Comprehensive Report on Expanded Program on Immunization (EPI)
VerifiedAdded on 2023/05/12
|14
|4440
|79
Report
AI Summary
This report provides a comprehensive overview of the Expanded Program on Immunization (EPI), a World Health Organization initiative aimed at providing vaccines to children globally. It covers the scope, history, and components of EPI, including routine immunization, supplemental immunization activities, disease surveillance, and mopping-up campaigns. The report details the goals of EPI, such as sustaining polio-free status, eliminating maternal and neonatal tetanus and measles, and accelerating control of hepatitis B, along with methods for evaluating immunization programs. It also discusses the diseases covered by EPI and provides a Bangladesh-specific perspective, highlighting the program's success in improving vaccination coverage. Additionally, the report touches on EPI schedules in different countries, including Pakistan, and emphasizes the importance of various strategies for implementing immunization programs effectively. Desklib offers this and other solved assignments for students.
An Assignment on Overall EPI (Expanded Program on
Immunization)
Course: PHI 208 Reproductive and Child Health
Submitted to Submitted by(Group-B)
Most. Zannatul Ferdous Arpita Chakrabarty(1599)
Lecturer Sayeda Sumaiya
Nahrin(1601)
Dept. Of Public Health and Informatics Rabeya Akter Mohua(1602)
Jahangirnagar University Fareha Hasan(1603)
Tasmiya Tabassum(1604)
1
Immunization)
Course: PHI 208 Reproductive and Child Health
Submitted to Submitted by(Group-B)
Most. Zannatul Ferdous Arpita Chakrabarty(1599)
Lecturer Sayeda Sumaiya
Nahrin(1601)
Dept. Of Public Health and Informatics Rabeya Akter Mohua(1602)
Jahangirnagar University Fareha Hasan(1603)
Tasmiya Tabassum(1604)
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Introduction
The Expanded Program on Immunization is a World Health Organization program with the goal
to make vaccines available to all children throughout the world.
‘Expanded’ means –
● Expanding the number of diseases to be covered
● Expanding the number of children and target population to be covered
● Expanding coverage to all corners of the country and spreading services to reach the less
privileged sectors of the society. (Masud & Navaratne, 2012)
Scope of EPI (Expanded Program on Immunization)
a) Experience with smallpox eradication program showed the world that immunization was
the most powerful and the cost-effective weapon against vaccine preventable diseases.
b) In 1974, the WHO launched its “Expanded Program of Immunization” (EPI) against six
most common preventable diseases (diphtheria, pertussis, tetanus, polio, tuberculosis,
measles and recently added pneumococcal vaccine). (Kaewkungwal et al., 2015)
History of EPI
The World Health Organization (WHO) initiated the Expanded Program on Immunization (EPI)
in May 1974 with the objective to vaccinate children throughout the world.
Ten years later, in 1984, the WHO established a standardized vaccination schedule for the
original EPI vaccines: Bacillus Calmette-Guérin (BCG), diphtheria-tetanus-pertussis (DTP), oral
polio, and measles. Increased knowledge of the immunologic factors of disease led to new
vaccines being developed and added to the EPI’s list of recommended vaccines: Hepatitis B
(HepB), yellow fever in countries endemic for the disease, and Haemophilus influenzae
meningitis (Hib) conjugate vaccine in countries with high burden of disease.
In 1999, the Global Alliance for Vaccines and Immunization (GAVI) was created with the sole
purpose of improving child health in the poorest countries by extending the reach of the EPI. The
GAVI brought together a grand coalition, including the UN agencies and institutions (WHO,
UNICEF, the World Bank), public health institutes, donor and implementing countries, the Bill
and Melinda Gates Foundation and The Rockefeller Foundation, the vaccine industry,
non-governmental organizations (NGOs) and many more. The creation of the GAVI has helped
2
The Expanded Program on Immunization is a World Health Organization program with the goal
to make vaccines available to all children throughout the world.
‘Expanded’ means –
● Expanding the number of diseases to be covered
● Expanding the number of children and target population to be covered
● Expanding coverage to all corners of the country and spreading services to reach the less
privileged sectors of the society. (Masud & Navaratne, 2012)
Scope of EPI (Expanded Program on Immunization)
a) Experience with smallpox eradication program showed the world that immunization was
the most powerful and the cost-effective weapon against vaccine preventable diseases.
b) In 1974, the WHO launched its “Expanded Program of Immunization” (EPI) against six
most common preventable diseases (diphtheria, pertussis, tetanus, polio, tuberculosis,
measles and recently added pneumococcal vaccine). (Kaewkungwal et al., 2015)
History of EPI
The World Health Organization (WHO) initiated the Expanded Program on Immunization (EPI)
in May 1974 with the objective to vaccinate children throughout the world.
Ten years later, in 1984, the WHO established a standardized vaccination schedule for the
original EPI vaccines: Bacillus Calmette-Guérin (BCG), diphtheria-tetanus-pertussis (DTP), oral
polio, and measles. Increased knowledge of the immunologic factors of disease led to new
vaccines being developed and added to the EPI’s list of recommended vaccines: Hepatitis B
(HepB), yellow fever in countries endemic for the disease, and Haemophilus influenzae
meningitis (Hib) conjugate vaccine in countries with high burden of disease.
In 1999, the Global Alliance for Vaccines and Immunization (GAVI) was created with the sole
purpose of improving child health in the poorest countries by extending the reach of the EPI. The
GAVI brought together a grand coalition, including the UN agencies and institutions (WHO,
UNICEF, the World Bank), public health institutes, donor and implementing countries, the Bill
and Melinda Gates Foundation and The Rockefeller Foundation, the vaccine industry,
non-governmental organizations (NGOs) and many more. The creation of the GAVI has helped
2
to renew interest and maintain the importance of immunizations in battling the world’s large
burden of infectious diseases. In addition, the GAVI has set up specific milestones to achieve the
EPI goals: that by 2010 all countries have routine immunization coverage of 90% of their child
population, that HepB be introduced in 80% of all countries by 2007, and that 50% of the poorest
countries have Hib vaccine by 2005.(Sarkar et al., 2017)
Component of EPI
Routine Immunization:
❏ Children 0-23 months-immunization with & EPI antigens
❏ Pregnant ladies by TT
Supplemental Immunization Activities:
❏ Routine immunization does not ensure 100% coverage of mobile population
i.e. nomads, NAs, hard to reach areas/missed areas. So SIAs are scheduled to ensure
coverage of these areas/population.
❏ NIDs/SNIDs: Children<5 years receive polio drops (3-days campaign)
Disease Surveillance:
❏ To detect case target diseases, the suspected cases of seven VPDs are reported by health
facilities to the distinct heath authorities for immediate launching of the control measures.
Mopping Up:
❏ Special campaign to 5-8 km around the infected locality to localize the disease and stop
transmission. (Masud and Navaratne, 2012)
Goals of EPI:
Vaccination has prevented millions of deaths and disabilities in the Western Pacific Region.
However, inequitable access to vaccination remains a major problem in many countries. The
Expanded Programme on Immunization (EPI) unit aims to build a Region free from
vaccine-preventable diseases. This is achieved by supporting Member States to achieve the goals
of the Regional Framework for Implementation of the Global Vaccine Action Plan.
3
burden of infectious diseases. In addition, the GAVI has set up specific milestones to achieve the
EPI goals: that by 2010 all countries have routine immunization coverage of 90% of their child
population, that HepB be introduced in 80% of all countries by 2007, and that 50% of the poorest
countries have Hib vaccine by 2005.(Sarkar et al., 2017)
Component of EPI
Routine Immunization:
❏ Children 0-23 months-immunization with & EPI antigens
❏ Pregnant ladies by TT
Supplemental Immunization Activities:
❏ Routine immunization does not ensure 100% coverage of mobile population
i.e. nomads, NAs, hard to reach areas/missed areas. So SIAs are scheduled to ensure
coverage of these areas/population.
