Procalcitonin: Infection Diagnosis and Monitoring
VerifiedAdded on 2020/04/07
|13
|3009
|39
AI Summary
The assignment requires a critical analysis of a set of research papers focusing on procalcitonin's use as a biomarker for infection diagnosis and management. The provided papers cover studies investigating procalcitonin's efficacy in various conditions like pneumonia, sepsis, and infective endocarditis. The analysis should delve into the strengths and limitations of using procalcitonin, considering its impact on antibiotic stewardship and clinical decision-making.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: PROCALCITONIN
Procalcitonin Guided Diagnosis and Antibiotic Stewardship Revisited
Name of the Student
Name of the University
Author Note
Procalcitonin Guided Diagnosis and Antibiotic Stewardship Revisited
Name of the Student
Name of the University
Author Note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1
PROCALCITONIN
Table of Contents
A. Introduction...........................................................................................................................2
B. Summary of the Article.........................................................................................................5
C. Critical Evaluation of the Article..........................................................................................7
D. Summary and Discussion......................................................................................................8
E. References............................................................................................................................10
PROCALCITONIN
Table of Contents
A. Introduction...........................................................................................................................2
B. Summary of the Article.........................................................................................................5
C. Critical Evaluation of the Article..........................................................................................7
D. Summary and Discussion......................................................................................................8
E. References............................................................................................................................10
2
PROCALCITONIN
A. Introduction
The emerging resistance of the bacteria towards the antimicrobial therapy has leaded
the awareness to reduce the overuse of the antibiotics in the treatment of the infectious
disease. In spite of the use of the diagnostic marker in different fields of medicine, timely and
accurate diagnosis of the bacteria induced disease remains a major challenge. There is a huge
dearth in reliable microbiological and clinical parameters, which can be used to diagnose
bacterial infection via ruling out other associated infection (1, 2). Inflammation markers such
as C-reactive protein (CRP) or White Blood Cells (WBC) lack the desired specificity
required to detect the bacterial infection (3). In the midst of this diagnostic dilemma,
procalcitonin (PCT) is regarded as the potential biomarker for the bacterial infection. PCT is
produced via ubiquitous reaction in response to the mediators or endotoxins generated
because of bacterial infection. Interleukins (IL), tumour necrosis factor (TNF) are chemical
mediators released because of the bacterial reactions and these mediators up regulate the
concentration of PCT in blood. However, PCT is not suitable biomarker for viral infection
because the pro-inflammatory cytokine, interferon gamma produced in response of viral
propagation has been found to attenuate the synthesis of PCT. Nevertheless, this variance of
up regulation and don regulation of PCT is used to discriminate between viral and bacterial
infection (4-7). The concentration of PCT in blood increases with in 6 to 12 hours post
bacterial stimulation and the concentration of circulating PCT decreases into half of the
existing amount when the host immune system or antibiotics controls the infection. The
amount of PCT in blood is co-related with the severity of infection and bacterial load (6-10).
PCT exhibit high diagnostic performance for the differentiating blood stream
infection and bacteraemia. It is also used to discriminate contamination of blood from true
infection in the blood stream, which is common in patients having growth of coagulase-
PROCALCITONIN
A. Introduction
The emerging resistance of the bacteria towards the antimicrobial therapy has leaded
the awareness to reduce the overuse of the antibiotics in the treatment of the infectious
disease. In spite of the use of the diagnostic marker in different fields of medicine, timely and
accurate diagnosis of the bacteria induced disease remains a major challenge. There is a huge
dearth in reliable microbiological and clinical parameters, which can be used to diagnose
bacterial infection via ruling out other associated infection (1, 2). Inflammation markers such
as C-reactive protein (CRP) or White Blood Cells (WBC) lack the desired specificity
required to detect the bacterial infection (3). In the midst of this diagnostic dilemma,
procalcitonin (PCT) is regarded as the potential biomarker for the bacterial infection. PCT is
produced via ubiquitous reaction in response to the mediators or endotoxins generated
because of bacterial infection. Interleukins (IL), tumour necrosis factor (TNF) are chemical
mediators released because of the bacterial reactions and these mediators up regulate the
concentration of PCT in blood. However, PCT is not suitable biomarker for viral infection
because the pro-inflammatory cytokine, interferon gamma produced in response of viral
propagation has been found to attenuate the synthesis of PCT. Nevertheless, this variance of
up regulation and don regulation of PCT is used to discriminate between viral and bacterial
infection (4-7). The concentration of PCT in blood increases with in 6 to 12 hours post
bacterial stimulation and the concentration of circulating PCT decreases into half of the
existing amount when the host immune system or antibiotics controls the infection. The
amount of PCT in blood is co-related with the severity of infection and bacterial load (6-10).
