Quality Management in Health: Analysis of Adverse Events and Systems
VerifiedAdded on 2021/04/16

Quality Management in Health
Author:
Course Name:
Institution:
Paraphrase This Document
Contents
Workbook Activity 1.......................................................................................................................4
Workbook Activity 2.......................................................................................................................7
Adverse Events............................................................................................................................7
Workbook Activity 3.......................................................................................................................8
Public Inquiries............................................................................................................................8
Workbook Activity 4.....................................................................................................................11
Workbook Activity 5.....................................................................................................................13
Domains of Quality – Effectiveness and Efficiency..................................................................13
Domains of Quality – Patient Centredness................................................................................14
Workbook Activity 6.....................................................................................................................15
References......................................................................................................................................18
Workbook Activity 1.
1.1 Compare and contrast the key features of the Deming, Juran and Ishikawa approaches to
quality management.
Deming, Juran and Ishakawa approaches agree that the sole purpose of organizations are to stay
in business resulting to stable communities and serving the needs of the community (Hackman
& Wageman, 1995). Their works do differ. First difference is in the impact that quality has in
organizations. Juran and Ishakawa believed that quality leads to cost reductions as compared to
poor workmanship. Deming believes that the production of quality goods and services will
merely affect the cost but it is important for the long term running of the business (Hackman &
Wageman, 1995). The other difference is related to the running of the organizations. Deming
and Juran believe that organizations are interdependent and that problems need to be sorted out
by members of the different functional teams. However, Ishakawa holds that cross functional
teams should not set the direction of the organisation but rather individual teams need to have
their own goals and objectives. According to Ishakawa organizations are less system-oriented
(Hackman & Wageman, 1995).
The structures of these approaches differ in that Deming’s approach is characterized by fourteen
points of management (Best & Neuhauser, 2005). Juran’s approach is composed of ten steps
for quality improvement. Another difference is that they all have different preferred analytical
tools. Deming is associated with the PDCA approach. PDCA stands for plan, do, check and act.
Juran worked with the Pareto principle that is used to identify main contributors to a problem.
Ishikawa is identified with the famously used fishbone diagram that assesses the root causes and
effects of a problem (Hackman & Wageman, 1995).
1.2 How do these approaches differ from quality control and quality assurance, activities
traditionally used in industry to ensure production quality?
Traditional activities focused on inspection that was carried out at the end of the process
(Berwick, 1993). This differs from Deming, Juran and Ishikawa approaches in that these
activities occur at every stage of the production process. They are continuous. Another difference
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
is that they seek to understand to underlying production processes while the traditional activities
are concerned with the outcomes. Problems in the traditional approaches were attributed to
inefficiency of the people. This is contrary to the new approaches that hold that problems arise
from poor job design, leadership failures or unclear purposes (Berwick, 1993).
1.3 The Toyota Total Production System (TPS) utilises a range of quality strategies attributable
to these and other quality ‘gurus’. What are the key elements of the system? How are they
integrated?
One main element is the avoidance and reduction of waste. This is achieved through the
production of only needed products which are of the best quality. This leads to a major reduction
in costs (Fritze, 2016). Other elements include; hejunka/product levelling, kaizen and
standardization. The other elements are kanban or just in time concept and autonomation or
jidoka (Fritze, 2016).
Standardization forms the base of the production process as it stipulates the materials, activities
and duration to be taken. The just in time concept ensures that the needed materials are available
at the needed time. This ensures a progressive process. As the process continues, hejunka allows
for its visualisation and identification of problems. This brings about autonomation which
ensures the problems are assessed and dealt with. Kaizen can be applied in every stage in order
to ensure that quality goods are produced. This brings out the overall waste avoidance and
reduction, cost reduction, quality goods and efficient personnel and process (Fritze, 2016).
