Frequency Definition & Meaning
VerifiedAdded on 2022/08/13
|30
|7637
|13
AI Summary
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: PARAPHRASING
Paraphrasing
Name of the student
Name of the university
Author’s name
Paraphrasing
Name of the student
Name of the university
Author’s name
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1PARAPHRASING
Question1. Consider the patient's needs or concerns, medication-related problems and
medication management issues. What further information would assist in making your
assessment of this patient? Explain the reasons for obtaining this information. Who/where
would you obtain this information?
A transcript of her document on "medication supply history" of the last six months from her
ordinary pharmacy would be collected before an interview with Mrs. Mitchell to find out
whether she was finishing her writing immediately. I would also ask the physician's clinic for a
"patient health overview" report to know all the medical concerns the patient submitted to the
doctor during various periods, all the diagnoses made, the prescription medications, the
pathology tests demanded and the clinical outcomes. In the questionnaire the following statement
would be useful to evaluate patient adherence, drug comprehension and management:
Seeing how Ms. Mitchell takes the medications and whether she is conscious of the intent
of each medication.
Figure out if drugs are complicated and what does it do when a dosage is missing.
Figure out if she has trouble with medical items such as opening the bottle, opening bags,
choosing or identifying the tablets / capsules.
And if she has any medications that have expired.
Figure out if any adverse event had occurred to her.
Any further drugs are obtained.
Question1. Consider the patient's needs or concerns, medication-related problems and
medication management issues. What further information would assist in making your
assessment of this patient? Explain the reasons for obtaining this information. Who/where
would you obtain this information?
A transcript of her document on "medication supply history" of the last six months from her
ordinary pharmacy would be collected before an interview with Mrs. Mitchell to find out
whether she was finishing her writing immediately. I would also ask the physician's clinic for a
"patient health overview" report to know all the medical concerns the patient submitted to the
doctor during various periods, all the diagnoses made, the prescription medications, the
pathology tests demanded and the clinical outcomes. In the questionnaire the following statement
would be useful to evaluate patient adherence, drug comprehension and management:
Seeing how Ms. Mitchell takes the medications and whether she is conscious of the intent
of each medication.
Figure out if drugs are complicated and what does it do when a dosage is missing.
Figure out if she has trouble with medical items such as opening the bottle, opening bags,
choosing or identifying the tablets / capsules.
And if she has any medications that have expired.
Figure out if any adverse event had occurred to her.
Any further drugs are obtained.
2PARAPHRASING
Hypertension
Ensure if the blood pressure is known to the patient
Figure out how the patient feels -faint or dizzy when she/he gets up from a sitting or lying
posture to detect and reduce the risk of drug-related postural hypotension.
Test whether she is controlling household blood pressure? If so, demonstration of the
technique
The discussion on salt intake is necessary to check that Ms. Mitchell knows about the
moderate restriction of sodium (BP goal with an non-added salt diet complementing her
anti-hypertensive drug therapy)
IHD and Angina
With respect to the experience of patient ischaemic heart disease (IHD), I would like to question
Mrs. Mitchell about how successful recommended treatment is:
How long have you suffered from angina symptoms? How often do the symptoms occur
during the day? (i.e. at night or during the day–were they more severe during the night or
were symptoms normal during the day?)
I would also inquire if the headache occurs after a few hours of Glyceryl Trinitrate
(GTN) spray given, to see if it is the adverse effects of GTN, as Ms. Mitchell said she
was worried regarding the headache.
GTN mist, which has to be used as needed to relieve chest pain, has been prescribed for Mrs.
Mitchell. The frequency of use should be known:
How often have you used the spray now a week?
Hypertension
Ensure if the blood pressure is known to the patient
Figure out how the patient feels -faint or dizzy when she/he gets up from a sitting or lying
posture to detect and reduce the risk of drug-related postural hypotension.
Test whether she is controlling household blood pressure? If so, demonstration of the
technique
The discussion on salt intake is necessary to check that Ms. Mitchell knows about the
moderate restriction of sodium (BP goal with an non-added salt diet complementing her
anti-hypertensive drug therapy)
IHD and Angina
With respect to the experience of patient ischaemic heart disease (IHD), I would like to question
Mrs. Mitchell about how successful recommended treatment is:
How long have you suffered from angina symptoms? How often do the symptoms occur
during the day? (i.e. at night or during the day–were they more severe during the night or
were symptoms normal during the day?)
I would also inquire if the headache occurs after a few hours of Glyceryl Trinitrate
(GTN) spray given, to see if it is the adverse effects of GTN, as Ms. Mitchell said she
was worried regarding the headache.
GTN mist, which has to be used as needed to relieve chest pain, has been prescribed for Mrs.
Mitchell. The frequency of use should be known:
How often have you used the spray now a week?
3PARAPHRASING
If you were using the spray did it alleviate the symptoms? For each segment, how many
sprays were needed?
If your ailments were not alleviated (to see if she knows when she is going to call a chest
pain ambulance that is not relieved by GTN spray), please inform me what you should
do?
What is the expiration date on your spray and do you know when you began this specific
spray? (To test the procedure & spray is adequately primed)
Where are you putting it in the house? (In order to evaluate efficacy and sufficient spray
storage)
Diabetes
Knowledge, understanding, and management of diabetes by Mrs Mitchell (to determine
the self-handling degree and the need of a diabetes educator or nurse for additional
assistance or learning).
Information on exercise and diet (to assess whether Ms. Mitchell understands the
importance for the treatment and prevention of type 2 diabetes of healthy eating and
regular physical activities).
Any symptoms such as weakness, dizziness, hunger, palpitations, blackened vision,
sweating or trembling, and their administration (to check whether Ms. Mitchell ever
experiences and knows how to deal with hypoglycemia).
Self-Glucose Monitoring (SBGM) and the use and interpretation of metering and results
as necessary. SBGM Test if she held the documents.
If Mrs. Mitchell is not doing SBGM at the moment, see how she is encouraged to start it.
If you were using the spray did it alleviate the symptoms? For each segment, how many
sprays were needed?
If your ailments were not alleviated (to see if she knows when she is going to call a chest
pain ambulance that is not relieved by GTN spray), please inform me what you should
do?
What is the expiration date on your spray and do you know when you began this specific
spray? (To test the procedure & spray is adequately primed)
Where are you putting it in the house? (In order to evaluate efficacy and sufficient spray
storage)
Diabetes
Knowledge, understanding, and management of diabetes by Mrs Mitchell (to determine
the self-handling degree and the need of a diabetes educator or nurse for additional
assistance or learning).
Information on exercise and diet (to assess whether Ms. Mitchell understands the
importance for the treatment and prevention of type 2 diabetes of healthy eating and
regular physical activities).
Any symptoms such as weakness, dizziness, hunger, palpitations, blackened vision,
sweating or trembling, and their administration (to check whether Ms. Mitchell ever
experiences and knows how to deal with hypoglycemia).
Self-Glucose Monitoring (SBGM) and the use and interpretation of metering and results
as necessary. SBGM Test if she held the documents.
If Mrs. Mitchell is not doing SBGM at the moment, see how she is encouraged to start it.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4PARAPHRASING
Confirm that Mrs. Mitchell has spoken with her GP or a diabetes educationist about the
SBGM in the past, and what guidance she received, particularly in terms of tracking
frequency.
Show Mrs. Mitchell how to use blood glucose meters if appropriate. (For all people with
type 2 diabetes, self blood glucose control is advised).
Confirm that Ms Mitchell has regular checks on eyes and feet (to see if any signs or
threats of diabetic problems are present)
Restless leg syndrome
Since no solution occurs for RLS, there might be complications, but many different treatment
options are available for RLS. Treatment will be influenced based upon whether the health
and/or quality of life are often impaired by the symptoms. Discussions with Mrs. Mitchell on the
following points would be helpful when focusing on her own advice.
Iron supplements if low iron rates are suggested by blood tests.
Modifications of the diet, including eliminating cigarettes and reducing the ingestion of
caffeine which can contribute to symptoms.
The discussion of behavior involves relaxation, walking, yoga, enjoying a warm or cool
bath, soothing, adding warmer or cooler packets or emotionally exhausting tasks, such as
jigsaw puzzles, crocheting or chatting in an individual. Aerobic exercise during the day
may also be beneficial with symptoms. A discussion of activities
Bed health debates.
For some people fitness can be beneficial.
Confirm that Mrs. Mitchell has spoken with her GP or a diabetes educationist about the
SBGM in the past, and what guidance she received, particularly in terms of tracking
frequency.
Show Mrs. Mitchell how to use blood glucose meters if appropriate. (For all people with
type 2 diabetes, self blood glucose control is advised).
Confirm that Ms Mitchell has regular checks on eyes and feet (to see if any signs or
threats of diabetic problems are present)
Restless leg syndrome
Since no solution occurs for RLS, there might be complications, but many different treatment
options are available for RLS. Treatment will be influenced based upon whether the health
and/or quality of life are often impaired by the symptoms. Discussions with Mrs. Mitchell on the
following points would be helpful when focusing on her own advice.
Iron supplements if low iron rates are suggested by blood tests.
Modifications of the diet, including eliminating cigarettes and reducing the ingestion of
caffeine which can contribute to symptoms.
The discussion of behavior involves relaxation, walking, yoga, enjoying a warm or cool
bath, soothing, adding warmer or cooler packets or emotionally exhausting tasks, such as
jigsaw puzzles, crocheting or chatting in an individual. Aerobic exercise during the day
may also be beneficial with symptoms. A discussion of activities
Bed health debates.
For some people fitness can be beneficial.
5PARAPHRASING
CVA
Patient's knowledge, comprehension, and cholesterol strategic planning.
Any unhealthy cholesterol checks.
Analysis of the impacts of smoking. (Not smoking is particularly important to people
with diabetes as both smoking and diabetes can harm blood vessels, so that the heart will
have to work much harder) Highlight the value of a healthy lifestyle low in saturated
(animal) fats and high in vegetables and fruit.
Debate on physical activity.
Keep healthy weight.
Neuropathic foot pain
Frequency of experienced pain. How often does the agony get? Do you get to see it every
day? At night, morning, or all of the time, or at times? When do you do some of the
activities?
Impact on the day to day living. Does the discomfort impair your health, or your family's
ability to walk, eat, function, drive or care?
External signs. How does the discomfort feel? Is it just a warm feeling? Or is the
discomfort slicing, stinging and jabbing any more? What about tingling or numbness,
prickling pins-and-needles, shooting discomfort or extreme sensitivity to touch?
Kind of discomfort. Where does the suffering lie? Do you only have discomfort in your
knees, hands or the two?
Determine if Mrs. Mitchell is conscious of various control strategies, such as mindfulness and
mediation methods, cognitive behavioral therapy, transcutaneous electrical nerve stimulation,
CVA
Patient's knowledge, comprehension, and cholesterol strategic planning.
Any unhealthy cholesterol checks.
Analysis of the impacts of smoking. (Not smoking is particularly important to people
with diabetes as both smoking and diabetes can harm blood vessels, so that the heart will
have to work much harder) Highlight the value of a healthy lifestyle low in saturated
(animal) fats and high in vegetables and fruit.
Debate on physical activity.
Keep healthy weight.
Neuropathic foot pain
Frequency of experienced pain. How often does the agony get? Do you get to see it every
day? At night, morning, or all of the time, or at times? When do you do some of the
activities?
Impact on the day to day living. Does the discomfort impair your health, or your family's
ability to walk, eat, function, drive or care?
External signs. How does the discomfort feel? Is it just a warm feeling? Or is the
discomfort slicing, stinging and jabbing any more? What about tingling or numbness,
prickling pins-and-needles, shooting discomfort or extreme sensitivity to touch?
