Implementing Psychoeducation for Bipolar Disorder Management in Psychiatric Ward
VerifiedAdded on 2023/06/10
|37
|10904
|259
AI Summary
This dissertation proposal aims to implement psychoeducation as an effective therapeutic tool that can be used by nursing professionals in a psychiatric ward for the management of bipolar disorder symptoms among admitted patients. The literature review suggests that psychoeducation can improve medication adherence, reduce relapse of symptoms, and enhance mental health. The proposal will be implemented in the psychiatric ward.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: BSC MENTAL HEALTH NURSING
NU3163 Toolkit for professional registration
Name of the Student
Name of the University
Author Note
NU3163 Toolkit for professional registration
Name of the Student
Name of the University
Author Note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1BSC MENTAL HEALTH NURSING
Table of Contents
1.0 Full Dissertation title............................................................................................................2
2.0 Key words............................................................................................................................2
3.0 Rationale/need for the project..............................................................................................2
4.0 Project Methodology............................................................................................................4
4.0.1 Aims..............................................................................................................................4
4.0.2 Literature search strategy..............................................................................................4
4.0.3 Literature review...........................................................................................................5
5.0 Change management..........................................................................................................14
5.0.1 Project initiation..........................................................................................................16
6.0 Conclusion..........................................................................................................................21
References................................................................................................................................22
Appendix..................................................................................................................................34
Table of Contents
1.0 Full Dissertation title............................................................................................................2
2.0 Key words............................................................................................................................2
3.0 Rationale/need for the project..............................................................................................2
4.0 Project Methodology............................................................................................................4
4.0.1 Aims..............................................................................................................................4
4.0.2 Literature search strategy..............................................................................................4
4.0.3 Literature review...........................................................................................................5
5.0 Change management..........................................................................................................14
5.0.1 Project initiation..........................................................................................................16
6.0 Conclusion..........................................................................................................................21
References................................................................................................................................22
Appendix..................................................................................................................................34
2BSC MENTAL HEALTH NURSING
1.0 Full Dissertation title
A proposal to introduce psychoeducation approaches for implementation by nursing
professionals to treat patients suffering from bipolar disorder. The proposal will be
implemented in the psychiatric ward.
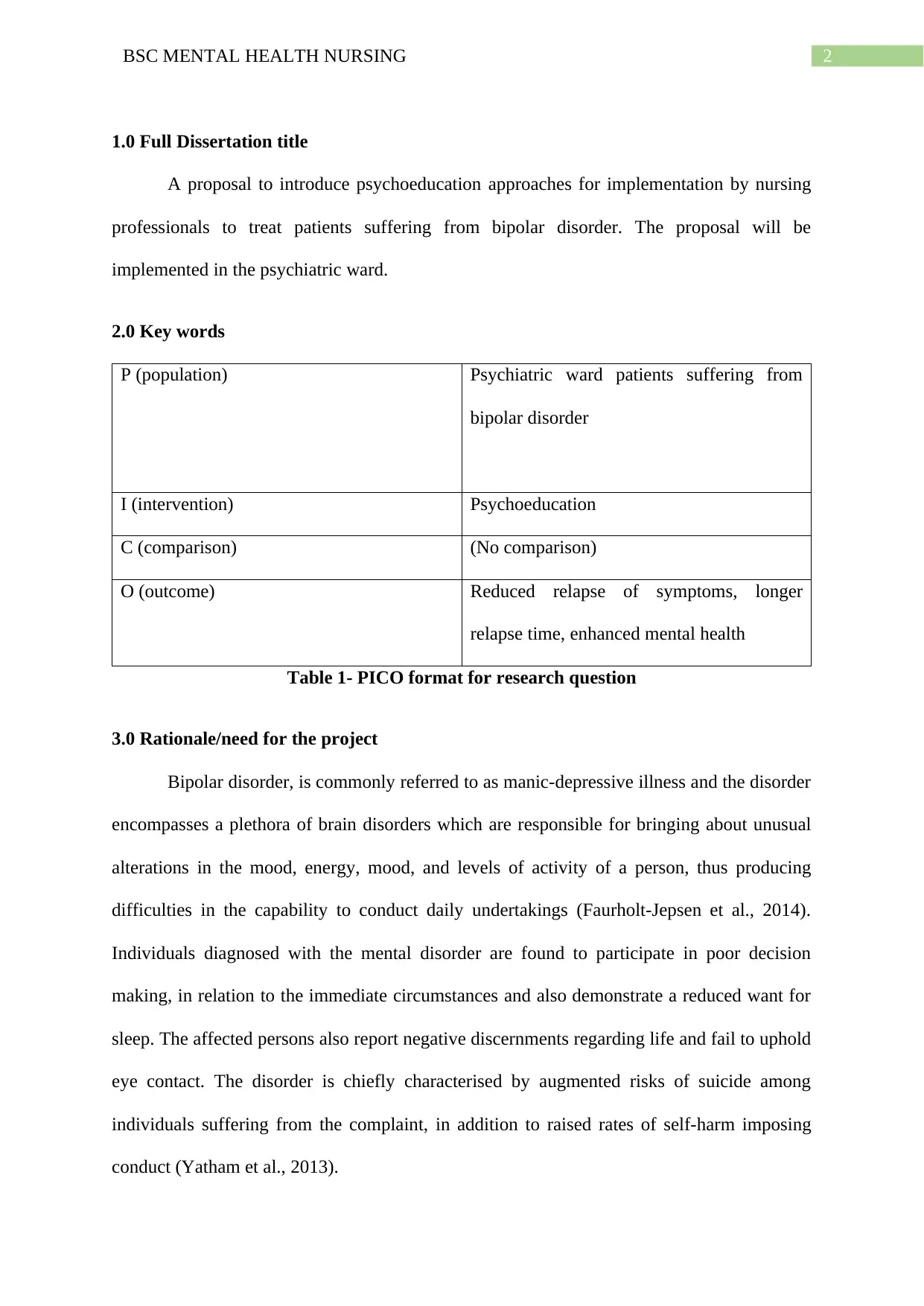
2.0 Key words
P (population) Psychiatric ward patients suffering from
bipolar disorder
I (intervention) Psychoeducation
C (comparison) (No comparison)
O (outcome) Reduced relapse of symptoms, longer
relapse time, enhanced mental health
Table 1- PICO format for research question
3.0 Rationale/need for the project
Bipolar disorder, is commonly referred to as manic-depressive illness and the disorder
encompasses a plethora of brain disorders which are responsible for bringing about unusual
alterations in the mood, energy, mood, and levels of activity of a person, thus producing
difficulties in the capability to conduct daily undertakings (Faurholt-Jepsen et al., 2014).
Individuals diagnosed with the mental disorder are found to participate in poor decision
making, in relation to the immediate circumstances and also demonstrate a reduced want for
sleep. The affected persons also report negative discernments regarding life and fail to uphold
eye contact. The disorder is chiefly characterised by augmented risks of suicide among
individuals suffering from the complaint, in addition to raised rates of self-harm imposing
conduct (Yatham et al., 2013).
1.0 Full Dissertation title
A proposal to introduce psychoeducation approaches for implementation by nursing
professionals to treat patients suffering from bipolar disorder. The proposal will be
implemented in the psychiatric ward.
2.0 Key words
P (population) Psychiatric ward patients suffering from
bipolar disorder
I (intervention) Psychoeducation
C (comparison) (No comparison)
O (outcome) Reduced relapse of symptoms, longer
relapse time, enhanced mental health
Table 1- PICO format for research question
3.0 Rationale/need for the project
Bipolar disorder, is commonly referred to as manic-depressive illness and the disorder
encompasses a plethora of brain disorders which are responsible for bringing about unusual
alterations in the mood, energy, mood, and levels of activity of a person, thus producing
difficulties in the capability to conduct daily undertakings (Faurholt-Jepsen et al., 2014).
Individuals diagnosed with the mental disorder are found to participate in poor decision
making, in relation to the immediate circumstances and also demonstrate a reduced want for
sleep. The affected persons also report negative discernments regarding life and fail to uphold
eye contact. The disorder is chiefly characterised by augmented risks of suicide among
individuals suffering from the complaint, in addition to raised rates of self-harm imposing
conduct (Yatham et al., 2013).
3BSC MENTAL HEALTH NURSING
There were an estimated 4 million cases of mood disorders that also comprised of
bipolar disorder among people living in the UK in 2013. Furthermore, the youth were also
found at an increased likelihood of suffering from bipolar disorder, when compared to their
older counterparts in 2014. While 3-4% of young people aged 16-24 years showed a positive
screening for the mental illness, only 0.4% of older adults aged 65-74 years reported the same
(Mental health foundation, 2015).
While the lifetime prevalence of bipolar disorder in the UK population is 1-2%, it
takes approximately 10.5 years for an affected person to obtain the correct health diagnosis
for the condition (Bipolar UK, 2018). Addiction is a major problem among people suffering
from bipolar disorder. Most patients diagnosed with the mental illness report attempts of self-
medication for reducing the severity of depression and often resort to the use of drugs and
alcohol, with the aim of promoting sleep. Mixed mood episodes that are primarily
characterised by the incidence of both hypomanic or manic and depressive symptoms, in
association with a rapid change of the symptom types, are being progressively recognised as
more prevalent among people diagnosed with bipolar disorder (Phillips & Kupfer, 2013).
Furthermore, there are several medications that are used for treating people suffering
from bipolar disorder. These medications are prescribed with the intent of reducing the
depressive and maniac symptoms (Bourne et al., 2013). Although valproic acid, lithium, and
lamotrigine are commonly used under such circumstances, it often becomes difficult for
nursing professionals and psychiatrists to determine the correct combination of medications
that would prove effective (Malhi, Adams & Berk, 2010). Patients suffering from bipolar
disorder also report an increased susceptibility to a plethora of other social and physical
problems (Piterman, Jones, & Castle, 2010). While the psychological comorbidities most
commonly assume the form of anxiety symptoms that get superimposed on depression or
hypomania, there is a need to detect the exact difference between them. Physical
There were an estimated 4 million cases of mood disorders that also comprised of
bipolar disorder among people living in the UK in 2013. Furthermore, the youth were also
found at an increased likelihood of suffering from bipolar disorder, when compared to their
older counterparts in 2014. While 3-4% of young people aged 16-24 years showed a positive
screening for the mental illness, only 0.4% of older adults aged 65-74 years reported the same
(Mental health foundation, 2015).
While the lifetime prevalence of bipolar disorder in the UK population is 1-2%, it
takes approximately 10.5 years for an affected person to obtain the correct health diagnosis
for the condition (Bipolar UK, 2018). Addiction is a major problem among people suffering
from bipolar disorder. Most patients diagnosed with the mental illness report attempts of self-
medication for reducing the severity of depression and often resort to the use of drugs and
alcohol, with the aim of promoting sleep. Mixed mood episodes that are primarily
characterised by the incidence of both hypomanic or manic and depressive symptoms, in
association with a rapid change of the symptom types, are being progressively recognised as
more prevalent among people diagnosed with bipolar disorder (Phillips & Kupfer, 2013).
Furthermore, there are several medications that are used for treating people suffering
from bipolar disorder. These medications are prescribed with the intent of reducing the
depressive and maniac symptoms (Bourne et al., 2013). Although valproic acid, lithium, and
lamotrigine are commonly used under such circumstances, it often becomes difficult for
nursing professionals and psychiatrists to determine the correct combination of medications
that would prove effective (Malhi, Adams & Berk, 2010). Patients suffering from bipolar
disorder also report an increased susceptibility to a plethora of other social and physical
problems (Piterman, Jones, & Castle, 2010). While the psychological comorbidities most
commonly assume the form of anxiety symptoms that get superimposed on depression or
hypomania, there is a need to detect the exact difference between them. Physical
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4BSC MENTAL HEALTH NURSING
comorbidities also express in the form of cardiovascular complications, poor diet, obesity,
and hyperlipidaemia (Amann, Radua, Wunsch, König & Simhandl, 2017). Thus, it is
essential for the healthcare professionals to adapt to the use of other non-pharmacological
approaches as well for management of bipolar disorder symptoms among patients admitted to
a psychiatric ward. Thus, the proposal aims at implementing psychoeducation, an evidence-
based therapeutic intervention by nursing professionals for educating the people seeking
treatment for bipolar disorder, and effectively managing their illness and other comorbidities.
4.0 Project Methodology
4.0.1 Aims
The project will aim to implement a change strategy that focuses on psychoeducation
as an effective therapeutic tool that can be used by nursing professionals in a psychiatric ward
for the management of bipolar disorder symptoms among admitted patients. The change
management strategies will also be followed by recommendations that can help in operation
of the intervention in nursing practice.
4.0.2 Literature search strategy
The strategy used in this dissertation focuses on a narrative literature review that is
based upon previous findings, pertinent to the research question. Some keywords and search
phrases that were used along with specific boolean operators were ‘AND’ and ‘OR’. These
helped in either broadening or narrowing down the search results and facilitated extraction of
relevant scholarly pieces of literature (McGowan et al., 2016). Three electronic databases
namely, MEDLINE, CINAHL, and PubMed were used for the data extraction. Input of the
search terms were accompanied by addition of filters and limiters that narrowed down the
emphasis of the search, thus ensuring that the exploration was restricted in accordance to the
research question (Aromataris & Riitano, 2014) (refer to appendix). The Appraisal Skills
comorbidities also express in the form of cardiovascular complications, poor diet, obesity,
and hyperlipidaemia (Amann, Radua, Wunsch, König & Simhandl, 2017). Thus, it is
essential for the healthcare professionals to adapt to the use of other non-pharmacological
approaches as well for management of bipolar disorder symptoms among patients admitted to
a psychiatric ward. Thus, the proposal aims at implementing psychoeducation, an evidence-
based therapeutic intervention by nursing professionals for educating the people seeking
treatment for bipolar disorder, and effectively managing their illness and other comorbidities.
4.0 Project Methodology
4.0.1 Aims
The project will aim to implement a change strategy that focuses on psychoeducation
as an effective therapeutic tool that can be used by nursing professionals in a psychiatric ward
for the management of bipolar disorder symptoms among admitted patients. The change
management strategies will also be followed by recommendations that can help in operation
of the intervention in nursing practice.
4.0.2 Literature search strategy
The strategy used in this dissertation focuses on a narrative literature review that is
based upon previous findings, pertinent to the research question. Some keywords and search
phrases that were used along with specific boolean operators were ‘AND’ and ‘OR’. These
helped in either broadening or narrowing down the search results and facilitated extraction of
relevant scholarly pieces of literature (McGowan et al., 2016). Three electronic databases
namely, MEDLINE, CINAHL, and PubMed were used for the data extraction. Input of the
search terms were accompanied by addition of filters and limiters that narrowed down the
emphasis of the search, thus ensuring that the exploration was restricted in accordance to the
research question (Aromataris & Riitano, 2014) (refer to appendix). The Appraisal Skills
5BSC MENTAL HEALTH NURSING
Programme checklist (CASP) was also used to review the articles, with the aim of obtaining
appropriate and evidence-based literature on psychoeducation in mental health practice.
4.0.3 Literature review
Psychoeducation is defined as the procedure that encompasses the delivery of
education and pertinent information to people who seek or receive appropriate mental health
services (Chan, Yip, Tso, Cheng & Tam, 2009). This is usually required by individuals
diagnosed with different mental health condition and their family members. Zhao, Sampson,
Xia and Jayaram (2015) define psychoeducation as the education of a person who has been
diagnosed with a psychiatric disorder regarding the presenting complaints, symptoms,
prognosis and treatment of the illness. They also elaborated on the fact that brief
psychoeducation for any mental illness reports significant reduction in the relapse of the
illness in medium term, and also promotes medication compliance among the affected people
in short term. The statements are consistent with other articles that illustrated the importance
of psychoeducation in improving the compliance to schizophrenia symptoms and health
outcomes, without bringing about any noteworthy onset of adverse health effects (Bäuml et
al., 2016).
In other words, psychoeducation have been found beneficial in improving the
adherence to prescribed treatment regimen and also motivates the mentally ill patients to
accept the recommended maintenance therapy, as per the healthcare guidelines. The
information that is offered to patients seeking psychoeducation support often range from
educating the patients on the potential benefits of the prescribed medication to enhancing
their adherence, to complex, intensive interventions that cover all information related to drugs
and the illness. There often exists a considerable overlap between specific psychotherapies
Programme checklist (CASP) was also used to review the articles, with the aim of obtaining
appropriate and evidence-based literature on psychoeducation in mental health practice.
4.0.3 Literature review
Psychoeducation is defined as the procedure that encompasses the delivery of
education and pertinent information to people who seek or receive appropriate mental health
services (Chan, Yip, Tso, Cheng & Tam, 2009). This is usually required by individuals
diagnosed with different mental health condition and their family members. Zhao, Sampson,
Xia and Jayaram (2015) define psychoeducation as the education of a person who has been
diagnosed with a psychiatric disorder regarding the presenting complaints, symptoms,
prognosis and treatment of the illness. They also elaborated on the fact that brief
psychoeducation for any mental illness reports significant reduction in the relapse of the
illness in medium term, and also promotes medication compliance among the affected people
in short term. The statements are consistent with other articles that illustrated the importance
of psychoeducation in improving the compliance to schizophrenia symptoms and health
outcomes, without bringing about any noteworthy onset of adverse health effects (Bäuml et
al., 2016).