❏ NIDs/SNIDs: Children<5 years receive polio drops (3-days campaign)
Disease Surveillance:
❏ To detect case target diseases, the suspected cases of seven VPDs are reported by health
facilities to the distinct heath authorities for immediate launching of the control measures.
Mopping Up:
❏ Special campaign to 5-8 km around the infected locality to localize the disease and stop
transmission. (Masud and Navaratne, 2012)
Goals of EPI:
Vaccination has prevented millions of deaths and disabilities in the Western Pacific Region.
However, inequitable access to vaccination remains a major problem in many countries. The
Expanded Programme on Immunization (EPI) unit aims to build a Region free from
vaccine-preventable diseases. This is achieved by supporting Member States to achieve the goals
of the Regional Framework for Implementation of the Global Vaccine Action Plan.
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
The immunization goals for the Western Pacific Region are:
● Sustaining polio-free status
● Eliminating maternal and neonatal tetanus
● Eliminating measles
● Accelerating control of hepatitis B
● Eliminating rubella
● Introducing new vaccines
● Meeting regional vaccination coverage targets
● Accelerating control of Japanese encephalitis.(Program & Office, 2016)
Evaluation of EPI:
In each country, immunization programs are monitored using two methods: an administrative
method and through community-based surveys. The administrative method uses immunization
data from public, private, and NGO clinics. Thus, the accuracy of the administrative method is
limited by the availability and accuracy of reports from these facilities. This method is easily
performed in areas where government services deliver the immunizations directly or where the
government supplies the vaccines to the clinics. In countries without the infrastructure to do this,
community-based surveys are used to estimate immunization coverage.
Community-based surveys are applied using a modified cluster sampling survey method
developed by the World Health Organization. Vaccine coverage is evaluated using a two-stage
sampling approach in which 30 clusters and seven children in each cluster are selected. Health
care workers with no or limited background in statistics and sampling are able to carry out data
collection with minimal training. Such a survey implementation provides a way to get
information from areas where there is no reliable data source. It is also used to validate reported
vaccine coverage (for example, from administrative reports) and is expected to estimate vaccine
coverage within 10 percent.
Surveys or questionnaires, though frequently considered inaccurate due to self-reporting, can
provide more detailed information than administrative reports alone. If home-based records are
available, vaccination status be determined and dates of vaccination can be reviewed to
determine if they were given at an ideal age and in appropriate intervals. Missed immunizations
can be identified and further qualified. Importantly, systems of vaccine delivery besides clinics
used for administrative evaluation can be identified and included in the analysis.(Dietz & Cutts,
1997)
4
● Sustaining polio-free status
● Eliminating maternal and neonatal tetanus
● Eliminating measles
● Accelerating control of hepatitis B
● Eliminating rubella
● Introducing new vaccines
● Meeting regional vaccination coverage targets
● Accelerating control of Japanese encephalitis.(Program & Office, 2016)
Evaluation of EPI:
In each country, immunization programs are monitored using two methods: an administrative
method and through community-based surveys. The administrative method uses immunization
data from public, private, and NGO clinics. Thus, the accuracy of the administrative method is
limited by the availability and accuracy of reports from these facilities. This method is easily
performed in areas where government services deliver the immunizations directly or where the
government supplies the vaccines to the clinics. In countries without the infrastructure to do this,
community-based surveys are used to estimate immunization coverage.
Community-based surveys are applied using a modified cluster sampling survey method
developed by the World Health Organization. Vaccine coverage is evaluated using a two-stage
sampling approach in which 30 clusters and seven children in each cluster are selected. Health
care workers with no or limited background in statistics and sampling are able to carry out data
collection with minimal training. Such a survey implementation provides a way to get
information from areas where there is no reliable data source. It is also used to validate reported
vaccine coverage (for example, from administrative reports) and is expected to estimate vaccine
coverage within 10 percent.
Surveys or questionnaires, though frequently considered inaccurate due to self-reporting, can
provide more detailed information than administrative reports alone. If home-based records are
available, vaccination status be determined and dates of vaccination can be reviewed to
determine if they were given at an ideal age and in appropriate intervals. Missed immunizations
can be identified and further qualified. Importantly, systems of vaccine delivery besides clinics
used for administrative evaluation can be identified and included in the analysis.(Dietz & Cutts,
1997)
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
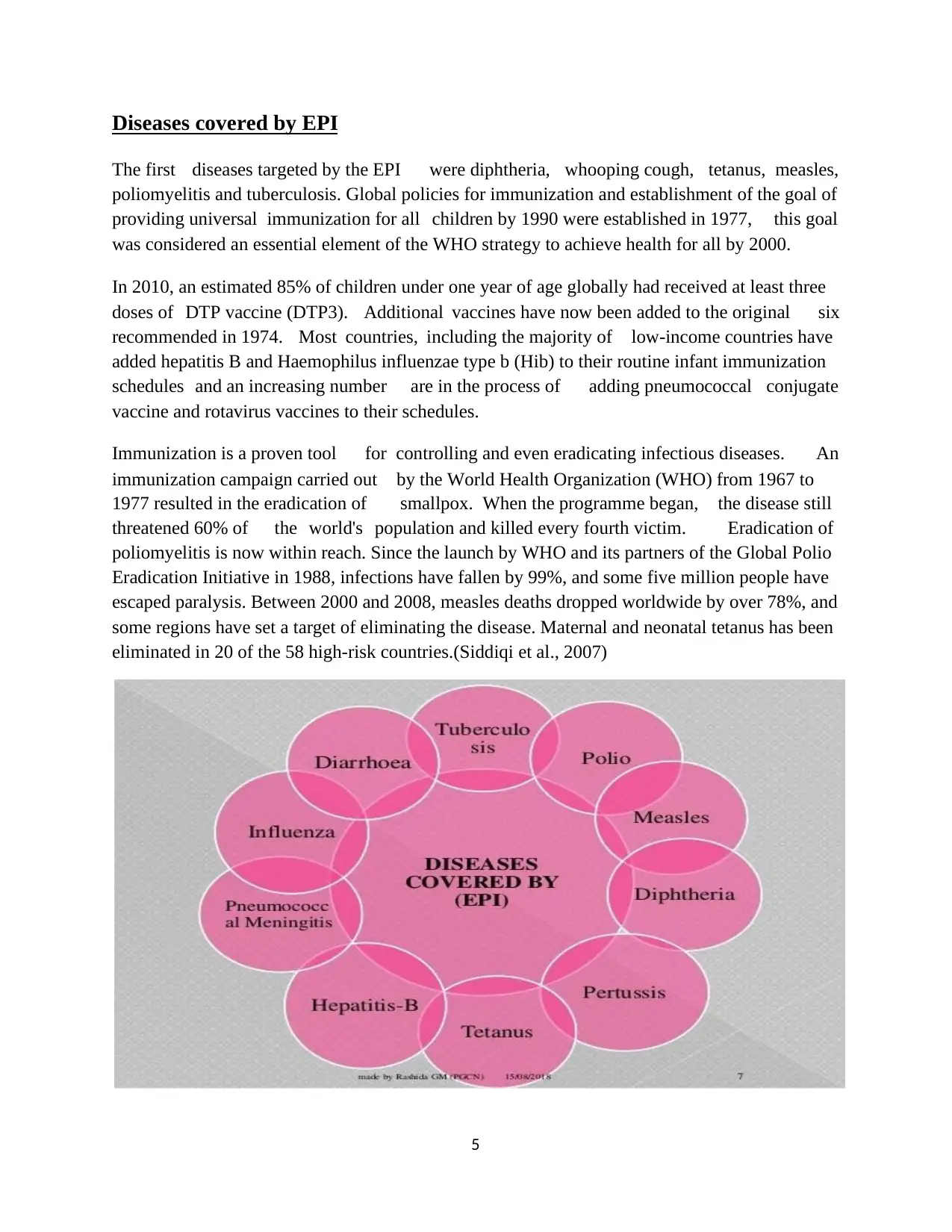
Diseases covered by EPI
The first diseases targeted by the EPI were diphtheria, whooping cough, tetanus, measles,
poliomyelitis and tuberculosis. Global policies for immunization and establishment of the goal of
providing universal immunization for all children by 1990 were established in 1977, this goal
was considered an essential element of the WHO strategy to achieve health for all by 2000.
