/frequency AMH or MIMS recommended
dose duration or frequency
Morphine 5mg every 6-7 hours
Laboratory results:
Parameters Normal reference Mr. Tom results Significance
Bronchocopy Di 0.88 High, confirmation of
central tumor.
CBC Abnormal number of
blood platelets and
High
Biopsy Detection of cancerous
cells
Abnormal cancerous
cells
High
Fasting PP 70-99 mg/dl 150mg/dl, High
Table of Recommendations:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
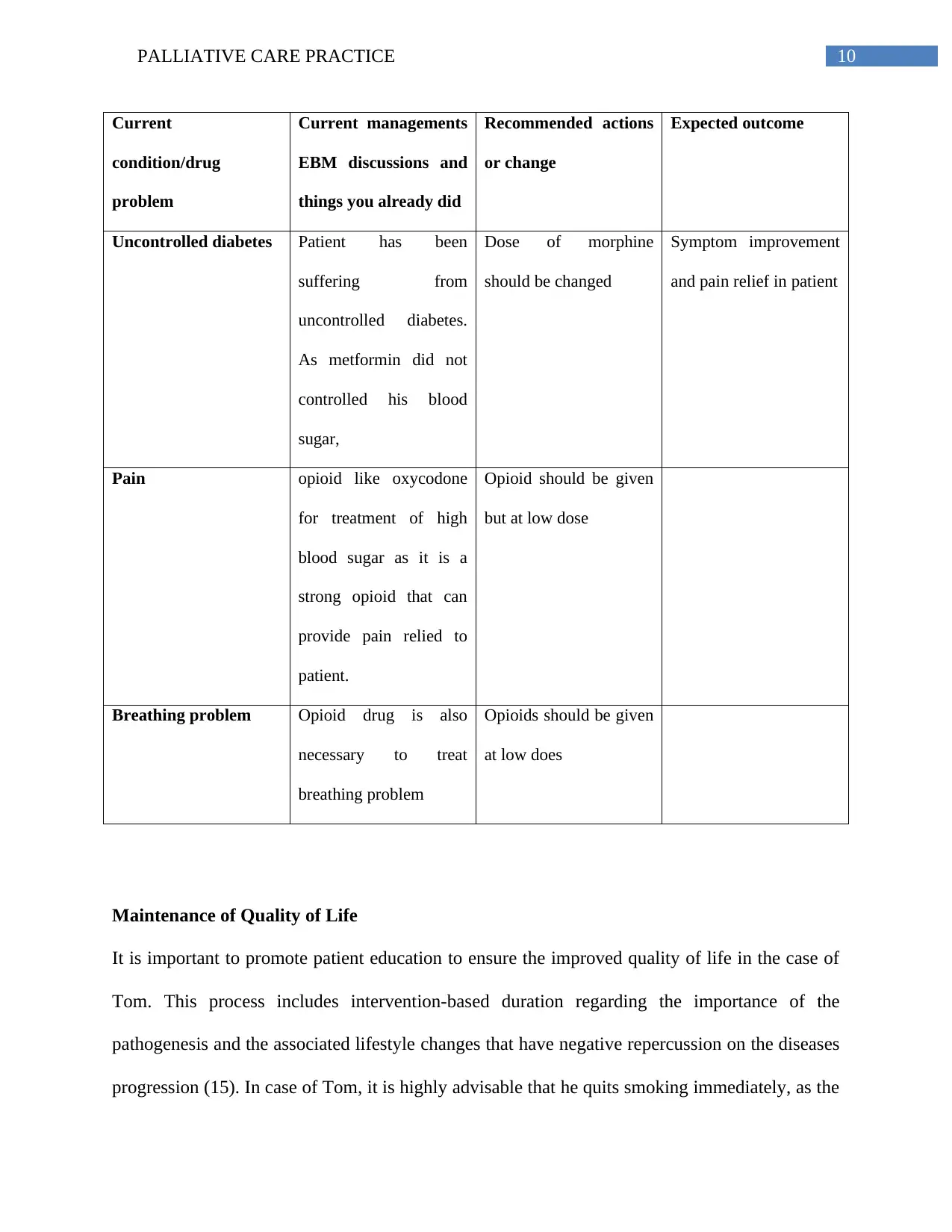
10PALLIATIVE CARE PRACTICE
Current
condition/drug
problem
Current managements
EBM discussions and
things you already did
Recommended actions
or change
Expected outcome
Uncontrolled diabetes Patient has been
suffering from
uncontrolled diabetes.
