Public Health Essay: Cultural Competency and Healthcare Access
VerifiedAdded on 2023/04/04
|10
|1799
|456
Essay
AI Summary
This essay discusses the importance of cultural competency training for public health professionals, focusing on the need to respect and understand diverse cultures to address public health needs. The author reflects on their experiences and suitability as a cultural liaison, emphasizing the importance of cross-cultural interactions in reducing healthcare disparities and improving access for culturally and linguistically diverse (CALD) communities, including indigenous populations. The essay examines the NHMRC's cultural competency policies, professional guidelines, and the concept of cultural safety, highlighting the need for healthcare practitioners to examine their own biases and promote inclusivity. It also addresses barriers to culturally safe care, such as linguistic barriers and institutional racism, and suggests enablers like collaboration and respectful relationships with patients. The author concludes by asserting their readiness to serve as a cultural liaison officer, drawing upon their training, experience, and commitment to addressing the cultural needs of vulnerable populations, with reference to relevant legislation and ethical guidelines. Desklib provides more solved assignments and study resources for students.

Running head: PUBLIC HEALTH
PUBLIC HEALTH
Name of the Student
Name of the university
Author’s not
PUBLIC HEALTH
Name of the Student
Name of the university
Author’s not
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1PUBLIC HEALTH
1. I am enrolled in a course of public health. Students studying about public health and thriving
to be public health professionals have to be trained in cultural competency training. Being a
student is public health, I have underwent training in cultural competency, that has enabled in
me, the seed of cultural acceptance, that is respecting and understand my own culture and
other cultures to address the needs of the public. The attitude based programming, my past
experience and my habit of self-evaluation and self -critiquing and my capability of
intercultural learning and interaction makes me suitable to become a cultural liaison (Fleckma
et al., 2016). Furthermore, I believe that I am well acquainted with all the legislation related to
the preservation of CALD or indigenous rights. I believe that I also possess the capability to
work in collaboration with culturally and linguistically diverse communities (CALD) as my
discipline, profession called for an amalgamation with other cultures in order to understand
their cultural needs and the social determinants of their health.
2. Being a student of public health, it is my duty to understand that the diversity of our nation is
growing rapidly, along with the increasing cross cultural interactions. While researching
about public health, I have come to know that cross cultural interactions and cultural
competence has been described to be critical for the reduction of the health care disparities
and improving the access to a high quality of health care (Powell, 2016). I have always
determined culture, to be an important social determinants of health. The overall wellbeing
of the people belonging to ethnic minorities is dependent on their spirituality and cultural
beliefs. Hence, preservation of the culture and ethnicity is necessary for preserving their
1. I am enrolled in a course of public health. Students studying about public health and thriving
to be public health professionals have to be trained in cultural competency training. Being a
student is public health, I have underwent training in cultural competency, that has enabled in
me, the seed of cultural acceptance, that is respecting and understand my own culture and
other cultures to address the needs of the public. The attitude based programming, my past
experience and my habit of self-evaluation and self -critiquing and my capability of
intercultural learning and interaction makes me suitable to become a cultural liaison (Fleckma
et al., 2016). Furthermore, I believe that I am well acquainted with all the legislation related to
the preservation of CALD or indigenous rights. I believe that I also possess the capability to
work in collaboration with culturally and linguistically diverse communities (CALD) as my
discipline, profession called for an amalgamation with other cultures in order to understand
their cultural needs and the social determinants of their health.
2. Being a student of public health, it is my duty to understand that the diversity of our nation is
growing rapidly, along with the increasing cross cultural interactions. While researching
about public health, I have come to know that cross cultural interactions and cultural
competence has been described to be critical for the reduction of the health care disparities
and improving the access to a high quality of health care (Powell, 2016). I have always
determined culture, to be an important social determinants of health. The overall wellbeing
of the people belonging to ethnic minorities is dependent on their spirituality and cultural
beliefs. Hence, preservation of the culture and ethnicity is necessary for preserving their
2PUBLIC HEALTH
health (Powell, 2016). I was working with the indigenous people under a clinical setting, I
came to know that they often have to wait in long queues and even face communication
difficulties during the health checkup. Considering the basic human rights, that every citizen
has got the right to access health care, it is necessary to provide equal health care access to
the CALD or the indigenous communities of Australia (Skellett, 2012). I suggested for
giving the members of the CALD communities with an ID card with a unique registration
number, that would not only give them free healthcare services all over the country but will
also be treated in an urgent basis if emergency condition has been detected. Through cross-
cultural interaction with CALD and the indigenous patient, did I came to know about the
difficulties of the CALD communities while endeavoring to access an equitable health care.
