SBAR Implementation: Facilitating Safe Patient Information Transfer
VerifiedAdded on 2023/04/23
|12
|3841
|161
Literature Review
AI Summary
This literature review investigates the effectiveness of the SBAR (Situation, Background, Assessment, Recommendation) communication tool in facilitating prompt and safe transfer of critical patient information by healthcare professionals, aiming to reduce preventable errors. It highlights that communication breakdown is a major contributor to errors leading to patient harm and emphasizes SBAR's role in improving handover quality and patient safety across various departments such as anesthesia, emergency medicine, and pediatrics. The review analyzes studies that demonstrate SBAR's positive impact on communication, confidence, and quality of patient service, while also acknowledging challenges like its use in complex clinical scenarios and the need for educational training. The review concludes that SBAR is a valuable tool for enhancing communication and patient safety in healthcare settings, with recommendations for further research on its impact on patient outcomes and comparison with other communication frameworks.

Introduction
To deliver quality care, patient safety is one of the important aspect. WHO defined patient safety
as the decrease of risk of unnecessary harm related to healthcare to an appropriate minimum
(World Health Organisation, 2009). The effect of patient safety on the quality of healthcare is
frequently indicated by the occurrence of adverse events. One of the reports suggested that poor
communication is a source of adverse events in over 60% of all adverse events at the hospital
settings (The Joint Commission, 2014). Poor or ineffective communication can be seen in several
healthcare facilities and is specifically noticeable in patient hand-overs and in divisions where
quick and efficient management is crucial. These divisions include perioperative period, ICU and
the emergency departments. Communication has various elements and processes which are
complex and can be easily misunderstood. These barriers can be overcome by devising certain
communication strategies which are not time-consuming, do not require much effort and at the
same time offer detailed information effectively, promote inter-professional partnership and
restrict the likelihood of error. SBAR (situation, background, assessment, recommendation)
framework is a communication tool which fulfil these needs. Various derivatives of SBAR
include ISBAR, SBAR-R, ISBARR and ISOBAR. SBAR is used widely in a range of healthcare
settings as a communication and hand-off tool (Dossow & Zwissler, 2016). SBAR has a clear
structure which ensures delivery of all suitable information, planned in a logical manner. In
addition, it facilitates the preparation process prior to commencement of communication. SBAR
communication tool is currently considered the ‘best practice’ for provision of information in
critical situations. It is the gold standard handoff structure which was originally formulated and
used by the US Navy at the time of submarine duty handoff. In the SBAR communication tool S
is Situation which denotes the reason of calling the physician, B is for Background which
signifies the background information, A is the Assessment which refers to the assessment of the
issue and R is the Recommendation which is the way in which the problem should be corrected.
SBAR tool was first introduced in a healthcare facility at Kaiser Permanente in 2003 as a tool for
organizing the conversations between physicians and nurses regarding scenarios which needed
immediate attention. However, certain challenges in its use are also observed. This review is
conducted to evaluate and analyse the literature to find out the effectiveness of SBAR in
To deliver quality care, patient safety is one of the important aspect. WHO defined patient safety
as the decrease of risk of unnecessary harm related to healthcare to an appropriate minimum
(World Health Organisation, 2009). The effect of patient safety on the quality of healthcare is
frequently indicated by the occurrence of adverse events. One of the reports suggested that poor
communication is a source of adverse events in over 60% of all adverse events at the hospital
settings (The Joint Commission, 2014). Poor or ineffective communication can be seen in several
healthcare facilities and is specifically noticeable in patient hand-overs and in divisions where
quick and efficient management is crucial. These divisions include perioperative period, ICU and
the emergency departments. Communication has various elements and processes which are
complex and can be easily misunderstood. These barriers can be overcome by devising certain
communication strategies which are not time-consuming, do not require much effort and at the
same time offer detailed information effectively, promote inter-professional partnership and
restrict the likelihood of error. SBAR (situation, background, assessment, recommendation)
framework is a communication tool which fulfil these needs. Various derivatives of SBAR
include ISBAR, SBAR-R, ISBARR and ISOBAR. SBAR is used widely in a range of healthcare
settings as a communication and hand-off tool (Dossow & Zwissler, 2016). SBAR has a clear
structure which ensures delivery of all suitable information, planned in a logical manner. In
addition, it facilitates the preparation process prior to commencement of communication. SBAR
communication tool is currently considered the ‘best practice’ for provision of information in
critical situations. It is the gold standard handoff structure which was originally formulated and
used by the US Navy at the time of submarine duty handoff. In the SBAR communication tool S
is Situation which denotes the reason of calling the physician, B is for Background which
signifies the background information, A is the Assessment which refers to the assessment of the
issue and R is the Recommendation which is the way in which the problem should be corrected.
SBAR tool was first introduced in a healthcare facility at Kaiser Permanente in 2003 as a tool for
organizing the conversations between physicians and nurses regarding scenarios which needed
immediate attention. However, certain challenges in its use are also observed. This review is
conducted to evaluate and analyse the literature to find out the effectiveness of SBAR in
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
facilitating prompt and safe transfer of critical patient information by healthcare professional to
reduce preventable errors.
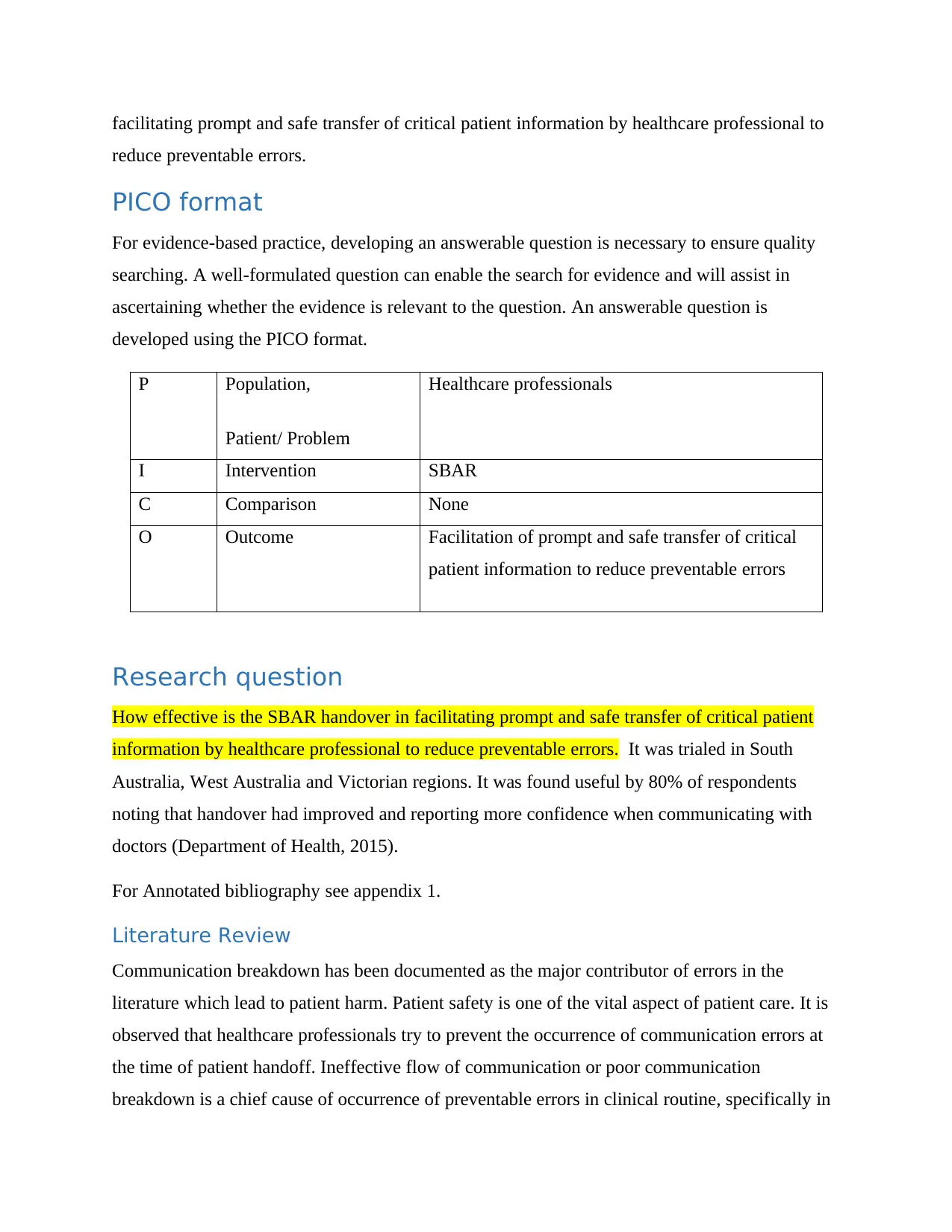
PICO format
For evidence-based practice, developing an answerable question is necessary to ensure quality
searching. A well-formulated question can enable the search for evidence and will assist in
ascertaining whether the evidence is relevant to the question. An answerable question is
developed using the PICO format.