As metformin did not
controlled his blood
sugar,
Dose of morphine
should be changed
Symptom improvement
and pain relief in patient
Pain opioid like oxycodone
for treatment of high
blood sugar as it is a
strong opioid that can
provide pain relied to
patient.
Opioid should be given
but at low dose
Breathing problem Opioid drug is also
necessary to treat
breathing problem
Opioids should be given
at low does
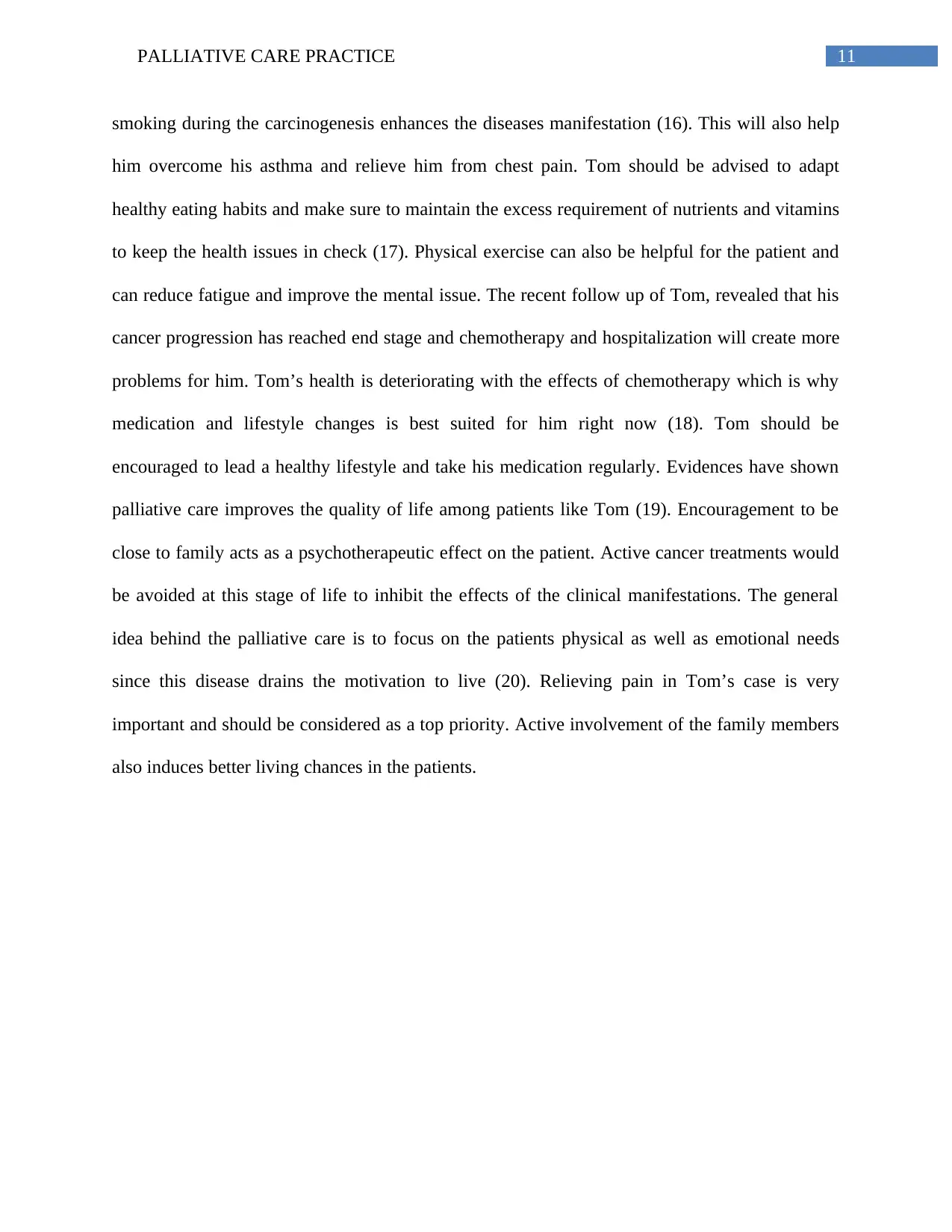
Maintenance of Quality of Life
It is important to promote patient education to ensure the improved quality of life in the case of
Tom. This process includes intervention-based duration regarding the importance of the
pathogenesis and the associated lifestyle changes that have negative repercussion on the diseases
progression (15). In case of Tom, it is highly advisable that he quits smoking immediately, as the
Current
condition/drug
problem
Current managements
EBM discussions and
things you already did
Recommended actions
or change
Expected outcome
Uncontrolled diabetes Patient has been
suffering from
uncontrolled diabetes.
