TUM202: Polypharmacy Case Study - Judy's Complex Medication Regimen
VerifiedAdded on 2023/06/17
|6
|2103
|468
Case Study
AI Summary
This case study examines the effects of polypharmacy on Judy, a 61-year-old female presenting with various symptoms potentially linked to her complex medication regimen. Judy, who is self-medicating due to irregular doctor visits, takes multiple medications, increasing her risk of adverse drug reactions and drug-drug interactions. The analysis identifies potential interactions between her medications, such as perindopril and digoxin, and highlights the importance of registered nurses in monitoring drug interactions and advocating for patient-centered care. Strategies for preventing polypharmacy include adherence to prescribed dosages, healthcare provider assessments, and avoiding self-medication. The case emphasizes the role of registered nurses in medication administration, documentation, and collaboration with multidisciplinary teams to ensure patient safety and optimal health outcomes, focusing on educating Judy about her medications and potential risks.

TJudyapeutic Use of Medicines (TUM202) T3
2021
Assessment 2 - Polypharmacy case study
A Female aged 61, Judy, has presented to the clinic with (SOB), chest complaints, review of asthma medication
and changes in Judy oedema. The patient is also mentioned feeling general aches and pains over Judy body. The
Polypharmacy case study is about a geriatric patient who has multiple chronic conditions and is self-medicating;
Julie is adjusting her drug dosage given by the General Practitioner due to irregular visits because of the covert
19 pandemic. The case study intends to show the effects of Polypharmacy on Julie, who is taking numerous
medications and not following Judy doctors subscription dosage. Judy is currently not taking fluticasone.
Polypharmacy definition from the word "poly", meaning "many", indicates individuals who use many
medicines/drugs due to having more than one medical condition. Polypharmacy occurs when a person is taking
a variety of different medications at the same time. It is defined as the concurrent use of five or more medicines
by the same person. This often happens when a person has many chronic diseases, such as diabetes, high blood
pressure, heart failure, osteoporosis, and symptoms such as pain or insomnia or requires long-term treatment
with medications. (Onder & Marengoni, (2017)) The majority of the population symptoms accumulate with age.
For this reason, older adults are at greater risk of Polypharmacy.
Risks of Polypharmacy and the demographics at risk.
In most cases, adults and those with numerous debilitating diseases are at higher risk of Polypharmacy. They are
vulnerable to acquiring different medical conditions that may require them to take medications and eventually
lead to Polypharmacy. Research in patients seeing multiple physicians for various situations contributes to
Polypharmacy mentioned in the Journal (Mortazavi et al., (2019)) due to the lack of a regular physician.
Polypharmacy is an area of concern for the elderly because of several reasons. Older adults are at a greater risk
for adverse drug reactions (ADRs) because of the metabolic changes associated with age and reduced drug
clearance associated with ageing; this risk is exacerbated by increasing the number of drugs used. The use of
multiple medications increases the potential of drug-drug interactions. Polypharmacy may sometimes lead to
"prescribing cascades." Prescribing cascade is said when signs and symptoms (multiple and nonspecific) of an
ADR are misinterpreted as a disease. A new treatment/drug therapy is compounded to the earlier prescribed
treatment to treat the condition. (Rushabh J Dagli, (2021)) Judy is at higher risk of potentially developing side-
effects and thus making a prescribing cascade a concern for Polypharmacy.
2021
Assessment 2 - Polypharmacy case study
A Female aged 61, Judy, has presented to the clinic with (SOB), chest complaints, review of asthma medication
and changes in Judy oedema. The patient is also mentioned feeling general aches and pains over Judy body. The
Polypharmacy case study is about a geriatric patient who has multiple chronic conditions and is self-medicating;
Julie is adjusting her drug dosage given by the General Practitioner due to irregular visits because of the covert
19 pandemic. The case study intends to show the effects of Polypharmacy on Julie, who is taking numerous
medications and not following Judy doctors subscription dosage. Judy is currently not taking fluticasone.
Polypharmacy definition from the word "poly", meaning "many", indicates individuals who use many
medicines/drugs due to having more than one medical condition. Polypharmacy occurs when a person is taking
a variety of different medications at the same time. It is defined as the concurrent use of five or more medicines
by the same person. This often happens when a person has many chronic diseases, such as diabetes, high blood
pressure, heart failure, osteoporosis, and symptoms such as pain or insomnia or requires long-term treatment
with medications. (Onder & Marengoni, (2017)) The majority of the population symptoms accumulate with age.