Kind of discomfort. Where does the suffering lie? Do you only have discomfort in your
knees, hands or the two?
Determine if Mrs. Mitchell is conscious of various control strategies, such as mindfulness and
mediation methods, cognitive behavioral therapy, transcutaneous electrical nerve stimulation,
6PARAPHRASING
percutaneous electrical nerve stimulation, and various support services regarding neuropathic
pain.
Asthma
Call on Mrs. Mitchell to demonstrate inhaler strategies.
Test whether Mrs. MItchell has used spacer systems now or in the past and knows correct
cleaning methods As smoking status is not stated on HMR referral, address cigarette
smoking. Cigarette smoking has been shown to be the principal cause of COPD. For
smokers the incidence of COPD is dose-related.
Check out the age at smoking launch, cigarette cumulative pack-years and existing
smoking status. We also estimate COPD mortality. Need to assess context over the pack-
year.
Share her feelings on her quit smoking with Mrs. MItchell. If she already stopped
smoking, find out if she was ever tempted to smoke again, or not.
Discover if it has established some clear self-management strategies to help it deal with
its reduction of smoking.
Address the severity of breathing difficulties or shortness of breath and the effect on
quality of life (to determine need for supplementary medication)
GORD
Address the duration and efficacy of pantoprazole treatment as long-term use can induce
a deficit of vitamin B12.
Ask if there is any diet that causes problems in particular (Ms. MItchell should be told
that some foods that precipitate symptoms and may also be helpful in reducing alcohol,
high-fat meals, chocolate and coffee) Address the timing of symptoms regarding food,
percutaneous electrical nerve stimulation, and various support services regarding neuropathic
pain.
Asthma
Call on Mrs. Mitchell to demonstrate inhaler strategies.
Test whether Mrs. MItchell has used spacer systems now or in the past and knows correct
cleaning methods As smoking status is not stated on HMR referral, address cigarette
smoking. Cigarette smoking has been shown to be the principal cause of COPD. For
smokers the incidence of COPD is dose-related.
Check out the age at smoking launch, cigarette cumulative pack-years and existing
smoking status. We also estimate COPD mortality. Need to assess context over the pack-
year.
Share her feelings on her quit smoking with Mrs. MItchell. If she already stopped
smoking, find out if she was ever tempted to smoke again, or not.
Discover if it has established some clear self-management strategies to help it deal with
its reduction of smoking.
Address the severity of breathing difficulties or shortness of breath and the effect on
quality of life (to determine need for supplementary medication)
GORD
Address the duration and efficacy of pantoprazole treatment as long-term use can induce
a deficit of vitamin B12.
Ask if there is any diet that causes problems in particular (Ms. MItchell should be told
that some foods that precipitate symptoms and may also be helpful in reducing alcohol,
high-fat meals, chocolate and coffee) Address the timing of symptoms regarding food,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7PARAPHRASING
bedtime or other activity? (Patients with nocturnal symptoms can benefit from dosing
nightly or twice daily) About antacid therapy
Chronic abdominal pain/motility disorder
Address the symptoms of abdominal discomfort, nausea or vomiting, cramping, constant
air, pain, and rectal fullness with Mrs. Mitchell
Note the duration, number, and timing of regular defecation and any recent changes.
Tell her the amount, purity and colour of last passing feces
Talk type of diet, use of laxatives or enemas and use of medications
Incontinence
The following points should be discussed with Mrs. Mitchell:
Consider the number of periods of incontinence, and the volume of urinary leakage.
Consult with her if the issues escalated, and the duration of the case.
Address the causing causes or incidents (e.g. cough, sneeze, raising, turning, sense of
pressure, sound of running water) Test whether there is a continuous or irregular lack of
urine;
Search for painfulness.
Figure out if she has a history of urinary tract infections (UTIs) Find out if her fecal
incontinence is concomitant.
Headache
Place of the headaches, frequency, worst headache ever, period and character (dull, hard,
throbbing, etc.)?
Triggering conditions (some foods, bright light, heat, fasting or sleep disturbances)?
bedtime or other activity? (Patients with nocturnal symptoms can benefit from dosing
nightly or twice daily) About antacid therapy
Chronic abdominal pain/motility disorder
Address the symptoms of abdominal discomfort, nausea or vomiting, cramping, constant
air, pain, and rectal fullness with Mrs. Mitchell
Note the duration, number, and timing of regular defecation and any recent changes.
Tell her the amount, purity and colour of last passing feces
Talk type of diet, use of laxatives or enemas and use of medications
Incontinence
The following points should be discussed with Mrs. Mitchell:
Consider the number of periods of incontinence, and the volume of urinary leakage.
Consult with her if the issues escalated, and the duration of the case.
Address the causing causes or incidents (e.g. cough, sneeze, raising, turning, sense of
pressure, sound of running water) Test whether there is a continuous or irregular lack of
urine;
Search for painfulness.
Figure out if she has a history of urinary tract infections (UTIs) Find out if her fecal
incontinence is concomitant.
Headache
Place of the headaches, frequency, worst headache ever, period and character (dull, hard,
throbbing, etc.)?
Triggering conditions (some foods, bright light, heat, fasting or sleep disturbances)?
8PARAPHRASING
Factors which aggravate (exertion, leaning, coughing)?
Who soothes them? Use of paracetamol in information and duration of "prn."
How long have you been having headaches?
How often do you get in? Occurring on weekdays or weekends?
Were warning signs such as exhaustion, yawning, sleepiness or euphoria sometimes
accompanied by these headaches?
Are these headaches associated with visual disturbances, pallor, cold hands and feet,
nausea and vomiting, seizures, weakness or unusual sensations of the arm or leg,
unsteady gait, slurred speech, or fever?
Have you had recent head trauma or a fall?
References
Giannaki, C.D., Hadjigeorgiou, G.M., Karatzaferi, C., Maridaki, M.D., Koutedakis, Y., Founta,
P., Tsianas, N., Stefanidis, I. and Sakkas, G.K., 2013. A single-blind randomized controlled trial
to evaluate the effect of 6 months of progressive aerobic exercise training in patients with
uraemic restless legs syndrome. Nephrology Dialysis Transplantation, 28(11), pp.2834-2840.
Factors which aggravate (exertion, leaning, coughing)?
Who soothes them? Use of paracetamol in information and duration of "prn."
How long have you been having headaches?
How often do you get in? Occurring on weekdays or weekends?
Were warning signs such as exhaustion, yawning, sleepiness or euphoria sometimes
accompanied by these headaches?
Are these headaches associated with visual disturbances, pallor, cold hands and feet,
nausea and vomiting, seizures, weakness or unusual sensations of the arm or leg,
unsteady gait, slurred speech, or fever?
Have you had recent head trauma or a fall?
References
Giannaki, C.D., Hadjigeorgiou, G.M., Karatzaferi, C., Maridaki, M.D., Koutedakis, Y., Founta,
P., Tsianas, N., Stefanidis, I. and Sakkas, G.K., 2013. A single-blind randomized controlled trial
to evaluate the effect of 6 months of progressive aerobic exercise training in patients with
uraemic restless legs syndrome. Nephrology Dialysis Transplantation, 28(11), pp.2834-2840.
9PARAPHRASING
Question2. Consider the patient's needs or concerns, medication-related problems and
medication management issues Based on the information provided, identify potential and
actual medication-related and disease-related problems, and patient concerns. Suggest how
these could be addressed and/or monitored.
Potential medication-related problems
Allergy
Ms. Mitchell may be allergic to prescription formoterol and terbutaline pharmaceutical items
belonging to the same family of ventolin (salbutamol) sympathomimetic beta-agonists as
recognized allergens.
Hyperkalemia:
There are few medications prescribed to Mrs. Mitchell which have the potential to cause
hyperkalemia individually or in combinations. Those medications are Irbesartan, Movicol (which
contains potassium chloride) and Amiloride. Hyperkalemia is defined as a serum potassium
concentration greater than approximately 5.0-5.5 mEq/L in adults. Levels higher than 7 mEq/L
can lead to significant hemodynamic and neurologic consequences, whereas levels exceeding 8.5
mEq/L can cause respiratory paralysis or cardiac arrest and can quickly be fatal. Many
individuals with hyperkalemia are asymptomatic. When present, symptoms are nonspecific and
predominantly related to muscular or cardiac function. Thus Mrs. Mitchell should be
recommended to have her blood potassium level tested.
Prednisolone and Aspirin
Ms. Mitchell has not yet taken the recommended 25 mg Prednisolone drug yet sent it to her
house. On the other side, she was taking 25 mg of aspirin taken regularly in the morning. The
Question2. Consider the patient's needs or concerns, medication-related problems and
medication management issues Based on the information provided, identify potential and
actual medication-related and disease-related problems, and patient concerns. Suggest how
these could be addressed and/or monitored.
Potential medication-related problems
Allergy
Ms. Mitchell may be allergic to prescription formoterol and terbutaline pharmaceutical items
belonging to the same family of ventolin (salbutamol) sympathomimetic beta-agonists as
recognized allergens.
Hyperkalemia:
There are few medications prescribed to Mrs. Mitchell which have the potential to cause
hyperkalemia individually or in combinations. Those medications are Irbesartan, Movicol (which
contains potassium chloride) and Amiloride. Hyperkalemia is defined as a serum potassium
concentration greater than approximately 5.0-5.5 mEq/L in adults. Levels higher than 7 mEq/L
can lead to significant hemodynamic and neurologic consequences, whereas levels exceeding 8.5
mEq/L can cause respiratory paralysis or cardiac arrest and can quickly be fatal. Many
individuals with hyperkalemia are asymptomatic. When present, symptoms are nonspecific and
predominantly related to muscular or cardiac function. Thus Mrs. Mitchell should be
recommended to have her blood potassium level tested.
Prednisolone and Aspirin
Ms. Mitchell has not yet taken the recommended 25 mg Prednisolone drug yet sent it to her
house. On the other side, she was taking 25 mg of aspirin taken regularly in the morning. The
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10PARAPHRASING
combined use of glucocorticoids(prednisolone) and salicylates(aspirin) can decrease the
salicylates ' serum levels and results. Glucocorticoids have been proposed to improve the
salicylate synthesis and/or removal.
A study found that combined high-dose glucocorticoid (10mg / day prednisolone) and low-dose
aspirin were associated with a higher incidence of upper gastrointestinal bleed.1 It should be
noted here that Mrs. Mitchell has a history with GORD treatment and still gets reflux at night.
And she should not have it with aspirin and transfer the prescription for RUM (return of expired
medicines) to the pharmacy.
Actual medication-related problems
Dipyridamole/ aspirin:
The recommended dose of dipyridamole is one pill twice daily, typically one in the morning and
one in the evening, ideally with meals whereas the drug was taken once daily by Mrs. Mitchell.
The tablet to be withdrawn from the package just before use; if it is not covered by the wrapping,
aspirin will break down easily.
Paracetamol:
Mrs. Mitchell takes 3 paracetamol-stat pills for severe headache. Mrs. Mitchell sent me this
detail so by reading the report I would validate the dose protocol. If so, I will advise Dr Peters to
recommend 0.5–1 g (two tablets) per 4–6 hours; a total average of 4 g. I will encourage Mrs
Mitchell to find out the causes that cause and aggravate this. I will suggest that she practice
headache hygiene and outlines potential ways to make any lifestyle changes that can have a
significant impact on the occurrence of headaches
combined use of glucocorticoids(prednisolone) and salicylates(aspirin) can decrease the
salicylates ' serum levels and results. Glucocorticoids have been proposed to improve the
salicylate synthesis and/or removal.
