Patient Case Scenario Report: Surgical Ward Patient Care Analysis
VerifiedAdded on 2022/08/19
|15
|3430
|16
Report
AI Summary
This report presents a comprehensive analysis of a patient case scenario involving a 33-year-old male admitted to a surgical ward following a temporary ileostomy due to Crohn's disease. The report delves into the pathophysiology of acute pain, differentiating it from chronic pain, and examines the role of narcotic analgesia, specifically morphine, in pain management. It outlines three crucial nursing assessments: neurovascular, oxygen saturation, and blood pressure, providing rationales for their implementation. The report further explores interventions such as relaxation therapy, oxygen therapy, and the use of Midodrine to address the patient's low blood pressure and oxygen saturation. It details the administration, benefits, risks, contraindications, and patient education related to morphine. Finally, the report discusses the potential side effects of morphine and the importance of mandatory reporting. The case study emphasizes the importance of comprehensive patient care, encompassing both pharmacological and non-pharmacological interventions.

Running head: PATIENT CASE SCENARIO
PATIENT CASE SCENARIO
Name of the student:
Name of the university:
Author note:
PATIENT CASE SCENARIO
Name of the student:
Name of the university:
Author note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1PATIENT CASE SCENARIO
Table of Contents
Introduction:....................................................................................................................................2
Question 1.1:....................................................................................................................................2
Pathophysiology of acute pain:.................................................................................................2
The difference between chronic pain and acute pain:............................................................3
Role of narcotic analgesia in reducing acute pain:.................................................................3
Question 1.2:....................................................................................................................................4
Three types of nursing assessment and rationale for it:........................................................4
Neurovascular assessment (pain):............................................................................................4
Physiological assessment (oxygen saturation):........................................................................4
Physiological assessment ( blood pressure):............................................................................5
Question 1.3:....................................................................................................................................5
Oxygen therapy:.........................................................................................................................6
Midodrine:..................................................................................................................................6
Question 1.4:....................................................................................................................................7
Administration:..........................................................................................................................7
Benefits:......................................................................................................................................7
Patient education:......................................................................................................................8
Question 1.5:....................................................................................................................................9
Side effects of the medication and rationale behind mandatory reporting:.........................9
Conclusion:....................................................................................................................................10
Table of Contents
Introduction:....................................................................................................................................2
Question 1.1:....................................................................................................................................2
Pathophysiology of acute pain:.................................................................................................2
The difference between chronic pain and acute pain:............................................................3
Role of narcotic analgesia in reducing acute pain:.................................................................3
Question 1.2:....................................................................................................................................4
Three types of nursing assessment and rationale for it:........................................................4
Neurovascular assessment (pain):............................................................................................4
Physiological assessment (oxygen saturation):........................................................................4
Physiological assessment ( blood pressure):............................................................................5
Question 1.3:....................................................................................................................................5
Oxygen therapy:.........................................................................................................................6
Midodrine:..................................................................................................................................6
Question 1.4:....................................................................................................................................7
Administration:..........................................................................................................................7
Benefits:......................................................................................................................................7
Patient education:......................................................................................................................8
Question 1.5:....................................................................................................................................9
Side effects of the medication and rationale behind mandatory reporting:.........................9
Conclusion:....................................................................................................................................10
2PATIENT CASE SCENARIO
Introduction:
The purpose of the report is to discuss pathophysiological changes in the
disease .pharmacological management of disease and planned nursing care and evaluation of
care by using a case scenario. The case study involves a 33-year-old, William Tran admitted to
the surgical ward for a temporary ileostomy. The case history suggested that he had a history of
Crohn’s disease and experienced multiple hospitalizations due to Crohns related illnesses
including mal-absorption and weight loss. He had elevated vital signs and administrated with a
range of medication for the management of the disease.
