Nurses' Attitude and Knowledge of ECT: Practice Change Proposal
VerifiedAdded on 2023/02/01
|16
|4337
|76
Report
AI Summary
This practice change proposal, authored by a mental health nurse with extensive experience, addresses the need to improve nurses' attitudes and knowledge regarding electroconvulsive therapy (ECT). The project aims to understand the factors contributing to negative perceptions of ECT, including inadequate training, adherence to guidelines, and multidisciplinary incoherence. The proposal outlines a mixed-methods approach to assess nurses' current attitudes and knowledge, followed by the implementation of a practice change model involving knowledge transformation, exchange, and organizational change theory. The project seeks to enhance nurses' understanding of ECT's efficacy, ethical considerations, and its role in treating severe mental health conditions like depression and schizophrenia. The ultimate goal is to foster a more positive and informed approach to ECT, leading to improved patient care and outcomes. The project emphasizes the importance of therapeutic relationships and the need for nurses to be well-equipped to support patients undergoing ECT.

RUNNING HEAD: PRACTISE PROPOSAL
PRACTISE PROPOSAL
Name of Student
Name of University
Author note
PRACTISE PROPOSAL
Name of Student
Name of University
Author note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1PRACTICE PROPOSAL
Assessment – Practice change proposal
Changing nurses attitude towards the practice and knowledge of ECT
Applicant’s details:-
As a mental health nurse with an experience of more than 10 years and working as a
mental clinical nurse consultant, I have observed many changes in the interventional
approaches of mental health care – in order to manage many acute and chronic condition in
an evolved way. My qualifications are B.Sc and M.Sc in nursing. My good and bad
experiences with clinical practice of mental health has pushed me to take up a project on
practice change in negative or awkward attitudes in nursing practice towards the application
of electroconvulsive therapy.
Overview of Project:-
This practise development project will be aimed at improving the attitude of nurses
towards the knowledge and practise of electroconvulsive therapy in mental health care. The
project uses an evidence based practise change model to address the aim and methodology of
the study. The model uses explanatory (Nardi 2018) and analytic methods (Hirschi and Selvin
2017) to analyse the rationale to bring in a purposeful change. The project focuses on
understanding the covert social and cognitive mechanisms (Dahl, Lutz and Davidson 2015)
leading to the development of negative or frantic behaviours (Sinclair, Seydel, and Shaw
2017) in nurses when asked to relate to electroconvulsive therapy. The project also extends
its framework to analyse the perceptual blocks (Witt, Tenhundfeld and Bielak 2017) in many
nurses about the ‘experience’ of electro convulsive therapy in patients, they had been treating
for a long time and has developed a therapeutic bond with. The project uses varied data
collection and data analysis methods in order to inter – relate with ongoing perceptions about
the clinical practise of electroconvulsive therapy and how ethically correct – the therapy is.
Assessment – Practice change proposal
Changing nurses attitude towards the practice and knowledge of ECT
Applicant’s details:-
As a mental health nurse with an experience of more than 10 years and working as a
mental clinical nurse consultant, I have observed many changes in the interventional
approaches of mental health care – in order to manage many acute and chronic condition in
an evolved way. My qualifications are B.Sc and M.Sc in nursing. My good and bad
experiences with clinical practice of mental health has pushed me to take up a project on
practice change in negative or awkward attitudes in nursing practice towards the application
of electroconvulsive therapy.
Overview of Project:-
This practise development project will be aimed at improving the attitude of nurses
towards the knowledge and practise of electroconvulsive therapy in mental health care. The
project uses an evidence based practise change model to address the aim and methodology of
the study. The model uses explanatory (Nardi 2018) and analytic methods (Hirschi and Selvin
2017) to analyse the rationale to bring in a purposeful change. The project focuses on
understanding the covert social and cognitive mechanisms (Dahl, Lutz and Davidson 2015)
leading to the development of negative or frantic behaviours (Sinclair, Seydel, and Shaw
2017) in nurses when asked to relate to electroconvulsive therapy. The project also extends
its framework to analyse the perceptual blocks (Witt, Tenhundfeld and Bielak 2017) in many
nurses about the ‘experience’ of electro convulsive therapy in patients, they had been treating
for a long time and has developed a therapeutic bond with. The project uses varied data
collection and data analysis methods in order to inter – relate with ongoing perceptions about
the clinical practise of electroconvulsive therapy and how ethically correct – the therapy is.
2PRACTICE PROPOSAL
Hence, the study will explore into many areas of ethical dilemmas related to the use of
‘electroconvulsive therapy’ (Joshi et al.2016) in the modern clinical environment and how
does it affects the other patients in the wards and professionals working closely with them.
