Priority Grid Analysis: Young People Health Needs in Kettering
VerifiedAdded on 2019/09/20
|9
|6907
|105
Report
AI Summary
This report presents a priority grid analysis of health needs among children and young people aged 11-16 in Kettering, Northamptonshire. It examines three key health needs: reduction of mental health admissions, reduction of self-harm admissions, and reduction of teenage pregnancy. The report utilizes data from various sources, including NCC JSNA Northamptonshire, CAMHS, and NICE, to assess the size, severity, and score of each health need. Findings reveal high rates of mental health admissions, self-harm, and teenage pregnancies compared to regional and national averages. The report highlights the prevalence of mental disorders, including conduct, emotional, and hyperkinetic disorders, and their associated risks such as school exclusions, risky behaviors, and increased risk of suicide. The analysis underscores the significant impact of these health issues on the young people, their families, and the wider community, emphasizing the need for targeted interventions and support services. The report concludes with a call to address these pressing health concerns through effective strategies and resource allocation.
Priority Grid Criterion Table: Children and Young people among 11-16yrs
in Kettering, Northamptonshire
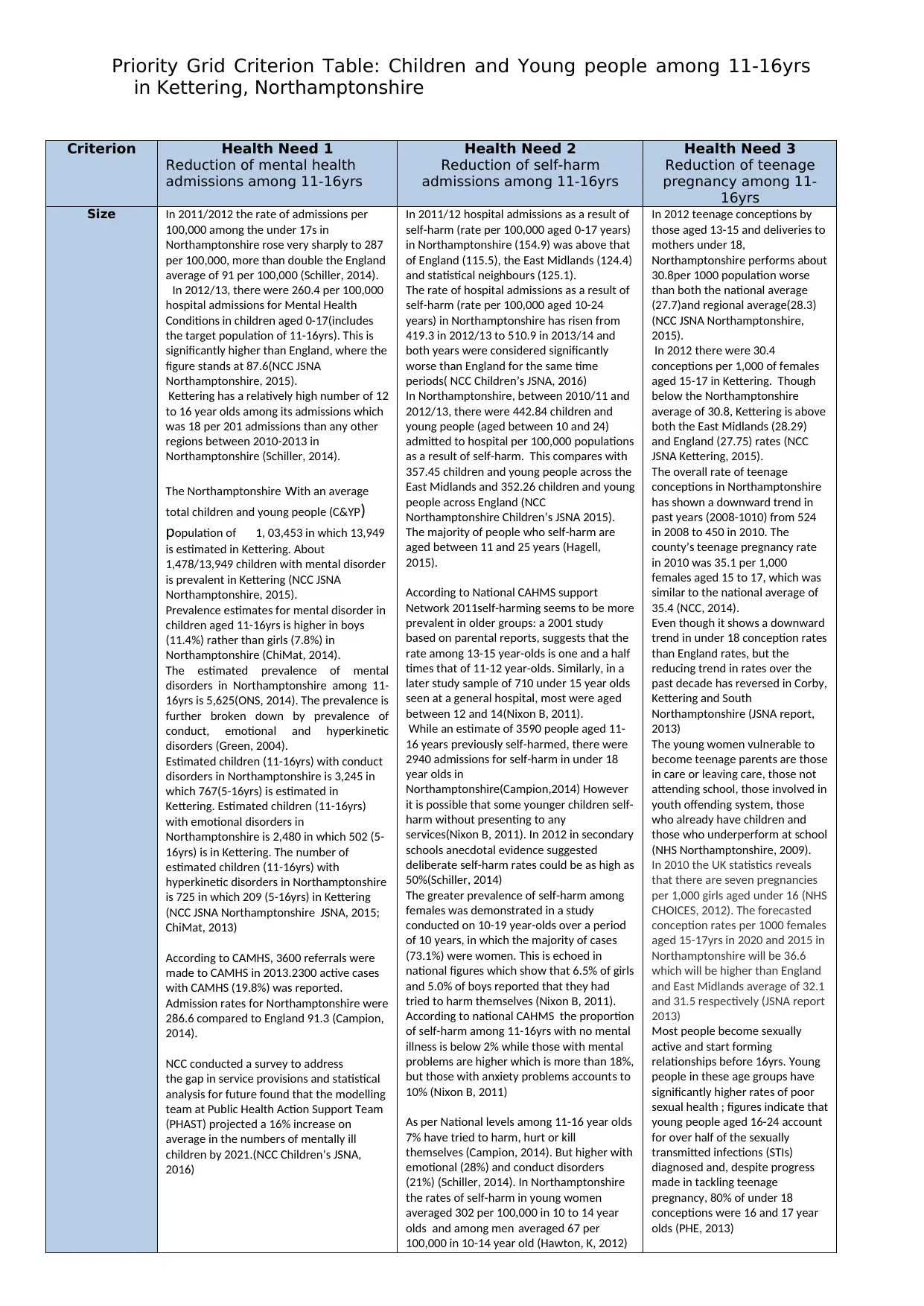
Criterion Health Need 1
Reduction of mental health
admissions among 11-16yrs
Health Need 2
Reduction of self-harm
admissions among 11-16yrs
Health Need 3
Reduction of teenage
pregnancy among 11-
16yrs
Size In 2011/2012 the rate of admissions per
100,000 among the under 17s in
Northamptonshire rose very sharply to 287
per 100,000, more than double the England
average of 91 per 100,000 (Schiller, 2014).
In 2012/13, there were 260.4 per 100,000
hospital admissions for Mental Health
Conditions in children aged 0-17(includes
the target population of 11-16yrs). This is
significantly higher than England, where the
figure stands at 87.6(NCC JSNA
Northamptonshire, 2015).
Kettering has a relatively high number of 12
to 16 year olds among its admissions which
was 18 per 201 admissions than any other
regions between 2010-2013 in
Northamptonshire (Schiller, 2014).
The Northamptonshire with an average
total children and young people (C&YP)
population of 1, 03,453 in which 13,949
is estimated in Kettering. About
1,478/13,949 children with mental disorder
is prevalent in Kettering (NCC JSNA
Northamptonshire, 2015).
Prevalence estimates for mental disorder in
children aged 11-16yrs is higher in boys
(11.4%) rather than girls (7.8%) in
Northamptonshire (ChiMat, 2014).
The estimated prevalence of mental
disorders in Northamptonshire among 11-
16yrs is 5,625(ONS, 2014). The prevalence is
further broken down by prevalence of
conduct, emotional and hyperkinetic
disorders (Green, 2004).
Estimated children (11-16yrs) with conduct
disorders in Northamptonshire is 3,245 in
which 767(5-16yrs) is estimated in
Kettering. Estimated children (11-16yrs)
with emotional disorders in
Northamptonshire is 2,480 in which 502 (5-
16yrs) is in Kettering. The number of
estimated children (11-16yrs) with
hyperkinetic disorders in Northamptonshire
is 725 in which 209 (5-16yrs) in Kettering
(NCC JSNA Northamptonshire JSNA, 2015;
ChiMat, 2013)
According to CAMHS, 3600 referrals were
made to CAMHS in 2013.2300 active cases
with CAMHS (19.8%) was reported.
Admission rates for Northamptonshire were
286.6 compared to England 91.3 (Campion,
2014).
NCC conducted a survey to address
the gap in service provisions and statistical
analysis for future found that the modelling
team at Public Health Action Support Team
(PHAST) projected a 16% increase on
average in the numbers of mentally ill
children by 2021.(NCC Children’s JSNA,
2016)
In 2011/12 hospital admissions as a result of
self-harm (rate per 100,000 aged 0-17 years)
in Northamptonshire (154.9) was above that
of England (115.5), the East Midlands (124.4)
and statistical neighbours (125.1).
The rate of hospital admissions as a result of
self-harm (rate per 100,000 aged 10-24
years) in Northamptonshire has risen from
419.3 in 2012/13 to 510.9 in 2013/14 and
both years were considered significantly
worse than England for the same time
periods( NCC Children’s JSNA, 2016)
In Northamptonshire, between 2010/11 and
2012/13, there were 442.84 children and
young people (aged between 10 and 24)
admitted to hospital per 100,000 populations
as a result of self-harm. This compares with
357.45 children and young people across the
East Midlands and 352.26 children and young
people across England (NCC
Northamptonshire Children’s JSNA 2015).
The majority of people who self-harm are
aged between 11 and 25 years (Hagell,
2015).
According to National CAHMS support
Network 2011self-harming seems to be more
prevalent in older groups: a 2001 study
based on parental reports, suggests that the
rate among 13-15 year-olds is one and a half
times that of 11-12 year-olds. Similarly, in a
later study sample of 710 under 15 year olds
seen at a general hospital, most were aged
between 12 and 14(Nixon B, 2011).
While an estimate of 3590 people aged 11-
16 years previously self-harmed, there were
2940 admissions for self-harm in under 18
year olds in
Northamptonshire(Campion,2014) However
it is possible that some younger children self-
harm without presenting to any
services(Nixon B, 2011). In 2012 in secondary
schools anecdotal evidence suggested
deliberate self-harm rates could be as high as
50%(Schiller, 2014)
The greater prevalence of self-harm among
females was demonstrated in a study
conducted on 10-19 year-olds over a period
of 10 years, in which the majority of cases
(73.1%) were women. This is echoed in
national figures which show that 6.5% of girls
and 5.0% of boys reported that they had
tried to harm themselves (Nixon B, 2011).
According to national CAHMS the proportion
of self-harm among 11-16yrs with no mental
illness is below 2% while those with mental
problems are higher which is more than 18%,
but those with anxiety problems accounts to
10% (Nixon B, 2011)
As per National levels among 11-16 year olds
7% have tried to harm, hurt or kill
themselves (Campion, 2014). But higher with
emotional (28%) and conduct disorders
(21%) (Schiller, 2014). In Northamptonshire
the rates of self-harm in young women
averaged 302 per 100,000 in 10 to 14 year
olds and among men averaged 67 per
100,000 in 10-14 year old (Hawton, K, 2012)
In 2012 teenage conceptions by
those aged 13-15 and deliveries to
mothers under 18,
Northamptonshire performs about
30.8per 1000 population worse
than both the national average
(27.7)and regional average(28.3)
(NCC JSNA Northamptonshire,
2015).
In 2012 there were 30.4
conceptions per 1,000 of females
aged 15-17 in Kettering. Though
below the Northamptonshire
average of 30.8, Kettering is above
both the East Midlands (28.29)
and England (27.75) rates (NCC
JSNA Kettering, 2015).
The overall rate of teenage
conceptions in Northamptonshire
has shown a downward trend in
past years (2008-1010) from 524
in 2008 to 450 in 2010. The
county’s teenage pregnancy rate
in 2010 was 35.1 per 1,000
females aged 15 to 17, which was
similar to the national average of
35.4 (NCC, 2014).
Even though it shows a downward
trend in under 18 conception rates
than England rates, but the
reducing trend in rates over the
past decade has reversed in Corby,
Kettering and South
Northamptonshire (JSNA report,
2013)
The young women vulnerable to
become teenage parents are those
in care or leaving care, those not
attending school, those involved in
youth offending system, those
who already have children and
those who underperform at school
(NHS Northamptonshire, 2009).
In 2010 the UK statistics reveals
that there are seven pregnancies
per 1,000 girls aged under 16 (NHS
CHOICES, 2012). The forecasted
conception rates per 1000 females
aged 15-17yrs in 2020 and 2015 in
Northamptonshire will be 36.6
which will be higher than England
and East Midlands average of 32.1
and 31.5 respectively (JSNA report
2013)
Most people become sexually
active and start forming
relationships before 16yrs. Young
people in these age groups have
significantly higher rates of poor
sexual health ; figures indicate that
young people aged 16-24 account
for over half of the sexually
transmitted infections (STIs)
diagnosed and, despite progress
made in tackling teenage
pregnancy, 80% of under 18
conceptions were 16 and 17 year
olds (PHE, 2013)
in Kettering, Northamptonshire
Criterion Health Need 1
Reduction of mental health
admissions among 11-16yrs
Health Need 2
Reduction of self-harm
admissions among 11-16yrs
Health Need 3
Reduction of teenage
pregnancy among 11-
16yrs
Size In 2011/2012 the rate of admissions per
100,000 among the under 17s in
Northamptonshire rose very sharply to 287
per 100,000, more than double the England
average of 91 per 100,000 (Schiller, 2014).
