NRS312 Case Study: Clinical Reasoning, Deterioration & ISBAR Tool
VerifiedAdded on 2023/04/23
|12
|2536
|148
Case Study
AI Summary
This nursing assignment presents a comprehensive analysis of a patient case using the clinical reasoning cycle. The case study focuses on an 85-year-old female patient who underwent a total knee replacement surgery and subsequently experienced complications. The analysis includes collecting cues, processing information, identifying problems such as potential sepsis, and establishing goals for patient care. The assignment details specific nursing actions, including pain management strategies, nutritional support, and diabetes management. Furthermore, it addresses moments of patient deterioration, suggesting evidence-based interventions and justifying them using the 'slippery slope' concept. The assignment also incorporates the ISBAR communication tool to develop a handover script for effective communication with the medical officer. This detailed case study demonstrates the application of critical thinking and evidence-based practice in a complex post-operative nursing scenario. Desklib offers a wide range of similar solved assignments and past papers for students.

Running head: Nursing assignment
Nursing assignment
Name of the Student
Name of the university
Author’s note
Nursing assignment
Name of the Student
Name of the university
Author’s note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1Nursing assignment
Clinical reasoning process
Patient situation
The patient is in the emergency ward and is experiencing pain of intensity 7/10 in her left knee as
she had underwent a total knee replacement surgery under general anesthesia.
Collect cues
The patient had a past history of osteoarthritis in both the knees, having a limited range of
movements and the pain on weight bearing in the left knee (Wylde et al., 2015). After prolonged
suffering from osteoarthritis, the patient might have opted for osteoarthritis, as it provides the
greatest improvement in the quality of life of the patient with functional impairment. She also
had a history of Type 2 diabetes, hypertension, and fatty liver and diabetic neuropathy in both the
feet with mild neuropathic pain, without any neurologic deficit (Wylde et al., 2015).
Mar is fully alert and her GCs is 15/15, her surgical wound is dry and her PCS has not
been assessed in the past hours. She had been suffering from pain at an intensity of 7/10 in her
left knee. Most of the patients who have undergone a hip replacement surgery experience chronic
pain after total knee replacement arthoplasty. Mary had been feeling lightheaded and had less
appetite for food. There is a 18 G IV catheter in the tight hand and 200 mL isotonic saline in the
IV bag, running at 80 mL per hour and the PCA circuit is attached to the line. Her BP 60 minutes
ago was 123/70, radial pulse was 55, RR20, SpO2 is 93 %, FiO2 0.21, T36.2, peripheral
capillary refill 2 seconds. The current vital signs were- BP- 105/56, RR20, radial pulse 66
Clinical reasoning process
Patient situation
The patient is in the emergency ward and is experiencing pain of intensity 7/10 in her left knee as
she had underwent a total knee replacement surgery under general anesthesia.
Collect cues
The patient had a past history of osteoarthritis in both the knees, having a limited range of
movements and the pain on weight bearing in the left knee (Wylde et al., 2015). After prolonged
suffering from osteoarthritis, the patient might have opted for osteoarthritis, as it provides the
greatest improvement in the quality of life of the patient with functional impairment. She also
had a history of Type 2 diabetes, hypertension, and fatty liver and diabetic neuropathy in both the
feet with mild neuropathic pain, without any neurologic deficit (Wylde et al., 2015).
Mar is fully alert and her GCs is 15/15, her surgical wound is dry and her PCS has not
been assessed in the past hours. She had been suffering from pain at an intensity of 7/10 in her
left knee. Most of the patients who have undergone a hip replacement surgery experience chronic
pain after total knee replacement arthoplasty. Mary had been feeling lightheaded and had less
appetite for food. There is a 18 G IV catheter in the tight hand and 200 mL isotonic saline in the
IV bag, running at 80 mL per hour and the PCA circuit is attached to the line. Her BP 60 minutes
ago was 123/70, radial pulse was 55, RR20, SpO2 is 93 %, FiO2 0.21, T36.2, peripheral
capillary refill 2 seconds. The current vital signs were- BP- 105/56, RR20, radial pulse 66
2Nursing assignment
regular, SpO2 93%, FiO2 0.21, T36.4 tympanic. BGL11.5mmol/L, the peripheral capillary refill
is 2 seconds and pale cool digits.
