Quality Improvement Report: Aventura Hospital's Readmission Strategy
VerifiedAdded on 2023/05/30
|12
|2729
|258
Report
AI Summary
This report assesses the healthcare services provided by Aventura Hospital and Medical Centre, comparing its service quality with other state-level organizations like Bartow Regional Medical Center and Bethesda Hospital East, focusing on readmission rates. The analysis reveals that Aventura Hospital's readmission rate is higher than its competitors and the national average, primarily due to a poor patient discharge management plan. A fishbone analysis identifies key issues such as lack of post-discharge management tools, poor communication, and insufficient workforce training. To address these gaps, a development plan is proposed, emphasizing the need for an effective discharge management system, caregiver support, improved communication skills for staff, and regular patient monitoring. The implementation and control phase includes using Run and Control charts to measure the success rate by monitoring patient readmissions within 30 days of discharge. To ensure the successful adoption of these changes, the report suggests strategies for promoting the new plan and gaining support from the workforce, including creating a shared vision, fostering effective communication, sharing values, and setting short-term goals to maintain motivation and collaboration.

Running head: QUALITY IMPROVEMENT
Quality comparison and Improvement
Name of the Student
Name of the University
Author note
Quality comparison and Improvement
Name of the Student
Name of the University
Author note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2QUALITY IMPROVEMENT
Introduction
Quality improvement is a systematic approach in healthcare industry that allows any
organization to increase the efficiency of their services to a sustainable, satisfactory and
profitable level. The process of improvement often consists of several essential phase namely
gap analysis; implement theory of knowledge, development planning, implement changes,
monitoring and evaluation (Kaplan et al., 2012). The aims of any improvement in healthcare
service are safe structure to avoid any injuries of patients, Timing that ensures the punctuality of
the process, Effectiveness that provides more stable outcomes, Efficiency for sustainable
development, Equitability to ensure unbiased service providing and Patient Cantered approach to
prioritize patient’s perspectives.
In this paper the healthcare service provided by the organization named Aventura
Hospital and Medical Centre will be assessed to find the scope for improvement. For this the
service quality will be compared with other state level organizations and regional as well as
national average records. For this comparing the chosen organizations are Bartow Regional
Medical Center and Bethesda Hospital East. All these three institutes are situated in the state of
Florida. In this paper the development plan will be also developed with the discussion of
implementation process. Furthermore, the strategy to develop adequate support and promotional
scope for this improvement will be discussed.
Essentiality of Rate of readmission
Returning to the hospital after discharging the patient from the hospital as an unplanned
care disrupts the regular life and wellbeing of the patients. This type of repeated readmission also
increases the risk of harmful events such as healthcare associate infection. Apart from that this
Introduction
Quality improvement is a systematic approach in healthcare industry that allows any
organization to increase the efficiency of their services to a sustainable, satisfactory and
profitable level. The process of improvement often consists of several essential phase namely
gap analysis; implement theory of knowledge, development planning, implement changes,
monitoring and evaluation (Kaplan et al., 2012). The aims of any improvement in healthcare
service are safe structure to avoid any injuries of patients, Timing that ensures the punctuality of
the process, Effectiveness that provides more stable outcomes, Efficiency for sustainable
development, Equitability to ensure unbiased service providing and Patient Cantered approach to
prioritize patient’s perspectives.
In this paper the healthcare service provided by the organization named Aventura
Hospital and Medical Centre will be assessed to find the scope for improvement. For this the
service quality will be compared with other state level organizations and regional as well as
national average records. For this comparing the chosen organizations are Bartow Regional
Medical Center and Bethesda Hospital East. All these three institutes are situated in the state of
Florida. In this paper the development plan will be also developed with the discussion of
implementation process. Furthermore, the strategy to develop adequate support and promotional
scope for this improvement will be discussed.
Essentiality of Rate of readmission
Returning to the hospital after discharging the patient from the hospital as an unplanned
care disrupts the regular life and wellbeing of the patients. This type of repeated readmission also
increases the risk of harmful events such as healthcare associate infection. Apart from that this
3QUALITY IMPROVEMENT
repeated procedure also cost extra money from the patients and extra energy from the healthcare
workforce (Al-Abri & Al-Balushi, 2014). The rate of readmission also directly emphasize the
quality of the healthcare system and the communication level with patient care integrity. In some
cases after reappearing the symptoms of treated problems the patients go to another healthcare
organization for having better experience. In these cases, the healthcare organization even does
not have proper records of rate of readmission for the patients with COPD, Heart issue,
Pneumonia, Stroke, CABG surgery, hip or knee replacement and other issues (Unützer et al.,
2012). Many healthcare measures can be utilized to monitor and keep records of the rate of
readmission for patient after discharge from the healthcare facilities. In most of the hospitals and
healthcare organizations the returning of the patients within 30 days after previous discharge are
counted. Apart from that for chronic diseases the rate of readmission also helps the healthcare
professionals to formulate the existing condition of patients and to find their potential immunity.
