Nursing Care Plan: Complex Patient Case Study, Jessica Fong
VerifiedAdded on 2022/09/02
|11
|2258
|22
Homework Assignment
AI Summary
This assignment presents a comprehensive case study of a 30-year-old patient, Jessica Fong, who sustained multiple injuries in a motor vehicle accident, including a closed head injury, fractured tibia and fibula, and a perforated bowel leading to paralytic ileus and a loop ileostomy. The assignment covers various aspects of nursing care, including NGT insertion, indications for ileostomy and colostomy, management of hypoxemia through oxygen therapy, ECG interpretation, venepuncture techniques, and stoma care. It explores the rationale behind nursing interventions, potential complications, and the importance of patient education and interprofessional collaboration. The document also addresses the assessment of respiratory distress, pain management, and the application of the six rights of medication administration. The case study provides a detailed analysis of nursing interventions, assessment, and care plans related to the complex medical and surgical issues faced by the patient.

Running Head: QUESTION ANSWERS ON COMPLEX PATIENT CASE STUDY
QUESTION ANSWERS ON COMPLEX PATIENT CASE STUDY
Name of the Student:
Name of the University:
Author Note:
QUESTION ANSWERS ON COMPLEX PATIENT CASE STUDY
Name of the Student:
Name of the University:
Author Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1QUESTION ANSWERS ON COMPLEX PATIENT CASE STUDY
1. Explain why a paralytic ileus requires an NGT insertion as part of its management?
Ans. In the cases of bowel obstruction or paralytic ileus, the insertion of Nasogastric tube
(NGT) is done in order to prevent the aspiration of vomit, which is a very common case
scenario in the patients.
2. You have been asked to insert a nasogastric tube (NGT). Is this contraindicated for
this patient? If so, explain the reason?
Ans. As the patient have a traumatic closed head injury, it is risky to try to insert a NGT,
and thus it is contraindicated.
3. Why might a loop ileostomy be performed instead of a regular ileostomy?
Ans. Loop ileostomy is a temporary condition and patient was in need of an ileostomy
since the accident resulted in a perforated bowel in the patient, even though there was not
any other complication in regards to the bowel actions. Thus there was no need of regular
ileostomy.
4. D Select two indications from the list below and provide an appropriate rationale
for the insertion of the NGT in each case.
Stroke,
Fractured Hip,
AMI,
Anorexia,
COPD
Ans.
Stroke: Difficulty in moving food around the mouth and shallowing it is called dysphagia
and this can result in difficulty in eating and drinking, since the food and drink might
1. Explain why a paralytic ileus requires an NGT insertion as part of its management?
Ans. In the cases of bowel obstruction or paralytic ileus, the insertion of Nasogastric tube
(NGT) is done in order to prevent the aspiration of vomit, which is a very common case
scenario in the patients.
2. You have been asked to insert a nasogastric tube (NGT). Is this contraindicated for
this patient? If so, explain the reason?
Ans. As the patient have a traumatic closed head injury, it is risky to try to insert a NGT,
and thus it is contraindicated.
3. Why might a loop ileostomy be performed instead of a regular ileostomy?
Ans. Loop ileostomy is a temporary condition and patient was in need of an ileostomy
since the accident resulted in a perforated bowel in the patient, even though there was not
any other complication in regards to the bowel actions. Thus there was no need of regular
ileostomy.
4. D Select two indications from the list below and provide an appropriate rationale
for the insertion of the NGT in each case.
Stroke,
Fractured Hip,
AMI,
Anorexia,
COPD
Ans.
Stroke: Difficulty in moving food around the mouth and shallowing it is called dysphagia
and this can result in difficulty in eating and drinking, since the food and drink might
2QUESTION ANSWERS ON COMPLEX PATIENT CASE STUDY
reach the lungs while going down the wrong way. Dysphagia can be resulting from
stroke.