Process information
Knee pain after a total knee replacement might occur due to the loosening of the implant,
infection, other palletofemoral problems or the alignment problems. Knee pain can also be
caused due to pinched nerve in the lower back (Wylde et al., 2015). The common peritoneal
nerve, the branch of sciatic nerve that courses from a knee over the top of the fibula bone , are
affected after a total knee replacement (Uesugi et al., 2014). This nerve is susceptible to injury
after the total knee replacement. It is evident from the case study that Mary is 85 years old and it
is normal to feel fatigued after a big surgery. Lightheadedness can also be caused due t the
prolonged intake of the medicines like metoprolol.
The patient had past history of hypertension but acute hypotension can occur after a total
knee arthoplasty (Zhang et al., 2015). It is clear that the BP of the patient had lowered suddenly
within a span of 60 minutes. The anesthetic drugs used at the time of the surgery can affect the
blood pressure. Again losing a large amount of blood at the time of the surgery can lead to
hypovolemic shock leading to a drop in the blood pressure levels. The factors responsible for the
increase in the post-operative hypotension is related to age, the pressure of the tourniquet and the
type of surgery conducted. According to Zhang et al., (2015), the elderly patients cannot regulate
the tension in the blood capillary bed after the surgery and the interstitial fluid cannot be
transferred to the blood vessel timely causing hypotension. Initially, the radial pulse was low
which became normal after 60 minutes. Again increased respiratory rate right after the surgery
regular, SpO2 93%, FiO2 0.21, T36.4 tympanic. BGL11.5mmol/L, the peripheral capillary refill
is 2 seconds and pale cool digits.
Process information
Knee pain after a total knee replacement might occur due to the loosening of the implant,
infection, other palletofemoral problems or the alignment problems. Knee pain can also be
caused due to pinched nerve in the lower back (Wylde et al., 2015). The common peritoneal
nerve, the branch of sciatic nerve that courses from a knee over the top of the fibula bone , are
affected after a total knee replacement (Uesugi et al., 2014). This nerve is susceptible to injury
after the total knee replacement. It is evident from the case study that Mary is 85 years old and it
is normal to feel fatigued after a big surgery. Lightheadedness can also be caused due t the
prolonged intake of the medicines like metoprolol.
The patient had past history of hypertension but acute hypotension can occur after a total
knee arthoplasty (Zhang et al., 2015). It is clear that the BP of the patient had lowered suddenly
within a span of 60 minutes. The anesthetic drugs used at the time of the surgery can affect the
blood pressure. Again losing a large amount of blood at the time of the surgery can lead to
hypovolemic shock leading to a drop in the blood pressure levels. The factors responsible for the
increase in the post-operative hypotension is related to age, the pressure of the tourniquet and the
type of surgery conducted. According to Zhang et al., (2015), the elderly patients cannot regulate
the tension in the blood capillary bed after the surgery and the interstitial fluid cannot be
transferred to the blood vessel timely causing hypotension. Initially, the radial pulse was low
which became normal after 60 minutes. Again increased respiratory rate right after the surgery
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3Nursing assignment
can be a sign of the advent of some major adverse events like the development of the sepsis
(King, Morton & Bevan, 2014)..
Again the normal blood glucose value is 5.6mmmol/L, hence 11.mmol/L is a quite high
value.
According to the case scenario, the patient had lack of appetite and hence the food intake
is too low. In such cases the patient might develop hypoglycemia and develop light headedness
(Rajamäki et al., 2015). The capillary refill time for the patient is also increasing as per the
standard value. A prolonged capillary refill time might indicate towards the development of the
sepsis or shock and might also indicate towards decreased peripheral perfusion.
Identify the problems
It can inferred from the symptoms, that sepsis might have occurred, which can be
understood by the prolonged capillary refill time, the pale skin and the increased respiratory rate.
The septic shock might also be caused due to infection or due to diabetes (Nielen et al., 2015).
