University Report: Pathophysiology, Risk Factors of Ependymoma Cancer
VerifiedAdded on 2023/06/07
|10
|2360
|69
Report
AI Summary
This report provides a detailed analysis of ependymoma cancer, a tumor originating from the ependyma, often affecting the central nervous system. The report begins with an introduction to ependymoma, its prevalence in pediatric cases, and its common location in the fourth ventricle. A case study of an infant with ependymoma is presented, focusing on the pathophysiology, which involves hydrocephalus due to the tumor's location and its impact on cerebrospinal fluid flow. The report outlines predisposing factors like age, gender, and race, alongside precipitating factors such as hydrocephalus and the tumor itself. The document also discusses statistical data on ependymoma incidence, survival rates, and treatment modalities like chemotherapy and surgical interventions, supported by relevant references. Furthermore, it highlights the challenges in vascular access for infants undergoing treatment and the need for oxygen support. The conclusion summarizes the key findings, emphasizing the importance of early diagnosis and multidisciplinary approaches in managing this challenging form of cancer.

Running head: PATHOPHYSIOLOGY OF EPENDYMOMA CANCER
PATHOPHYSIOLOGY OF EPENDYMOMA CANCER
Name of the Student
Name of the University
Author Note
PATHOPHYSIOLOGY OF EPENDYMOMA CANCER
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1PATHOPHYSIOLOGY OF EPENDYMOMA CANCER
Introduction
Ependymoma is a tumour that emerges from the ependyma which is a tissue of the
focal sensory system or the central nervous system. Normally, in paediatric cases the area is
intracranial, while in grown-ups it is spinal. The normal area of intracranial ependymoma is
the fourth ventricle. Once in a while, ependymoma can happen in the pelvic depression as
well. Ependymoma is the third most normal cerebrum tumour in infants or in children,
representing roughly 10% of central nervous system (CNS) neoplasms (Spennato et al. 2015).