Anorexia: When the treatment of anorexia nervosa involves NG tube feeding, it has many
beneficial conditions. During the initiation of the treatment, this method is used
additionally with the oral feeding as it facilitates the weight gain to provide some medical
stability and to improve the cognitive skills of a patient for the promotion of readiness
and the engagement in treatment which leads to the psychological recovery.
5. The Doctor has decided to go ahead with the NGT insertion. Whilst you are
inserting the NGT, Jessica shows signs of respiratory distress. What could be the
cause of this?
Ans. Aspiration might be resulting from the incorrect placement of the NGT due to
intubation down the trachea or leading to respiratory tree. If the accidental placement of
the NGT involves bronchopulmonary system intubation, it may result into hemothorax,
pneumothorax or death.
6. What would be your priority nursing action/s when Jessica shows signs of
respiratory distress during the NGT insertion?
Ans. While observing for the respiratory distress, a checking should be done considering
the possibility of the tube being curled up at the back of the mouth of the patient, since
the tube is supposed to be advancing into the respiratory tree.
In conditions like that the tube must be withdrawn at once and the patient must be
comforted and reassured. Keeping some intervals in time another attempt of reinsertion
must be made. In case of failure, the complications and the reasons must be documented
and the situation must be consulted with MO
reach the lungs while going down the wrong way. Dysphagia can be resulting from
stroke.
Anorexia: When the treatment of anorexia nervosa involves NG tube feeding, it has many
beneficial conditions. During the initiation of the treatment, this method is used
additionally with the oral feeding as it facilitates the weight gain to provide some medical
stability and to improve the cognitive skills of a patient for the promotion of readiness
and the engagement in treatment which leads to the psychological recovery.
5. The Doctor has decided to go ahead with the NGT insertion. Whilst you are
inserting the NGT, Jessica shows signs of respiratory distress. What could be the
cause of this?
Ans. Aspiration might be resulting from the incorrect placement of the NGT due to
intubation down the trachea or leading to respiratory tree. If the accidental placement of
the NGT involves bronchopulmonary system intubation, it may result into hemothorax,
pneumothorax or death.
6. What would be your priority nursing action/s when Jessica shows signs of
respiratory distress during the NGT insertion?
Ans. While observing for the respiratory distress, a checking should be done considering
the possibility of the tube being curled up at the back of the mouth of the patient, since
the tube is supposed to be advancing into the respiratory tree.
In conditions like that the tube must be withdrawn at once and the patient must be
comforted and reassured. Keeping some intervals in time another attempt of reinsertion
must be made. In case of failure, the complications and the reasons must be documented
and the situation must be consulted with MO
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3QUESTION ANSWERS ON COMPLEX PATIENT CASE STUDY
7. Several days later, after bowel sounds are present, the doctor asks for the NGT to be
removed. Outline three (3) prioritized steps to ensure the safe removal of the NGT?
Ans. The first step involves verifying the order for removing the NGT from the medical
team assigned for the care of the patient. The second step involves washing hands prior to
the preparation of the equipment required, as advised by the local infection control
policy. The third step is to remove the Naso-Fix dressing or the adhesive strips. The
instruction to the patient should involve to take a deep breath and hold the breath, so the
glottis can be closed off and the risk of aspiration during the tube removal in minimised.
The tube must be taken out without ceasing movement.
8. Jessica has gone into urinary retention, possibly due to bladder irritation from the
surgery. The doctor has ordered an IDC to be inserted to drain the urine. Identify
three (3) other indications (reasons) for insertion of an IDC?
Ans.
a. To provide assistance with the incontinence resulting from the neurological
disorders.
b. To start the instillation of fluids or in order to administer antibiotic into the
bladder.
c. To provide temporary relief from the bladder outlet obstruction.
9. You have just finished inserting Jessica’s IDC and have taped the catheter securely
to the leg for comfort and safety.
Identify three (3) other specific nursing interventions that are relevant to the care of
Jessica’s IDC. Give a rationale for each nursing care action?
Ans.