In 2010, an estimated 85% of children under one year of age globally had received at least three
doses of DTP vaccine (DTP3). Additional vaccines have now been added to the original six
recommended in 1974. Most countries, including the majority of low-income countries have
added hepatitis B and Haemophilus influenzae type b (Hib) to their routine infant immunization
schedules and an increasing number are in the process of adding pneumococcal conjugate
vaccine and rotavirus vaccines to their schedules.
Immunization is a proven tool for controlling and even eradicating infectious diseases. An
immunization campaign carried out by the World Health Organization (WHO) from 1967 to
1977 resulted in the eradication of smallpox. When the programme began, the disease still
threatened 60% of the world's population and killed every fourth victim. Eradication of
poliomyelitis is now within reach. Since the launch by WHO and its partners of the Global Polio
Eradication Initiative in 1988, infections have fallen by 99%, and some five million people have
escaped paralysis. Between 2000 and 2008, measles deaths dropped worldwide by over 78%, and
some regions have set a target of eliminating the disease. Maternal and neonatal tetanus has been
eliminated in 20 of the 58 high-risk countries.(Siddiqi et al., 2007)
5
The first diseases targeted by the EPI were diphtheria, whooping cough, tetanus, measles,
poliomyelitis and tuberculosis. Global policies for immunization and establishment of the goal of
providing universal immunization for all children by 1990 were established in 1977, this goal
was considered an essential element of the WHO strategy to achieve health for all by 2000.
In 2010, an estimated 85% of children under one year of age globally had received at least three
doses of DTP vaccine (DTP3). Additional vaccines have now been added to the original six
recommended in 1974. Most countries, including the majority of low-income countries have
added hepatitis B and Haemophilus influenzae type b (Hib) to their routine infant immunization
schedules and an increasing number are in the process of adding pneumococcal conjugate
vaccine and rotavirus vaccines to their schedules.
Immunization is a proven tool for controlling and even eradicating infectious diseases. An
immunization campaign carried out by the World Health Organization (WHO) from 1967 to
1977 resulted in the eradication of smallpox. When the programme began, the disease still
threatened 60% of the world's population and killed every fourth victim. Eradication of
poliomyelitis is now within reach. Since the launch by WHO and its partners of the Global Polio
Eradication Initiative in 1988, infections have fallen by 99%, and some five million people have
escaped paralysis. Between 2000 and 2008, measles deaths dropped worldwide by over 78%, and
some regions have set a target of eliminating the disease. Maternal and neonatal tetanus has been
eliminated in 20 of the 58 high-risk countries.(Siddiqi et al., 2007)
5
EPI in Bangladesh Perspective
The Expanded Program on Immunization (EPI) vaccines are provided by the Government of
Bangladesh. The EPI vaccination service is open seven days a week, 8:30am – 5:00pm
(including national holidays) at the Dhaka Hospital.
The following EPI vaccines are available for age group 0-2 years.
√BCG
√Pentavalent
√Inactivated Poliomyelitis Vaccine (IPV)
√Pneumococcal conjugate vaccine (PCV)
√Measles and Rubella Vaccine
√Tetanus toxoid available for women within age group 15-49 years.
Immunization is the process of inducing to an infectious organism or agent in an individual
through vaccination. The WHO initiated the Expanded Program on Immunization (EPI) in May,
1974 but EPI in Bangladesh was inaugurated on April 7, 1979 (World Health Day) to ensure that
infants/children and mothers have access to routinely recommended infant/childhood vaccines.
Six vaccine-preventable diseases were initially included in the EPI: tuberculosis, poliomyelitis,
diphtheria, tetanus, pertussis and measles. This study was reviewed by local and international
development partners including WHO, UNICEF, World Bank, Ministry and Welfare in
Bangladesh and so on. The results strongly suggested that routine immunization has played a
vital role significantly in improving the vaccination coverage in Bangladesh since 1985, it’s
about 2% vaccine coverage to till now its 82.5% vaccine coverage by 2015. The Expanded
Program on Immunization (EPI) in Bangladesh is one of the successful programs which aims to
assess the routine Childhood vaccination coverage; Measles Second Dose (MSD) coverage; TT
vaccination coverage among women with children 0-11 months; TT5 Coverage and Vitamin A
coverage among the children aged 6-59 months etc.
The Expanded Program on Immunization (EPI) is one of the most successful public health
interventions in Bangladesh, and has contributed significantly to reducing mortality and
morbidity from vaccine preventable diseases. The service delivery mechanism of EPI throughout
the country has been used as the role model and a platform to deliver other interventions. The
latest report shows that the coverage of the fully vaccinated children who had taken the doses as
per schedule before celebrating their first birth day was 81 percent in 2013. Though the rate is
still much lower than the government’s target of 90 percent by 2016, the Expanded Program of
Immunization (EPI) that oversees child immunization finds it to be “a success”. The coverage
has been consistently increasing by one percentage point for the last six years. Bangladesh is
much appreciated for its high vaccine coverage in routine immunization and it received two
‘GAVI best performance award’ within the past six years.(Benichou, 2014)
6
The Expanded Program on Immunization (EPI) vaccines are provided by the Government of
Bangladesh. The EPI vaccination service is open seven days a week, 8:30am – 5:00pm
(including national holidays) at the Dhaka Hospital.
The following EPI vaccines are available for age group 0-2 years.
√BCG
√Pentavalent
√Inactivated Poliomyelitis Vaccine (IPV)
√Pneumococcal conjugate vaccine (PCV)
√Measles and Rubella Vaccine
√Tetanus toxoid available for women within age group 15-49 years.
Immunization is the process of inducing to an infectious organism or agent in an individual
through vaccination. The WHO initiated the Expanded Program on Immunization (EPI) in May,
1974 but EPI in Bangladesh was inaugurated on April 7, 1979 (World Health Day) to ensure that
infants/children and mothers have access to routinely recommended infant/childhood vaccines.
Six vaccine-preventable diseases were initially included in the EPI: tuberculosis, poliomyelitis,
diphtheria, tetanus, pertussis and measles. This study was reviewed by local and international
development partners including WHO, UNICEF, World Bank, Ministry and Welfare in
Bangladesh and so on. The results strongly suggested that routine immunization has played a
vital role significantly in improving the vaccination coverage in Bangladesh since 1985, it’s
about 2% vaccine coverage to till now its 82.5% vaccine coverage by 2015. The Expanded
Program on Immunization (EPI) in Bangladesh is one of the successful programs which aims to
assess the routine Childhood vaccination coverage; Measles Second Dose (MSD) coverage; TT
vaccination coverage among women with children 0-11 months; TT5 Coverage and Vitamin A
coverage among the children aged 6-59 months etc.