In 2012/13, there were 260.4 per 100,000
hospital admissions for Mental Health
Conditions in children aged 0-17(includes
the target population of 11-16yrs). This is
significantly higher than England, where the
figure stands at 87.6(NCC JSNA
Northamptonshire, 2015).
Kettering has a relatively high number of 12
to 16 year olds among its admissions which
was 18 per 201 admissions than any other
regions between 2010-2013 in
Northamptonshire (Schiller, 2014).
The Northamptonshire with an average
total children and young people (C&YP)
population of 1, 03,453 in which 13,949
is estimated in Kettering. About
1,478/13,949 children with mental disorder
is prevalent in Kettering (NCC JSNA
Northamptonshire, 2015).
Prevalence estimates for mental disorder in
children aged 11-16yrs is higher in boys
(11.4%) rather than girls (7.8%) in
Northamptonshire (ChiMat, 2014).
The estimated prevalence of mental
disorders in Northamptonshire among 11-
16yrs is 5,625(ONS, 2014). The prevalence is
further broken down by prevalence of
conduct, emotional and hyperkinetic
disorders (Green, 2004).
Estimated children (11-16yrs) with conduct
disorders in Northamptonshire is 3,245 in
which 767(5-16yrs) is estimated in
Kettering. Estimated children (11-16yrs)
with emotional disorders in
Northamptonshire is 2,480 in which 502 (5-
16yrs) is in Kettering. The number of
estimated children (11-16yrs) with
hyperkinetic disorders in Northamptonshire
is 725 in which 209 (5-16yrs) in Kettering
(NCC JSNA Northamptonshire JSNA, 2015;
ChiMat, 2013)
According to CAMHS, 3600 referrals were
made to CAMHS in 2013.2300 active cases
with CAMHS (19.8%) was reported.
Admission rates for Northamptonshire were
286.6 compared to England 91.3 (Campion,
2014).
NCC conducted a survey to address
the gap in service provisions and statistical
analysis for future found that the modelling
team at Public Health Action Support Team
(PHAST) projected a 16% increase on
average in the numbers of mentally ill
children by 2021.(NCC Children’s JSNA,
2016)
In 2011/12 hospital admissions as a result of
self-harm (rate per 100,000 aged 0-17 years)
in Northamptonshire (154.9) was above that
of England (115.5), the East Midlands (124.4)
and statistical neighbours (125.1).
The rate of hospital admissions as a result of
self-harm (rate per 100,000 aged 10-24
years) in Northamptonshire has risen from
419.3 in 2012/13 to 510.9 in 2013/14 and
both years were considered significantly
worse than England for the same time
periods( NCC Children’s JSNA, 2016)
In Northamptonshire, between 2010/11 and
2012/13, there were 442.84 children and
young people (aged between 10 and 24)
admitted to hospital per 100,000 populations
as a result of self-harm. This compares with
357.45 children and young people across the
East Midlands and 352.26 children and young
people across England (NCC
Northamptonshire Children’s JSNA 2015).
The majority of people who self-harm are
aged between 11 and 25 years (Hagell,
2015).
According to National CAHMS support
Network 2011self-harming seems to be more
prevalent in older groups: a 2001 study
based on parental reports, suggests that the
rate among 13-15 year-olds is one and a half
times that of 11-12 year-olds. Similarly, in a
later study sample of 710 under 15 year olds
seen at a general hospital, most were aged
between 12 and 14(Nixon B, 2011).
While an estimate of 3590 people aged 11-
16 years previously self-harmed, there were
2940 admissions for self-harm in under 18
year olds in
Northamptonshire(Campion,2014) However
it is possible that some younger children self-
harm without presenting to any
services(Nixon B, 2011). In 2012 in secondary
schools anecdotal evidence suggested
deliberate self-harm rates could be as high as
50%(Schiller, 2014)
The greater prevalence of self-harm among
females was demonstrated in a study
conducted on 10-19 year-olds over a period
of 10 years, in which the majority of cases
(73.1%) were women. This is echoed in
national figures which show that 6.5% of girls
and 5.0% of boys reported that they had
tried to harm themselves (Nixon B, 2011).
According to national CAHMS the proportion
of self-harm among 11-16yrs with no mental
illness is below 2% while those with mental
problems are higher which is more than 18%,
but those with anxiety problems accounts to
10% (Nixon B, 2011)
As per National levels among 11-16 year olds
7% have tried to harm, hurt or kill
themselves (Campion, 2014). But higher with
emotional (28%) and conduct disorders
(21%) (Schiller, 2014). In Northamptonshire
the rates of self-harm in young women
averaged 302 per 100,000 in 10 to 14 year
olds and among men averaged 67 per
100,000 in 10-14 year old (Hawton, K, 2012)
In 2012 teenage conceptions by
those aged 13-15 and deliveries to
mothers under 18,
Northamptonshire performs about
30.8per 1000 population worse
than both the national average
(27.7)and regional average(28.3)
(NCC JSNA Northamptonshire,
2015).
In 2012 there were 30.4
conceptions per 1,000 of females
aged 15-17 in Kettering. Though
below the Northamptonshire
average of 30.8, Kettering is above
both the East Midlands (28.29)
and England (27.75) rates (NCC
JSNA Kettering, 2015).
The overall rate of teenage
conceptions in Northamptonshire
has shown a downward trend in
past years (2008-1010) from 524
in 2008 to 450 in 2010. The
county’s teenage pregnancy rate
in 2010 was 35.1 per 1,000
females aged 15 to 17, which was
similar to the national average of
35.4 (NCC, 2014).
Even though it shows a downward
trend in under 18 conception rates
than England rates, but the
reducing trend in rates over the
past decade has reversed in Corby,
Kettering and South
Northamptonshire (JSNA report,
2013)
The young women vulnerable to
become teenage parents are those
in care or leaving care, those not
attending school, those involved in
youth offending system, those
who already have children and
those who underperform at school
(NHS Northamptonshire, 2009).
In 2010 the UK statistics reveals
that there are seven pregnancies
per 1,000 girls aged under 16 (NHS
CHOICES, 2012). The forecasted
conception rates per 1000 females
aged 15-17yrs in 2020 and 2015 in
Northamptonshire will be 36.6
which will be higher than England
and East Midlands average of 32.1
and 31.5 respectively (JSNA report
2013)
Most people become sexually
active and start forming
relationships before 16yrs. Young
people in these age groups have
significantly higher rates of poor
sexual health ; figures indicate that
young people aged 16-24 account
for over half of the sexually
transmitted infections (STIs)
diagnosed and, despite progress
made in tackling teenage
pregnancy, 80% of under 18
conceptions were 16 and 17 year
olds (PHE, 2013)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Priority Grid Criterion Table: Children and Young people among 11-16yrs
in Kettering, Northamptonshire
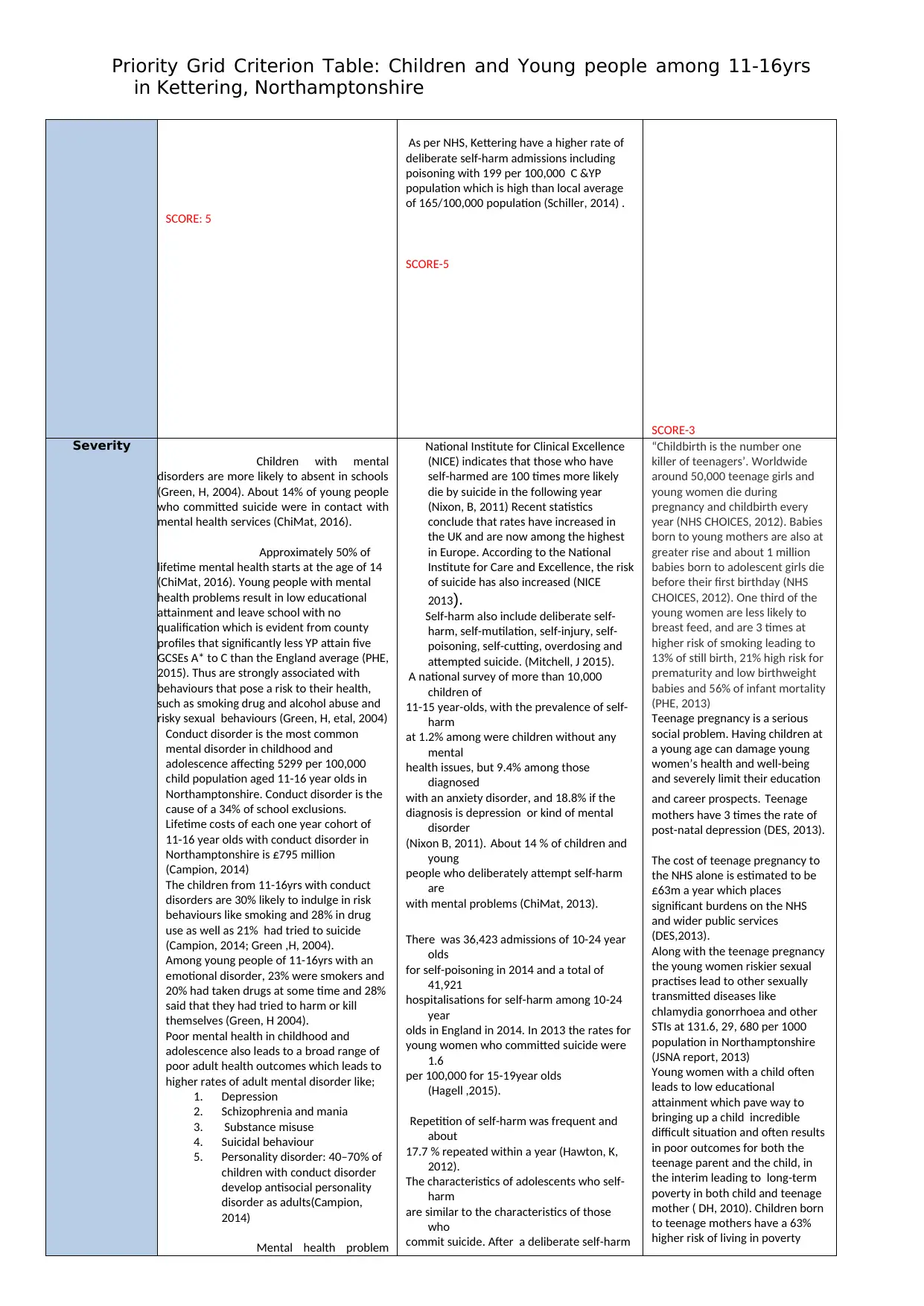
SCORE: 5
As per NHS, Kettering have a higher rate of
deliberate self-harm admissions including
poisoning with 199 per 100,000 C &YP
population which is high than local average
of 165/100,000 population (Schiller, 2014) .
SCORE-5
SCORE-3
Severity
Children with mental
disorders are more likely to absent in schools
(Green, H, 2004). About 14% of young people
who committed suicide were in contact with
mental health services (ChiMat, 2016).
Approximately 50% of
lifetime mental health starts at the age of 14
(ChiMat, 2016). Young people with mental
health problems result in low educational
attainment and leave school with no
qualification which is evident from county
profiles that significantly less YP attain five
GCSEs A* to C than the England average (PHE,
2015). Thus are strongly associated with
behaviours that pose a risk to their health,
such as smoking drug and alcohol abuse and
risky sexual behaviours (Green, H, etal, 2004)
Conduct disorder is the most common
mental disorder in childhood and
adolescence affecting 5299 per 100,000
child population aged 11-16 year olds in
Northamptonshire. Conduct disorder is the
cause of a 34% of school exclusions.
Lifetime costs of each one year cohort of
11-16 year olds with conduct disorder in
Northamptonshire is £795 million
(Campion, 2014)
The children from 11-16yrs with conduct
disorders are 30% likely to indulge in risk
behaviours like smoking and 28% in drug
use as well as 21% had tried to suicide
(Campion, 2014; Green ,H, 2004).