7. Several days later, after bowel sounds are present, the doctor asks for the NGT to be
removed. Outline three (3) prioritized steps to ensure the safe removal of the NGT?
Ans. The first step involves verifying the order for removing the NGT from the medical
team assigned for the care of the patient. The second step involves washing hands prior to
the preparation of the equipment required, as advised by the local infection control
policy. The third step is to remove the Naso-Fix dressing or the adhesive strips. The
instruction to the patient should involve to take a deep breath and hold the breath, so the
glottis can be closed off and the risk of aspiration during the tube removal in minimised.
The tube must be taken out without ceasing movement.
8. Jessica has gone into urinary retention, possibly due to bladder irritation from the
surgery. The doctor has ordered an IDC to be inserted to drain the urine. Identify
three (3) other indications (reasons) for insertion of an IDC?
Ans.
a. To provide assistance with the incontinence resulting from the neurological
disorders.
b. To start the instillation of fluids or in order to administer antibiotic into the
bladder.
c. To provide temporary relief from the bladder outlet obstruction.
9. You have just finished inserting Jessica’s IDC and have taped the catheter securely
to the leg for comfort and safety.
Identify three (3) other specific nursing interventions that are relevant to the care of
Jessica’s IDC. Give a rationale for each nursing care action?
Ans.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4QUESTION ANSWERS ON COMPLEX PATIENT CASE STUDY
Intervention: The infection control practices should be taken into consideration when
changing the urinary drainage bags as per the need and also moisture the skin where the
tubes are in proximity with the skin.
Rationale: In minimising the risk of infection, maintaining the proper hand hygiene along
with the skin that is in contact with the tubes and the aseptic techniques can be used.
Intervention: A urine analysis must be performed if required.
Rationale: The reason behind this analysis is to check for various foreign substances and
infections.
Intervention: A fluid balance chart must be prepared documenting the measurement of
the intake and output of the fluid, odour, appearance and the colour of the urine.
Rationale: The reason behind this intervention is to monitor the possibility of renal
failure.
10. Jessica’s SpO2 drops to 87% on room air (RA). The doctor has prescribed 6L/min
of oxygen therapy. What device would you use to deliver this oxygen?
Ans. By using Hudson mask, which is a simple face mask.
11. List three (3) signs and symptoms of hypoxaemia?
Ans.
1. Shortness of breath or dyspnoea with the usage of accessory muscles while breathing.
2. Development of confusion and cyanosis.
3. Diaphoresis to a degree that is quite unusual.
12. Given that oxygen is considered as a medication, what are the 6 rights of
oxygenation you would check before applying oxygen for Jessica?
Ans.
Intervention: The infection control practices should be taken into consideration when
changing the urinary drainage bags as per the need and also moisture the skin where the
tubes are in proximity with the skin.
Rationale: In minimising the risk of infection, maintaining the proper hand hygiene along
with the skin that is in contact with the tubes and the aseptic techniques can be used.
Intervention: A urine analysis must be performed if required.
Rationale: The reason behind this analysis is to check for various foreign substances and
infections.
Intervention: A fluid balance chart must be prepared documenting the measurement of
the intake and output of the fluid, odour, appearance and the colour of the urine.
Rationale: The reason behind this intervention is to monitor the possibility of renal
failure.
10. Jessica’s SpO2 drops to 87% on room air (RA). The doctor has prescribed 6L/min
of oxygen therapy. What device would you use to deliver this oxygen?
Ans. By using Hudson mask, which is a simple face mask.
11. List three (3) signs and symptoms of hypoxaemia?
Ans.
1. Shortness of breath or dyspnoea with the usage of accessory muscles while breathing.
2. Development of confusion and cyanosis.
3. Diaphoresis to a degree that is quite unusual.
12. Given that oxygen is considered as a medication, what are the 6 rights of
oxygenation you would check before applying oxygen for Jessica?
Ans.
