Polycystic Ovarian Syndrome: Symptoms, Diagnosis and Treatment
VerifiedAdded on 2023/05/30
|11
|2808
|53
AI Summary
Polycystic Ovarian Syndrome is an endocrine disorder that manifests with menstrual dysfunction, formation of multiple cysts in the ovaries and increased serum concentrations of androgenic hormones. It affects women of the reproductive age and its onset is normally seen at adolescence. The etiology and pathophysiology of the condition largely remains unknown. There is no cure for the condition hence most treatment methods focus on the management of clinical symptoms such as hyper-androgenism, diabetes type 2 and anovulation. Diagnosis of the condition is mainly through exclusion because there is
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: POLYCYSTIC OVARIAN SYNDROME 1
Polycystic Ovarian Syndrome
Name
Institution
Polycystic Ovarian Syndrome
Name
Institution
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Polycystic Ovarian Syndrome 2
Introduction
Polycystic Ovarian Syndrome, hereafter referred to as PCOS is one of the most prevalent
conditions among women in their reproductive age. It is a hormonal disorder that manifests with
an elevation in the serum amounts of male hormones (androgens) in the vascular system of the
woman. According to Williams (2016), approximately 7% of women in their reproductive age
are affected by PCOS although in most women it is usually not diagnosed. PCOS is a
heterogeneous syndrome which normally presents from the onset of adolescence. The
characteristic signs that accompany PCOS include, ovulation dysfunction (which may present
with oligo-menorrhea, amenorrhea or abnormal menstruation), alongside symptoms associated
with excess androgenic hormones such as acne, increased growth of facial and body hair and
alopecia (Williams 2016). PCOS accounts for the highest number of cases of ano-ovulatory
infertility among women. Generally it affects all women of child bearing age and is a major risk
factor for diabetes. There is a shortage of population based studies looking into the prevalence of
PCOS among adolescents. In the US, the estimated prevalence among adolescent girls is 0.8%.
Etiology of PCOS
The specific etiology of PCOS is still unknown although Chandrasekaran & Sagili (2018)
contend that PCOS is a dominant condition linked to the X-chromosome. Although the
pathophysiology of PCOS is still unclear, Chandrasekaran & Sagili like most scientists opine that
the condition is familial and that most of the time, it’s carried down through genes from one
generation to the next. More than 100 genomic sequences have been isolated and are under
investigation with anticipated discovery of a definitive diagnosis and treatment for PCOS but the
findings as of now cannot be applied in clinical practice. The bodies of women who have PCOS
Introduction
Polycystic Ovarian Syndrome, hereafter referred to as PCOS is one of the most prevalent
conditions among women in their reproductive age. It is a hormonal disorder that manifests with
an elevation in the serum amounts of male hormones (androgens) in the vascular system of the
woman. According to Williams (2016), approximately 7% of women in their reproductive age
are affected by PCOS although in most women it is usually not diagnosed. PCOS is a
heterogeneous syndrome which normally presents from the onset of adolescence. The
characteristic signs that accompany PCOS include, ovulation dysfunction (which may present
with oligo-menorrhea, amenorrhea or abnormal menstruation), alongside symptoms associated
with excess androgenic hormones such as acne, increased growth of facial and body hair and
alopecia (Williams 2016). PCOS accounts for the highest number of cases of ano-ovulatory
infertility among women. Generally it affects all women of child bearing age and is a major risk
factor for diabetes. There is a shortage of population based studies looking into the prevalence of
PCOS among adolescents. In the US, the estimated prevalence among adolescent girls is 0.8%.
Etiology of PCOS
The specific etiology of PCOS is still unknown although Chandrasekaran & Sagili (2018)
contend that PCOS is a dominant condition linked to the X-chromosome. Although the
pathophysiology of PCOS is still unclear, Chandrasekaran & Sagili like most scientists opine that
the condition is familial and that most of the time, it’s carried down through genes from one
generation to the next. More than 100 genomic sequences have been isolated and are under
investigation with anticipated discovery of a definitive diagnosis and treatment for PCOS but the
findings as of now cannot be applied in clinical practice. The bodies of women who have PCOS
Polycystic Ovarian Syndrome 3
have malfunctions with the metabolism of androgens and estrogen and hence develop difficulties
with regulating the production and release of androgens (Chandrasekaran & Sagili 2018). This
leads to an elevation in the serum amounts of male sex hormones such as androsteinedione,
testosterone and dehydroepiandrosterone. As a result of having an excess of the male sex
hormones, the ovaries develop fluid filled sacs called cysts. Higher serum levels of androgens
frequently causes an interruption in the release of the egg hence causing mal-ovulation which
commonly presents as abnormal menstrual flow.
