Utilizing LUCAS-2 Device in Percutaneous Noncoronary Interventions
VerifiedAdded on 2023/06/15
|4
|1909
|361
Case Study
AI Summary
This case study examines the application of the LUCAS-2 mechanical chest compression device during percutaneous noncoronary interventions in two patients who experienced cardiac arrest. The first patient, an 84-year-old man with a massive pulmonary embolism, underwent pulmonary thrombectomy with the aid of the LUCAS-2 device after experiencing multiple episodes of pulseless electrical activity. The device facilitated the fragmentation of pulmonary thrombi and local thrombolysis, leading to improved pulmonary and systemic perfusion, although the patient later died due to multi-organ failure. The second patient, a 75-year-old male with severe aortic stenosis, underwent a rescue PCI and subsequent aortic balloon valvuloplasty, both performed under mechanical resuscitation with the LUCAS-2, after developing pulseless electrical activity during the PCI. Despite successful interventions, the patient did not survive. The study suggests that the LUCAS-2 device can effectively support CPR during a range of noncoronary procedures, especially in situations where manual chest compressions are challenging. The device's radiotranslucency allows for fluoroscopic-guided interventions without interrupting chest compression, potentially improving patient outcomes during critical procedures.
See discussions, stats, and author profiles for this publication at: https://www.researchga
The LUCAS 2 Chest Compression Device Is Not
AlwaysEfficient: An Echographic Confirmation
Article in Annals of emergency medicine · February 2014
DOI: 10.1016/j.annemergmed.2014.01.020 · Source: PubMed
CITATIONS
6
READS
456
7 authors, including:
Some of the authors of this publication are also working on these
Biodegradable material in cardiac surgeryView project
ShockOmicsView project
Raphael Giraud
Hôpitaux Universitaires de Genève
62PUBLICATIONS219CITATIONS
SEE PROFILE
Nils Siegenthaler
Hôpitaux Universitaires de Genève
58PUBLICATIONS351CITATIONS
SEE PROFILE
Olivier Schussler
University of Geneva
39PUBLICATIONS1,051CITATIONS
SEE PROFILE
Afksendiyos Kalangos
MITERA HOSPITAL
341PUBLICATIONS3,734CITATIONS
SEE PROFILE
All content following this page was uploaded by Karim Bendjelid on
The user has requested enhancement of the downloaded file.
The LUCAS 2 Chest Compression Device Is Not
AlwaysEfficient: An Echographic Confirmation
Article in Annals of emergency medicine · February 2014
DOI: 10.1016/j.annemergmed.2014.01.020 · Source: PubMed
CITATIONS
6
READS
456
7 authors, including:
Some of the authors of this publication are also working on these
Biodegradable material in cardiac surgeryView project
ShockOmicsView project
Raphael Giraud
Hôpitaux Universitaires de Genève
62PUBLICATIONS219CITATIONS
SEE PROFILE
Nils Siegenthaler
Hôpitaux Universitaires de Genève
58PUBLICATIONS351CITATIONS
SEE PROFILE
Olivier Schussler
University of Geneva
39PUBLICATIONS1,051CITATIONS
SEE PROFILE
Afksendiyos Kalangos
MITERA HOSPITAL
341PUBLICATIONS3,734CITATIONS
SEE PROFILE
All content following this page was uploaded by Karim Bendjelid on
The user has requested enhancement of the downloaded file.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Case Report
Percutaneous noncoronary interventions during
continuous mechanical chest compression with the
LUCAS-2 device☆
Abstract
Cardiac arrestin the catheterization laboratory during
percutaneous coronary interventions (PCI) is associated with
high mortality,among otherthingsbecauseit may be
difficultto perform efficacious cardiopulmonary resuscita-
tion while continuing the coronary intervention.We report
on 2 patientswho havebenefitfrom ongoing external
mechanicalchestcompressionwith LUCAS-2 device
becauseof cardiacarrestoccurred during non-coronary
interventions. Added to the existing data on PCIs performed
during cardiac arrest,these first reported cases suggest that
the application ofthe LUCAS-2 devicein the cardiac
catheterization laboratory may be also expanded to patients
undergoing noncoronary interventions.
