NSC2500: Pulmonary Arterial Hypertension, Pharmacology and Physiology
VerifiedAdded on 2023/06/03
|12
|1173
|334
Project
AI Summary
This assignment delves into the physiology and pharmacology of pulmonary arterial hypertension (PAH). It begins by defining PAH and outlining its physiological impact, including the narrowing of pulmonary arteries and the resulting strain on the heart. The pathophysiology section details the mechanisms behind PAH, such as vasoconstriction, endothelial proliferation, and inflammation, as well as factors like gene mutations and autoantibodies. The pharmacology section focuses on Iloprost, a drug used to improve blood flow by widening blood vessels. It explores the drug's pharmacodynamics, mechanism of action, and pharmacokinetics, including its administration routes and half-life. The document also covers indications, contraindications, precautions, and side effects of Iloprost, and highlights the relevance of this information for healthcare professionals. References from credible sources are included.
Pulmonary Arterial
hypertension
hypertension
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
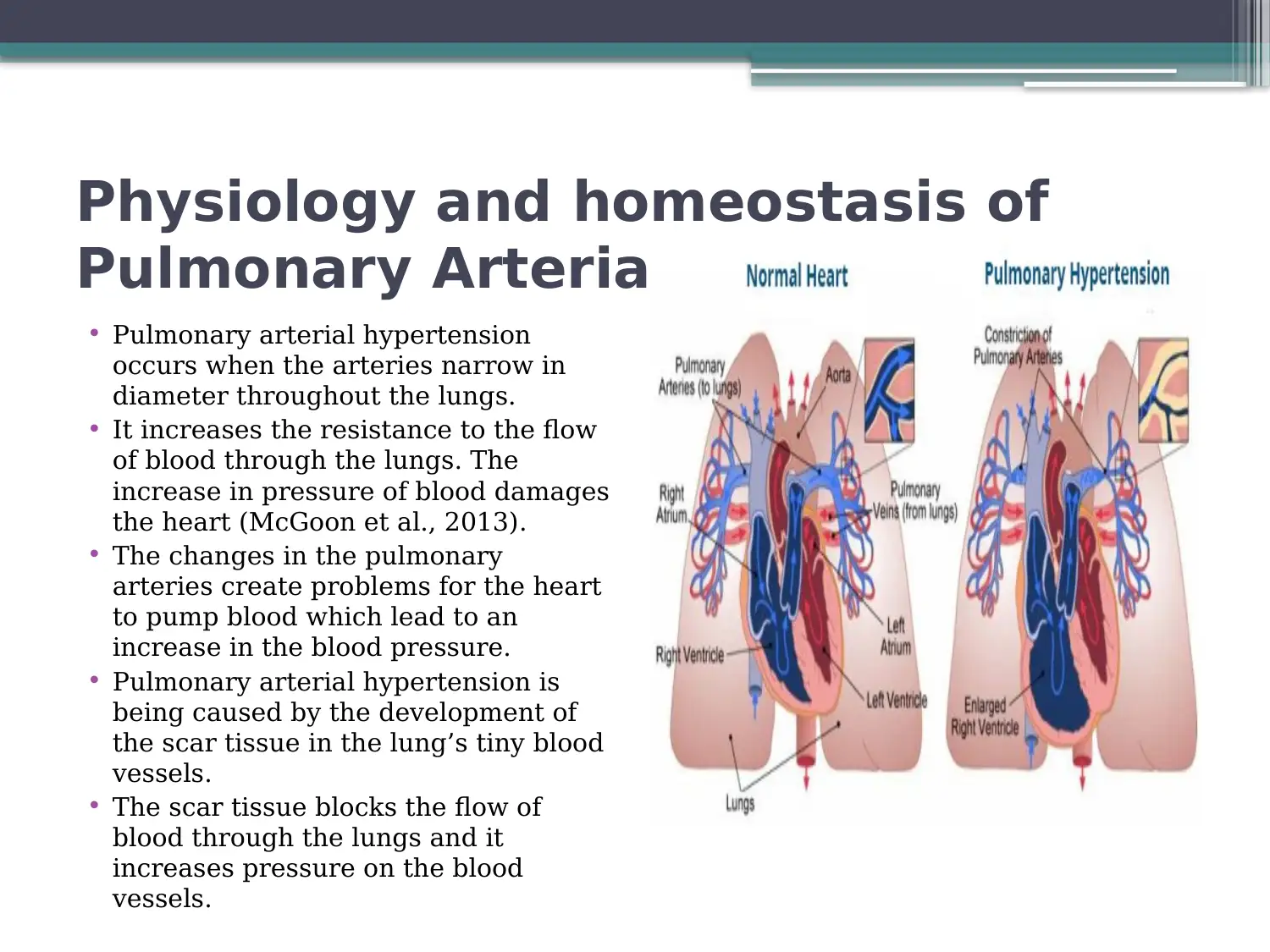
Physiology and homeostasis of
Pulmonary Arterial Hypertension
• Pulmonary arterial hypertension
occurs when the arteries narrow in
diameter throughout the lungs.
