Pediatric Nurses' Views on Obstacles and Support in End-of-Life Care
VerifiedAdded on 2023/06/09
|11
|9084
|485
Report
AI Summary
This report investigates pediatric intensive care unit (PICU) nurses' perceptions of obstacles and supportive behaviors in providing end-of-life care to children. A national survey of AACN members revealed that language barriers and parental discomfort with withholding or withdrawing mechanical ventilation were significant obstacles. Supportive behaviors included allowing time alone with the child after death. The study highlights the importance of addressing communication barriers and providing adequate support to nurses in these emotionally challenging situations, ultimately aiming to improve the end-of-life experience for dying children and their families. Desklib provides a platform for students to access similar reports and solved assignments.
By Renea L. Beckstrand,RN, PhD, CCRN, CNE,Nicole L. Rawle,RN, MS, APRN,
Lynn Callister,RN, PhD,and Barbara L. Mandleco,RN, PhD
Background Each year 55 000 children die in the United States,
and most of these deaths occur in hospitals. The barriers and
supportive behaviors in providing end-of-life care to children
should be determined.
Objective To determine pediatric intensive care unit nurses’
perceptions of sizes, frequencies, and magnitudes of selected
obstacles and helpful behaviors in providing end-of-life care
to children.
Method A national sample of 1047 pediatric intensive care
unit nurses who were members of the American Association
of Critical-Care Nurses were surveyed. A 76-item questionnaire
adapted from 3 similar surveys with critical care, emergency,
and oncology nurses was mailed to possible participants.
Nurses who did not respond to the first mailing were sent a
second mailing. Nurses were asked to rate the size and fre-
quency of listed obstacles and supportive behaviors in caring
for children at the end of life.
Results A total of 474 usable questionnaires were received
from 985 eligible respondents (return rate, 48%). The 2 items
with the highest perceived obstacle magnitude scores for size
and frequency means were language barriers and parental
discomfort in withholding and/or withdrawing mechanical
ventilation. The highest supportive behavior item was allowing
time alone with the child when he or she has died.
Conclusions Pediatric intensive care unit nurses play a vital
role in caring for dying children and the children’s families.
Overcoming language and communication barriers with chil-
dren’s families and between interdisciplinary team members
could greatly improve the end-of-life experience for dying
children. (American Journal of Critical Care. 2010;19:543-552)
PEDIATRIC NURSES’
PERCEPTIONS OFOBSTACLES
AND SUPPORTIVEBEHAVIORS
IN END-OF-LIFE CARE
End-of-Life Care
©2009 American Association of Critical-Care Nurses
doi: 10.4037/ajcc2009497
www.ajcconline.org AA JJCCCC AMERICAN JOURNAL OF CRITICAL CARE, November 2010, Volume 19, No. 6543
by AACN on September 7, 2018http://ajcc.aacnjournals.org/Downloaded from
Lynn Callister,RN, PhD,and Barbara L. Mandleco,RN, PhD
Background Each year 55 000 children die in the United States,
and most of these deaths occur in hospitals. The barriers and
supportive behaviors in providing end-of-life care to children
should be determined.
Objective To determine pediatric intensive care unit nurses’
perceptions of sizes, frequencies, and magnitudes of selected
obstacles and helpful behaviors in providing end-of-life care
to children.
Method A national sample of 1047 pediatric intensive care
unit nurses who were members of the American Association
of Critical-Care Nurses were surveyed. A 76-item questionnaire
adapted from 3 similar surveys with critical care, emergency,
and oncology nurses was mailed to possible participants.
Nurses who did not respond to the first mailing were sent a
second mailing. Nurses were asked to rate the size and fre-
quency of listed obstacles and supportive behaviors in caring
for children at the end of life.
Results A total of 474 usable questionnaires were received
from 985 eligible respondents (return rate, 48%). The 2 items
with the highest perceived obstacle magnitude scores for size
and frequency means were language barriers and parental
discomfort in withholding and/or withdrawing mechanical
ventilation. The highest supportive behavior item was allowing
time alone with the child when he or she has died.
Conclusions Pediatric intensive care unit nurses play a vital
role in caring for dying children and the children’s families.
Overcoming language and communication barriers with chil-
dren’s families and between interdisciplinary team members
could greatly improve the end-of-life experience for dying
children. (American Journal of Critical Care. 2010;19:543-552)
PEDIATRIC NURSES’
PERCEPTIONS OFOBSTACLES
AND SUPPORTIVEBEHAVIORS
IN END-OF-LIFE CARE
End-of-Life Care
©2009 American Association of Critical-Care Nurses
doi: 10.4037/ajcc2009497
www.ajcconline.org AA JJCCCC AMERICAN JOURNAL OF CRITICAL CARE, November 2010, Volume 19, No. 6543
by AACN on September 7, 2018http://ajcc.aacnjournals.org/Downloaded from
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Caring for dying children involves unique barri-
ers. Conflicts arise when futile efforts are continued
to save what society has determined should not be
lost. In a study4 of pediatric palliative health care
providers, barriers included uncertain prognosis,
unwillingness of patients’ family members to acknowl-
edge incurable conditions, language barriers, and
time constraints.
In another study,5 a total of 446 staff members
and physicians were asked about their comfort and
expertise in providing end-of-life care to children.
Staff members felt inexperienced in communicating
about end-of-life issues with patients and patients’
families. Staff members also reported feeling unpre-
pared to deal with pain and symp-
tom management, and a majority
(54%) felt personally unsupported
as they cared for dying children.
Lee and Dupree6 conducted
32 interviews with 29 nurses, physi-
cians, and psychosocial support
personnel about 8 patient deaths
in a large, multidisciplinary PICU.
Themes included the importance
of communication, accommodating the wishes of
others despite a staff member’s own preferences,
issues about use of technology, sadness, and emo-
tional support. The participants reported that they
did not feel adequately supported in dealing with
their grief after caring for a dying child; however,
many welcomed the sadness as a sign of their emo-
tional availability and humanity. Lee and Dupree
concluded that grief, rather than moral distress, was
the dominant response of these caregivers and empha-
sized that research on better communication skills and
emotional support of caregivers was needed.
No published material specifically addresses both
common barriers and supportive behaviors as perceived
by pediatric nurses in end-of-life care. In addition, rela-
tively few researchers4,7,8have addressed the perspectives
of nurses who direct the development of end-of-life care
programs, although nurses bear the major responsibility
for implementing those programs. More than half of
PICU nurses surveyed in 2001 reported that nurses wer
the caregivers who initiated discussions with patients’
families about forgoing life-sustaining treatment.7 Nurses
may feel at a loss as they provide care, because researc
on what really helps dying children and the children’s
families at the end of life is limited.3
Educating clinicians and nurses about end-of-life
decision making and management of infants and chil-
dren, in the context of family-centered care, has not
kept pace with advances in medicine.2,7,8 Care dilemmas
arise as dying patients are placed in an environment
created to sustain life.9 Solomon et al10 found that con-
cerns about overly burdensome treatment were greater
in pediatric end- of-life care than in adult end-of-life
care. They also discovered that nurses were more than
20 times as worried about saving children who
“should not be saved” as about giving up too soon.
Research Questions
The research questions for our study were as follow
• What are the sizes (intensities) and frequencies
of obstacles and supportive behaviors in providing
end-of-life care to infants and children as perceived by
PICU nurses?
• What are the perceived obstacle magnitude
(POM) scores?
• What are the perceived supportive behavior
magnitude (PSBM) scores?
Methods
Design
This was a descriptive quantitative study of PICU
nurses’ perceptions of the size (intensity) of selected
Death of a child evokes deep feelings of tragedy, devastation, and painful co
fusion at the injustice of a life being ended prematurely. Each year 55000
children die in the United States.1,2 Most of the deaths (75%-85%) occur in a
hospital, and most of the hospital deaths take place in pediatric intensive c
units (PICUs).3 The leading cause of death of children more than 1 year old i
unintentional injury. Other major causes include complications of prematurity, death fro
congenital anomalies, cancer, and intentional injuries.2
About the Authors
Renea L. Beckstrand is an associate professor, Nicole L.
Rawle is working in pediatrics, and Lynn Callister and
Barbara L. Mandleco are professors in the College of
Nursing, Brigham Young University, Provo, Utah.
Corresponding author: Renea L. Beckstrand,RN, PhD, CCRN,
CNE, Brigham Young University, College of Nursing, 422
SWKT, PO Box 25432, Provo, UT 84602-5432 (e-mail:
renea@byu.edu).
544 AA JJCCCC AMERICAN JOURNAL OF CRITICAL CARE, November 2010, Volume 19, No. 6 www.ajcconline.org
Research on the
magnitude of
specified obstacles
or supportive
behaviors is limited.
by AACN on September 7, 2018http://ajcc.aacnjournals.org/Downloaded from
ers. Conflicts arise when futile efforts are continued
to save what society has determined should not be
lost. In a study4 of pediatric palliative health care
providers, barriers included uncertain prognosis,
unwillingness of patients’ family members to acknowl-
edge incurable conditions, language barriers, and
time constraints.
In another study,5 a total of 446 staff members
and physicians were asked about their comfort and
expertise in providing end-of-life care to children.
Staff members felt inexperienced in communicating
about end-of-life issues with patients and patients’
families. Staff members also reported feeling unpre-
pared to deal with pain and symp-
tom management, and a majority
(54%) felt personally unsupported
as they cared for dying children.
Lee and Dupree6 conducted
32 interviews with 29 nurses, physi-
cians, and psychosocial support
personnel about 8 patient deaths
in a large, multidisciplinary PICU.
Themes included the importance
of communication, accommodating the wishes of
others despite a staff member’s own preferences,
issues about use of technology, sadness, and emo-
tional support. The participants reported that they
did not feel adequately supported in dealing with
their grief after caring for a dying child; however,
many welcomed the sadness as a sign of their emo-
tional availability and humanity. Lee and Dupree
concluded that grief, rather than moral distress, was
the dominant response of these caregivers and empha-
sized that research on better communication skills and
emotional support of caregivers was needed.
No published material specifically addresses both
common barriers and supportive behaviors as perceived
by pediatric nurses in end-of-life care. In addition, rela-
tively few researchers4,7,8have addressed the perspectives
of nurses who direct the development of end-of-life care
programs, although nurses bear the major responsibility
for implementing those programs. More than half of
PICU nurses surveyed in 2001 reported that nurses wer
the caregivers who initiated discussions with patients’
families about forgoing life-sustaining treatment.7 Nurses
may feel at a loss as they provide care, because researc
on what really helps dying children and the children’s
families at the end of life is limited.3
Educating clinicians and nurses about end-of-life
decision making and management of infants and chil-
dren, in the context of family-centered care, has not
kept pace with advances in medicine.2,7,8 Care dilemmas
arise as dying patients are placed in an environment
created to sustain life.9 Solomon et al10 found that con-
cerns about overly burdensome treatment were greater
in pediatric end- of-life care than in adult end-of-life
care. They also discovered that nurses were more than
20 times as worried about saving children who
“should not be saved” as about giving up too soon.
Research Questions
The research questions for our study were as follow
• What are the sizes (intensities) and frequencies
of obstacles and supportive behaviors in providing
end-of-life care to infants and children as perceived by
PICU nurses?
• What are the perceived obstacle magnitude
(POM) scores?
• What are the perceived supportive behavior
magnitude (PSBM) scores?
Methods
Design
This was a descriptive quantitative study of PICU
nurses’ perceptions of the size (intensity) of selected
Death of a child evokes deep feelings of tragedy, devastation, and painful co
fusion at the injustice of a life being ended prematurely. Each year 55000
children die in the United States.1,2 Most of the deaths (75%-85%) occur in a
hospital, and most of the hospital deaths take place in pediatric intensive c
units (PICUs).3 The leading cause of death of children more than 1 year old i
unintentional injury. Other major causes include complications of prematurity, death fro
congenital anomalies, cancer, and intentional injuries.2
About the Authors
Renea L. Beckstrand is an associate professor, Nicole L.
Rawle is working in pediatrics, and Lynn Callister and
Barbara L. Mandleco are professors in the College of
Nursing, Brigham Young University, Provo, Utah.
Corresponding author: Renea L. Beckstrand,RN, PhD, CCRN,
CNE, Brigham Young University, College of Nursing, 422
SWKT, PO Box 25432, Provo, UT 84602-5432 (e-mail:
renea@byu.edu).