For this reason, older adults are at greater risk of Polypharmacy.
Risks of Polypharmacy and the demographics at risk.
In most cases, adults and those with numerous debilitating diseases are at higher risk of Polypharmacy. They are
vulnerable to acquiring different medical conditions that may require them to take medications and eventually
lead to Polypharmacy. Research in patients seeing multiple physicians for various situations contributes to
Polypharmacy mentioned in the Journal (Mortazavi et al., (2019)) due to the lack of a regular physician.
Polypharmacy is an area of concern for the elderly because of several reasons. Older adults are at a greater risk
for adverse drug reactions (ADRs) because of the metabolic changes associated with age and reduced drug
clearance associated with ageing; this risk is exacerbated by increasing the number of drugs used. The use of
multiple medications increases the potential of drug-drug interactions. Polypharmacy may sometimes lead to
"prescribing cascades." Prescribing cascade is said when signs and symptoms (multiple and nonspecific) of an
ADR are misinterpreted as a disease. A new treatment/drug therapy is compounded to the earlier prescribed
treatment to treat the condition. (Rushabh J Dagli, (2021)) Judy is at higher risk of potentially developing side-
effects and thus making a prescribing cascade a concern for Polypharmacy.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

The impacts of Polypharmacy on the older person and the healthcare system.
The risk of Polypharmacy increases with age, and we are more susceptible to chronic conditions. Some of the
side effects resulting in adverse drug interactions may include Tiredness, sleepiness, or decreased alertness,
constipation, diarrhea, or incontinence, loss of appetite, confusion, falls, depression, delirium, and
nonadherence. Polypharmacy is associated with resulting increased physician visits and hospitalisations and
increased costs of care for individuals.
Polypharmacy often contributes to increased healthcare costs for patients and the healthcare system and can
manifest in various ways. (Justin J. SJudyman, (2021)) Polypharmacy is the increased monthly copayments that
patients may incur because of a high number of prescribed medications. Duplications in medications or drug
interactions may cause side effects that can increase outpatient visits as well as hospitalisations and even death,
which can then significantly increase medical costs for patients as well as the providers or hospitals that treat
them. The recent Journal ("Polypharmacy, 75 years and over", (2021)) found that nearly 700,000 people in
Australia over 75 were in the polypharmacy bracket, with 8% having more than 11 different medications
prescribed.
The symptoms that Julie is experiencing covers human error (self-medicating) and drug interactions. As
discussed above, the pathology for this is the increased intake of prescribed medicines, causing most of Judy
signs & symptoms. The registered nurse would monitor the drug interactions between the following after
checking MIMS Australia ("MIMS Australia", (2021)) Judy is not taking fluticasone. Suddenly stopping this
medication can have withdrawal symptoms such as weakness, weight loss, nausea, muscle pain, headache,
tiredness, dizziness.
• Perindopril + Digoxin. Perindopril increases levels of Digoxin by unspecified interaction mechanism.
• Amiloride + Digoxin. Amiloride and Digoxin both increase potassium levels in the blood.
• Perindopril + Amiloride. Perindopril, Amiloride Mechanism: additive drug effects. The combination
increases blood potassium levels.
• Perindopril + Insulin. Lispro Perindopril increases the effects of Insulin Lispro.
Although the increase of potassium due to Polypharmacy would reduce oedema, it does not seem to be the case
in Judy's condition. These side-effects that Judy is facing by Polypharmacy and the misuse of her prescription
drugs. By Judy self-medicating, she has inadvertently worsened her condition due to human error. Judy is
currently under the polypharmacy drug category. Many of these drugs have interactions with one another, and
here are some of the signs and symptoms that a registered nurse would look out for in a patient.
In the case study, it seems the drugs taken for Judy asthma are the ones that are causing Judy signs and
symptoms, such as fluticasone, salmeterol and albuterol. Judy oedema might be related to Judy taking
prednisolone almost every day for the last month, giving the effect of increased blood glucose level. Since
prednisolone is a steroid medication, it can cause an increase in Judy blood sugar level by making the liver
resistant to Insulin. Fluid retention is also one side effect of long-term steroids intake that caused Judy oedema
on Judy lower & upper extremities. Because of the oedema, Julie will be experiencing more pain generally
around Judy body because of excess fluid storage.
