Professional Nursing Practice: A Critical Incident Analysis
VerifiedAdded on 2023/06/09
|7
|1625
|362
AI Summary
This essay focuses on a critical incident in nursing practice that led to the death of a patient due to a nursing professional's carelessness. The incident highlights the importance of patient care and the need for healthcare professionals to be extra cautious while performing their duty.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: PROFESSIONAL NURSING PRACTICE
PROFESSIONAL NURSING PRACTICE
Name of the Student:
Name of the University:
Author Note:
PROFESSIONAL NURSING PRACTICE
Name of the Student:
Name of the University:
Author Note:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1PROFESSIONAL NURSING PRACTICE
Introduction:
The nursing job role involves the management of many tasks at the same time with
accurate precision, however it should be critically noted that at times due to carelessness of
the nursing professionals, blunders and mishaps can take place which are irreversible and
unrecoverable (Ehsani et al., 2013). This essay will focus on one such blunder that had
happened due to the carelessness of a nurse in handling the pathological sample of a patient
about to undergo a blood transfusion. The careless led to fatal consequences that ultimately
led to the death of the patient within six days of the blood transfusion procedure. In light of
the historical background of nursing practice and medical interventions, many a times due to
improper handling of patients biological reports or samples or even due to delay in conveying
information or conveying misinformation leads to the occurrence of fatal scenarios even
death to be precise (Karavasiliadou & Athanasakis, 2014).
Discussion:
According to a news article published by the ABC news on 12th March, 2003, it has
been made mandatory by the Coroner of South Australia to encourage the engagement of
family members and friends to accompany patients affected with heart-disorders in order to
avoid any discrepancy in terms of manhandling of the patient during pre-surgical procedures
(Laurie & Porter, 2016). This was made mandatory after the massive accidental death of the
71- year old patient due to wrong blood transfusion during the surgery. The incident took
place in Clinpath Laboratories, where two patients Mrs. Ruth Stoll and Mrs. Martha Kovendy
had gone to get their blood samples tested before opting for the transfusion procedure. Mrs.
Stoll had been accompanied by her sister-in-law and Mrs. Kovendy was accompanied by her
husband but both the accompanists were asked to wait at the waiting are with the patients
taken inside to collect the blood. While the collection of the sample was going on, the nursing
professional mislabelled the blood samples. Following this during the surgery, Mrs. Stoll was
monitored with the wrong blood group and as a result she died within six days of her
Introduction:
The nursing job role involves the management of many tasks at the same time with
accurate precision, however it should be critically noted that at times due to carelessness of
the nursing professionals, blunders and mishaps can take place which are irreversible and
unrecoverable (Ehsani et al., 2013). This essay will focus on one such blunder that had
happened due to the carelessness of a nurse in handling the pathological sample of a patient
about to undergo a blood transfusion. The careless led to fatal consequences that ultimately
led to the death of the patient within six days of the blood transfusion procedure. In light of
the historical background of nursing practice and medical interventions, many a times due to
improper handling of patients biological reports or samples or even due to delay in conveying
information or conveying misinformation leads to the occurrence of fatal scenarios even
death to be precise (Karavasiliadou & Athanasakis, 2014).
Discussion:
According to a news article published by the ABC news on 12th March, 2003, it has
been made mandatory by the Coroner of South Australia to encourage the engagement of
family members and friends to accompany patients affected with heart-disorders in order to
avoid any discrepancy in terms of manhandling of the patient during pre-surgical procedures
(Laurie & Porter, 2016). This was made mandatory after the massive accidental death of the
71- year old patient due to wrong blood transfusion during the surgery. The incident took
place in Clinpath Laboratories, where two patients Mrs. Ruth Stoll and Mrs. Martha Kovendy
had gone to get their blood samples tested before opting for the transfusion procedure. Mrs.