PCT exhibit high diagnostic performance for the differentiating blood stream
infection and bacteraemia. It is also used to discriminate contamination of blood from true
infection in the blood stream, which is common in patients having growth of coagulase-
3
PROCALCITONIN
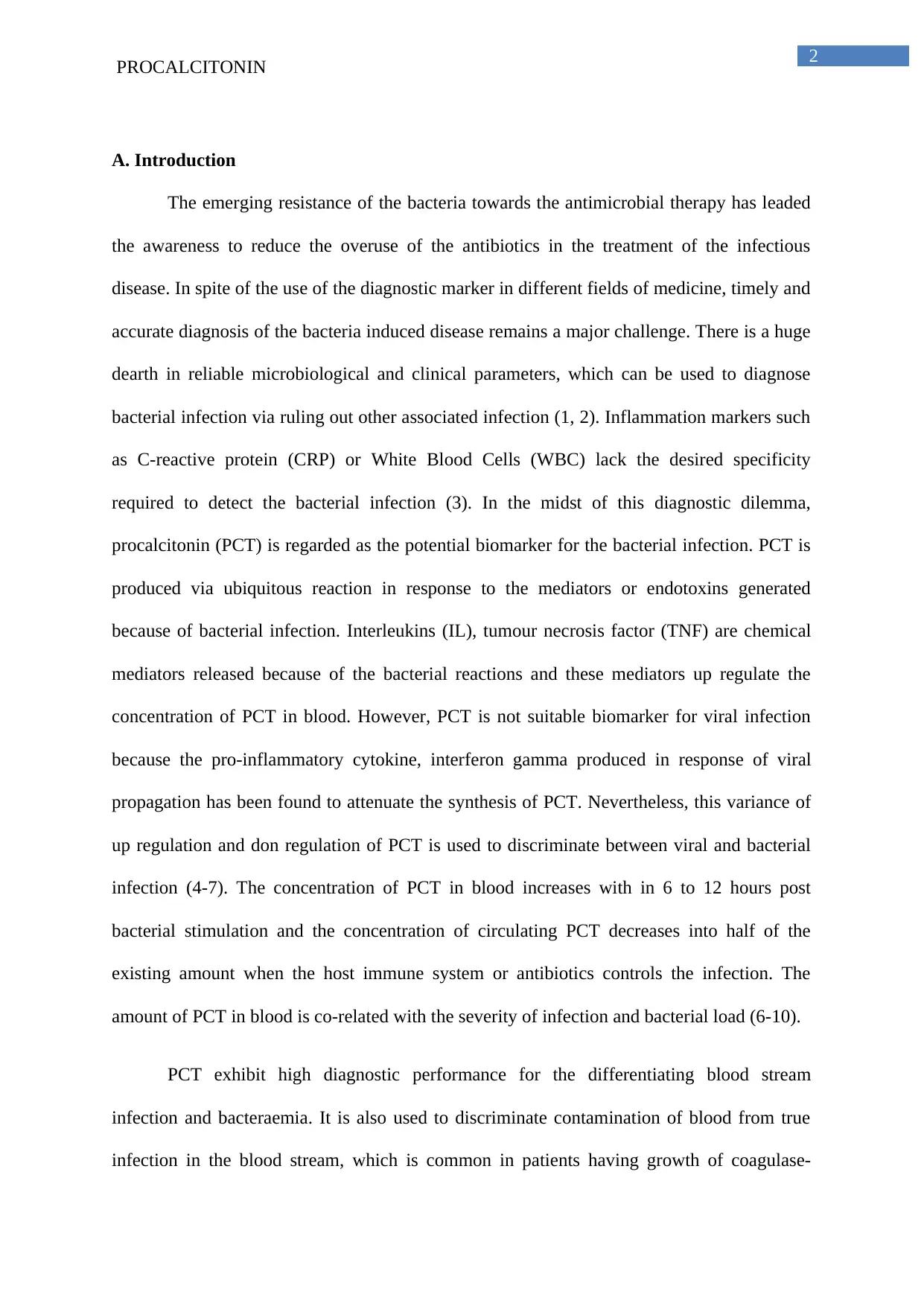
negative staphylococci (11). 0.1 micro gram per litre of PCT has extremely high sensitivity to
selectively exclude true infection in the blood (11). A cut of 0.25 micro grams per litre of
PCT is used to predict the level of bacterial load in patient with urinary tract infection (UTI).
In case of infectious endocarditic, the circulating levels of PCT get increased in comparison
to the non-infected patients (12). PCT is used as a prognostic marker for sever bacterial
diseases having adverse outcome. However, localized infections do not certainly induce the
concentration of PCT (13).
Source: 14
Source: 14
PROCALCITONIN
negative staphylococci (11). 0.1 micro gram per litre of PCT has extremely high sensitivity to
selectively exclude true infection in the blood (11). A cut of 0.25 micro grams per litre of
PCT is used to predict the level of bacterial load in patient with urinary tract infection (UTI).
In case of infectious endocarditic, the circulating levels of PCT get increased in comparison
to the non-infected patients (12). PCT is used as a prognostic marker for sever bacterial
diseases having adverse outcome. However, localized infections do not certainly induce the
concentration of PCT (13).
Source: 14
Source: 14
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4
PROCALCITONIN
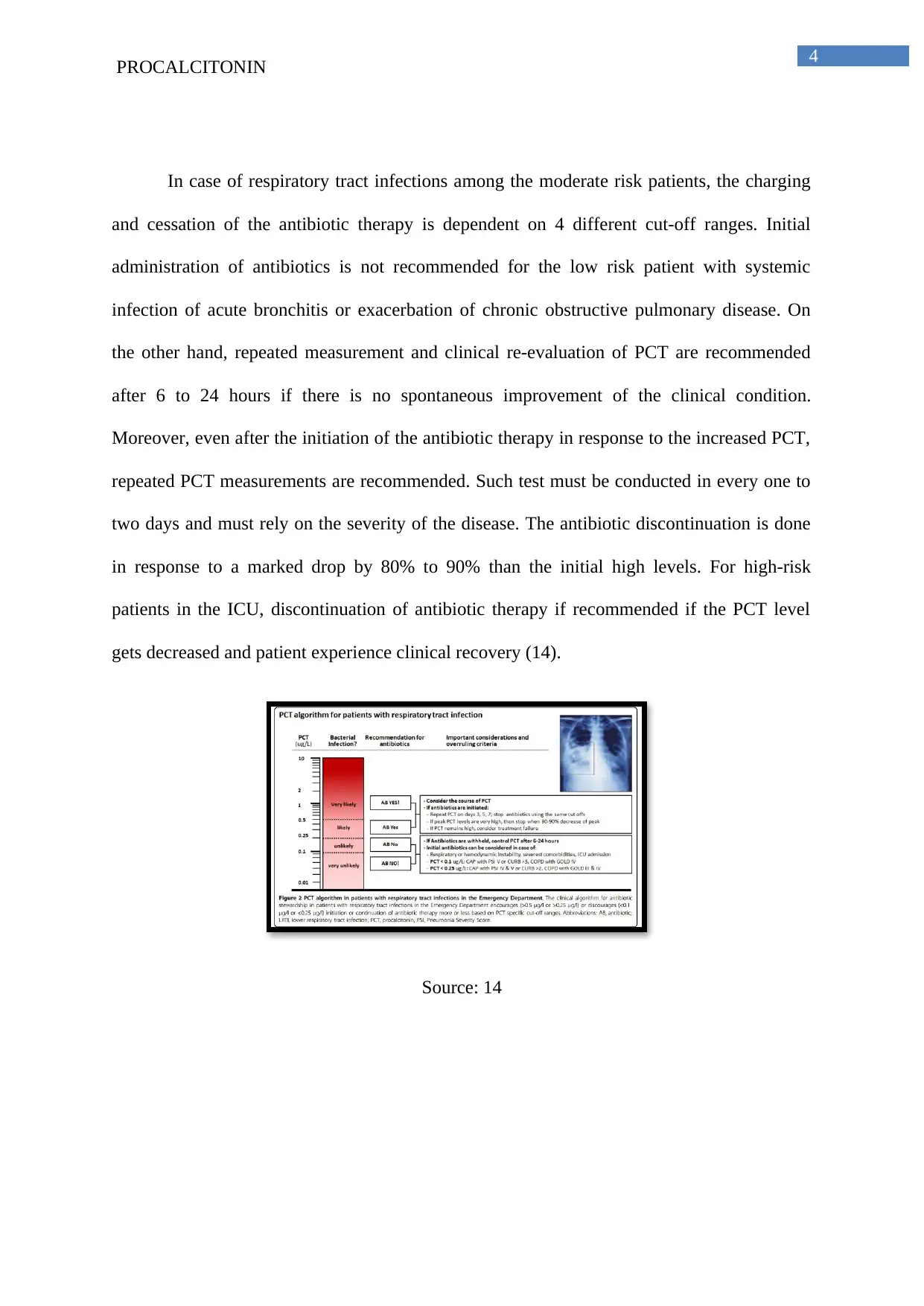
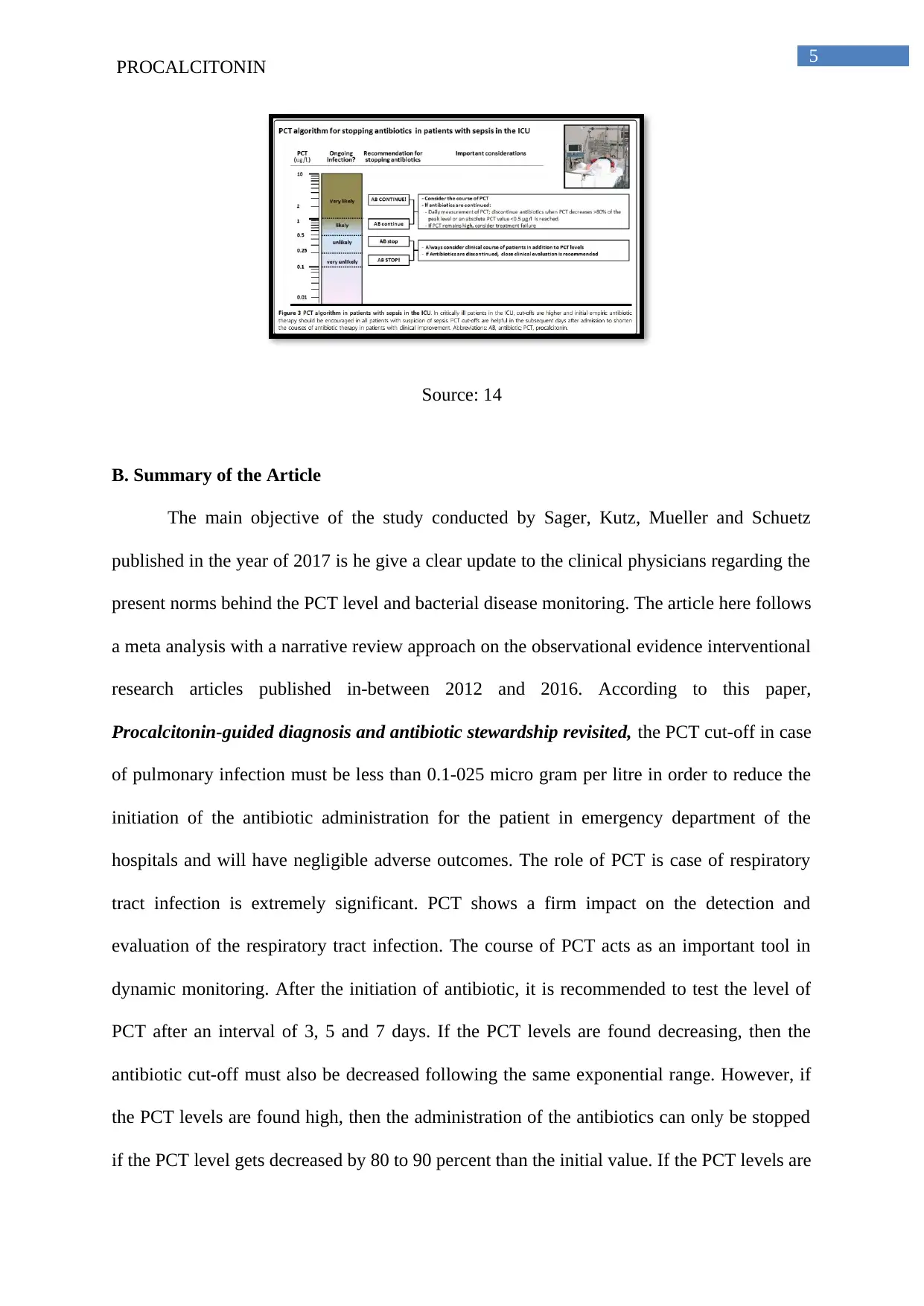
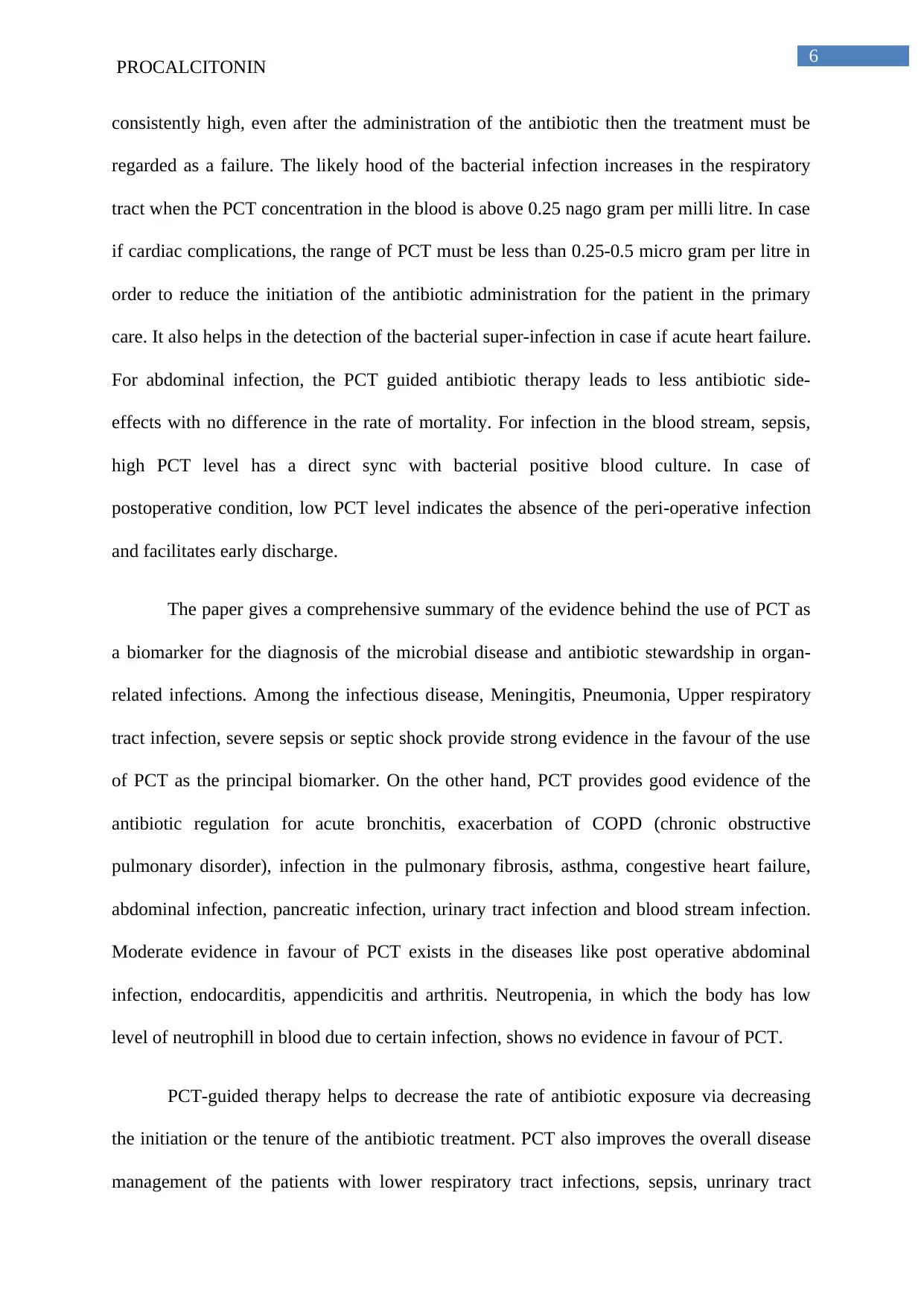
In case of respiratory tract infections among the moderate risk patients, the charging
and cessation of the antibiotic therapy is dependent on 4 different cut-off ranges. Initial
administration of antibiotics is not recommended for the low risk patient with systemic
infection of acute bronchitis or exacerbation of chronic obstructive pulmonary disease. On
the other hand, repeated measurement and clinical re-evaluation of PCT are recommended
after 6 to 24 hours if there is no spontaneous improvement of the clinical condition.
Moreover, even after the initiation of the antibiotic therapy in response to the increased PCT,
repeated PCT measurements are recommended. Such test must be conducted in every one to