Among young people of 11-16yrs with an
emotional disorder, 23% were smokers and
20% had taken drugs at some time and 28%
said that they had tried to harm or kill
themselves (Green, H 2004).
Poor mental health in childhood and
adolescence also leads to a broad range of
poor adult health outcomes which leads to
higher rates of adult mental disorder like;
1. Depression
2. Schizophrenia and mania
3. Substance misuse
4. Suicidal behaviour
5. Personality disorder: 40–70% of
children with conduct disorder
develop antisocial personality
disorder as adults(Campion,
2014)
Mental health problem
National Institute for Clinical Excellence
(NICE) indicates that those who have
self-harmed are 100 times more likely
die by suicide in the following year
(Nixon, B, 2011) Recent statistics
conclude that rates have increased in
the UK and are now among the highest
in Europe. According to the National
Institute for Care and Excellence, the risk
of suicide has also increased (NICE
2013).
Self-harm also include deliberate self-
harm, self-mutilation, self-injury, self-
poisoning, self-cutting, overdosing and
attempted suicide. (Mitchell, J 2015).
A national survey of more than 10,000
children of
11-15 year-olds, with the prevalence of self-
harm
at 1.2% among were children without any
mental
health issues, but 9.4% among those
diagnosed
with an anxiety disorder, and 18.8% if the
diagnosis is depression or kind of mental
disorder
(Nixon B, 2011). About 14 % of children and
young
people who deliberately attempt self-harm
are
with mental problems (ChiMat, 2013).
There was 36,423 admissions of 10-24 year
olds
for self-poisoning in 2014 and a total of
41,921
hospitalisations for self-harm among 10-24
year
olds in England in 2014. In 2013 the rates for
young women who committed suicide were
1.6
per 100,000 for 15-19year olds
(Hagell ,2015).
Repetition of self-harm was frequent and
about
17.7 % repeated within a year (Hawton, K,
2012).
The characteristics of adolescents who self-
harm
are similar to the characteristics of those
who
commit suicide. After a deliberate self-harm
“Childbirth is the number one
killer of teenagers’. Worldwide
around 50,000 teenage girls and
young women die during
pregnancy and childbirth every
year (NHS CHOICES, 2012). Babies
born to young mothers are also at
greater rise and about 1 million
babies born to adolescent girls die
before their first birthday (NHS
CHOICES, 2012). One third of the
young women are less likely to
breast feed, and are 3 times at
higher risk of smoking leading to
13% of still birth, 21% high risk for
prematurity and low birthweight
babies and 56% of infant mortality
(PHE, 2013)
Teenage pregnancy is a serious
social problem. Having children at
a young age can damage young
women’s health and well-being
and severely limit their education
and career prospects. Teenage
mothers have 3 times the rate of
post-natal depression (DES, 2013).
The cost of teenage pregnancy to
the NHS alone is estimated to be
£63m a year which places
significant burdens on the NHS
and wider public services
(DES,2013).
Along with the teenage pregnancy
the young women riskier sexual
practises lead to other sexually
transmitted diseases like
chlamydia gonorrhoea and other
STIs at 131.6, 29, 680 per 1000
population in Northamptonshire
(JSNA report, 2013)
Young women with a child often
leads to low educational
attainment which pave way to
bringing up a child incredible
difficult situation and often results
in poor outcomes for both the
teenage parent and the child, in
the interim leading to long-term
poverty in both child and teenage
mother ( DH, 2010). Children born
to teenage mothers have a 63%
higher risk of living in poverty
in Kettering, Northamptonshire
SCORE: 5
As per NHS, Kettering have a higher rate of
deliberate self-harm admissions including
poisoning with 199 per 100,000 C &YP
population which is high than local average
of 165/100,000 population (Schiller, 2014) .
SCORE-5
SCORE-3
Severity
Children with mental
disorders are more likely to absent in schools
(Green, H, 2004). About 14% of young people
who committed suicide were in contact with
mental health services (ChiMat, 2016).
Approximately 50% of
lifetime mental health starts at the age of 14
(ChiMat, 2016). Young people with mental
health problems result in low educational
attainment and leave school with no
qualification which is evident from county
profiles that significantly less YP attain five
GCSEs A* to C than the England average (PHE,
2015). Thus are strongly associated with
behaviours that pose a risk to their health,
such as smoking drug and alcohol abuse and
risky sexual behaviours (Green, H, etal, 2004)
Conduct disorder is the most common
mental disorder in childhood and
adolescence affecting 5299 per 100,000
child population aged 11-16 year olds in
Northamptonshire. Conduct disorder is the
cause of a 34% of school exclusions.
Lifetime costs of each one year cohort of
11-16 year olds with conduct disorder in
Northamptonshire is £795 million
(Campion, 2014)
The children from 11-16yrs with conduct
disorders are 30% likely to indulge in risk
behaviours like smoking and 28% in drug
use as well as 21% had tried to suicide
(Campion, 2014; Green ,H, 2004).
Among young people of 11-16yrs with an
emotional disorder, 23% were smokers and
20% had taken drugs at some time and 28%
said that they had tried to harm or kill
themselves (Green, H 2004).
Poor mental health in childhood and
adolescence also leads to a broad range of
poor adult health outcomes which leads to
higher rates of adult mental disorder like;
1. Depression
2. Schizophrenia and mania
3. Substance misuse
4. Suicidal behaviour
5. Personality disorder: 40–70% of
children with conduct disorder
develop antisocial personality
disorder as adults(Campion,
2014)
Mental health problem
National Institute for Clinical Excellence
(NICE) indicates that those who have
self-harmed are 100 times more likely
die by suicide in the following year
(Nixon, B, 2011) Recent statistics
conclude that rates have increased in
the UK and are now among the highest
in Europe. According to the National
Institute for Care and Excellence, the risk
of suicide has also increased (NICE
2013).
Self-harm also include deliberate self-
harm, self-mutilation, self-injury, self-
poisoning, self-cutting, overdosing and
attempted suicide. (Mitchell, J 2015).
A national survey of more than 10,000
children of
11-15 year-olds, with the prevalence of self-
harm
at 1.2% among were children without any
mental
health issues, but 9.4% among those
diagnosed
with an anxiety disorder, and 18.8% if the
diagnosis is depression or kind of mental
disorder
(Nixon B, 2011). About 14 % of children and
young
people who deliberately attempt self-harm
are
with mental problems (ChiMat, 2013).
There was 36,423 admissions of 10-24 year
olds
for self-poisoning in 2014 and a total of
41,921
hospitalisations for self-harm among 10-24
year
olds in England in 2014. In 2013 the rates for
young women who committed suicide were
1.6
per 100,000 for 15-19year olds
(Hagell ,2015).
Repetition of self-harm was frequent and
about
17.7 % repeated within a year (Hawton, K,
2012).
The characteristics of adolescents who self-
harm
are similar to the characteristics of those
who
commit suicide. After a deliberate self-harm
“Childbirth is the number one
killer of teenagers’. Worldwide
around 50,000 teenage girls and
young women die during
pregnancy and childbirth every
year (NHS CHOICES, 2012). Babies
born to young mothers are also at
greater rise and about 1 million
babies born to adolescent girls die
before their first birthday (NHS
CHOICES, 2012). One third of the
young women are less likely to
breast feed, and are 3 times at
higher risk of smoking leading to
13% of still birth, 21% high risk for
prematurity and low birthweight
babies and 56% of infant mortality
(PHE, 2013)
Teenage pregnancy is a serious
social problem. Having children at
a young age can damage young
women’s health and well-being
and severely limit their education
and career prospects. Teenage
mothers have 3 times the rate of
post-natal depression (DES, 2013).
The cost of teenage pregnancy to
the NHS alone is estimated to be
£63m a year which places
significant burdens on the NHS
and wider public services
(DES,2013).
Along with the teenage pregnancy
the young women riskier sexual
practises lead to other sexually
transmitted diseases like
chlamydia gonorrhoea and other
STIs at 131.6, 29, 680 per 1000
population in Northamptonshire
(JSNA report, 2013)
Young women with a child often
leads to low educational
attainment which pave way to
bringing up a child incredible
difficult situation and often results
in poor outcomes for both the
teenage parent and the child, in
the interim leading to long-term
poverty in both child and teenage
mother ( DH, 2010). Children born
to teenage mothers have a 63%
higher risk of living in poverty
Priority Grid Criterion Table: Children and Young people among 11-16yrs
in Kettering, Northamptonshire
that go untreated result in distress in children
and their families, carers and communities.
Within NHS its accounts for more than 12%of
total budget. It is estimated that in 2007, the
cost of mental health care across services was
22.5 billion pound, taking into account loss of
employment and other associated costs this
rises to 48.6 billion pound, which is 3.6%
GDP. By 2026 it is estimated that these
combined costs will have risen to 88.5 billion
pound which is 6.6%of GDP (NHS, 2013).
SCORE-5
there
is 30-66% increased chance of suicide
(Hawton, K, 2005).
Challenging behaviour can take many forms
from self-harm, aggression, sleeplessness,
risk taking behaviours, anti-social behaviour
and may lead to poor outcomes such as
school and social exclusion.(YHMP, 2011).
SCORE-4
(PHE, 2013). Women who were
teenage mothers are 22% more
likely to be living in poverty at age
30 (PHE, 2013)
SCORE-3
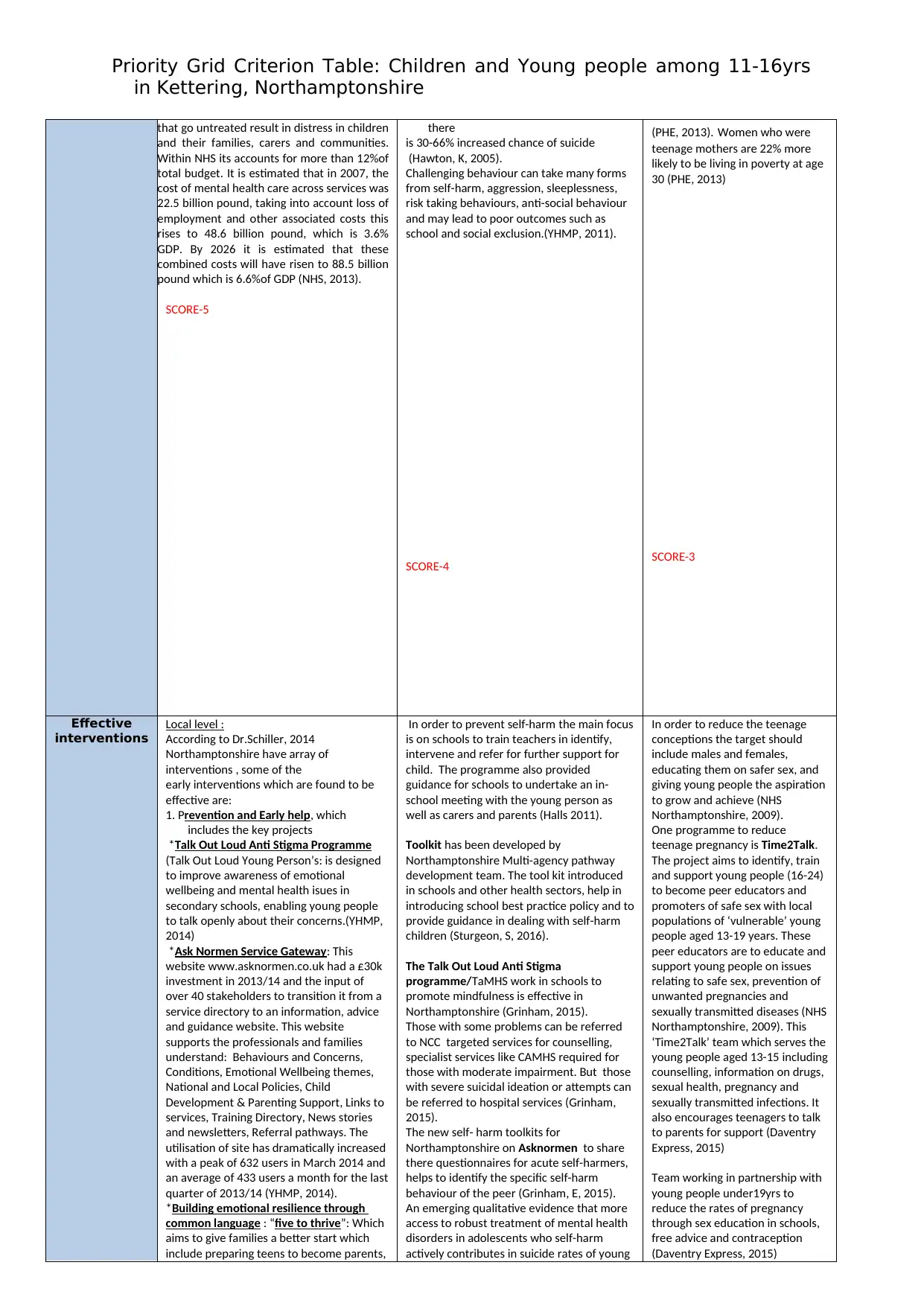
Effective
interventions
Local level :
According to Dr.Schiller, 2014
Northamptonshire have array of
interventions , some of the
early interventions which are found to be
effective are:
1. Prevention and Early help, which
includes the key projects
*Talk Out Loud Anti Stigma Programme
(Talk Out Loud Young Person’s: is designed
to improve awareness of emotional
wellbeing and mental health isues in
secondary schools, enabling young people
to talk openly about their concerns.(YHMP,
2014)
*Ask Normen Service Gateway: This
website www.asknormen.co.uk had a £30k
investment in 2013/14 and the input of
over 40 stakeholders to transition it from a
service directory to an information, advice
and guidance website. This website
supports the professionals and families
understand: Behaviours and Concerns,
Conditions, Emotional Wellbeing themes,
National and Local Policies, Child
Development & Parenting Support, Links to
services, Training Directory, News stories
and newsletters, Referral pathways. The
utilisation of site has dramatically increased
with a peak of 632 users in March 2014 and
an average of 433 users a month for the last
quarter of 2013/14 (YHMP, 2014).