Stoll had been accompanied by her sister-in-law and Mrs. Kovendy was accompanied by her
husband but both the accompanists were asked to wait at the waiting are with the patients
taken inside to collect the blood. While the collection of the sample was going on, the nursing
professional mislabelled the blood samples. Following this during the surgery, Mrs. Stoll was
monitored with the wrong blood group and as a result she died within six days of her
2PROFESSIONAL NURSING PRACTICE
operation (Shahrokhi et al., 2013). In relation to the incident, the Coroner in charge at that
point of time, Mr. Wayne Chivell commented that it must be made mandatory that patients
must be accompanied to the spot of collection with their loved ones, as it has been inferred
from the incident that heart-patients are often nervous and are not able to clearly dispense the
correct information about them. Also, the NSQHS, standard 2, launched an initiative of
collaborating with consumers in order to ensure effective service planning, service delivery,
close monitoring and evaluation of all the services combined such that it is more conveniently
accessible to the consumers to avail ("Nursing and Midwifery Board of Australia -
Guidelines", 2018)
Using the Gibb’s reflecting cycle, after critically analysing the event I felt that it was
indeed a fault on the part of the nursing professional who was entrusted with the
responsibility of sample collection. Mislabelling of two different blood samples collected
from different patients can lead to the generation of a fatal effect. At the same time, I feel that
the Coroner’s decision was justified because, company of a loved one would not only help in
reducing the nervousness of the patient but at the same time, the process would take place
under the vigilance of a care provider who would double-ensure that the sample collected is
addressed properly but at the same time I feel that this also exposes the lacunae of our
professional ability. If the assigned job is carried out with extreme precision then there is no
requirement of external factors to serve as a scrutinising tool (Dolansky et al., 2013).
The event was an unfortunate one and it elicited a negative effect on the family
members of the patient, which cannot be argued upon. The family lost a valued family-
member because of the carelessness of a nursing professional who is entrusted with the role
of providing care and not to take away an innocent life. The family would not only be
devastated by the loss of the family member but would not be able to trust the healthcare
organization again.
operation (Shahrokhi et al., 2013). In relation to the incident, the Coroner in charge at that
point of time, Mr. Wayne Chivell commented that it must be made mandatory that patients
must be accompanied to the spot of collection with their loved ones, as it has been inferred
from the incident that heart-patients are often nervous and are not able to clearly dispense the
correct information about them. Also, the NSQHS, standard 2, launched an initiative of
collaborating with consumers in order to ensure effective service planning, service delivery,
close monitoring and evaluation of all the services combined such that it is more conveniently
accessible to the consumers to avail ("Nursing and Midwifery Board of Australia -
Guidelines", 2018)
Using the Gibb’s reflecting cycle, after critically analysing the event I felt that it was
indeed a fault on the part of the nursing professional who was entrusted with the
responsibility of sample collection. Mislabelling of two different blood samples collected
from different patients can lead to the generation of a fatal effect. At the same time, I feel that
the Coroner’s decision was justified because, company of a loved one would not only help in
reducing the nervousness of the patient but at the same time, the process would take place
under the vigilance of a care provider who would double-ensure that the sample collected is
addressed properly but at the same time I feel that this also exposes the lacunae of our
professional ability. If the assigned job is carried out with extreme precision then there is no
requirement of external factors to serve as a scrutinising tool (Dolansky et al., 2013).
The event was an unfortunate one and it elicited a negative effect on the family
members of the patient, which cannot be argued upon. The family lost a valued family-
member because of the carelessness of a nursing professional who is entrusted with the role
of providing care and not to take away an innocent life. The family would not only be
devastated by the loss of the family member but would not be able to trust the healthcare
organization again.
3PROFESSIONAL NURSING PRACTICE
This critical incident has helped me in accessing my capability towards being able to
practice as a care-provider efficiently. It has helped me understand two most important
aspects of my profession and that can be summed up into two factors, firstly to prioritize
patient care and secondly to always keep in mind that what might happen because of an act of
carelessness from my side (Eburn & Dovers, 2015). My profession expects me to cater to the
needs of the patient and contribute efficiently in providing a decent standard of living to the
patient and any casualty from my side would not only prove to fatal for the patient but would
also lead to the devastation of the patient’s family for an entire life-time.