two days and must rely on the severity of the disease. The antibiotic discontinuation is done
in response to a marked drop by 80% to 90% than the initial high levels. For high-risk
patients in the ICU, discontinuation of antibiotic therapy if recommended if the PCT level
gets decreased and patient experience clinical recovery (14).
Source: 14
PROCALCITONIN
In case of respiratory tract infections among the moderate risk patients, the charging
and cessation of the antibiotic therapy is dependent on 4 different cut-off ranges. Initial
administration of antibiotics is not recommended for the low risk patient with systemic
infection of acute bronchitis or exacerbation of chronic obstructive pulmonary disease. On
the other hand, repeated measurement and clinical re-evaluation of PCT are recommended
after 6 to 24 hours if there is no spontaneous improvement of the clinical condition.
Moreover, even after the initiation of the antibiotic therapy in response to the increased PCT,
repeated PCT measurements are recommended. Such test must be conducted in every one to
two days and must rely on the severity of the disease. The antibiotic discontinuation is done
in response to a marked drop by 80% to 90% than the initial high levels. For high-risk
patients in the ICU, discontinuation of antibiotic therapy if recommended if the PCT level
gets decreased and patient experience clinical recovery (14).
Source: 14
5
PROCALCITONIN
Source: 14
B. Summary of the Article
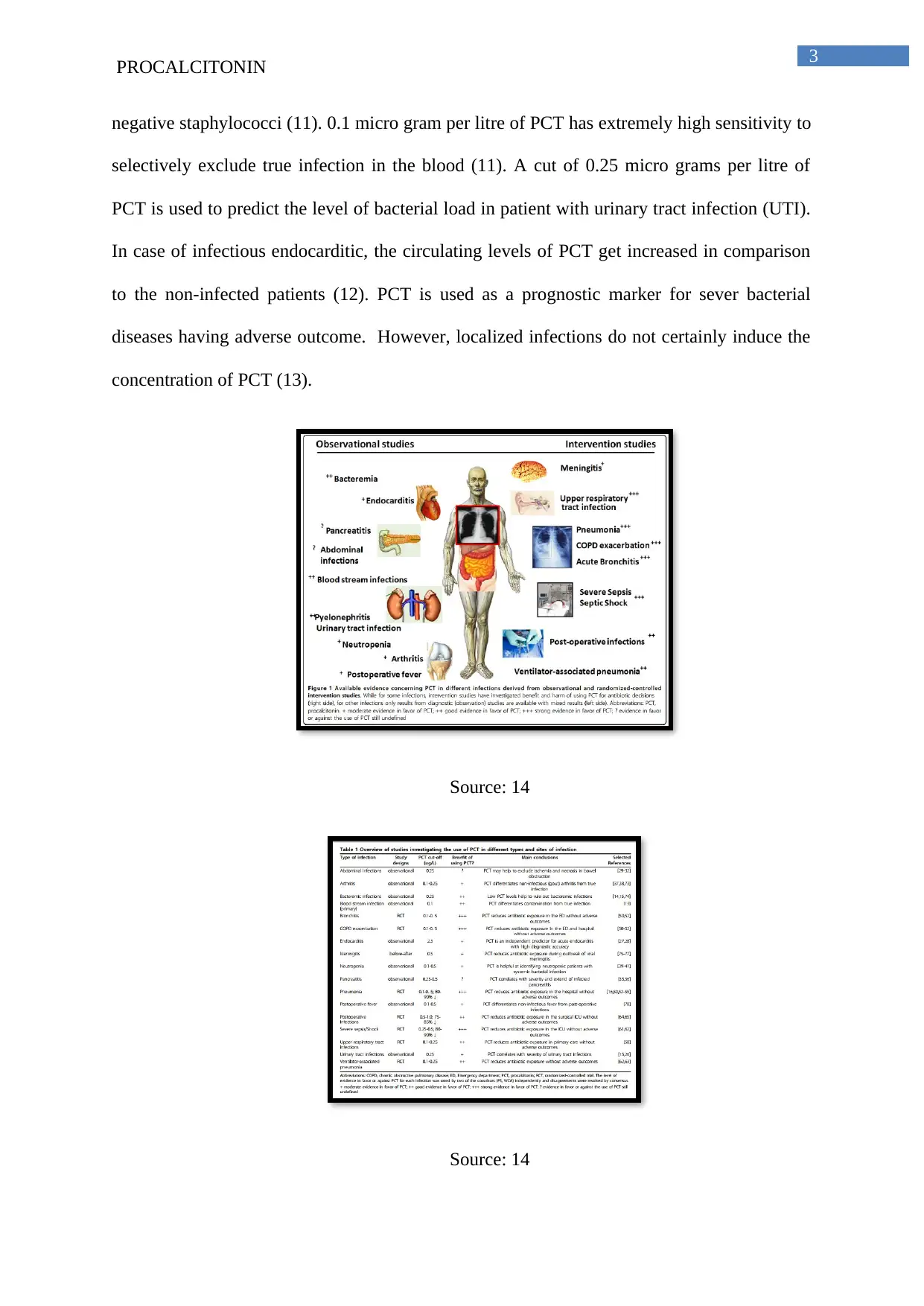
The main objective of the study conducted by Sager, Kutz, Mueller and Schuetz
published in the year of 2017 is he give a clear update to the clinical physicians regarding the
present norms behind the PCT level and bacterial disease monitoring. The article here follows
a meta analysis with a narrative review approach on the observational evidence interventional
research articles published in-between 2012 and 2016. According to this paper,
Procalcitonin-guided diagnosis and antibiotic stewardship revisited, the PCT cut-off in case
of pulmonary infection must be less than 0.1-025 micro gram per litre in order to reduce the
initiation of the antibiotic administration for the patient in emergency department of the
hospitals and will have negligible adverse outcomes. The role of PCT is case of respiratory
tract infection is extremely significant. PCT shows a firm impact on the detection and