In other words, psychoeducation have been found beneficial in improving the
adherence to prescribed treatment regimen and also motivates the mentally ill patients to
accept the recommended maintenance therapy, as per the healthcare guidelines. The
information that is offered to patients seeking psychoeducation support often range from
educating the patients on the potential benefits of the prescribed medication to enhancing
their adherence, to complex, intensive interventions that cover all information related to drugs
and the illness. There often exists a considerable overlap between specific psychotherapies
6BSC MENTAL HEALTH NURSING
such as, interpersonal and social rhythm therapy (IPSRT), cognitive behavioural therapy
(CBT), and family-focused therapy (FFT) and psychoeducation (Lefley, 2009). D’Souza et
al. (2010) conducted a randomised controlled trial to determine the impacts of
psychoeducation program on the relapse rates of bipolar disorder among patients. Findings of
the RCT suggested that the intervention group participants showed reduced likelihood of
relapse symptoms and also had a longer relapse time (11 weeks), in comparison to the
treatment-as-usual group. Although the sample size was small, further improvements were
also associated with a reduction in the maniac symptoms and improved adherence to
medications, thus suggesting the utility of psychoeducation in bipolar disorder management.
However, Bond and Anderson (2015) argued that individual psychoeducation
programs were not much beneficial in preventing bipolar disorder relapse. Upon conducting a
systematic review of randomised controlled trials, the findings suggested that
psychoeducation was effective in averting any reversion of symptoms (n = 7; OR: 1.98–2.75;
number needed to treat (NNT): 5–7) and hypomanic or manic recurrence (n = 8; OR: 1.68–
2.52; NNT: 6–8). Showing consistency with previous findings, psychoeducation was found to
improve the short‐term medication knowledge and medication adherence. However, failure of
the psychoeducation interventions in preventing bipolar associated depressive symptom
relapse explained the presence of heterogeneity in the individual interventions.
Nonetheless, the interventions that focus on psychoeducation were found operational
in bringing about statistically momentous enhancement in the compliance to medications
among bipolar disorder patients in another RCT (P = 0.008). Upon subjecting patients to 50
minutes of psychoeducation sessions, lower cases of hospital admissions and disorder relapse
were also found in the intervention group, compared to the control group (P = 0.000)
(Javadpour, Hedayati, Dehbozorgi & Azizi, 2013). These were in contrast to the findings
presented by de Azevedo Cardoso et al. (2014) who conducted an RCT for assessing the
such as, interpersonal and social rhythm therapy (IPSRT), cognitive behavioural therapy
(CBT), and family-focused therapy (FFT) and psychoeducation (Lefley, 2009). D’Souza et
al. (2010) conducted a randomised controlled trial to determine the impacts of
psychoeducation program on the relapse rates of bipolar disorder among patients. Findings of
the RCT suggested that the intervention group participants showed reduced likelihood of
relapse symptoms and also had a longer relapse time (11 weeks), in comparison to the
treatment-as-usual group. Although the sample size was small, further improvements were
also associated with a reduction in the maniac symptoms and improved adherence to
medications, thus suggesting the utility of psychoeducation in bipolar disorder management.
However, Bond and Anderson (2015) argued that individual psychoeducation
programs were not much beneficial in preventing bipolar disorder relapse. Upon conducting a
systematic review of randomised controlled trials, the findings suggested that
psychoeducation was effective in averting any reversion of symptoms (n = 7; OR: 1.98–2.75;
number needed to treat (NNT): 5–7) and hypomanic or manic recurrence (n = 8; OR: 1.68–
2.52; NNT: 6–8). Showing consistency with previous findings, psychoeducation was found to
improve the short‐term medication knowledge and medication adherence. However, failure of
the psychoeducation interventions in preventing bipolar associated depressive symptom
relapse explained the presence of heterogeneity in the individual interventions.
Nonetheless, the interventions that focus on psychoeducation were found operational
in bringing about statistically momentous enhancement in the compliance to medications
among bipolar disorder patients in another RCT (P = 0.008). Upon subjecting patients to 50
minutes of psychoeducation sessions, lower cases of hospital admissions and disorder relapse
were also found in the intervention group, compared to the control group (P = 0.000)
(Javadpour, Hedayati, Dehbozorgi & Azizi, 2013). These were in contrast to the findings
presented by de Azevedo Cardoso et al. (2014) who conducted an RCT for assessing the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7BSC MENTAL HEALTH NURSING
effects of brief psychoeducation on bipolar disorder. While there was no statistically
significant difference in the quality of life of patients subjected to psychoeducation and
medication, and the usual care group, the improvement persisted during 6-month follow-up
period, thus establishing the fact that psychoeducation in addition to pharmacological
intervention might prove effective in enhancing quality of life of bipolar disorder patients.
In the words of Gumus, Buzlu and Cakir (2015) individual psychoeducation program
do not prove helpful in reducing recurrence rates of bipolar disorder and its comorbid
psychological symptoms. Although recurrence rate among patients in the experimental study
was 18.9% in intervention group, in comparison to 34.1% in the control group, failure to
achieve a statistical significance between the both made the researchers conclude that
although individual psychoeducation sessions produce positive impacts, they are ineffective
in the prevention of relapse. Besides, it was reinforced by other researchers that
psychoeducation programs in addition to pharmacotherapy are a potential treatment option
that can improve global functioning and medication adherence of bipolar disorder patients.
Increase in medication adherence score of the psycho-educational group from 6.27(0.88) to
7.92(1.38) provided evidence for the worth of psychoeducation as an intervention in mental
health settings (Bahredar, Farid, Ghanizadeh & Birashk, 2014).
Rahmani, Ebrahimi, Ranjbar, Razavi and Asghari (2016) also recommended the
implementation of interventions that focused on psychoeducation in clinical settings by
psychiatric nurses. Significant increase in the mean scores related to medication adherence in
the experimental group than the control group established the fact that educating the patients
on the benefits of the prescribed medications are a good strategy for increasing their
compliance, thus managing the bipolar disorder symptoms. Psychoeducation was confirmed
as the key component of collaborative models related to treatment of mental disorder that
campaigns the rights of all patients being informed about the proposed plan of treatment plan.
effects of brief psychoeducation on bipolar disorder. While there was no statistically
significant difference in the quality of life of patients subjected to psychoeducation and
medication, and the usual care group, the improvement persisted during 6-month follow-up
period, thus establishing the fact that psychoeducation in addition to pharmacological
intervention might prove effective in enhancing quality of life of bipolar disorder patients.
In the words of Gumus, Buzlu and Cakir (2015) individual psychoeducation program
do not prove helpful in reducing recurrence rates of bipolar disorder and its comorbid
psychological symptoms. Although recurrence rate among patients in the experimental study
was 18.9% in intervention group, in comparison to 34.1% in the control group, failure to
achieve a statistical significance between the both made the researchers conclude that
although individual psychoeducation sessions produce positive impacts, they are ineffective
in the prevention of relapse. Besides, it was reinforced by other researchers that
psychoeducation programs in addition to pharmacotherapy are a potential treatment option
that can improve global functioning and medication adherence of bipolar disorder patients.
Increase in medication adherence score of the psycho-educational group from 6.27(0.88) to
7.92(1.38) provided evidence for the worth of psychoeducation as an intervention in mental
health settings (Bahredar, Farid, Ghanizadeh & Birashk, 2014).
Rahmani, Ebrahimi, Ranjbar, Razavi and Asghari (2016) also recommended the
implementation of interventions that focused on psychoeducation in clinical settings by
psychiatric nurses. Significant increase in the mean scores related to medication adherence in
the experimental group than the control group established the fact that educating the patients
on the benefits of the prescribed medications are a good strategy for increasing their
compliance, thus managing the bipolar disorder symptoms. Psychoeducation was confirmed
as the key component of collaborative models related to treatment of mental disorder that
campaigns the rights of all patients being informed about the proposed plan of treatment plan.
8BSC MENTAL HEALTH NURSING
Increase in treatment adherence rate of patients in intervention group from 40.0% (14
patients/pre-test) to 86.7% (26 patients/post-test) established the benefits of six-week
psychoeducation programs on adherence improvement (Eker & Harkın, 2012).
In the words of Husain et al. (2017) a pilot study confirmed the feasibility and
acceptability of psychoeducation intervention in the treatment of bipolar disorder patients by
enhancing their mood and knowledge attitudes. Improved patient satisfaction (ES = 1.41),
greater medication adherence (MMAS-4: ES = 0.81), enhanced measures related to quality of
life (EQ-5D: ES ⇒ 0.88) and improved knowledge towards mania (YMRS: ES = 1.18),
bipolar (BKAQ: ES = 0.68), and depression (BDI: ES = 1.17) helped in establishing the value
of culturally adapted bipolar psychoeducation programmes (CaPE). These were consistent
with findings presented by Chen et al. (2018) who conducted a qualitative study with the
intent of understanding the impact of group psychoeducation on perception of inpatients after
remission of manic episode in bipolar I disorder. Some of the common themes that emerged
from the results were namely, (1) increased patient engagement, (2) recommendation of the
intervention to others, (3) learning environment, (4) facilitators, (5) time, (6) class-taught
versus discussion, and (7) suggestions, among others. It was found that psychoeducation
made the patients more confident, enhanced self-acceptance of the mental disorder, helped
the patients understand the side effects, and also prevented relapse. Similar findings were
reported in another RCT where the patients were subjected to eight group‐based
psychoeducation sessions in the intervention group. Psychoeducation proved beneficial in
management of bipolar disorder by reducing the mania recurrence, showing lower
hospitalisation rates, and bringing about changes in depression scores, global functioning and
mania (Chen et al., 2018).
Soo et al. (2018) conducted a systematic review with the aim of summarising the
effectiveness of psychoeducation and its four modalities (individual, internet- based, group,
Increase in treatment adherence rate of patients in intervention group from 40.0% (14
patients/pre-test) to 86.7% (26 patients/post-test) established the benefits of six-week
psychoeducation programs on adherence improvement (Eker & Harkın, 2012).
In the words of Husain et al. (2017) a pilot study confirmed the feasibility and
acceptability of psychoeducation intervention in the treatment of bipolar disorder patients by
enhancing their mood and knowledge attitudes. Improved patient satisfaction (ES = 1.41),
greater medication adherence (MMAS-4: ES = 0.81), enhanced measures related to quality of
life (EQ-5D: ES ⇒ 0.88) and improved knowledge towards mania (YMRS: ES = 1.18),
bipolar (BKAQ: ES = 0.68), and depression (BDI: ES = 1.17) helped in establishing the value
of culturally adapted bipolar psychoeducation programmes (CaPE). These were consistent
with findings presented by Chen et al. (2018) who conducted a qualitative study with the
intent of understanding the impact of group psychoeducation on perception of inpatients after
remission of manic episode in bipolar I disorder. Some of the common themes that emerged
from the results were namely, (1) increased patient engagement, (2) recommendation of the
intervention to others, (3) learning environment, (4) facilitators, (5) time, (6) class-taught
versus discussion, and (7) suggestions, among others. It was found that psychoeducation
made the patients more confident, enhanced self-acceptance of the mental disorder, helped
the patients understand the side effects, and also prevented relapse. Similar findings were
reported in another RCT where the patients were subjected to eight group‐based
psychoeducation sessions in the intervention group. Psychoeducation proved beneficial in
management of bipolar disorder by reducing the mania recurrence, showing lower
hospitalisation rates, and bringing about changes in depression scores, global functioning and
mania (Chen et al., 2018).
Soo et al. (2018) conducted a systematic review with the aim of summarising the
effectiveness of psychoeducation and its four modalities (individual, internet- based, group,
9BSC MENTAL HEALTH NURSING
family) upon bipolar disorder patients and found that the intervention played a major role in
reducing illness recurrences, decreasing the duration and number of hospitalizations,
increasing time to relapse of illness, enhancing treatment adherence, and reducing stigma
related to mental illnesses. However, Gumus (2017) argued that individual psycho-education
proved ineffective in bringing about an improvement in global functioning and quality of life
of bipolar disorder patients. Nonetheless, the intervention was successful in improving
participation of patients in social activities (T = 2.011; P = 0.048) and taking the initiative for
self-management of condition (T =2.093; P = 0.040). The effectiveness of psychoeducation
programs were also not consistent with the findings presented in another trial where the
intervention was related to constraints in rate of participation among patients and a sense of
motivation among them (Cakir, Bensusan, Akca & Yazici, 2009).
Batista, Baes and Juruena (2011) opined that psychoeducation based interventions had
the potential of significantly improving the treatment adherence, clinical course, and
psychosocial functioning of all bipolar patients. It also decreased the number of recurrences
and relapses per patient and augmented the time to manic, depressive, mixed, and hypomanic
recurrences. The length and instances of hospitalizations were also lower among patients
subjected to the intervention. This was consistent with results of another RCT where
psychoeducation reduced percentages of mood relapse (χ2=6.53; p=0.011) and increased the
relapse free time periods experienced by bipolar disorder patients (log‐rank χ2=4.04;
p=0.044). This helped the authors conclude that group based psychoeducation intervention
for caregivers of bipolar patients can be considered as an useful adjunct to typical treatment
for patients in dropping the risk of relapses, particularly hypomania and mania, in bipolar
disorder (Reinares et al., 2009).
However, Zaretsky, Lancee, Miller, Harris and Parikh (2008) contended that
following optimisation of pharmacological treatment, longer duration of adjunctive CBT was
family) upon bipolar disorder patients and found that the intervention played a major role in
reducing illness recurrences, decreasing the duration and number of hospitalizations,
increasing time to relapse of illness, enhancing treatment adherence, and reducing stigma
related to mental illnesses. However, Gumus (2017) argued that individual psycho-education
proved ineffective in bringing about an improvement in global functioning and quality of life
of bipolar disorder patients. Nonetheless, the intervention was successful in improving
participation of patients in social activities (T = 2.011; P = 0.048) and taking the initiative for
self-management of condition (T =2.093; P = 0.040). The effectiveness of psychoeducation
programs were also not consistent with the findings presented in another trial where the
intervention was related to constraints in rate of participation among patients and a sense of
motivation among them (Cakir, Bensusan, Akca & Yazici, 2009).
Batista, Baes and Juruena (2011) opined that psychoeducation based interventions had
the potential of significantly improving the treatment adherence, clinical course, and
psychosocial functioning of all bipolar patients. It also decreased the number of recurrences
and relapses per patient and augmented the time to manic, depressive, mixed, and hypomanic
recurrences. The length and instances of hospitalizations were also lower among patients
subjected to the intervention. This was consistent with results of another RCT where
psychoeducation reduced percentages of mood relapse (χ2=6.53; p=0.011) and increased the
relapse free time periods experienced by bipolar disorder patients (log‐rank χ2=4.04;
p=0.044). This helped the authors conclude that group based psychoeducation intervention
for caregivers of bipolar patients can be considered as an useful adjunct to typical treatment
for patients in dropping the risk of relapses, particularly hypomania and mania, in bipolar
disorder (Reinares et al., 2009).
However, Zaretsky, Lancee, Miller, Harris and Parikh (2008) contended that
following optimisation of pharmacological treatment, longer duration of adjunctive CBT was
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10BSC MENTAL HEALTH NURSING
found to deliver supplementary benefits over short-term psychoeducation programs for
management and treatment of bipolar disorder. Findings from another cluster feasibility
randomised trial that comprised of community mental health programs (hourly sessions of
psychoeducation) suggested that the intervention was an effective approach in preventing
relapse of bipolar disorder symptoms and also improved the occupational and social
functioning among the patients (regression coefficient 0.68, 95% CI 0.05–1.32) (Lobban et
al., 2010). Morriss et al. (2016) suggested that although structured group psychoeducation
was not able to prove its clinically effectiveness, when compared to parallel intensive un-
structured peer support programs, the former was better acceptable and helped in enhancing
the outcomes among participants by reducing their bipolar episodes. The findings reported
higher attendance in the psychoeducation groups, in comparison to peer support (median 14
sessions vs nine sessions; p=0·026). Furthermore, only 58% participants subjected to
psychoeducation experienced relapse of next episode of bipolar disorder, compared to 65% in
the other group.
According to Kallestad, Wullum, Scott, Stiles and Morken (2016) bipolar disorder
patients who were subjected to group psychoeducation (GP) demonstrated lengthier survival
times when compared to individual psychoeducation (IP), over a period of 27 months
(p<0.05). GP cases associated with harmful substance abuse comorbidity reported shortest
survival time, while those without the comorbidity survived more (p=0.02). Significant
lessening in hospital admissions upon implementation of the group based intervention also
proved the efficacy of psychoeducation in bipolar disorder management (p=0.04).