3.
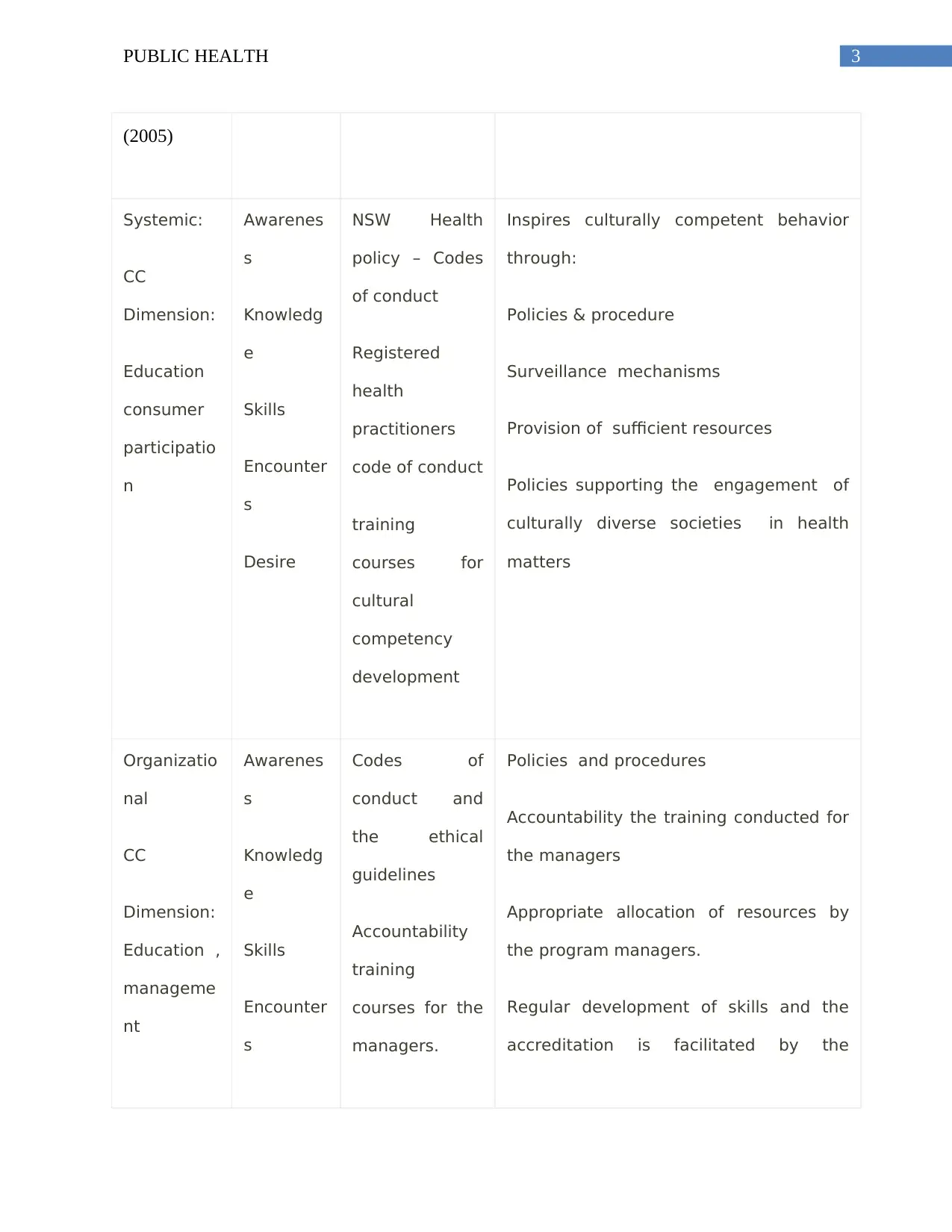
NHMRC
(National
medical
research
council)
levels & CC
Dimensions
(National
health and
Medical
research
council,
CC
Construct
s
Polices/
Guidelines for
public health
professionals
NHMRC Actions
health (Powell, 2016). I was working with the indigenous people under a clinical setting, I
came to know that they often have to wait in long queues and even face communication
difficulties during the health checkup. Considering the basic human rights, that every citizen
has got the right to access health care, it is necessary to provide equal health care access to
the CALD or the indigenous communities of Australia (Skellett, 2012). I suggested for
giving the members of the CALD communities with an ID card with a unique registration
number, that would not only give them free healthcare services all over the country but will
also be treated in an urgent basis if emergency condition has been detected. Through cross-
cultural interaction with CALD and the indigenous patient, did I came to know about the
difficulties of the CALD communities while endeavoring to access an equitable health care.