Question 1.1:
Pathophysiology of acute pain:
Acute pain is pain defined as pain with sharp and well-defined onset pain that lasts for
less than 3 to 6. Acute pain usually experienced in response to tissue injury. The common
etiology of the acute pain is nociceptive and inflammatory which disappeared with tissue
healing. When tissue injury recognized within the body, in response to the tissue injury,
peripheral pain receptors along with their specific A-delta as well as C sensory nerve fibers
(nociceptors) activated. Nociceptors are free nerve endings located in skin, bone and other
connective tissues. When tissue injury is encountered, Afferent A-delta and C fibers of periphery
convey the pain stimulus with the assistance of action potentials to the dorsal horn of the spinal
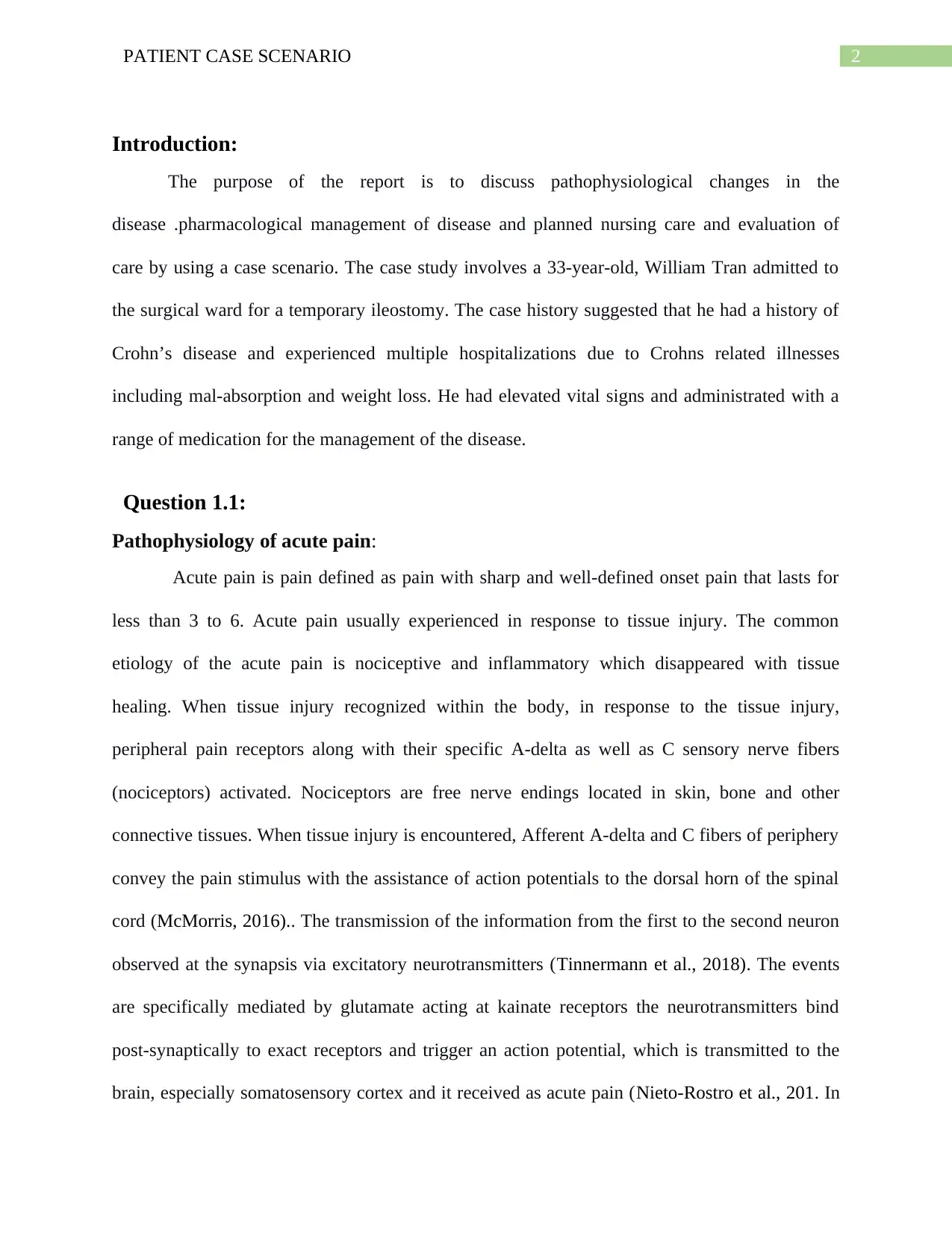
cord (McMorris, 2016).. The transmission of the information from the first to the second neuron
observed at the synapsis via excitatory neurotransmitters (Tinnermann et al., 2018). The events
are specifically mediated by glutamate acting at kainate receptors the neurotransmitters bind
post-synaptically to exact receptors and trigger an action potential, which is transmitted to the
brain, especially somatosensory cortex and it received as acute pain (Nieto-Rostro et al., 201. In
Introduction:
The purpose of the report is to discuss pathophysiological changes in the
disease .pharmacological management of disease and planned nursing care and evaluation of
care by using a case scenario. The case study involves a 33-year-old, William Tran admitted to
the surgical ward for a temporary ileostomy. The case history suggested that he had a history of
Crohn’s disease and experienced multiple hospitalizations due to Crohns related illnesses
including mal-absorption and weight loss. He had elevated vital signs and administrated with a
range of medication for the management of the disease.