Gap in healthcare practice
After comparing the records of chosen three healthcare organizations namely Aventura
Hospital and Medical Centre, Bartow Regional Medical Center and Bethesda Hospital East it has
been found that in Aventura Hospital the rate of readmission is higher than the other two
competitors. In this hospital the rate of readmission after discharge from hospital is worse than
the national rate (13%) (medicare.gov., 2018). At the same time, where Bethesda Hospital East
has lower rate in after hi[ or knee replacement, Aventura Hospital remains at the national rate of
readmission ration for this orthopedic procedure. In colonoscopy Bartow Regional Medical has
very low rate of readmission, however Aventura Hospital remains same to the national rate in
this case as well. In case of Heart attack, hospital return days for heart attack patients is higher
than the average rate for 100 discharge in Aventura Hospital. However, both of competitors
repeated procedure also cost extra money from the patients and extra energy from the healthcare
workforce (Al-Abri & Al-Balushi, 2014). The rate of readmission also directly emphasize the
quality of the healthcare system and the communication level with patient care integrity. In some
cases after reappearing the symptoms of treated problems the patients go to another healthcare
organization for having better experience. In these cases, the healthcare organization even does
not have proper records of rate of readmission for the patients with COPD, Heart issue,
Pneumonia, Stroke, CABG surgery, hip or knee replacement and other issues (Unützer et al.,
2012). Many healthcare measures can be utilized to monitor and keep records of the rate of
readmission for patient after discharge from the healthcare facilities. In most of the hospitals and
healthcare organizations the returning of the patients within 30 days after previous discharge are
counted. Apart from that for chronic diseases the rate of readmission also helps the healthcare
professionals to formulate the existing condition of patients and to find their potential immunity.
Gap in healthcare practice
After comparing the records of chosen three healthcare organizations namely Aventura
Hospital and Medical Centre, Bartow Regional Medical Center and Bethesda Hospital East it has
been found that in Aventura Hospital the rate of readmission is higher than the other two
competitors. In this hospital the rate of readmission after discharge from hospital is worse than
the national rate (13%) (medicare.gov., 2018). At the same time, where Bethesda Hospital East
has lower rate in after hi[ or knee replacement, Aventura Hospital remains at the national rate of
readmission ration for this orthopedic procedure. In colonoscopy Bartow Regional Medical has
very low rate of readmission, however Aventura Hospital remains same to the national rate in
this case as well. In case of Heart attack, hospital return days for heart attack patients is higher