3.
NHMRC
(National
medical
research
council)
levels & CC
Dimensions
(National
health and
Medical
research
council,
CC
Construct
s
Polices/
Guidelines for
public health
professionals
NHMRC Actions
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3PUBLIC HEALTH
(2005)
Systemic:
CC
Dimension:
Education
consumer
participatio
n
Awarenes
s
Knowledg
e
Skills
Encounter
s
Desire
NSW Health
policy – Codes
of conduct
Registered
health
practitioners
code of conduct
training
courses for
cultural
competency
development
Inspires culturally competent behavior
through:
Policies & procedure
Surveillance mechanisms
Provision of sufficient resources
Policies supporting the engagement of
culturally diverse societies in health
matters
Organizatio
nal
CC
Dimension:
Education ,
manageme
nt
Awarenes
s
Knowledg
e
Skills
Encounter
s
Codes of
conduct and
the ethical
guidelines
Accountability
training
courses for the
managers.
Policies and procedures
Accountability the training conducted for
the managers
Appropriate allocation of resources by
the program managers.
Regular development of skills and the
accreditation is facilitated by the
(2005)
Systemic:
CC
Dimension:
Education
consumer
participatio
n
Awarenes
s
Knowledg
e
Skills
Encounter
s
Desire
NSW Health
policy – Codes
of conduct
Registered
health
practitioners
code of conduct
training
courses for
cultural
competency
development
Inspires culturally competent behavior
through:
Policies & procedure
Surveillance mechanisms
Provision of sufficient resources
Policies supporting the engagement of
culturally diverse societies in health
matters
Organizatio
nal
CC
Dimension:
Education ,
manageme
nt
Awarenes
s
Knowledg
e
Skills
Encounter
s
Codes of
conduct and
the ethical
guidelines
Accountability
training
courses for the
managers.
Policies and procedures
Accountability the training conducted for
the managers
Appropriate allocation of resources by
the program managers.