Question 1.1:
Pathophysiology of acute pain:
Acute pain is pain defined as pain with sharp and well-defined onset pain that lasts for
less than 3 to 6. Acute pain usually experienced in response to tissue injury. The common
etiology of the acute pain is nociceptive and inflammatory which disappeared with tissue
healing. When tissue injury recognized within the body, in response to the tissue injury,
peripheral pain receptors along with their specific A-delta as well as C sensory nerve fibers
(nociceptors) activated. Nociceptors are free nerve endings located in skin, bone and other
connective tissues. When tissue injury is encountered, Afferent A-delta and C fibers of periphery
convey the pain stimulus with the assistance of action potentials to the dorsal horn of the spinal
cord (McMorris, 2016).. The transmission of the information from the first to the second neuron
observed at the synapsis via excitatory neurotransmitters (Tinnermann et al., 2018). The events
are specifically mediated by glutamate acting at kainate receptors the neurotransmitters bind
post-synaptically to exact receptors and trigger an action potential, which is transmitted to the
brain, especially somatosensory cortex and it received as acute pain (Nieto-Rostro et al., 201. In
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3PATIENT CASE SCENARIO
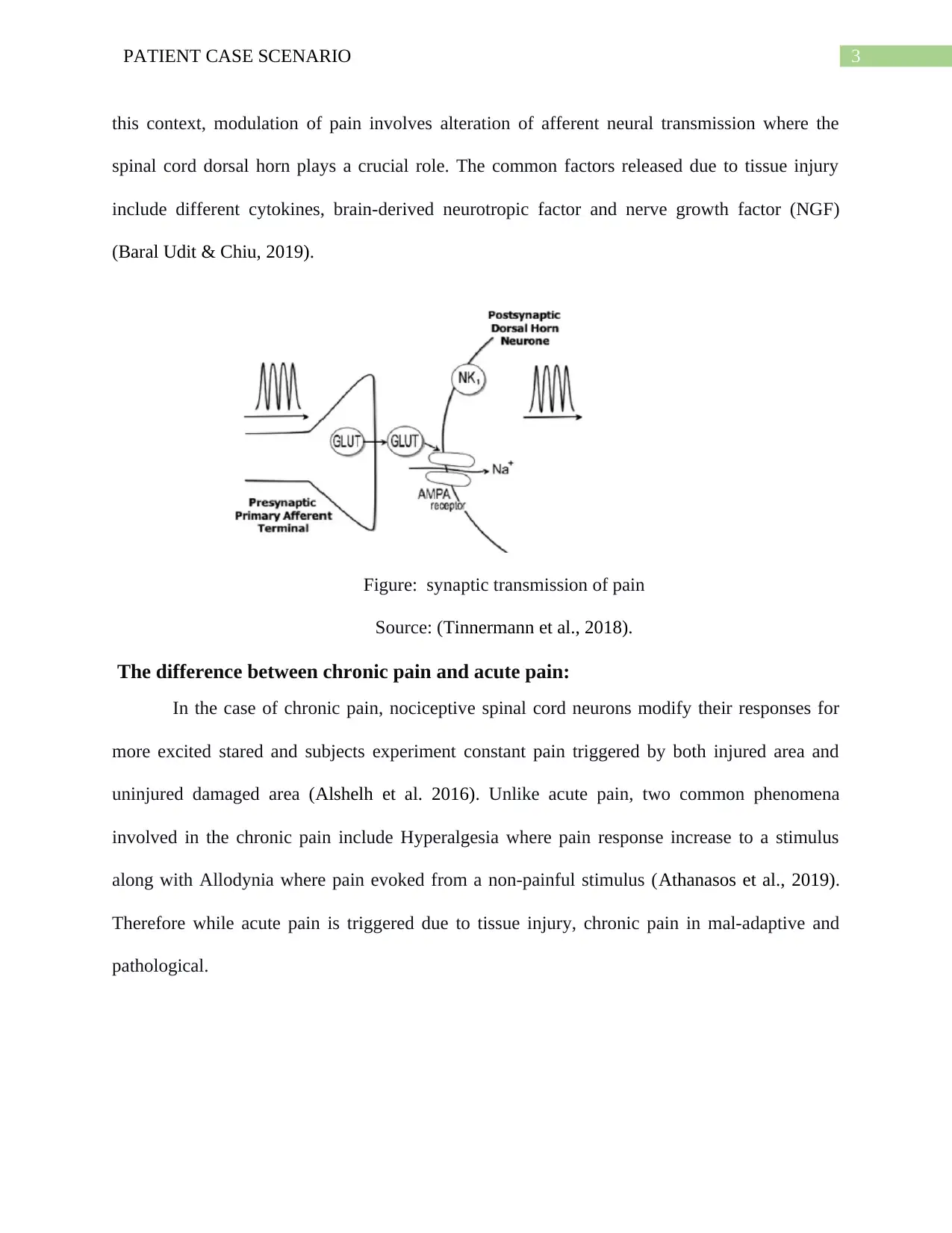
this context, modulation of pain involves alteration of afferent neural transmission where the
spinal cord dorsal horn plays a crucial role. The common factors released due to tissue injury
include different cytokines, brain-derived neurotropic factor and nerve growth factor (NGF)
(Baral Udit & Chiu, 2019).
