Physiological Effects of Altitude on Respiratory System
VerifiedAdded on 2022/10/04
|10
|1855
|466
AI Summary
This presentation discusses the physiological effects of altitude on respiratory system, partial pressure at Everest Base Camp, arterial pO2 & Hb saturation, physiological response to changes & HAPE, prevention & treatment. It also provides evidence and formulas to calculate alveolar partial pressure of Oxygen and oxygen content of arteria or CaO2. The subject is related to respiratory system and the course code, course name, and college/university are not mentioned.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: PHYSIOLOGICAL EFFECTS OF ALTITUDE ON RESPIRATORY SYSTEM
PHYSIOLOGICAL EFFECTS OF ALTITUDE ON RESPIRATORY SYSTEM
Name of the Student
Name of the University
Author Note
PHYSIOLOGICAL EFFECTS OF ALTITUDE ON RESPIRATORY SYSTEM
Name of the Student
Name of the University
Author Note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1PHYSIOLOGICAL EFFECTS OF ALTITUDE ON RESPIRATORY SYSTEM
Introduction
Everest Base Camp is located at an altitude of 5364m or 17,600ft above sea level, and
the atmospheric pressure at that altitude is 401 mmHg. The atmospheric pressure is far lower
than the pressure at sea level, which is 760mm. The physiological fluctuations, taking place
in the body while high-altitude trekking is known as acclimatisation (Smith et al., 2017). The
atmospheric pressure is higher at sea level because more number of air molecules are exerting
pressure downwards. However, with the increase in altitude, this pressure decreases and also
the number of oxygen molecules. To cope up with this environment, the body undergoes
various changes that will be discussed in this presentation along with calculative evidence.
Partial Pressure at Everest Base Camp
At higher altitude, the body undergoes physiological changes to be able to breathe in
thinner air with less oxygen. With an increase in vertical height, a non-linear decrease in
barometric pressure can be observed. The percentage of oxygen present in that altitude is
same, i.e. 21%. However, with the decrease in barometric pressure, which is 401mmHg, the
oxygen level decrease and it becomes 53% of the availability at sea level. To maintain the apt
amount of oxygen supply, the human body starts to breathe heavily and faster, along with the
heart pumping in more blood in the body.
The following formula can calculate the alveolar partial pressure of Oxygen:
PATO2 =(PAtm – PH2O) FiO2 – PaCO2/ RQ
Where PATO2 = Partial Pressure of Oxygen in the Alveoli
PAtm = Atmospheric Pressure
PH2O = Partial Pressure of water
FiO2 = Fraction of Inspired Oxygen
Introduction
Everest Base Camp is located at an altitude of 5364m or 17,600ft above sea level, and
the atmospheric pressure at that altitude is 401 mmHg. The atmospheric pressure is far lower
than the pressure at sea level, which is 760mm. The physiological fluctuations, taking place
in the body while high-altitude trekking is known as acclimatisation (Smith et al., 2017). The
atmospheric pressure is higher at sea level because more number of air molecules are exerting
pressure downwards. However, with the increase in altitude, this pressure decreases and also
the number of oxygen molecules. To cope up with this environment, the body undergoes
various changes that will be discussed in this presentation along with calculative evidence.
Partial Pressure at Everest Base Camp
At higher altitude, the body undergoes physiological changes to be able to breathe in
thinner air with less oxygen. With an increase in vertical height, a non-linear decrease in
barometric pressure can be observed. The percentage of oxygen present in that altitude is
same, i.e. 21%. However, with the decrease in barometric pressure, which is 401mmHg, the
oxygen level decrease and it becomes 53% of the availability at sea level. To maintain the apt
amount of oxygen supply, the human body starts to breathe heavily and faster, along with the
heart pumping in more blood in the body.
