NURS90092: Emergency Nursing 2 - Burn Injury Case Study Analysis
VerifiedAdded on 2023/06/09
|13
|3501
|311
Case Study
AI Summary
This case study comprehensively analyzes the pathophysiology, clinical signs, and immediate nursing care priorities for a patient with extensive burn injuries. It uses the ABCDE approach to outline the initial management in the emergency department, focusing on airway, breathing, circulation, disability, and exposure. The study details fluid resuscitation calculations based on the Parkland formula and Wallace Rule of Nines, along with ongoing nursing interventions to maintain oxygenation, ventilation, circulation, and thermoregulation. It also addresses potential early complications like acute respiratory failure and compartment syndrome, emphasizing the importance of continuous monitoring and timely interventions. This document is available on Desklib, a platform offering a wide range of study tools and resources for students.

Running Header: PHYSIOLOGY OF BURNS AND THE MANAGEMENT 1
PHYSIOLOGY OF BURNS AND THE MANAGEMENT
Student’s name
Institutional affiliation
Course name
Date
PHYSIOLOGY OF BURNS AND THE MANAGEMENT
Student’s name
Institutional affiliation
Course name
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
PHYSIOLOGY OF BURNS AND THE MANAGEMENT 2
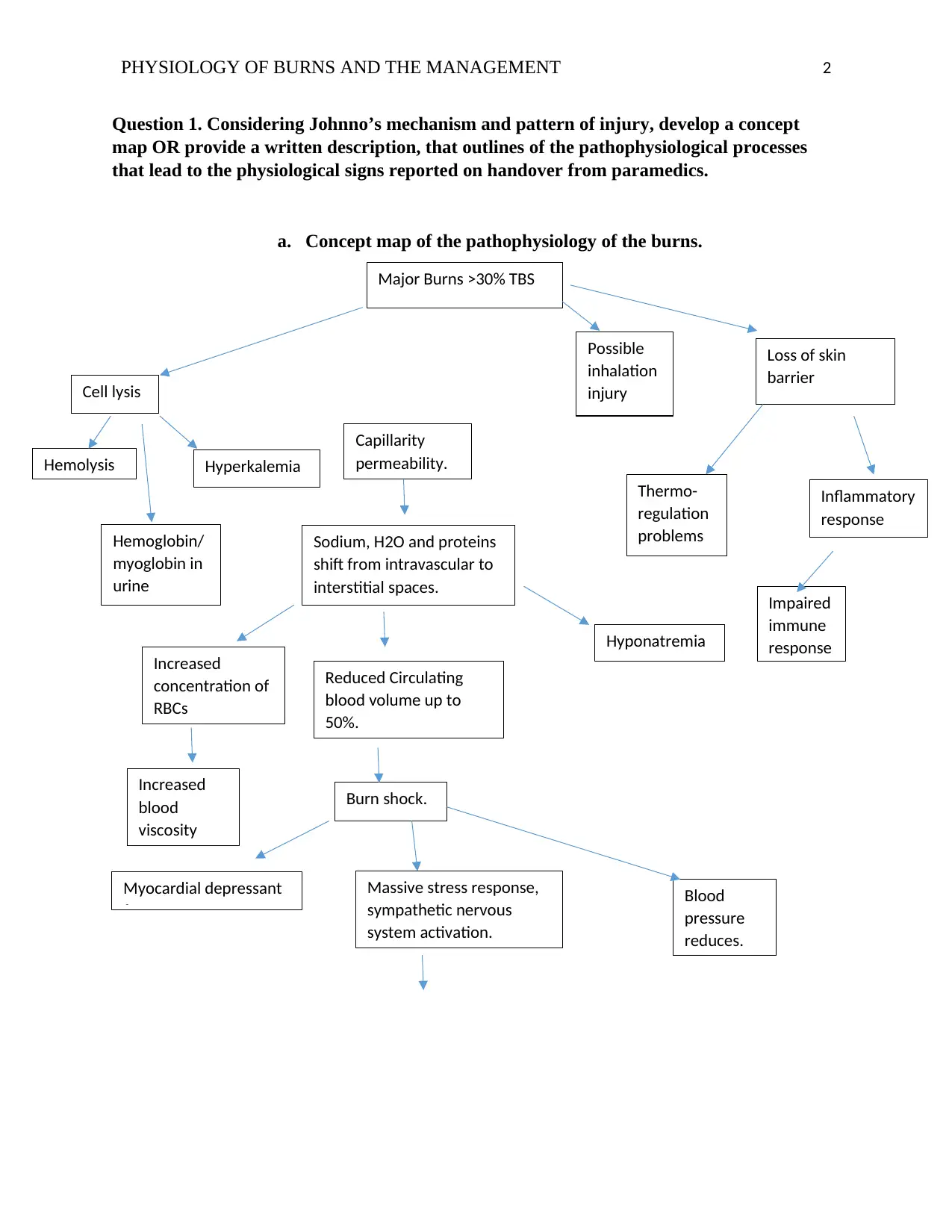
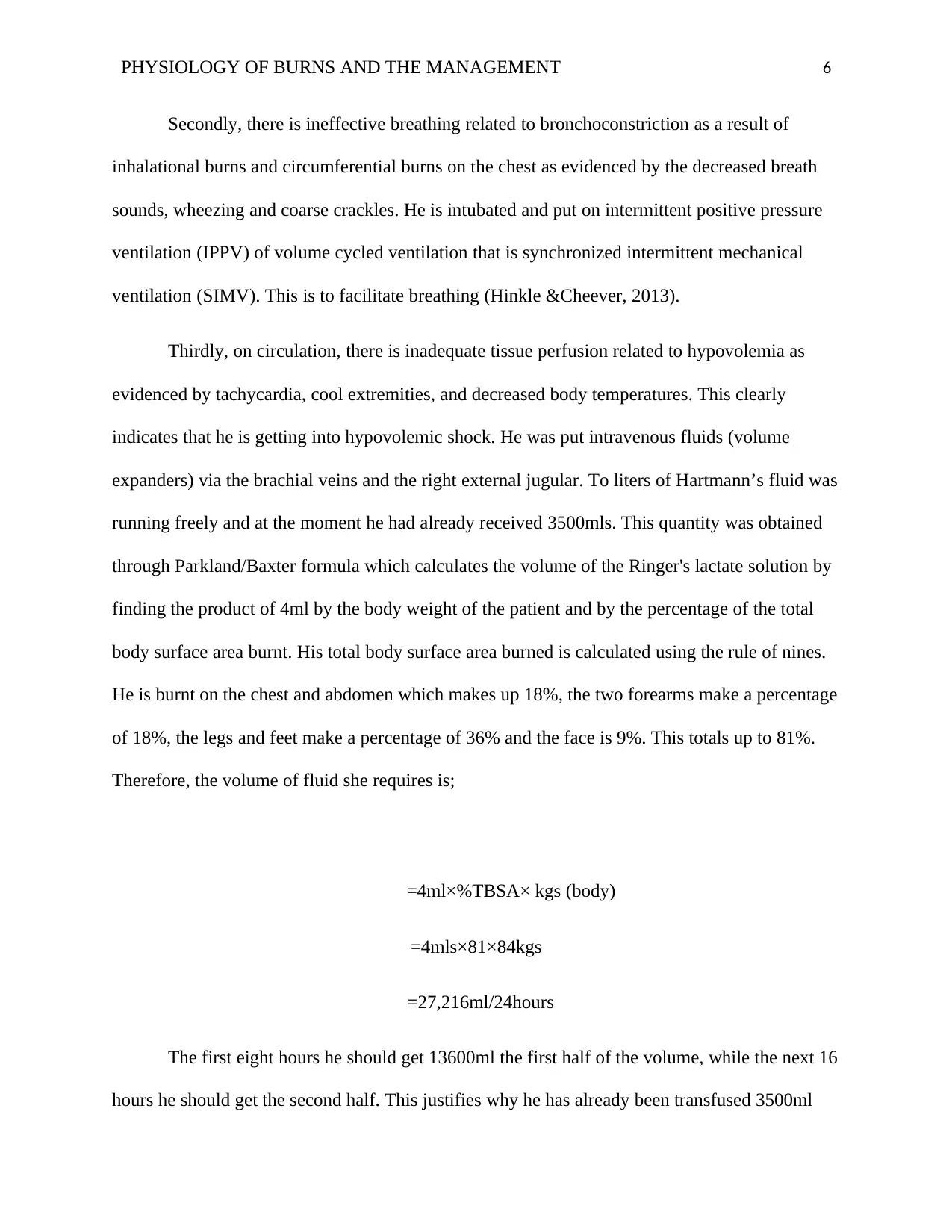
Question 1. Considering Johnno’s mechanism and pattern of injury, develop a concept
map OR provide a written description, that outlines of the pathophysiological processes
that lead to the physiological signs reported on handover from paramedics.
a. Concept map of the pathophysiology of the burns.