It is a neuroepithelial tumour that emerges from inside, or contiguous to the ependymal
coating of the ventricular framework or the central canal of the spinal cord (Nichtweiß 2015).
The following part of the essay will describe about a case study which mainly focuses on a
baby who has ependymoma cancer or had gone through several operations. Alongside the
pathophysiology, risk factors and the precipitating factors are discussed in a table format.
Introduction
Ependymoma is a tumour that emerges from the ependyma which is a tissue of the
focal sensory system or the central nervous system. Normally, in paediatric cases the area is
intracranial, while in grown-ups it is spinal. The normal area of intracranial ependymoma is
the fourth ventricle. Once in a while, ependymoma can happen in the pelvic depression as
well. Ependymoma is the third most normal cerebrum tumour in infants or in children,
representing roughly 10% of central nervous system (CNS) neoplasms (Spennato et al. 2015).
It is a neuroepithelial tumour that emerges from inside, or contiguous to the ependymal
coating of the ventricular framework or the central canal of the spinal cord (Nichtweiß 2015).
The following part of the essay will describe about a case study which mainly focuses on a
baby who has ependymoma cancer or had gone through several operations. Alongside the
pathophysiology, risk factors and the precipitating factors are discussed in a table format.
2PATHOPHYSIOLOGY OF EPENDYMOMA CANCER
Predisposing factors
Age- Age is one of the factors that
cause ependymoma cancer.
Etiology (Cause of
ependymoma is still not
known clearly)
Precipitating
factors:
Ependymoma,
Hydrocephalus
Predisposing factors
Age- Age is one of the factors that
cause ependymoma cancer.
Etiology (Cause of
ependymoma is still not
known clearly)
Precipitating
factors:
Ependymoma,
Hydrocephalus
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

3PATHOPHYSIOLOGY OF EPENDYMOMA CANCER
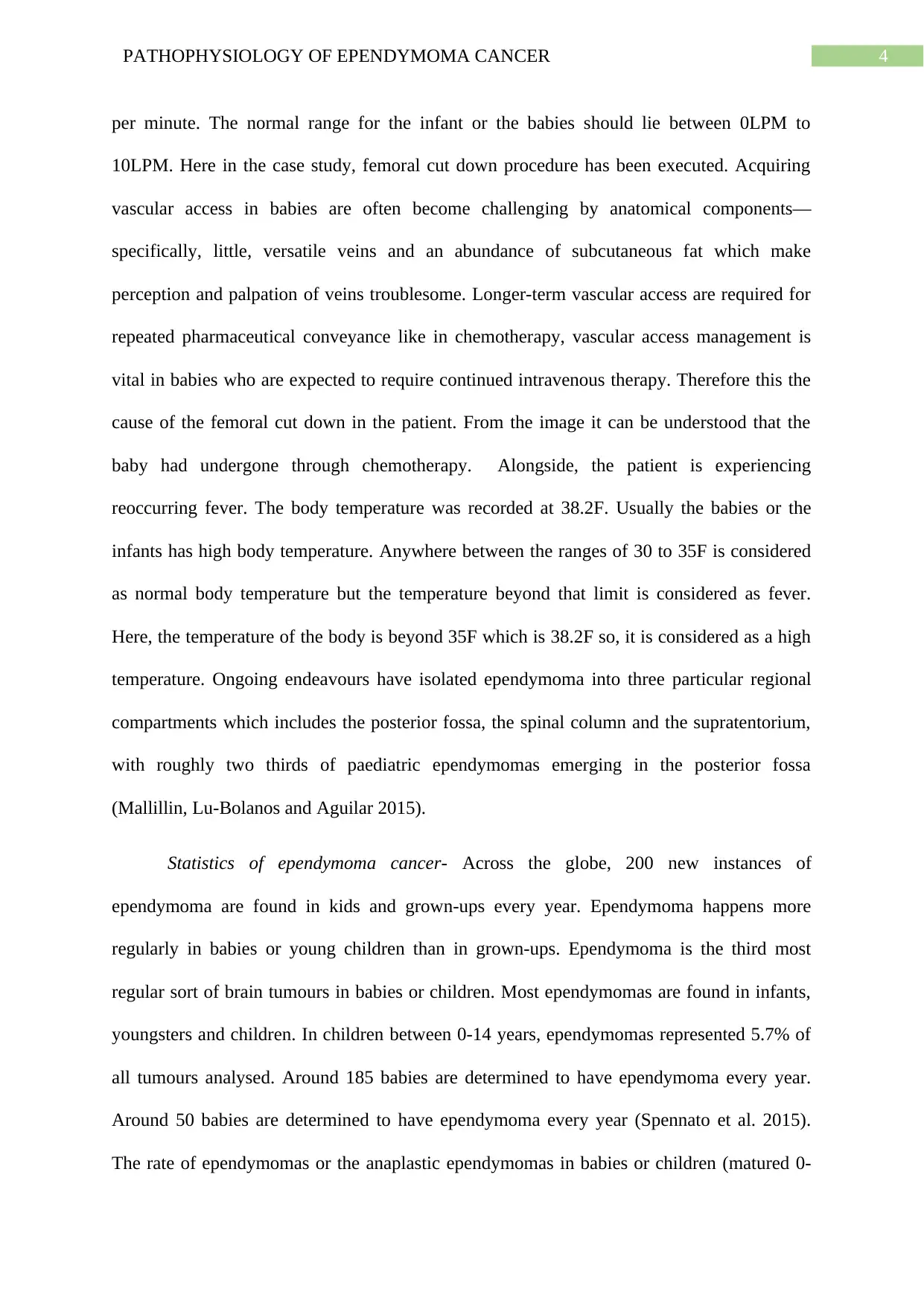
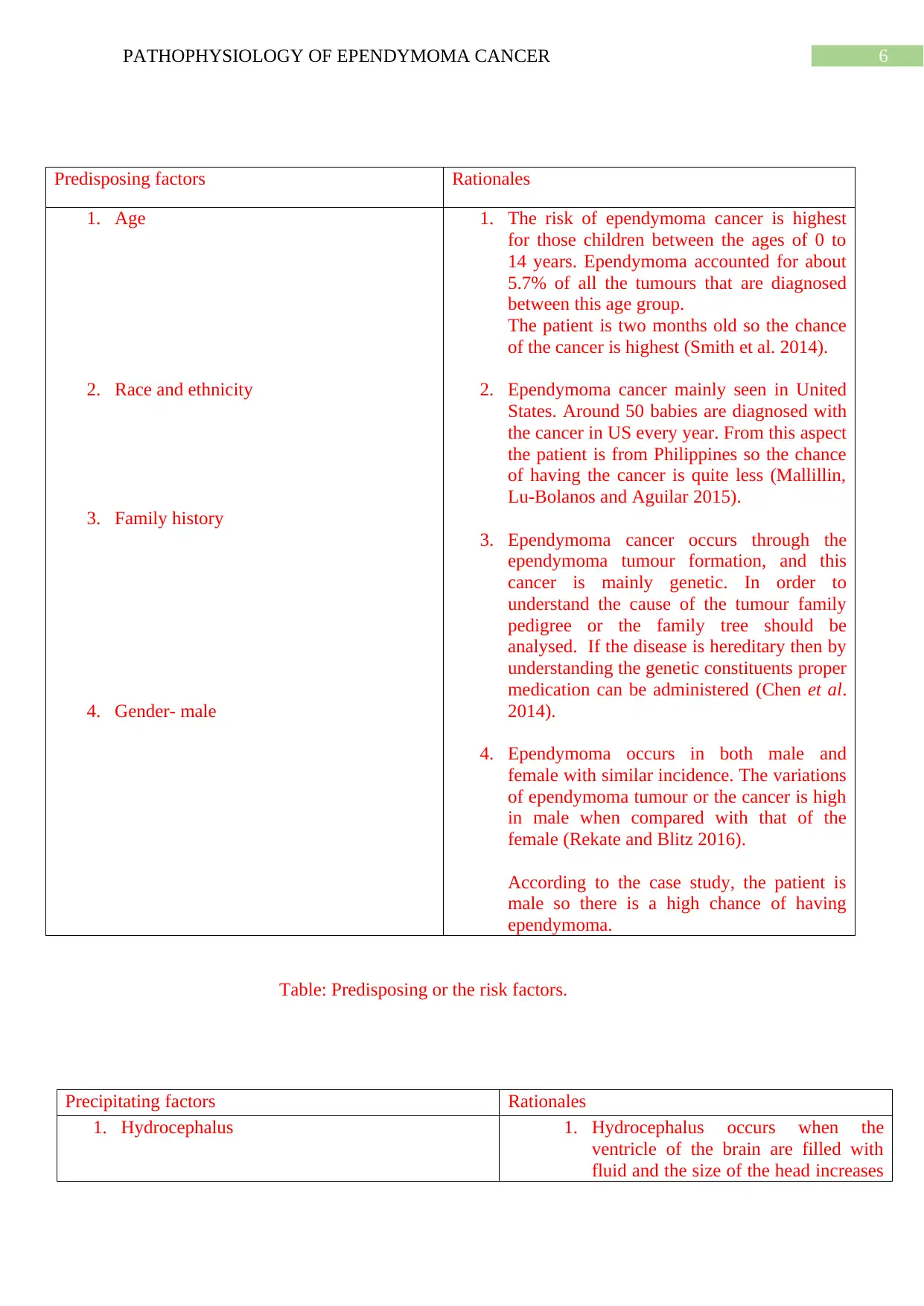
The above diagram is the pathophysiology of the ependymoma cancer.
