Psychotherapy Case Study: Social Anxiety Disorder Assessment
VerifiedAdded on 2023/04/21
|31
|11756
|155
Case Study
AI Summary
This case study presents a comprehensive analysis of the psychotherapeutic assessment and management of a 45-year-old female patient, Anna, suffering from social anxiety disorder. The case details Anna's patient demographics, referral history, presenting complaint of 22 years of performance anxiety, past psychiatric and medical history, substance use, and personal and social history. It includes a mental state examination and physical examination, leading to a formulation and diagnosis of social anxiety disorder. The management plan incorporates medication (propranolol and diazepam) and psychotherapy, with a detailed assessment of her suitability for therapy. The study outlines the goals of psychotherapy, supervision, learning objectives, and the therapeutic setting. A summary of psychotherapy sessions (1-40) highlights progress, challenges, and interventions used. The case study concludes with a discussion and conclusion, emphasizing the importance of tailored psychotherapeutic interventions for managing social anxiety disorder. Desklib provides access to this and many other solved assignments for students.
Psychology
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of Contents
Introduction......................................................................................................................................4
Patient Demographics......................................................................................................................4
Referral............................................................................................................................................4
History of Presenting Complaint.....................................................................................................4
Past psychiatric history....................................................................................................................6
Past medical history.........................................................................................................................6
Medications......................................................................................................................................6
Substance use history.......................................................................................................................7
Personal history...............................................................................................................................7
Forensic history...............................................................................................................................8
Occupational history........................................................................................................................8
Social history...................................................................................................................................9
Mental state examination.................................................................................................................9
Physical Examination....................................................................................................................10
Formulation....................................................................................................................................10
Diagnosis.......................................................................................................................................11
Management Plan..........................................................................................................................12
Medication.................................................................................................................................12
Psychotherapy............................................................................................................................12
Assessment of Suitability for Psychotherapy................................................................................14
Health-sickness dimension........................................................................................................14
Psychological dimension...........................................................................................................15
Therapy dimension....................................................................................................................15
Goals of psychotherapy.................................................................................................................15
Introduction......................................................................................................................................4
Patient Demographics......................................................................................................................4
Referral............................................................................................................................................4
History of Presenting Complaint.....................................................................................................4
Past psychiatric history....................................................................................................................6
Past medical history.........................................................................................................................6
Medications......................................................................................................................................6
Substance use history.......................................................................................................................7
Personal history...............................................................................................................................7
Forensic history...............................................................................................................................8
Occupational history........................................................................................................................8
Social history...................................................................................................................................9
Mental state examination.................................................................................................................9
Physical Examination....................................................................................................................10
Formulation....................................................................................................................................10
Diagnosis.......................................................................................................................................11
Management Plan..........................................................................................................................12
Medication.................................................................................................................................12
Psychotherapy............................................................................................................................12
Assessment of Suitability for Psychotherapy................................................................................14
Health-sickness dimension........................................................................................................14
Psychological dimension...........................................................................................................15
Therapy dimension....................................................................................................................15
Goals of psychotherapy.................................................................................................................15
Supervision and learning goals......................................................................................................16
Setting and frame...........................................................................................................................18
Progress: Summary of Psychotherapy Sessions............................................................................18
Session 1-5.................................................................................................................................18
Session 6-10...............................................................................................................................20
Session 11-15.............................................................................................................................21
Session 16-20.............................................................................................................................22
Session 21-25.............................................................................................................................24
Session 26-30.............................................................................................................................25
Session 31-35.............................................................................................................................26
Session 36-40.............................................................................................................................28
Discussion......................................................................................................................................29
Conclusion.....................................................................................................................................30
Reference List................................................................................................................................30
Setting and frame...........................................................................................................................18
Progress: Summary of Psychotherapy Sessions............................................................................18
Session 1-5.................................................................................................................................18
Session 6-10...............................................................................................................................20
Session 11-15.............................................................................................................................21
Session 16-20.............................................................................................................................22
Session 21-25.............................................................................................................................24
Session 26-30.............................................................................................................................25
Session 31-35.............................................................................................................................26
Session 36-40.............................................................................................................................28
Discussion......................................................................................................................................29
Conclusion.....................................................................................................................................30
Reference List................................................................................................................................30
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Introduction
This case details the psychotherapeutic assessment and management of a patient suffering from
social anxiety disorder and psychological vulnerabilities.