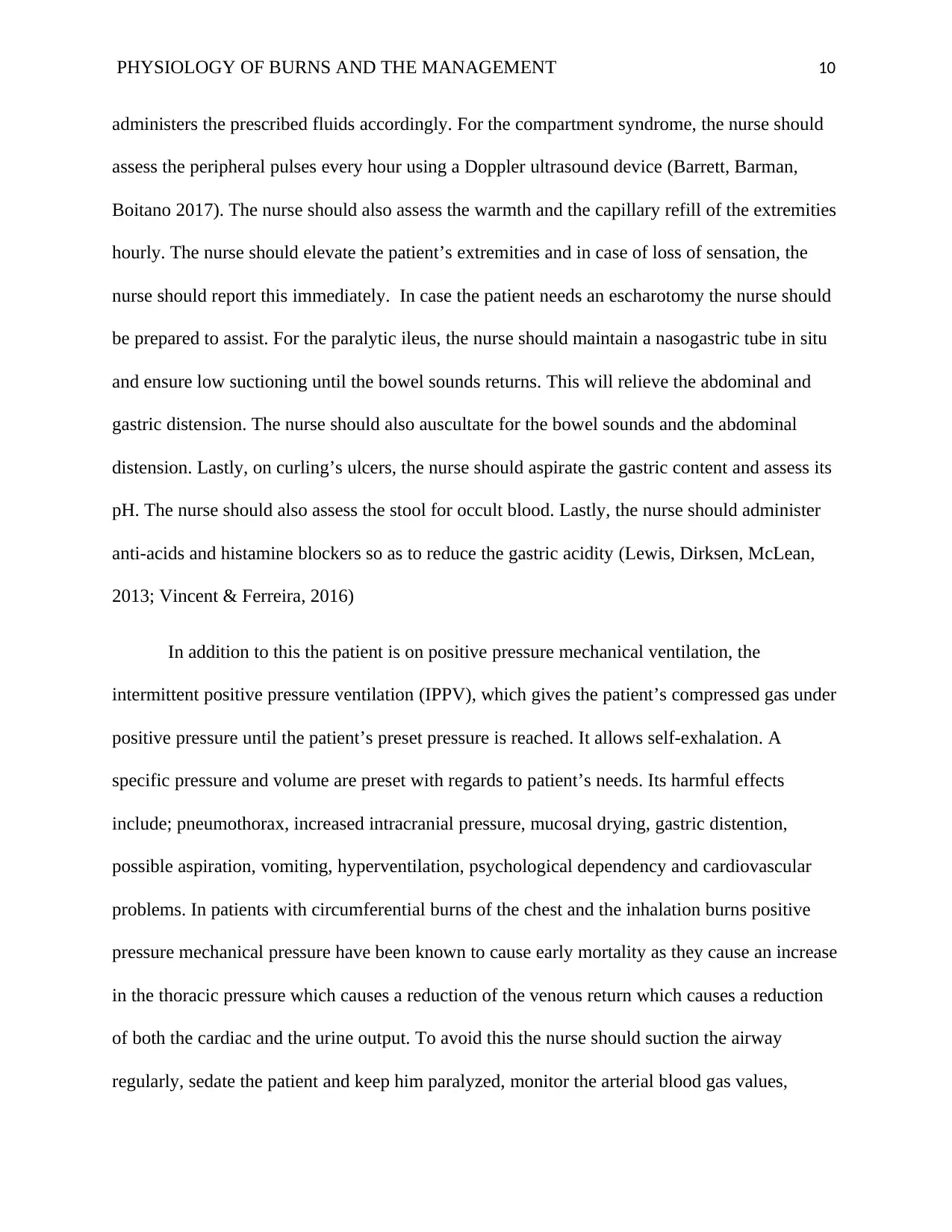
Major Burns >30% TBS
Cell lysis
Possible
inhalation
injury
Loss of skin
barrier
Capillarity
permeability.
Sodium, H2O and proteins
shift from intravascular to
interstitial spaces.
Reduced Circulating
blood volume up to
50%.
Burn shock.
Myocardial depressant
factor
Massive stress response,
sympathetic nervous
system activation.
Blood
pressure
reduces.
Hemolysis Hyperkalemia
Hemoglobin/
myoglobin in
urine
Increased
concentration of
RBCs
Increased
blood
viscosity
Hyponatremia
Thermo-
regulation
problems
Impaired
immune
response
Inflammatory
response
Question 1. Considering Johnno’s mechanism and pattern of injury, develop a concept
map OR provide a written description, that outlines of the pathophysiological processes
that lead to the physiological signs reported on handover from paramedics.
a. Concept map of the pathophysiology of the burns.
Major Burns >30% TBS
Cell lysis
Possible
inhalation
injury
Loss of skin
barrier
Capillarity
permeability.
Sodium, H2O and proteins
shift from intravascular to
interstitial spaces.
Reduced Circulating
blood volume up to
50%.
Burn shock.
Myocardial depressant
factor
Massive stress response,
sympathetic nervous
system activation.
Blood
pressure
reduces.
