Patient Education: Norspan Medication Script for Mrs. Caroline Morris
VerifiedAdded on 2022/09/01
|5
|1518
|23
Practical Assignment
AI Summary
This assignment presents a detailed Registered Nurse's script designed to educate Mrs. Caroline Morris, a patient on the GI ward recovering from bowel resection with ileostomy formation, about Norspan, a transdermal pain medication. The script addresses Mrs. Morris's concerns, including her reluctance to use pain medication due to fear of side effects. The nurse introduces Norspan, explains its benefits, and provides comprehensive instructions on application, including site selection and changing the patch. The script also covers potential side effects like drowsiness, dizziness, and constipation, ensuring the patient is informed and prepared. The nurse emphasizes the importance of communication, encouraging Mrs. Morris to report any unusual symptoms. The interaction incorporates empathetic language and active listening to build rapport and trust, ensuring patient understanding and adherence to the treatment plan. The assignment highlights the nurse's role in patient education and support within a clinical setting.
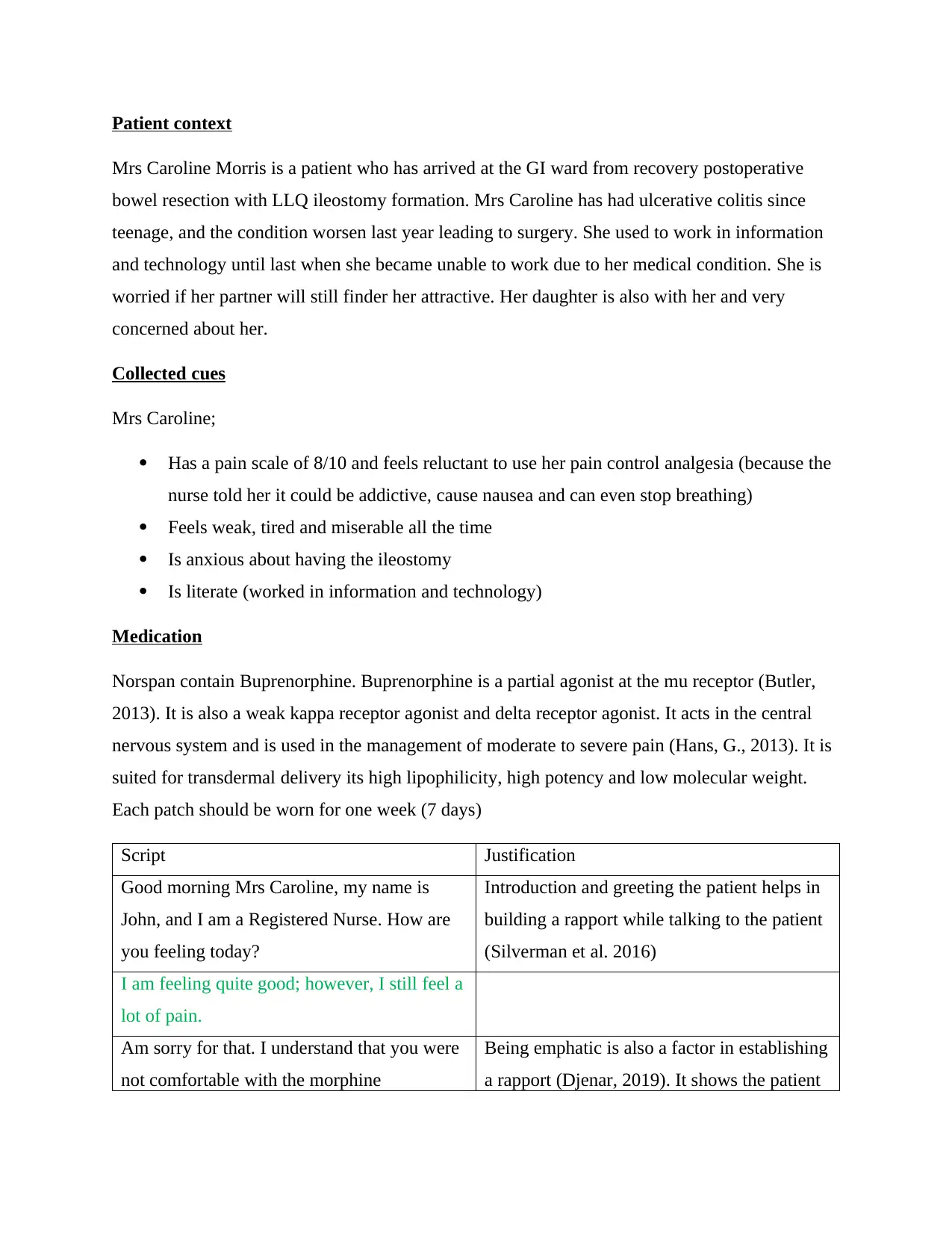
Patient context
Mrs Caroline Morris is a patient who has arrived at the GI ward from recovery postoperative
bowel resection with LLQ ileostomy formation. Mrs Caroline has had ulcerative colitis since
teenage, and the condition worsen last year leading to surgery. She used to work in information
and technology until last when she became unable to work due to her medical condition. She is
worried if her partner will still finder her attractive. Her daughter is also with her and very
concerned about her.