Pathophysiology of the ependymoma cancer- Pathophysiology of the ependymoma
cancer- According to the case study and the above image the patient is having ependymoma.
Ependymoma can occur in anyplace in the liquid - filled ventricles and ways in the junction
between the spinal cord and the cerebrum. Usually the ependymomas occur in the fourth
ventricle and influence the cerebellum and the mind stem and from the image it can be
understood that the tumour has formed in the left portion of the brain (Rekate and Blitz 2016.
Due to this ependymoma the patient is dealing with hydrocephalus which can be clearly
understood from the image. Hydrocephalus is a condition in the brain which occurs when
cerebrospinal liquid (CSF) which is watery liquid that accumulates around the cerebrum and
spinal line. The fluid cannot be reduced from the cerebrum. Due to this there is a
development of fluid in the brain or in the ventricles. Hydrocephalus (likewise called "water
on the mind") can make children and the infants’ head swell due to the accumulation of
abundance liquid (Kahle et al. 2016). This has happened to the patient in the case study and
accordingly due to this, it is important to remove the liquid from the brain by surgical
procedure. According to the case study the patient had undergone ten times surgeries on his
head and there is a scar mark on his head. Baby having hydrocephalus will seem to have a
strangely shaped head and the head is normally much bigger than the other babies of same
age. The symptoms and the signs of the childhood ependymoma is different for the different
child. According to the case study the baby has not able to respond to the intake of medicines.
The patient is provided with a naso gastric tube or NGT. These tubes are useful to provide the
medicines and the feedings in the stomach. The other reasons for incorporation of naso
gastric tube includes the irregular weight gains or lack of weight gain patterns. The patient is
not able to breathe properly and he has a lot of problems in inhaling and exhaling. According
to the case study the patient is provided with 5LPM which is equivalent to 5 litres of oxygen
Ependymoma cancer
forms from
ependymoma tumour.
Develop from precursor
cell
Precursor cell line are
forms adjacent to the
ventricles in the brain
Fluid when increases in the brain
causes hydrocephalus.
(Enlargement of ventricles)
The tumour can cause anywhere in
the brain and spinal cord. In baby it
cause in the brain and blocks the flow
of cerebrospinal fluid.
Blockage of the fluid can cause the
tumour formation and removal is
done through surgical procedures.
The tumour can occur in repeated times in the
same position. If someone is having
ependymoma tumour then he or she will have
ependymoma cancer. The clinicians and the
doctors are still investigating on the main causes
of the cancer.
Chemotherapy is required for the patient
having ependymoma cancer. It may be a
relevant solution for the cancer.
The above diagram is the pathophysiology of the ependymoma cancer.
Pathophysiology of the ependymoma cancer- Pathophysiology of the ependymoma
cancer- According to the case study and the above image the patient is having ependymoma.
Ependymoma can occur in anyplace in the liquid - filled ventricles and ways in the junction
between the spinal cord and the cerebrum. Usually the ependymomas occur in the fourth
ventricle and influence the cerebellum and the mind stem and from the image it can be
understood that the tumour has formed in the left portion of the brain (Rekate and Blitz 2016.
Due to this ependymoma the patient is dealing with hydrocephalus which can be clearly
understood from the image. Hydrocephalus is a condition in the brain which occurs when
cerebrospinal liquid (CSF) which is watery liquid that accumulates around the cerebrum and
spinal line. The fluid cannot be reduced from the cerebrum. Due to this there is a
development of fluid in the brain or in the ventricles. Hydrocephalus (likewise called "water
on the mind") can make children and the infants’ head swell due to the accumulation of
abundance liquid (Kahle et al. 2016). This has happened to the patient in the case study and
accordingly due to this, it is important to remove the liquid from the brain by surgical
procedure. According to the case study the patient had undergone ten times surgeries on his
head and there is a scar mark on his head. Baby having hydrocephalus will seem to have a
strangely shaped head and the head is normally much bigger than the other babies of same
age. The symptoms and the signs of the childhood ependymoma is different for the different
child. According to the case study the baby has not able to respond to the intake of medicines.