Figure: synaptic transmission of pain
Source: (Tinnermann et al., 2018).
The difference between chronic pain and acute pain:
In the case of chronic pain, nociceptive spinal cord neurons modify their responses for
more excited stared and subjects experiment constant pain triggered by both injured area and
uninjured damaged area (Alshelh et al. 2016). Unlike acute pain, two common phenomena
involved in the chronic pain include Hyperalgesia where pain response increase to a stimulus
along with Allodynia where pain evoked from a non-painful stimulus (Athanasos et al., 2019).
Therefore while acute pain is triggered due to tissue injury, chronic pain in mal-adaptive and
pathological.
this context, modulation of pain involves alteration of afferent neural transmission where the
spinal cord dorsal horn plays a crucial role. The common factors released due to tissue injury
include different cytokines, brain-derived neurotropic factor and nerve growth factor (NGF)
(Baral Udit & Chiu, 2019).
Figure: synaptic transmission of pain
Source: (Tinnermann et al., 2018).
The difference between chronic pain and acute pain:
In the case of chronic pain, nociceptive spinal cord neurons modify their responses for
more excited stared and subjects experiment constant pain triggered by both injured area and
uninjured damaged area (Alshelh et al. 2016). Unlike acute pain, two common phenomena
involved in the chronic pain include Hyperalgesia where pain response increase to a stimulus
along with Allodynia where pain evoked from a non-painful stimulus (Athanasos et al., 2019).
Therefore while acute pain is triggered due to tissue injury, chronic pain in mal-adaptive and
pathological.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4PATIENT CASE SCENARIO
Figure: immunology of pain
Source: (Baral Udit & Chiu, 2019).
Role of narcotic analgesia in reducing acute pain:
Macintyre Roberts and Huxtable (2020), suggested that narcotic analgesia or opioid acts
selectively for depressing pain-sensitive cells by involving in the descending pathway
responsible for neural pathway alteration. When Opioid attached to the opioid receptors delta,
mu, and kappa, it reduces afferent responses by inhibiting transmission of pain information to the
spinal cord and other parts of the central nervous system. As the case study suggested that patient
was experiencing acute pain after a temporary ileostomy and administrated with narcotic
analgesia, narcotic analgesia can reduce his pain session by binding to the opioid receptors and
modulating sensation of pain.
Figure: immunology of pain
Source: (Baral Udit & Chiu, 2019).
Role of narcotic analgesia in reducing acute pain:
Macintyre Roberts and Huxtable (2020), suggested that narcotic analgesia or opioid acts
selectively for depressing pain-sensitive cells by involving in the descending pathway
responsible for neural pathway alteration. When Opioid attached to the opioid receptors delta,
mu, and kappa, it reduces afferent responses by inhibiting transmission of pain information to the
spinal cord and other parts of the central nervous system. As the case study suggested that patient
was experiencing acute pain after a temporary ileostomy and administrated with narcotic
analgesia, narcotic analgesia can reduce his pain session by binding to the opioid receptors and
modulating sensation of pain.