than the average rate for 100 discharge in Aventura Hospital. However, both of competitors
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
4QUALITY IMPROVEMENT
Materials Method Workforce
Measures Environment Investment
High
Readmission
Rate
Lack post
discharge
Management tool
Lack of advance e-
health monitoring
and evaluation
Poor
communication
Lack of information
providing for post
discharge period
Lack of
knowledge in
discharge planning
and
Poor performance
monitoring system
Lack of safety
measures for
patient
engagement
Lack of
cleanliness
Poor sound
protection
system
Poor financial
investment for
workforce
development
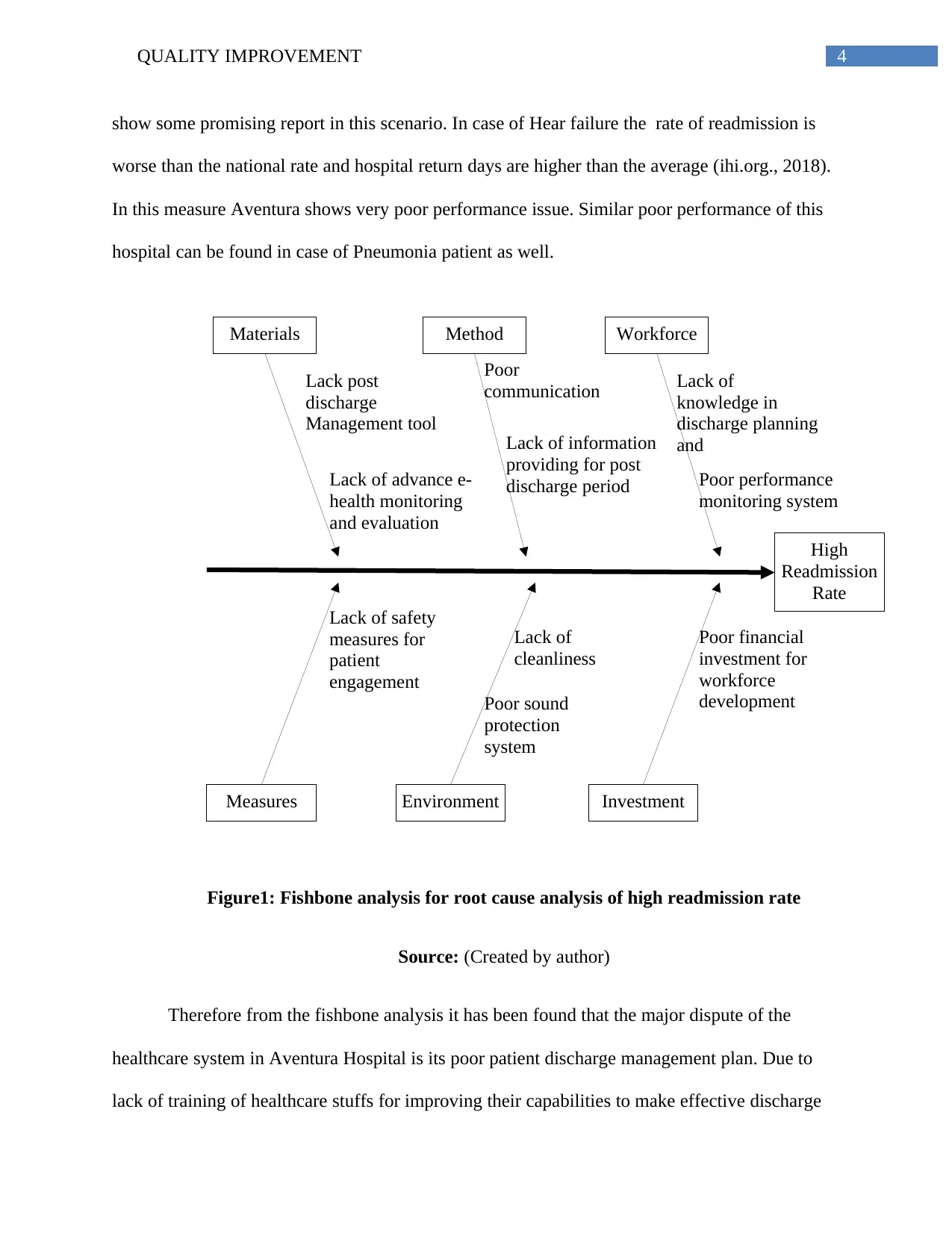
show some promising report in this scenario. In case of Hear failure the rate of readmission is
worse than the national rate and hospital return days are higher than the average (ihi.org., 2018).
In this measure Aventura shows very poor performance issue. Similar poor performance of this
hospital can be found in case of Pneumonia patient as well.
Figure1: Fishbone analysis for root cause analysis of high readmission rate
Source: (Created by author)
Therefore from the fishbone analysis it has been found that the major dispute of the
healthcare system in Aventura Hospital is its poor patient discharge management plan. Due to
lack of training of healthcare stuffs for improving their capabilities to make effective discharge
Materials Method Workforce
Measures Environment Investment
High
Readmission
Rate
Lack post
discharge
Management tool
Lack of advance e-
health monitoring
and evaluation
Poor
communication
Lack of information
providing for post
discharge period
Lack of
knowledge in
discharge planning
and
Poor performance
monitoring system
Lack of safety
measures for
patient
engagement
Lack of
cleanliness
Poor sound
protection
system
Poor financial
investment for
workforce
development
show some promising report in this scenario. In case of Hear failure the rate of readmission is
worse than the national rate and hospital return days are higher than the average (ihi.org., 2018).
In this measure Aventura shows very poor performance issue. Similar poor performance of this
hospital can be found in case of Pneumonia patient as well.
Figure1: Fishbone analysis for root cause analysis of high readmission rate
Source: (Created by author)
Therefore from the fishbone analysis it has been found that the major dispute of the
healthcare system in Aventura Hospital is its poor patient discharge management plan. Due to
lack of training of healthcare stuffs for improving their capabilities to make effective discharge
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5QUALITY IMPROVEMENT
management plan, the patients are unable to maintain a post treatment guideline for a sustainable
health (Kripalani et al., 2014). Along with that, the patients reviews also suggest that this
hospital has a poor communication system that reduce the potentiality of patient engagement
through communicational and emotional interaction.