The following formula can calculate the alveolar partial pressure of Oxygen:
PATO2 =(PAtm – PH2O) FiO2 – PaCO2/ RQ
Where PATO2 = Partial Pressure of Oxygen in the Alveoli
PAtm = Atmospheric Pressure
PH2O = Partial Pressure of water
FiO2 = Fraction of Inspired Oxygen
2PHYSIOLOGICAL EFFECTS OF ALTITUDE ON RESPIRATORY SYSTEM
PaCO2 = Partial Pressure of Carbon Dioxide in the alveoli
RQ = Respiratory Quotient
Arterial pO2 & Hb Saturation
Alveolar ventilation (VA) increases with an increase in altitude. For sea level, VA does
increase because of mild hypoxia. The reason for this is anticipated to be the central
chemoreceptor inhibition and hypoxic peripheral chemoreceptor stimulation from reduced
cerebral partial pressure of CO2 annulling each other. Moreover, a central alkaline
environment is produced when CO2 is washed out due to delivery of cerebral oxygen in case
of arterial hypoxemia, stimulated by increased cerebral blood flow (Sarkar, Niranjan &
Banyal., 2017). However, during acclimatisation, this central response gets inhibited, and VA
increases for any given PaO2.
PaCO2 = Partial Pressure of Carbon Dioxide in the alveoli
RQ = Respiratory Quotient
Arterial pO2 & Hb Saturation
Alveolar ventilation (VA) increases with an increase in altitude. For sea level, VA does
increase because of mild hypoxia. The reason for this is anticipated to be the central
chemoreceptor inhibition and hypoxic peripheral chemoreceptor stimulation from reduced