P Population,
Patient/ Problem
Healthcare professionals
I Intervention SBAR
C Comparison None
O Outcome Facilitation of prompt and safe transfer of critical
patient information to reduce preventable errors
Research question
How effective is the SBAR handover in facilitating prompt and safe transfer of critical patient
information by healthcare professional to reduce preventable errors. It was trialed in South
Australia, West Australia and Victorian regions. It was found useful by 80% of respondents
noting that handover had improved and reporting more confidence when communicating with
doctors (Department of Health, 2015).
For Annotated bibliography see appendix 1.
Literature Review
Communication breakdown has been documented as the major contributor of errors in the
literature which lead to patient harm. Patient safety is one of the vital aspect of patient care. It is
observed that healthcare professionals try to prevent the occurrence of communication errors at
the time of patient handoff. Ineffective flow of communication or poor communication
breakdown is a chief cause of occurrence of preventable errors in clinical routine, specifically in
reduce preventable errors.
PICO format
For evidence-based practice, developing an answerable question is necessary to ensure quality
searching. A well-formulated question can enable the search for evidence and will assist in
ascertaining whether the evidence is relevant to the question. An answerable question is
developed using the PICO format.
P Population,
Patient/ Problem
Healthcare professionals
I Intervention SBAR
C Comparison None
O Outcome Facilitation of prompt and safe transfer of critical
patient information to reduce preventable errors
Research question
How effective is the SBAR handover in facilitating prompt and safe transfer of critical patient
information by healthcare professional to reduce preventable errors. It was trialed in South
Australia, West Australia and Victorian regions. It was found useful by 80% of respondents
noting that handover had improved and reporting more confidence when communicating with
doctors (Department of Health, 2015).
For Annotated bibliography see appendix 1.
Literature Review
Communication breakdown has been documented as the major contributor of errors in the
literature which lead to patient harm. Patient safety is one of the vital aspect of patient care. It is
observed that healthcare professionals try to prevent the occurrence of communication errors at
the time of patient handoff. Ineffective flow of communication or poor communication
breakdown is a chief cause of occurrence of preventable errors in clinical routine, specifically in
handover. SBAR is recommended by the WHO, the Joint Commission, Agency for Healthcare
Research and Quality (AHRQ) and Institute for Health Care Improvement (IHI) as a useful
communication tool during patient handoff. SBAR assists in communicating important
information in an organized and systematic manner which needs immediate notice and action.
Therefore, it contributes to successful escalation of management and improved patient safety.
SBAR has been found to be effective in increasing the handover quality and patient safety. On
reviewing the literature SBAR tool during was found effective for handoff in a range of
departments which include anesthesia (Randmaa, Swenne, Mårtensson, Högberg, & Engström,
2016), perioperative medicine (Merkel & Zwißler, 2017), postoperative medicine (Fabila, et al.,
2016), obstetrics (Scott, 2016), emergency medicine (Ozekcin, Tuite, Willner, & Hravnak,
2015), acute care medicine (Panesar, Albert, Messina, & Parker, 2016), pediatrics (Kotsakis,
Mercer, Mohseni-Bod, Gaiteiro, & Agbeko, 2015), and neonatology (Raymond & Harrison, The
structured communication tool SBAR (Situation, Background, Assessment and
Recommendation) improves communication in neonatology, 2014).
A review was conducted to identify the effect of application of SBAR on patient safety. It
revealed moderate evidence in terms of improvement of patient safety on using SBAR
particularly when it was utilized to organize communication over telephone. But the review has
the limitation of high-quality research which can serve as strong evidence for the effectiveness of
SBAR. The review highlighted that SBAR can be an adaptive means that is appropriate for
various healthcare settings, especially where clear and efficient interpersonal communication is
needed (Müller, et al., 2018). Another study was conducted ascertain the efficiency of
implementing the SBAR tool in an acute clinical facility in South Africa. It was done through
telephone audit which showed a surge in the use of SBAR by registrars from 29% to 70% when
calling consultants for assistance. Most of the staff after receiving training established that SBAR
assisted in communication, confidence, and quality of patient service. Qualitative evidence was
found that SBAR resulted in increased promptness in providing care to the acutely sick
patients. So, the study concluded that by implementing SBAR, communication between
professionals can be improved and enhanced quality and safety of patient can be achieved. The
study recommended the introduction of the tool in other health settings of South Africa
(Raymond, & Harrison, 2014)
Research and Quality (AHRQ) and Institute for Health Care Improvement (IHI) as a useful
communication tool during patient handoff. SBAR assists in communicating important
information in an organized and systematic manner which needs immediate notice and action.
Therefore, it contributes to successful escalation of management and improved patient safety.
SBAR has been found to be effective in increasing the handover quality and patient safety. On
reviewing the literature SBAR tool during was found effective for handoff in a range of
departments which include anesthesia (Randmaa, Swenne, Mårtensson, Högberg, & Engström,
2016), perioperative medicine (Merkel & Zwißler, 2017), postoperative medicine (Fabila, et al.,
2016), obstetrics (Scott, 2016), emergency medicine (Ozekcin, Tuite, Willner, & Hravnak,
2015), acute care medicine (Panesar, Albert, Messina, & Parker, 2016), pediatrics (Kotsakis,
Mercer, Mohseni-Bod, Gaiteiro, & Agbeko, 2015), and neonatology (Raymond & Harrison, The