The methods that will be used in the research design should be able to analyse the
deficiencies of mental health nursing (Brown 2015) in regards to managing acute
behavioural, cognitive, personality and neuropsychological cases. The deficiencies would be
investigated from different perspectives like –
a) inadequate nursing education (Barton, Bruce and Schreiber 2018)
b).non-adherence to clinical guidelines (Arts et al. 2016)
c). incoherence in multidisciplinary approach planned around an acute mental condition
d). Lack in nursing training programs (Douglas and Affoo 2018).
e) knowledge gap(Démeh and Rosengren 2015)
f) missed areas in clinical mental nursing (Orthwein 2017).
The study will be aimed to an understanding of nurses' attitude and knowledge towards
electro-convulsive therapy and to explore whether this knowledge and the previous
experiences of electroconvulsive therapy can be correlated with a gradually developed
positive attitude towards the ‘controversial’ treatment (Sadowsky 2016) that has question
logic, reasoning and ethical dilemmas (Doherty & Purtilo 2015) over the decades. The
practice change will also focus on immediate and long term goals to be achieved within an
organizational framework for sustenance of the ‘attitude change’ and how this ‘acquired
knowledge’ can be blended with the learning of future nurses (Glegg et al. 2017). Of course,
that would take a standardization, quality check and a ‘drastic’ change in the practice
perception in accordance with usage of electroconvulsive therapy. As to cater to the practice
Hence, the study will explore into many areas of ethical dilemmas related to the use of
‘electroconvulsive therapy’ (Joshi et al.2016) in the modern clinical environment and how
does it affects the other patients in the wards and professionals working closely with them.
The methods that will be used in the research design should be able to analyse the
deficiencies of mental health nursing (Brown 2015) in regards to managing acute
behavioural, cognitive, personality and neuropsychological cases. The deficiencies would be
investigated from different perspectives like –
a) inadequate nursing education (Barton, Bruce and Schreiber 2018)
b).non-adherence to clinical guidelines (Arts et al. 2016)
c). incoherence in multidisciplinary approach planned around an acute mental condition
d). Lack in nursing training programs (Douglas and Affoo 2018).
e) knowledge gap(Démeh and Rosengren 2015)
f) missed areas in clinical mental nursing (Orthwein 2017).
The study will be aimed to an understanding of nurses' attitude and knowledge towards
electro-convulsive therapy and to explore whether this knowledge and the previous
experiences of electroconvulsive therapy can be correlated with a gradually developed
positive attitude towards the ‘controversial’ treatment (Sadowsky 2016) that has question
logic, reasoning and ethical dilemmas (Doherty & Purtilo 2015) over the decades. The
practice change will also focus on immediate and long term goals to be achieved within an
organizational framework for sustenance of the ‘attitude change’ and how this ‘acquired
knowledge’ can be blended with the learning of future nurses (Glegg et al. 2017). Of course,
that would take a standardization, quality check and a ‘drastic’ change in the practice
perception in accordance with usage of electroconvulsive therapy. As to cater to the practice
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3PRACTICE PROPOSAL
change model that is to be used in the proposed research would be will act by knowledge
transformation process (Pham & Nguyen 2017), knowledge exchange (Tjoflåt et al. 2017)
within the professional and organizations social and cultural framework, ‘synthesis of
application and inquiry’ (Moran, Burson and Conrad 2016) organizational change theory to
adopt to new practice setting and the pace in uptake of the new clinical environment and
practice modifications. The project methodology will be determined on studying the nurse –
patient collaboration in a mental health setting and to what extend a pact is feasible, given the
behavioral and personality distortions resulting in aggressive, indifferent or extremely
unexpected patient behaviors. A mixed methods procedure will be incorporated with research
design to achieve the desired results with any personal bias from the researcher’s side. The
analysis and interpretation techniques will keep in check, any sort of patient irritation or
digression from the main aim of the project.
Background and Need for Project:
For a therapeutic relationship to take place - the nurse has to generally work inside the
emotional loop of the patient. Nurses tend to spend most of the therapeutic time that a patient
spends in the hospital. Hence, nursing knowledge complemented with a positive attitude to
electroconvulsive therapy is vital because through the therapeutic bond, the nurses will be
able to transfer the same knowledge to the patients. The history of electroconvulsive therapy
runs back to 1930s when it was first devised and administered as a therapeutic method in the
psychiatry world. Slowly with randomized and regular practices – Electro Convulsive
Therapy proved to a life-saving intervention in extreme depression, as it acted on the neural
circuits acting on behavioral planning to reduce suicidal ideations and attempts. Some studies
indicated Electro Convulsive Therapy for depression while in majority of the western world
especially in Europe, ECT was primarily indicated for schizophrenia. It was thought that
electro convulsive therapy might cause brain tissue damage, functional circuit breaks,
change model that is to be used in the proposed research would be will act by knowledge
transformation process (Pham & Nguyen 2017), knowledge exchange (Tjoflåt et al. 2017)
within the professional and organizations social and cultural framework, ‘synthesis of
application and inquiry’ (Moran, Burson and Conrad 2016) organizational change theory to
adopt to new practice setting and the pace in uptake of the new clinical environment and
practice modifications. The project methodology will be determined on studying the nurse –
patient collaboration in a mental health setting and to what extend a pact is feasible, given the
behavioral and personality distortions resulting in aggressive, indifferent or extremely
unexpected patient behaviors. A mixed methods procedure will be incorporated with research
design to achieve the desired results with any personal bias from the researcher’s side. The
analysis and interpretation techniques will keep in check, any sort of patient irritation or
digression from the main aim of the project.