cerebral partial pressure of CO2 annulling each other. Moreover, a central alkaline
environment is produced when CO2 is washed out due to delivery of cerebral oxygen in case
of arterial hypoxemia, stimulated by increased cerebral blood flow (Sarkar, Niranjan &
Banyal., 2017). However, during acclimatisation, this central response gets inhibited, and VA
increases for any given PaO2.
3PHYSIOLOGICAL EFFECTS OF ALTITUDE ON RESPIRATORY SYSTEM
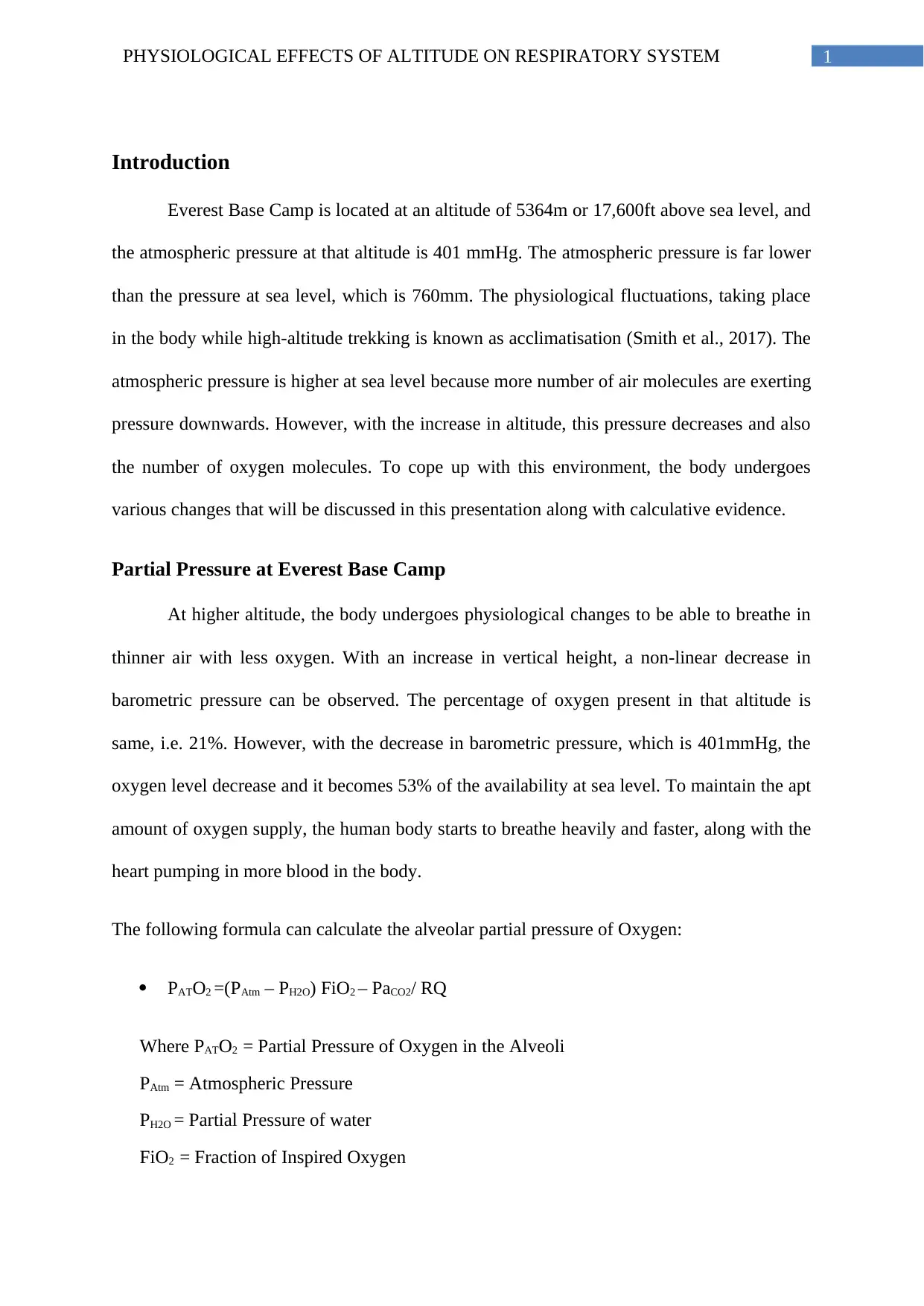
The following formula can calculate the oxygen content of arteria or CaO2.
CaO2 = (SaO2 x 1.34 x Hb x 0.01) + (0.023 x PaO2 in kPa),
Where, SaO2 = Arterial oxygen saturation (%)
1.34 = Huffner’s constant (milliliters of oxygen carried by 1 g of Hb in vivo)
Figure 1
Source: (Grocott et al., 2013)
The following formula can calculate the oxygen content of arteria or CaO2.
CaO2 = (SaO2 x 1.34 x Hb x 0.01) + (0.023 x PaO2 in kPa),
Where, SaO2 = Arterial oxygen saturation (%)
1.34 = Huffner’s constant (milliliters of oxygen carried by 1 g of Hb in vivo)
Figure 1
Source: (Grocott et al., 2013)
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4PHYSIOLOGICAL EFFECTS OF ALTITUDE ON RESPIRATORY SYSTEM
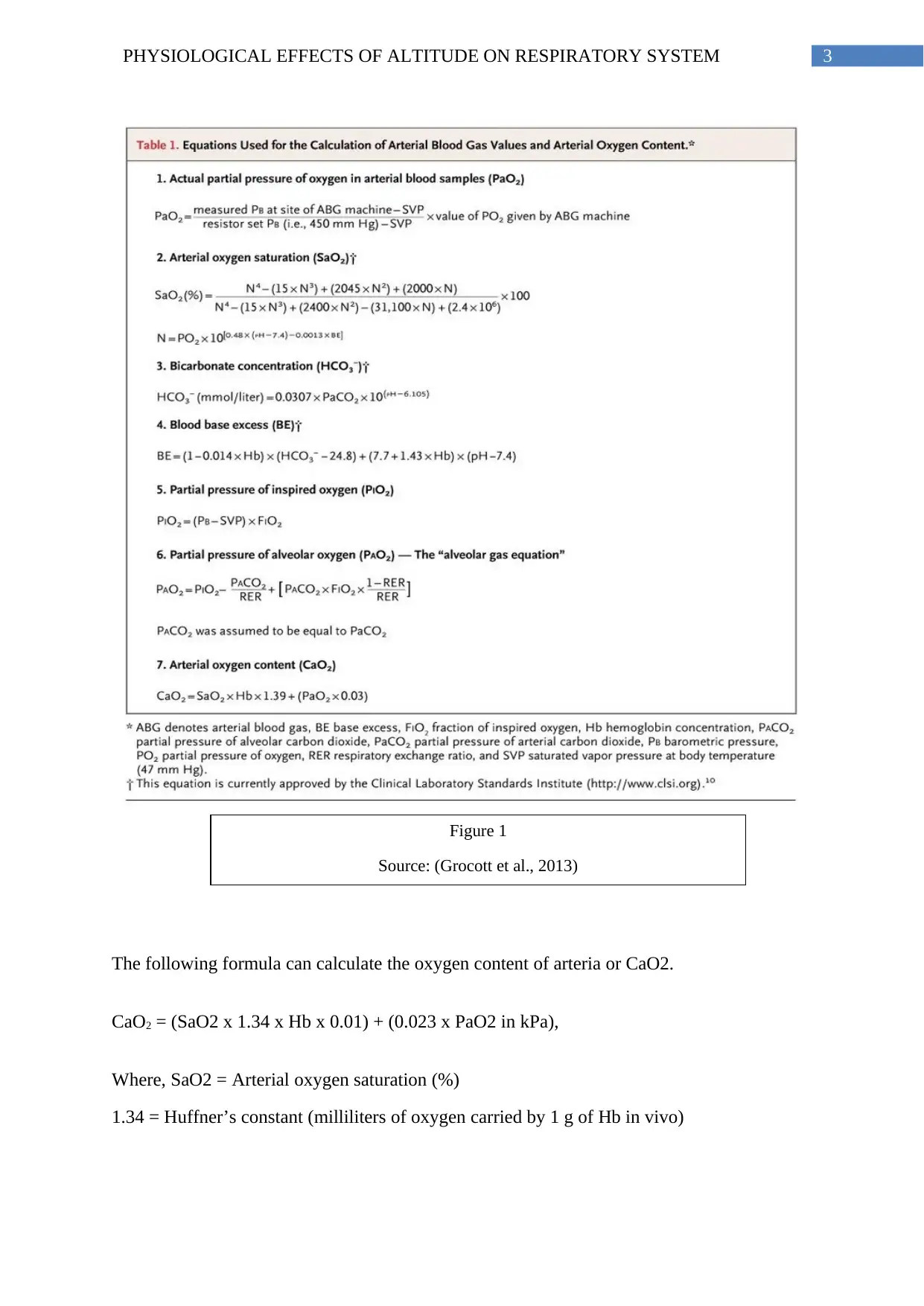
0.023 = solubility coefficient of oxygen
The mean partial arterial pressure of
O2 at the altitude of 5300m is 50±3 mmHg.
Haemoglobin saturation (SPO2) this arterial
pO2 is over 80% (Grocott et al., 2013).
Physiological Response To Changes & HAPE