1.4. Toyota has been widely regarded as a leader in quality management for decades and yet
since 2009 Toyota has been in serious trouble over quality control, issuing recall notices for
millions of vehicles. Explain possible reasons for this failure
First there was a change of focus from quality to growth. This made them to disregard safety and
meet the growth standard set in 1998 at 15% (Cole, 2011). Another reason could have been the
disbanding of the Customer First task force that was key in the regulation and maintenance of
quality of cars produced (Cole, 2011). This reflect that Toyota became more organization
oriented rather than customer oriented. There were conflicts between the management. This
could be attributed to the problem as Deming did relate poor leadership to being the cause of
Paraphrase This Document
problems (Best & Neuhauser, 2005). Another reason could be the influence of media which
propagated the issue to be more than it was. The more they reported on the recall and the quality
problems, the more the public’s perception changed making it hard for Toyota to recover (Cole,
2011).
1.5 From the readings provided:
a) What is health care quality?
Health care quality is the provision of good services that help in serving and meeting the needs
of the community bringing about both patient and provider satisfaction and a general well being
of the society (Luce, Bindman, & Lee, 1994). It is associated with increased quality of life,
reduced incidence and prevalence of diseases and decreased mortality.
b) Why do these authors consider quality improvement an important aspect of health service
management?
Quality improvement is important in health care as it is a vital aspect of the society as it deals
with life. Various reasons have been cited for quality improvement. First, Quality improvement
brings about an open and supportive culture that facilitates learning. This helps to build a
relationship that is characterized by trust, respect and cooperation. It also helps to bring about
transparency which ensures that quality services are provided. Another reason is that it ensures
integrated care in that it encourages multidisciplinary service provision. Custome/patient
participation is key in that it helps the organization to understand his/her needs. It is also
important as it brings about provider satisfaction in that it changes the view of one’s job to one
that has meaning and brings joy. It also facilitates growth of knowledge and skills through
medical education (Leape, et al., 2009).
c) what are the necessary conditions required for quality improvement?
There is a need for leaders to be part and parcel of the improvement action. This is due to the
effect and impact they have on organizations. Substantial investment is also needed in quality
improvement. The worry on cost shouldn’t be a hindrance as quality helps in the reduction of
costs. Respect of the healthcare workers is necessary as it ensure they are motivated and
committed to be part of quality improvement as is builds on trust and cooperation. For one to
understand the needs of the community/ customer there is need for open dialogue between the
producer and the customer. Theoretically grounded tools should be used during assessment so as
to ensure only factual information is collected and analysed. There is also need for organizations
that facilitate quality improvement. This signifies the structures and managerial approaches
should enable this action (Berwick, 1993).
Workbook Activity 2.
Adverse Events
2.1 What are adverse events?
Adverse events (AE) are defined as an injury or complication that is not intentional and causes
disability, death or longer hospital stay and is not caused by the disease of the patient but rather
health care management (de Vries, Ramrattan, Smorenburg, Gouma, & Boermeester,
2008).
2.2 Use the readings provided to describe the commonest types of adverse events. Why do you
think there is variation across the studies in the types of adverse events described?
Adverse effects (AEs) can be divided into operative and non-operative. Examples of operative
AEs are wound infection, technical complications and surgical failure. Drug complications,
diagnostic and therapeutic mishap and procedure examples of non operative AEs (Brennan, et
al., 1991). These complications are mainly attributed to negligence which is care that is below
the expected standard (Brennan, et al., 1991)
The difference in the epidemiology of AEs could be attributed to a number of reasons. First,
there are methodological differences whereby some AEs are included in one study and excluded
in another. Another methodological difference is the use of different data collection procedures.
There is also definition difference leading to the underestimation of AEs. This was seen in the
Harvard study. Insufficient information on outpatient cases leads to the underestimation of AEs.
The studies were carried out at different times. Learning and interventions may have been
implemented and bring about variation.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
2.3 Are all adverse events preventable? Explain your answer and provide examples of
preventable and non preventable adverse events.