Establish goals
To increase her blood pressure level
To increase her capillary refill time
To increase her appetite to the food in order to prevent any chance of the occurrence of
the hypotension.
To alleviate pain within 2 hours.
can be a sign of the advent of some major adverse events like the development of the sepsis
(King, Morton & Bevan, 2014)..
Again the normal blood glucose value is 5.6mmmol/L, hence 11.mmol/L is a quite high
value.
According to the case scenario, the patient had lack of appetite and hence the food intake
is too low. In such cases the patient might develop hypoglycemia and develop light headedness
(Rajamäki et al., 2015). The capillary refill time for the patient is also increasing as per the
standard value. A prolonged capillary refill time might indicate towards the development of the
sepsis or shock and might also indicate towards decreased peripheral perfusion.
Identify the problems
It can inferred from the symptoms, that sepsis might have occurred, which can be
understood by the prolonged capillary refill time, the pale skin and the increased respiratory rate.
The septic shock might also be caused due to infection or due to diabetes (Nielen et al., 2015).
Establish goals
To increase her blood pressure level
To increase her capillary refill time
To increase her appetite to the food in order to prevent any chance of the occurrence of
the hypotension.
To alleviate pain within 2 hours.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4Nursing assignment
Take actions
One of the main strategy for the management of the post-operative pain is the
administration of the preemptive analgesics. Mary should be encouraged to intake liquid food
and high protein diet with roughage as this helps to maintain the nutritional and the fluid balance
supporting tissue perfusion and provision of the nutrients necessary to prevent the chance of
hypotension (Webb et al., 2014). Medicines for the diabetes should be commenced by the
supervision of the surgeon. Comfort measures and diversional activities can be used to get relief
from the pain. Application of ice packs can also be useful for alleviating pain to a milder extent.
In order to prevent any chances of infection, it is necessary to maintain the patency of the
drainage devices to reduce the risk of infection. Clean and aseptic techniques should be used
while handling the drains.
Evaluate
It is necessary to keep an eye on the blood glucose level as the level is high that might
have caused a diabetic shock in the patient. Furthermore, the pain should also decrease after the
administration of the analgesics. The oxygen saturation level should also be restored after the
application of the oxygen therapy.
Reflect on the process
From this experience, I have understood that I could have assessed the PCA after the
patient has gained his consciousness, as it is mentioned in the case study that the patient was
feeling lightheaded , which can be due to the prolonged action of the anesthesia. Furthermore, I
need to check about the contraindication of the analgesics before their application. Again,
medications like Hypericum might have side effects like dizziness and tiredness.
Take actions
One of the main strategy for the management of the post-operative pain is the
administration of the preemptive analgesics. Mary should be encouraged to intake liquid food
and high protein diet with roughage as this helps to maintain the nutritional and the fluid balance
supporting tissue perfusion and provision of the nutrients necessary to prevent the chance of
hypotension (Webb et al., 2014). Medicines for the diabetes should be commenced by the
supervision of the surgeon. Comfort measures and diversional activities can be used to get relief
from the pain. Application of ice packs can also be useful for alleviating pain to a milder extent.
In order to prevent any chances of infection, it is necessary to maintain the patency of the
drainage devices to reduce the risk of infection. Clean and aseptic techniques should be used
while handling the drains.
Evaluate
It is necessary to keep an eye on the blood glucose level as the level is high that might
have caused a diabetic shock in the patient. Furthermore, the pain should also decrease after the
administration of the analgesics. The oxygen saturation level should also be restored after the
application of the oxygen therapy.
Reflect on the process
From this experience, I have understood that I could have assessed the PCA after the
patient has gained his consciousness, as it is mentioned in the case study that the patient was
feeling lightheaded , which can be due to the prolonged action of the anesthesia. Furthermore, I
need to check about the contraindication of the analgesics before their application. Again,
medications like Hypericum might have side effects like dizziness and tiredness.