BalancingMySwing, a nursing based psychoeducation program was also found to improve the
adherence to medications among Taiwanese Han-Chinese bipolar II disorder patients. Owing
to the fact that medication adherence is considered crucial for long-term management of
mental illness management, and non-adherence can pose major challenges while treating
found to deliver supplementary benefits over short-term psychoeducation programs for
management and treatment of bipolar disorder. Findings from another cluster feasibility
randomised trial that comprised of community mental health programs (hourly sessions of
psychoeducation) suggested that the intervention was an effective approach in preventing
relapse of bipolar disorder symptoms and also improved the occupational and social
functioning among the patients (regression coefficient 0.68, 95% CI 0.05–1.32) (Lobban et
al., 2010). Morriss et al. (2016) suggested that although structured group psychoeducation
was not able to prove its clinically effectiveness, when compared to parallel intensive un-
structured peer support programs, the former was better acceptable and helped in enhancing
the outcomes among participants by reducing their bipolar episodes. The findings reported
higher attendance in the psychoeducation groups, in comparison to peer support (median 14
sessions vs nine sessions; p=0·026). Furthermore, only 58% participants subjected to
psychoeducation experienced relapse of next episode of bipolar disorder, compared to 65% in
the other group.
According to Kallestad, Wullum, Scott, Stiles and Morken (2016) bipolar disorder
patients who were subjected to group psychoeducation (GP) demonstrated lengthier survival
times when compared to individual psychoeducation (IP), over a period of 27 months
(p<0.05). GP cases associated with harmful substance abuse comorbidity reported shortest
survival time, while those without the comorbidity survived more (p=0.02). Significant
lessening in hospital admissions upon implementation of the group based intervention also
proved the efficacy of psychoeducation in bipolar disorder management (p=0.04).
BalancingMySwing, a nursing based psychoeducation program was also found to improve the
adherence to medications among Taiwanese Han-Chinese bipolar II disorder patients. Owing
to the fact that medication adherence is considered crucial for long-term management of
mental illness management, and non-adherence can pose major challenges while treating
11BSC MENTAL HEALTH NURSING
bipolar disorder patients, the results helped the authors to establish the efficacy and worth of
the nurse-led psychoeducation program (Lin, Berk & Hsu, 2017).
In the words of George, Sharma and Nair (2013) significant improvements were
observed in a randomised controlled trial among the patients suffering from bipolar disorder
who were placed in the intervention group that comprised of four sessions of
psychoeducation. Substantial enhancement of attitude and knowledge scores among the
investigational group, compared to the control group (p =0.001) established the worth of the
psychoeducation program. Although not noteworthy, differences were also observed in the
adherence to intervention between the two groups (p = 0.111). Thus, the results confirmed the
fact that psychoeducation based intervention concomitant with pharmacotherapy acted as an
easy, cost-effective and feasible intervention for enhancing treatment adherence among
bipolar disorder patients.
Pakpour et al. (2017) also conducted a study where patients with bipolar
disorder were randomised to an intervention group that encompassed five sessions of
psychoeducation and motivational interviewing, together with their family members. Patients
in the intervention group demonstrated enhancement in adherence to medications (baseline
score: 6.03; score at the sixth month: 9.55) when compared to those in the usual care group.
Furthermore, those subjected to psychoeducation and motivational interviewing sessions
were able to manifest improvement in all scores related to their secondary outcomes as well.
This confirmed the effectiveness of psychoeducation approaches on functional and clinical
outcomes of bipolar disorder patients. Parallel to the aforementioned findings,
psychoeducation was found to exert long-term prophylactic impacts on bipolar disorder
affected individuals in another RCT. Patients who had been administered the
psychoeducation program manifested longer time to recurrence for bipolar disorder (log
rank=9.953, P<0.002). The intervention group also reported lesser instances of disease
bipolar disorder patients, the results helped the authors to establish the efficacy and worth of
the nurse-led psychoeducation program (Lin, Berk & Hsu, 2017).
In the words of George, Sharma and Nair (2013) significant improvements were
observed in a randomised controlled trial among the patients suffering from bipolar disorder
who were placed in the intervention group that comprised of four sessions of
psychoeducation. Substantial enhancement of attitude and knowledge scores among the
investigational group, compared to the control group (p =0.001) established the worth of the
psychoeducation program. Although not noteworthy, differences were also observed in the
adherence to intervention between the two groups (p = 0.111). Thus, the results confirmed the
fact that psychoeducation based intervention concomitant with pharmacotherapy acted as an
easy, cost-effective and feasible intervention for enhancing treatment adherence among
bipolar disorder patients.
Pakpour et al. (2017) also conducted a study where patients with bipolar
disorder were randomised to an intervention group that encompassed five sessions of
psychoeducation and motivational interviewing, together with their family members. Patients
in the intervention group demonstrated enhancement in adherence to medications (baseline
score: 6.03; score at the sixth month: 9.55) when compared to those in the usual care group.
Furthermore, those subjected to psychoeducation and motivational interviewing sessions
were able to manifest improvement in all scores related to their secondary outcomes as well.
This confirmed the effectiveness of psychoeducation approaches on functional and clinical
outcomes of bipolar disorder patients. Parallel to the aforementioned findings,
psychoeducation was found to exert long-term prophylactic impacts on bipolar disorder
affected individuals in another RCT. Patients who had been administered the
psychoeducation program manifested longer time to recurrence for bipolar disorder (log
rank=9.953, P<0.002). The intervention group also reported lesser instances of disease
12BSC MENTAL HEALTH NURSING
recurrence (3.86 v. 8.37, F=23.6, P<0.0001) of any kind. Additionally, the patients were
found to spend less time in being acutely ill (154 v. 586 days, F=31.66, P=0.0001) (Colom et
al., 2009).
Conversely, the impacts of a psychoeducation intervention Beating Bipolar on the
psychological quality of life were not adequately established in another study (Smith et al.,
2011). Following randomisation of bipolar disorder patients to the intervention group that
comprised of Beating Bipolar intervention, no significant differences were found between
them and the control group, in relation to the measures of primary outcomes (WHOQOL–
BREF scores). Although the psychoeducation program brought about modest enhancement in
the psychological subsection of the outcome measures, lack of variation in the secondary
outcomes failed to confirm the worth of the program. According to Proudfoot et al. (2012)
online psychoeducation program was not able to result in any momentous improvement in
relation of perceptions of symptom control, reduced stigmatisation perceptions, and
enhancements in the depression and anxiety symptoms among the bipolar disorder patients.
This made the authors elaborate on the need of longer term coaching for online
psychoeducation programs, before they are implemented upon bipolar disorder patients.
However, the Beating Bipolar proved its efficacy in another trial where it assisted
bipolar disorder patients gain an insight into their illness, adopt a healthy behaviour, adhere to
personal routines and adopt a positive attitudes towards their medications. Owing to the fact
that most participants considered the programme likely to be advantageous for the recently
diagnosed patients, this online psychoeducation package proved its worth for managing the
mental disorder in question (Poole, Simpson & Smith, 2012). Colom (2011) also illustrated
that psychoeducation can be categorised as a simple intervention for treatment of mood
disorder and act in the form of an illness-focused and simple therapy that has prophylactic
usefulness in all chief mood disorders. Successful implementation of these psychoeducation
recurrence (3.86 v. 8.37, F=23.6, P<0.0001) of any kind. Additionally, the patients were
found to spend less time in being acutely ill (154 v. 586 days, F=31.66, P=0.0001) (Colom et
al., 2009).
Conversely, the impacts of a psychoeducation intervention Beating Bipolar on the
psychological quality of life were not adequately established in another study (Smith et al.,
2011). Following randomisation of bipolar disorder patients to the intervention group that
comprised of Beating Bipolar intervention, no significant differences were found between
them and the control group, in relation to the measures of primary outcomes (WHOQOL–
BREF scores). Although the psychoeducation program brought about modest enhancement in
the psychological subsection of the outcome measures, lack of variation in the secondary
outcomes failed to confirm the worth of the program. According to Proudfoot et al. (2012)
online psychoeducation program was not able to result in any momentous improvement in
relation of perceptions of symptom control, reduced stigmatisation perceptions, and
enhancements in the depression and anxiety symptoms among the bipolar disorder patients.
This made the authors elaborate on the need of longer term coaching for online
psychoeducation programs, before they are implemented upon bipolar disorder patients.
However, the Beating Bipolar proved its efficacy in another trial where it assisted
bipolar disorder patients gain an insight into their illness, adopt a healthy behaviour, adhere to
personal routines and adopt a positive attitudes towards their medications. Owing to the fact
that most participants considered the programme likely to be advantageous for the recently
diagnosed patients, this online psychoeducation package proved its worth for managing the
mental disorder in question (Poole, Simpson & Smith, 2012). Colom (2011) also illustrated
that psychoeducation can be categorised as a simple intervention for treatment of mood
disorder and act in the form of an illness-focused and simple therapy that has prophylactic
usefulness in all chief mood disorders. Successful implementation of these psychoeducation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13BSC MENTAL HEALTH NURSING
programs require an appropriate setting that includes team effort, open-door policy, and
empowerment of therapeutic coalition.
Contrariwise, results of a post hoc analysis that encompassed a 5-year follow-up study
failed to establish the benefits that psychoeducation exerts on bipolar disorder patients. The
intervention was found beneficial in only treating patients who reported six previous episodes
of the mental disorder. Patients with seven or more episodes did not display any significant
development with psychoeducation, in relation to time to relapse. Patients with greater than
14 episodes were not benefitted from psychoeducation, in terms illness time reduction.
However, the intervention brought about benefits in relation to reduced time spent in
depression, hypomania and mixed episodes among those with 7-8 episodes (except mania)
(Colom et al., 2010). Stafford and Colom (2013) also confirmed the role of psychoeducation
in stabilising bipolar disorder symptoms, reducing chances of relapses, and increasing the
time required for recurrence of the complaints. They elaborated on the fact that
psychoeducation acts as an unassuming method of supporting the prevention of future bipolar
episodes by conveying behavioural training, with the aim of improving insight of illness,
identifying early symptoms and developing coping strategies. The intervention was also
found to empower all the patients for their active participation in their treatment regimen,
thus providing them independence, counteracting the prevailing disengagement of the
therapist and the patients, and increasing the awareness and acceptance of the challenges that
might be encountered during the treatment of bipolar disorder.
Isasi, Echeburua, Liminana and Gonzalez-Pinto (2014) opined that combination of
psychoeducation and cognitive behavioural therapy is effective in the long run for managing
patients diagnosed with refractory bipolar disorder. While those subjected to the intervention
reported fewer rates of hospitalization, in comparison to the control group during the 12-
month evaluation (P = 0.015), they also demonstrated reduced symptoms of anxiety and
programs require an appropriate setting that includes team effort, open-door policy, and
empowerment of therapeutic coalition.
Contrariwise, results of a post hoc analysis that encompassed a 5-year follow-up study
failed to establish the benefits that psychoeducation exerts on bipolar disorder patients. The
intervention was found beneficial in only treating patients who reported six previous episodes
of the mental disorder. Patients with seven or more episodes did not display any significant
development with psychoeducation, in relation to time to relapse. Patients with greater than
14 episodes were not benefitted from psychoeducation, in terms illness time reduction.
However, the intervention brought about benefits in relation to reduced time spent in
depression, hypomania and mixed episodes among those with 7-8 episodes (except mania)
(Colom et al., 2010). Stafford and Colom (2013) also confirmed the role of psychoeducation
in stabilising bipolar disorder symptoms, reducing chances of relapses, and increasing the
time required for recurrence of the complaints. They elaborated on the fact that
psychoeducation acts as an unassuming method of supporting the prevention of future bipolar
episodes by conveying behavioural training, with the aim of improving insight of illness,
identifying early symptoms and developing coping strategies. The intervention was also
found to empower all the patients for their active participation in their treatment regimen,
thus providing them independence, counteracting the prevailing disengagement of the
therapist and the patients, and increasing the awareness and acceptance of the challenges that
might be encountered during the treatment of bipolar disorder.
Isasi, Echeburua, Liminana and Gonzalez-Pinto (2014) opined that combination of
psychoeducation and cognitive behavioural therapy is effective in the long run for managing
patients diagnosed with refractory bipolar disorder. While those subjected to the intervention
reported fewer rates of hospitalization, in comparison to the control group during the 12-
month evaluation (P = 0.015), they also demonstrated reduced symptoms of anxiety and
14BSC MENTAL HEALTH NURSING
depression in 6 months (P=0.006; P=0.019), 12 months (P=0.001; P<0.001) and 5 years
(P<0.001, P<0.001). Substantial differences that appeared in mania and misadjustment
(P=0.009; P<0.001) also established the role of the combination treatment in bipolar disorder
management. The effectiveness of two online programs MoodSwings (MS) and MoodSwings-
Plus (MS-Plus) were also confirmed by a reduction in the mania and depression symptoms in
another study where the program that contained CBT along with psychoeducation (MS-Plus)
proved more beneficial in management of the mental disorder (Lauder et al., 2015). These
aforementioned literature form the rationale for the implementation of psychoeducation as a
change management strategy across a psychiatric ward.
5.0 Change management
Change management can be defined as the procedure that has the prospective of
managing the way by which accountable individuals prepare, upkeep and equip others in
effectively adopting change, with the purpose of driving organisation results and success
(Burke, 2017). While all changes are exceptional in their individual kind, all individuals are
diverse and decades of investigation have recommended that activities can also be undertaken
for manipulating people in discrete transitions (Kuipers et al., 2014). In other arguments,
change management policy offers some type of organized approach for assisting people in
administration that traffics from the current position to the future circumstances. Some of the
most shared change management replicas are the Lewin’s change management model,
ADKAR model, PDSA model (Ashkenas, 2013). The PDSA change management model will
be adopted in this healthcare scenario.
The primary advantage of the PDSA model is related to the fact that it places a due focus
on the development and improvement, in addition to implementation of the change that is
required. PDSA model will be favoured over other change management strategy due to the
fact that it is a powerful approach for fetching a spurt in quality enhancement (Moule, Evans
depression in 6 months (P=0.006; P=0.019), 12 months (P=0.001; P<0.001) and 5 years
(P<0.001, P<0.001). Substantial differences that appeared in mania and misadjustment
(P=0.009; P<0.001) also established the role of the combination treatment in bipolar disorder
management. The effectiveness of two online programs MoodSwings (MS) and MoodSwings-
Plus (MS-Plus) were also confirmed by a reduction in the mania and depression symptoms in
another study where the program that contained CBT along with psychoeducation (MS-Plus)
proved more beneficial in management of the mental disorder (Lauder et al., 2015). These
aforementioned literature form the rationale for the implementation of psychoeducation as a
change management strategy across a psychiatric ward.
5.0 Change management
Change management can be defined as the procedure that has the prospective of
managing the way by which accountable individuals prepare, upkeep and equip others in
effectively adopting change, with the purpose of driving organisation results and success
(Burke, 2017). While all changes are exceptional in their individual kind, all individuals are
diverse and decades of investigation have recommended that activities can also be undertaken
for manipulating people in discrete transitions (Kuipers et al., 2014). In other arguments,
change management policy offers some type of organized approach for assisting people in
administration that traffics from the current position to the future circumstances. Some of the
most shared change management replicas are the Lewin’s change management model,
ADKAR model, PDSA model (Ashkenas, 2013). The PDSA change management model will
be adopted in this healthcare scenario.
The primary advantage of the PDSA model is related to the fact that it places a due focus
on the development and improvement, in addition to implementation of the change that is
required. PDSA model will be favoured over other change management strategy due to the
fact that it is a powerful approach for fetching a spurt in quality enhancement (Moule, Evans
15BSC MENTAL HEALTH NURSING
& Pollard, 2013). This can be accredited to the fact the model creates the provision for its
leaders to evaluate and explore the change on a small care, with the intent of determining the
effectiveness, prior to its complete implementation on a wider scale. The model also allows
the leaders to recognise the worth and lucrativeness of the change, upon its application in
real-time settings, on a wider scale. Furthermore, the fact that the PDSA approach facilitates
the implementing leaders to identify the potential barriers and challenges that are not
ostensible prior to the application of the proposed tactic creates the provision for bringing
about much needed modifications and amendments before the actual change. The model can
be defined as a shorthand for assessing a change, and emphases on its preparation, operation,
reflexion of results and acting on the evidence that has been obtained (Donnelly & Kirk,
2015). The foundation for application of the PDSA model is demonstrated by the systems
theory that places an attention on the type of the complex organisations (Rice, 2013). The
theory embraces the opinion that alterations made in one segment of the organisation have the
competence of disturbing the other portions, with foreseeable behavioural configurations (Al-
Haddad & Kotnour, 2015). Hence, while articulating an effective organisation strategy for
psychoeducation based treatment adoption in the psychiatric unit, the fact that minor
modifications can bring about great variations in the entire administration will considered.