Majority of the effects are preventable as they occur as a result of negligence, physician error
and cognitive error. Stringent measures can be put in place to reduce the level of negligence.
Physician error and cognitive error can be prevented through effective information and decision
support system, collaboration among the staff and provision of protocols. Wound infection is an
example of a preventable AE as it occurs through lack of proper cleaning and monitoring. Other
examples of preventable AEs are diagnostic mishap and therapeutic mishap that might occur due
to lack of information or knowledge.
Some AEs are not preventable. These might have been through lack of knowledge of both the
patient and physician or due to unavoidable circumstances. Examples of this are allergic
reactions to drugs which the patient had not been exposed to previously and marrow depression
as a result of antitumor drugs (Brennan, et al., 1991).
Workbook Activity 3.
Public Inquiries
Read the summary of findings and recommendations from the Bristol and Bundaberg reports
and from one other report from the readings above.
3.1 Use a table format to identify common themes or contributing factors to the adverse events
described in the Bristol, Bundaberg and one other report.
Themes Bristol Bundaberg Liverpool
Leadership Lack of
leadership in
providing
direction
regarding the
paediatric
cardiac
Management
laxity in
assessment
before
employment
Lack of response
after whistle
Lack of proper
procedure for
recruitment
Paraphrase This Document
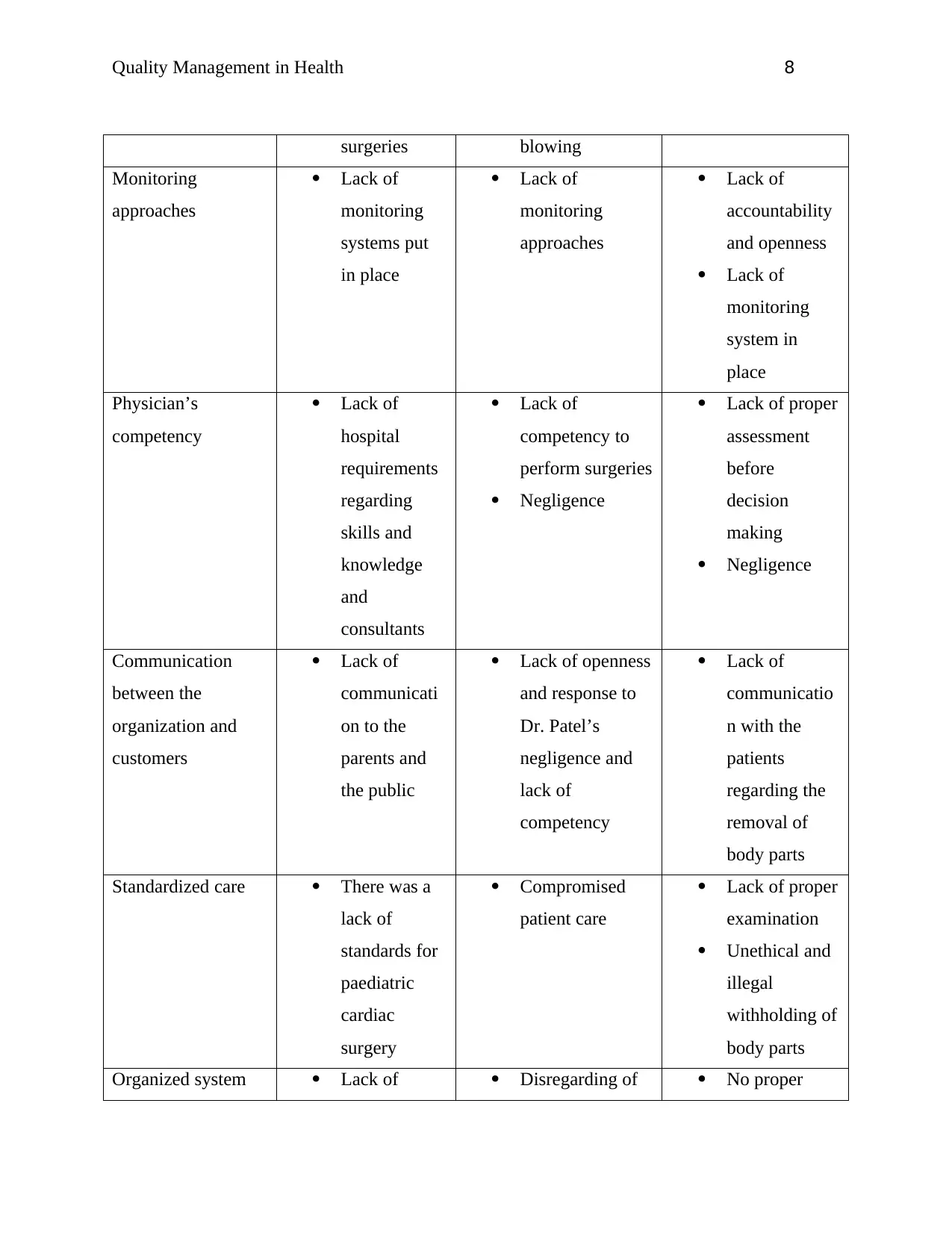
surgeries blowing
Monitoring
approaches
Lack of
monitoring
systems put
in place
Lack of
monitoring
approaches
Lack of
accountability
and openness
Lack of
monitoring
system in
place
Physician’s
competency
Lack of
hospital
requirements
regarding
skills and
knowledge
and
consultants
Lack of
competency to
perform surgeries
Negligence
Lack of proper
assessment
before
decision
making
Negligence
Communication
between the
organization and
customers
Lack of
communicati
on to the
parents and
the public
Lack of openness
and response to
Dr. Patel’s
negligence and
lack of
competency
Lack of
communicatio
n with the
patients
regarding the
removal of
body parts
Standardized care There was a
lack of
standards for
paediatric
cardiac
surgery
Compromised
patient care
Lack of proper
examination
Unethical and
illegal
withholding of
body parts