Collected cues
Mrs Caroline;
Has a pain scale of 8/10 and feels reluctant to use her pain control analgesia (because the
nurse told her it could be addictive, cause nausea and can even stop breathing)
Feels weak, tired and miserable all the time
Is anxious about having the ileostomy
Is literate (worked in information and technology)
Medication
Norspan contain Buprenorphine. Buprenorphine is a partial agonist at the mu receptor (Butler,
2013). It is also a weak kappa receptor agonist and delta receptor agonist. It acts in the central
nervous system and is used in the management of moderate to severe pain (Hans, G., 2013). It is
suited for transdermal delivery its high lipophilicity, high potency and low molecular weight.
Each patch should be worn for one week (7 days)
Script Justification
Good morning Mrs Caroline, my name is
John, and I am a Registered Nurse. How are
you feeling today?
Introduction and greeting the patient helps in
building a rapport while talking to the patient
(Silverman et al. 2016)
I am feeling quite good; however, I still feel a
lot of pain.
Am sorry for that. I understand that you were
not comfortable with the morphine
Being emphatic is also a factor in establishing
a rapport (Djenar, 2019). It shows the patient
Mrs Caroline Morris is a patient who has arrived at the GI ward from recovery postoperative
bowel resection with LLQ ileostomy formation. Mrs Caroline has had ulcerative colitis since
teenage, and the condition worsen last year leading to surgery. She used to work in information
and technology until last when she became unable to work due to her medical condition. She is
worried if her partner will still finder her attractive. Her daughter is also with her and very
concerned about her.
Collected cues
Mrs Caroline;
Has a pain scale of 8/10 and feels reluctant to use her pain control analgesia (because the
nurse told her it could be addictive, cause nausea and can even stop breathing)
Feels weak, tired and miserable all the time
Is anxious about having the ileostomy
Is literate (worked in information and technology)
Medication
Norspan contain Buprenorphine. Buprenorphine is a partial agonist at the mu receptor (Butler,
2013). It is also a weak kappa receptor agonist and delta receptor agonist. It acts in the central
nervous system and is used in the management of moderate to severe pain (Hans, G., 2013). It is
suited for transdermal delivery its high lipophilicity, high potency and low molecular weight.
Each patch should be worn for one week (7 days)
Script Justification
Good morning Mrs Caroline, my name is
John, and I am a Registered Nurse. How are
you feeling today?
Introduction and greeting the patient helps in
building a rapport while talking to the patient
(Silverman et al. 2016)
I am feeling quite good; however, I still feel a
lot of pain.