The individuals need to allow sufficient time to let their bodies acclimatised or
otherwise would suffer from acute high-altitude illness (Casey et al., 2019). Faster breathing
is quite normal when the ascent is quick, however, breathlessness while resting mean that the
lungs are incapable of providing sufficient oxygen to the blood and indicates the development
of High Altitude Pulmonary Edema (HAPE).
Factors Causing HAPE
HAPE is a severe high-altitude sickness that can get fatal. HAPE is thought to occur
secondary to hypoxia and is a type of non-cardiogenic pulmonary edema (Jensen & Vincent.,
2018). Lowlanders trying to ascend to higher altitudes rapidly are the main population
suffering from HAPE. Following are the few factors causing HAPE:
Figure 2: Oxy–hemoglobin dissociation curve
Source: (Baumstark et al., 2019)
0.023 = solubility coefficient of oxygen
The mean partial arterial pressure of
O2 at the altitude of 5300m is 50±3 mmHg.
Haemoglobin saturation (SPO2) this arterial
pO2 is over 80% (Grocott et al., 2013).
Physiological Response To Changes & HAPE
The individuals need to allow sufficient time to let their bodies acclimatised or
otherwise would suffer from acute high-altitude illness (Casey et al., 2019). Faster breathing
is quite normal when the ascent is quick, however, breathlessness while resting mean that the
lungs are incapable of providing sufficient oxygen to the blood and indicates the development
of High Altitude Pulmonary Edema (HAPE).