Organized system Lack of Disregarding of No proper
cooperation
between
health care
professionals
Lack of
facilities to
perform open
heart
surgeries
information by
management
Lack of clinical
governance
practices
system to
regulate the
need of
histological
examination
hence they
were
overlooked
Lack of
premises and
equipment for
Safety Unsafe
practices and
lack of
resources
Unsafe practices
and negligence
Carrying out
of unethical
and illegal
practices
3.2 Why are causal factors associated with adverse events identified as either systems or
individual issues? Why are contributing factors classified as either system or individually based?
Causal and contributing factors are identified as either systems or individual. This helps to
provide a better understanding. System factors are issues associated with the structure and
leadership of the organization. It looks at resources present at the hospital. This helps one to
isolate issues regarding the organization and focus interventions on that. The individual factors
are factors that are attributed to either the physician or the patient. These include behaviours,
personality, skills, knowledge, motivation and cultural competency.
3.3 All of the hospitals that were the subject of inquiries were subject to formal accreditation.
Why were the problems identified during the inquiries not identified through accreditation?
First there was a lack of proper guidelines for assessment and recruitment. For institutions that
had, they were not followed due to a need and a lax by the management. Secondly, there was a
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
lack of monitoring system in place in these institutions. This led to the lack of accountability and
taking responsibility of the health care providers and organization. Lack of openness was another
problem in that issues were not articulated. Communication and collaboration between the health
care professionals and the patients and family members was lacking. This was profound to the
extent of not seeking consent before performing a procedure.
3.4 How effective do you think public inquiries are in achieving long term improvement in the
quality and safety of health services? Provide some reasons for your answer.
Public enquiries are effective in bring about quality improvement. Public inquiries are important
in that they provide an avenue for issues to be discussed. They help create awareness on issues.
