Nursing Assignment Report: Pressure Sores Education Tool Proposal
VerifiedAdded on 2023/05/27
|22
|2394
|444
Report
AI Summary
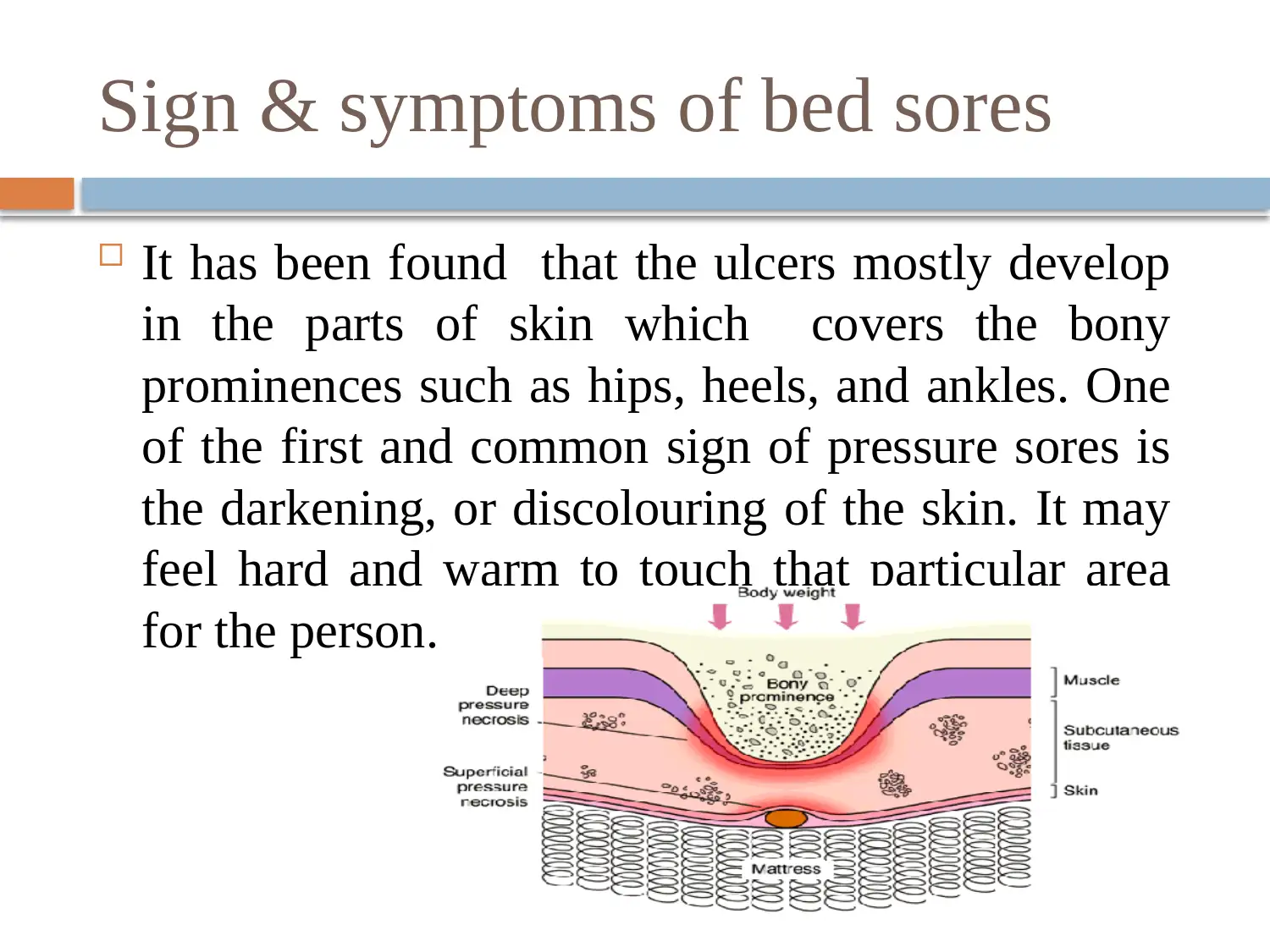
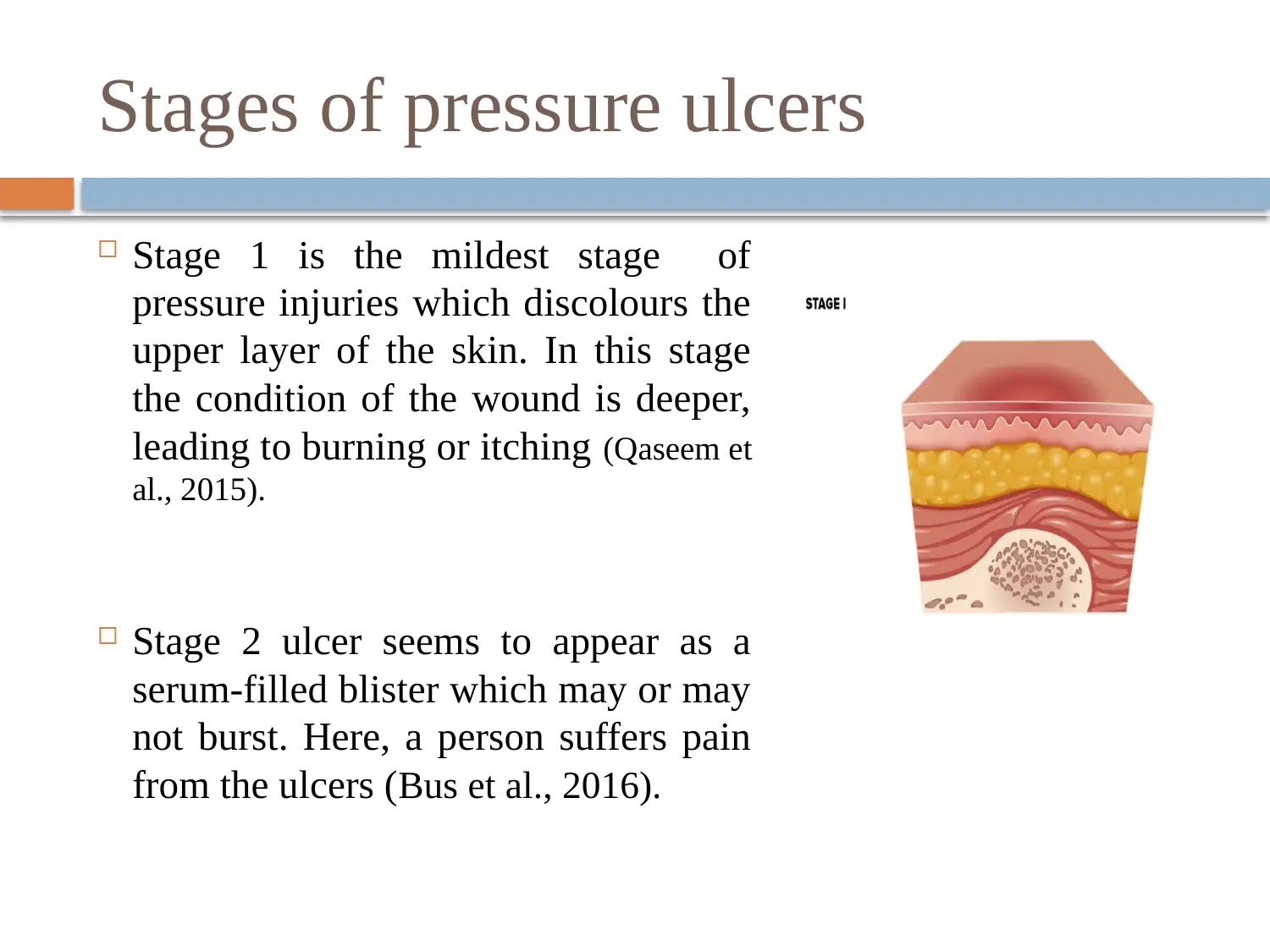
This report focuses on pressure sores, also known as pressure ulcers, which are localized injuries to the skin or underlying tissue caused by pressure, often over bony prominences. It explores the signs, symptoms, and risk factors, including immobility and poor nutrition, along with potential complications like cellulitis and sepsis. The report delves into the pathophysiology, stages of pressure ulcers, and clinical manifestations, including treatments like antibacterial drugs and debridement. The target audience is identified as clinicians, emphasizing the need for education and training. The educational intervention process, including comprehensive wound assessment and documentation, is detailed. The report highlights gaps in education and training and introduces the PUSH tool for monitoring ulcer healing. The overall goal is to improve outcomes through education, prevention strategies, and patient awareness.
1 out of 22









![[object Object]](/_next/static/media/star-bottom.7253800d.svg)