Nursing Care Plan for an Elderly Patient with Recurrent Falls
VerifiedAdded on 2023/04/25
|18
|2536
|195
AI Summary
This nursing care plan outlines the management of an elderly patient with recurrent falls. It covers medical diagnosis, age-related issues, preparation for procedures, privacy and dignity, ongoing assessment, and a wellness approach to health. The document includes actual and potential problems, goals, strategies, and outcomes.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

laiba
[COMPANY NAME] [Company address]
[DOCUMENT TITLE]
[COMPANY NAME] [Company address]
[DOCUMENT TITLE]
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

Table of Contents
Part A – Introduction.................................................................................................................................... 3
Medical Diagnosis.................................................................................................................................... 3
Age-related issues................................................................................................................................... 3
Preparation for procedures...................................................................................................................... 4
Privacy and Dignity.................................................................................................................................. 6
Ongoing assessment............................................................................................................................... 6
Wellness approach to health.................................................................................................................... 8
Part B – Nursing care plan........................................................................................................................... 9
3 Actual problems of John........................................................................................................................ 9
Actual Problem 1.................................................................................................................................. 9
Actual Problem 2................................................................................................................................ 12
Actual problem 3................................................................................................................................. 15
Potential problem 1............................................................................................................................. 17
Potential problem 2............................................................................................................................. 20
References................................................................................................................................................ 22
Part A – Introduction.................................................................................................................................... 3
Medical Diagnosis.................................................................................................................................... 3
Age-related issues................................................................................................................................... 3
Preparation for procedures...................................................................................................................... 4
Privacy and Dignity.................................................................................................................................. 6
Ongoing assessment............................................................................................................................... 6
Wellness approach to health.................................................................................................................... 8
Part B – Nursing care plan........................................................................................................................... 9
3 Actual problems of John........................................................................................................................ 9
Actual Problem 1.................................................................................................................................. 9
Actual Problem 2................................................................................................................................ 12
Actual problem 3................................................................................................................................. 15
Potential problem 1............................................................................................................................. 17
Potential problem 2............................................................................................................................. 20
References................................................................................................................................................ 22

Part A – Introduction
Medical Diagnosis
John is an 84 year old man who was admitted in the hospital as he suffers from
recurrent falls due to functional and cognitive decline. John has past history of
hypercholesterolemia, hypertension, Type-2 Diabetes Mellitus, Benign prostatic
hyperplasia, Parkinson’s disease and dementia.
Certain assessments were performed during his hospital stay which are \ assessment of
gait, balance and mobility, and muscle weakness, assessment of osteoporosis risk,
assessment of the John’s perceived functional ability and fear relating to falling,
assessment of visual and cognitive impairment and urinary incontinence assessment.
People over the age of 65 like John are at increased risk of falls in home settings as
well as outside. When he suffers from an incident of fall, it is linked with other distress
such as mild to severe pain and injury depending upon the severity of fall. He can also
experience loss of confidence, compromise in his independence and declined mortality.
Age-related issues
John is 84 year old and the age will affect his ability to meet various activities of daily
living needs such as:
Medical Diagnosis
John is an 84 year old man who was admitted in the hospital as he suffers from
recurrent falls due to functional and cognitive decline. John has past history of
hypercholesterolemia, hypertension, Type-2 Diabetes Mellitus, Benign prostatic
hyperplasia, Parkinson’s disease and dementia.
Certain assessments were performed during his hospital stay which are \ assessment of
gait, balance and mobility, and muscle weakness, assessment of osteoporosis risk,
assessment of the John’s perceived functional ability and fear relating to falling,
assessment of visual and cognitive impairment and urinary incontinence assessment.
People over the age of 65 like John are at increased risk of falls in home settings as
well as outside. When he suffers from an incident of fall, it is linked with other distress
such as mild to severe pain and injury depending upon the severity of fall. He can also
experience loss of confidence, compromise in his independence and declined mortality.
Age-related issues
John is 84 year old and the age will affect his ability to meet various activities of daily
living needs such as:

Decision-making: Due to the dementia his judgment gets hampered which will
lead to poor decision-making which will affect the minor to major activities of daily
life such as bathing, choosing outfits, etc. (Heerema, 2018).