Am sorry for that. I understand that you were
not comfortable with the morphine
Being emphatic is also a factor in establishing
a rapport (Djenar, 2019). It shows the patient
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
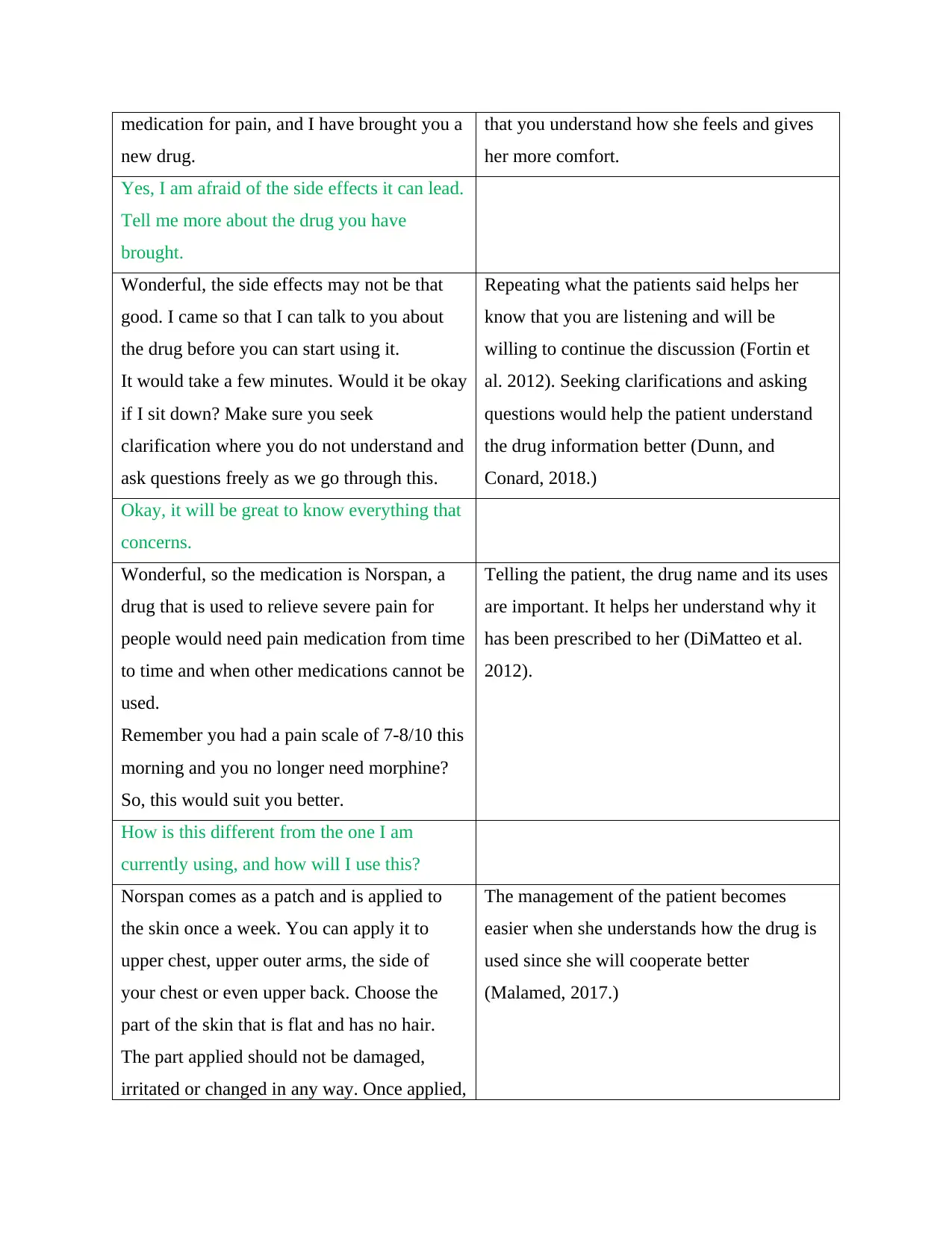
medication for pain, and I have brought you a
new drug.
that you understand how she feels and gives
her more comfort.
Yes, I am afraid of the side effects it can lead.
Tell me more about the drug you have
brought.
Wonderful, the side effects may not be that
good. I came so that I can talk to you about
the drug before you can start using it.
It would take a few minutes. Would it be okay
if I sit down? Make sure you seek
clarification where you do not understand and
ask questions freely as we go through this.
Repeating what the patients said helps her
know that you are listening and will be
willing to continue the discussion (Fortin et
al. 2012). Seeking clarifications and asking
questions would help the patient understand
the drug information better (Dunn, and
Conard, 2018.)
Okay, it will be great to know everything that
concerns.
Wonderful, so the medication is Norspan, a
drug that is used to relieve severe pain for
people would need pain medication from time
to time and when other medications cannot be
used.
Remember you had a pain scale of 7-8/10 this
morning and you no longer need morphine?
So, this would suit you better.