Background and Need for Project:
For a therapeutic relationship to take place - the nurse has to generally work inside the
emotional loop of the patient. Nurses tend to spend most of the therapeutic time that a patient
spends in the hospital. Hence, nursing knowledge complemented with a positive attitude to
electroconvulsive therapy is vital because through the therapeutic bond, the nurses will be
able to transfer the same knowledge to the patients. The history of electroconvulsive therapy
runs back to 1930s when it was first devised and administered as a therapeutic method in the
psychiatry world. Slowly with randomized and regular practices – Electro Convulsive
Therapy proved to a life-saving intervention in extreme depression, as it acted on the neural
circuits acting on behavioral planning to reduce suicidal ideations and attempts. Some studies
indicated Electro Convulsive Therapy for depression while in majority of the western world
especially in Europe, ECT was primarily indicated for schizophrenia. It was thought that
electro convulsive therapy might cause brain tissue damage, functional circuit breaks,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4PRACTICE PROPOSAL
epilepsy and slowed neuronal processing but many research studies confirmed otherwise. It
was also feared that ECT causes total amnesia but later with scientific researches undertaken
in the field of psychology and psychiatry assured that loss of memory is generally temporary
in ECT and it never affects the autobiographical and emotional memories.
Hungarian studies on the contrary, showed a decline by 80% in the last few years.
Even Chuvash Republic psychiatrists proposed ECT to be used at very last when other
interventions has failed. One-third of Greek psychiatrists accepted ECT as a positive
treatment while most of the Romanian psychiatrists exhibited a receptive behavior towards
the usage of ECT. The prime reason behind the declined usage of ECT is the lack of scientific
knowledge. Various studies on an average, have recommended the availability of ECT
devices in their clinics so that they can use it when it is absolutely required.
Electroconvulsive therapy was first used as a cure for patients with schizophrenia in
the year of 1938 (Selek, S. and Quevedo, J., 2019). With the turn of the decade, the
emergence of antipsychotic medicines dominated the psychiatry practice – thus reducing the
usage of ECT considerably. However, to manage treatment-resistant schizophrenia, the prime
and only form is of treatment of ECT. ECT can also be used in conjunction with
antipsychotics medications in the management of schizophrenia (Li 2017) Combination of
antipsychotic medication and ECT has a better prognostic outcome advantage. ECT has been
also reported to be very useful in treating schizophrenia associated catatonia.
In the timeline from 1950 to 1970, ECT was been reported to be done without using
anaesthetic and without consent as well which led to conception of negative social perception
and resistance to the usage of ECT. Films have often exaggerated the barbaric aspect of the
medical procedure which never the complete truth. The worst possible adverse effect of ECT
can be memory loss which can also happen in epileptic seizures. As mentioned above – it is
epilepsy and slowed neuronal processing but many research studies confirmed otherwise. It
was also feared that ECT causes total amnesia but later with scientific researches undertaken
in the field of psychology and psychiatry assured that loss of memory is generally temporary
in ECT and it never affects the autobiographical and emotional memories.
Hungarian studies on the contrary, showed a decline by 80% in the last few years.
Even Chuvash Republic psychiatrists proposed ECT to be used at very last when other
interventions has failed. One-third of Greek psychiatrists accepted ECT as a positive
treatment while most of the Romanian psychiatrists exhibited a receptive behavior towards
the usage of ECT. The prime reason behind the declined usage of ECT is the lack of scientific
knowledge. Various studies on an average, have recommended the availability of ECT
devices in their clinics so that they can use it when it is absolutely required.
Electroconvulsive therapy was first used as a cure for patients with schizophrenia in
the year of 1938 (Selek, S. and Quevedo, J., 2019). With the turn of the decade, the
emergence of antipsychotic medicines dominated the psychiatry practice – thus reducing the
usage of ECT considerably. However, to manage treatment-resistant schizophrenia, the prime
and only form is of treatment of ECT. ECT can also be used in conjunction with
antipsychotics medications in the management of schizophrenia (Li 2017) Combination of
antipsychotic medication and ECT has a better prognostic outcome advantage. ECT has been
also reported to be very useful in treating schizophrenia associated catatonia.