As metformin did not
controlled his blood
sugar,
Dose of morphine
should be changed
Symptom improvement
and pain relief in patient
Pain opioid like oxycodone
for treatment of high
blood sugar as it is a
strong opioid that can
provide pain relied to
patient.
Opioid should be given
but at low dose
Breathing problem Opioid drug is also
necessary to treat
breathing problem
Opioids should be given
at low does
Maintenance of Quality of Life
It is important to promote patient education to ensure the improved quality of life in the case of
Tom. This process includes intervention-based duration regarding the importance of the
pathogenesis and the associated lifestyle changes that have negative repercussion on the diseases
progression (15). In case of Tom, it is highly advisable that he quits smoking immediately, as the
11PALLIATIVE CARE PRACTICE
smoking during the carcinogenesis enhances the diseases manifestation (16). This will also help
him overcome his asthma and relieve him from chest pain. Tom should be advised to adapt
healthy eating habits and make sure to maintain the excess requirement of nutrients and vitamins
to keep the health issues in check (17). Physical exercise can also be helpful for the patient and
can reduce fatigue and improve the mental issue. The recent follow up of Tom, revealed that his
cancer progression has reached end stage and chemotherapy and hospitalization will create more
problems for him. Tom’s health is deteriorating with the effects of chemotherapy which is why
medication and lifestyle changes is best suited for him right now (18). Tom should be
encouraged to lead a healthy lifestyle and take his medication regularly. Evidences have shown
palliative care improves the quality of life among patients like Tom (19). Encouragement to be
close to family acts as a psychotherapeutic effect on the patient. Active cancer treatments would
be avoided at this stage of life to inhibit the effects of the clinical manifestations. The general
idea behind the palliative care is to focus on the patients physical as well as emotional needs
since this disease drains the motivation to live (20). Relieving pain in Tom’s case is very
important and should be considered as a top priority. Active involvement of the family members
also induces better living chances in the patients.
smoking during the carcinogenesis enhances the diseases manifestation (16). This will also help
him overcome his asthma and relieve him from chest pain. Tom should be advised to adapt
healthy eating habits and make sure to maintain the excess requirement of nutrients and vitamins
to keep the health issues in check (17). Physical exercise can also be helpful for the patient and
can reduce fatigue and improve the mental issue. The recent follow up of Tom, revealed that his
cancer progression has reached end stage and chemotherapy and hospitalization will create more
problems for him. Tom’s health is deteriorating with the effects of chemotherapy which is why
medication and lifestyle changes is best suited for him right now (18). Tom should be
encouraged to lead a healthy lifestyle and take his medication regularly. Evidences have shown
palliative care improves the quality of life among patients like Tom (19). Encouragement to be
close to family acts as a psychotherapeutic effect on the patient. Active cancer treatments would
be avoided at this stage of life to inhibit the effects of the clinical manifestations. The general
idea behind the palliative care is to focus on the patients physical as well as emotional needs
since this disease drains the motivation to live (20). Relieving pain in Tom’s case is very
important and should be considered as a top priority. Active involvement of the family members
also induces better living chances in the patients.
12PALLIATIVE CARE PRACTICE
References:
1. Lindeman NI, Cagle PT, Beasley MB, Chitale DA, Dacic S, Giaccone G, Jenkins RB,
Kwiatkowski DJ, Saldivar JS, Squire J, Thunnissen E. Molecular testing guideline for
selection of lung cancer patients for EGFR and ALK tyrosine kinase inhibitors: guideline
from the College of American Pathologists, International Association for the Study of
Lung Cancer, and Association for Molecular Pathology. Journal of Thoracic Oncology.
2013 Jul 1;8(7):823-59.
2. Cheng S, Hideshima S, Kuroiwa S, Nakanishi T, Osaka T. Label-free detection of tumor
markers using field effect transistor (FET)-based biosensors for lung cancer diagnosis.
Sensors and Actuators B: Chemical. 2015 Jun 1;212:329-34.
3. Gridelli C, Rossi A, Carbone DP, Guarize J, Karachaliou N, Mok T, Petrella F, Spaggiari
L, Rosell R. Non-small-cell lung cancer. Nature Reviews Disease Primers. 2015 May
21;1:15009.
4. Abe M, Okada K, Maruyama T, Maruyama N, Matsumoto K. Efficacy and safety of
mitiglinide in diabetic patients on maintenance hemodialysis. Endocrine journal.
2010;57(7):579-86.