Hemolysis Hyperkalemia
Hemoglobin/
myoglobin in
urine
Increased
concentration of
RBCs
Increased
blood
viscosity
Hyponatremia
Thermo-
regulation
problems
Impaired
immune
response
Inflammatory
response
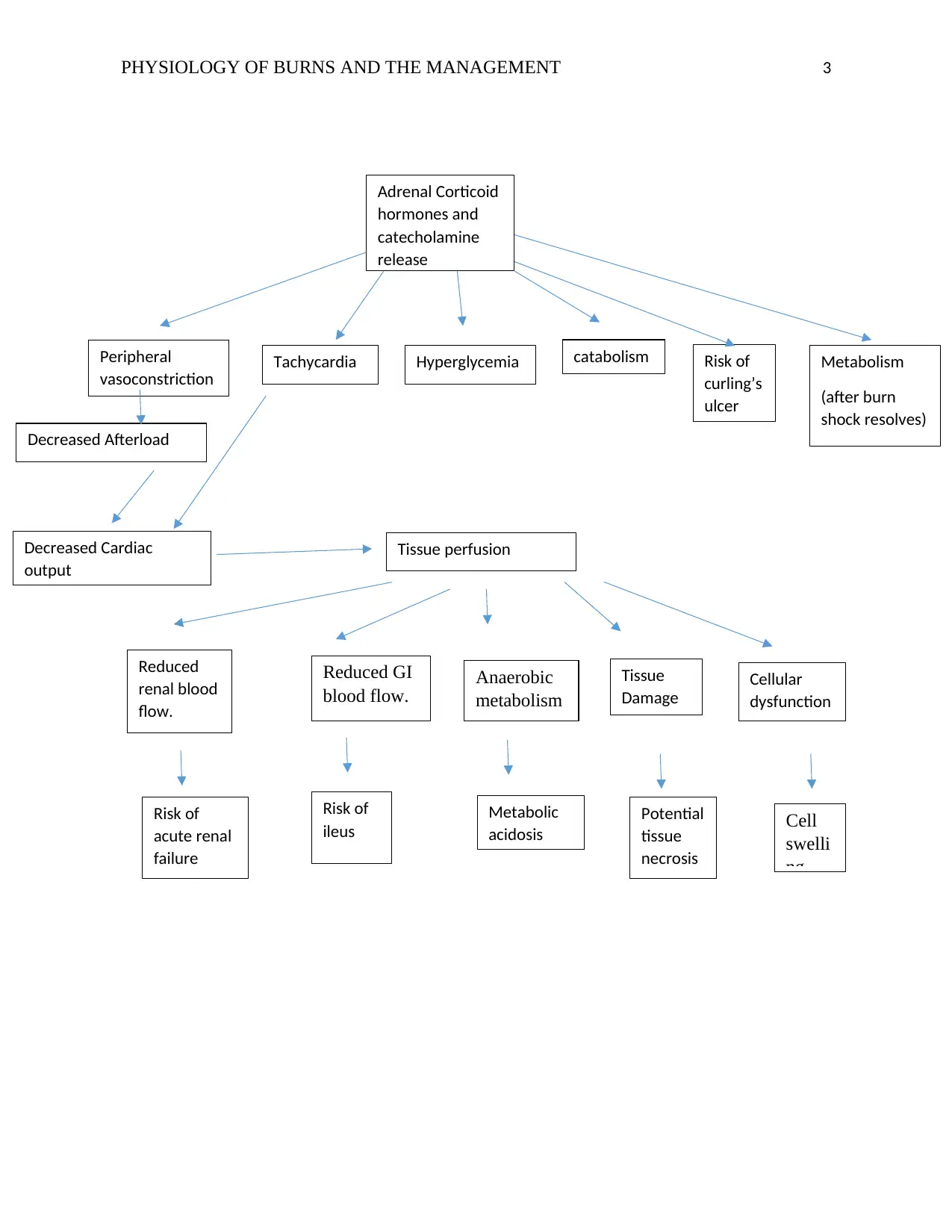
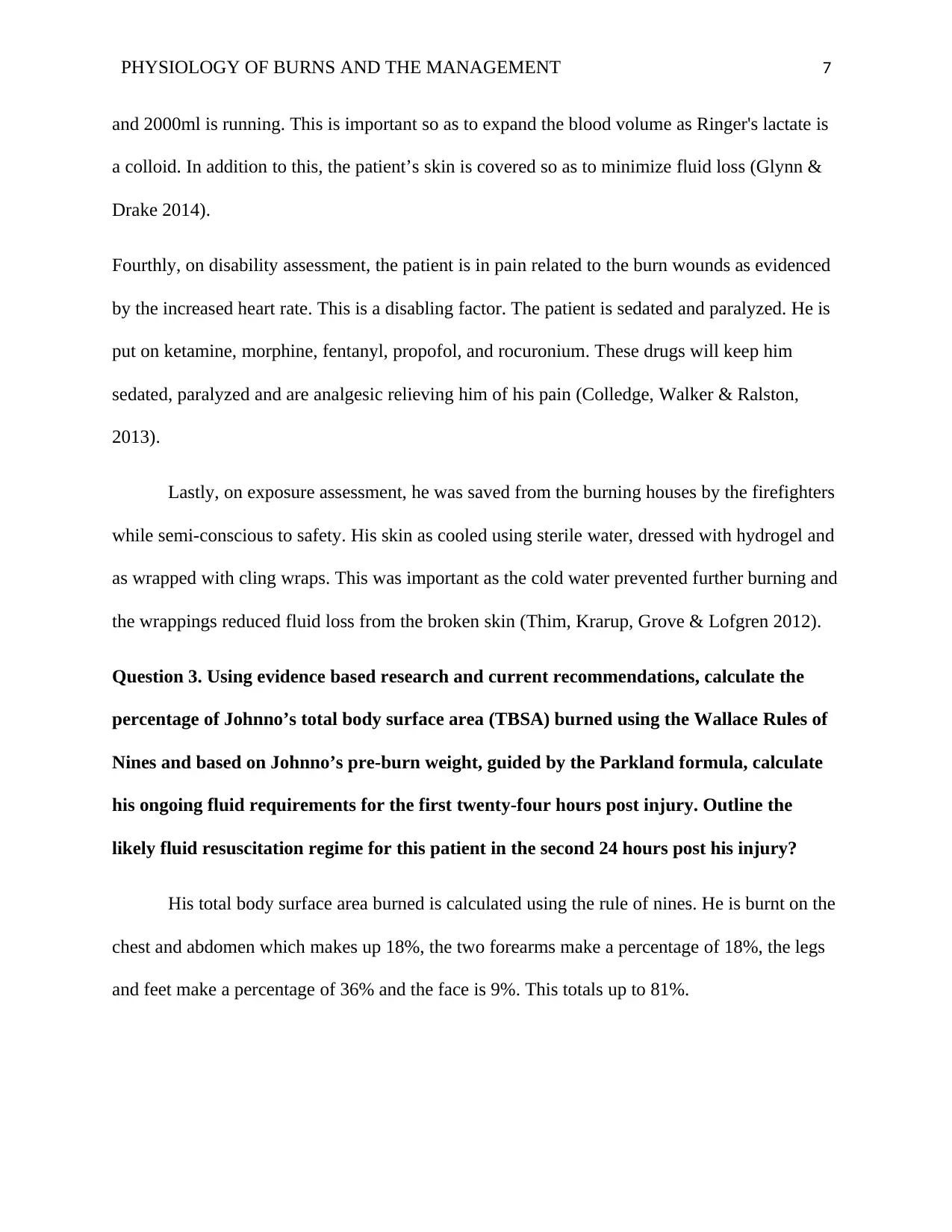
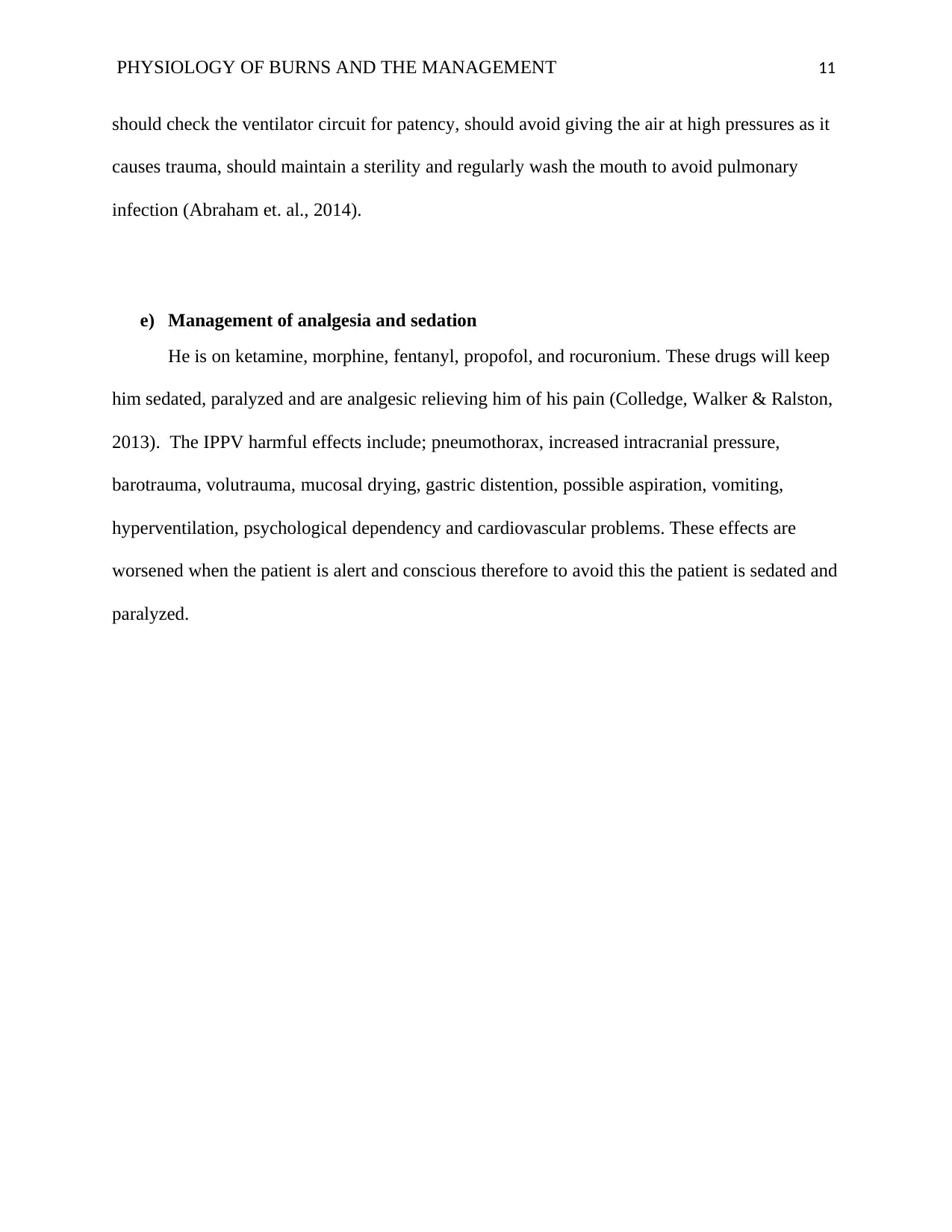
PHYSIOLOGY OF BURNS AND THE MANAGEMENT 3
Adrenal Corticoid
hormones and
catecholamine
release
Peripheral
vasoconstriction
.
