Paramedic Case Study: Assessment, Management, and Communication
VerifiedAdded on 2020/10/22
|14
|3234
|361
Case Study
AI Summary
This paramedic case study presents two scenarios: a 26-year-old female experiencing postpartum hemorrhage and an 18-year-old female in imminent delivery. The first case focuses on assessing the patient's condition, including vital signs and blood loss, and implementing the QAS clinical practi...
Paramedic Case study 1 – 800 Words
Case: 26 Year Old Female – Delivered and ?Blood loss++
Dispatch:
You are working as an ACPII crew at a Coolangatta Station
You receive a Code 1C case on the pager
Case details are: 26 YO F patient - baby delivered and ?blood loss
You are 15 minutes from scene
You are 20 minutes from nearest obstetric hospital
1. En route you received an update. Baby is appears to be doing well but Husband states
there is a lot of blood. What information would you like to know? What other history
do you need??
1. How far apart are contractions.
2. How long since the mother is bleeding.
3. Is the mother conscious.
4. Antenatal history
5. Blood group
6. Is there too much bleeding.
7. Did mother hit something or fallen down.
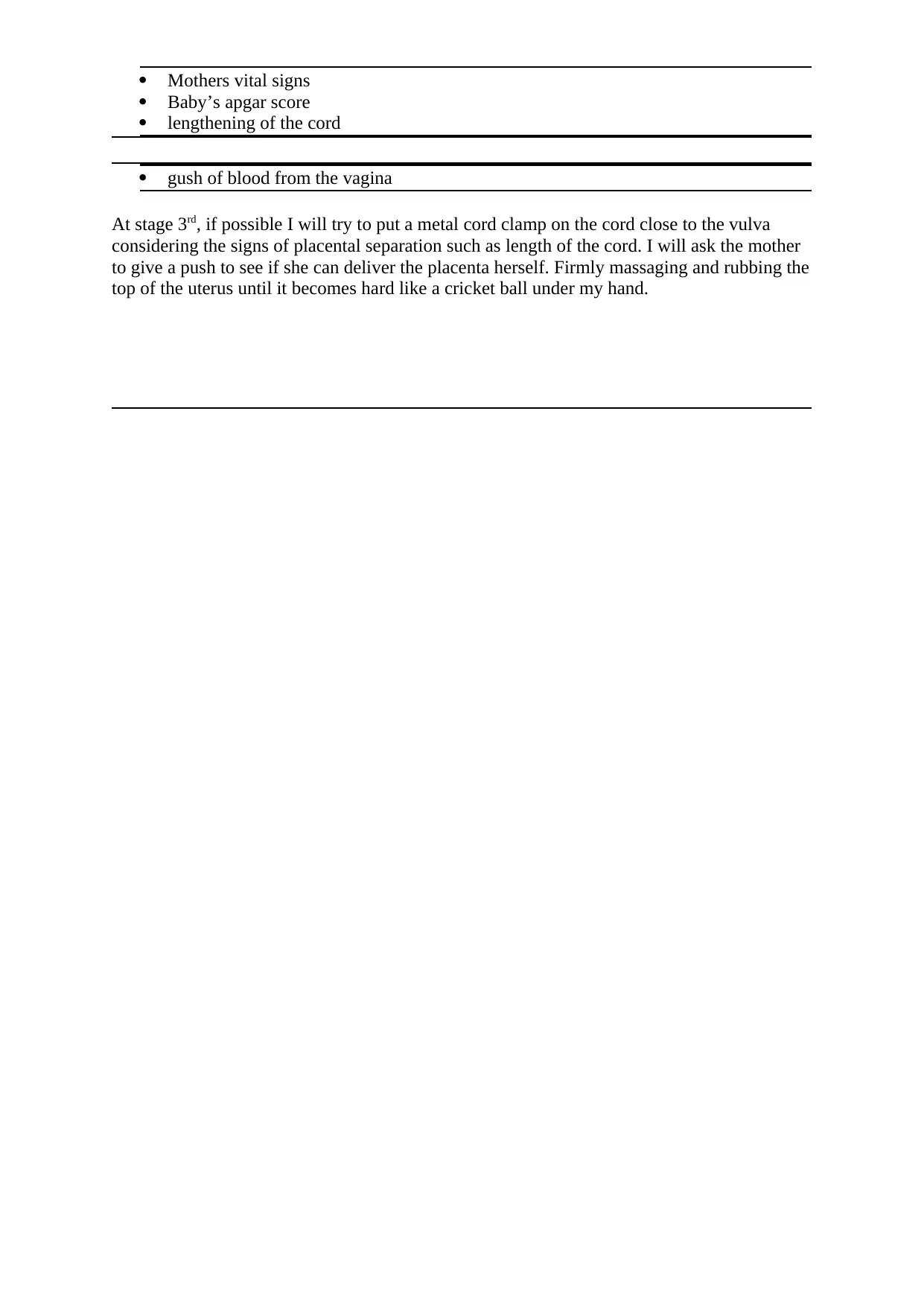
You approach the house you can see through the flywire door and there is blood on the
floorboards. The husband rushes to the door and escorts you to the baby and mother who are
positioned on the bed. Stage 3 of labour has occurred and baby is on the father’s chest and
they are wrapped in towels.