evaluation of the respiratory tract infection. The course of PCT acts as an important tool in
dynamic monitoring. After the initiation of antibiotic, it is recommended to test the level of
PCT after an interval of 3, 5 and 7 days. If the PCT levels are found decreasing, then the
antibiotic cut-off must also be decreased following the same exponential range. However, if
the PCT levels are found high, then the administration of the antibiotics can only be stopped
if the PCT level gets decreased by 80 to 90 percent than the initial value. If the PCT levels are
PROCALCITONIN
Source: 14
B. Summary of the Article
The main objective of the study conducted by Sager, Kutz, Mueller and Schuetz
published in the year of 2017 is he give a clear update to the clinical physicians regarding the
present norms behind the PCT level and bacterial disease monitoring. The article here follows
a meta analysis with a narrative review approach on the observational evidence interventional
research articles published in-between 2012 and 2016. According to this paper,
Procalcitonin-guided diagnosis and antibiotic stewardship revisited, the PCT cut-off in case
of pulmonary infection must be less than 0.1-025 micro gram per litre in order to reduce the
initiation of the antibiotic administration for the patient in emergency department of the
hospitals and will have negligible adverse outcomes. The role of PCT is case of respiratory
tract infection is extremely significant. PCT shows a firm impact on the detection and
evaluation of the respiratory tract infection. The course of PCT acts as an important tool in
dynamic monitoring. After the initiation of antibiotic, it is recommended to test the level of
PCT after an interval of 3, 5 and 7 days. If the PCT levels are found decreasing, then the
antibiotic cut-off must also be decreased following the same exponential range. However, if
the PCT levels are found high, then the administration of the antibiotics can only be stopped
if the PCT level gets decreased by 80 to 90 percent than the initial value. If the PCT levels are
6
PROCALCITONIN
consistently high, even after the administration of the antibiotic then the treatment must be
regarded as a failure. The likely hood of the bacterial infection increases in the respiratory
tract when the PCT concentration in the blood is above 0.25 nago gram per milli litre. In case
if cardiac complications, the range of PCT must be less than 0.25-0.5 micro gram per litre in
