Collision of a 19 year old boy with a car in Newcastle
VerifiedAdded on 2022/08/20
|13
|4123
|12
AI Summary
His blood pressure was 35.70/80 mmole/L; GCS: 14; chest pain; Weight: 85 kg BGL: 4.0-7.8 mmole/L (Dan Queensland, 2015); GCS: >8(BrainLine, 2020); Weight: 57-58 kg at the age of 19-20 (Centers for Disease Control and Prevention, 2020) Exposure Fracture of the left fourth to ninth ribs; fractured chest from fifth to the seventh rib.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: CASE STUDY
CASE STUDY
Name of the Student
Name of the University
Author Note
CASE STUDY
Name of the Student
Name of the University
Author Note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1CASE STUDY
PATIENT PRESENTATION
At around 9 PM, an 18 year old boy named Dan Jones having a probationary driving
license met with a motor vehicle collision on the road outside Newcastle. His car was hit by
another car at 80 km/hr in the front. The airbag of Dan’s car was deployed, and he was held
back by the seatbelt. When the ambulance arrived at the accident scene, the crew noted Dan’s
situation. Dan’s condition in the Glasgow Coma Scale reading showed 15, which depicts his
consciousness. His respiration rate (RR) was 24. Dan’s blood pressure (BP) was 110/80,
heart rate (HR) was 90, and peripheral capillary oxygen saturation (SpO2) was 96%. Apart
from this, Dan complained of a pain in his right chest during inhalation. He was then brought
to the Jong Hunter Hospital within 9.35 PM by the ambulance after applying a few
precautions to support him.
CUE COLLECTION
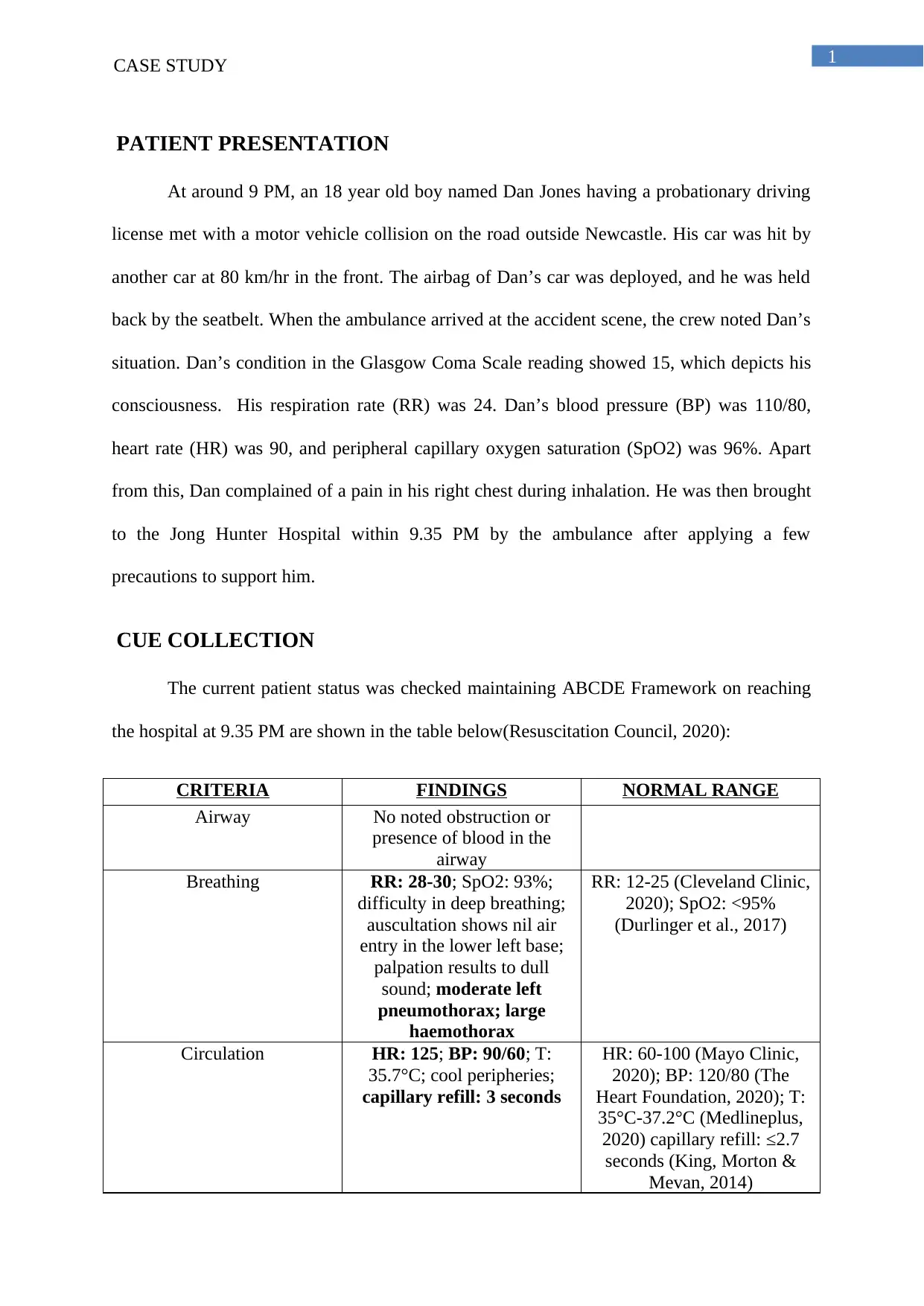
The current patient status was checked maintaining ABCDE Framework on reaching
the hospital at 9.35 PM are shown in the table below(Resuscitation Council, 2020):
CRITERIA FINDINGS NORMAL RANGE
Airway No noted obstruction or
presence of blood in the
airway
Breathing RR: 28-30; SpO2: 93%;
difficulty in deep breathing;
auscultation shows nil air
entry in the lower left base;
palpation results to dull
sound; moderate left
pneumothorax; large
haemothorax
RR: 12-25 (Cleveland Clinic,
2020); SpO2: <95%
(Durlinger et al., 2017)
Circulation HR: 125; BP: 90/60; T:
35.7°C; cool peripheries;
capillary refill: 3 seconds
HR: 60-100 (Mayo Clinic,
2020); BP: 120/80 (The
Heart Foundation, 2020); T:
35°C-37.2°C (Medlineplus,
2020) capillary refill: ≤2.7
seconds (King, Morton &
Mevan, 2014)
PATIENT PRESENTATION
At around 9 PM, an 18 year old boy named Dan Jones having a probationary driving
license met with a motor vehicle collision on the road outside Newcastle. His car was hit by
another car at 80 km/hr in the front. The airbag of Dan’s car was deployed, and he was held
back by the seatbelt. When the ambulance arrived at the accident scene, the crew noted Dan’s
situation. Dan’s condition in the Glasgow Coma Scale reading showed 15, which depicts his
consciousness. His respiration rate (RR) was 24. Dan’s blood pressure (BP) was 110/80,
heart rate (HR) was 90, and peripheral capillary oxygen saturation (SpO2) was 96%. Apart
from this, Dan complained of a pain in his right chest during inhalation. He was then brought
to the Jong Hunter Hospital within 9.35 PM by the ambulance after applying a few
precautions to support him.