*Building emotional resilience through
common language : “five to thrive”: Which
aims to give families a better start which
include preparing teens to become parents,
In order to prevent self-harm the main focus
is on schools to train teachers in identify,
intervene and refer for further support for
child. The programme also provided
guidance for schools to undertake an in-
school meeting with the young person as
well as carers and parents (Halls 2011).
Toolkit has been developed by
Northamptonshire Multi-agency pathway
development team. The tool kit introduced
in schools and other health sectors, help in
introducing school best practice policy and to
provide guidance in dealing with self-harm
children (Sturgeon, S, 2016).
The Talk Out Loud Anti Stigma
programme/TaMHS work in schools to
promote mindfulness is effective in
Northamptonshire (Grinham, 2015).
Those with some problems can be referred
to NCC targeted services for counselling,
specialist services like CAMHS required for
those with moderate impairment. But those
with severe suicidal ideation or attempts can
be referred to hospital services (Grinham,
2015).
The new self- harm toolkits for
Northamptonshire on Asknormen to share
there questionnaires for acute self-harmers,
helps to identify the specific self-harm
behaviour of the peer (Grinham, E, 2015).
An emerging qualitative evidence that more
access to robust treatment of mental health
disorders in adolescents who self-harm
actively contributes in suicide rates of young
In order to reduce the teenage
conceptions the target should
include males and females,
educating them on safer sex, and
giving young people the aspiration
to grow and achieve (NHS
Northamptonshire, 2009).
One programme to reduce
teenage pregnancy is Time2Talk.
The project aims to identify, train
and support young people (16-24)
to become peer educators and
promoters of safe sex with local
populations of ‘vulnerable’ young
people aged 13-19 years. These
peer educators are to educate and
support young people on issues
relating to safe sex, prevention of
unwanted pregnancies and
sexually transmitted diseases (NHS
Northamptonshire, 2009). This
‘Time2Talk’ team which serves the
young people aged 13-15 including
counselling, information on drugs,
sexual health, pregnancy and
sexually transmitted infections. It
also encourages teenagers to talk
to parents for support (Daventry
Express, 2015)
Team working in partnership with
young people under19yrs to
reduce the rates of pregnancy
through sex education in schools,
free advice and contraception
(Daventry Express, 2015)
in Kettering, Northamptonshire
that go untreated result in distress in children
and their families, carers and communities.
Within NHS its accounts for more than 12%of
total budget. It is estimated that in 2007, the
cost of mental health care across services was
22.5 billion pound, taking into account loss of
employment and other associated costs this
rises to 48.6 billion pound, which is 3.6%
GDP. By 2026 it is estimated that these
combined costs will have risen to 88.5 billion
pound which is 6.6%of GDP (NHS, 2013).
SCORE-5
there
is 30-66% increased chance of suicide
(Hawton, K, 2005).
Challenging behaviour can take many forms
from self-harm, aggression, sleeplessness,
risk taking behaviours, anti-social behaviour
and may lead to poor outcomes such as
school and social exclusion.(YHMP, 2011).
SCORE-4
(PHE, 2013). Women who were
teenage mothers are 22% more
likely to be living in poverty at age
30 (PHE, 2013)
SCORE-3
Effective
interventions
Local level :
According to Dr.Schiller, 2014
Northamptonshire have array of
interventions , some of the
early interventions which are found to be
effective are:
1. Prevention and Early help, which
includes the key projects
*Talk Out Loud Anti Stigma Programme
(Talk Out Loud Young Person’s: is designed
to improve awareness of emotional
wellbeing and mental health isues in
secondary schools, enabling young people
to talk openly about their concerns.(YHMP,
2014)
*Ask Normen Service Gateway: This
website www.asknormen.co.uk had a £30k
investment in 2013/14 and the input of
over 40 stakeholders to transition it from a
service directory to an information, advice
and guidance website. This website
supports the professionals and families
understand: Behaviours and Concerns,
Conditions, Emotional Wellbeing themes,
National and Local Policies, Child
Development & Parenting Support, Links to
services, Training Directory, News stories
and newsletters, Referral pathways. The
utilisation of site has dramatically increased
with a peak of 632 users in March 2014 and
an average of 433 users a month for the last
quarter of 2013/14 (YHMP, 2014).
*Building emotional resilience through
common language : “five to thrive”: Which
aims to give families a better start which
include preparing teens to become parents,
In order to prevent self-harm the main focus
is on schools to train teachers in identify,
intervene and refer for further support for
child. The programme also provided
guidance for schools to undertake an in-
school meeting with the young person as
well as carers and parents (Halls 2011).
Toolkit has been developed by
Northamptonshire Multi-agency pathway
development team. The tool kit introduced
in schools and other health sectors, help in
introducing school best practice policy and to
provide guidance in dealing with self-harm
children (Sturgeon, S, 2016).
The Talk Out Loud Anti Stigma
programme/TaMHS work in schools to
promote mindfulness is effective in
Northamptonshire (Grinham, 2015).
Those with some problems can be referred
to NCC targeted services for counselling,
specialist services like CAMHS required for
those with moderate impairment. But those
with severe suicidal ideation or attempts can
be referred to hospital services (Grinham,
2015).
The new self- harm toolkits for
Northamptonshire on Asknormen to share
there questionnaires for acute self-harmers,
helps to identify the specific self-harm
behaviour of the peer (Grinham, E, 2015).
An emerging qualitative evidence that more
access to robust treatment of mental health
disorders in adolescents who self-harm
actively contributes in suicide rates of young
In order to reduce the teenage
conceptions the target should
include males and females,
educating them on safer sex, and
giving young people the aspiration
to grow and achieve (NHS
Northamptonshire, 2009).
One programme to reduce
teenage pregnancy is Time2Talk.
The project aims to identify, train
and support young people (16-24)
to become peer educators and
promoters of safe sex with local
populations of ‘vulnerable’ young
people aged 13-19 years. These
peer educators are to educate and
support young people on issues
relating to safe sex, prevention of
unwanted pregnancies and
sexually transmitted diseases (NHS
Northamptonshire, 2009). This
‘Time2Talk’ team which serves the
young people aged 13-15 including
counselling, information on drugs,
sexual health, pregnancy and
sexually transmitted infections. It
also encourages teenagers to talk
to parents for support (Daventry
Express, 2015)
Team working in partnership with
young people under19yrs to
reduce the rates of pregnancy
through sex education in schools,
free advice and contraception
(Daventry Express, 2015)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Priority Grid Criterion Table: Children and Young people among 11-16yrs
in Kettering, Northamptonshire
midwifery services, health visiting, foster
carers, disability support, youth justice
worker(YHMA, 2014).
In addition to these, other cost effective
interventions to improve healthy
relationship between parents and their
children are:
1.Parenting programmes: 1930 parents of
over 5 year olds accessed parenting
programmes. 379 parents of children with
special education needs and 1243 parents
with particular needs attended the
programme.(Campion,2014)
2.School based programmes:
The mental health strategy highlights that
school based social emotional learning
programmes result in net savings of £84 for
each £ spent (Campion, 2014)
3.Educational outcomes: Improved
educational outcomes are associated with
improved mental health: percentage of
pupils achieving 5 A* to C grades at GCSE is
55% for Northamptonshire (England 58.0%)
(Campion,2014).
4.Community activities to promote child
and adolescent mental health: Youth
engagement in local decision making and
some targeted small programmes provided
by third sector organisations .Increasing
participation in positive activities: 55% of
children in Northamptonshire participated
in positive activities compared to 65.8% in
England.(Campion, 2014)
5.Employment : Work based mental health
promotion programmes can result in net
savings of £10 for each £ spent although no
such interventions are happening in
Northamptonshire( Campion, 2014).
2. The Northamptonshire Targeted Mental
Health in Schools (TaMHS) is a co-ordinated
multi-agency programme for building
capacity within schools through training,
support and introducing new programmes
and approaches to better meet the mental
health needs of all children: at universal,
targeted and more specialist levels,
including through systemic work with
parents, staff and locality agencies. By
meeting mental health needs in this way,
sustainable positive impact on children’s
mental health, attainments, bullying,
attendance and exclusions can be achieved.
85% of schools use at least one intervention
from the team ( YHMP, 2014).
Northamptonshire transformation plan
includes: Early help, Communication,
Workforce development, Access to
Services, Specific pathway(NCC
Children’s JSNA, 2016).
Northamptonshire Local Transformation
Plan with the national policy published by
NHS and director of health in March 2015
is:
Future in Mind which describes a vision for
a comprehensive approach to promoting,
supporting and treating our children and
young people’s mental health; and to
supporting their families. Future in minds is
the government aspirations to be achieved
by 2020 (NCC Children’s JSNA, 2016)
SCORE-4
children (Foster, C. Allen, S, 2013).
The two pathway system includes the
community and school pathway and acute
pathway: the community and school
pathways includes communication between
the home schools and other agencies,
referrals to CAMHS and telephonic
consultation and risk assessment and
participation of parents and carers(Grinham,
E. Loyd Hearn, D, 2015)
SCORE-3
Open-access sexual health services
are now commissioned by local
authorities, and abortion services
are commissioned by clinical
commissioning groups (JSNA
Report, 2013).
The international evidence-base
for the Strategy shows that the
two measures for which there is
the strongest evidence of impact
on teenage pregnancy rates are:
comprehensive information advice
and support from parents, schools
and other professionals combined
with accessible, young people-
friendly sexual and reproductive
health (SRH) services (DH, 2010).
Sure start plus programme was
established as a part of teenage
pregnancy strategy, family nurse
partnership programme was
commissioned by department of
health, care to learn programme
which provide funding for child
care and further education (PHE,
2013)
in Kettering, Northamptonshire
midwifery services, health visiting, foster
carers, disability support, youth justice
worker(YHMA, 2014).