structured communication tool SBAR (Situation, Background, Assessment and
Recommendation) improves communication in neonatology, 2014).
A review was conducted to identify the effect of application of SBAR on patient safety. It
revealed moderate evidence in terms of improvement of patient safety on using SBAR
particularly when it was utilized to organize communication over telephone. But the review has
the limitation of high-quality research which can serve as strong evidence for the effectiveness of
SBAR. The review highlighted that SBAR can be an adaptive means that is appropriate for
various healthcare settings, especially where clear and efficient interpersonal communication is
needed (Müller, et al., 2018). Another study was conducted ascertain the efficiency of
implementing the SBAR tool in an acute clinical facility in South Africa. It was done through
telephone audit which showed a surge in the use of SBAR by registrars from 29% to 70% when
calling consultants for assistance. Most of the staff after receiving training established that SBAR
assisted in communication, confidence, and quality of patient service. Qualitative evidence was
found that SBAR resulted in increased promptness in providing care to the acutely sick
patients. So, the study concluded that by implementing SBAR, communication between
professionals can be improved and enhanced quality and safety of patient can be achieved. The
study recommended the introduction of the tool in other health settings of South Africa
(Raymond, & Harrison, 2014)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
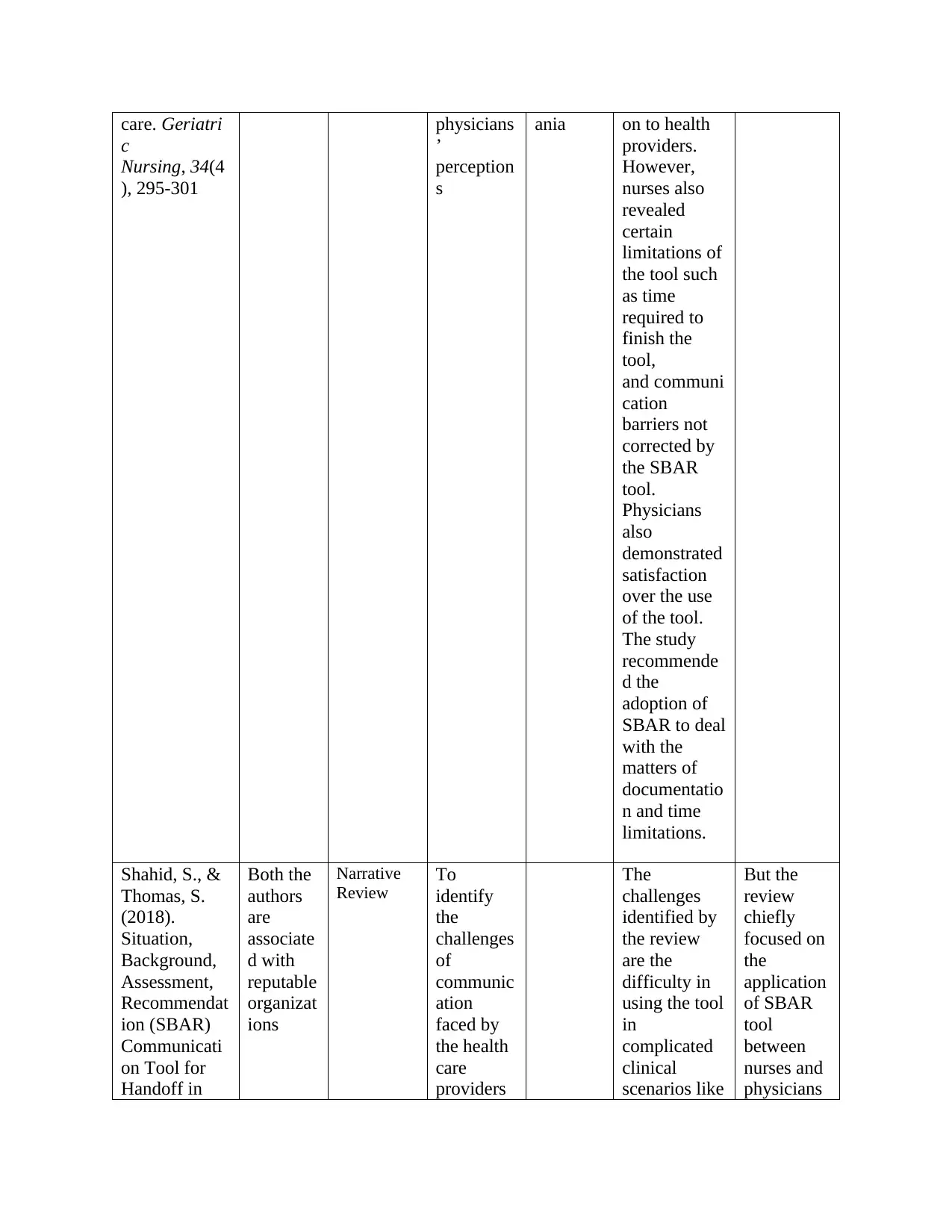
It is recorded that poor nurse–physician communication in the various health settings affect the
care of the service users and the work environment adversely for both nurses as well as
physicians. A study was done by utilizing the repeated measures design to evaluate the impact of
SBAR tool and training on communication between nurse and health providers, as nurses and
physicians’ perceptions. 87.5% of the nursing staff who participated in the study rated the tool as
useful in structuring information and offering cues on the content of communication to health
providers. However, nurses also revealed certain limitations of the tool such as time required to
finish the tool, and communication barriers not corrected by the SBAR tool. Physicians also
demonstrated satisfaction over the use of the tool. The study recommended the adoption of
SBAR to deal with the matters of documentation and time limitations (Renz, Boltz, Wagner,
Capezuti, & Lawrence, 2013). Another study focuses on the nurse-physician communication as in
most of the healthcare settings, majority of the communication regarding patient care takes place
between the physicians and nurses. Continuation of the quality care of the patient is also
dependent upon the effective sharing of the patient information from one health care professional
to another during the handoffs. It will reduce the preventable medical errors occurring due to
communication failure. Situational awareness is required during the handoff when the patient
information is exchanged. A narrative review was done to identify the challenges of
communication faced by the health care providers during the routine exchange of patient care
and offers a wider utilization of the SBAR tool for patient handoff in several care facilities. The
challenges identified by the review are the difficulty in using the tool in complicated clinical
scenarios like ICU, need of educational training and change management to learn and sustain the
clinical use of SBAR (Shahid & Thomas, 2018).
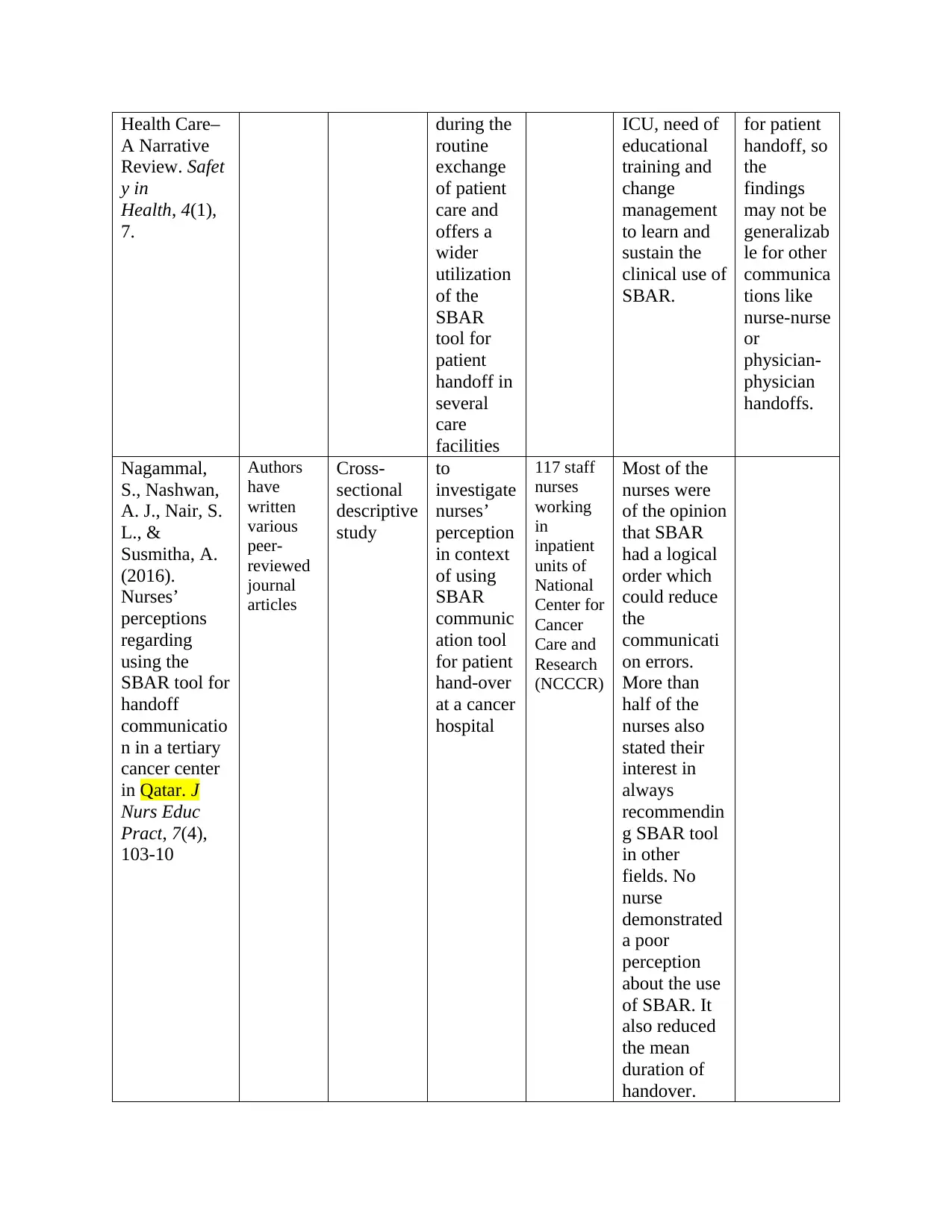
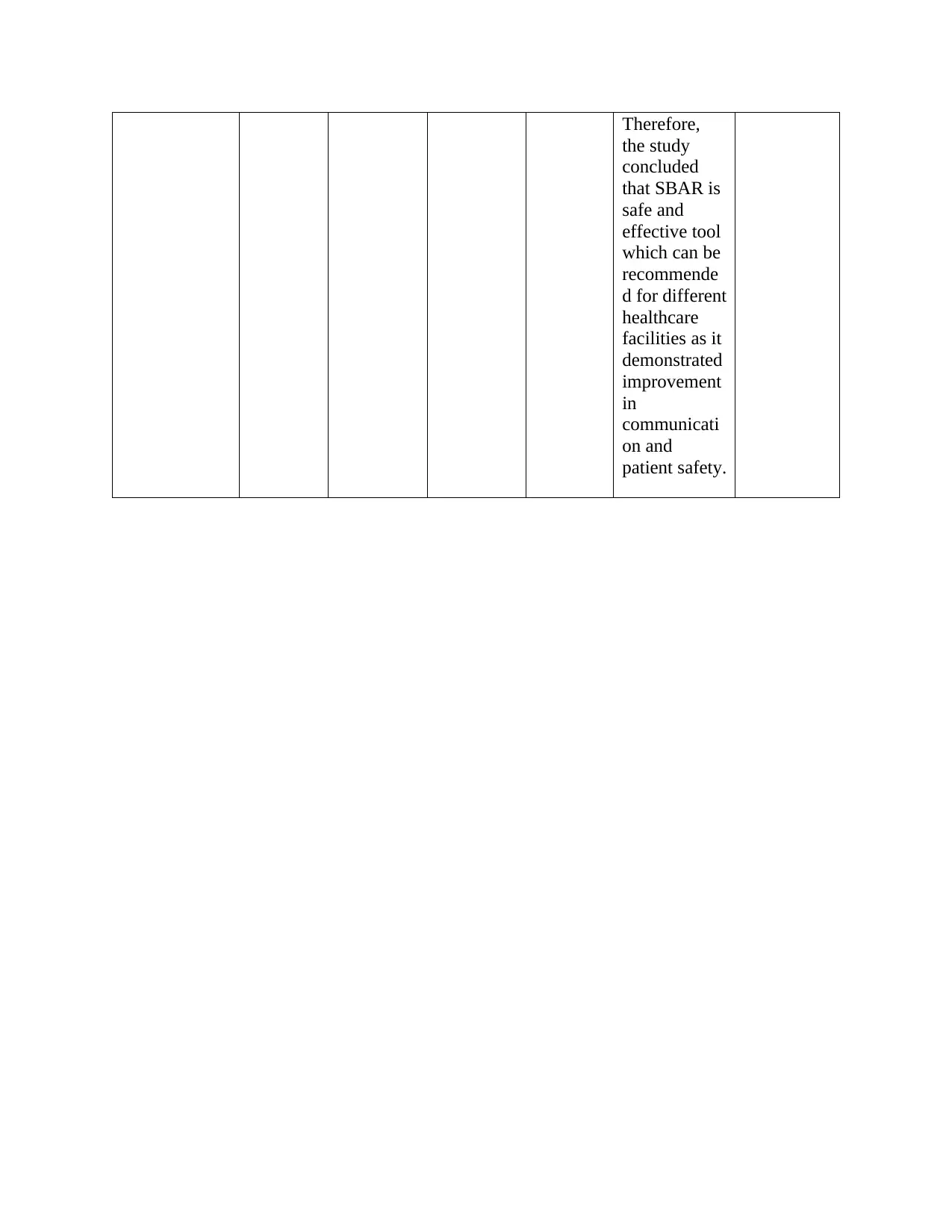
A cross-sectional descriptive study was done to investigate nurses’ perception in context of using
SBAR communication tool for patient hand-over at a cancer hospital. Most of the nurses were of
the opinion that SBAR had a logical order which could reduce the communication errors. More
than half of the nurses also stated their interest in always recommending SBAR tool in other
fields. No nurse demonstrated a poor perception about the use of SBAR. It also reduced the mean
duration of handover. Therefore, the study concluded that SBAR is safe and effective tool which
can be recommended for different healthcare facilities as it demonstrated improvement in
communication and patient safety (Nagammal, Nashwan, Nair, & Susmitha, 2017).
care of the service users and the work environment adversely for both nurses as well as
physicians. A study was done by utilizing the repeated measures design to evaluate the impact of
SBAR tool and training on communication between nurse and health providers, as nurses and
physicians’ perceptions. 87.5% of the nursing staff who participated in the study rated the tool as
useful in structuring information and offering cues on the content of communication to health
providers. However, nurses also revealed certain limitations of the tool such as time required to
finish the tool, and communication barriers not corrected by the SBAR tool. Physicians also
demonstrated satisfaction over the use of the tool. The study recommended the adoption of
SBAR to deal with the matters of documentation and time limitations (Renz, Boltz, Wagner,
Capezuti, & Lawrence, 2013). Another study focuses on the nurse-physician communication as in
most of the healthcare settings, majority of the communication regarding patient care takes place
between the physicians and nurses. Continuation of the quality care of the patient is also
dependent upon the effective sharing of the patient information from one health care professional
to another during the handoffs. It will reduce the preventable medical errors occurring due to
communication failure. Situational awareness is required during the handoff when the patient
information is exchanged. A narrative review was done to identify the challenges of
communication faced by the health care providers during the routine exchange of patient care
and offers a wider utilization of the SBAR tool for patient handoff in several care facilities. The
challenges identified by the review are the difficulty in using the tool in complicated clinical