CUE COLLECTION
The current patient status was checked maintaining ABCDE Framework on reaching
the hospital at 9.35 PM are shown in the table below(Resuscitation Council, 2020):
CRITERIA FINDINGS NORMAL RANGE
Airway No noted obstruction or
presence of blood in the
airway
Breathing RR: 28-30; SpO2: 93%;
difficulty in deep breathing;
auscultation shows nil air
entry in the lower left base;
palpation results to dull
sound; moderate left
pneumothorax; large
haemothorax
RR: 12-25 (Cleveland Clinic,
2020); SpO2: <95%
(Durlinger et al., 2017)
Circulation HR: 125; BP: 90/60; T:
35.7°C; cool peripheries;
capillary refill: 3 seconds
HR: 60-100 (Mayo Clinic,
2020); BP: 120/80 (The
Heart Foundation, 2020); T:
35°C-37.2°C (Medlineplus,
2020) capillary refill: ≤2.7
seconds (King, Morton &
Mevan, 2014)
2CASE STUDY
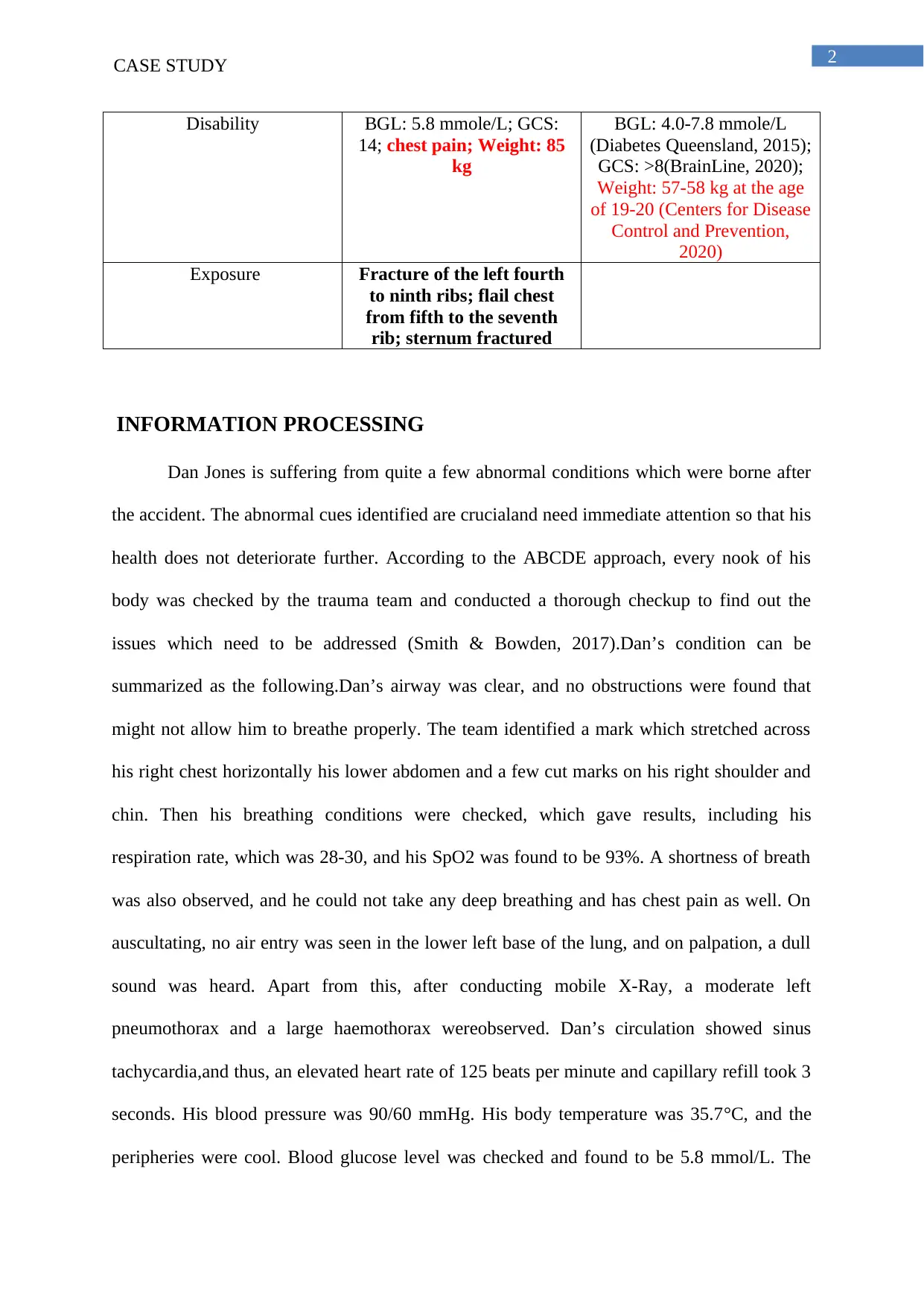
Disability BGL: 5.8 mmole/L; GCS:
14; chest pain; Weight: 85
kg
BGL: 4.0-7.8 mmole/L
(Diabetes Queensland, 2015);
GCS: >8(BrainLine, 2020);
Weight: 57-58 kg at the age
of 19-20 (Centers for Disease
Control and Prevention,
2020)
Exposure Fracture of the left fourth
to ninth ribs; flail chest
from fifth to the seventh
rib; sternum fractured
INFORMATION PROCESSING
Dan Jones is suffering from quite a few abnormal conditions which were borne after
the accident. The abnormal cues identified are crucialand need immediate attention so that his
health does not deteriorate further. According to the ABCDE approach, every nook of his
body was checked by the trauma team and conducted a thorough checkup to find out the
issues which need to be addressed (Smith & Bowden, 2017).Dan’s condition can be
summarized as the following.Dan’s airway was clear, and no obstructions were found that
might not allow him to breathe properly. The team identified a mark which stretched across
his right chest horizontally his lower abdomen and a few cut marks on his right shoulder and
chin. Then his breathing conditions were checked, which gave results, including his
respiration rate, which was 28-30, and his SpO2 was found to be 93%. A shortness of breath
was also observed, and he could not take any deep breathing and has chest pain as well. On
auscultating, no air entry was seen in the lower left base of the lung, and on palpation, a dull
sound was heard. Apart from this, after conducting mobile X-Ray, a moderate left
pneumothorax and a large haemothorax wereobserved. Dan’s circulation showed sinus
tachycardia,and thus, an elevated heart rate of 125 beats per minute and capillary refill took 3
seconds. His blood pressure was 90/60 mmHg. His body temperature was 35.7°C, and the
peripheries were cool. Blood glucose level was checked and found to be 5.8 mmol/L. The
Disability BGL: 5.8 mmole/L; GCS:
14; chest pain; Weight: 85
kg
BGL: 4.0-7.8 mmole/L
(Diabetes Queensland, 2015);
GCS: >8(BrainLine, 2020);
Weight: 57-58 kg at the age
of 19-20 (Centers for Disease
Control and Prevention,
2020)
Exposure Fracture of the left fourth
to ninth ribs; flail chest
from fifth to the seventh
rib; sternum fractured
INFORMATION PROCESSING
Dan Jones is suffering from quite a few abnormal conditions which were borne after
the accident. The abnormal cues identified are crucialand need immediate attention so that his
health does not deteriorate further. According to the ABCDE approach, every nook of his
body was checked by the trauma team and conducted a thorough checkup to find out the
issues which need to be addressed (Smith & Bowden, 2017).Dan’s condition can be
summarized as the following.Dan’s airway was clear, and no obstructions were found that
might not allow him to breathe properly. The team identified a mark which stretched across
his right chest horizontally his lower abdomen and a few cut marks on his right shoulder and
chin. Then his breathing conditions were checked, which gave results, including his
respiration rate, which was 28-30, and his SpO2 was found to be 93%. A shortness of breath
was also observed, and he could not take any deep breathing and has chest pain as well. On
auscultating, no air entry was seen in the lower left base of the lung, and on palpation, a dull
sound was heard. Apart from this, after conducting mobile X-Ray, a moderate left
pneumothorax and a large haemothorax wereobserved. Dan’s circulation showed sinus
tachycardia,and thus, an elevated heart rate of 125 beats per minute and capillary refill took 3
seconds. His blood pressure was 90/60 mmHg. His body temperature was 35.7°C, and the
peripheries were cool. Blood glucose level was checked and found to be 5.8 mmol/L. The
3CASE STUDY
summation of his health attributes in the Glasglow Coma Scale came out to be 14. The X-Ray
results also showed that his sternum was cracked, and fractures were observed from the
fourth left rib to the ninth rib.
Some attributes of Dan’s health are in the normal state. However, a few attributesof
Dan’s health are in serious condition. The abnormal cues include the respiration rate, heart
rate, blood pressure, capillary refill, which are found to be in a range that is much more than
the normal range. Apart from these health vitals, he is suffering from moderate left
pneumothorax and a large haemothorax. His left ribs from the fourth to the ninth is fractured,
his chest is injured from the fifth to seventh rib, and his sternum is also broken.