544 AA JJCCCC AMERICAN JOURNAL OF CRITICAL CARE, November 2010, Volume 19, No. 6 www.ajcconline.org
Research on the
magnitude of
specified obstacles
or supportive
behaviors is limited.
by AACN on September 7, 2018http://ajcc.aacnjournals.org/Downloaded from

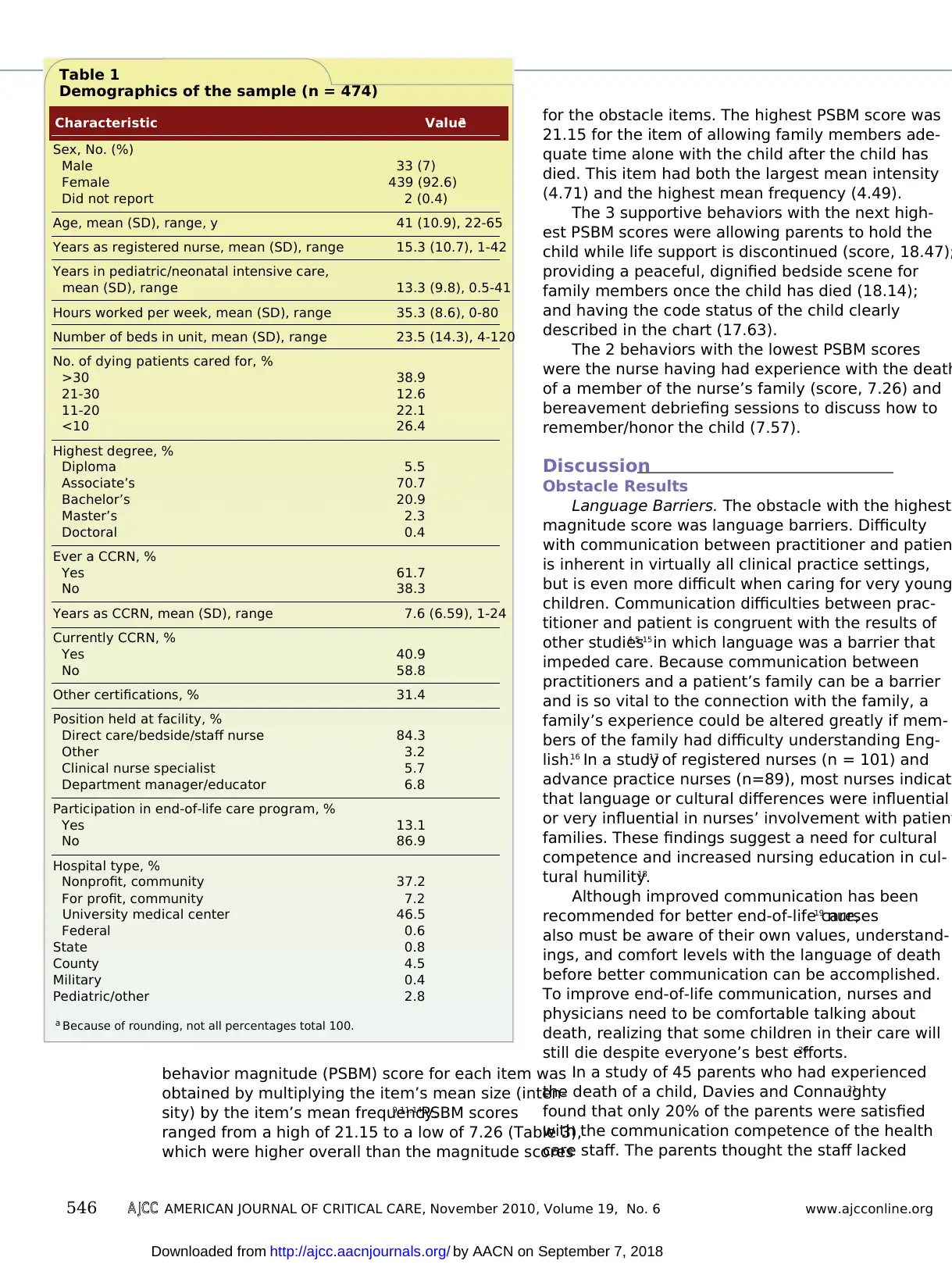
Results
Demographic Data
Of the 1047 potential respondents, 536 returned
questionnaires. A total of 62 questionnaires were
considered ineligible because they were returned by
respondents who did not feel qualified to complete
the questionnaire, were retired, or were no longer
working in a PICU. A few questionnaires were returned
as undeliverable and so were also unusable. Usable
responses were received from 474 of 985 eligible
respondents, for a response rate of 48% after 2 mail-
ings.13 Because the sample was randomly selected,
geographically dispersed, and of adequate size,
results are generalizable to PICU nurses who are
members of AACN. Of the 472 respondents, 439
(92.6%) were women and 33
(7.0%) were men (Table 1). This
percentage of men is slightly lower
than the national AACN member-
ship demographics of 11% men.
Obstacle Magnitude
Respondents ranked all obstacle
items in the questionnaire by both
size and frequency. The scale used for
obstacle size ranged from 0 (not an
obstacle) to 5 (extremely large). A
similar scale of 0 (never occurs) to 5
(always occurs) was used for scoring
item frequencies. An obstacle’s perceived magnitude or
impact was determined by multiplying its mean size
(intensity) by its mean frequency to obtain a POM
score.9,11,14
For the 32 rated obstacles, the POM scores
ranged from a high of 17.73 to a low of 1.99 (Table
2). The item with the highest POM score was language
barriers (score, 17.73), which had both the highest
mean intensity and the highest mean frequency.
The next 3 obstacles with the highest POM scores
were parental discomfort in withholding and/or with-
drawing mechanical ventilation (score, 17.69), dis-
continuity of care of the dying child due to lack of
communication between interdisciplinary team mem-
bers (13.49), and the nurse’s opinion about the direc-
tion of the patient’s care not being valued (13.36).
The 2 obstacles with the lowest POM scores were
nurses believing that life-saving measures or treatments
are stopped too soon (score, 1.99) and nurses getting
vague orders such as “titrate to effect” for pain (2.65).
Supportive Behavior Magnitude
Supportive behaviors were ranked on a scale of 0
(not a help) to 5 (extremely large). Perceived frequen-
cies for each item were ranked on a scale of 0 (never
occurs) to 5 (always occurs). The perceived supportive
barriers and supportive behaviors in caring for dying
children. The frequency of occurrence of the obstacles
and supportive behaviors also was measured, and
magnitude scores were calculated.
Sample
After the study was approved by the appropri-
ate institutional review board, a geographically
diverse sample of 1047 PICU nurses was obtained
from the American Association of Critical-Care
Nurses (AACN). AACN members who read English,
cared for infants and children, and had experience
in end-of-life care were considered eligible for the
study. Return of the questionnaire was considered
consent to participate in the study.
Instrument
The National Survey of Pediatric Nurses’ Per-
ceptions of End-of-Life Care questionnaire used for
the study was adapted from 3 similar surveys with
critical care nurses,9 emergency nurses,11 and oncol-
ogy nurses.12 In order to strengthen content validity,
information from experts was used to further revise
questionnaire items. The questionnaire was pretested
by 27 pediatric nurses experienced in the care of dying
children. Changes in items were made on the basis of
the nurses’ comments and suggestions. The question-
naire took approximately 23 minutes to complete.
Procedure
Mailing information for the survey was pur-
chased from AACN. Questionnaires were mailed
with a cover letter explaining the purposes of the
study and with a self-addressed, stamped return
envelope. One additional mailing to nonresponders
was completed several months after the initial mail-
ing. The second mailing consisted of a new cover
letter, another copy of the questionnaire, and a
self-addressed stamped envelope for ease of return.
Data Analysis
SPSS software (SPSS Inc, Chicago, Illinois) was
used for data analysis. Frequencies, measures of cen-
tral tendency, dispersion, and reliability statistics were
calculated. Items were ranked from highest to lowest
on the basis of the mean scores. Items on obstacles
and supportive behaviors also were ranked from most
frequently occurring to least frequently occurring on
the basis of the items’ mean frequency scores. Cron-
bachα scores were calculated to determine internal
consistency estimates of reliability for the size and
the frequency of the obstacle items (0.93 and 0.88,
respectively) and of the supportive behavior items
(0.85 and 0.79, respectively).
www.ajcconline.org AA JJCCCC AMERICAN JOURNAL OF CRITICAL CARE, November 2010, Volume 19, No. 6545
Obstacles with the
greatest impact
were language ba
riers and parents’
discomfort with
withdrawing
mechanical
ventilation.
by AACN on September 7, 2018http://ajcc.aacnjournals.org/Downloaded from
Demographic Data
Of the 1047 potential respondents, 536 returned
questionnaires. A total of 62 questionnaires were
considered ineligible because they were returned by
respondents who did not feel qualified to complete
the questionnaire, were retired, or were no longer
working in a PICU. A few questionnaires were returned
as undeliverable and so were also unusable. Usable
responses were received from 474 of 985 eligible
respondents, for a response rate of 48% after 2 mail-
ings.13 Because the sample was randomly selected,
geographically dispersed, and of adequate size,
results are generalizable to PICU nurses who are
members of AACN. Of the 472 respondents, 439
(92.6%) were women and 33
(7.0%) were men (Table 1). This
percentage of men is slightly lower
than the national AACN member-
ship demographics of 11% men.
Obstacle Magnitude
Respondents ranked all obstacle
items in the questionnaire by both
size and frequency. The scale used for
obstacle size ranged from 0 (not an
obstacle) to 5 (extremely large). A
similar scale of 0 (never occurs) to 5
(always occurs) was used for scoring
item frequencies. An obstacle’s perceived magnitude or
impact was determined by multiplying its mean size
(intensity) by its mean frequency to obtain a POM
score.9,11,14
For the 32 rated obstacles, the POM scores
ranged from a high of 17.73 to a low of 1.99 (Table
2). The item with the highest POM score was language
barriers (score, 17.73), which had both the highest
mean intensity and the highest mean frequency.
The next 3 obstacles with the highest POM scores
were parental discomfort in withholding and/or with-
drawing mechanical ventilation (score, 17.69), dis-
continuity of care of the dying child due to lack of
communication between interdisciplinary team mem-
bers (13.49), and the nurse’s opinion about the direc-
tion of the patient’s care not being valued (13.36).
The 2 obstacles with the lowest POM scores were
nurses believing that life-saving measures or treatments
are stopped too soon (score, 1.99) and nurses getting
vague orders such as “titrate to effect” for pain (2.65).
Supportive Behavior Magnitude
Supportive behaviors were ranked on a scale of 0
(not a help) to 5 (extremely large). Perceived frequen-
cies for each item were ranked on a scale of 0 (never
occurs) to 5 (always occurs). The perceived supportive
barriers and supportive behaviors in caring for dying
children. The frequency of occurrence of the obstacles
and supportive behaviors also was measured, and
magnitude scores were calculated.
Sample
After the study was approved by the appropri-
ate institutional review board, a geographically
diverse sample of 1047 PICU nurses was obtained
from the American Association of Critical-Care
Nurses (AACN). AACN members who read English,
cared for infants and children, and had experience
in end-of-life care were considered eligible for the
study. Return of the questionnaire was considered
consent to participate in the study.
Instrument
The National Survey of Pediatric Nurses’ Per-
ceptions of End-of-Life Care questionnaire used for
the study was adapted from 3 similar surveys with
critical care nurses,9 emergency nurses,11 and oncol-
ogy nurses.12 In order to strengthen content validity,
information from experts was used to further revise
questionnaire items. The questionnaire was pretested
by 27 pediatric nurses experienced in the care of dying
children. Changes in items were made on the basis of
the nurses’ comments and suggestions. The question-
naire took approximately 23 minutes to complete.
Procedure
Mailing information for the survey was pur-
chased from AACN. Questionnaires were mailed
with a cover letter explaining the purposes of the
study and with a self-addressed, stamped return
envelope. One additional mailing to nonresponders
was completed several months after the initial mail-
ing. The second mailing consisted of a new cover
letter, another copy of the questionnaire, and a
self-addressed stamped envelope for ease of return.