Percutaneous coronary interventions during cardiac arrest
may be attempted even ifperforming adequate coronary
revascularisation under this reanimation condition may result
very challenging.A novel mechanicalchestcompression
device,LUCAS-2 (Lund UniversityCardiopulmonary
Assistance System;Lund,Sweden)[1] delivers automatic
chest compression and active decompression. Although few
reports on the application ofthis device during PCIhave
been published [2],here the authors describe their prelim-
inary experience with 2 patients who have benefit from this
device during non-coronary interventions.
Patient 1: an 84-year-old man was found unconscious in
his hospitalroom with pulseless electricalactivity one day
after elective hip surgery. After several minutes of standard
cardiopulmonary resuscitation (CPR),the patientregained
circulationbut remaineddependenton high dose of
catecholamines.Emergenttransthoracic echocardiography
confirmed the clinical suspicion of a massive PE. Thereafter,
two additionalepisodesof pulselesselectricalactivity
necessitating shortperiods of CPR and an increasing dose
of vasopressors occurred. Because of the absolute contrain-
dication forsystemic thrombolysis (ie,day 1 aftermajor
orthopedic surgery), it was decided to attempt a percutan
mechanical pulmonary thrombectomy.
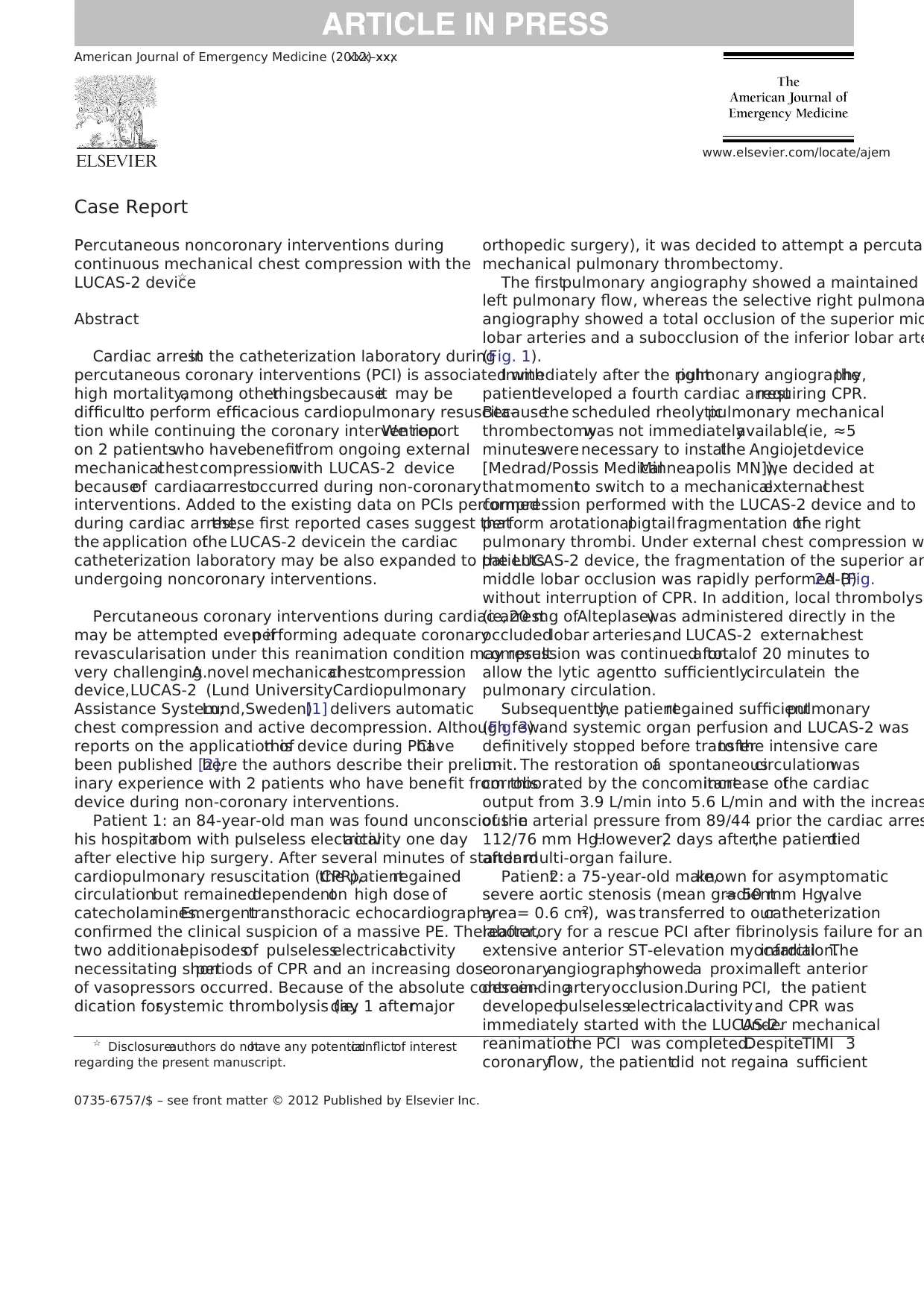
The firstpulmonary angiography showed a maintained
left pulmonary flow, whereas the selective right pulmona
angiography showed a total occlusion of the superior mid
lobar arteries and a subocclusion of the inferior lobar arte
(Fig. 1).