In the timeline from 1950 to 1970, ECT was been reported to be done without using
anaesthetic and without consent as well which led to conception of negative social perception
and resistance to the usage of ECT. Films have often exaggerated the barbaric aspect of the
medical procedure which never the complete truth. The worst possible adverse effect of ECT
can be memory loss which can also happen in epileptic seizures. As mentioned above – it is
5PRACTICE PROPOSAL
often transient but it can be experienced differently by different subject with varied levels of
anxiety.
ECT is a psychiatry treatment which acts on the neuropsychological system by
transmitting a wave of electric current into specific areas of the brain to intentionally trigger a
seizure which breaks the disruptive cognitive cycle – relieving the patients of symptoms.
ECT is primarily used in life-threatening stages of depression, or medication resistant
schizophrenia and severe stages of postnatal depression. The ECT treatment is administered
under a preliminary cover of using muscle relaxants and general anesthesia so as to prevent
any chances of actual convulsions in the body. Psychotic episode and manic patients
exhibiting medication-resistant episodes of catatonia can be treated well with ECT. It can be
used in disease related depression with much good effect. But ECT has always proven to be
highly efficient in relieving patients with major depression. ECT has proven its efficacy in
major depression by improving the disruptive symptoms by almost 80 per cent. Other mental
illness with bipolar disorder and hallucination disorders can be treated with controlled ECT.
Catatonia is a human condition when the subject becomes increasingly frozen and agitated
with repetition of one particular movement over a period of time. Catatonia can be life
threatening as it can lead to self-harm, self-injury and even dehydration.. ECT can be
administered as a rapid prognostic betterment intervention in suicidal behaviors. ECT’s
effectiveness has been recognized by the National Institute of Mental Health, the American
Medical Association and American Psychiatric Association. Globally, with boom of clinical
knowledge and clinical reasoning protocols – ECT has also gained importance in countries
like Canada and Great Britain. Although ECT is useful in limiting violent life threatening
behaviors, it is not a complete cure. Counseling, psychotherapy and medications should be
continued in conjunction with ECT for complete recovery.
often transient but it can be experienced differently by different subject with varied levels of
anxiety.
ECT is a psychiatry treatment which acts on the neuropsychological system by
transmitting a wave of electric current into specific areas of the brain to intentionally trigger a
seizure which breaks the disruptive cognitive cycle – relieving the patients of symptoms.
ECT is primarily used in life-threatening stages of depression, or medication resistant
schizophrenia and severe stages of postnatal depression. The ECT treatment is administered
under a preliminary cover of using muscle relaxants and general anesthesia so as to prevent
any chances of actual convulsions in the body. Psychotic episode and manic patients
exhibiting medication-resistant episodes of catatonia can be treated well with ECT. It can be
used in disease related depression with much good effect. But ECT has always proven to be
highly efficient in relieving patients with major depression. ECT has proven its efficacy in
major depression by improving the disruptive symptoms by almost 80 per cent. Other mental
illness with bipolar disorder and hallucination disorders can be treated with controlled ECT.
Catatonia is a human condition when the subject becomes increasingly frozen and agitated
with repetition of one particular movement over a period of time. Catatonia can be life
threatening as it can lead to self-harm, self-injury and even dehydration.. ECT can be
administered as a rapid prognostic betterment intervention in suicidal behaviors. ECT’s
effectiveness has been recognized by the National Institute of Mental Health, the American
Medical Association and American Psychiatric Association. Globally, with boom of clinical
knowledge and clinical reasoning protocols – ECT has also gained importance in countries
like Canada and Great Britain. Although ECT is useful in limiting violent life threatening
behaviors, it is not a complete cure. Counseling, psychotherapy and medications should be
continued in conjunction with ECT for complete recovery.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6PRACTICE PROPOSAL
Procedure of application – Before starting ECT sessions, a patient must be
sedated under anesthesia and should be administered with a prescribed dose of muscle
relaxants. The electrodes are then placed on scalp of the subject. Then a finely timed and
therapeutic dose of electric current is administered that triggers a controlled seizure in the
brain. The influence of muscle relaxants keeps the subject from painful and any severe
convulsive attacks. The seizure also limits the ‘circuit break’ to just a frail movement of feet
and hands. Patients should be carefully and closely monitored by the practitioner and nurses
during the course of intervention. The subject should be awakened after the intervention who
should wake up remembering nothing about it. The dose of ECT – is generally three times a
week for a period of 2 to four weeks.