Data Analysis
SPSS software (SPSS Inc, Chicago, Illinois) was
used for data analysis. Frequencies, measures of cen-
tral tendency, dispersion, and reliability statistics were
calculated. Items were ranked from highest to lowest
on the basis of the mean scores. Items on obstacles
and supportive behaviors also were ranked from most
frequently occurring to least frequently occurring on
the basis of the items’ mean frequency scores. Cron-
bachα scores were calculated to determine internal
consistency estimates of reliability for the size and
the frequency of the obstacle items (0.93 and 0.88,
respectively) and of the supportive behavior items
(0.85 and 0.79, respectively).
www.ajcconline.org AA JJCCCC AMERICAN JOURNAL OF CRITICAL CARE, November 2010, Volume 19, No. 6545
Obstacles with the
greatest impact
were language ba
riers and parents’
discomfort with
withdrawing
mechanical
ventilation.
by AACN on September 7, 2018http://ajcc.aacnjournals.org/Downloaded from
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
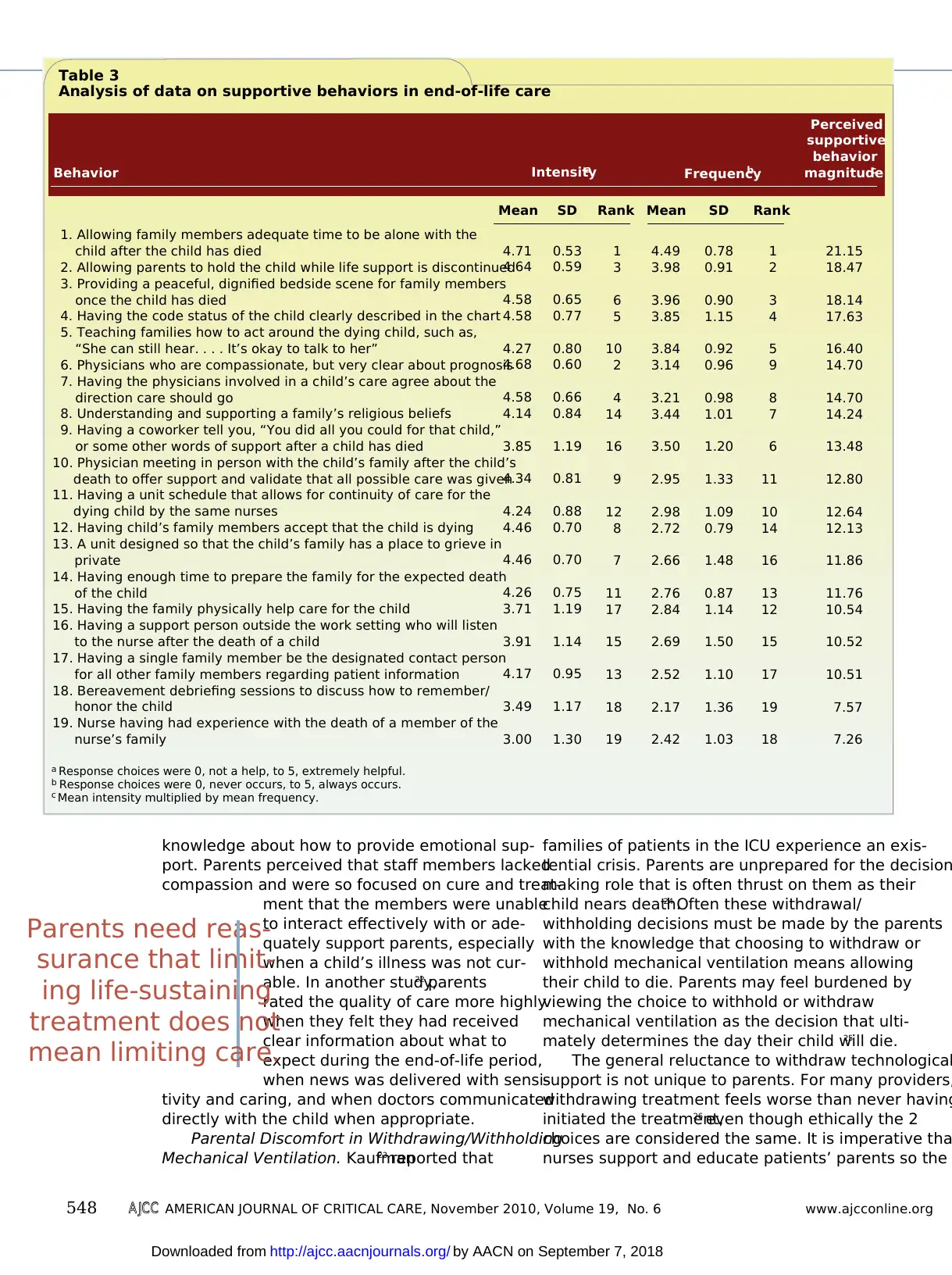
behavior magnitude (PSBM) score for each item was
obtained by multiplying the item’s mean size (inten-
sity) by the item’s mean frequency.9,11,14PSBM scores
ranged from a high of 21.15 to a low of 7.26 (Table 3),
which were higher overall than the magnitude scores
for the obstacle items. The highest PSBM score was
21.15 for the item of allowing family members ade-
quate time alone with the child after the child has
died. This item had both the largest mean intensity
(4.71) and the highest mean frequency (4.49).
The 3 supportive behaviors with the next high-
est PSBM scores were allowing parents to hold the
child while life support is discontinued (score, 18.47);
providing a peaceful, dignified bedside scene for
family members once the child has died (18.14);
and having the code status of the child clearly
described in the chart (17.63).
The 2 behaviors with the lowest PSBM scores
were the nurse having had experience with the death
of a member of the nurse’s family (score, 7.26) and
bereavement debriefing sessions to discuss how to
remember/honor the child (7.57).
Discussion
Obstacle Results
Language Barriers. The obstacle with the highest
magnitude score was language barriers. Difficulty
with communication between practitioner and patien
is inherent in virtually all clinical practice settings,
but is even more difficult when caring for very young
children. Communication difficulties between prac-
titioner and patient is congruent with the results of
other studies4,5,15in which language was a barrier that
impeded care. Because communication between
practitioners and a patient’s family can be a barrier
and is so vital to the connection with the family, a
family’s experience could be altered greatly if mem-
bers of the family had difficulty understanding Eng-
lish.16 In a study17 of registered nurses (n = 101) and
advance practice nurses (n=89), most nurses indicate
that language or cultural differences were influential
or very influential in nurses’ involvement with patient
families. These findings suggest a need for cultural
competence and increased nursing education in cul-
tural humility.18
Although improved communication has been
recommended for better end-of-life care,19 nurses
also must be aware of their own values, understand-
ings, and comfort levels with the language of death
before better communication can be accomplished.
To improve end-of-life communication, nurses and
physicians need to be comfortable talking about
death, realizing that some children in their care will
still die despite everyone’s best efforts.20
In a study of 45 parents who had experienced
the death of a child, Davies and Connaughty21
found that only 20% of the parents were satisfied
with the communication competence of the health
care staff. The parents thought the staff lacked
Table 1
Demographics of the sample (n = 474)
Characteristic Valuea
a Because of rounding, not all percentages total 100.
Sex, No. (%)
Male
Female
Did not report
Age, mean (SD), range, y
Years as registered nurse, mean (SD), range
Years in pediatric/neonatal intensive care,
mean (SD), range
Hours worked per week, mean (SD), range
Number of beds in unit, mean (SD), range
No. of dying patients cared for, %
>30
21-30
11-20
<10
Highest degree, %
Diploma
Associate’s
Bachelor’s
Master’s
Doctoral
Ever a CCRN, %
Yes
No
Years as CCRN, mean (SD), range
Currently CCRN, %
Yes
No
Other certifications, %
Position held at facility, %
Direct care/bedside/staff nurse
Other
Clinical nurse specialist
Department manager/educator
Participation in end-of-life care program, %
Yes
No
Hospital type, %
Nonprofit, community
For profit, community
University medical center
Federal
State
County
Military
Pediatric/other
33 (7)
439 (92.6)
2 (0.4)
41 (10.9), 22-65
15.3 (10.7), 1-42
13.3 (9.8), 0.5-41
35.3 (8.6), 0-80
23.5 (14.3), 4-120
38.9
12.6
22.1
26.4
5.5
70.7
20.9
2.3
0.4
61.7
38.3
7.6 (6.59), 1-24
40.9
58.8
31.4
84.3
3.2
5.7
6.8
13.1
86.9
37.2
7.2
46.5
0.6
0.8
4.5
0.4
2.8
546 AA JJCCCC AMERICAN JOURNAL OF CRITICAL CARE, November 2010, Volume 19, No. 6 www.ajcconline.org
by AACN on September 7, 2018http://ajcc.aacnjournals.org/Downloaded from
obtained by multiplying the item’s mean size (inten-
sity) by the item’s mean frequency.9,11,14PSBM scores
ranged from a high of 21.15 to a low of 7.26 (Table 3),
which were higher overall than the magnitude scores
for the obstacle items. The highest PSBM score was
21.15 for the item of allowing family members ade-
quate time alone with the child after the child has
died. This item had both the largest mean intensity
(4.71) and the highest mean frequency (4.49).
The 3 supportive behaviors with the next high-
est PSBM scores were allowing parents to hold the
child while life support is discontinued (score, 18.47);
providing a peaceful, dignified bedside scene for
family members once the child has died (18.14);
and having the code status of the child clearly
described in the chart (17.63).
The 2 behaviors with the lowest PSBM scores
were the nurse having had experience with the death
of a member of the nurse’s family (score, 7.26) and
bereavement debriefing sessions to discuss how to
remember/honor the child (7.57).
Discussion
Obstacle Results
Language Barriers. The obstacle with the highest
magnitude score was language barriers. Difficulty
with communication between practitioner and patien
is inherent in virtually all clinical practice settings,
but is even more difficult when caring for very young
children. Communication difficulties between prac-
titioner and patient is congruent with the results of
other studies4,5,15in which language was a barrier that
impeded care. Because communication between
practitioners and a patient’s family can be a barrier
and is so vital to the connection with the family, a
family’s experience could be altered greatly if mem-
bers of the family had difficulty understanding Eng-
lish.16 In a study17 of registered nurses (n = 101) and
advance practice nurses (n=89), most nurses indicate
that language or cultural differences were influential
or very influential in nurses’ involvement with patient
families. These findings suggest a need for cultural
competence and increased nursing education in cul-
tural humility.18
Although improved communication has been
recommended for better end-of-life care,19 nurses
also must be aware of their own values, understand-
ings, and comfort levels with the language of death
before better communication can be accomplished.
To improve end-of-life communication, nurses and
physicians need to be comfortable talking about
death, realizing that some children in their care will
still die despite everyone’s best efforts.20
In a study of 45 parents who had experienced
the death of a child, Davies and Connaughty21
found that only 20% of the parents were satisfied
with the communication competence of the health
care staff. The parents thought the staff lacked
Table 1
Demographics of the sample (n = 474)
Characteristic Valuea
a Because of rounding, not all percentages total 100.