There arequite a few evidence that individualsmet with motor vehicle injury leads to
symptoms like elevated blood pressure, heart rate, and respiration rate, and they also have a
higher mortality rate (Bhandarkar et al., 2017). The other critical conditions Dan is having
include pneumothorax, haemothorax, flail chest, and sternum fracture.
Pneumothorax is a phenomenon where the pleural cavity around the lungs gets
connected with the pulmonary alveoli, and the inhaled air gets transferred from the alveoli to
the pleural cavity creating an equilibrium destroying the normal state where there is a
pressure difference. This condition decreases the capacity of the pulmonary alveoli by about
33%. The air which enters the pleural cavity makes way for itself by compressing the lungs
by 25%. This change in pressure elevates the volume of the thorax and alters the recoil
mechanism of the thoracic wall by creating a decrease in vital capacity by 8%. As the
pressure exerted on the pleural cavity increases gradually, the thorax of that side expands and
thus, the diaphragm gets much more depressed than the normal state (Choi, 2014).
Hemothorax is the condition in which blood gets accumulated in the pleural cavity. It
causes pain in the chest which ultimately leads to breathing problem and also increases the
summation of his health attributes in the Glasglow Coma Scale came out to be 14. The X-Ray
results also showed that his sternum was cracked, and fractures were observed from the
fourth left rib to the ninth rib.
Some attributes of Dan’s health are in the normal state. However, a few attributesof
Dan’s health are in serious condition. The abnormal cues include the respiration rate, heart
rate, blood pressure, capillary refill, which are found to be in a range that is much more than
the normal range. Apart from these health vitals, he is suffering from moderate left
pneumothorax and a large haemothorax. His left ribs from the fourth to the ninth is fractured,
his chest is injured from the fifth to seventh rib, and his sternum is also broken.
There arequite a few evidence that individualsmet with motor vehicle injury leads to
symptoms like elevated blood pressure, heart rate, and respiration rate, and they also have a
higher mortality rate (Bhandarkar et al., 2017). The other critical conditions Dan is having
include pneumothorax, haemothorax, flail chest, and sternum fracture.
Pneumothorax is a phenomenon where the pleural cavity around the lungs gets
connected with the pulmonary alveoli, and the inhaled air gets transferred from the alveoli to
the pleural cavity creating an equilibrium destroying the normal state where there is a
pressure difference. This condition decreases the capacity of the pulmonary alveoli by about
33%. The air which enters the pleural cavity makes way for itself by compressing the lungs
by 25%. This change in pressure elevates the volume of the thorax and alters the recoil
mechanism of the thoracic wall by creating a decrease in vital capacity by 8%. As the
pressure exerted on the pleural cavity increases gradually, the thorax of that side expands and
thus, the diaphragm gets much more depressed than the normal state (Choi, 2014).
Hemothorax is the condition in which blood gets accumulated in the pleural cavity. It
causes pain in the chest which ultimately leads to breathing problem and also increases the
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4CASE STUDY
heart rate rapidly. This might be the reason for Dan’s increased heart rate (Gomez & Vu,
2019).
Flail chest is the condition in which rib segments get broken and detached from the
rib cage due to injury. The detached part freely moves around the chest region because of
difference in pressure. This might give rise to newer complications if the broken segment is
sharp it might puncture various other organs like the lungs or pleural cavity and might also
give rise to pneumothorax. It causes breath shortness and pain in the chest. This might also
explain the reason for Dan’s pneumothorax, chest pain and shortness of breathing (Dehghan
et al., 2014).
Fracture in the sternum is an adverse medical condition that is life threatening and
generally occurs during car crashes either by hitting the chest in the driving wheel or
dashboard or by the attachment of seatbelt. It also causes shortness of breath and pain in the
chest (Tiwari, Nair & Baker, 2015).
CRITICAL PROBLEMS, INTERVENTIONS AND RATIONALE
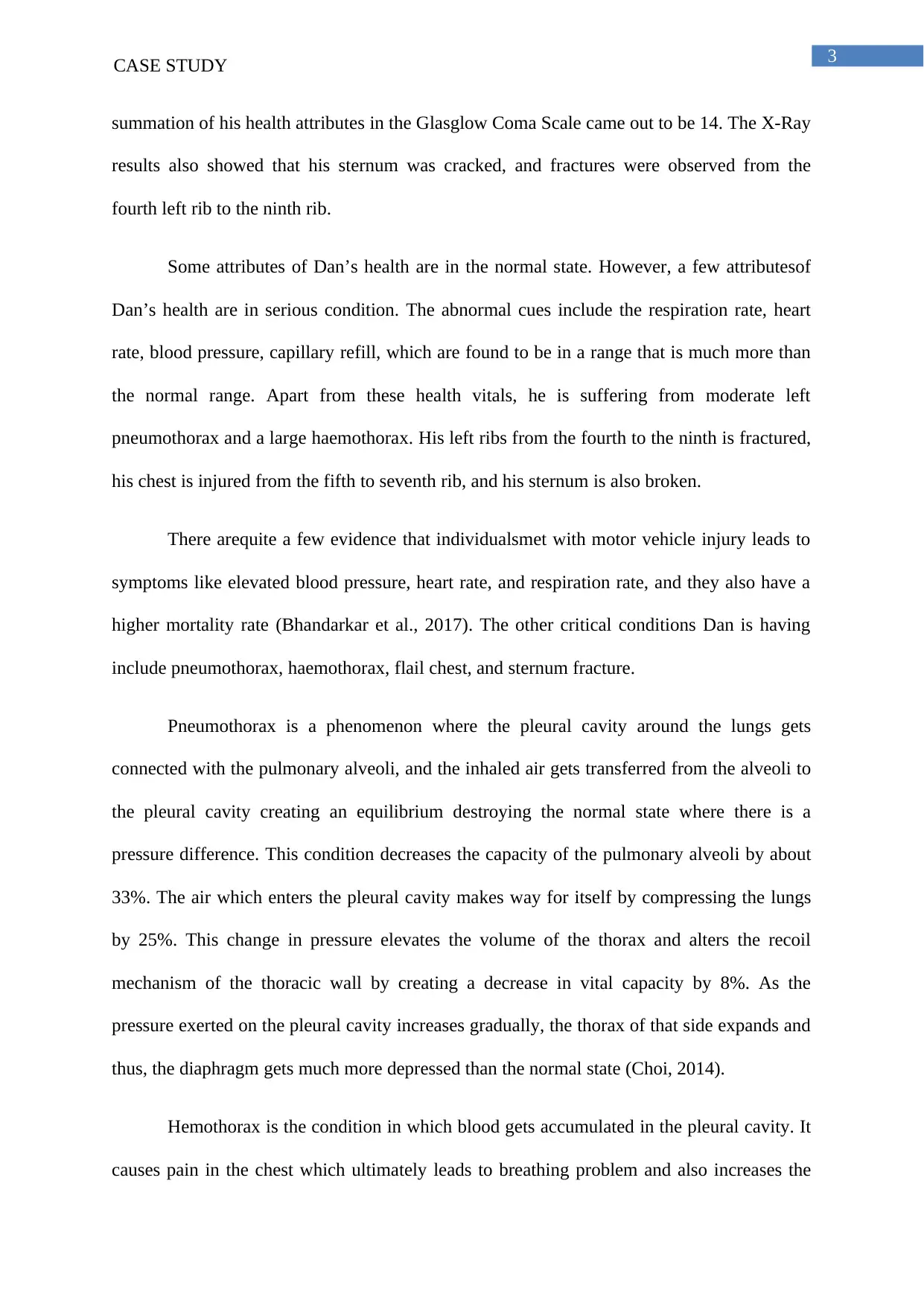
According to the Nursing Diagnosis Framework, the patient’s condition must be
assessed based on the cues collected earlier (NANDA. International, 2014). The priorities of
care was assessed and interventions were planned as follows.