Factors Causing HAPE
HAPE is a severe high-altitude sickness that can get fatal. HAPE is thought to occur
secondary to hypoxia and is a type of non-cardiogenic pulmonary edema (Jensen & Vincent.,
2018). Lowlanders trying to ascend to higher altitudes rapidly are the main population
suffering from HAPE. Following are the few factors causing HAPE:
Figure 2: Oxy–hemoglobin dissociation curve
Source: (Baumstark et al., 2019)
5PHYSIOLOGICAL EFFECTS OF ALTITUDE ON RESPIRATORY SYSTEM
Stress failure and leaks in capillary walls
Elevated pulmonary artery pressure
Elevated hypoxic pulmonary vasoconstriction
HAPE commonly occurs in two forms, among which the first form constitutes the lowlanders
with the un-acclimatized body, rapidly ascending and the other form occurs in highlanders
who rapidly descend to lowlands (Breitnauer et al., 2016). The latter is also known as re-entry
HAPE.
Pathophysiological Mechanism of HAPE
Pulmonary blood vessels gets constricted in reaction to hypoxia, in contrast to
systemic blood vessels, which dilates. Two major pathophysiological mechanisms are
accounting for pulmonary hypertension. First is regional over perfusion of capillaries in
zones of low arterial vasoconstriction caused by inhomogeneous pulmonary vasoconstriction.
Second is pulmonary vein level hypoxic constriction, which increases the resistance
downstream of fluid filtration region (Griva et al., 2017). To conclude the pathophysiological
mechanisms of HAPE, it can be stated that excessive hypoxic pulmonary vasoconstriction of
small veins and arteries leads to distension of vessel walls, which then opens up cellular
junctions and causes stress failure of alveolo-capillary membrane (Dunham-Snary et al.,
2017). Hypoxic ventilatory response, resting ventilation, oxygen saturation of arterial
hemoglobin and hemoglobin concentration are the four adaptations to overcome restraints of
high altitude hypoxia.
Signs of HAPE
While travelling to high altitude, the body will first experience minute ventilation,
which results in respiratory alkalosis. A shift to the left in the oxygen dissociation curve
(increased oxygen affinity by haemoglobin) can be observed post this. In response to this,
Stress failure and leaks in capillary walls
Elevated pulmonary artery pressure
Elevated hypoxic pulmonary vasoconstriction
HAPE commonly occurs in two forms, among which the first form constitutes the lowlanders
with the un-acclimatized body, rapidly ascending and the other form occurs in highlanders
who rapidly descend to lowlands (Breitnauer et al., 2016). The latter is also known as re-entry
HAPE.
Pathophysiological Mechanism of HAPE
Pulmonary blood vessels gets constricted in reaction to hypoxia, in contrast to
systemic blood vessels, which dilates. Two major pathophysiological mechanisms are
accounting for pulmonary hypertension. First is regional over perfusion of capillaries in
zones of low arterial vasoconstriction caused by inhomogeneous pulmonary vasoconstriction.
Second is pulmonary vein level hypoxic constriction, which increases the resistance
downstream of fluid filtration region (Griva et al., 2017). To conclude the pathophysiological
mechanisms of HAPE, it can be stated that excessive hypoxic pulmonary vasoconstriction of
small veins and arteries leads to distension of vessel walls, which then opens up cellular
junctions and causes stress failure of alveolo-capillary membrane (Dunham-Snary et al.,
2017). Hypoxic ventilatory response, resting ventilation, oxygen saturation of arterial
hemoglobin and hemoglobin concentration are the four adaptations to overcome restraints of
high altitude hypoxia.
Signs of HAPE
While travelling to high altitude, the body will first experience minute ventilation,
which results in respiratory alkalosis. A shift to the left in the oxygen dissociation curve
(increased oxygen affinity by haemoglobin) can be observed post this. In response to this,
6PHYSIOLOGICAL EFFECTS OF ALTITUDE ON RESPIRATORY SYSTEM
blood pH stabilization starts with the kidney rapidly increasing protein reabsorption. After
TBC 2,3-DPG levels start increasing, the Hgb-O2 dissociation curve shifts to the right
(decreased O2 affinity by hemoglobin) (Baumstark et al., 2019). This allows the stressed
tissues (due to trekking) to get more oxygen.
However, if HVR is blunted, it will lead to hypoxia and then cause escalated HPV. If
such conditions are left untreated, it will lead to dyspnea while resting, cyanosis, rales and
even prove to be fatal. The various signs that the trekkers should look out for are shortness of
breath while at rest, dyspnea, clammy skin, blue-tinged lips, a blood-tinged cough that has
frothy sputum and palpitations.