order to reduce the initiation of the antibiotic administration for the patient in the primary
care. It also helps in the detection of the bacterial super-infection in case if acute heart failure.
For abdominal infection, the PCT guided antibiotic therapy leads to less antibiotic side-
effects with no difference in the rate of mortality. For infection in the blood stream, sepsis,
high PCT level has a direct sync with bacterial positive blood culture. In case of
postoperative condition, low PCT level indicates the absence of the peri-operative infection
and facilitates early discharge.
The paper gives a comprehensive summary of the evidence behind the use of PCT as
a biomarker for the diagnosis of the microbial disease and antibiotic stewardship in organ-
related infections. Among the infectious disease, Meningitis, Pneumonia, Upper respiratory
tract infection, severe sepsis or septic shock provide strong evidence in the favour of the use
of PCT as the principal biomarker. On the other hand, PCT provides good evidence of the
antibiotic regulation for acute bronchitis, exacerbation of COPD (chronic obstructive
pulmonary disorder), infection in the pulmonary fibrosis, asthma, congestive heart failure,
abdominal infection, pancreatic infection, urinary tract infection and blood stream infection.
Moderate evidence in favour of PCT exists in the diseases like post operative abdominal
infection, endocarditis, appendicitis and arthritis. Neutropenia, in which the body has low
level of neutrophill in blood due to certain infection, shows no evidence in favour of PCT.
PCT-guided therapy helps to decrease the rate of antibiotic exposure via decreasing
the initiation or the tenure of the antibiotic treatment. PCT also improves the overall disease
management of the patients with lower respiratory tract infections, sepsis, unrinary tract
PROCALCITONIN
consistently high, even after the administration of the antibiotic then the treatment must be
regarded as a failure. The likely hood of the bacterial infection increases in the respiratory
tract when the PCT concentration in the blood is above 0.25 nago gram per milli litre. In case
if cardiac complications, the range of PCT must be less than 0.25-0.5 micro gram per litre in
order to reduce the initiation of the antibiotic administration for the patient in the primary
care. It also helps in the detection of the bacterial super-infection in case if acute heart failure.