Patient Demographics
Anna was a 45 year old* mother of three. She has two daughters* and a son*. She was married
and lived with her husband and children. Anna worked as a full time freelance performer* and
really enjoyed her job. In her house, she was the primary financial provider as her husband took
care of all the household work. She had been suffering from social anxiety symptoms from 22
years. It was primarily due to difficult experiences in her early age and she also had a very
complicated relationship with her mother. It was reported that her mother had suffered from
hypochondriasis. Currently, Anna consumes alcohol more than the levels of safe drinking,
however, has been working to reduce the same. She was ex-smoker. She had never engaged in to
self harming or suicidal behaviors.
Referral
Initially, the general practitioner of Anna referred to an anxiety clinic for the GAD assessment.
The practitioner prescribed her with propranolol 10 mg to be used 30 minutes before any
performance. The general practitioner also prescribed Anna with 2mg of diazepam at her review.
According to the practitioner, no chronic medical conditions were found within Anna, however,
slight rosacea and an insertion of Mirena was found within her.
History of Presenting Complaint
It was described by Anna that she had a history of 22 years of warning and waxing symptoms
related to performance anxiety. This was followed by an embarrassing scenario which took place
during her live performance where she ran out of breath. Running towards the location, caused
Anna to struggle with words and fall short of breath. She was questioned by people if she was
fine which made her fear that people might have come to know about her anxiety issues. As
stated by Anna, severe amount of anticipatory anxiety was developed inside her before live
performances. This often made her scared to be judged negatively due to which signs of anxiety
and embarrassment had developed more inside her. The primary symptoms of anxiety faced by
This case details the psychotherapeutic assessment and management of a patient suffering from
social anxiety disorder and psychological vulnerabilities.
Patient Demographics
Anna was a 45 year old* mother of three. She has two daughters* and a son*. She was married
and lived with her husband and children. Anna worked as a full time freelance performer* and
really enjoyed her job. In her house, she was the primary financial provider as her husband took
care of all the household work. She had been suffering from social anxiety symptoms from 22
years. It was primarily due to difficult experiences in her early age and she also had a very
complicated relationship with her mother. It was reported that her mother had suffered from
hypochondriasis. Currently, Anna consumes alcohol more than the levels of safe drinking,
however, has been working to reduce the same. She was ex-smoker. She had never engaged in to
self harming or suicidal behaviors.
Referral
Initially, the general practitioner of Anna referred to an anxiety clinic for the GAD assessment.
The practitioner prescribed her with propranolol 10 mg to be used 30 minutes before any
performance. The general practitioner also prescribed Anna with 2mg of diazepam at her review.
According to the practitioner, no chronic medical conditions were found within Anna, however,
slight rosacea and an insertion of Mirena was found within her.
History of Presenting Complaint
It was described by Anna that she had a history of 22 years of warning and waxing symptoms
related to performance anxiety. This was followed by an embarrassing scenario which took place
during her live performance where she ran out of breath. Running towards the location, caused
Anna to struggle with words and fall short of breath. She was questioned by people if she was
fine which made her fear that people might have come to know about her anxiety issues. As
stated by Anna, severe amount of anticipatory anxiety was developed inside her before live
performances. This often made her scared to be judged negatively due to which signs of anxiety
and embarrassment had developed more inside her. The primary symptoms of anxiety faced by
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Anna were shortness of breath, a shaky voice and trembling. Before I feared performance, the
anticipatory anxiety of Anna could build for several days. During such times, she claimed of
getting several unhelpful thoughts. It was also recognized by her that she used to compare herself
with her colleagues in a negative manner. The constant fears of Anna were the repetition of the
scenario, and people noticing her anxious stare and making fun of it. Any kind of rumination
after the event was denied by Anna to which she explained that if her performance went well, she
felt good about it and if vice-versa, she tried to forget it. Such fears are a part and parcel of the
mental health issue related to Social Anxiety Disorder.
It was recognized by her that often her anxiety was triggered by some specific performances then
the others. Anna also explained about experiencing panic symptoms which were situation bound
such as a feeling of dizzy, twitchy, bushing and racing heart. Any kind of paraesthesia or
diaphoresis was denied by her. Dissociative symptoms like depersonalization or derealisation
were also denied by her. No associated panic cognitions were found either. Anna explained that
the panic symptoms experienced by her only occurred at times when she was already highly
anxious and not out of the blue.