Prevention & Treatment
When signs of HAPE are recognized, one should stop their ascend uphill. Supplement
oxygenation and treatment with 20mg nifedipine, if medications are available. However, if
possible, the foremost priority should be a rapid descent. Slow ascend gives the body
appropriate time to acclimatize, Hence should always be kept in mind.
Conclusion
Hence, it can be concluded from the presentation that partial pressure of oxygen (pO2)
decreases with the increase in height. At the altitude of 5300m, where the Everest Base camp
is situated, only 53% of oxygen is present, compared to that in sea level. Acclimatization of
the body will occur to adapt with the changing altitude and environment. If the ability to
acclimatize fails, severe disorders like HAPE (High Altitude Pulmonary Edema) can occur.
Dyspnea, cyanosis and rales can develop if HAPE is left untreated. To prevent HAPE, one
has to gradually ascend and give proper time to the body to acclimatize. One has to stop
ascend and start descent if signs & symptoms of HAPE are confirmed.
blood pH stabilization starts with the kidney rapidly increasing protein reabsorption. After
TBC 2,3-DPG levels start increasing, the Hgb-O2 dissociation curve shifts to the right
(decreased O2 affinity by hemoglobin) (Baumstark et al., 2019). This allows the stressed
tissues (due to trekking) to get more oxygen.
However, if HVR is blunted, it will lead to hypoxia and then cause escalated HPV. If
such conditions are left untreated, it will lead to dyspnea while resting, cyanosis, rales and
even prove to be fatal. The various signs that the trekkers should look out for are shortness of
breath while at rest, dyspnea, clammy skin, blue-tinged lips, a blood-tinged cough that has
frothy sputum and palpitations.
Prevention & Treatment
When signs of HAPE are recognized, one should stop their ascend uphill. Supplement
oxygenation and treatment with 20mg nifedipine, if medications are available. However, if
possible, the foremost priority should be a rapid descent. Slow ascend gives the body
appropriate time to acclimatize, Hence should always be kept in mind.
Conclusion
Hence, it can be concluded from the presentation that partial pressure of oxygen (pO2)
decreases with the increase in height. At the altitude of 5300m, where the Everest Base camp
is situated, only 53% of oxygen is present, compared to that in sea level. Acclimatization of
the body will occur to adapt with the changing altitude and environment. If the ability to
acclimatize fails, severe disorders like HAPE (High Altitude Pulmonary Edema) can occur.
Dyspnea, cyanosis and rales can develop if HAPE is left untreated. To prevent HAPE, one
has to gradually ascend and give proper time to the body to acclimatize. One has to stop
ascend and start descent if signs & symptoms of HAPE are confirmed.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

7PHYSIOLOGICAL EFFECTS OF ALTITUDE ON RESPIRATORY SYSTEM
8PHYSIOLOGICAL EFFECTS OF ALTITUDE ON RESPIRATORY SYSTEM
References
Baumstark, A., Pleus, S., Jendrike, N., Liebing, C., Hinzmann, R., Haug, C., & Freckmann,
G. (2019). Proof of Concept Study to Assess the Influence of Oxygen Partial Pressure
in Capillary Blood on SMBG Measurements. Journal Of Diabetes Science And
Technology, 193229681983336. doi: 10.1177/1932296819833369
Breitnauer, N., Bush, D., Stillwell, P. C., & Carpenter, T. (2016). A Case Of Pulmonary
Edema At Moderate Altitude: Extending The Spectrum Of Hape?. In C62.
PEDIATRIC CASES I (pp. A5627-A5627). American Thoracic Society.
Casey, J., Janz, D., Russell, D., Vonderhaar, D., Joffe, A., & Dischert, K. (2019). Bag-Mask
Ventilation during Tracheal Intubation of Critically Ill Adults. New England Journal
Of Medicine, 380(9), 811-821. doi: 10.1056/nejmoa1812405
Dunham-Snary, K. J., Wu, D., Sykes, E. A., Thakrar, A., Parlow, L. R., Mewburn, J. D., ... &
Archer, S. L. (2017). Hypoxic pulmonary vasoconstriction: from molecular
mechanisms to medicine. Chest, 151(1), 181-192.