5PATIENT CASE SCENARIO
Question 1.2:
Three types of nursing assessment and rationale for it:
The case study highlighted that during the initial assessment, the patient was non-verbal,
difficult to rouse and eyes were closed. The patient exhibited elevated vital signs. Therefore,
three types of assessments that are required to conduct in this context would be :
Neurovascular assessment (pain):
Neurovascular assessment is conducted by nursing professionals for assessing a patient's
experience of pain. In this context, the patient was experiencing pain post temporary ileostomy
which resulted in closed eyes and nonverbal. In this context, pain assessment must be one of the
prime priorities so that pain management can be done. Glasgow Coma Scale in combination with
a numeric rating scale would be the most suitable tool for the assessment. Waterhouse, C.
(2017), suggested that the Glasgow Coma Scale enables nurses to assess the patient based on
best eye response, best verbal response and best motor response to pain as observed in this case
scene. On the other hand, the numeric rating scale will enable nurses to conduct subjective
measures in 0 to 10 based on the frequency and intensity of pain (Tong et al., 2018).
Physiological assessment (oxygen saturation):
The case study highlighted that the patient had low oxygen saturation 93% after the vital
sign assessment. In case of healthy individuals, the normal oxygen saturation is 98%. Cardona-
Morrell et al. (2016), suggested that patients often exhibit low oxygen saturation due to
difficulties in breathing where the lungs of the patient unable to transport the oxygen to the
tissue. Consequently, the respiratory rate also rapidly reduced as observed in this context where
the respiratory rate of the patient is 6 (normal 12to 24 bpm). Therefore, a spirometer can be used
for assessment of the lung function. Blake et al. (2020) suggested that spirometer enable nursing
Question 1.2:
Three types of nursing assessment and rationale for it:
The case study highlighted that during the initial assessment, the patient was non-verbal,
difficult to rouse and eyes were closed. The patient exhibited elevated vital signs. Therefore,
three types of assessments that are required to conduct in this context would be :
Neurovascular assessment (pain):
Neurovascular assessment is conducted by nursing professionals for assessing a patient's
experience of pain. In this context, the patient was experiencing pain post temporary ileostomy
which resulted in closed eyes and nonverbal. In this context, pain assessment must be one of the
prime priorities so that pain management can be done. Glasgow Coma Scale in combination with
a numeric rating scale would be the most suitable tool for the assessment. Waterhouse, C.
(2017), suggested that the Glasgow Coma Scale enables nurses to assess the patient based on
best eye response, best verbal response and best motor response to pain as observed in this case
scene. On the other hand, the numeric rating scale will enable nurses to conduct subjective
measures in 0 to 10 based on the frequency and intensity of pain (Tong et al., 2018).
Physiological assessment (oxygen saturation):
The case study highlighted that the patient had low oxygen saturation 93% after the vital
sign assessment. In case of healthy individuals, the normal oxygen saturation is 98%. Cardona-
Morrell et al. (2016), suggested that patients often exhibit low oxygen saturation due to
difficulties in breathing where the lungs of the patient unable to transport the oxygen to the
tissue. Consequently, the respiratory rate also rapidly reduced as observed in this context where
the respiratory rate of the patient is 6 (normal 12to 24 bpm). Therefore, a spirometer can be used
for assessment of the lung function. Blake et al. (2020) suggested that spirometer enable nursing
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6PATIENT CASE SCENARIO
professionals to measure the volume of air inhaled and exhaled by lungs and evaluate the
functionality of the lungs.
Physiological assessment ( blood pressure):
The case study suggested that the patient has low blood pressure after the vital sign
assessment. In case of healthy individuals, the normal blood pressure is 120/80 whereas the
patient exhibited 98/55. Cardona-Morrell et al. (2016), low blood pressure often a common
phenomenon during surgery, especially after surgery and it can be observed due to pain or
emotional stress. In this context, for assessing the blood pressure more accurately
sphygmomanometer can be used.
Question 1.3:
As discussed above, the patient had severe pain and exhibited elevated vital signs such as high
blood pressure and low oxygen therapy. Therefore, three types of interventions that are required
to provide to Tran in this context would be the following:
1. Relaxation therapy:
The case study suggested that the patient is experiencing acute pain which impacted his
consciousness. In this current context, the patient can be involved in relaxation therapy such as
deep breathing. Dos Santos Felix et al. (2019), suggested that deep breathing is considered as the
most suitable relaxation therapy that not only reduces the stress of the body but also reduces the
sensation of pain. The common mechanism in this context is that deep breathing enables oxygen
transportation to a different part of the cells and tissues which resulted in the reduction of muscle
tension (Ju et al., 2019). Moreover, deep breathing modulates pain responses and releases natural
endorphins. Consequently, the improved mood with reduced pain sensation observed. Therefore,
deep breathing can reduce the pain sensation of Tran and improve his mood. It will also improve
professionals to measure the volume of air inhaled and exhaled by lungs and evaluate the
functionality of the lungs.