The patient is provided with a naso gastric tube or NGT. These tubes are useful to provide the
medicines and the feedings in the stomach. The other reasons for incorporation of naso
gastric tube includes the irregular weight gains or lack of weight gain patterns. The patient is
not able to breathe properly and he has a lot of problems in inhaling and exhaling. According
to the case study the patient is provided with 5LPM which is equivalent to 5 litres of oxygen
Ependymoma cancer
forms from
ependymoma tumour.
Develop from precursor
cell
Precursor cell line are
forms adjacent to the
ventricles in the brain
Fluid when increases in the brain
causes hydrocephalus.
(Enlargement of ventricles)
The tumour can cause anywhere in
the brain and spinal cord. In baby it
cause in the brain and blocks the flow
of cerebrospinal fluid.
Blockage of the fluid can cause the
tumour formation and removal is
done through surgical procedures.
The tumour can occur in repeated times in the
same position. If someone is having
ependymoma tumour then he or she will have
ependymoma cancer. The clinicians and the
doctors are still investigating on the main causes
of the cancer.
Chemotherapy is required for the patient
having ependymoma cancer. It may be a
relevant solution for the cancer.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4PATHOPHYSIOLOGY OF EPENDYMOMA CANCER
per minute. The normal range for the infant or the babies should lie between 0LPM to
10LPM. Here in the case study, femoral cut down procedure has been executed. Acquiring
vascular access in babies are often become challenging by anatomical components—
specifically, little, versatile veins and an abundance of subcutaneous fat which make
perception and palpation of veins troublesome. Longer-term vascular access are required for
repeated pharmaceutical conveyance like in chemotherapy, vascular access management is
vital in babies who are expected to require continued intravenous therapy. Therefore this the
cause of the femoral cut down in the patient. From the image it can be understood that the
baby had undergone through chemotherapy. Alongside, the patient is experiencing
reoccurring fever. The body temperature was recorded at 38.2F. Usually the babies or the
infants has high body temperature. Anywhere between the ranges of 30 to 35F is considered
as normal body temperature but the temperature beyond that limit is considered as fever.
Here, the temperature of the body is beyond 35F which is 38.2F so, it is considered as a high
temperature. Ongoing endeavours have isolated ependymoma into three particular regional
compartments which includes the posterior fossa, the spinal column and the supratentorium,
with roughly two thirds of paediatric ependymomas emerging in the posterior fossa
(Mallillin, Lu-Bolanos and Aguilar 2015).
Statistics of ependymoma cancer- Across the globe, 200 new instances of
ependymoma are found in kids and grown-ups every year. Ependymoma happens more
regularly in babies or young children than in grown-ups. Ependymoma is the third most
regular sort of brain tumours in babies or children. Most ependymomas are found in infants,
youngsters and children. In children between 0-14 years, ependymomas represented 5.7% of
all tumours analysed. Around 185 babies are determined to have ependymoma every year.
Around 50 babies are determined to have ependymoma every year (Spennato et al. 2015).
The rate of ependymomas or the anaplastic ependymomas in babies or children (matured 0-
per minute. The normal range for the infant or the babies should lie between 0LPM to
10LPM. Here in the case study, femoral cut down procedure has been executed. Acquiring
vascular access in babies are often become challenging by anatomical components—
specifically, little, versatile veins and an abundance of subcutaneous fat which make
perception and palpation of veins troublesome. Longer-term vascular access are required for
repeated pharmaceutical conveyance like in chemotherapy, vascular access management is
vital in babies who are expected to require continued intravenous therapy. Therefore this the
cause of the femoral cut down in the patient. From the image it can be understood that the
baby had undergone through chemotherapy. Alongside, the patient is experiencing
reoccurring fever. The body temperature was recorded at 38.2F. Usually the babies or the
infants has high body temperature. Anywhere between the ranges of 30 to 35F is considered
as normal body temperature but the temperature beyond that limit is considered as fever.
Here, the temperature of the body is beyond 35F which is 38.2F so, it is considered as a high
temperature. Ongoing endeavours have isolated ependymoma into three particular regional
compartments which includes the posterior fossa, the spinal column and the supratentorium,
with roughly two thirds of paediatric ependymomas emerging in the posterior fossa
(Mallillin, Lu-Bolanos and Aguilar 2015).
Statistics of ependymoma cancer- Across the globe, 200 new instances of
ependymoma are found in kids and grown-ups every year. Ependymoma happens more
regularly in babies or young children than in grown-ups. Ependymoma is the third most
regular sort of brain tumours in babies or children. Most ependymomas are found in infants,
youngsters and children. In children between 0-14 years, ependymomas represented 5.7% of
all tumours analysed. Around 185 babies are determined to have ependymoma every year.
Around 50 babies are determined to have ependymoma every year (Spennato et al. 2015).