CRITICAL PROBLEMS INTERVENTIONS RATIONALE
The most critical problem is
patient is suffering from a
hemothorax that signifies
that the patient’s chest is
filling up with blood. The
patient also has moderate
pneumothorax.
Haemothorax can prove to
be fatal very quickly due to
rapid blood loss.
Haemothorax and
The primary work of the
nursing staff is to drain
Dan’s chest to remove the
blood that has collected
there. This is extremely
important as this reduces
the pressure on the lung,
enabling Dan to breathe
properly. This is done by
inserting a tube through the
chest muscles and tissues to
The chest drain must be
used to stabilize the patient
in case of the haemothorax.
In this case, a tube is
inserted through the chest
muscles and tissues to drain
the fluid in the lungs.
Haemothorax causes blood
to build up in the pleural
cavity, which exerts
pressure on the lung and in
heart rate rapidly. This might be the reason for Dan’s increased heart rate (Gomez & Vu,
2019).
Flail chest is the condition in which rib segments get broken and detached from the
rib cage due to injury. The detached part freely moves around the chest region because of
difference in pressure. This might give rise to newer complications if the broken segment is
sharp it might puncture various other organs like the lungs or pleural cavity and might also
give rise to pneumothorax. It causes breath shortness and pain in the chest. This might also
explain the reason for Dan’s pneumothorax, chest pain and shortness of breathing (Dehghan
et al., 2014).
Fracture in the sternum is an adverse medical condition that is life threatening and
generally occurs during car crashes either by hitting the chest in the driving wheel or
dashboard or by the attachment of seatbelt. It also causes shortness of breath and pain in the
chest (Tiwari, Nair & Baker, 2015).
CRITICAL PROBLEMS, INTERVENTIONS AND RATIONALE
According to the Nursing Diagnosis Framework, the patient’s condition must be
assessed based on the cues collected earlier (NANDA. International, 2014). The priorities of
care was assessed and interventions were planned as follows.
CRITICAL PROBLEMS INTERVENTIONS RATIONALE
The most critical problem is
patient is suffering from a
hemothorax that signifies
that the patient’s chest is
filling up with blood. The
patient also has moderate
pneumothorax.
Haemothorax can prove to
be fatal very quickly due to
rapid blood loss.
Haemothorax and
The primary work of the
nursing staff is to drain
Dan’s chest to remove the
blood that has collected
there. This is extremely
important as this reduces
the pressure on the lung,
enabling Dan to breathe
properly. This is done by
inserting a tube through the
chest muscles and tissues to
The chest drain must be
used to stabilize the patient
in case of the haemothorax.
In this case, a tube is
inserted through the chest
muscles and tissues to drain
the fluid in the lungs.
Haemothorax causes blood
to build up in the pleural
cavity, which exerts
pressure on the lung and in
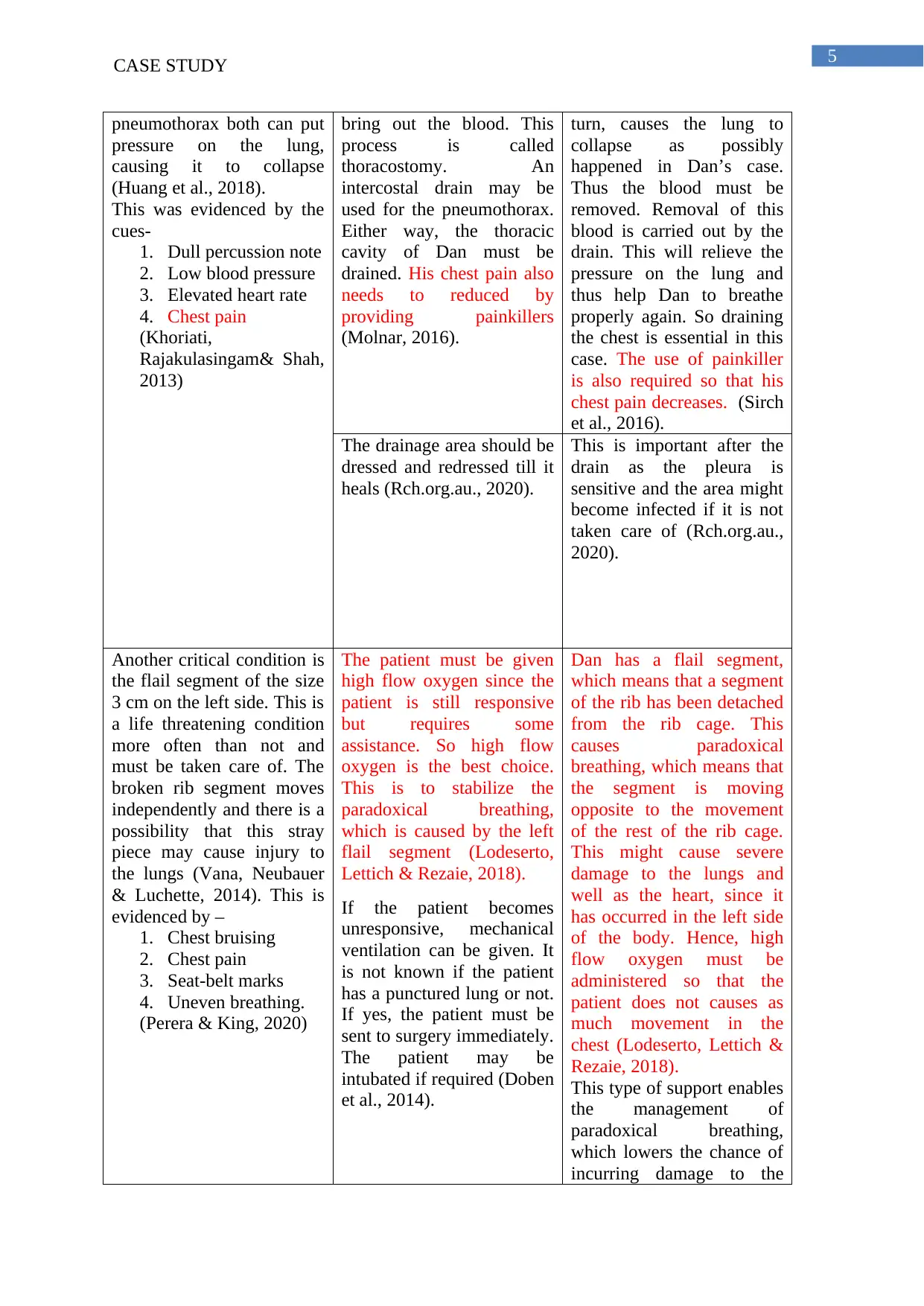
5CASE STUDY
pneumothorax both can put
pressure on the lung,
causing it to collapse
(Huang et al., 2018).
This was evidenced by the
cues-
1. Dull percussion note
2. Low blood pressure
3. Elevated heart rate
4. Chest pain
(Khoriati,
Rajakulasingam& Shah,
2013)
bring out the blood. This
process is called
thoracostomy. An
intercostal drain may be
used for the pneumothorax.
Either way, the thoracic
cavity of Dan must be
drained. His chest pain also
needs to reduced by
providing painkillers
(Molnar, 2016).
turn, causes the lung to
collapse as possibly
happened in Dan’s case.
Thus the blood must be
removed. Removal of this
blood is carried out by the
drain. This will relieve the
pressure on the lung and
thus help Dan to breathe
properly again. So draining
the chest is essential in this
case. The use of painkiller
is also required so that his
chest pain decreases. (Sirch
et al., 2016).
The drainage area should be
dressed and redressed till it
heals (Rch.org.au., 2020).
This is important after the
drain as the pleura is
sensitive and the area might
become infected if it is not
taken care of (Rch.org.au.,
2020).