scenarios like ICU, need of educational training and change management to learn and sustain the
clinical use of SBAR (Shahid & Thomas, 2018).
A cross-sectional descriptive study was done to investigate nurses’ perception in context of using
SBAR communication tool for patient hand-over at a cancer hospital. Most of the nurses were of
the opinion that SBAR had a logical order which could reduce the communication errors. More
than half of the nurses also stated their interest in always recommending SBAR tool in other
fields. No nurse demonstrated a poor perception about the use of SBAR. It also reduced the mean
duration of handover. Therefore, the study concluded that SBAR is safe and effective tool which
can be recommended for different healthcare facilities as it demonstrated improvement in
communication and patient safety (Nagammal, Nashwan, Nair, & Susmitha, 2017).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Principles of Practice Development and Transformational Leadership can be used to achieve best
practice in developing handover plan. The healthcare must use the principle of facilitation of the
transformational leadership to ensure that they provide their staff the learning tools so that a
standardized approach to exchange information between staff can be implemented such as
implementing the SBAR. The leaders must use the principle of simplification and provide
adequate time to communicate crucial information and for the care workers to ask and reply to
queries without disruptions in possible scenarios. They can include repeat-back and read-back
steps in the hand-over process. Leaders in the healthcare must simplify the processes and
information for the nurses and other professionals so that they become generalizable and easy to
use for everyone. Same principle can be used in restraining the exchange of patient information
to that which is required in delivering safe care and avoiding preventable medical errors. The
health leaders must make sure that the healthcare settings utilize systems which during discharge
ensure that the patient and the next health-care provider are provided with important information
about discharge diagnoses, treatment regimes, medications, and investigation reports. The
leaders must integrate training on efficient hand-over communication into the continuing
professional development for care workers and motivate the health workers to undertake that
training. The principle of innovation must also be used by the leaders to initiate the change
required to implement the SBAR.
Conclusion
Communication breakdown has been documented as the major contributor of errors in the
literature which lead to patient harm. Patient safety is one of the vital aspect of patient care. It is
observed that healthcare professionals try to prevent the occurrence of communication errors at
the time of patient handoff. Continuation of the quality care of the patient is also dependent upon
the effective sharing of the patient information from one health care professional to another
during the handoffs. After reviewing the literature, it can be concluded that SBAR
communication tool is an organized communication tool which has proved its efficacy in
decreasing the incidence of errors and thereby adverse events in various healthcare facilities.
SBAR assists in communicating important information in an organized and systematic manner
which needs immediate notice and action. Therefore, it contributes to successful escalation of
management and improved patient safety. Several leading medical agencies and health
practice in developing handover plan. The healthcare must use the principle of facilitation of the
transformational leadership to ensure that they provide their staff the learning tools so that a
standardized approach to exchange information between staff can be implemented such as
implementing the SBAR. The leaders must use the principle of simplification and provide
adequate time to communicate crucial information and for the care workers to ask and reply to
queries without disruptions in possible scenarios. They can include repeat-back and read-back
steps in the hand-over process. Leaders in the healthcare must simplify the processes and
information for the nurses and other professionals so that they become generalizable and easy to
use for everyone. Same principle can be used in restraining the exchange of patient information
to that which is required in delivering safe care and avoiding preventable medical errors. The
health leaders must make sure that the healthcare settings utilize systems which during discharge
ensure that the patient and the next health-care provider are provided with important information
about discharge diagnoses, treatment regimes, medications, and investigation reports. The
leaders must integrate training on efficient hand-over communication into the continuing
professional development for care workers and motivate the health workers to undertake that
training. The principle of innovation must also be used by the leaders to initiate the change
required to implement the SBAR.
Conclusion
Communication breakdown has been documented as the major contributor of errors in the
literature which lead to patient harm. Patient safety is one of the vital aspect of patient care. It is
observed that healthcare professionals try to prevent the occurrence of communication errors at
the time of patient handoff. Continuation of the quality care of the patient is also dependent upon
the effective sharing of the patient information from one health care professional to another
during the handoffs. After reviewing the literature, it can be concluded that SBAR
communication tool is an organized communication tool which has proved its efficacy in
decreasing the incidence of errors and thereby adverse events in various healthcare facilities.
SBAR assists in communicating important information in an organized and systematic manner
which needs immediate notice and action. Therefore, it contributes to successful escalation of
management and improved patient safety. Several leading medical agencies and health
organizations have recommended SBAR for patient handoff to the health care professionals.