2. How are you going to manage this scene?
Firstly it is essential to ensure that the baby is breathing well, it is also important to ensure
that placenta is out from mother's body. I will try to dry off the new born by directly placing
baby on chest. Running fingers across along the side of baby's nose will help to take away
mucus (Singh and Kaur, 2017). The next I will check the condition of mother and the amount
of blood loss, with the help of my co worker I will take the mother in Ambulance on
stretcher. It is very important to provide blood transfusion to maintain the level of blood
within the mother's body. Careful assessment of the mother will be undertaken including -
Full set of vital signs
Has there been any tearing of the perineum
Appearance of the baby including heart rate, temperature and respiratory rate.
Case: 26 Year Old Female – Delivered and ?Blood loss++
Dispatch:
You are working as an ACPII crew at a Coolangatta Station
You receive a Code 1C case on the pager
Case details are: 26 YO F patient - baby delivered and ?blood loss
You are 15 minutes from scene
You are 20 minutes from nearest obstetric hospital
1. En route you received an update. Baby is appears to be doing well but Husband states
there is a lot of blood. What information would you like to know? What other history
do you need??
1. How far apart are contractions.
2. How long since the mother is bleeding.
3. Is the mother conscious.
4. Antenatal history
5. Blood group
6. Is there too much bleeding.
7. Did mother hit something or fallen down.
You approach the house you can see through the flywire door and there is blood on the
floorboards. The husband rushes to the door and escorts you to the baby and mother who are
positioned on the bed. Stage 3 of labour has occurred and baby is on the father’s chest and
they are wrapped in towels.
2. How are you going to manage this scene?
Firstly it is essential to ensure that the baby is breathing well, it is also important to ensure
that placenta is out from mother's body. I will try to dry off the new born by directly placing
baby on chest. Running fingers across along the side of baby's nose will help to take away
mucus (Singh and Kaur, 2017). The next I will check the condition of mother and the amount
of blood loss, with the help of my co worker I will take the mother in Ambulance on
stretcher. It is very important to provide blood transfusion to maintain the level of blood
within the mother's body. Careful assessment of the mother will be undertaken including -
Full set of vital signs
Has there been any tearing of the perineum
Appearance of the baby including heart rate, temperature and respiratory rate.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Mothers vital signs
Baby’s apgar score
lengthening of the cord
gush of blood from the vagina
At stage 3rd, if possible I will try to put a metal cord clamp on the cord close to the vulva
considering the signs of placental separation such as length of the cord. I will ask the mother
to give a push to see if she can deliver the placenta herself. Firmly massaging and rubbing the
top of the uterus until it becomes hard like a cricket ball under my hand.
Baby’s apgar score
lengthening of the cord
gush of blood from the vagina
At stage 3rd, if possible I will try to put a metal cord clamp on the cord close to the vulva
considering the signs of placental separation such as length of the cord. I will ask the mother
to give a push to see if she can deliver the placenta herself. Firmly massaging and rubbing the
top of the uterus until it becomes hard like a cricket ball under my hand.
Your primary assessment is as follows:
D – Nil
R – Alert to voice
A – Patent
B – Good TV
C – Present, weak thready and fast.
H – Blood on floorboards from bathroom to bed, blood soaked towels x 4, and 1m
diameter blood stain on bed under mother.
E – Cold (winter) - 20 minutes from nearest obstetric hospital
Your secondary assessment reveals:
GCS – E = voice, V = orientated, M = obeys =
HR – 120 weak
BP 80/50
RR – 28
Sp02 – 92% RA
BGL – 5.2 mmol/L
Temp – 35
Auscultation: AE - R=L
Patient Centred Interview
Allergies: NKA
Medications: NIL
Past Medical Hx:
• 38/40
• G2P0
• Excellent antenatal history
• Usually fit and well
Last Meal: Breakfast
Events leading up: Started cramping last night about 3am. Progressed to this…Contractions
every three minutes.