Freedom of movement: As John’s age increases, muscles in his body are
gradually replaced by fibrous tissue. Specifically the muscles of upper and lower
extremities become flabby and weak which makes an individual inactive. In
addition, with age bones get brittle, loss of bone is seen due to reduced bone
density, which leads to increased risk of fractures. The injury from even a minor
trauma can increase risk and prevalence of osteoporosis. Further, restriction of
joint mobility, appearance of spurs and points on bone ends, limits the range of
motion and increases the frequency and intensity of joint pain. Changes in gait
with person’s increasing age is also seen because of the structural and postural
changes. Overall due to all these changes John’s mobility is affected.
Memory: With increasing age of John, his speed of processing sensory
information gets slower. Changes in central as well as peripheral nervous system
lead to this. Due to changes in storage and retrieval of information, John would not
be slowed down in performing various tasks of daily living. Further due to memory
issues, the chances of redundancy or duplication of tasks also increases (Williams,
2016).
Preparation for procedures
lead to poor decision-making which will affect the minor to major activities of daily
life such as bathing, choosing outfits, etc. (Heerema, 2018).
Freedom of movement: As John’s age increases, muscles in his body are
gradually replaced by fibrous tissue. Specifically the muscles of upper and lower
extremities become flabby and weak which makes an individual inactive. In
addition, with age bones get brittle, loss of bone is seen due to reduced bone
density, which leads to increased risk of fractures. The injury from even a minor
trauma can increase risk and prevalence of osteoporosis. Further, restriction of
joint mobility, appearance of spurs and points on bone ends, limits the range of
motion and increases the frequency and intensity of joint pain. Changes in gait
with person’s increasing age is also seen because of the structural and postural
changes. Overall due to all these changes John’s mobility is affected.
Memory: With increasing age of John, his speed of processing sensory
information gets slower. Changes in central as well as peripheral nervous system
lead to this. Due to changes in storage and retrieval of information, John would not
be slowed down in performing various tasks of daily living. Further due to memory
issues, the chances of redundancy or duplication of tasks also increases (Williams,
2016).
Preparation for procedures
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

When John was admitted into the hospital, he was sent in elderly ward. Nurse took
various action on his admission which are listed below:
Nurse undertook several assessments of John as mentioned above so that a
tailored intervention could be prepared from him. She explained him about each
assessment in simple language before commencing them so that he could
understand the need of those assessments.
After explaining every procedure verbal consent was obtained from him.
Since John had cognitive decline at various instances his wife was referred to for
obtaining consent.
Since John’s mobility was restricted, nurse assisted her in tasks of hygiene,
eating, etc.
Nurse ensured than John was safe from any risk hazards of falling.
She always followed hand hygiene.
She kept and maintained records of John’s health progress timely.
She checked ID before any routine activity such as medicine administration.
Since John also experienced functional decline nurses always ensured that he
was placed in a comfortable and suitable position so that he doesn’t face any pain
or discomfort.
Nurse reviewed his requirements for pre-medication, sedation, and monitoring.
She followed up to ensure John’s safety.
Privacy and Dignity
various action on his admission which are listed below:
Nurse undertook several assessments of John as mentioned above so that a
tailored intervention could be prepared from him. She explained him about each
assessment in simple language before commencing them so that he could
understand the need of those assessments.
After explaining every procedure verbal consent was obtained from him.
Since John had cognitive decline at various instances his wife was referred to for
obtaining consent.
Since John’s mobility was restricted, nurse assisted her in tasks of hygiene,
eating, etc.
Nurse ensured than John was safe from any risk hazards of falling.
She always followed hand hygiene.
She kept and maintained records of John’s health progress timely.
She checked ID before any routine activity such as medicine administration.
Since John also experienced functional decline nurses always ensured that he
was placed in a comfortable and suitable position so that he doesn’t face any pain
or discomfort.
Nurse reviewed his requirements for pre-medication, sedation, and monitoring.
She followed up to ensure John’s safety.
Privacy and Dignity

It was ensured that John’s privacy and dignity were always maintained while
caring for him.
Nurse always obtained verbal consent from him before undertaking any task
which gave him the choice to deny if he felt uneasy or violated. John or his wife
were completely involved at every step of decision making during their care
management.
During carrying out tasks of personal care, nurses ensured that sufficient privacy
was maintained so that John didn’t feel vulnerable.