A study found that combined high-dose glucocorticoid (10mg / day prednisolone) and low-dose
aspirin were associated with a higher incidence of upper gastrointestinal bleed.1 It should be
noted here that Mrs. Mitchell has a history with GORD treatment and still gets reflux at night.
And she should not have it with aspirin and transfer the prescription for RUM (return of expired
medicines) to the pharmacy.
Actual medication-related problems
Dipyridamole/ aspirin:
The recommended dose of dipyridamole is one pill twice daily, typically one in the morning and
one in the evening, ideally with meals whereas the drug was taken once daily by Mrs. Mitchell.
The tablet to be withdrawn from the package just before use; if it is not covered by the wrapping,
aspirin will break down easily.
Paracetamol:
Mrs. Mitchell takes 3 paracetamol-stat pills for severe headache. Mrs. Mitchell sent me this
detail so by reading the report I would validate the dose protocol. If so, I will advise Dr Peters to
recommend 0.5–1 g (two tablets) per 4–6 hours; a total average of 4 g. I will encourage Mrs
Mitchell to find out the causes that cause and aggravate this. I will suggest that she practice
headache hygiene and outlines potential ways to make any lifestyle changes that can have a
significant impact on the occurrence of headaches
11PARAPHRASING
Hydroxocobalamin:
As per Mrs. Mitchell, she had been prescribed Neo-B12 ( hydroxocobalamin) which she was
supposed to take once every three months. However, she hasn’t had it for 6 months. It is very
important to take Neo-B12 for her, the reasons being
a) She is on Metformin 850mg BD. Metformin does, however, cause vitamin B-12
malabsorption, which may increase the risk of developing vitamin B-12 deficiency--a
clinically important and treatable condition2.
b) Mrs. Mitchell has been suffering from neuropathic foot pain. She has numbness and burning
in feet and currently going up to the knees. Most often, neuropathy is the cause of burning
feet. Nerve fibers, which are damaged, are more likely to become overactive and misfire. The
damaged nerves shoot pain signals to the brain even though there is no wound. A deficiency
of B12 damages the myelin sheath that surrounds and protects nerves. Without this
protection, nerves stop to function properly and conditions such as peripheral neuropathy
occur.
c) She has been taking pantoprazole 40mg two tablets in the morning. Stomach acid is helpful
in the absorption of B-12, so it makes sense that taking pantoprazole that reduces the amount
of stomach acid would decrease vitamin B-12 absorption. Taking proton pump inhibitors
(PPIs) to ease the symptoms of excess stomach acid for more than two years was linked to a
65 percent increase in the risk of vitamin B-12 deficiency.
Pantoprazole:
In the night, Mrs. Mitchell develops reflux again. She was prescribed two tablets of 40 mg
pantoprazole in the morning. I'd prefer that she have one in the morning and once in the evening.
Hydroxocobalamin:
As per Mrs. Mitchell, she had been prescribed Neo-B12 ( hydroxocobalamin) which she was
supposed to take once every three months. However, she hasn’t had it for 6 months. It is very
important to take Neo-B12 for her, the reasons being
a) She is on Metformin 850mg BD. Metformin does, however, cause vitamin B-12
malabsorption, which may increase the risk of developing vitamin B-12 deficiency--a
clinically important and treatable condition2.
b) Mrs. Mitchell has been suffering from neuropathic foot pain. She has numbness and burning
in feet and currently going up to the knees. Most often, neuropathy is the cause of burning
feet. Nerve fibers, which are damaged, are more likely to become overactive and misfire. The
damaged nerves shoot pain signals to the brain even though there is no wound. A deficiency
of B12 damages the myelin sheath that surrounds and protects nerves. Without this
protection, nerves stop to function properly and conditions such as peripheral neuropathy
occur.
c) She has been taking pantoprazole 40mg two tablets in the morning. Stomach acid is helpful
in the absorption of B-12, so it makes sense that taking pantoprazole that reduces the amount
of stomach acid would decrease vitamin B-12 absorption. Taking proton pump inhibitors
(PPIs) to ease the symptoms of excess stomach acid for more than two years was linked to a
65 percent increase in the risk of vitamin B-12 deficiency.
Pantoprazole:
In the night, Mrs. Mitchell develops reflux again. She was prescribed two tablets of 40 mg
pantoprazole in the morning. I'd prefer that she have one in the morning and once in the evening.
12PARAPHRASING
Tramadol:
Mrs. Mitchell told me she was still having reflux at night and that tramadol didn't help the
stomach. If needed for stomach pain, tramadol was administered four times a day for a single
pill. I tell her to avoid tramadol which will cause constipation worse in exchange. Increases in
the pantoprazole dosing regimen will improve. In fact, liquid antacid may be prescribed to
alleviate her reflux and pressure in the stomach. She also said if she has abdominal pain a hot
pad is safer, and I recommend she sticks to it.
Prednisolone and Picolax:
Those two drugs may be withdrawn as they have not been used, and they have the potential to
give Mrs. Mitchell adverse effects.
Missing Drug
Iron:
Restless legs syndrome (RLS) is a common neurologic syndrome and is associated with iron
deficiency in many patients4. A study has shown that in patients whose serum ferritin was < 75
μg/l, oral iron therapy (325 mg ferrous sulfate twice a day on an empty stomach) on average
improved RLS symptoms after 3 months. A recent study has shown that giving oral iron more
than once a day or at a dose greater than 85 mg per day does not necessarily lead to a greater
increase in absorbable iron. Oral iron equivalent to 65-85 mg of elemental iron will be best
absorbed if given once a day. It should not be given with solid or liquid food/dietary supplements
or with milk. It should be given on an empty stomach an hour before eating or two hours after
eating along with 100-200 mg of vitamin C. An iron panel (early morning fasting blood to check
iron, ferritin, total iron-binding capacity (TIBC), and percent iron saturation) should be done
Tramadol:
Mrs. Mitchell told me she was still having reflux at night and that tramadol didn't help the
stomach. If needed for stomach pain, tramadol was administered four times a day for a single
pill. I tell her to avoid tramadol which will cause constipation worse in exchange. Increases in
the pantoprazole dosing regimen will improve. In fact, liquid antacid may be prescribed to
alleviate her reflux and pressure in the stomach. She also said if she has abdominal pain a hot
pad is safer, and I recommend she sticks to it.
Prednisolone and Picolax:
Those two drugs may be withdrawn as they have not been used, and they have the potential to
give Mrs. Mitchell adverse effects.
Missing Drug
Iron:
Restless legs syndrome (RLS) is a common neurologic syndrome and is associated with iron
deficiency in many patients4. A study has shown that in patients whose serum ferritin was < 75
μg/l, oral iron therapy (325 mg ferrous sulfate twice a day on an empty stomach) on average
improved RLS symptoms after 3 months. A recent study has shown that giving oral iron more
than once a day or at a dose greater than 85 mg per day does not necessarily lead to a greater
increase in absorbable iron. Oral iron equivalent to 65-85 mg of elemental iron will be best
absorbed if given once a day. It should not be given with solid or liquid food/dietary supplements
or with milk. It should be given on an empty stomach an hour before eating or two hours after
eating along with 100-200 mg of vitamin C. An iron panel (early morning fasting blood to check
iron, ferritin, total iron-binding capacity (TIBC), and percent iron saturation) should be done
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13PARAPHRASING
after three months to check on progress of the treatment. Oral iron should be stopped 2 days
before the iron studies are done. The goal is to get the serum ferritin above 100 μg/l.22, 23
Medication management with the same preferable brands
I will encourage Mrs. Mitchell to go to the nearest dosage administration help pharmacy (DAA)
where she filled out her order as she has a number of prescribed medications owing to the
treatment of many diseases. Through DAA's support, she doesn't need to think about which
medications she will take at what time and how many days. She just needs to open the DAA
compartment by breakfast, lunch or dinner and she'll get all the tablets to take. The pharmacy
would not replace the brand without her consent, either. Thus, either doctor can put a tick mark
on the script where it is mentioned “substitution not permitted “ or Mrs. Mitchell herself can tell
the pharmacy that she would like the same brands what she has been taken all the time.
Drug Interactions
Irbesartan with Amiloride
Coadministration of irbesartan and amiloride can give rise to risk of additive hyperkalemia.
There were cases of severe hyperkalemia that involved dialysis or induced death with combined
use of an angiotensin II antagonist (e.g. irbesartan, losartan, candesartan) and a potassium-
sparing diuretic (e.g. spironolactone) were reported. Serum potassium and renal function should
be closely monitored during combined usage, particularly in patients with additional risk factors
for hyperkalemia (e.g. renal dysfunction, advanced age, diabetes, > 25 mg / day spironolactone
dose).
after three months to check on progress of the treatment. Oral iron should be stopped 2 days
before the iron studies are done. The goal is to get the serum ferritin above 100 μg/l.22, 23
Medication management with the same preferable brands
I will encourage Mrs. Mitchell to go to the nearest dosage administration help pharmacy (DAA)
where she filled out her order as she has a number of prescribed medications owing to the
treatment of many diseases. Through DAA's support, she doesn't need to think about which
medications she will take at what time and how many days. She just needs to open the DAA
compartment by breakfast, lunch or dinner and she'll get all the tablets to take. The pharmacy
would not replace the brand without her consent, either. Thus, either doctor can put a tick mark
on the script where it is mentioned “substitution not permitted “ or Mrs. Mitchell herself can tell
the pharmacy that she would like the same brands what she has been taken all the time.
Drug Interactions
Irbesartan with Amiloride
Coadministration of irbesartan and amiloride can give rise to risk of additive hyperkalemia.
There were cases of severe hyperkalemia that involved dialysis or induced death with combined
use of an angiotensin II antagonist (e.g. irbesartan, losartan, candesartan) and a potassium-
sparing diuretic (e.g. spironolactone) were reported. Serum potassium and renal function should
be closely monitored during combined usage, particularly in patients with additional risk factors
for hyperkalemia (e.g. renal dysfunction, advanced age, diabetes, > 25 mg / day spironolactone
dose).
14PARAPHRASING
Movicol and Amiloride
Severe hyperkalemia can result from coadministration of amiloride and potassium (Movicol
contains 50.2 mg of potassium chloride). During the concurrent use of spironolactone and
potassium supplements, episodes of cardiac arrhythmia and at times extreme hyperkalemia were
recorded. The mixture should be stopped, unless hypokalaemia is verified and potassium
supplementation could be closely monitored. This interaction can also be induced by potassium-
containing salt substitutes, particularly those that can increase the potassium intake by 50-
60mmol per day.
Oxybutynin and Amitriptyline
Concurrent use of amitriptyline and oxybutynin may contribute to additional adverse effects of
anticholinergic agents. Hyperthermia, especially during hot weather, and paralytic ileus have
been recorded to be induced. The patient should be controlled during drug use for elevated
anticholinergic adverse effects (e.g. constipation, dry mouth, sedation and blurred vision). Mrs.
Mitchell has constipation, severe abdominal pain and a motility condition. The mixture of
pharmaceutical items should be treated with caution.
Aspirin and Gliclazide and Metformin
Low aspirin doses will reduce blood glucose levels and improve metformin's effectiveness.
Hypoglycemia can be caused by combined management. Blood glucose should be controlled
when prescribing aspirin (particularly high doses) in conjunction with oral antidiabetic agents. If
required a dosage of the antidiabetic drug should be changed.