The chance of side effects depends on the dose, type of drug and length of treatment. Some side effects are more
severe than others. Common side effects include weight gain, mood changes, muscle weakness, blurred vision,
worsening of diabetes & blood pressure, cataracts or glaucoma and water retention that may cause swollen
extremities. These effects mentioned were shown to Judy in the case study.
The risk of Polypharmacy increases with age, and we are more susceptible to chronic conditions. Some of the
side effects resulting in adverse drug interactions may include Tiredness, sleepiness, or decreased alertness,
constipation, diarrhea, or incontinence, loss of appetite, confusion, falls, depression, delirium, and
nonadherence. Polypharmacy is associated with resulting increased physician visits and hospitalisations and
increased costs of care for individuals.
Polypharmacy often contributes to increased healthcare costs for patients and the healthcare system and can
manifest in various ways. (Justin J. SJudyman, (2021)) Polypharmacy is the increased monthly copayments that
patients may incur because of a high number of prescribed medications. Duplications in medications or drug
interactions may cause side effects that can increase outpatient visits as well as hospitalisations and even death,
which can then significantly increase medical costs for patients as well as the providers or hospitals that treat
them. The recent Journal ("Polypharmacy, 75 years and over", (2021)) found that nearly 700,000 people in
Australia over 75 were in the polypharmacy bracket, with 8% having more than 11 different medications
prescribed.
The symptoms that Julie is experiencing covers human error (self-medicating) and drug interactions. As
discussed above, the pathology for this is the increased intake of prescribed medicines, causing most of Judy
signs & symptoms. The registered nurse would monitor the drug interactions between the following after
checking MIMS Australia ("MIMS Australia", (2021)) Judy is not taking fluticasone. Suddenly stopping this
medication can have withdrawal symptoms such as weakness, weight loss, nausea, muscle pain, headache,
tiredness, dizziness.
• Perindopril + Digoxin. Perindopril increases levels of Digoxin by unspecified interaction mechanism.
• Amiloride + Digoxin. Amiloride and Digoxin both increase potassium levels in the blood.
• Perindopril + Amiloride. Perindopril, Amiloride Mechanism: additive drug effects. The combination
increases blood potassium levels.
• Perindopril + Insulin. Lispro Perindopril increases the effects of Insulin Lispro.
Although the increase of potassium due to Polypharmacy would reduce oedema, it does not seem to be the case
in Judy's condition. These side-effects that Judy is facing by Polypharmacy and the misuse of her prescription
drugs. By Judy self-medicating, she has inadvertently worsened her condition due to human error. Judy is
currently under the polypharmacy drug category. Many of these drugs have interactions with one another, and
here are some of the signs and symptoms that a registered nurse would look out for in a patient.
In the case study, it seems the drugs taken for Judy asthma are the ones that are causing Judy signs and
symptoms, such as fluticasone, salmeterol and albuterol. Judy oedema might be related to Judy taking
prednisolone almost every day for the last month, giving the effect of increased blood glucose level. Since
prednisolone is a steroid medication, it can cause an increase in Judy blood sugar level by making the liver
resistant to Insulin. Fluid retention is also one side effect of long-term steroids intake that caused Judy oedema
on Judy lower & upper extremities. Because of the oedema, Julie will be experiencing more pain generally
around Judy body because of excess fluid storage.
The chance of side effects depends on the dose, type of drug and length of treatment. Some side effects are more
severe than others. Common side effects include weight gain, mood changes, muscle weakness, blurred vision,
worsening of diabetes & blood pressure, cataracts or glaucoma and water retention that may cause swollen
extremities. These effects mentioned were shown to Judy in the case study.
Strategies that can be implemented to identify and prevent Polypharmacy.
As discussed in detail in the Journal British pharmacology societies principles of good prescribing: (Ross &
Loke, (2010)), Some of their main recommendations below that a registered nurse would consider when
reviewing a patient that may be at risk of complications from Polypharmacy.
1. reasons for the-prescribing.
2. Take into account intellectual disabilities and health literacy.
4. patient's/carer's/families/advocates ideas, concerns, and expectations.