Nurses always sought permission from John before touching or moving any of
his personal belongings so that his personal space is respected.
Ongoing assessment
The Ongoing assessment of John include:
Neurological examination
Pressure injury assessment
Falls risk assessment
Mobility assessment
Urine incontinence assessment
caring for him.
Nurse always obtained verbal consent from him before undertaking any task
which gave him the choice to deny if he felt uneasy or violated. John or his wife
were completely involved at every step of decision making during their care
management.
During carrying out tasks of personal care, nurses ensured that sufficient privacy
was maintained so that John didn’t feel vulnerable.
Nurses always sought permission from John before touching or moving any of
his personal belongings so that his personal space is respected.
Ongoing assessment
The Ongoing assessment of John include:
Neurological examination
Pressure injury assessment
Falls risk assessment
Mobility assessment
Urine incontinence assessment

Impulsive close monitoring is going on to observe respiratory rate, heart rate, blood
pressure, temperature, pain score, skin integrity, urinalysis, BSL, weight.
Several devices are used for the purpose of these observations and assessments such
as sphygnomanometer, pulse oximeter, weighing machine, glucometer and
thermometer.
Observation of John as per the devices are:
DATE
Respiratory rate 18 bpm
SPo2 98%
Blood pressure Lying:140/84 mm/hg
Standing: 132/82 mm/hg
Heart rate 78bpm
Temperature 37.4
Neurological Alert
Pain score 3/10
Weight 74.36kg
Urinalysis NAD
Fasting BSL 136
pressure, temperature, pain score, skin integrity, urinalysis, BSL, weight.
Several devices are used for the purpose of these observations and assessments such
as sphygnomanometer, pulse oximeter, weighing machine, glucometer and
thermometer.
Observation of John as per the devices are:
DATE
Respiratory rate 18 bpm
SPo2 98%
Blood pressure Lying:140/84 mm/hg
Standing: 132/82 mm/hg
Heart rate 78bpm
Temperature 37.4
Neurological Alert
Pain score 3/10
Weight 74.36kg
Urinalysis NAD
Fasting BSL 136
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Wellness approach to health
A recovery approach based on holistic care is adopted by the nurse so that all the
needs of John can be taken care of including physiological, mental and social. John’s
care plan should not only focus on his incidences of falls but also on his functional and
cognitive deficits. The wellness approach will include a collaborative efforts from nurses,
OT, physiotherapists, social worker and his family. John was non-ambulant, continent
but required assistance in mobility so he will be required to learn skills which can cope
up with his compromised mobility so that he can back his optimum independence
considering his age and medical history. Use of assisted technologies can be used to
meet the requirements of his cognitive deficits. His mental status must always be
reviewed timely so that his psychological well-being is maintained.
A recovery approach based on holistic care is adopted by the nurse so that all the
needs of John can be taken care of including physiological, mental and social. John’s
care plan should not only focus on his incidences of falls but also on his functional and
cognitive deficits. The wellness approach will include a collaborative efforts from nurses,
OT, physiotherapists, social worker and his family. John was non-ambulant, continent
but required assistance in mobility so he will be required to learn skills which can cope
up with his compromised mobility so that he can back his optimum independence
considering his age and medical history. Use of assisted technologies can be used to
meet the requirements of his cognitive deficits. His mental status must always be
reviewed timely so that his psychological well-being is maintained.

Part B – Nursing care plan
3 Actual problems of John
Actual Problem 1
Identification of
problems
Establishment of
Goals (with Time
Frame)
Taking Action
(Nursing management
strategies)
Evaluation
of
Outcomes
Reflection
on process
1. Increased
incidence
s of falls
Minimise the
number of falls by
ensuring
elimination of all
the preventable
falls during hospital
stay and after
going home
1. John will be trained
as per his mental
capacity to orient
him to his
environment such
as using call bells,
bed rails, etc.
Incidence
of falls
minimised.
I believe a
collaborative
effort from
patients,
professionals
and family is
required to
orient the
patient and
his
environment
so that falls
could be
minimised, if
not prevented
(Vonnes &
Wolf, 2017).
3. Nurse will regularly
review his
surroundings for
any kinds of
hazards and
remove them.
5. His wife and other
family members will
be trained to identify
the risk factors of
falls so that falls can
be prevented.