In addition to these, other cost effective
interventions to improve healthy
relationship between parents and their
children are:
1.Parenting programmes: 1930 parents of
over 5 year olds accessed parenting
programmes. 379 parents of children with
special education needs and 1243 parents
with particular needs attended the
programme.(Campion,2014)
2.School based programmes:
The mental health strategy highlights that
school based social emotional learning
programmes result in net savings of £84 for
each £ spent (Campion, 2014)
3.Educational outcomes: Improved
educational outcomes are associated with
improved mental health: percentage of
pupils achieving 5 A* to C grades at GCSE is
55% for Northamptonshire (England 58.0%)
(Campion,2014).
4.Community activities to promote child
and adolescent mental health: Youth
engagement in local decision making and
some targeted small programmes provided
by third sector organisations .Increasing
participation in positive activities: 55% of
children in Northamptonshire participated
in positive activities compared to 65.8% in
England.(Campion, 2014)
5.Employment : Work based mental health
promotion programmes can result in net
savings of £10 for each £ spent although no
such interventions are happening in
Northamptonshire( Campion, 2014).
2. The Northamptonshire Targeted Mental
Health in Schools (TaMHS) is a co-ordinated
multi-agency programme for building
capacity within schools through training,
support and introducing new programmes
and approaches to better meet the mental
health needs of all children: at universal,
targeted and more specialist levels,
including through systemic work with
parents, staff and locality agencies. By
meeting mental health needs in this way,
sustainable positive impact on children’s
mental health, attainments, bullying,
attendance and exclusions can be achieved.
85% of schools use at least one intervention
from the team ( YHMP, 2014).
Northamptonshire transformation plan
includes: Early help, Communication,
Workforce development, Access to
Services, Specific pathway(NCC
Children’s JSNA, 2016).
Northamptonshire Local Transformation
Plan with the national policy published by
NHS and director of health in March 2015
is:
Future in Mind which describes a vision for
a comprehensive approach to promoting,
supporting and treating our children and
young people’s mental health; and to
supporting their families. Future in minds is
the government aspirations to be achieved
by 2020 (NCC Children’s JSNA, 2016)
SCORE-4
children (Foster, C. Allen, S, 2013).
The two pathway system includes the
community and school pathway and acute
pathway: the community and school
pathways includes communication between
the home schools and other agencies,
referrals to CAMHS and telephonic
consultation and risk assessment and
participation of parents and carers(Grinham,
E. Loyd Hearn, D, 2015)
SCORE-3
Open-access sexual health services
are now commissioned by local
authorities, and abortion services
are commissioned by clinical
commissioning groups (JSNA
Report, 2013).
The international evidence-base
for the Strategy shows that the
two measures for which there is
the strongest evidence of impact
on teenage pregnancy rates are:
comprehensive information advice
and support from parents, schools
and other professionals combined
with accessible, young people-
friendly sexual and reproductive
health (SRH) services (DH, 2010).
Sure start plus programme was
established as a part of teenage
pregnancy strategy, family nurse
partnership programme was
commissioned by department of
health, care to learn programme
which provide funding for child
care and further education (PHE,
2013)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Priority Grid Criterion Table: Children and Young people among 11-16yrs
in Kettering, Northamptonshire
SCORE-3
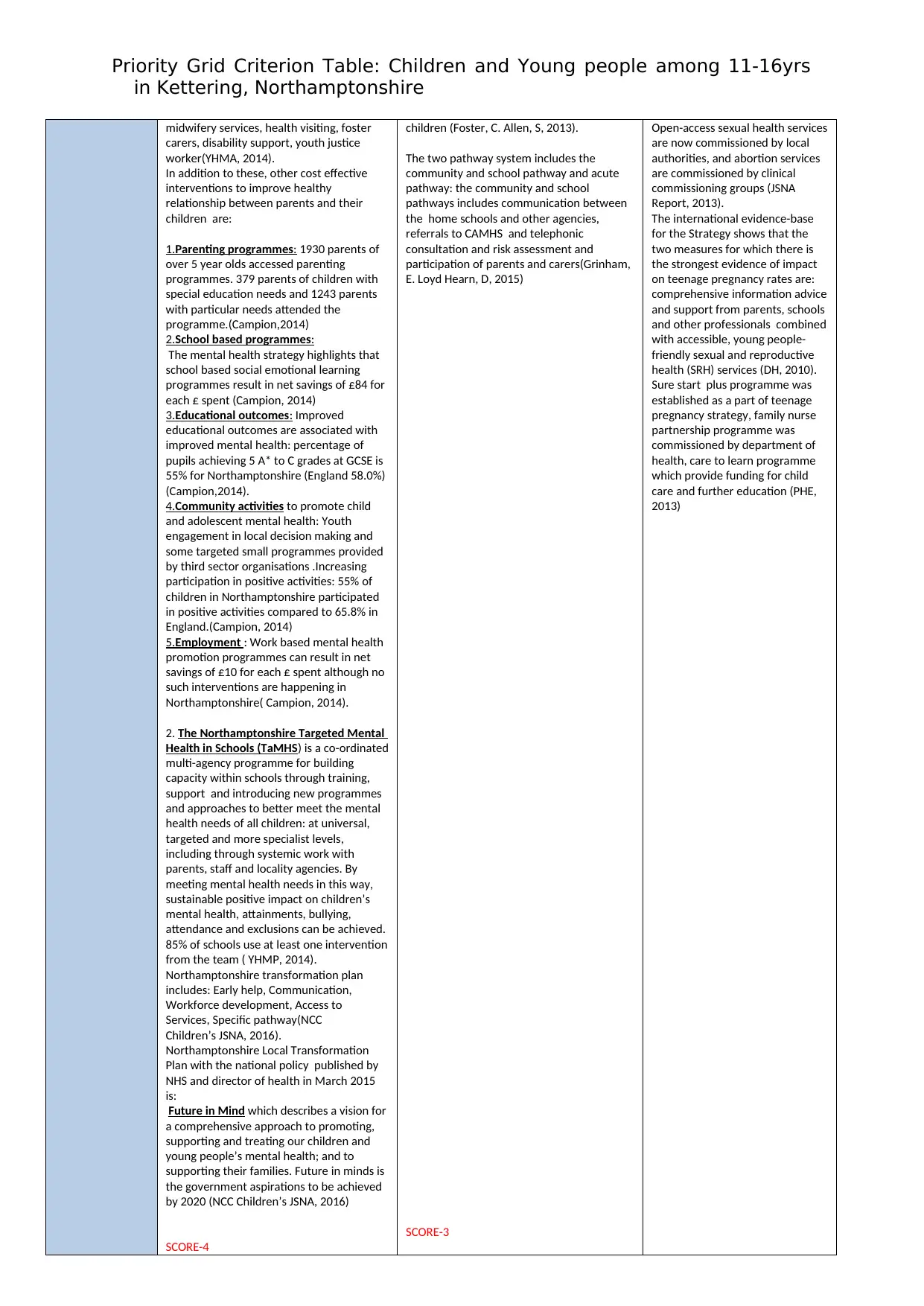
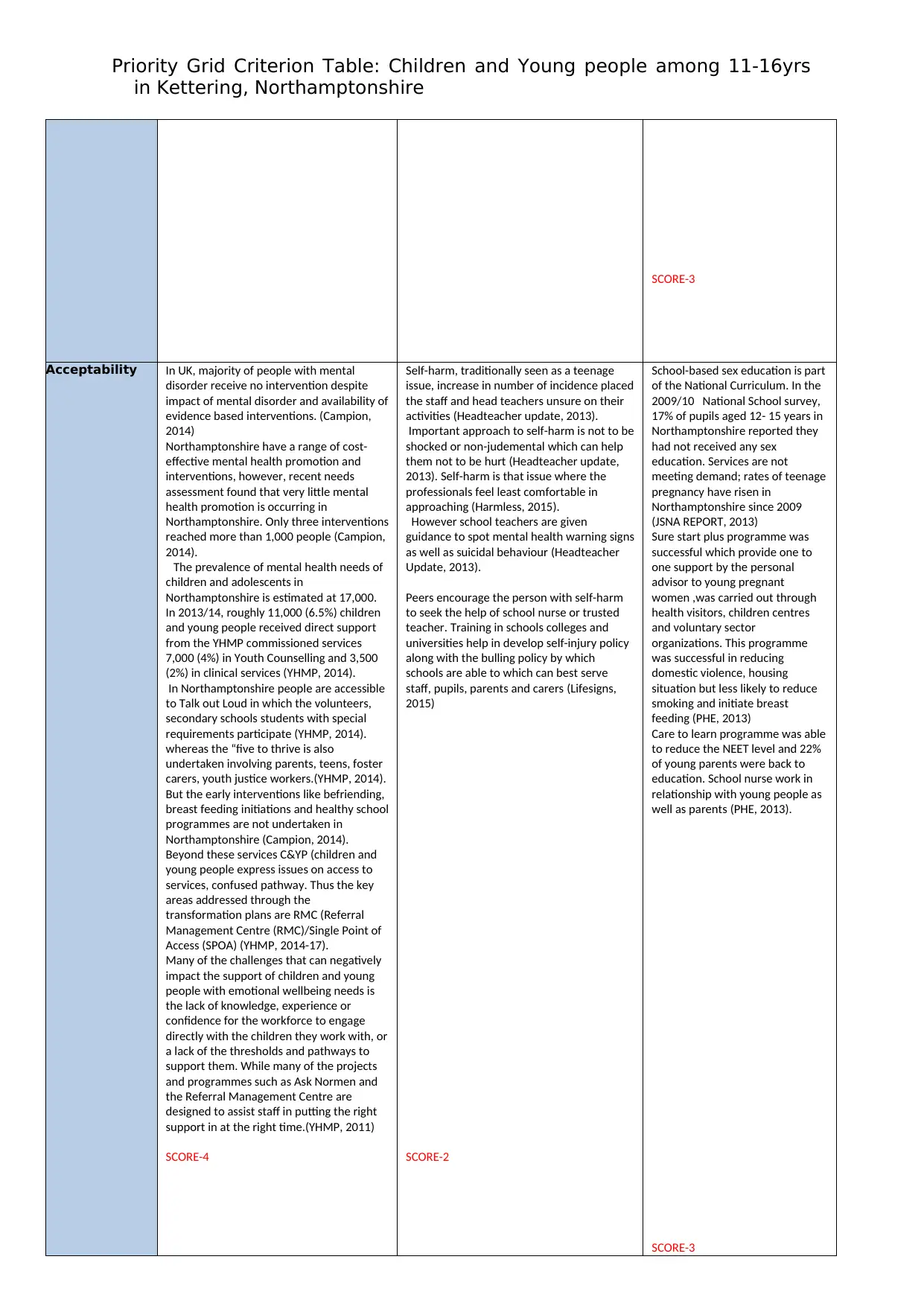
Acceptability In UK, majority of people with mental
disorder receive no intervention despite
impact of mental disorder and availability of
evidence based interventions. (Campion,
2014)
Northamptonshire have a range of cost-
effective mental health promotion and
interventions, however, recent needs
assessment found that very little mental
health promotion is occurring in
Northamptonshire. Only three interventions
reached more than 1,000 people (Campion,
2014).
The prevalence of mental health needs of
children and adolescents in
Northamptonshire is estimated at 17,000.
In 2013/14, roughly 11,000 (6.5%) children
and young people received direct support
from the YHMP commissioned services
7,000 (4%) in Youth Counselling and 3,500
(2%) in clinical services (YHMP, 2014).
In Northamptonshire people are accessible
to Talk out Loud in which the volunteers,
secondary schools students with special
requirements participate (YHMP, 2014).
whereas the “five to thrive is also
undertaken involving parents, teens, foster
carers, youth justice workers.(YHMP, 2014).
But the early interventions like befriending,
breast feeding initiations and healthy school
programmes are not undertaken in
Northamptonshire (Campion, 2014).
Beyond these services C&YP (children and
young people express issues on access to
services, confused pathway. Thus the key
areas addressed through the
transformation plans are RMC (Referral
Management Centre (RMC)/Single Point of
Access (SPOA) (YHMP, 2014-17).
