Postoperative Management of Frank Wright: Nursing Care Plan Analysis
VerifiedAdded on 2022/11/25
|15
|2801
|491
Essay
AI Summary
This essay provides a comprehensive overview of the postoperative management of Frank Wright, a 76-year-old patient who underwent a right total knee replacement. The essay critically examines the patient's post-surgical plan of care, considering the impact of comorbidities and general anesthe...

Running head: POSTOPERATIVE MANAGEMENT 1
Postoperative Management
Name
Institutional Affiliation
Postoperative Management
Name
Institutional Affiliation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
POSTOPERATIVE MANAGEMENT
2
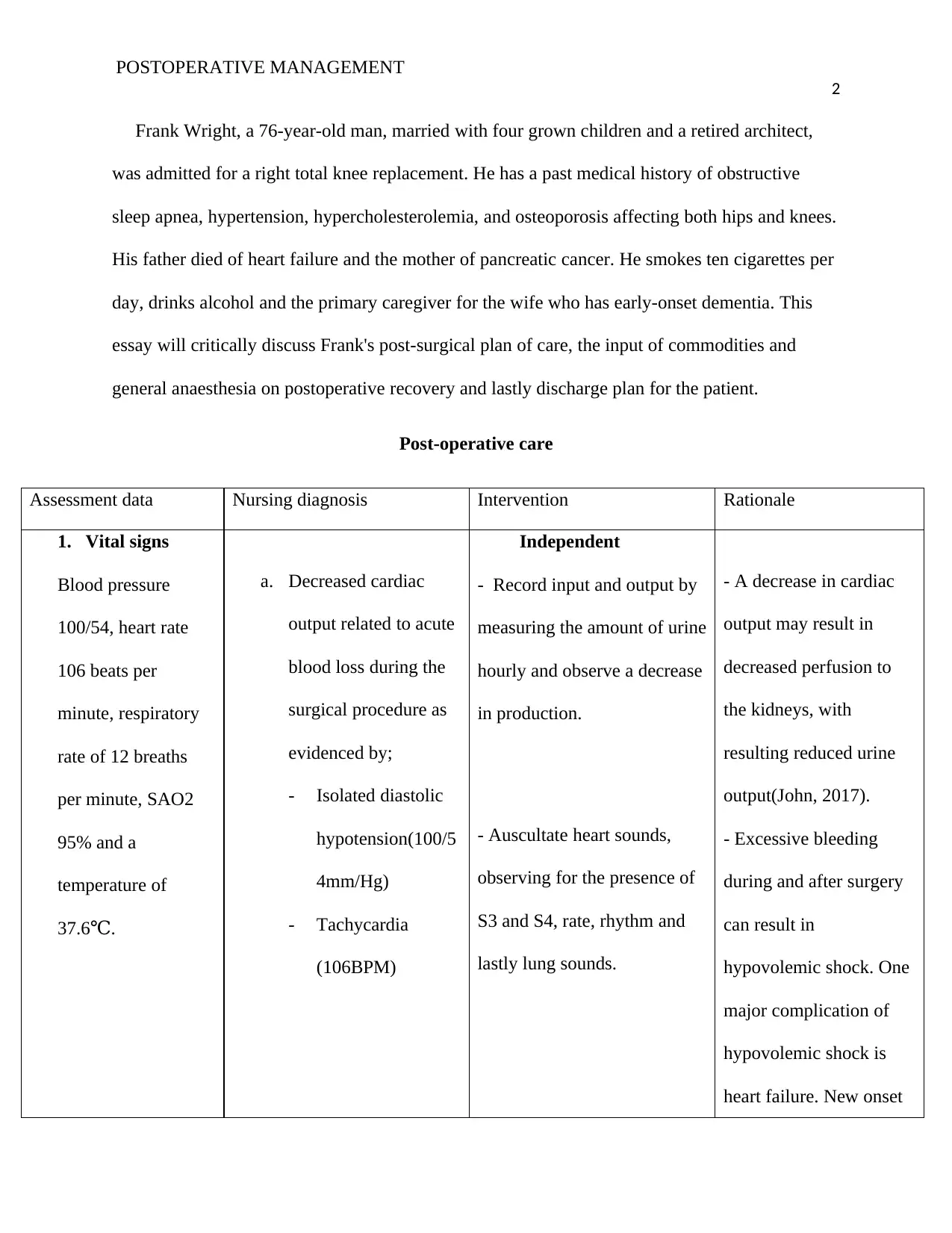
Frank Wright, a 76-year-old man, married with four grown children and a retired architect,
was admitted for a right total knee replacement. He has a past medical history of obstructive
sleep apnea, hypertension, hypercholesterolemia, and osteoporosis affecting both hips and knees.
His father died of heart failure and the mother of pancreatic cancer. He smokes ten cigarettes per
day, drinks alcohol and the primary caregiver for the wife who has early-onset dementia. This
essay will critically discuss Frank's post-surgical plan of care, the input of commodities and
general anaesthesia on postoperative recovery and lastly discharge plan for the patient.
Post-operative care
Assessment data Nursing diagnosis Intervention Rationale
1. Vital signs
Blood pressure
100/54, heart rate
106 beats per
minute, respiratory
rate of 12 breaths
per minute, SAO2
95% and a
temperature of
37.6 .℃
a. Decreased cardiac
output related to acute
blood loss during the
surgical procedure as
evidenced by;
- Isolated diastolic
hypotension(100/5
4mm/Hg)
- Tachycardia
(106BPM)
Independent
- Record input and output by
measuring the amount of urine
hourly and observe a decrease
in production.
- Auscultate heart sounds,
observing for the presence of
S3 and S4, rate, rhythm and
lastly lung sounds.
- A decrease in cardiac
output may result in
decreased perfusion to
the kidneys, with
resulting reduced urine
output(John, 2017).
- Excessive bleeding
during and after surgery
can result in
hypovolemic shock. One
major complication of
hypovolemic shock is
heart failure. New onset
2
Frank Wright, a 76-year-old man, married with four grown children and a retired architect,
was admitted for a right total knee replacement. He has a past medical history of obstructive
sleep apnea, hypertension, hypercholesterolemia, and osteoporosis affecting both hips and knees.
His father died of heart failure and the mother of pancreatic cancer. He smokes ten cigarettes per
day, drinks alcohol and the primary caregiver for the wife who has early-onset dementia. This
essay will critically discuss Frank's post-surgical plan of care, the input of commodities and
general anaesthesia on postoperative recovery and lastly discharge plan for the patient.
Post-operative care
Assessment data Nursing diagnosis Intervention Rationale
1. Vital signs
Blood pressure
100/54, heart rate
106 beats per
minute, respiratory
rate of 12 breaths
per minute, SAO2
95% and a
temperature of
37.6 .℃
a. Decreased cardiac
output related to acute
blood loss during the
surgical procedure as
evidenced by;
- Isolated diastolic
hypotension(100/5
4mm/Hg)
- Tachycardia
(106BPM)
Independent
- Record input and output by
measuring the amount of urine
hourly and observe a decrease
in production.
- Auscultate heart sounds,
observing for the presence of
S3 and S4, rate, rhythm and
lastly lung sounds.
- A decrease in cardiac
output may result in
decreased perfusion to
the kidneys, with
resulting reduced urine
output(John, 2017).
- Excessive bleeding
during and after surgery
can result in
hypovolemic shock. One
major complication of
hypovolemic shock is
heart failure. New onset
POSTOPERATIVE MANAGEMENT
3
- Monitor breath sounds,
respiratory rate, and rhythm.
Note any presence of
orthopnea and paroxysmal
nocturnal dyspnea.
Collaborative
- Monitor electrocardiogram
for ectopy, rate and rhythm.
- Monitor for Hct,
of tachycardia, fine
crackles in lungs and
gallop rhythm may
indicate the start of heart
failure(John, 2017).
- Shallow and rapid
respirations show
decreased cardiac output.
Crackles is a
characteristic of impaired
left ventricular emptying
due to fluid buildup
(John, 2017).
- Cardiac dysrhythmias
are caused by hypoxia,
low perfusion and
acidosis. Tachycardia
and ectopic beats may
further compromise the
cardiac output, especially
in older patients(Abbott,
2016).
3
- Monitor breath sounds,
respiratory rate, and rhythm.
Note any presence of
orthopnea and paroxysmal
nocturnal dyspnea.
Collaborative
- Monitor electrocardiogram
for ectopy, rate and rhythm.
- Monitor for Hct,
of tachycardia, fine
crackles in lungs and
gallop rhythm may
indicate the start of heart
failure(John, 2017).