Studies proved its reliability and validity as a communication tool. It has been found to be useful
in a range of sub-specialities. It is structured, easy to use and modifiable as per the needs of the
care settings. But certain challenges are found associated with the use of SBAR such as its usage
in complicated clinical scenarios like ICU, need of educational training and change management
to implement and sustain its use. Research is required in future to examine effect of the SBAR
tool on patient outcomes and its comparison with other communication frameworks like I-PASS.
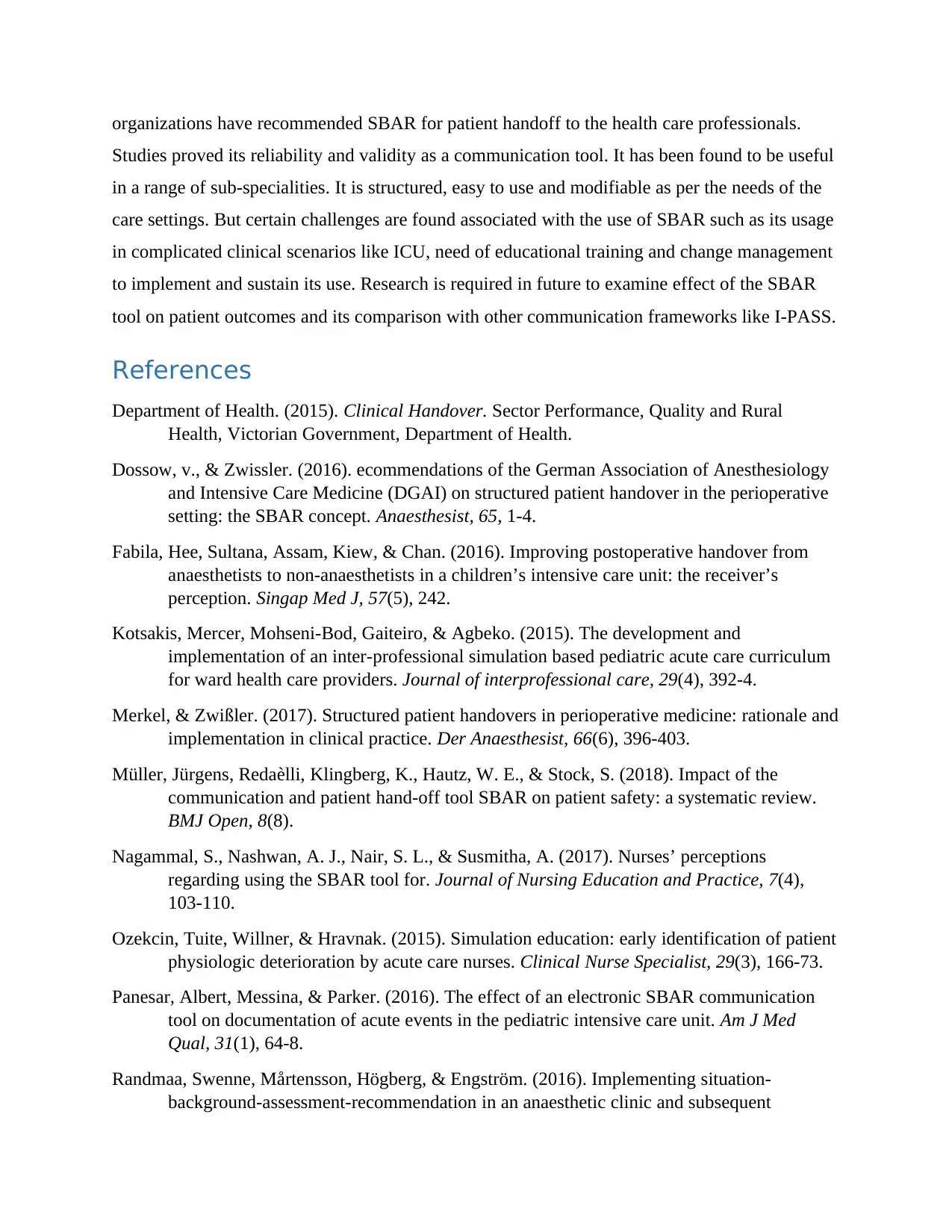
References
Department of Health. (2015). Clinical Handover. Sector Performance, Quality and Rural
Health, Victorian Government, Department of Health.
Dossow, v., & Zwissler. (2016). ecommendations of the German Association of Anesthesiology
and Intensive Care Medicine (DGAI) on structured patient handover in the perioperative
setting: the SBAR concept. Anaesthesist, 65, 1-4.
Fabila, Hee, Sultana, Assam, Kiew, & Chan. (2016). Improving postoperative handover from
anaesthetists to non-anaesthetists in a children’s intensive care unit: the receiver’s
perception. Singap Med J, 57(5), 242.
Kotsakis, Mercer, Mohseni-Bod, Gaiteiro, & Agbeko. (2015). The development and
implementation of an inter-professional simulation based pediatric acute care curriculum
for ward health care providers. Journal of interprofessional care, 29(4), 392-4.
Merkel, & Zwißler. (2017). Structured patient handovers in perioperative medicine: rationale and
implementation in clinical practice. Der Anaesthesist, 66(6), 396-403.
Müller, Jürgens, Redaèlli, Klingberg, K., Hautz, W. E., & Stock, S. (2018). Impact of the
communication and patient hand-off tool SBAR on patient safety: a systematic review.
BMJ Open, 8(8).
Nagammal, S., Nashwan, A. J., Nair, S. L., & Susmitha, A. (2017). Nurses’ perceptions
regarding using the SBAR tool for. Journal of Nursing Education and Practice, 7(4),
103-110.
Ozekcin, Tuite, Willner, & Hravnak. (2015). Simulation education: early identification of patient
physiologic deterioration by acute care nurses. Clinical Nurse Specialist, 29(3), 166-73.
Panesar, Albert, Messina, & Parker. (2016). The effect of an electronic SBAR communication
tool on documentation of acute events in the pediatric intensive care unit. Am J Med
Qual, 31(1), 64-8.
Randmaa, Swenne, Mårtensson, Högberg, & Engström. (2016). Implementing situation-
background-assessment-recommendation in an anaesthetic clinic and subsequent
Studies proved its reliability and validity as a communication tool. It has been found to be useful
in a range of sub-specialities. It is structured, easy to use and modifiable as per the needs of the
care settings. But certain challenges are found associated with the use of SBAR such as its usage
in complicated clinical scenarios like ICU, need of educational training and change management
to implement and sustain its use. Research is required in future to examine effect of the SBAR
tool on patient outcomes and its comparison with other communication frameworks like I-PASS.
References
Department of Health. (2015). Clinical Handover. Sector Performance, Quality and Rural
Health, Victorian Government, Department of Health.
Dossow, v., & Zwissler. (2016). ecommendations of the German Association of Anesthesiology
and Intensive Care Medicine (DGAI) on structured patient handover in the perioperative
setting: the SBAR concept. Anaesthesist, 65, 1-4.
Fabila, Hee, Sultana, Assam, Kiew, & Chan. (2016). Improving postoperative handover from
anaesthetists to non-anaesthetists in a children’s intensive care unit: the receiver’s
perception. Singap Med J, 57(5), 242.
Kotsakis, Mercer, Mohseni-Bod, Gaiteiro, & Agbeko. (2015). The development and
implementation of an inter-professional simulation based pediatric acute care curriculum
for ward health care providers. Journal of interprofessional care, 29(4), 392-4.
Merkel, & Zwißler. (2017). Structured patient handovers in perioperative medicine: rationale and
implementation in clinical practice. Der Anaesthesist, 66(6), 396-403.
Müller, Jürgens, Redaèlli, Klingberg, K., Hautz, W. E., & Stock, S. (2018). Impact of the
communication and patient hand-off tool SBAR on patient safety: a systematic review.
BMJ Open, 8(8).
Nagammal, S., Nashwan, A. J., Nair, S. L., & Susmitha, A. (2017). Nurses’ perceptions
regarding using the SBAR tool for. Journal of Nursing Education and Practice, 7(4),
103-110.
Ozekcin, Tuite, Willner, & Hravnak. (2015). Simulation education: early identification of patient
physiologic deterioration by acute care nurses. Clinical Nurse Specialist, 29(3), 166-73.
Panesar, Albert, Messina, & Parker. (2016). The effect of an electronic SBAR communication
tool on documentation of acute events in the pediatric intensive care unit. Am J Med
Qual, 31(1), 64-8.
Randmaa, Swenne, Mårtensson, Högberg, & Engström. (2016). Implementing situation-
background-assessment-recommendation in an anaesthetic clinic and subsequent
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
information retention among receivers: a prospective interventional study of
postoperative handovers. European Journal of Anaesthesiology, 33(3), 172–8.