Tachycardia Hyperglycemia catabolism Risk of
curling’s
ulcer
Metabolism
(after burn
shock resolves)
Decreased Afterload
Decreased Cardiac
output
Tissue perfusion
Reduced GI
blood flow.
Reduced
renal blood
flow.
Anaerobic
metabolism
Tissue
Damage
Cellular
dysfunction
Risk of
acute renal
failure
Risk of
ileus
Metabolic
acidosis
Potential
tissue
necrosis
Cell
swelli
ng
Adrenal Corticoid
hormones and
catecholamine
release
Peripheral
vasoconstriction
.
Tachycardia Hyperglycemia catabolism Risk of
curling’s
ulcer
Metabolism
(after burn
shock resolves)
Decreased Afterload
Decreased Cardiac
output
Tissue perfusion
Reduced GI
blood flow.
Reduced
renal blood
flow.
Anaerobic
metabolism
Tissue
Damage
Cellular
dysfunction
Risk of
acute renal
failure
Risk of
ileus
Metabolic
acidosis
Potential
tissue
necrosis
Cell
swelli
ng
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
PHYSIOLOGY OF BURNS AND THE MANAGEMENT 4
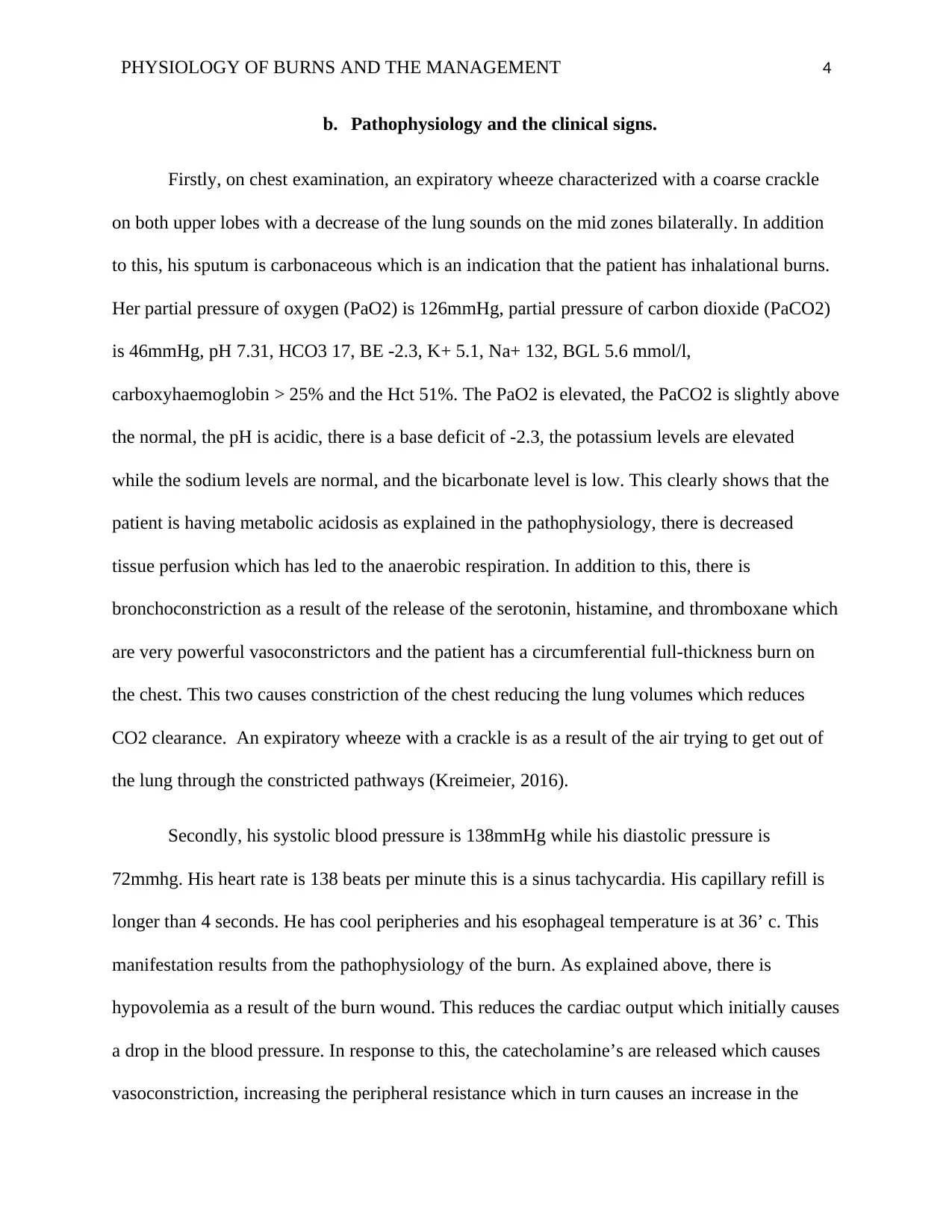
b. Pathophysiology and the clinical signs.
Firstly, on chest examination, an expiratory wheeze characterized with a coarse crackle
on both upper lobes with a decrease of the lung sounds on the mid zones bilaterally. In addition
to this, his sputum is carbonaceous which is an indication that the patient has inhalational burns.
Her partial pressure of oxygen (PaO2) is 126mmHg, partial pressure of carbon dioxide (PaCO2)
is 46mmHg, pH 7.31, HCO3 17, BE -2.3, K+ 5.1, Na+ 132, BGL 5.6 mmol/l,
carboxyhaemoglobin > 25% and the Hct 51%. The PaO2 is elevated, the PaCO2 is slightly above
the normal, the pH is acidic, there is a base deficit of -2.3, the potassium levels are elevated
while the sodium levels are normal, and the bicarbonate level is low. This clearly shows that the
patient is having metabolic acidosis as explained in the pathophysiology, there is decreased
tissue perfusion which has led to the anaerobic respiration. In addition to this, there is
bronchoconstriction as a result of the release of the serotonin, histamine, and thromboxane which
are very powerful vasoconstrictors and the patient has a circumferential full-thickness burn on
the chest. This two causes constriction of the chest reducing the lung volumes which reduces
CO2 clearance. An expiratory wheeze with a crackle is as a result of the air trying to get out of
the lung through the constricted pathways (Kreimeier, 2016).