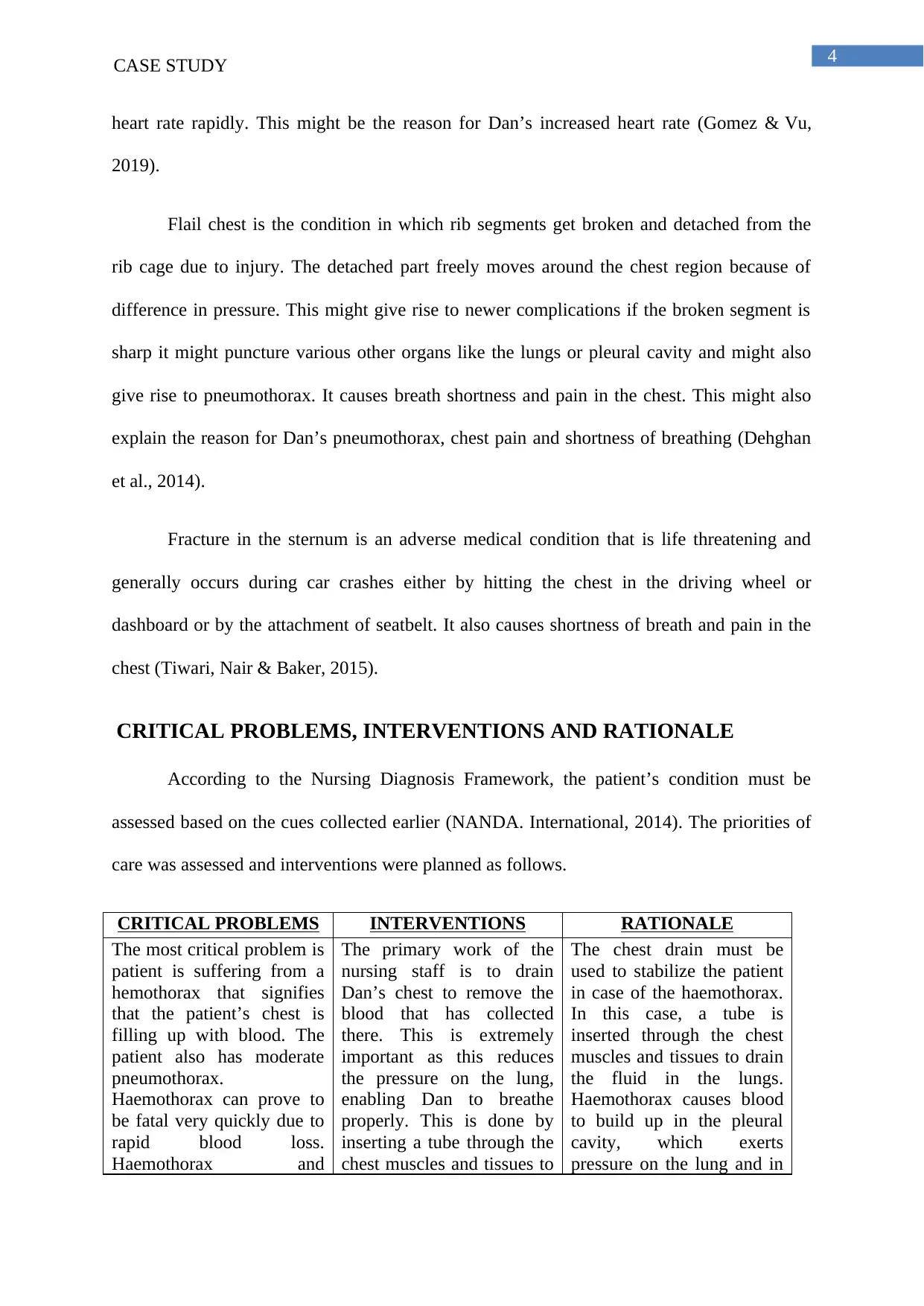
Another critical condition is
the flail segment of the size
3 cm on the left side. This is
a life threatening condition
more often than not and
must be taken care of. The
broken rib segment moves
independently and there is a
possibility that this stray
piece may cause injury to
the lungs (Vana, Neubauer
& Luchette, 2014). This is
evidenced by –
1. Chest bruising
2. Chest pain
3. Seat-belt marks
4. Uneven breathing.
(Perera & King, 2020)
The patient must be given
high flow oxygen since the
patient is still responsive
but requires some
assistance. So high flow
oxygen is the best choice.
This is to stabilize the
paradoxical breathing,
which is caused by the left
flail segment (Lodeserto,
Lettich & Rezaie, 2018).
If the patient becomes
unresponsive, mechanical
ventilation can be given. It
is not known if the patient
has a punctured lung or not.
If yes, the patient must be
sent to surgery immediately.
The patient may be
intubated if required (Doben
et al., 2014).
Dan has a flail segment,
which means that a segment
of the rib has been detached
from the rib cage. This
causes paradoxical
breathing, which means that
the segment is moving
opposite to the movement
of the rest of the rib cage.
This might cause severe
damage to the lungs and
well as the heart, since it
has occurred in the left side
of the body. Hence, high
flow oxygen must be
administered so that the
patient does not causes as
much movement in the
chest (Lodeserto, Lettich &
Rezaie, 2018).
This type of support enables
the management of
paradoxical breathing,
which lowers the chance of
incurring damage to the
pneumothorax both can put
pressure on the lung,
causing it to collapse
(Huang et al., 2018).
This was evidenced by the
cues-
1. Dull percussion note
2. Low blood pressure
3. Elevated heart rate
4. Chest pain
(Khoriati,
Rajakulasingam& Shah,
2013)
bring out the blood. This
process is called
thoracostomy. An
intercostal drain may be
used for the pneumothorax.
Either way, the thoracic
cavity of Dan must be
drained. His chest pain also
needs to reduced by
providing painkillers
(Molnar, 2016).
turn, causes the lung to
collapse as possibly
happened in Dan’s case.
Thus the blood must be
removed. Removal of this
blood is carried out by the
drain. This will relieve the
pressure on the lung and
thus help Dan to breathe
properly again. So draining
the chest is essential in this
case. The use of painkiller
is also required so that his
chest pain decreases. (Sirch
et al., 2016).
The drainage area should be
dressed and redressed till it
heals (Rch.org.au., 2020).
This is important after the
drain as the pleura is
sensitive and the area might
become infected if it is not
taken care of (Rch.org.au.,
2020).
Another critical condition is
the flail segment of the size
3 cm on the left side. This is
a life threatening condition
more often than not and
must be taken care of. The
broken rib segment moves
independently and there is a
possibility that this stray
piece may cause injury to
the lungs (Vana, Neubauer
& Luchette, 2014). This is
evidenced by –
1. Chest bruising
2. Chest pain
3. Seat-belt marks
4. Uneven breathing.
(Perera & King, 2020)
The patient must be given
high flow oxygen since the
patient is still responsive
but requires some
assistance. So high flow
oxygen is the best choice.
This is to stabilize the
paradoxical breathing,
which is caused by the left
flail segment (Lodeserto,
Lettich & Rezaie, 2018).
If the patient becomes
unresponsive, mechanical
ventilation can be given. It
is not known if the patient
has a punctured lung or not.
If yes, the patient must be
sent to surgery immediately.
The patient may be
intubated if required (Doben
et al., 2014).
Dan has a flail segment,
which means that a segment
of the rib has been detached
from the rib cage. This
causes paradoxical
breathing, which means that
the segment is moving
opposite to the movement
of the rest of the rib cage.
This might cause severe
damage to the lungs and
well as the heart, since it
has occurred in the left side
of the body. Hence, high
flow oxygen must be
administered so that the
patient does not causes as
much movement in the
chest (Lodeserto, Lettich &
Rezaie, 2018).