Development plan
In order to improve the existing situation Aventura Hospital has to develop appropriate
discharge management system. The aim of this development plan is to develop a effective and
sustainable discharge management practice that can reduce the rate or readmission significantly
Requirements
The following requirements will needed for the holistic development of effecting discharge
management system:
Activity Reason Deadline
Developing a post discharge
checklist
Supporting the caregiver to
execute necessary activities
required for discharge
management
Next 1 moth
Training and development Improving the communication
skill of stuff and also increasing
patient engagement
Next 6 months
Developing post discharge
monitoring plan
To monitor if the patient is
maintaining proper healthy
procedure regularly during the
recovery time in home
Next 3 months
Calling patient in every 5 days for
next 2 months after discharge
Keeping track of home recovery
update of patients
Next 1 months
management plan, the patients are unable to maintain a post treatment guideline for a sustainable
health (Kripalani et al., 2014). Along with that, the patients reviews also suggest that this
hospital has a poor communication system that reduce the potentiality of patient engagement
through communicational and emotional interaction.
Development plan
In order to improve the existing situation Aventura Hospital has to develop appropriate
discharge management system. The aim of this development plan is to develop a effective and
sustainable discharge management practice that can reduce the rate or readmission significantly
Requirements
The following requirements will needed for the holistic development of effecting discharge
management system:
Activity Reason Deadline
Developing a post discharge
checklist
Supporting the caregiver to
execute necessary activities
required for discharge
management
Next 1 moth
Training and development Improving the communication
skill of stuff and also increasing
patient engagement
Next 6 months
Developing post discharge
monitoring plan
To monitor if the patient is
maintaining proper healthy
procedure regularly during the
recovery time in home
Next 3 months
Calling patient in every 5 days for
next 2 months after discharge
Keeping track of home recovery
update of patients
Next 1 months
6QUALITY IMPROVEMENT
Providing appropriate chart to the
patient during the discharge from
the hospital explaining
To provide all the necessary
measures during home recovery
phase
Next 4 months
Stakeholders and responsibilities
Stakeholder Responsibilities
Human Resource management Providing training to the healthcare stuffs regarding
discharge management plan
Caregivers and healthcare
professionals
Maintaining the newly imposed discharge management
system according to the guidance
Patients Showing cooperative attitude with the caregivers through
maintaining the home recovery guidelines appropriately
Consumer communication Maintain strong communication with the patients and
developing records as per the patients feedbacks
Throughout the development phase all stakeholders should maintain a cooperative and
collaborative relationship with each other to maintain the workflow and information interiority
within the team. Apart from that, effective monitoring system is also essential to ensure the
compliance of medical and non medical workforce (Nguyen et al., 2018). The organization
should also develop an appropriate financial plan to implement all this activities for discharge
management system.
Implementation and control
After planning the activities for new patient discharge management system appropriate
control management will be highly essential. In this phase the management has to identify an
appropriate measurement system to control the workflow towards the most efficiency. Many
Providing appropriate chart to the
patient during the discharge from
the hospital explaining
To provide all the necessary
measures during home recovery
phase
Next 4 months
Stakeholders and responsibilities
Stakeholder Responsibilities
Human Resource management Providing training to the healthcare stuffs regarding
discharge management plan
Caregivers and healthcare
professionals
Maintaining the newly imposed discharge management
system according to the guidance
Patients Showing cooperative attitude with the caregivers through
maintaining the home recovery guidelines appropriately
Consumer communication Maintain strong communication with the patients and
developing records as per the patients feedbacks
Throughout the development phase all stakeholders should maintain a cooperative and
collaborative relationship with each other to maintain the workflow and information interiority
within the team. Apart from that, effective monitoring system is also essential to ensure the
compliance of medical and non medical workforce (Nguyen et al., 2018). The organization
should also develop an appropriate financial plan to implement all this activities for discharge
management system.
Implementation and control
After planning the activities for new patient discharge management system appropriate
control management will be highly essential. In this phase the management has to identify an
appropriate measurement system to control the workflow towards the most efficiency. Many
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
7QUALITY IMPROVEMENT
control methods are available for the measuring system including Run Chart and control chart,
Histogram, Pareto chart and scatter plot. In this implementation the management has to measure
the success rate by measuring the rate of readmission of the patients within the next 30 days after
receiving the discharge paper from the Hospital Authority (Dixon-Woods, McNicol & Martin,
2012). Therefore, in this case the measurement system has to handle a continuous measurement
system to control the implementation effectiveness. Therefore the most effective control method
will be the Run and Control chart.