D – Nil
R – Alert to voice
A – Patent
B – Good TV
C – Present, weak thready and fast.
H – Blood on floorboards from bathroom to bed, blood soaked towels x 4, and 1m
diameter blood stain on bed under mother.
E – Cold (winter) - 20 minutes from nearest obstetric hospital
Your secondary assessment reveals:
GCS – E = voice, V = orientated, M = obeys =
HR – 120 weak
BP 80/50
RR – 28
Sp02 – 92% RA
BGL – 5.2 mmol/L
Temp – 35
Auscultation: AE - R=L
Patient Centred Interview
Allergies: NKA
Medications: NIL
Past Medical Hx:
• 38/40
• G2P0
• Excellent antenatal history
• Usually fit and well
Last Meal: Breakfast
Events leading up: Started cramping last night about 3am. Progressed to this…Contractions
every three minutes.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3. Normally after the birth the placenta detaches from the uterine wall with the
assistance of uterine contractions and hormones. Using the timeline below describe
what is happening at each stage.
Birth
Once the baby is delivered, the umbilical cord will be cut and clamped by the doctor
or midwife. The stump shrinks in a few days to develop the belly button (Diriba and
et.al., 2017).
The doctor or midwife gives a drug called oxytocin through an injection in mother's
thigh just as the head of the baby is crowning in order to help the uterus to contract
down to speed up the delivery of the placenta. Active management of third stage is
faster around 5 to 10 minutes and has shown to reduce blood loss after delivery.
5 minutes
Medication that helps in relaxing the patient's uterus to make it contract can also be
utilised to assist expel of the placenta from the womb if the doctor can not succeed
manually.
10 minutes
The mother feels an urge to push and she pushes the placenta out or more commonly
it slides out is the patient moves to a more upright position. The contractions may be
painful but the placenta can be managed with the use of drugs (Hirani and et.al.,
2017).
15 minutes
Due to various reasons such as lack in contraction of the uterus, any tissue injury can
be a barrier in the delivery of placenta that can cause continuous bleeding.
Patient Concern 1
Haemorrhage
4. It is clear that this is a Primary PPH? What differentiates this from a secondary?
It was a primary Postpartum Hemorrhage, PPH is vaginal blood loss in excess of 500 ml
following the childbirth. Primary as referred to the blood loss that occurs in the first 24 hours
following delivery on the other hand secondary post-partum haemorrhage is defined as
excessive vaginal bleeding between 24 hours and six weeks following childbirth. The cause
of bleeding observed in this case was uterine atony that refers to the failure of uterus to
assistance of uterine contractions and hormones. Using the timeline below describe
what is happening at each stage.
Birth
Once the baby is delivered, the umbilical cord will be cut and clamped by the doctor
or midwife. The stump shrinks in a few days to develop the belly button (Diriba and
et.al., 2017).
The doctor or midwife gives a drug called oxytocin through an injection in mother's
thigh just as the head of the baby is crowning in order to help the uterus to contract
down to speed up the delivery of the placenta. Active management of third stage is
faster around 5 to 10 minutes and has shown to reduce blood loss after delivery.
5 minutes
Medication that helps in relaxing the patient's uterus to make it contract can also be
utilised to assist expel of the placenta from the womb if the doctor can not succeed
manually.
10 minutes
The mother feels an urge to push and she pushes the placenta out or more commonly
it slides out is the patient moves to a more upright position. The contractions may be
painful but the placenta can be managed with the use of drugs (Hirani and et.al.,
2017).
15 minutes
Due to various reasons such as lack in contraction of the uterus, any tissue injury can
be a barrier in the delivery of placenta that can cause continuous bleeding.
Patient Concern 1
Haemorrhage
4. It is clear that this is a Primary PPH? What differentiates this from a secondary?
It was a primary Postpartum Hemorrhage, PPH is vaginal blood loss in excess of 500 ml
following the childbirth. Primary as referred to the blood loss that occurs in the first 24 hours
following delivery on the other hand secondary post-partum haemorrhage is defined as
excessive vaginal bleeding between 24 hours and six weeks following childbirth. The cause
of bleeding observed in this case was uterine atony that refers to the failure of uterus to
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
contract down following delivery of the placenta. Therefore, it was clear that it was a primary
post-partum haemorrhage.