Sex, No. (%)
Male
Female
Did not report
Age, mean (SD), range, y
Years as registered nurse, mean (SD), range
Years in pediatric/neonatal intensive care,
mean (SD), range
Hours worked per week, mean (SD), range
Number of beds in unit, mean (SD), range
No. of dying patients cared for, %
>30
21-30
11-20
<10
Highest degree, %
Diploma
Associate’s
Bachelor’s
Master’s
Doctoral
Ever a CCRN, %
Yes
No
Years as CCRN, mean (SD), range
Currently CCRN, %
Yes
No
Other certifications, %
Position held at facility, %
Direct care/bedside/staff nurse
Other
Clinical nurse specialist
Department manager/educator
Participation in end-of-life care program, %
Yes
No
Hospital type, %
Nonprofit, community
For profit, community
University medical center
Federal
State
County
Military
Pediatric/other
33 (7)
439 (92.6)
2 (0.4)
41 (10.9), 22-65
15.3 (10.7), 1-42
13.3 (9.8), 0.5-41
35.3 (8.6), 0-80
23.5 (14.3), 4-120
38.9
12.6
22.1
26.4
5.5
70.7
20.9
2.3
0.4
61.7
38.3
7.6 (6.59), 1-24
40.9
58.8
31.4
84.3
3.2
5.7
6.8
13.1
86.9
37.2
7.2
46.5
0.6
0.8
4.5
0.4
2.8
546 AA JJCCCC AMERICAN JOURNAL OF CRITICAL CARE, November 2010, Volume 19, No. 6 www.ajcconline.org
by AACN on September 7, 2018http://ajcc.aacnjournals.org/Downloaded from
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
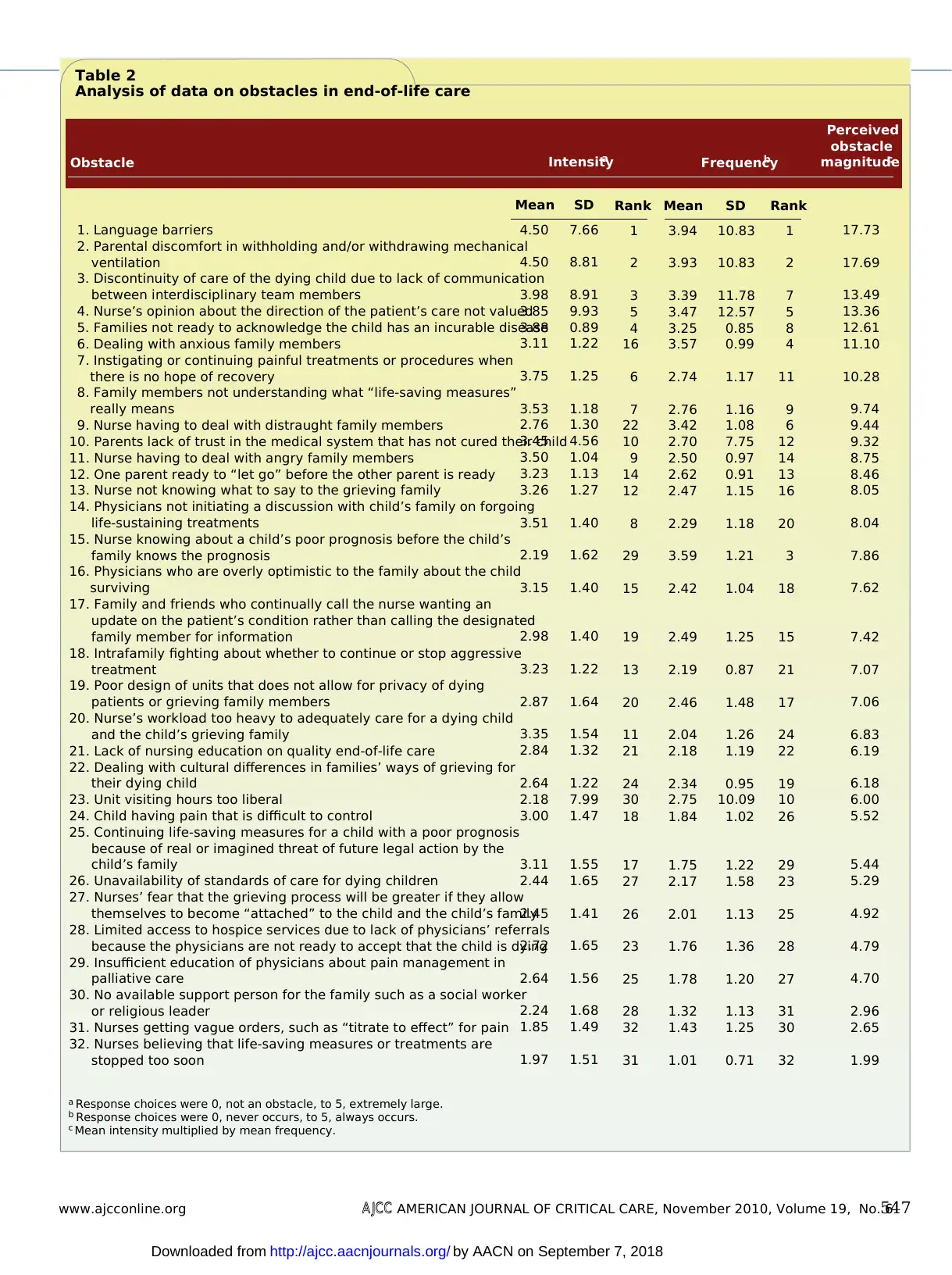
Table 2
Analysis of data on obstacles in end-of-life care
1. Language barriers
2. Parental discomfort in withholding and/or withdrawing mechanical
ventilation
3. Discontinuity of care of the dying child due to lack of communication
between interdisciplinary team members
4. Nurse’s opinion about the direction of the patient’s care not valued
5. Families not ready to acknowledge the child has an incurable disease
6. Dealing with anxious family members
7. Instigating or continuing painful treatments or procedures when
there is no hope of recovery
8. Family members not understanding what “life-saving measures”
really means
9. Nurse having to deal with distraught family members
10. Parents lack of trust in the medical system that has not cured their child
11. Nurse having to deal with angry family members
12. One parent ready to “let go” before the other parent is ready
13. Nurse not knowing what to say to the grieving family
14. Physicians not initiating a discussion with child’s family on forgoing
life-sustaining treatments
15. Nurse knowing about a child’s poor prognosis before the child’s
family knows the prognosis
16. Physicians who are overly optimistic to the family about the child
surviving
17. Family and friends who continually call the nurse wanting an
update on the patient’s condition rather than calling the designated
family member for information
18. Intrafamily fighting about whether to continue or stop aggressive
treatment
19. Poor design of units that does not allow for privacy of dying
patients or grieving family members
20. Nurse’s workload too heavy to adequately care for a dying child
and the child’s grieving family
21. Lack of nursing education on quality end-of-life care
22. Dealing with cultural differences in families’ ways of grieving for
their dying child
23. Unit visiting hours too liberal
24. Child having pain that is difficult to control
25. Continuing life-saving measures for a child with a poor prognosis
because of real or imagined threat of future legal action by the
child’s family
26. Unavailability of standards of care for dying children
27. Nurses’ fear that the grieving process will be greater if they allow
themselves to become “attached” to the child and the child’s family
28. Limited access to hospice services due to lack of physicians’ referrals
because the physicians are not ready to accept that the child is dying
29. Insufficient education of physicians about pain management in
palliative care
30. No available support person for the family such as a social worker
or religious leader
31. Nurses getting vague orders, such as “titrate to effect” for pain
32. Nurses believing that life-saving measures or treatments are
stopped too soon
17.73
17.69
13.49
13.36
12.61
11.10
10.28
9.74
9.44
9.32
8.75
8.46
8.05
8.04
7.86
7.62
7.42
7.07
7.06
6.83
6.19
6.18
6.00
5.52
5.44
5.29
4.92
4.79
4.70
2.96
2.65
1.99
Rank
1
2
7
5
8
4
11
9
6
12
14
13
16
20
3
18
15
21
17
24
22
19
10
26
29
23
25
28
27
31
30
32
SD
10.83
10.83
11.78
12.57
0.85
0.99
1.17
1.16
1.08
7.75
0.97
0.91
1.15
1.18
1.21
1.04
1.25
0.87
1.48
1.26
1.19
0.95
10.09
1.02
1.22
1.58
1.13
1.36
1.20
1.13
1.25
0.71
Mean
3.94
3.93
3.39
3.47
3.25
3.57
2.74
2.76
3.42
2.70
2.50
2.62
2.47
2.29
3.59
2.42
2.49
2.19
2.46
2.04
2.18
2.34
2.75
1.84
1.75
2.17
2.01
1.76
1.78
1.32
1.43
1.01
Rank
1
2
3
5
4
16
6
7
22
10
9
14
12
8
29
15
19
13
20
11
21
24
30
18
17
27
26
23
25
28
32
31
SD
7.66
8.81
8.91
9.93
0.89
1.22
1.25
1.18
1.30
4.56
1.04
1.13
1.27
1.40
1.62
1.40
1.40
1.22
1.64
1.54
1.32
1.22
7.99
1.47
1.55
1.65
1.41
1.65
1.56
1.68
1.49
1.51
Mean
4.50
4.50
3.98
3.85
3.88
3.11
3.75
3.53
2.76
3.45
3.50
3.23
3.26
3.51
2.19
3.15
2.98
3.23
2.87
3.35
2.84
2.64
2.18
3.00
3.11
2.44
2.45
2.72
2.64
2.24
1.85
1.97
Obstacle FrequencybIntensitya
Perceived
obstacle
magnitudec
a Response choices were 0, not an obstacle, to 5, extremely large.
b Response choices were 0, never occurs, to 5, always occurs.
c Mean intensity multiplied by mean frequency.
www.ajcconline.org AA JJCCCC AMERICAN JOURNAL OF CRITICAL CARE, November 2010, Volume 19, No. 6547
by AACN on September 7, 2018http://ajcc.aacnjournals.org/Downloaded from
Analysis of data on obstacles in end-of-life care
1. Language barriers
2. Parental discomfort in withholding and/or withdrawing mechanical
ventilation
3. Discontinuity of care of the dying child due to lack of communication
between interdisciplinary team members
4. Nurse’s opinion about the direction of the patient’s care not valued
5. Families not ready to acknowledge the child has an incurable disease
6. Dealing with anxious family members
7. Instigating or continuing painful treatments or procedures when
there is no hope of recovery
8. Family members not understanding what “life-saving measures”
really means
9. Nurse having to deal with distraught family members
10. Parents lack of trust in the medical system that has not cured their child
11. Nurse having to deal with angry family members
12. One parent ready to “let go” before the other parent is ready
13. Nurse not knowing what to say to the grieving family
14. Physicians not initiating a discussion with child’s family on forgoing
life-sustaining treatments
15. Nurse knowing about a child’s poor prognosis before the child’s
family knows the prognosis
16. Physicians who are overly optimistic to the family about the child
surviving
17. Family and friends who continually call the nurse wanting an
update on the patient’s condition rather than calling the designated
family member for information
18. Intrafamily fighting about whether to continue or stop aggressive
treatment
19. Poor design of units that does not allow for privacy of dying
patients or grieving family members
20. Nurse’s workload too heavy to adequately care for a dying child
and the child’s grieving family
21. Lack of nursing education on quality end-of-life care
22. Dealing with cultural differences in families’ ways of grieving for
their dying child
23. Unit visiting hours too liberal
24. Child having pain that is difficult to control
25. Continuing life-saving measures for a child with a poor prognosis
because of real or imagined threat of future legal action by the
child’s family
26. Unavailability of standards of care for dying children
27. Nurses’ fear that the grieving process will be greater if they allow
themselves to become “attached” to the child and the child’s family
28. Limited access to hospice services due to lack of physicians’ referrals
because the physicians are not ready to accept that the child is dying
29. Insufficient education of physicians about pain management in
palliative care
30. No available support person for the family such as a social worker
or religious leader
31. Nurses getting vague orders, such as “titrate to effect” for pain
32. Nurses believing that life-saving measures or treatments are
stopped too soon
17.73
17.69
13.49
13.36
12.61
11.10
10.28
9.74
9.44
9.32
8.75
8.46
8.05
8.04
7.86
7.62
7.42
7.07
7.06
6.83
6.19
6.18
6.00
5.52
5.44
5.29
4.92
4.79
4.70
2.96
2.65
1.99
Rank
1
2
7
5
8
4
11
9
6
12
14
13
16
20
3
18
15
21
17
24
22
19
10
26
29
23
25
28
27
31
30
32
SD
10.83
10.83
11.78
12.57
0.85
0.99
1.17
1.16
1.08
7.75
0.97
0.91
1.15
1.18
1.21
1.04
1.25
0.87
1.48
1.26
1.19
0.95
10.09
1.02
1.22
1.58
1.13
1.36
1.20
1.13
1.25
0.71
Mean
3.94
3.93
3.39
3.47
3.25
3.57
2.74
2.76
3.42
2.70
2.50
2.62
2.47
2.29
3.59
2.42
2.49
2.19
2.46
2.04
2.18
2.34
2.75
1.84
1.75
2.17
2.01
1.76
1.78
1.32
1.43
1.01
Rank
1
2
3
5
4
16
6
7
22
10
9
14
12
8
29
15
19
13
20
11
21
24
30
18
17
27
26
23
25
28
32
31
SD
7.66
8.81
8.91
9.93
0.89
1.22
1.25
1.18
1.30
4.56
1.04
1.13
1.27
1.40
1.62
1.40
1.40
1.22
1.64
1.54
1.32
1.22
7.99
1.47
1.55
1.65
1.41
1.65
1.56
1.68
1.49
1.51
Mean
4.50
4.50
3.98
3.85
3.88
3.11
3.75
3.53
2.76
3.45
3.50
3.23
3.26
3.51
2.19
3.15
2.98
3.23
2.87
3.35
2.84
2.64
2.18
3.00
3.11
2.44
2.45
2.72
2.64
2.24
1.85
1.97
Obstacle FrequencybIntensitya
Perceived
obstacle
magnitudec
a Response choices were 0, not an obstacle, to 5, extremely large.
b Response choices were 0, never occurs, to 5, always occurs.
c Mean intensity multiplied by mean frequency.
www.ajcconline.org AA JJCCCC AMERICAN JOURNAL OF CRITICAL CARE, November 2010, Volume 19, No. 6547
by AACN on September 7, 2018http://ajcc.aacnjournals.org/Downloaded from
knowledge about how to provide emotional sup-
port. Parents perceived that staff members lacked
compassion and were so focused on cure and treat-
ment that the members were unable
to interact effectively with or ade-
quately support parents, especially
when a child’s illness was not cur-
able. In another study,22 parents
rated the quality of care more highly
when they felt they had received
clear information about what to
expect during the end-of-life period,
when news was delivered with sensi-
tivity and caring, and when doctors communicated
directly with the child when appropriate.
Parental Discomfort in Withdrawing/Withholding
Mechanical Ventilation. Kaufman23 reported that
families of patients in the ICU experience an exis-
tential crisis. Parents are unprepared for the decision
making role that is often thrust on them as their
child nears death.24 Often these withdrawal/
withholding decisions must be made by the parents
with the knowledge that choosing to withdraw or
withhold mechanical ventilation means allowing
their child to die. Parents may feel burdened by
viewing the choice to withhold or withdraw
mechanical ventilation as the decision that ulti-
mately determines the day their child will die.25
The general reluctance to withdraw technological
support is not unique to parents. For many providers,
withdrawing treatment feels worse than never having
initiated the treatment,26 even though ethically the 2
choices are considered the same. It is imperative tha
nurses support and educate patients’ parents so the
Table 3
Analysis of data on supportive behaviors in end-of-life care
1. Allowing family members adequate time to be alone with the
child after the child has died
2. Allowing parents to hold the child while life support is discontinued
3. Providing a peaceful, dignified bedside scene for family members
once the child has died
4. Having the code status of the child clearly described in the chart
5. Teaching families how to act around the dying child, such as,
“She can still hear. . . . It’s okay to talk to her”
6. Physicians who are compassionate, but very clear about prognosis
7. Having the physicians involved in a child’s care agree about the
direction care should go
8. Understanding and supporting a family’s religious beliefs
9. Having a coworker tell you, “You did all you could for that child,”
or some other words of support after a child has died
10. Physician meeting in person with the child’s family after the child’s
death to offer support and validate that all possible care was given
11. Having a unit schedule that allows for continuity of care for the
dying child by the same nurses
12. Having child’s family members accept that the child is dying
13. A unit designed so that the child’s family has a place to grieve in
private
14. Having enough time to prepare the family for the expected death
of the child
15. Having the family physically help care for the child
16. Having a support person outside the work setting who will listen
to the nurse after the death of a child
17. Having a single family member be the designated contact person
for all other family members regarding patient information
18. Bereavement debriefing sessions to discuss how to remember/
honor the child
19. Nurse having had experience with the death of a member of the
nurse’s family
21.15
18.47
18.14
17.63
16.40
14.70
14.70
14.24
13.48
12.80
12.64
12.13
11.86
11.76
10.54
10.52
10.51
7.57
7.26
Rank
1
2
3
4
5
9
8
7
6
11
10
14
16
13
12
15
17
19
18
SD
0.78
0.91
0.90
1.15
0.92
0.96
0.98
1.01
1.20
1.33
1.09
0.79
1.48
0.87
1.14
1.50
1.10
1.36
1.03
Mean
4.49
3.98
3.96
3.85
3.84
3.14
3.21
3.44
3.50
2.95
2.98
2.72
2.66
2.76
2.84
2.69
2.52
2.17
2.42
Rank
1
3
6
5
10
2
4
14
16
9
12
8
7
11
17
15
13
18
19
SD
0.53
0.59
0.65
0.77
0.80
0.60
0.66
0.84
1.19
0.81
0.88
0.70
0.70
0.75
1.19
1.14
0.95
1.17
1.30
Mean
4.71
4.64
4.58
4.58
4.27
4.68
4.58
4.14
3.85
4.34
4.24
4.46
4.46
4.26
3.71
3.91
4.17
3.49
3.00
Behavior FrequencybIntensitya
Perceived
supportive
behavior
magnitudec
a Response choices were 0, not a help, to 5, extremely helpful.
b Response choices were 0, never occurs, to 5, always occurs.
c Mean intensity multiplied by mean frequency.