Raymond, & Harrison. (2014). The structured communication tool SBAR (Situation,
Background, Assessment and Recommendation) improves communication in
neonatology. SAMJ: South African Medical Journal, 104(12), 850-2.
Raymond, & Harrison. (2014). The structured communication tool SBAR (Situation,
Background, Assessment and Recommendation) improves communication in
neonatology. SAMJ: South African Medical Journal, 104(12).
Renz, Boltz, Wagner, Capezuti, & Lawrence. (2013). Examining the feasibility and utility of an
SBAR protocol in long-term care. Geriatric Nursing, 34(4), 295-301.
Scott, J. (2016). Obstetric transport. Obstet Gynecol Clin N Am, 43(4), 821–40.
Shahid, & Thomas. (2018). Situation, Background, Assessment, Recommendation (SBAR)
Communication Tool for Handoff in Health Care – A Narrative Review. Safety in
Health, 4(7).
The Joint Commission. (2014). Sentinel event data: root causes by event type 2004–2014.
Retrieved from http://www.tsigconsulting.com/tolcam/wp-content/uploads/2015/04/TJC-
Sentinel-Event-Root_Causes_by_Event_Type_2004-2014.pdf
World Health Organisation. (2009). Conceptual Framework for the International Classification
for Patient Safety. Retrieved from WHO:
http://www.who.int/patientsafety/taxonomy/icps_full_report.pdf
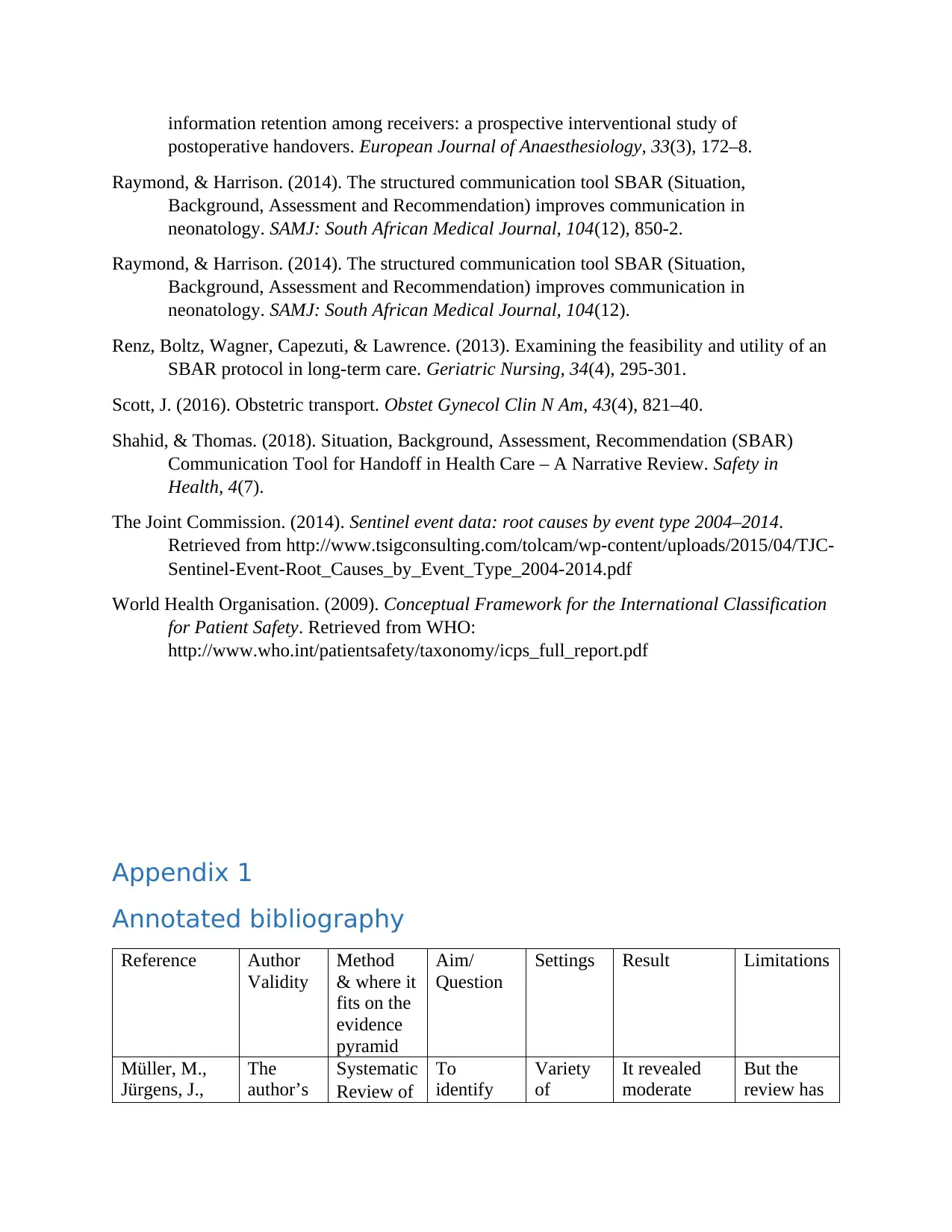
Appendix 1
Annotated bibliography
Reference Author
Validity
Method
& where it
fits on the
evidence
pyramid
Aim/
Question
Settings Result Limitations
Müller, M.,
Jürgens, J.,
The
author’s
Systematic
Review of
To
identify
Variety
of
It revealed
moderate
But the
review has
postoperative handovers. European Journal of Anaesthesiology, 33(3), 172–8.
Raymond, & Harrison. (2014). The structured communication tool SBAR (Situation,
Background, Assessment and Recommendation) improves communication in
neonatology. SAMJ: South African Medical Journal, 104(12), 850-2.
Raymond, & Harrison. (2014). The structured communication tool SBAR (Situation,
Background, Assessment and Recommendation) improves communication in
neonatology. SAMJ: South African Medical Journal, 104(12).
Renz, Boltz, Wagner, Capezuti, & Lawrence. (2013). Examining the feasibility and utility of an
SBAR protocol in long-term care. Geriatric Nursing, 34(4), 295-301.
Scott, J. (2016). Obstetric transport. Obstet Gynecol Clin N Am, 43(4), 821–40.
Shahid, & Thomas. (2018). Situation, Background, Assessment, Recommendation (SBAR)
Communication Tool for Handoff in Health Care – A Narrative Review. Safety in
Health, 4(7).
The Joint Commission. (2014). Sentinel event data: root causes by event type 2004–2014.
Retrieved from http://www.tsigconsulting.com/tolcam/wp-content/uploads/2015/04/TJC-
Sentinel-Event-Root_Causes_by_Event_Type_2004-2014.pdf
World Health Organisation. (2009). Conceptual Framework for the International Classification
for Patient Safety. Retrieved from WHO:
http://www.who.int/patientsafety/taxonomy/icps_full_report.pdf
Appendix 1
Annotated bibliography
Reference Author
Validity
Method
& where it
fits on the
evidence
pyramid
Aim/
Question
Settings Result Limitations
Müller, M.,
Jürgens, J.,
The
author’s
Systematic
Review of
To
identify
Variety
of
It revealed
moderate
But the
review has
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Redaèlli, M.,
Klingberg, K.,
Hautz, W. E.,
& Stock, S.
(2018).
Impact of the
communicatio
n and patient
hand-off tool
SBAR on
patient safety:
a systematic
review. BMJ
open, 8(8),
e022202.
qualificat
ions are
valid and
they are
associate
d with
renowne
d
institutio
ns.
8 studies
which
stands on
top of the
evidence
pyramid
the effect
of
applicatio
n of
SBAR on
patient
safety.
settings
within
primary
and
secondar
y care
and
nursing
homes
were
included.
evidence in
terms of
improvement
of patient
safety on
using SBAR
particularly
when it was
utilized to
organize
communicati
on over
telephone.
The review
highlighted
that SBAR
can be an
adaptive
means that is
appropriate
for various
healthcare
settings,
especially
where clear
and efficient
interpersonal
communicati
on is needed.
the
limitation
of high-
quality
research
which can
serve as
strong
evidence
for the
effectivene
ss of
SBAR.