They are also important in getting organizations to respond to concerns. Like in the case of
Bundaberg, it helped the assessment and evaluation of the increased number of deaths. Through
public inquiries, causal and contributing factors are identified. This provides a platform to solve
the problems and bring about long term improvement in quality and safety of health services.
Workbook Activity 4
4.1 What is a ‘blame free’ culture?
It is a culture where individual actors are not responsible for the actions believed to deserve
condemnation. It is believed to be the intervention for the uncovering and reduction of errors
(Collins, Block, Arnold, & Christakis, 2009).
4.2 How is a ‘blame free’ culture different from a ‘just culture’? Why is the distinction
important?
A blame free culture is associated with highly hierarchical functional systems which inhibits one
from speaking out against evils or errors as one is afraid of condemnation. This is associated
with an increase in errors (Collins, Block, Arnold, & Christakis, 2009). This is the clear
difference with just culture in that in just culture one is free to speak out against errors so that
they can be managed and provides a platform for learning and improvement. This change is
important as it brings out the clear impact that both cultures have on healthcare.
Paraphrase This Document
4.3 Why does Berwick believe that traditional approaches to quality control and quality
assurance contribute to a ‘blame culture’?
Traditional quality control and quality assurance hold on to inspection as a measure of quality.
This is highly associated with the picking of low quality goods/ services and discarding them
while retaining the good quality ones. This also occurs in service production. Healthcare
providers feel an intense need to prove their competencies. According to Berwick, blaming is
one way of separating oneself from an error or a problem (Berwick, 1989). This contributes to
the blame culture in organizations.
4.4 Why are doctors in particular likely to self blame?
Doctors are guided by the do no harm ethical principle. Aside from this, the medical field has
high standards accorded to it due to its life or death nature. This puts a heavy responsibility on
the doctor. Just as he is responsible for the health of the patient, he/ she is responsible for the
errors that may occur in care provision (Radhakrishna, 2005).
4.5 What quality improvement and quality management activities require an ‘open’ or ‘just’
culture to be effective?
Quality improvement requires a just culture to be effective. This is due to the fact a just culture
promotes openness and communication. This is important in error or problem identification
allowing for the management and control of errors. A just culture also helps in the reduction of
fear from health care providers. Fear is the main cause of the withholding of information by
healthcare providers as they are afraid of condemnation and the consequences that will follow
(Leape L. L., 1994). A just culture also promotes collaboration among healthcare providers as
it allows one to freely share and deliberate upon an issue bringing about effective supportive
clinical decision making.
Workbook Activity 5.
Domains of Quality – Effectiveness and Efficiency
5.1 The use of evidence based health care is often cited as a means of ensuring clinical
effectiveness. (McSherry and Pearce, 2007; Wolff and Taylor, 2009). Using the readings
provided and your own research, provide examples of how evidence based health care practice
(EBP) may improve clinical effectiveness and describe the limitations and criticisms of EBP.
Evidence based health care practice has been defined as’ the conscientious, explicit, and
judicious use of current best evidence in making decisions about the care of individual patients’
(Timmermans & Mauck, 2005). This is the current trend in health care deliver and it has
received a lot of focus internationally. It is the knowledge and skills that health care providers
gain through experience and practice. This is also received through research (Sackett,
Rosenberg, Muir Gray, Haynes, & Richardson, 1996). Evidence based care is known for
its positive outcomes. These include; increased patient safety, improved clinical outcomes,
reduce healthcare costs, and decreased patient outcomes variation (Black, Balneaves,
Garossino, Puyat, & Qian, 2015).
First, evidence based care (EBC) is associated with the availability of factual information. This
information is derived through researches and experience. This helps health care professionals to
assess and understand the community’s needs and tailoring their services to meet these needs
(Moreno-Casbas, 2015). Information on epidemiology of diseases and conditions, their causes
and risk factors is identified and guides the implementation of interventions. This is associated
with the general well being of the community. Organizations like World Health Organization and
CDC rely on evidence based data in the development of health care guidelines.