5Nursing assignment
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6Nursing assignment
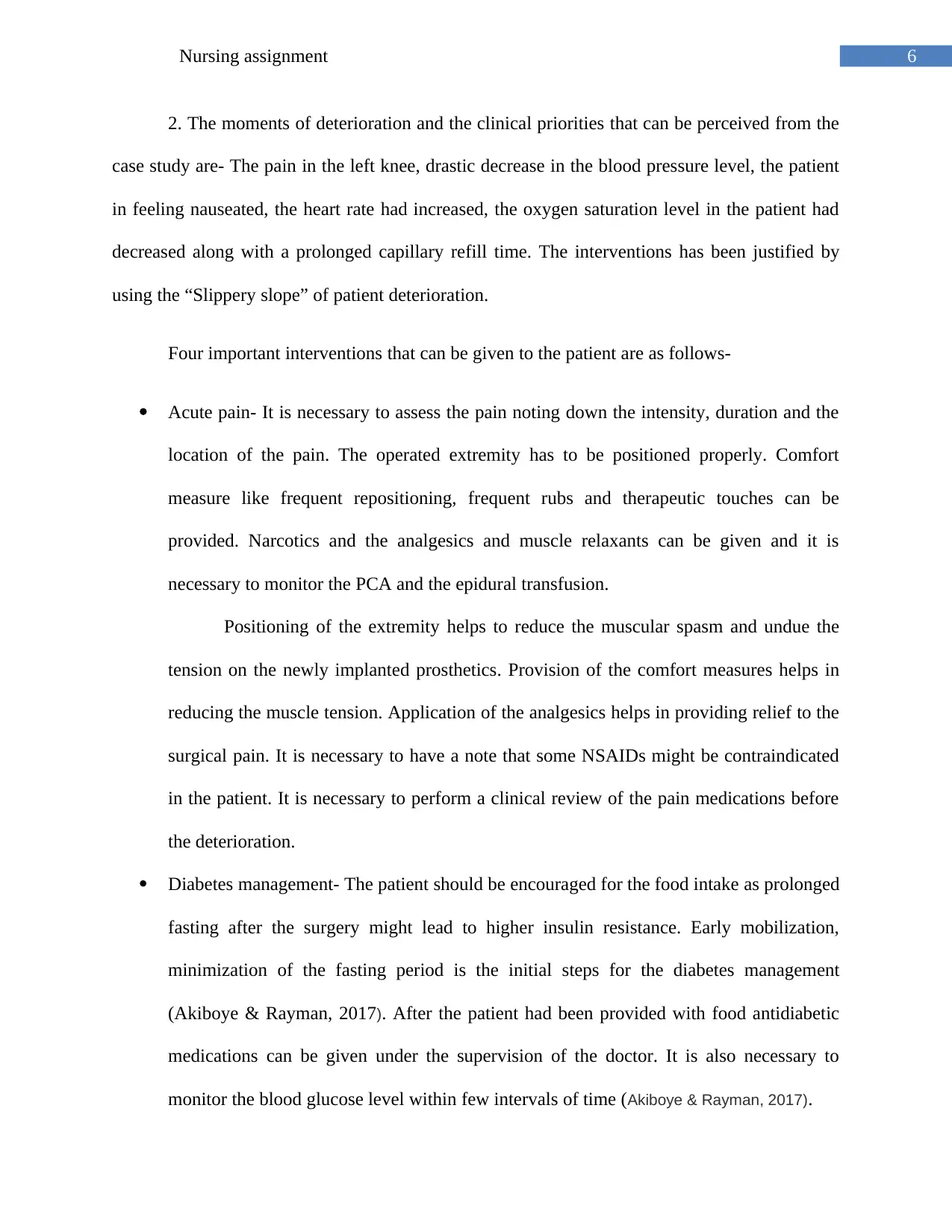
2. The moments of deterioration and the clinical priorities that can be perceived from the
case study are- The pain in the left knee, drastic decrease in the blood pressure level, the patient
in feeling nauseated, the heart rate had increased, the oxygen saturation level in the patient had
decreased along with a prolonged capillary refill time. The interventions has been justified by
using the “Slippery slope” of patient deterioration.