Hence strategies including attitude, knowledge and practice change is imperative to
bring about a positive attitude change in the nursing community regarding the ethical
incorporation of nursing principles while treating patients of mental health. Being
compassionate, kind and open to the mental health patients is the first thing that has to
practiced and then from an important nursing point of view – avoiding confrontation and
complying with patient centered treatment guidelines has to be an important facet of best
clinical practice. While handling acute mental health patients suffering with schizophrenia,
bipolar disorder or depression, extra skills in term of behavioral, social and humanitarian –
are cardinal to become a good and competent mental health nurse. More than just managing a
depressed or neuropsychological patient with hallucinations and severe self-harm threats –
compliance with the aggressive behavior control or symptomatic control strategies like
electro convulsive therapies often creates a negative perception in an attending nurse’s mind.
This is where knowledge and proper training of a nurse in developing a reasoned and
practical attitude towards the treatment of a depressed or schizophrenic patient with electro
convulsive therapy is pivotal towards a better patient centered care in mental health setting.
Procedure of application – Before starting ECT sessions, a patient must be
sedated under anesthesia and should be administered with a prescribed dose of muscle
relaxants. The electrodes are then placed on scalp of the subject. Then a finely timed and
therapeutic dose of electric current is administered that triggers a controlled seizure in the
brain. The influence of muscle relaxants keeps the subject from painful and any severe
convulsive attacks. The seizure also limits the ‘circuit break’ to just a frail movement of feet
and hands. Patients should be carefully and closely monitored by the practitioner and nurses
during the course of intervention. The subject should be awakened after the intervention who
should wake up remembering nothing about it. The dose of ECT – is generally three times a
week for a period of 2 to four weeks.
Hence strategies including attitude, knowledge and practice change is imperative to
bring about a positive attitude change in the nursing community regarding the ethical
incorporation of nursing principles while treating patients of mental health. Being
compassionate, kind and open to the mental health patients is the first thing that has to
practiced and then from an important nursing point of view – avoiding confrontation and
complying with patient centered treatment guidelines has to be an important facet of best
clinical practice. While handling acute mental health patients suffering with schizophrenia,
bipolar disorder or depression, extra skills in term of behavioral, social and humanitarian –
are cardinal to become a good and competent mental health nurse. More than just managing a
depressed or neuropsychological patient with hallucinations and severe self-harm threats –
compliance with the aggressive behavior control or symptomatic control strategies like
electro convulsive therapies often creates a negative perception in an attending nurse’s mind.
This is where knowledge and proper training of a nurse in developing a reasoned and
practical attitude towards the treatment of a depressed or schizophrenic patient with electro
convulsive therapy is pivotal towards a better patient centered care in mental health setting.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7PRACTICE PROPOSAL
Project aims and objectives:
To achieve the project objectives which is to address the attitude and knowledge
issues in nursing are to be altered through a practice change model. To mark the major
problem areas, a proper data collection and analysis method will be used. A nursing team will
be approached who works in the same mental health department. A mixed method of
qualitative questionnaire filling and semi structured will be used before starting with the
practice change project. At first, a self-administered questionnaire will be used as a method to
analyze the different perceptual and knowledge deficits contributing to a negative attitude in
the nurses. The questions should be formulated covering different aspects of mental health
management starting from acute mental conditions like bipolar diseases (Zhang et al. 2018)
schizophrenia, the specific nursing principles to be used in specific disease and the
interventions used to address severe impairments or behavioral distress. A semi structured
interview will be conducted with the participant nurses where open ended questions will be
used to explore their perceptions and experiences regarding the application of electro
convulsive therapy. The data would be coded and then analyzed to reach a consensus on
coding tree. Finally, the data cluster would be utilized to determine the major themes which
needs to ‘corrected’ by sing the practice change framework.
The project will be using a ‘Colorado model’ (Gover and Richards 2017) to bring in
an evidence based practice change in the attitude and knowledge of nurses with respect to
electroconvulsive therapy. The identified factors relating to treatment quality, patient safety
and evidence-based practice constitutes the major changes in the healthcare framework.
Nurses nowadays are very interested in knowing how to apply good evidence into their daily
practice in order to optimize the patient’s treatment outcomes. Nurses do benefit from the
Project aims and objectives:
To achieve the project objectives which is to address the attitude and knowledge
issues in nursing are to be altered through a practice change model. To mark the major
problem areas, a proper data collection and analysis method will be used. A nursing team will
be approached who works in the same mental health department. A mixed method of
qualitative questionnaire filling and semi structured will be used before starting with the
practice change project. At first, a self-administered questionnaire will be used as a method to
analyze the different perceptual and knowledge deficits contributing to a negative attitude in
the nurses. The questions should be formulated covering different aspects of mental health
management starting from acute mental conditions like bipolar diseases (Zhang et al. 2018)
schizophrenia, the specific nursing principles to be used in specific disease and the
interventions used to address severe impairments or behavioral distress. A semi structured
interview will be conducted with the participant nurses where open ended questions will be
used to explore their perceptions and experiences regarding the application of electro
convulsive therapy. The data would be coded and then analyzed to reach a consensus on
coding tree. Finally, the data cluster would be utilized to determine the major themes which
needs to ‘corrected’ by sing the practice change framework.