Immediately after the rightpulmonary angiography,the
patientdeveloped a fourth cardiac arrestrequiring CPR.
Becausethe scheduled rheolyticpulmonary mechanical
thrombectomywas not immediatelyavailable(ie, ≈5
minuteswere necessary to installthe Angiojetdevice
[Medrad/Possis MedicalMinneapolis MN]),we decided at
thatmomentto switch to a mechanicalexternalchest
compression performed with the LUCAS-2 device and to
perform arotationalpigtailfragmentation ofthe right
pulmonary thrombi. Under external chest compression w
the LUCAS-2 device, the fragmentation of the superior an
middle lobar occlusion was rapidly performed (Fig.2A-B)
without interruption of CPR. In addition, local thrombolysi
(ie, 20 mg ofAlteplase)was administered directly in the
occludedlobar arteries,and LUCAS-2 externalchest
compression was continued fora totalof 20 minutes to
allow the lytic agentto sufficientlycirculatein the
pulmonary circulation.
Subsequently,the patientregained sufficientpulmonary
(Fig. 3) and systemic organ perfusion and LUCAS-2 was
definitively stopped before transferto the intensive care
unit. The restoration ofa spontaneouscirculationwas
corroborated by the concomitantincrease ofthe cardiac
output from 3.9 L/min into 5.6 L/min and with the increas
of the arterial pressure from 89/44 prior the cardiac arres
112/76 mm Hg.However,2 days after,the patientdied
after multi-organ failure.
Patient2: a 75-year-old male,known for asymptomatic
severe aortic stenosis (mean gradient= 50 mm Hg,valve
area= 0.6 cm2), was transferred to ourcatheterization
laboratory for a rescue PCI after fibrinolysis failure for an
extensive anterior ST-elevation myocardialinfarction.The
coronaryangiographyshoweda proximalleft anterior
descendingarteryocclusion.During PCI, the patient
developedpulselesselectricalactivityand CPR was
immediately started with the LUCAS-2.Under mechanical
reanimationthe PCI was completed.DespiteTIMI 3
coronaryflow, the patientdid not regaina sufficient
☆ Disclosure:authors do nothave any potentialconflictof interest
regarding the present manuscript.
www.elsevier.com/locate/ajem
0735-6757/$ – see front matter © 2012 Published by Elsevier Inc.
American Journal of Emergency Medicine (2012) xx,xxx–xxx
Percutaneous noncoronary interventions during
continuous mechanical chest compression with the
LUCAS-2 device☆
Abstract
Cardiac arrestin the catheterization laboratory during
percutaneous coronary interventions (PCI) is associated with
high mortality,among otherthingsbecauseit may be
difficultto perform efficacious cardiopulmonary resuscita-
tion while continuing the coronary intervention.We report
on 2 patientswho havebenefitfrom ongoing external
mechanicalchestcompressionwith LUCAS-2 device
becauseof cardiacarrestoccurred during non-coronary
interventions. Added to the existing data on PCIs performed
during cardiac arrest,these first reported cases suggest that
the application ofthe LUCAS-2 devicein the cardiac
catheterization laboratory may be also expanded to patients
undergoing noncoronary interventions.