5QUESTION ANSWERS ON COMPLEX PATIENT CASE STUDY
1. Correct patient
2. Correct reason or time
3. Correct documentation
4. Correct dose
5. Correct device or route of delivery
6. Correct medicine
13. You have applied the oxygen therapy. Provide three (3) nursing interventions you
may initiate at this time to promote oxygenation for Jessica?
Ans.
1. The patient should be positioned correctly to open airways possibly by positioning
them into a sit up position.
2. The patient should be enquired if experiencing pain and also a respiratory assessment
and monitoring the heart rate should be done possibly by auscultation.
3. The communication with the patient should be done while maintaining calm.
14. It is decided to continue oxygen therapy for Jessica. What are 2 (two) further
nursing interventions you would initiate for long term oxygen therapy?
Ans.
1. It should be ensured that the patient understands the oxygen therapy and encouraged
to receive the therapy both at home or the hospital.
2. Keeping in mind about the Infection control. The examples include hand hygiene.
15. Jessica has a new loop ileostomy due to bowel trauma from her accident. List three
(3) other indications for the formation of a colostomy or ileostomy?
Ans.
1. Correct patient
2. Correct reason or time
3. Correct documentation
4. Correct dose
5. Correct device or route of delivery
6. Correct medicine
13. You have applied the oxygen therapy. Provide three (3) nursing interventions you
may initiate at this time to promote oxygenation for Jessica?
Ans.
1. The patient should be positioned correctly to open airways possibly by positioning
them into a sit up position.
2. The patient should be enquired if experiencing pain and also a respiratory assessment
and monitoring the heart rate should be done possibly by auscultation.
3. The communication with the patient should be done while maintaining calm.
14. It is decided to continue oxygen therapy for Jessica. What are 2 (two) further
nursing interventions you would initiate for long term oxygen therapy?
Ans.
1. It should be ensured that the patient understands the oxygen therapy and encouraged
to receive the therapy both at home or the hospital.
2. Keeping in mind about the Infection control. The examples include hand hygiene.
15. Jessica has a new loop ileostomy due to bowel trauma from her accident. List three
(3) other indications for the formation of a colostomy or ileostomy?
Ans.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6QUESTION ANSWERS ON COMPLEX PATIENT CASE STUDY
1. Anal incontinence
2. Colorectal cancer
3. Crohn’s disease
16. What is the purpose of an ileostomy and explain why a stoma is needed?
Ans. To bypass the large intestine a stoma is created by a surgical procedure in which a
part of small intestine is attached with the wall of the abdomen.
Ileostomy helps in bypassing the digestive waste from the body.
When there is a damage, inflammation in the colon due to a few complications, the
ileostomy is required. The example of those complications include Bowel carcinoma,
Crohn’s disease, Ulcerative colitis.
17. Identify two (2) nursing, Allied Health, or other, professionals that Jessica could be
referred to regarding her current medical situation and describe how they could
help?
Ans.
1. Physiotherapist: This medical professional can assess the improvement of the muscle
strength in the patient, the correctness of the posture. They may also advise a few
exercises that may help in improving the strength of the limbs.
2. Stomal Nurse: This nursing professional can help in both monitoring and assessing
the stromal situation along with the risk of complications.
18. You are starting an afternoon shift and are allocated to care for Jessica. Describe
briefly any assessments you would make regarding these below?
Ans.
1. Anal incontinence
2. Colorectal cancer
3. Crohn’s disease
16. What is the purpose of an ileostomy and explain why a stoma is needed?
Ans. To bypass the large intestine a stoma is created by a surgical procedure in which a
part of small intestine is attached with the wall of the abdomen.
Ileostomy helps in bypassing the digestive waste from the body.
When there is a damage, inflammation in the colon due to a few complications, the
ileostomy is required. The example of those complications include Bowel carcinoma,
Crohn’s disease, Ulcerative colitis.
17. Identify two (2) nursing, Allied Health, or other, professionals that Jessica could be
referred to regarding her current medical situation and describe how they could
help?
Ans.