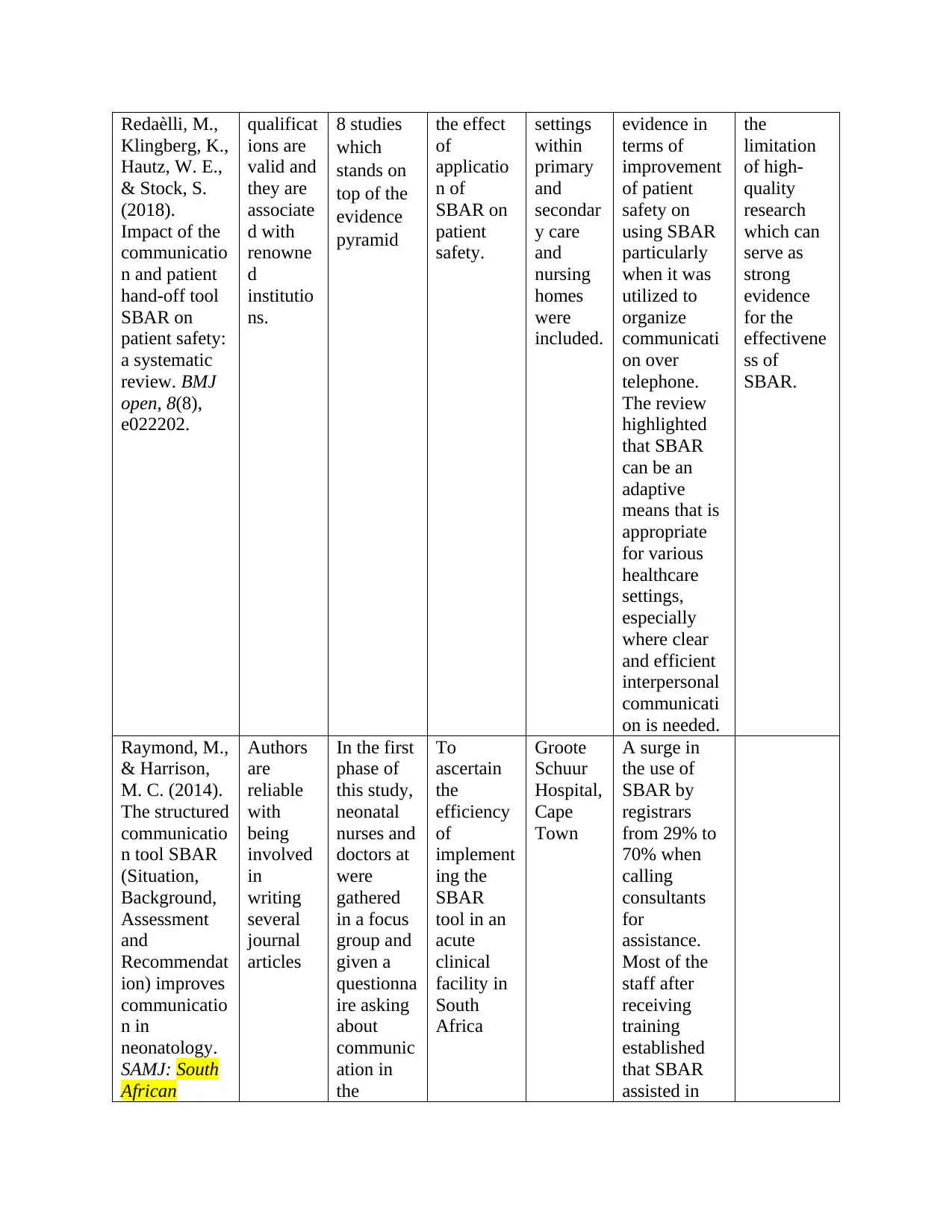
Raymond, M.,
& Harrison,
M. C. (2014).
The structured
communicatio
n tool SBAR
(Situation,
Background,
Assessment
and
Recommendat
ion) improves
communicatio
n in
neonatology.
SAMJ: South
African
Authors
are
reliable
with
being
involved
in
writing
several
journal
articles
In the first
phase of
this study,
neonatal
nurses and
doctors at
were
gathered
in a focus
group and
given a
questionna
ire asking
about
communic
ation in
the
To
ascertain
the
efficiency
of
implement
ing the
SBAR
tool in an
acute
clinical
facility in
South
Africa
Groote
Schuur
Hospital,
Cape
Town
A surge in
the use of
SBAR by
registrars
from 29% to
70% when
calling
consultants
for
assistance.
Most of the
staff after
receiving
training
established
that SBAR
assisted in
Klingberg, K.,
Hautz, W. E.,
& Stock, S.
(2018).
Impact of the
communicatio
n and patient
hand-off tool
SBAR on
patient safety:
a systematic
review. BMJ
open, 8(8),
e022202.
qualificat
ions are
valid and
they are
associate
d with
renowne
d
institutio
ns.
8 studies
which
stands on
top of the
evidence
pyramid
the effect
of
applicatio
n of
SBAR on
patient
safety.
settings
within
primary
and
secondar
y care
and
nursing
homes
were
included.
evidence in
terms of
improvement
of patient
safety on
using SBAR
particularly
when it was
utilized to
organize
communicati
on over
telephone.
The review
highlighted
that SBAR
can be an
adaptive
means that is
appropriate
for various
healthcare
settings,
especially
where clear
and efficient
interpersonal
communicati
on is needed.
the
limitation
of high-
quality
research
which can
serve as
strong
evidence
for the
effectivene
ss of
SBAR.
Raymond, M.,
& Harrison,
M. C. (2014).
The structured
communicatio
n tool SBAR
(Situation,
Background,
Assessment
and
Recommendat
ion) improves
communicatio
n in
neonatology.
SAMJ: South
African
Authors
are
reliable
with
being
involved
in
writing
several
journal
articles
In the first
phase of
this study,
neonatal
nurses and
doctors at
were
gathered
in a focus
group and
given a
questionna
ire asking
about
communic
ation in
the
To
ascertain
the
efficiency
of
implement
ing the
SBAR
tool in an
acute
clinical
facility in
South
Africa
Groote
Schuur
Hospital,
Cape
Town
A surge in
the use of
SBAR by
registrars
from 29% to
70% when
calling
consultants
for
assistance.
Most of the
staff after
receiving
training
established
that SBAR
assisted in
Medical
Journal, 104(
12), 850-852
neonatal
departmen
t. Neonatal
nurses and
doctors
were then
trained to
use
SBAR.
communicati
on,
confidence,
and quality of
patient
service.
Qualitative
evidence was
found that
SBAR
resulted in
increased
promptness
in providing
care to the
acutely sick
patients. So,
the study
concluded
that by
implementing
SBAR,
communicati
on between
professionals
can be
improved and
enhanced
quality and
safety of
patient can be
achieved.
Renz, S. M.,
Boltz, M. P.,
Wagner, L.
M., Capezuti,
E. A., &
Lawrence, T.
E. (2013).
Examining the
feasibility and
utility of an
SBAR
protocol in
long-term
All the
authors
are
associate
d with
reputable
organizat
ions in
USA
repeated
measures
design
to evaluate
the impact
of SBAR
tool and
training on
communic
ation
between
nurse and
health
providers,
as nurses
and
Nursing
home,
part of a
faith-
based
continuin
g care
retireme
nt
communi
ty in
suburban
Pennsylv
87.5% of the
nursing staff
who
participated
in the study
rated the tool
as useful in
structuring
information
and offering
cues on the
content of
communicati
The small
sample
size, single
site and
possibility
of recall
bias in the
responses
of both
nurses and
physicians.
Journal, 104(
12), 850-852
neonatal
departmen
t. Neonatal
nurses and
doctors
were then
trained to
use
SBAR.
communicati
on,
confidence,
and quality of
patient
service.
Qualitative
evidence was
found that
SBAR
resulted in
increased
promptness
in providing
care to the
acutely sick
patients. So,
the study
concluded
that by
implementing
SBAR,
communicati
on between
professionals
can be
improved and
enhanced
quality and
safety of
patient can be
achieved.
Renz, S. M.,
Boltz, M. P.,
Wagner, L.
M., Capezuti,
E. A., &
Lawrence, T.
E. (2013).
Examining the
feasibility and
utility of an
SBAR
protocol in
long-term
All the
authors
are
associate
d with
reputable
organizat
ions in
USA
repeated
measures
design
to evaluate
the impact
of SBAR
tool and
training on
communic
ation
between
nurse and
health
providers,
as nurses
and
Nursing
home,
part of a
faith-
based
continuin
g care
retireme
nt
communi
ty in
suburban
Pennsylv
87.5% of the
nursing staff
who
participated
in the study
rated the tool
as useful in
structuring
information
and offering
cues on the
content of
communicati
The small
sample
size, single
site and
possibility
of recall
bias in the
responses
of both
nurses and
physicians.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
care. Geriatri
c
Nursing, 34(4
), 295-301
physicians
’
perception
s
ania on to health
providers.
However,
nurses also
revealed
certain
limitations of
the tool such
as time
required to
finish the
tool,
and communi
cation
barriers not
corrected by
the SBAR
tool.