For abdominal infection, the PCT guided antibiotic therapy leads to less antibiotic side-
effects with no difference in the rate of mortality. For infection in the blood stream, sepsis,
high PCT level has a direct sync with bacterial positive blood culture. In case of
postoperative condition, low PCT level indicates the absence of the peri-operative infection
and facilitates early discharge.
The paper gives a comprehensive summary of the evidence behind the use of PCT as
a biomarker for the diagnosis of the microbial disease and antibiotic stewardship in organ-
related infections. Among the infectious disease, Meningitis, Pneumonia, Upper respiratory
tract infection, severe sepsis or septic shock provide strong evidence in the favour of the use
of PCT as the principal biomarker. On the other hand, PCT provides good evidence of the
antibiotic regulation for acute bronchitis, exacerbation of COPD (chronic obstructive
pulmonary disorder), infection in the pulmonary fibrosis, asthma, congestive heart failure,
abdominal infection, pancreatic infection, urinary tract infection and blood stream infection.
Moderate evidence in favour of PCT exists in the diseases like post operative abdominal
infection, endocarditis, appendicitis and arthritis. Neutropenia, in which the body has low
level of neutrophill in blood due to certain infection, shows no evidence in favour of PCT.
PCT-guided therapy helps to decrease the rate of antibiotic exposure via decreasing
the initiation or the tenure of the antibiotic treatment. PCT also improves the overall disease
management of the patients with lower respiratory tract infections, sepsis, unrinary tract
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
PROCALCITONIN
infection, postoperative infections, meningitis and other bacterial super infection like
pneumonia. Recording the levels of PCT post hospitalization substantially reduces the use of
antibiotic in low-risk situations. For infections, PCT kinetics helped in cutting short the
duration of the antibiotic treatment. These strategies are safe and do not increase the chances
of mortality, recurrent infections, or failure of the treatment.
C. Critical Evaluation of the Article
According to me, this comprehensive review paper tried to clearly address the
importance of monitoring the PCT level in blood during the management of the infectious
disease. The paper also took a significant attempt to guide the clinicians to with the role of
PCT in disease treatment and antibiotic administration. The authors here looked for the right
and appropriate papers to perform this systemic review and have stringently cited recent
studies conducted during the tenure of 2012 to 2016 focusing the role of PCT is disease
treatment. All the important and relevant studies that have been conducted in this particular
field are included in this research paper and clearly discussed in a collated manner. All the
important outcomes, which are associated with the level of PCT in the blood are considered
in detail and this include, the characterization of the infectious disease on the basis of their
evidence in favour of PCT. The results obtained will be extremely useful for the healthcare
professionals show nurture a common aim of providing the patients a relief from the
symptoms, which are arising out of the bacterial infection. Moreover, the results are precise
and are represented in a tabular format, further making it easier for the reviewer to
comprehend the data.
However, I spotted certain loop holes in the study. The weakness of the study lies in
the fact that it did not conduct a systematic review, rather selected articles in random from.
Pubmed and hence the obtained conclusion is a bit enthusiastic or directed towards a single
PROCALCITONIN
infection, postoperative infections, meningitis and other bacterial super infection like
pneumonia. Recording the levels of PCT post hospitalization substantially reduces the use of
antibiotic in low-risk situations. For infections, PCT kinetics helped in cutting short the
duration of the antibiotic treatment. These strategies are safe and do not increase the chances
of mortality, recurrent infections, or failure of the treatment.
C. Critical Evaluation of the Article
According to me, this comprehensive review paper tried to clearly address the
importance of monitoring the PCT level in blood during the management of the infectious
disease. The paper also took a significant attempt to guide the clinicians to with the role of
PCT in disease treatment and antibiotic administration. The authors here looked for the right
and appropriate papers to perform this systemic review and have stringently cited recent
studies conducted during the tenure of 2012 to 2016 focusing the role of PCT is disease
treatment. All the important and relevant studies that have been conducted in this particular
field are included in this research paper and clearly discussed in a collated manner. All the
important outcomes, which are associated with the level of PCT in the blood are considered
in detail and this include, the characterization of the infectious disease on the basis of their
evidence in favour of PCT. The results obtained will be extremely useful for the healthcare
professionals show nurture a common aim of providing the patients a relief from the
symptoms, which are arising out of the bacterial infection. Moreover, the results are precise
and are represented in a tabular format, further making it easier for the reviewer to
comprehend the data.
However, I spotted certain loop holes in the study. The weakness of the study lies in
the fact that it did not conduct a systematic review, rather selected articles in random from.
Pubmed and hence the obtained conclusion is a bit enthusiastic or directed towards a single
8
PROCALCITONIN
direction. Moreover, the selected papers did not blind investigators or patients and hence
leading to possible chance of biasness. The meta analysis is performed over the research
papers that are published during the tenure of 2012 and mid-2016. Papers before or after this
particular time frame may have certain different approach on the PCT and its relation with
biomarker of bacterial infection and hence, the possible conflicting data may have got
missed. Moreover, the paper also failed to site a comparative analysis of the CRP and PCT
and their role as a biomarker for infection and antibiotic stewardship. Moreover, the level of
PCT in blood increases even in the absence of bacterial infection and such cases are common
in patients with severe trauma or under post-operative condition (16). The paper only focused
on the PCT as a biomarker for infection but failed to highlight the exceptional scenarios. In
order to perform a comparative the study, the paper might have taken the approach as used by
the paper Infection biomarkers in primary care patients with acute respiratory tract
infections–comparison of Procalcitonin and C-reactive protein, such comparative approach
will help the clinicians to understand the relation between CRP and PCT and how their blood
levels helps in ascertaining the chronicity of the infection.