1. Physiotherapist: This medical professional can assess the improvement of the muscle
strength in the patient, the correctness of the posture. They may also advise a few
exercises that may help in improving the strength of the limbs.
2. Stomal Nurse: This nursing professional can help in both monitoring and assessing
the stromal situation along with the risk of complications.
18. You are starting an afternoon shift and are allocated to care for Jessica. Describe
briefly any assessments you would make regarding these below?
Ans.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7QUESTION ANSWERS ON COMPLEX PATIENT CASE STUDY
Peri-Stomal skin: To protect the skin from maceration, the protective cream or powder
must be applied.
Stoma: The stoma should be checked for swelling, warm temperature and pink
coloration.
Stoma appliance/ bag: The fittings of stoma to the ostomy baseplate should be done
carefully so it fits properly, while taking care of the diameter of the baseplate.
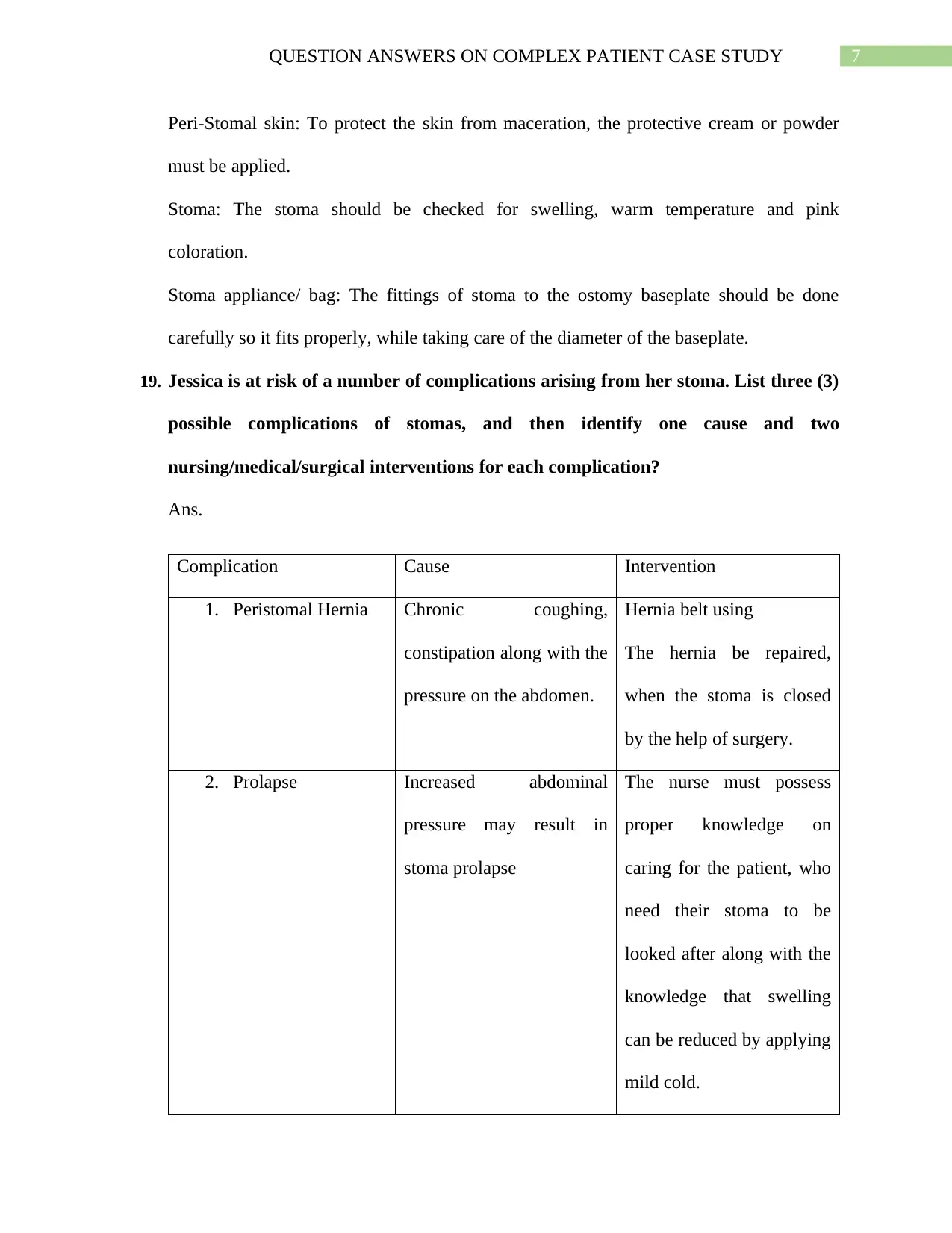
19. Jessica is at risk of a number of complications arising from her stoma. List three (3)
possible complications of stomas, and then identify one cause and two
nursing/medical/surgical interventions for each complication?