548 AA JJCCCC AMERICAN JOURNAL OF CRITICAL CARE, November 2010, Volume 19, No. 6 www.ajcconline.org
Parents need reas-
surance that limit-
ing life-sustaining
treatment does not
mean limiting care.
by AACN on September 7, 2018http://ajcc.aacnjournals.org/Downloaded from
port. Parents perceived that staff members lacked
compassion and were so focused on cure and treat-
ment that the members were unable
to interact effectively with or ade-
quately support parents, especially
when a child’s illness was not cur-
able. In another study,22 parents
rated the quality of care more highly
when they felt they had received
clear information about what to
expect during the end-of-life period,
when news was delivered with sensi-
tivity and caring, and when doctors communicated
directly with the child when appropriate.
Parental Discomfort in Withdrawing/Withholding
Mechanical Ventilation. Kaufman23 reported that
families of patients in the ICU experience an exis-
tential crisis. Parents are unprepared for the decision
making role that is often thrust on them as their
child nears death.24 Often these withdrawal/
withholding decisions must be made by the parents
with the knowledge that choosing to withdraw or
withhold mechanical ventilation means allowing
their child to die. Parents may feel burdened by
viewing the choice to withhold or withdraw
mechanical ventilation as the decision that ulti-
mately determines the day their child will die.25
The general reluctance to withdraw technological
support is not unique to parents. For many providers,
withdrawing treatment feels worse than never having
initiated the treatment,26 even though ethically the 2
choices are considered the same. It is imperative tha
nurses support and educate patients’ parents so the
Table 3
Analysis of data on supportive behaviors in end-of-life care
1. Allowing family members adequate time to be alone with the
child after the child has died
2. Allowing parents to hold the child while life support is discontinued
3. Providing a peaceful, dignified bedside scene for family members
once the child has died
4. Having the code status of the child clearly described in the chart
5. Teaching families how to act around the dying child, such as,
“She can still hear. . . . It’s okay to talk to her”
6. Physicians who are compassionate, but very clear about prognosis
7. Having the physicians involved in a child’s care agree about the
direction care should go
8. Understanding and supporting a family’s religious beliefs
9. Having a coworker tell you, “You did all you could for that child,”
or some other words of support after a child has died
10. Physician meeting in person with the child’s family after the child’s
death to offer support and validate that all possible care was given
11. Having a unit schedule that allows for continuity of care for the
dying child by the same nurses
12. Having child’s family members accept that the child is dying
13. A unit designed so that the child’s family has a place to grieve in
private
14. Having enough time to prepare the family for the expected death
of the child
15. Having the family physically help care for the child
16. Having a support person outside the work setting who will listen
to the nurse after the death of a child
17. Having a single family member be the designated contact person
for all other family members regarding patient information
18. Bereavement debriefing sessions to discuss how to remember/
honor the child
19. Nurse having had experience with the death of a member of the
nurse’s family
21.15
18.47
18.14
17.63
16.40
14.70
14.70
14.24
13.48
12.80
12.64
12.13
11.86
11.76
10.54
10.52
10.51
7.57
7.26
Rank
1
2
3
4
5
9
8
7
6
11
10
14
16
13
12
15
17
19
18
SD
0.78
0.91
0.90
1.15
0.92
0.96
0.98
1.01
1.20
1.33
1.09
0.79
1.48
0.87
1.14
1.50
1.10
1.36
1.03
Mean
4.49
3.98
3.96
3.85
3.84
3.14
3.21
3.44
3.50
2.95
2.98
2.72
2.66
2.76
2.84
2.69
2.52
2.17
2.42
Rank
1
3
6
5
10
2
4
14
16
9
12
8
7
11
17
15
13
18
19
SD
0.53
0.59
0.65
0.77
0.80
0.60
0.66
0.84
1.19
0.81
0.88
0.70
0.70
0.75
1.19
1.14
0.95
1.17
1.30
Mean
4.71
4.64
4.58
4.58
4.27
4.68
4.58
4.14
3.85
4.34
4.24
4.46
4.46
4.26
3.71
3.91
4.17
3.49
3.00
Behavior FrequencybIntensitya
Perceived
supportive
behavior
magnitudec
a Response choices were 0, not a help, to 5, extremely helpful.
b Response choices were 0, never occurs, to 5, always occurs.
c Mean intensity multiplied by mean frequency.
548 AA JJCCCC AMERICAN JOURNAL OF CRITICAL CARE, November 2010, Volume 19, No. 6 www.ajcconline.org
Parents need reas-
surance that limit-
ing life-sustaining
treatment does not
mean limiting care.
by AACN on September 7, 2018http://ajcc.aacnjournals.org/Downloaded from
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

palliative and curative therapies beginning at diagno-
sis so no delay occurs in establishing either type of
therapy and respite care for children and children’s
families who are going through such a difficult process.
Nurse’s Opinions Not Valued. Although Miller et al33
reported that most research findings suggest nurses
have a limited role in end-of-life
decision making and care planning,
nurses are often the first to be aware
of the transition from potential
recovery to a realization that curative
efforts most likely are futile.24 Critical
care nurses play a pivotal role in cli-
nician- family communication in the
ICU and may have valuable insights
into the progress of a disease, the
families’ perceptions and wishes,
and the families’ level of under-
standing and unique needs. Nurses
are an important part of the health
care team. More importantly, families rate nurses’
communication skills as one of the most important
skills of ICU clinicians.19
Lowest Scoring Obstacles. Nurses believing that
life-saving measures or treatments are stopped too
soon was the lowest scoring obstacle. Possibly the
nurses in our sample believe that stopping treatment
too soon does not often happen, or perhaps the
impact of this obstacle was low. Solomon et al26
reported that the number of physicians and nurses
who were concerned about the provision of overly
burdensome treatment was 4 times greater than the
number who were concerned about undertreatment.
Another low scoring item was nurses getting
vague orders, such as “titrate to effect” for pain med-
ications. This score may have been low because nurses
feel competent and actually prefer
being able to decide how much pain
medication to give dying children.
Feudtner et al34 found that nurses
felt most competent about pain
management and least competent
about talking with children and the
children’s families about dying. Of
note, nurses in the future should
receive fewer titrate-to-effect orders
for pain medication because cur-
rent Joint Commission guidelines35
state that all medication orders must
include “the degree of accuracy,
completeness, and discrimination necessary for
their intended use.” Thus, physicians are required
to order specific dosages and frequencies of med-
ications, and a nurse who determines dosages and
parents can make decisions for continuation or with-
drawal of treatment. Robichaux and Clark24 wrote of
the need for nurses to protect and oftentimes be the
voice of the patient in order to prevent further tech-
nological intrusion. The real choice may not be
between life or death, but how the child will live
until death occurs.20 Nurses have acknowledged that
although mechanical ventilation is often associated
with the breath of life, use of this technology can
also extend suffering. In a study27 with critical care
nurses on end-of-life care, a participant stated, “We
[nurses] are trapped between technology and reality.”
Parents need reassurance that limiting life-
sustaining treatment does not mean limiting care.25
Ideally, parents should be educated that withdrawal
of aggressive therapies is not seen as surrendering
to death or abandoning hope. Parents should have
an understanding of what is best for the child and
what the child would want, if she or he could com-
municate, should curative efforts be unsuccessful.
Brandon et al28 found that children who died
in critical care areas were more likely to have experi-
enced withdrawal of respiratory or medical support
as end-of-life interventions, whereas children who
died in intermediate units were more likely to have a
do-not-resuscitate order, including no use of endo-
tracheal intubation or use of only drugs to resusci-
tate the child if he or she stopped breathing or the
heart stopped. These findings partly reflect the fact
that respiratory compromise requiring endotracheal
intubation is an intervention reserved for critical care
settings and that ICUs have unique and often chal-
lenging issues associated with ethical end-of-life care.
The finding that most children die in the ICU may
indicate that hospitalized children are receiving more
complex medical treatments than can be provided
on general pediatric units, and once therapy is initi-
ated, discontinuing it is often difficult.25,29
Discontinuity of Care Between Interdisciplinary Team
Members. Frustration occurs when providers do not
share the same perspectives and goals for a patient.
Having even a single physician unable to recognize
that a child is terminal can give the child’s family
false hope. Having medical subspecialists contradict
one another creates confusion for a patient’s family
and may result in digression when time is critical.
When a patient is not correctly recognized as termi-
nal, curative regimens take precedence and a child’s
unnecessary suffering may be prolonged.19
Many nurses in our study commented on the
need for early recognition of likely death rather
than waiting until a child starts to decompensate
dramatically before palliative care is initiated. Cur-
rent research30-32 supports a coexistent approach with
www.ajcconline.org AA JJCCCC AMERICAN JOURNAL OF CRITICAL CARE, November 2010, Volume 19, No. 6549
The supportive
behavior with the
greatest impact
was allowing fam-
ily members ade-
quate time with th
child after the
child has died.
Further research
is needed to
decrease highly
rated obstacles
and to continue
to support highly
rated supportive
behaviors.
by AACN on September 7, 2018http://ajcc.aacnjournals.org/Downloaded from
sis so no delay occurs in establishing either type of
therapy and respite care for children and children’s
families who are going through such a difficult process.
Nurse’s Opinions Not Valued. Although Miller et al33
reported that most research findings suggest nurses
have a limited role in end-of-life
decision making and care planning,
nurses are often the first to be aware
of the transition from potential
recovery to a realization that curative
efforts most likely are futile.24 Critical
care nurses play a pivotal role in cli-
nician- family communication in the
ICU and may have valuable insights
into the progress of a disease, the
families’ perceptions and wishes,
and the families’ level of under-
standing and unique needs. Nurses
are an important part of the health
care team. More importantly, families rate nurses’
communication skills as one of the most important
skills of ICU clinicians.19
Lowest Scoring Obstacles. Nurses believing that
life-saving measures or treatments are stopped too
soon was the lowest scoring obstacle. Possibly the
nurses in our sample believe that stopping treatment
too soon does not often happen, or perhaps the
impact of this obstacle was low. Solomon et al26
reported that the number of physicians and nurses
who were concerned about the provision of overly
burdensome treatment was 4 times greater than the
number who were concerned about undertreatment.
Another low scoring item was nurses getting
vague orders, such as “titrate to effect” for pain med-
ications. This score may have been low because nurses
feel competent and actually prefer
being able to decide how much pain
medication to give dying children.
Feudtner et al34 found that nurses
felt most competent about pain
management and least competent
about talking with children and the
children’s families about dying. Of
note, nurses in the future should
receive fewer titrate-to-effect orders
for pain medication because cur-
rent Joint Commission guidelines35
state that all medication orders must
include “the degree of accuracy,
completeness, and discrimination necessary for
their intended use.” Thus, physicians are required
to order specific dosages and frequencies of med-
ications, and a nurse who determines dosages and
parents can make decisions for continuation or with-
drawal of treatment. Robichaux and Clark24 wrote of
the need for nurses to protect and oftentimes be the
voice of the patient in order to prevent further tech-
nological intrusion. The real choice may not be
between life or death, but how the child will live
until death occurs.20 Nurses have acknowledged that
although mechanical ventilation is often associated
with the breath of life, use of this technology can
also extend suffering. In a study27 with critical care
nurses on end-of-life care, a participant stated, “We
[nurses] are trapped between technology and reality.”
Parents need reassurance that limiting life-
sustaining treatment does not mean limiting care.25
Ideally, parents should be educated that withdrawal
of aggressive therapies is not seen as surrendering
to death or abandoning hope. Parents should have
an understanding of what is best for the child and
what the child would want, if she or he could com-
municate, should curative efforts be unsuccessful.