Situations where Anna was the centre of attention, like a doctor’s appointment or a party, she
reported of having social anxiety which was more generalized.
In the past years, she had been trying to manage herself and fight anxiety in her own ways. She
took precautionary measures such as keeping a water bottle nearby, making small talks, taking
propranolol and so on.
According to her, the symptoms became worse one and half year back. It took place after an
encounter of Anna with her mother. She explained that she did not like her mother and tried to
block all possible contacts with her. She described that since her last meeting with her mother,
the symptoms of anxiety had increased and become very intense and frequent. Although her
mood had been stable, a reduction in memory and concentration was reported by her.
No symptoms of dysthymia or depression were found in her. There were no instances of diurnal
mode variation. She described of having good energy levels, stable weight, healthy appetite, ok
sleep and normal libido. Any kind of perceptual disturbances delusional ideation and thoughts of
anticipatory anxiety of Anna could build for several days. During such times, she claimed of
getting several unhelpful thoughts. It was also recognized by her that she used to compare herself
with her colleagues in a negative manner. The constant fears of Anna were the repetition of the
scenario, and people noticing her anxious stare and making fun of it. Any kind of rumination
after the event was denied by Anna to which she explained that if her performance went well, she
felt good about it and if vice-versa, she tried to forget it. Such fears are a part and parcel of the
mental health issue related to Social Anxiety Disorder.
It was recognized by her that often her anxiety was triggered by some specific performances then
the others. Anna also explained about experiencing panic symptoms which were situation bound
such as a feeling of dizzy, twitchy, bushing and racing heart. Any kind of paraesthesia or
diaphoresis was denied by her. Dissociative symptoms like depersonalization or derealisation
were also denied by her. No associated panic cognitions were found either. Anna explained that
the panic symptoms experienced by her only occurred at times when she was already highly
anxious and not out of the blue.
Situations where Anna was the centre of attention, like a doctor’s appointment or a party, she
reported of having social anxiety which was more generalized.
In the past years, she had been trying to manage herself and fight anxiety in her own ways. She
took precautionary measures such as keeping a water bottle nearby, making small talks, taking
propranolol and so on.
According to her, the symptoms became worse one and half year back. It took place after an
encounter of Anna with her mother. She explained that she did not like her mother and tried to
block all possible contacts with her. She described that since her last meeting with her mother,
the symptoms of anxiety had increased and become very intense and frequent. Although her
mood had been stable, a reduction in memory and concentration was reported by her.
No symptoms of dysthymia or depression were found in her. There were no instances of diurnal
mode variation. She described of having good energy levels, stable weight, healthy appetite, ok
sleep and normal libido. Any kind of perceptual disturbances delusional ideation and thoughts of
self harm or harming others were denied by her. A strong desire of engaging into views was
expressed by Anna.
Past psychiatric history
The first instance of seeking help for anxiety symptoms was made by Anna in 2001. During that
point of time, she experienced occasional panic related symptoms and mild anxiety. The general
practitioner of Anna referred her to a psychologist whom she visited thrice for sessions of CBT.
There she learned about breath controlling and other relation techniques. And I was able to
recognize the abnormal nature of the behavior of her mother and how it affected her
psychological development. According to her, she never had any previous psychiatric diagnosis,
had not visited any psychiatrist and was not prescribed with any medications related to the same.
She denied of having Mania, psychotic symptoms, hypomania or depression previously.
Family Psychiatric and Medical History
No kind of formal psychiatric diagnosis was found in the history of Anna's family. However,
according to her beliefs, her grandmother as well as mother suffered from excessive health and
anxiety concerns which were not fixed by test results and normal examinations from their
respective general practitioners. There was no history of suicide in her family.
Past medical history
Any kind of significant medical history was denied by Anna. History of TOP in 2015 and
rosacea was provided by her general practitioner. A more detailed medical history has been
provided in session 2 by Anna. She was only able to recall minor health issues from her
childhood which required medical attention. As an infant, she suffered from croup and was
provided with treatment in hospital. At the age of 4, Anna had fell off from the balcony of a one
storey, however suffered from no fractures. At the age of 9, she suffered from appendicitis and
required appendectomy. She wore braces and was required to remove a number of teeth.