The rate of ependymomas or the anaplastic ependymomas in babies or children (matured 0-
5PATHOPHYSIOLOGY OF EPENDYMOMA CANCER
19 years) was similar in guys and females. The rate of ependymoma variations is higher in
guys than females. Ependymoma is the most common type of primary spinal cord tumour
which mainly occurs in the infants, babies or young children. The general five-year survival
rate for those with ependymoma is around 82 percent. For children up to 19 years old, the
five-year survival rate is around 72 percent.
In advanced country like Philippines ependymoma tumour is more prevalent than that
of the previous years. Two thirds of the young children or the babies in Philippines are
diagnosed with cancer and the most common type of cancer which occurred include the
ependymoma cancer. In Philippines 3% of the ependymoma cancer occurs at below four
years of age. It is recorded that for every 1800 people of Philippines one will develop
ependymoma cancer annually. Child mortality is very high due to the ependymoma cancer in
Philippines. It is an unfortunate for the people of Philippines that though multi-disciplinary
organisation is accessible and could cure 80% of the cancer cases only about 10% to 20%
actually achieves long-term existence (Smith et al. 2014).
.
19 years) was similar in guys and females. The rate of ependymoma variations is higher in
guys than females. Ependymoma is the most common type of primary spinal cord tumour
which mainly occurs in the infants, babies or young children. The general five-year survival
rate for those with ependymoma is around 82 percent. For children up to 19 years old, the
five-year survival rate is around 72 percent.
In advanced country like Philippines ependymoma tumour is more prevalent than that
of the previous years. Two thirds of the young children or the babies in Philippines are
diagnosed with cancer and the most common type of cancer which occurred include the
ependymoma cancer. In Philippines 3% of the ependymoma cancer occurs at below four
years of age. It is recorded that for every 1800 people of Philippines one will develop
ependymoma cancer annually. Child mortality is very high due to the ependymoma cancer in
Philippines. It is an unfortunate for the people of Philippines that though multi-disciplinary
organisation is accessible and could cure 80% of the cancer cases only about 10% to 20%
actually achieves long-term existence (Smith et al. 2014).
.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6PATHOPHYSIOLOGY OF EPENDYMOMA CANCER
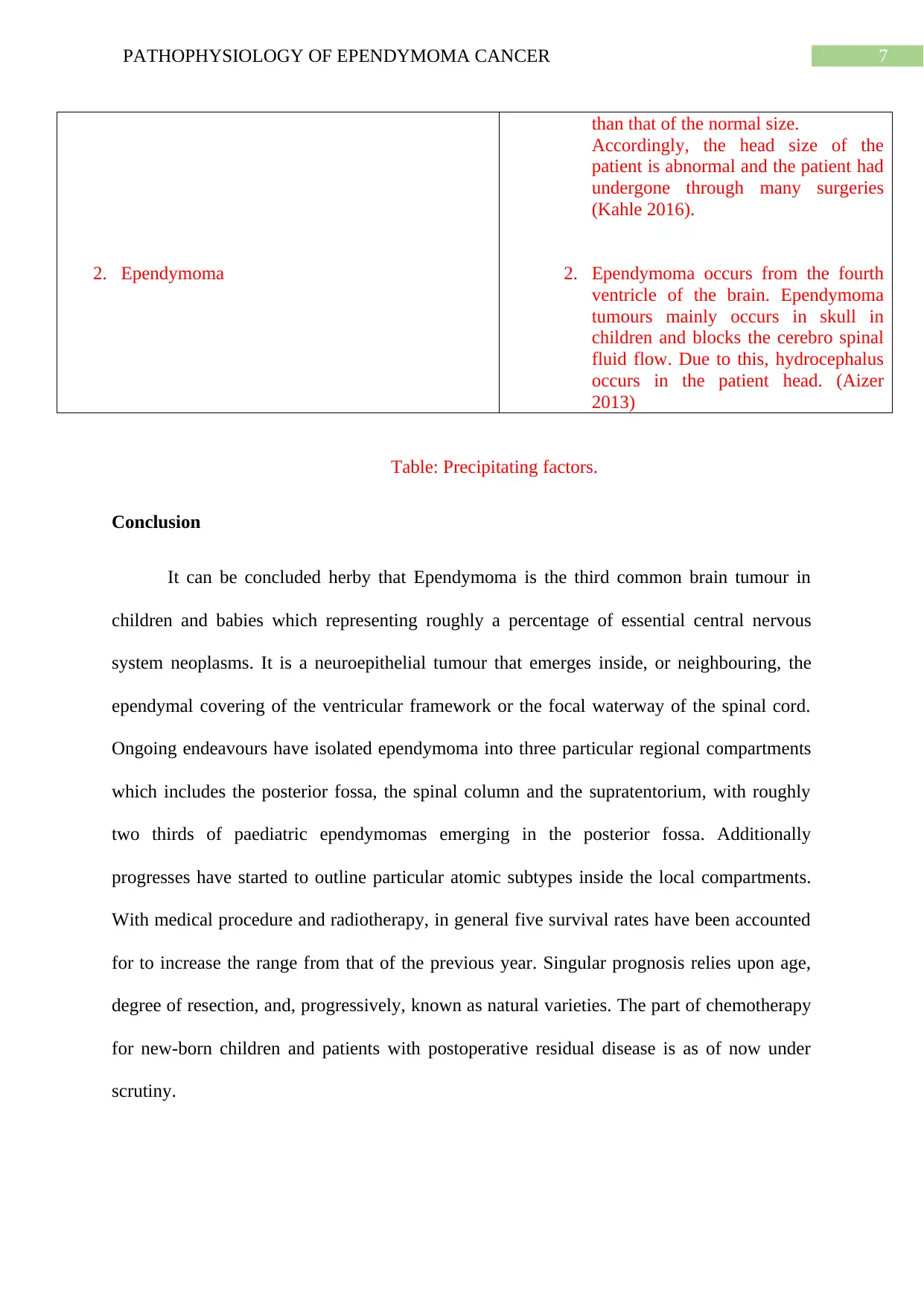
Predisposing factors Rationales
1. Age
2. Race and ethnicity
3. Family history
4. Gender- male
1. The risk of ependymoma cancer is highest
for those children between the ages of 0 to
14 years. Ependymoma accounted for about
5.7% of all the tumours that are diagnosed
between this age group.