- Shallow and rapid
respirations show
decreased cardiac output.
Crackles is a
characteristic of impaired
left ventricular emptying
due to fluid buildup
(John, 2017).
- Cardiac dysrhythmias
are caused by hypoxia,
low perfusion and
acidosis. Tachycardia
and ectopic beats may
further compromise the
cardiac output, especially
in older patients(Abbott,
2016).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
POSTOPERATIVE MANAGEMENT
4
b. Ineffective breathing
patterns related to
opioids causing
prothrombin time, platelet
count, Hgb and activated
clotting time.
- Administer blood products
and intravenous fluid as
needed (Sodium chloride
0.9% 100mls/hour).
- Administer supplemental
oxygen (Oxygen 2L via
nasal).
Independent
- Investigate the cause of
- Useful in recognizing
bleeding or clotting
problems related to the
surgery that may further
compromise the cardiac
output(Albert & Miracle,
2016).
- Red blood cell
replacement is usually
recommended to restore
and maintain enough
circulating blood volume
and increase oxygen-
carrying capacity to the
tissues(Abbott, 2016).
- Increases oxygenation
to the tissues hence
decreasing cardiac
workload and helps in
resolving
dysrhythmias(Albert &
Miracle, 2016).
4
b. Ineffective breathing
patterns related to
opioids causing
prothrombin time, platelet
count, Hgb and activated
clotting time.
- Administer blood products
and intravenous fluid as
needed (Sodium chloride
0.9% 100mls/hour).
- Administer supplemental
oxygen (Oxygen 2L via
nasal).
Independent
- Investigate the cause of
- Useful in recognizing
bleeding or clotting
problems related to the
surgery that may further
compromise the cardiac
output(Albert & Miracle,
2016).
- Red blood cell
replacement is usually
recommended to restore
and maintain enough
circulating blood volume
and increase oxygen-
carrying capacity to the
tissues(Abbott, 2016).
- Increases oxygenation
to the tissues hence
decreasing cardiac
workload and helps in
resolving
dysrhythmias(Albert &
Miracle, 2016).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
POSTOPERATIVE MANAGEMENT
5
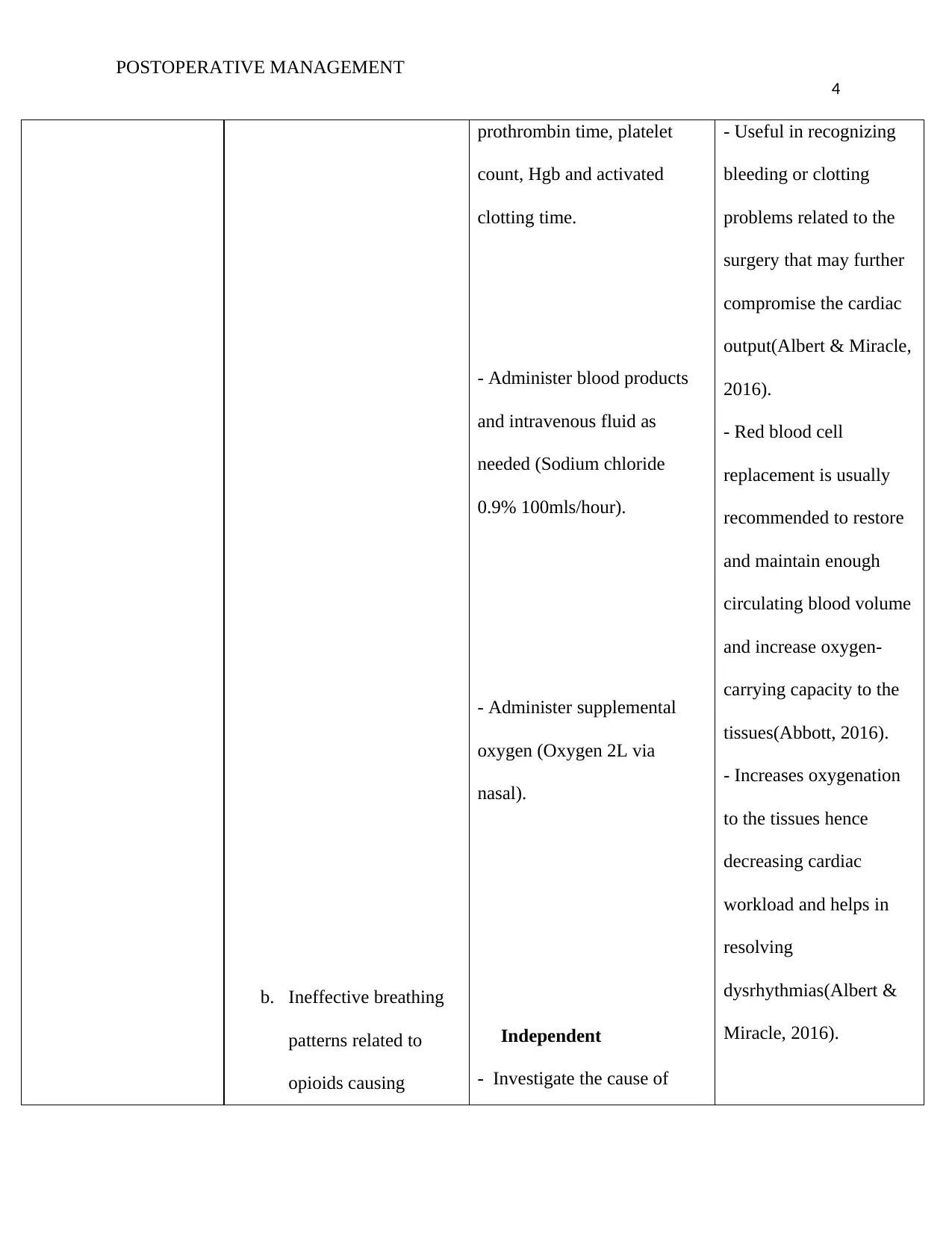
respiratory centre
depression as
evidenced by;
- Bradypnea (12
breaths per
minute)
respiratory failure.
- Monitor overall breathing
pattern. Taking note of the
respiratory rate,
differentiating between
ventilator breaths and
spontaneous respirations.
- Determine the number of
respirations for 1 minute and
compare with normal
respirations and ventilator
adjusted rate.
- Realizing the root cause
of the patient's particular
ventilatory problem is
vital to the care of the
patient, for example,
decisions on future
ventilator needs and the
suitable type of ventilator
support (John, 2017).
- A patient on a
ventilator may
experience
hypoventilation,
hyperventilation or
dyspnea and may try to
adjust the deficiency by
over-breathing(Dasta,
2017).
- Breathing patterns vary
depending on the issue
requiring ventilatory
assistance. For instance,
a patient may be relying
5
respiratory centre
depression as
evidenced by;
- Bradypnea (12
breaths per
minute)
respiratory failure.
- Monitor overall breathing
pattern. Taking note of the
respiratory rate,
differentiating between
ventilator breaths and
spontaneous respirations.
- Determine the number of
respirations for 1 minute and
compare with normal
respirations and ventilator
adjusted rate.
- Realizing the root cause
of the patient's particular
ventilatory problem is
vital to the care of the
patient, for example,
decisions on future
ventilator needs and the
suitable type of ventilator
support (John, 2017).
- A patient on a
ventilator may
experience
hypoventilation,
hyperventilation or
dyspnea and may try to
adjust the deficiency by
over-breathing(Dasta,
2017).