Telling the patient, the drug name and its uses
are important. It helps her understand why it
has been prescribed to her (DiMatteo et al.
2012).
How is this different from the one I am
currently using, and how will I use this?
Norspan comes as a patch and is applied to
the skin once a week. You can apply it to
upper chest, upper outer arms, the side of
your chest or even upper back. Choose the
part of the skin that is flat and has no hair.
The part applied should not be damaged,
irritated or changed in any way. Once applied,
The management of the patient becomes
easier when she understands how the drug is
used since she will cooperate better
(Malamed, 2017.)
new drug.
that you understand how she feels and gives
her more comfort.
Yes, I am afraid of the side effects it can lead.
Tell me more about the drug you have
brought.
Wonderful, the side effects may not be that
good. I came so that I can talk to you about
the drug before you can start using it.
It would take a few minutes. Would it be okay
if I sit down? Make sure you seek
clarification where you do not understand and
ask questions freely as we go through this.
Repeating what the patients said helps her
know that you are listening and will be
willing to continue the discussion (Fortin et
al. 2012). Seeking clarifications and asking
questions would help the patient understand
the drug information better (Dunn, and
Conard, 2018.)
Okay, it will be great to know everything that
concerns.
Wonderful, so the medication is Norspan, a
drug that is used to relieve severe pain for
people would need pain medication from time
to time and when other medications cannot be
used.
Remember you had a pain scale of 7-8/10 this
morning and you no longer need morphine?
So, this would suit you better.
Telling the patient, the drug name and its uses
are important. It helps her understand why it
has been prescribed to her (DiMatteo et al.
2012).
How is this different from the one I am
currently using, and how will I use this?
Norspan comes as a patch and is applied to
the skin once a week. You can apply it to
upper chest, upper outer arms, the side of
your chest or even upper back. Choose the
part of the skin that is flat and has no hair.
The part applied should not be damaged,
irritated or changed in any way. Once applied,
The management of the patient becomes
easier when she understands how the drug is
used since she will cooperate better
(Malamed, 2017.)
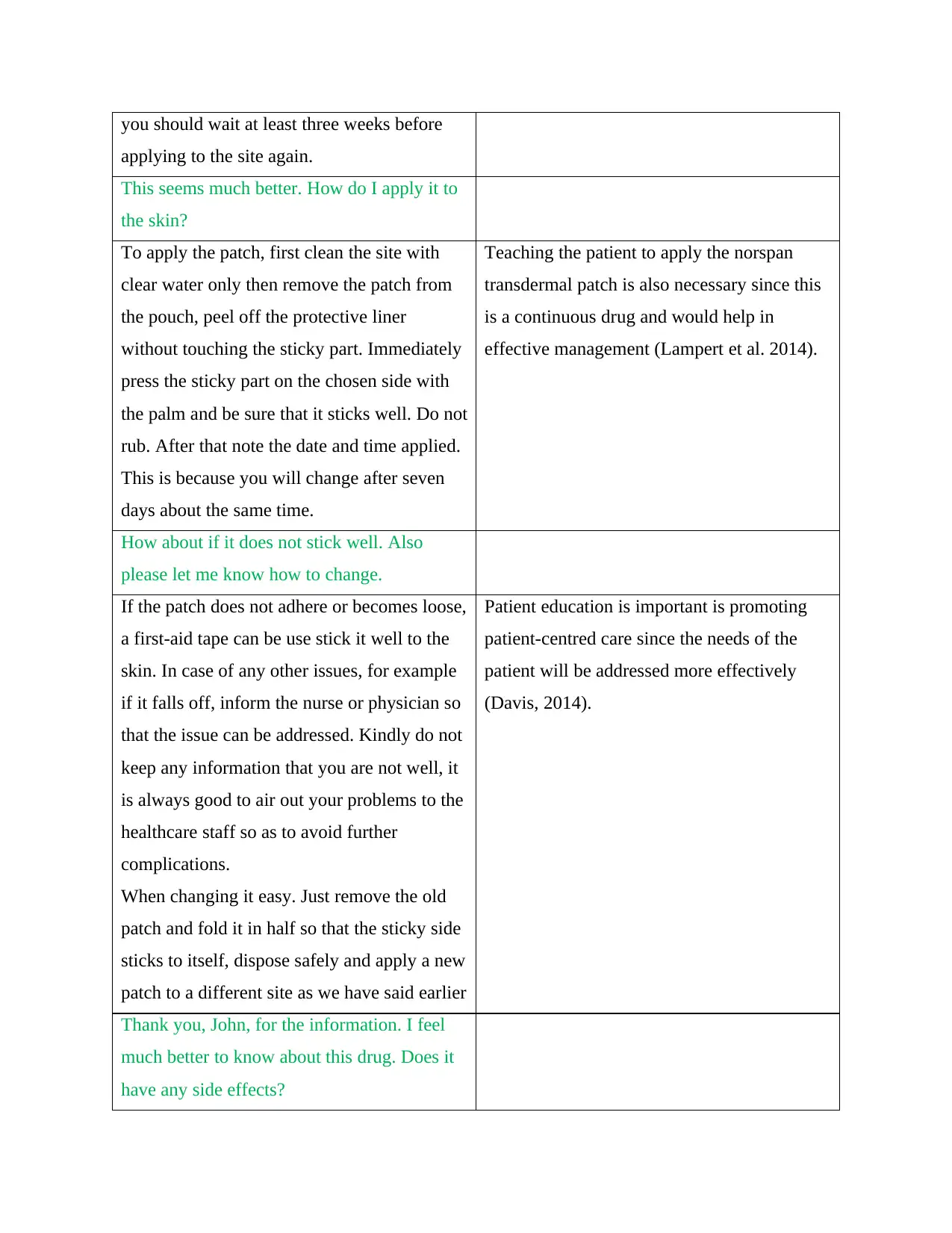
you should wait at least three weeks before
applying to the site again.
This seems much better. How do I apply it to
the skin?
To apply the patch, first clean the site with
clear water only then remove the patch from
the pouch, peel off the protective liner
without touching the sticky part. Immediately
press the sticky part on the chosen side with