Li, Zhu, Duan & Tan (2016) define PCOS as a hormonal disorder that characteristically
presents with elevated serum androgen levels, development of cysts in the ovaries and menstrual
flow dysfunction. It suffices to say that the aforementioned three are the major signs associated
with PCOS; however, variations in the signs and symptoms occur from one woman to another
(Li et al, 2016). More importantly, not all women who have ovarian cysts have PCOS; likewise
not all women who have PCOS have ovarian cysts. Even so, Li et al (2016) hold that PCOS is
closely linked to reproductive complications, metabolic disruptions and cardiovascular problems
in the affected persons.
Increased growth of facial and body hair, especially on the back, belly and chest, a
condition referred to as hirsutism is common in women with PCOS. As contended by Gupta,
Gupta & Ahmed (2018), this results as a consequence of the elevated levels of androgens which
stimulate hair growth (a feature associated with male sex hormones). Hirsutism is observed in
more than 70% of women who have the condition. Acnes and male pattern balding of the head
are also androgen related signs that may also occur in PCOS. Male sex hormones cause the skin
to become oilier than normal and may result in development of acnes.
have malfunctions with the metabolism of androgens and estrogen and hence develop difficulties
with regulating the production and release of androgens (Chandrasekaran & Sagili 2018). This
leads to an elevation in the serum amounts of male sex hormones such as androsteinedione,
testosterone and dehydroepiandrosterone. As a result of having an excess of the male sex
hormones, the ovaries develop fluid filled sacs called cysts. Higher serum levels of androgens
frequently causes an interruption in the release of the egg hence causing mal-ovulation which
commonly presents as abnormal menstrual flow.
Li, Zhu, Duan & Tan (2016) define PCOS as a hormonal disorder that characteristically
presents with elevated serum androgen levels, development of cysts in the ovaries and menstrual
flow dysfunction. It suffices to say that the aforementioned three are the major signs associated
with PCOS; however, variations in the signs and symptoms occur from one woman to another
(Li et al, 2016). More importantly, not all women who have ovarian cysts have PCOS; likewise
not all women who have PCOS have ovarian cysts. Even so, Li et al (2016) hold that PCOS is
closely linked to reproductive complications, metabolic disruptions and cardiovascular problems
in the affected persons.
Increased growth of facial and body hair, especially on the back, belly and chest, a
condition referred to as hirsutism is common in women with PCOS. As contended by Gupta,
Gupta & Ahmed (2018), this results as a consequence of the elevated levels of androgens which
stimulate hair growth (a feature associated with male sex hormones). Hirsutism is observed in
more than 70% of women who have the condition. Acnes and male pattern balding of the head
are also androgen related signs that may also occur in PCOS. Male sex hormones cause the skin
to become oilier than normal and may result in development of acnes.
Polycystic Ovarian Syndrome 4
Weight gain is frequently observed in women with PCOS, in fact Williams (2016) reports
that over 80% of women suffering from PCOS are either overweight or obese. This is
attributable to metabolic disruptions. PCOS may also present with heavy bleeding of the uterine
wall; owing to the disruption of the menstrual flow occasioning delays in ovulation, the uterine
walls tend to thicken a lot and the few periods that the woman has therefore tend to be thicker
and heavier than normal menstrual flows.
McEwen & Hartmann (2018) argue that PCOS is closely associated with increased
peripheral insulin resistance as well as an elevation of serum concentrations of insulin which
predispose the individual to diabetes. Both abnormalities are amplified in patients with
concurrent obesity or overweight. Abnormalities in insulin receptor signaling pathways such as
defects in post-binding receptor sites may result in resistance to insulin in PCOS patients
(McEwen & Hartmann 2018). Lower blood serum concentrations of adiponectin, a hormone
released from the adipocytes has also been associated with insulin resistance in women with
PCOS. Adiponectin is a hormone that is responsible for the regulation of the metabolism of
lipids and to a large extent, the glucose levels. According to McEwen & Hartmann (2018),
concurrent low levels of adiponectin and insulin resistance work together to cause diabetes in a
woman who has PCOS. High serum amounts of insulin elevate the effect of the gonadotropin on
the function of the ovaries.