Ans.
Complication Cause Intervention
1. Peristomal Hernia Chronic coughing,
constipation along with the
pressure on the abdomen.
Hernia belt using
The hernia be repaired,
when the stoma is closed
by the help of surgery.
2. Prolapse Increased abdominal
pressure may result in
stoma prolapse
The nurse must possess
proper knowledge on
caring for the patient, who
need their stoma to be
looked after along with the
knowledge that swelling
can be reduced by applying
mild cold.
Peri-Stomal skin: To protect the skin from maceration, the protective cream or powder
must be applied.
Stoma: The stoma should be checked for swelling, warm temperature and pink
coloration.
Stoma appliance/ bag: The fittings of stoma to the ostomy baseplate should be done
carefully so it fits properly, while taking care of the diameter of the baseplate.
19. Jessica is at risk of a number of complications arising from her stoma. List three (3)
possible complications of stomas, and then identify one cause and two
nursing/medical/surgical interventions for each complication?
Ans.
Complication Cause Intervention
1. Peristomal Hernia Chronic coughing,
constipation along with the
pressure on the abdomen.
Hernia belt using
The hernia be repaired,
when the stoma is closed
by the help of surgery.
2. Prolapse Increased abdominal
pressure may result in
stoma prolapse
The nurse must possess
proper knowledge on
caring for the patient, who
need their stoma to be
looked after along with the
knowledge that swelling
can be reduced by applying
mild cold.
8QUESTION ANSWERS ON COMPLEX PATIENT CASE STUDY
If the prolapse is too large
to handle conservatively,
surgery should be
suggested.
3. Stenosis Inappropriate sized
opening in skin results in
the stenosis.
The patient should be
provided with a diet that is
low-residue, encouraged to
intake more fluid and the
knowledge on how to use
the stool softeners and
laxatives correctly.
Surgery should be
suggested if the stenosis is
too severe.
20. Jessica states she is experiencing some chest pain. What would be the first
assessment you would make for this patient and why?
Ans. PQRST pain assessment should be made, since the pain can be pointing to a
potentially life-risking and much more. The example include acute myocardial infarction.
21. You decide to perform an ECG on Jessica. How would you explain the procedure to
Jessica? Use terms easily understood by Jessica and include any instructions you
would give her?
Ans. ECG or EKG is an electrocardiogram that is used to measure the electrical activity
of the patient’s heart.
If the prolapse is too large
to handle conservatively,
surgery should be
suggested.
3. Stenosis Inappropriate sized
opening in skin results in
the stenosis.
The patient should be
provided with a diet that is
low-residue, encouraged to
intake more fluid and the
knowledge on how to use
the stool softeners and
laxatives correctly.
Surgery should be
suggested if the stenosis is
too severe.
20. Jessica states she is experiencing some chest pain. What would be the first
assessment you would make for this patient and why?
Ans. PQRST pain assessment should be made, since the pain can be pointing to a
potentially life-risking and much more. The example include acute myocardial infarction.
21. You decide to perform an ECG on Jessica. How would you explain the procedure to
Jessica? Use terms easily understood by Jessica and include any instructions you
would give her?