Four important interventions that can be given to the patient are as follows-
Acute pain- It is necessary to assess the pain noting down the intensity, duration and the
location of the pain. The operated extremity has to be positioned properly. Comfort
measure like frequent repositioning, frequent rubs and therapeutic touches can be
provided. Narcotics and the analgesics and muscle relaxants can be given and it is
necessary to monitor the PCA and the epidural transfusion.
Positioning of the extremity helps to reduce the muscular spasm and undue the
tension on the newly implanted prosthetics. Provision of the comfort measures helps in
reducing the muscle tension. Application of the analgesics helps in providing relief to the
surgical pain. It is necessary to have a note that some NSAIDs might be contraindicated
in the patient. It is necessary to perform a clinical review of the pain medications before
the deterioration.
Diabetes management- The patient should be encouraged for the food intake as prolonged
fasting after the surgery might lead to higher insulin resistance. Early mobilization,
minimization of the fasting period is the initial steps for the diabetes management
(Akiboye & Rayman, 2017). After the patient had been provided with food antidiabetic
medications can be given under the supervision of the doctor. It is also necessary to
monitor the blood glucose level within few intervals of time (Akiboye & Rayman, 2017).
2. The moments of deterioration and the clinical priorities that can be perceived from the
case study are- The pain in the left knee, drastic decrease in the blood pressure level, the patient
in feeling nauseated, the heart rate had increased, the oxygen saturation level in the patient had
decreased along with a prolonged capillary refill time. The interventions has been justified by
using the “Slippery slope” of patient deterioration.
Four important interventions that can be given to the patient are as follows-
Acute pain- It is necessary to assess the pain noting down the intensity, duration and the
location of the pain. The operated extremity has to be positioned properly. Comfort
measure like frequent repositioning, frequent rubs and therapeutic touches can be
provided. Narcotics and the analgesics and muscle relaxants can be given and it is
necessary to monitor the PCA and the epidural transfusion.
Positioning of the extremity helps to reduce the muscular spasm and undue the
tension on the newly implanted prosthetics. Provision of the comfort measures helps in
reducing the muscle tension. Application of the analgesics helps in providing relief to the
surgical pain. It is necessary to have a note that some NSAIDs might be contraindicated
in the patient. It is necessary to perform a clinical review of the pain medications before
the deterioration.
Diabetes management- The patient should be encouraged for the food intake as prolonged
fasting after the surgery might lead to higher insulin resistance. Early mobilization,
minimization of the fasting period is the initial steps for the diabetes management
(Akiboye & Rayman, 2017). After the patient had been provided with food antidiabetic
medications can be given under the supervision of the doctor. It is also necessary to
monitor the blood glucose level within few intervals of time (Akiboye & Rayman, 2017).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7Nursing assignment
Increasing the oxygen saturation level- Oxygen therapy can be commenced with in case
of severe respiratory trouble, but some of the other methods include – Raising the head of
the bed and positioning the patient in the semi-fowler position can helps in lung
expansion and decreases the work of breathing (Broens et al., 2014).
Management of the BP- standard monitoring of the arterial blood gases and the ,
the oxyhemoglobin saturation, the heart rhythm should be monitored. It is necessary to
consider the blood pressure pulse, the central venous pressure and some of the other
parameters for preventing the incidence of acute hypotension. Medications can be given
or some of the post-operative exercises like active ankle and knee movement and the
isometric contraction of the quadriceps femoris can help to prevent acute hypotension.
Increasing the oxygen saturation level- Oxygen therapy can be commenced with in case
of severe respiratory trouble, but some of the other methods include – Raising the head of
the bed and positioning the patient in the semi-fowler position can helps in lung
expansion and decreases the work of breathing (Broens et al., 2014).
Management of the BP- standard monitoring of the arterial blood gases and the ,
the oxyhemoglobin saturation, the heart rhythm should be monitored. It is necessary to
consider the blood pressure pulse, the central venous pressure and some of the other
parameters for preventing the incidence of acute hypotension. Medications can be given
or some of the post-operative exercises like active ankle and knee movement and the
isometric contraction of the quadriceps femoris can help to prevent acute hypotension.