Brandon et al28 found that children who died
in critical care areas were more likely to have experi-
enced withdrawal of respiratory or medical support
as end-of-life interventions, whereas children who
died in intermediate units were more likely to have a
do-not-resuscitate order, including no use of endo-
tracheal intubation or use of only drugs to resusci-
tate the child if he or she stopped breathing or the
heart stopped. These findings partly reflect the fact
that respiratory compromise requiring endotracheal
intubation is an intervention reserved for critical care
settings and that ICUs have unique and often chal-
lenging issues associated with ethical end-of-life care.
The finding that most children die in the ICU may
indicate that hospitalized children are receiving more
complex medical treatments than can be provided
on general pediatric units, and once therapy is initi-
ated, discontinuing it is often difficult.25,29
Discontinuity of Care Between Interdisciplinary Team
Members. Frustration occurs when providers do not
share the same perspectives and goals for a patient.
Having even a single physician unable to recognize
that a child is terminal can give the child’s family
false hope. Having medical subspecialists contradict
one another creates confusion for a patient’s family
and may result in digression when time is critical.
When a patient is not correctly recognized as termi-
nal, curative regimens take precedence and a child’s
unnecessary suffering may be prolonged.19
Many nurses in our study commented on the
need for early recognition of likely death rather
than waiting until a child starts to decompensate
dramatically before palliative care is initiated. Cur-
rent research30-32 supports a coexistent approach with
www.ajcconline.org AA JJCCCC AMERICAN JOURNAL OF CRITICAL CARE, November 2010, Volume 19, No. 6549
The supportive
behavior with the
greatest impact
was allowing fam-
ily members ade-
quate time with th
child after the
child has died.
Further research
is needed to
decrease highly
rated obstacles
and to continue
to support highly
rated supportive
behaviors.
by AACN on September 7, 2018http://ajcc.aacnjournals.org/Downloaded from
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

frequencies of medications may be practicing out-
side the nurse’s licensure.
Supportive Behaviors
PSBM scores for supportive behaviors were much
higher than POM scores were because the highest
scoring behaviors were usually under a nurse’s con-
trol and thus were perceived as very helpful. The 3
PSBM items with the highest scores are interrelated
and occur after a child’s death.
Top 3 Supportive Behaviors. Allowing family
members adequate time to be alone with a child
after the child has died was also the top supportive
behavior in other studies9,11,12of nurses’ perspectives
in end-of-life care. Adequate time alone indicates
respect for the parent-child relation-
ship, because the grieving process
should not be rushed. Nurses appar-
ently appreciate being able to offer
this time alone to children’s families.
The second highest rated sup-
portive behavior was allowing par-
ents to hold the child while life
support was discontinued, another
element within a nurse’s control.
Providing support to families around
the time of death may positively
affect long- term bereavement out-
comes for them for years. Holding
their child one last time would be a
valuable memory for parents and
may be important in the grieving process. This con-
trol of the environment at the time of death is also
related to the third highest rated supportive behav-
ior: providing a peaceful, dignified bedside scene
for family members once the child has died.
Physicians’ Involvement. Four other highly rated
supportive behaviors were associated with physicians’
actions. Having physicians provide a clear code status
and being clear about a child’s diagnosis were per-
ceived as very supportive behaviors in end-of-life care.
Physicians who agreed with a child’s prognosis and
who told the family that all possible care was done
for the child were also perceived as very supportive.
These highly ranked items indicate the need for a
collaborative, unified, interdisciplinary end-of-life team.
Andresen et al36 reported that physicians were more
likely to talk to a child’s family about decision making
at the end of life, whereas nurses were more likely
to be involved in talking about sibling, psychosocial,
and religious issues. A pooled, collective effort of all
health care team members, with consideration of their
opinions and abilities, is needed to help alleviate suf-
fering when a child dies.
Nurse Having Had Experience With the Death of a
Member of the Nurse’s Family. Although the item “nu
having had experience with the death of a member o
the nurse’s family” scored in the top 10 in other stud
ies of nurses’ perceptions of end-of-life care,9,11it was
the lowest scoring supportive behavior in our study.
Perhaps the death of a child differs greatly from the
death of an adult family member and presents a diffe
ent set of psychological and social issues. Other low
scoring supportive behaviors included bereavement
debriefing sessions to discuss how to remember/hono
the child and having a single family member as the
designated contact person for all other family mem-
bers regarding patient information.
Limitations
We did not distinguish between neonatal and
PICU nurses in this study; rather, we focused on
pediatric critical care nurses working in acute care.
Differences between ICU and non-ICU staff mem-
bers’ perceptions of end-of-life care were reported by
Davies et al.4 In that study, time constraints, staff
shortages, and parental discomfort about withhold-
ing/ withdrawing medical nutrition or hydration
were reported more frequently by non-ICU staff than
by ICU staff. Further research may be indicated to
differentiate neonatal nurses’ perceptions of barriers
and supportive behaviors from those of pediatric
nurses. Also, our sample consisted of nurses from
only a single specialty nursing organization, AACN.
How nurses from exclusively pediatric organizations
perceive end-of-life care is not known. Future researc
on these nurses’ perceptions is planned.
Implications
Pediatric nurses play a vital role in caring for
dying children and the children’s families. Parents
of children who died in the ICU have reported that
they relied more heavily on nursing professionals
than on the parents’ own family members when
making end-of-life decisions.37
Improving Communication
Overcoming communication barriers with the
family and within the interdisciplinary team can
positively affect end-of-life care. Better communica-
tion would help parents confront the difficult situa-
tions they face and would better prepare families
and support them through the dying process of their
child.34 The availability of round-the-clock translators
is critical for improving pediatric end-of-life care.
Further, if physicians were clearer in presenting infor
mation about treatment options and prognosis, par-
ents might be more proactive in planning the location
550 AA JJCCCC AMERICAN JOURNAL OF CRITICAL CARE, November 2010, Volume 19, No. 6 www.ajcconline.org
A collective effort
of all health care
team members,
with consideration
of their opinions
and abilities, is
needed to alleviate
suffering when a
child dies.
by AACN on September 7, 2018http://ajcc.aacnjournals.org/Downloaded from
side the nurse’s licensure.
Supportive Behaviors
PSBM scores for supportive behaviors were much
higher than POM scores were because the highest
scoring behaviors were usually under a nurse’s con-
trol and thus were perceived as very helpful. The 3
PSBM items with the highest scores are interrelated
and occur after a child’s death.
Top 3 Supportive Behaviors. Allowing family
members adequate time to be alone with a child
after the child has died was also the top supportive
behavior in other studies9,11,12of nurses’ perspectives
in end-of-life care. Adequate time alone indicates
respect for the parent-child relation-
ship, because the grieving process
should not be rushed. Nurses appar-
ently appreciate being able to offer
this time alone to children’s families.
The second highest rated sup-
portive behavior was allowing par-
ents to hold the child while life
support was discontinued, another
element within a nurse’s control.
Providing support to families around
the time of death may positively
affect long- term bereavement out-
comes for them for years. Holding
their child one last time would be a
valuable memory for parents and
may be important in the grieving process. This con-
trol of the environment at the time of death is also
related to the third highest rated supportive behav-
ior: providing a peaceful, dignified bedside scene
for family members once the child has died.
Physicians’ Involvement. Four other highly rated
supportive behaviors were associated with physicians’
actions. Having physicians provide a clear code status
and being clear about a child’s diagnosis were per-
ceived as very supportive behaviors in end-of-life care.
Physicians who agreed with a child’s prognosis and
who told the family that all possible care was done
for the child were also perceived as very supportive.
These highly ranked items indicate the need for a
collaborative, unified, interdisciplinary end-of-life team.
Andresen et al36 reported that physicians were more
likely to talk to a child’s family about decision making
at the end of life, whereas nurses were more likely
to be involved in talking about sibling, psychosocial,
and religious issues. A pooled, collective effort of all
health care team members, with consideration of their
opinions and abilities, is needed to help alleviate suf-
fering when a child dies.
Nurse Having Had Experience With the Death of a
Member of the Nurse’s Family. Although the item “nu
having had experience with the death of a member o
the nurse’s family” scored in the top 10 in other stud
ies of nurses’ perceptions of end-of-life care,9,11it was
the lowest scoring supportive behavior in our study.
Perhaps the death of a child differs greatly from the
death of an adult family member and presents a diffe
ent set of psychological and social issues. Other low
scoring supportive behaviors included bereavement
debriefing sessions to discuss how to remember/hono
the child and having a single family member as the
designated contact person for all other family mem-
bers regarding patient information.
Limitations
We did not distinguish between neonatal and
PICU nurses in this study; rather, we focused on
pediatric critical care nurses working in acute care.
Differences between ICU and non-ICU staff mem-
bers’ perceptions of end-of-life care were reported by
Davies et al.4 In that study, time constraints, staff
shortages, and parental discomfort about withhold-
ing/ withdrawing medical nutrition or hydration
were reported more frequently by non-ICU staff than
by ICU staff. Further research may be indicated to
differentiate neonatal nurses’ perceptions of barriers
and supportive behaviors from those of pediatric
nurses. Also, our sample consisted of nurses from
only a single specialty nursing organization, AACN.
How nurses from exclusively pediatric organizations
perceive end-of-life care is not known. Future researc
on these nurses’ perceptions is planned.
Implications
Pediatric nurses play a vital role in caring for
dying children and the children’s families. Parents
of children who died in the ICU have reported that
they relied more heavily on nursing professionals
than on the parents’ own family members when
making end-of-life decisions.37
Improving Communication
Overcoming communication barriers with the
family and within the interdisciplinary team can
positively affect end-of-life care. Better communica-
tion would help parents confront the difficult situa-
tions they face and would better prepare families
and support them through the dying process of their
child.34 The availability of round-the-clock translators
is critical for improving pediatric end-of-life care.
Further, if physicians were clearer in presenting infor
mation about treatment options and prognosis, par-
ents might be more proactive in planning the location
550 AA JJCCCC AMERICAN JOURNAL OF CRITICAL CARE, November 2010, Volume 19, No. 6 www.ajcconline.org
A collective effort
of all health care
team members,
with consideration
of their opinions
and abilities, is
needed to alleviate
suffering when a
child dies.
by AACN on September 7, 2018http://ajcc.aacnjournals.org/Downloaded from
setting, and any other area where a terminally ill
child feels comfortable.39,41
The American Academy of Pediatrics31 has
called for the writing of policies and clinical stan-
dards that support children who are living with ter-
minal conditions. The goal of care for these sick
children is providing equitable, effective help to
cure, prolong life, or provide palliative care.
Integrating palliative with curative care, begin-
ning at diagnosis, may be difficult in the treatment
of children. The success of medicine in improving
survival rates among certain children with serious
illnesses (eg, cancer, prematurity, congenital heart
disease) may have had the unintended consequence
of offering false hope to parents that death of their
child can always be averted.39 The uncertain progno-
sis of a seriously ill child makes it difficult to pre-
dict the progression of the child’s disease.30-32
Physicians may be reluctant to communicate to a
child’s family that the child is dying. Wolfe et al42
found that health care providers realized up to a
year before parents did that a child would die.
Although hospice personnel are better equipped
than hospital caregivers to handle issues associated
with end-of-life care, many hospice programs lack
staff with expertise in caring for children, depriving
children and children’s families of the benefits of
palliative care.31 In addition, the Medicare model of
hospice was designed for adults with cancer. There-
fore, the American Academy of Pediatrics called for
changes in the regulation of and reimbursement for
palliative care and hospice to improve access for chil-
dren and children’s families in need of these services.
Limited access also could be attributed to the
requirement of some hospice programs that patients
and patients’ families agree to forgo life-prolonging
or curative treatments in order to qualify for services
and meet the mandated life expectancy of 6 months
or less. Because of the difficulty in predicting length
of survival, this requirement is a significant barrier to
implementing palliative care and may contribute to
the less than 1% of all dying children in America
who receive palliative care or hospice in the home.43
Further Research
Further research is needed to identify and
implement ways to decrease highly rated obstacles
and to continue to support highly rated supportive
behaviors. Pediatric palliative care is still in its infancy.
Quality end-of-life care is still not being implemented
or being documented in most hospitals.28 We hope
that this study will promote further research and
discussion on this most important topic, which typ-
ifies the art of nursing.
of death, increasing the possibility of having fewer
deaths occur in the ICU and fewer intubations and
increasing the number of “good deaths” in the hos-
pital or at home with peaceful surroundings.38
Changing the Language
Attention to specific words used with the families
of dying children can have an impact on perceived
care. Terminology needs to be changed from words
such as withdrawing and withholding to allowing
death to naturally occur. Rushton20 emphasized that
telling patients’ families that nothing more can be
done undermines the ability to integrate palliative
care into practice. Being told that nothing can be
done conveys 2 unintended messages to patients and
patients’ families. First, being told nothing can be
done implies that compassionate actions aimed at
healing do not have the same value as aggressive
medical treatment does. Second, it suggests that the
health care professionals may abandon the patient
and the patient’s family if medical technologies and
therapies can no longer be used. By consciously not
using such statements in end-of-life discussions,
nurses can send a powerful message of commitment
and support to patients and patients’ families.