Physiological assessment ( blood pressure):
The case study suggested that the patient has low blood pressure after the vital sign
assessment. In case of healthy individuals, the normal blood pressure is 120/80 whereas the
patient exhibited 98/55. Cardona-Morrell et al. (2016), low blood pressure often a common
phenomenon during surgery, especially after surgery and it can be observed due to pain or
emotional stress. In this context, for assessing the blood pressure more accurately
sphygmomanometer can be used.
Question 1.3:
As discussed above, the patient had severe pain and exhibited elevated vital signs such as high
blood pressure and low oxygen therapy. Therefore, three types of interventions that are required
to provide to Tran in this context would be the following:
1. Relaxation therapy:
The case study suggested that the patient is experiencing acute pain which impacted his
consciousness. In this current context, the patient can be involved in relaxation therapy such as
deep breathing. Dos Santos Felix et al. (2019), suggested that deep breathing is considered as the
most suitable relaxation therapy that not only reduces the stress of the body but also reduces the
sensation of pain. The common mechanism in this context is that deep breathing enables oxygen
transportation to a different part of the cells and tissues which resulted in the reduction of muscle
tension (Ju et al., 2019). Moreover, deep breathing modulates pain responses and releases natural
endorphins. Consequently, the improved mood with reduced pain sensation observed. Therefore,
deep breathing can reduce the pain sensation of Tran and improve his mood. It will also improve
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7PATIENT CASE SCENARIO
his sleep and consciousness resulted from acute pain. His family members can be incorporated
while assisting him in the relaxation therapy as it improves empower him and provide comfort to
him.
Oxygen therapy:
As discussed above patient had low oxygen saturation 93% after the vital sign
assessment. For improving oxygen saturation, the patient can be provided with oxygen therapy.
Kamran, Chia and Tobin (2018), suggested that oxygen therapy provided by a nurse to patients
who are experiencing hypoxia for improving oxygen saturation of the patients. The delivery of
oxygen gas improves the function of the lungs by increasing the oxygen concentration of the
blood for transporting to the cells and tissues. In oxygen therapy, the patients are usually
provided with tubes resting on the nose or face mask. The benefit in this context of the case
study is it will improve oxygen saturation to 98% and increase the consciousness of Tran and
improve the ability to carry out daily activities.
Midodrine:
The case study suggested that the patient has low blood pressure such as 98/ 55 after the
vital sign assessment. In this context, for the management of hypotension, the patient can be
provided with Midodrine. Wong et al. (2017), suggested that Midodrine can increase blood
pressure amongst patients suffering from hypotension by working on blood vessels and
constriction of blood vessels. Therefore, after administration of the medication, it can stabilize
the blood pressure to 120/80. Additionally, it can improve heart function, light-headed feeling or
severe dizziness.
his sleep and consciousness resulted from acute pain. His family members can be incorporated
while assisting him in the relaxation therapy as it improves empower him and provide comfort to
him.
Oxygen therapy:
As discussed above patient had low oxygen saturation 93% after the vital sign
assessment. For improving oxygen saturation, the patient can be provided with oxygen therapy.
Kamran, Chia and Tobin (2018), suggested that oxygen therapy provided by a nurse to patients
who are experiencing hypoxia for improving oxygen saturation of the patients. The delivery of
oxygen gas improves the function of the lungs by increasing the oxygen concentration of the
blood for transporting to the cells and tissues. In oxygen therapy, the patients are usually
provided with tubes resting on the nose or face mask. The benefit in this context of the case
study is it will improve oxygen saturation to 98% and increase the consciousness of Tran and
improve the ability to carry out daily activities.
Midodrine:
The case study suggested that the patient has low blood pressure such as 98/ 55 after the
vital sign assessment. In this context, for the management of hypotension, the patient can be
provided with Midodrine. Wong et al. (2017), suggested that Midodrine can increase blood
pressure amongst patients suffering from hypotension by working on blood vessels and
constriction of blood vessels. Therefore, after administration of the medication, it can stabilize
the blood pressure to 120/80. Additionally, it can improve heart function, light-headed feeling or
severe dizziness.