This type of support enables
the management of
paradoxical breathing,
which lowers the chance of
incurring damage to the
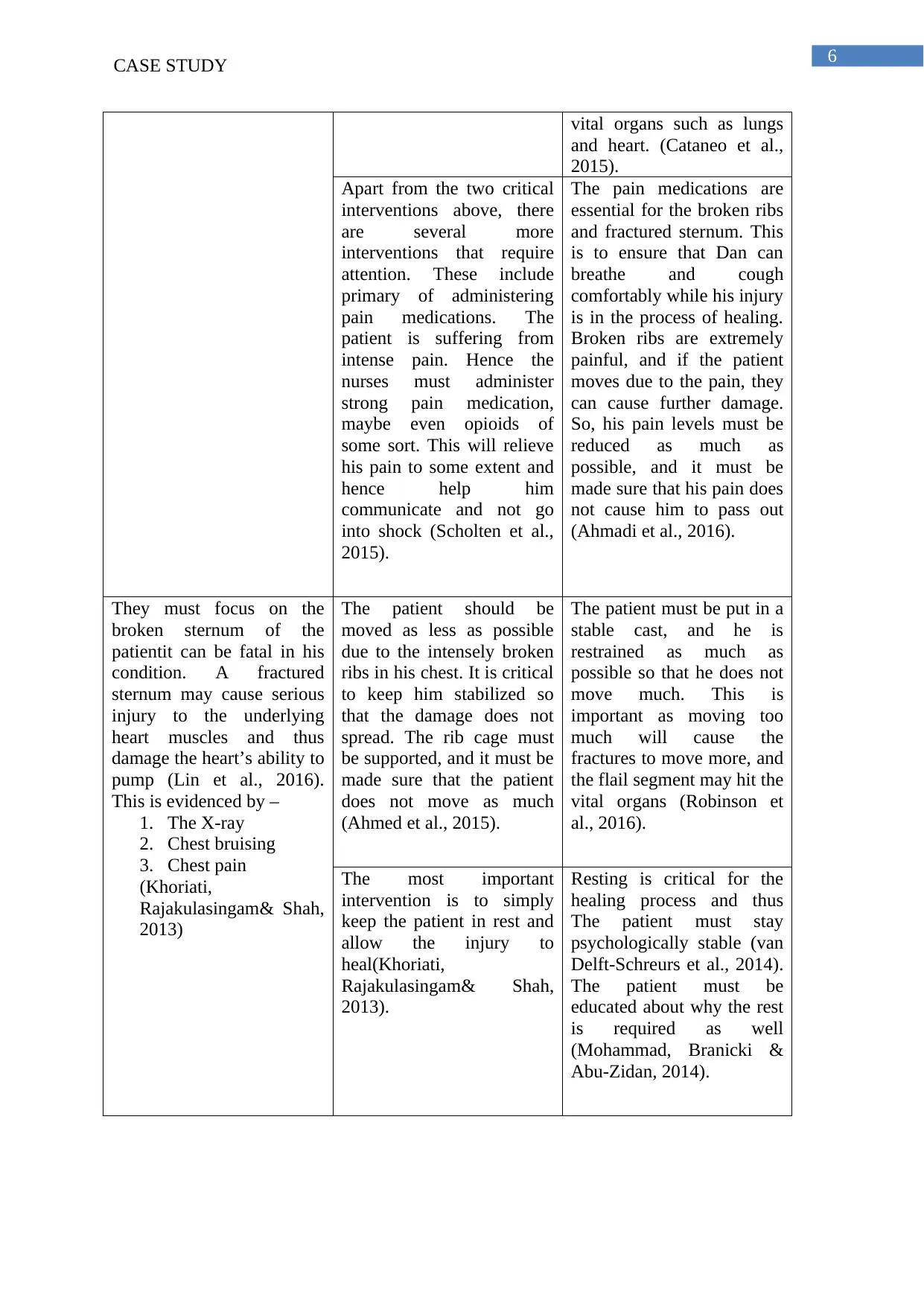
6CASE STUDY
vital organs such as lungs
and heart. (Cataneo et al.,
2015).
Apart from the two critical
interventions above, there
are several more
interventions that require
attention. These include
primary of administering
pain medications. The
patient is suffering from
intense pain. Hence the
nurses must administer
strong pain medication,
maybe even opioids of
some sort. This will relieve
his pain to some extent and
hence help him
communicate and not go
into shock (Scholten et al.,
2015).
The pain medications are
essential for the broken ribs
and fractured sternum. This
is to ensure that Dan can
breathe and cough
comfortably while his injury
is in the process of healing.
Broken ribs are extremely
painful, and if the patient
moves due to the pain, they
can cause further damage.
So, his pain levels must be
reduced as much as
possible, and it must be
made sure that his pain does
not cause him to pass out
(Ahmadi et al., 2016).
They must focus on the
broken sternum of the
patientit can be fatal in his
condition. A fractured
sternum may cause serious
injury to the underlying
heart muscles and thus
damage the heart’s ability to
pump (Lin et al., 2016).
This is evidenced by –
1. The X-ray
2. Chest bruising
3. Chest pain
(Khoriati,
Rajakulasingam& Shah,
2013)
The patient should be
moved as less as possible
due to the intensely broken
ribs in his chest. It is critical
to keep him stabilized so
that the damage does not
spread. The rib cage must
be supported, and it must be
made sure that the patient
does not move as much
(Ahmed et al., 2015).
The patient must be put in a
stable cast, and he is
restrained as much as
possible so that he does not
move much. This is
important as moving too
much will cause the
fractures to move more, and
the flail segment may hit the
vital organs (Robinson et
al., 2016).
The most important
intervention is to simply
keep the patient in rest and
allow the injury to
heal(Khoriati,
Rajakulasingam& Shah,
2013).
Resting is critical for the
healing process and thus
The patient must stay
psychologically stable (van
Delft-Schreurs et al., 2014).
The patient must be
educated about why the rest
is required as well
(Mohammad, Branicki &
Abu-Zidan, 2014).
vital organs such as lungs
and heart. (Cataneo et al.,
2015).
Apart from the two critical
interventions above, there
are several more
interventions that require
attention. These include
primary of administering
pain medications. The
patient is suffering from
intense pain. Hence the
nurses must administer
strong pain medication,
maybe even opioids of
some sort. This will relieve
his pain to some extent and
hence help him
communicate and not go
into shock (Scholten et al.,
2015).
The pain medications are
essential for the broken ribs
and fractured sternum. This
is to ensure that Dan can
breathe and cough
comfortably while his injury
is in the process of healing.
Broken ribs are extremely
painful, and if the patient
moves due to the pain, they
can cause further damage.
So, his pain levels must be
reduced as much as
possible, and it must be
made sure that his pain does
not cause him to pass out
(Ahmadi et al., 2016).
They must focus on the
broken sternum of the
patientit can be fatal in his
condition. A fractured
sternum may cause serious
injury to the underlying
heart muscles and thus
damage the heart’s ability to
pump (Lin et al., 2016).
This is evidenced by –
1. The X-ray
2. Chest bruising
3. Chest pain
(Khoriati,
Rajakulasingam& Shah,
2013)
The patient should be
moved as less as possible
due to the intensely broken
ribs in his chest. It is critical
to keep him stabilized so
that the damage does not
spread. The rib cage must
be supported, and it must be
made sure that the patient
does not move as much
(Ahmed et al., 2015).
The patient must be put in a
stable cast, and he is
restrained as much as
possible so that he does not
move much. This is
important as moving too
much will cause the
fractures to move more, and
the flail segment may hit the
vital organs (Robinson et
al., 2016).
The most important
intervention is to simply
keep the patient in rest and
allow the injury to
heal(Khoriati,
Rajakulasingam& Shah,
2013).
Resting is critical for the
healing process and thus
The patient must stay
psychologically stable (van
Delft-Schreurs et al., 2014).
The patient must be
educated about why the rest
is required as well
(Mohammad, Branicki &
Abu-Zidan, 2014).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7CASE STUDY
OUTCOME
It can be expected that after the care has been administered, the patient will be
stabilized. The patient should be able to breathe on his own without any difficulty and
without causing any harm to his vital organs. His vitals should go back to a comparatively
normal range. The patient would likely require the pain medication for an extended period, at
least till the injuries are fully healed. The patient should be asked whether he can feel any
pain or not, and he should be out of danger. His collapsed lung should be fixed, and his chest
should be stabilized. The patient’s respiration rate and heart rate should come down to
normal, i.e., 12-25 and 60-100, respectively (Caetano & Alves, 2015).