The PDSA method to be used for operative change management will encompass the
following stages:
P- planning the implemented change
D- conducting change
S- studying data before and after the change and reflecting on the information
A- acting on the obtained information and devising future plans
However, one major drawback of the selected change management model is that it needs
extra time from the concerned staff and administrative personnel for working through the
& Pollard, 2013). This can be accredited to the fact the model creates the provision for its
leaders to evaluate and explore the change on a small care, with the intent of determining the
effectiveness, prior to its complete implementation on a wider scale. The model also allows
the leaders to recognise the worth and lucrativeness of the change, upon its application in
real-time settings, on a wider scale. Furthermore, the fact that the PDSA approach facilitates
the implementing leaders to identify the potential barriers and challenges that are not
ostensible prior to the application of the proposed tactic creates the provision for bringing
about much needed modifications and amendments before the actual change. The model can
be defined as a shorthand for assessing a change, and emphases on its preparation, operation,
reflexion of results and acting on the evidence that has been obtained (Donnelly & Kirk,
2015). The foundation for application of the PDSA model is demonstrated by the systems
theory that places an attention on the type of the complex organisations (Rice, 2013). The
theory embraces the opinion that alterations made in one segment of the organisation have the
competence of disturbing the other portions, with foreseeable behavioural configurations (Al-
Haddad & Kotnour, 2015). Hence, while articulating an effective organisation strategy for
psychoeducation based treatment adoption in the psychiatric unit, the fact that minor
modifications can bring about great variations in the entire administration will considered.
The PDSA method to be used for operative change management will encompass the
following stages:
P- planning the implemented change
D- conducting change
S- studying data before and after the change and reflecting on the information
A- acting on the obtained information and devising future plans
However, one major drawback of the selected change management model is that it needs
extra time from the concerned staff and administrative personnel for working through the
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
16BSC MENTAL HEALTH NURSING
aforementioned four stages of the model. This often leads to difficulties in the
implementation of the proposed change in a stressful and complex work environment.
Although the PDSA model is habitually used in the context of healthcare and is permitted all
healthcare institutes as well, its implementation does not appear quite easy. In theory, it is
advised not to use the PDSA Cycle for once, because it is imagined to be a unceasing
improvement device. Upon completion of one PDSA Cycle, another one begins, using the
information learned from the preceding cycle as a preliminary point. Nonetheless, most
healthcare facilities would execute a single cycle and not repeat it. They might even fail to
utilise data from previous cycles, prior to beginning the second one. Failure to achieve the
four steps in precise order is another challenge that might be encountered in healthcare
scenario.
5.0.1 Project initiation
The mental and physical health of the persons suffering from the recognised mental
illness must be perceived that would enable the early acknowledgement of co-morbid
conditions and the obligation for realizing major lifestyle variations or introducing rapid
action. Project initiation would start with the implementation of a care plan that would be
executed by three persons working in the psychiatric ward (Gareis, 2013). The plan would
primarily encompass screening the patients for the severity of comorbid and bipolar disorder
symptoms with the use of standardised questionnaires, and determining their knowledge on
the disorder. This would be achieved by recruiting experienced mental health nursing
professionals and members of the hospital administration. While the former will be directly
involved in subjecting the patients suffering from bipolar disorder to the psychoeducation
sessions, the latter will have the role of explaining potential benefits of the proposed change
to the key stakeholders.
aforementioned four stages of the model. This often leads to difficulties in the
implementation of the proposed change in a stressful and complex work environment.
Although the PDSA model is habitually used in the context of healthcare and is permitted all
healthcare institutes as well, its implementation does not appear quite easy. In theory, it is
advised not to use the PDSA Cycle for once, because it is imagined to be a unceasing
improvement device. Upon completion of one PDSA Cycle, another one begins, using the
information learned from the preceding cycle as a preliminary point. Nonetheless, most
healthcare facilities would execute a single cycle and not repeat it. They might even fail to
utilise data from previous cycles, prior to beginning the second one. Failure to achieve the
four steps in precise order is another challenge that might be encountered in healthcare
scenario.
5.0.1 Project initiation
The mental and physical health of the persons suffering from the recognised mental
illness must be perceived that would enable the early acknowledgement of co-morbid
conditions and the obligation for realizing major lifestyle variations or introducing rapid
action. Project initiation would start with the implementation of a care plan that would be
executed by three persons working in the psychiatric ward (Gareis, 2013). The plan would
primarily encompass screening the patients for the severity of comorbid and bipolar disorder
symptoms with the use of standardised questionnaires, and determining their knowledge on
the disorder. This would be achieved by recruiting experienced mental health nursing
professionals and members of the hospital administration. While the former will be directly
involved in subjecting the patients suffering from bipolar disorder to the psychoeducation
sessions, the latter will have the role of explaining potential benefits of the proposed change
to the key stakeholders.
17BSC MENTAL HEALTH NURSING
The nursing staff would examine the patients in the psychiatric ward by monitoring
their current stages of physical and mental health through several examinations. The nursing
staff would be authorised with the duty of growing a consciousness of the intervention
(psychoeducation) that needs to be implemented. There would be some mandatory
contraindications such as acute suicidal ideations, hearing of imperative sounds, massive
though disorders, and manic heightened mood.
i. Plan- The first stage would encompass a plan that will help in introducing
psychoeducation sessions in the psychiatric ward, with an emphasis on bipolar
disorder patients. All the nursing professionals (fresh graduates and experienced
registered nurses) will be introduced to the plan of action. Prior to the application
of the intervention, the psychiatric ward manager will be requested to sanction the
proposed transformation. There is mounting evidence for the fact that change
leadership focuses on the capability of an individual (the leader) to encourage and
excite others via vision, personal advocacy, and increased access to essential
resources (Kouzes, 2014). These help in the formulation of a platform that
facilitates the change process. Internal communications also play a vital role in the
change processes. Thus, the ward manager must demonstrate best communication
skills by being specific, clear and direct, while allowing the concerned nurse gain
a thorough understanding of the need for implementing psychoeducation as a part
of treatment program. Cooperation and teamwork have been found imperative in
healthcare settings, with the aim of resolving all kinds of conflicts (Shrader, Kern,
Zoller & Blue, 2013). Thus, following organisation of meetings and seminars that
help others to understand the advantages of the proposed intervention, regular
feedback will be taken from the receivers in the form of surveys and
questionnaires to determine their opinion on the projected change. Further efforts
The nursing staff would examine the patients in the psychiatric ward by monitoring
their current stages of physical and mental health through several examinations. The nursing
staff would be authorised with the duty of growing a consciousness of the intervention
(psychoeducation) that needs to be implemented. There would be some mandatory
contraindications such as acute suicidal ideations, hearing of imperative sounds, massive
though disorders, and manic heightened mood.
i. Plan- The first stage would encompass a plan that will help in introducing
psychoeducation sessions in the psychiatric ward, with an emphasis on bipolar
disorder patients. All the nursing professionals (fresh graduates and experienced
registered nurses) will be introduced to the plan of action. Prior to the application
of the intervention, the psychiatric ward manager will be requested to sanction the
proposed transformation. There is mounting evidence for the fact that change
leadership focuses on the capability of an individual (the leader) to encourage and
excite others via vision, personal advocacy, and increased access to essential
resources (Kouzes, 2014). These help in the formulation of a platform that
facilitates the change process. Internal communications also play a vital role in the
change processes. Thus, the ward manager must demonstrate best communication
skills by being specific, clear and direct, while allowing the concerned nurse gain
a thorough understanding of the need for implementing psychoeducation as a part
of treatment program. Cooperation and teamwork have been found imperative in
healthcare settings, with the aim of resolving all kinds of conflicts (Shrader, Kern,
Zoller & Blue, 2013). Thus, following organisation of meetings and seminars that
help others to understand the advantages of the proposed intervention, regular
feedback will be taken from the receivers in the form of surveys and
questionnaires to determine their opinion on the projected change. Further efforts
18BSC MENTAL HEALTH NURSING
must also be taken by the ward manager to educate the fresh graduate nurses on
the potential advantages that the service users (bipolar disorder patients) might
gain upon adherence to the psychoeducation sessions, in relation to their mental
state, health and overall wellbeing.
ii. Do- The stage will encompass the nursing staff working across the psychiatric
wards who will help in successful implementation of the psychoeducation
program by attending different workshops and training sessions. These programs
will be responsible for educating the concerned staff and advocating for the rights
of the patients (Ailey, Lamb, Friese & Christopher, 2015). The selected nurses
will assign the bipolar disorder patients admitted to the psychiatric wards into
different groups where they will receive two weekly sessions of psychoeducation,
each lasting for 60 minutes. The sessions will be conducted over a period of four
months. The major topics that will be addressed during such sessions would
comprise of recognition of mental illness, treatment modalities, and coping skills
(Lyman et al., 2014). The sessions will culminate with the formulation of a
personal care plan that will be put to practice, upon observing relapse of any
manic or depressive symptoms of the illness. In addition to the nurses, a
psychotherapist will also supervise the sessions.
iii. Study- An analysis of the functioning will be done by collecting responses to
specific questionnaires that will determine the success of the nursing professionals
in adapting to the change process. Discussions will also be held by the ward
manager with each group member to gain a sound understanding of the feelings
and experiences of the patients, subjected to the sessions. Conducting clinical
audits will also help in supervising the implemented change and identifying
regions of improvement (Taylor et al., 2013).
must also be taken by the ward manager to educate the fresh graduate nurses on
the potential advantages that the service users (bipolar disorder patients) might
gain upon adherence to the psychoeducation sessions, in relation to their mental
state, health and overall wellbeing.
ii. Do- The stage will encompass the nursing staff working across the psychiatric
wards who will help in successful implementation of the psychoeducation
program by attending different workshops and training sessions. These programs
will be responsible for educating the concerned staff and advocating for the rights
of the patients (Ailey, Lamb, Friese & Christopher, 2015). The selected nurses
will assign the bipolar disorder patients admitted to the psychiatric wards into
different groups where they will receive two weekly sessions of psychoeducation,
each lasting for 60 minutes. The sessions will be conducted over a period of four
months. The major topics that will be addressed during such sessions would
comprise of recognition of mental illness, treatment modalities, and coping skills
(Lyman et al., 2014). The sessions will culminate with the formulation of a
personal care plan that will be put to practice, upon observing relapse of any
manic or depressive symptoms of the illness. In addition to the nurses, a
psychotherapist will also supervise the sessions.
iii. Study- An analysis of the functioning will be done by collecting responses to
specific questionnaires that will determine the success of the nursing professionals
in adapting to the change process. Discussions will also be held by the ward
manager with each group member to gain a sound understanding of the feelings
and experiences of the patients, subjected to the sessions. Conducting clinical
audits will also help in supervising the implemented change and identifying
regions of improvement (Taylor et al., 2013).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
19BSC MENTAL HEALTH NURSING
iv. Act- Changes in mood burden, depressive episodes, manic episodes, and social
adjustment will be evaluated by dissemination of standardised questionnaires. All
the nurses and the psychotherapist will be reminded to regularly record patient
observations and shall be trained about the significance of finishing the
intervention.
My character in this change management occasion will be that of an associate of the
project team. I would acts as the project manager and would be responsible for justifying the
funding and cost of the proposed plan. A comparison shall be made between the costs of
usual care and psychoeducation by formulating cost-effectiveness acceptability curves that
will help me to demonstrate the cost differences between the conventional treatment methods
and the change process. Recording the reduction in relapses would also help in the process. I
would take all conceivable labour to guarantee that the project obtains sufficient capitals,
while handling the dealings with the key shareholders and the funder. I would look for funds
for the change management by applying for a district mental health grant to the government. I
would embrace a visionary headship style and would try to look outside the trials and
ambiguity of the current scenario.
Although I would support the team members to regulate their best potential and realise
the ideas, implementation of a paternalistic leadership will be crucial in the scenario (M.
Taylor, Cornelius & Colvin, 2014). I would adopt a managerial approach that will make me
act as a dominant authority. I would use my organisational power for supporting the team
members in the change management process. The major benefit of this leadership style can
be attributed to the completion of tasks within stipulated time, thus exceeding the goals
(Aycan, 2015). I will develop the action plan and accomplish its deliverables, enlist qualified
nursing staff for the change process, manage the team, and take regular updates on the
success of the program. The unit cost of psychoeducation are an estimated £119 per session
iv. Act- Changes in mood burden, depressive episodes, manic episodes, and social
adjustment will be evaluated by dissemination of standardised questionnaires. All
the nurses and the psychotherapist will be reminded to regularly record patient
observations and shall be trained about the significance of finishing the
intervention.
My character in this change management occasion will be that of an associate of the
project team. I would acts as the project manager and would be responsible for justifying the
funding and cost of the proposed plan. A comparison shall be made between the costs of
usual care and psychoeducation by formulating cost-effectiveness acceptability curves that
will help me to demonstrate the cost differences between the conventional treatment methods
and the change process. Recording the reduction in relapses would also help in the process. I
would take all conceivable labour to guarantee that the project obtains sufficient capitals,
while handling the dealings with the key shareholders and the funder. I would look for funds
for the change management by applying for a district mental health grant to the government. I
would embrace a visionary headship style and would try to look outside the trials and
ambiguity of the current scenario.
Although I would support the team members to regulate their best potential and realise
the ideas, implementation of a paternalistic leadership will be crucial in the scenario (M.
Taylor, Cornelius & Colvin, 2014). I would adopt a managerial approach that will make me
act as a dominant authority. I would use my organisational power for supporting the team
members in the change management process. The major benefit of this leadership style can
be attributed to the completion of tasks within stipulated time, thus exceeding the goals
(Aycan, 2015). I will develop the action plan and accomplish its deliverables, enlist qualified
nursing staff for the change process, manage the team, and take regular updates on the
success of the program. The unit cost of psychoeducation are an estimated £119 per session
20BSC MENTAL HEALTH NURSING
that are conducted over a period of one hour. We would try to restrict the costs to £150 for
each session of 90 minutes (McMurran et al., 2011). These costs will be subsidised by the
health department, government, and eminent non-profit organisations that are mindful of the
probable benefits of the plan. Analysis of the articles included in the review propose that
apparent benefits will overshadow the costs and jeopardies (if any).
Subsidy will be assimilated by inspecting whether the zone we are concerned with, is
addressed by the NIH mission. A cautious preparation will initiate by lettering a grant about
the scheme in a way that will excite the fund granting authorities. A budget plan will
accompany the grant proposal, prior to its submission. A baseline valuation will be steered to
classify the definite barriers to the process. Lack of employee involvement and inadequate
communication strategies might make the staff repel changes in the treatment for bipolar
disorder (Doppelt, 2017). Approaches for actual communication can help in plummeting
communication barriers. Additionally, taking all likely efforts not to oversee the inclinations
and approaches of the employees would aid in reducing odds of resentment and clash (Kadu
& Stolee, 2015).
The measurable outcomes will encompass assessing the organisational performance. The
primary question would encompass ‘whether the results obtained were anticipated from the
plan’ (Bourne, Pavlov, Franco-Santos, Lucianetti & Mura, 2013). The primary outcome will
be related to investigating the impacts of the psychoeducation on the relapse of bipolat
disorder symptoms. These will be measured with the use of Longitudinal Interval Follow-up
Evaluation (LIFE) scale, Modified Social Adjustment Scale, Clinician-Administered Rating
Scale for Mania, and 17-item Hamilton Depression Rating Scale (Gunderson et al., 2011).
Some of the secondary parameters that would be measured are namely performance
enhancement, willingness to change, plan adherence, and speed with which the plan was
executed (Lozano, Ceulemans & Seatter, 2015). The change management process will also be
that are conducted over a period of one hour. We would try to restrict the costs to £150 for
each session of 90 minutes (McMurran et al., 2011). These costs will be subsidised by the
health department, government, and eminent non-profit organisations that are mindful of the
probable benefits of the plan. Analysis of the articles included in the review propose that
apparent benefits will overshadow the costs and jeopardies (if any).
Subsidy will be assimilated by inspecting whether the zone we are concerned with, is
addressed by the NIH mission. A cautious preparation will initiate by lettering a grant about
the scheme in a way that will excite the fund granting authorities. A budget plan will
accompany the grant proposal, prior to its submission. A baseline valuation will be steered to
classify the definite barriers to the process. Lack of employee involvement and inadequate
communication strategies might make the staff repel changes in the treatment for bipolar
disorder (Doppelt, 2017). Approaches for actual communication can help in plummeting
communication barriers. Additionally, taking all likely efforts not to oversee the inclinations
and approaches of the employees would aid in reducing odds of resentment and clash (Kadu
& Stolee, 2015).
The measurable outcomes will encompass assessing the organisational performance. The
primary question would encompass ‘whether the results obtained were anticipated from the
plan’ (Bourne, Pavlov, Franco-Santos, Lucianetti & Mura, 2013). The primary outcome will
be related to investigating the impacts of the psychoeducation on the relapse of bipolat
disorder symptoms. These will be measured with the use of Longitudinal Interval Follow-up
Evaluation (LIFE) scale, Modified Social Adjustment Scale, Clinician-Administered Rating
Scale for Mania, and 17-item Hamilton Depression Rating Scale (Gunderson et al., 2011).
Some of the secondary parameters that would be measured are namely performance
enhancement, willingness to change, plan adherence, and speed with which the plan was
executed (Lozano, Ceulemans & Seatter, 2015). The change management process will also be
21BSC MENTAL HEALTH NURSING
evaluated using different procedures such as, presence and training participation figures,
tracking change management, communication effectiveness, profit realisation, timeframe
observance, and plan progress (Kenny & Bourne, 2015).