7. Nurse will
3 Actual problems of John
Actual Problem 1
Identification of
problems
Establishment of
Goals (with Time
Frame)
Taking Action
(Nursing management
strategies)
Evaluation
of
Outcomes
Reflection
on process
1. Increased
incidence
s of falls
Minimise the
number of falls by
ensuring
elimination of all
the preventable
falls during hospital
stay and after
going home
1. John will be trained
as per his mental
capacity to orient
him to his
environment such
as using call bells,
bed rails, etc.
Incidence
of falls
minimised.
I believe a
collaborative
effort from
patients,
professionals
and family is
required to
orient the
patient and
his
environment
so that falls
could be
minimised, if
not prevented
(Vonnes &
Wolf, 2017).
3. Nurse will regularly
review his
surroundings for
any kinds of
hazards and
remove them.
5. His wife and other
family members will
be trained to identify
the risk factors of
falls so that falls can
be prevented.
7. Nurse will
collaborate with OT
and social worker to
ensure John’s
safety by identifying
the assistive aids
required by him in
hospital and at
home.
9. Falls risk
assessment will be
reviewed weekly.
11. Nurse will instruct
him to use non-
slippery shoes,
shoes without laces
to maintain comfort
while walking.
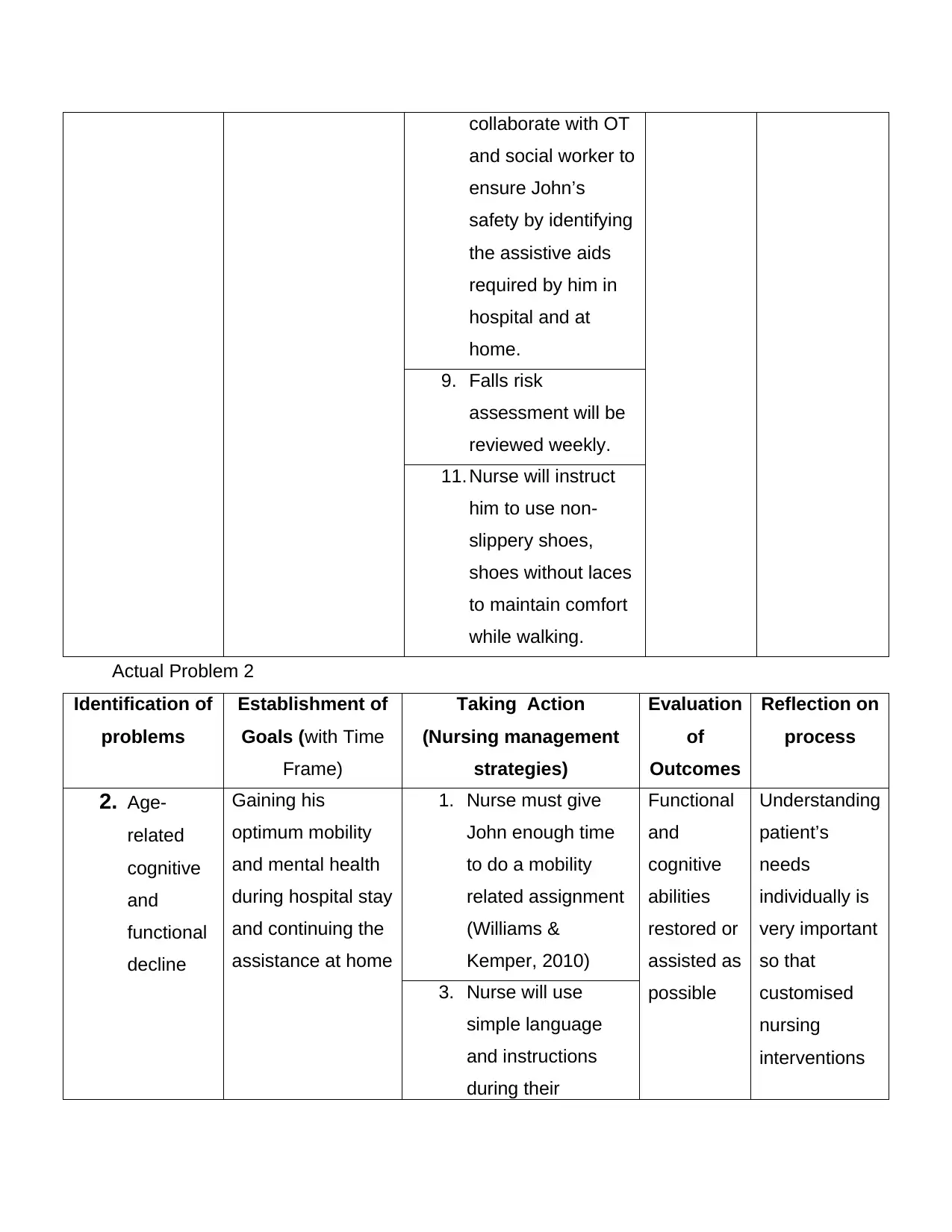
Actual Problem 2
Identification of
problems
Establishment of
Goals (with Time
Frame)
Taking Action
(Nursing management
strategies)
Evaluation
of
Outcomes
Reflection on
process
2. Age-
related
cognitive
and
functional
decline
Gaining his
optimum mobility
and mental health
during hospital stay
and continuing the
assistance at home
1. Nurse must give
John enough time
to do a mobility
related assignment
(Williams &
Kemper, 2010)
Functional
and
cognitive
abilities
restored or
assisted as
possible
Understanding
patient’s
needs
individually is
very important
so that
customised
nursing
interventions
3. Nurse will use
simple language
and instructions
during their
and social worker to
ensure John’s
safety by identifying
the assistive aids
required by him in
hospital and at
home.
9. Falls risk
assessment will be
reviewed weekly.
11. Nurse will instruct
him to use non-
slippery shoes,
shoes without laces
to maintain comfort
while walking.
Actual Problem 2
Identification of
problems
Establishment of
Goals (with Time
Frame)
Taking Action
(Nursing management
strategies)
Evaluation
of
Outcomes
Reflection on