OUTCOME
It can be expected that after the care has been administered, the patient will be
stabilized. The patient should be able to breathe on his own without any difficulty and
without causing any harm to his vital organs. His vitals should go back to a comparatively
normal range. The patient would likely require the pain medication for an extended period, at
least till the injuries are fully healed. The patient should be asked whether he can feel any
pain or not, and he should be out of danger. His collapsed lung should be fixed, and his chest
should be stabilized. The patient’s respiration rate and heart rate should come down to
normal, i.e., 12-25 and 60-100, respectively (Caetano & Alves, 2015).
8CASE STUDY
REFERENCES
Ahmadi, A., Bazargan-Hejazi, S., Zadie, Z. H., Euasobhon, P., Ketumarn, P., Karbasfrushan,
A., & Mohammadi, R. (2016). Pain management in trauma: A review study. Journal
of Injury and Violence Research, 8(2), 89.
Ahmed, S. M., Athar, M., Ali, S., Doley, K., Siddiqi, O. A., & Usmani, H. (2015). Acute pain
services in flail chest-a prospective randomized trial of epidural versus parenteral
analgesia in mechanically ventilated ICU patients. Egyptian Journal of
Anaesthesia, 31(4), 327-330.
Bhandarkar, P., Munivenkatappa, A., Roy, N., Kumar, V., Samudrala, V. D., Kamble, J., &
Agrawal, A. (2017). On-admission blood pressure and pulse rate in trauma patients
and their correlation with mortality: Cushing's phenomenon revisited. International
journal of critical illness and injury science, 7(1), 14.
BrainLine. (2020). What Is the Glasgow Coma Scale? | BrainLine. BrainLine. Retrieved 14
March 2020, from https://www.brainline.org/article/what-glasgow-coma-scale.
Cataneo, A. J. M., Cataneo, D. C., de Oliveira, F. H., Arruda, K. A., El Dib, R., & de Oliveira
Carvalho, P. E. (2015). Surgical versus nonsurgical interventions for flail
chest. Cochrane Database of Systematic Reviews, (7).
Centers for Disease Control and Prevention. (2020). Height & Weight. Retrieved 22 March
2020, from https://www.cdc.gov/growthcharts/data/set1clinical/cj41l021.pdf
Choi, W. I. (2014). Pneumothorax. Tuberculosis and respiratory diseases, 76(3), 99-104.
Cleveland Clinic. (2020). Vital Signs. Cleveland Clinic. Retrieved 14 March 2020, from
https://my.clevelandclinic.org/health/articles/10881-vital-signs.
REFERENCES
Ahmadi, A., Bazargan-Hejazi, S., Zadie, Z. H., Euasobhon, P., Ketumarn, P., Karbasfrushan,
A., & Mohammadi, R. (2016). Pain management in trauma: A review study. Journal
of Injury and Violence Research, 8(2), 89.
Ahmed, S. M., Athar, M., Ali, S., Doley, K., Siddiqi, O. A., & Usmani, H. (2015). Acute pain
services in flail chest-a prospective randomized trial of epidural versus parenteral
analgesia in mechanically ventilated ICU patients. Egyptian Journal of
Anaesthesia, 31(4), 327-330.
Bhandarkar, P., Munivenkatappa, A., Roy, N., Kumar, V., Samudrala, V. D., Kamble, J., &
Agrawal, A. (2017). On-admission blood pressure and pulse rate in trauma patients
and their correlation with mortality: Cushing's phenomenon revisited. International
journal of critical illness and injury science, 7(1), 14.
BrainLine. (2020). What Is the Glasgow Coma Scale? | BrainLine. BrainLine. Retrieved 14
March 2020, from https://www.brainline.org/article/what-glasgow-coma-scale.
Cataneo, A. J. M., Cataneo, D. C., de Oliveira, F. H., Arruda, K. A., El Dib, R., & de Oliveira
Carvalho, P. E. (2015). Surgical versus nonsurgical interventions for flail
chest. Cochrane Database of Systematic Reviews, (7).
Centers for Disease Control and Prevention. (2020). Height & Weight. Retrieved 22 March
2020, from https://www.cdc.gov/growthcharts/data/set1clinical/cj41l021.pdf
Choi, W. I. (2014). Pneumothorax. Tuberculosis and respiratory diseases, 76(3), 99-104.
Cleveland Clinic. (2020). Vital Signs. Cleveland Clinic. Retrieved 14 March 2020, from
https://my.clevelandclinic.org/health/articles/10881-vital-signs.
9CASE STUDY
Dehghan, N., De Mestral, C., McKee, M. D., Schemitsch, E. H., & Nathens, A. (2014). Flail
chest injuries: a review of outcomes and treatment practices from the National
Trauma Data Bank. Journal of Trauma and Acute Care Surgery, 76(2), 462-468.
Diabetes Queensland. (2015). What’s the ‘right’ range of BGLs?. Diabetes Queensland.
Retrieved 14 March 2020, from
https://www.diabetesqld.org.au/media-centre/2015/november/right-range-of-
bgls.aspx.
Doben, A. R., Eriksson, E. A., Denlinger, C. E., Leon, S. M., Couillard, D. J., Fakhry, S. M.,
& Minshall, C. T. (2014). Surgical rib fixation for flail chest deformity improves
liberation from mechanical ventilation. Journal of critical care, 29(1), 139-143.
Durlinger, E. M. J., Spoelstra-de Man, A. M. E., Smit, B., de Grooth, H. J., Girbes, A. R. J.,
Oudemans-van Straaten, H. M., & Smulders, Y. M. (2017). Hyperoxia: At what level
of SpO2 is a patient safe? A study in mechanically ventilated ICU patients. Journal of
critical care, 39, 199-204.
Huang, F. D., Yeh, W. B., Chen, S. S., Liu, Y. Y., Lu, I. Y., Chou, Y. P., & Wu, T. C. (2018).
Early management of retained hemothorax in blunt head and chest trauma. World
journal of surgery, 42(7), 2061-2066.
Khoriati, A. A., Rajakulasingam, R., & Shah, R. (2013). Sternal fractures and their
management. Journal of emergencies, trauma, and shock, 6(2), 113.
King, D., Morton, R., & Bevan, C. (2014). How to use capillary refill time. Archives of
Disease in Childhood-Education and Practice, 99(3), 111-116.
Laura Pumarejo Gomez; Vu H. Tran. 2019. Hemothorax. Aventura Hospital and Medical
Center.
Dehghan, N., De Mestral, C., McKee, M. D., Schemitsch, E. H., & Nathens, A. (2014). Flail
chest injuries: a review of outcomes and treatment practices from the National
Trauma Data Bank. Journal of Trauma and Acute Care Surgery, 76(2), 462-468.
Diabetes Queensland. (2015). What’s the ‘right’ range of BGLs?. Diabetes Queensland.
Retrieved 14 March 2020, from
https://www.diabetesqld.org.au/media-centre/2015/november/right-range-of-
bgls.aspx.
Doben, A. R., Eriksson, E. A., Denlinger, C. E., Leon, S. M., Couillard, D. J., Fakhry, S. M.,
& Minshall, C. T. (2014). Surgical rib fixation for flail chest deformity improves
liberation from mechanical ventilation. Journal of critical care, 29(1), 139-143.
Durlinger, E. M. J., Spoelstra-de Man, A. M. E., Smit, B., de Grooth, H. J., Girbes, A. R. J.,
Oudemans-van Straaten, H. M., & Smulders, Y. M. (2017). Hyperoxia: At what level
of SpO2 is a patient safe? A study in mechanically ventilated ICU patients. Journal of
critical care, 39, 199-204.
Huang, F. D., Yeh, W. B., Chen, S. S., Liu, Y. Y., Lu, I. Y., Chou, Y. P., & Wu, T. C. (2018).
Early management of retained hemothorax in blunt head and chest trauma. World
journal of surgery, 42(7), 2061-2066.
Khoriati, A. A., Rajakulasingam, R., & Shah, R. (2013). Sternal fractures and their
management. Journal of emergencies, trauma, and shock, 6(2), 113.
King, D., Morton, R., & Bevan, C. (2014). How to use capillary refill time. Archives of
Disease in Childhood-Education and Practice, 99(3), 111-116.