According to her, she was a happy child.
Medications
expressed by Anna.
Past psychiatric history
The first instance of seeking help for anxiety symptoms was made by Anna in 2001. During that
point of time, she experienced occasional panic related symptoms and mild anxiety. The general
practitioner of Anna referred her to a psychologist whom she visited thrice for sessions of CBT.
There she learned about breath controlling and other relation techniques. And I was able to
recognize the abnormal nature of the behavior of her mother and how it affected her
psychological development. According to her, she never had any previous psychiatric diagnosis,
had not visited any psychiatrist and was not prescribed with any medications related to the same.
She denied of having Mania, psychotic symptoms, hypomania or depression previously.
Family Psychiatric and Medical History
No kind of formal psychiatric diagnosis was found in the history of Anna's family. However,
according to her beliefs, her grandmother as well as mother suffered from excessive health and
anxiety concerns which were not fixed by test results and normal examinations from their
respective general practitioners. There was no history of suicide in her family.
Past medical history
Any kind of significant medical history was denied by Anna. History of TOP in 2015 and
rosacea was provided by her general practitioner. A more detailed medical history has been
provided in session 2 by Anna. She was only able to recall minor health issues from her
childhood which required medical attention. As an infant, she suffered from croup and was
provided with treatment in hospital. At the age of 4, Anna had fell off from the balcony of a one
storey, however suffered from no fractures. At the age of 9, she suffered from appendicitis and
required appendectomy. She wore braces and was required to remove a number of teeth.
According to her, she was a happy child.
Medications
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
As instructed and prescribed by her general practitioner, Anna has been using propranolol 10 mg
PRN for once or twice in a week before her performances. A Mirena IUD was inserted in 2015.
She was also prescribed with a Ceased diazepam PRN.
Substance use history
Alcohol was consumed by Anna more than what was specified by the guidelines of NHMRC.
Currently, she consumes an average of 3 to 4 drinks every night, and in a week she does the
same for 3 nights. This has been a routine for the last 4 years. According to her, she has reduced
this consumption in the last month after her review with Dr. Wyatt. During the 2 week period of
het review with the doctor, any kind of withdrawal symptoms were denied by her. It was
admitted by Anna regarding her over consumption of alcohol than that of the recommended
levels and also expressed a desire for reducing the same. As described by her, alcohol helps in
reducing anxiety, however she did not use the same before her performances. She had no craving
for alcohol and there were no significant effect on our health. Her parenting was also not