process
2. Age-
related
cognitive
and
functional
decline
Gaining his
optimum mobility
and mental health
during hospital stay
and continuing the
assistance at home
1. Nurse must give
John enough time
to do a mobility
related assignment
(Williams &
Kemper, 2010)
Functional
and
cognitive
abilities
restored or
assisted as
possible
Understanding
patient’s
needs
individually is
very important
so that
customised
nursing
interventions
3. Nurse will use
simple language
and instructions
during their
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

sessions can be
planned5. Including possible
range of motion
exercises in the
care plan (Laver,
dyer, Whitehead, &
Clemson, 2016)
7. Provision of
assistive devices
such as alarm
clock, cane etc.
9. Instruct the family
regarding his
personal care
11. Maintain clear
pathway with
adequate light for
him
planned5. Including possible
range of motion
exercises in the
care plan (Laver,
dyer, Whitehead, &
Clemson, 2016)
7. Provision of
assistive devices
such as alarm
clock, cane etc.
9. Instruct the family
regarding his
personal care
11. Maintain clear
pathway with
adequate light for
him

Actual problem 3
Identification of
problems
Establishment of
Goals (with Time
Frame)
Taking Action
(Nursing management
strategies)
Evaluation
of
Outcomes
Reflection
on process
3. Disturbed
skin
integrity
due to
restricted
mobility
Ensure the
maintenance of
skin integrity by
preventing
development of
pressure injuries
during hospital
stay.
1. Repositioning of
John every four
hours so that
pressure from the
sore can be
relieved (Murphree,
2017)
Maintenanc
e of skin
integrity and
prevention
of
occurrence
of pressure
injury
I learnt
several
methods
apart from
repositioning
which can be
used to
prevent
pressure
injury
3. Nurse will apply
moisturiser if any
region of the body
gets reddened
5. Bathing daily for
skin hygiene and
ensure circulation
of blood flow
7. Pressure relieving
aids such as foams
or air mattress can
be used
9. Skin will be
massaged at the
bony prominences.
11. Bedsheets must be
changed regularly,
kept dry and
wrinkle free
Identification of
problems
Establishment of
Goals (with Time
Frame)
Taking Action
(Nursing management
strategies)
Evaluation
of
Outcomes
Reflection
on process
3. Disturbed
skin
integrity
due to
restricted
mobility
Ensure the
maintenance of
skin integrity by
preventing
development of
pressure injuries
during hospital
stay.