The future insinuations are related with the fact that the change model will enable
building of new knowledge into the investigational process of directing psychoeducation
among bipolar disorder patients across the psychiatric ward. It will assess if the trial has fixed
the clinical problem. Flexibility of the PDSA model will also permit acceptance of other non-
pharmaceutical mediations for the management of mental illnesses.
6.0 Conclusion
To conclude, the change management method should be realised for enabling the
administration of psychoeducation based intervention among bipolar disorder service users in
a psychiatric unit. Thus, psychoeducation will be implemented with the aim of reducing
severity of mania and depression symptom relapse among bipolar disorder patients, with the
aim of enhancing their health outcomes.
evaluated using different procedures such as, presence and training participation figures,
tracking change management, communication effectiveness, profit realisation, timeframe
observance, and plan progress (Kenny & Bourne, 2015).
The future insinuations are related with the fact that the change model will enable
building of new knowledge into the investigational process of directing psychoeducation
among bipolar disorder patients across the psychiatric ward. It will assess if the trial has fixed
the clinical problem. Flexibility of the PDSA model will also permit acceptance of other non-
pharmaceutical mediations for the management of mental illnesses.
6.0 Conclusion
To conclude, the change management method should be realised for enabling the
administration of psychoeducation based intervention among bipolar disorder service users in
a psychiatric unit. Thus, psychoeducation will be implemented with the aim of reducing
severity of mania and depression symptom relapse among bipolar disorder patients, with the
aim of enhancing their health outcomes.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
22BSC MENTAL HEALTH NURSING
References
Ailey, S., Lamb, K., Friese, T., & Christopher, B. A. (2015). Educating nursing students in
clinical leadership. Nursing Management (2014+), 21(9), 23. Retrieved from
https://search.proquest.com/openview/e61b8bf1ab81702d21e1f7fe3ffb84d4/1?pq-
origsite=gscholar&cbl=2042231
Al-Haddad, S., & Kotnour, T. (2015). Integrating the organizational change literature: a
model for successful change. Journal of Organizational Change Management, 28(2),
234-262. https://doi.org/10.1108/JOCM-11-2013-0215
Amann, B. L., Radua, J., Wunsch, C., König, B., & Simhandl, C. (2017). Psychiatric and
physical comorbidities and their impact on the course of bipolar disorder: A
prospective, naturalistic 4‐year follow‐up study. Bipolar disorders, 19(3), 225-234.
https://doi.org/10.1111/bdi.12495
Aromataris, E., & Riitano, D. (2014). Systematic reviews: constructing a search strategy and
searching for evidence. AJN The American Journal of Nursing, 114(5), 49-56. doi:
10.1097/01.NAJ.0000446779.99522.f6
Ashkenas, R. (2013). Change management needs to change. Harvard Business
Review, 16(April). Retrieved from
http://www.newoaksconsulting.com/assets/docs/Change_Management_Needs_to_Cha
nge_-_HBR.pdf
Aycan, Z. (2015). Paternalistic leadership. Wiley Encyclopedia of Management, 1-2.
https://doi.org/10.1002/9781118785317.weom060156
Bahredar, M. J., Farid, A. A. A., Ghanizadeh, A., & Birashk, B. (2014). The efficacy of
psycho-educational group program on medication adherence and global functioning
References
Ailey, S., Lamb, K., Friese, T., & Christopher, B. A. (2015). Educating nursing students in
clinical leadership. Nursing Management (2014+), 21(9), 23. Retrieved from
https://search.proquest.com/openview/e61b8bf1ab81702d21e1f7fe3ffb84d4/1?pq-
origsite=gscholar&cbl=2042231
Al-Haddad, S., & Kotnour, T. (2015). Integrating the organizational change literature: a
model for successful change. Journal of Organizational Change Management, 28(2),
234-262. https://doi.org/10.1108/JOCM-11-2013-0215
Amann, B. L., Radua, J., Wunsch, C., König, B., & Simhandl, C. (2017). Psychiatric and
physical comorbidities and their impact on the course of bipolar disorder: A
prospective, naturalistic 4‐year follow‐up study. Bipolar disorders, 19(3), 225-234.
https://doi.org/10.1111/bdi.12495
Aromataris, E., & Riitano, D. (2014). Systematic reviews: constructing a search strategy and
searching for evidence. AJN The American Journal of Nursing, 114(5), 49-56. doi:
10.1097/01.NAJ.0000446779.99522.f6
Ashkenas, R. (2013). Change management needs to change. Harvard Business
Review, 16(April). Retrieved from
http://www.newoaksconsulting.com/assets/docs/Change_Management_Needs_to_Cha
nge_-_HBR.pdf
Aycan, Z. (2015). Paternalistic leadership. Wiley Encyclopedia of Management, 1-2.
https://doi.org/10.1002/9781118785317.weom060156
Bahredar, M. J., Farid, A. A. A., Ghanizadeh, A., & Birashk, B. (2014). The efficacy of
psycho-educational group program on medication adherence and global functioning
23BSC MENTAL HEALTH NURSING
of patients with bipolar disorder type I. International journal of community based
nursing and midwifery, 2(1), 12. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4201187/pdf/ijcbnm-2-12.pdf
Batista, T. A., Baes, C. V. W., & Juruena, M. F. (2011). Efficacy of psychoeducation in
bipolar patients: systematic review of randomized trials. Psychology &
Neuroscience, 4(3), 409-416. http://dx.doi.org/10.3922/j.psns.2011.3.014
Bäuml, J., Pitschel-Walz, G., Volz, A., Lüscher, S., Rentrop, M., Kissling, W., & Jahn, T.
(2016). Psychoeducation improves compliance and outcome in Schizophrenia without
an increase of adverse side effects: a 7-year follow-up of the Munich PIP-
Study. Schizophrenia bulletin, 42(suppl_1), S62-S70.
https://doi.org/10.1093/schbul/sbw008
Bipolar UK. (2018). Bipolar - The Facts. Retrieved from
https://www.bipolaruk.org/faqs/bipolar-the-facts.
Bond, K., & Anderson, I. M. (2015). Psychoeducation for relapse prevention in bipolar
disorder: a systematic review of efficacy in randomized controlled trials. Bipolar
disorders, 17(4), 349-362. https://doi.org/10.1111/bdi.12287
Bourne, C., Aydemir, Ö., Balanzá‐Martínez, V., Bora, E., Brissos, S., Cavanagh, J. T. O., ...
& Ferrier, I. N. (2013). Neuropsychological testing of cognitive impairment in
euthymic bipolar disorder: an individual patient data meta‐analysis. Acta Psychiatrica
Scandinavica, 128(3), 149-162. https://doi.org/10.1111/acps.12133
Bourne, M., Pavlov, A., Franco-Santos, M., Lucianetti, L., & Mura, M. (2013). Generating
organisational performance: The contributing effects of performance measurement
and human resource management practices. International Journal of Operations &
of patients with bipolar disorder type I. International journal of community based
nursing and midwifery, 2(1), 12. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4201187/pdf/ijcbnm-2-12.pdf
Batista, T. A., Baes, C. V. W., & Juruena, M. F. (2011). Efficacy of psychoeducation in
bipolar patients: systematic review of randomized trials. Psychology &
Neuroscience, 4(3), 409-416. http://dx.doi.org/10.3922/j.psns.2011.3.014
Bäuml, J., Pitschel-Walz, G., Volz, A., Lüscher, S., Rentrop, M., Kissling, W., & Jahn, T.
(2016). Psychoeducation improves compliance and outcome in Schizophrenia without
an increase of adverse side effects: a 7-year follow-up of the Munich PIP-
Study. Schizophrenia bulletin, 42(suppl_1), S62-S70.
https://doi.org/10.1093/schbul/sbw008
Bipolar UK. (2018). Bipolar - The Facts. Retrieved from
https://www.bipolaruk.org/faqs/bipolar-the-facts.
Bond, K., & Anderson, I. M. (2015). Psychoeducation for relapse prevention in bipolar
disorder: a systematic review of efficacy in randomized controlled trials. Bipolar
disorders, 17(4), 349-362. https://doi.org/10.1111/bdi.12287
Bourne, C., Aydemir, Ö., Balanzá‐Martínez, V., Bora, E., Brissos, S., Cavanagh, J. T. O., ...
& Ferrier, I. N. (2013). Neuropsychological testing of cognitive impairment in
euthymic bipolar disorder: an individual patient data meta‐analysis. Acta Psychiatrica
Scandinavica, 128(3), 149-162. https://doi.org/10.1111/acps.12133
Bourne, M., Pavlov, A., Franco-Santos, M., Lucianetti, L., & Mura, M. (2013). Generating
organisational performance: The contributing effects of performance measurement
and human resource management practices. International Journal of Operations &
24BSC MENTAL HEALTH NURSING
Production Management, 33(11/12), 1599-1622. https://doi.org/10.1108/IJOPM-07-
2010-0200
Burke, W. W. (2017). Organization change: Theory and practice. Sage Publications.
Retrieved from http://www.dias.ac.in/download/2015/DIAS%20Technology
%20Review%20(14th%20Edition%20of%20DTR).pdf#page=74
Cakir, S., Bensusan, R., Akca, Z. K., & Yazici, O. (2009). Does a psychoeducational
approach reach targeted patients with bipolar disorder?. Journal of affective
disorders, 119(1-3), 190-193. https://doi.org/10.1016/j.jad.2009.08.016
Chan, S. W. C., Yip, B., Tso, S., Cheng, B. S., & Tam, W. (2009). Evaluation of a
psychoeducation program for Chinese clients with schizophrenia and their family
caregivers. Patient education and counseling, 75(1), 67-76.
https://doi.org/10.1016/j.pec.2008.08.028
Chen, R., Xi, Y., Wang, X., Li, Y., He, Y., & Luo, J. (2018). Perception of inpatients
following remission of a manic episode in bipolar I disorder on a group-based
Psychoeducation program: a qualitative study. BMC psychiatry, 18(1), 26.
https://doi.org/10.1186/s12888-018-1614-1
Chen, R., Zhu, X., Capitão, L. P., Zhang, H., Luo, J., Wang, X., ... & Malhi, G. S. (2018).
Psychoeducation for psychiatric inpatients following remission of a manic episode in
bipolar I disorder: A randomized controlled trial. Bipolar disorders.
https://doi.org/10.1111/bdi.12642
Colom, F. (2011). Keeping therapies simple: psychoeducation in the prevention of relapse in
affective disorders. The British Journal of Psychiatry, 198(5), 338-340.
https://doi.org/10.1192/bjp.bp.110.090209
Production Management, 33(11/12), 1599-1622. https://doi.org/10.1108/IJOPM-07-
2010-0200
Burke, W. W. (2017). Organization change: Theory and practice. Sage Publications.
Retrieved from http://www.dias.ac.in/download/2015/DIAS%20Technology
%20Review%20(14th%20Edition%20of%20DTR).pdf#page=74
Cakir, S., Bensusan, R., Akca, Z. K., & Yazici, O. (2009). Does a psychoeducational
approach reach targeted patients with bipolar disorder?. Journal of affective
disorders, 119(1-3), 190-193. https://doi.org/10.1016/j.jad.2009.08.016
Chan, S. W. C., Yip, B., Tso, S., Cheng, B. S., & Tam, W. (2009). Evaluation of a
psychoeducation program for Chinese clients with schizophrenia and their family
caregivers. Patient education and counseling, 75(1), 67-76.
https://doi.org/10.1016/j.pec.2008.08.028
Chen, R., Xi, Y., Wang, X., Li, Y., He, Y., & Luo, J. (2018). Perception of inpatients
following remission of a manic episode in bipolar I disorder on a group-based
Psychoeducation program: a qualitative study. BMC psychiatry, 18(1), 26.
https://doi.org/10.1186/s12888-018-1614-1
Chen, R., Zhu, X., Capitão, L. P., Zhang, H., Luo, J., Wang, X., ... & Malhi, G. S. (2018).
Psychoeducation for psychiatric inpatients following remission of a manic episode in
bipolar I disorder: A randomized controlled trial. Bipolar disorders.
https://doi.org/10.1111/bdi.12642
Colom, F. (2011). Keeping therapies simple: psychoeducation in the prevention of relapse in
affective disorders. The British Journal of Psychiatry, 198(5), 338-340.
https://doi.org/10.1192/bjp.bp.110.090209
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
25BSC MENTAL HEALTH NURSING
Colom, F., Reinares, M., Pacchiarotti, I., Popovic, D., Mazzarini, L., Martínez-Arán, A., ... &
Bonnin, C. M. (2010). Has number of previous episodes any effect on response to
group psychoeducation in bipolar patients? A 5-year follow-up post hoc
analysis. Acta Neuropsychiatrica, 22(2), 50-53. https://doi.org/10.1111/j.1601-
5215.2010.00450.x
Colom, F., Vieta, E., Sanchez-Moreno, J., Palomino-Otiniano, R., Reinares, M., Goikolea, J.
M., ... & Martinez-Aran, A. (2009). Group psychoeducation for stabilised bipolar
disorders: 5-year outcome of a randomised clinical trial. The British Journal of
Psychiatry, 194(3), 260-265. https://doi.org/10.1192/bjp.bp.107.040485
de Azevedo Cardoso, T., de Azambuja Farias, C., Mondin, T. C., Da Silva, G. D. G., de
Mattos Souza, L. D., da Silva, R. A., ... & Jansen, K. (2014). Brief psychoeducation
for bipolar disorder: impact on quality of life in young adults in a 6-month follow-up
of a randomized controlled trial. Psychiatry research, 220(3), 896-902.
https://doi.org/10.1016/j.psychres.2014.09.013
Donnelly, P., & Kirk, P. (2015). Use the PDSA model for effective change
management. Education for Primary Care, 26(4), 279-281.
https://doi.org/10.1080/14739879.2015.11494356
Doppelt, B. (2017). Leading change toward sustainability: A change-management guide for
business, government and civil society. Routledge. Retrieved from
https://www.taylorfrancis.com/books/9781351278959
D'Souza, R., Piskulic, D., & Sundram, S. (2010). A brief dyadic group based
psychoeducation program improves relapse rates in recently remitted bipolar disorder:
a pilot randomised controlled trial. Journal of Affective Disorders, 120(1-3), 272-276.
https://doi.org/10.1016/j.jad.2009.03.018
Colom, F., Reinares, M., Pacchiarotti, I., Popovic, D., Mazzarini, L., Martínez-Arán, A., ... &
Bonnin, C. M. (2010). Has number of previous episodes any effect on response to
group psychoeducation in bipolar patients? A 5-year follow-up post hoc
analysis. Acta Neuropsychiatrica, 22(2), 50-53. https://doi.org/10.1111/j.1601-
5215.2010.00450.x
Colom, F., Vieta, E., Sanchez-Moreno, J., Palomino-Otiniano, R., Reinares, M., Goikolea, J.
M., ... & Martinez-Aran, A. (2009). Group psychoeducation for stabilised bipolar
disorders: 5-year outcome of a randomised clinical trial. The British Journal of
Psychiatry, 194(3), 260-265. https://doi.org/10.1192/bjp.bp.107.040485
de Azevedo Cardoso, T., de Azambuja Farias, C., Mondin, T. C., Da Silva, G. D. G., de
Mattos Souza, L. D., da Silva, R. A., ... & Jansen, K. (2014). Brief psychoeducation
for bipolar disorder: impact on quality of life in young adults in a 6-month follow-up
of a randomized controlled trial. Psychiatry research, 220(3), 896-902.
https://doi.org/10.1016/j.psychres.2014.09.013
Donnelly, P., & Kirk, P. (2015). Use the PDSA model for effective change
management. Education for Primary Care, 26(4), 279-281.
https://doi.org/10.1080/14739879.2015.11494356
Doppelt, B. (2017). Leading change toward sustainability: A change-management guide for
business, government and civil society. Routledge. Retrieved from
https://www.taylorfrancis.com/books/9781351278959
D'Souza, R., Piskulic, D., & Sundram, S. (2010). A brief dyadic group based
psychoeducation program improves relapse rates in recently remitted bipolar disorder:
a pilot randomised controlled trial. Journal of Affective Disorders, 120(1-3), 272-276.
https://doi.org/10.1016/j.jad.2009.03.018
26BSC MENTAL HEALTH NURSING
Eker, F., & Harkın, S. (2012). Effectiveness of six-week psychoeducation program on
adherence of patients with bipolar affective disorder. Journal of affective
disorders, 138(3), 409-416. https://doi.org/10.1016/j.jad.2012.01.004
Faurholt-Jepsen, M., Frost, M., Vinberg, M., Christensen, E. M., Bardram, J. E., & Kessing,
L. V. (2014). Smartphone data as objective measures of bipolar disorder
symptoms. Psychiatry research, 217(1-2), 124-127.
https://doi.org/10.1016/j.psychres.2014.03.009
Gareis, R. (2013). Re-thinking project initiation and project management by considering
principles of sustainable development. In Sustainability Integration for Effective
Project Management (pp. 129-143). IGI Global. Retrieved from https://www.igi-
global.com/chapter/thinking-project-initiation-project-management/76817
George, L. S., Sharma, P. S. V. N., & Nair, S. (2013). Effect of Psycho-Educative
Intervention on Adherence to Treatment, Knowledge and Attitude among Persons
with Bipolar Affective Disorder (BPAD)–Randomized Controlled Trial. J. Nurs.