Regular development of skills and the
accreditation is facilitated by the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4PUBLIC HEALTH
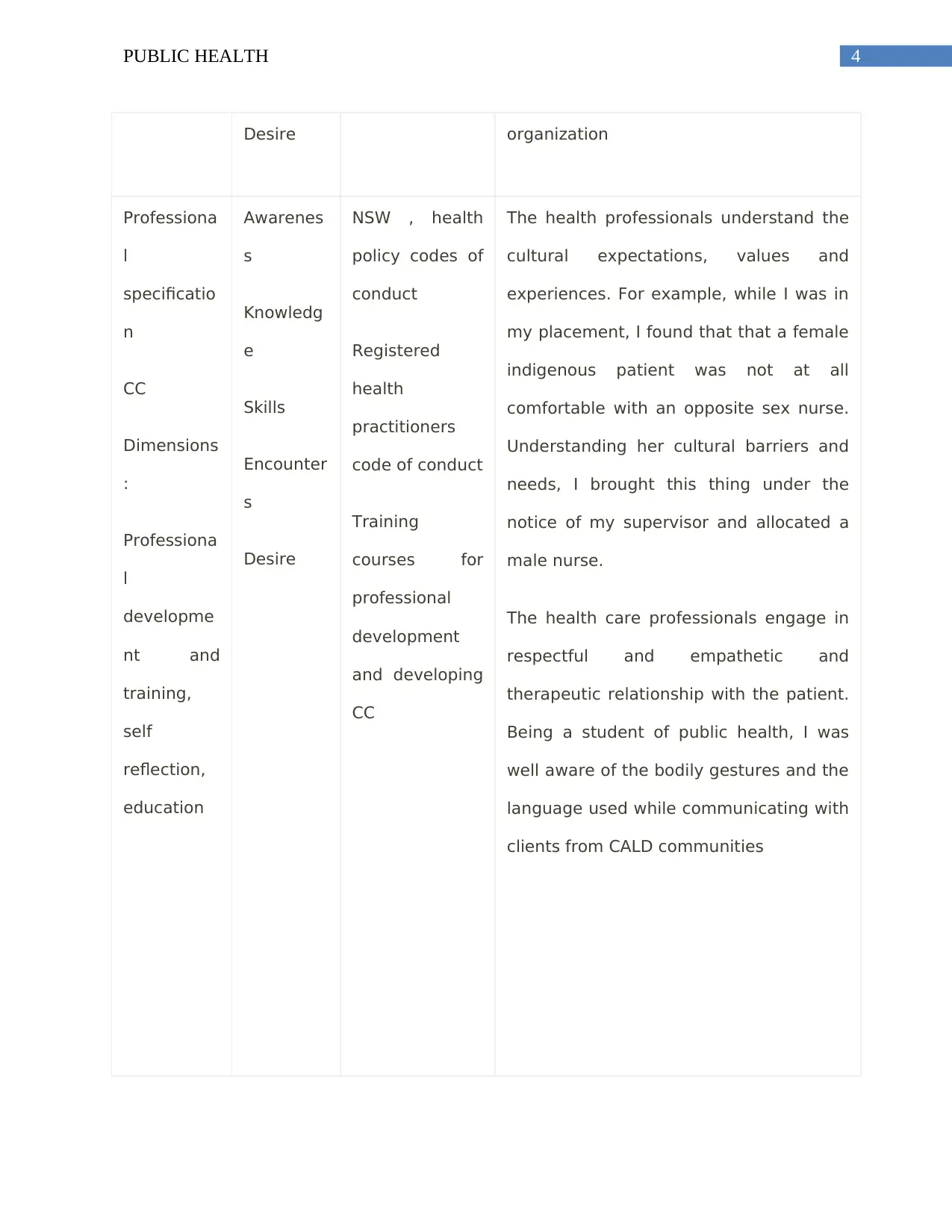
Desire organization
Professiona
l
specificatio
n
CC
Dimensions
:
Professiona
l
developme
nt and
training,
self
reflection,
education
Awarenes
s
Knowledg
e
Skills
Encounter
s
Desire
NSW , health
policy codes of
conduct
Registered
health
practitioners
code of conduct
Training
courses for
professional
development
and developing
CC
The health professionals understand the
cultural expectations, values and
experiences. For example, while I was in
my placement, I found that that a female
indigenous patient was not at all
comfortable with an opposite sex nurse.
Understanding her cultural barriers and
needs, I brought this thing under the
notice of my supervisor and allocated a
male nurse.
The health care professionals engage in
respectful and empathetic and
therapeutic relationship with the patient.
Being a student of public health, I was
well aware of the bodily gestures and the
language used while communicating with
clients from CALD communities
Desire organization
Professiona
l
specificatio
n
CC
Dimensions
:
Professiona
l
developme
nt and
training,
self
reflection,
education
Awarenes
s
Knowledg
e
Skills
Encounter
s
Desire
NSW , health
policy codes of
conduct
Registered
health
practitioners
code of conduct
Training
courses for
professional
development
and developing
CC
The health professionals understand the
cultural expectations, values and
experiences. For example, while I was in
my placement, I found that that a female
indigenous patient was not at all
comfortable with an opposite sex nurse.