Shahzan, Priya & Devi (2018) propose a mechanism for the development of anovulation.
They suggest that an increase in serum concentrations of androgenic hormones stimulates the
activity of the luteinizing hormone (LH). LH is a gonadotropic hormone secreted by the anterior
lobe of the pituitary gland and it functions to trigger ovulation and the development of the corpus
luteum. Its secretion therefore causes an increased stimulation of the theca cells of the ovaries.
Weight gain is frequently observed in women with PCOS, in fact Williams (2016) reports
that over 80% of women suffering from PCOS are either overweight or obese. This is
attributable to metabolic disruptions. PCOS may also present with heavy bleeding of the uterine
wall; owing to the disruption of the menstrual flow occasioning delays in ovulation, the uterine
walls tend to thicken a lot and the few periods that the woman has therefore tend to be thicker
and heavier than normal menstrual flows.
McEwen & Hartmann (2018) argue that PCOS is closely associated with increased
peripheral insulin resistance as well as an elevation of serum concentrations of insulin which
predispose the individual to diabetes. Both abnormalities are amplified in patients with
concurrent obesity or overweight. Abnormalities in insulin receptor signaling pathways such as
defects in post-binding receptor sites may result in resistance to insulin in PCOS patients
(McEwen & Hartmann 2018). Lower blood serum concentrations of adiponectin, a hormone
released from the adipocytes has also been associated with insulin resistance in women with
PCOS. Adiponectin is a hormone that is responsible for the regulation of the metabolism of
lipids and to a large extent, the glucose levels. According to McEwen & Hartmann (2018),
concurrent low levels of adiponectin and insulin resistance work together to cause diabetes in a
woman who has PCOS. High serum amounts of insulin elevate the effect of the gonadotropin on
the function of the ovaries.
Shahzan, Priya & Devi (2018) propose a mechanism for the development of anovulation.
They suggest that an increase in serum concentrations of androgenic hormones stimulates the
activity of the luteinizing hormone (LH). LH is a gonadotropic hormone secreted by the anterior
lobe of the pituitary gland and it functions to trigger ovulation and the development of the corpus
luteum. Its secretion therefore causes an increased stimulation of the theca cells of the ovaries.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Polycystic Ovarian Syndrome 5
Consequentially, the production and release of androgens by the theca cells is elevated. The
result is a state where the relative amount of follicle stimulation hormone (FSH) to that of LH is
reduced and as a result, the follicular cells of the ovaries are not able to carry out the aromatase-
mediated conversion of the androgens to estradiol, a process that precedes ovulation. This
augments the decrease in estrogen levels followed by anovulation.
Diagnosis of PCOS
The diagnosis of PCOS does not rely on any one test because there isn’t a single
definitive test that confirms the presence of the condition; rather, the condition is diagnosed by
differential diagnosis which involves ruling out other conditions. According to Li et al (2016), 8
out of 10 women who present symptoms of excessive androgenic levels end up having PCOS
and 7 out of 10 women who have signs of hyper-androgenism have been shown to have PCOS.
As such, hirsutism is an important clinical tool for diagnosis.
Hirsutism can be evaluated using the Ferriman-Gallway technique which assesses the
growth of hair in 7 areas of the female body including the chin or face, abdomen, chest, back,
thighs, arms and upper lips. This system as posited by Tehrani, Simbar, Tohidi, Hosseinpanah &
Azizi (2011) allocates a score of 0 to indicate the absence of terminal hair growth and a score of
4 to indicate extensive hair growth in the said sites. A score of 8 on the Ferriman-Gallway scale
indicates hirsutism. 9 out of 10 women whose Ferriman-Gallway score is 8 are normally
confirmed to have polycystic ovaries through ultrasound scans (Tehrani et al, 2011). Three
diagnostic criteria have been proposed by three bodies namely, the National Institute of Health,
the American Society for Reproductive Medicine and the European Society for Human
Reproduction as contained in Figure1 below. Each of the three organizations agrees that
Consequentially, the production and release of androgens by the theca cells is elevated. The
result is a state where the relative amount of follicle stimulation hormone (FSH) to that of LH is
reduced and as a result, the follicular cells of the ovaries are not able to carry out the aromatase-
mediated conversion of the androgens to estradiol, a process that precedes ovulation. This
augments the decrease in estrogen levels followed by anovulation.