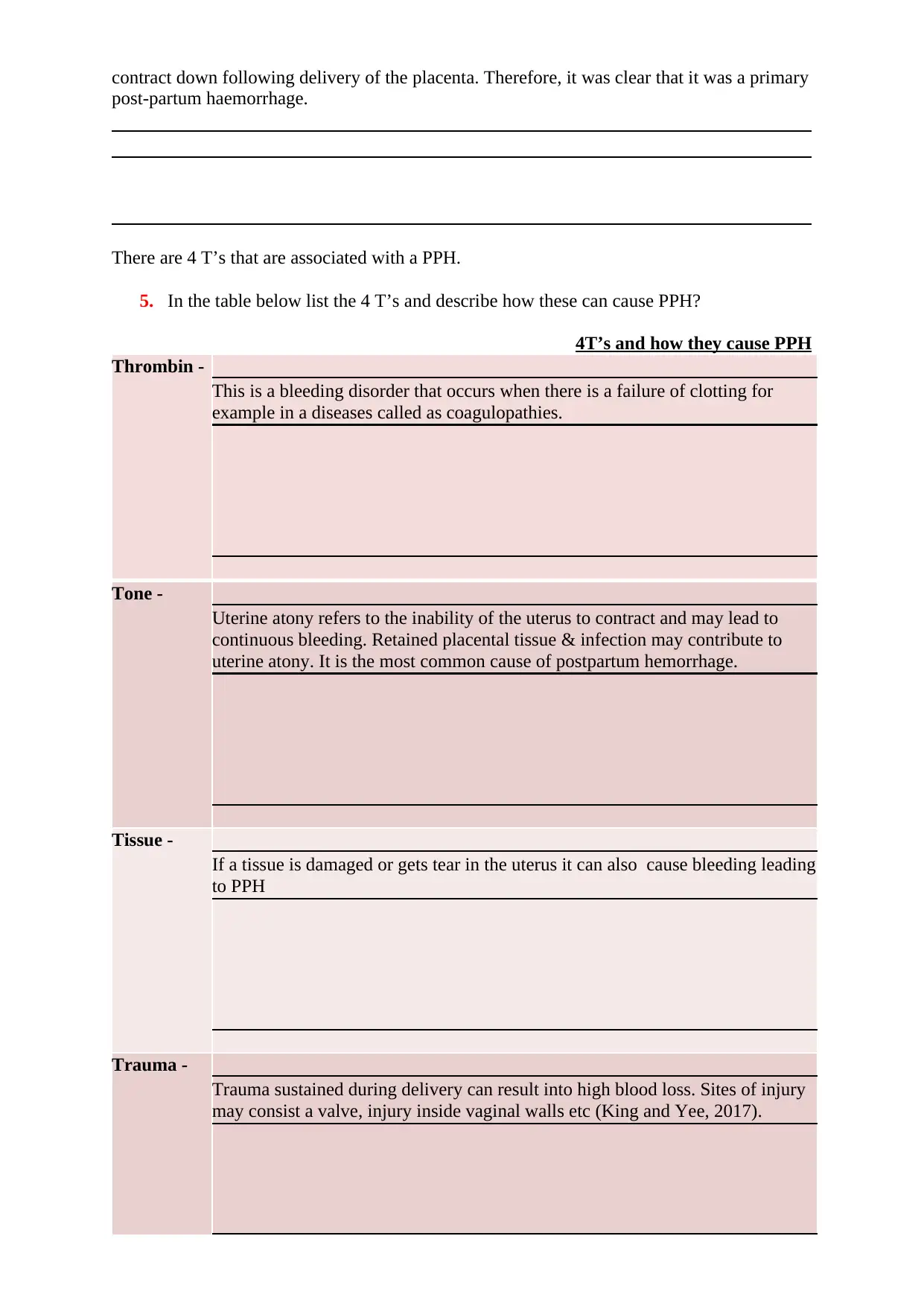
There are 4 T’s that are associated with a PPH.
5. In the table below list the 4 T’s and describe how these can cause PPH?
4T’s and how they cause PPH
Thrombin -
This is a bleeding disorder that occurs when there is a failure of clotting for
example in a diseases called as coagulopathies.
Tone -
Uterine atony refers to the inability of the uterus to contract and may lead to
continuous bleeding. Retained placental tissue & infection may contribute to
uterine atony. It is the most common cause of postpartum hemorrhage.
Tissue -
If a tissue is damaged or gets tear in the uterus it can also cause bleeding leading
to PPH
Trauma -
Trauma sustained during delivery can result into high blood loss. Sites of injury
may consist a valve, injury inside vaginal walls etc (King and Yee, 2017).
post-partum haemorrhage.
There are 4 T’s that are associated with a PPH.