8Nursing assignment
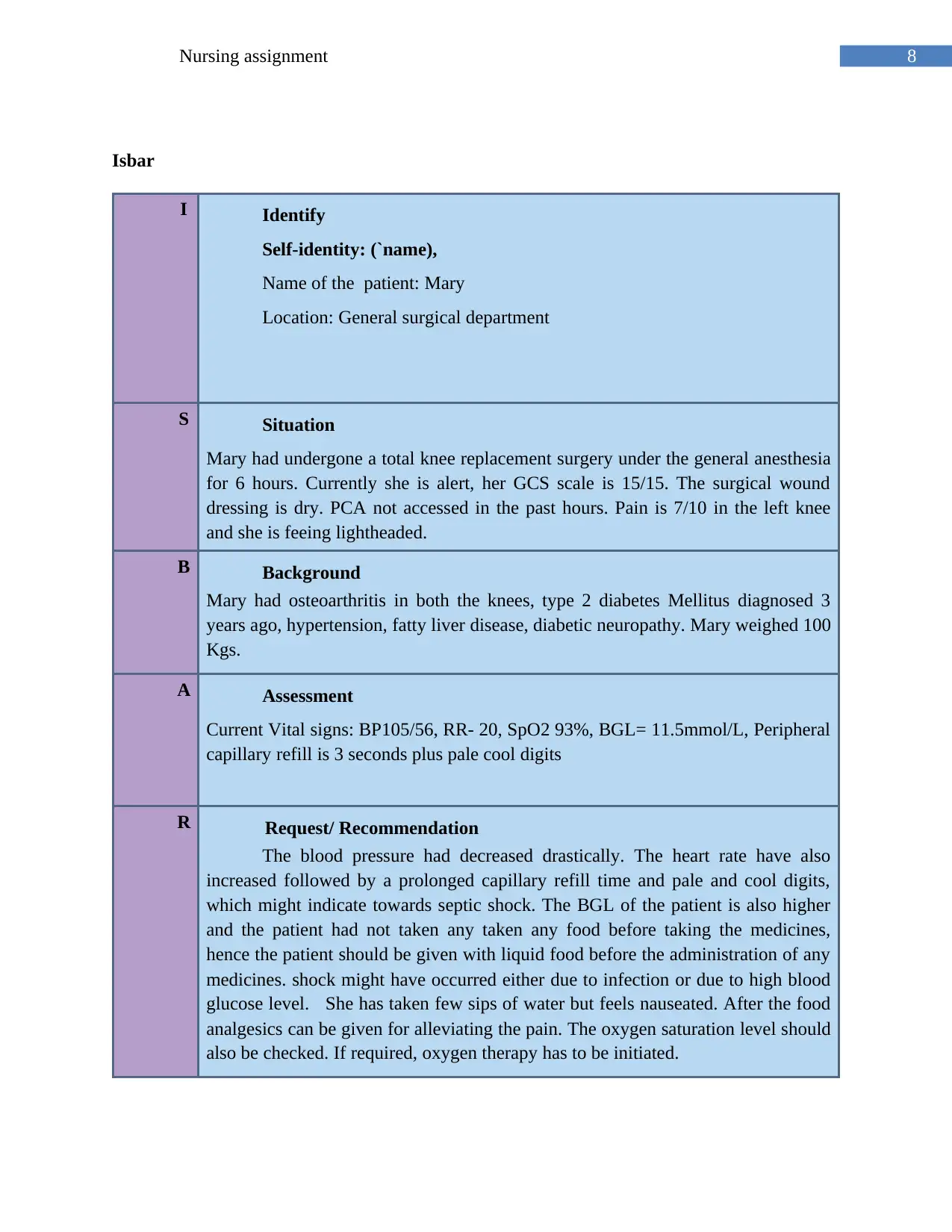
Isbar
I Identify
Self-identity: (`name),
Name of the patient: Mary
Location: General surgical department
S Situation
Mary had undergone a total knee replacement surgery under the general anesthesia
for 6 hours. Currently she is alert, her GCS scale is 15/15. The surgical wound
dressing is dry. PCA not accessed in the past hours. Pain is 7/10 in the left knee
and she is feeing lightheaded.