Diagnosis of PCOS
The diagnosis of PCOS does not rely on any one test because there isn’t a single
definitive test that confirms the presence of the condition; rather, the condition is diagnosed by
differential diagnosis which involves ruling out other conditions. According to Li et al (2016), 8
out of 10 women who present symptoms of excessive androgenic levels end up having PCOS
and 7 out of 10 women who have signs of hyper-androgenism have been shown to have PCOS.
As such, hirsutism is an important clinical tool for diagnosis.
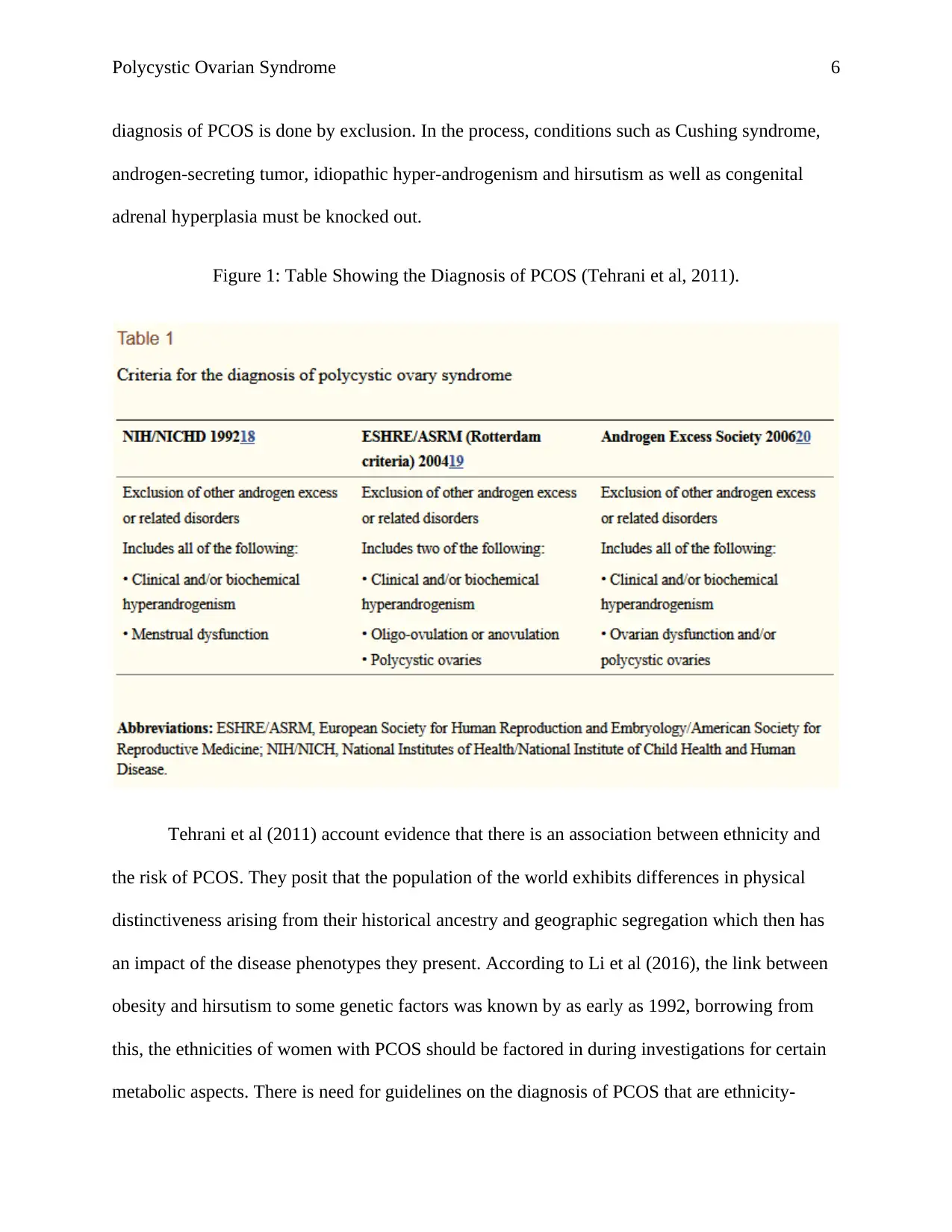
Hirsutism can be evaluated using the Ferriman-Gallway technique which assesses the
growth of hair in 7 areas of the female body including the chin or face, abdomen, chest, back,
thighs, arms and upper lips. This system as posited by Tehrani, Simbar, Tohidi, Hosseinpanah &
Azizi (2011) allocates a score of 0 to indicate the absence of terminal hair growth and a score of
4 to indicate extensive hair growth in the said sites. A score of 8 on the Ferriman-Gallway scale
indicates hirsutism. 9 out of 10 women whose Ferriman-Gallway score is 8 are normally
confirmed to have polycystic ovaries through ultrasound scans (Tehrani et al, 2011). Three
diagnostic criteria have been proposed by three bodies namely, the National Institute of Health,
the American Society for Reproductive Medicine and the European Society for Human
Reproduction as contained in Figure1 below. Each of the three organizations agrees that
Polycystic Ovarian Syndrome 6
diagnosis of PCOS is done by exclusion. In the process, conditions such as Cushing syndrome,
androgen-secreting tumor, idiopathic hyper-androgenism and hirsutism as well as congenital
adrenal hyperplasia must be knocked out.
Figure 1: Table Showing the Diagnosis of PCOS (Tehrani et al, 2011).
Tehrani et al (2011) account evidence that there is an association between ethnicity and
the risk of PCOS. They posit that the population of the world exhibits differences in physical
distinctiveness arising from their historical ancestry and geographic segregation which then has
an impact of the disease phenotypes they present. According to Li et al (2016), the link between