the palm and be sure that it sticks well. Do not
rub. After that note the date and time applied.
This is because you will change after seven
days about the same time.
Teaching the patient to apply the norspan
transdermal patch is also necessary since this
is a continuous drug and would help in
effective management (Lampert et al. 2014).
How about if it does not stick well. Also
please let me know how to change.
If the patch does not adhere or becomes loose,
a first-aid tape can be use stick it well to the
skin. In case of any other issues, for example
if it falls off, inform the nurse or physician so
that the issue can be addressed. Kindly do not
keep any information that you are not well, it
is always good to air out your problems to the
healthcare staff so as to avoid further
complications.
When changing it easy. Just remove the old
patch and fold it in half so that the sticky side
sticks to itself, dispose safely and apply a new
patch to a different site as we have said earlier
Patient education is important is promoting
patient-centred care since the needs of the
patient will be addressed more effectively
(Davis, 2014).
Thank you, John, for the information. I feel
much better to know about this drug. Does it
have any side effects?
applying to the site again.
This seems much better. How do I apply it to
the skin?
To apply the patch, first clean the site with
clear water only then remove the patch from
the pouch, peel off the protective liner
without touching the sticky part. Immediately
press the sticky part on the chosen side with
the palm and be sure that it sticks well. Do not
rub. After that note the date and time applied.
This is because you will change after seven
days about the same time.
Teaching the patient to apply the norspan
transdermal patch is also necessary since this
is a continuous drug and would help in
effective management (Lampert et al. 2014).
How about if it does not stick well. Also
please let me know how to change.
If the patch does not adhere or becomes loose,
a first-aid tape can be use stick it well to the
skin. In case of any other issues, for example
if it falls off, inform the nurse or physician so
that the issue can be addressed. Kindly do not
keep any information that you are not well, it
is always good to air out your problems to the
healthcare staff so as to avoid further
complications.
When changing it easy. Just remove the old
patch and fold it in half so that the sticky side
sticks to itself, dispose safely and apply a new
patch to a different site as we have said earlier
Patient education is important is promoting
patient-centred care since the needs of the
patient will be addressed more effectively
(Davis, 2014).
Thank you, John, for the information. I feel
much better to know about this drug. Does it
have any side effects?