From the insight that I developed after critically going through the case of Ruth Stoll,
I could decipher the facts that Mrs. Stoll had taken her last breath on 4th April, 2001 at the
Wakefield hospital in Adelaide (Middleton & Buist,2013). In the year 1983, she had
undergone a replacement surgery of her aortic valve but had developed ‘aneurysm’, to fix
that another surgery was carried out by Doctor John Stubberfield to replace the aneurysmal
aorta with a Dacron graft, however the process resulted in acute loss of blood that had to be
compensated with blood transfusion and due to the mismatched ABO blood group, blood
transfusion the patient died as a result of acute haemolysis.
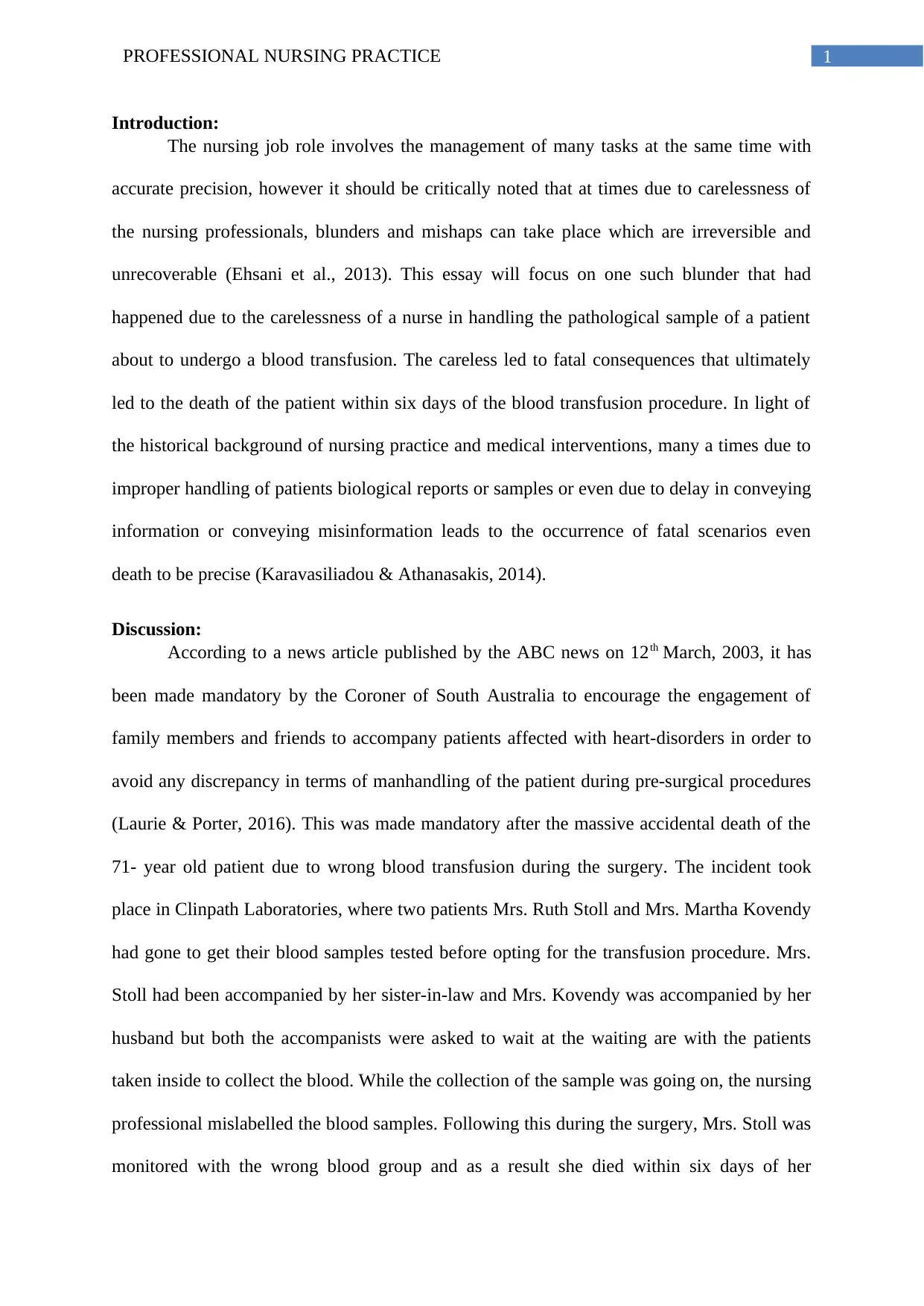
To enhance my effectiveness, the following action-plan would be adopted by me,
Objectives Task Success Criteria Time-frame Resources
Skill-
development
Participation in
training courses
Certified
completion of
training
2-3 weeks In-house
training
department
Error-reporting Being able to
report errors
voluntarily
Being able to
report errors
independently
4 weeks Supervision
under seniors
and trainers
This critical incident has helped me in accessing my capability towards being able to
practice as a care-provider efficiently. It has helped me understand two most important
aspects of my profession and that can be summed up into two factors, firstly to prioritize