EBC is associated with the development and increase of the knowledge base and skills of health
care providers (Sackett, Rosenberg, Muir Gray, Haynes, & Richardson, 1996). Data
collected informs them on the effective interventions in the management of various conditions.
This helps tailor trainings, seminars and conferences where evidence based data is presented.
Health care providers are able to find out new changes in the environment and how this
influences one’s health. An example of this is the impact of lifestyle change on the prevalence of
chronic diseases.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Patient satisfaction is an important outcome of evidence based care. This is also brought about by
the implementation of the best proven interventions for the management of various conditions.
The interventions implemented have been standardized and evaluated with objective measures
(Mullen & Streiner, 2004). This leads to better clinical outcomes and less hospital stays.
It does have some limitations. First it disregards the beliefs and values of the patient. It focuses
on the data collected rather than the different needs of the patients. Another limitation is that
there some areas where there is insufficiency of data. This affects the implementation of EBC.
EBC is criticized for its cookbook approach. This means that interventions are based on the data
researched and published rather than on one’s expertise and knowledge (Mullen & Streiner,
2004).
Domains of Quality – Patient Centredness
5.2. There is general agreement about the need to place patients at the centre of their own care,
and at the centre of the health system. At the same time there is also agreement that health care
organisations and health care professionals find this difficult. What are the benefits of and
barriers to patient/person centred care? In your answer include discussion about how a patient’s
cultural background may make a difference to their experience of health care.
Patient centred care has become the new trend in health care where the patient if the main focus
of care. It has been associated mainly with both patient and provider satisfaction as the outcomes
of its implementation. Patient centred care is highly dependent on the establishment of a
therapeutic relationship.
Patient satisfaction is brought about by the inclusion of patient participation and engagement
(Coulter & Cleary, 2001). The patient is involved in every step of patient care, i.e. planning,
decision making and implementation. This inclusiveness makes the patient to feel respected and
dignified. Patient participation has also helped in the fostering of therapeutic relationships
between the patient and the health care provider. It is through this relationship that empathy,
emotional support and respect are expressed. This builds on mutual trust and cooperation.
Patient centred care is also associated with provider satisfaction. This is important as it brings
about motivation and commitment among the health care providers. Patient centered care enables
Paraphrase This Document
the providers to fully understand the needs, values and preferences of the patient. This results to
patient tailored treatment interventions. This is characterized with positive clinical outcomes,
increased quality of life and increases adherence to treatment (Consumers Health Forum of
Australia, 2016).
Better communication and flow of information has been noted (Coulter, 2006). This is
facilitated by the therapeutic relation between the patient and the health care provider. This
enables the patient to better understand the condition, risk factors and interventions for
management. This also ahs a positive outcome of the adherence rate to treatment by patients.
Patient centred care has faced a number of barriers. The first barrier is organizational structures.
A lot of changes have to be mad to both the structure and the working of health care providers.
The other barrier is time constraints whereby health care professionals find it hard for them to
focus solely on one patient. Professional attitude is the other barriers whereby healthcare
professionals find themselves going back to not having interest in the patient’s values and
preferences(Moore, Britten, Lydahl, Naldemirci, Elam, & Wolf, 2016).
Cultural differences affect patient centred care. It affects both the patient and the provider.
Culture affects language, health seeking behaviour, symptom presentation and also adherence to
treatment (Almutairi, 2015). Language differences do affect communication and hinders
effective care provision. Culture affects the health seeking behaviour and adherence to treatment
in that there are cultures that do not believe in seeking professional advice when sick. As a health
care provider, it is paramount to be culturally competent so as to better understand our patients.
Workbook Activity 6.