Percutaneous coronary interventions during cardiac arrest
may be attempted even ifperforming adequate coronary
revascularisation under this reanimation condition may result
very challenging.A novel mechanicalchestcompression
device,LUCAS-2 (Lund UniversityCardiopulmonary
Assistance System;Lund,Sweden)[1] delivers automatic
chest compression and active decompression. Although few
reports on the application ofthis device during PCIhave
been published [2],here the authors describe their prelim-
inary experience with 2 patients who have benefit from this
device during non-coronary interventions.
Patient 1: an 84-year-old man was found unconscious in
his hospitalroom with pulseless electricalactivity one day
after elective hip surgery. After several minutes of standard
cardiopulmonary resuscitation (CPR),the patientregained
circulationbut remaineddependenton high dose of
catecholamines.Emergenttransthoracic echocardiography
confirmed the clinical suspicion of a massive PE. Thereafter,
two additionalepisodesof pulselesselectricalactivity
necessitating shortperiods of CPR and an increasing dose
of vasopressors occurred. Because of the absolute contrain-
dication forsystemic thrombolysis (ie,day 1 aftermajor
orthopedic surgery), it was decided to attempt a percutan
mechanical pulmonary thrombectomy.
The firstpulmonary angiography showed a maintained
left pulmonary flow, whereas the selective right pulmona
angiography showed a total occlusion of the superior mid
lobar arteries and a subocclusion of the inferior lobar arte
(Fig. 1).
Immediately after the rightpulmonary angiography,the
patientdeveloped a fourth cardiac arrestrequiring CPR.
Becausethe scheduled rheolyticpulmonary mechanical
thrombectomywas not immediatelyavailable(ie, ≈5
minuteswere necessary to installthe Angiojetdevice
[Medrad/Possis MedicalMinneapolis MN]),we decided at
thatmomentto switch to a mechanicalexternalchest
compression performed with the LUCAS-2 device and to
perform arotationalpigtailfragmentation ofthe right
pulmonary thrombi. Under external chest compression w
the LUCAS-2 device, the fragmentation of the superior an
middle lobar occlusion was rapidly performed (Fig.2A-B)
without interruption of CPR. In addition, local thrombolysi
(ie, 20 mg ofAlteplase)was administered directly in the
occludedlobar arteries,and LUCAS-2 externalchest
compression was continued fora totalof 20 minutes to
allow the lytic agentto sufficientlycirculatein the
pulmonary circulation.
Subsequently,the patientregained sufficientpulmonary
(Fig. 3) and systemic organ perfusion and LUCAS-2 was
definitively stopped before transferto the intensive care
unit. The restoration ofa spontaneouscirculationwas
corroborated by the concomitantincrease ofthe cardiac
output from 3.9 L/min into 5.6 L/min and with the increas
of the arterial pressure from 89/44 prior the cardiac arres
112/76 mm Hg.However,2 days after,the patientdied
after multi-organ failure.
Patient2: a 75-year-old male,known for asymptomatic
severe aortic stenosis (mean gradient= 50 mm Hg,valve
area= 0.6 cm2), was transferred to ourcatheterization
laboratory for a rescue PCI after fibrinolysis failure for an
extensive anterior ST-elevation myocardialinfarction.The
coronaryangiographyshoweda proximalleft anterior
descendingarteryocclusion.During PCI, the patient
developedpulselesselectricalactivityand CPR was
immediately started with the LUCAS-2.Under mechanical
reanimationthe PCI was completed.DespiteTIMI 3
coronaryflow, the patientdid not regaina sufficient
☆ Disclosure:authors do nothave any potentialconflictof interest
regarding the present manuscript.
www.elsevier.com/locate/ajem
0735-6757/$ – see front matter © 2012 Published by Elsevier Inc.
American Journal of Emergency Medicine (2012) xx,xxx–xxx
mechanicalintrinsiccardiaccontractility,and remained
LUCAS-2 dependent,mandatingperformingan urgent
aortic balloon valvuloplasty.