Understanding her cultural barriers and
needs, I brought this thing under the
notice of my supervisor and allocated a
male nurse.
The health care professionals engage in
respectful and empathetic and
therapeutic relationship with the patient.
Being a student of public health, I was
well aware of the bodily gestures and the
language used while communicating with
clients from CALD communities
5PUBLIC HEALTH
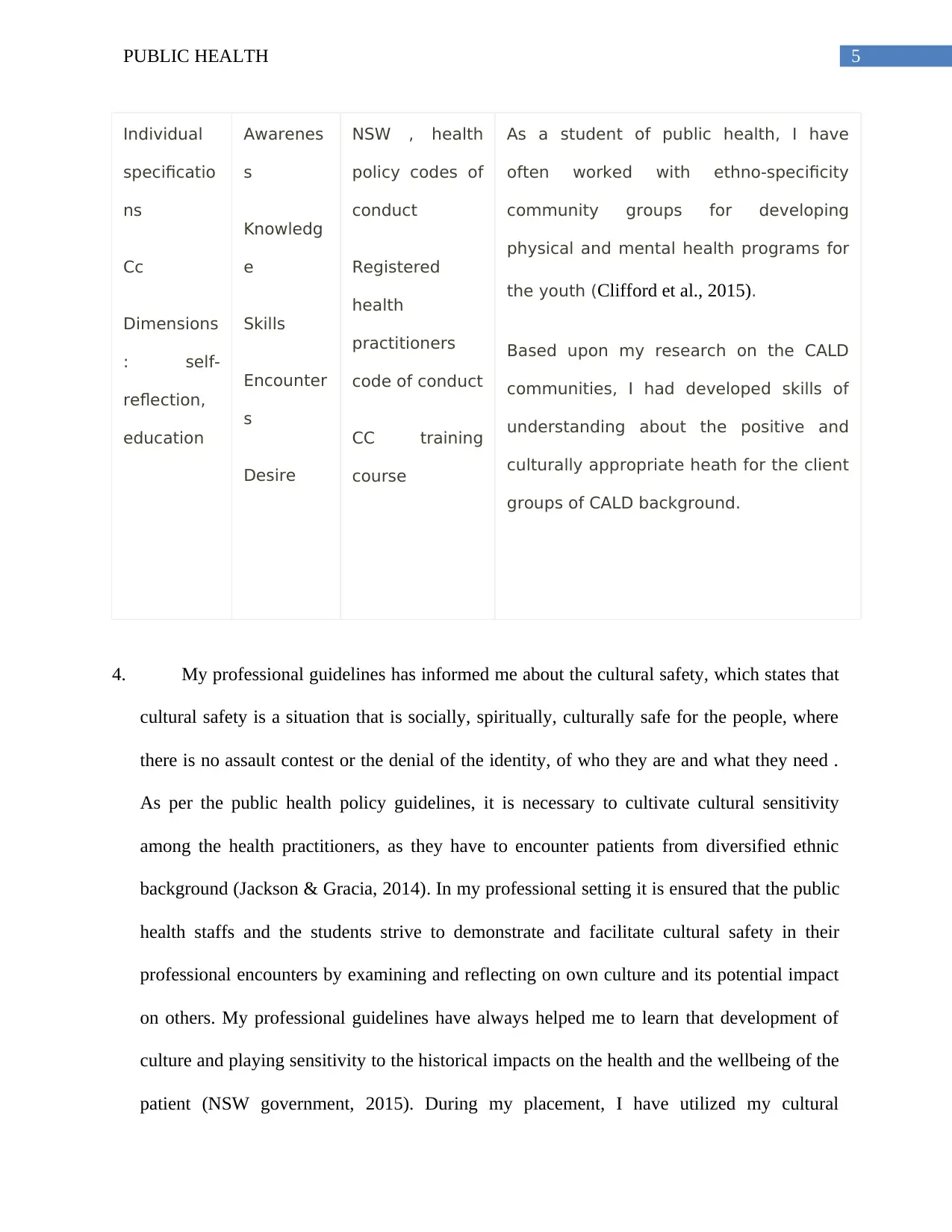
Individual
specificatio
ns
Cc
Dimensions
: self-
reflection,
education
Awarenes
s
Knowledg
e
Skills
Encounter
s
Desire
NSW , health
policy codes of
conduct
Registered
health
practitioners
code of conduct
CC training
course
As a student of public health, I have
often worked with ethno-specificity
community groups for developing
physical and mental health programs for
the youth (Clifford et al., 2015).