The patient is two months old so the chance
of the cancer is highest (Smith et al. 2014).
2. Ependymoma cancer mainly seen in United
States. Around 50 babies are diagnosed with
the cancer in US every year. From this aspect
the patient is from Philippines so the chance
of having the cancer is quite less (Mallillin,
Lu-Bolanos and Aguilar 2015).
3. Ependymoma cancer occurs through the
ependymoma tumour formation, and this
cancer is mainly genetic. In order to
understand the cause of the tumour family
pedigree or the family tree should be
analysed. If the disease is hereditary then by
understanding the genetic constituents proper
medication can be administered (Chen et al.
2014).
4. Ependymoma occurs in both male and
female with similar incidence. The variations
of ependymoma tumour or the cancer is high
in male when compared with that of the
female (Rekate and Blitz 2016).
According to the case study, the patient is
male so there is a high chance of having
ependymoma.
Table: Predisposing or the risk factors.
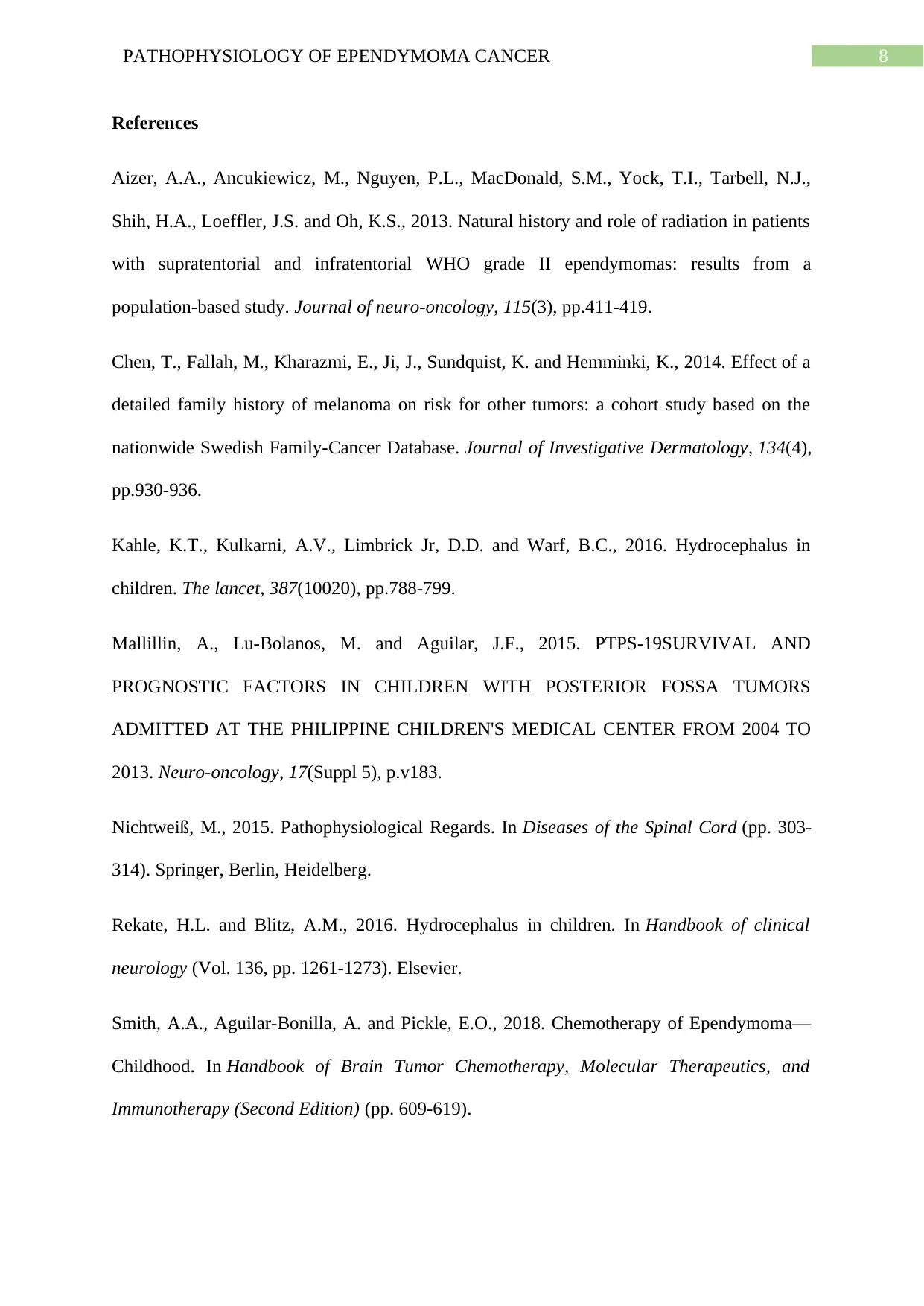
Precipitating factors Rationales
1. Hydrocephalus 1. Hydrocephalus occurs when the
ventricle of the brain are filled with
fluid and the size of the head increases
Predisposing factors Rationales
1. Age
2. Race and ethnicity
3. Family history
4. Gender- male
1. The risk of ependymoma cancer is highest
for those children between the ages of 0 to
14 years. Ependymoma accounted for about
5.7% of all the tumours that are diagnosed
between this age group.