- Breathing patterns vary
depending on the issue
requiring ventilatory
assistance. For instance,
a patient may be relying
POSTOPERATIVE MANAGEMENT
6
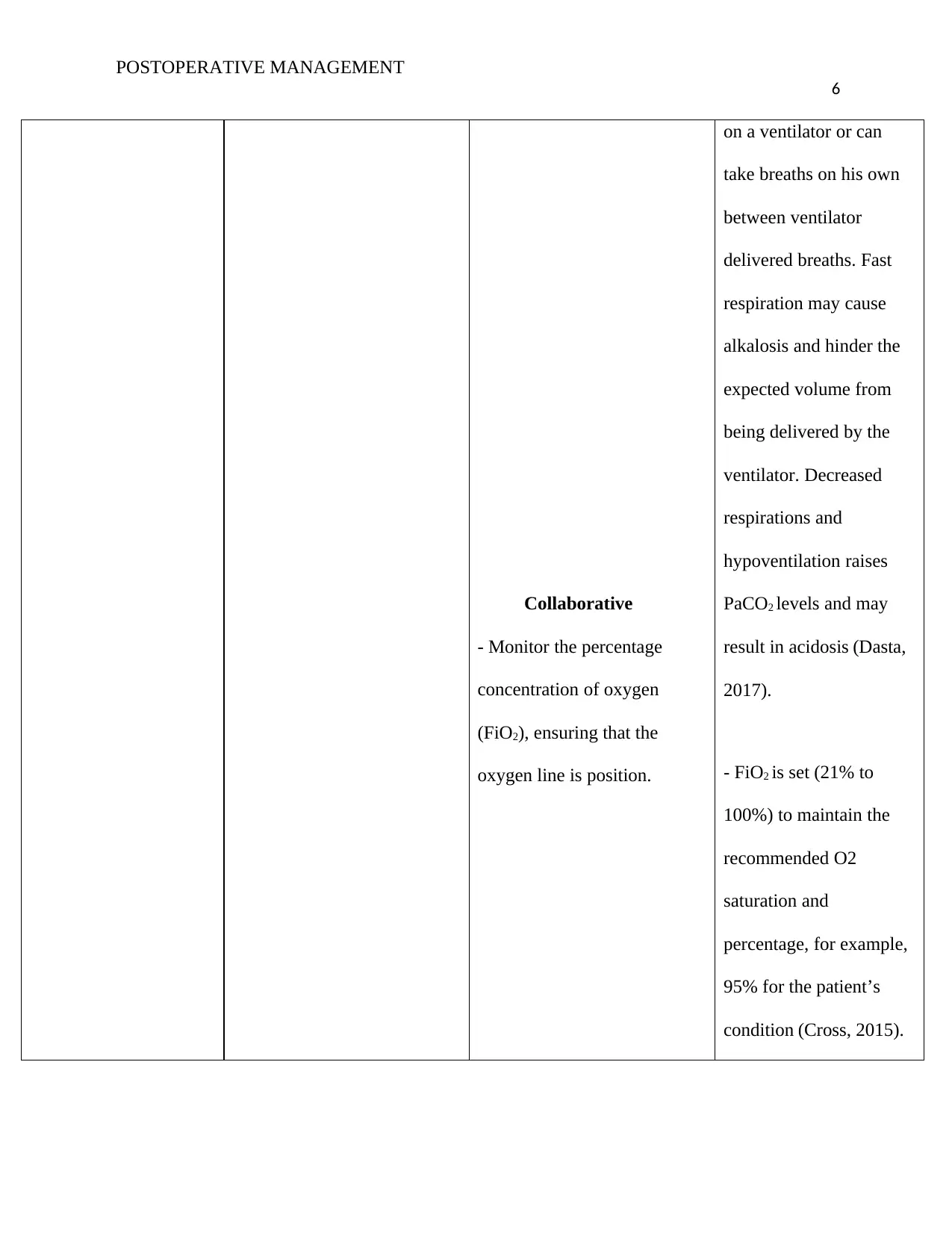
Collaborative
- Monitor the percentage
concentration of oxygen
(FiO2), ensuring that the
oxygen line is position.
on a ventilator or can
take breaths on his own
between ventilator
delivered breaths. Fast
respiration may cause
alkalosis and hinder the
expected volume from
being delivered by the
ventilator. Decreased
respirations and
hypoventilation raises
PaCO2 levels and may
result in acidosis (Dasta,
2017).
- FiO2 is set (21% to
100%) to maintain the
recommended O2
saturation and
percentage, for example,
95% for the patient’s
condition (Cross, 2015).
6
Collaborative
- Monitor the percentage
concentration of oxygen
(FiO2), ensuring that the
oxygen line is position.
on a ventilator or can
take breaths on his own
between ventilator
delivered breaths. Fast
respiration may cause
alkalosis and hinder the
expected volume from
being delivered by the
ventilator. Decreased
respirations and
hypoventilation raises
PaCO2 levels and may
result in acidosis (Dasta,
2017).
- FiO2 is set (21% to
100%) to maintain the
recommended O2
saturation and
percentage, for example,
95% for the patient’s
condition (Cross, 2015).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
POSTOPERATIVE MANAGEMENT
7
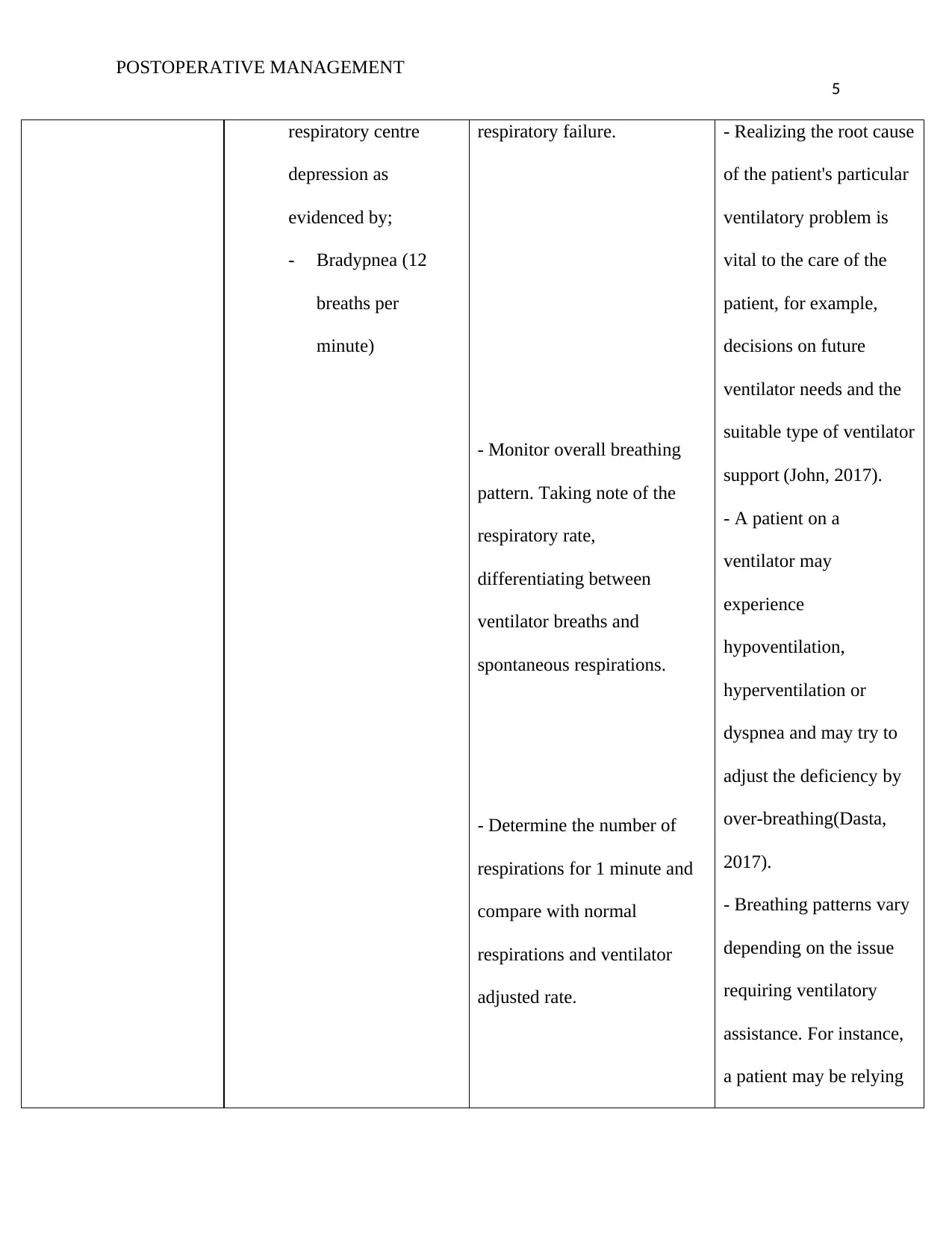
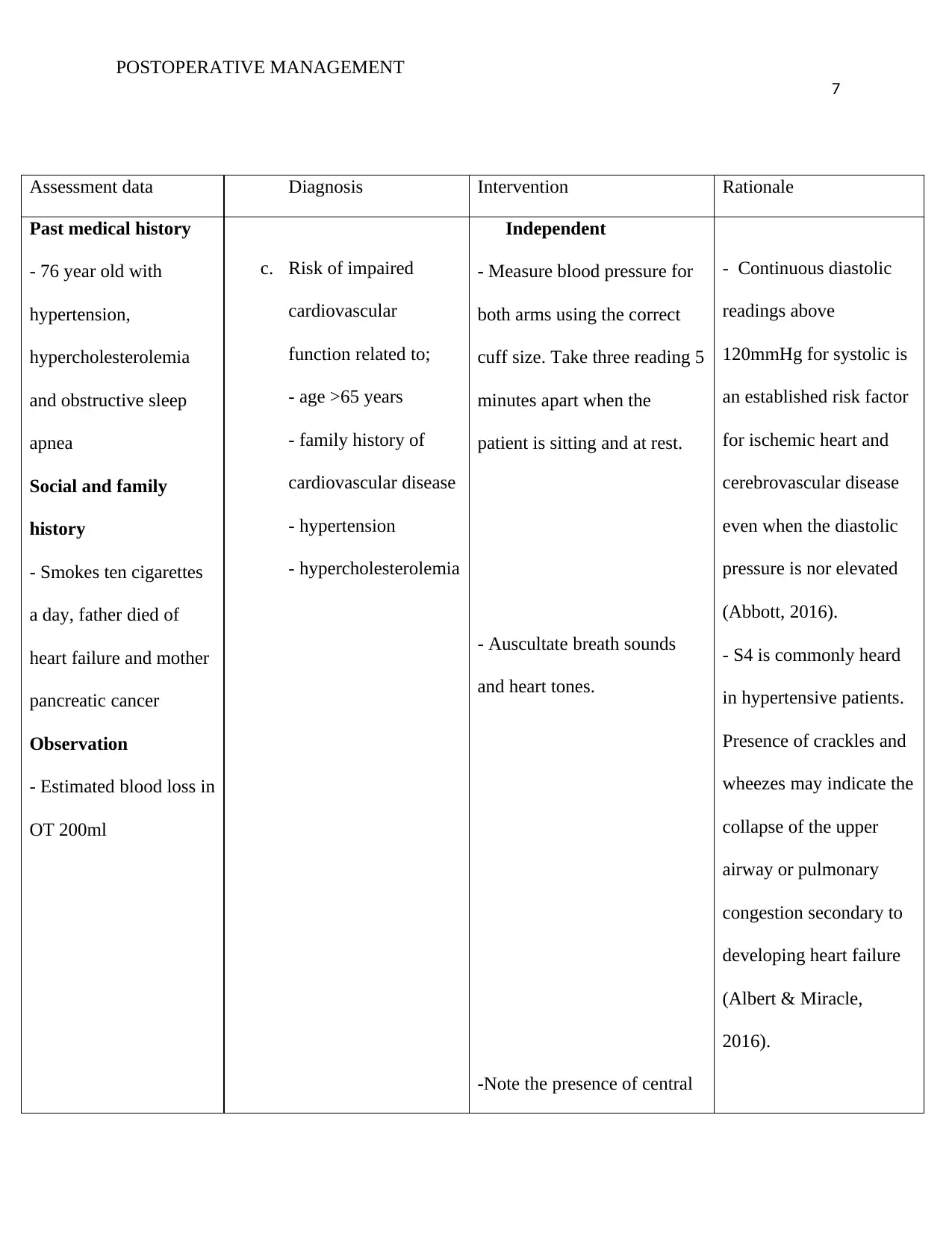
Assessment data Diagnosis Intervention Rationale
Past medical history
- 76 year old with
hypertension,
hypercholesterolemia
and obstructive sleep
apnea
Social and family
history
- Smokes ten cigarettes
a day, father died of
heart failure and mother
pancreatic cancer
Observation
- Estimated blood loss in
OT 200ml
c. Risk of impaired
cardiovascular
function related to;
- age >65 years
- family history of
cardiovascular disease
- hypertension