Based upon my research on the CALD
communities, I had developed skills of
understanding about the positive and
culturally appropriate heath for the client
groups of CALD background.
4. My professional guidelines has informed me about the cultural safety, which states that
cultural safety is a situation that is socially, spiritually, culturally safe for the people, where
there is no assault contest or the denial of the identity, of who they are and what they need .
As per the public health policy guidelines, it is necessary to cultivate cultural sensitivity
among the health practitioners, as they have to encounter patients from diversified ethnic
background (Jackson & Gracia, 2014). In my professional setting it is ensured that the public
health staffs and the students strive to demonstrate and facilitate cultural safety in their
professional encounters by examining and reflecting on own culture and its potential impact
on others. My professional guidelines have always helped me to learn that development of
culture and playing sensitivity to the historical impacts on the health and the wellbeing of the
patient (NSW government, 2015). During my placement, I have utilized my cultural
Individual
specificatio
ns
Cc
Dimensions
: self-
reflection,
education
Awarenes
s
Knowledg
e
Skills
Encounter
s
Desire
NSW , health
policy codes of
conduct
Registered
health
practitioners
code of conduct
CC training
course
As a student of public health, I have
often worked with ethno-specificity
community groups for developing
physical and mental health programs for
the youth (Clifford et al., 2015).
Based upon my research on the CALD
communities, I had developed skills of
understanding about the positive and
culturally appropriate heath for the client
groups of CALD background.
4. My professional guidelines has informed me about the cultural safety, which states that
cultural safety is a situation that is socially, spiritually, culturally safe for the people, where
there is no assault contest or the denial of the identity, of who they are and what they need .
As per the public health policy guidelines, it is necessary to cultivate cultural sensitivity
among the health practitioners, as they have to encounter patients from diversified ethnic
background (Jackson & Gracia, 2014). In my professional setting it is ensured that the public
health staffs and the students strive to demonstrate and facilitate cultural safety in their
professional encounters by examining and reflecting on own culture and its potential impact
on others. My professional guidelines have always helped me to learn that development of
culture and playing sensitivity to the historical impacts on the health and the wellbeing of the
patient (NSW government, 2015). During my placement, I have utilized my cultural
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6PUBLIC HEALTH
competency training, which I had received at the time of the induction of the hospital policy.
My mentor and I specifically visited those words having the indigenous patients. It was nice
to see that the organization has arranged for an interpreter, as many of the patients belonging
to the CALD communities and their families were having difficulties in communicating with
the health care workers. Hence, use of \an interpreter for effective communication with the
patients belonging to different ethnic minorities is a part of the organization policy.
Furthermore, it should be notified that self-reflection and critiquing helps a public health
administrator working as a cultural liaison to take up approaches for serving the diverse
ethnic group (Skellett, 2012).
5. At first we should understand the meaning of culturally safe care. It involves the health care
professionals examining their own practices, beliefs, behaviors as well as issues like
institutional racism for ensuring that their services are perceived to be safe by the patient
rather than the provider (Cushman, et al, 2014). Although the government and each and
every organization are thriving to provide a culturally safe care, there are several barriers or
enablers to the provision of a culturally safe care.
One of the main barriers to equal access to health care are the linguistic barrier. It might
become challenging to communicate with the patients of the CALD communities, due to their
different language, in the absence of any interpreters. Another barrier to a culturally safe care is
the incidence of institutional racism and discrimination that restricts the health care provisions
for the vulnerable public (Betancourt et al., 2016). In order to remove the barriers, I would make
use of my cultural competence training and would definitely thrive to update by cultural
competency training, which I had received at the time of the induction of the hospital policy.