Movicol and Amiloride
Severe hyperkalemia can result from coadministration of amiloride and potassium (Movicol
contains 50.2 mg of potassium chloride). During the concurrent use of spironolactone and
potassium supplements, episodes of cardiac arrhythmia and at times extreme hyperkalemia were
recorded. The mixture should be stopped, unless hypokalaemia is verified and potassium
supplementation could be closely monitored. This interaction can also be induced by potassium-
containing salt substitutes, particularly those that can increase the potassium intake by 50-
60mmol per day.
Oxybutynin and Amitriptyline
Concurrent use of amitriptyline and oxybutynin may contribute to additional adverse effects of
anticholinergic agents. Hyperthermia, especially during hot weather, and paralytic ileus have
been recorded to be induced. The patient should be controlled during drug use for elevated
anticholinergic adverse effects (e.g. constipation, dry mouth, sedation and blurred vision). Mrs.
Mitchell has constipation, severe abdominal pain and a motility condition. The mixture of
pharmaceutical items should be treated with caution.
Aspirin and Gliclazide and Metformin
Low aspirin doses will reduce blood glucose levels and improve metformin's effectiveness.
Hypoglycemia can be caused by combined management. Blood glucose should be controlled
when prescribing aspirin (particularly high doses) in conjunction with oral antidiabetic agents. If
required a dosage of the antidiabetic drug should be changed.
15PARAPHRASING
Diazepam and Amitriptyline
Benzodiazepines (diazepam) and tricyclic antidepressants (amitriptyline) may be used together to
induce additional CNS distress like prolonged sedation. Studies found reduced function of the
psychomotor, loss in memory and decreased sedation during coadministration of these drugs.
Meta-analysis also indicates concomitant use of benzodiazepines and subsequent sedation with
TCAs of elderly patients with an elevated risk of accidents and crashes in motor vehicles. Mrs
Mitchell is a 66-year-old woman who lives by herself. For her, the mix is dangerous. She should
therefore be cautioned about the dangers of slipping and undertaking complex tasks like driving.
Tramadol and Amitriptyline
Co-administering tricyclic antidepressants (amitriptyline) with tramadol can increase the risk of
seizures and serotonin syndrome. Cases of epilepsy and serotonin depression with concomitant
use of these compounds have been reported. Two severe instances of serotonin syndrome have
been reported on serotonergic drugs that triggered tramadol treatment in patients. Throughout
mixture use, Mrs. Mitchell should be closely monitored for signs and symptoms of epilepsy
and/or serotonin syndrome (agitation, shifts in mental status, myoclonus, diaphoresis, fever).
Cessation of amitriptyline and starting of pregabalin
One of Mrs. Mitchell's prescribed drugs, which is amitriptyline, does not get along with a few
medicines, including oxybutynin, diazepam, and tramadol. The repeated use of any of them with
amitriptyline has an adverse effect on Ms Mitchell. Amitriptyline has been recommended for
foot pain, but according to Mrs. Mitchell, she is still burning in the feet and is now moving up to
the knee, which indicates that it was not successful for the neuropathic foot pain of Mrs.
Mitchell. It is therefore advised that Mrs. Mitchell take a dose of 150 mg pregabalin per day,
given in two separated dosages. Based on the response and tolerability, the dosage may be
Diazepam and Amitriptyline
Benzodiazepines (diazepam) and tricyclic antidepressants (amitriptyline) may be used together to
induce additional CNS distress like prolonged sedation. Studies found reduced function of the
psychomotor, loss in memory and decreased sedation during coadministration of these drugs.
Meta-analysis also indicates concomitant use of benzodiazepines and subsequent sedation with
TCAs of elderly patients with an elevated risk of accidents and crashes in motor vehicles. Mrs
Mitchell is a 66-year-old woman who lives by herself. For her, the mix is dangerous. She should
therefore be cautioned about the dangers of slipping and undertaking complex tasks like driving.
Tramadol and Amitriptyline
Co-administering tricyclic antidepressants (amitriptyline) with tramadol can increase the risk of
seizures and serotonin syndrome. Cases of epilepsy and serotonin depression with concomitant
use of these compounds have been reported. Two severe instances of serotonin syndrome have
been reported on serotonergic drugs that triggered tramadol treatment in patients. Throughout
mixture use, Mrs. Mitchell should be closely monitored for signs and symptoms of epilepsy
and/or serotonin syndrome (agitation, shifts in mental status, myoclonus, diaphoresis, fever).
Cessation of amitriptyline and starting of pregabalin
One of Mrs. Mitchell's prescribed drugs, which is amitriptyline, does not get along with a few
medicines, including oxybutynin, diazepam, and tramadol. The repeated use of any of them with
amitriptyline has an adverse effect on Ms Mitchell. Amitriptyline has been recommended for
foot pain, but according to Mrs. Mitchell, she is still burning in the feet and is now moving up to
the knee, which indicates that it was not successful for the neuropathic foot pain of Mrs.
Mitchell. It is therefore advised that Mrs. Mitchell take a dose of 150 mg pregabalin per day,
given in two separated dosages. Based on the response and tolerability, the dosage may be
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
16PARAPHRASING
increased to 300mg / day, given as two divided doses, after 3-7 days and if required, can be
given to maximum doses of 600mg / day after an additional 7 days interval.
Disease-related problems
Constipation / Chronic abdominal pain / motility disorder
She is diagnosed with chronic abdominal pain and motility dysfunction. In fact, she was
diagnosed with diabetes too. For patients with diabetes mellitus, gastrointestinal symptoms such
as diarrhea, constipation, diarrhoea, and fecal incontinence are normal. Chronic constipation is
normal in adults over the age of 60, and signs appear in up to 50 percent of occupants in nursing
homes. It is advised that Mrs. Mitchell implement certain lifestyle changes, such as planned after
meal bath, improved fluid consumption and enhanced intake of dietary fibre. Additional intake
of fiber in the form of polycarbophil, methylcellulose, or psyllium can improve symptoms. Fiber
intake should be gradually increased over several weeks to decrease adverse effects.
Diabetic Neuropathy
Ms. Mitchell has diabetic conditions that affect both her legs and feet. She's had numbness and
foot pain and now going up to the elbows. The legs and feet are common sites for problems in
people with diabetes and this is why it is very important to look into foot care. Diabetes can
destroy the nerves and blood vessels which provide legs and feet. I propose that Mrs. Mitchell
take good care of her foot which is very important for people with diabetes.
Wash feet in warm (not hot) water every day and dry carefully, including between toes.
apply a moisturizer to feet after drying but avoid moisturizing between toes.
increased to 300mg / day, given as two divided doses, after 3-7 days and if required, can be
given to maximum doses of 600mg / day after an additional 7 days interval.
Disease-related problems
Constipation / Chronic abdominal pain / motility disorder
She is diagnosed with chronic abdominal pain and motility dysfunction. In fact, she was
diagnosed with diabetes too. For patients with diabetes mellitus, gastrointestinal symptoms such
as diarrhea, constipation, diarrhoea, and fecal incontinence are normal. Chronic constipation is
normal in adults over the age of 60, and signs appear in up to 50 percent of occupants in nursing
homes. It is advised that Mrs. Mitchell implement certain lifestyle changes, such as planned after
meal bath, improved fluid consumption and enhanced intake of dietary fibre. Additional intake
of fiber in the form of polycarbophil, methylcellulose, or psyllium can improve symptoms. Fiber
intake should be gradually increased over several weeks to decrease adverse effects.
Diabetic Neuropathy
Ms. Mitchell has diabetic conditions that affect both her legs and feet. She's had numbness and
foot pain and now going up to the elbows. The legs and feet are common sites for problems in
people with diabetes and this is why it is very important to look into foot care. Diabetes can
destroy the nerves and blood vessels which provide legs and feet. I propose that Mrs. Mitchell
take good care of her foot which is very important for people with diabetes.
Wash feet in warm (not hot) water every day and dry carefully, including between toes.
apply a moisturizer to feet after drying but avoid moisturizing between toes.
17PARAPHRASING
I noticed any callus forming, try to gently remove it. However, once formed, calluses
should only be treated by professionals.
When cutting toenails, cut straight across and file down any sharp edges. Use a nail
trimmer rather than scissors.
Always wear socks and shoes and choose shoes carefully. Shoes should be large enough
to be comfortable, but not large enough to be slipping off. They should have resilient (but
not soft) insoles, and be smooth on the inside, with no rough areas.
Corn plasters should not be used as they can cause foot ulcers.
I recommend her to check feet each night, looking for:
Dry, scaly, red, itching or cracked skin;
Areas where something has been rubbing on feet;
Blisters;
Cuts or abrasions;
Corns or calluses;
Infections;
Thickened or discolored nails;
Blueness or any swelling; and
Any red, hot or swollen areas.
Support groups for neuropathic pain
Living of neuropathic pain is extremely difficult. There are support groups that can provide an
opportunity to meet with others who are having a similar experience. Understanding from
I noticed any callus forming, try to gently remove it. However, once formed, calluses
should only be treated by professionals.
When cutting toenails, cut straight across and file down any sharp edges. Use a nail
trimmer rather than scissors.
Always wear socks and shoes and choose shoes carefully. Shoes should be large enough
to be comfortable, but not large enough to be slipping off. They should have resilient (but
not soft) insoles, and be smooth on the inside, with no rough areas.
Corn plasters should not be used as they can cause foot ulcers.
I recommend her to check feet each night, looking for:
Dry, scaly, red, itching or cracked skin;
Areas where something has been rubbing on feet;
Blisters;
Cuts or abrasions;
Corns or calluses;
Infections;
Thickened or discolored nails;
Blueness or any swelling; and
Any red, hot or swollen areas.
Support groups for neuropathic pain
Living of neuropathic pain is extremely difficult. There are support groups that can provide an
opportunity to meet with others who are having a similar experience. Understanding from
18PARAPHRASING
another can make us feel less alone, and can even share ideas about how to cope with pain and
how to handle it.
Hypertension
Mrs. Mitchell has a recent blood pressure result of 145/195 mmHg. For the patient with diabetes,
hypertension and a history of TIA/stroke, a blood pressure target of <140/90mmHg is
recommended and blood pressure control reduces both macro and microvascular complications.
To achieve Mrs. Mitchell in achieving target BP readings, she should be encouraged to maintain
a healthy weight with attention to her diet and physical activity. As per her, she has just 10
minutes' walk every day which should be extended up to half an hour or one hour. Her blood
pressure should continue to be regularly monitored and addition of cardioselective beta-blocker
atenolol Oral, initially 25–50 mg once daily considered since the BP target was not reached;
increase if required to 100 mg daily in 1 or 2 doses.
Gastro-oesophageal reflux (GORD)
Ms. Mitchell's on 40 mg pantoprazole which is two daily pills to be given. She reported that she
still had reflux at night. Attention to the already listed lifestyle factors will have a positive effect
on symptom management. Some ideas may include eating small meals, not eating until bedtime,
increasing bedside and preventing tight clothing. Consideration could be given in splitting the
pantoprazole 40 mg two tablets in the morning into taking one in the morning and one at night on
an empty stomach and addition of antacid in liquid or tablet form. As an infrequent adverse
effect of long term proton pump inhibitor use decrease absorption of vitamin B12. Ms. Mitchell
had been given hydroxocobalamin six months before telling her to take hydroxocobalamin for
three months she did not take and it also suggests that she was a defective person with vitamin
another can make us feel less alone, and can even share ideas about how to cope with pain and
how to handle it.
Hypertension
Mrs. Mitchell has a recent blood pressure result of 145/195 mmHg. For the patient with diabetes,
hypertension and a history of TIA/stroke, a blood pressure target of <140/90mmHg is
recommended and blood pressure control reduces both macro and microvascular complications.