Interdisciplinary team members can establish a
mutual understanding of what ultimately is best for a
child. Prendergast and Puntillo25 noted that shifting
the perspective from giving up to letting go allows for
a more self-effacing, even altruistic interpretation of
care and acknowledges that care will be continued as
the child dies. The goal of this care should not be to
convert the family or patient to the health care profes-
sional’s view, but to work together in discovering what
will honor the family’s values, preferences, and goals.20
Integrating Palliative and End-of-Life Care
Dying children and their families require com-
prehensive, compassionate, and developmentally
appropriate palliative care.39 Palliative care is active
involvement, not passive withdrawal.20 Palliative
care is defined as health services with a focus on
relieving both the physical and the mental suffering
of terminally ill patients and the patients’ families.40
Palliative care is considered appropriate for ill chil-
dren with many different medical conditions, even
when cure for a child remains a distinct possibility.
The American Academy of Pediatrics reinforced this
concept of palliative care for critically ill children by
saying that many of the components of palliative
care could be offered at the beginning (diagnosis)
and continued for the child regardless of whether
the outcome is cure or death. Palliative care should
be accessible in the home, ICU or other hospital
www.ajcconline.org AA JJCCCC AMERICAN JOURNAL OF CRITICAL CARE, November 2010, Volume 19, No. 6551
by AACN on September 7, 2018http://ajcc.aacnjournals.org/Downloaded from
child feels comfortable.39,41
The American Academy of Pediatrics31 has
called for the writing of policies and clinical stan-
dards that support children who are living with ter-
minal conditions. The goal of care for these sick
children is providing equitable, effective help to
cure, prolong life, or provide palliative care.
Integrating palliative with curative care, begin-
ning at diagnosis, may be difficult in the treatment
of children. The success of medicine in improving
survival rates among certain children with serious
illnesses (eg, cancer, prematurity, congenital heart
disease) may have had the unintended consequence
of offering false hope to parents that death of their
child can always be averted.39 The uncertain progno-
sis of a seriously ill child makes it difficult to pre-
dict the progression of the child’s disease.30-32
Physicians may be reluctant to communicate to a
child’s family that the child is dying. Wolfe et al42
found that health care providers realized up to a
year before parents did that a child would die.
Although hospice personnel are better equipped
than hospital caregivers to handle issues associated
with end-of-life care, many hospice programs lack
staff with expertise in caring for children, depriving
children and children’s families of the benefits of
palliative care.31 In addition, the Medicare model of
hospice was designed for adults with cancer. There-
fore, the American Academy of Pediatrics called for
changes in the regulation of and reimbursement for
palliative care and hospice to improve access for chil-
dren and children’s families in need of these services.
Limited access also could be attributed to the
requirement of some hospice programs that patients
and patients’ families agree to forgo life-prolonging
or curative treatments in order to qualify for services
and meet the mandated life expectancy of 6 months
or less. Because of the difficulty in predicting length
of survival, this requirement is a significant barrier to
implementing palliative care and may contribute to
the less than 1% of all dying children in America
who receive palliative care or hospice in the home.43
Further Research
Further research is needed to identify and
implement ways to decrease highly rated obstacles
and to continue to support highly rated supportive
behaviors. Pediatric palliative care is still in its infancy.
Quality end-of-life care is still not being implemented
or being documented in most hospitals.28 We hope
that this study will promote further research and
discussion on this most important topic, which typ-
ifies the art of nursing.
of death, increasing the possibility of having fewer
deaths occur in the ICU and fewer intubations and
increasing the number of “good deaths” in the hos-
pital or at home with peaceful surroundings.38
Changing the Language
Attention to specific words used with the families
of dying children can have an impact on perceived
care. Terminology needs to be changed from words
such as withdrawing and withholding to allowing
death to naturally occur. Rushton20 emphasized that
telling patients’ families that nothing more can be
done undermines the ability to integrate palliative
care into practice. Being told that nothing can be
done conveys 2 unintended messages to patients and
patients’ families. First, being told nothing can be
done implies that compassionate actions aimed at
healing do not have the same value as aggressive
medical treatment does. Second, it suggests that the
health care professionals may abandon the patient
and the patient’s family if medical technologies and
therapies can no longer be used. By consciously not
using such statements in end-of-life discussions,
nurses can send a powerful message of commitment
and support to patients and patients’ families.
Interdisciplinary team members can establish a
mutual understanding of what ultimately is best for a
child. Prendergast and Puntillo25 noted that shifting
the perspective from giving up to letting go allows for
a more self-effacing, even altruistic interpretation of
care and acknowledges that care will be continued as
the child dies. The goal of this care should not be to
convert the family or patient to the health care profes-
sional’s view, but to work together in discovering what
will honor the family’s values, preferences, and goals.20
Integrating Palliative and End-of-Life Care
Dying children and their families require com-
prehensive, compassionate, and developmentally
appropriate palliative care.39 Palliative care is active
involvement, not passive withdrawal.20 Palliative
care is defined as health services with a focus on
relieving both the physical and the mental suffering
of terminally ill patients and the patients’ families.40
Palliative care is considered appropriate for ill chil-
dren with many different medical conditions, even
when cure for a child remains a distinct possibility.
The American Academy of Pediatrics reinforced this
concept of palliative care for critically ill children by
saying that many of the components of palliative
care could be offered at the beginning (diagnosis)
and continued for the child regardless of whether
the outcome is cure or death. Palliative care should
be accessible in the home, ICU or other hospital
www.ajcconline.org AA JJCCCC AMERICAN JOURNAL OF CRITICAL CARE, November 2010, Volume 19, No. 6551
by AACN on September 7, 2018http://ajcc.aacnjournals.org/Downloaded from
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

FINANCIAL DISCLOSURES
This study was funded, in part, by the College of Nurs-
ing, Brigham Young University, and by a graduate men-
toring grant from Brigham Young University Graduate
Studies Office.
REFERENCES
1. About children’s hospice, palliative and end-of-life care. Chil-
drens Hospice International Web site: http://www.chionline
.org/resources/about.php. Accessed November 17, 2009.
2. IPPC’s focus. Initiative for Pediatric Palliative Care Web site.
http://www.ippcweb.org/about.asp. Accessed November
25, 2009.
3. Field MJ, Behrman RE, eds. When Children Die: Improving
Palliative and End-of-Life Care for Children and Their Fami-
lies. Washington, DC: National Academy Press; 2003.
4. Davies B, Sehring SA, Partridge JC, et al. Barriers to pallia-
tive care for children: perceptions of pediatric health care
providers. Pediatrics. 2008;121(2):282-288.
5. Contro NA, Larson J, Scofield S, Sourkes B, Cohen HJ.
Hospital staff and family perspectives regarding quality of
pediatric palliative care. Pediatrics. 2004;114(5):1248-1252.
6. Lee KJ, Dupree CY. Staff experiences with end-of-life care in
the pediatric intensive care unit. J Palliat Med. 2008;11(7):
986-990.
7. Burns JP, Mitchell C, Griffith JL, Truog RD. End-of-life care
in the pediatric intensive care unit: attitudes and practices
of pediatric critical care physicians and nurses. Crit Care
Med. 2001;29(3):658-664.
8. Rushton CH, Reder E, Hall B, Comello K, Sellers DE, Hutton
N. Interdisciplinary interventions to improve pediatric pal-
liative care and reduce health care professional suffering.
J Palliat Med. 2006;9(4):922-933.
9. Beckstrand RL, Kirchhoff KT. Providing end-of-life care to
patients: critical nurses’ perceived obstacles and support-
ive behaviors. Am J Crit Care. 2005;14(5):395-403.
10. Solomon MZ, Sellers DE, Heller KS, et al. New and linger-
ing controversies in pediatric end-of-life care. Pediatrics.
2005;116(4):872-883.
11. Beckstrand RL, Smith MD, Heaston S, Bond AE. Emergency
nurses’ perceptions of size, frequency, and magnitude of
obstacles and supportive behaviors in end-of-life care. J
Emerg Nurs. 2008;34(4):290-300.
12. Beckstrand RL, Moore JF, Callister LC, Bond AE. Oncology
nurses’ perceptions of obstacles and supportive behaviors
at the end of life. Oncol Nurs Forum. 2009;36(4):446-453.
13. Kirchhoff KT. Design of questionnaires and structured inter-
views. In: Matea MA, Kirchhoff KT, eds. Using and Con-
ducting Nursing Research in the Clinical Setting. 2nd ed.
Philadelphia, PA: WB Saunders Co; 1999:229-239.
14. Sawatzky JA. Stress in critical care nurses: actual and per-
ceived. Heart Lung. 1996;25(5):409-417.
15. Ferrell B, Virani R, Grant M, Coyne P, Uman G. Beyond the
Supreme Court decision: nursing perspectives on end-of-life
care. Oncol Nurs Forum. 2000;27(3):445-455.
16. Contro N, Larson J, Scofield S, Sourkes B, Cohen H. Family
perspectives on the quality of pediatric palliative care. Arch
Pediatr Adolesc Med. 2002;156(1):14-19.
17. Engler AJ, Cusson RM, Brockett RT, et al. Neonatal staff and
advanced practice nurses’ perceptions of bereavement/end-
of-life care of families of critically ill and/or dying infants.
Am J Crit Care. 2004;13(6):489-498.
18. Terhune CP. “Can we talk?” Using critical self-reflection and
dialogue to build diversity and change organizational culture
in nursing schools. J Cult Divers. 2006;13(3):141-145.
19. Curtis JR, Patrick DL. How to discuss dying and death in
the ICU. In: Curtis JR, Rubenfeld GD, eds. Managing Death
in the ICU: The Transition From Cure to Comfort. New York,
NY: Oxford University Press; 2001:85-102.
20. Rushton CH. A framework for integrated pediatric palliative
care: being with dying. J Pediatr Nurs. 2005;20(5):311-325.
21. Davies B, Connaughty S. Pediatric end-of-life care: lessons
learned from parents. J Nurs Adm. 2002;32(1):5-6.
22. Mack JW, Hilden JM, Watterson J, et al. Parent and physician
perspectives on quality of care at the end of life in children
with cancer. J Clin Oncol. 2005;23(36):9155-9161.
23. Kaufman SR. Intensive care, old age, and the problem of
death in America. Gerontologist. 1998;38:715-725.
24. Robichaux CM, Clark AP. Practice of expert critical care nurses
in situations of prognostic conflict at the end of life. Am J
Crit Care. 2006;15(5):480-491.
25. Prendergast TJ, Puntillo KA. Withdrawal of life support: inten-
sive caring at the end of life. JAMA. 2002;288(21):2732-2740.
26. Solomon MZ, O’Donnell L, Jennings B, et al. Decisions near
the end of life: professional views on life-sustaining treat-
ments. Am J Public Health. 1993;83(1):14-23.
27. Beckstrand RL, Calllister LC, Kirchhoff KT. Providing a “good
death”: critical care nurses’ suggestions for improving
end-of-life care. Am J Crit Care. 2006;15:38-45.
28. Brandon D, Docherty SL, Thorpe J. Infant and child deaths in
acute care settings: implications for palliative care. J Palliat
Med. 2007;10(4):910-918.
29. Wiegand DM. Withdrawal of life-sustaining therapy after sud-
den, unexpected, life-threatening illness or injury: interac-
tions between patients’ families, healthcare providers, and the
healthcare system. Am J Crit Care. 2006;15:178-187.
30. Vats TS, Reynolds PD. Pediatric hospital dying trajectories: what
we learned and can share. Pediatr Nurs. 2006;32(4):386-392.
31. American Academy of Pediatrics, Committee on Bioethics
and Committee on Hospital Care. Palliative care for children.
Pediatrics. 2000;106(2, pt 1):351-357.
32. Sahler OJ, Frager G, Levetown M, Cohn FG, Lipson MA. Med-
ical education about end-of-life care in the pediatric setting:
principles, challenges, and opportunities. Pediatrics. 2000;
105(3, pt 1):575-584.
33. Miller PA, Forbes S, Boyle DK. End-of-life care in the intensive
care unit: a challenge for nurses. Am J Crit Care. 2001;10(4):
230-237.
34. Feudtner C, Santucci G, Feinstein JA, Snyder CR, Rourke MT,
Kang TI. Hopeful thinking and level of comfort regarding pro-
viding pediatric palliative care: a survey of hospital nurses.
Pediatrics. 2007;119(1):e186-e192.
35. Sentinel event alert: medication errors related to potentially
dangerous abbreviations. Joint Commission Web site. http://
www.jointcommission.org/SentinelEvents/SentinelEventAlert
/sea_23.htm. Issue 23. Published September 1, 2001. Accessed
November 19, 2009.
36. Andresen EM, Seecharan GA, Toce SS. Provider perceptions of
child deaths. Arch Pediatr Adolesc Med. 2004;158(5):430-435.
37. Meyer E, Burns JP, Griffith JL, Truog RD. Parental perspec-
tives on end-of-life care in the pediatric intensive care unit.
Crit Care Med. 2002;30(1):226-231.