5. In the table below list the 4 T’s and describe how these can cause PPH?
4T’s and how they cause PPH
Thrombin -
This is a bleeding disorder that occurs when there is a failure of clotting for
example in a diseases called as coagulopathies.
Tone -
Uterine atony refers to the inability of the uterus to contract and may lead to
continuous bleeding. Retained placental tissue & infection may contribute to
uterine atony. It is the most common cause of postpartum hemorrhage.
Tissue -
If a tissue is damaged or gets tear in the uterus it can also cause bleeding leading
to PPH
Trauma -
Trauma sustained during delivery can result into high blood loss. Sites of injury
may consist a valve, injury inside vaginal walls etc (King and Yee, 2017).

⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6. What is your management regime as per QAS Clinical Practice Manual?
Management of third stage -
1. Prophylactic use of oxytocics drugs -
Oxytocin – It is a pituitary extract which causes contraction of smooth muscle and
hence a strong impact on uterine muscle. It acts within 2.5 minutes when provided
intramuscularly but its action is not sustained. The benefit is that it has quick action
and does not cause any side effects.
Ergometrine – It is a combination of ergot which can be given intravenously or
intramuscularly. It takes around 6 to 7 minutes to take effect when provided
intramuscularly and 45 seconds when given intravenously. It causes market spasm of
the uterus by a series of rapid contractions. It has an effect lasting for 2 to 4 hours
2. Active management of the third stage -
Injection of oxytocin 10 units IM after the delivery
Placing the left hand on the mother's abdomen at the fundus to make sure that the
uterus is contracted properly(Alam and et.al., 2018).
Setting an intravenous line due to blood loss more than 500 ml
3. Monitoring blood pressure, colour, temperature of the body and pulse
4. Checking that the uterus is well contracted at regular intervals
5. Checking the pad to examine excessive bleeding
6. Continuous oxytocin drip
7. How are you going to load this patient? What manual handling equipment will you
use?
Management of third stage -
1. Prophylactic use of oxytocics drugs -
Oxytocin – It is a pituitary extract which causes contraction of smooth muscle and
hence a strong impact on uterine muscle. It acts within 2.5 minutes when provided
intramuscularly but its action is not sustained. The benefit is that it has quick action
and does not cause any side effects.
Ergometrine – It is a combination of ergot which can be given intravenously or
intramuscularly. It takes around 6 to 7 minutes to take effect when provided
intramuscularly and 45 seconds when given intravenously. It causes market spasm of
the uterus by a series of rapid contractions. It has an effect lasting for 2 to 4 hours
2. Active management of the third stage -
Injection of oxytocin 10 units IM after the delivery
Placing the left hand on the mother's abdomen at the fundus to make sure that the
uterus is contracted properly(Alam and et.al., 2018).
Setting an intravenous line due to blood loss more than 500 ml
3. Monitoring blood pressure, colour, temperature of the body and pulse
4. Checking that the uterus is well contracted at regular intervals
5. Checking the pad to examine excessive bleeding
6. Continuous oxytocin drip
7. How are you going to load this patient? What manual handling equipment will you
use?
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1. Developing a plan with other responders and will work as a team
2. Using proper mechanics for lifting and moving patient safely
3. Ensuring safety hook is engaged properly
4. Lifting carriage
5. The stretcher will be positioned
6. Locking pin will be engaged
7. Ensuring safety of the patient and self
8. Properly securing patient in the ambulance then placing patient in the proper position.
The father is clearly distress.
8. Write down three key points that you would like to communicate with the father?
1. The hospital is near there is no need to worry.
2. You can call other family members if any to reach to the hospital
3. Be patient and control yourself.
9. If the patient deteriorates, what is your management regime as per QAS Clinical
Practice Manual?
2. Using proper mechanics for lifting and moving patient safely
3. Ensuring safety hook is engaged properly
4. Lifting carriage
5. The stretcher will be positioned
6. Locking pin will be engaged
7. Ensuring safety of the patient and self
8. Properly securing patient in the ambulance then placing patient in the proper position.
The father is clearly distress.
8. Write down three key points that you would like to communicate with the father?
1. The hospital is near there is no need to worry.
2. You can call other family members if any to reach to the hospital
3. Be patient and control yourself.
9. If the patient deteriorates, what is your management regime as per QAS Clinical
Practice Manual?
increasing the frequency of observations
possible nursing or midwifery and medical interventions at ward level
review by the attending medical officer or team
obtaining emergency assistance or advice
transferring the patient to a higher level of care (Deepanjali and Subedi, 2018).
10. What is your hospital destination of choice? Justify.
The hospital destination is the nearest obstetric hospital, the reason for this choice it the
continuous and heavy blood loss, the placenta is important to be removed within 30 minutes
or it can lead to patient's death.