To achieve Mrs. Mitchell in achieving target BP readings, she should be encouraged to maintain
a healthy weight with attention to her diet and physical activity. As per her, she has just 10
minutes' walk every day which should be extended up to half an hour or one hour. Her blood
pressure should continue to be regularly monitored and addition of cardioselective beta-blocker
atenolol Oral, initially 25–50 mg once daily considered since the BP target was not reached;
increase if required to 100 mg daily in 1 or 2 doses.
Gastro-oesophageal reflux (GORD)
Ms. Mitchell's on 40 mg pantoprazole which is two daily pills to be given. She reported that she
still had reflux at night. Attention to the already listed lifestyle factors will have a positive effect
on symptom management. Some ideas may include eating small meals, not eating until bedtime,
increasing bedside and preventing tight clothing. Consideration could be given in splitting the
pantoprazole 40 mg two tablets in the morning into taking one in the morning and one at night on
an empty stomach and addition of antacid in liquid or tablet form. As an infrequent adverse
effect of long term proton pump inhibitor use decrease absorption of vitamin B12. Ms. Mitchell
had been given hydroxocobalamin six months before telling her to take hydroxocobalamin for
three months she did not take and it also suggests that she was a defective person with vitamin
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
19PARAPHRASING
B12. Thus the amount of vitamin B12 should be asked to decide whether to know the current
standard. This is also a known long-term metformin problem where she took 850 mg twice a day.
Restless leg syndrome
Successful treatment of an underlying condition such as iron deficiency anemia or diabetes may
help relieve RLS symptoms at times. For mild cases of RLS the development of healthy sleep
schedules (also known as sleep hygiene) can be very beneficial. It covers things like trying to
build a normal room, eliminating caffeinated drinks during lunch and limiting excessive alcohol
and toba consumption As a trial, I would recommend her to be prescribed iron with the usual
starting dose of one tablet of 325 milligrams of ferrous sulfate once per day. it's best absorbed
when the stomach is acidic so to be taken on an empty stomach or with vitamin C to acidify the
stomach. Oral iron can induce stomach upset and constipation, and having it every other day
rather than regularly will improve. Both patients with RLS signs will undergo iron deficiency
examination. A ferritin amount should be obtained at least, although it is better to have a full iron
list, including the following, as ferritin can be falsely elevated in acute inflammatory states: iron
amounts, ferritin, transferrin saturation, overall iron-binding capacity.
References
MedicinesComplete: Baxter K (ed). Aspirin or other Salicylates + Corticosteroids or
Corticotropin: Stockleys Drug Interactions. RPS Publishing, London, UK, Available from
URL: http://www.medicinescomplete.com/mc [Accessed on 14/05/2013]
Kumthekar, A.A., Gidwani, H.V. and Kumthekar, A.B., 2012. Metformin associated B12
deficiency. J Assoc Physicians India, 60, pp.58-60.
B12. Thus the amount of vitamin B12 should be asked to decide whether to know the current
standard. This is also a known long-term metformin problem where she took 850 mg twice a day.
Restless leg syndrome
Successful treatment of an underlying condition such as iron deficiency anemia or diabetes may
help relieve RLS symptoms at times. For mild cases of RLS the development of healthy sleep
schedules (also known as sleep hygiene) can be very beneficial. It covers things like trying to
build a normal room, eliminating caffeinated drinks during lunch and limiting excessive alcohol
and toba consumption As a trial, I would recommend her to be prescribed iron with the usual
starting dose of one tablet of 325 milligrams of ferrous sulfate once per day. it's best absorbed
when the stomach is acidic so to be taken on an empty stomach or with vitamin C to acidify the
stomach. Oral iron can induce stomach upset and constipation, and having it every other day
rather than regularly will improve. Both patients with RLS signs will undergo iron deficiency
examination. A ferritin amount should be obtained at least, although it is better to have a full iron
list, including the following, as ferritin can be falsely elevated in acute inflammatory states: iron
amounts, ferritin, transferrin saturation, overall iron-binding capacity.
References
MedicinesComplete: Baxter K (ed). Aspirin or other Salicylates + Corticosteroids or
Corticotropin: Stockleys Drug Interactions. RPS Publishing, London, UK, Available from
URL: http://www.medicinescomplete.com/mc [Accessed on 14/05/2013]
Kumthekar, A.A., Gidwani, H.V. and Kumthekar, A.B., 2012. Metformin associated B12
deficiency. J Assoc Physicians India, 60, pp.58-60.
20PARAPHRASING
Heidelbaugh, J.J., 2013. Proton pump inhibitors and risk of vitamin and mineral deficiency:
evidence and clinical implications. Therapeutic advances in drug safety, 4(3), pp.125-133.
Trotti, L.M., Bhadriraju, S. and Becker, L.A., 2012. Iron for restless legs syndrome. Cochrane
Database of Systematic Reviews, (5).
Yutaka, M., Mifune, M., Kubota, E., Itoh, H. and Saito, I., 2009. Comparison of effects of low
dose of spironolactone and a thiazide diuretic in patients with hypertension treated with an
angiotensin-converting enzyme inhibitor or an angiotensin type 1 receptor blocker. Clinical and
experimental hypertension, 31(8), pp.648-656.
Fujii, H., Nakahama, H., Yoshihara, F., Nakamura, S., Inenaga, T. and Kawano, Y., 2005. Life-
threatening hyperkalemia during a combined therapy with the angiotensin receptor blocker
candesartan and spironolactone. Kobe Journal of Medical Sciences, 51(1/2), p.1.
Yap, V., Patel, A. and Thomsen, J., 1976. Hyperkalemia with cardiac arrhythmia: Induction by
salt substitutes, spironolactone, and azotemia. Jama, 236(24), pp.2775-2776.
MedicinesComplete: Baxter K (ed). Potassium-sparing diuretics + Potassium compounds:
Stockleys Drug Interactions. RPS Publishing, London, UK, Available from
URL: http://www.medicinescomplete.com/mc [Accessed on 25/11/2014]
Frizelle, F.A. and Colls, B.M., 2005. Hyponatremia and seizures after bowel preparation: report
of three cases. Diseases of the colon & rectum, 48(2), p.393.
Cho, Y.S., Nam, K.M., Park, J.H., Byun, S.H., Ryu, J.S. and Kim, H.J., 2014. Acute
hyponatremia with seizure and mental change after oral sodium picosulfate/magnesium citrate
bowel preparation. Annals of coloproctology, 30(6), p.290.
Heidelbaugh, J.J., 2013. Proton pump inhibitors and risk of vitamin and mineral deficiency:
evidence and clinical implications. Therapeutic advances in drug safety, 4(3), pp.125-133.
Trotti, L.M., Bhadriraju, S. and Becker, L.A., 2012. Iron for restless legs syndrome. Cochrane
Database of Systematic Reviews, (5).
Yutaka, M., Mifune, M., Kubota, E., Itoh, H. and Saito, I., 2009. Comparison of effects of low
dose of spironolactone and a thiazide diuretic in patients with hypertension treated with an
angiotensin-converting enzyme inhibitor or an angiotensin type 1 receptor blocker. Clinical and
experimental hypertension, 31(8), pp.648-656.
Fujii, H., Nakahama, H., Yoshihara, F., Nakamura, S., Inenaga, T. and Kawano, Y., 2005. Life-
threatening hyperkalemia during a combined therapy with the angiotensin receptor blocker
candesartan and spironolactone. Kobe Journal of Medical Sciences, 51(1/2), p.1.
Yap, V., Patel, A. and Thomsen, J., 1976. Hyperkalemia with cardiac arrhythmia: Induction by
salt substitutes, spironolactone, and azotemia. Jama, 236(24), pp.2775-2776.
MedicinesComplete: Baxter K (ed). Potassium-sparing diuretics + Potassium compounds:
Stockleys Drug Interactions. RPS Publishing, London, UK, Available from
URL: http://www.medicinescomplete.com/mc [Accessed on 25/11/2014]
Frizelle, F.A. and Colls, B.M., 2005. Hyponatremia and seizures after bowel preparation: report
of three cases. Diseases of the colon & rectum, 48(2), p.393.
Cho, Y.S., Nam, K.M., Park, J.H., Byun, S.H., Ryu, J.S. and Kim, H.J., 2014. Acute
hyponatremia with seizure and mental change after oral sodium picosulfate/magnesium citrate
bowel preparation. Annals of coloproctology, 30(6), p.290.
21PARAPHRASING
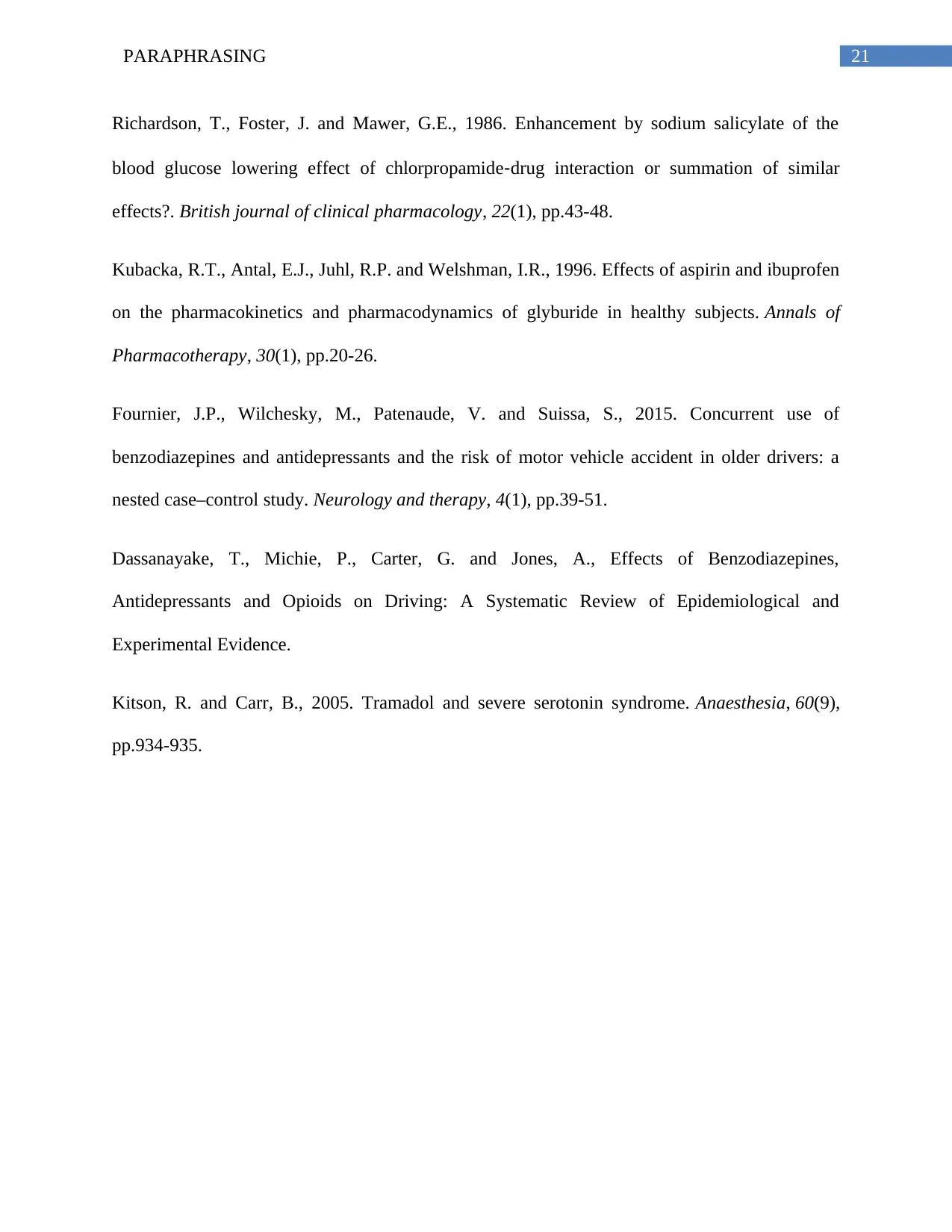
Richardson, T., Foster, J. and Mawer, G.E., 1986. Enhancement by sodium salicylate of the
blood glucose lowering effect of chlorpropamide‐drug interaction or summation of similar
effects?. British journal of clinical pharmacology, 22(1), pp.43-48.