The Expanded Program on Immunization (EPI) is one of the most successful public health
interventions in Bangladesh, and has contributed significantly to reducing mortality and
morbidity from vaccine preventable diseases. The service delivery mechanism of EPI throughout
the country has been used as the role model and a platform to deliver other interventions. The
latest report shows that the coverage of the fully vaccinated children who had taken the doses as
per schedule before celebrating their first birth day was 81 percent in 2013. Though the rate is
still much lower than the government’s target of 90 percent by 2016, the Expanded Program of
Immunization (EPI) that oversees child immunization finds it to be “a success”. The coverage
has been consistently increasing by one percentage point for the last six years. Bangladesh is
much appreciated for its high vaccine coverage in routine immunization and it received two
‘GAVI best performance award’ within the past six years.(Benichou, 2014)
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
EPI Schedule
Each region has slightly varying ways of setting up and implementing their immunization
programs shedule based on their level of health infrastructure.
Some areas will have fixed sites for vaccination. Health care facilities such as hospitals or health
posts that include vaccination with many other health care activities. But in areas where the
number of structured health facilities is small, mobile vaccination teams consisting of staff
members from a health facility can deliver vaccines straight to individual towns and villages.
These ‘outreach’ services are often scheduled throughout the year. However, in especially
under-developed countries where proper communication and infrastructure is absent,
cancellation of the planned immunization visits leads to deterioration of the program. A better
strategy in such countries is the ‘pulse immunization’ technique, where ‘pulses’ of vaccines are
given to children in annual vaccination campaigns.
Additional strategies are needed if the area of the program consists of poor urban communities
because such areas tend to have low uptake of vaccination programs. Door-to-door canvassing,
also referred to as channeling, is used to increase uptake in such hard to reach groups. Finally,
periodic national-level mass vaccination campaigns are being increasingly included in the
programs.(Masud & Navaratne, 2012)
The EPI schedule discussion of some country are given below:
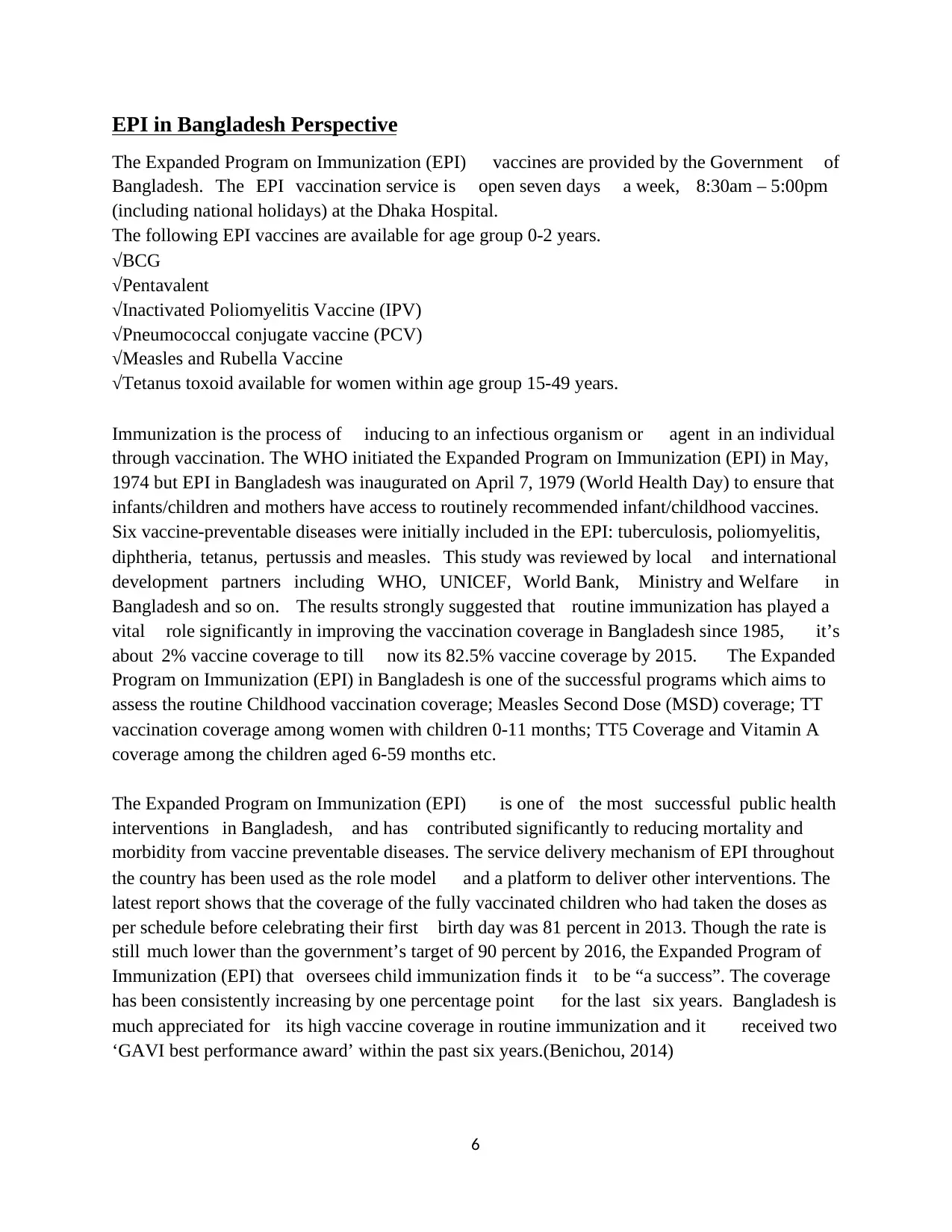
Pakistan:
The Expanded Program on Immunization (EPI) was initiated by World Health Organization
(WHO) in 1974 in order to save children from life threatening, disabling childhood illnesses.
The aim was to immunize children against 6 vaccine-preventable diseases (VPDs) i.e.
poliomyelitis, neonatal tetanus, measles, diphtheria, pertussis and tuberculosis. In Pakistan, this
program was launched in 1978 with the main objectives of eradicating polio by 2012,
eliminating measles and neonatal tetanus by 2015, and minimizing the incidence of other VPDs.
. Later, vaccines against hepatitis B (2002), hemophilus influenzae type B (2008) and were also
added with support from the government and development partners. Above table provides an
overview of the current EPI schedule in Pakistan. According to the 2010 report of Pakistan
Institute of Legislative Development and Transparency (PILDAT), presently 15% of deaths
below the age 5 years make up 50% of overall mortality in Pakistan, showing children as the
most neglected part of Pakistan’s society. Although there has been a big improvement in EPI
coverage in Pakistan in recent years, stronger measures are still required to achieve the desired
results. The percentage of Pakistani children (age 12–23 months) receiving all the vaccines is
only 47%, and 6% of children remain non vaccinated. Complete EPI coverage from province to
7
Each region has slightly varying ways of setting up and implementing their immunization
programs shedule based on their level of health infrastructure.
Some areas will have fixed sites for vaccination. Health care facilities such as hospitals or health
posts that include vaccination with many other health care activities. But in areas where the
number of structured health facilities is small, mobile vaccination teams consisting of staff
members from a health facility can deliver vaccines straight to individual towns and villages.
These ‘outreach’ services are often scheduled throughout the year. However, in especially
under-developed countries where proper communication and infrastructure is absent,
cancellation of the planned immunization visits leads to deterioration of the program. A better
strategy in such countries is the ‘pulse immunization’ technique, where ‘pulses’ of vaccines are
given to children in annual vaccination campaigns.
Additional strategies are needed if the area of the program consists of poor urban communities
because such areas tend to have low uptake of vaccination programs. Door-to-door canvassing,
also referred to as channeling, is used to increase uptake in such hard to reach groups. Finally,
periodic national-level mass vaccination campaigns are being increasingly included in the
programs.(Masud & Navaratne, 2012)
The EPI schedule discussion of some country are given below:
Pakistan:
The Expanded Program on Immunization (EPI) was initiated by World Health Organization
(WHO) in 1974 in order to save children from life threatening, disabling childhood illnesses.