D. Summary and Discussion
This narrative review put forward several interesting clinical settings for PCT-guided
therapy. The therapy aims to decrease the level of antibiotic exposure via regulating the
initiation or the duration of the overall treatment. PCT has been found to improve the overall
management plan of the patients who are suffering from respiratory tract infections,
septicaemia, UTIs, postoperative infections, meningitis and pneumonia. The reference of the
PCT concentration in blood has helped to reduce the chances of initiation of strong antibiotic
treatment in low-risk disease situations. In case of severe infections like pneumonia,
antibiotic stewardship by regulating PCT kinetics helped in shortening the tenure of the
PROCALCITONIN
direction. Moreover, the selected papers did not blind investigators or patients and hence
leading to possible chance of biasness. The meta analysis is performed over the research
papers that are published during the tenure of 2012 and mid-2016. Papers before or after this
particular time frame may have certain different approach on the PCT and its relation with
biomarker of bacterial infection and hence, the possible conflicting data may have got
missed. Moreover, the paper also failed to site a comparative analysis of the CRP and PCT
and their role as a biomarker for infection and antibiotic stewardship. Moreover, the level of
PCT in blood increases even in the absence of bacterial infection and such cases are common
in patients with severe trauma or under post-operative condition (16). The paper only focused
on the PCT as a biomarker for infection but failed to highlight the exceptional scenarios. In
order to perform a comparative the study, the paper might have taken the approach as used by
the paper Infection biomarkers in primary care patients with acute respiratory tract
infections–comparison of Procalcitonin and C-reactive protein, such comparative approach
will help the clinicians to understand the relation between CRP and PCT and how their blood
levels helps in ascertaining the chronicity of the infection.
D. Summary and Discussion
This narrative review put forward several interesting clinical settings for PCT-guided
therapy. The therapy aims to decrease the level of antibiotic exposure via regulating the
initiation or the duration of the overall treatment. PCT has been found to improve the overall
management plan of the patients who are suffering from respiratory tract infections,
septicaemia, UTIs, postoperative infections, meningitis and pneumonia. The reference of the
PCT concentration in blood has helped to reduce the chances of initiation of strong antibiotic
treatment in low-risk disease situations. In case of severe infections like pneumonia,
antibiotic stewardship by regulating PCT kinetics helped in shortening the tenure of the
9
PROCALCITONIN
antibiotic treatment and early cessation of therapy. These strategies are safe do not include
the chance of mortality, recurrent infections and overall treatment failure.
There lays a strong relation with the antibiotic stewardship in the field of respiratory
infection and sepsis of the blood. However, the concentration of PCT in the blood and it
relation with other types of infectious disease has not been studied in details for several other
types of infections. Thus, the scope of the future research lies on the relation of the PCT
levels in the antibiotic treatment of the non-respiratory infections. The scope will also fall
under the domain of investigating whether the concentration of PCT improves the antibiotic
decision making process in these patients (non-respiratory infections). PCT must also be
tallied with other biomarkers for infection such as CRP, on the scale of diagnostic accuracy
and cost-effectiveness. The emergence of multidrug resistance bacteria has led to generation
of the urgency of designing effective plan to reduce prolong and unnecessary intake
antibiotics. The condition will again be of prime importance in case of self-limiting
nonbacterial diseases.
The healthcare practitioner nurtures a common goal of achieving instant disease
recovery via quick symptom relief in case of bacterial infection. In order to achieve the same,
they administered high-dose antibiotic and the result is the generation of the multi-drug
resistance bacteria ad recurrent infection. The importance of PCT lies in the fact that it
promotes rational use of antibiotics in effective disease treatment.
PROCALCITONIN
antibiotic treatment and early cessation of therapy. These strategies are safe do not include
the chance of mortality, recurrent infections and overall treatment failure.
There lays a strong relation with the antibiotic stewardship in the field of respiratory
infection and sepsis of the blood. However, the concentration of PCT in the blood and it
relation with other types of infectious disease has not been studied in details for several other
types of infections. Thus, the scope of the future research lies on the relation of the PCT
levels in the antibiotic treatment of the non-respiratory infections. The scope will also fall
under the domain of investigating whether the concentration of PCT improves the antibiotic
decision making process in these patients (non-respiratory infections). PCT must also be
tallied with other biomarkers for infection such as CRP, on the scale of diagnostic accuracy
and cost-effectiveness. The emergence of multidrug resistance bacteria has led to generation
of the urgency of designing effective plan to reduce prolong and unnecessary intake
antibiotics. The condition will again be of prime importance in case of self-limiting
nonbacterial diseases.
The healthcare practitioner nurtures a common goal of achieving instant disease
recovery via quick symptom relief in case of bacterial infection. In order to achieve the same,
they administered high-dose antibiotic and the result is the generation of the multi-drug
resistance bacteria ad recurrent infection. The importance of PCT lies in the fact that it
promotes rational use of antibiotics in effective disease treatment.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10
PROCALCITONIN
E. References
1. Lee TH, Goldman L. Evaluation of the patient with acute chest pain. New England
Journal of Medicine. 2000 Apr 20;342(16):1187-95.
2. Agnelli G, Becattini C. Acute pulmonary embolism. New England Journal of
Medicine. 2010 Jul 15;363(3):266-74.
3. Müller B, Harbarth S, Stolz D, Bingisser R, Mueller C, Leuppi J, Nusbaumer C,
Tamm M, Christ-Crain M. Diagnostic and prognostic accuracy of clinical and
laboratory parameters in community-acquired pneumonia. BMC infectious diseases.
2007 Mar 2;7(1):10.
4. Christ-Crain M, MuLLER BE. Procalcitonin in bacterial infections-hype, hope, more
or less?. Swiss Medical Weekly. 2005 Aug 6;135(31-32):451-60.
5. Christ-Crain M, Müller B. Biomarkers in respiratory tract infections: diagnostic
guides to antibiotic prescription, prognostic markers and mediators. European
Respiratory Journal. 2007 Sep 1;30(3):556-73.
6. Linscheid P, Seboek D, Zulewski H, Keller U, Muller B. Autocrine/paracrine role of
inflammation-mediated calcitonin gene-related peptide and adrenomedullin
expression in human adipose tissue. Endocrinology. 2005 Jun 1;146(6):2699-708.
7. Schuetz P, Christ-Crain M, Muller B. Procalcitonin and other biomarkers to improve
assessment and antibiotic stewardship in infections--hope for hype?. Swiss medical
weekly. 2009 Jun 13;139(23):318.
8. Christ-Crain M, Stolz D, Bingisser R, Muller C, Miedinger D, Huber PR, Zimmerli
W, Harbarth S, Tamm M, Muller B. Procalcitonin guidance of antibiotic therapy in
community-acquired pneumonia: a randomized trial. American journal of respiratory
and critical care medicine. 2006 Jul 1;174(1):84-93.
PROCALCITONIN
E. References
1. Lee TH, Goldman L. Evaluation of the patient with acute chest pain. New England
Journal of Medicine. 2000 Apr 20;342(16):1187-95.
2. Agnelli G, Becattini C. Acute pulmonary embolism. New England Journal of
Medicine. 2010 Jul 15;363(3):266-74.