My mentor and I specifically visited those words having the indigenous patients. It was nice
to see that the organization has arranged for an interpreter, as many of the patients belonging
to the CALD communities and their families were having difficulties in communicating with
the health care workers. Hence, use of \an interpreter for effective communication with the
patients belonging to different ethnic minorities is a part of the organization policy.
Furthermore, it should be notified that self-reflection and critiquing helps a public health
administrator working as a cultural liaison to take up approaches for serving the diverse
ethnic group (Skellett, 2012).
5. At first we should understand the meaning of culturally safe care. It involves the health care
professionals examining their own practices, beliefs, behaviors as well as issues like
institutional racism for ensuring that their services are perceived to be safe by the patient
rather than the provider (Cushman, et al, 2014). Although the government and each and
every organization are thriving to provide a culturally safe care, there are several barriers or
enablers to the provision of a culturally safe care.
One of the main barriers to equal access to health care are the linguistic barrier. It might
become challenging to communicate with the patients of the CALD communities, due to their
different language, in the absence of any interpreters. Another barrier to a culturally safe care is
the incidence of institutional racism and discrimination that restricts the health care provisions
for the vulnerable public (Betancourt et al., 2016). In order to remove the barriers, I would make
use of my cultural competence training and would definitely thrive to update by cultural
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7PUBLIC HEALTH
sensitivity. This is again possible by developing partnership with the indigenous support workers
and the CALD community.
Just like the barriers, there were several enablers or facilitators to a culturally safe and
competent specialized practice for the staffs in the profession and the consumers of health. They
are collaborating with the patient. A respectful relationship between the client and the patient
ensures that they are appropriately supported while seeking health care facilities (Schouler-Ocak
et al., 2016).
6. I consider myself to be a suitable candidate for the job of cultural liaison officer, as I believe
that my work experience, my cultural competence training and my the habit of self-critiquing
and to indulge in life-long learning would help me to become a cultural liaison officer and
function in accordance with the requirement of the relevant legislation for the registered
profession. The codes of conduct for the registered health practitioners and the ethical
guidelines that I have studied in my course would assist me in understanding the social
determinants linked with the health outcomes of the vulnerable section of people. addressing
the cultural needs of the CALD communities. Extensive research about public health, social
determinants of health and human rights would further assist me in understanding the gaps in
cultural needs of the different ethnic minority groups.
sensitivity. This is again possible by developing partnership with the indigenous support workers
and the CALD community.
Just like the barriers, there were several enablers or facilitators to a culturally safe and
competent specialized practice for the staffs in the profession and the consumers of health. They
are collaborating with the patient. A respectful relationship between the client and the patient
ensures that they are appropriately supported while seeking health care facilities (Schouler-Ocak
et al., 2016).
6. I consider myself to be a suitable candidate for the job of cultural liaison officer, as I believe
that my work experience, my cultural competence training and my the habit of self-critiquing
and to indulge in life-long learning would help me to become a cultural liaison officer and
function in accordance with the requirement of the relevant legislation for the registered
profession. The codes of conduct for the registered health practitioners and the ethical
guidelines that I have studied in my course would assist me in understanding the social
determinants linked with the health outcomes of the vulnerable section of people. addressing
the cultural needs of the CALD communities. Extensive research about public health, social
determinants of health and human rights would further assist me in understanding the gaps in
cultural needs of the different ethnic minority groups.
8PUBLIC HEALTH
References
Betancourt, J. R., Green, A. R., Carrillo, J. E., & Owusu Ananeh-Firempong, I. I. (2016).
Defining cultural competence: a practical framework for addressing racial/ethnic
disparities in health and health care. Public health reports.
Clifford, A., McCalman, J., Bainbridge, R., & Tsey, K. (2015). Interventions to improve cultural
competency in health care for Indigenous peoples of Australia, New Zealand, Canada and
the USA: a systematic review. International Journal for Quality in Health Care, 27(2),
89-98.