B Background
Mary had osteoarthritis in both the knees, type 2 diabetes Mellitus diagnosed 3
years ago, hypertension, fatty liver disease, diabetic neuropathy. Mary weighed 100
Kgs.
A Assessment
Current Vital signs: BP105/56, RR- 20, SpO2 93%, BGL= 11.5mmol/L, Peripheral
capillary refill is 3 seconds plus pale cool digits
R Request/ Recommendation
The blood pressure had decreased drastically. The heart rate have also
increased followed by a prolonged capillary refill time and pale and cool digits,
which might indicate towards septic shock. The BGL of the patient is also higher
and the patient had not taken any taken any food before taking the medicines,
hence the patient should be given with liquid food before the administration of any
medicines. shock might have occurred either due to infection or due to high blood
glucose level. She has taken few sips of water but feels nauseated. After the food
analgesics can be given for alleviating the pain. The oxygen saturation level should
also be checked. If required, oxygen therapy has to be initiated.
Isbar
I Identify
Self-identity: (`name),
Name of the patient: Mary
Location: General surgical department
S Situation
Mary had undergone a total knee replacement surgery under the general anesthesia
for 6 hours. Currently she is alert, her GCS scale is 15/15. The surgical wound
dressing is dry. PCA not accessed in the past hours. Pain is 7/10 in the left knee
and she is feeing lightheaded.
B Background
Mary had osteoarthritis in both the knees, type 2 diabetes Mellitus diagnosed 3
years ago, hypertension, fatty liver disease, diabetic neuropathy. Mary weighed 100
Kgs.
A Assessment
Current Vital signs: BP105/56, RR- 20, SpO2 93%, BGL= 11.5mmol/L, Peripheral
capillary refill is 3 seconds plus pale cool digits
R Request/ Recommendation
The blood pressure had decreased drastically. The heart rate have also
increased followed by a prolonged capillary refill time and pale and cool digits,
which might indicate towards septic shock. The BGL of the patient is also higher
and the patient had not taken any taken any food before taking the medicines,
hence the patient should be given with liquid food before the administration of any
medicines. shock might have occurred either due to infection or due to high blood
glucose level. She has taken few sips of water but feels nauseated. After the food
analgesics can be given for alleviating the pain. The oxygen saturation level should
also be checked. If required, oxygen therapy has to be initiated.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

9Nursing assignment
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10Nursing assignment
References
Akiboye, F., & Rayman, G. (2017). Management of Hyperglycemia and Diabetes in Orthopedic
Surgery. Current diabetes reports, 17(2), 13.
Broens, S. J., He, X., Evley, R., Olofsen, E., Niesters, M., Mahajan, R. P., Dahan, A., … van
Velzen, M. (2017). Frequent respiratory events in postoperative patients aged 60 years
and above. Therapeutics and clinical risk management, 13, 1091-1098.
doi:10.2147/TCRM.S135923
Egli, S., Pfister, M., Ludin, S. M., de la Vega, K. P., Busato, A., & Fischer, L. (2015). Long-term
results of therapeutic local anesthesia (neural therapy) in 280 referred refractory chronic
pain patients. BMC complementary and alternative medicine, 15(1), 200.
King, D., Morton, R., & Bevan, C. (2014). How to use capillary refill time. Archives of Disease
in Childhood-Education and Practice, 99(3), 111-116.
Korean Knee Society (2012). Guidelines for the management of postoperative pain after total
knee arthroplasty. Knee surgery & related research, 24(4), 201-7.
Nielen, J. T., Emans, P. J., Dagnelie, P. C., Boonen, A., Lalmohamed, A., de Boer, A., ... & de
Vries, F. (2016). Severity of Diabetes Mellitus and Total Hip or Knee Replacement: A
Population-Based Case–Control Study. Medicine, 95(20).
References
Akiboye, F., & Rayman, G. (2017). Management of Hyperglycemia and Diabetes in Orthopedic
Surgery. Current diabetes reports, 17(2), 13.