impacted since she drank with her husband after her children had gone to bed. Any kind of abuse
of prescription medications were denied by her. Benzodiazepines were used by her whichwere
prescribed by her general practitioner.
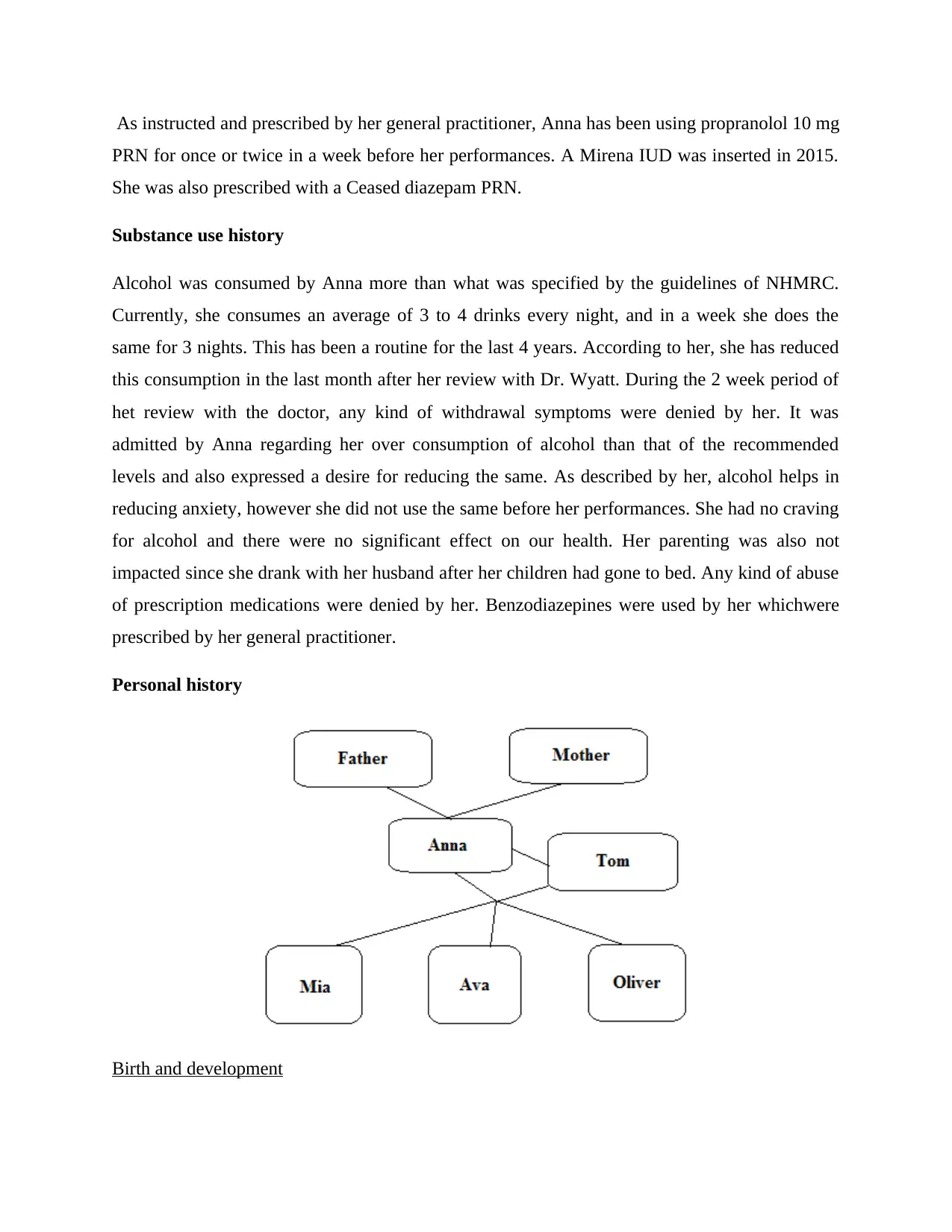
Personal history
Birth and development
PRN for once or twice in a week before her performances. A Mirena IUD was inserted in 2015.
She was also prescribed with a Ceased diazepam PRN.
Substance use history
Alcohol was consumed by Anna more than what was specified by the guidelines of NHMRC.
Currently, she consumes an average of 3 to 4 drinks every night, and in a week she does the
same for 3 nights. This has been a routine for the last 4 years. According to her, she has reduced
this consumption in the last month after her review with Dr. Wyatt. During the 2 week period of
het review with the doctor, any kind of withdrawal symptoms were denied by her. It was
admitted by Anna regarding her over consumption of alcohol than that of the recommended
levels and also expressed a desire for reducing the same. As described by her, alcohol helps in
reducing anxiety, however she did not use the same before her performances. She had no craving
for alcohol and there were no significant effect on our health. Her parenting was also not
impacted since she drank with her husband after her children had gone to bed. Any kind of abuse
of prescription medications were denied by her. Benzodiazepines were used by her whichwere
prescribed by her general practitioner.
Personal history
Birth and development
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Anna was born and raised in the inner east and the inner west of Sydney* respectively. She was
the only child of her parents, and throughout her childhood she lived with her parents and
grandmother.
Childhood
It was reported by Anna that she usually was a well and happy child would like to play alone.
She admitted that she often felt out of place while she was in primary school which was greatly
due to the intervention of a mother in her clothing and attendance on the basis of her health
concerns. However, Anna tried to overcome this while she was in high school since she wanted
to make friends. She admitted that she disliked and tried to avoid conflicts wherever possible.
Family members and relationships
Father
Her father was an architect and mother was a house wife. According to Anna, her father was a
rational, scene and lovely person. She had a great bonding with him and was significantly
supported by him.
Mother
She described her mother as a shallow, fearful, jittery and detached person. She did not share any
kind of bonding with her and explained her as an anxious hypochondriac person.
Husband
Anna described her husband Tom, as a supporting, caring and loving person. He was on full-time
household duties as Anna herself was the primary financial provider oh the house.0020
Forensic history
Any previous court hearing for criminal charges was denied by Anna.