The project will be using a ‘Colorado model’ (Gover and Richards 2017) to bring in
an evidence based practice change in the attitude and knowledge of nurses with respect to
electroconvulsive therapy. The identified factors relating to treatment quality, patient safety
and evidence-based practice constitutes the major changes in the healthcare framework.
Nurses nowadays are very interested in knowing how to apply good evidence into their daily
practice in order to optimize the patient’s treatment outcomes. Nurses do benefit from the
8PRACTICE PROPOSAL
acquired training about the application or to work within the framework of evidence based
practice models. These EBP models such as Colorado model can be used to develop the
conception of new and senior nurses regarding the transfer the research evidence into clinical
practice. These models can help assist registered nurses in substantiating efforts derived from
clinical issues and the ideation towards a more coherent and meaningful adherence to
guidelines. Usage of EBP models can actually prevents incomplete implementation of
nursing and other clinical protocols while promoting timely evaluation and maximizing the
usage of resources and time. Nurse staffing strategies collaboration with incorporation of
leadership skills in the organizational network is an important intervention of a practice
change model.
Project Implementation:
First step while selecting a practice change model involve meticulously driven
discussions and presentations about different EBP models (Straus et al. 2018) along with
marking of their disadvantages and strengths. The presenter must be able to provide
accountability for the model’s applicability to chosen clinical needs of organization. Several
strategies include: 1. usage of an EBP model in pre-existent nursing research committee to
evaluate their annual; goals and resolutions 2. An EBP council formation which has the prime
responsibility of deciding on a specific nursing model 3.A task force appointment who is in
charge with confirming the chosen EBP model 4.Conducting seminars, meetings and
workshops within the organization to increase the knowledge vessel regarding the chosen
practice change model 5. focus groups are to be used from different disciplines including
nursing to reflect on the efficiency of the in- system practice change model. The second step
is identifying the effectiveness of a practice change model to close the targeted gaps in
organizational framework. Nurse managers, nurse educators and clinical nurse specialists
should takes up leadership in implementing the various constituents of chosen model. The
acquired training about the application or to work within the framework of evidence based
practice models. These EBP models such as Colorado model can be used to develop the
conception of new and senior nurses regarding the transfer the research evidence into clinical
practice. These models can help assist registered nurses in substantiating efforts derived from
clinical issues and the ideation towards a more coherent and meaningful adherence to
guidelines. Usage of EBP models can actually prevents incomplete implementation of
nursing and other clinical protocols while promoting timely evaluation and maximizing the
usage of resources and time. Nurse staffing strategies collaboration with incorporation of
leadership skills in the organizational network is an important intervention of a practice
change model.
Project Implementation:
First step while selecting a practice change model involve meticulously driven
discussions and presentations about different EBP models (Straus et al. 2018) along with
marking of their disadvantages and strengths. The presenter must be able to provide
accountability for the model’s applicability to chosen clinical needs of organization. Several
strategies include: 1. usage of an EBP model in pre-existent nursing research committee to
evaluate their annual; goals and resolutions 2. An EBP council formation which has the prime
responsibility of deciding on a specific nursing model 3.A task force appointment who is in
charge with confirming the chosen EBP model 4.Conducting seminars, meetings and
workshops within the organization to increase the knowledge vessel regarding the chosen
practice change model 5. focus groups are to be used from different disciplines including
nursing to reflect on the efficiency of the in- system practice change model. The second step
is identifying the effectiveness of a practice change model to close the targeted gaps in
organizational framework. Nurse managers, nurse educators and clinical nurse specialists
should takes up leadership in implementing the various constituents of chosen model. The
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9PRACTICE PROPOSAL
educational hierarchy coupled with practical efficiency must be taken into consideration to
decide the goals to be embedded into the Model’s practice design. In addition, the model
must be implemented directly by the heads of each department inside the organization.
Meetings should be conducted and the responsibilities should be distributed to various
committee members. The leader should survey the functionality of group members to analyze
the optimal time, date and right location for the meeting. The weaknesses and strengths of the
Colorado model should be communicated to the stake holders and administrators of the
organization.
Colorado patient centered inter-professional evidence based model focusses on the
following action areas such as – Cost effective analysis, Clinical expertise, Benchmarking
data, Qualitative improvement and risk data, Pathophysiology, Infection control themes,
Adherence to international, national and local standards and Retrospective medical record
review. The practice change models works on three themes –
a. Patient experience
b. patient values
c. Patient preferences.