- hypercholesterolemia
Independent
- Measure blood pressure for
both arms using the correct
cuff size. Take three reading 5
minutes apart when the
patient is sitting and at rest.
- Auscultate breath sounds
and heart tones.
-Note the presence of central
- Continuous diastolic
readings above
120mmHg for systolic is
an established risk factor
for ischemic heart and
cerebrovascular disease
even when the diastolic
pressure is nor elevated
(Abbott, 2016).
- S4 is commonly heard
in hypertensive patients.
Presence of crackles and
wheezes may indicate the
collapse of the upper
airway or pulmonary
congestion secondary to
developing heart failure
(Albert & Miracle,
2016).
7
Assessment data Diagnosis Intervention Rationale
Past medical history
- 76 year old with
hypertension,
hypercholesterolemia
and obstructive sleep
apnea
Social and family
history
- Smokes ten cigarettes
a day, father died of
heart failure and mother
pancreatic cancer
Observation
- Estimated blood loss in
OT 200ml
c. Risk of impaired
cardiovascular
function related to;
- age >65 years
- family history of
cardiovascular disease
- hypertension
- hypercholesterolemia
Independent
- Measure blood pressure for
both arms using the correct
cuff size. Take three reading 5
minutes apart when the
patient is sitting and at rest.
- Auscultate breath sounds
and heart tones.
-Note the presence of central
- Continuous diastolic
readings above
120mmHg for systolic is
an established risk factor
for ischemic heart and
cerebrovascular disease
even when the diastolic
pressure is nor elevated
(Abbott, 2016).
- S4 is commonly heard
in hypertensive patients.
Presence of crackles and
wheezes may indicate the
collapse of the upper
airway or pulmonary
congestion secondary to
developing heart failure
(Albert & Miracle,
2016).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
POSTOPERATIVE MANAGEMENT
8
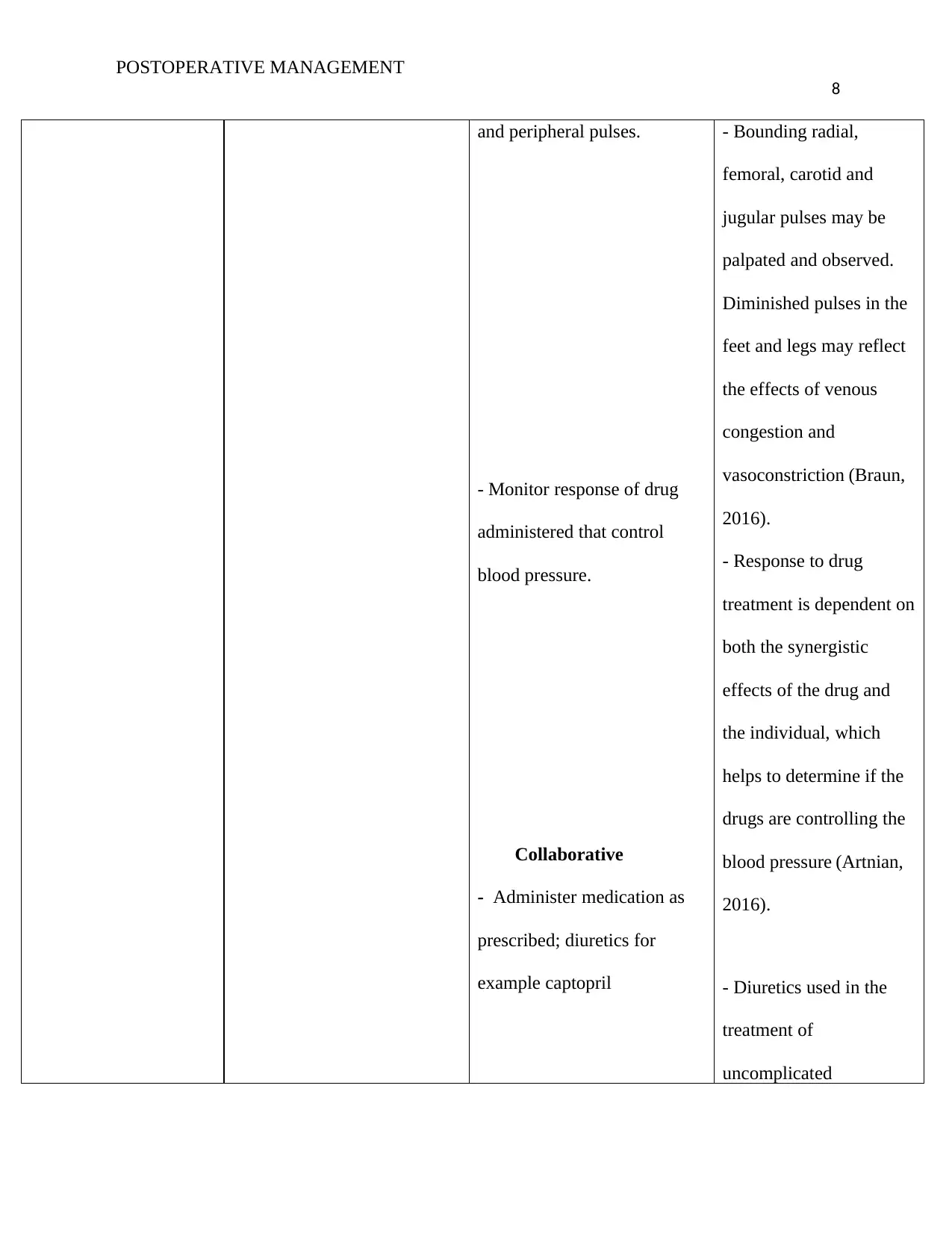
and peripheral pulses.