Occupational history
Anna worked as a full time freelance performer and enjoyed her job. In her house, she was the
primary financial provider.
the only child of her parents, and throughout her childhood she lived with her parents and
grandmother.
Childhood
It was reported by Anna that she usually was a well and happy child would like to play alone.
She admitted that she often felt out of place while she was in primary school which was greatly
due to the intervention of a mother in her clothing and attendance on the basis of her health
concerns. However, Anna tried to overcome this while she was in high school since she wanted
to make friends. She admitted that she disliked and tried to avoid conflicts wherever possible.
Family members and relationships
Father
Her father was an architect and mother was a house wife. According to Anna, her father was a
rational, scene and lovely person. She had a great bonding with him and was significantly
supported by him.
Mother
She described her mother as a shallow, fearful, jittery and detached person. She did not share any
kind of bonding with her and explained her as an anxious hypochondriac person.
Husband
Anna described her husband Tom, as a supporting, caring and loving person. He was on full-time
household duties as Anna herself was the primary financial provider oh the house.0020
Forensic history
Any previous court hearing for criminal charges was denied by Anna.
Occupational history
Anna worked as a full time freelance performer and enjoyed her job. In her house, she was the
primary financial provider.
Social history
According to Anna, she enjoyed and loved her work. She took pride in her success. In her
family, Anna earned more than her husband of which she felt very proud, and hence they decided
upon the husband being a full-time parent and staying at home. She liked to catch up with her
female friends, exercise daily and spend quality time with her children. In order to reduce stress,
she attended gym an indulged into high energy aerobic classes.
Mental state examination
Appearance
Anna is presented as a woman of pale skin, small build, stated age and short wavy dark hair. She
wore minimum makeup, usually dressed up in casuals and jeans, exhibited good hygiene, and
wore block heeled shoes. She did not have any pierces or tattoos on her body.
Behavior
With her family, Anna was a co-operative and polite person. She explained of engaging easily
and maintained a good eye contact with people. However, at times when she recalled traumatic
events, she seemed to loom away.
Speech
The speech of Anna was spontaneous with normal variation, tone and rate. She was comfortable
in raising her voice while expressing anger and her tone would lower down while expressing
sadness.
Mood
Her mood usually remained good however; the same became somewhat anxious during a
meeting with a new doctor.
Thought
She possessed a linear and logical thought form and was able to maintain a continuous narrative
even while discussing her trauma.
According to Anna, she enjoyed and loved her work. She took pride in her success. In her
family, Anna earned more than her husband of which she felt very proud, and hence they decided
upon the husband being a full-time parent and staying at home. She liked to catch up with her
female friends, exercise daily and spend quality time with her children. In order to reduce stress,
she attended gym an indulged into high energy aerobic classes.
Mental state examination
Appearance
Anna is presented as a woman of pale skin, small build, stated age and short wavy dark hair. She
wore minimum makeup, usually dressed up in casuals and jeans, exhibited good hygiene, and
wore block heeled shoes. She did not have any pierces or tattoos on her body.
Behavior
With her family, Anna was a co-operative and polite person. She explained of engaging easily
and maintained a good eye contact with people. However, at times when she recalled traumatic
events, she seemed to loom away.
Speech
The speech of Anna was spontaneous with normal variation, tone and rate. She was comfortable
in raising her voice while expressing anger and her tone would lower down while expressing
sadness.
Mood
Her mood usually remained good however; the same became somewhat anxious during a
meeting with a new doctor.
Thought
She possessed a linear and logical thought form and was able to maintain a continuous narrative
even while discussing her trauma.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Perception
No reports or evidences of hallucinatory phenomena were found.
Cognition
Anna was quite alert in general, and had good orientation towards people and places. She had a
good memory and concentration, however, some instances such as visiting a new doctor or
performing at stages in front a lot of people often made her lose focus.
Insight
She had a good insight into the quality and nature of symptoms. Significant judgment has been
exhibited by her in seeking proactive treatment, engaging into review and reducing her alcohol
consumption.
Judgment
Anna’s judgment was unimpaired.
Physical Examination
A physical examination of Anna was completed by her general practitioner. A normal range of
psychomotor activity was exhibited by her. No psychomotor agitation or abnormal movements
were recorded.