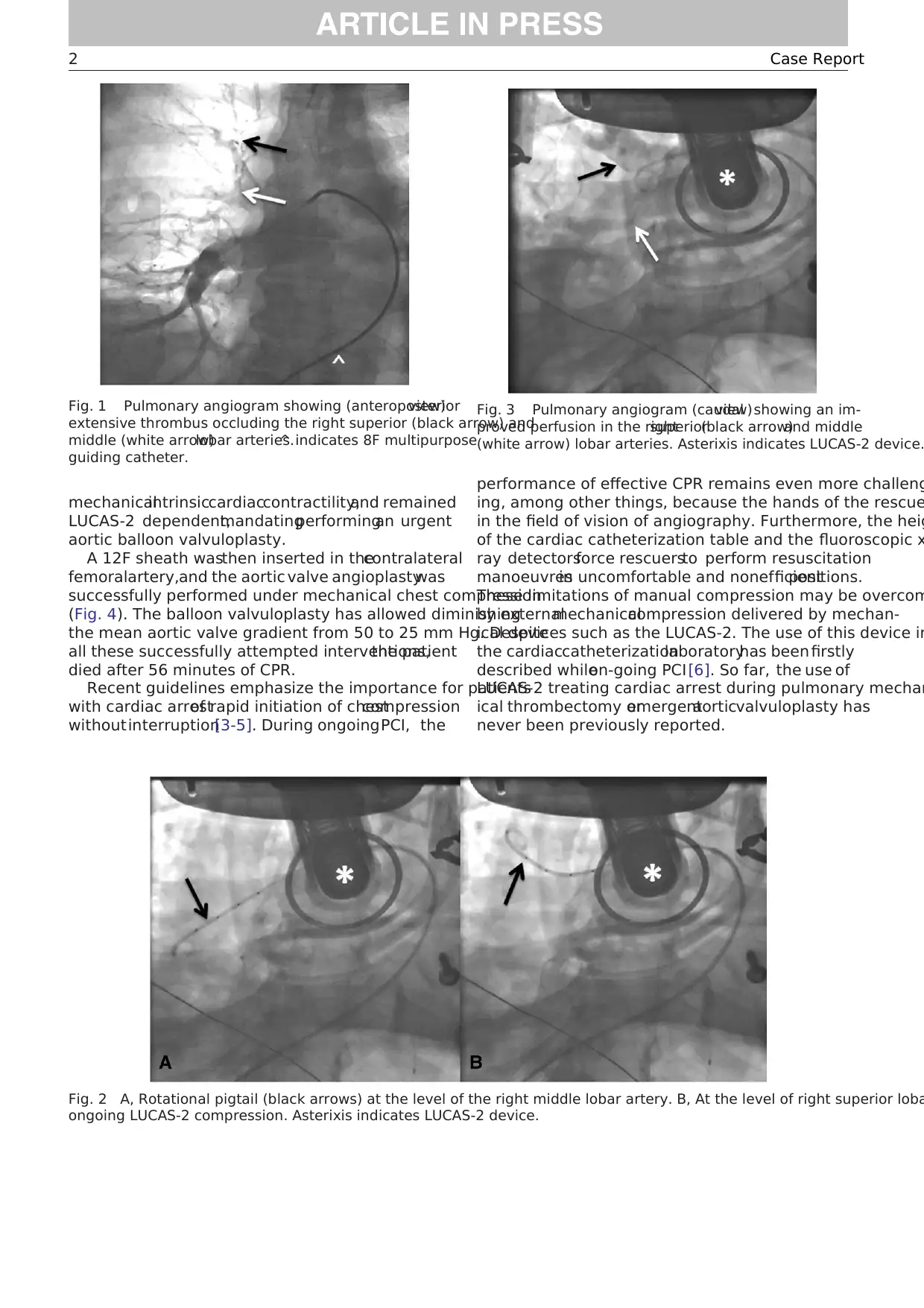
A 12F sheath wasthen inserted in thecontralateral
femoralartery,and the aortic valve angioplastywas
successfully performed under mechanical chest compression
(Fig. 4). The balloon valvuloplasty has allowed diminishing
the mean aortic valve gradient from 50 to 25 mm Hg. Despite
all these successfully attempted interventions,the patient
died after 56 minutes of CPR.