5. Timmerman R, Paulus R, Galvin J, Michalski J, Straube W, Bradley J, Fakiris A, Bezjak
A, Videtic G, Johnstone D, Fowler J. Stereotactic body radiation therapy for inoperable
early stage lung cancer. Jama. 2010 Mar 17;303(11):1070-6.
6. De Backer W, Devolder A, Poli G, Acerbi D, Monno R, Herpich C, Sommerer K, Meyer
T, Mariotti F. Lung deposition of BDP/formoterol HFA pMDI in healthy volunteers,
asthmatic, and COPD patients. Journal of aerosol medicine and pulmonary drug delivery.
2010 Jun 1;23(3):137-48.
References:
1. Lindeman NI, Cagle PT, Beasley MB, Chitale DA, Dacic S, Giaccone G, Jenkins RB,
Kwiatkowski DJ, Saldivar JS, Squire J, Thunnissen E. Molecular testing guideline for
selection of lung cancer patients for EGFR and ALK tyrosine kinase inhibitors: guideline
from the College of American Pathologists, International Association for the Study of
Lung Cancer, and Association for Molecular Pathology. Journal of Thoracic Oncology.
2013 Jul 1;8(7):823-59.
2. Cheng S, Hideshima S, Kuroiwa S, Nakanishi T, Osaka T. Label-free detection of tumor
markers using field effect transistor (FET)-based biosensors for lung cancer diagnosis.
Sensors and Actuators B: Chemical. 2015 Jun 1;212:329-34.
3. Gridelli C, Rossi A, Carbone DP, Guarize J, Karachaliou N, Mok T, Petrella F, Spaggiari
L, Rosell R. Non-small-cell lung cancer. Nature Reviews Disease Primers. 2015 May
21;1:15009.
4. Abe M, Okada K, Maruyama T, Maruyama N, Matsumoto K. Efficacy and safety of
mitiglinide in diabetic patients on maintenance hemodialysis. Endocrine journal.
2010;57(7):579-86.
5. Timmerman R, Paulus R, Galvin J, Michalski J, Straube W, Bradley J, Fakiris A, Bezjak
A, Videtic G, Johnstone D, Fowler J. Stereotactic body radiation therapy for inoperable
early stage lung cancer. Jama. 2010 Mar 17;303(11):1070-6.
6. De Backer W, Devolder A, Poli G, Acerbi D, Monno R, Herpich C, Sommerer K, Meyer
T, Mariotti F. Lung deposition of BDP/formoterol HFA pMDI in healthy volunteers,
asthmatic, and COPD patients. Journal of aerosol medicine and pulmonary drug delivery.
2010 Jun 1;23(3):137-48.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13PALLIATIVE CARE PRACTICE
7. Wilson TR, Fridlyand J, Yan Y, Penuel E, Burton L, Chan E, Peng J, Lin E, Wang Y,
Sosman J, Ribas A. Widespread potential for growth-factor-driven resistance to
anticancer kinase inhibitors. Nature. 2012 Jul;487(7408):505.
8. Minami S, Fujimoto K, Ogata Y, Yamamoto S, Komuta K. Opioids have no negative
effect on the survival time of patients with advanced lung cancer in an acute care
hospital. Supportive Care in Cancer. 2015 Aug 1;23(8):2245-54.
9. Simmons CP, MacLeod N, Laird BJ. Clinical management of pain in advanced lung
cancer. Clinical Medicine Insights: Oncology. 2012 Jan;6:CMO-S8360.
10. Lim RB. End-of-life care in patients with advanced lung cancer. Therapeutic advances in
respiratory disease. 2016 Oct;10(5):455-67.
11. Bausewein C, Simon ST. Shortness of breath and cough in patients in palliative care.
Deutsches Ärzteblatt International. 2013 Aug;110(33-34):563.
12. Pirie K, Peto R, Green J, Reeves GK, Beral V, Million Women Study Collaborators.
Lung cancer in never smokers in the UK Million Women Study. International journal of
cancer. 2016 Jul 15;139(2):347-54.
13. Qu YL, Liu J, Zhang LX, Wu CM, Chu AJ, Wen BL, Ma C, Yan XY, Zhang X, Wang
DM, Lv X. Asthma and the risk of lung cancer: a meta-analysis. Oncotarget. 2017 Feb
14;8(7):11614.
14. Mosher CE, Ott MA, Hanna N, Jalal SI, Champion VL. Coping with physical and
psychological symptoms: a qualitative study of advanced lung cancer patients and their
family caregivers. Supportive Care in Cancer. 2015 Jul 1;23(7):2053-60
7. Wilson TR, Fridlyand J, Yan Y, Penuel E, Burton L, Chan E, Peng J, Lin E, Wang Y,
Sosman J, Ribas A. Widespread potential for growth-factor-driven resistance to
anticancer kinase inhibitors. Nature. 2012 Jul;487(7408):505.