Health Sci, 1(5), 12-17. Retrieved from
https://www.researchgate.net/publication/271256473
Gumus, F. (2017). The Effectiveness of Individual Psychoeducation on Functioning and
Quality of Life with Bipolar Disorder in Turkey: A Randomized Controlled
Study. International Journal of Caring Sciences, 10(1), 490. Retrieved from
http://www.internationaljournalofcaringsciences.org/docs/53_gumuz_original_10_1.p
df
Gumus, F., Buzlu, S., & Cakir, S. (2015). Effectiveness of individual psychoeducation on
recurrence in bipolar disorder; a controlled study. Archives of psychiatric
nursing, 29(3), 174-179. https://doi.org/10.1016/j.apnu.2015.01.005
Eker, F., & Harkın, S. (2012). Effectiveness of six-week psychoeducation program on
adherence of patients with bipolar affective disorder. Journal of affective
disorders, 138(3), 409-416. https://doi.org/10.1016/j.jad.2012.01.004
Faurholt-Jepsen, M., Frost, M., Vinberg, M., Christensen, E. M., Bardram, J. E., & Kessing,
L. V. (2014). Smartphone data as objective measures of bipolar disorder
symptoms. Psychiatry research, 217(1-2), 124-127.
https://doi.org/10.1016/j.psychres.2014.03.009
Gareis, R. (2013). Re-thinking project initiation and project management by considering
principles of sustainable development. In Sustainability Integration for Effective
Project Management (pp. 129-143). IGI Global. Retrieved from https://www.igi-
global.com/chapter/thinking-project-initiation-project-management/76817
George, L. S., Sharma, P. S. V. N., & Nair, S. (2013). Effect of Psycho-Educative
Intervention on Adherence to Treatment, Knowledge and Attitude among Persons
with Bipolar Affective Disorder (BPAD)–Randomized Controlled Trial. J. Nurs.
Health Sci, 1(5), 12-17. Retrieved from
https://www.researchgate.net/publication/271256473
Gumus, F. (2017). The Effectiveness of Individual Psychoeducation on Functioning and
Quality of Life with Bipolar Disorder in Turkey: A Randomized Controlled
Study. International Journal of Caring Sciences, 10(1), 490. Retrieved from
http://www.internationaljournalofcaringsciences.org/docs/53_gumuz_original_10_1.p
df
Gumus, F., Buzlu, S., & Cakir, S. (2015). Effectiveness of individual psychoeducation on
recurrence in bipolar disorder; a controlled study. Archives of psychiatric
nursing, 29(3), 174-179. https://doi.org/10.1016/j.apnu.2015.01.005
27BSC MENTAL HEALTH NURSING
Gunderson, J. G., Stout, R. L., McGlashan, T. H., Shea, M. T., Morey, L. C., Grilo, C. M., ...
& Ansell, E. (2011). Ten-year course of borderline personality disorder:
psychopathology and function from the Collaborative Longitudinal Personality
Disorders study. Archives of general psychiatry, 68(8), 827-837.
doi:10.1001/archgenpsychiatry.2011.37
Husain, M. I., Chaudhry, I. B., Rahman, R. R., Hamirani, M. M., Mehmood, N., Haddad, P.
M., ... & Husain, N. (2017). Pilot study of a culturally adapted psychoeducation
(CaPE) intervention for bipolar disorder in Pakistan. International journal of bipolar
disorders, 5(1), 3. https://doi.org/10.1186/s40345-017-0074-8
Isasi, A. G., Echeburua, E., Liminana, J. M., & Gonzalez-Pinto, A. (2014). Psychoeducation
and cognitive-behavioral therapy for patients with refractory bipolar disorder: a 5-year
controlled clinical trial. European psychiatry, 29(3), 134-141.
https://doi.org/10.1016/j.eurpsy.2012.11.002
Javadpour, A., Hedayati, A., Dehbozorgi, G. R., & Azizi, A. (2013). The impact of a simple
individual psycho-education program on quality of life, rate of relapse and medication
adherence in bipolar disorder patients. Asian journal of psychiatry, 6(3), 208-213.
https://doi.org/10.1016/j.ajp.2012.12.005
Kadu, M. K., & Stolee, P. (2015). Facilitators and barriers of implementing the chronic care
model in primary care: a systematic review. BMC family practice, 16(1), 12.
https://doi.org/10.1186/s12875-014-0219-0
Kallestad, H., Wullum, E., Scott, J., Stiles, T. C., & Morken, G. (2016). The long-term
outcomes of an effectiveness trial of group versus individual psychoeducation for
bipolar disorders. Journal of affective disorders, 202, 32-38.
https://doi.org/10.1016/j.jad.2016.05.043
Gunderson, J. G., Stout, R. L., McGlashan, T. H., Shea, M. T., Morey, L. C., Grilo, C. M., ...
& Ansell, E. (2011). Ten-year course of borderline personality disorder:
psychopathology and function from the Collaborative Longitudinal Personality
Disorders study. Archives of general psychiatry, 68(8), 827-837.
doi:10.1001/archgenpsychiatry.2011.37
Husain, M. I., Chaudhry, I. B., Rahman, R. R., Hamirani, M. M., Mehmood, N., Haddad, P.
M., ... & Husain, N. (2017). Pilot study of a culturally adapted psychoeducation
(CaPE) intervention for bipolar disorder in Pakistan. International journal of bipolar
disorders, 5(1), 3. https://doi.org/10.1186/s40345-017-0074-8
Isasi, A. G., Echeburua, E., Liminana, J. M., & Gonzalez-Pinto, A. (2014). Psychoeducation
and cognitive-behavioral therapy for patients with refractory bipolar disorder: a 5-year
controlled clinical trial. European psychiatry, 29(3), 134-141.
https://doi.org/10.1016/j.eurpsy.2012.11.002
Javadpour, A., Hedayati, A., Dehbozorgi, G. R., & Azizi, A. (2013). The impact of a simple
individual psycho-education program on quality of life, rate of relapse and medication
adherence in bipolar disorder patients. Asian journal of psychiatry, 6(3), 208-213.
https://doi.org/10.1016/j.ajp.2012.12.005
Kadu, M. K., & Stolee, P. (2015). Facilitators and barriers of implementing the chronic care
model in primary care: a systematic review. BMC family practice, 16(1), 12.
https://doi.org/10.1186/s12875-014-0219-0
Kallestad, H., Wullum, E., Scott, J., Stiles, T. C., & Morken, G. (2016). The long-term
outcomes of an effectiveness trial of group versus individual psychoeducation for
bipolar disorders. Journal of affective disorders, 202, 32-38.
https://doi.org/10.1016/j.jad.2016.05.043
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
28BSC MENTAL HEALTH NURSING
Kenny, G., & Bourne, M. (2015). Performance measurement. Wiley Encyclopedia of
Management, 1-3. https://doi.org/10.1002/9781118785317.weom120139
Kouzes, J. M. (2014). The Five Practices of Exemplary Leadership-Technology (Vol. 292).
John Wiley & Sons. Retrieved from https://books.google.co.in/books?
hl=en&lr=&id=ETgeAwAAQBAJ&oi=fnd&pg=PA1&dq=leadership+vision+person
al+advocacy&ots=ZC53uTg7iT&sig=QZEWF3bkKUX3hfvi6Mrct-peA0E
Kuipers, B. S., Higgs, M., Kickert, W., Tummers, L., Grandia, J., & Van der Voet, J. (2014).
The management of change in public organizations: A literature review. Public
administration, 92(1), 1-20. https://doi.org/10.1111/padm.12040
Lauder, S., Chester, A., Castle, D., Dodd, S., Gliddon, E., Berk, L., ... & Berk, M. (2015). A
randomized head to head trial of MoodSwings. net. au: an internet based self-help
program for bipolar disorder. Journal of affective disorders, 171, 13-21.
https://doi.org/10.1016/j.jad.2014.08.008
Lefley, H. P. (2009). A psychoeducational support group for serious mental illness. The
Journal for Specialists in Group Work, 34(4), 369-381.
https://doi.org/10.1080/01933920903219094
Lin, E. C. L., Berk, M., & Hsu, P. C. (2017). A nurse-led psychoeducational program
BalancingMySwing improves medication adherence among Taiwanese Han-Chinese
with bipolar II disorder. Neuropsychiatry, 7(4), 302-309. Retrieved from
http://www.jneuropsychiatry.org/peer-review/a-nurseled-psychoeducational-program-
balancingmyswing-improves-medication-adherence-among-taiwanese-hanchinese-
with-bipolar-ii-dis.html
Lobban, F., Taylor, L., Chandler, C., Tyler, E., Kinderman, P., Kolamunnage-Dona, R., ... &
Morriss, R. K. (2010). Enhanced relapse prevention for bipolar disorder by
Kenny, G., & Bourne, M. (2015). Performance measurement. Wiley Encyclopedia of
Management, 1-3. https://doi.org/10.1002/9781118785317.weom120139
Kouzes, J. M. (2014). The Five Practices of Exemplary Leadership-Technology (Vol. 292).
John Wiley & Sons. Retrieved from https://books.google.co.in/books?
hl=en&lr=&id=ETgeAwAAQBAJ&oi=fnd&pg=PA1&dq=leadership+vision+person
al+advocacy&ots=ZC53uTg7iT&sig=QZEWF3bkKUX3hfvi6Mrct-peA0E
Kuipers, B. S., Higgs, M., Kickert, W., Tummers, L., Grandia, J., & Van der Voet, J. (2014).
The management of change in public organizations: A literature review. Public
administration, 92(1), 1-20. https://doi.org/10.1111/padm.12040
Lauder, S., Chester, A., Castle, D., Dodd, S., Gliddon, E., Berk, L., ... & Berk, M. (2015). A
randomized head to head trial of MoodSwings. net. au: an internet based self-help
program for bipolar disorder. Journal of affective disorders, 171, 13-21.
https://doi.org/10.1016/j.jad.2014.08.008
Lefley, H. P. (2009). A psychoeducational support group for serious mental illness. The
Journal for Specialists in Group Work, 34(4), 369-381.
https://doi.org/10.1080/01933920903219094
Lin, E. C. L., Berk, M., & Hsu, P. C. (2017). A nurse-led psychoeducational program
BalancingMySwing improves medication adherence among Taiwanese Han-Chinese
with bipolar II disorder. Neuropsychiatry, 7(4), 302-309. Retrieved from
http://www.jneuropsychiatry.org/peer-review/a-nurseled-psychoeducational-program-
balancingmyswing-improves-medication-adherence-among-taiwanese-hanchinese-
with-bipolar-ii-dis.html
Lobban, F., Taylor, L., Chandler, C., Tyler, E., Kinderman, P., Kolamunnage-Dona, R., ... &
Morriss, R. K. (2010). Enhanced relapse prevention for bipolar disorder by
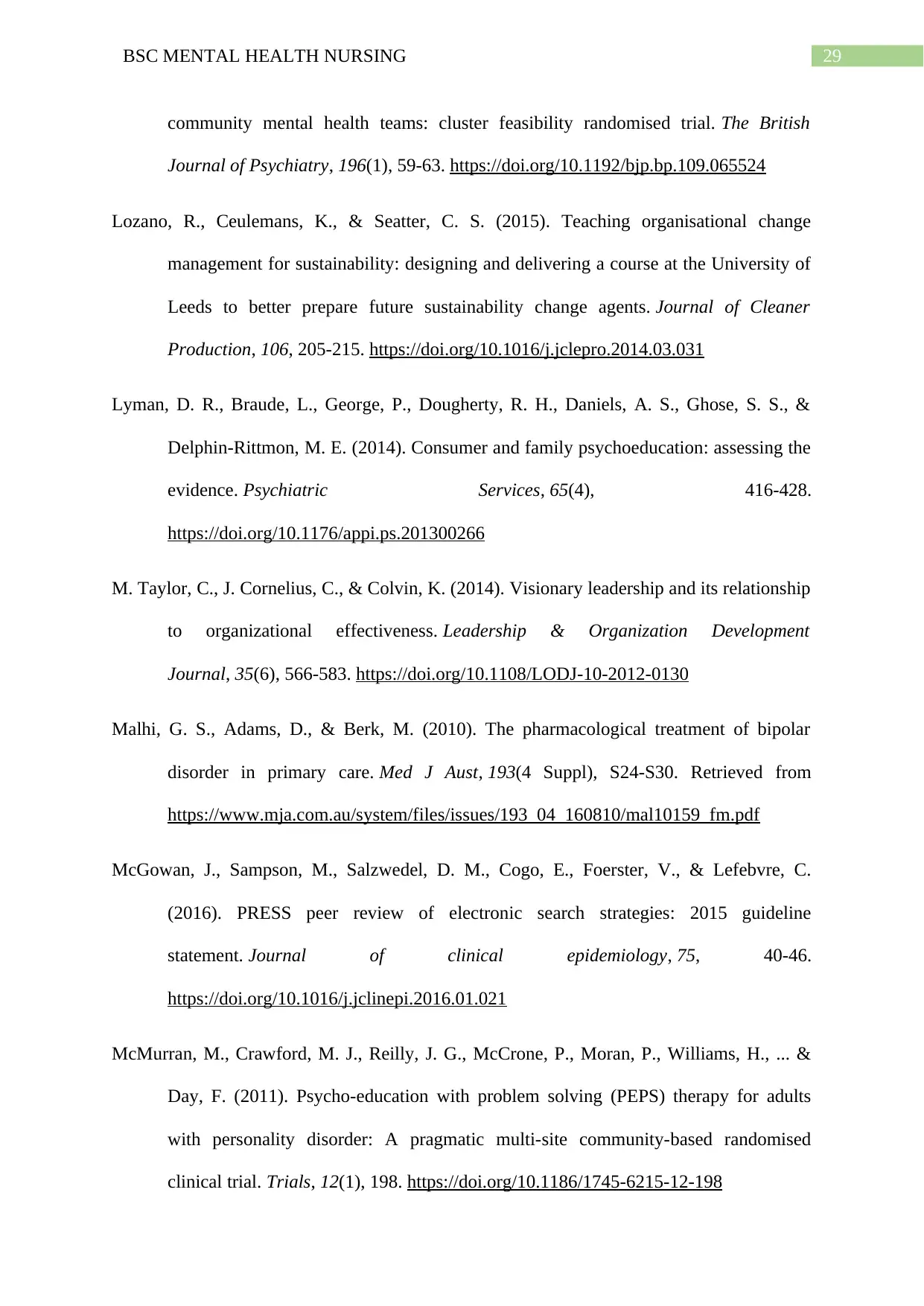
29BSC MENTAL HEALTH NURSING
community mental health teams: cluster feasibility randomised trial. The British
Journal of Psychiatry, 196(1), 59-63. https://doi.org/10.1192/bjp.bp.109.065524
Lozano, R., Ceulemans, K., & Seatter, C. S. (2015). Teaching organisational change
management for sustainability: designing and delivering a course at the University of
Leeds to better prepare future sustainability change agents. Journal of Cleaner
Production, 106, 205-215. https://doi.org/10.1016/j.jclepro.2014.03.031
Lyman, D. R., Braude, L., George, P., Dougherty, R. H., Daniels, A. S., Ghose, S. S., &
Delphin-Rittmon, M. E. (2014). Consumer and family psychoeducation: assessing the
evidence. Psychiatric Services, 65(4), 416-428.
https://doi.org/10.1176/appi.ps.201300266
M. Taylor, C., J. Cornelius, C., & Colvin, K. (2014). Visionary leadership and its relationship
to organizational effectiveness. Leadership & Organization Development
Journal, 35(6), 566-583. https://doi.org/10.1108/LODJ-10-2012-0130
Malhi, G. S., Adams, D., & Berk, M. (2010). The pharmacological treatment of bipolar
disorder in primary care. Med J Aust, 193(4 Suppl), S24-S30. Retrieved from
https://www.mja.com.au/system/files/issues/193_04_160810/mal10159_fm.pdf
McGowan, J., Sampson, M., Salzwedel, D. M., Cogo, E., Foerster, V., & Lefebvre, C.