obesity and hirsutism to some genetic factors was known by as early as 1992, borrowing from
this, the ethnicities of women with PCOS should be factored in during investigations for certain
metabolic aspects. There is need for guidelines on the diagnosis of PCOS that are ethnicity-
diagnosis of PCOS is done by exclusion. In the process, conditions such as Cushing syndrome,
androgen-secreting tumor, idiopathic hyper-androgenism and hirsutism as well as congenital
adrenal hyperplasia must be knocked out.
Figure 1: Table Showing the Diagnosis of PCOS (Tehrani et al, 2011).
Tehrani et al (2011) account evidence that there is an association between ethnicity and
the risk of PCOS. They posit that the population of the world exhibits differences in physical
distinctiveness arising from their historical ancestry and geographic segregation which then has
an impact of the disease phenotypes they present. According to Li et al (2016), the link between
obesity and hirsutism to some genetic factors was known by as early as 1992, borrowing from
this, the ethnicities of women with PCOS should be factored in during investigations for certain
metabolic aspects. There is need for guidelines on the diagnosis of PCOS that are ethnicity-
Polycystic Ovarian Syndrome 7
specific in order to aid in the determination of anthropometric thresholds. Besides, such
guidelines will though better identification of phenotypic expression help in enhancing screening
and treatment of ethnic populations at risk.
Treatment of PCOS
This section of the essay looks at the up to date treatment methods for the different
aspects of PCOS from correcting hyper-androgenism to mal-ovulation. The main issue that is
emphasized in the treatment of PCOS is the management of the clinical symptoms given the fact
that the major concern for women with PCOS is the risk posed by long term metabolic
disruptions (Gupta, Gupta & Ahmed, 2018). In order to achieve better results in clinical
management, it is advisable that an early diagnosis be done and that management is commenced
immediately after to avert the worsening of symptoms into complications such as the
development of diabetes mellitus type 2.