• It increases the resistance to the flow
of blood through the lungs. The
increase in pressure of blood damages
the heart (McGoon et al., 2013).
• The changes in the pulmonary
arteries create problems for the heart
to pump blood which lead to an
increase in the blood pressure.
• Pulmonary arterial hypertension is
being caused by the development of
the scar tissue in the lung’s tiny blood
vessels.
• The scar tissue blocks the flow of
blood through the lungs and it
increases pressure on the blood
vessels.
Pulmonary Arterial Hypertension
• Pulmonary arterial hypertension
occurs when the arteries narrow in
diameter throughout the lungs.
• It increases the resistance to the flow
of blood through the lungs. The
increase in pressure of blood damages
the heart (McGoon et al., 2013).
• The changes in the pulmonary
arteries create problems for the heart
to pump blood which lead to an
increase in the blood pressure.
• Pulmonary arterial hypertension is
being caused by the development of
the scar tissue in the lung’s tiny blood
vessels.
• The scar tissue blocks the flow of
blood through the lungs and it
increases pressure on the blood
vessels.
Pathophysiology
• Obliteration in the pulmonary vascular wall and pathologic vasoconstriction is
mainly responsible for pulmonary vascular resistance.
• Pulmonary hypertension is caused by various factors like pathologic
vasoconstriction endothelial and smooth muscle proliferation, hypertrophy and
chronic inflammation.
• Vascular obstruction is also responsible for activating coagulation, which is caused
by an increase in pulmonary pressure and endothelium injuries.
• Pulmonary hypertension increases pulmonary venous pressure, which harms the left
side of the heart by increasing pressure in the left heart ventricle (Humbert, 2010).
• Pulmonary arteries also gain high pressure due to excessive stress which results in
causing injuries to the alveolar-capillary wall and edema.
• Pulmonary hypertension can be associated with gene mutation encoding bone
morphogenetic protein receptor type II, HIV infection and heart disease.
• In patients with high Pulmonary hypertension, high level of pro-inflammatory
cytokines like interleukin I, interleukin 6 and macrophage inflammatory protein are
found.
• Circulating autoantibodies are also found in the peripheral blood of the Pulmonary
hypertension patient.
• Obliteration in the pulmonary vascular wall and pathologic vasoconstriction is
mainly responsible for pulmonary vascular resistance.
• Pulmonary hypertension is caused by various factors like pathologic
vasoconstriction endothelial and smooth muscle proliferation, hypertrophy and
chronic inflammation.
• Vascular obstruction is also responsible for activating coagulation, which is caused
by an increase in pulmonary pressure and endothelium injuries.
• Pulmonary hypertension increases pulmonary venous pressure, which harms the left
side of the heart by increasing pressure in the left heart ventricle (Humbert, 2010).
• Pulmonary arteries also gain high pressure due to excessive stress which results in
causing injuries to the alveolar-capillary wall and edema.
• Pulmonary hypertension can be associated with gene mutation encoding bone
morphogenetic protein receptor type II, HIV infection and heart disease.
• In patients with high Pulmonary hypertension, high level of pro-inflammatory
cytokines like interleukin I, interleukin 6 and macrophage inflammatory protein are
found.
• Circulating autoantibodies are also found in the peripheral blood of the Pulmonary
hypertension patient.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Pharmacology
• Iloprost is being used for improving the flow of blood
who faces problems due to bad circulation.
• The drug works by widening the smaller blood
vessels and increases the flow of blood through them
(Heresi, 2010).
• It widens and relaxes the blood vessels in the lungs
and decreases the pulmonary pressure of blood in
order to improve its function.
• The decrease in the pressure of blood in the lungs
results in the ability to become more active.
• I-neb delivery system is a decision which is used for
administrating Iloprost.
• Iloprost is being used for improving the flow of blood
who faces problems due to bad circulation.
• The drug works by widening the smaller blood
vessels and increases the flow of blood through them
(Heresi, 2010).