(2016). PRESS peer review of electronic search strategies: 2015 guideline
statement. Journal of clinical epidemiology, 75, 40-46.
https://doi.org/10.1016/j.jclinepi.2016.01.021
McMurran, M., Crawford, M. J., Reilly, J. G., McCrone, P., Moran, P., Williams, H., ... &
Day, F. (2011). Psycho-education with problem solving (PEPS) therapy for adults
with personality disorder: A pragmatic multi-site community-based randomised
clinical trial. Trials, 12(1), 198. https://doi.org/10.1186/1745-6215-12-198
community mental health teams: cluster feasibility randomised trial. The British
Journal of Psychiatry, 196(1), 59-63. https://doi.org/10.1192/bjp.bp.109.065524
Lozano, R., Ceulemans, K., & Seatter, C. S. (2015). Teaching organisational change
management for sustainability: designing and delivering a course at the University of
Leeds to better prepare future sustainability change agents. Journal of Cleaner
Production, 106, 205-215. https://doi.org/10.1016/j.jclepro.2014.03.031
Lyman, D. R., Braude, L., George, P., Dougherty, R. H., Daniels, A. S., Ghose, S. S., &
Delphin-Rittmon, M. E. (2014). Consumer and family psychoeducation: assessing the
evidence. Psychiatric Services, 65(4), 416-428.
https://doi.org/10.1176/appi.ps.201300266
M. Taylor, C., J. Cornelius, C., & Colvin, K. (2014). Visionary leadership and its relationship
to organizational effectiveness. Leadership & Organization Development
Journal, 35(6), 566-583. https://doi.org/10.1108/LODJ-10-2012-0130
Malhi, G. S., Adams, D., & Berk, M. (2010). The pharmacological treatment of bipolar
disorder in primary care. Med J Aust, 193(4 Suppl), S24-S30. Retrieved from
https://www.mja.com.au/system/files/issues/193_04_160810/mal10159_fm.pdf
McGowan, J., Sampson, M., Salzwedel, D. M., Cogo, E., Foerster, V., & Lefebvre, C.
(2016). PRESS peer review of electronic search strategies: 2015 guideline
statement. Journal of clinical epidemiology, 75, 40-46.
https://doi.org/10.1016/j.jclinepi.2016.01.021
McMurran, M., Crawford, M. J., Reilly, J. G., McCrone, P., Moran, P., Williams, H., ... &
Day, F. (2011). Psycho-education with problem solving (PEPS) therapy for adults
with personality disorder: A pragmatic multi-site community-based randomised
clinical trial. Trials, 12(1), 198. https://doi.org/10.1186/1745-6215-12-198
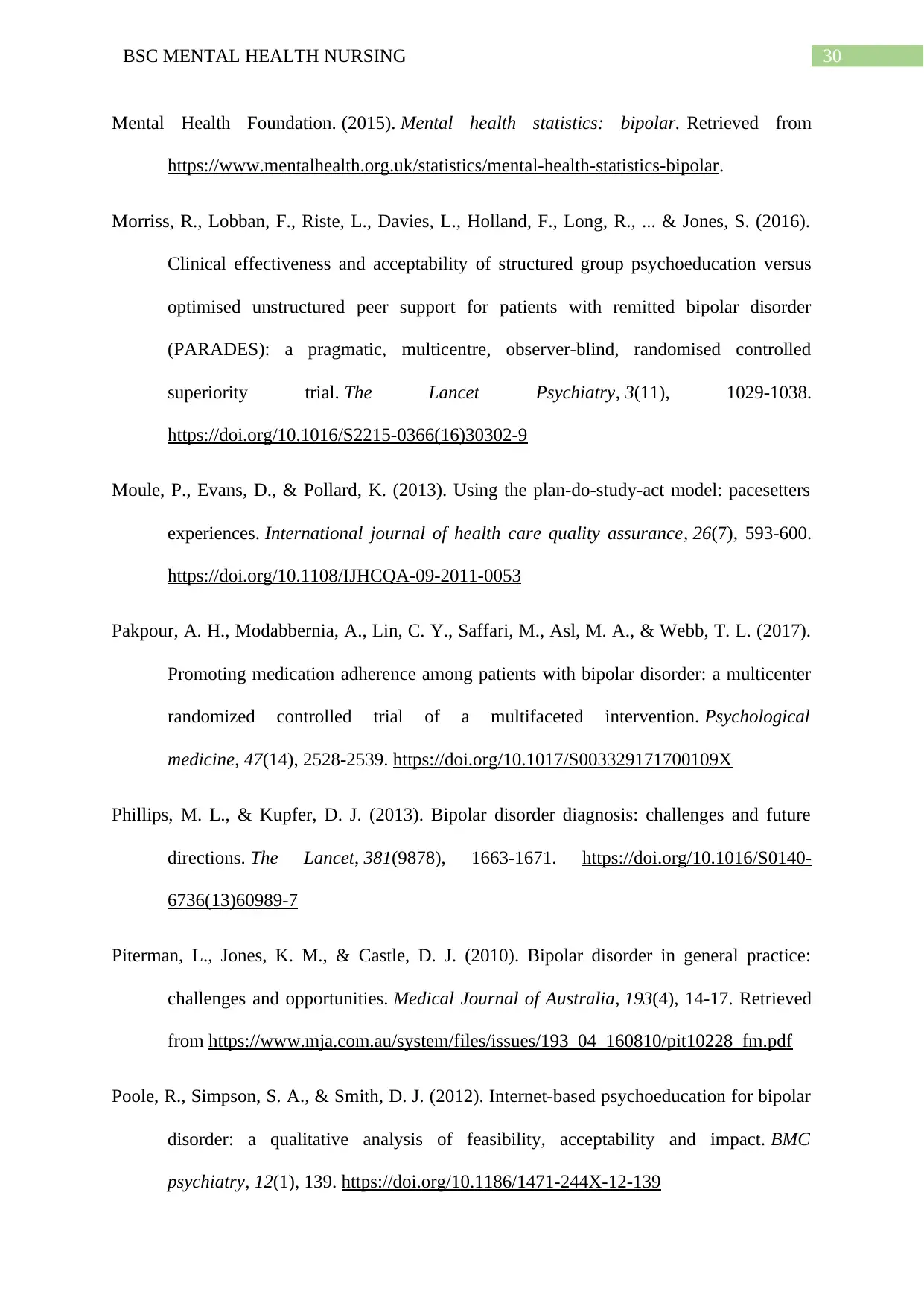
30BSC MENTAL HEALTH NURSING
Mental Health Foundation. (2015). Mental health statistics: bipolar. Retrieved from
https://www.mentalhealth.org.uk/statistics/mental-health-statistics-bipolar.
Morriss, R., Lobban, F., Riste, L., Davies, L., Holland, F., Long, R., ... & Jones, S. (2016).
Clinical effectiveness and acceptability of structured group psychoeducation versus
optimised unstructured peer support for patients with remitted bipolar disorder
(PARADES): a pragmatic, multicentre, observer-blind, randomised controlled
superiority trial. The Lancet Psychiatry, 3(11), 1029-1038.
https://doi.org/10.1016/S2215-0366(16)30302-9
Moule, P., Evans, D., & Pollard, K. (2013). Using the plan-do-study-act model: pacesetters
experiences. International journal of health care quality assurance, 26(7), 593-600.
https://doi.org/10.1108/IJHCQA-09-2011-0053
Pakpour, A. H., Modabbernia, A., Lin, C. Y., Saffari, M., Asl, M. A., & Webb, T. L. (2017).
Promoting medication adherence among patients with bipolar disorder: a multicenter
randomized controlled trial of a multifaceted intervention. Psychological
medicine, 47(14), 2528-2539. https://doi.org/10.1017/S003329171700109X
Phillips, M. L., & Kupfer, D. J. (2013). Bipolar disorder diagnosis: challenges and future
directions. The Lancet, 381(9878), 1663-1671. https://doi.org/10.1016/S0140-
6736(13)60989-7
Piterman, L., Jones, K. M., & Castle, D. J. (2010). Bipolar disorder in general practice:
challenges and opportunities. Medical Journal of Australia, 193(4), 14-17. Retrieved
from https://www.mja.com.au/system/files/issues/193_04_160810/pit10228_fm.pdf
Poole, R., Simpson, S. A., & Smith, D. J. (2012). Internet-based psychoeducation for bipolar
disorder: a qualitative analysis of feasibility, acceptability and impact. BMC
psychiatry, 12(1), 139. https://doi.org/10.1186/1471-244X-12-139
Mental Health Foundation. (2015). Mental health statistics: bipolar. Retrieved from
https://www.mentalhealth.org.uk/statistics/mental-health-statistics-bipolar.
Morriss, R., Lobban, F., Riste, L., Davies, L., Holland, F., Long, R., ... & Jones, S. (2016).
Clinical effectiveness and acceptability of structured group psychoeducation versus
optimised unstructured peer support for patients with remitted bipolar disorder
(PARADES): a pragmatic, multicentre, observer-blind, randomised controlled
superiority trial. The Lancet Psychiatry, 3(11), 1029-1038.
https://doi.org/10.1016/S2215-0366(16)30302-9
Moule, P., Evans, D., & Pollard, K. (2013). Using the plan-do-study-act model: pacesetters
experiences. International journal of health care quality assurance, 26(7), 593-600.
https://doi.org/10.1108/IJHCQA-09-2011-0053
Pakpour, A. H., Modabbernia, A., Lin, C. Y., Saffari, M., Asl, M. A., & Webb, T. L. (2017).
Promoting medication adherence among patients with bipolar disorder: a multicenter
randomized controlled trial of a multifaceted intervention. Psychological
medicine, 47(14), 2528-2539. https://doi.org/10.1017/S003329171700109X
Phillips, M. L., & Kupfer, D. J. (2013). Bipolar disorder diagnosis: challenges and future
directions. The Lancet, 381(9878), 1663-1671. https://doi.org/10.1016/S0140-
6736(13)60989-7
Piterman, L., Jones, K. M., & Castle, D. J. (2010). Bipolar disorder in general practice:
challenges and opportunities. Medical Journal of Australia, 193(4), 14-17. Retrieved
from https://www.mja.com.au/system/files/issues/193_04_160810/pit10228_fm.pdf
Poole, R., Simpson, S. A., & Smith, D. J. (2012). Internet-based psychoeducation for bipolar
disorder: a qualitative analysis of feasibility, acceptability and impact. BMC
psychiatry, 12(1), 139. https://doi.org/10.1186/1471-244X-12-139
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

31BSC MENTAL HEALTH NURSING
Proudfoot, J., Parker, G., Manicavasagar, V., Hadzi-Pavlovic, D., Whitton, A., Nicholas,
J., ... & Burckhardt, R. (2012). Effects of adjunctive peer support on perceptions of
illness control and understanding in an online psychoeducation program for bipolar
disorder: a randomised controlled trial. Journal of affective disorders, 142(1-3), 98-
105. https://doi.org/10.1016/j.jad.2012.04.007
Rahmani, F., Ebrahimi, H., Ranjbar, F., Razavi, S. S., & Asghari, E. (2016). The effect of
group psychoeducation program on medication adherence in patients with bipolar
mood disorders: A randomized controlled trial. Journal of caring sciences, 5(4), 287.
doi: 10.15171/jcs.2016.030
Reinares, M., Colom, F., Sánchez‐Moreno, J., Torrent, C., Martínez‐Arán, A., Comes, M., ...
& Vieta, E. (2008). Impact of caregiver group psychoeducation on the course and
outcome of bipolar patients in remission: a randomized controlled trial. Bipolar
disorders, 10(4), 511-519. https://doi.org/10.1111/j.1399-5618.2008.00588.x
Rice, A. L. (2013). The enterprise and its environment: A system theory of management
organization. Routledge.
Retrieved from https://content.taylorfrancis.com/books/download?dac=C2004-0-
01289-4&isbn=9781136431739&format=googlePreviewPdf
Shrader, S., Kern, D., Zoller, J., & Blue, A. (2013). Interprofessional teamwork skills as
predictors of clinical outcomes in a simulated healthcare setting. Journal of Allied
Health, 42(1), 1E-6E. Retrieved from
http://docserver.ingentaconnect.com/deliver/connect/asahp/00907421/v42n1/s11.pdf?
expires=1538560814&id=0000&titleid=6329&checksum=87EB2BDF9331BBC9738
0195BD4AB9BEF
Proudfoot, J., Parker, G., Manicavasagar, V., Hadzi-Pavlovic, D., Whitton, A., Nicholas,
J., ... & Burckhardt, R. (2012). Effects of adjunctive peer support on perceptions of
illness control and understanding in an online psychoeducation program for bipolar
disorder: a randomised controlled trial. Journal of affective disorders, 142(1-3), 98-
105. https://doi.org/10.1016/j.jad.2012.04.007
Rahmani, F., Ebrahimi, H., Ranjbar, F., Razavi, S. S., & Asghari, E. (2016). The effect of
group psychoeducation program on medication adherence in patients with bipolar
mood disorders: A randomized controlled trial. Journal of caring sciences, 5(4), 287.
doi: 10.15171/jcs.2016.030
Reinares, M., Colom, F., Sánchez‐Moreno, J., Torrent, C., Martínez‐Arán, A., Comes, M., ...
& Vieta, E. (2008). Impact of caregiver group psychoeducation on the course and
outcome of bipolar patients in remission: a randomized controlled trial. Bipolar
disorders, 10(4), 511-519. https://doi.org/10.1111/j.1399-5618.2008.00588.x
Rice, A. L. (2013). The enterprise and its environment: A system theory of management
organization. Routledge.
Retrieved from https://content.taylorfrancis.com/books/download?dac=C2004-0-
01289-4&isbn=9781136431739&format=googlePreviewPdf
Shrader, S., Kern, D., Zoller, J., & Blue, A. (2013). Interprofessional teamwork skills as
predictors of clinical outcomes in a simulated healthcare setting. Journal of Allied
Health, 42(1), 1E-6E. Retrieved from
http://docserver.ingentaconnect.com/deliver/connect/asahp/00907421/v42n1/s11.pdf?
expires=1538560814&id=0000&titleid=6329&checksum=87EB2BDF9331BBC9738
0195BD4AB9BEF
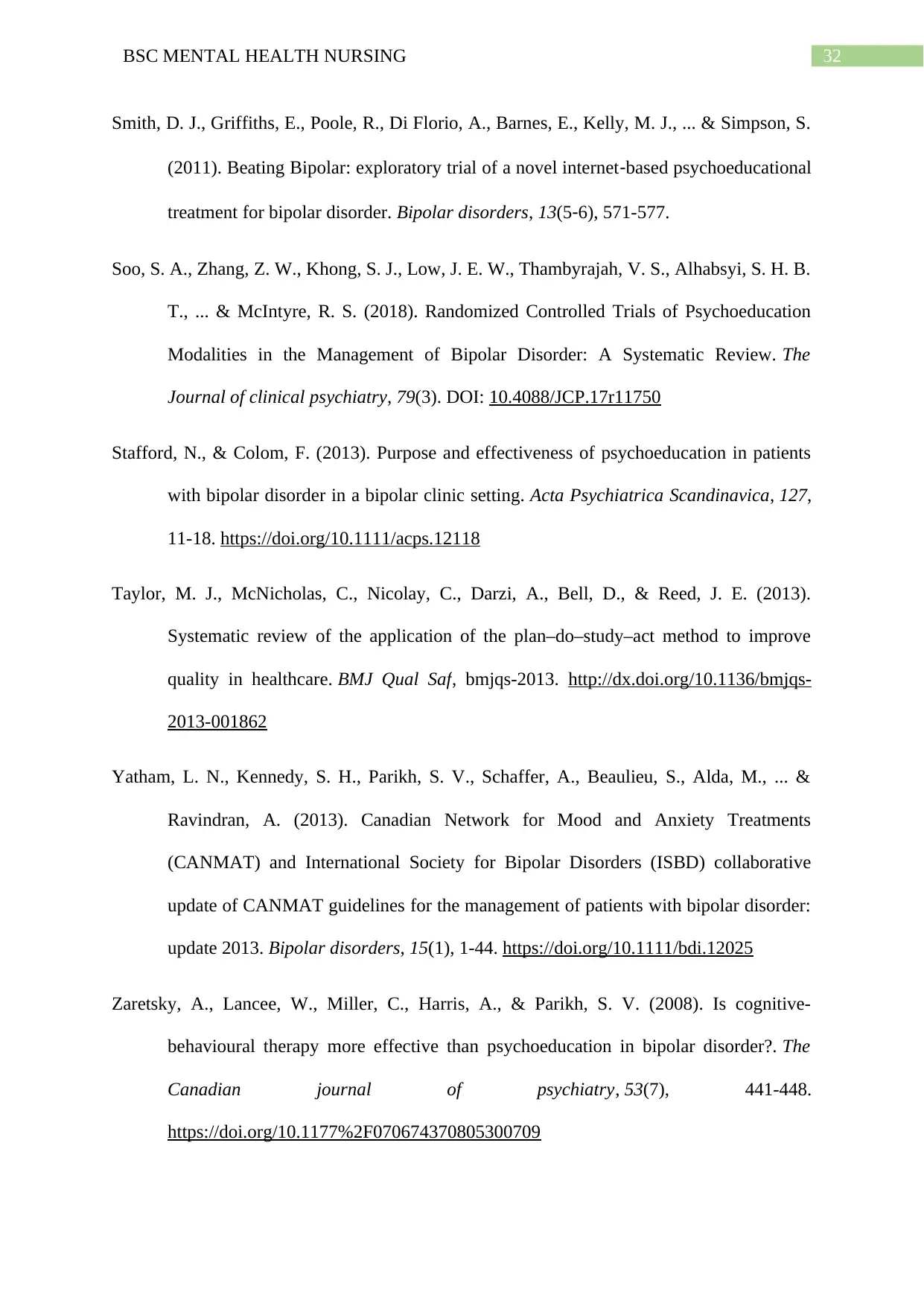
32BSC MENTAL HEALTH NURSING
Smith, D. J., Griffiths, E., Poole, R., Di Florio, A., Barnes, E., Kelly, M. J., ... & Simpson, S.