8PATIENT CASE SCENARIO
Question 1.4:
Administration of morphine:
The case study suggested that patient was administrated a loading dose of intravenous morphine
(5mg) before transferring to the ward. In this context, administration, benefits, risks, and
contraindications of morphine for Tran are the following:
Administration:
In order to administrate morphine, usually, intravenous administration is recommended
since intravenous administration has 100% bioavailability and intravenous administration avoids
the first-pass metabolism. Food and Drug Administration suggested that for direct intravenous
injection, the usual starting dose is 0.1 mg to2.0mg per kg every 4 hours based on the severity of
the pain, age, and disease (Www.accessdata.fda.gov, 2020). Therefore, while administrating
morphine to Tran, these factors are required to consider. In this context, the loading dose of
intravenous morphine (5mg) will reduce the severity of acute pain. The degree of opioid
tolerance, concurrent medications, and history of substance abuse are also required to consider.
Benefits:
The common benefit of morphine use include reduced level of pain sensation, improved verbal
response, improved consciousness, and improved mood (Www.accessdata.fda.gov, 2020).
Therefore, after the administration of morphine, Tran will exhibit improved mood, improved
verbal response, and improved consciousness.
Risk and contraindication:
The morphine contraindicated
in patients with hypersensitivity
In patients with respiratory depression in the absence in absence of resuscitative
apparatus.
Question 1.4:
Administration of morphine:
The case study suggested that patient was administrated a loading dose of intravenous morphine
(5mg) before transferring to the ward. In this context, administration, benefits, risks, and
contraindications of morphine for Tran are the following:
Administration:
In order to administrate morphine, usually, intravenous administration is recommended
since intravenous administration has 100% bioavailability and intravenous administration avoids
the first-pass metabolism. Food and Drug Administration suggested that for direct intravenous
injection, the usual starting dose is 0.1 mg to2.0mg per kg every 4 hours based on the severity of
the pain, age, and disease (Www.accessdata.fda.gov, 2020). Therefore, while administrating
morphine to Tran, these factors are required to consider. In this context, the loading dose of
intravenous morphine (5mg) will reduce the severity of acute pain. The degree of opioid
tolerance, concurrent medications, and history of substance abuse are also required to consider.
Benefits:
The common benefit of morphine use include reduced level of pain sensation, improved verbal
response, improved consciousness, and improved mood (Www.accessdata.fda.gov, 2020).
Therefore, after the administration of morphine, Tran will exhibit improved mood, improved
verbal response, and improved consciousness.
Risk and contraindication:
The morphine contraindicated
in patients with hypersensitivity
In patients with respiratory depression in the absence in absence of resuscitative
apparatus.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9PATIENT CASE SCENARIO
In patients with acute asthma or suffering from hypercarbia.
In patients with paralytic ileus.
In patients with Addison’s disease
In patients with hypothyroidism
In this context, patients with the above disease are at high risk of subjecting to the potential
harm. Therefore, while administrating morphine, the registered nurse must assess these diseases
for avoiding negative side effects. Tran may experience CNS depression, Cardiovascular
Instability, and overuse of the morphine. Since Tran exhibited low blood pressure, the use of
morphine may facilitate severe hypotensive effects (Www.accessdata.fda.gov, 2020). Moreover,
patients with GI tract obstructions must not be administered with morphine. In this context, this
factor must be considered before administrating the medication.
Patient education:
In order to provide education, the nursing professional is required to inform the treatment
plan, type of dose and rationale behind using morphine and benefit from morphine. Additionally,
by following appropriate guidelines of intravenous administration and policy, the nurse can
provide literacy regarding education side effects and contraindication of morphine. The nurse
can assist Tran to assess the intravenous injection site frequently for recognizing any
hypersensitivity reaction, skin rash, and abnormalities of the extremity before and after
administration of medication and report immediately (Www.accessdata.fda.gov, 2020). The
nurse can provide education regarding the management of side effects and hand hygiene prior to
touch the education. His family members can be incorporated into the treatment procedure so
that he can feel empowered and safe.
In patients with acute asthma or suffering from hypercarbia.
In patients with paralytic ileus.