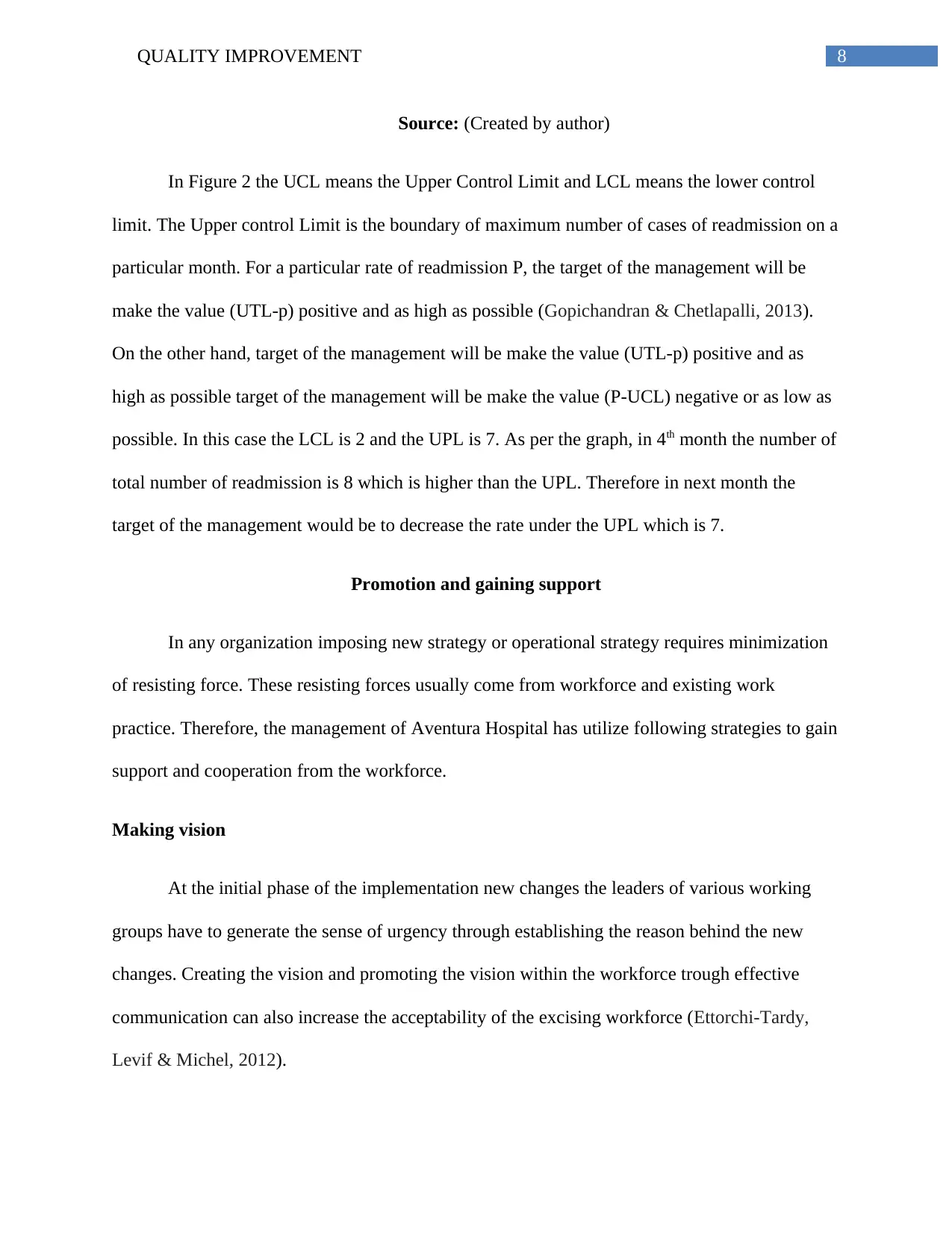
In Run control char the management has to keep the record of each discharge and the
readmission of the patients. Therefore in this control char the X axis will imply the period of
reviewing records and the Y axis will imply the number of patient readmission within next 30
days after the executing the imposed discharge management process. The figure 2 will be a
perfect example of control chart of sampling.