(2011). Beating Bipolar: exploratory trial of a novel internet‐based psychoeducational
treatment for bipolar disorder. Bipolar disorders, 13(5‐6), 571-577.
Soo, S. A., Zhang, Z. W., Khong, S. J., Low, J. E. W., Thambyrajah, V. S., Alhabsyi, S. H. B.
T., ... & McIntyre, R. S. (2018). Randomized Controlled Trials of Psychoeducation
Modalities in the Management of Bipolar Disorder: A Systematic Review. The
Journal of clinical psychiatry, 79(3). DOI: 10.4088/JCP.17r11750
Stafford, N., & Colom, F. (2013). Purpose and effectiveness of psychoeducation in patients
with bipolar disorder in a bipolar clinic setting. Acta Psychiatrica Scandinavica, 127,
11-18. https://doi.org/10.1111/acps.12118
Taylor, M. J., McNicholas, C., Nicolay, C., Darzi, A., Bell, D., & Reed, J. E. (2013).
Systematic review of the application of the plan–do–study–act method to improve
quality in healthcare. BMJ Qual Saf, bmjqs-2013. http://dx.doi.org/10.1136/bmjqs-
2013-001862
Yatham, L. N., Kennedy, S. H., Parikh, S. V., Schaffer, A., Beaulieu, S., Alda, M., ... &
Ravindran, A. (2013). Canadian Network for Mood and Anxiety Treatments
(CANMAT) and International Society for Bipolar Disorders (ISBD) collaborative
update of CANMAT guidelines for the management of patients with bipolar disorder:
update 2013. Bipolar disorders, 15(1), 1-44. https://doi.org/10.1111/bdi.12025
Zaretsky, A., Lancee, W., Miller, C., Harris, A., & Parikh, S. V. (2008). Is cognitive-
behavioural therapy more effective than psychoeducation in bipolar disorder?. The
Canadian journal of psychiatry, 53(7), 441-448.
https://doi.org/10.1177%2F070674370805300709
Smith, D. J., Griffiths, E., Poole, R., Di Florio, A., Barnes, E., Kelly, M. J., ... & Simpson, S.
(2011). Beating Bipolar: exploratory trial of a novel internet‐based psychoeducational
treatment for bipolar disorder. Bipolar disorders, 13(5‐6), 571-577.
Soo, S. A., Zhang, Z. W., Khong, S. J., Low, J. E. W., Thambyrajah, V. S., Alhabsyi, S. H. B.
T., ... & McIntyre, R. S. (2018). Randomized Controlled Trials of Psychoeducation
Modalities in the Management of Bipolar Disorder: A Systematic Review. The
Journal of clinical psychiatry, 79(3). DOI: 10.4088/JCP.17r11750
Stafford, N., & Colom, F. (2013). Purpose and effectiveness of psychoeducation in patients
with bipolar disorder in a bipolar clinic setting. Acta Psychiatrica Scandinavica, 127,
11-18. https://doi.org/10.1111/acps.12118
Taylor, M. J., McNicholas, C., Nicolay, C., Darzi, A., Bell, D., & Reed, J. E. (2013).
Systematic review of the application of the plan–do–study–act method to improve
quality in healthcare. BMJ Qual Saf, bmjqs-2013. http://dx.doi.org/10.1136/bmjqs-
2013-001862
Yatham, L. N., Kennedy, S. H., Parikh, S. V., Schaffer, A., Beaulieu, S., Alda, M., ... &
Ravindran, A. (2013). Canadian Network for Mood and Anxiety Treatments
(CANMAT) and International Society for Bipolar Disorders (ISBD) collaborative
update of CANMAT guidelines for the management of patients with bipolar disorder:
update 2013. Bipolar disorders, 15(1), 1-44. https://doi.org/10.1111/bdi.12025
Zaretsky, A., Lancee, W., Miller, C., Harris, A., & Parikh, S. V. (2008). Is cognitive-
behavioural therapy more effective than psychoeducation in bipolar disorder?. The
Canadian journal of psychiatry, 53(7), 441-448.
https://doi.org/10.1177%2F070674370805300709

33BSC MENTAL HEALTH NURSING
Zhao, S., Sampson, S., Xia, J., & Jayaram, M. B. (2015). Psychoeducation (brief) for people
with serious mental illness. Cochrane Database of Systematic Reviews, (4). doi:
10.1002/14651858.CD010823.pub2
Zhao, S., Sampson, S., Xia, J., & Jayaram, M. B. (2015). Psychoeducation (brief) for people
with serious mental illness. Cochrane Database of Systematic Reviews, (4). doi:
10.1002/14651858.CD010823.pub2
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
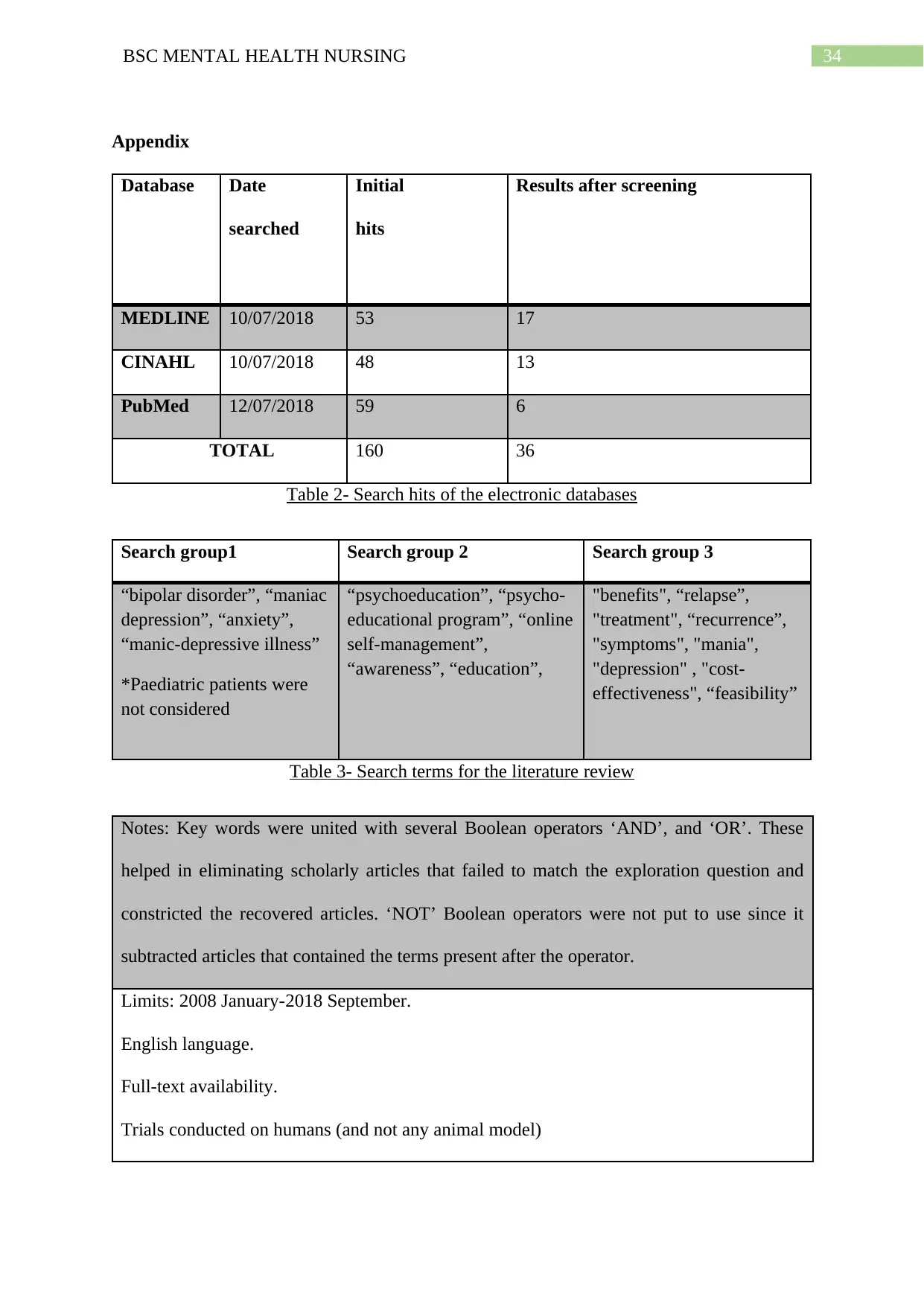
34BSC MENTAL HEALTH NURSING
Appendix
Database Date
searched
Initial
hits
Results after screening
MEDLINE 10/07/2018 53 17
CINAHL 10/07/2018 48 13
PubMed 12/07/2018 59 6
TOTAL 160 36
Table 2- Search hits of the electronic databases
Search group1 Search group 2 Search group 3
“bipolar disorder”, “maniac
depression”, “anxiety”,
“manic-depressive illness”
*Paediatric patients were
not considered
“psychoeducation”, “psycho-
educational program”, “online
self-management”,
“awareness”, “education”,
"benefits", “relapse”,
"treatment", “recurrence”,
"symptoms", "mania",
"depression" , "cost-
effectiveness", “feasibility”
Table 3- Search terms for the literature review
Notes: Key words were united with several Boolean operators ‘AND’, and ‘OR’. These
helped in eliminating scholarly articles that failed to match the exploration question and
constricted the recovered articles. ‘NOT’ Boolean operators were not put to use since it
subtracted articles that contained the terms present after the operator.
Limits: 2008 January-2018 September.
English language.
Full-text availability.
Trials conducted on humans (and not any animal model)
Appendix
Database Date
searched
Initial
hits
Results after screening
MEDLINE 10/07/2018 53 17
CINAHL 10/07/2018 48 13
PubMed 12/07/2018 59 6
TOTAL 160 36
Table 2- Search hits of the electronic databases
Search group1 Search group 2 Search group 3
“bipolar disorder”, “maniac
depression”, “anxiety”,
“manic-depressive illness”
*Paediatric patients were
not considered
“psychoeducation”, “psycho-
educational program”, “online
self-management”,
“awareness”, “education”,
"benefits", “relapse”,
"treatment", “recurrence”,
"symptoms", "mania",
"depression" , "cost-
effectiveness", “feasibility”
Table 3- Search terms for the literature review
Notes: Key words were united with several Boolean operators ‘AND’, and ‘OR’. These
helped in eliminating scholarly articles that failed to match the exploration question and
constricted the recovered articles. ‘NOT’ Boolean operators were not put to use since it
subtracted articles that contained the terms present after the operator.
Limits: 2008 January-2018 September.
English language.
Full-text availability.
Trials conducted on humans (and not any animal model)
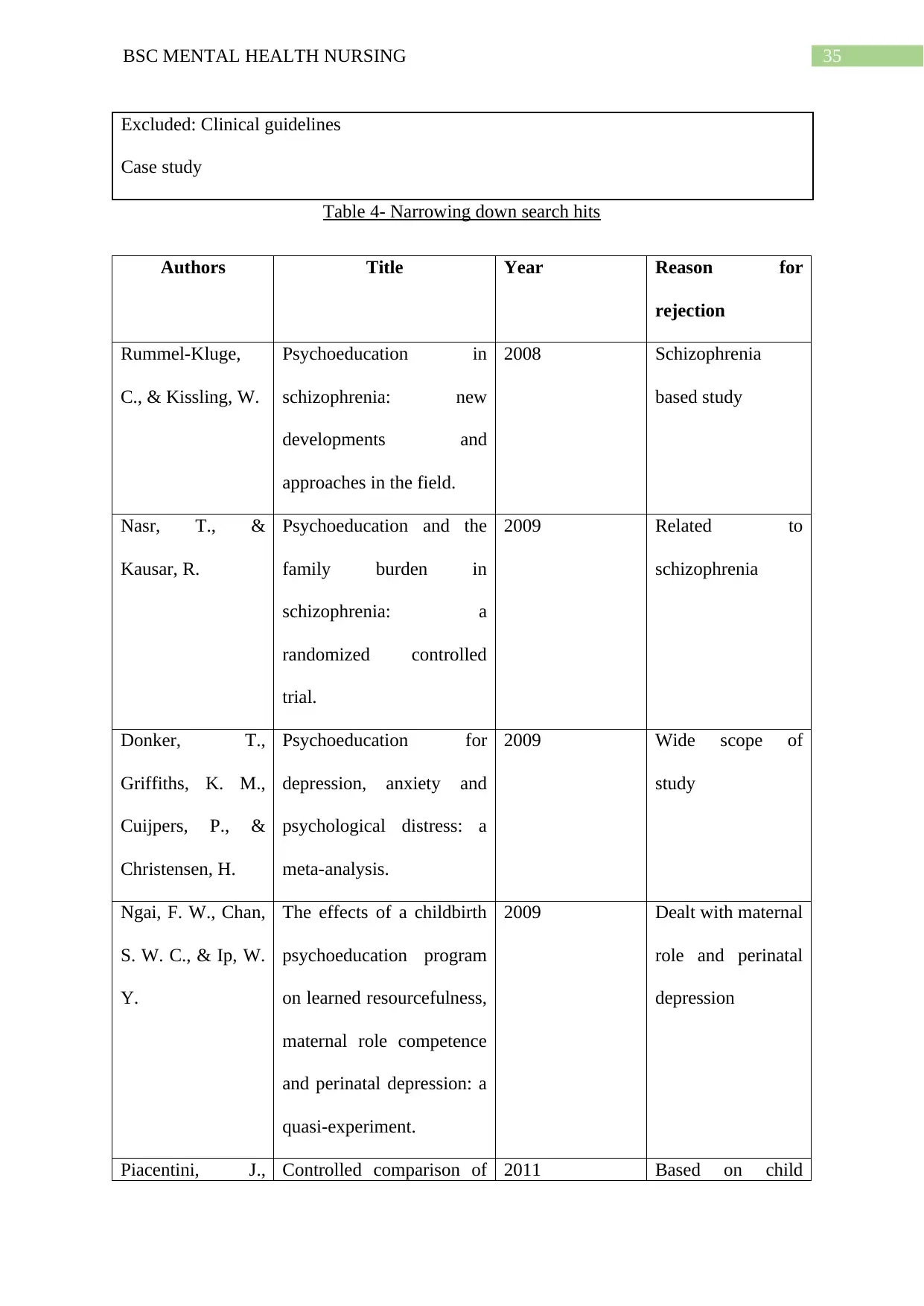
35BSC MENTAL HEALTH NURSING
Excluded: Clinical guidelines
Case study
Table 4- Narrowing down search hits
Authors Title Year Reason for
rejection
Rummel-Kluge,
C., & Kissling, W.
Psychoeducation in
schizophrenia: new
developments and
approaches in the field.
2008 Schizophrenia
based study
Nasr, T., &
Kausar, R.
Psychoeducation and the
family burden in
schizophrenia: a
randomized controlled
trial.
2009 Related to
schizophrenia
Donker, T.,
Griffiths, K. M.,
Cuijpers, P., &
Christensen, H.
Psychoeducation for
depression, anxiety and
psychological distress: a
meta-analysis.
2009 Wide scope of
study
Ngai, F. W., Chan,
S. W. C., & Ip, W.
Y.
The effects of a childbirth
psychoeducation program
on learned resourcefulness,
maternal role competence
and perinatal depression: a
quasi-experiment.
2009 Dealt with maternal
role and perinatal
depression
Piacentini, J., Controlled comparison of 2011 Based on child
Excluded: Clinical guidelines
Case study
Table 4- Narrowing down search hits
Authors Title Year Reason for
rejection
Rummel-Kluge,
C., & Kissling, W.
Psychoeducation in
schizophrenia: new
developments and
approaches in the field.
2008 Schizophrenia
based study
Nasr, T., &
Kausar, R.
Psychoeducation and the
family burden in
schizophrenia: a
randomized controlled
trial.
2009 Related to
schizophrenia
Donker, T.,
Griffiths, K. M.,
Cuijpers, P., &
Christensen, H.
Psychoeducation for
depression, anxiety and
psychological distress: a
meta-analysis.
2009 Wide scope of
study
Ngai, F. W., Chan,
S. W. C., & Ip, W.
Y.
The effects of a childbirth
psychoeducation program
on learned resourcefulness,
maternal role competence
and perinatal depression: a
quasi-experiment.
2009 Dealt with maternal
role and perinatal
depression
Piacentini, J., Controlled comparison of 2011 Based on child
36BSC MENTAL HEALTH NURSING
Bergman, R. L.,
Chang, S.,
Langley, A., Peris,
T., Wood, J. J., &
McCracken, J.
family cognitive
behavioral therapy and
psychoeducation/relaxation
training for child
obsessive-compulsive
disorder.
OCD
Table 5- Some articles that were excluded
Bergman, R. L.,
Chang, S.,
Langley, A., Peris,
T., Wood, J. J., &
McCracken, J.
family cognitive
behavioral therapy and
psychoeducation/relaxation
training for child
obsessive-compulsive
disorder.
OCD
Table 5- Some articles that were excluded
1 out of 37
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