Secondly, his systolic blood pressure is 138mmHg while his diastolic pressure is
72mmhg. His heart rate is 138 beats per minute this is a sinus tachycardia. His capillary refill is
longer than 4 seconds. He has cool peripheries and his esophageal temperature is at 36’ c. This
manifestation results from the pathophysiology of the burn. As explained above, there is
hypovolemia as a result of the burn wound. This reduces the cardiac output which initially causes
a drop in the blood pressure. In response to this, the catecholamine’s are released which causes
vasoconstriction, increasing the peripheral resistance which in turn causes an increase in the
b. Pathophysiology and the clinical signs.
Firstly, on chest examination, an expiratory wheeze characterized with a coarse crackle
on both upper lobes with a decrease of the lung sounds on the mid zones bilaterally. In addition
to this, his sputum is carbonaceous which is an indication that the patient has inhalational burns.
Her partial pressure of oxygen (PaO2) is 126mmHg, partial pressure of carbon dioxide (PaCO2)
is 46mmHg, pH 7.31, HCO3 17, BE -2.3, K+ 5.1, Na+ 132, BGL 5.6 mmol/l,
carboxyhaemoglobin > 25% and the Hct 51%. The PaO2 is elevated, the PaCO2 is slightly above
the normal, the pH is acidic, there is a base deficit of -2.3, the potassium levels are elevated
while the sodium levels are normal, and the bicarbonate level is low. This clearly shows that the
patient is having metabolic acidosis as explained in the pathophysiology, there is decreased
tissue perfusion which has led to the anaerobic respiration. In addition to this, there is
bronchoconstriction as a result of the release of the serotonin, histamine, and thromboxane which
are very powerful vasoconstrictors and the patient has a circumferential full-thickness burn on
the chest. This two causes constriction of the chest reducing the lung volumes which reduces
CO2 clearance. An expiratory wheeze with a crackle is as a result of the air trying to get out of
the lung through the constricted pathways (Kreimeier, 2016).
Secondly, his systolic blood pressure is 138mmHg while his diastolic pressure is
72mmhg. His heart rate is 138 beats per minute this is a sinus tachycardia. His capillary refill is
longer than 4 seconds. He has cool peripheries and his esophageal temperature is at 36’ c. This
manifestation results from the pathophysiology of the burn. As explained above, there is
hypovolemia as a result of the burn wound. This reduces the cardiac output which initially causes
a drop in the blood pressure. In response to this, the catecholamine’s are released which causes
vasoconstriction, increasing the peripheral resistance which in turn causes an increase in the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
PHYSIOLOGY OF BURNS AND THE MANAGEMENT 5
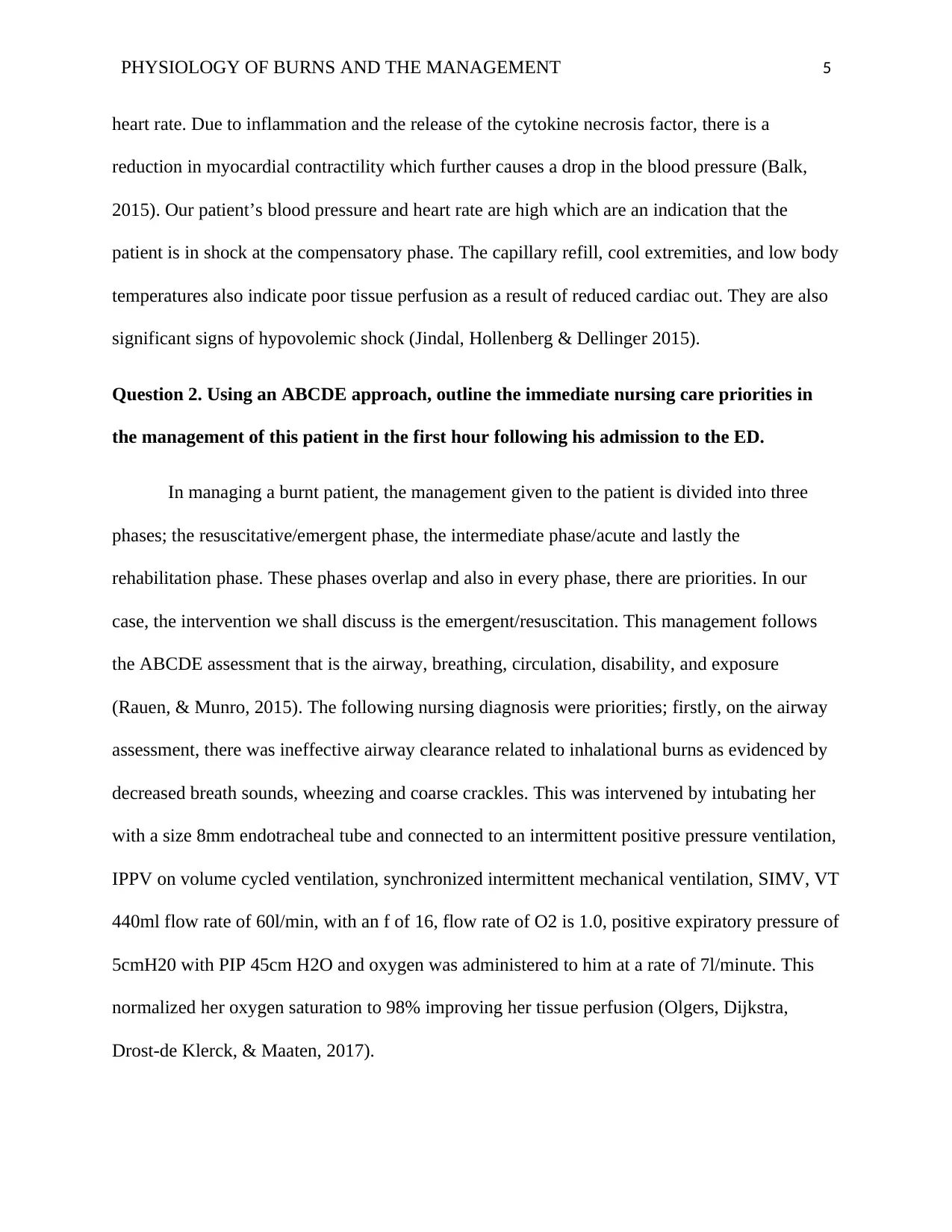
heart rate. Due to inflammation and the release of the cytokine necrosis factor, there is a
reduction in myocardial contractility which further causes a drop in the blood pressure (Balk,
2015). Our patient’s blood pressure and heart rate are high which are an indication that the
patient is in shock at the compensatory phase. The capillary refill, cool extremities, and low body
temperatures also indicate poor tissue perfusion as a result of reduced cardiac out. They are also
significant signs of hypovolemic shock (Jindal, Hollenberg & Dellinger 2015).
Question 2. Using an ABCDE approach, outline the immediate nursing care priorities in
the management of this patient in the first hour following his admission to the ED.