- Monitor response of drug
administered that control
blood pressure.
Collaborative
- Administer medication as
prescribed; diuretics for
example captopril
- Bounding radial,
femoral, carotid and
jugular pulses may be
palpated and observed.
Diminished pulses in the
feet and legs may reflect
the effects of venous
congestion and
vasoconstriction (Braun,
2016).
- Response to drug
treatment is dependent on
both the synergistic
effects of the drug and
the individual, which
helps to determine if the
drugs are controlling the
blood pressure (Artnian,
2016).
- Diuretics used in the
treatment of
uncomplicated
8
and peripheral pulses.
- Monitor response of drug
administered that control
blood pressure.
Collaborative
- Administer medication as
prescribed; diuretics for
example captopril
- Bounding radial,
femoral, carotid and
jugular pulses may be
palpated and observed.
Diminished pulses in the
feet and legs may reflect
the effects of venous
congestion and
vasoconstriction (Braun,
2016).
- Response to drug
treatment is dependent on
both the synergistic
effects of the drug and
the individual, which
helps to determine if the
drugs are controlling the
blood pressure (Artnian,
2016).
- Diuretics used in the
treatment of
uncomplicated
POSTOPERATIVE MANAGEMENT
9
hypertension. They
reduce blood pressure in
patients with a normal
renal function (Braun,
2016).
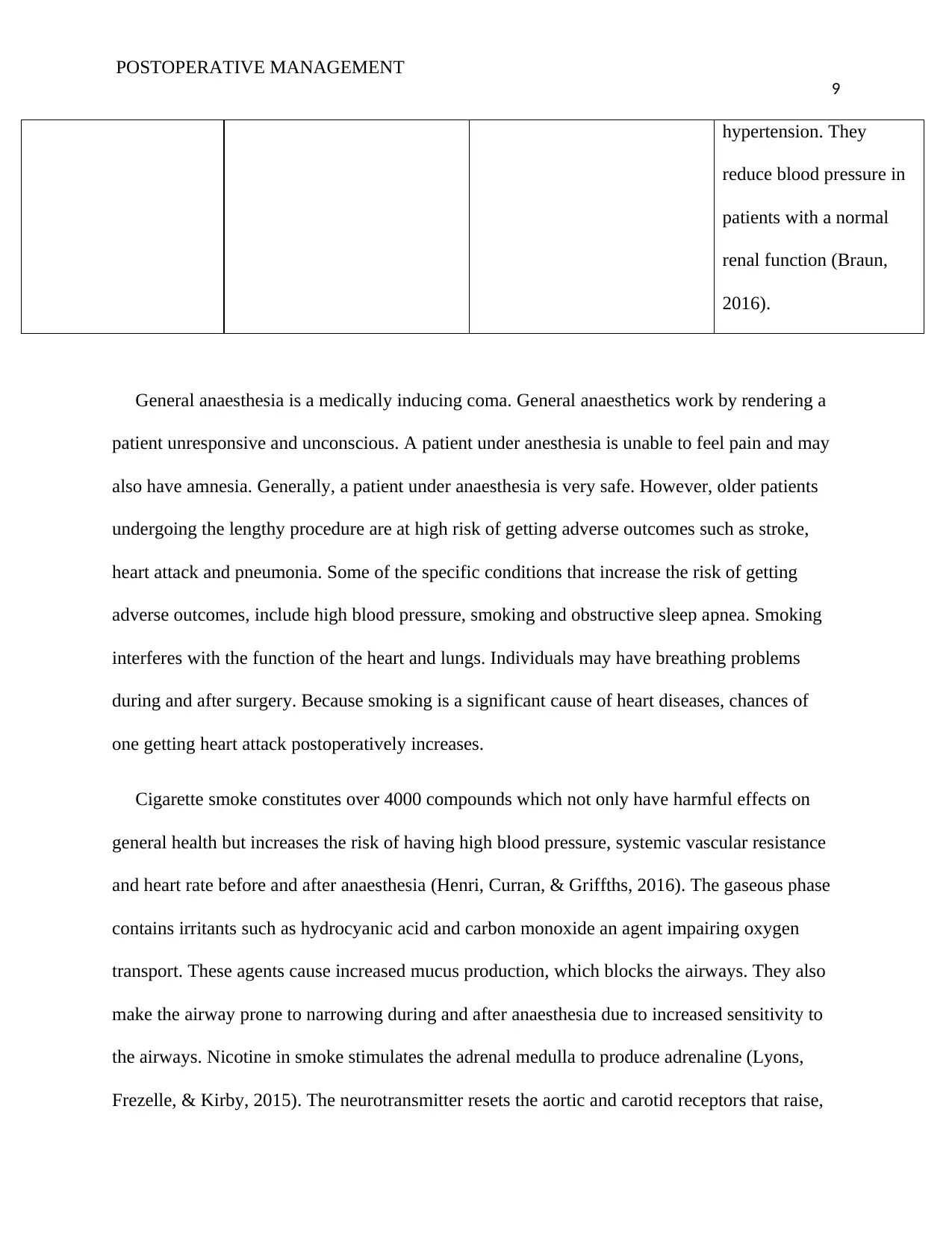
General anaesthesia is a medically inducing coma. General anaesthetics work by rendering a
patient unresponsive and unconscious. A patient under anesthesia is unable to feel pain and may
also have amnesia. Generally, a patient under anaesthesia is very safe. However, older patients
undergoing the lengthy procedure are at high risk of getting adverse outcomes such as stroke,
heart attack and pneumonia. Some of the specific conditions that increase the risk of getting
adverse outcomes, include high blood pressure, smoking and obstructive sleep apnea. Smoking
interferes with the function of the heart and lungs. Individuals may have breathing problems
during and after surgery. Because smoking is a significant cause of heart diseases, chances of
one getting heart attack postoperatively increases.
Cigarette smoke constitutes over 4000 compounds which not only have harmful effects on
general health but increases the risk of having high blood pressure, systemic vascular resistance
and heart rate before and after anaesthesia (Henri, Curran, & Griffths, 2016). The gaseous phase
contains irritants such as hydrocyanic acid and carbon monoxide an agent impairing oxygen
transport. These agents cause increased mucus production, which blocks the airways. They also
make the airway prone to narrowing during and after anaesthesia due to increased sensitivity to
the airways. Nicotine in smoke stimulates the adrenal medulla to produce adrenaline (Lyons,
Frezelle, & Kirby, 2015). The neurotransmitter resets the aortic and carotid receptors that raise,
9
hypertension. They
reduce blood pressure in
patients with a normal
renal function (Braun,
2016).
General anaesthesia is a medically inducing coma. General anaesthetics work by rendering a
patient unresponsive and unconscious. A patient under anesthesia is unable to feel pain and may
also have amnesia. Generally, a patient under anaesthesia is very safe. However, older patients
undergoing the lengthy procedure are at high risk of getting adverse outcomes such as stroke,
heart attack and pneumonia. Some of the specific conditions that increase the risk of getting
adverse outcomes, include high blood pressure, smoking and obstructive sleep apnea. Smoking
interferes with the function of the heart and lungs. Individuals may have breathing problems
during and after surgery. Because smoking is a significant cause of heart diseases, chances of
one getting heart attack postoperatively increases.