1st
month 4th
month 7th
month 10th
month 13th
month 16th
month 19th
month
0
1
2
3
4
5
6
7
8
9
6
8
4
7
5
7
4 Number of Readmission
Figure 2: Control Chart for Rate of Readmission
UCL
LCL
control methods are available for the measuring system including Run Chart and control chart,
Histogram, Pareto chart and scatter plot. In this implementation the management has to measure
the success rate by measuring the rate of readmission of the patients within the next 30 days after
receiving the discharge paper from the Hospital Authority (Dixon-Woods, McNicol & Martin,
2012). Therefore, in this case the measurement system has to handle a continuous measurement
system to control the implementation effectiveness. Therefore the most effective control method
will be the Run and Control chart.
In Run control char the management has to keep the record of each discharge and the
readmission of the patients. Therefore in this control char the X axis will imply the period of
reviewing records and the Y axis will imply the number of patient readmission within next 30
days after the executing the imposed discharge management process. The figure 2 will be a
perfect example of control chart of sampling.
1st
month 4th
month 7th
month 10th
month 13th
month 16th
month 19th
month
0
1
2
3
4
5
6
7
8
9
6
8
4
7
5
7
4 Number of Readmission
Figure 2: Control Chart for Rate of Readmission
UCL
LCL
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
8QUALITY IMPROVEMENT
Source: (Created by author)
In Figure 2 the UCL means the Upper Control Limit and LCL means the lower control
limit. The Upper control Limit is the boundary of maximum number of cases of readmission on a
particular month. For a particular rate of readmission P, the target of the management will be
make the value (UTL-p) positive and as high as possible (Gopichandran & Chetlapalli, 2013).
On the other hand, target of the management will be make the value (UTL-p) positive and as
high as possible target of the management will be make the value (P-UCL) negative or as low as
possible. In this case the LCL is 2 and the UPL is 7. As per the graph, in 4th month the number of
total number of readmission is 8 which is higher than the UPL. Therefore in next month the
target of the management would be to decrease the rate under the UPL which is 7.
Promotion and gaining support
In any organization imposing new strategy or operational strategy requires minimization
of resisting force. These resisting forces usually come from workforce and existing work
practice. Therefore, the management of Aventura Hospital has utilize following strategies to gain
support and cooperation from the workforce.
Making vision
At the initial phase of the implementation new changes the leaders of various working
groups have to generate the sense of urgency through establishing the reason behind the new
changes. Creating the vision and promoting the vision within the workforce trough effective
communication can also increase the acceptability of the excising workforce (Ettorchi-Tardy,
Levif & Michel, 2012).
Source: (Created by author)
In Figure 2 the UCL means the Upper Control Limit and LCL means the lower control
limit. The Upper control Limit is the boundary of maximum number of cases of readmission on a
particular month. For a particular rate of readmission P, the target of the management will be
make the value (UTL-p) positive and as high as possible (Gopichandran & Chetlapalli, 2013).
On the other hand, target of the management will be make the value (UTL-p) positive and as
high as possible target of the management will be make the value (P-UCL) negative or as low as
possible. In this case the LCL is 2 and the UPL is 7. As per the graph, in 4th month the number of
total number of readmission is 8 which is higher than the UPL. Therefore in next month the
target of the management would be to decrease the rate under the UPL which is 7.
Promotion and gaining support
In any organization imposing new strategy or operational strategy requires minimization
of resisting force. These resisting forces usually come from workforce and existing work
practice. Therefore, the management of Aventura Hospital has utilize following strategies to gain
support and cooperation from the workforce.
Making vision
At the initial phase of the implementation new changes the leaders of various working
groups have to generate the sense of urgency through establishing the reason behind the new
changes. Creating the vision and promoting the vision within the workforce trough effective
communication can also increase the acceptability of the excising workforce (Ettorchi-Tardy,
Levif & Michel, 2012).
9QUALITY IMPROVEMENT
Effective communication
Communication is the key of any change management plan where all the stuffs can
maintain a integrity and healthy relationship through friendly and cooperative relationship. In
order to ensure the effective communication the management of Aventura Hospital should also
develop and effective communication plan and all the necessary arrangement.
Shared value
Sharing value is another essential aspect of the support development process. By sharing
value the workforce of any organization can grow collectively with collaborative interaction
within various departments (Dixon-Woods, McNicol & Martin, 2012). Sharing value also
implies an ethic that says every stuff of a organization should share their knowledge and
experience with the team member to help them developing effective mitigation plan.
Short term accomplishment
Human mind can focus more on short time goal consistently than a long time
achievement with lengthy procedures. Therefore, creating short time accomplishment by
effective benchmarking system will allow the healthcare workforce to be motivated
(Gopichandran & Chetlapalli, 2013). After each achievement the workers can focus on the next
short time achievement with more dedication.