• It widens and relaxes the blood vessels in the lungs
and decreases the pulmonary pressure of blood in
order to improve its function.
• The decrease in the pressure of blood in the lungs
results in the ability to become more active.
• I-neb delivery system is a decision which is used for
administrating Iloprost.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Pharmacodynamics and
Mechanism of Action
• Iloprost is considered to be the synthetic analog of the
prostacyclin PG12.
• Iloprost dilates pulmonary and systemic arterial vascular
beds.
• It affects the platelet aggregation but is not known the
relevance of the impact on the pulmonary hypertension
treatment (McLaughlin, Shah, Souza & Humbert, 2018).
• The diastereoisomers of the iloprost differ in the potency in
dilating the vessels of blood with 4S isomer is more potent
substantially than 4R isomer.
• Iloprost is considered to be the second generation analog
structural of prostacyclin with about ten greater fold
potency in comparison to the first generation stable analogs.
Mechanism of Action
• Iloprost is considered to be the synthetic analog of the
prostacyclin PG12.
• Iloprost dilates pulmonary and systemic arterial vascular
beds.
• It affects the platelet aggregation but is not known the
relevance of the impact on the pulmonary hypertension
treatment (McLaughlin, Shah, Souza & Humbert, 2018).
• The diastereoisomers of the iloprost differ in the potency in
dilating the vessels of blood with 4S isomer is more potent
substantially than 4R isomer.
• Iloprost is considered to be the second generation analog
structural of prostacyclin with about ten greater fold
potency in comparison to the first generation stable analogs.
Pharmacokinetics of iloprost in
pulmonary hypertension
• Inhalation of iloprost is an effective therapy for
pulmonary hypertension but has certain side effects.
• Inhaling iloprost decreases pulmonary vascular
resistance and pulmonary artery pressure. However,
systemic arterial pressure remains the same (Montani
et al., 2013).
• A standard dose of iloprost induces pharmacodynamic
and pharmacokinetic responses.
• The nebulizers use the various technologies to
increase alveolar targeting, Ventstream, and HaloLite.
Measurements are done using swan-ganz catheter
and by determining the arterial iloprost plasma level.
pulmonary hypertension
• Inhalation of iloprost is an effective therapy for
pulmonary hypertension but has certain side effects.
• Inhaling iloprost decreases pulmonary vascular
resistance and pulmonary artery pressure. However,
systemic arterial pressure remains the same (Montani
et al., 2013).
• A standard dose of iloprost induces pharmacodynamic
and pharmacokinetic responses.
• The nebulizers use the various technologies to
increase alveolar targeting, Ventstream, and HaloLite.
Measurements are done using swan-ganz catheter
and by determining the arterial iloprost plasma level.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Route of administration
• Iloprost intravenously administered has the
linear pharmacokinetics more than the dose
ranges from 1 to 3 ng/kg/min.
• Iloprost half-life is from 20 to 30 minutes
(Heresi, 2010).
• Iloprost inhalation (5mcg) by the patient can
lead to iloprost peak levels of serum of 150
pg/m.
• Iloprost was not detectable generally in the
plasma thirty to one hour after inhalation.
• Iloprost intravenously administered has the
linear pharmacokinetics more than the dose
ranges from 1 to 3 ng/kg/min.
• Iloprost half-life is from 20 to 30 minutes
(Heresi, 2010).
• Iloprost inhalation (5mcg) by the patient can
lead to iloprost peak levels of serum of 150
pg/m.
• Iloprost was not detectable generally in the
plasma thirty to one hour after inhalation.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Indications and contraindications
• Iloprost is considered to be a useful drug used
for the treatment of the patient suffering from
pulmonary arterial hypertension.
• The conditions that need to be contradicted
with Iloprost are abnormally low blood
pressure, fluid in lungs, bronchospasm, liver
disease, and chronic lung disease (Humbert,
2010).
• The restrictions on contraindicated populations,
co-administration and more obstruct the use of
the drug.
• Iloprost is considered to be a useful drug used
for the treatment of the patient suffering from
pulmonary arterial hypertension.
• The conditions that need to be contradicted
with Iloprost are abnormally low blood
pressure, fluid in lungs, bronchospasm, liver
disease, and chronic lung disease (Humbert,
2010).
• The restrictions on contraindicated populations,
co-administration and more obstruct the use of
the drug.
Precautions and side effects of
iloprost
• Inhaling of iloprost causes congestive heart failure, chest
pain, supraventricular tachycardia, dyspnea, peripheral
edema, and kidney failure.