Cigarette smoke constitutes over 4000 compounds which not only have harmful effects on
general health but increases the risk of having high blood pressure, systemic vascular resistance
and heart rate before and after anaesthesia (Henri, Curran, & Griffths, 2016). The gaseous phase
contains irritants such as hydrocyanic acid and carbon monoxide an agent impairing oxygen
transport. These agents cause increased mucus production, which blocks the airways. They also
make the airway prone to narrowing during and after anaesthesia due to increased sensitivity to
the airways. Nicotine in smoke stimulates the adrenal medulla to produce adrenaline (Lyons,
Frezelle, & Kirby, 2015). The neurotransmitter resets the aortic and carotid receptors that raise,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
POSTOPERATIVE MANAGEMENT
10
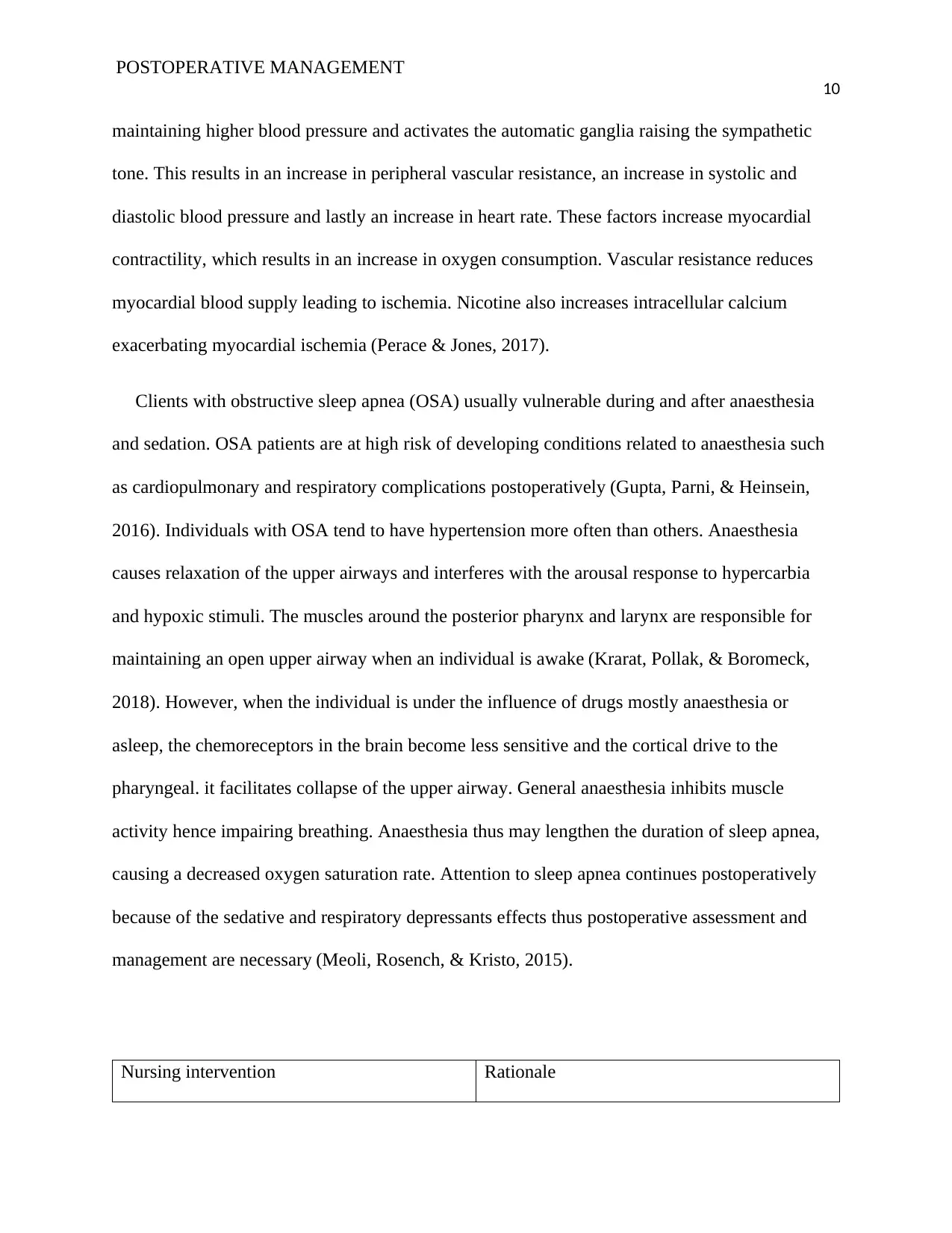
maintaining higher blood pressure and activates the automatic ganglia raising the sympathetic
tone. This results in an increase in peripheral vascular resistance, an increase in systolic and
diastolic blood pressure and lastly an increase in heart rate. These factors increase myocardial
contractility, which results in an increase in oxygen consumption. Vascular resistance reduces
myocardial blood supply leading to ischemia. Nicotine also increases intracellular calcium
exacerbating myocardial ischemia (Perace & Jones, 2017).
Clients with obstructive sleep apnea (OSA) usually vulnerable during and after anaesthesia
and sedation. OSA patients are at high risk of developing conditions related to anaesthesia such
as cardiopulmonary and respiratory complications postoperatively (Gupta, Parni, & Heinsein,
2016). Individuals with OSA tend to have hypertension more often than others. Anaesthesia
causes relaxation of the upper airways and interferes with the arousal response to hypercarbia
and hypoxic stimuli. The muscles around the posterior pharynx and larynx are responsible for
maintaining an open upper airway when an individual is awake (Krarat, Pollak, & Boromeck,
2018). However, when the individual is under the influence of drugs mostly anaesthesia or
asleep, the chemoreceptors in the brain become less sensitive and the cortical drive to the
pharyngeal. it facilitates collapse of the upper airway. General anaesthesia inhibits muscle
activity hence impairing breathing. Anaesthesia thus may lengthen the duration of sleep apnea,
causing a decreased oxygen saturation rate. Attention to sleep apnea continues postoperatively
because of the sedative and respiratory depressants effects thus postoperative assessment and
management are necessary (Meoli, Rosench, & Kristo, 2015).
Nursing intervention Rationale
10
maintaining higher blood pressure and activates the automatic ganglia raising the sympathetic
tone. This results in an increase in peripheral vascular resistance, an increase in systolic and
diastolic blood pressure and lastly an increase in heart rate. These factors increase myocardial
contractility, which results in an increase in oxygen consumption. Vascular resistance reduces
myocardial blood supply leading to ischemia. Nicotine also increases intracellular calcium
exacerbating myocardial ischemia (Perace & Jones, 2017).
Clients with obstructive sleep apnea (OSA) usually vulnerable during and after anaesthesia
and sedation. OSA patients are at high risk of developing conditions related to anaesthesia such
as cardiopulmonary and respiratory complications postoperatively (Gupta, Parni, & Heinsein,
2016). Individuals with OSA tend to have hypertension more often than others. Anaesthesia
causes relaxation of the upper airways and interferes with the arousal response to hypercarbia
and hypoxic stimuli. The muscles around the posterior pharynx and larynx are responsible for
maintaining an open upper airway when an individual is awake (Krarat, Pollak, & Boromeck,
2018). However, when the individual is under the influence of drugs mostly anaesthesia or
asleep, the chemoreceptors in the brain become less sensitive and the cortical drive to the
pharyngeal. it facilitates collapse of the upper airway. General anaesthesia inhibits muscle
activity hence impairing breathing. Anaesthesia thus may lengthen the duration of sleep apnea,
causing a decreased oxygen saturation rate. Attention to sleep apnea continues postoperatively
because of the sedative and respiratory depressants effects thus postoperative assessment and
management are necessary (Meoli, Rosench, & Kristo, 2015).