patient care and secondly to always keep in mind that what might happen because of an act of
carelessness from my side (Eburn & Dovers, 2015). My profession expects me to cater to the
needs of the patient and contribute efficiently in providing a decent standard of living to the
patient and any casualty from my side would not only prove to fatal for the patient but would
also lead to the devastation of the patient’s family for an entire life-time.
From the insight that I developed after critically going through the case of Ruth Stoll,
I could decipher the facts that Mrs. Stoll had taken her last breath on 4th April, 2001 at the
Wakefield hospital in Adelaide (Middleton & Buist,2013). In the year 1983, she had
undergone a replacement surgery of her aortic valve but had developed ‘aneurysm’, to fix
that another surgery was carried out by Doctor John Stubberfield to replace the aneurysmal
aorta with a Dacron graft, however the process resulted in acute loss of blood that had to be
compensated with blood transfusion and due to the mismatched ABO blood group, blood
transfusion the patient died as a result of acute haemolysis.
To enhance my effectiveness, the following action-plan would be adopted by me,
Objectives Task Success Criteria Time-frame Resources
Skill-
development
Participation in
training courses
Certified
completion of
training
2-3 weeks In-house
training
department
Error-reporting Being able to
report errors
voluntarily
Being able to
report errors
independently
4 weeks Supervision
under seniors
and trainers
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4PROFESSIONAL NURSING PRACTICE
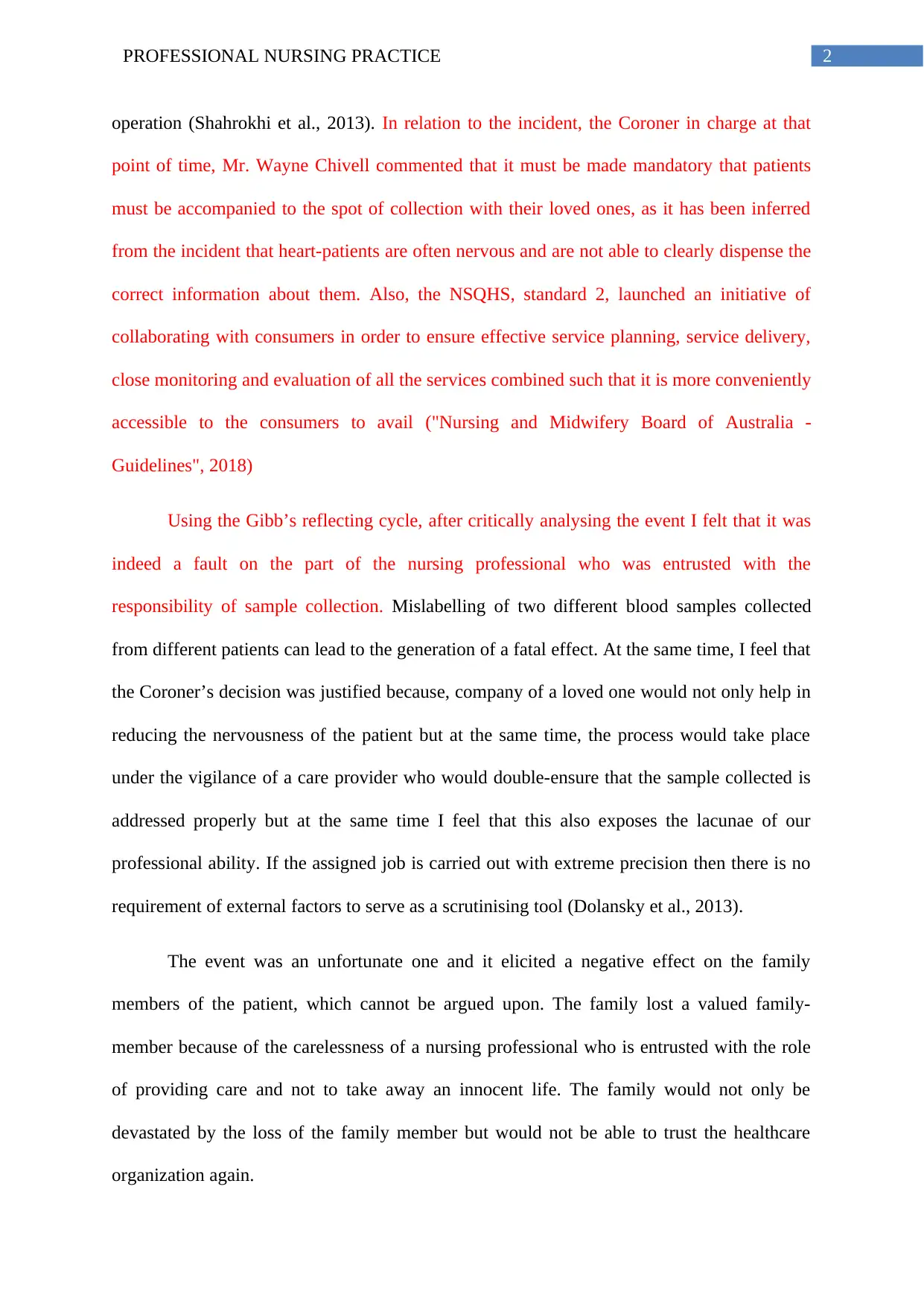
using
organizational
system
Be able to
identify Joint
commission’s
national safety
goals
Be able to
identify
patient’s
correctly and
maintain
records
efficiently
Positive
feedback from
trainers and
supervisors
32 weeks Guidance of
supervisors and
conceptual
knowledge.
Identify patient-
safety risks
Be able to
concentrate
while collecting
samples or use
medicines
safely
Positive
feedback from
patients
< 60 weeks Thorough
practicum and
strong
theoretical
knowledge
Conclusion:
Therefore to conclude, I would like to state that with strict adherence to the action
plan that I have set for myself I would be able to avoid any critical medical error while
carrying out an intervention. At the same time it should also be noted that healthcare
professionals are care providers on who the responsibility of maintenance of the quality life
of the patients depend, hence it is inevitable for them to be extra cautious while performing
their duty.
using
organizational
system
Be able to
identify Joint
commission’s
national safety
goals
Be able to
identify
patient’s
correctly and
maintain
records
efficiently
Positive
feedback from
trainers and
supervisors
32 weeks Guidance of
supervisors and
conceptual
knowledge.