What is clinical governance? Why do you think clinical governance is context dependent? From
your reading what are some of the barriers to change that organisations will need to address in
order to ensure the effective adoption of clinical governance within the organisation? What do
you think are the challenges for leaders in achieving successful change? (no more than 500
words)
Clinical governance is defined as a systematic and integrated approach that reviews the
responsibility and accountability of clinical activities leading to their quality and safety. This is
responsible for positive clinical outcomes and the overall well being (Braithwaite &
Travaglia, 2008). Clinical governance is comprised of four approaches that help in the
measurement and improvement of quality of health care. The approaches are quality assessment,
quality assurance, clinical audit and quality improvement (Buetow & Roland, 1999).
Clinical governance is context dependent. This is brought about by the different organizational
culture that exits. Each organisation has its own system and its own goals and objectives to
achieve. These two factors determine the running of the organization. The mode of
communication, level or risk taking and innovation, degree of central direction, authority
hierarchies, competitiveness, person orientation and outcome orientation differ from one
organization to another. This makes it difficult for the clinical governance applied in one
organization to be applied in another.
For effective clinical governance, organizations need to implement the following changes. First
there is need for regulations that limit the amount of risk allowed. This puts a limit in the
activities to be done to attain the maximum potential. It allows for the right procedures to be
followed. The second barrier is that there is need to have restrictions on the autonomy of
providers. This allows for all healthcare providers to put aside their own goals for the goals of
the organizations. The other change is to allow for team work rather than working alone. Team
work is important as it provides better communication, better flow of information and an
effective clinical decision support. This also provides an avenue for monitoring and assessment
as the health care providers are able to review each other’s work. There is also a need for system
arbitration for clinical malpractice. We should focus on improving the whole system and not the
individual. When we create an environment that favours growth of the health professionals,
ensure the availability and accessibility of resources and the implementation of both top-down
and bottom- up management approach, we are able to have safer and quality care. Lastly there is
a need for the simplification of the rules and regulation enacted on the health professionals. His
will help to create an environment where they can share and even voice out errors and issues.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
This will provide a platform for leaning and improving (Amalberti, Auroy, Berwick, &
Barach, 2005).
Leaders have a big challenge in achieving successful change. This has been attributed to the time
constraints, a need for training courses on quality improvement and monitoring, change in
hierarchy levels and interprofessional collaboration. This has made it difficult for the whole
system to come to place.
References
Paraphrase This Document
Almutairi, K. M. (2015). Culture and language differences as a barrier to provision of quality
care by the health workforce in Saudi Arabia. Saudi Medical Journl , 425–431.
Amalberti, R., Auroy, Y., Berwick, D., & Barach, P. (2005). Five System Barriers To Achieving
Ultrasafe Health Care. Annals of Internal Medicine , 756 – 764.
Berwick, D. M. (1989). Sounding Board: Continuous Improvement as an Ideal in Health Care.
New England Journal of Medicine , 53-56.
Berwick, D. M. (1993). Sounding Board: Continuous Improvement as an Ideal in Health Care. In
A. F. Al-Assaf, & J. A. Schmerle, The Textbook of Total Quality in Healthcare (pp. 53-
56). Delray Beach: St Lucie Press.
Best, M., & Neuhauser, D. (2005). W Edwards Deming: father of quality management, patient
and composer. Quality and Safety in Health Care , 310-312.
Black, A. T., Balneaves, L. G., Garossino, C., Puyat, J. H., & Qian, H. (2015). Promoting
Evidence-Based Practice Through a Research Training Program for Point-of-Care
Clinicians. Journal of Nursing Administration , 14-20.
Braithwaite, J., & Travaglia, J. F. (2008). An overview of clinical governance policies, practices
and initiatives. Australian Health Review , 10-22.
Brennan, R. A., Leape, L. L., Laird, N. M., Hebert, L., Localio, A. R., Lawthers, A. G., et al.
(1991). Incidence of Adverse Events and Negligence in Hospitalized Patients — Results
of the Harvard Medical Practice Study I. The New England Journal of Medicine , 370-
376.