The aim was to immunize children against 6 vaccine-preventable diseases (VPDs) i.e.
poliomyelitis, neonatal tetanus, measles, diphtheria, pertussis and tuberculosis. In Pakistan, this
program was launched in 1978 with the main objectives of eradicating polio by 2012,
eliminating measles and neonatal tetanus by 2015, and minimizing the incidence of other VPDs.
. Later, vaccines against hepatitis B (2002), hemophilus influenzae type B (2008) and were also
added with support from the government and development partners. Above table provides an
overview of the current EPI schedule in Pakistan. According to the 2010 report of Pakistan
Institute of Legislative Development and Transparency (PILDAT), presently 15% of deaths
below the age 5 years make up 50% of overall mortality in Pakistan, showing children as the
most neglected part of Pakistan’s society. Although there has been a big improvement in EPI
coverage in Pakistan in recent years, stronger measures are still required to achieve the desired
results. The percentage of Pakistani children (age 12–23 months) receiving all the vaccines is
only 47%, and 6% of children remain non vaccinated. Complete EPI coverage from province to
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
province also shows marked variation, being 35% in Baluchistan, 37% in Sindh, 53% in Punjab,
47% in Khyber Pakhtunkhwa (KPK). Routine EPI coverage as of 2007 was: BCG - 89%, Polio -
83%, DPT - 83%, Hepatitis B - 83% and Tetanus Toxoid - 46%. These numbers showed
improvements in 2012 to 95%, 89%, 89%, 89% and 68% respectively. Despite the mentioned
coverage, Pakistan is still among the 3 countries of the world where wild poliovirus remains
endemic. The government of Pakistan provides only 20% of total immunization expenditure
while, EPI with the help of UNICEF, WHO, GAVI-ALLIANCE shares the major burden of
funding. Despite the funding provided by EPI and routine immunization coverage, Pakistan has
seen outbreaks of measles and diphtheria in 2012, and an increased in number of tuberculosis
and tetanus cases due to weak implementation and the major focus of government being on the
polio eradication. About 1000 deaths of children less than 5 years of age will occur if the EPI
program is discontinued, which signifies its importance.(Owais et al., 2013)
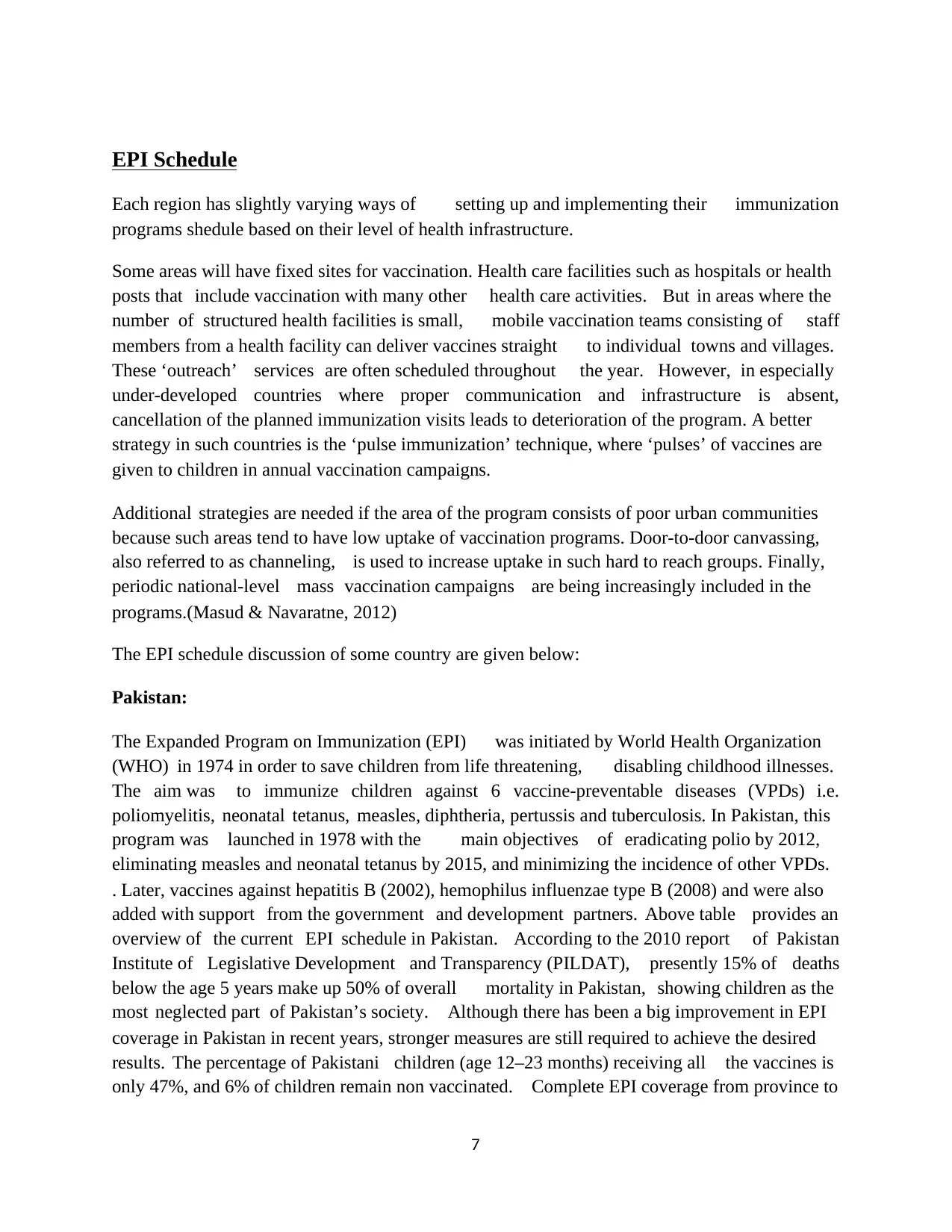
Bangladesh :
EPI activities in Bangladesh were launched on April 7, 1979 (World Health Day) with the