Many of the challenges that can negatively
impact the support of children and young
people with emotional wellbeing needs is
the lack of knowledge, experience or
confidence for the workforce to engage
directly with the children they work with, or
a lack of the thresholds and pathways to
support them. While many of the projects
and programmes such as Ask Normen and
the Referral Management Centre are
designed to assist staff in putting the right
support in at the right time.(YHMP, 2011)
SCORE-4
Self-harm, traditionally seen as a teenage
issue, increase in number of incidence placed
the staff and head teachers unsure on their
activities (Headteacher update, 2013).
Important approach to self-harm is not to be
shocked or non-judemental which can help
them not to be hurt (Headteacher update,
2013). Self-harm is that issue where the
professionals feel least comfortable in
approaching (Harmless, 2015).
However school teachers are given
guidance to spot mental health warning signs
as well as suicidal behaviour (Headteacher
Update, 2013).
Peers encourage the person with self-harm
to seek the help of school nurse or trusted
teacher. Training in schools colleges and
universities help in develop self-injury policy
along with the bulling policy by which
schools are able to which can best serve
staff, pupils, parents and carers (Lifesigns,
2015)
SCORE-2
School-based sex education is part
of the National Curriculum. In the
2009/10 National School survey,
17% of pupils aged 12- 15 years in
Northamptonshire reported they
had not received any sex
education. Services are not
meeting demand; rates of teenage
pregnancy have risen in
Northamptonshire since 2009
(JSNA REPORT, 2013)
Sure start plus programme was
successful which provide one to
one support by the personal
advisor to young pregnant
women ,was carried out through
health visitors, children centres
and voluntary sector
organizations. This programme
was successful in reducing
domestic violence, housing
situation but less likely to reduce
smoking and initiate breast
feeding (PHE, 2013)
Care to learn programme was able
to reduce the NEET level and 22%
of young parents were back to
education. School nurse work in
relationship with young people as
well as parents (PHE, 2013).
SCORE-3
in Kettering, Northamptonshire
SCORE-3
Acceptability In UK, majority of people with mental
disorder receive no intervention despite
impact of mental disorder and availability of
evidence based interventions. (Campion,
2014)
Northamptonshire have a range of cost-
effective mental health promotion and
interventions, however, recent needs
assessment found that very little mental
health promotion is occurring in
Northamptonshire. Only three interventions
reached more than 1,000 people (Campion,
2014).
The prevalence of mental health needs of
children and adolescents in
Northamptonshire is estimated at 17,000.
In 2013/14, roughly 11,000 (6.5%) children
and young people received direct support
from the YHMP commissioned services
7,000 (4%) in Youth Counselling and 3,500
(2%) in clinical services (YHMP, 2014).
In Northamptonshire people are accessible
to Talk out Loud in which the volunteers,
secondary schools students with special
requirements participate (YHMP, 2014).
whereas the “five to thrive is also
undertaken involving parents, teens, foster
carers, youth justice workers.(YHMP, 2014).
But the early interventions like befriending,
breast feeding initiations and healthy school
programmes are not undertaken in
Northamptonshire (Campion, 2014).
Beyond these services C&YP (children and
young people express issues on access to
services, confused pathway. Thus the key
areas addressed through the
transformation plans are RMC (Referral
Management Centre (RMC)/Single Point of
Access (SPOA) (YHMP, 2014-17).
Many of the challenges that can negatively
impact the support of children and young
people with emotional wellbeing needs is
the lack of knowledge, experience or
confidence for the workforce to engage
directly with the children they work with, or
a lack of the thresholds and pathways to
support them. While many of the projects
and programmes such as Ask Normen and
the Referral Management Centre are
designed to assist staff in putting the right
support in at the right time.(YHMP, 2011)
SCORE-4
Self-harm, traditionally seen as a teenage
issue, increase in number of incidence placed
the staff and head teachers unsure on their
activities (Headteacher update, 2013).
Important approach to self-harm is not to be
shocked or non-judemental which can help
them not to be hurt (Headteacher update,
2013). Self-harm is that issue where the
professionals feel least comfortable in
approaching (Harmless, 2015).
However school teachers are given
guidance to spot mental health warning signs
as well as suicidal behaviour (Headteacher
Update, 2013).
Peers encourage the person with self-harm
to seek the help of school nurse or trusted
teacher. Training in schools colleges and
universities help in develop self-injury policy
along with the bulling policy by which
schools are able to which can best serve
staff, pupils, parents and carers (Lifesigns,
2015)
SCORE-2
School-based sex education is part
of the National Curriculum. In the
2009/10 National School survey,
17% of pupils aged 12- 15 years in
Northamptonshire reported they
had not received any sex
education. Services are not
meeting demand; rates of teenage
pregnancy have risen in
Northamptonshire since 2009
(JSNA REPORT, 2013)
Sure start plus programme was
successful which provide one to
one support by the personal
advisor to young pregnant
women ,was carried out through
health visitors, children centres
and voluntary sector
organizations. This programme
was successful in reducing
domestic violence, housing
situation but less likely to reduce
smoking and initiate breast
feeding (PHE, 2013)
Care to learn programme was able
to reduce the NEET level and 22%
of young parents were back to
education. School nurse work in
relationship with young people as
well as parents (PHE, 2013).
SCORE-3
Priority Grid Criterion Table: Children and Young people among 11-16yrs
in Kettering, Northamptonshire
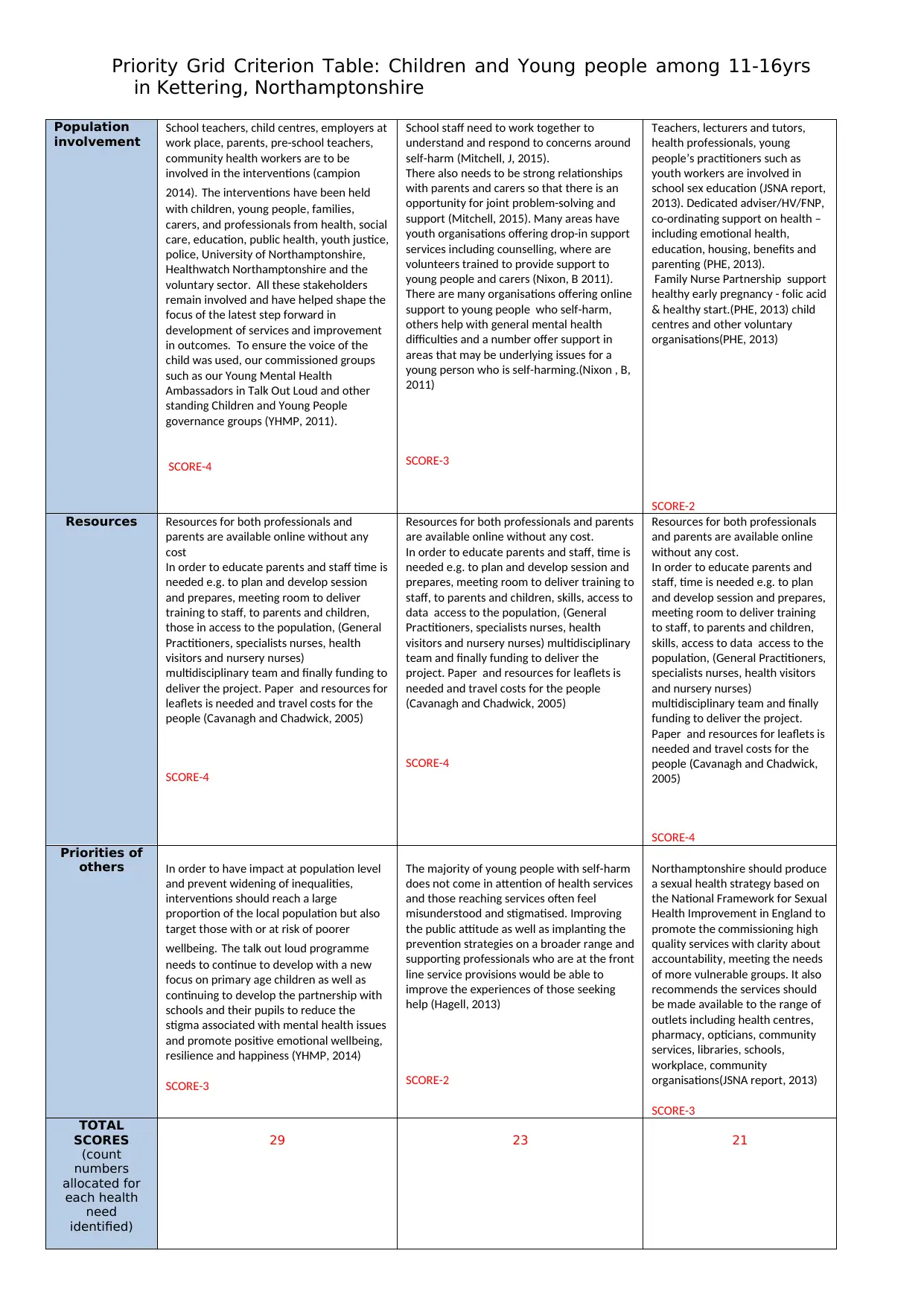
Population
involvement
School teachers, child centres, employers at
work place, parents, pre-school teachers,
community health workers are to be
involved in the interventions (campion
2014). The interventions have been held
with children, young people, families,
carers, and professionals from health, social
care, education, public health, youth justice,
police, University of Northamptonshire,
Healthwatch Northamptonshire and the
voluntary sector. All these stakeholders
remain involved and have helped shape the
focus of the latest step forward in
development of services and improvement
in outcomes. To ensure the voice of the
child was used, our commissioned groups
such as our Young Mental Health
Ambassadors in Talk Out Loud and other
standing Children and Young People
governance groups (YHMP, 2011).
SCORE-4
School staff need to work together to
understand and respond to concerns around
self-harm (Mitchell, J, 2015).
There also needs to be strong relationships
with parents and carers so that there is an
opportunity for joint problem-solving and
support (Mitchell, 2015). Many areas have
youth organisations offering drop-in support
services including counselling, where are
volunteers trained to provide support to
young people and carers (Nixon, B 2011).
There are many organisations offering online
support to young people who self-harm,
others help with general mental health
difficulties and a number offer support in
areas that may be underlying issues for a
young person who is self-harming.(Nixon , B,
2011)
SCORE-3
Teachers, lecturers and tutors,
health professionals, young
people’s practitioners such as
youth workers are involved in
school sex education (JSNA report,
2013). Dedicated adviser/HV/FNP,
co-ordinating support on health –
including emotional health,
education, housing, benefits and
parenting (PHE, 2013).
Family Nurse Partnership support
healthy early pregnancy - folic acid
& healthy start.(PHE, 2013) child
centres and other voluntary
organisations(PHE, 2013)
SCORE-2
Resources Resources for both professionals and
parents are available online without any
cost
In order to educate parents and staff time is
needed e.g. to plan and develop session
and prepares, meeting room to deliver
training to staff, to parents and children,
those in access to the population, (General
Practitioners, specialists nurses, health
visitors and nursery nurses)
multidisciplinary team and finally funding to
deliver the project. Paper and resources for
leaflets is needed and travel costs for the
people (Cavanagh and Chadwick, 2005)
SCORE-4
Resources for both professionals and parents
are available online without any cost.
In order to educate parents and staff, time is
needed e.g. to plan and develop session and
prepares, meeting room to deliver training to
staff, to parents and children, skills, access to
data access to the population, (General
Practitioners, specialists nurses, health
visitors and nursery nurses) multidisciplinary
team and finally funding to deliver the
project. Paper and resources for leaflets is
needed and travel costs for the people
(Cavanagh and Chadwick, 2005)
SCORE-4
Resources for both professionals
and parents are available online
without any cost.
In order to educate parents and
staff, time is needed e.g. to plan
and develop session and prepares,
meeting room to deliver training
to staff, to parents and children,
skills, access to data access to the
population, (General Practitioners,
specialists nurses, health visitors
and nursery nurses)
multidisciplinary team and finally
funding to deliver the project.