3. Müller B, Harbarth S, Stolz D, Bingisser R, Mueller C, Leuppi J, Nusbaumer C,
Tamm M, Christ-Crain M. Diagnostic and prognostic accuracy of clinical and
laboratory parameters in community-acquired pneumonia. BMC infectious diseases.
2007 Mar 2;7(1):10.
4. Christ-Crain M, MuLLER BE. Procalcitonin in bacterial infections-hype, hope, more
or less?. Swiss Medical Weekly. 2005 Aug 6;135(31-32):451-60.
5. Christ-Crain M, Müller B. Biomarkers in respiratory tract infections: diagnostic
guides to antibiotic prescription, prognostic markers and mediators. European
Respiratory Journal. 2007 Sep 1;30(3):556-73.
6. Linscheid P, Seboek D, Zulewski H, Keller U, Muller B. Autocrine/paracrine role of
inflammation-mediated calcitonin gene-related peptide and adrenomedullin
expression in human adipose tissue. Endocrinology. 2005 Jun 1;146(6):2699-708.
7. Schuetz P, Christ-Crain M, Muller B. Procalcitonin and other biomarkers to improve
assessment and antibiotic stewardship in infections--hope for hype?. Swiss medical
weekly. 2009 Jun 13;139(23):318.
8. Christ-Crain M, Stolz D, Bingisser R, Muller C, Miedinger D, Huber PR, Zimmerli
W, Harbarth S, Tamm M, Muller B. Procalcitonin guidance of antibiotic therapy in
community-acquired pneumonia: a randomized trial. American journal of respiratory
and critical care medicine. 2006 Jul 1;174(1):84-93.
11
PROCALCITONIN
9. Schuetz P, Christ-Crain M, Albrich W, Zimmerli W, Mueller B. Guidance of
antibiotic therapy with procalcitonin in lower respiratory tract infections: insights into
the ProHOSP study. Virulence. 2010 Mar 1;1(2):88-92.
10. Schuetz P, Suter-Widmer I, Chaudri A, Christ-Crain M, Zimmerli W, Mueller B.
Prognostic value of procalcitonin in community-acquired pneumonia. European
Respiratory Journal. 2011 Feb 1;37(2):384-92.
11. van Nieuwkoop C, Bonten TN, van't Wout JW, Kuijper EJ, Groeneveld GH, Becker
MJ, Koster T, Wattel-Louis GH, Delfos NM, Ablij HC, Leyten EM. Procalcitonin
reflects bacteremia and bacterial load in urosepsis syndrome: a prospective
observational study. Critical care. 2010 Nov 17;14(6):R206.
12. Knudsen JB, Fuursted K, Petersen E, Wierup P, Mølgaard H, Poulsen SH, Egeblad H.
Procalcitonin in 759 patients clinically suspected of infective endocarditis. The
American journal of medicine. 2010 Dec 31;123(12):1121-7.
13. Hugle T, Schuetz P, Mueller B, Laifer G, Tyndall A, Regenass S, Daikeler T. Serum
procalcitonin for discrimination between septic and non-septic arthritis. Clinical &
Experimental Rheumatology. 2008 May 1;26(3):453.
14. Schuetz P, Albrich W, Mueller B. Procalcitonin for diagnosis of infection and guide
to antibiotic decisions: past, present and future. BMC medicine. 2011 Sep
22;9(1):107.
15. Meili M, Kutz A, Briel M, Christ-Crain M, Bucher HC, Mueller B, Schuetz P.
Infection biomarkers in primary care patients with acute respiratory tract infections–
comparison of Procalcitonin and C-reactive protein. BMC pulmonary medicine. 2016
Mar 24;16(1):43.
16. Hunziker S, Hügle T, Schuchardt K, Groeschl I, Schuetz P, Mueller B, Dick W,
Eriksson U, Trampuz A. The value of serum procalcitonin level for differentiation of
PROCALCITONIN
9. Schuetz P, Christ-Crain M, Albrich W, Zimmerli W, Mueller B. Guidance of
antibiotic therapy with procalcitonin in lower respiratory tract infections: insights into
the ProHOSP study. Virulence. 2010 Mar 1;1(2):88-92.
10. Schuetz P, Suter-Widmer I, Chaudri A, Christ-Crain M, Zimmerli W, Mueller B.
Prognostic value of procalcitonin in community-acquired pneumonia. European
Respiratory Journal. 2011 Feb 1;37(2):384-92.
11. van Nieuwkoop C, Bonten TN, van't Wout JW, Kuijper EJ, Groeneveld GH, Becker
MJ, Koster T, Wattel-Louis GH, Delfos NM, Ablij HC, Leyten EM. Procalcitonin
reflects bacteremia and bacterial load in urosepsis syndrome: a prospective
observational study. Critical care. 2010 Nov 17;14(6):R206.
12. Knudsen JB, Fuursted K, Petersen E, Wierup P, Mølgaard H, Poulsen SH, Egeblad H.
Procalcitonin in 759 patients clinically suspected of infective endocarditis. The
American journal of medicine. 2010 Dec 31;123(12):1121-7.
13. Hugle T, Schuetz P, Mueller B, Laifer G, Tyndall A, Regenass S, Daikeler T. Serum
procalcitonin for discrimination between septic and non-septic arthritis. Clinical &
Experimental Rheumatology. 2008 May 1;26(3):453.
14. Schuetz P, Albrich W, Mueller B. Procalcitonin for diagnosis of infection and guide
to antibiotic decisions: past, present and future. BMC medicine. 2011 Sep
22;9(1):107.
15. Meili M, Kutz A, Briel M, Christ-Crain M, Bucher HC, Mueller B, Schuetz P.
Infection biomarkers in primary care patients with acute respiratory tract infections–
comparison of Procalcitonin and C-reactive protein. BMC pulmonary medicine. 2016
Mar 24;16(1):43.
16. Hunziker S, Hügle T, Schuchardt K, Groeschl I, Schuetz P, Mueller B, Dick W,
Eriksson U, Trampuz A. The value of serum procalcitonin level for differentiation of

12
PROCALCITONIN
infectious from noninfectious causes of fever after orthopaedic surgery. JBJS. 2010
Jan 1;92(1):138-48.
PROCALCITONIN
infectious from noninfectious causes of fever after orthopaedic surgery. JBJS. 2010
Jan 1;92(1):138-48.
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.