Formulation
Anna was the forty five year old woman, who was married and had 3 children. She worked as a
full time freelance performer. She suffered from panic attacks and social anxiety disorder of
which she held a history of 22 years. She also suffered from binge alcohol usage.
The criteria for the disorder of generalized anxiety and panic disorder that was not fulfilled by
her. The criteria for other specific in society disorders were not fulfilled either. No kind of
psychotic symptoms were experienced by her.
The symptoms which Anna held had occurred on a background of genetic predisposition to
health anxiety's early modeling and anxiety by her grandmother and mother.
No reports or evidences of hallucinatory phenomena were found.
Cognition
Anna was quite alert in general, and had good orientation towards people and places. She had a
good memory and concentration, however, some instances such as visiting a new doctor or
performing at stages in front a lot of people often made her lose focus.
Insight
She had a good insight into the quality and nature of symptoms. Significant judgment has been
exhibited by her in seeking proactive treatment, engaging into review and reducing her alcohol
consumption.
Judgment
Anna’s judgment was unimpaired.
Physical Examination
A physical examination of Anna was completed by her general practitioner. A normal range of
psychomotor activity was exhibited by her. No psychomotor agitation or abnormal movements
were recorded.
Formulation
Anna was the forty five year old woman, who was married and had 3 children. She worked as a
full time freelance performer. She suffered from panic attacks and social anxiety disorder of
which she held a history of 22 years. She also suffered from binge alcohol usage.
The criteria for the disorder of generalized anxiety and panic disorder that was not fulfilled by
her. The criteria for other specific in society disorders were not fulfilled either. No kind of
psychotic symptoms were experienced by her.
The symptoms which Anna held had occurred on a background of genetic predisposition to
health anxiety's early modeling and anxiety by her grandmother and mother.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Evidences of significant difficulties of attachment were found related to Anna and her mother.
The psychological vulnerabilities exhibited by Anna resulted from the difficulties during her
developmental stage which can be described as personality structure of the cluster C.
In spite of the issues, the trauma was used by Anna constructively for driving her career and
attachment parenting style.
Furthermore, new suicidal, self harming tendencies were found in Anna. She found herself to be
well supported by her husband and had a good bonding with the children.
The primary objective of the psychodynamic therapy would be to be placed at the place of the
mother, Hold and hear the anger of Anna and allow her for stepping towards the depressive
position. The other part of the work would also be to assist her for acquiring the ability of
regulating her own impact without dress using to her safety behavior and helping her in
improving her self esteem. It would also include helping her to reduce her fears of rejection and
shame.
Diagnosis
The symptoms of Anna were considered to be mild as they affected only about 10% of the
performances. However, it was required by the DSM criterion C that fears or anxiety was always
provoked by the social situations. The full criteria for diagnosis of alcohol usage disorder were
not met, even though the disorder was considered. Anna had been working up on reducing her
alcohol consumption. However, the amount consumed by her is still above the recommended
levels.
No evidence of cluster C personality structure was found. Out of the seven criteria for the
disorder of avoidant personality, Anna met 3; however, in order to conduct a diagnosis, a
minimum of four criteria should have been met. Hence, the required number of criteria was not
met for the disorder of avoidant personality.
No evidences of secondary or comorbid major depressive dysthymia or disorder was found. The
criteria for other specified disorders of anxiety was not fulfilled either. No current symptoms or
history of mania or psychosis was found. Anna had certain low acute risk issues. The primary
risk was the usage of alcohol.
The psychological vulnerabilities exhibited by Anna resulted from the difficulties during her
developmental stage which can be described as personality structure of the cluster C.
In spite of the issues, the trauma was used by Anna constructively for driving her career and
attachment parenting style.
Furthermore, new suicidal, self harming tendencies were found in Anna. She found herself to be
well supported by her husband and had a good bonding with the children.
The primary objective of the psychodynamic therapy would be to be placed at the place of the
mother, Hold and hear the anger of Anna and allow her for stepping towards the depressive
position. The other part of the work would also be to assist her for acquiring the ability of
regulating her own impact without dress using to her safety behavior and helping her in
improving her self esteem. It would also include helping her to reduce her fears of rejection and
shame.