• Bronchospasm and wheezing are observed in patients
with hyperreactive airways (McGoon et al., 2013).
• Organs like eyes and skin should not come in contact with
iloprost. Oral ingestion of iloprost should be avoided.
• Iloprost cannot be administered in patients with systolic
blood pressure.
• If pulmonary edema occurs while administering iloprost,
the treatment should be stopped immediately as this can
be a sign of pulmonary venous hypertension.
iloprost
• Inhaling of iloprost causes congestive heart failure, chest
pain, supraventricular tachycardia, dyspnea, peripheral
edema, and kidney failure.
• Bronchospasm and wheezing are observed in patients
with hyperreactive airways (McGoon et al., 2013).
• Organs like eyes and skin should not come in contact with
iloprost. Oral ingestion of iloprost should be avoided.
• Iloprost cannot be administered in patients with systolic
blood pressure.
• If pulmonary edema occurs while administering iloprost,
the treatment should be stopped immediately as this can
be a sign of pulmonary venous hypertension.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Relevance to practice
• The nurses should gain information on the
pathophysiology and physiology of
pulmonary arterial hypertension.
• The nurses will be able to determine and
evaluate indications and symptoms
(McLaughlin, Shah, Souza & Humbert,
2018).
• The registered nurses should take the
responsibility of carrying out the
medication process.
• The nurses should gain information on the
pathophysiology and physiology of
pulmonary arterial hypertension.
• The nurses will be able to determine and
evaluate indications and symptoms
(McLaughlin, Shah, Souza & Humbert,
2018).
• The registered nurses should take the
responsibility of carrying out the
medication process.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Conclusion and other
consideration
• The early detection of pulmonary arterial
hypertension will be very much useful for
healthcare professionals.
• There are many drugs that can be used
for providing treatment to the patient
suffering from the disease (Montani et al.,
2013).
• Healthcare professionals should
determine the benefits and side effects of
drugs.
consideration
• The early detection of pulmonary arterial
hypertension will be very much useful for
healthcare professionals.
• There are many drugs that can be used
for providing treatment to the patient
suffering from the disease (Montani et al.,
2013).
• Healthcare professionals should
determine the benefits and side effects of
drugs.
References
Heresi, G. (2010). Clinical perspective: biomarkers in pulmonary arterial
hypertension. International Journal Of Clinical Practice, 65, 5-7. doi:
10.1111/j.1742-1241.2010.02598.x
Humbert, M. (2010). Pulmonary arterial hypertension and chronic
thromboembolic pulmonary hypertension: pathophysiology. European
Respiratory Review, 19(115), 59-63. doi: 10.1183/09059180.00007309
McGoon, M., Benza, R., Escribano-Subias, P., Jiang, X., Miller, D., &
Peacock, A. et al. (2013). Pulmonary Arterial Hypertension. Retrieved
from http://www.onlinejacc.org/content/62/25_Supplement/D51.full
McLaughlin, V., Shah, S., Souza, R., & Humbert, M. (2018). Management
of Pulmonary Arterial Hypertension. Retrieved from
http://www.onlinejacc.org/content/65/18/1976.full
Montani, D., Günther, S., Dorfmüller, P., Perros, F., Girerd, B., & Garcia, G.
et al. (2013). Pulmonary arterial hypertension. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3750932/
Heresi, G. (2010). Clinical perspective: biomarkers in pulmonary arterial
hypertension. International Journal Of Clinical Practice, 65, 5-7. doi:
10.1111/j.1742-1241.2010.02598.x
Humbert, M. (2010). Pulmonary arterial hypertension and chronic
thromboembolic pulmonary hypertension: pathophysiology. European
Respiratory Review, 19(115), 59-63. doi: 10.1183/09059180.00007309
McGoon, M., Benza, R., Escribano-Subias, P., Jiang, X., Miller, D., &
Peacock, A. et al. (2013). Pulmonary Arterial Hypertension. Retrieved
from http://www.onlinejacc.org/content/62/25_Supplement/D51.full
McLaughlin, V., Shah, S., Souza, R., & Humbert, M. (2018). Management
of Pulmonary Arterial Hypertension. Retrieved from
http://www.onlinejacc.org/content/65/18/1976.full
Montani, D., Günther, S., Dorfmüller, P., Perros, F., Girerd, B., & Garcia, G.
et al. (2013). Pulmonary arterial hypertension. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3750932/
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