In managing a burnt patient, the management given to the patient is divided into three
phases; the resuscitative/emergent phase, the intermediate phase/acute and lastly the
rehabilitation phase. These phases overlap and also in every phase, there are priorities. In our
case, the intervention we shall discuss is the emergent/resuscitation. This management follows
the ABCDE assessment that is the airway, breathing, circulation, disability, and exposure
(Rauen, & Munro, 2015). The following nursing diagnosis were priorities; firstly, on the airway
assessment, there was ineffective airway clearance related to inhalational burns as evidenced by
decreased breath sounds, wheezing and coarse crackles. This was intervened by intubating her
with a size 8mm endotracheal tube and connected to an intermittent positive pressure ventilation,
IPPV on volume cycled ventilation, synchronized intermittent mechanical ventilation, SIMV, VT
440ml flow rate of 60l/min, with an f of 16, flow rate of O2 is 1.0, positive expiratory pressure of
5cmH20 with PIP 45cm H2O and oxygen was administered to him at a rate of 7l/minute. This
normalized her oxygen saturation to 98% improving her tissue perfusion (Olgers, Dijkstra,
Drost-de Klerck, & Maaten, 2017).
heart rate. Due to inflammation and the release of the cytokine necrosis factor, there is a
reduction in myocardial contractility which further causes a drop in the blood pressure (Balk,
2015). Our patient’s blood pressure and heart rate are high which are an indication that the
patient is in shock at the compensatory phase. The capillary refill, cool extremities, and low body
temperatures also indicate poor tissue perfusion as a result of reduced cardiac out. They are also
significant signs of hypovolemic shock (Jindal, Hollenberg & Dellinger 2015).
Question 2. Using an ABCDE approach, outline the immediate nursing care priorities in
the management of this patient in the first hour following his admission to the ED.
In managing a burnt patient, the management given to the patient is divided into three
phases; the resuscitative/emergent phase, the intermediate phase/acute and lastly the
rehabilitation phase. These phases overlap and also in every phase, there are priorities. In our
case, the intervention we shall discuss is the emergent/resuscitation. This management follows
the ABCDE assessment that is the airway, breathing, circulation, disability, and exposure
(Rauen, & Munro, 2015). The following nursing diagnosis were priorities; firstly, on the airway
assessment, there was ineffective airway clearance related to inhalational burns as evidenced by
decreased breath sounds, wheezing and coarse crackles. This was intervened by intubating her
with a size 8mm endotracheal tube and connected to an intermittent positive pressure ventilation,
IPPV on volume cycled ventilation, synchronized intermittent mechanical ventilation, SIMV, VT
440ml flow rate of 60l/min, with an f of 16, flow rate of O2 is 1.0, positive expiratory pressure of
5cmH20 with PIP 45cm H2O and oxygen was administered to him at a rate of 7l/minute. This
normalized her oxygen saturation to 98% improving her tissue perfusion (Olgers, Dijkstra,
Drost-de Klerck, & Maaten, 2017).
PHYSIOLOGY OF BURNS AND THE MANAGEMENT 6
Secondly, there is ineffective breathing related to bronchoconstriction as a result of
inhalational burns and circumferential burns on the chest as evidenced by the decreased breath
sounds, wheezing and coarse crackles. He is intubated and put on intermittent positive pressure
ventilation (IPPV) of volume cycled ventilation that is synchronized intermittent mechanical
ventilation (SIMV). This is to facilitate breathing (Hinkle &Cheever, 2013).
Thirdly, on circulation, there is inadequate tissue perfusion related to hypovolemia as
evidenced by tachycardia, cool extremities, and decreased body temperatures. This clearly
indicates that he is getting into hypovolemic shock. He was put intravenous fluids (volume
expanders) via the brachial veins and the right external jugular. To liters of Hartmann’s fluid was
running freely and at the moment he had already received 3500mls. This quantity was obtained
through Parkland/Baxter formula which calculates the volume of the Ringer's lactate solution by
finding the product of 4ml by the body weight of the patient and by the percentage of the total
body surface area burnt. His total body surface area burned is calculated using the rule of nines.
He is burnt on the chest and abdomen which makes up 18%, the two forearms make a percentage
of 18%, the legs and feet make a percentage of 36% and the face is 9%. This totals up to 81%.
Therefore, the volume of fluid she requires is;
=4ml×%TBSA× kgs (body)
=4mls×81×84kgs
=27,216ml/24hours
The first eight hours he should get 13600ml the first half of the volume, while the next 16
hours he should get the second half. This justifies why he has already been transfused 3500ml
Secondly, there is ineffective breathing related to bronchoconstriction as a result of
inhalational burns and circumferential burns on the chest as evidenced by the decreased breath
sounds, wheezing and coarse crackles. He is intubated and put on intermittent positive pressure
ventilation (IPPV) of volume cycled ventilation that is synchronized intermittent mechanical
ventilation (SIMV). This is to facilitate breathing (Hinkle &Cheever, 2013).
Thirdly, on circulation, there is inadequate tissue perfusion related to hypovolemia as
evidenced by tachycardia, cool extremities, and decreased body temperatures. This clearly
indicates that he is getting into hypovolemic shock. He was put intravenous fluids (volume
expanders) via the brachial veins and the right external jugular. To liters of Hartmann’s fluid was
running freely and at the moment he had already received 3500mls. This quantity was obtained
through Parkland/Baxter formula which calculates the volume of the Ringer's lactate solution by
finding the product of 4ml by the body weight of the patient and by the percentage of the total
body surface area burnt. His total body surface area burned is calculated using the rule of nines.
He is burnt on the chest and abdomen which makes up 18%, the two forearms make a percentage
of 18%, the legs and feet make a percentage of 36% and the face is 9%. This totals up to 81%.
Therefore, the volume of fluid she requires is;
=4ml×%TBSA× kgs (body)
=4mls×81×84kgs
=27,216ml/24hours
The first eight hours he should get 13600ml the first half of the volume, while the next 16
hours he should get the second half. This justifies why he has already been transfused 3500ml
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
PHYSIOLOGY OF BURNS AND THE MANAGEMENT 7
and 2000ml is running. This is important so as to expand the blood volume as Ringer's lactate is
a colloid. In addition to this, the patient’s skin is covered so as to minimize fluid loss (Glynn &
Drake 2014).
Fourthly, on disability assessment, the patient is in pain related to the burn wounds as evidenced
by the increased heart rate. This is a disabling factor. The patient is sedated and paralyzed. He is
put on ketamine, morphine, fentanyl, propofol, and rocuronium. These drugs will keep him
sedated, paralyzed and are analgesic relieving him of his pain (Colledge, Walker & Ralston,
2013).
Lastly, on exposure assessment, he was saved from the burning houses by the firefighters
while semi-conscious to safety. His skin as cooled using sterile water, dressed with hydrogel and
as wrapped with cling wraps. This was important as the cold water prevented further burning and
the wrappings reduced fluid loss from the broken skin (Thim, Krarup, Grove & Lofgren 2012).
Question 3. Using evidence based research and current recommendations, calculate the
percentage of Johnno’s total body surface area (TBSA) burned using the Wallace Rules of
Nines and based on Johnno’s pre-burn weight, guided by the Parkland formula, calculate
his ongoing fluid requirements for the first twenty-four hours post injury. Outline the
likely fluid resuscitation regime for this patient in the second 24 hours post his injury?
His total body surface area burned is calculated using the rule of nines. He is burnt on the
chest and abdomen which makes up 18%, the two forearms make a percentage of 18%, the legs
and feet make a percentage of 36% and the face is 9%. This totals up to 81%.
and 2000ml is running. This is important so as to expand the blood volume as Ringer's lactate is
a colloid. In addition to this, the patient’s skin is covered so as to minimize fluid loss (Glynn &
Drake 2014).
Fourthly, on disability assessment, the patient is in pain related to the burn wounds as evidenced
by the increased heart rate. This is a disabling factor. The patient is sedated and paralyzed. He is
put on ketamine, morphine, fentanyl, propofol, and rocuronium. These drugs will keep him
sedated, paralyzed and are analgesic relieving him of his pain (Colledge, Walker & Ralston,
2013).
Lastly, on exposure assessment, he was saved from the burning houses by the firefighters
while semi-conscious to safety. His skin as cooled using sterile water, dressed with hydrogel and
as wrapped with cling wraps. This was important as the cold water prevented further burning and
the wrappings reduced fluid loss from the broken skin (Thim, Krarup, Grove & Lofgren 2012).