Epidemiology of PCOS
People
PCOS occurs in women of the child veering age and commonly appears with the onset of
adolescence. According to Gupta, Gupta & Ahmed (2018), PCOS occurs in approximately 7% of
women in the reproductive age. PCOS has been shown to affect both women of normal weight as
well as overweight and obese women although obesity or overweight is a major co-morbidity
factor that predisposes to the condition. Liu et al (2017) suggests that excess body weight
elevates the risk of developing several complications of the cardiovascular system and
metabolism that are linked to PCOS, besides raising the clinical severity of the condition.
specific in order to aid in the determination of anthropometric thresholds. Besides, such
guidelines will though better identification of phenotypic expression help in enhancing screening
and treatment of ethnic populations at risk.
Treatment of PCOS
This section of the essay looks at the up to date treatment methods for the different
aspects of PCOS from correcting hyper-androgenism to mal-ovulation. The main issue that is
emphasized in the treatment of PCOS is the management of the clinical symptoms given the fact
that the major concern for women with PCOS is the risk posed by long term metabolic
disruptions (Gupta, Gupta & Ahmed, 2018). In order to achieve better results in clinical
management, it is advisable that an early diagnosis be done and that management is commenced
immediately after to avert the worsening of symptoms into complications such as the
development of diabetes mellitus type 2.
Epidemiology of PCOS
People
PCOS occurs in women of the child veering age and commonly appears with the onset of
adolescence. According to Gupta, Gupta & Ahmed (2018), PCOS occurs in approximately 7% of
women in the reproductive age. PCOS has been shown to affect both women of normal weight as
well as overweight and obese women although obesity or overweight is a major co-morbidity
factor that predisposes to the condition. Liu et al (2017) suggests that excess body weight
elevates the risk of developing several complications of the cardiovascular system and
metabolism that are linked to PCOS, besides raising the clinical severity of the condition.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Polycystic Ovarian Syndrome 8
Women who have conditions such as hypertension, peripheral insulin resistance, hyperlipidemia
and atherosclerosis have a greater risk of developing PCOS. Recent rises in the cases of
childhood obesity including a higher percentage of girls becoming extremely overweight raises
concerns of the impact on the general reproductive health of adolescent girls and in particular,
their possibility of developing PCOS owing to the role of obesity and overweight in it etiology
(Liu et al, 2017). Unfortunately, population based studies investigating the prevalence of PCOS
among girls who are obese are scant although scientists generally hold that a higher body mass
index is related to higher risks of developing PCOS.
Place
Despite the fact that several studies have looked into the prevalence of PCOS, there are
notable discrepancies in their findings even in instances where researchers deployed similar
subsets of diagnostic methods (Williams, 2016). These variations in the findings of
epidemiological studies could be attributed to unique features of study populations, limitations in
sampling methods and population sizes and variations in protocols employed in studies (Tehrani
et al, 2011). To a large extent, there is a lack of standardization with regards to the definitions of
phenotypic features which is also a potential source of variations. Inconsistencies may also arise
from the effects of ethnicity and race on the clinical manifestations of androgenic excesses.
Tehrani et al (2011) report that women of Caucasian origin living in Europe and the
United States of America face a lower risk of developing PCOS as compared with Caucasian
females living in the Arab countries. They report that in the US, Afro-Brazilians and African-
Americans show the highest risk of PCOS. According to their study, the lowest risk of
developing PCOS was reported among the Chinese women at 4.4%. Caucasian women showed a
Women who have conditions such as hypertension, peripheral insulin resistance, hyperlipidemia
and atherosclerosis have a greater risk of developing PCOS. Recent rises in the cases of
childhood obesity including a higher percentage of girls becoming extremely overweight raises
concerns of the impact on the general reproductive health of adolescent girls and in particular,
their possibility of developing PCOS owing to the role of obesity and overweight in it etiology
(Liu et al, 2017). Unfortunately, population based studies investigating the prevalence of PCOS
among girls who are obese are scant although scientists generally hold that a higher body mass
index is related to higher risks of developing PCOS.
Place
Despite the fact that several studies have looked into the prevalence of PCOS, there are
notable discrepancies in their findings even in instances where researchers deployed similar
subsets of diagnostic methods (Williams, 2016). These variations in the findings of
epidemiological studies could be attributed to unique features of study populations, limitations in
sampling methods and population sizes and variations in protocols employed in studies (Tehrani
et al, 2011). To a large extent, there is a lack of standardization with regards to the definitions of
phenotypic features which is also a potential source of variations. Inconsistencies may also arise
from the effects of ethnicity and race on the clinical manifestations of androgenic excesses.