Conclusion:
From the above discussion it can be said that, quality improvement is a systematic
approach in healthcare industry that allows any organization to increase the efficiency of their
services to a sustainable, satisfactory and profitable level. It has been also found that returning to
Effective communication
Communication is the key of any change management plan where all the stuffs can
maintain a integrity and healthy relationship through friendly and cooperative relationship. In
order to ensure the effective communication the management of Aventura Hospital should also
develop and effective communication plan and all the necessary arrangement.
Shared value
Sharing value is another essential aspect of the support development process. By sharing
value the workforce of any organization can grow collectively with collaborative interaction
within various departments (Dixon-Woods, McNicol & Martin, 2012). Sharing value also
implies an ethic that says every stuff of a organization should share their knowledge and
experience with the team member to help them developing effective mitigation plan.
Short term accomplishment
Human mind can focus more on short time goal consistently than a long time
achievement with lengthy procedures. Therefore, creating short time accomplishment by
effective benchmarking system will allow the healthcare workforce to be motivated
(Gopichandran & Chetlapalli, 2013). After each achievement the workers can focus on the next
short time achievement with more dedication.
Conclusion:
From the above discussion it can be said that, quality improvement is a systematic
approach in healthcare industry that allows any organization to increase the efficiency of their
services to a sustainable, satisfactory and profitable level. It has been also found that returning to
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
10QUALITY IMPROVEMENT
the hospital after discharging the patient from the hospital as an unplanned care disrupts the
regular life and wellbeing of the patients. According the to record analysis and comparison it has
been found that the major dispute of the healthcare system in Aventura Hospital is its poor
patient discharge management plan. Due to lack of training of healthcare stuffs for improving
their capabilities to make effective discharge management plan, the patients are unable to
maintain a post treatment guideline for a sustainable health.
From the performance improvement development plan it can be concluded that
throughout the development phase all stakeholders should maintain a cooperative and
collaborative relationship with each other to maintain the workflow and information interiority
within the team. It has been found that, in implementation phase, through Run control char the
management has to keep the record of each discharge and the readmission of the patients.
Making vision, effective communication, Sharing value and Short time accomplishment are the
most effective strategy to gain the support from the healthcare workforce.
the hospital after discharging the patient from the hospital as an unplanned care disrupts the
regular life and wellbeing of the patients. According the to record analysis and comparison it has
been found that the major dispute of the healthcare system in Aventura Hospital is its poor
patient discharge management plan. Due to lack of training of healthcare stuffs for improving
their capabilities to make effective discharge management plan, the patients are unable to
maintain a post treatment guideline for a sustainable health.
From the performance improvement development plan it can be concluded that
throughout the development phase all stakeholders should maintain a cooperative and
collaborative relationship with each other to maintain the workflow and information interiority
within the team. It has been found that, in implementation phase, through Run control char the
management has to keep the record of each discharge and the readmission of the patients.
Making vision, effective communication, Sharing value and Short time accomplishment are the
most effective strategy to gain the support from the healthcare workforce.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
11QUALITY IMPROVEMENT
Reference
Al-Abri, R., & Al-Balushi, A. (2014). Patient satisfaction survey as a tool towards quality
improvement. Oman medical journal, 29(1), 3. doi: 10.5001/omj.2014.02
Dixon-Woods, M., McNicol, S., & Martin, G. (2012). Ten challenges in improving quality in
healthcare: lessons from the Health Foundation's programme evaluations and relevant
literature. BMJ Qual Saf, bmjqs-2011., doi: 10.1136/bmjqs-2011-000760
Ettorchi-Tardy, A., Levif, M., & Michel, P. (2012). Benchmarking: a method for continuous
quality improvement in health. Healthcare policy, 7(4), e101. Retrieved from:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3359088/
Gopichandran, V., & Chetlapalli, S. K. (2013). Factors influencing trust in doctors: a community
segmentation strategy for quality improvement in healthcare. BMJ open, 3(12), e004115.