Nursing intervention Rationale
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
POSTOPERATIVE MANAGEMENT
11
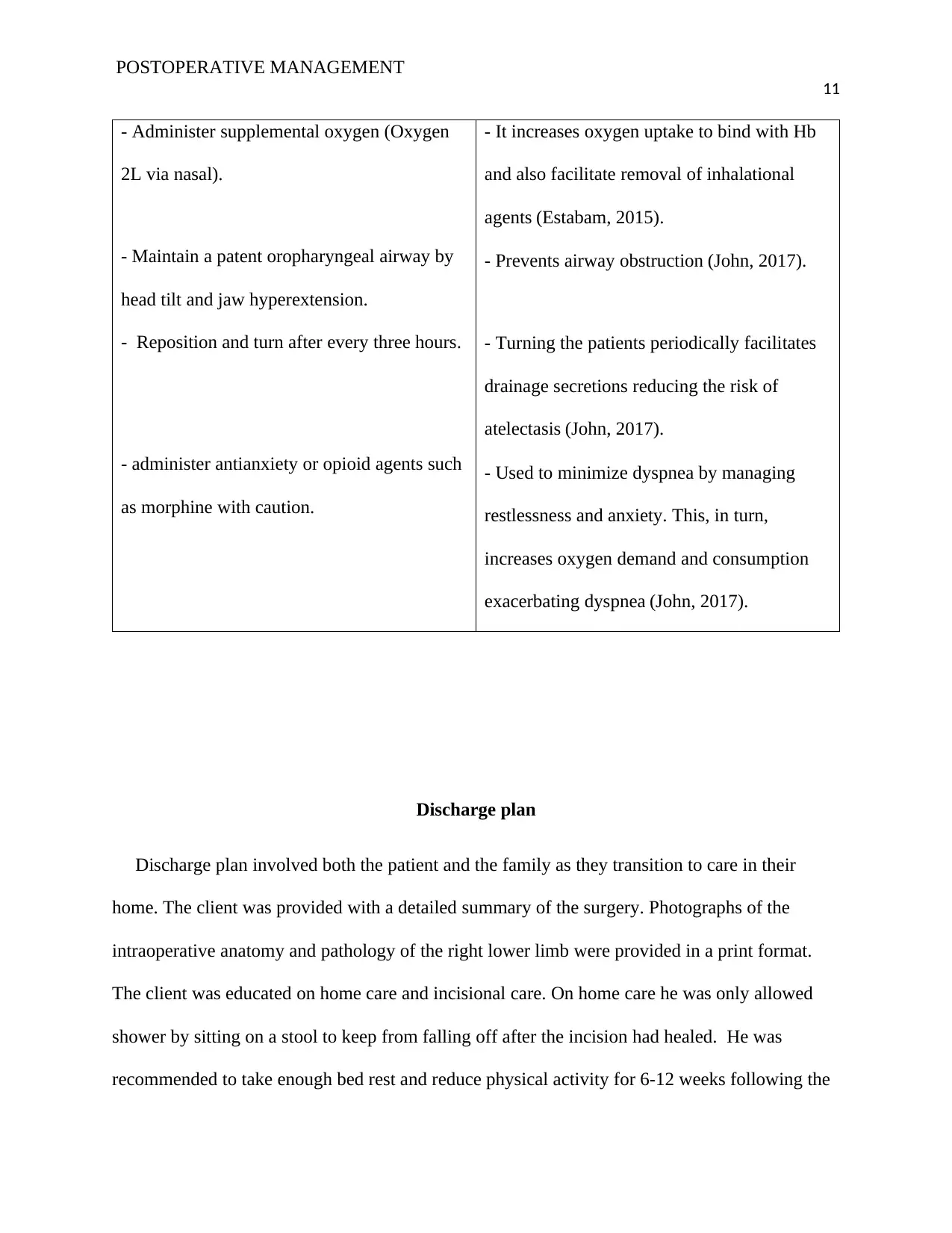
- Administer supplemental oxygen (Oxygen
2L via nasal).
- Maintain a patent oropharyngeal airway by
head tilt and jaw hyperextension.
- Reposition and turn after every three hours.
- administer antianxiety or opioid agents such
as morphine with caution.
- It increases oxygen uptake to bind with Hb
and also facilitate removal of inhalational
agents (Estabam, 2015).
- Prevents airway obstruction (John, 2017).
- Turning the patients periodically facilitates
drainage secretions reducing the risk of
atelectasis (John, 2017).
- Used to minimize dyspnea by managing
restlessness and anxiety. This, in turn,
increases oxygen demand and consumption
exacerbating dyspnea (John, 2017).
Discharge plan
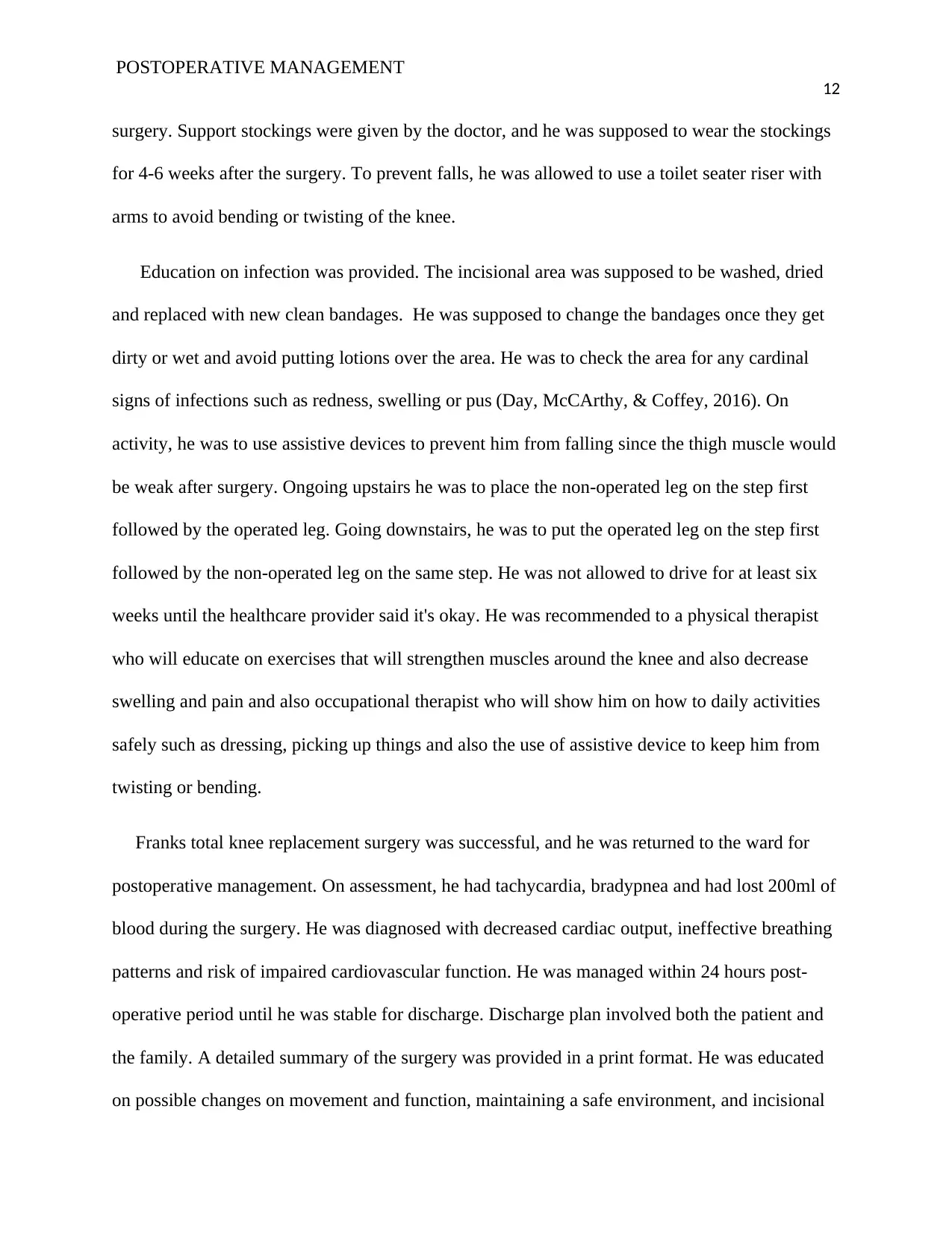
Discharge plan involved both the patient and the family as they transition to care in their
home. The client was provided with a detailed summary of the surgery. Photographs of the
intraoperative anatomy and pathology of the right lower limb were provided in a print format.
The client was educated on home care and incisional care. On home care he was only allowed
shower by sitting on a stool to keep from falling off after the incision had healed. He was
recommended to take enough bed rest and reduce physical activity for 6-12 weeks following the
11
- Administer supplemental oxygen (Oxygen
2L via nasal).
- Maintain a patent oropharyngeal airway by
head tilt and jaw hyperextension.
- Reposition and turn after every three hours.
- administer antianxiety or opioid agents such
as morphine with caution.
- It increases oxygen uptake to bind with Hb
and also facilitate removal of inhalational
agents (Estabam, 2015).
- Prevents airway obstruction (John, 2017).
- Turning the patients periodically facilitates
drainage secretions reducing the risk of
atelectasis (John, 2017).
- Used to minimize dyspnea by managing
restlessness and anxiety. This, in turn,
increases oxygen demand and consumption
exacerbating dyspnea (John, 2017).
Discharge plan
Discharge plan involved both the patient and the family as they transition to care in their
home. The client was provided with a detailed summary of the surgery. Photographs of the
intraoperative anatomy and pathology of the right lower limb were provided in a print format.
The client was educated on home care and incisional care. On home care he was only allowed
shower by sitting on a stool to keep from falling off after the incision had healed. He was
recommended to take enough bed rest and reduce physical activity for 6-12 weeks following the
POSTOPERATIVE MANAGEMENT
12
surgery. Support stockings were given by the doctor, and he was supposed to wear the stockings
for 4-6 weeks after the surgery. To prevent falls, he was allowed to use a toilet seater riser with
arms to avoid bending or twisting of the knee.