Question 3. Using evidence based research and current recommendations, calculate the
percentage of Johnno’s total body surface area (TBSA) burned using the Wallace Rules of
Nines and based on Johnno’s pre-burn weight, guided by the Parkland formula, calculate
his ongoing fluid requirements for the first twenty-four hours post injury. Outline the
likely fluid resuscitation regime for this patient in the second 24 hours post his injury?
His total body surface area burned is calculated using the rule of nines. He is burnt on the
chest and abdomen which makes up 18%, the two forearms make a percentage of 18%, the legs
and feet make a percentage of 36% and the face is 9%. This totals up to 81%.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
PHYSIOLOGY OF BURNS AND THE MANAGEMENT 8
Therefore, the volume of fluid she requires using the parkland’s formula will be;
=4ml×%TBSA× kgs (body)
=4mls×81×84kgs
=27,216ml/24hours
The first eight hours he should get 13600ml, that is, the first half of the volume, while the next
16 hours he should get the second half. This justifies why he has already been transfused 3500ml
and 2000ml is running.
Question 4: Outline the ongoing nursing care you would implement to manage him in
relation to:
a) Maintain adequate oxygenation and ventilation.
The emergency department nurse places very vital roles, firstly, he/she assesses and
maintains adequate oxygenation and ventilation. The nurse does this by providing the patient
with humidified oxygen, constantly assesses his breath sounds, the respiratory rate, depth,
rhythm and symmetry and looks out for signs of hypoxia, monitors the arterial blood gas values,
carboxyhaemoglobin levels and the pulse oximetry, monitors the patient closely on the
mechanical ventilator and adjusts it accordingly for example in case of decreased oxygenation
this can be adjusted by increasing the tidal volume and flow rate given per minute. In addition to
this, the nurse should ensure that the patient is positioned properly so as to maintain a patent
airway and also suctioning should be done so as to clear the airway (Beck, 2015).
b) Maintain adequate circulation.
Therefore, the volume of fluid she requires using the parkland’s formula will be;
=4ml×%TBSA× kgs (body)
=4mls×81×84kgs
=27,216ml/24hours
The first eight hours he should get 13600ml, that is, the first half of the volume, while the next
16 hours he should get the second half. This justifies why he has already been transfused 3500ml
and 2000ml is running.
Question 4: Outline the ongoing nursing care you would implement to manage him in
relation to:
a) Maintain adequate oxygenation and ventilation.
The emergency department nurse places very vital roles, firstly, he/she assesses and
maintains adequate oxygenation and ventilation. The nurse does this by providing the patient
with humidified oxygen, constantly assesses his breath sounds, the respiratory rate, depth,
rhythm and symmetry and looks out for signs of hypoxia, monitors the arterial blood gas values,
carboxyhaemoglobin levels and the pulse oximetry, monitors the patient closely on the
mechanical ventilator and adjusts it accordingly for example in case of decreased oxygenation
this can be adjusted by increasing the tidal volume and flow rate given per minute. In addition to
this, the nurse should ensure that the patient is positioned properly so as to maintain a patent
airway and also suctioning should be done so as to clear the airway (Beck, 2015).
b) Maintain adequate circulation.
PHYSIOLOGY OF BURNS AND THE MANAGEMENT 9
Secondly, on circulation assessment so as to maintain adequate circulation the nurse should
constantly observe the patient’s vital signs that is the central venous pressure, the pulmonary
artery pressure, the urine output hourly, signs for hypovolemia or the signs of fluid overload as
he is on intravenous fluids. Should maintain the intravenous lines and regulate/monitor the fluids
to be given at the prescribed rates. Should observe the signs of increased or decreased sodium,
potassium, calcium, phosphorous and the bicarbonates. Should also elevate the patient’s head
and the extremities that are burnt. Lastly, on circulation, in case of any changes on the urine
output, the blood pressure and pulse rates/heart rate the physician should be notified immediately
by the nurse (Kumar, Haery & Parrillo 2015).
c) Maintain thermoregulation.
Thirdly, on managing the thermoregulation, the nurse should ensure the patient is kept in a
warm environment by using a heat shield, heat lights, space blankets or blankets. This will aid in
minimizing the heat loss via evaporation. The nurse should work quickly in the event of wound
exposure. This will ensure that there is minimal exposure, therefore, minimizing the heat loss.
Lastly, the nurse should frequently assess the core body temperature of the patient so as to detect
signs of hypovolemia early (Choi, Yip, Quinonez & Cook, 2014).
d) Managing potential early complication as a result of the burn injury.
This patient is at the risk of getting into acute respiratory failure, acute renal failure,
distributive shock, curling’s ulcer, paralytic ileus and compartment syndrome. To avoid this, the
nurse should monitor the patient’s respiration closely, the oxygen saturation, partial pressure of
oxygen, the partial pressure of carbon dioxide. For the renal function, the nurse should monitor
the urine output, the creatinine levels, the blood urea nitrogen. She should also ensure that she
Secondly, on circulation assessment so as to maintain adequate circulation the nurse should
constantly observe the patient’s vital signs that is the central venous pressure, the pulmonary
artery pressure, the urine output hourly, signs for hypovolemia or the signs of fluid overload as
he is on intravenous fluids. Should maintain the intravenous lines and regulate/monitor the fluids
to be given at the prescribed rates. Should observe the signs of increased or decreased sodium,
potassium, calcium, phosphorous and the bicarbonates. Should also elevate the patient’s head
and the extremities that are burnt. Lastly, on circulation, in case of any changes on the urine
output, the blood pressure and pulse rates/heart rate the physician should be notified immediately
by the nurse (Kumar, Haery & Parrillo 2015).
c) Maintain thermoregulation.
Thirdly, on managing the thermoregulation, the nurse should ensure the patient is kept in a
warm environment by using a heat shield, heat lights, space blankets or blankets. This will aid in
minimizing the heat loss via evaporation. The nurse should work quickly in the event of wound
exposure. This will ensure that there is minimal exposure, therefore, minimizing the heat loss.
Lastly, the nurse should frequently assess the core body temperature of the patient so as to detect
signs of hypovolemia early (Choi, Yip, Quinonez & Cook, 2014).
d) Managing potential early complication as a result of the burn injury.