The patient is placed at the middle of the new model as because the care decisions are based
on the personal preferences of the patient which keeps in consideration, their cultural and
spiritual values, and also previous healthcare experiences. The nurses and other
interdisciplinary team members should partner with the patients and then advocate for the
patient interests to make informed decisions. Practitioners should encourage patient learning
through the practice of research evidenced treatment. The patients should be allowed to
express their views. The Colorado Model is framed by four concepts essential to embedding
research and evidence in practice. Facilitators, management leaders and executives extend
educational hierarchy coupled with practical efficiency must be taken into consideration to
decide the goals to be embedded into the Model’s practice design. In addition, the model
must be implemented directly by the heads of each department inside the organization.
Meetings should be conducted and the responsibilities should be distributed to various
committee members. The leader should survey the functionality of group members to analyze
the optimal time, date and right location for the meeting. The weaknesses and strengths of the
Colorado model should be communicated to the stake holders and administrators of the
organization.
Colorado patient centered inter-professional evidence based model focusses on the
following action areas such as – Cost effective analysis, Clinical expertise, Benchmarking
data, Qualitative improvement and risk data, Pathophysiology, Infection control themes,
Adherence to international, national and local standards and Retrospective medical record
review. The practice change models works on three themes –
a. Patient experience
b. patient values
c. Patient preferences.
The patient is placed at the middle of the new model as because the care decisions are based
on the personal preferences of the patient which keeps in consideration, their cultural and
spiritual values, and also previous healthcare experiences. The nurses and other
interdisciplinary team members should partner with the patients and then advocate for the
patient interests to make informed decisions. Practitioners should encourage patient learning
through the practice of research evidenced treatment. The patients should be allowed to
express their views. The Colorado Model is framed by four concepts essential to embedding
research and evidence in practice. Facilitators, management leaders and executives extend
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10PRACTICE PROPOSAL
organizational support that is integral to sustaining of an evidence-based culture.
Organizational support have been reported to play a greater role than individual attributes.
There are certain issues though associated with this model – that is its high expense of
application, the ask for highly skilled clinicians to act meticulously within the model’s
fastidious framework which is a huge challenge in a high strung clinical environment but it
has to be managed skillfully by the organizational leaders. Organizational support in the
model, is placed at bottom, almost strategically to signify the vitality of contextual variable in
evidence based practice.
Project Evaluation & Expected Outcomes:
The project will be evaluated by
1. Asking a clinical question.
2. Obtaining the best research literature
3. By auditing and collecting quality report of the ‘changed’ environment and nursing attitude
4. By taking feedback from the organisational heads and employees on an equity basis
5. By integrating the evidence with patient preferences and clinical expertise. 6. By critically
appraising the evidence.
6. By incorporation of quality control indicators.
The expected outcomes are –
1. A far efficient clinical environment
2. Positive attitude towards the usage of electroconvulsive therapy
3. Positive nursing knowledge accumulation that would contribute positively affect the
patient- centred care
organizational support that is integral to sustaining of an evidence-based culture.
Organizational support have been reported to play a greater role than individual attributes.
There are certain issues though associated with this model – that is its high expense of
application, the ask for highly skilled clinicians to act meticulously within the model’s
fastidious framework which is a huge challenge in a high strung clinical environment but it
has to be managed skillfully by the organizational leaders. Organizational support in the
model, is placed at bottom, almost strategically to signify the vitality of contextual variable in
evidence based practice.
Project Evaluation & Expected Outcomes:
The project will be evaluated by
1. Asking a clinical question.
2. Obtaining the best research literature
3. By auditing and collecting quality report of the ‘changed’ environment and nursing attitude
4. By taking feedback from the organisational heads and employees on an equity basis
5. By integrating the evidence with patient preferences and clinical expertise. 6. By critically
appraising the evidence.
6. By incorporation of quality control indicators.
The expected outcomes are –
1. A far efficient clinical environment
2. Positive attitude towards the usage of electroconvulsive therapy
3. Positive nursing knowledge accumulation that would contribute positively affect the
patient- centred care
11PRACTICE PROPOSAL
4. Adherence to best clinical practice guidelines and increase in organizational efficiency
towards treating a complex psychological or mental health case.