1. Repositioning of
John every four
hours so that
pressure from the
sore can be
relieved (Murphree,
2017)
Maintenanc
e of skin
integrity and
prevention
of
occurrence
of pressure
injury
I learnt
several
methods
apart from
repositioning
which can be
used to
prevent
pressure
injury
3. Nurse will apply
moisturiser if any
region of the body
gets reddened
5. Bathing daily for
skin hygiene and
ensure circulation
of blood flow
7. Pressure relieving
aids such as foams
or air mattress can
be used
9. Skin will be
massaged at the
bony prominences.
11. Bedsheets must be
changed regularly,
kept dry and
wrinkle free

Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Potential problem 1
Identification of
problems
Establishment of
Goals (with Time
Frame)
Taking Action
(Nursing management
strategies)
Evaluation
of
Outcomes
Reflection
on process
1. Risk of
mental
distress
which may
lead to
depression
(Ohrnberger
, Fichera, &
Sutton,
2017)
Ensure his mental
status is healthy
by keeping him
engaged and
assuring that he is
recovering
gradually
1. Since his short
term memory is
intact, he must be
oriented to
environment so
that he feels
involved.
He never
seemed
distress
during the
hospital
stay except
only at
times of
physical
issues.
I learnt that
mental
health may
not show its
visible signs
at early
stage but it
should be
included in
care plans
especially if
dealing with
elderly
patients.
2. He must be given
appropriate
amount of freedom
to move.
5. Regular
psychoanalysis
7. He must be
positive feedbacks
when he shows
progress even if
minor
9. Nurse must
develop a
relationship with
John so that he is
comfortable in
communicating his
issues
11. Family members
Identification of
problems
Establishment of
Goals (with Time
Frame)
Taking Action
(Nursing management
strategies)
Evaluation
of
Outcomes
Reflection
on process
1. Risk of
mental
distress
which may
lead to
depression
(Ohrnberger
, Fichera, &
Sutton,
2017)
Ensure his mental
status is healthy
by keeping him
engaged and
assuring that he is
recovering
gradually
1. Since his short
term memory is
intact, he must be
oriented to
environment so
that he feels
involved.
He never
seemed
distress
during the
hospital
stay except
only at
times of
physical
issues.
I learnt that
mental
health may
not show its
visible signs
at early
stage but it
should be
included in
care plans
especially if
dealing with
elderly
patients.
2. He must be given
appropriate
amount of freedom
to move.
5. Regular
psychoanalysis
7. He must be
positive feedbacks
when he shows
progress even if
minor
9. Nurse must
develop a
relationship with
John so that he is
comfortable in
communicating his
issues
11. Family members

can be called to
pay visits
pay visits