This patient is at the risk of getting into acute respiratory failure, acute renal failure,
distributive shock, curling’s ulcer, paralytic ileus and compartment syndrome. To avoid this, the
nurse should monitor the patient’s respiration closely, the oxygen saturation, partial pressure of
oxygen, the partial pressure of carbon dioxide. For the renal function, the nurse should monitor
the urine output, the creatinine levels, the blood urea nitrogen. She should also ensure that she
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
PHYSIOLOGY OF BURNS AND THE MANAGEMENT 10
administers the prescribed fluids accordingly. For the compartment syndrome, the nurse should
assess the peripheral pulses every hour using a Doppler ultrasound device (Barrett, Barman,
Boitano 2017). The nurse should also assess the warmth and the capillary refill of the extremities
hourly. The nurse should elevate the patient’s extremities and in case of loss of sensation, the
nurse should report this immediately. In case the patient needs an escharotomy the nurse should
be prepared to assist. For the paralytic ileus, the nurse should maintain a nasogastric tube in situ
and ensure low suctioning until the bowel sounds returns. This will relieve the abdominal and
gastric distension. The nurse should also auscultate for the bowel sounds and the abdominal
distension. Lastly, on curling’s ulcers, the nurse should aspirate the gastric content and assess its
pH. The nurse should also assess the stool for occult blood. Lastly, the nurse should administer
anti-acids and histamine blockers so as to reduce the gastric acidity (Lewis, Dirksen, McLean,
2013; Vincent & Ferreira, 2016)
In addition to this the patient is on positive pressure mechanical ventilation, the
intermittent positive pressure ventilation (IPPV), which gives the patient’s compressed gas under
positive pressure until the patient’s preset pressure is reached. It allows self-exhalation. A
specific pressure and volume are preset with regards to patient’s needs. Its harmful effects
include; pneumothorax, increased intracranial pressure, mucosal drying, gastric distention,
possible aspiration, vomiting, hyperventilation, psychological dependency and cardiovascular
problems. In patients with circumferential burns of the chest and the inhalation burns positive
pressure mechanical pressure have been known to cause early mortality as they cause an increase
in the thoracic pressure which causes a reduction of the venous return which causes a reduction
of both the cardiac and the urine output. To avoid this the nurse should suction the airway
regularly, sedate the patient and keep him paralyzed, monitor the arterial blood gas values,
administers the prescribed fluids accordingly. For the compartment syndrome, the nurse should
assess the peripheral pulses every hour using a Doppler ultrasound device (Barrett, Barman,
Boitano 2017). The nurse should also assess the warmth and the capillary refill of the extremities
hourly. The nurse should elevate the patient’s extremities and in case of loss of sensation, the
nurse should report this immediately. In case the patient needs an escharotomy the nurse should
be prepared to assist. For the paralytic ileus, the nurse should maintain a nasogastric tube in situ
and ensure low suctioning until the bowel sounds returns. This will relieve the abdominal and
gastric distension. The nurse should also auscultate for the bowel sounds and the abdominal
distension. Lastly, on curling’s ulcers, the nurse should aspirate the gastric content and assess its
pH. The nurse should also assess the stool for occult blood. Lastly, the nurse should administer
anti-acids and histamine blockers so as to reduce the gastric acidity (Lewis, Dirksen, McLean,
2013; Vincent & Ferreira, 2016)
In addition to this the patient is on positive pressure mechanical ventilation, the
intermittent positive pressure ventilation (IPPV), which gives the patient’s compressed gas under
positive pressure until the patient’s preset pressure is reached. It allows self-exhalation. A
specific pressure and volume are preset with regards to patient’s needs. Its harmful effects
include; pneumothorax, increased intracranial pressure, mucosal drying, gastric distention,
possible aspiration, vomiting, hyperventilation, psychological dependency and cardiovascular
problems. In patients with circumferential burns of the chest and the inhalation burns positive
pressure mechanical pressure have been known to cause early mortality as they cause an increase
in the thoracic pressure which causes a reduction of the venous return which causes a reduction
of both the cardiac and the urine output. To avoid this the nurse should suction the airway
regularly, sedate the patient and keep him paralyzed, monitor the arterial blood gas values,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
PHYSIOLOGY OF BURNS AND THE MANAGEMENT 11
should check the ventilator circuit for patency, should avoid giving the air at high pressures as it
causes trauma, should maintain a sterility and regularly wash the mouth to avoid pulmonary
infection (Abraham et. al., 2014).
e) Management of analgesia and sedation
He is on ketamine, morphine, fentanyl, propofol, and rocuronium. These drugs will keep
him sedated, paralyzed and are analgesic relieving him of his pain (Colledge, Walker & Ralston,
2013). The IPPV harmful effects include; pneumothorax, increased intracranial pressure,
barotrauma, volutrauma, mucosal drying, gastric distention, possible aspiration, vomiting,
hyperventilation, psychological dependency and cardiovascular problems. These effects are
worsened when the patient is alert and conscious therefore to avoid this the patient is sedated and
paralyzed.
should check the ventilator circuit for patency, should avoid giving the air at high pressures as it
causes trauma, should maintain a sterility and regularly wash the mouth to avoid pulmonary
infection (Abraham et. al., 2014).
e) Management of analgesia and sedation
He is on ketamine, morphine, fentanyl, propofol, and rocuronium. These drugs will keep
him sedated, paralyzed and are analgesic relieving him of his pain (Colledge, Walker & Ralston,
2013). The IPPV harmful effects include; pneumothorax, increased intracranial pressure,
barotrauma, volutrauma, mucosal drying, gastric distention, possible aspiration, vomiting,
hyperventilation, psychological dependency and cardiovascular problems. These effects are
worsened when the patient is alert and conscious therefore to avoid this the patient is sedated and
paralyzed.
PHYSIOLOGY OF BURNS AND THE MANAGEMENT 12
References.
Abraham, E., Matthay, M. A., Dinarello, C. A., et al. (2014). Consensus conference definitions for
hypovolemia, hypovolemic shock, acute lung injury, and acute respiratory distress syndrome:
Time for a reevaluation. Critical Care Medicine, 28 (1), 232–235
Balk, R. A. (2015). Pathogenesis and management of multiple organ dysfunction or failure in severe
hypovolemia and hypovolemic shock. Critical Care Clinics, 16(2), 337–351.
Barrett, E., Barman, M., Boitano, S. (2017). Burns. Ganong’s Review of Medical Physiology. (24th ed).
New York, N.Y: McGraw Hill Medical.
Beck, L. H. (2015). The aging kidney. Defending a delicate balance of fluid and electrolytes. Geriatrics,
55(4), 26–28, 31–32.
Choi, P., Yip, G., Quinonez, L., & Cook, D. (2014). Crystalloids vs. colloids in fluid resuscitation: A
systematic review. Critical Care Medicine. 27(1), 200–209.
Colledge, N., Walker, R, & Ralston, S. (2013). Burns. Davidson’s Principles and Practice of Medicine.
(21st ed). New York, N.Y: Edinburgh.
Glynn, M. & Drake, W. (2014). Burns. Hutchinson’s Clinical Methods: an integrated approach to
clinical practice. London: Elsevier.
Hinkle, J.L, Cheever, K.H. (2013). Burns. Brunner and Saddarth’s Textbook of Medical and Surgical
Nursing, (13th ed) Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins.
Jindal, N., Hollenberg, S. M., & Dellinger, R. P. (2015). Pharmacologic issues in the management of
hypovolemic shock. Critical Care Clinics, 16(2), 233–248.
Kreimeier, U. (2016). Pathophysiology of fluid imbalance. Critical Care (London), 8, Suppl 2: S3–S7.
References.
Abraham, E., Matthay, M. A., Dinarello, C. A., et al. (2014). Consensus conference definitions for
hypovolemia, hypovolemic shock, acute lung injury, and acute respiratory distress syndrome:
Time for a reevaluation. Critical Care Medicine, 28 (1), 232–235
Balk, R. A. (2015). Pathogenesis and management of multiple organ dysfunction or failure in severe
hypovolemia and hypovolemic shock. Critical Care Clinics, 16(2), 337–351.
Barrett, E., Barman, M., Boitano, S. (2017). Burns. Ganong’s Review of Medical Physiology. (24th ed).
New York, N.Y: McGraw Hill Medical.
Beck, L. H. (2015). The aging kidney. Defending a delicate balance of fluid and electrolytes. Geriatrics,
55(4), 26–28, 31–32.
Choi, P., Yip, G., Quinonez, L., & Cook, D. (2014). Crystalloids vs. colloids in fluid resuscitation: A
systematic review. Critical Care Medicine. 27(1), 200–209.
Colledge, N., Walker, R, & Ralston, S. (2013). Burns. Davidson’s Principles and Practice of Medicine.
(21st ed). New York, N.Y: Edinburgh.
Glynn, M. & Drake, W. (2014). Burns. Hutchinson’s Clinical Methods: an integrated approach to
clinical practice. London: Elsevier.
Hinkle, J.L, Cheever, K.H. (2013). Burns. Brunner and Saddarth’s Textbook of Medical and Surgical
Nursing, (13th ed) Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins.
Jindal, N., Hollenberg, S. M., & Dellinger, R. P. (2015). Pharmacologic issues in the management of
hypovolemic shock. Critical Care Clinics, 16(2), 233–248.
Kreimeier, U. (2016). Pathophysiology of fluid imbalance. Critical Care (London), 8, Suppl 2: S3–S7.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