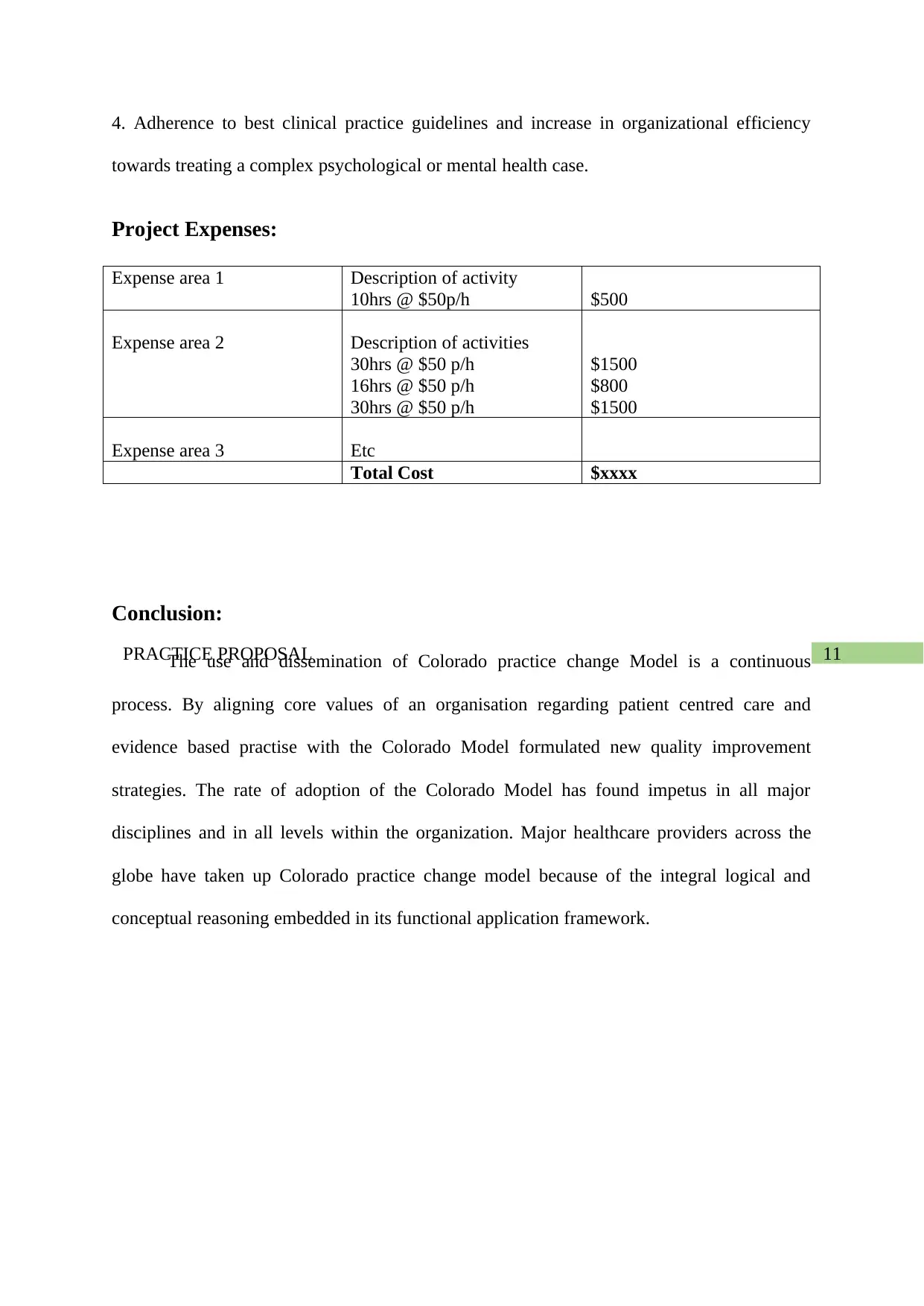
Project Expenses:
Expense area 1 Description of activity
10hrs @ $50p/h $500
Expense area 2 Description of activities
30hrs @ $50 p/h
16hrs @ $50 p/h
30hrs @ $50 p/h
$1500
$800
$1500
Expense area 3 Etc
Total Cost $xxxx
Conclusion:
The use and dissemination of Colorado practice change Model is a continuous
process. By aligning core values of an organisation regarding patient centred care and
evidence based practise with the Colorado Model formulated new quality improvement
strategies. The rate of adoption of the Colorado Model has found impetus in all major
disciplines and in all levels within the organization. Major healthcare providers across the
globe have taken up Colorado practice change model because of the integral logical and
conceptual reasoning embedded in its functional application framework.
4. Adherence to best clinical practice guidelines and increase in organizational efficiency
towards treating a complex psychological or mental health case.
Project Expenses:
Expense area 1 Description of activity
10hrs @ $50p/h $500
Expense area 2 Description of activities
30hrs @ $50 p/h
16hrs @ $50 p/h
30hrs @ $50 p/h
$1500
$800
$1500
Expense area 3 Etc
Total Cost $xxxx
Conclusion:
The use and dissemination of Colorado practice change Model is a continuous
process. By aligning core values of an organisation regarding patient centred care and
evidence based practise with the Colorado Model formulated new quality improvement
strategies. The rate of adoption of the Colorado Model has found impetus in all major
disciplines and in all levels within the organization. Major healthcare providers across the
globe have taken up Colorado practice change model because of the integral logical and
conceptual reasoning embedded in its functional application framework.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 16
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