ihi.org. (2018). Tools. Retrieved from http://www.ihi.org/resources/Pages/Tools/default.aspx
Kaplan, H. C., Provost, L. P., Froehle, C. M., & Margolis, P. A. (2012). The Model for
Understanding Success in Quality (MUSIQ): building a theory of context in healthcare
quality improvement. BMJ Qual Saf, 21(1), 13-20., doi: 10.1136/bmjqs-2011-000010
Kripalani, S., Theobald, C. N., Anctil, B., & Vasilevskis, E. E. (2014). Reducing hospital
readmission rates: current strategies and future directions. Annual review of medicine, 65,
471-485. doi: 10.1146/annurev-med-022613-090415
medicare.gov. (2018). Medicare Hospital Comparison. Retrieved from
https://www.medicare.gov/hospitalcompare/compare.html#cmprTab=1&cmprID=100131
Reference
Al-Abri, R., & Al-Balushi, A. (2014). Patient satisfaction survey as a tool towards quality
improvement. Oman medical journal, 29(1), 3. doi: 10.5001/omj.2014.02
Dixon-Woods, M., McNicol, S., & Martin, G. (2012). Ten challenges in improving quality in
healthcare: lessons from the Health Foundation's programme evaluations and relevant
literature. BMJ Qual Saf, bmjqs-2011., doi: 10.1136/bmjqs-2011-000760
Ettorchi-Tardy, A., Levif, M., & Michel, P. (2012). Benchmarking: a method for continuous
quality improvement in health. Healthcare policy, 7(4), e101. Retrieved from:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3359088/
Gopichandran, V., & Chetlapalli, S. K. (2013). Factors influencing trust in doctors: a community
segmentation strategy for quality improvement in healthcare. BMJ open, 3(12), e004115.
ihi.org. (2018). Tools. Retrieved from http://www.ihi.org/resources/Pages/Tools/default.aspx
Kaplan, H. C., Provost, L. P., Froehle, C. M., & Margolis, P. A. (2012). The Model for
Understanding Success in Quality (MUSIQ): building a theory of context in healthcare
quality improvement. BMJ Qual Saf, 21(1), 13-20., doi: 10.1136/bmjqs-2011-000010
Kripalani, S., Theobald, C. N., Anctil, B., & Vasilevskis, E. E. (2014). Reducing hospital
readmission rates: current strategies and future directions. Annual review of medicine, 65,
471-485. doi: 10.1146/annurev-med-022613-090415
medicare.gov. (2018). Medicare Hospital Comparison. Retrieved from
https://www.medicare.gov/hospitalcompare/compare.html#cmprTab=1&cmprID=100131
12QUALITY IMPROVEMENT
%2C100121%2C100002&cmprDist=0.0%2C0.0%2C0.0&stsltd=FL&dist=25&lat=0&ln
g=0&state=FL
Nadeem, E., Olin, S. S., Hill, L. C., Hoagwood, K. E., & Horwitz, S. M. (2013). Understanding
the components of quality improvement collaboratives: a systematic literature
review. The Milbank Quarterly, 91(2), 354-394. doi: 10.5001/omj.2014.02
Nguyen, J. T., Vakil, K., Adabag, S., Westanmo, A., Madlon-Kay, R., Ishani, A., ... & McFalls,
E. O. (2018). Hospital Readmission Rates Following AMI: Potential Interventions to
Improve Efficiency. Southern medical journal, 111(2), 93-97. doi: 10.1136/bmjopen-
2013-004115
Unützer, J., Chan, Y. F., Hafer, E., Knaster, J., Shields, A., Powers, D., & Veith, R. C. (2012).
Quality improvement with pay-for-performance incentives in integrated behavioral health
care. American Journal of Public Health, 102(6), e41-e45.,
doi: 10.2105/AJPH.2011.300555
%2C100121%2C100002&cmprDist=0.0%2C0.0%2C0.0&stsltd=FL&dist=25&lat=0&ln
g=0&state=FL
Nadeem, E., Olin, S. S., Hill, L. C., Hoagwood, K. E., & Horwitz, S. M. (2013). Understanding
the components of quality improvement collaboratives: a systematic literature
review. The Milbank Quarterly, 91(2), 354-394. doi: 10.5001/omj.2014.02
Nguyen, J. T., Vakil, K., Adabag, S., Westanmo, A., Madlon-Kay, R., Ishani, A., ... & McFalls,
E. O. (2018). Hospital Readmission Rates Following AMI: Potential Interventions to
Improve Efficiency. Southern medical journal, 111(2), 93-97. doi: 10.1136/bmjopen-
2013-004115
Unützer, J., Chan, Y. F., Hafer, E., Knaster, J., Shields, A., Powers, D., & Veith, R. C. (2012).
Quality improvement with pay-for-performance incentives in integrated behavioral health
care. American Journal of Public Health, 102(6), e41-e45.,
doi: 10.2105/AJPH.2011.300555
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