The patient is two months old so the chance
of the cancer is highest (Smith et al. 2014).
2. Ependymoma cancer mainly seen in United
States. Around 50 babies are diagnosed with
the cancer in US every year. From this aspect
the patient is from Philippines so the chance
of having the cancer is quite less (Mallillin,
Lu-Bolanos and Aguilar 2015).
3. Ependymoma cancer occurs through the
ependymoma tumour formation, and this
cancer is mainly genetic. In order to
understand the cause of the tumour family
pedigree or the family tree should be
analysed. If the disease is hereditary then by
understanding the genetic constituents proper
medication can be administered (Chen et al.
2014).
4. Ependymoma occurs in both male and
female with similar incidence. The variations
of ependymoma tumour or the cancer is high
in male when compared with that of the
female (Rekate and Blitz 2016).
According to the case study, the patient is
male so there is a high chance of having
ependymoma.
Table: Predisposing or the risk factors.
Precipitating factors Rationales
1. Hydrocephalus 1. Hydrocephalus occurs when the
ventricle of the brain are filled with
fluid and the size of the head increases
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7PATHOPHYSIOLOGY OF EPENDYMOMA CANCER
2. Ependymoma
than that of the normal size.
Accordingly, the head size of the
patient is abnormal and the patient had
undergone through many surgeries
(Kahle 2016).
2. Ependymoma occurs from the fourth
ventricle of the brain. Ependymoma
tumours mainly occurs in skull in
children and blocks the cerebro spinal
fluid flow. Due to this, hydrocephalus
occurs in the patient head. (Aizer
2013)
Table: Precipitating factors.
Conclusion
It can be concluded herby that Ependymoma is the third common brain tumour in
children and babies which representing roughly a percentage of essential central nervous
system neoplasms. It is a neuroepithelial tumour that emerges inside, or neighbouring, the
ependymal covering of the ventricular framework or the focal waterway of the spinal cord.
Ongoing endeavours have isolated ependymoma into three particular regional compartments
which includes the posterior fossa, the spinal column and the supratentorium, with roughly
two thirds of paediatric ependymomas emerging in the posterior fossa. Additionally
progresses have started to outline particular atomic subtypes inside the local compartments.
With medical procedure and radiotherapy, in general five survival rates have been accounted
for to increase the range from that of the previous year. Singular prognosis relies upon age,
degree of resection, and, progressively, known as natural varieties. The part of chemotherapy
for new-born children and patients with postoperative residual disease is as of now under
scrutiny.
2. Ependymoma
than that of the normal size.
Accordingly, the head size of the
patient is abnormal and the patient had
undergone through many surgeries
(Kahle 2016).
2. Ependymoma occurs from the fourth
ventricle of the brain. Ependymoma
tumours mainly occurs in skull in
children and blocks the cerebro spinal
fluid flow. Due to this, hydrocephalus
occurs in the patient head. (Aizer
2013)
Table: Precipitating factors.
Conclusion
It can be concluded herby that Ependymoma is the third common brain tumour in
children and babies which representing roughly a percentage of essential central nervous
system neoplasms. It is a neuroepithelial tumour that emerges inside, or neighbouring, the
ependymal covering of the ventricular framework or the focal waterway of the spinal cord.
Ongoing endeavours have isolated ependymoma into three particular regional compartments
which includes the posterior fossa, the spinal column and the supratentorium, with roughly
two thirds of paediatric ependymomas emerging in the posterior fossa. Additionally
progresses have started to outline particular atomic subtypes inside the local compartments.
With medical procedure and radiotherapy, in general five survival rates have been accounted
for to increase the range from that of the previous year. Singular prognosis relies upon age,
degree of resection, and, progressively, known as natural varieties. The part of chemotherapy
for new-born children and patients with postoperative residual disease is as of now under
scrutiny.