Case: 18 Year Old Pregnant Female – Imminent Delivery
(NEONATE FOCUS)
Dispatch:
You are working as an ACPII crew at a Robina Station
Its 0830 hours and you’ve had your coffee.
You receive a Code 1C case on the pager
Case details are: 18 YO F patient imminent delivery
You are 5 minutes from scene
You are 10 minutes from nearest obstetric hospital
11. En route consider the pertinent information that will like to gather in your patient
centred interview. What information would you like to know? What other history do
you need??
Antenatal history
Age of the patient
Is there any bleeding
Pregnancy week
Time since the mother reached into third stage of labour
possible nursing or midwifery and medical interventions at ward level
review by the attending medical officer or team
obtaining emergency assistance or advice
transferring the patient to a higher level of care (Deepanjali and Subedi, 2018).
10. What is your hospital destination of choice? Justify.
The hospital destination is the nearest obstetric hospital, the reason for this choice it the
continuous and heavy blood loss, the placenta is important to be removed within 30 minutes
or it can lead to patient's death.
Case: 18 Year Old Pregnant Female – Imminent Delivery
(NEONATE FOCUS)
Dispatch:
You are working as an ACPII crew at a Robina Station
Its 0830 hours and you’ve had your coffee.
You receive a Code 1C case on the pager
Case details are: 18 YO F patient imminent delivery
You are 5 minutes from scene
You are 10 minutes from nearest obstetric hospital
11. En route consider the pertinent information that will like to gather in your patient
centred interview. What information would you like to know? What other history do
you need??
Antenatal history
Age of the patient
Is there any bleeding
Pregnancy week
Time since the mother reached into third stage of labour
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
You approach the house and you can hear the patient moaning. You enter the house and you
find the patient on the couch. She is obviously distress and is finding it challenging to find a
position of comfort.
12. How are you going to manage this scene?
Firstly, it is important to calm her down and ask her to let us help her so that we can take care
of her effectively.
We appreciate that during cases such as this there is an importance of caring for and
communicating with women in a way that considers and respects their rights to feel, and to
be, culturally and emotionally safe.
13. Write two examples of how you would care and communicate with enable a culturally
and emotionally safe environment for the patient (Lugani and et.al., 2017).
1. I would ask her to do not worry as we are there to take care of her and her baby, I will
also tell her to pray to god and everything will be alright.
2. I will ask her to help her as she is comfortable, and try to make her calm and relax.
Your primary assessment is as follows:
D – Nil
R – Alert
A – Patent
B - Breathing
C – Present
Your secondary assessment reveals:
GCS – 15
HR – 110 regular
BP 110/70
RR – 30
Sp02 – 99% RA
BGL – 4.8mmol/L
Temp – 36.5
ECG: ST 110 bpm
find the patient on the couch. She is obviously distress and is finding it challenging to find a
position of comfort.
12. How are you going to manage this scene?
Firstly, it is important to calm her down and ask her to let us help her so that we can take care
of her effectively.
We appreciate that during cases such as this there is an importance of caring for and
communicating with women in a way that considers and respects their rights to feel, and to
be, culturally and emotionally safe.
13. Write two examples of how you would care and communicate with enable a culturally
and emotionally safe environment for the patient (Lugani and et.al., 2017).
1. I would ask her to do not worry as we are there to take care of her and her baby, I will
also tell her to pray to god and everything will be alright.
2. I will ask her to help her as she is comfortable, and try to make her calm and relax.
Your primary assessment is as follows:
D – Nil
R – Alert
A – Patent
B - Breathing
C – Present
Your secondary assessment reveals:
GCS – 15
HR – 110 regular
BP 110/70
RR – 30
Sp02 – 99% RA
BGL – 4.8mmol/L
Temp – 36.5
ECG: ST 110 bpm
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Auscultation: AE - R=L
Patient Centred Interview
Allergies: NKA
Medications: NIL
Past Medical Hx:
• 38/40
• G2P1
• Excellent antenatal history
• Usually fit and well
Last Meal: Breakfast
Events leading up:
Started cramping last night about 3am. Progressed to this…Contractions every three minutes.
Patient Concern 1
Imminent Delivery
14. The head is crowning. Within four contractions the baby is out. What is your
immediate management of the baby?
Drying the baby with warm clothes or towels while being placed on the mother's abdomen
chest to keep her warm. Evaluating breathing of the baby, using sterile method to cut the
cord and Initiating exclusive breastfeeding in the first hour.