Recent guidelines emphasize the importance for patients
with cardiac arrestof rapid initiation of chestcompression
withoutinterruption[3-5]. During ongoingPCI, the
performance of effective CPR remains even more challeng
ing, among other things, because the hands of the rescue
in the field of vision of angiography. Furthermore, the heig
of the cardiac catheterization table and the fluoroscopic x
ray detectorsforce rescuersto perform resuscitation
manoeuvresin uncomfortable and nonefficientpositions.
These limitations of manual compression may be overcom
by externalmechanicalcompression delivered by mechan-
ical devices such as the LUCAS-2. The use of this device in
the cardiaccatheterizationlaboratoryhas been firstly
described whileon-going PCI [6]. So far, the use of
LUCAS-2 treating cardiac arrest during pulmonary mechan
ical thrombectomy oremergentaorticvalvuloplasty has
never been previously reported.
Fig. 1 Pulmonary angiogram showing (anteroposteriorview)
extensive thrombus occluding the right superior (black arrow) and
middle (white arrow)lobar arteries.^ indicates 8F multipurpose
guiding catheter.
Fig. 2 A, Rotational pigtail (black arrows) at the level of the right middle lobar artery. B, At the level of right superior loba
ongoing LUCAS-2 compression. Asterixis indicates LUCAS-2 device.
Fig. 3 Pulmonary angiogram (caudalview)showing an im-
proved perfusion in the rightsuperior(black arrow)and middle
(white arrow) lobar arteries. Asterixis indicates LUCAS-2 device.
2 Case Report
LUCAS-2 dependent,mandatingperformingan urgent
aortic balloon valvuloplasty.
A 12F sheath wasthen inserted in thecontralateral
femoralartery,and the aortic valve angioplastywas
successfully performed under mechanical chest compression
(Fig. 4). The balloon valvuloplasty has allowed diminishing
the mean aortic valve gradient from 50 to 25 mm Hg. Despite
all these successfully attempted interventions,the patient
died after 56 minutes of CPR.
Recent guidelines emphasize the importance for patients
with cardiac arrestof rapid initiation of chestcompression
withoutinterruption[3-5]. During ongoingPCI, the
performance of effective CPR remains even more challeng
ing, among other things, because the hands of the rescue
in the field of vision of angiography. Furthermore, the heig
of the cardiac catheterization table and the fluoroscopic x
ray detectorsforce rescuersto perform resuscitation
manoeuvresin uncomfortable and nonefficientpositions.
These limitations of manual compression may be overcom
by externalmechanicalcompression delivered by mechan-
ical devices such as the LUCAS-2. The use of this device in
the cardiaccatheterizationlaboratoryhas been firstly
described whileon-going PCI [6]. So far, the use of
LUCAS-2 treating cardiac arrest during pulmonary mechan
ical thrombectomy oremergentaorticvalvuloplasty has
never been previously reported.
Fig. 1 Pulmonary angiogram showing (anteroposteriorview)
extensive thrombus occluding the right superior (black arrow) and
middle (white arrow)lobar arteries.^ indicates 8F multipurpose
guiding catheter.
Fig. 2 A, Rotational pigtail (black arrows) at the level of the right middle lobar artery. B, At the level of right superior loba
ongoing LUCAS-2 compression. Asterixis indicates LUCAS-2 device.
Fig. 3 Pulmonary angiogram (caudalview)showing an im-
proved perfusion in the rightsuperior(black arrow)and middle
(white arrow) lobar arteries. Asterixis indicates LUCAS-2 device.
2 Case Report
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Experimentalstudieshave showedthat the use of
LUCAS-2 was associated with sustained coronary and
cerebralperfusion in an animalmodelwith cardiac arrest
[1,7]So far,only few case reports [8-10]and smallcase
series [6,11,12]have addressed its efficacy and safety in
humans with so far encouraging results.
The main advantageof the LUCAS-2 deviceis its
radiotranslucency,which allows performing fluoroscopic-
guided rescuing interventions without interrupting effective
chestcompression.Accordingly,our casessuggestthat
LUCAS-2 may effectively supportCPR manoeuvre per-
formed during a wide spectrum of noncoronary procedures.