Physicians
also
demonstrated
satisfaction
over the use
of the tool.
The study
recommende
d the
adoption of
SBAR to deal
with the
matters of
documentatio
n and time
limitations.
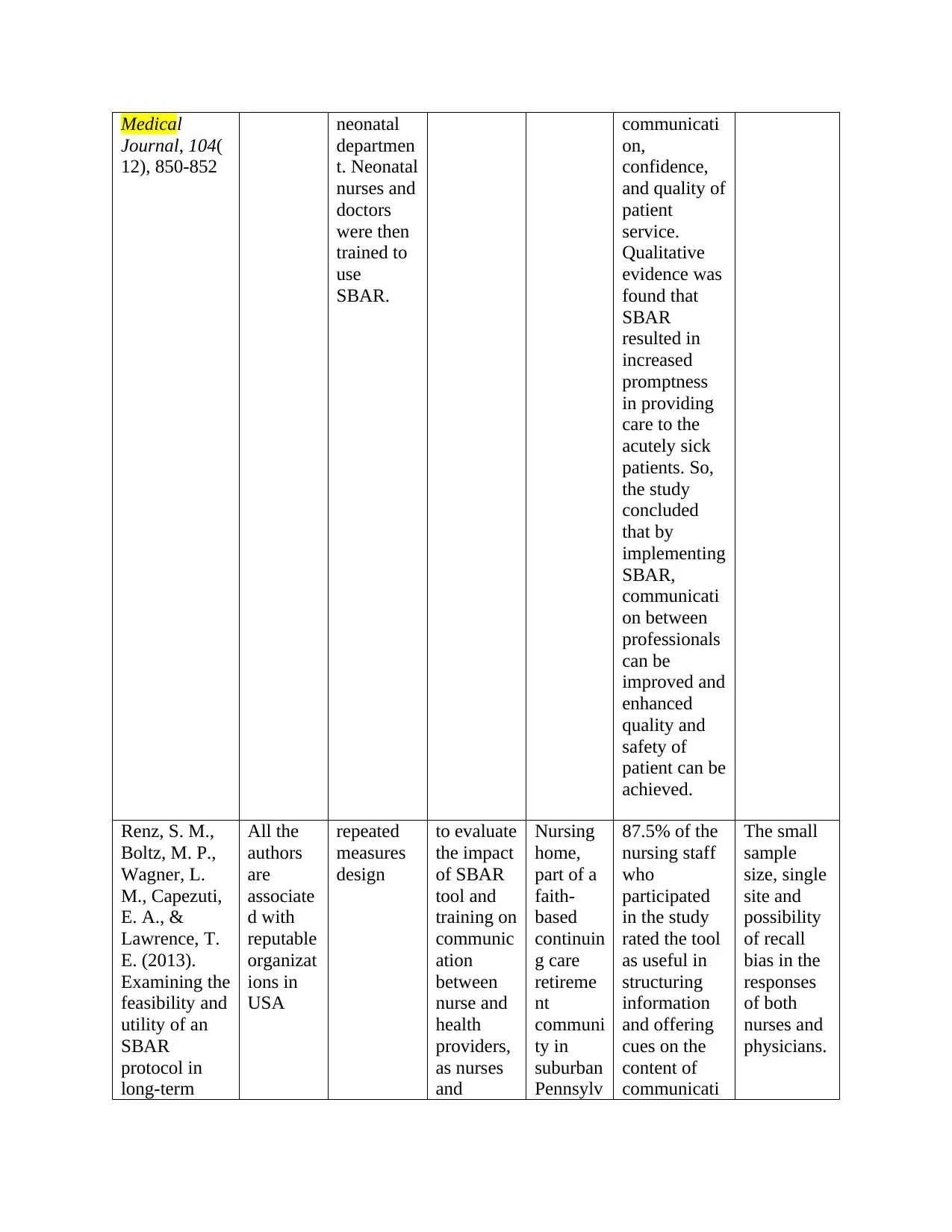
Shahid, S., &
Thomas, S.
(2018).
Situation,
Background,
Assessment,
Recommendat
ion (SBAR)
Communicati
on Tool for
Handoff in
Both the
authors
are
associate
d with
reputable
organizat
ions
Narrative
Review
To
identify
the
challenges
of
communic
ation
faced by
the health
care
providers
The
challenges
identified by
the review
are the
difficulty in
using the tool
in
complicated
clinical
scenarios like
But the
review
chiefly
focused on
the
application
of SBAR
tool
between
nurses and
physicians
c
Nursing, 34(4
), 295-301
physicians
’
perception
s
ania on to health
providers.
However,
nurses also
revealed
certain
limitations of
the tool such
as time
required to
finish the
tool,
and communi
cation
barriers not
corrected by
the SBAR
tool.
Physicians
also
demonstrated
satisfaction
over the use
of the tool.
The study
recommende
d the
adoption of
SBAR to deal
with the
matters of
documentatio
n and time
limitations.
Shahid, S., &
Thomas, S.
(2018).
Situation,
Background,
Assessment,
Recommendat
ion (SBAR)
Communicati
on Tool for
Handoff in
Both the
authors
are
associate
d with
reputable
organizat
ions
Narrative
Review
To
identify
the
challenges
of
communic
ation
faced by
the health
care
providers
The
challenges
identified by
the review
are the
difficulty in
using the tool
in
complicated
clinical
scenarios like
But the
review
chiefly
focused on
the
application
of SBAR
tool
between
nurses and
physicians
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Health Care–
A Narrative
Review. Safet
y in
Health, 4(1),
7.
during the
routine
exchange
of patient
care and
offers a
wider
utilization
of the
SBAR
tool for
patient
handoff in
several
care
facilities
ICU, need of
educational
training and
change
management
to learn and
sustain the
clinical use of
SBAR.
for patient
handoff, so
the
findings
may not be
generalizab
le for other
communica
tions like
nurse-nurse
or
physician-
physician
handoffs.
Nagammal,
S., Nashwan,
A. J., Nair, S.
L., &
Susmitha, A.
(2016).
Nurses’
perceptions
regarding
using the
SBAR tool for
handoff
communicatio
n in a tertiary
cancer center
in Qatar. J
Nurs Educ
Pract, 7(4),
103-10
Authors
have
written
various
peer-
reviewed
journal
articles
Cross-
sectional
descriptive
study
to
investigate
nurses’
perception
in context
of using
SBAR
communic
ation tool
for patient
hand-over
at a cancer
hospital
117 staff
nurses
working
in
inpatient
units of
National
Center for
Cancer
Care and
Research
(NCCCR)
Most of the
nurses were
of the opinion
that SBAR
had a logical
order which
could reduce
the
communicati
on errors.
More than
half of the
nurses also
stated their
interest in
always
recommendin
g SBAR tool
in other
fields. No
nurse
demonstrated
a poor
perception
about the use
of SBAR. It
also reduced
the mean
duration of
handover.
A Narrative
Review. Safet
y in
Health, 4(1),
7.
during the
routine
exchange
of patient
care and
offers a
wider
utilization
of the
SBAR
tool for
patient
handoff in
several
care
facilities
ICU, need of
educational
training and
change
management
to learn and
sustain the
clinical use of
SBAR.
for patient
handoff, so
the
findings
may not be
generalizab
le for other
communica
tions like
nurse-nurse
or
physician-
physician
handoffs.
Nagammal,
S., Nashwan,
A. J., Nair, S.
L., &
Susmitha, A.
(2016).
Nurses’
perceptions
regarding
using the
SBAR tool for
handoff
communicatio
n in a tertiary
cancer center
in Qatar. J
Nurs Educ
Pract, 7(4),
103-10
Authors
have
written
various
peer-
reviewed
journal
articles
Cross-
sectional
descriptive
study
to
investigate
nurses’
perception
in context
of using
SBAR
communic
ation tool
for patient
hand-over
at a cancer
hospital
117 staff
nurses
working
in
inpatient
units of
National
Center for
Cancer
Care and
Research
(NCCCR)
Most of the
nurses were
of the opinion
that SBAR
had a logical
order which
could reduce
the
communicati
on errors.
More than
half of the
nurses also
stated their
interest in
always
recommendin
g SBAR tool
in other
fields. No
nurse
demonstrated
a poor
perception
about the use
of SBAR. It
also reduced
the mean
duration of
handover.
Therefore,
the study
concluded
that SBAR is
safe and
effective tool
which can be
recommende
d for different
healthcare
facilities as it
demonstrated
improvement
in
communicati
on and
patient safety.
the study
concluded
that SBAR is
safe and
effective tool
which can be
recommende
d for different
healthcare
facilities as it
demonstrated
improvement
in
communicati
on and
patient safety.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