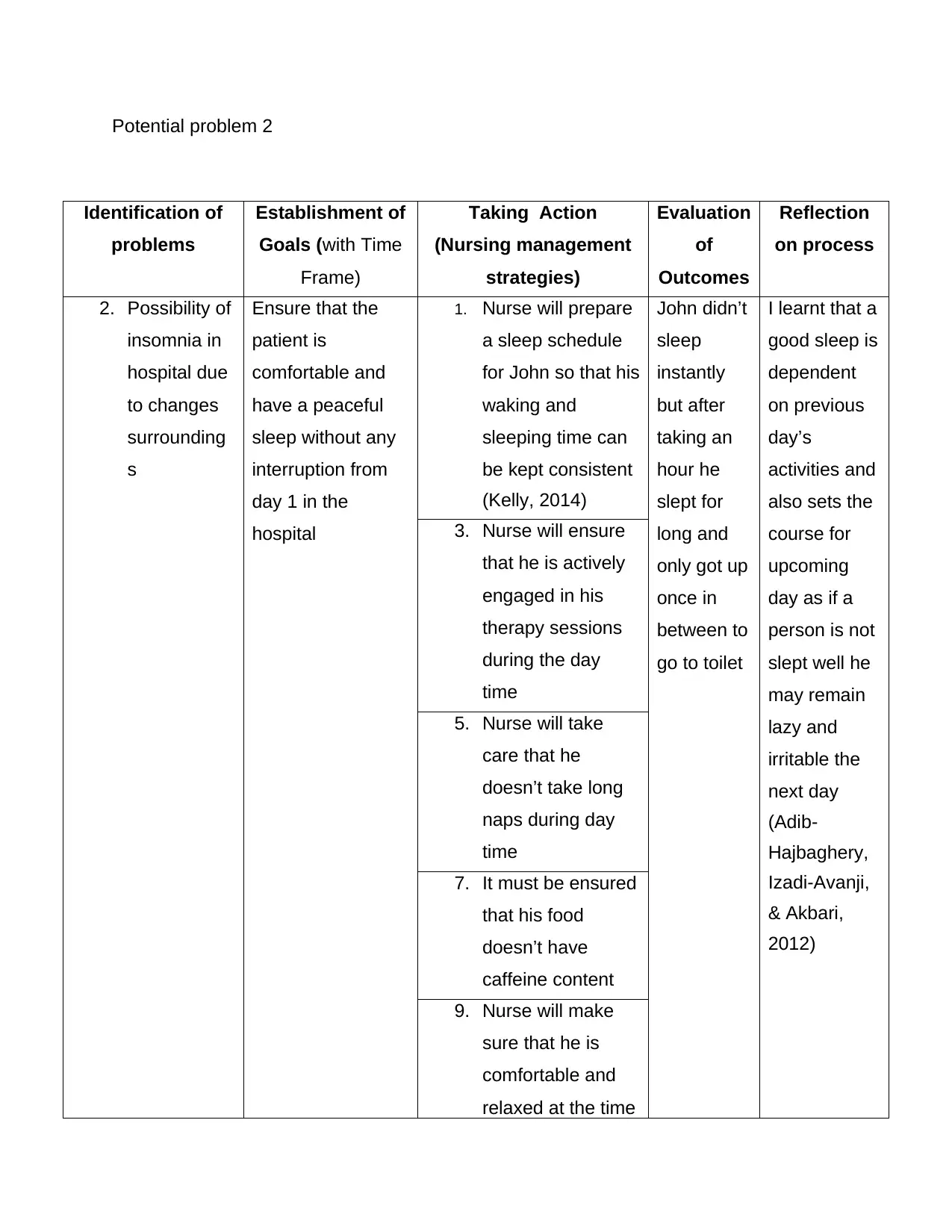
Potential problem 2
Identification of
problems
Establishment of
Goals (with Time
Frame)
Taking Action
(Nursing management
strategies)
Evaluation
of
Outcomes
Reflection
on process
2. Possibility of
insomnia in
hospital due
to changes
surrounding
s
Ensure that the
patient is
comfortable and
have a peaceful
sleep without any
interruption from
day 1 in the
hospital
1. Nurse will prepare
a sleep schedule
for John so that his
waking and
sleeping time can
be kept consistent
(Kelly, 2014)
John didn’t
sleep
instantly
but after
taking an
hour he
slept for
long and
only got up
once in
between to
go to toilet
I learnt that a
good sleep is
dependent
on previous
day’s
activities and
also sets the
course for
upcoming
day as if a
person is not
slept well he
may remain
lazy and
irritable the
next day
(Adib-
Hajbaghery,
Izadi-Avanji,
& Akbari,
2012)
3. Nurse will ensure
that he is actively
engaged in his
therapy sessions
during the day
time
5. Nurse will take
care that he
doesn’t take long
naps during day
time
7. It must be ensured
that his food
doesn’t have
caffeine content
9. Nurse will make
sure that he is
comfortable and
relaxed at the time
Identification of
problems
Establishment of
Goals (with Time
Frame)
Taking Action
(Nursing management
strategies)
Evaluation
of
Outcomes
Reflection
on process
2. Possibility of
insomnia in
hospital due
to changes
surrounding
s
Ensure that the
patient is
comfortable and
have a peaceful
sleep without any
interruption from
day 1 in the
hospital
1. Nurse will prepare
a sleep schedule
for John so that his
waking and
sleeping time can
be kept consistent
(Kelly, 2014)
John didn’t
sleep
instantly
but after
taking an
hour he
slept for
long and
only got up
once in
between to
go to toilet
I learnt that a
good sleep is
dependent
on previous
day’s
activities and
also sets the
course for
upcoming
day as if a
person is not
slept well he
may remain
lazy and
irritable the
next day
(Adib-
Hajbaghery,
Izadi-Avanji,
& Akbari,
2012)
3. Nurse will ensure
that he is actively
engaged in his
therapy sessions
during the day
time
5. Nurse will take
care that he
doesn’t take long
naps during day
time
7. It must be ensured
that his food
doesn’t have
caffeine content
9. Nurse will make
sure that he is
comfortable and
relaxed at the time
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

of going to bed
and is done with
toileting activities
11. Nurse will make
sure that John’s
room is dark and
quiet with
adequate
temperature
maintenance
(DuBose & Hadi,
2016)
References
Adib-Hajbaghery, M., Izadi-Avanji, F., & Akbari, H. (2012). Quality of sleep and its
related risk factors in hospitalized older patients in Kashan’s Hospitals, Iran 2009.