5. Ensure all medicines are effective, safe, cost-effective in appropriate form individualised
6. Adhere to national guidelines and local formularies where appropriate.
7. Write detailed, correct documentation detailing the reason for de-prescribing.
8. Monitor the beneficial and adverse effects of de-prescribing medicines and any products on behaviour.
9. Communicate and document all de-prescribing decisions and the reasons for them, such as transferred to
appropriate personnel such as GP, pharmacist, psychiatrist, epileptologist, carer and patient.
10. De -prescribe within the limitations of your knowledge, skills and experience of the population with
intellectual disabilities and behaviour disorders.
Preventing Polypharmacy can be achieved on both sides. The patient can religiously take medications by
following the dosage given by their practitioner. On the other side, healthcare providers can assess/inspect
before administering drugs to their patients and identifying drug interactions. Each patient care team is
responsible when administering or reviewing patients medication. Another concern that is to be avoided is Self-
medication. This leads to Polypharmacy; people tend to take different kinds of drugs or over the counter drugs.
It will also be helpful not to jump from one practitioner to another to prevent being prescribed various medicines
and dosages.
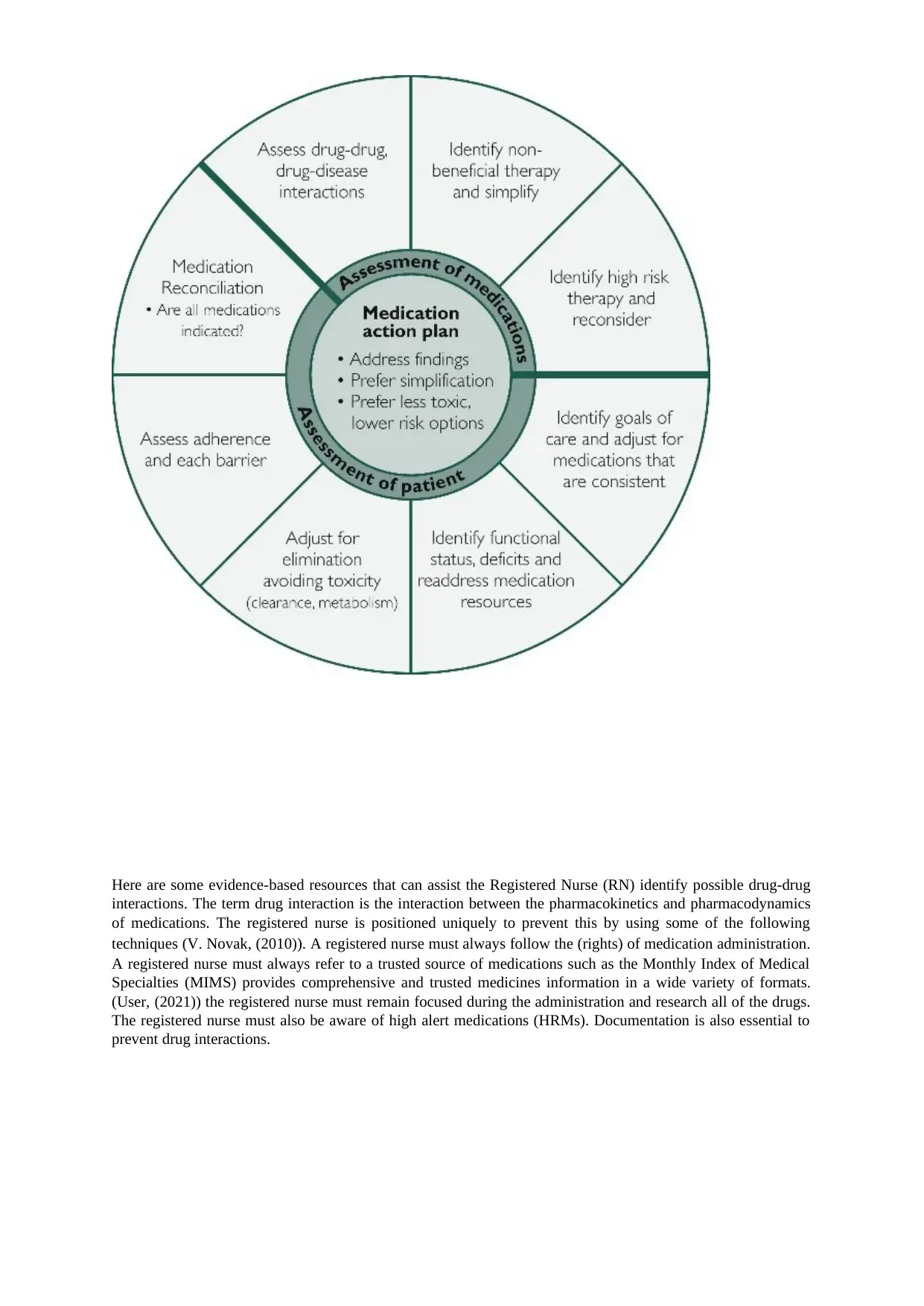
The diagram below shows some strategies to manage Polypharmacy. It defines the assessment of the medication
or drug is given, planning which is crucial to see if there are drug-drug interactions to each medication, and
patient evaluation.