Griva, K., Stygall, J., Wilson, M. H., Martin, D., Levett, D., Mitchell, K., & Edsell, M.
(2017). Caudwell Xtreme Everest: A prospective study of the effects of environmental
hypoxia on cognitive functioning. PloS one, 12(3), e0174277.
Grocott, M., Martin, D., Levett, D., McMorrow, R., Windsor, J., & Montgomery, H. (2013).
Arterial Blood Gases and Oxygen Content in Climbers on Mount Everest. New
England Journal Of Medicine, 360(2), 140-149. doi: 10.1056/nejmoa0801581
Jensen, J. D., & Vincent, A. L. (2018). High Altitude Pulmonary Edema (HAPE).
In StatPearls [Internet]. StatPearls Publishing.
References
Baumstark, A., Pleus, S., Jendrike, N., Liebing, C., Hinzmann, R., Haug, C., & Freckmann,
G. (2019). Proof of Concept Study to Assess the Influence of Oxygen Partial Pressure
in Capillary Blood on SMBG Measurements. Journal Of Diabetes Science And
Technology, 193229681983336. doi: 10.1177/1932296819833369
Breitnauer, N., Bush, D., Stillwell, P. C., & Carpenter, T. (2016). A Case Of Pulmonary
Edema At Moderate Altitude: Extending The Spectrum Of Hape?. In C62.
PEDIATRIC CASES I (pp. A5627-A5627). American Thoracic Society.
Casey, J., Janz, D., Russell, D., Vonderhaar, D., Joffe, A., & Dischert, K. (2019). Bag-Mask
Ventilation during Tracheal Intubation of Critically Ill Adults. New England Journal
Of Medicine, 380(9), 811-821. doi: 10.1056/nejmoa1812405
Dunham-Snary, K. J., Wu, D., Sykes, E. A., Thakrar, A., Parlow, L. R., Mewburn, J. D., ... &
Archer, S. L. (2017). Hypoxic pulmonary vasoconstriction: from molecular
mechanisms to medicine. Chest, 151(1), 181-192.
Griva, K., Stygall, J., Wilson, M. H., Martin, D., Levett, D., Mitchell, K., & Edsell, M.
(2017). Caudwell Xtreme Everest: A prospective study of the effects of environmental
hypoxia on cognitive functioning. PloS one, 12(3), e0174277.
Grocott, M., Martin, D., Levett, D., McMorrow, R., Windsor, J., & Montgomery, H. (2013).
Arterial Blood Gases and Oxygen Content in Climbers on Mount Everest. New
England Journal Of Medicine, 360(2), 140-149. doi: 10.1056/nejmoa0801581
Jensen, J. D., & Vincent, A. L. (2018). High Altitude Pulmonary Edema (HAPE).
In StatPearls [Internet]. StatPearls Publishing.

9PHYSIOLOGICAL EFFECTS OF ALTITUDE ON RESPIRATORY SYSTEM
Sarkar, M., Niranjan, N., & Banyal, P. K. (2017). Mechanisms of hypoxemia. Lung India:
official organ of Indian Chest Society, 34(1), 47.
Smith, Z. M., Krizay, E., Sá, R. C., Li, E. T., Scadeng, M., Powell Jr, F. L., & Dubowitz, D.
J. (2017). Evidence from high-altitude acclimatization for an integrated
cerebrovascular and ventilatory hypercapnic response but different responses to
hypoxia. Journal of Applied Physiology, 123(6), 1477-1486.
Sarkar, M., Niranjan, N., & Banyal, P. K. (2017). Mechanisms of hypoxemia. Lung India:
official organ of Indian Chest Society, 34(1), 47.
Smith, Z. M., Krizay, E., Sá, R. C., Li, E. T., Scadeng, M., Powell Jr, F. L., & Dubowitz, D.
J. (2017). Evidence from high-altitude acclimatization for an integrated
cerebrovascular and ventilatory hypercapnic response but different responses to
hypoxia. Journal of Applied Physiology, 123(6), 1477-1486.
1 out of 10
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.