Diagnosis
The symptoms of Anna were considered to be mild as they affected only about 10% of the
performances. However, it was required by the DSM criterion C that fears or anxiety was always
provoked by the social situations. The full criteria for diagnosis of alcohol usage disorder were
not met, even though the disorder was considered. Anna had been working up on reducing her
alcohol consumption. However, the amount consumed by her is still above the recommended
levels.
No evidence of cluster C personality structure was found. Out of the seven criteria for the
disorder of avoidant personality, Anna met 3; however, in order to conduct a diagnosis, a
minimum of four criteria should have been met. Hence, the required number of criteria was not
met for the disorder of avoidant personality.
No evidences of secondary or comorbid major depressive dysthymia or disorder was found. The
criteria for other specified disorders of anxiety was not fulfilled either. No current symptoms or
history of mania or psychosis was found. Anna had certain low acute risk issues. The primary
risk was the usage of alcohol.

Anna had suitability for psychotherapy. She had the potential of benefiting from CBT for getting
rid of the disorder of social anxiety. She could also be a good candidate for the psychodynamic
psychotherapy.
Management Plan
I furnished the details of the past history of Anna with reference to her treatment. The aspects
which were taken into account are as follows:
Medication
Appropriate antidepressants have been prescribed for Anna as far as the course of her treatment
is concerned. However, she has expressed dissatisfaction since none of the antidepressants have
hitherto helped her in the long run. Additionally, some of the antidepressants have caused side-
effects to a massive extent. As a result, her general practitioner suggested the alteration of the
course of the intake of such antidepressants which helped her to recover to a certain extent as far
as the improvement in mental health is concerned. This led her general practitioner to continue
prescribing the antidepressants on a periodic basis taking account of her signs of recovery and
improvement as far as her moods are concerned depending upon the situation in question. Her
present medications are inclusive of ten milligrams of Propranolol and 2 milligrams of
Diazepam.
Psychotherapy
The kind of psychotherapy involved in her treatment was the short-term dynamic therapy. Such a
therapy implies the principles related to psychoanalysis in order to formulate an understanding
with reference to the attraction of patients and clients at the sessions related to the concerned
therapy. Such a therapy involves forty sessions thereby resulting in motivation with reference to
the prevention of avoidance (Prochaska and Norcross, 2018). It also includes interaction in a
flexible manner as far as expression is concerned. Additionally, the aspects of interpersonal
relationships are to be improved as a result of the Levels of Personality Functioning Scale DSM-
5 alternative models of personality disorders in order to provide an opportunity to Anna for
identifying her actions relating to the situations concerned with reference to the addressing of the
issues relating to the making of conversations with others. It would help in the improvement of
rid of the disorder of social anxiety. She could also be a good candidate for the psychodynamic
psychotherapy.
Management Plan
I furnished the details of the past history of Anna with reference to her treatment. The aspects
which were taken into account are as follows:
Medication
Appropriate antidepressants have been prescribed for Anna as far as the course of her treatment
is concerned. However, she has expressed dissatisfaction since none of the antidepressants have
hitherto helped her in the long run. Additionally, some of the antidepressants have caused side-
effects to a massive extent. As a result, her general practitioner suggested the alteration of the
course of the intake of such antidepressants which helped her to recover to a certain extent as far
as the improvement in mental health is concerned. This led her general practitioner to continue
prescribing the antidepressants on a periodic basis taking account of her signs of recovery and
improvement as far as her moods are concerned depending upon the situation in question. Her
present medications are inclusive of ten milligrams of Propranolol and 2 milligrams of
Diazepam.
Psychotherapy
The kind of psychotherapy involved in her treatment was the short-term dynamic therapy. Such a
therapy implies the principles related to psychoanalysis in order to formulate an understanding
with reference to the attraction of patients and clients at the sessions related to the concerned
therapy. Such a therapy involves forty sessions thereby resulting in motivation with reference to
the prevention of avoidance (Prochaska and Norcross, 2018). It also includes interaction in a
flexible manner as far as expression is concerned. Additionally, the aspects of interpersonal
relationships are to be improved as a result of the Levels of Personality Functioning Scale DSM-
5 alternative models of personality disorders in order to provide an opportunity to Anna for
identifying her actions relating to the situations concerned with reference to the addressing of the
issues relating to the making of conversations with others. It would help in the improvement of
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 31
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