Broens, S. J., He, X., Evley, R., Olofsen, E., Niesters, M., Mahajan, R. P., Dahan, A., … van
Velzen, M. (2017). Frequent respiratory events in postoperative patients aged 60 years
and above. Therapeutics and clinical risk management, 13, 1091-1098.
doi:10.2147/TCRM.S135923
Egli, S., Pfister, M., Ludin, S. M., de la Vega, K. P., Busato, A., & Fischer, L. (2015). Long-term
results of therapeutic local anesthesia (neural therapy) in 280 referred refractory chronic
pain patients. BMC complementary and alternative medicine, 15(1), 200.
King, D., Morton, R., & Bevan, C. (2014). How to use capillary refill time. Archives of Disease
in Childhood-Education and Practice, 99(3), 111-116.
Korean Knee Society (2012). Guidelines for the management of postoperative pain after total
knee arthroplasty. Knee surgery & related research, 24(4), 201-7.
Nielen, J. T., Emans, P. J., Dagnelie, P. C., Boonen, A., Lalmohamed, A., de Boer, A., ... & de
Vries, F. (2016). Severity of Diabetes Mellitus and Total Hip or Knee Replacement: A
Population-Based Case–Control Study. Medicine, 95(20).
11Nursing assignment
Rajamäki, T. J., Jämsen, E., Puolakka, P. A., Nevalainen, P. I., & Moilanen, T. (2015). Diabetes
is associated with persistent pain after hip and knee replacement. Acta orthopaedica,
86(5), 586-593.
Uesugi, K., Kitano, N., Kikuchi, T., Sekiguchi, M., & Konno, S. I. (2014). Comparison of
peripheral nerve block with periarticular injection analgesia after total knee arthroplasty:
a randomized, controlled study. The Knee, 21(4), 848-852.
Webb, M. L., Golinvaux, N. S., Ibe, I. K., Bovonratwet, P., Ellman, M. S., & Grauer, J. N.
(2017). Comparison of perioperative adverse event rates after total knee arthroplasty in
patients with diabetes: insulin dependence makes a difference. The Journal of
arthroplasty, 32(10), 2947-2951.
Wylde, V., Beswick, A., Bruce, J., Blom, A., Howells, N., & Gooberman-Hill, R. (2018).
Chronic pain after total knee arthroplasty. EFORT open reviews, 3(8), 461-470.
doi:10.1302/2058-5241.3.180004
Zhang, Y. M., He, J., Zhou, C., Li, Y., Yi, D. K., & Zhang, X. (2015). Acute hypotension after
total knee arthroplasty and its nursing strategy. International journal of clinical and
experimental medicine, 8(8), 13946-53.
Rajamäki, T. J., Jämsen, E., Puolakka, P. A., Nevalainen, P. I., & Moilanen, T. (2015). Diabetes
is associated with persistent pain after hip and knee replacement. Acta orthopaedica,
86(5), 586-593.
Uesugi, K., Kitano, N., Kikuchi, T., Sekiguchi, M., & Konno, S. I. (2014). Comparison of
peripheral nerve block with periarticular injection analgesia after total knee arthroplasty:
a randomized, controlled study. The Knee, 21(4), 848-852.
Webb, M. L., Golinvaux, N. S., Ibe, I. K., Bovonratwet, P., Ellman, M. S., & Grauer, J. N.
(2017). Comparison of perioperative adverse event rates after total knee arthroplasty in
patients with diabetes: insulin dependence makes a difference. The Journal of
arthroplasty, 32(10), 2947-2951.
Wylde, V., Beswick, A., Bruce, J., Blom, A., Howells, N., & Gooberman-Hill, R. (2018).
Chronic pain after total knee arthroplasty. EFORT open reviews, 3(8), 461-470.
doi:10.1302/2058-5241.3.180004
Zhang, Y. M., He, J., Zhou, C., Li, Y., Yi, D. K., & Zhang, X. (2015). Acute hypotension after
total knee arthroplasty and its nursing strategy. International journal of clinical and
experimental medicine, 8(8), 13946-53.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