Kubacka, R.T., Antal, E.J., Juhl, R.P. and Welshman, I.R., 1996. Effects of aspirin and ibuprofen
on the pharmacokinetics and pharmacodynamics of glyburide in healthy subjects. Annals of
Pharmacotherapy, 30(1), pp.20-26.
Fournier, J.P., Wilchesky, M., Patenaude, V. and Suissa, S., 2015. Concurrent use of
benzodiazepines and antidepressants and the risk of motor vehicle accident in older drivers: a
nested case–control study. Neurology and therapy, 4(1), pp.39-51.
Dassanayake, T., Michie, P., Carter, G. and Jones, A., Effects of Benzodiazepines,
Antidepressants and Opioids on Driving: A Systematic Review of Epidemiological and
Experimental Evidence.
Kitson, R. and Carr, B., 2005. Tramadol and severe serotonin syndrome. Anaesthesia, 60(9),
pp.934-935.
Richardson, T., Foster, J. and Mawer, G.E., 1986. Enhancement by sodium salicylate of the
blood glucose lowering effect of chlorpropamide‐drug interaction or summation of similar
effects?. British journal of clinical pharmacology, 22(1), pp.43-48.
Kubacka, R.T., Antal, E.J., Juhl, R.P. and Welshman, I.R., 1996. Effects of aspirin and ibuprofen
on the pharmacokinetics and pharmacodynamics of glyburide in healthy subjects. Annals of
Pharmacotherapy, 30(1), pp.20-26.
Fournier, J.P., Wilchesky, M., Patenaude, V. and Suissa, S., 2015. Concurrent use of
benzodiazepines and antidepressants and the risk of motor vehicle accident in older drivers: a
nested case–control study. Neurology and therapy, 4(1), pp.39-51.
Dassanayake, T., Michie, P., Carter, G. and Jones, A., Effects of Benzodiazepines,
Antidepressants and Opioids on Driving: A Systematic Review of Epidemiological and
Experimental Evidence.
Kitson, R. and Carr, B., 2005. Tramadol and severe serotonin syndrome. Anaesthesia, 60(9),
pp.934-935.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
22PARAPHRASING
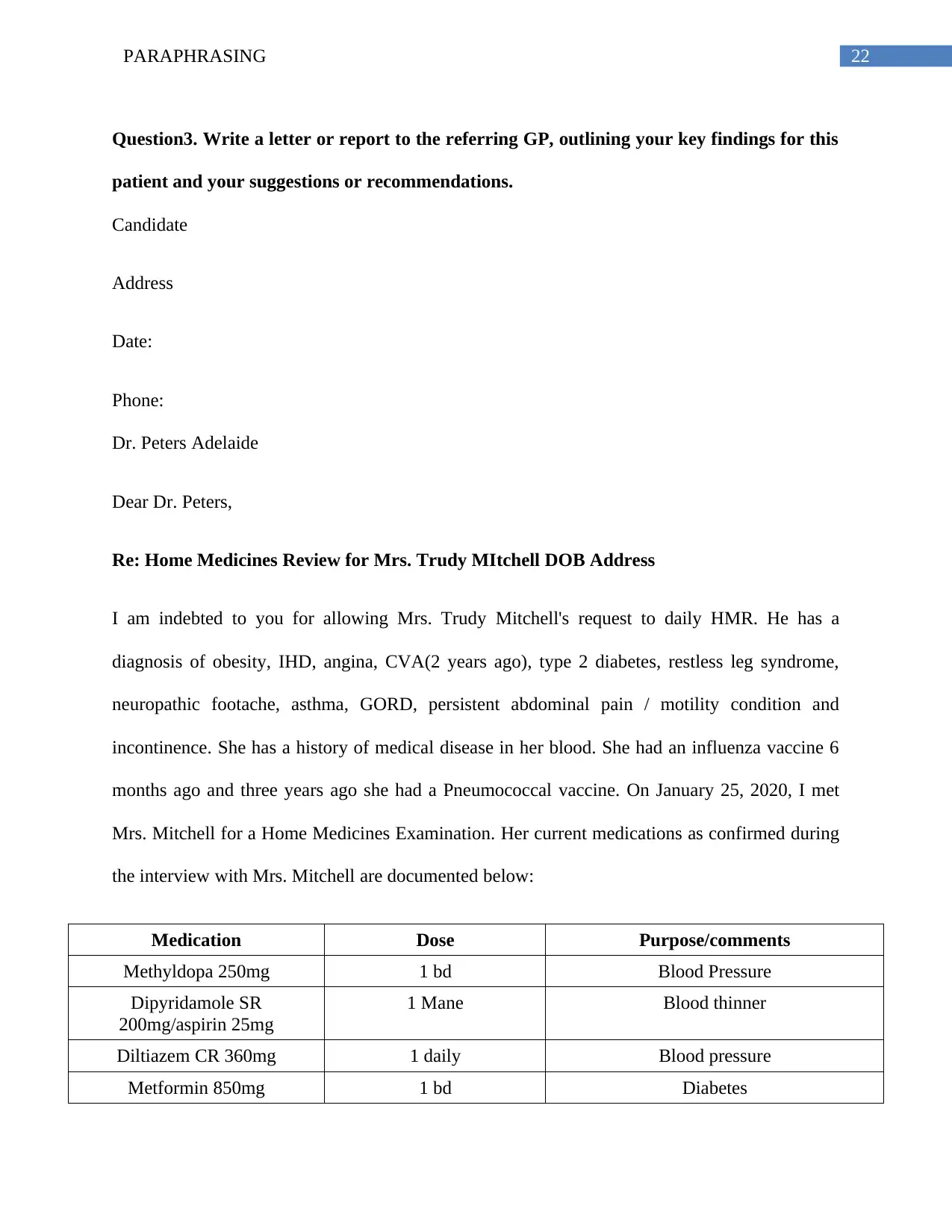
Question3. Write a letter or report to the referring GP, outlining your key findings for this
patient and your suggestions or recommendations.
Candidate
Address
Date:
Phone:
Dr. Peters Adelaide
Dear Dr. Peters,
Re: Home Medicines Review for Mrs. Trudy MItchell DOB Address
I am indebted to you for allowing Mrs. Trudy Mitchell's request to daily HMR. He has a
diagnosis of obesity, IHD, angina, CVA(2 years ago), type 2 diabetes, restless leg syndrome,
neuropathic footache, asthma, GORD, persistent abdominal pain / motility condition and
incontinence. She has a history of medical disease in her blood. She had an influenza vaccine 6
months ago and three years ago she had a Pneumococcal vaccine. On January 25, 2020, I met
Mrs. Mitchell for a Home Medicines Examination. Her current medications as confirmed during
the interview with Mrs. Mitchell are documented below:
Medication Dose Purpose/comments
Methyldopa 250mg 1 bd Blood Pressure
Dipyridamole SR
200mg/aspirin 25mg
1 Mane Blood thinner
Diltiazem CR 360mg 1 daily Blood pressure
Metformin 850mg 1 bd Diabetes
Question3. Write a letter or report to the referring GP, outlining your key findings for this
patient and your suggestions or recommendations.
Candidate
Address
Date:
Phone:
Dr. Peters Adelaide
Dear Dr. Peters,
Re: Home Medicines Review for Mrs. Trudy MItchell DOB Address
I am indebted to you for allowing Mrs. Trudy Mitchell's request to daily HMR. He has a
diagnosis of obesity, IHD, angina, CVA(2 years ago), type 2 diabetes, restless leg syndrome,
neuropathic footache, asthma, GORD, persistent abdominal pain / motility condition and
incontinence. She has a history of medical disease in her blood. She had an influenza vaccine 6
months ago and three years ago she had a Pneumococcal vaccine. On January 25, 2020, I met
Mrs. Mitchell for a Home Medicines Examination. Her current medications as confirmed during
the interview with Mrs. Mitchell are documented below:
Medication Dose Purpose/comments
Methyldopa 250mg 1 bd Blood Pressure
Dipyridamole SR
200mg/aspirin 25mg
1 Mane Blood thinner
Diltiazem CR 360mg 1 daily Blood pressure
Metformin 850mg 1 bd Diabetes
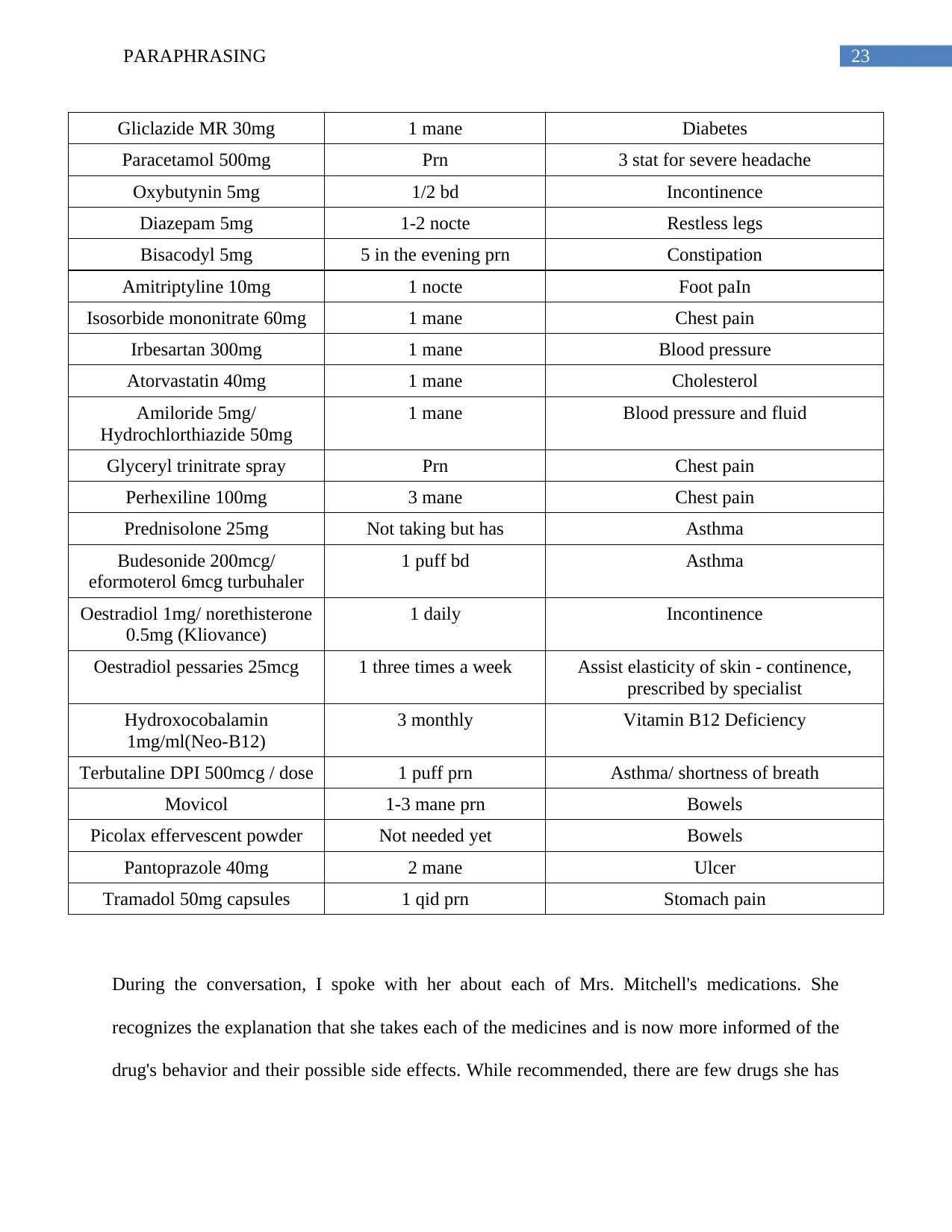
23PARAPHRASING
Gliclazide MR 30mg 1 mane Diabetes
Paracetamol 500mg Prn 3 stat for severe headache
Oxybutynin 5mg 1/2 bd Incontinence
Diazepam 5mg 1-2 nocte Restless legs
Bisacodyl 5mg 5 in the evening prn Constipation
Amitriptyline 10mg 1 nocte Foot paIn
Isosorbide mononitrate 60mg 1 mane Chest pain
Irbesartan 300mg 1 mane Blood pressure
Atorvastatin 40mg 1 mane Cholesterol
Amiloride 5mg/
Hydrochlorthiazide 50mg
1 mane Blood pressure and fluid
Glyceryl trinitrate spray Prn Chest pain
Perhexiline 100mg 3 mane Chest pain
Prednisolone 25mg Not taking but has Asthma
Budesonide 200mcg/
eformoterol 6mcg turbuhaler
1 puff bd Asthma
Oestradiol 1mg/ norethisterone
0.5mg (Kliovance)
1 daily Incontinence
Oestradiol pessaries 25mcg 1 three times a week Assist elasticity of skin - continence,
prescribed by specialist
Hydroxocobalamin
1mg/ml(Neo-B12)
3 monthly Vitamin B12 Deficiency
Terbutaline DPI 500mcg / dose 1 puff prn Asthma/ shortness of breath
Movicol 1-3 mane prn Bowels
Picolax effervescent powder Not needed yet Bowels
Pantoprazole 40mg 2 mane Ulcer
Tramadol 50mg capsules 1 qid prn Stomach pain
During the conversation, I spoke with her about each of Mrs. Mitchell's medications. She
recognizes the explanation that she takes each of the medicines and is now more informed of the
drug's behavior and their possible side effects. While recommended, there are few drugs she has
Gliclazide MR 30mg 1 mane Diabetes
Paracetamol 500mg Prn 3 stat for severe headache
Oxybutynin 5mg 1/2 bd Incontinence
Diazepam 5mg 1-2 nocte Restless legs
Bisacodyl 5mg 5 in the evening prn Constipation