Tehrani et al (2011) report that women of Caucasian origin living in Europe and the
United States of America face a lower risk of developing PCOS as compared with Caucasian
females living in the Arab countries. They report that in the US, Afro-Brazilians and African-
Americans show the highest risk of PCOS. According to their study, the lowest risk of
developing PCOS was reported among the Chinese women at 4.4%. Caucasian women showed a
Polycystic Ovarian Syndrome 9
prevalence of 4.5%, while the prevalence of PCOS among Middle-Eastern women was the
highest at 6.1%. Among African-American women, the prevalence of PCOS was 5.3% being the
highest among ethnic groups residing in the US. These results demonstrate the need for diagnosis
protocols that are ethnicity-specific in order to avoid over-diagnosis or under-diagnosis.
Conclusion
Polycystic Ovarian Syndrome is an endocrine disorder that manifests with menstrual
dysfunction, formation of multiple cysts in the ovaries and increased serum concentrations of
androgenic hormones. It affects women of the reproductive age and its onset is normally seen at
adolescence. The etiology and pathophysiology of the condition largely remains unknown. There
is no cure for the condition hence most treatment methods focus on the management of clinical
symptoms such as hyper-androgenism, diabetes type 2 and anovulation. Diagnosis of the
condition is mainly through exclusion because there is no single test that can effectively confirm
the presence of PCOS. The prevalence of PCOS has been demonstrated to vary among different
ethnic groups in the US with the highest rates recorded among Black-American women. This
paper therefore recommends the development of ethnicity-specific protocols for diagnosis of
PCOS to avoid the common incidences of under diagnosis and over diagnosis.
prevalence of 4.5%, while the prevalence of PCOS among Middle-Eastern women was the
highest at 6.1%. Among African-American women, the prevalence of PCOS was 5.3% being the
highest among ethnic groups residing in the US. These results demonstrate the need for diagnosis
protocols that are ethnicity-specific in order to avoid over-diagnosis or under-diagnosis.
Conclusion
Polycystic Ovarian Syndrome is an endocrine disorder that manifests with menstrual
dysfunction, formation of multiple cysts in the ovaries and increased serum concentrations of
androgenic hormones. It affects women of the reproductive age and its onset is normally seen at
adolescence. The etiology and pathophysiology of the condition largely remains unknown. There
is no cure for the condition hence most treatment methods focus on the management of clinical
symptoms such as hyper-androgenism, diabetes type 2 and anovulation. Diagnosis of the
condition is mainly through exclusion because there is no single test that can effectively confirm
the presence of PCOS. The prevalence of PCOS has been demonstrated to vary among different
ethnic groups in the US with the highest rates recorded among Black-American women. This
paper therefore recommends the development of ethnicity-specific protocols for diagnosis of
PCOS to avoid the common incidences of under diagnosis and over diagnosis.
Polycystic Ovarian Syndrome
10
References
Chandrasekaran, S., & Sagili, H. (2018). Metabolic Syndrome in Women with Polycystic Ovary
Syndrome. Obstetrician & Gynaecologist, 20(4), 245–252.
https://doi.org/10.1111/tog.12519
Gupta, R., Gupta, B. M., & Ahmed, K. K. M. (2018). Polycystic Ovary Syndrome Research: A
Scientometric Assessment of Global Publications Output During 2007-16. Oncology,
Gastroenterology & Hepatology Reports, 7(1), 8–15.
https://doi.org/10.5530/ogh.2018.7.1.3
Li, S., Zhu, D., Duan, H., & Tan, Q. (2016). The Epigenomics of Polycystic Ovarian Syndrome:
From Pathogenesis to Clinical Manifestations. Gynecological Endocrinology, 32(12),
942–946. https://doi.org/10.1080/09513590.2016.1203409
Liu, A., Xie, H., Xie, H., Liu, J., Yin, J., Hu, J., & Peng, C. (2017). Association between Fat
Mass and Obesity associated (FTO) gene rs9939609 A/T Polymorphism and Polycystic
Ovary Syndrome: A Systematic Review and Meta-analysis. BMC Medical Genetics,
18(1), 1–7. https://doi.org/10.1186/s12881-017-0452-1
McEwen, B., & Hartmann, G. (2018). Insulin Resistance and Polycystic Ovary Syndrome
(PCOS): Part 1. The impact of Insulin Resistance. Journal of the Australian Traditional-
Medicine Society, 24(4), 214–219. Retrieved from
http://search.ebscohost.com/login.aspx?