15. What is your management of the mother?
Use of pads in the lochia which is a process where the uterine lining is shed after delivery and
the patient will bleed. Using tampons may cause infection therefore it is essential use pads.
Applying ice packs for pain around the vaginal area to reduce it. I will use warm water to
clean the patient. Proper rest will be provided to the patient.
16. The baby takes it’s first breath approximately 15 seconds after the birth. Explain what
happens to ductus venosus, foramen ovale, ductus arteriosus in this transition?
In some cases the umbilical cord is clamped and the baby no longer receives oxygen and
nutrients from the mother, from the first breath of life the lungs begin to expand, the alveoli
in the lungs are cleared of fluid. An increase in the blood pressure and the reduction in the
pulmonary pressures reduces the requirement for the ductus artesiosus to shunt the blood.
These transition increases the pressure in the left atrium of the heart which leads to reduced
pressure in the right atrium. This shift in pressure stimulates the foramen ovale to close.
Patient Centred Interview
Allergies: NKA
Medications: NIL
Past Medical Hx:
• 38/40
• G2P1
• Excellent antenatal history
• Usually fit and well
Last Meal: Breakfast
Events leading up:
Started cramping last night about 3am. Progressed to this…Contractions every three minutes.
Patient Concern 1
Imminent Delivery
14. The head is crowning. Within four contractions the baby is out. What is your
immediate management of the baby?
Drying the baby with warm clothes or towels while being placed on the mother's abdomen
chest to keep her warm. Evaluating breathing of the baby, using sterile method to cut the
cord and Initiating exclusive breastfeeding in the first hour.
15. What is your management of the mother?
Use of pads in the lochia which is a process where the uterine lining is shed after delivery and
the patient will bleed. Using tampons may cause infection therefore it is essential use pads.
Applying ice packs for pain around the vaginal area to reduce it. I will use warm water to
clean the patient. Proper rest will be provided to the patient.
16. The baby takes it’s first breath approximately 15 seconds after the birth. Explain what
happens to ductus venosus, foramen ovale, ductus arteriosus in this transition?
In some cases the umbilical cord is clamped and the baby no longer receives oxygen and
nutrients from the mother, from the first breath of life the lungs begin to expand, the alveoli
in the lungs are cleared of fluid. An increase in the blood pressure and the reduction in the
pulmonary pressures reduces the requirement for the ductus artesiosus to shunt the blood.
These transition increases the pressure in the left atrium of the heart which leads to reduced
pressure in the right atrium. This shift in pressure stimulates the foramen ovale to close.
17. At one minute you find the baby’s whole body is blue, has a weak cry, arms and legs
are flexed, HR < 100, grimaces. What is the APGAR?
APGAR score is 1
18. At 5 minutes the baby’s extremities are blue, HR > 100, has a good cry and pulls
away and is actively moving. What is the APGAR? And do you continue to record
the APGAR score en route hospital?
The APGAR score is 2 and it can be tested again after 5 minutes and after reaching the
hospital.
19. How do we manage the third stage of labour?
The third stage consist delivery of placenta, this is also known as the shortage stage. The time
it takes for delivering placenta can be 5 to 30 minutes. After the delivery of the baby,small
contraction will begin, the contractions signal that the placenta is getting separated from the
uterine wall and it ready to be delivered. Pressure can be provided by massage to the patient's
uterus and the umbilical cord may be gently pulled. The result will be the placenta delivery
also known as the afterbirth. The patient may experience heavy shivering and shaking after
the placenta is delivered. It is a common sigh and not a major cause of concern.
are flexed, HR < 100, grimaces. What is the APGAR?
APGAR score is 1
18. At 5 minutes the baby’s extremities are blue, HR > 100, has a good cry and pulls
away and is actively moving. What is the APGAR? And do you continue to record
the APGAR score en route hospital?
The APGAR score is 2 and it can be tested again after 5 minutes and after reaching the
hospital.
19. How do we manage the third stage of labour?
The third stage consist delivery of placenta, this is also known as the shortage stage. The time
it takes for delivering placenta can be 5 to 30 minutes. After the delivery of the baby,small
contraction will begin, the contractions signal that the placenta is getting separated from the
uterine wall and it ready to be delivered. Pressure can be provided by massage to the patient's
uterus and the umbilical cord may be gently pulled. The result will be the placenta delivery
also known as the afterbirth. The patient may experience heavy shivering and shaking after
the placenta is delivered. It is a common sigh and not a major cause of concern.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
20. How are you going to load this patient? What manual handling equipment will you
use?