support of World Health Organization (WHO) and UNICEF EPI coverage remained less than 2
% by 1985, with 82.5 % by 2015 children were fully vaccinated. In 1985, the Government of the
People’s Republic of Bangladesh committed to the Global Universal Child Immunization
Initiative (UCI), and began phase – wise process of EPI intensification from 1985-1990
throughout 476 Upazila, 92 major Municipalities and 6 City Corporations. EPI was made
available to all target groups (infants and pregnant mothers) by 1990. (Park, 2015)
8
47% in Khyber Pakhtunkhwa (KPK). Routine EPI coverage as of 2007 was: BCG - 89%, Polio -
83%, DPT - 83%, Hepatitis B - 83% and Tetanus Toxoid - 46%. These numbers showed
improvements in 2012 to 95%, 89%, 89%, 89% and 68% respectively. Despite the mentioned
coverage, Pakistan is still among the 3 countries of the world where wild poliovirus remains
endemic. The government of Pakistan provides only 20% of total immunization expenditure
while, EPI with the help of UNICEF, WHO, GAVI-ALLIANCE shares the major burden of
funding. Despite the funding provided by EPI and routine immunization coverage, Pakistan has
seen outbreaks of measles and diphtheria in 2012, and an increased in number of tuberculosis
and tetanus cases due to weak implementation and the major focus of government being on the
polio eradication. About 1000 deaths of children less than 5 years of age will occur if the EPI
program is discontinued, which signifies its importance.(Owais et al., 2013)
Bangladesh :
EPI activities in Bangladesh were launched on April 7, 1979 (World Health Day) with the
support of World Health Organization (WHO) and UNICEF EPI coverage remained less than 2
% by 1985, with 82.5 % by 2015 children were fully vaccinated. In 1985, the Government of the
People’s Republic of Bangladesh committed to the Global Universal Child Immunization
Initiative (UCI), and began phase – wise process of EPI intensification from 1985-1990
throughout 476 Upazila, 92 major Municipalities and 6 City Corporations. EPI was made
available to all target groups (infants and pregnant mothers) by 1990. (Park, 2015)
8
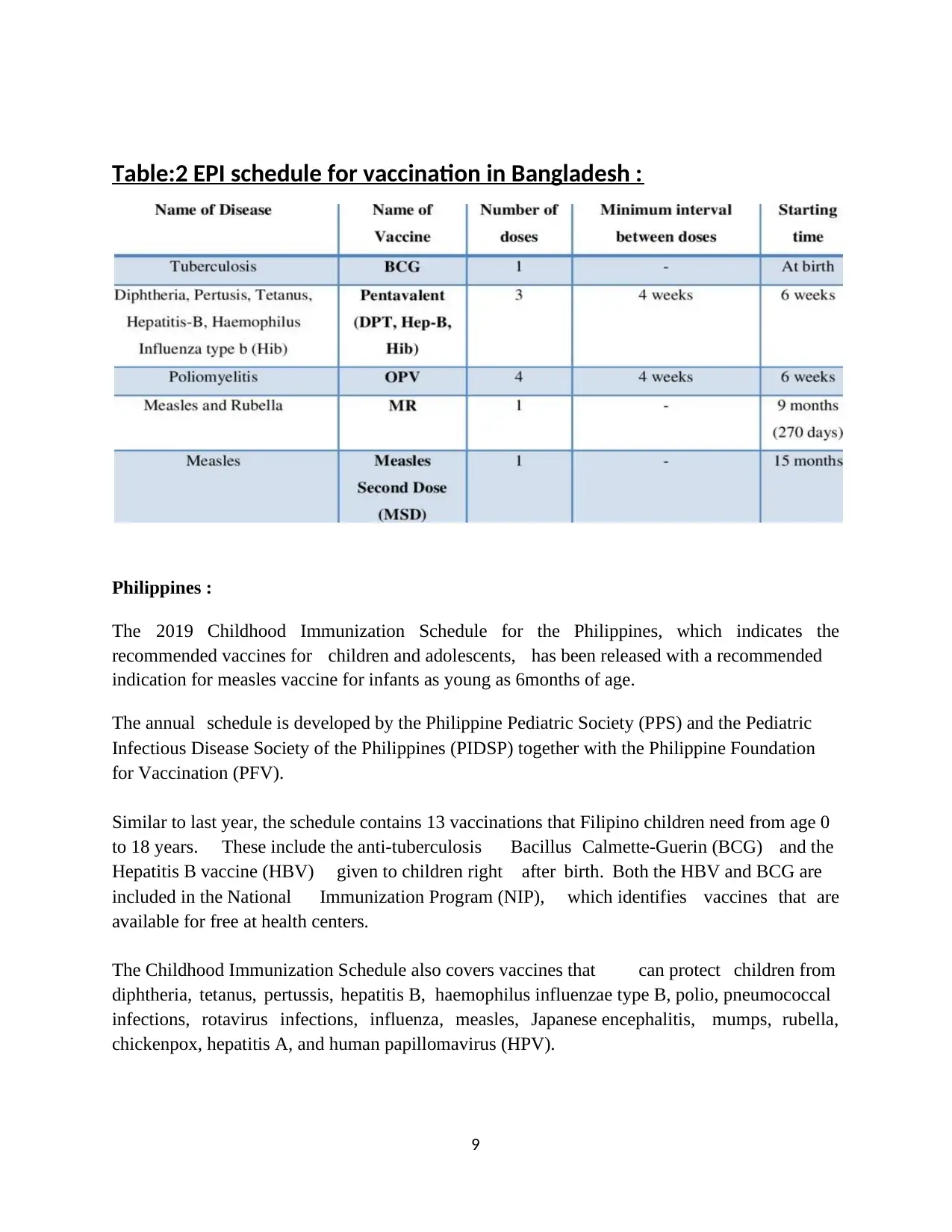
Table:2 EPI schedule for vaccination in Bangladesh :
Philippines :
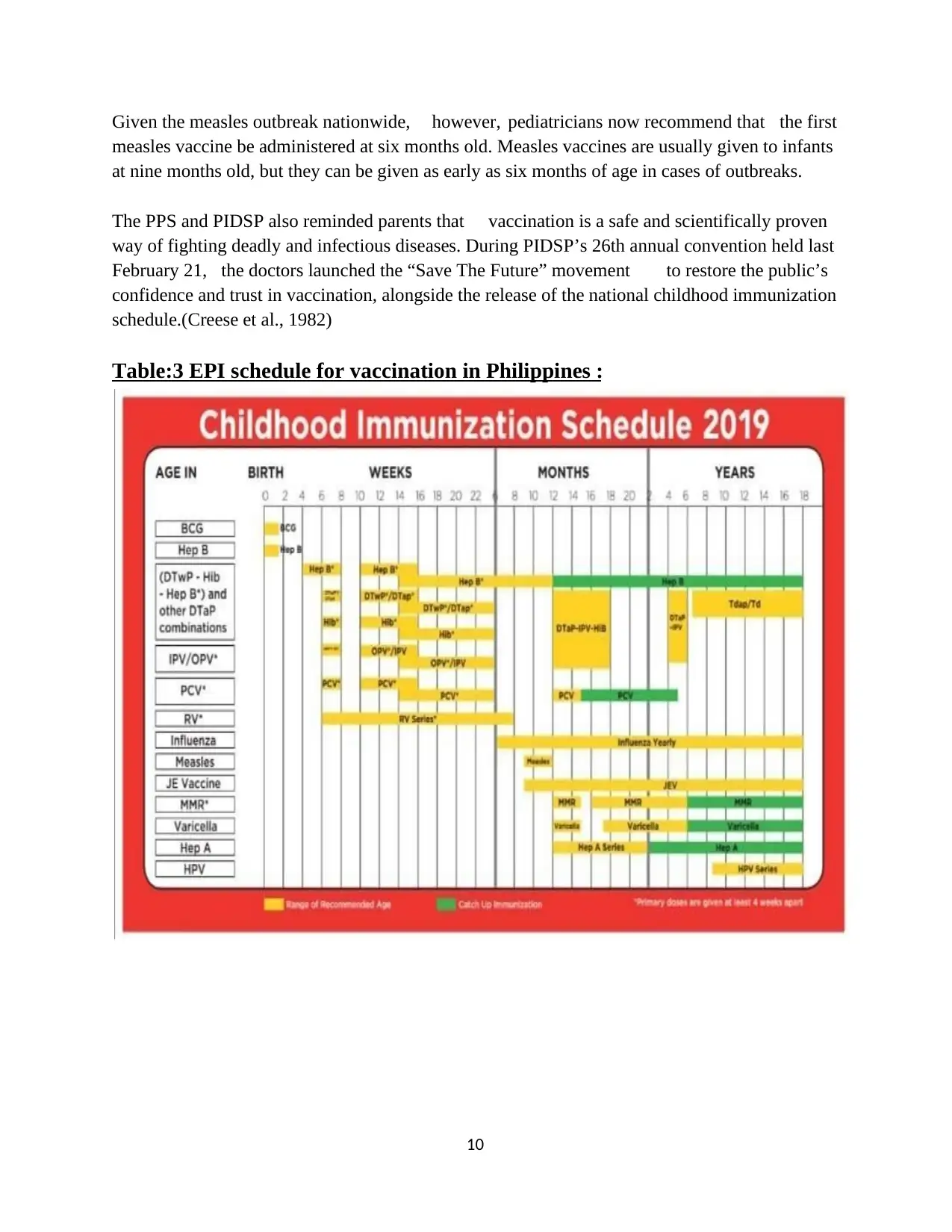
The 2019 Childhood Immunization Schedule for the Philippines, which indicates the
recommended vaccines for children and adolescents, has been released with a recommended
indication for measles vaccine for infants as young as 6months of age.