In patients with Addison’s disease
In patients with hypothyroidism
In this context, patients with the above disease are at high risk of subjecting to the potential
harm. Therefore, while administrating morphine, the registered nurse must assess these diseases
for avoiding negative side effects. Tran may experience CNS depression, Cardiovascular
Instability, and overuse of the morphine. Since Tran exhibited low blood pressure, the use of
morphine may facilitate severe hypotensive effects (Www.accessdata.fda.gov, 2020). Moreover,
patients with GI tract obstructions must not be administered with morphine. In this context, this
factor must be considered before administrating the medication.
Patient education:
In order to provide education, the nursing professional is required to inform the treatment
plan, type of dose and rationale behind using morphine and benefit from morphine. Additionally,
by following appropriate guidelines of intravenous administration and policy, the nurse can
provide literacy regarding education side effects and contraindication of morphine. The nurse
can assist Tran to assess the intravenous injection site frequently for recognizing any
hypersensitivity reaction, skin rash, and abnormalities of the extremity before and after
administration of medication and report immediately (Www.accessdata.fda.gov, 2020). The
nurse can provide education regarding the management of side effects and hand hygiene prior to
touch the education. His family members can be incorporated into the treatment procedure so
that he can feel empowered and safe.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10PATIENT CASE SCENARIO
Question 1.5:
Side effects of the medication and rationale behind mandatory reporting:
The major side effects of administration of morphine for Tran are following:
Gastrointestinal reaction:
Morphine may contributed to prolonged gastrointestinal obstruction, as the intravenous
injection of the drug propulsive peristaltic waves in the gastrointestinal tract
(Www.accessdata.fda.gov, 2020). Tran had a history of Ulcerative colitis which is an
inflammatory bowel disease that triggered long-lasting inflammation and sore in the GI tract.
Therefore, even after temporary ileostomy, Tran might experience abdominal issues.
Cardiovascular issues:
Due to morphine administration, the patient may experience Tachycardia, syncope, and
hypotension (Www.accessdata.fda.gov, 2020). The case study suggested that the patient had
a high heart rate such as 110 bpm and low blood pressure such as 98/5. Therefore, the
administration of medication can result in worsening the vital signs of Tran. Therefore, these
findings are required to report the physicians immediately.
Additional side effects: due to intravenous injection, the patient may experience flushed
face, skin rash and local tissue inflammation (Www.accessdata.fda.gov, 2020). These
side effects will aggravate the health condition of the patient. Therefore, while
administrating the medication, the flushed face and skin race are required to report to the
physician for immediate management of the side effects of Morphine administration.
Question 1.5:
Side effects of the medication and rationale behind mandatory reporting:
The major side effects of administration of morphine for Tran are following:
Gastrointestinal reaction:
Morphine may contributed to prolonged gastrointestinal obstruction, as the intravenous
injection of the drug propulsive peristaltic waves in the gastrointestinal tract
(Www.accessdata.fda.gov, 2020). Tran had a history of Ulcerative colitis which is an
inflammatory bowel disease that triggered long-lasting inflammation and sore in the GI tract.
Therefore, even after temporary ileostomy, Tran might experience abdominal issues.
Cardiovascular issues:
Due to morphine administration, the patient may experience Tachycardia, syncope, and
hypotension (Www.accessdata.fda.gov, 2020). The case study suggested that the patient had
a high heart rate such as 110 bpm and low blood pressure such as 98/5. Therefore, the
administration of medication can result in worsening the vital signs of Tran. Therefore, these
findings are required to report the physicians immediately.
Additional side effects: due to intravenous injection, the patient may experience flushed
face, skin rash and local tissue inflammation (Www.accessdata.fda.gov, 2020). These
side effects will aggravate the health condition of the patient. Therefore, while
administrating the medication, the flushed face and skin race are required to report to the
physician for immediate management of the side effects of Morphine administration.
11PATIENT CASE SCENARIO
Conclusion:
Concluding note, it can be said that patients often experience severe pain after temporary
ileostomy, especially patients with a history of ulcerative colitis. In this context, three
assessments would be one neurovascular assessment and two physical assessments. The patient
can be provided with three different interventions. Additionally, education must be provided to
the patient so that the side effects of the intervention can be provided.
Conclusion:
Concluding note, it can be said that patients often experience severe pain after temporary
ileostomy, especially patients with a history of ulcerative colitis. In this context, three
assessments would be one neurovascular assessment and two physical assessments. The patient
can be provided with three different interventions. Additionally, education must be provided to
the patient so that the side effects of the intervention can be provided.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 15
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