Chan-il Park MD
Marco Roffi MD
Division of Cardiology
Department of Internal Medicine
Geneva University Hospitals
Switzerland
Karim Bendjelid MD,PhD
Intensive Care Department
Geneva University Hospitals
Switzerland
E-mail address: Karim.Bendjelid@hcuge.ch
Robert F.Bonvini MD
Division of Cardiology
Department of Internal Medicine
Geneva University Hospitals
Switzerland
http://dx.doi.org/10.1016/j.ajem.2012.07.022
References
[1] Steen S,Liao Q,Pierre L,Paskevicius A,Sjoberg T.Evaluation of
LUCAS, a new device forautomatic mechanicalcompression and
active decompression resuscitation. Resuscitation 2002;55:285-99.
[2] SundeK. Experimentaland clinicaluse of ongoing mechanical
cardiopulmonary resuscitation during angiography and percutaneou
coronary intervention. Crit Care Med 2008;36:S405-8.
[3] Field JM, Hazinski MF, Sayre MR, et al. Part 1: executive summary:
2010 American HeartAssociation Guidelines forCardiopulmonary
Resuscitationand EmergencyCardiovascularCare. Circulation
2010;122:S640-56.
[4] Abella BS, Alvarado JP, Myklebust H, et al. Quality of cardiopulmo-
nary resuscitation during in-hospital cardiac arrest.JAMA 2005;293:
305-10.
[5] Hightower D,Thomas SH,Stone CK,Dunn K,March JA.Decay in
quality ofclosed-chestcompressionsovertime.Ann Emerg Med
1995;26:300-3.
[6] WagnerH, Terkelsen CJ,Friberg H,et al. Cardiac arrestin the
catheterisation laboratory:a 5-yearexperience ofusing mechanical
chestcompressions to facilitate PCIduring prolonged resuscitation
efforts. Resuscitation 2010;81:383-7.
[7] Rubertsson S, Karlsten R. Increased cortical cerebral blood flow with
LUCAS; a new device for mechanical chest compressions compared
standard external compressions during experimental cardiopulmon
resuscitation. Resuscitation 2005;65:357-63.
[8] Nielsen N, Sandhall L, Schersten F, Friberg H, Olsson SE. Successful
resuscitation with mechanicalCPR, therapeutichypothermiaand
coronary intervention during manual CPR after out-of-hospital cardi
arrest. Resuscitation 2005;65:111-3.
[9] AgostoniP, CornelisK, Vermeersch P.Successfulpercutaneous
treatmentof an intraproceduralleft main stentthrombosis with the
supportof an automatic mechanicalchestcompression device.Int J
Cardiol 2008;124:e19-21.
[10] Grogaard HK,Wik L, Eriksen M,Brekke M,Sunde K.Continuous
mechanicalchestcompressionsduring cardiacarrestto facilitate
restorationof coronarycirculationwith percutaneouscoronary
intervention. J Am Coll Cardiol 2007;50:1093-4.
[11] Larsen AI,Hjornevik AS,Ellingsen CL,Nilsen DW.Cardiac arrest
with continuous mechanicalchestcompression during percutaneous
coronary intervention.A reporton the use ofthe LUCAS device.
Resuscitation 2007;75:454-9.
[12] Bonnemeier H, Olivecrona G, Simonis G, et al. Automated continuou
chestcompression forin-hospitalcardiopulmonary resuscitation of
patients with pulseless electrical activity: a report of five cases.Int J
Cardiol 2009;136:e39-50.
Fig. 4 Anteroposterior cranialview showing the aortic balloon
valvulopasty.Black arrows indicate Numed nucleus balloon 22
mm;white arrows,inflated intra-aortic balloon pump;Asterixis,
LUCAS-2 device; ^, temporary pacemaker lead.
3Case Report
View publication statsView publication stats
LUCAS-2 was associated with sustained coronary and
cerebralperfusion in an animalmodelwith cardiac arrest
[1,7]So far,only few case reports [8-10]and smallcase
series [6,11,12]have addressed its efficacy and safety in
humans with so far encouraging results.