The annual schedule is developed by the Philippine Pediatric Society (PPS) and the Pediatric
Infectious Disease Society of the Philippines (PIDSP) together with the Philippine Foundation
for Vaccination (PFV).
Similar to last year, the schedule contains 13 vaccinations that Filipino children need from age 0
to 18 years. These include the anti-tuberculosis Bacillus Calmette-Guerin (BCG) and the
Hepatitis B vaccine (HBV) given to children right after birth. Both the HBV and BCG are
included in the National Immunization Program (NIP), which identifies vaccines that are
available for free at health centers.
The Childhood Immunization Schedule also covers vaccines that can protect children from
diphtheria, tetanus, pertussis, hepatitis B, haemophilus influenzae type B, polio, pneumococcal
infections, rotavirus infections, influenza, measles, Japanese encephalitis, mumps, rubella,
chickenpox, hepatitis A, and human papillomavirus (HPV).
9
Philippines :
The 2019 Childhood Immunization Schedule for the Philippines, which indicates the
recommended vaccines for children and adolescents, has been released with a recommended
indication for measles vaccine for infants as young as 6months of age.
The annual schedule is developed by the Philippine Pediatric Society (PPS) and the Pediatric
Infectious Disease Society of the Philippines (PIDSP) together with the Philippine Foundation
for Vaccination (PFV).
Similar to last year, the schedule contains 13 vaccinations that Filipino children need from age 0
to 18 years. These include the anti-tuberculosis Bacillus Calmette-Guerin (BCG) and the
Hepatitis B vaccine (HBV) given to children right after birth. Both the HBV and BCG are
included in the National Immunization Program (NIP), which identifies vaccines that are
available for free at health centers.
The Childhood Immunization Schedule also covers vaccines that can protect children from
diphtheria, tetanus, pertussis, hepatitis B, haemophilus influenzae type B, polio, pneumococcal
infections, rotavirus infections, influenza, measles, Japanese encephalitis, mumps, rubella,
chickenpox, hepatitis A, and human papillomavirus (HPV).
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Given the measles outbreak nationwide, however, pediatricians now recommend that the first
measles vaccine be administered at six months old. Measles vaccines are usually given to infants
at nine months old, but they can be given as early as six months of age in cases of outbreaks.
The PPS and PIDSP also reminded parents that vaccination is a safe and scientifically proven
way of fighting deadly and infectious diseases. During PIDSP’s 26th annual convention held last
February 21, the doctors launched the “Save The Future” movement to restore the public’s
confidence and trust in vaccination, alongside the release of the national childhood immunization
schedule.(Creese et al., 1982)
Table:3 EPI schedule for vaccination in Philippines :
10
measles vaccine be administered at six months old. Measles vaccines are usually given to infants
at nine months old, but they can be given as early as six months of age in cases of outbreaks.
The PPS and PIDSP also reminded parents that vaccination is a safe and scientifically proven
way of fighting deadly and infectious diseases. During PIDSP’s 26th annual convention held last
February 21, the doctors launched the “Save The Future” movement to restore the public’s
confidence and trust in vaccination, alongside the release of the national childhood immunization
schedule.(Creese et al., 1982)
Table:3 EPI schedule for vaccination in Philippines :
10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
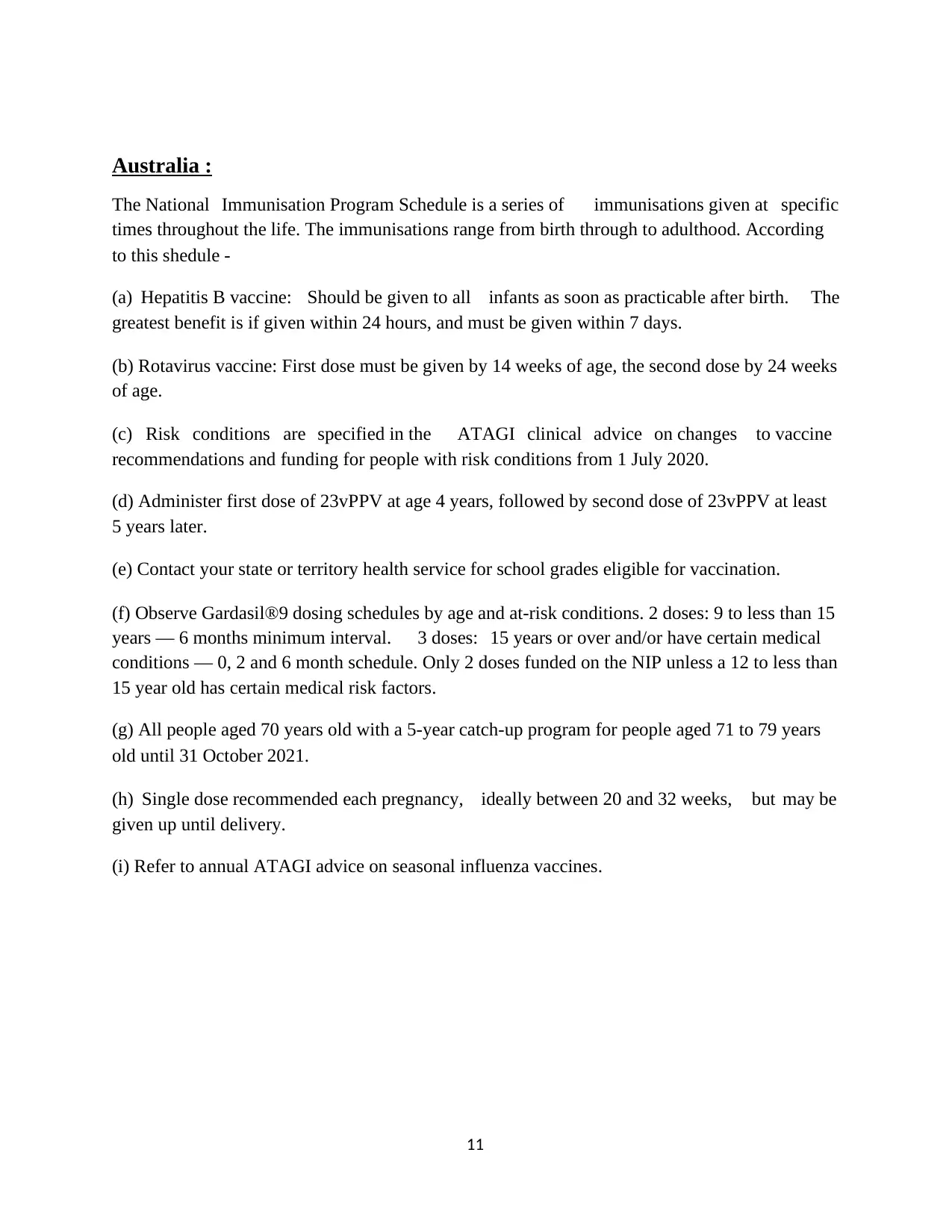
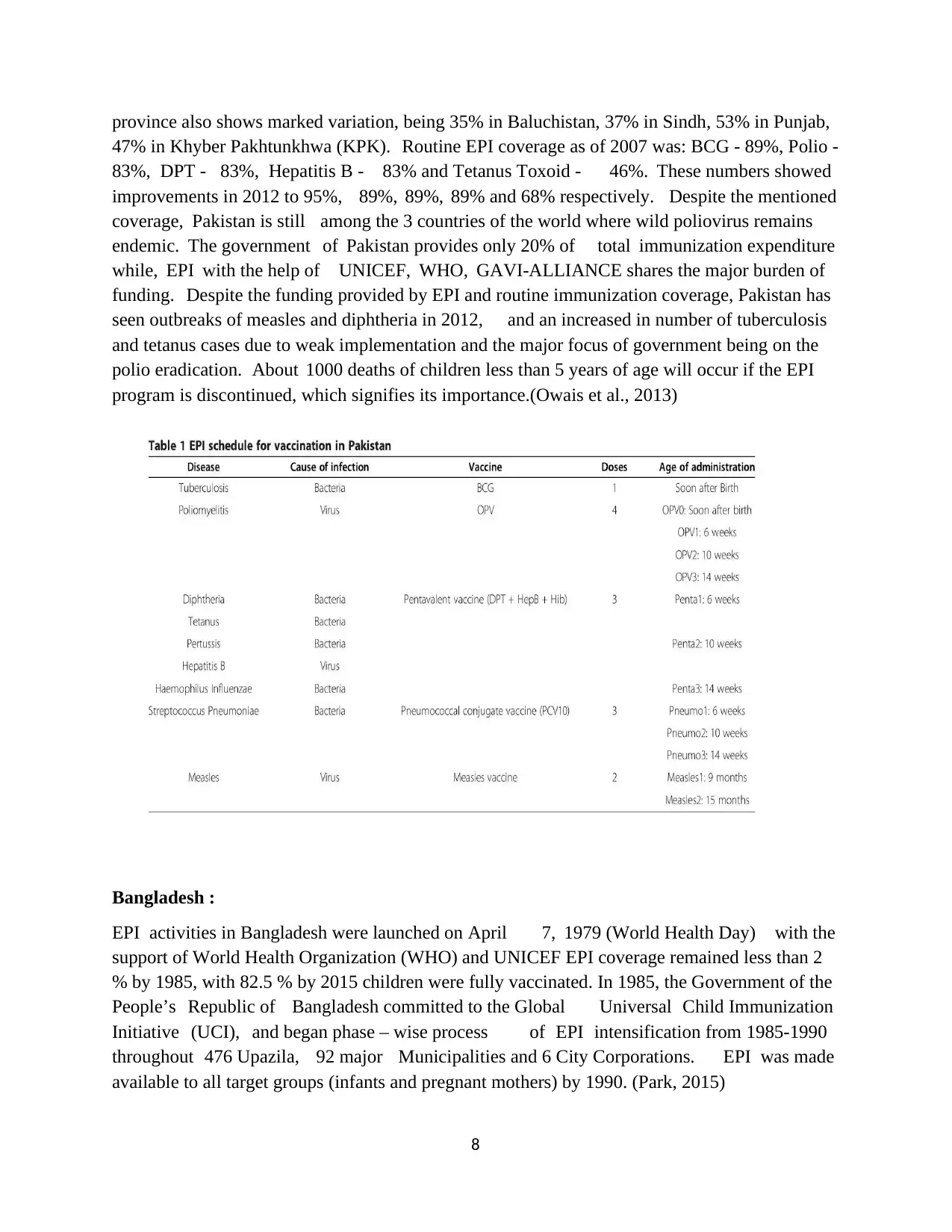
Australia :
The National Immunisation Program Schedule is a series of immunisations given at specific
times throughout the life. The immunisations range from birth through to adulthood. According
to this shedule -
(a) Hepatitis B vaccine: Should be given to all infants as soon as practicable after birth. The
greatest benefit is if given within 24 hours, and must be given within 7 days.
(b) Rotavirus vaccine: First dose must be given by 14 weeks of age, the second dose by 24 weeks