Identify patient-
safety risks
Be able to
concentrate
while collecting
samples or use
medicines
safely
Positive
feedback from
patients
< 60 weeks Thorough
practicum and
strong
theoretical
knowledge
Conclusion:
Therefore to conclude, I would like to state that with strict adherence to the action
plan that I have set for myself I would be able to avoid any critical medical error while
carrying out an intervention. At the same time it should also be noted that healthcare
professionals are care providers on who the responsibility of maintenance of the quality life
of the patients depend, hence it is inevitable for them to be extra cautious while performing
their duty.
5PROFESSIONAL NURSING PRACTICE
References:
Dolansky, M. A., Druschel, K., Helba, M., & Courtney, K. (2013). Nursing student
medication errors: a case study using root cause analysis. Journal of professional
nursing, 29(2), 102-108.
Eburn, M., & Dovers, S. (2015). Learning Lessons from Disasters: Alternatives to Royal
Commissions and Other Quasi‐Judicial Inquiries. Australian Journal of Public
Administration, 74(4), 495-508.
Ehsani, S. R., Cheraghi, M. A., Nejati, A., Salari, A., Esmaeilpoor, A. H., & Nejad, E. M.
(2013). Medication errors of nurses in the emergency department. Journal of medical
ethics and history of medicine, 6.
Karavasiliadou, S., & Athanasakis, E. (2014). An inside look into the factors contributing to
medication errors in the clinical nursing practice. Health Science Journal, 8(1).
Laurie, G. T., & Porter, G. (2016). Mason and McCall Smith's law and medical ethics.
Oxford University Press. Pp 135-140
Nursing and Midwifery Board of Australia - Guidelines. (2018). Retrieved from
http://www.nursingmidwiferyboard.gov.au/Codes-Guidelines-Statements/Codes-
Guidelines.aspx
Middleton, S., & Buist, M. (2013). The coronial reporting of medical-setting deaths: a legal
analysis of the variation in Australian jurisdictions. Melb. UL Rev., 37, 699.
Paterson, C., & Chapman, J. (2013). Enhancing skills of critical reflection to evidence
learning in professional practice. Physical Therapy in Sport, 14(3), 133-138.
References:
Dolansky, M. A., Druschel, K., Helba, M., & Courtney, K. (2013). Nursing student
medication errors: a case study using root cause analysis. Journal of professional
nursing, 29(2), 102-108.
Eburn, M., & Dovers, S. (2015). Learning Lessons from Disasters: Alternatives to Royal
Commissions and Other Quasi‐Judicial Inquiries. Australian Journal of Public
Administration, 74(4), 495-508.
Ehsani, S. R., Cheraghi, M. A., Nejati, A., Salari, A., Esmaeilpoor, A. H., & Nejad, E. M.
(2013). Medication errors of nurses in the emergency department. Journal of medical
ethics and history of medicine, 6.
Karavasiliadou, S., & Athanasakis, E. (2014). An inside look into the factors contributing to
medication errors in the clinical nursing practice. Health Science Journal, 8(1).
Laurie, G. T., & Porter, G. (2016). Mason and McCall Smith's law and medical ethics.
Oxford University Press. Pp 135-140
Nursing and Midwifery Board of Australia - Guidelines. (2018). Retrieved from
http://www.nursingmidwiferyboard.gov.au/Codes-Guidelines-Statements/Codes-
Guidelines.aspx
Middleton, S., & Buist, M. (2013). The coronial reporting of medical-setting deaths: a legal
analysis of the variation in Australian jurisdictions. Melb. UL Rev., 37, 699.
Paterson, C., & Chapman, J. (2013). Enhancing skills of critical reflection to evidence
learning in professional practice. Physical Therapy in Sport, 14(3), 133-138.

6PROFESSIONAL NURSING PRACTICE
Shahrokhi, A., Ebrahimpour, F., & Ghodousi, A. (2013). Factors effective on medication
errors: A nursing view. Journal of research in pharmacy practice, 2(1), 18.
Shahrokhi, A., Ebrahimpour, F., & Ghodousi, A. (2013). Factors effective on medication
errors: A nursing view. Journal of research in pharmacy practice, 2(1), 18.
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