Laura Pumarejo Gomez; Vu H. Tran. 2019. Hemothorax. Aventura Hospital and Medical
Center.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10CASE STUDY
Lin, F. C. F., Li, R. Y., Tung, Y. W., Jeng, K. C., & Tsai, S. C. S. (2016). Morbidity,
mortality, associated injuries, and management of traumatic rib fractures. Journal of
the Chinese Medical Association, 79(6), 329-334.
Lodeserto, F. J., Lettich, T. M., & Rezaie, S. R. (2018). High-flow Nasal Cannula:
Mechanisms of Action and Adult and Pediatric Indications. Cureus, 10(11).
Mayo Clinic. (2020). 2 easy, accurate ways to measure your heart rate. Mayo Clinic.
Retrieved 14 March 2020, from
https://www.mayoclinic.org/healthy-lifestyle/fitness/expert-answers/heart-rate/faq-
20057979.
Mohammad, A., Branicki, F., & Abu-Zidan, F. M. (2014). Educational and clinical impact of
Advanced Trauma Life Support (ATLS) courses: a systematic review. World journal
of surgery, 38(2), 322-329.
Molnar, T. F. (2017). Thoracic Trauma: Which chest tube when and where?. Thoracic
surgery clinics, 27(1), 13-23.
NANDA. International. (2014). Nursing Diagnoses 2012-14: Definitions and Classification.
Wiley.
Perera, T., & King, K. (2020). Flail Chest. Ncbi.nlm.nih.gov. Retrieved 18 March 2020, from
https://www.ncbi.nlm.nih.gov/books/NBK534090/.
Rch.org.au. (2020). Clinical Guidelines (Nursing) : Chest drain management. Retrieved 18
March 2020, from
https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Chest_drain_manag
ement/.
Lin, F. C. F., Li, R. Y., Tung, Y. W., Jeng, K. C., & Tsai, S. C. S. (2016). Morbidity,
mortality, associated injuries, and management of traumatic rib fractures. Journal of
the Chinese Medical Association, 79(6), 329-334.
Lodeserto, F. J., Lettich, T. M., & Rezaie, S. R. (2018). High-flow Nasal Cannula:
Mechanisms of Action and Adult and Pediatric Indications. Cureus, 10(11).
Mayo Clinic. (2020). 2 easy, accurate ways to measure your heart rate. Mayo Clinic.
Retrieved 14 March 2020, from
https://www.mayoclinic.org/healthy-lifestyle/fitness/expert-answers/heart-rate/faq-
20057979.
Mohammad, A., Branicki, F., & Abu-Zidan, F. M. (2014). Educational and clinical impact of
Advanced Trauma Life Support (ATLS) courses: a systematic review. World journal
of surgery, 38(2), 322-329.
Molnar, T. F. (2017). Thoracic Trauma: Which chest tube when and where?. Thoracic
surgery clinics, 27(1), 13-23.
NANDA. International. (2014). Nursing Diagnoses 2012-14: Definitions and Classification.
Wiley.
Perera, T., & King, K. (2020). Flail Chest. Ncbi.nlm.nih.gov. Retrieved 18 March 2020, from
https://www.ncbi.nlm.nih.gov/books/NBK534090/.
Rch.org.au. (2020). Clinical Guidelines (Nursing) : Chest drain management. Retrieved 18
March 2020, from
https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Chest_drain_manag
ement/.
11CASE STUDY
Resuscitation Council. (2020). ABCDE approach. Resus.org.uk. Retrieved 14 March 2020,
from https://www.resus.org.uk/resuscitation-guidelines/abcde-approach/.
Robinson, L. A., & Grubbs, D. M. (2016). Using “Rebar” to Stabilize Rigid Chest Wall
Reconstruction. The Thoracic and cardiovascular surgeon, 64(03), 266-269.
Scholten, A. C., Berben, S. A. A., Westmaas, A. H., van Grunsven, P. M., de Vaal, E. T.,
Rood, P. P., & Emergency Pain Study Group. (2015). Pain management in trauma
patients in (pre) hospital based emergency care: current practice versus new
guideline. Injury, 46(5), 798-806.
Sirch, J., Ledwon, M., Püski, T., Boyle, E. M., Pfeiffer, S., & Fischlein, T. (2016). Active
clearance of chest drainage catheters reduces retained blood. The Journal of thoracic
and cardiovascular surgery, 151(3), 832-838.
Smith, D., & Bowden, T. (2017). Using the ABCDE approach to assess the deteriorating
patient. Nursing Standard (2014+), 32(14), 51.
Steinhausen, S., Ommen, O., Thüm, S., Lefering, R., Koehler, T., Neugebauer, E., & Pfaff,
H. (2014). Physician empathy and subjective evaluation of medical treatment outcome
in trauma surgery patients. Patient education and counseling, 95(1), 53-60.
The Heart Foundation. (2020). Is my blood pressure normal?. The Heart Foundation.
Retrieved 14 March 2020, from https://www.heartfoundation.org.au/your-heart/know-
your-risks/blood-pressure/is-my-blood-pressure-normal.
Tiwari, A., Nair, S., & Baker, A. (2015). The pathophysiology of flail chest injury. In Injuries
to the Chest Wall (pp. 19-32). Springer, Cham.
Resuscitation Council. (2020). ABCDE approach. Resus.org.uk. Retrieved 14 March 2020,
from https://www.resus.org.uk/resuscitation-guidelines/abcde-approach/.
Robinson, L. A., & Grubbs, D. M. (2016). Using “Rebar” to Stabilize Rigid Chest Wall
Reconstruction. The Thoracic and cardiovascular surgeon, 64(03), 266-269.
Scholten, A. C., Berben, S. A. A., Westmaas, A. H., van Grunsven, P. M., de Vaal, E. T.,
Rood, P. P., & Emergency Pain Study Group. (2015). Pain management in trauma
patients in (pre) hospital based emergency care: current practice versus new
guideline. Injury, 46(5), 798-806.
Sirch, J., Ledwon, M., Püski, T., Boyle, E. M., Pfeiffer, S., & Fischlein, T. (2016). Active
clearance of chest drainage catheters reduces retained blood. The Journal of thoracic
and cardiovascular surgery, 151(3), 832-838.
Smith, D., & Bowden, T. (2017). Using the ABCDE approach to assess the deteriorating
patient. Nursing Standard (2014+), 32(14), 51.
Steinhausen, S., Ommen, O., Thüm, S., Lefering, R., Koehler, T., Neugebauer, E., & Pfaff,
H. (2014). Physician empathy and subjective evaluation of medical treatment outcome
in trauma surgery patients. Patient education and counseling, 95(1), 53-60.
The Heart Foundation. (2020). Is my blood pressure normal?. The Heart Foundation.
Retrieved 14 March 2020, from https://www.heartfoundation.org.au/your-heart/know-
your-risks/blood-pressure/is-my-blood-pressure-normal.
Tiwari, A., Nair, S., & Baker, A. (2015). The pathophysiology of flail chest injury. In Injuries
to the Chest Wall (pp. 19-32). Springer, Cham.
12CASE STUDY
van Delft-Schreurs, C. C. H. M., van Bergen, J. J. M., van de Sande, P., Verhofstad, M. H. J.,
De Vries, J., & de Jongh, M. A. C. (2014). A cross-sectional study of psychological
complaints and quality of life in severely injured patients. Quality of Life
Research, 23(4), 1353-1362.
Vana, P. G., Neubauer, D. C., & Luchette, F. A. (2014). Contemporary management of flail
chest. The American Surgeon, 80(6), 527-535.
van Delft-Schreurs, C. C. H. M., van Bergen, J. J. M., van de Sande, P., Verhofstad, M. H. J.,
De Vries, J., & de Jongh, M. A. C. (2014). A cross-sectional study of psychological
complaints and quality of life in severely injured patients. Quality of Life
Research, 23(4), 1353-1362.
Vana, P. G., Neubauer, D. C., & Luchette, F. A. (2014). Contemporary management of flail
chest. The American Surgeon, 80(6), 527-535.
1 out of 13
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.