8PATHOPHYSIOLOGY OF EPENDYMOMA CANCER
References
Aizer, A.A., Ancukiewicz, M., Nguyen, P.L., MacDonald, S.M., Yock, T.I., Tarbell, N.J.,
Shih, H.A., Loeffler, J.S. and Oh, K.S., 2013. Natural history and role of radiation in patients
with supratentorial and infratentorial WHO grade II ependymomas: results from a
population-based study. Journal of neuro-oncology, 115(3), pp.411-419.
Chen, T., Fallah, M., Kharazmi, E., Ji, J., Sundquist, K. and Hemminki, K., 2014. Effect of a
detailed family history of melanoma on risk for other tumors: a cohort study based on the
nationwide Swedish Family-Cancer Database. Journal of Investigative Dermatology, 134(4),
pp.930-936.
Kahle, K.T., Kulkarni, A.V., Limbrick Jr, D.D. and Warf, B.C., 2016. Hydrocephalus in
children. The lancet, 387(10020), pp.788-799.
Mallillin, A., Lu-Bolanos, M. and Aguilar, J.F., 2015. PTPS-19SURVIVAL AND
PROGNOSTIC FACTORS IN CHILDREN WITH POSTERIOR FOSSA TUMORS
ADMITTED AT THE PHILIPPINE CHILDREN'S MEDICAL CENTER FROM 2004 TO
2013. Neuro-oncology, 17(Suppl 5), p.v183.
Nichtweiß, M., 2015. Pathophysiological Regards. In Diseases of the Spinal Cord (pp. 303-
314). Springer, Berlin, Heidelberg.
Rekate, H.L. and Blitz, A.M., 2016. Hydrocephalus in children. In Handbook of clinical
neurology (Vol. 136, pp. 1261-1273). Elsevier.
Smith, A.A., Aguilar-Bonilla, A. and Pickle, E.O., 2018. Chemotherapy of Ependymoma—
Childhood. In Handbook of Brain Tumor Chemotherapy, Molecular Therapeutics, and
Immunotherapy (Second Edition) (pp. 609-619).
References
Aizer, A.A., Ancukiewicz, M., Nguyen, P.L., MacDonald, S.M., Yock, T.I., Tarbell, N.J.,
Shih, H.A., Loeffler, J.S. and Oh, K.S., 2013. Natural history and role of radiation in patients
with supratentorial and infratentorial WHO grade II ependymomas: results from a
population-based study. Journal of neuro-oncology, 115(3), pp.411-419.
Chen, T., Fallah, M., Kharazmi, E., Ji, J., Sundquist, K. and Hemminki, K., 2014. Effect of a
detailed family history of melanoma on risk for other tumors: a cohort study based on the
nationwide Swedish Family-Cancer Database. Journal of Investigative Dermatology, 134(4),
pp.930-936.
Kahle, K.T., Kulkarni, A.V., Limbrick Jr, D.D. and Warf, B.C., 2016. Hydrocephalus in
children. The lancet, 387(10020), pp.788-799.
Mallillin, A., Lu-Bolanos, M. and Aguilar, J.F., 2015. PTPS-19SURVIVAL AND
PROGNOSTIC FACTORS IN CHILDREN WITH POSTERIOR FOSSA TUMORS
ADMITTED AT THE PHILIPPINE CHILDREN'S MEDICAL CENTER FROM 2004 TO
2013. Neuro-oncology, 17(Suppl 5), p.v183.
Nichtweiß, M., 2015. Pathophysiological Regards. In Diseases of the Spinal Cord (pp. 303-
314). Springer, Berlin, Heidelberg.
Rekate, H.L. and Blitz, A.M., 2016. Hydrocephalus in children. In Handbook of clinical
neurology (Vol. 136, pp. 1261-1273). Elsevier.
Smith, A.A., Aguilar-Bonilla, A. and Pickle, E.O., 2018. Chemotherapy of Ependymoma—
Childhood. In Handbook of Brain Tumor Chemotherapy, Molecular Therapeutics, and
Immunotherapy (Second Edition) (pp. 609-619).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9PATHOPHYSIOLOGY OF EPENDYMOMA CANCER
Smith, M.A., Altekruse, S.F., Adamson, P.C., Reaman, G.H. and Seibel, N.L., 2014.
Declining childhood and adolescent cancer mortality. Cancer, 120(16), pp.2497-2506.
Spennato, P., Nicosia, G., Quaglietta, L., Donofrio, V., Mirone, G., Di Martino, G.,
Guadagno, E., de Caro, M.L.D.B., Cascone, D. and Cinalli, G., 2015. Posterior fossa tumors
in infants and neonates. Child's Nervous System, 31(10), pp.1751-1772.
Smith, M.A., Altekruse, S.F., Adamson, P.C., Reaman, G.H. and Seibel, N.L., 2014.
Declining childhood and adolescent cancer mortality. Cancer, 120(16), pp.2497-2506.
Spennato, P., Nicosia, G., Quaglietta, L., Donofrio, V., Mirone, G., Di Martino, G.,
Guadagno, E., de Caro, M.L.D.B., Cascone, D. and Cinalli, G., 2015. Posterior fossa tumors
in infants and neonates. Child's Nervous System, 31(10), pp.1751-1772.
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.