The main advantageof the LUCAS-2 deviceis its
radiotranslucency,which allows performing fluoroscopic-
guided rescuing interventions without interrupting effective
chestcompression.Accordingly,our casessuggestthat
LUCAS-2 may effectively supportCPR manoeuvre per-
formed during a wide spectrum of noncoronary procedures.
Chan-il Park MD
Marco Roffi MD
Division of Cardiology
Department of Internal Medicine
Geneva University Hospitals
Switzerland
Karim Bendjelid MD,PhD
Intensive Care Department
Geneva University Hospitals
Switzerland
E-mail address: Karim.Bendjelid@hcuge.ch
Robert F.Bonvini MD
Division of Cardiology
Department of Internal Medicine
Geneva University Hospitals
Switzerland
http://dx.doi.org/10.1016/j.ajem.2012.07.022
References
[1] Steen S,Liao Q,Pierre L,Paskevicius A,Sjoberg T.Evaluation of
LUCAS, a new device forautomatic mechanicalcompression and
active decompression resuscitation. Resuscitation 2002;55:285-99.
[2] SundeK. Experimentaland clinicaluse of ongoing mechanical
cardiopulmonary resuscitation during angiography and percutaneou
coronary intervention. Crit Care Med 2008;36:S405-8.
[3] Field JM, Hazinski MF, Sayre MR, et al. Part 1: executive summary:
2010 American HeartAssociation Guidelines forCardiopulmonary
Resuscitationand EmergencyCardiovascularCare. Circulation
2010;122:S640-56.
[4] Abella BS, Alvarado JP, Myklebust H, et al. Quality of cardiopulmo-
nary resuscitation during in-hospital cardiac arrest.JAMA 2005;293:
305-10.
[5] Hightower D,Thomas SH,Stone CK,Dunn K,March JA.Decay in
quality ofclosed-chestcompressionsovertime.Ann Emerg Med
1995;26:300-3.
[6] WagnerH, Terkelsen CJ,Friberg H,et al. Cardiac arrestin the
catheterisation laboratory:a 5-yearexperience ofusing mechanical
chestcompressions to facilitate PCIduring prolonged resuscitation
efforts. Resuscitation 2010;81:383-7.
[7] Rubertsson S, Karlsten R. Increased cortical cerebral blood flow with
LUCAS; a new device for mechanical chest compressions compared
standard external compressions during experimental cardiopulmon
resuscitation. Resuscitation 2005;65:357-63.
[8] Nielsen N, Sandhall L, Schersten F, Friberg H, Olsson SE. Successful
resuscitation with mechanicalCPR, therapeutichypothermiaand
coronary intervention during manual CPR after out-of-hospital cardi
arrest. Resuscitation 2005;65:111-3.
[9] AgostoniP, CornelisK, Vermeersch P.Successfulpercutaneous
treatmentof an intraproceduralleft main stentthrombosis with the
supportof an automatic mechanicalchestcompression device.Int J
Cardiol 2008;124:e19-21.
[10] Grogaard HK,Wik L, Eriksen M,Brekke M,Sunde K.Continuous
mechanicalchestcompressionsduring cardiacarrestto facilitate
restorationof coronarycirculationwith percutaneouscoronary
intervention. J Am Coll Cardiol 2007;50:1093-4.
[11] Larsen AI,Hjornevik AS,Ellingsen CL,Nilsen DW.Cardiac arrest
with continuous mechanicalchestcompression during percutaneous
coronary intervention.A reporton the use ofthe LUCAS device.
Resuscitation 2007;75:454-9.
[12] Bonnemeier H, Olivecrona G, Simonis G, et al. Automated continuou
chestcompression forin-hospitalcardiopulmonary resuscitation of
patients with pulseless electrical activity: a report of five cases.Int J
Cardiol 2009;136:e39-50.
Fig. 4 Anteroposterior cranialview showing the aortic balloon
valvulopasty.Black arrows indicate Numed nucleus balloon 22
mm;white arrows,inflated intra-aortic balloon pump;Asterixis,
LUCAS-2 device; ^, temporary pacemaker lead.
3Case Report
View publication statsView publication stats
1 out of 4