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
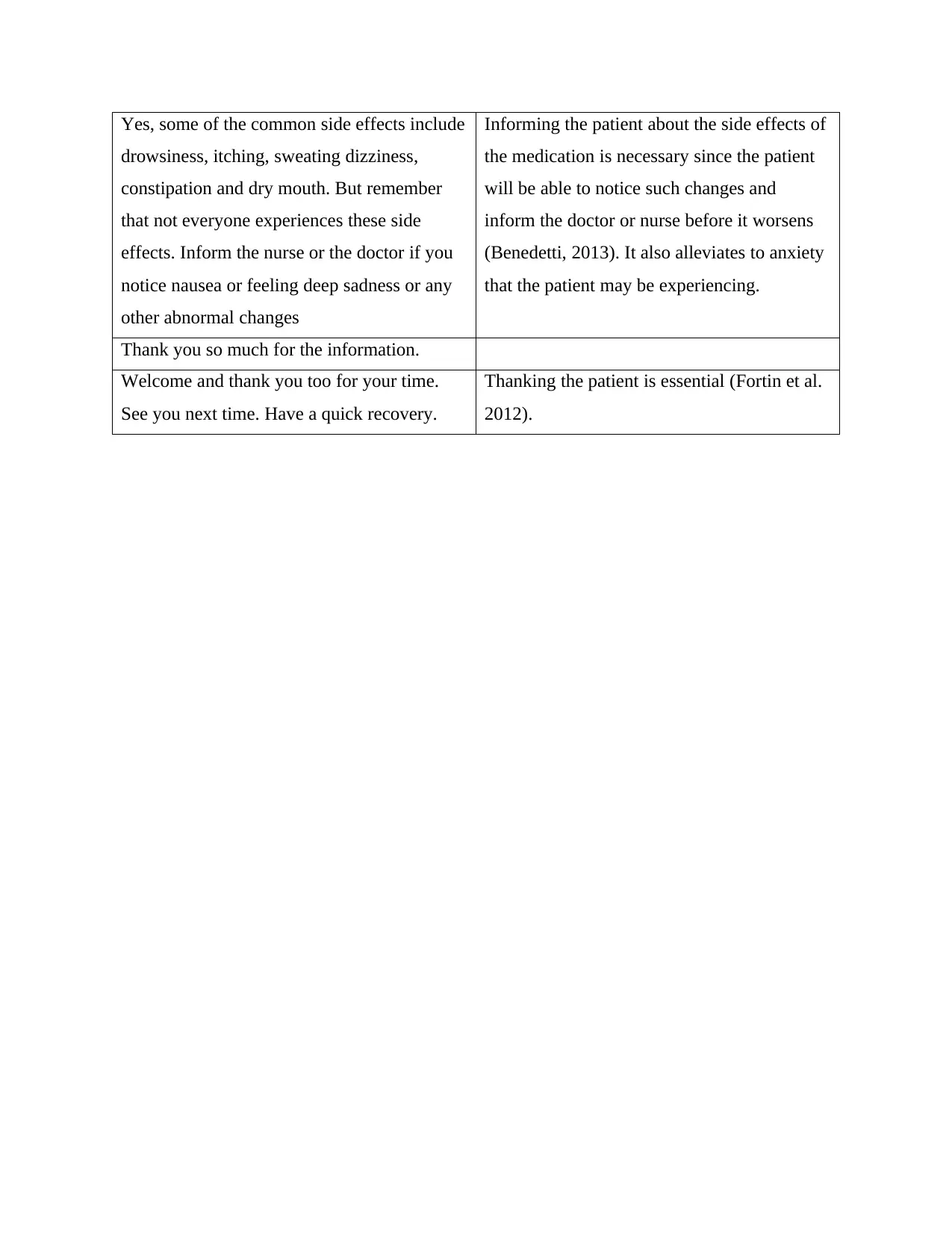
Yes, some of the common side effects include
drowsiness, itching, sweating dizziness,
constipation and dry mouth. But remember
that not everyone experiences these side
effects. Inform the nurse or the doctor if you
notice nausea or feeling deep sadness or any
other abnormal changes
Informing the patient about the side effects of
the medication is necessary since the patient
will be able to notice such changes and
inform the doctor or nurse before it worsens
(Benedetti, 2013). It also alleviates to anxiety
that the patient may be experiencing.
Thank you so much for the information.
Welcome and thank you too for your time.
See you next time. Have a quick recovery.
Thanking the patient is essential (Fortin et al.