As discussed in detail in the Journal British pharmacology societies principles of good prescribing: (Ross &
Loke, (2010)), Some of their main recommendations below that a registered nurse would consider when
reviewing a patient that may be at risk of complications from Polypharmacy.
1. reasons for the-prescribing.
2. Take into account intellectual disabilities and health literacy.
4. patient's/carer's/families/advocates ideas, concerns, and expectations.
5. Ensure all medicines are effective, safe, cost-effective in appropriate form individualised
6. Adhere to national guidelines and local formularies where appropriate.
7. Write detailed, correct documentation detailing the reason for de-prescribing.
8. Monitor the beneficial and adverse effects of de-prescribing medicines and any products on behaviour.
9. Communicate and document all de-prescribing decisions and the reasons for them, such as transferred to
appropriate personnel such as GP, pharmacist, psychiatrist, epileptologist, carer and patient.
10. De -prescribe within the limitations of your knowledge, skills and experience of the population with
intellectual disabilities and behaviour disorders.
Preventing Polypharmacy can be achieved on both sides. The patient can religiously take medications by
following the dosage given by their practitioner. On the other side, healthcare providers can assess/inspect
before administering drugs to their patients and identifying drug interactions. Each patient care team is
responsible when administering or reviewing patients medication. Another concern that is to be avoided is Self-
medication. This leads to Polypharmacy; people tend to take different kinds of drugs or over the counter drugs.
It will also be helpful not to jump from one practitioner to another to prevent being prescribed various medicines
and dosages.
The diagram below shows some strategies to manage Polypharmacy. It defines the assessment of the medication
or drug is given, planning which is crucial to see if there are drug-drug interactions to each medication, and
patient evaluation.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Here are some evidence-based resources that can assist the Registered Nurse (RN) identify possible drug-drug
interactions. The term drug interaction is the interaction between the pharmacokinetics and pharmacodynamics
of medications. The registered nurse is positioned uniquely to prevent this by using some of the following
techniques (V. Novak, (2010)). A registered nurse must always follow the (rights) of medication administration.
A registered nurse must always refer to a trusted source of medications such as the Monthly Index of Medical
Specialties (MIMS) provides comprehensive and trusted medicines information in a wide variety of formats.
(User, (2021)) the registered nurse must remain focused during the administration and research all of the drugs.
The registered nurse must also be aware of high alert medications (HRMs). Documentation is also essential to
prevent drug interactions.
interactions. The term drug interaction is the interaction between the pharmacokinetics and pharmacodynamics
of medications. The registered nurse is positioned uniquely to prevent this by using some of the following
techniques (V. Novak, (2010)). A registered nurse must always follow the (rights) of medication administration.
A registered nurse must always refer to a trusted source of medications such as the Monthly Index of Medical
Specialties (MIMS) provides comprehensive and trusted medicines information in a wide variety of formats.
(User, (2021)) the registered nurse must remain focused during the administration and research all of the drugs.
The registered nurse must also be aware of high alert medications (HRMs). Documentation is also essential to
prevent drug interactions.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
The RN will incorporate a person-centred approach when advocating for the case study patient The registered
nurse must ensure that all the multidisciplinary team is aware of the patient's goals outcomes and health literacy
concerning their medication. The RN needs to ask Judy what her goals and expectations are concerning her
medications and general health. The RN needs to educate Judy on what each of her medications does and why
she has to take them. The RN also needs to explain to Judy the risks if she does not take her medications and
follow doctors' advice. If necessary, the RN can also speak to Judy's husband to let him know to assist her with
her medications. The RN will also need to be aware that all multi-disciplined team members have access to
Judy's medication and her expectations and goals.
nurse must ensure that all the multidisciplinary team is aware of the patient's goals outcomes and health literacy
concerning their medication. The RN needs to ask Judy what her goals and expectations are concerning her
medications and general health. The RN needs to educate Judy on what each of her medications does and why
she has to take them. The RN also needs to explain to Judy the risks if she does not take her medications and
follow doctors' advice. If necessary, the RN can also speak to Judy's husband to let him know to assist her with
her medications. The RN will also need to be aware that all multi-disciplined team members have access to
Judy's medication and her expectations and goals.