Paper and resources for leaflets is
needed and travel costs for the
people (Cavanagh and Chadwick,
2005)
SCORE-4
Priorities of
others In order to have impact at population level
and prevent widening of inequalities,
interventions should reach a large
proportion of the local population but also
target those with or at risk of poorer
wellbeing. The talk out loud programme
needs to continue to develop with a new
focus on primary age children as well as
continuing to develop the partnership with
schools and their pupils to reduce the
stigma associated with mental health issues
and promote positive emotional wellbeing,
resilience and happiness (YHMP, 2014)
SCORE-3
The majority of young people with self-harm
does not come in attention of health services
and those reaching services often feel
misunderstood and stigmatised. Improving
the public attitude as well as implanting the
prevention strategies on a broader range and
supporting professionals who are at the front
line service provisions would be able to
improve the experiences of those seeking
help (Hagell, 2013)
SCORE-2
Northamptonshire should produce
a sexual health strategy based on
the National Framework for Sexual
Health Improvement in England to
promote the commissioning high
quality services with clarity about
accountability, meeting the needs
of more vulnerable groups. It also
recommends the services should
be made available to the range of
outlets including health centres,
pharmacy, opticians, community
services, libraries, schools,
workplace, community
organisations(JSNA report, 2013)
SCORE-3
TOTAL
SCORES
(count
numbers
allocated for
each health
need
identified)
29 23 21
in Kettering, Northamptonshire
Population
involvement
School teachers, child centres, employers at
work place, parents, pre-school teachers,
community health workers are to be
involved in the interventions (campion
2014). The interventions have been held
with children, young people, families,
carers, and professionals from health, social
care, education, public health, youth justice,
police, University of Northamptonshire,
Healthwatch Northamptonshire and the
voluntary sector. All these stakeholders
remain involved and have helped shape the
focus of the latest step forward in
development of services and improvement
in outcomes. To ensure the voice of the
child was used, our commissioned groups
such as our Young Mental Health
Ambassadors in Talk Out Loud and other
standing Children and Young People
governance groups (YHMP, 2011).
SCORE-4
School staff need to work together to
understand and respond to concerns around
self-harm (Mitchell, J, 2015).
There also needs to be strong relationships
with parents and carers so that there is an
opportunity for joint problem-solving and
support (Mitchell, 2015). Many areas have
youth organisations offering drop-in support
services including counselling, where are
volunteers trained to provide support to
young people and carers (Nixon, B 2011).
There are many organisations offering online
support to young people who self-harm,
others help with general mental health
difficulties and a number offer support in
areas that may be underlying issues for a
young person who is self-harming.(Nixon , B,
2011)
SCORE-3
Teachers, lecturers and tutors,
health professionals, young
people’s practitioners such as
youth workers are involved in
school sex education (JSNA report,
2013). Dedicated adviser/HV/FNP,
co-ordinating support on health –
including emotional health,
education, housing, benefits and
parenting (PHE, 2013).
Family Nurse Partnership support
healthy early pregnancy - folic acid
& healthy start.(PHE, 2013) child
centres and other voluntary
organisations(PHE, 2013)
SCORE-2
Resources Resources for both professionals and
parents are available online without any
cost
In order to educate parents and staff time is
needed e.g. to plan and develop session
and prepares, meeting room to deliver
training to staff, to parents and children,
those in access to the population, (General
Practitioners, specialists nurses, health
visitors and nursery nurses)
multidisciplinary team and finally funding to
deliver the project. Paper and resources for
leaflets is needed and travel costs for the
people (Cavanagh and Chadwick, 2005)
SCORE-4
Resources for both professionals and parents
are available online without any cost.
In order to educate parents and staff, time is
needed e.g. to plan and develop session and
prepares, meeting room to deliver training to
staff, to parents and children, skills, access to
data access to the population, (General
Practitioners, specialists nurses, health
visitors and nursery nurses) multidisciplinary
team and finally funding to deliver the
project. Paper and resources for leaflets is
needed and travel costs for the people
(Cavanagh and Chadwick, 2005)
SCORE-4
Resources for both professionals
and parents are available online
without any cost.
In order to educate parents and
staff, time is needed e.g. to plan
and develop session and prepares,
meeting room to deliver training
to staff, to parents and children,
skills, access to data access to the
population, (General Practitioners,
specialists nurses, health visitors
and nursery nurses)
multidisciplinary team and finally
funding to deliver the project.
Paper and resources for leaflets is
needed and travel costs for the
people (Cavanagh and Chadwick,
2005)
SCORE-4
Priorities of
others In order to have impact at population level
and prevent widening of inequalities,
interventions should reach a large
proportion of the local population but also
target those with or at risk of poorer
wellbeing. The talk out loud programme
needs to continue to develop with a new
focus on primary age children as well as
continuing to develop the partnership with
schools and their pupils to reduce the
stigma associated with mental health issues
and promote positive emotional wellbeing,
resilience and happiness (YHMP, 2014)
SCORE-3
The majority of young people with self-harm
does not come in attention of health services
and those reaching services often feel
misunderstood and stigmatised. Improving
the public attitude as well as implanting the
prevention strategies on a broader range and
supporting professionals who are at the front
line service provisions would be able to
improve the experiences of those seeking
help (Hagell, 2013)
SCORE-2
Northamptonshire should produce
a sexual health strategy based on
the National Framework for Sexual
Health Improvement in England to
promote the commissioning high
quality services with clarity about
accountability, meeting the needs
of more vulnerable groups. It also
recommends the services should
be made available to the range of
outlets including health centres,
pharmacy, opticians, community
services, libraries, schools,
workplace, community
organisations(JSNA report, 2013)
SCORE-3
TOTAL
SCORES
(count
numbers
allocated for
each health
need
identified)
29 23 21
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

Priority Grid Criterion Table: Children and Young people among 11-16yrs
in Kettering, Northamptonshire
Identify the health need to be taken forward with supporting rationale (accurately referenced). 300 words
maximum.
The identified health need is mental health admissions among 11-16yrs. NHS England identifies the mental health as the
largest cause of disability in UK, with an estimated cost of 105 billion pounds in a year (NHS, England, 2016). According to
health service executives it is estimated that one in four will experience mental health problems in lifetime (HSE, 2015). It
is estimated that average age at which mental health problem starts is at 14yrs (ChiMat, 2013). The statistics highlights
that the local levels are high than the national levels that are 260.4 per 100, 000 populations when compared to 87.6 (NCC
JSNA Northamptonshire, 2015). As per NCC projected increase in percentage of mentally ill children by 2021is 16% (NCC
Children’s JSNA, 2016).
Mental health is everyone’s responsibility; individual, families, employers, educators and communities who plays major role
in reduction of stigma or discrimination (HM, 2011). In the interim to achieve the objectives of employment, education,
crime reduction, alcohol abuse reduction, self-harm reduction and homelessness cannot be achieved without the
improvement in mental health (HM, 2011).
In 2011, government published its mental health strategy “No health without mental health”(DH, 2014). However
despite of these initiatives, there was a worsening outcome with the increase in demand of health services and number of
people taking their lives (NHS England, 2016). Moreover public attitude and stigma was able to reduce but there is a need
to reenergise and improve mental health across NHS and outside to meet the increasing demand (NHS England, 2016).
In this context NHS England and Department of Health published Future in Minds in 2015 which makes it obvious about
the way in which how children and young people can access high quality mental health care and build strong foundations
(NHS England, 2016).
in Kettering, Northamptonshire
Identify the health need to be taken forward with supporting rationale (accurately referenced). 300 words
maximum.
The identified health need is mental health admissions among 11-16yrs. NHS England identifies the mental health as the
largest cause of disability in UK, with an estimated cost of 105 billion pounds in a year (NHS, England, 2016). According to
health service executives it is estimated that one in four will experience mental health problems in lifetime (HSE, 2015). It
is estimated that average age at which mental health problem starts is at 14yrs (ChiMat, 2013). The statistics highlights
that the local levels are high than the national levels that are 260.4 per 100, 000 populations when compared to 87.6 (NCC
JSNA Northamptonshire, 2015). As per NCC projected increase in percentage of mentally ill children by 2021is 16% (NCC
Children’s JSNA, 2016).
Mental health is everyone’s responsibility; individual, families, employers, educators and communities who plays major role
in reduction of stigma or discrimination (HM, 2011). In the interim to achieve the objectives of employment, education,
crime reduction, alcohol abuse reduction, self-harm reduction and homelessness cannot be achieved without the
improvement in mental health (HM, 2011).
In 2011, government published its mental health strategy “No health without mental health”(DH, 2014). However
despite of these initiatives, there was a worsening outcome with the increase in demand of health services and number of
people taking their lives (NHS England, 2016). Moreover public attitude and stigma was able to reduce but there is a need
to reenergise and improve mental health across NHS and outside to meet the increasing demand (NHS England, 2016).
In this context NHS England and Department of Health published Future in Minds in 2015 which makes it obvious about
the way in which how children and young people can access high quality mental health care and build strong foundations
(NHS England, 2016).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Priority Grid Criterion Table: Children and Young people among 11-16yrs
in Kettering, Northamptonshire
References:
Campion, J (2014) Oppurtunities for action on mental wellbeing and disorder in Northamptonshire. NHS
Northamptonshire [online]. Available from: file:///C:/Opportunities%20for%20action%20on%20mental
%20wellbeing%20and%20disorder%20in%20Northampton%20%20%20%20(1).pdf [4/11/16]
Campion, J (2014) Public Mental Health presentation with focus on children and family. UCL Partners [online].
Available from: file:///E:/PMH_EPBU_seminar_Campion_29-1-14.pdf [1/11/16].
Cavanagh and Chadwick (2005) Health Need Assessment : A Practical Guide. NILE. Available from:
https://nile.northampton.ac.uk/bbcswebdav/pid-3135398-dt-content-rid-3037656_1/courses/NURM009-SEP-
1617/NURM009-SEP-17_ImportedContent_20160919092532/
Health_Needs_Assessment_A_Practical_[9/11/16].
ChiMat (2015) CAMHS need assessment: Northamptonshire. Public Health England [online]. Available from:
http://atlas.chimat.org.uk/IAS/profiles/profile?profileId=34&geoTypeId=#iasProfileSection9 [15/10/16].
Dyer, A (2015) Working to cut Teen Pregnancy. Daventry Express. 10 August. Pp: 21-22
Department for education and skill (2013) Teenage pregnancy next steps guidance for local authorities.
Department of education and skill [online]. Available from:
http://webarchive.nationalarchives.gov.uk/20130401151715/http://www.education.gov.uk/publications/
eOrderingDownload/6597-DfES-ECM-TeenPreg.pdf [9/11/16]
DH (2010) Teenage pregnancy strategy: Beyond 2010. Department For Children, School and Families[online].
Available from: https://www.education.gov.uk/consultations/downloadableDocs/4287_Teenage%20pregnancy
%20strategy_aw8.pdf [11/11/16]
DH (2014) Closing The Gap: Priorities for essential change in Mental health. Department Of Health [online].
Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/281250/
Closing_the_gap_V2_-_17_Feb_2014.pdf [11/11/16]
Foster, C. Allen, S. Rayner, G (2013) Self harm and Suicide amongst children and young people. University of
Salford Manchester [online]. Available from: http://usir.salford.ac.uk/29407/1/Knowsley_SH_Final_Report.pdf
[9/11/16].
Green, H. Meltzer, H. McGinnity, A. Ford, T. Goodman, R (2004) Mental health of children and young people in
Great Britain. New York. Palgrave Macmillan.
HSE (2015) Mental Health Services. Health services Executives [online]. Available from:
http://www.hse.ie/eng/services/list/4/Mental_Health_Services/[11/11/16]
Hagell,A. Coleman,J. Brroks, F.(2015) Key data on Adolescence 2015. The association for young people’s health
[online]. Available from:
http://www.youngpeopleshealth.org.uk/wp-content/uploads/2015/09/KeyData2015.pdf [9/11/2016]
Hawton, K. Bergen, H. Waters, K. Ness, J. Cooper, J. Steeg, S. Kapur, N. (2012) Epidemiology and nature of self-
harm in children and adolescents: findings from the multicentre study of self-harm in England. European
child & adolescent psychiatry, 21 (7), 369-77.