Amitriptyline 10mg 1 nocte Foot paIn
Isosorbide mononitrate 60mg 1 mane Chest pain
Irbesartan 300mg 1 mane Blood pressure
Atorvastatin 40mg 1 mane Cholesterol
Amiloride 5mg/
Hydrochlorthiazide 50mg
1 mane Blood pressure and fluid
Glyceryl trinitrate spray Prn Chest pain
Perhexiline 100mg 3 mane Chest pain
Prednisolone 25mg Not taking but has Asthma
Budesonide 200mcg/
eformoterol 6mcg turbuhaler
1 puff bd Asthma
Oestradiol 1mg/ norethisterone
0.5mg (Kliovance)
1 daily Incontinence
Oestradiol pessaries 25mcg 1 three times a week Assist elasticity of skin - continence,
prescribed by specialist
Hydroxocobalamin
1mg/ml(Neo-B12)
3 monthly Vitamin B12 Deficiency
Terbutaline DPI 500mcg / dose 1 puff prn Asthma/ shortness of breath
Movicol 1-3 mane prn Bowels
Picolax effervescent powder Not needed yet Bowels
Pantoprazole 40mg 2 mane Ulcer
Tramadol 50mg capsules 1 qid prn Stomach pain
During the conversation, I spoke with her about each of Mrs. Mitchell's medications. She
recognizes the explanation that she takes each of the medicines and is now more informed of the
drug's behavior and their possible side effects. While recommended, there are few drugs she has
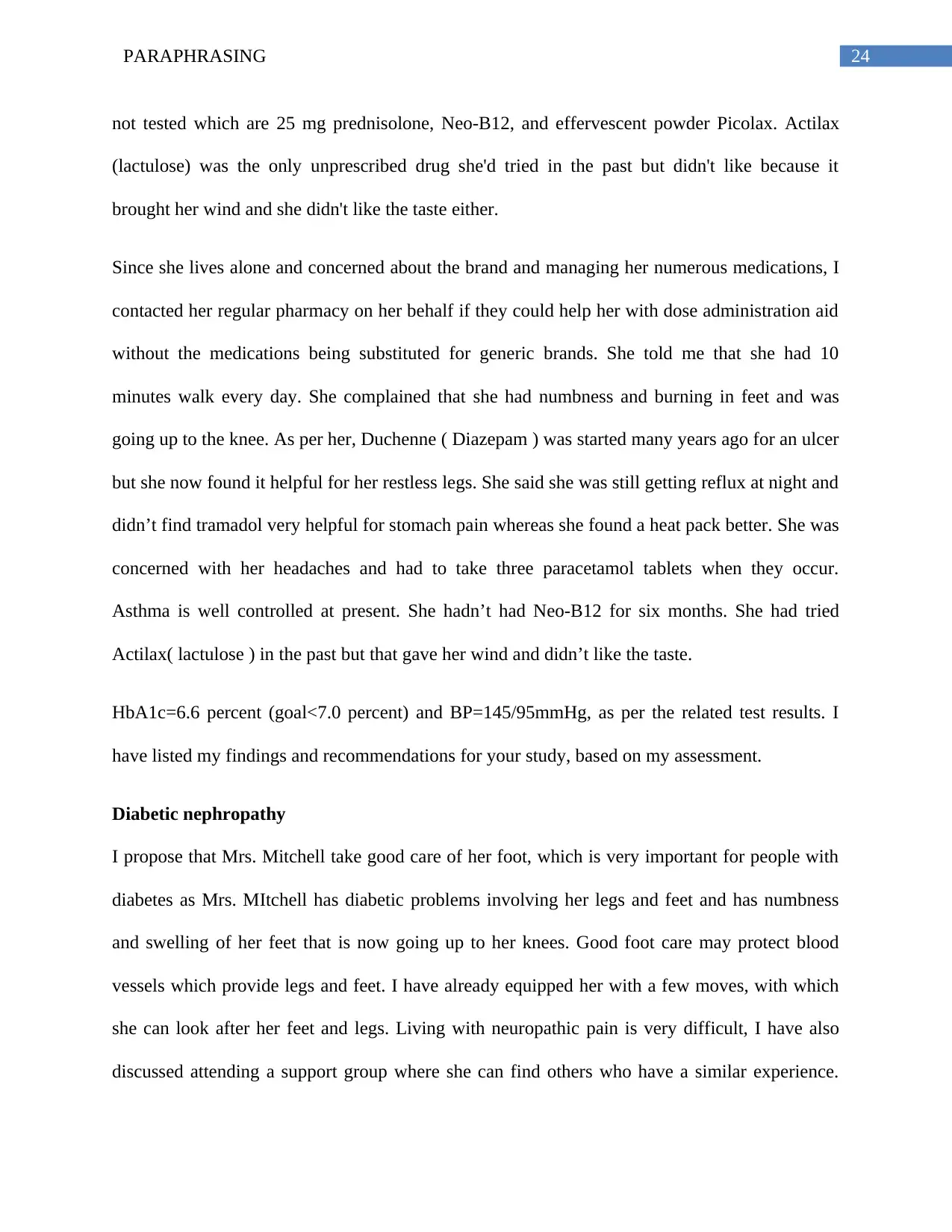
24PARAPHRASING
not tested which are 25 mg prednisolone, Neo-B12, and effervescent powder Picolax. Actilax
(lactulose) was the only unprescribed drug she'd tried in the past but didn't like because it
brought her wind and she didn't like the taste either.
Since she lives alone and concerned about the brand and managing her numerous medications, I
contacted her regular pharmacy on her behalf if they could help her with dose administration aid
without the medications being substituted for generic brands. She told me that she had 10
minutes walk every day. She complained that she had numbness and burning in feet and was
going up to the knee. As per her, Duchenne ( Diazepam ) was started many years ago for an ulcer
but she now found it helpful for her restless legs. She said she was still getting reflux at night and
didn’t find tramadol very helpful for stomach pain whereas she found a heat pack better. She was
concerned with her headaches and had to take three paracetamol tablets when they occur.
Asthma is well controlled at present. She hadn’t had Neo-B12 for six months. She had tried
Actilax( lactulose ) in the past but that gave her wind and didn’t like the taste.
HbA1c=6.6 percent (goal<7.0 percent) and BP=145/95mmHg, as per the related test results. I
have listed my findings and recommendations for your study, based on my assessment.
Diabetic nephropathy
I propose that Mrs. Mitchell take good care of her foot, which is very important for people with
diabetes as Mrs. MItchell has diabetic problems involving her legs and feet and has numbness
and swelling of her feet that is now going up to her knees. Good foot care may protect blood
vessels which provide legs and feet. I have already equipped her with a few moves, with which
she can look after her feet and legs. Living with neuropathic pain is very difficult, I have also
discussed attending a support group where she can find others who have a similar experience.
not tested which are 25 mg prednisolone, Neo-B12, and effervescent powder Picolax. Actilax
(lactulose) was the only unprescribed drug she'd tried in the past but didn't like because it
brought her wind and she didn't like the taste either.
Since she lives alone and concerned about the brand and managing her numerous medications, I
contacted her regular pharmacy on her behalf if they could help her with dose administration aid
without the medications being substituted for generic brands. She told me that she had 10
minutes walk every day. She complained that she had numbness and burning in feet and was
going up to the knee. As per her, Duchenne ( Diazepam ) was started many years ago for an ulcer
but she now found it helpful for her restless legs. She said she was still getting reflux at night and
didn’t find tramadol very helpful for stomach pain whereas she found a heat pack better. She was
concerned with her headaches and had to take three paracetamol tablets when they occur.
Asthma is well controlled at present. She hadn’t had Neo-B12 for six months. She had tried
Actilax( lactulose ) in the past but that gave her wind and didn’t like the taste.
HbA1c=6.6 percent (goal<7.0 percent) and BP=145/95mmHg, as per the related test results. I
have listed my findings and recommendations for your study, based on my assessment.
Diabetic nephropathy
I propose that Mrs. Mitchell take good care of her foot, which is very important for people with
diabetes as Mrs. MItchell has diabetic problems involving her legs and feet and has numbness
and swelling of her feet that is now going up to her knees. Good foot care may protect blood
vessels which provide legs and feet. I have already equipped her with a few moves, with which
she can look after her feet and legs. Living with neuropathic pain is very difficult, I have also
discussed attending a support group where she can find others who have a similar experience.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
25PARAPHRASING
That will make her feel less alone and she will also be able to exchange ideas on how to deal
with suffering and how to handle it.
Reflux
Ms. Mitchell still has reflux night for which she was given 40 mg pantoprazole which is two
morning pills to be taken. I recommend taking 40 mg pantoprazole one tablet twice a day; once
in the morning and one in the evening on an empty stomach and incorporating antacid in liquid
or tablet form if appropriate.