Education on infection was provided. The incisional area was supposed to be washed, dried
and replaced with new clean bandages. He was supposed to change the bandages once they get
dirty or wet and avoid putting lotions over the area. He was to check the area for any cardinal
signs of infections such as redness, swelling or pus (Day, McCArthy, & Coffey, 2016). On
activity, he was to use assistive devices to prevent him from falling since the thigh muscle would
be weak after surgery. Ongoing upstairs he was to place the non-operated leg on the step first
followed by the operated leg. Going downstairs, he was to put the operated leg on the step first
followed by the non-operated leg on the same step. He was not allowed to drive for at least six
weeks until the healthcare provider said it's okay. He was recommended to a physical therapist
who will educate on exercises that will strengthen muscles around the knee and also decrease
swelling and pain and also occupational therapist who will show him on how to daily activities
safely such as dressing, picking up things and also the use of assistive device to keep him from
twisting or bending.
Franks total knee replacement surgery was successful, and he was returned to the ward for
postoperative management. On assessment, he had tachycardia, bradypnea and had lost 200ml of
blood during the surgery. He was diagnosed with decreased cardiac output, ineffective breathing
patterns and risk of impaired cardiovascular function. He was managed within 24 hours post-
operative period until he was stable for discharge. Discharge plan involved both the patient and
the family. A detailed summary of the surgery was provided in a print format. He was educated
on possible changes on movement and function, maintaining a safe environment, and incisional
12
surgery. Support stockings were given by the doctor, and he was supposed to wear the stockings
for 4-6 weeks after the surgery. To prevent falls, he was allowed to use a toilet seater riser with
arms to avoid bending or twisting of the knee.
Education on infection was provided. The incisional area was supposed to be washed, dried
and replaced with new clean bandages. He was supposed to change the bandages once they get
dirty or wet and avoid putting lotions over the area. He was to check the area for any cardinal
signs of infections such as redness, swelling or pus (Day, McCArthy, & Coffey, 2016). On
activity, he was to use assistive devices to prevent him from falling since the thigh muscle would
be weak after surgery. Ongoing upstairs he was to place the non-operated leg on the step first
followed by the operated leg. Going downstairs, he was to put the operated leg on the step first
followed by the non-operated leg on the same step. He was not allowed to drive for at least six
weeks until the healthcare provider said it's okay. He was recommended to a physical therapist
who will educate on exercises that will strengthen muscles around the knee and also decrease
swelling and pain and also occupational therapist who will show him on how to daily activities
safely such as dressing, picking up things and also the use of assistive device to keep him from
twisting or bending.
Franks total knee replacement surgery was successful, and he was returned to the ward for
postoperative management. On assessment, he had tachycardia, bradypnea and had lost 200ml of
blood during the surgery. He was diagnosed with decreased cardiac output, ineffective breathing
patterns and risk of impaired cardiovascular function. He was managed within 24 hours post-
operative period until he was stable for discharge. Discharge plan involved both the patient and
the family. A detailed summary of the surgery was provided in a print format. He was educated
on possible changes on movement and function, maintaining a safe environment, and incisional
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
POSTOPERATIVE MANAGEMENT
13
care. He was recommended to an occupational therapist and physical therapist who will educate
on exercise that would strengthen the muscle around the knee and decrease swelling.
References
Abbott, A. (2016). Diagnostic approach to palpitations. Am Fam Physician, 71(4), 743-755.
Albert, N., & Miracle, V. (2016). Cardiac biomarkers: Past, present, and future. Am J Crit
Care, 7(6), 418-423.
Artnian, M. (2016). Innovations in blood pressure monitoring. AJN, 104(8), 53-60.
Braun, L. (2016). Cardiovascular disease: Strategies for risk assessment and modification.
Cardiovas Nurs, 21(6), 20-42.
13
care. He was recommended to an occupational therapist and physical therapist who will educate
on exercise that would strengthen the muscle around the knee and decrease swelling.
References
Abbott, A. (2016). Diagnostic approach to palpitations. Am Fam Physician, 71(4), 743-755.
Albert, N., & Miracle, V. (2016). Cardiac biomarkers: Past, present, and future. Am J Crit
Care, 7(6), 418-423.
Artnian, M. (2016). Innovations in blood pressure monitoring. AJN, 104(8), 53-60.
Braun, L. (2016). Cardiovascular disease: Strategies for risk assessment and modification.
Cardiovas Nurs, 21(6), 20-42.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
POSTOPERATIVE MANAGEMENT
14
Braun, L. (2016). Cholesterol-lowering drugs bring benefits to high-risk populations, even
when LDL is normal. J Cardiovasc Nurs, 18(1), 44-49.
Cross, S. (2015). Managing exacerbations of chronic obstructive pulmonary disease. Br J
Nurs, 14(11), 607-609.
Dasta, J. (2017). The daily cost of an intensive care unit day: The contribution of mechanical
ventilation. Crit Care Med, 33(6), 1266-1271.
Day, M., McCArthy, G., & Coffey, A. (2016). Discharge planning: the role of the discharge
coordinator. Nursing older people, 34, 67-69.
Estabam, A. (2015). Characteristics and outcomes in adult patients receiving mechanical
ventilation. JAMA, 287, 354-355.
Gupta, R., Parni, J., & Heinsein, J. (2016). Postoperative complication in patients with
obstructive sleep apnea syndrome undergoing hip or knee replacement; a case-control
study. Mayo Clinic, 23, 897.
Henri, J., Curran, J., & Griffths, D. (2016). Smokers and hemodynamics responses to
desflurane. Anesthesia, 54, 800-802.
John, S. (2017). Protocols for practice: Applying research at the bedside— airway
management. Crit Care Nurse, 19(4), 79-83.
Krarat, R., Pollak, P., & Boromeck, B. (2018). Obstructive sleep apnea and death associated
with surgical corrections of velopharyngeal incompetence. J Pediatric, 96, 645-648.
Lyons, B., Frezelle, H., & Kirby, F. (2015). The effects of passive smoking on the incidence
of airway complication in adults undergoing anesthesia. Anesthesia, 51, 324-326.
14
Braun, L. (2016). Cholesterol-lowering drugs bring benefits to high-risk populations, even
when LDL is normal. J Cardiovasc Nurs, 18(1), 44-49.
Cross, S. (2015). Managing exacerbations of chronic obstructive pulmonary disease. Br J
Nurs, 14(11), 607-609.
Dasta, J. (2017). The daily cost of an intensive care unit day: The contribution of mechanical
ventilation. Crit Care Med, 33(6), 1266-1271.
Day, M., McCArthy, G., & Coffey, A. (2016). Discharge planning: the role of the discharge
coordinator. Nursing older people, 34, 67-69.
Estabam, A. (2015). Characteristics and outcomes in adult patients receiving mechanical
ventilation. JAMA, 287, 354-355.
Gupta, R., Parni, J., & Heinsein, J. (2016). Postoperative complication in patients with
obstructive sleep apnea syndrome undergoing hip or knee replacement; a case-control
study. Mayo Clinic, 23, 897.
Henri, J., Curran, J., & Griffths, D. (2016). Smokers and hemodynamics responses to
desflurane. Anesthesia, 54, 800-802.
John, S. (2017). Protocols for practice: Applying research at the bedside— airway
management. Crit Care Nurse, 19(4), 79-83.
Krarat, R., Pollak, P., & Boromeck, B. (2018). Obstructive sleep apnea and death associated
with surgical corrections of velopharyngeal incompetence. J Pediatric, 96, 645-648.
Lyons, B., Frezelle, H., & Kirby, F. (2015). The effects of passive smoking on the incidence
of airway complication in adults undergoing anesthesia. Anesthesia, 51, 324-326.
POSTOPERATIVE MANAGEMENT
15
Meoli, A., Rosench, L., & Kristo, D. (2015). Upper airway management of adult patients
with obstructive sleep apnea in the perioperative period-avoiding complications.
Sleep, 45, 1060-1065.
Perace, A., & Jones, M. (2017). Smoking and anesthesia: preoperative abstinence and
perioperative morbidity. Anesthesiology, 61, 576-584.
15
Meoli, A., Rosench, L., & Kristo, D. (2015). Upper airway management of adult patients
with obstructive sleep apnea in the perioperative period-avoiding complications.
Sleep, 45, 1060-1065.
Perace, A., & Jones, M. (2017). Smoking and anesthesia: preoperative abstinence and
perioperative morbidity. Anesthesiology, 61, 576-584.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 15
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