Cushman, L. F., Delva, M., Franks, C. L., Jimenez-Bautista, A., Moon-Howard, J., Glover, J., &
Begg, M. D. (2015). Cultural competency training for public health students: Integrating
self, social, and global awareness into a master of public health curriculum. American
journal of public health, 105(S1), S132-S140.
Fleckman, J. M., Dal Corso, M., Ramirez, S., Begalieva, M., & Johnson, C. C. (2015).
Intercultural Competency in Public Health: A Call for Action to Incorporate Training into
Public Health Education. Frontiers in public health, 3, 210.
doi:10.3389/fpubh.2015.00210
Jackson, C. S., & Gracia, J. N. (2014). Addressing health and health-care disparities: the role of a
diverse workforce and the social determinants of health. Public Health Reports,
129(1_suppl2), 57-61.
References
Betancourt, J. R., Green, A. R., Carrillo, J. E., & Owusu Ananeh-Firempong, I. I. (2016).
Defining cultural competence: a practical framework for addressing racial/ethnic
disparities in health and health care. Public health reports.
Clifford, A., McCalman, J., Bainbridge, R., & Tsey, K. (2015). Interventions to improve cultural
competency in health care for Indigenous peoples of Australia, New Zealand, Canada and
the USA: a systematic review. International Journal for Quality in Health Care, 27(2),
89-98.
Cushman, L. F., Delva, M., Franks, C. L., Jimenez-Bautista, A., Moon-Howard, J., Glover, J., &
Begg, M. D. (2015). Cultural competency training for public health students: Integrating
self, social, and global awareness into a master of public health curriculum. American
journal of public health, 105(S1), S132-S140.
Fleckman, J. M., Dal Corso, M., Ramirez, S., Begalieva, M., & Johnson, C. C. (2015).
Intercultural Competency in Public Health: A Call for Action to Incorporate Training into
Public Health Education. Frontiers in public health, 3, 210.
doi:10.3389/fpubh.2015.00210
Jackson, C. S., & Gracia, J. N. (2014). Addressing health and health-care disparities: the role of a
diverse workforce and the social determinants of health. Public Health Reports,
129(1_suppl2), 57-61.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9PUBLIC HEALTH
National health and Medical research council, (2005) .Cultural Competency in health: A guide
for policy, partnerships and participation. Access date: 23.5.2019. Retrieved from:
https://www.mhahs.org.au/images/cald/CulturalCompetencyInHealth.pdf
NSW government, (2015).NSW Heath Code of Conduct. Access date: 23.5.2019. Retrieved
from: https://www1.health.nsw.gov.au/pds/ActivePDSDocuments/PD2015_049.pdf
Powell, D. L. (2016). Social determinants of health: Cultural competence is not enough.
Schouler-Ocak, M., Graef-Calliess, I. T., Tarricone, I., Qureshi, A., Kastrup, M. C., & Bhugra,
D. (2015). EPA guidance on cultural competence training. European Psychiatry, 30(3),
431-440.
Skellett, L. (2012). Cultural awareness and cultural safety. Australian Pharmacist, 31(5), 382.
National health and Medical research council, (2005) .Cultural Competency in health: A guide
for policy, partnerships and participation. Access date: 23.5.2019. Retrieved from:
https://www.mhahs.org.au/images/cald/CulturalCompetencyInHealth.pdf
NSW government, (2015).NSW Heath Code of Conduct. Access date: 23.5.2019. Retrieved
from: https://www1.health.nsw.gov.au/pds/ActivePDSDocuments/PD2015_049.pdf
Powell, D. L. (2016). Social determinants of health: Cultural competence is not enough.
Schouler-Ocak, M., Graef-Calliess, I. T., Tarricone, I., Qureshi, A., Kastrup, M. C., & Bhugra,
D. (2015). EPA guidance on cultural competence training. European Psychiatry, 30(3),
431-440.
Skellett, L. (2012). Cultural awareness and cultural safety. Australian Pharmacist, 31(5), 382.
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