Reference:
Onder, G., & Marengoni, A. (2017). Polypharmacy. Jama, 318(17), 1728–1728.
https://doi.org/10.1001/jama.2017.15764
Polypharmacy, 75 years and over. (2021). Retrieved 1 November 2021, from
https://www.safetyandquality.gov.au/sites/default/files/2021-04/fourth_atlas_2021_-
_6.1_polypharmacy_75_years_and_over.pdf
Rushabh J Dagli, A. (2021). Polypharmacy: A Global Risk Factor for Elderly People. Retrieved 18 October
2021, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4295469/
MIMS Australia. (2021). Retrieved 1 November 2021, from https://mims.com.au
Mortazavi, S., Shati, M., Malakouti, S., Khankeh, H., Mehravaran, S., & Ahmadi, F. (2019). Physicians' role in
the development of inappropriate Polypharmacy among older adults in Iran: a qualitative study. BMJ
Open, 9(5), e024128. doi: 10.1136/bmjopen-2018-024128
Justin J. SJudyman, M. (2021). Addressing the Polypharmacy Conundrum. Retrieved 14 October 2021, from
https://www.uspharmacist.com/article/addressing-the-polypharmacy-conundrum
https://www.mayoclinicproceedings.org/article/S0025-6196(20)30616-9/fulltext
(Table & Diagram reference)
Ross, S., & Loke, Y. (2010). Development of learning outcomes for an undergraduate prescribing curriculum
(British Pharmacological Society prescribing initiative). British Journal Of Clinical Pharmacology,
70(4), 604-608. doi: 10.1111/j.1365-2125.2009.03581.x
https://my.clevelandclinic.org/health/drugs/4812-corticosteroids
V. Novak, B. (2010). Adverse Drug Reactions: A Handbook for Prescribers. Nurse Prescribing, 8(6), 291-291.
doi: 10.12968/npre.2010.8.6.48413
https://www.pharmacytimes.com/view/2004-12-9094
Onder, G., & Marengoni, A. (2017). Polypharmacy. Jama, 318(17), 1728–1728.
https://doi.org/10.1001/jama.2017.15764
Polypharmacy, 75 years and over. (2021). Retrieved 1 November 2021, from
https://www.safetyandquality.gov.au/sites/default/files/2021-04/fourth_atlas_2021_-
_6.1_polypharmacy_75_years_and_over.pdf
Rushabh J Dagli, A. (2021). Polypharmacy: A Global Risk Factor for Elderly People. Retrieved 18 October
2021, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4295469/
MIMS Australia. (2021). Retrieved 1 November 2021, from https://mims.com.au
Mortazavi, S., Shati, M., Malakouti, S., Khankeh, H., Mehravaran, S., & Ahmadi, F. (2019). Physicians' role in
the development of inappropriate Polypharmacy among older adults in Iran: a qualitative study. BMJ
Open, 9(5), e024128. doi: 10.1136/bmjopen-2018-024128
Justin J. SJudyman, M. (2021). Addressing the Polypharmacy Conundrum. Retrieved 14 October 2021, from
https://www.uspharmacist.com/article/addressing-the-polypharmacy-conundrum
https://www.mayoclinicproceedings.org/article/S0025-6196(20)30616-9/fulltext
(Table & Diagram reference)
Ross, S., & Loke, Y. (2010). Development of learning outcomes for an undergraduate prescribing curriculum
(British Pharmacological Society prescribing initiative). British Journal Of Clinical Pharmacology,
70(4), 604-608. doi: 10.1111/j.1365-2125.2009.03581.x
https://my.clevelandclinic.org/health/drugs/4812-corticosteroids
V. Novak, B. (2010). Adverse Drug Reactions: A Handbook for Prescribers. Nurse Prescribing, 8(6), 291-291.
doi: 10.12968/npre.2010.8.6.48413
https://www.pharmacytimes.com/view/2004-12-9094
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 6
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