Attention to the already listed lifestyle factors will have a positive effect on symptom
management. I propose that she eat small meals, not feed until bed, lift her head to remove tight
clothes. The use of long term proton pump inhibitor as an unusual adverse effect reduces the
synthesis of vitamin B12. Ms. Mitchell had been given hydroxocobalamin six months before
telling her to take hydroxocobalamin for three months she did not take and it also suggests that
she was a defective person with vitamin B12. And I encourage her to have the amount of vitamin
B12 checked to assess the current level. This is also a known long-term metformin problem
where she took 850 mg twice a day.
Headaches
A headache might be the side effect of glyceryl trinitrate spray that she is supposed to take as
appropriate. Mrs. Mitchell takes 3 paracetamol-stat pills for severe headache. I will suggest Dr.
Peters to administer an average of 4 g daily with 0.5–1 g (two tablets) per 4–6 hours; I will
encourage Mrs Mitchell to find out the causes that cause and aggravate this. I will suggest that
she practice headache hygiene and outlines potential ways to make any lifestyle changes that can
have a significant impact on the incidence of headaches
That will make her feel less alone and she will also be able to exchange ideas on how to deal
with suffering and how to handle it.
Reflux
Ms. Mitchell still has reflux night for which she was given 40 mg pantoprazole which is two
morning pills to be taken. I recommend taking 40 mg pantoprazole one tablet twice a day; once
in the morning and one in the evening on an empty stomach and incorporating antacid in liquid
or tablet form if appropriate.
Attention to the already listed lifestyle factors will have a positive effect on symptom
management. I propose that she eat small meals, not feed until bed, lift her head to remove tight
clothes. The use of long term proton pump inhibitor as an unusual adverse effect reduces the
synthesis of vitamin B12. Ms. Mitchell had been given hydroxocobalamin six months before
telling her to take hydroxocobalamin for three months she did not take and it also suggests that
she was a defective person with vitamin B12. And I encourage her to have the amount of vitamin
B12 checked to assess the current level. This is also a known long-term metformin problem
where she took 850 mg twice a day.
Headaches
A headache might be the side effect of glyceryl trinitrate spray that she is supposed to take as
appropriate. Mrs. Mitchell takes 3 paracetamol-stat pills for severe headache. I will suggest Dr.
Peters to administer an average of 4 g daily with 0.5–1 g (two tablets) per 4–6 hours; I will
encourage Mrs Mitchell to find out the causes that cause and aggravate this. I will suggest that
she practice headache hygiene and outlines potential ways to make any lifestyle changes that can
have a significant impact on the incidence of headaches
26PARAPHRASING
Hypertension
Mrs. Mitchell has a recent blood pressure result of 145/195 mmHg. For a patient with diabetes,
hypertension and a history of TIA/stroke, a blood pressure target of <140/90mmHg is
recommended and blood pressure control reduces both macro and microvascular complications.
I recommend her to maintain a healthy weight with attention to her diet and physical activity to
achieve target BP readings. As per her, she has just 10 minutes’ walk every day, I also advised
her to extend that up to half an hour or one hour. Her blood pressure should continue to be
regularly monitored and addition of cardioselective beta-blocker atenolol oral, initially 25–50
mg once daily considered since the BP target was not reached; increase if required to 100 mg
daily in 1 or 2 doses.
Restless legs
As a trial, I recommend her an iron with the usual starting dose of one tablet of 325 milligrams of
ferrous sulfate once per day. it's absorption good when the stomach is acidic so it has to be taken
on an empty stomach or with vitamin C to acidify the stomach. Stomach upset and constipation
can be caused by oral iron, so it may help to take it every other day rather than daily.
Successfully treating an underlying condition such as iron deficiency anemia or diabetes can
sometimes help relieve the symptoms of RLS.
Establishing healthy sleep patterns (also known as sleep hygiene) can be very helpful in mild
cases of RLS. This includes such things as trying to develop a regular bedtime, avoiding
caffeinated drinks after lunch, and preventing excessive alcohol intake and tobacco. Doing a
relaxing and quiet activity before bed.
Hypertension
Mrs. Mitchell has a recent blood pressure result of 145/195 mmHg. For a patient with diabetes,
hypertension and a history of TIA/stroke, a blood pressure target of <140/90mmHg is
recommended and blood pressure control reduces both macro and microvascular complications.
I recommend her to maintain a healthy weight with attention to her diet and physical activity to
achieve target BP readings. As per her, she has just 10 minutes’ walk every day, I also advised
her to extend that up to half an hour or one hour. Her blood pressure should continue to be
regularly monitored and addition of cardioselective beta-blocker atenolol oral, initially 25–50
mg once daily considered since the BP target was not reached; increase if required to 100 mg
daily in 1 or 2 doses.
Restless legs
As a trial, I recommend her an iron with the usual starting dose of one tablet of 325 milligrams of
ferrous sulfate once per day. it's absorption good when the stomach is acidic so it has to be taken
on an empty stomach or with vitamin C to acidify the stomach. Stomach upset and constipation
can be caused by oral iron, so it may help to take it every other day rather than daily.
Successfully treating an underlying condition such as iron deficiency anemia or diabetes can
sometimes help relieve the symptoms of RLS.
Establishing healthy sleep patterns (also known as sleep hygiene) can be very helpful in mild
cases of RLS. This includes such things as trying to develop a regular bedtime, avoiding
caffeinated drinks after lunch, and preventing excessive alcohol intake and tobacco. Doing a
relaxing and quiet activity before bed.
27PARAPHRASING
All patients with symptoms of RLS should be tested for iron deficiency. At a minimum, a ferritin
level should be obtained, although a complete iron panel, including the following, is preferable
since ferritin can be falsely elevated in acute inflammatory states: Iron levels, Ferritin,
Transferrin saturation, Total iron-binding capacity
Constipation
It is recommended that Mrs. Mitchell should initiate some lifestyle modifications, such as
scheduled after meal toilet, increased intake of fluid and increased dietary fiber intake.
Additional intake of fiber in the form of polycarbophil, methylcellulose, or psyllium can improve
symptoms. Fiber intake should be gradually increased over several weeks to decrease adverse
effects.
Cessation of drugs
Tramadol
Because tramadol doesn't support her stomach ache and heat pack is safer as per her, I suggest
avoiding tramadol which makes constipation worse in exchange. Improvements in the
pantoprazole dosing regimen would also improve. In fact, liquid antacid may be prescribed to
relieve her reflux and pressure in the stomach.
Prednisolone and Picola
These two medications can be ceased as they haven’t been used and they have the potential to
give adverse effects to Mrs. Mitchell.
All patients with symptoms of RLS should be tested for iron deficiency. At a minimum, a ferritin
level should be obtained, although a complete iron panel, including the following, is preferable
since ferritin can be falsely elevated in acute inflammatory states: Iron levels, Ferritin,
Transferrin saturation, Total iron-binding capacity
Constipation
It is recommended that Mrs. Mitchell should initiate some lifestyle modifications, such as
scheduled after meal toilet, increased intake of fluid and increased dietary fiber intake.
Additional intake of fiber in the form of polycarbophil, methylcellulose, or psyllium can improve
symptoms. Fiber intake should be gradually increased over several weeks to decrease adverse
effects.
Cessation of drugs
Tramadol
Because tramadol doesn't support her stomach ache and heat pack is safer as per her, I suggest
avoiding tramadol which makes constipation worse in exchange. Improvements in the
pantoprazole dosing regimen would also improve. In fact, liquid antacid may be prescribed to
relieve her reflux and pressure in the stomach.
Prednisolone and Picola
These two medications can be ceased as they haven’t been used and they have the potential to
give adverse effects to Mrs. Mitchell.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
28PARAPHRASING
Modification dosage regimen
Dipyridamole/ aspirin
The recommended amount of dipyridamole is one pill twice daily, typically one in the morning
and one in the evening, ideally with meals whereas the drug was taken once daily by Mrs.
Mitchell. The tablet to be withdrawn from the package just before use; if it is not covered by the
wrapping, aspirin will break down easily.
Hyperkalemia
Irbesartan, Movicol (which includes potassium chloride) and Amiloride are just a few drugs
given to Mrs. Mitchell which can induce hyperkalemia either individually or in combination. I
suggest that Mrs. Mitchell have her blood potassium checked. Hyperkalemia is characterized in
adults as a serum potassium concentration greater than around 5.0-5.5 mEq / L. Rates above 7
mEq / L can lead to significant psychological and hemodynamic symptoms, while rates over 8.5
mEq / L can induce respiratory failure or cardiac arrest and can be lethal rapidly. Most
hyperkalemia-patients are asymptomatic. Symptoms are nonspecific as occurring and are
primarily related to muscle or heart activity. As the pharmacist in charge of carrying out this
analysis of medication management, I recognize that there may be strong scientific explanations
that my guidelines may not be deemed appropriate for this case. I accept guidance on this and
how you can render such reports more valuable. I would be happy to provide literature
addressing or clarifying any issue raised in this article.
Yours Sincerely,
………………….
Modification dosage regimen
Dipyridamole/ aspirin
The recommended amount of dipyridamole is one pill twice daily, typically one in the morning
and one in the evening, ideally with meals whereas the drug was taken once daily by Mrs.
Mitchell. The tablet to be withdrawn from the package just before use; if it is not covered by the
wrapping, aspirin will break down easily.
Hyperkalemia
Irbesartan, Movicol (which includes potassium chloride) and Amiloride are just a few drugs
given to Mrs. Mitchell which can induce hyperkalemia either individually or in combination. I
suggest that Mrs. Mitchell have her blood potassium checked. Hyperkalemia is characterized in
adults as a serum potassium concentration greater than around 5.0-5.5 mEq / L. Rates above 7
mEq / L can lead to significant psychological and hemodynamic symptoms, while rates over 8.5
mEq / L can induce respiratory failure or cardiac arrest and can be lethal rapidly. Most
hyperkalemia-patients are asymptomatic. Symptoms are nonspecific as occurring and are
primarily related to muscle or heart activity. As the pharmacist in charge of carrying out this
analysis of medication management, I recognize that there may be strong scientific explanations
that my guidelines may not be deemed appropriate for this case. I accept guidance on this and
how you can render such reports more valuable. I would be happy to provide literature
addressing or clarifying any issue raised in this article.
Yours Sincerely,
………………….
29PARAPHRASING
References
Ross S, managing editor, Australian Medicines Handbook. Adelaide: Australian Medicines
Handbook Pty. Ltd. 2010. p. 465
Ross S, managing editor, Australian Medicines Handbook. Adelaide: Australian Medicines
Handbook Pty. Ltd. 2010. p. 472
Ross S, managing editor, Australian Medicines Handbook. Adelaide: Australian Medicines
Handbook Pty. Ltd. 2010. p. 610
Gamaldo CE, Earley CJ. Restless legs syndrome: a clinical update. Chest. 2006 Nov.
130(5):1596-604. [Medline].
Hening WA. Restless Legs Syndrome. Curr Treat Options Neurol.1999 Sep. 1(4):309-319.
References
Ross S, managing editor, Australian Medicines Handbook. Adelaide: Australian Medicines
Handbook Pty. Ltd. 2010. p. 465
Ross S, managing editor, Australian Medicines Handbook. Adelaide: Australian Medicines
Handbook Pty. Ltd. 2010. p. 472
Ross S, managing editor, Australian Medicines Handbook. Adelaide: Australian Medicines
Handbook Pty. Ltd. 2010. p. 610
Gamaldo CE, Earley CJ. Restless legs syndrome: a clinical update. Chest. 2006 Nov.
130(5):1596-604. [Medline].
Hening WA. Restless Legs Syndrome. Curr Treat Options Neurol.1999 Sep. 1(4):309-319.
1 out of 30
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.