Developing a plan with other responders and will work as a team
Using proper mechanics for lifting and moving patient while handling baby's head
safely
Ensuring safety hook is engaged properly
The stretcher will be positioned
Locking pin will be engaged
Ensuring safety of the patient, child and self
Properly securing patient in the ambulance then placing patient in the proper position
21. What is your hospital destination of choice? Justify.
The hospital destination is the nearest obstetric hospital, the reason for this choice is it is
important to control the patient's pain and there can be any emergency which can be
effectively handled at the hospital as soon the patient will be taken to the hospital.
use?
Developing a plan with other responders and will work as a team
Using proper mechanics for lifting and moving patient while handling baby's head
safely
Ensuring safety hook is engaged properly
The stretcher will be positioned
Locking pin will be engaged
Ensuring safety of the patient, child and self
Properly securing patient in the ambulance then placing patient in the proper position
21. What is your hospital destination of choice? Justify.
The hospital destination is the nearest obstetric hospital, the reason for this choice is it is
important to control the patient's pain and there can be any emergency which can be
effectively handled at the hospital as soon the patient will be taken to the hospital.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
REFERENCES
Lugani, Y., Oberoi, S., Rai, S. K., & Sooch, B. S. (2018). NANOMEDICINE: THE
IMMINENT GAUNTLET OF MEDICAL SCIENCE.
Subedi, N., & Deepanjali Sharma, R. D. (2018). COMPARISON OF MISOPROSTOL,
WITH OXYTOCIN IN THIRD STAGE OF LABOUR. Journal of Universal College
of Medical Sciences, 6(01), 17.
Alam, A., Bopardikar, A., Au, S., Barrett, J., Callum, J., Kiss, A., & Choi, S. (2017). Protocol
for a pilot, randomised, double-blinded, placebo-controlled trial of prophylactic use
of tranexamic acid for preventing postpartum haemorrhage (TAPPH-1). BMJ open,
7(10), e018586.
Yee, J., & King, A. (2017). Precipitous Birth. Journal of Education and Teaching in
Emergency Medicine, 2(4).
Hirani, B. A., Mchome, B. L., Mazuguni, N. S., & Mahande, M. J. (2017). The decision
delivery interval in emergency caesarean section and its associated maternal and fetal
outcomes at a referral hospital in northern Tanzania: a cross-sectional study. BMC
pregnancy and childbirth, 17(1), 411.
Diriba, T. D. (2017). Incidence, Maternal and Perinatal Outcome of Premature Rupture of
Fetal Membrane Cases in Jimma University Teaching Hospital, South West Ethiopia.
EC Gynaecology, 5, 163-172.
Kaur, G., & Singh, S. (2017). To study the maternal and perinatal outcome following vaginal
birth after caesarean section after one previous lower segment caesarean section.
International Journal of Reproduction, Contraception, Obstetrics and Gynecology,
4(3), 658-663.
Lugani, Y., Oberoi, S., Rai, S. K., & Sooch, B. S. (2018). NANOMEDICINE: THE
IMMINENT GAUNTLET OF MEDICAL SCIENCE.
Subedi, N., & Deepanjali Sharma, R. D. (2018). COMPARISON OF MISOPROSTOL,
WITH OXYTOCIN IN THIRD STAGE OF LABOUR. Journal of Universal College
of Medical Sciences, 6(01), 17.
Alam, A., Bopardikar, A., Au, S., Barrett, J., Callum, J., Kiss, A., & Choi, S. (2017). Protocol
for a pilot, randomised, double-blinded, placebo-controlled trial of prophylactic use
of tranexamic acid for preventing postpartum haemorrhage (TAPPH-1). BMJ open,
7(10), e018586.
Yee, J., & King, A. (2017). Precipitous Birth. Journal of Education and Teaching in
Emergency Medicine, 2(4).
Hirani, B. A., Mchome, B. L., Mazuguni, N. S., & Mahande, M. J. (2017). The decision
delivery interval in emergency caesarean section and its associated maternal and fetal
outcomes at a referral hospital in northern Tanzania: a cross-sectional study. BMC
pregnancy and childbirth, 17(1), 411.
Diriba, T. D. (2017). Incidence, Maternal and Perinatal Outcome of Premature Rupture of
Fetal Membrane Cases in Jimma University Teaching Hospital, South West Ethiopia.
EC Gynaecology, 5, 163-172.
Kaur, G., & Singh, S. (2017). To study the maternal and perinatal outcome following vaginal
birth after caesarean section after one previous lower segment caesarean section.
International Journal of Reproduction, Contraception, Obstetrics and Gynecology,
4(3), 658-663.
1 out of 14
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.