38. Dussel V, Kreicbergs U, Hilden JM, et al. Looking beyond where
children die: determinants and effects of planning a child’s loca-
tion of death. J Pain Symptom Manage. 2009;37(1):33-43.
39. Himelstein BP, Hilden JM, Boldt AM, Weissman D. Pediatric
palliative care. N Engl J Med. 2004;350(17):1753-1762.
40. Definition of palliative. Dictionary.com Web site. http://
dictionary.reference.com/browse/palliative. Accessed Novem-
ber 19, 2009.
41. Rollins JA. New initiatives in end-of-life care. Pediatr Nurs.
2002;28(3):292-293.
42. Wolfe J, Klar N, Grier HE, et al. Understanding of prognosis
among parents of children who died of cancer: impact on
treatment goals and integration of palliative care. JAMA.
2000;284(19):2469-2475.
43. Kane J, Barber R, Jordan M, Tichenor KT, Camp K. Supportive/
palliative care of children suffering from life-threatening and
terminal illness. Am J Hosp Palliat Care. 2000;17(3):165-172.
eLetters
Now that you’ve read the article, create or contribute to an
online discussion on this topic. Visit www.ajcconline.org
and click “Respond to This Article” in either the full-text or
PDF view of the article.
To purchase electronic or print reprints, contact The
InnoVision Group, 101 Columbia, Aliso Viejo, CA 92656.
Phone, (800) 899-1712 or (949) 362-2050 (ext 532); fax,
(949) 362-2049; e-mail, reprints@aacn.org.
552 AA JJCCCC AMERICAN JOURNAL OF CRITICAL CARE, November 2010, Volume 19, No. 6 www.ajcconline.org
by AACN on September 7, 2018http://ajcc.aacnjournals.org/Downloaded from
This study was funded, in part, by the College of Nurs-
ing, Brigham Young University, and by a graduate men-
toring grant from Brigham Young University Graduate
Studies Office.
REFERENCES
1. About children’s hospice, palliative and end-of-life care. Chil-
drens Hospice International Web site: http://www.chionline
.org/resources/about.php. Accessed November 17, 2009.
2. IPPC’s focus. Initiative for Pediatric Palliative Care Web site.
http://www.ippcweb.org/about.asp. Accessed November
25, 2009.
3. Field MJ, Behrman RE, eds. When Children Die: Improving
Palliative and End-of-Life Care for Children and Their Fami-
lies. Washington, DC: National Academy Press; 2003.
4. Davies B, Sehring SA, Partridge JC, et al. Barriers to pallia-
tive care for children: perceptions of pediatric health care
providers. Pediatrics. 2008;121(2):282-288.
5. Contro NA, Larson J, Scofield S, Sourkes B, Cohen HJ.
Hospital staff and family perspectives regarding quality of
pediatric palliative care. Pediatrics. 2004;114(5):1248-1252.
6. Lee KJ, Dupree CY. Staff experiences with end-of-life care in
the pediatric intensive care unit. J Palliat Med. 2008;11(7):
986-990.
7. Burns JP, Mitchell C, Griffith JL, Truog RD. End-of-life care
in the pediatric intensive care unit: attitudes and practices
of pediatric critical care physicians and nurses. Crit Care
Med. 2001;29(3):658-664.
8. Rushton CH, Reder E, Hall B, Comello K, Sellers DE, Hutton
N. Interdisciplinary interventions to improve pediatric pal-
liative care and reduce health care professional suffering.
J Palliat Med. 2006;9(4):922-933.
9. Beckstrand RL, Kirchhoff KT. Providing end-of-life care to
patients: critical nurses’ perceived obstacles and support-
ive behaviors. Am J Crit Care. 2005;14(5):395-403.
10. Solomon MZ, Sellers DE, Heller KS, et al. New and linger-
ing controversies in pediatric end-of-life care. Pediatrics.
2005;116(4):872-883.
11. Beckstrand RL, Smith MD, Heaston S, Bond AE. Emergency
nurses’ perceptions of size, frequency, and magnitude of
obstacles and supportive behaviors in end-of-life care. J
Emerg Nurs. 2008;34(4):290-300.
12. Beckstrand RL, Moore JF, Callister LC, Bond AE. Oncology
nurses’ perceptions of obstacles and supportive behaviors
at the end of life. Oncol Nurs Forum. 2009;36(4):446-453.
13. Kirchhoff KT. Design of questionnaires and structured inter-
views. In: Matea MA, Kirchhoff KT, eds. Using and Con-
ducting Nursing Research in the Clinical Setting. 2nd ed.
Philadelphia, PA: WB Saunders Co; 1999:229-239.
14. Sawatzky JA. Stress in critical care nurses: actual and per-
ceived. Heart Lung. 1996;25(5):409-417.
15. Ferrell B, Virani R, Grant M, Coyne P, Uman G. Beyond the
Supreme Court decision: nursing perspectives on end-of-life
care. Oncol Nurs Forum. 2000;27(3):445-455.
16. Contro N, Larson J, Scofield S, Sourkes B, Cohen H. Family
perspectives on the quality of pediatric palliative care. Arch
Pediatr Adolesc Med. 2002;156(1):14-19.
17. Engler AJ, Cusson RM, Brockett RT, et al. Neonatal staff and
advanced practice nurses’ perceptions of bereavement/end-
of-life care of families of critically ill and/or dying infants.
Am J Crit Care. 2004;13(6):489-498.
18. Terhune CP. “Can we talk?” Using critical self-reflection and
dialogue to build diversity and change organizational culture
in nursing schools. J Cult Divers. 2006;13(3):141-145.
19. Curtis JR, Patrick DL. How to discuss dying and death in
the ICU. In: Curtis JR, Rubenfeld GD, eds. Managing Death
in the ICU: The Transition From Cure to Comfort. New York,
NY: Oxford University Press; 2001:85-102.
20. Rushton CH. A framework for integrated pediatric palliative
care: being with dying. J Pediatr Nurs. 2005;20(5):311-325.
21. Davies B, Connaughty S. Pediatric end-of-life care: lessons
learned from parents. J Nurs Adm. 2002;32(1):5-6.
22. Mack JW, Hilden JM, Watterson J, et al. Parent and physician
perspectives on quality of care at the end of life in children
with cancer. J Clin Oncol. 2005;23(36):9155-9161.
23. Kaufman SR. Intensive care, old age, and the problem of
death in America. Gerontologist. 1998;38:715-725.
24. Robichaux CM, Clark AP. Practice of expert critical care nurses
in situations of prognostic conflict at the end of life. Am J
Crit Care. 2006;15(5):480-491.
25. Prendergast TJ, Puntillo KA. Withdrawal of life support: inten-
sive caring at the end of life. JAMA. 2002;288(21):2732-2740.
26. Solomon MZ, O’Donnell L, Jennings B, et al. Decisions near
the end of life: professional views on life-sustaining treat-
ments. Am J Public Health. 1993;83(1):14-23.
27. Beckstrand RL, Calllister LC, Kirchhoff KT. Providing a “good
death”: critical care nurses’ suggestions for improving
end-of-life care. Am J Crit Care. 2006;15:38-45.
28. Brandon D, Docherty SL, Thorpe J. Infant and child deaths in
acute care settings: implications for palliative care. J Palliat
Med. 2007;10(4):910-918.
29. Wiegand DM. Withdrawal of life-sustaining therapy after sud-
den, unexpected, life-threatening illness or injury: interac-
tions between patients’ families, healthcare providers, and the
healthcare system. Am J Crit Care. 2006;15:178-187.
30. Vats TS, Reynolds PD. Pediatric hospital dying trajectories: what
we learned and can share. Pediatr Nurs. 2006;32(4):386-392.
31. American Academy of Pediatrics, Committee on Bioethics
and Committee on Hospital Care. Palliative care for children.
Pediatrics. 2000;106(2, pt 1):351-357.
32. Sahler OJ, Frager G, Levetown M, Cohn FG, Lipson MA. Med-
ical education about end-of-life care in the pediatric setting:
principles, challenges, and opportunities. Pediatrics. 2000;
105(3, pt 1):575-584.
33. Miller PA, Forbes S, Boyle DK. End-of-life care in the intensive
care unit: a challenge for nurses. Am J Crit Care. 2001;10(4):
230-237.
34. Feudtner C, Santucci G, Feinstein JA, Snyder CR, Rourke MT,
Kang TI. Hopeful thinking and level of comfort regarding pro-
viding pediatric palliative care: a survey of hospital nurses.
Pediatrics. 2007;119(1):e186-e192.
35. Sentinel event alert: medication errors related to potentially
dangerous abbreviations. Joint Commission Web site. http://
www.jointcommission.org/SentinelEvents/SentinelEventAlert
/sea_23.htm. Issue 23. Published September 1, 2001. Accessed
November 19, 2009.
36. Andresen EM, Seecharan GA, Toce SS. Provider perceptions of
child deaths. Arch Pediatr Adolesc Med. 2004;158(5):430-435.
37. Meyer E, Burns JP, Griffith JL, Truog RD. Parental perspec-
tives on end-of-life care in the pediatric intensive care unit.
Crit Care Med. 2002;30(1):226-231.
38. Dussel V, Kreicbergs U, Hilden JM, et al. Looking beyond where
children die: determinants and effects of planning a child’s loca-
tion of death. J Pain Symptom Manage. 2009;37(1):33-43.
39. Himelstein BP, Hilden JM, Boldt AM, Weissman D. Pediatric
palliative care. N Engl J Med. 2004;350(17):1753-1762.
40. Definition of palliative. Dictionary.com Web site. http://
dictionary.reference.com/browse/palliative. Accessed Novem-
ber 19, 2009.
41. Rollins JA. New initiatives in end-of-life care. Pediatr Nurs.
2002;28(3):292-293.
42. Wolfe J, Klar N, Grier HE, et al. Understanding of prognosis
among parents of children who died of cancer: impact on
treatment goals and integration of palliative care. JAMA.
2000;284(19):2469-2475.
43. Kane J, Barber R, Jordan M, Tichenor KT, Camp K. Supportive/
palliative care of children suffering from life-threatening and
terminal illness. Am J Hosp Palliat Care. 2000;17(3):165-172.
eLetters
Now that you’ve read the article, create or contribute to an
online discussion on this topic. Visit www.ajcconline.org
and click “Respond to This Article” in either the full-text or
PDF view of the article.
To purchase electronic or print reprints, contact The
InnoVision Group, 101 Columbia, Aliso Viejo, CA 92656.
Phone, (800) 899-1712 or (949) 362-2050 (ext 532); fax,
(949) 362-2049; e-mail, reprints@aacn.org.
552 AA JJCCCC AMERICAN JOURNAL OF CRITICAL CARE, November 2010, Volume 19, No. 6 www.ajcconline.org
by AACN on September 7, 2018http://ajcc.aacnjournals.org/Downloaded from
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Renea L. Beckstrand, Nicole L. Rawle, Lynn Callister and Barbara L. Mandleco
Pediatric Nurses' Perceptions of Obstacles and Supportive Behaviors in End-of-Life Care
http://ajcc.aacnjournals.org/Published online
©2010 American Association of Critical-Care Nurses
10.4037/ajcc2009497543-552192010;Am J Crit Care
http://ajcc.aacnjournals.org/cgi/external_ref?link_type=PERMISSIONDIRECT
Personal use only. For copyright permission information:
http://ajcc.aacnjournals.org/subscriptions/
Subscription Information
http://ajcc.aacnjournals.org/misc/ifora.xhtml
Information for authors
http://www.editorialmanager.com/ajcc
Submit a manuscript
http://ajcc.aacnjournals.org/subscriptions/etoc.xhtml
Email alerts
.532. Fax: (949) 362-2049. Copyright ©2016 by AACN. All rights reserved
(AACN) published bimonthly by AACN, 101 Columbia, Aliso Viejo, CA 92656. Telephone: (800) 899-1712, (949) 362-2050, ext.
The American Journal of Critical Care is an official peer-reviewed journal of the American Association of Critical-Care Nurses
by AACN on September 7, 2018http://ajcc.aacnjournals.org/Downloaded from
Pediatric Nurses' Perceptions of Obstacles and Supportive Behaviors in End-of-Life Care
http://ajcc.aacnjournals.org/Published online
©2010 American Association of Critical-Care Nurses
10.4037/ajcc2009497543-552192010;Am J Crit Care
http://ajcc.aacnjournals.org/cgi/external_ref?link_type=PERMISSIONDIRECT
Personal use only. For copyright permission information:
http://ajcc.aacnjournals.org/subscriptions/
Subscription Information
http://ajcc.aacnjournals.org/misc/ifora.xhtml
Information for authors
http://www.editorialmanager.com/ajcc
Submit a manuscript
http://ajcc.aacnjournals.org/subscriptions/etoc.xhtml
Email alerts
.532. Fax: (949) 362-2049. Copyright ©2016 by AACN. All rights reserved
(AACN) published bimonthly by AACN, 101 Columbia, Aliso Viejo, CA 92656. Telephone: (800) 899-1712, (949) 362-2050, ext.
The American Journal of Critical Care is an official peer-reviewed journal of the American Association of Critical-Care Nurses
by AACN on September 7, 2018http://ajcc.aacnjournals.org/Downloaded from
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.