of age.
(c) Risk conditions are specified in the ATAGI clinical advice on changes to vaccine
recommendations and funding for people with risk conditions from 1 July 2020.
(d) Administer first dose of 23vPPV at age 4 years, followed by second dose of 23vPPV at least
5 years later.
(e) Contact your state or territory health service for school grades eligible for vaccination.
(f) Observe Gardasil®9 dosing schedules by age and at-risk conditions. 2 doses: 9 to less than 15
years — 6 months minimum interval. 3 doses: 15 years or over and/or have certain medical
conditions — 0, 2 and 6 month schedule. Only 2 doses funded on the NIP unless a 12 to less than
15 year old has certain medical risk factors.
(g) All people aged 70 years old with a 5-year catch-up program for people aged 71 to 79 years
old until 31 October 2021.
(h) Single dose recommended each pregnancy, ideally between 20 and 32 weeks, but may be
given up until delivery.
(i) Refer to annual ATAGI advice on seasonal influenza vaccines.
11
The National Immunisation Program Schedule is a series of immunisations given at specific
times throughout the life. The immunisations range from birth through to adulthood. According
to this shedule -
(a) Hepatitis B vaccine: Should be given to all infants as soon as practicable after birth. The
greatest benefit is if given within 24 hours, and must be given within 7 days.
(b) Rotavirus vaccine: First dose must be given by 14 weeks of age, the second dose by 24 weeks
of age.
(c) Risk conditions are specified in the ATAGI clinical advice on changes to vaccine
recommendations and funding for people with risk conditions from 1 July 2020.
(d) Administer first dose of 23vPPV at age 4 years, followed by second dose of 23vPPV at least
5 years later.
(e) Contact your state or territory health service for school grades eligible for vaccination.
(f) Observe Gardasil®9 dosing schedules by age and at-risk conditions. 2 doses: 9 to less than 15
years — 6 months minimum interval. 3 doses: 15 years or over and/or have certain medical
conditions — 0, 2 and 6 month schedule. Only 2 doses funded on the NIP unless a 12 to less than
15 year old has certain medical risk factors.
(g) All people aged 70 years old with a 5-year catch-up program for people aged 71 to 79 years
old until 31 October 2021.
(h) Single dose recommended each pregnancy, ideally between 20 and 32 weeks, but may be
given up until delivery.
(i) Refer to annual ATAGI advice on seasonal influenza vaccines.
11
Table:4 Immunization schedule in Australia
All people aged less than 20 years are eligible for free catch-up vaccines. Adult refugees and
humanitarian entrants are eligible for free catch-up vaccines. Refer to catch-up immunisations
information below.
People over 12 months of age with conditions that increase their risk of pneumococcal disease
require a dose of 13vPCV at diagnosis followed by 2 doses of 23vPPV. Refer to the Australian
Immunisation Handbook (the Handbook) for dose intervals. Not all risk conditions are funded
under the NIP. For eligibility refer to the ATAGI clinical advice on changes to vaccine
recommendations and funding for people with risk conditions from 1 July 2020.
The national immunisation also funds vaccines for people of all ages with the specified medical
conditions.(Koop et al., 2001)
12
All people aged less than 20 years are eligible for free catch-up vaccines. Adult refugees and
humanitarian entrants are eligible for free catch-up vaccines. Refer to catch-up immunisations
information below.
People over 12 months of age with conditions that increase their risk of pneumococcal disease
require a dose of 13vPCV at diagnosis followed by 2 doses of 23vPPV. Refer to the Australian
Immunisation Handbook (the Handbook) for dose intervals. Not all risk conditions are funded
under the NIP. For eligibility refer to the ATAGI clinical advice on changes to vaccine
recommendations and funding for people with risk conditions from 1 July 2020.
The national immunisation also funds vaccines for people of all ages with the specified medical
conditions.(Koop et al., 2001)
12
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