Hawton, K. James, A. (2005) Suicide and deliberate self-harm in young people. BMJ, 330 (7496), 891-894.
Harmless training consultancy (2015) Self harm :What should school staff be aware of?. HARMLESS [Online].
Available from: http://www.harmless.org.uk/blog/self-harm-what-should-school-staff-be-aware-of.html
[8/11/16]
Headteacher update (2013)when primary aged children self-harm. Headteacher update [online]. Available
from: http://www.headteacher-update.com/best-practice-article/when-primary-aged-pupils-self-harm/66713/
[10/11/2016]
Lifesigns (2015) Guidance for Others. Lifesigns [online]. Available from: http://www.lifesigns.org.uk/tag/self-
harm/ [9/11/16]
JSNA Report (2013) Sexual health. Northamptonshire County Council [online]. Available from:
file:///C:/JSNA_SexualHealth_Report%20(1).pdf [11/11/16]
Mitchell, J (2015) Self harm what should be aware of? Head Teacher Update [online]. Available from:
http://www.headteacher-update.com/best-practice-article/self-harm-what-should-school-staff-be-aware-of/
82466 / [9/11/16]
in Kettering, Northamptonshire
References:
Campion, J (2014) Oppurtunities for action on mental wellbeing and disorder in Northamptonshire. NHS
Northamptonshire [online]. Available from: file:///C:/Opportunities%20for%20action%20on%20mental
%20wellbeing%20and%20disorder%20in%20Northampton%20%20%20%20(1).pdf [4/11/16]
Campion, J (2014) Public Mental Health presentation with focus on children and family. UCL Partners [online].
Available from: file:///E:/PMH_EPBU_seminar_Campion_29-1-14.pdf [1/11/16].
Cavanagh and Chadwick (2005) Health Need Assessment : A Practical Guide. NILE. Available from:
https://nile.northampton.ac.uk/bbcswebdav/pid-3135398-dt-content-rid-3037656_1/courses/NURM009-SEP-
1617/NURM009-SEP-17_ImportedContent_20160919092532/
Health_Needs_Assessment_A_Practical_[9/11/16].
ChiMat (2015) CAMHS need assessment: Northamptonshire. Public Health England [online]. Available from:
http://atlas.chimat.org.uk/IAS/profiles/profile?profileId=34&geoTypeId=#iasProfileSection9 [15/10/16].
Dyer, A (2015) Working to cut Teen Pregnancy. Daventry Express. 10 August. Pp: 21-22
Department for education and skill (2013) Teenage pregnancy next steps guidance for local authorities.
Department of education and skill [online]. Available from:
http://webarchive.nationalarchives.gov.uk/20130401151715/http://www.education.gov.uk/publications/
eOrderingDownload/6597-DfES-ECM-TeenPreg.pdf [9/11/16]
DH (2010) Teenage pregnancy strategy: Beyond 2010. Department For Children, School and Families[online].
Available from: https://www.education.gov.uk/consultations/downloadableDocs/4287_Teenage%20pregnancy
%20strategy_aw8.pdf [11/11/16]
DH (2014) Closing The Gap: Priorities for essential change in Mental health. Department Of Health [online].
Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/281250/
Closing_the_gap_V2_-_17_Feb_2014.pdf [11/11/16]
Foster, C. Allen, S. Rayner, G (2013) Self harm and Suicide amongst children and young people. University of
Salford Manchester [online]. Available from: http://usir.salford.ac.uk/29407/1/Knowsley_SH_Final_Report.pdf
[9/11/16].
Green, H. Meltzer, H. McGinnity, A. Ford, T. Goodman, R (2004) Mental health of children and young people in
Great Britain. New York. Palgrave Macmillan.
HSE (2015) Mental Health Services. Health services Executives [online]. Available from:
http://www.hse.ie/eng/services/list/4/Mental_Health_Services/[11/11/16]
Hagell,A. Coleman,J. Brroks, F.(2015) Key data on Adolescence 2015. The association for young people’s health
[online]. Available from:
http://www.youngpeopleshealth.org.uk/wp-content/uploads/2015/09/KeyData2015.pdf [9/11/2016]
Hawton, K. Bergen, H. Waters, K. Ness, J. Cooper, J. Steeg, S. Kapur, N. (2012) Epidemiology and nature of self-
harm in children and adolescents: findings from the multicentre study of self-harm in England. European
child & adolescent psychiatry, 21 (7), 369-77.
Hawton, K. James, A. (2005) Suicide and deliberate self-harm in young people. BMJ, 330 (7496), 891-894.
Harmless training consultancy (2015) Self harm :What should school staff be aware of?. HARMLESS [Online].
Available from: http://www.harmless.org.uk/blog/self-harm-what-should-school-staff-be-aware-of.html
[8/11/16]
Headteacher update (2013)when primary aged children self-harm. Headteacher update [online]. Available
from: http://www.headteacher-update.com/best-practice-article/when-primary-aged-pupils-self-harm/66713/
[10/11/2016]
Lifesigns (2015) Guidance for Others. Lifesigns [online]. Available from: http://www.lifesigns.org.uk/tag/self-
harm/ [9/11/16]
JSNA Report (2013) Sexual health. Northamptonshire County Council [online]. Available from:
file:///C:/JSNA_SexualHealth_Report%20(1).pdf [11/11/16]
Mitchell, J (2015) Self harm what should be aware of? Head Teacher Update [online]. Available from:
http://www.headteacher-update.com/best-practice-article/self-harm-what-should-school-staff-be-aware-of/
82466 / [9/11/16]
Priority Grid Criterion Table: Children and Young people among 11-16yrs
in Kettering, Northamptonshire
NCC (2013-14) PREVENTION OF TEENAGE PREGNANACY. NCC [online]. Available from:
http://www.northamptonshire.gov.uk/en/councilservices/Council/equalities/Documents/PDF%20Documents/
Budget%202013-14/11-002-01-Prevention-TeenagePregnancy.pdf [9/11/16].
NHS Northamptonshire (2009) The story of health inequalities in Northamptonshire from Birth to End of life.
Public Health Annual Report [online]. Available from:
http://www.northamptonshire.nhs.uk/resources/uploads/files/PHAR%20web%20file_Part1.pdf [9/11/16].
NHS CHOICES (2012) Teenage pregnancy death concerns. NHS CHOICES [online]. Available from:
http://www.nhs.uk/news/2012/06june/Pages/teenage-pregnancy-death-rate-concern.aspx [9/11/16]
NCC (2015) Need assessment Report: Mental health of children and young people. NCC [online]. Available from:
file:///E:/Domain4_CYPMentalHealth_NeedsAssessment_Feb2015.pdf [3/11/16]
NCC JSNA Northamptonshire (2015) Health and wellbeing childrens services. NCC [online]. Available from:
file:///E:/Childrens%20JSNA%20Northamptonshire%20profile%20FINAL%20Feb%202015.pdf [15/10/16].
NCC Children’s JSNA (2016) Children and young people JSNA data update- Domain 4:Health and Wellbeing
status. NCC [online]. Available from: file:///E:/CYP_JSNA_DataRefresh_Domain4_March2016.pdf
[23/10/16]
NHS (2010-2013) Northamptonshire Strategy for the emotional wellbeing and Mental health of children and
young people. Northamptonshire Analysis [online]. Available from: file:///E:/CAMHS-Strategy%20for
%20Emotional%20Wellbeing%20and%20Mental%20Health-CIRr%20100510%20(2).pdf
[11/10/16]
NCC JSNA Kettering (2015) Locality profiles helath and wellbeing childrens services Kettering. Northamptonshire
Analysis [online]. Available from: file:///E:/CYP%20JSNA%20Kettering.pdf [ 20/10/16].
NHS England (2016) The five year forward view for mental health. Mental Health Taskforce Strategy [online].
Available from: https://www.england.nhs.uk/wp-content/uploads/2016/02/Mental-Health-Taskforce-FYFV-
final.pdf [11/11/16]
PHE (2013) A framework for supporting teenage mothers and young fathers. Local Government Association
[online]. Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/
524506/PHE_LGA_Framework_for_supporting_teenage_mothers_and_young_fathers.pdf [9/11/16]
Sturgeon,S (2016) NSCB self-harm conference and toolkit impact survey. CFE quality and performance
commissioning [online]. Available from: www.asknormen.co.uk/modules/downloads/download.php?
file_name=255 [ 9/11/16]
Schiller. G (2014) Health needs of Children and young people in Northamptonshire with emphasis on mental
health. PHAST[online]. Available from: file:///E:/my%20assignments/HNA%202/mental%20health/Children's
%20JSNA1.pdf [1/11/16].
YHMP (2014-2017) Northamptonshire strategy for emotional wellbeing and mental health of children and young
people. Northamptonshire county council [online]. Available from : file:///C:/YHMP_20014-
17_Strategy_Draft_v2_6_v1[1].pdf [4/11/16].
in Kettering, Northamptonshire
NCC (2013-14) PREVENTION OF TEENAGE PREGNANACY. NCC [online]. Available from:
http://www.northamptonshire.gov.uk/en/councilservices/Council/equalities/Documents/PDF%20Documents/
Budget%202013-14/11-002-01-Prevention-TeenagePregnancy.pdf [9/11/16].
NHS Northamptonshire (2009) The story of health inequalities in Northamptonshire from Birth to End of life.
Public Health Annual Report [online]. Available from:
http://www.northamptonshire.nhs.uk/resources/uploads/files/PHAR%20web%20file_Part1.pdf [9/11/16].
NHS CHOICES (2012) Teenage pregnancy death concerns. NHS CHOICES [online]. Available from:
http://www.nhs.uk/news/2012/06june/Pages/teenage-pregnancy-death-rate-concern.aspx [9/11/16]
NCC (2015) Need assessment Report: Mental health of children and young people. NCC [online]. Available from:
file:///E:/Domain4_CYPMentalHealth_NeedsAssessment_Feb2015.pdf [3/11/16]
NCC JSNA Northamptonshire (2015) Health and wellbeing childrens services. NCC [online]. Available from:
file:///E:/Childrens%20JSNA%20Northamptonshire%20profile%20FINAL%20Feb%202015.pdf [15/10/16].
NCC Children’s JSNA (2016) Children and young people JSNA data update- Domain 4:Health and Wellbeing
status. NCC [online]. Available from: file:///E:/CYP_JSNA_DataRefresh_Domain4_March2016.pdf
[23/10/16]
NHS (2010-2013) Northamptonshire Strategy for the emotional wellbeing and Mental health of children and
young people. Northamptonshire Analysis [online]. Available from: file:///E:/CAMHS-Strategy%20for
%20Emotional%20Wellbeing%20and%20Mental%20Health-CIRr%20100510%20(2).pdf
[11/10/16]
NCC JSNA Kettering (2015) Locality profiles helath and wellbeing childrens services Kettering. Northamptonshire
Analysis [online]. Available from: file:///E:/CYP%20JSNA%20Kettering.pdf [ 20/10/16].
NHS England (2016) The five year forward view for mental health. Mental Health Taskforce Strategy [online].
Available from: https://www.england.nhs.uk/wp-content/uploads/2016/02/Mental-Health-Taskforce-FYFV-
final.pdf [11/11/16]
PHE (2013) A framework for supporting teenage mothers and young fathers. Local Government Association
[online]. Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/
524506/PHE_LGA_Framework_for_supporting_teenage_mothers_and_young_fathers.pdf [9/11/16]
Sturgeon,S (2016) NSCB self-harm conference and toolkit impact survey. CFE quality and performance
commissioning [online]. Available from: www.asknormen.co.uk/modules/downloads/download.php?
file_name=255 [ 9/11/16]
Schiller. G (2014) Health needs of Children and young people in Northamptonshire with emphasis on mental
health. PHAST[online]. Available from: file:///E:/my%20assignments/HNA%202/mental%20health/Children's
%20JSNA1.pdf [1/11/16].
YHMP (2014-2017) Northamptonshire strategy for emotional wellbeing and mental health of children and young
people. Northamptonshire county council [online]. Available from : file:///C:/YHMP_20014-
17_Strategy_Draft_v2_6_v1[1].pdf [4/11/16].
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9