8. Minami S, Fujimoto K, Ogata Y, Yamamoto S, Komuta K. Opioids have no negative
effect on the survival time of patients with advanced lung cancer in an acute care
hospital. Supportive Care in Cancer. 2015 Aug 1;23(8):2245-54.
9. Simmons CP, MacLeod N, Laird BJ. Clinical management of pain in advanced lung
cancer. Clinical Medicine Insights: Oncology. 2012 Jan;6:CMO-S8360.
10. Lim RB. End-of-life care in patients with advanced lung cancer. Therapeutic advances in
respiratory disease. 2016 Oct;10(5):455-67.
11. Bausewein C, Simon ST. Shortness of breath and cough in patients in palliative care.
Deutsches Ärzteblatt International. 2013 Aug;110(33-34):563.
12. Pirie K, Peto R, Green J, Reeves GK, Beral V, Million Women Study Collaborators.
Lung cancer in never smokers in the UK Million Women Study. International journal of
cancer. 2016 Jul 15;139(2):347-54.
13. Qu YL, Liu J, Zhang LX, Wu CM, Chu AJ, Wen BL, Ma C, Yan XY, Zhang X, Wang
DM, Lv X. Asthma and the risk of lung cancer: a meta-analysis. Oncotarget. 2017 Feb
14;8(7):11614.
14. Mosher CE, Ott MA, Hanna N, Jalal SI, Champion VL. Coping with physical and
psychological symptoms: a qualitative study of advanced lung cancer patients and their
family caregivers. Supportive Care in Cancer. 2015 Jul 1;23(7):2053-60
14PALLIATIVE CARE PRACTICE
15. Hui D, Kim SH, Roquemore J, Dev R, Chisholm G, Bruera E. Impact of timing and
setting of palliative care referral on quality of end‐of‐life care in cancer patients. Cancer.
2014 Jun 1;120(11):1743-9.
16. Moyer VA. Screening for lung cancer: US Preventive Services Task Force
recommendation statement. Annals of internal medicine. 2014 Mar 4;160(5):330-8.
17. Bazzan AJ, Newberg AB, Cho WC, Monti DA. Diet and nutrition in cancer survivorship
and palliative care. Evidence-based Complementary and Alternative Medicine.
2013;2013.
18. Prigerson HG, Bao Y, Shah MA, Paulk ME, LeBlanc TW, Schneider BJ, Garrido MM,
Reid MC, Berlin DA, Adelson KB, Neugut AI. Chemotherapy use, performance status,
and quality of life at the end of life. JAMA oncology. 2015 Sep 1;1(6):778-84.
19. Wiener L, Weaver MS, Bell CJ, Sansom-Daly UM. Threading the cloak: palliative care
education for care providers of adolescents and young adults with cancer. Clinical
oncology in adolescents and young adults. 2015 Jan 1;5:1.
20. Quill TE, Abernethy AP. Generalist plus specialist palliative care—creating a more
sustainable model. New England Journal of Medicine. 2013 Mar 28;368(13):1173-5.
15. Hui D, Kim SH, Roquemore J, Dev R, Chisholm G, Bruera E. Impact of timing and
setting of palliative care referral on quality of end‐of‐life care in cancer patients. Cancer.
2014 Jun 1;120(11):1743-9.
16. Moyer VA. Screening for lung cancer: US Preventive Services Task Force
recommendation statement. Annals of internal medicine. 2014 Mar 4;160(5):330-8.
17. Bazzan AJ, Newberg AB, Cho WC, Monti DA. Diet and nutrition in cancer survivorship
and palliative care. Evidence-based Complementary and Alternative Medicine.
2013;2013.
18. Prigerson HG, Bao Y, Shah MA, Paulk ME, LeBlanc TW, Schneider BJ, Garrido MM,
Reid MC, Berlin DA, Adelson KB, Neugut AI. Chemotherapy use, performance status,
and quality of life at the end of life. JAMA oncology. 2015 Sep 1;1(6):778-84.
19. Wiener L, Weaver MS, Bell CJ, Sansom-Daly UM. Threading the cloak: palliative care
education for care providers of adolescents and young adults with cancer. Clinical
oncology in adolescents and young adults. 2015 Jan 1;5:1.
20. Quill TE, Abernethy AP. Generalist plus specialist palliative care—creating a more
sustainable model. New England Journal of Medicine. 2013 Mar 28;368(13):1173-5.
1 out of 15
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