Ans. ECG or EKG is an electrocardiogram that is used to measure the electrical activity
of the patient’s heart.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9QUESTION ANSWERS ON COMPLEX PATIENT CASE STUDY
The patient needs to be relaxing, lying down still while performing this test as the
machine records the information on a graph. The patient should be breathing normally
and refrain from talking.
22. List three interventions you may perform to improve the adherence of the electrodes
and reduce the chance of artefact on the ECG reading?
Ans.
1. The patient’s skin should be cleaned, jewellery should be taken off and the proper
electrode placement must be done.
2. The patients should be kept relaxed and lied down along with advising them to
breathe normally as the excessive movements may cause more damage.
3. the unnecessary electrical devices must be switched off in order to reduce electrical
interference.
23. The doctor has requested a blood test to be completed for Jessica, name the two (2)
different venepuncture methods you could to complete this task?
Ans.
1. Syringe and needle
2. Vacutainer equipment
24. What are two (2) contraindications for applying a tourniquet to a limb?
Ans.
1. Hypertension that is extreme and peripheral vascular disease.
2. Open injuries and wounds which require removal of the dead cells.
The patient needs to be relaxing, lying down still while performing this test as the
machine records the information on a graph. The patient should be breathing normally
and refrain from talking.
22. List three interventions you may perform to improve the adherence of the electrodes
and reduce the chance of artefact on the ECG reading?
Ans.
1. The patient’s skin should be cleaned, jewellery should be taken off and the proper
electrode placement must be done.
2. The patients should be kept relaxed and lied down along with advising them to
breathe normally as the excessive movements may cause more damage.
3. the unnecessary electrical devices must be switched off in order to reduce electrical
interference.
23. The doctor has requested a blood test to be completed for Jessica, name the two (2)
different venepuncture methods you could to complete this task?
Ans.
1. Syringe and needle
2. Vacutainer equipment
24. What are two (2) contraindications for applying a tourniquet to a limb?
Ans.
1. Hypertension that is extreme and peripheral vascular disease.
2. Open injuries and wounds which require removal of the dead cells.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10QUESTION ANSWERS ON COMPLEX PATIENT CASE STUDY
References
Emergency Medicine. (2019). Google Books. Retrieved 1 November 2019
Geriatric Trauma and Acute Care Surgery. (2019). Google Books. Retrieved 1 November 2019
Medical Equipment Management. (2019). Google Books. Retrieved 31 October 2019
Nurse, T. (2018). The Role of a Stoma Nurse - Bladder & Bowel Community. Bladder & Bowel
Community. Retrieved 31 October 2019, from
https://www.bladderandbowel.org/bowel/stoma/role-stoma-nurse/
Physical Medicine and Rehabilitation Board Review, Third Edition. (2019). Google Books.
Retrieved 1 November 2019
Understanding Anesthetic Equipment & Procedures: A Practical Approach. (2019). Google
Books. Retrieved 31 October 2019
Winningham's Critical Thinking Cases in Nursing. (2019). Google Books. Retrieved 1
November 2019
References
Emergency Medicine. (2019). Google Books. Retrieved 1 November 2019
Geriatric Trauma and Acute Care Surgery. (2019). Google Books. Retrieved 1 November 2019
Medical Equipment Management. (2019). Google Books. Retrieved 31 October 2019
Nurse, T. (2018). The Role of a Stoma Nurse - Bladder & Bowel Community. Bladder & Bowel
Community. Retrieved 31 October 2019, from
https://www.bladderandbowel.org/bowel/stoma/role-stoma-nurse/
Physical Medicine and Rehabilitation Board Review, Third Edition. (2019). Google Books.
Retrieved 1 November 2019
Understanding Anesthetic Equipment & Procedures: A Practical Approach. (2019). Google
Books. Retrieved 31 October 2019
Winningham's Critical Thinking Cases in Nursing. (2019). Google Books. Retrieved 1
November 2019
1 out of 11
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.