direct=true&db=aph&AN=133207977&site=ehost-live
10
References
Chandrasekaran, S., & Sagili, H. (2018). Metabolic Syndrome in Women with Polycystic Ovary
Syndrome. Obstetrician & Gynaecologist, 20(4), 245–252.
https://doi.org/10.1111/tog.12519
Gupta, R., Gupta, B. M., & Ahmed, K. K. M. (2018). Polycystic Ovary Syndrome Research: A
Scientometric Assessment of Global Publications Output During 2007-16. Oncology,
Gastroenterology & Hepatology Reports, 7(1), 8–15.
https://doi.org/10.5530/ogh.2018.7.1.3
Li, S., Zhu, D., Duan, H., & Tan, Q. (2016). The Epigenomics of Polycystic Ovarian Syndrome:
From Pathogenesis to Clinical Manifestations. Gynecological Endocrinology, 32(12),
942–946. https://doi.org/10.1080/09513590.2016.1203409
Liu, A., Xie, H., Xie, H., Liu, J., Yin, J., Hu, J., & Peng, C. (2017). Association between Fat
Mass and Obesity associated (FTO) gene rs9939609 A/T Polymorphism and Polycystic
Ovary Syndrome: A Systematic Review and Meta-analysis. BMC Medical Genetics,
18(1), 1–7. https://doi.org/10.1186/s12881-017-0452-1
McEwen, B., & Hartmann, G. (2018). Insulin Resistance and Polycystic Ovary Syndrome
(PCOS): Part 1. The impact of Insulin Resistance. Journal of the Australian Traditional-
Medicine Society, 24(4), 214–219. Retrieved from
http://search.ebscohost.com/login.aspx?
direct=true&db=aph&AN=133207977&site=ehost-live
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Polycystic Ovarian Syndrome
11
Shahzan, S., Priya, A. J., & Devi, G. (2018). Levels of Luteinizing Hormone in Patients with
Polycystic Ovarian Syndrome. Drug Invention Today, 10(11), 2205–2207. Retrieved
from http://search.ebscohost.com/login.aspx?
direct=true&db=aph&AN=132173474&site=ehost-live
Tehrani, F. R., Simbar, M., Tohidi, M., Hosseinpanah, F., & Azizi, F. (2011). The Prevalence of
Polycystic Ovary Syndrome in a Community Sample of Iranian population: Iranian
PCOS Prevalence Study. Reproductive Biology & Endocrinology, 9(1), 39–45.
https://doi.org/10.1186/1477-7827-9-39
Williams, J. (2016). Prevalence of PCOS in Adolescents and Correlation with Obesity. Fertility
Weekly, 1–2. Retrieved from http://search.ebscohost.com/login.aspx?
direct=true&db=aph&AN=91508703&site=ehost-live
11
Shahzan, S., Priya, A. J., & Devi, G. (2018). Levels of Luteinizing Hormone in Patients with
Polycystic Ovarian Syndrome. Drug Invention Today, 10(11), 2205–2207. Retrieved
from http://search.ebscohost.com/login.aspx?
direct=true&db=aph&AN=132173474&site=ehost-live
Tehrani, F. R., Simbar, M., Tohidi, M., Hosseinpanah, F., & Azizi, F. (2011). The Prevalence of
Polycystic Ovary Syndrome in a Community Sample of Iranian population: Iranian
PCOS Prevalence Study. Reproductive Biology & Endocrinology, 9(1), 39–45.
https://doi.org/10.1186/1477-7827-9-39
Williams, J. (2016). Prevalence of PCOS in Adolescents and Correlation with Obesity. Fertility
Weekly, 1–2. Retrieved from http://search.ebscohost.com/login.aspx?
direct=true&db=aph&AN=91508703&site=ehost-live
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