2012).
drowsiness, itching, sweating dizziness,
constipation and dry mouth. But remember
that not everyone experiences these side
effects. Inform the nurse or the doctor if you
notice nausea or feeling deep sadness or any
other abnormal changes
Informing the patient about the side effects of
the medication is necessary since the patient
will be able to notice such changes and
inform the doctor or nurse before it worsens
(Benedetti, 2013). It also alleviates to anxiety
that the patient may be experiencing.
Thank you so much for the information.
Welcome and thank you too for your time.
See you next time. Have a quick recovery.
Thanking the patient is essential (Fortin et al.
2012).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
References
Benedetti, F., 2013. Placebo and the new physiology of the doctor-patient
relationship. Physiological reviews, 93(3), pp.1207-1246.
Butler, S., 2013. Buprenorphine—Clinically useful but often misunderstood. Scandinavian
journal of pain, 4(3), pp.148-152.
Davis Boykins, A., 2014. Core communication competencies in patient-centered care. ABNF
Journal, 25(2).
DiMatteo, M.R., Haskard-Zolnierek, K.B. and Martin, L.R., 2012. Improving patient adherence:
a three-factor model to guide practice. Health Psychology Review, 6(1), pp.74-91.
Djenar, D.N., 2019. 11 Recognitional Reference and Rapport Building in the Author
Interview. Rapport and the Discursive Co-Construction of Social Relations in Fieldwork
Encounters, 19, p.163.
Dunn, P. and Conard, S., 2018. Improving health literacy in patients with chronic conditions: a
call to action. International journal of cardiology, 273, pp.249-251.
Fortin, A.H., Dwamena, F.C., Frankel, R.M. and Smith, R.C., 2012. Smith's patient centered
interviewing: an evidence-based method. McGraw Hill Professional.
Hans, G., 2013. Buprenorphine Analgesia in Chronic Pain. In Handbook of Methadone
Prescribing and Buprenorphine Therapy (pp. 109-137). Springer, New York, NY.
Lampert, A., Seiberth, J., Haefeli, W.E. and Seidling, H.M., 2014. A systematic review of
medication administration errors with transdermal patches. Expert opinion on drug safety, 13(8),
pp.1101-1114.
Malamed, S.F., 2017. Sedation-E-Book: A Guide to Patient Management. Elsevier Health
Sciences.
Silverman, J., Kurtz, S. and Draper, J., 2016. Skills for communicating with patients. crc press.
Benedetti, F., 2013. Placebo and the new physiology of the doctor-patient
relationship. Physiological reviews, 93(3), pp.1207-1246.
Butler, S., 2013. Buprenorphine—Clinically useful but often misunderstood. Scandinavian
journal of pain, 4(3), pp.148-152.
Davis Boykins, A., 2014. Core communication competencies in patient-centered care. ABNF
Journal, 25(2).
DiMatteo, M.R., Haskard-Zolnierek, K.B. and Martin, L.R., 2012. Improving patient adherence:
a three-factor model to guide practice. Health Psychology Review, 6(1), pp.74-91.
Djenar, D.N., 2019. 11 Recognitional Reference and Rapport Building in the Author
Interview. Rapport and the Discursive Co-Construction of Social Relations in Fieldwork
Encounters, 19, p.163.
Dunn, P. and Conard, S., 2018. Improving health literacy in patients with chronic conditions: a
call to action. International journal of cardiology, 273, pp.249-251.
Fortin, A.H., Dwamena, F.C., Frankel, R.M. and Smith, R.C., 2012. Smith's patient centered
interviewing: an evidence-based method. McGraw Hill Professional.
Hans, G., 2013. Buprenorphine Analgesia in Chronic Pain. In Handbook of Methadone
Prescribing and Buprenorphine Therapy (pp. 109-137). Springer, New York, NY.
Lampert, A., Seiberth, J., Haefeli, W.E. and Seidling, H.M., 2014. A systematic review of
medication administration errors with transdermal patches. Expert opinion on drug safety, 13(8),
pp.1101-1114.
Malamed, S.F., 2017. Sedation-E-Book: A Guide to Patient Management. Elsevier Health
Sciences.
Silverman, J., Kurtz, S. and Draper, J., 2016. Skills for communicating with patients. crc press.
1 out of 5
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