Iran J Nurs Midwifery Res, 17(6), 414-420.
DuBose, J. R., & Hadi, K. (2016). Improving inpatient environments to support patient
sleep. International Journal for Quality in Health Care, 28(5), 54-553.
Heerema, E. (2018, August 17). Dementia Effects on Activities of Daily Living (ADLs).
Retrieved from Verywell Health: https://www.verywellhealth.com/dementia-daily-
living-adls-97635
Kelly, J. (2014). Insomnia treatment for the medically ill hospitalized patient. Mental
Health Clinician, 4(2), 82-90.
Laver, dyer, Whitehead, & Clemson. (2016). Interventions to delay functional decline in
people with dementia: a systematic review of systematic reviews. BMJ, 6.
Murphree. (2017). Impairments in Skin Integrity. Nurs Clin North Am, 52(3), 405-417.
Ohrnberger, J., Fichera, E., & Sutton, M. (2017). The relationship between physical and
mental health: A mediation analysis. Social Science & Medicine, 195, 42-49.
and is done with
toileting activities
11. Nurse will make
sure that John’s
room is dark and
quiet with
adequate
temperature
maintenance
(DuBose & Hadi,
2016)
References
Adib-Hajbaghery, M., Izadi-Avanji, F., & Akbari, H. (2012). Quality of sleep and its
related risk factors in hospitalized older patients in Kashan’s Hospitals, Iran 2009.
Iran J Nurs Midwifery Res, 17(6), 414-420.
DuBose, J. R., & Hadi, K. (2016). Improving inpatient environments to support patient
sleep. International Journal for Quality in Health Care, 28(5), 54-553.
Heerema, E. (2018, August 17). Dementia Effects on Activities of Daily Living (ADLs).
Retrieved from Verywell Health: https://www.verywellhealth.com/dementia-daily-
living-adls-97635
Kelly, J. (2014). Insomnia treatment for the medically ill hospitalized patient. Mental
Health Clinician, 4(2), 82-90.
Laver, dyer, Whitehead, & Clemson. (2016). Interventions to delay functional decline in
people with dementia: a systematic review of systematic reviews. BMJ, 6.
Murphree. (2017). Impairments in Skin Integrity. Nurs Clin North Am, 52(3), 405-417.
Ohrnberger, J., Fichera, E., & Sutton, M. (2017). The relationship between physical and
mental health: A mediation analysis. Social Science & Medicine, 195, 42-49.

Vonnes, & Wolf. (2017). Fall risk and prevention agreement: engaging patients and
families with a partnership for patient safety. BMJ Open Qual , 6.
Williams, K., & Kemper, S. (2010). Exploring Interventions to Reduce Cognitive Decline
in Aging. J Psychosoc Nurs Ment Health Serv, 48(5), 42-51.
Williams, M. E. (2016, November 1). How Aging Affects Our Memory. Retrieved 2019,
from Psychology Today: https://www.psychologytoday.com/us/blog/the-art-and-
science-aging-well/201611/how-aging-affects-our-memory
families with a partnership for patient safety. BMJ Open Qual , 6.
Williams, K., & Kemper, S. (2010). Exploring Interventions to Reduce Cognitive Decline
in Aging. J Psychosoc Nurs Ment Health Serv, 48(5), 42-51.
Williams, M. E. (2016, November 1). How Aging Affects Our Memory. Retrieved 2019,
from Psychology Today: https://www.psychologytoday.com/us/blog/the-art-and-
science-aging-well/201611/how-aging-affects-our-memory
1 out of 18
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