Brennan, R. A., Leape, L. L., Laird, N. M., Hebert, L., Localio, A. R., Lawthers, A. G., et al.
(1991). The Nature of Adverse Events in Hospitalized Patients — Results of the Harvard
Medical Practice Study II. The New England Journal of Medicice , 377-384.
Buetow, S. A., & Roland, M. (1999). Clinical governance: bridging the gap between managerial
and clinical approaches to quality of care. Quality in Health Care , 184–190184.
Cole, R. E. (2011, May 1). Who Was Really at Fault for the Toyota Recalls? Retrieved April 2,
2018, from The Atlantic: https://www.theatlantic.com/business/archive/2011/05/who-
was-really-at-fault-for-the-toyota-recalls/238076/
Collins, M. E., Block, S. D., Arnold, R. M., & Christakis, N. A. (2009). On the prospects of
blame-free medical culture. Social Science and Medicine , 1287 – 1290.
Consumers Health Forum of Australia. (2016). Patient- Centred Healthcare Homes in Australia:
Towards Successful Implementation July 2016, Roundtable Report. Melbourne:
Consumers Health Forum of Australia.
Coulter, A. (2006). Trends in patients’ experience of the NHS. Oxford: Picker Institute Europe.
Coulter, A., & Cleary, P. D. (2001). Patient’s Experiences With Hospital Care In Five Countries.
Health Affairs , 244 – 252.
de Vries, E. N., Ramrattan, M. A., Smorenburg, S. M., Gouma, D. J., & Boermeester, M. A.
(2008). The incidence and nature of in-hospital adverse events: a systematic review.
Quality & Safety in Health Care , 216–223.
Fritze, C. (2016, January). The Toyota Production System - The Key Elements and the Role of
Kaizen within the System. Retrieved April 2, 2018, from Researchgate:
https://www.researchgate.net/publication/289519018_The_Toyota_Production_System_-
_The_Key_Elements_and_the_Role_of_Kaizen_within_the_System
Hackman, J. R., & Wageman, R. (1995). Total Quality Management: Empirical, Conceptual, and
Practical Issues. Administrative Science Quarterly , 309-342.
Leape, L. L. (1994). Error in Medicine. JAMA , 1851 – 1857.
Leape, L., Berwick, D., Clancy, C., Conway, J., Gluck, P., Guest, J., et al. (2009). Transforming
healthcare: a safety imperative. Quality and Safety in Health Care , 424 – 428.
Luce, J. M., Bindman, A. B., & Lee, P. R. (1994). A Brief History of Health Care Quality
Assessment and Improvement in the United States. Western Journal of Medicine , 263-
268.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Moore, L., Britten, N., Lydahl, D., Naldemirci, O., Elam, M., & Wolf, A. (2016). Barriers and
facilitators to the implementation of person‐centred care in different healthcare contexts.
Scandinavian Journal of Caring Sciences , 662–673.
Moreno-Casbas, T. (2015). Perspectives: Implementation Perspectives: Implementation integrate
evidence-based nursing. What are we doing? Journal of Research in Nursing , 729–733.
Mullen, E. J., & Streiner, D. L. (2004). The Evidence For and Against Evidence-Based Practice.
Brief Treatment and Crisis Intervention , 111-121.
Radhakrishna, S. (2005). Culture of blame in the National Health Service; consequences and
solutions. British Journal of Anaesthesia , 653.
Sackett, D. L., Rosenberg, W. M., Muir Gray, J. A., Haynes, R. B., & Richardson, W. S. (1996).
Evidence based medicine: what it is and what it isn’t. British Medical Journal , 71 – 72.
Timmermans, S., & Mauck, A. (2005). The Promises And Pitfalls Of Evidence-Based
Medicine. Health Affairs , 18-28.
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
© 2024 | Zucol Services PVT LTD | All rights reserved.

